Abstract
Healthcare systems deal with disease prevention, early detection, diagnosis, investigation, and timely, affordable, and safe treatment. For the delivery of services in the health sector, communication is the key to linking the service provider and the patients. Mobile technology in the recent past has rendered various platforms of communications for the healthcare system. Thus, in health, mobile technology has greatly contributed to time management and cost reduction for healthcare at every level including hospital visits to individual appointments with doctors, hence the convenience. With advancements in mobile technologies and the growing number of mobile users, newer opportunities have opened up for the use of mobiles for patient care. Emerging information and communication technologies with the help of the Internet of Things (IoT) have been instrumental in integrating different domains of the health sector with mobile technology. Thus, the technology may have the potential to become powerful medical tools to support the health sector at all levels of care. In this review, the concept, applications, and advantages of mobile technology for health and the present pandemic have been discussed. It also discusses mobile health technology, as a support system for convenient and safer healthcare for public health, and the opportunities to improve its applications for unseen future health crises.
Keywords: Healthcare, medical tool, mHealth, mobile technology, pandemic, telemedicine
Introduction
“Crisis breeds the strength to cope with it. The Corona crisis of 2020 has highlighted the need to be able to help patients without getting exposed to the infection. We do not know how many such crises, how soon, will be faced in future, but we definitely know how to fight better next time”.
Health care systems work on communication to provide all health-related services in any setting. It is the most essential requirement to establish a link between the health care provider and the patient. In earlier times, physical visits of patients to a hospital or a health care facility were the prime requirement to communicate about the ailments to seek health services.
Once considered a luxury of the rich, mobile phones are now an everyday communication necessity for people across the globe. There are over 7 billion wireless subscribers worldwide, and about 3.9 billion (51.2%) have access to the Internet.[1] It is predicted that the global distribution of smartphone users will be more than 4.78 billion in 2021.[2]
Mobile phones have proved to be a useful tool to provide an instant channel for communication for transmitting demographic, clinical, and investigational and progress data to health care providers and timely, credible advice to health care seekers.[3] The newer technologies have been translated for their applications in healthcare domains and thus have developed a concept of “mobile Health.” The World Health Organization (WHO) has defined mobile Health (mHealth) as “medical and public health practice supported by mobile devices, such as mobile phones, personal digital assistants, wireless devices, and patient monitoring devices”.[4] Although the concept of mHealth has been differently defined, still the definition “the use of mobile computing, medical sensor, and communication technologies for healthcare” gives a clear concept of mHealth.[5]
Hence, mobiles and smartphones can provide excellent support for healthcare; however, their full potential and best use have not been realized yet. To achieve this, a comprehensive list of what healthcare needs from mobiles should be assessed and prepared. Its advantage can be leveraged to express its maximum potential by small modifications in hardware and software but much larger modifications in system ware and person ware especially addressing the present pandemic of COVID-19.
This review highlights the applications of mobile technology for health and emphasizes the safe, effective, and affordable ways to combat this corona pandemic.
Evolution of Mobile Technology in Telemedicine
Telemedicine (TM)
The WHO refers to telemedicine (TM) as “healing from a distance.” TM is an application of telecommunication and information technology that permits health care professionals to evaluate, diagnose, and treat patients sitting at a distance. Experts in the Shandong Province found that the TM platform can play a considerable role in managing patients during pandemic situations. The Shandong Province expert group invited Chinese authorities to use the “Cloud ICU” platform to share their ideas managing critically ill COVID-19 patients to help mitigate the global spread of COVID-19 using telemedicine.[6]
Telemedicine is of three types: interactive telemedicine, asynchronous telemedicine, and telemonitoring.[7] Interactive telemedicine allows patients and physicians to communicate in real-time using phone consultations and video conferences. Lab reports, imaging reports, videos, and other records are shared by health care providers with another specialist by asynchronous telemedicine. Although telemonitoring is a method that allows health care professionals to track a patient’s vital signs and activities from a distance, usually applied for high-risk and elderly patients.
TM benefits equally to patients and healthcare providers. Electronic medical records, artificial intelligence diagnosis, and medical streaming devices are technologies that are integrated with TM and assist providers to monitor patients in real-time and adjust treatment plans accordingly. Also, they are benefited from increased revenue in limited staff and office space. Senior citizens and patients in remote areas can access it from home and those with contagious diseases can minimize exposure. Substance abuse disorders are also treated using various TM strategies. This way the cost per patient is cheaper and offers cost-saving across the board.[8]
Conditions that need in-person examination such as skin diseases, and eye infections, can be replaced by photo-based consultation shared with the doctor to give and seek opinion on diagnosis, or lab tests via apps followed by treatment. Also, the doctor can develop e-prescriptions, which saves time and improve communication. The doctor can understand patients’ past medical records easily and can prescribe and renew the prescription from their comfort zone and also, these e-prescriptions cannot be tampered with by anyone. These e-prescriptions can be linked to Electronic health record(EHR), which enables one to log the information and get a complete picture of treatment given to the patient throughout. This model of healthcare through TM can be instrumental in pandemic situations, which demand social distancing.
Applications of mobile technology for health
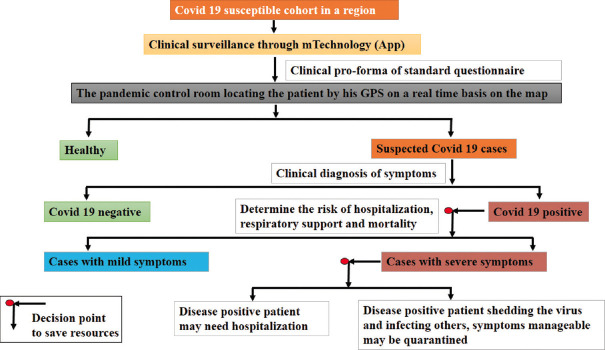
Mobile phones have the potential to become a powerful medical tool to support healthcare at all levels [Figure 1]. Some examples of their usage are as follow:
Figure 1.
Mobile Technology applications for Healthcare systems and patients. Platforms for different domains of health
Estimating calories and exercise to monitor pulse rate or electrocardiogram
Communicating with doctors in an emergency
Reporting disasters with an automated transmission of exact location and time
Using artificial intelligence to help the diagnosis
Detecting adverse drug reactions or pointing out drug interactions
Follow-ups and monitoring a patient’s progress
Sharing results post-discharge to provide credible real-time data with the identity hidden or with patients’ consent for research to guide practice or policy in healthcare.
In developed nations, healthcare providers can electronically send information for prescribed medicines for a patient directly to the pharmacy or medical store, which can be picked up by the patient. This application of mHealth still needs to be implemented in developing nations.[9] Its use in healthcare is still in the early stage.[10] Also, the United States had made more than 50% of its hospitals integrated with mobile-optimized patient portals in 2015.[11]
Mobile technology has saved time by appropriate use of the technology such as by generating a unique identification number that collects data from all points the patient ever visits. i.e., from the outpatient department to the operation theater, emergency, in-patient department, imaging, pathology, microbiology, and post-hospital follow-up at home.[12,13] One can get better access to the latest drug details for faster decision-making. They automate a lot of paperwork that frees up a physician’s or a clinician’s time. With identity hidden or with the patient’s consent, it can also be used for medical research and analysis to provide guidelines in practice or healthcare policy. This may even strengthen evidence-based medicine, which serves as a great support to clinicians.
Distant communication is a need during the pandemic to safeguard healthcare providers and the use of mobiles ensures distancing.
APPS, a new way to healthcare
Mobile devices have set foot in clinical practice partly and maximally due to the availability of medical software applications or apps. These are software programs developed to run on mobiles and computers to fulfill the assigned tasks. Mobile technology, through healthcare apps [Table 1] has benefited healthcare professionals (HCPs), as a point of care tool, with excellent clinical decision making for better patient care.[14]
Table 1.
List of healthcare applications or apps
| Name | Applications |
|---|---|
| Professional healthcare app | For patient’s details such as name, date of birth, address, and insurance number |
| Clinical communication app | Helps to enhance decision-making and communication among specialists in a hospital. |
| Patient communication app | Recruits relatives to the network within the app and sends preformed bulk messages for updates regarding patient care. |
| Medical record app | Updates patient’s data of blood pressure, prescription, medical visits, and examination details to monitor patient’s wellness throughout the treatment. |
| Risk assessment apps | Monitor patient’s condition in real-time, track heart rate, and identify patients at risk. |
| Medication dosage apps | Used by doctors to calculate the individualized dose of medicine based on patient’s age, body weight, and risk factors associated with the patients. |
| Fitness apps | Help the users with their daily activity, the number of calories burnt, diet monitoring with recommendations on calorie consumption based on users age, weight, and sex. |
| Diet and nutrition app | Helps to monitor weight, with a comprehensive library of food and its nutrients, calorie counter diary with meals, and a progress chart. |
| Meditation mobile app | Helps the users to reduce stress and improve sleep patterns through guided meditation. |
| Epilepsy app | Helps the epileptic patients to identify potential triggers for seizures with the symptoms, and duration with severity. |
mHealth Technology in Disease Prevention
To prevent and control any disease, there is always a need for coordinated communication to fight the disease best. There is a great contribution of mobile technology in disease-prevention programs, immunization programs, data collection, and motivating people for treatment adherence.[15]
A smartphone can comprehensively and correctly extract information from the patient on predesigned templates, and can easily use artificial intelligence to advise the standardized optimal “to-do list” and enhance the continuity of care through better maintenance of patient medical records, thus helping in disease prevention.[16]
Communicable diseases/infectious diseases
Mobile technology can be a boon in the prevention of communicable diseases such as COVID-19. The steps as suggested in pandemic situations such as social distancing, contact tracing, segregation, lockdown, and quarantine are some examples of preventive control measures and relevant to communicable diseases, that hit at transmission. Global positioning system (GPS) application of mobile technology can add the latitude–longitude information to the individual event-related data giving the crucial time, place, and person distribution of the event of interest (EoI). One example of the successful use of mHealth data in the development of disease prevention plans is the clean water campaign in Bihar, India (LINK). The use of mHealth data helped to conclude the water-borne transmission of acute encephalitis through a river that limited the epidemic in Bihar and thus helped reduce the number of cases from 1,347 in 2014 to 64 cases in 2015.[17]
Therefore, in 2020, there has been a growing use of mHealth in pandemic situations of COVID-19. Recently, a study has briefly reviewed the uses of mHealth in the recent epidemic/pandemic outbreaks worldwide to learn some lessons on how to deal with COVID-19.[18]
Non-communicable diseases
Multiple uses of mobile technology in the prevention and management of non-communicable diseases (NCD) has been in practice.[19] One important intervention is a short message, which helps in the self-management of chronic illness and follow-ups that are required.[20] The advantage of sending health-related messages in the community to communicate healthy practices has shown great outcomes.[19] A large number of populations is being benefitted from such technology in no time. Among most common NCDs, the usefulness of mHealth has shown great success in the management of diabetes, hypertension, and heart disease.[21,22] Short message service (SMS) for patients with diabetes has shown promising outcomes in disease management by compliance with medication regime.[21,23] Besides this, cancer patients are also greatly benefitted by mHealth-based applications by getting all possible information regarding their disease, even being distantly located.[24,25]
Mobile Technology for Community Health Programs
Mobile technology has greatly contributed to various community health programs, such as in part in declining the maternal and child morbidity and mortality rates and decreasing the burden of communicable and non-communicable diseases.[26] This has been achieved by educating the community health workers (CHWs) about the use of mobile technology for their services. Their involvement in various activities conducted by the public health department and non-governmental organizations (NGOs) are maternal, newborn and child health programs (MNCH), nutrition programs, vaccination programs, communicable disease control programs, and disease surveillance.[6] The appropriate use of mobile technology can improve the productivity of CHWs and reduce their workload.
Application of Mobile Technology in a Pandemic
Pandemic is considered an epidemic that has flared worldwide and has affected a large number of people.[27] COVID-19 is an infectious disease caused by a virus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). First identified in Wuhan, China, in December 2019, it has spread worldwide leading to an ongoing pandemic.[28,29] It has remarkably shaken the global economy too.[30]
The recommended preventive measures for COVID19 include social distancing, wearing face masks in public, ventilation and air-filtering, hand washing, covering one’s mouth when sneezing or coughing, disinfecting surfaces, and monitoring and self-isolation for people exposed or symptomatic. Several vaccines are being developed and distributed. In the recent past, the mHealth platform has been a respite to deal with epidemics, with some proposed solutions.[31]
Mobile technology, a boon in pandemic
In view of the current COVID19 pandemic, which emphasizes social distancing, the benefits of mHealth need to be reinforced to encourage its use. A very good example of such application was used by the Government of India in form of the Arogya-Setu App, which spots at-risk people being positive with SARC-CoV-2 virus. This app was created after observing the pattern and understanding the pandemic. If our healthcare system would have been prepared with such applications of mobile technology from the very beginning, the number of people sacrificed in this pandemic would have been definitely less.
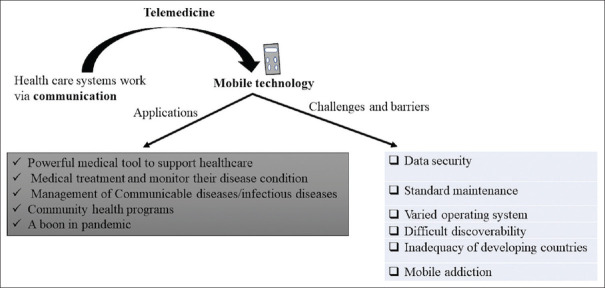
Figure 2 shows the strategy to be adopted by the use of mobile technology in the pandemic situation to save the lives of patients and healthcare resources.
Figure 2.
Strategies and algorithm of mobile use in COVID-19 pandemic. The appropriate use of mobile technology will be instrumental in ensuring distancing, saving on resources of the healthcare system, time, and human lives. Appropriate clinical advice to the stable patients at home and identifying critically ill patients for hospitalization
The appropriate use of mobile technology has proved to be instrumental in ensuring distancing, saving on resources of the healthcare system, time, and human lives. Appropriate clinical advice to the stable patients at home and identifying critically ill patients for hospitalization.
Other benefits of mHealth in Corona pandemic
Early correct credible advice at low cost would have been a boon for the patients and a very strong weapon against the virus.
The data collected could be used with identity hidden for analysis in research and the feedback used to manage the pandemic in an evidence-based manner both for policy setting, making guidelines, and real-time management of patients.
Mobile could be used as a comprehensive follow-up tool by sending and receiving information as many times as necessary at a click of a button using a standard pilot-tested questionnaire.
The video of pandemic/epidemic density and how it is changing would have helped to decide containment measures and coordinate the system of fight back.
Using susceptible, infected, and immune models to estimate the time when the pandemic/epidemic would end would be instantaneously available.
Surveillance is very critical in COVID-19 due to its high prevalence, and mHealth can play a pivotal role to address the same. Improper contact tracing mechanisms of COVID-19 are the major hindrances in preventing its spread[32] and researches show that contact tracing and monitoring by mHealth are an appropriate way to reduce the spread.[33,34] Also, mHealth can be used for tracking any epidemic, as vaccine reminders, making the public aware of health-seeking behavior, and self-monitoring.[35,36,37,38]
Challenges and Barriers
Various challenges and barriers hinder the universal adoption and success of mHealth [Table 2].
Table 2.
Challenges and barriers impacting the success of mHealth
| Challenges/Barriers of mHealth | Overall impact |
|---|---|
| Data security | Concerns with privacy, the social stigma of patients with HIV/AIDS, STDs, and psychiatric illness. Lack of basic authentication and threat of hacking. |
| Standard maintenance | Varied stakeholders for standard maintenance of mHealth apps, security, appropriateness, and suitability, transparency, safety, technical support, and updates. |
| Varied operating system | Lack of homogeneity in the operating system (Microsoft window, iOs, Android, Blackberry, etc.) is a challenge for data transfer |
| Difficult discoverability | Poor discoverability makes the apps not so user-friendly. |
| Inadequacy of developing countries | Illiteracy in developing countries hinders the large-scale acceptance of mHealth apps. |
| Mobile addiction | Overuse of mobiles causing addiction. |
| Others | Road accident, increasing E-waste |
2). These snag needs to be overcome to give full umbrella coverage of mHealth technology to society.
Discussion
The health sector is now transforming, with a paradigm shift from traditional care to technology cladded with wireless mobile health care, with a promise to bring tremendous benefits and opportunities for diagnosis, prognosis, treatment, and prevention of human diseases for a better quality of life.[39] Of the total US broadband users, 27% use at least one connected health device, and wireless fitness device (e.g., a smartwatch) or health apps are used by 25% of US citizens.[40] It indicates that the widely used health-based applications are of great help to the users as a guide for wellness but with limitations such as clinical guidelines for parameters that might be missing.[41]
For other challenges such as data security, it is highly desirable to design and implement new mHealth technologies to build reliable, accurate, efficient, and secure healthcare environments for optimal patient care.[42]
A critical issue to health informatics has been raised due to highly complex health data that need better machine learning and understanding of big data-oriented algorithms, models, systems, and platforms to support the analysis, use, interpretation, and integration of diverse health data.[43] This calls for further advancement in the technology after a thorough analysis of the need.
Most studies, including ours, so far have focused on the development of mobile applications, which concerns only with the patients’ mHealth use.[44] However, it is equally important to identify the primary mHealth stakeholders and the key issues that inhibit the more widespread use of applications. Also, important are the platforms in healthcare that need attention, changes required in the regulatory processes, and last but not the least the future mHealth research, to further add knowledge and fill gaps.[45]
To combat against COVID-19 pandemic, a global health movement developed a campaign with a mission to educate people worldwide regarding SARS-CoV-2 and a way to protect them from this virus. This was possible with the use of mHealth apps which were downloaded over 10 million times, with 6 million downloads on the first day.[46] It’s hard to believe, but still, there is no standard protocol to treat COVID-19 patients, thus preventive measures to control this pandemic become crucial and this becomes possible with the help of mobile apps.[47] It was because of these technologies that normal activities like teaching in medical fields continued even during the lockdown period. Also, patient care, be it a COVID-19 or a general patient, was maintained to some extent using telemedicine, thereby ensuring social distancing without compromising patient care. Also, COVID-19 patients were triaged based on information collected by smartphones and they were treated/segregated accordingly.[48]
Conclusion
mHealth is that powerful mobile technology that has the potential to change the face of health services. Thus, it needs to create its niche in the world of technology.
Although, it foresees many hurdles to overcome related to multiple domains of mHealth, which involves stakeholders, market, privacy, data security, funding, and research studies demonstrating efficacy and cost, which need to be addressed. The use of mobiles for healthcare has started with high hopes beyond communication amongst health providers. Although many studies have highlighted a brighter future for the health sector by the use of advanced technologies in smartphones,[9] formal standardized algorithms are more in the stage of being imagined rather than developed or used. During this catastrophe of the COVID-19 pandemic, mobile technology has set foot by its newer role and application to face such events in the future with minimal calamity.
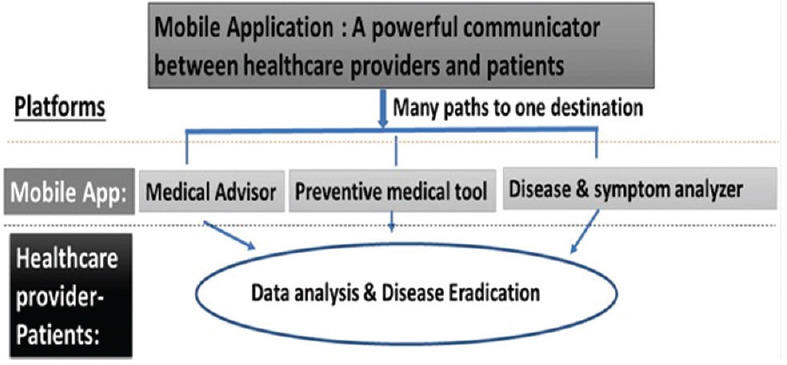
The key points and the take-home message from this review are summarized in Figure 3.
Figure 3.
Summary of the article
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Measuring the Information Society Report 2018 [Google Scholar]
- 2.Smartphone users worldwide 2020 |Statista [Google Scholar]
- 3.Ha JF, Longnecker N. Doctor-patient communication:A review. Ochsner J. 2010;10:38–43. [PMC free article] [PubMed] [Google Scholar]
- 4.Marshall C, Lewis D, Whittaker M. mHealth Technologies in Developing Countries:A Feasibility Assessment and a Proposed Framework. Herston, Australia: University of Queensland; 2013. pp. 1–47. [Google Scholar]
- 5.Jovanov E, Zhang YT. Introduction to the special section on M-Health:Beyond seamless mobility and global wireless health-care connectivity. IEEE Trans Inf Technol Biomedicine. 2004;8:405–14. doi: 10.1109/titb.2004.840019. [DOI] [PubMed] [Google Scholar]
- 6.Song X, Liu X, Wang C. The role of telemedicine during the COVID-19 epidemic in China—experience from Shandong province. Crit Care. 2020;24:1–4. doi: 10.1186/s13054-020-02884-9. doi:10.1186/s13054-020-02884-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith Y. 'Types of Telemedicine', News Medical-Life Sciences and Medicine. 2015 Available from: http://www.news-medical.net/health/Types-of-Telemedicine.aspx . [Google Scholar]
- 8.McLellan AT. Substance misuse and substance use disorders:Why do they matter in healthcare? Trans Am Clin Climatol Assoc. 2017;128:112. [PMC free article] [PubMed] [Google Scholar]
- 9.Park YT. Emerging new era of mobile health technologies. Healthc Inform Res. 2016;22:253–4. doi: 10.4258/hir.2016.22.4.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee JH. Future of the smartphone for patients and healthcare providers. Healthc Inform Res. 2016;22:1–2. doi: 10.4258/hir.2016.22.1.1. doi:10.4258/hir.2016.22.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Healthcare Information and Management Systems Society. 2016 [Google Scholar]
- 12.Litan RE. Vital signs via broadband:Remote health monitoring transmits savings, enhances lives. Better Health Care Together. 2008. Available from: http://www.broadbandillinois.org/uploads/cms/documents/litan.pdf .
- 13.Ascari A, Bakshi A, Grijpink F. mHealth:A New Vision for Healthcare. McKinsey &Company. Inc., and GSMA. 2010 [Google Scholar]
- 14.Ventola CL. Mobile devices and apps for health care professionals:Uses and benefits.PT. 2014;39:356. [PMC free article] [PubMed] [Google Scholar]
- 15.Pop-Eleches C, Thirumurthy H, Habyarimana JP, Zivin JG, Goldstein MP, De Walque D, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting:A randomized controlled trial of text message reminders. AIDS. 2011;25:825–34. doi: 10.1097/QAD.0b013e32834380c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lemon CA, Kim J, Haraguchi D, Sud A, Branley J, Khadra MH. Maintaining continuity of care in a multidisciplinary health service by using m-health technologies to develop patient medical records. In The International Conference on Health Informatics, Springer, Cham. 2014:84–7. [Google Scholar]
- 17.Singh GK, Singh CM, Ranjan A, Agarwal N, Pandey S, Kumar P, et al. Determinants of acute encephalitis syndrome (AES) in Muzaffarpur district of Bihar, India:A case–control study. Clin Epidemiol Global Health. 2016;4:181–7. [Google Scholar]
- 18.Aslani N, Lazem M, Mahdavi S, Garavand A. A review of mobile health applications in epidemic and pandemic outbreaks:Lessons learned for COVID-19. Arch Clin Infect Dis. 2020:15. doi:10.1016/j.pmedr.2021.101399. [Google Scholar]
- 19.MAjuMdAr A, Kar SS, GAneShkuMAr S, Palanivel C, Misra P. mHealth in the prevention and control of non-communicable diseases in India:Current possibilities and the way forward. J Clin Diagn Res. 2015;9:LE06–10. doi: 10.7860/JCDR/2015/11555.5573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rajavardhana T, Rajanandh MG, Geethavani M, Sreedhar V. Role of mhealth in the management of tuberculosis:A new approach to improve adherence. Int J Res Pharm Sci. 2020;11:5560–8. [Google Scholar]
- 21.Ferrer-Roca O, Cardenas A, Diaz-Cardama A, Pulido P. Mobile phone text messaging in the management of diabetes. J Telemed Telecare. 2004;10:282–5. doi: 10.1258/1357633042026341. [DOI] [PubMed] [Google Scholar]
- 22.Bove AA, Homko CJ, Santamore WP, Kashem M, Kerper M, Elliott DJ. Managing hypertension in urban underserved subjects using telemedicine—a clinical trial. Am Heart J. 2013;165:615–21. doi: 10.1016/j.ahj.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 23.Krishna S, Boren SA, Balas EA. Healthcare via cell phones:A systematic review. Telemed J E Health. 2009;15:231–40. doi: 10.1089/tmj.2008.0099. [DOI] [PubMed] [Google Scholar]
- 24.Bielli E, Carminati F, La Capra S, Lina M, Brunelli C, Tamburini M. A wireless health outcomes monitoring system (WHOMS):Development and field testing with cancer patients using mobile phones. BMC Med Inform Decis Mak. 2004;4:1–3. doi: 10.1186/1472-6947-4-7. doi:10.1186/1472-6947-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klasnja P, Hartzler A, Powell C, Pratt W. Supporting cancer patients'unanchored health information management with mobile technology. In AMIA Annual Symposium Proceedings, American Medical Informatics Association. 2011;Vol. 2011:732. [PMC free article] [PubMed] [Google Scholar]
- 26.Feroz A, Jabeen R, Saleem S. Using mobile phones to improve community health workers performance in low-and-middle-income countries. BMC Public Health. 2020;20:49. doi: 10.1186/s12889-020-8173-3. doi:10.1186/s12889-020-8173-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Feinleib M. A Dictionary of Epidemiology. John M, Last, Robert A, Spasoff, Susan S, Harris, editors. Am J Epidemiol. 2001;154:93–4. [Google Scholar]
- 28.Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Eurosurveillance. 2020;25:2000062. doi: 10.2807/1560-7917.ES.2020.25.5.2000062. doi:10.2807/1560-7917.ES.2020.25.5.2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission:A study of a family cluster. Lancet. 2020;395:514–23. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cossarizza A, Gibellini L, De Biasi S, Lo Tartaro D, Mattioli M, Paolini A, et al. Handling and processing of blood specimens from patients with COVID-19 for safe studies on cell phenotype and cytokine storm. Cytometry A. 2020;97:668–73. doi: 10.1002/cyto.a.24009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Navin K, Krishnan MM, Lavanya S, Shanthini A. A mobile health based smart hybrid epidemic surveillance system to support epidemic control programme in public health informatics. In 2017 International Conference on IoT and Application (ICIOT), IEEE. 2017 May 19;:1–4. doi:10.1109/ICIOTA.2017.8073606. [Google Scholar]
- 32.Maqbool A, Khan NZ. Analyzing barriers for implementation of public health and social measures to prevent the transmission of COVID-19 disease using DEMATEL method. Diabetes Metab Syndr. 2020;14:887–92. doi: 10.1016/j.dsx.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Danquah LO, Hasham N, MacFarlane M, Conteh FE, Momoh F, Tedesco AA, et al. Use of a mobile application for Ebola contact tracing and monitoring in northern Sierra Leone:A proof-of-concept study. BMC Infect Dis. 2019;19:1–2. doi: 10.1186/s12879-019-4354-z. doi:10.1186/s12879-019-4354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Altmann S, Milsom L, Zillessen H, Blasone R, Gerdon F, Bach R, et al. Acceptability of app-based contact tracing for COVID-19:Cross-country survey study. JMIR MHealth UHealth. 2020;8:e19857. doi: 10.2196/19857. doi:10.2196/19857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuehne A, Lynch E, Marshall E, Tiffany A, Alley I, Bawo L, et al. Mortality, morbidity and health-seeking behaviour during the Ebola epidemic 2014–2015 in Monrovia results from a Mobile phone survey. PLoS Negl Trop Dis. 2016;10:e0004899. doi: 10.1371/journal.pntd.0004899. doi:10.1371/journal.pntd. 0004899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alqahtani AS, Rashid H, Basyouni MH, Alhawassi TM, BinDhim NF. Public response to MERS-CoV in the Middle East:iPhone survey in six countries. J Infect Public Health. 2017;10:534–40. doi: 10.1016/j.jiph.2016.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Girond F, Randrianasolo L, Randriamampionona L, Rakotomanana F, Randrianarivelojosia M, Ratsitorahina M, et al. Analysing trends and forecasting malaria epidemics in Madagascar using a sentinel surveillance network:A web-based application. Malar J. 2017;16:1–1. doi: 10.1186/s12936-017-1728-9. doi:10.1186/s12936-017-1728-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fujibayashi K, Takahashi H, Tanei M, Uehara Y, Yokokawa H, Naito T. A new influenza-tracking smartphone app (Flu-Report) based on a self-administered questionnaire:Cross-sectional study. JMIR MHealth UHealth. 2018;6:e136. doi: 10.2196/mhealth.9834. doi:10.2196/mhealth. 9834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wu CQ, Wang Z, Chen G, Ferebee D. Recent advances and developments in mobile health. J Healthc Eng. 2018;2018:4747593. doi: 10.1155/2018/4747593. doi:10.1155/2018/4747593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pai A. Survey:74.9 percent of US adults do not track health or fitness with devices or apps. mobihealth news. 2014. Available from: https://www.mobihealthnews.com/content/aditi-pai?page=80 .
- 41.Kredo T, Bernhardsson S, Machingaidze S, Young T, Louw Q, Ochodo E, et al. Guide to clinical practice guidelines:The current state of play. Int J Qual Health Care. 2016;28:122–8. doi: 10.1093/intqhc/mzv115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jones DS. Masters of the Universe:Hayek, Friedman, and the Birth of Neoliberal Politics. 2014:1–418. doi:10.1093/jahist/jat346. [Google Scholar]
- 43.Dash S, Shakyawar SK, Sharma M, Kaushik S. Big data in healthcare:Management, analysis and future prospects. J Big Data. 2019;6:1–25. doi:10.1186/s40537-019-0217-0. [Google Scholar]
- 44.Lupton D. Apps as artefacts:Towards a critical perspective on mobile health and medical apps. Societies. 2014;4:606–22. [Google Scholar]
- 45.Petersen C, Adams SA, DeMuro PR. mHealth:Don't forget all the stakeholders in the business case. Med 2.0. 2015;4:e4. doi: 10.2196/med20.4349. doi:10.2196/med20.4349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Almalki M, Giannicchi A. Health apps for combating COVID-19:Descriptive review and taxonomy. JMIR MHealth UHealth. 2021;9:e24322. doi: 10.2196/24322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Asadzadeh A, Kalankesh LR. A scope of mobile health solutions in COVID-19 pandemics. Inform Med Unlocked. 2021;23:100558. doi: 10.1016/j.imu.2021.100558. doi:10.1016/j.imu.2021.100558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Giansanti D. The Role of the mHealth in the Fight against the Covid-19:Successes and failures. Healthcare. 2021;9:58. doi: 10.3390/healthcare9010058. doi:10.3390/healthcare9010058. [DOI] [PMC free article] [PubMed] [Google Scholar]