Abstract
Aims:
Chronic pain is increasingly considered to be an international public health issue, yet gender differences in chronic pain in Europe are under-examined. This work aimed to examine gender inequalities in pain across Europe.
Methods:
Data for 27,552 men and women aged 25–74 years in 19 European countries were taken from the social determinants of health module of the European Social Survey (2014). Inequalities in reporting pain were measured by means of adjusted rate differences (ARD) and relative adjusted rate risks (ARR).
Results:
At the pooled pan-European level, a greater proportion of women (62.3%) reported pain than men (55.5%) (ARD 5.5% (95% confidence intervals (CI) 4.1, 6.9), ARR 1.10 (95% CI 1.08, 1.13)). These inequalities were greatest for back/neck pain (ARD 5.8% (95% CI 4.4, 7.1), ARR 1.15 (95% CI 1.12, 1.19)), but were also significant for hand/arm pain (ARD 4.6% (95% CI 3.5, 5.7), ARR 1.24 (95% CI 1.17, 1.30)) and foot/leg pain (ARD 2.6% (95% CI 1.5, 3.8), ARR 1.12 (95% CI 1.07, 1.18)). There was considerable cross-national variation in gender pain inequalities across European countries.
Conclusions:
Significant gender pain inequalities exist across Europe whereby women experience more pain than men. The extent of the gender pain gap varies by country. The gender pain gap is a public health concern and should be considered in future prevention and management strategies.
Keywords: Pain, inequality, socioeconomic factors, gender, Europe
Background
‘Women get sicker, but men die quicker’ is a term used to describe gender inequalities in health, whereby women tend to have a higher life expectancy than men, although they live more of those years with morbidity [1]. In 2017, estimated life expectancies for people living in Europe were 83.5 years for women and 78.3 years for men, representing a gender gap of 5.2 years [2]. This ‘gender paradox’ is something that has been widely researched – with studies showing stark gender inequalities across various health outcomes and disease burden [3,4]. The reasons for this are complex, but it is thought that both sex (biological factors) and gender (social factors) play important, and interacting, roles. For example, increased incidence of osteoporosis in women can be largely explained by reduced levels of oestrogen associated with the menopause, while higher levels of depression amongst women are thought to have a genetic influence, as well as a social one (e.g. insecure life circumstances, feeling as though not in control, domestic and sexual violence) [5]. Social epidemiology has attributed some of women’s morbidity disadvantage – and men’s mortality disadvantage – to the restraints placed on women’s access to social and employment-related privileges and economic resources [6 –8]. There is a lack of research examining gender inequalities in pain at a country level, especially across different European countries.
Chronic pain is something that is receiving increasing international interest from the public health community, not least due to the opioid epidemic. Chronic pain, defined as pain that persists for more than three months, is a global problem, and has significant impact on patients, their families, employers, health services and the wider economy. In the USA, for example, chronic pain is estimated to cost over US$500 billion annually: a cost exceeding the annual costs of heart disease, cancer and diabetes [9]. Similar challenges related to chronic pain have also been reported across Europe, where the most recent estimates suggest that up to 40% of the European population experience chronic back pain [10]. Recent estimates suggest that, in Denmark for example, one million working days are lost each year due to chronic pain [11].
The aetiology of chronic pain is complex and is thought to be influenced by a range of biological, social and behavioural factors. It is this complexity that makes chronic pain challenging to manage effectively, with many treatment strategies often relying on the use of opioid analgesics. At present, however, there are very few studies to support the long-term use of opioid analgesics in chronic pain management; opioids also cause adverse effects, including sleep disturbances, endocrine disorders, reduced immune function and increased pain through opioid-induced hyperalgesia. Indeed, the challenges of prescribing opioid analgesics in chronic pain have been well described by the US ‘opioid epidemic’, which has reported increasing levels of opioid misuse and overdose-related mortalities. The trend of increased prescribing of opioid analgesics in chronic pain management has also been reported across Europe [12,13]. Given this complexity, like other diseases, there is potential for gender differences in chronic pain prevalence, owing to different biological, social and behavioural factors. It is important to acknowledge and understand these potential differences so that appropriate treatment strategies can be developed, especially considering coping strategies and health-seeking behaviours may differ between men and women [14,15].
Given that the majority of the chronic pain epidemiology literature relates to the US situation, it is important for studies to explore chronic pain prevalence – and the associated inequalities – in other countries with different healthcare and welfare systems. An extensive European pain survey was published in 2006 by Breivik and colleagues [16], but the major focus of this work was on overall pain prevalence, rather than examining any gender inequalities in pain and how they might vary in different European countries. We have previously reported pain prevalence across Europe, as well as socioeconomic inequalities in pain [10]; however, this is the first paper to report on gender inequalities in pain across Europe.
Aims
The aim of this study was to provide the first pan-European analysis of the gender inequalities in pain.
Methods
Data
This study was based on cross-sectional data concerning self-reported conditions from the ‘Social Inequalities in Health and their Determinants’ rotating module, which was included in the seventh round of the European Social Survey (ESS), 2014 [17,18]. The ESS is a cross-national survey conducted across Europe biennially that maps and illustrates interactions between institutional changes and social attitudes, beliefs and behaviour patterns. Data was obtained by presenting participants with a card listing several health problems, for example, muscular or joint pain in the back/neck, and were asked the following: ‘Which of the health problems on this card have you had or experienced in the last 12 months?’ Specifically, for the pain variables, survey participants could choose back/neck pain, arm/hand pain or foot/leg pain.
The health module used consisted of 40,185 respondents from 21 countries: Austria, Belgium, Czech Republic, Denmark, Estonia, Finland, France, Germany, Hungary, Ireland, Israel, Lithuania, Netherlands, Norway, Poland, Portugal, Slovenia, Spain, Sweden, Switzerland and the UK. The average response rate for all countries was 51.6%; Lithuania had the highest response rate with 68.9%, whereas Germany had the lowest with 31.4%. Data analysis was restricted to respondents aged 25–74 years to reflect ‘working age’. To ensure that the age exclusions did not impact on overall pain levels in the study population, we did a sensitivity analysis at the pan-European level comparing all ages (15+ years) to respondents aged 25–74 years (Supplemental Table 1).
Data concerning participants that did not have their gender or response to pain questions recorded were omitted from the analysis. Estonian responses were excluded from our analysis, as there was insufficient data relating to pain conditions reported. We also excluded Israel from our analysis, as it is not situated in Europe geographically, in line with previous work of Graham and colleagues [19]. After applying the above restrictions for in-eligible individuals and excluding cases for missing data (n = 383), our dataset included 27,552 participants (Supplemental Table 2).
Variables
Data were analysed for three forms of pain: back/neck pain, arm/hand pain and foot/leg pain. We amalgamated results from these three pain variables and created a dichotomous variable to signify if participants had experienced at least one of the three forms of pain. RStudio (R v.3.5.1) was used to appropriately weight different populations and obtain pain prevalence estimates. Prevalence estimates were calculated for the pooled dataset and across all 19 European countries for which we had data.
Analysis
Inequalities in reporting pain were measured by means of adjusted rate differences (ARDs) and relative adjusted rate risks (ARRs). Age-controlled ARDs and ARRs were calculated from predicted probabilities generated by means of binary logistic regression for pooled European data and country specific analysis. The ARD and ARR both express the relationship between two predicted probabilities based on observations and an estimated model. Stata 15.1 was used to conduct analyses concerning inequalities (obtaining ARD and ARR values); pain gender inequality was defined where both ARD and ARR were significantly different.
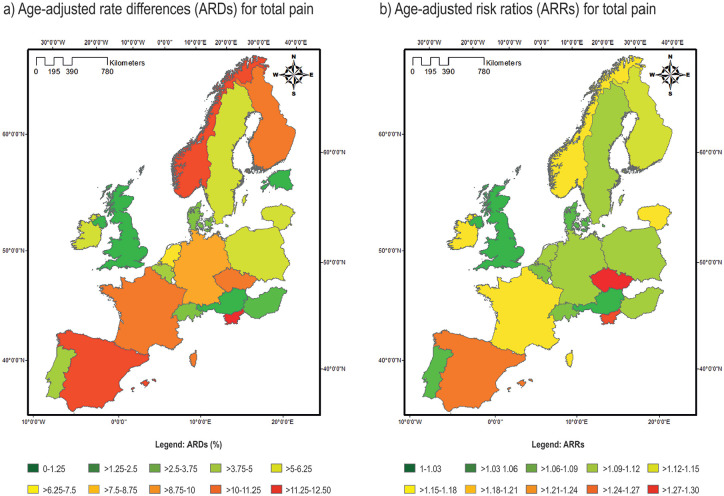
The ARD represents an absolute risk measure (absolute gender pain inequality/gap) and estimated whether the absolute difference is statistically different to zero. ARRs are calculated from predicted probabilities (the ratio of two probabilities); it compares the risk of a variable being present (taking place) when another variable (exposure) is present (relative gender pain inequality/gap). Here, we assessed the risk of pain among women in comparison to the risk of pain among men (reference group). An ARR value of > 1 indicated higher risk among women, whereas < 1 indicated lower risk among women. Data pertaining to ARDs and ARRs were input into Arc Map (v.10.5) in a comma-separated values (CSV) format. Shape files sourced from the Nomenclature of Territorial units for Statistics (NUTS) were attached to attribute data to produce choropleth maps using 10 equal interval categories.
Weights
Age was controlled with reference to 10 age groups that consisted of 5-year intervals. These age intervals were weighted in accordance with the European Standard Population (ESP) [20]. To calculate pooled weights, the population size weight (pweight) which corrects for different population sizes between countries was combined with the post-stratification weight (pspweight) which uses information on age group, gender, education and region to reduce the sampling error and potential non-response bias of the survey. For country-specific estimates, only the pspweight was used.
Results
Pan-European level
Our findings show that a notable percentage of men and women across Europe experience pain. The prevalence of pain varied largely between different countries, as did the degree of gender inequality in pain. Overall, a greater proportion of women (62.3%) reported pain than men (55.5%), which was observed across all three-pain variables: the most common location was back/neck pain, experienced by 47.3% of women and 40.8% men. Then foot/leg pain, experienced by 26.6% of women and 24.3% of men, while 27.4% of women and 22.8% for men experienced hand/arm pain (Table I).
Table I.
Prevalence of pain by gender in 19 European Countries.
| Pain variable | Back/neck (%) | Hand/arm (%) | Foot/leg (%) |
Any pain (% overall) |
||
|---|---|---|---|---|---|---|
| Europe (pooled) | Men | 40.8 | 22.8 | 24.3 | 55.5 | |
| Women | 47.3 | 27.4 | 26.6 | 62.3 | ||
| North | Denmark | Men | 49.5 | 25 | 24.1 | 65.6 |
| Women | 52.1 | 29.9 | 33.3 | 66.4 | ||
| Finland | Men | 48.6 | 24.9 | 30.4 | 66.1 | |
| Women | 58.6 | 25.6 | 32.9 | 75.7 | ||
| Norway | Men | 40.0 | 19.5 | 22.5 | 58.4 | |
| Women | 47.5 | 31.2 | 31.5 | 65.4 | ||
| Sweden | Men | 43.0 | 24.1 | 24.6 | 60.1 | |
| Women | 51.6 | 29.1 | 25.4 | 66.3 | ||
| West | Austria | Men | 32.2 | 14.1 | 17.3 | 44.0 |
| Women | 36.5 | 16.2 | 13.8 | 45.3 | ||
| Belgium | Men | 50.0 | 25.3 | 25.1 | 65.0 | |
| Women | 55.7 | 31.0 | 29.0 | 69.7 | ||
| Switzerland | Men | 37.8 | 17.3 | 24.4 | 54.4 | |
| Women | 43.6 | 20.8 | 20.7 | 58.0 | ||
| Germany | Men | 48.6 | 21.5 | 24.8 | 62.1 | |
| Women | 59.6 | 26.3 | 27.7 | 70.5 | ||
| France | Men | 46.6 | 28.7 | 28.1 | 62.2 | |
| Women | 54.9 | 35.0 | 26.2 | 73.1 | ||
| Ireland | Men | 20.0 | 9.2 | 12.6 | 31.0 | |
| Women | 24.3 | 12.4 | 13.8 | 34.6 | ||
| Netherlands | Men | 37.3 | 20.0 | 20.1 | 53.8 | |
| Women | 44.6 | 21.6 | 22.4 | 61.5 | ||
| UK | Men | 38.8 | 22.7 | 26.9 | 56.4 | |
| Women | 39.1 | 24.0 | 27.5 | 57.9 | ||
| Centre/east | Poland | Men | 30.7 | 23.0 | 22.0 | 47.3 |
| Women | 38.2 | 25.6 | 22.2 | 53.9 | ||
| Slovenia | Men | 38.1 | 22.0 | 17.2 | 49.6 | |
| Women | 46.7 | 21.2 | 22.5 | 49.6 | ||
| Lithuania | Men | 25.9 | 9.9 | 11.9 | 34.0 | |
| Women | 27.4 | 11.2 | 13.9 | 37.6 | ||
| Czech Republic | Men | 21.3 | 9.5 | 10.6 | 31.1 | |
| Women | 29.1 | 14.7 | 16.7 | 40.0 | ||
| Hungary | Men | 16.5 | 11.6 | 14.9 | 25.2 | |
| Women | 17.2 | 14.5 | 17.3 | 28.7 | ||
| South | Portugal | Men | 44.0 | 22.0 | 27.3 | 59.3 |
| Women | 50.7 | 40.2 | 36.6 | 68.4 | ||
| Spain | Men | 33.9 | 20.2 | 21.3 | 50.6 | |
| Women | 48.9 | 33.1 | 30.9 | 64.4 |
Prevalence’s were weighted using European Social Survey post-stratification weights and adjusted to the standard European population in accordance with the European Standard population (ESP) of 2013. Source: European Social Survey, 2014 [18].
At a pan-Europe level, when examining all pain variables, gender pain inequalities were seen in both absolute and relative terms, with women more likely to report pain (ARD 5.5% (95% confidence intervals (CI) 4.1%, 6.9%) and ARR 1.10 (95% CI 1.08, 1.13)) (Table II and visually in Figure 1). These inequalities were greatest for back/neck pain (ARD 5.8% (95% CI 4.4, 7.1) and (ARR 1.15 (95% CI 1.12, 1.19)), but were also significant for hand/arm pain (ARD 4.6% (95% CI 3.5, 5.7) and ARR 1.24 (95% CI 1.17, 1.30)) and foot/leg pain (ARD 2.6% (95% CI 1.5, 3.8) and ARR 1.12 (95% CI 1.07, 1.18)).
Table II.
Age-adjusted rate differences (ARDs) and age-adjusted rate ratios (ARRs) for gender inequalities in back/neck pain, hand/arm pain and foot/leg pain in 19 European Countries. Pain in men was the reference group. ARD estimated whether absolute difference is statistically different to 0, while ARR assessed if the rate ratio is significantly different to 1 (where 1 is equal risk). Gender pain inequality was defined where the ARD and ARR were both statistically significant.
| Pain variables | Back/neck pain | Hand/arm | Foot/leg | Total pain | |||||
|---|---|---|---|---|---|---|---|---|---|
| ARD (% (95% CI)) |
ARR (95% CI) |
ARD (% (95% CI)) |
ARR (95% CI) |
ARD (% (95% CI)) |
ARR (95% CI) |
ARD (% (95% CI)) |
ARR (95% CI) |
||
| Europe | 19 countries | 5.8 (4.4, 7.1) |
1.15 (1.12, 1.19) |
4.6 (3.5, 5.7) |
1.24 (1.17, 1.30) |
2.6 (1.5, 3.8) |
1.12 (1.07, 1.18) |
5.5 (4.1, 6.9) |
1.10 (1.08, 1.13) |
| North | Denmark | 3.4 (–3.2, 10.0) |
1.07 (0.94, 1.22) |
4.6 (–1.3, 10.5) |
1.18 (0.95, 1.47) |
8.6 (2.7, 14.5) |
1.35 (1.10, 1.70) |
3.0 (–3.1, 9.2) |
1.05 (0.95, 1.15) |
| Finland | 11.3 (5.7, 16.9) |
1.23 (1.11, 1.37) |
3.9 (–1.5, 9.2) |
1.16 (0.95, 1.42) |
3.0 (–2.3, 8.4) |
1.10 (0.93, 1.30) |
9.9 (5.0, 14.9) |
1.15 (1.07, 1.23) |
|
| Norway | 11.0 (4.7, 17.2) |
1.28 (1.11, 1.47) |
11.2 (5.3, 17.1) |
1.47 (1.20, 1.79) |
11.3 (5.5, 17.1) |
1.50 (1.22, 1.84) |
10.7 (4.8, 16.7) |
1.18 (1.08, 1.30) |
|
| Sweden | 8.2 (2.4, 14.0) |
1.19 (1.05, 1.34) |
7.5 (2.2, 12.7) |
1.30 (1.08, 1.57) |
3.1 (2.1, 8.2) |
1.12 (0.92, 1.37) |
6.2 (0.8, 11.7) |
1.10 (1.01, 1.20) |
|
| West | Austria | 3.5 (–1.6, 8.5) |
1.11 (0.95, 1.29) |
2.3 (–1.4, 6.1) |
1.17 (0.90, 1.51) |
–1.7 (–5.4, 2.1) |
0.90 (0.70, 1.15) |
0.9 (–4.3, 6.2) |
1.02 (0.90, 1.15) |
| Belgium | 5.7 (–0.1, 11.4) |
1.11 (1.00, 1.24) |
6.1 (0.8, 11.4) |
1.24 (1.03, 1.50) |
4.1 (–1.0, 9.0) |
1.16 (0.96, 1.41) |
5.0 (–0.3, 10.2) |
1.07 (1.00, 1.16) |
|
| Switzerland | 5.9 (0.3, 11.6) |
1.16 (1.01, 1.33) |
3.9 (–0.6, 8.4) |
1.22 (0.97, 1.54) |
–3.9 (–9.7, 1.0) |
0.84 (0.68, 1.04) |
3.7 (–2.0, 9.6) |
1.07 (0.97, 1.18) |
|
| Germany | 9.1 (4.4, 13.7) |
1.17 (1.08, 1.28) |
4.8 (0.6, 8.9) |
1.21 (1.03, 1.44) |
3.2 (–1.0, 7.4) |
1.13 (0.97, 1.32) |
7.6 (3.3, 11.9) |
1.12 (1.05, 1.19) |
|
| France | 7.4 (0.7, 14.0) |
1.2 (1.01, 1.31) |
5.8 (–0.5, 12.1) |
1.20 (0.98,1.46) |
–3.3 (–9.4, 2.8) |
0.89 (0.71, 1.12) |
9.9 (3.8, 16.0) |
1.16 (1.06, 1.27) |
|
| Ireland | 3.5 (–2.2, 9.1) |
1.13 (0.92, 1.38) |
1.8 (–2.1, 5.7) |
1.17 (0.83, 1.65) |
3.0 (–1.0, 7.0) |
1.26 (0.92, 1.72) |
6.1 (0.3, 11.9) |
1.18 (1.00, 1.38) |
|
| Netherlands | 8.3 (2.4, 14.2) |
1.22 (1.06, 1.42) |
1.6 (–3.1, 6.2) |
1.08 (0.85, 1.37) |
0.5 (–4.4, 5.3) |
1.02 (0.81, 1.30) |
6.6 (0.6, 12.6) |
1.12 (1.01, 1.24) |
|
| UK | –0.8 (–6.0, 4.5) |
0.98 (0.86, 1.12) |
–1.1 (–5.5, 3.3) |
0.95 (0.79, 1.15) |
0.0 (–4.7, 4.8) |
1.00 (0.84, 1.19) |
0.2 (–5.1, 5.5) |
1.00 (0.91, 1.10) |
|
| Centre/ east |
Poland | 6.7 (1.2, 12.1) |
1.22 (1.03, 1.43) |
0.6 (–4.1, 5.2) |
1.03 (0.83, 1.27) |
–0.2 (–4.7, 4.2) |
0.99 (0.80, 1.24) |
5.7 (–0.1, 11.5) |
1.12 (1.00, 1.27) |
| Slovenia | 10.9 (3.8, 18.0) |
1.29 (1.09, 1.54) |
1.4 (–4.6, 7.4) |
1.07 (0.81, 1.40) |
4.0 (–1.5, 9.5) |
1.22 (0.93, 1.60) |
12.4 (5.3, 19.4) |
1.25 (1.09, 1.42) |
|
| Lithuania | 3.5 (–2.2, 9.1) |
1.13 (0.92, 1.38) |
1.8 (–2.1, 5.7) |
1.17 (0.83, 1.65) |
3.0 (–1.0, 7.0) |
1.26 (0.92, 1.72) |
6.1 (0.3, 11.9) |
1.18 (1.00, 1.38) |
|
| Czech Republic | 7.4 (2.7, 12.1) |
1.35 (1.11, 1.64) |
5.2 (–1.5, 8.9) |
1.55 (1.13, 2.13) |
5.9 (2.1, 9.6) |
1.58 (1.17, 2.12) |
8.8 (3.7, 13.8) |
1.29 (1.11, 1.49) |
|
| Hungary | 0.5 (–4.2, 5.2) |
1.03 (0.77, 1.39) |
2.5 (–1.8, 6.7) |
1.22 (0.86, 1.71) |
2.0 (–2.7, 6.7) |
1.14 (0.84, 1.55) |
2.5 (–3.0, 7.9) |
1.10 (0.89, 1.34) |
|
| South | Spain | 12.7 (7.4, 18.1) |
1.36 (1.19, 1.55) |
12.5 (7.8, 17.2) |
1.61 (1.34, 1.94) |
8.3 (3.6, 13.0) |
1.38 (1.15, 1.66) |
11.2 (5.8, 16.5) |
1.22 (1.10, 1.34) |
| Portugal | –0.4 (–9.0, 8.3) |
0.99 (0.83, 1.18) |
20.6 (12.9, 28.3) |
1.85 (1.44, 2.38) |
10.5 (2.8, 18.2) |
1.37 (1.08, 1.74) |
4.1 (–4.0, 12.2) |
1.06 (0.94, 1.20) |
|
Figure 1.
A map illustrating (a) age-adjusted rate differences (ARDs) and (b) age-adjusted risk ratios (ARR) in pain between men and women across Europe, with men as the reference category.
Country level
At an individual country level for the pooled pain variables, a gender pain gap was observed in most countries, with nine countries showing significant gender inequalities for total pain (for which we define as a significant difference in ARD and ARR). The gender pain gap was greatest in Slovenia (ARD 12.4% (95% CI 5.3, 19.4) and ARR 1.25 (95% CI 1.09, 1.42)) according to absolute measures. According to relative measures, however, the gender pain was greatest in the Czech Republic (ARD 8.8% (95% CI 3.7, 13.8) and ARR 1.29 (95% CI 1.11, 1.49)). Overall, for the pooled analysis, there were no significant gender pain inequalities in relative or absolute measures reported in Denmark, Austria, Belgium, Switzerland, UK, Poland, Hungary and Portugal.
In terms of inequalities for each pain variable, there were significant gender pain inequalities observed in 11 countries for back/neck pain; Spain had the highest gender pain inequalities in both relative and absolute terms (ARD 12.7% (95% CI 7.4, 18.1)) and ARR 1.36 (95% CI 1.19, 1.55)), followed by Finland in absolute terms (ARD 11.3% (95% CI 5.7, 16.9)) and ARR 1.23 (95% CI 1.11, 1.37)) and the Czech Republic in relative terms (ARD 7.4% (95% 2.7, 12.1) and ARR 1.35 (95% CI 1.11, 1.64)). No significant gender pain inequalities in relative or absolute measures were reported for Denmark, Austria, Belgium, Ireland, UK, Lithuania, Hungary and Portugal.
For hand/arm pain, significant gender pain inequalities were observed in 6 countries, with Portugal showing the highest pain gap in both relative and absolute terms (ARD 20.6% (95% CI 12.9, 28.3) and ARR 1.85 (95% CI 1.44, 2.38)), followed by Spain (ARD 12.5% (95% CI 7.8, 17.2)) and ARR 1.61 (95% CI 1.34, 1.94)). No significant gender pain inequalities in relative or absolute measures were reported for Denmark, Finland, Austria, Switzerland, France, Ireland, Netherlands, UK, Poland, Slovenia, Lithuania and Hungary.
For foot/leg pain, significant gender pain inequalities were observed in 5 countries; Norway had the highest inequalities using absolute measures (ARD 11.3% (95% CI 5.5, 17.1) and ARR 1.50 (95% CI 1.22, 1.84)), while Czech Republic had the highest inequalities using relative measures (ARD 5.9% (95% CI 2.1, 9.6) and ARR 1.58 (95% CI 1.17, 2.12)). No significant pain inequalities in relative or absolute measures were reported for Finland, Austria, Belgium, Switzerland, Germany, France, Ireland, Netherlands, UK, Poland, Slovenia, Lithuania and Hungary.
Discussion
This paper used data from the seventh wave of the ESS from 2014 to establish the extent of gender pain inequality in 19 European countries. We have identified several key findings that may be important for researchers, practitioners and policy makers. Firstly, at the pan-European level, there are significant gender pain inequalities, with women more likely to experience pain than men, across all the three pain variables. Secondly, gender pain inequalities were more common for back/neck pain, with 11 out of 19 European countries showing significant inequalities, compared to hand/arm pain and foot/leg pain where only six and five countries respectively showed significant gender pain inequalities. Thirdly, the magnitude of the gender pain inequalities differed between European countries, with some countries exhibiting no gender pain divides.
Our work adds to the international literature on gender and health that shows women experience more morbidity than men. Research has found that although life expectancy is lower for men, women’s advantage does not translate into healthier years [21]. Women steadily report worse health status than men and suffer from a higher burden of non-fatal and debilitating conditions, such as arthritis, depression, or mobility problems [22]. Our research supports this by demonstrating significant gender inequalities in pain. Further, our work substantially extends the emerging international literature on the epidemiology of pain and inequalities in pain [10,23]. Previous research has similarly found that the prevalence of pain is higher in women; our work shows this is also the case in Europe [24 –26]. Previous work using the ESS has reported on socioeconomic inequalities in pain prevalence across Europe and showed that the inequalities were most pronounced for hand/arm pain and least pronounced for back/neck pain [10]. Research has also found that women have higher rates of severely and moderately limiting pain as well as greater pain intensity [23].
The reasons for these gender inequalities are complex and not completely understood, although there appears to be a biological basis that helps to account for these gender differences: for example, sex hormones, such as oestrogen, can influence pain sensitivity [27]. Similarly, among different animal models, it has been shown that female rodents are more sensitive to chemical, heat and electrical signals than males [28 –30]. Animal models have also shown that females have lower levels of stress-induced analgesia compared to males. Although these biological differences are well characterised, they do not fully explain our findings, given it is likely that pain sensitivity is also mediated by social and economic factors. Indeed, social epidemiological research has found that national and cross-national social policies implemented to support women and to promote gender equality (e.g. increasing gender equality in access to jobs, income, use of time, division of care work and political representation) are associated with improved health outcomes for women or decreased gender health inequalities [31 –33]. This may also be the case for chronic pain, and is something that future research could examine.
Our work also has important public health policy and healthcare practice implications: pain and gender inequalities in pain are not a marginal issue and should be acknowledged in any pain treatment strategies going forward especially as increased pain is associated with higher opioid use [23]. Women are therefore potentially more at risk from the multiple side effects of opioid treatments (which include sleep disturbances, endocrine disorders, reduced immune function and increased pain through opioid-induced hyperalgesia). Whilst little can be done about the biological factors associated with higher pain prevalence (e.g. hormone levels), there is potential to change social circumstances in order to reduce the gender pain gap and to provide additional support/tailor treatments to women. Given the magnitude of the gender pain inequalities was highly variable between European countries, there may be opportunities to reduce these inequalities through health care or other measures. Future work could explore this further.
This study provides a unique insight into gender pain inequalities at a pan-European level using a comparative and robust dataset. However, our work should be considered in view of several limitations, as described below. For a detailed discussion regarding the strengths and limitations of the ESS data, see the work by Eikemo and colleagues [17]. Regarding our choice of model, we acknowledge that the use of logistic regression models has limitations for comparing outcome across groups due to the unobserved differences between groups. We intended to examine the inequality in pain prevalence between male and females, across European countries and Linear Probability model (LPM) are also suitable for this purpose [34]. To ensure our methodology was appropriate, we estimated the coefficients from the LPM across 19 European countries and Europe overall. We then compared these data with findings from binary logistic regression, which showed results of the logistic regression and LPM were in broad agreement (Supplemental Table 3).
A further limitation is that pain measures included in the survey were self-reported; as such, it was the sole responsibility of the participant to correctly identify if they experienced pain in the last 12 months, participant responses were not verified using medical records. Although we do accept that people who experience pain may not necessarily seek medical treatment, meaning that not all types of pain will be able to be verified from medical records. Further, we did not explore the intensity, severity, or type of pain in the survey so we did not consider this in our analysis. It is also possible that people might respond to the questions on pain differently (e.g. people with different cultural backgrounds). Caution is also recommended when translating pain estimates produced by our work into statements concerning the wider population, as our data was obtained using a survey as opposed to examining registry data. Whilst precaution was taken to avoid bias through the use of weightings, the survey selection technique may have resulted in a non-representative sample, as those with severe health conditions may have been unable to partake in the survey. As well as that, the ESS only samples from the non-institutionalised population thus potentially leading to bias, given the institutionalised population are more likely to be affected by poor health. We also note that response rates varied from country to country: while the ESS sets out 70% response rate targets, there were several countries that did not reach this target, although it is worth noting that this is not a direct indicator of a poor-quality dataset. Although the ESS collects data from 19 European countries covering all regions, there were several European countries not covered in the survey. Thus, our findings cannot be generalised to all European countries. Finally, the primary focus of our work aimed to establish if there were gender inequalities in pain prevalence across European countries; we did not seek to explain or account for these inequalities in our analysis. Future work should be more explanatory in nature and seek to examine how different healthcare and welfare systems impact on gender inequalities in pain prevalence.
Conclusions
This study provides the first comprehensive overview of gender pain inequalities across Europe. The most common type of pain experienced by both men and women was back/neck pain. At the pan-European level, significant gender pain inequalities exist whereby women experience more pain than men. While this was found at a pan-European level, the extent of the gender pain inequality varied by country, as different degrees of inequality in pain were reported by different countries. This gender pain divide is a public health concern and it should be considered in any future pain prevention and management strategies going forward.
Supplemental Material
Supplemental material, sj-pdf-1-sjp-10.1177_1403494820987466 for The Gender Pain Gap: gender inequalities in pain across 19 European countries by Kweku Bimpong, Katie Thomson, Courtney L. Mcnamara, Mirza Balaj, Nasima Akhter, Clare Bambra and Adam Todd in Scandinavian Journal of Public Health
Supplemental material, sj-pdf-2-sjp-10.1177_1403494820987466 for The Gender Pain Gap: gender inequalities in pain across 19 European countries by Kweku Bimpong, Katie Thomson, Courtney L. Mcnamara, Mirza Balaj, Nasima Akhter, Clare Bambra and Adam Todd in Scandinavian Journal of Public Health
Supplemental material, sj-pdf-3-sjp-10.1177_1403494820987466 for The Gender Pain Gap: gender inequalities in pain across 19 European countries by Kweku Bimpong, Katie Thomson, Courtney L. Mcnamara, Mirza Balaj, Nasima Akhter, Clare Bambra and Adam Todd in Scandinavian Journal of Public Health
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: CM, MB, CB and AT are members of CHAIN: Centre for Global Health Inequalities Research (funded by the Norwegian Research Council Project Number 288638).
ORCID iDs: Katie Thomson  https://orcid.org/0000-0002-9614-728X
https://orcid.org/0000-0002-9614-728X
Adam Todd  https://orcid.org/0000-0003-1496-9341
https://orcid.org/0000-0003-1496-9341
Supplemental material: Supplemental material for this article is available online.
References
- [1]. Lorber J, Moore LJ. Gender and the Social Construction of Illness. Lanham, MD: Rowman Altamira, 2002 [Google Scholar]
- [2]. Eurostat. Life expectancy at birth in the EU: men vs. women, https://ec.europa.eu/eurostat/web/products-eurostat-news/-/DDN-20190725-1 (2019, accessed 26 April 2020).
- [3]. Waldron I, Johnston S. Why do women live longer than men? J Human Stress 1976; 2(2): 19–30. [DOI] [PubMed] [Google Scholar]
- [4]. Waldron I. Sex differences in illness incidence, prognosis and mortality: issues and evidence. Soc Sci Med 1983; 17: 1107–1123. [DOI] [PubMed] [Google Scholar]
- [5]. Buvinić M, Medici A, Fernández E, et al. Gender Differentials in Health. In: Jamison DT, Breman JG, Measham AR, et al. (eds) Disease Control Priorities in Developing Countries. 2nd ed. Washington, DC: The International Bank for Reconstruction and Development/The World Bank; New York: Oxford University Press, 2006, pp. 195–210. [Google Scholar]
- [6]. Gkiouleka A, Huijts T, Beckfield J, et al. Understanding the micro and macro politics of health: Inequalities, intersectionality and institutions – A research agenda. Soc Sci Med 2018; 200: 92–98. [DOI] [PubMed] [Google Scholar]
- [7]. Palència L, De Moortel D, Artazcoz L, et al. Gender policies and gender inequalities in health in europe: Results of the SOPHIE Project. Int J Heal Serv 2017; 47: 61–82. [DOI] [PubMed] [Google Scholar]
- [8]. Stanistreet D, Bambra C, Scott-Samuel A. Is patriarchy the source of men’s higher mortality? J Epidemiol Community Heal 2005; 59: 873–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain 2012; 13(8): 715–724. [DOI] [PubMed] [Google Scholar]
- [10]. Todd A, McNamara CL, Balaj M, et al. The European epidemic: Pain prevalence and socioeconomic inequalities in pain across 19 European countries. Eur J Pain 2019; 23(8): 1425–1436. [DOI] [PubMed] [Google Scholar]
- [11]. Eriksen J, Sjøgren P, Bruera E, et al. Critical issues on opioids in chronic non-cancer pain: An epidemiological study. Pain 2006; 125: 172–179. [DOI] [PubMed] [Google Scholar]
- [12]. Zin CS1, Chen LC, Knaggs RD. Changes in trends and pattern of strong opioid prescribing in primary care. Eur J Pain 2014; 18(9): 1343–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13]. Kalkman GA, Kramers C, van Dongen RT, et al. Trends in use and misuse of opioids in the Netherlands: a retrospective, multi-source database study. Lancet Public Health 2019; 4(10): e498–e505. [DOI] [PubMed] [Google Scholar]
- [14]. Verbrugge LM. Gender and health: an update on hypotheses and evidence. J Health Soc Behav 1985; 26(3): 156–182. [PubMed] [Google Scholar]
- [15]. Verbrugge LM, Ascione FJ. Exploring the iceberg. Common symptoms and how people care for them. Med Care 1987; 25(6): 539–569. [PubMed] [Google Scholar]
- [16]. Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur J Pain 2006; 10(4): 287–333. [DOI] [PubMed] [Google Scholar]
- [17]. Eikemo TA, Bambra C, Huijts T, et al. The First Pan-European Sociological Health Inequalities Survey of the General Population: The European Social Survey Rotating Module on the Social Determinants of Health. Eur Soc Review 2017; 33(1): 137–153. [Google Scholar]
- [18]. ESS Round 7: European Social Survey Round 7 Data (2014). Data file edition 2.2. NSD – Norwegian Centre for Research Data, Norway – Data Archive and distributor of ESS data for ESS ERIC. DOI: 10.21338/NSD-ESS7-2014. [DOI] [Google Scholar]
- [19]. Graham EA, Thomson KH, Bambra CL. The association between diabetes and depressive symptoms varies by quality of diabetes care across Europe. Eur J Public Health 2018; 28(5): 872–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20]. Pace M, Cayotte E, Agafitei L, et al. Revision of the European Standard Population: Report of Eurostat’s task force. 2013 edition. Luxembourg: Publications Office, 2013. [Google Scholar]
- [21]. Van Oyen H, Nusselder W, Jagger C, et al. Gender differences in healthy life years within the EU: an exploration of the ‘health–survival’ paradox. Int J Public Health 2013; 58: 143–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22]. Boerma T, Hosseinpoor AR, Verdes E, et al. A global assessment of the gender gap in self-reported health with survey data from 59 countries. BMC Public Health 2016; 16: 675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23]. Todd A, Akhter N, Cairns JM, et al. The Pain Divide: A cross-sectional analysis of chronic pain prevalence, pain intensity, and opioid utilisation in England. BMJ Open 2018; 8(7): e023391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24]. Dao TT, LeResche L. Gender differences in pain. J Orofac Pain 2000; 14(3): 169–184. [PubMed] [Google Scholar]
- [25]. Bartley EJ, Fillingim RB. Sex differences in pain: A brief review of clinical and experimental findings. Br J Anaesth 2013; 111(1): 52–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26]. Pieretti S, Di Giannuario A, Di Giovannandrea R, et al. Gender differences in pain and its relief. Ann Ist Super Sanita 2016; 52(2): 184–189. [DOI] [PubMed] [Google Scholar]
- [27]. Vincent K, Tracey I. Hormones and their interaction with the pain experience. Rev Pain 2008; 2(2): 20–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28]. Barrett AC, Smith ES, Picker MJ. Sex-related differences in mechanical nociception and antinociception produced by mu-and kappa-opioid receptor agonists in rats. Eur J Pharmacol 2002; 452: 163–173. [DOI] [PubMed] [Google Scholar]
- [29]. Gaumond I, Arsenault P, Marchand S. The role of sex hormones on formalin-induced nociceptive responses. Brain Res 2002; 958: 139–145. [DOI] [PubMed] [Google Scholar]
- [30]. Aloisi AM, Albonetti ME, Carli G. Sex differences in the behavioural response to persistent pain in rats. Neurosci Lett 1994; 179: 79–82. [DOI] [PubMed] [Google Scholar]
- [31]. Palencia L, Malmusi D, De Moortel D, et al. The influence of gender equality policies on gender inequalities in health in Europe. Soc Sci Med 2014; 117: 25–33. [DOI] [PubMed] [Google Scholar]
- [32]. Beckfield J, Morris KA, Bambra C. How social policy contributes to the distribution of population health: the case of gender health equity. Scand J Public Health 2018; 46: 6–17. [DOI] [PubMed] [Google Scholar]
- [33]. Morris KA, Beckfield J, Bambra C. Who benefits from social investment? The gendered effects of family and employment policies on cardiovascular disease in Europe. J Epidemiol Community Health 2019; 73: 206–213. [DOI] [PubMed] [Google Scholar]
- [34]. Mood C. Logistic regression: Why we cannot do what we think we can do, and what we can do about it. Eur Soc Rev 2010; 26: 67–82. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-sjp-10.1177_1403494820987466 for The Gender Pain Gap: gender inequalities in pain across 19 European countries by Kweku Bimpong, Katie Thomson, Courtney L. Mcnamara, Mirza Balaj, Nasima Akhter, Clare Bambra and Adam Todd in Scandinavian Journal of Public Health
Supplemental material, sj-pdf-2-sjp-10.1177_1403494820987466 for The Gender Pain Gap: gender inequalities in pain across 19 European countries by Kweku Bimpong, Katie Thomson, Courtney L. Mcnamara, Mirza Balaj, Nasima Akhter, Clare Bambra and Adam Todd in Scandinavian Journal of Public Health
Supplemental material, sj-pdf-3-sjp-10.1177_1403494820987466 for The Gender Pain Gap: gender inequalities in pain across 19 European countries by Kweku Bimpong, Katie Thomson, Courtney L. Mcnamara, Mirza Balaj, Nasima Akhter, Clare Bambra and Adam Todd in Scandinavian Journal of Public Health