Abstract
Background.
Current cardiac surgery risk algorithms and quality measures focus on perioperative outcomes. However, delivering high-value, patient-centered cardiac care will require a better understanding of long-term patient-reported quality of life after surgery. Our objective was to prospectively assess the effect of cardiac surgery on long-term patient-reported outcomes.
Methods.
Patients undergoing cardiac surgery at an academic medical center (2016 to 2017) were eligible for enrollment. Patient-reported outcomes were measured using the National Institutes of Health Patient-Reported Outcomes Measurement Information System preoperatively and 1 year postoperatively across five domains: mental health, physical health, physical functioning, social satisfaction, and applied cognition. Baseline data and perioperative outcomes were obtained from The Society of Thoracic Surgeons Database. The effect of cardiac surgery on long-term patient-reported quality of life was assessed.
Results.
Ninety-eight patients were enrolled and underwent cardiac surgery, with 92.9% (91 of 98) successful follow-up. The most common operation was coronary artery bypass graft surgery at 63.3% (62 of 98), with 60.2% (59 of 98) undergoing an elective operation. One-year all-cause mortality was 5.1% (5 of 98). Rate of major morbidity was 11.2% (11 of 98). Cardiac surgery significantly improved patient-reported outcomes at 1 year across four domains: mental health (preoperative 47.3 ± 7.7 vs postoperative 51.1 ± 8.9, P < .001), physical health(41.2 ± 8.2 vs 46.3 ± 9.3, P < .001), physical functioning(39.8 ± 8.6 vs 44.8 ± 8.5, P < .001), and social satisfaction(46.8 ± 10.9 vs 50.7 ± 10.8, P = .023). Hospital discharge to a facility did not affect 1-year patient-reported outcomes.
Conclusions.
Cardiac surgery improves long-term patient-reported quality of life. Mental, physical, and social well-being scores were significantly higher 1 year postoperatively. Data collection with the National Institutes of Health Patient-Reported Outcomes Measurement Information System provides meaningful, quantifiable results that may improve delivery of patient-centered care.
Patient-reported outcomes (PROs) are increasingly recognized as important adjuncts to traditional outcome measures such as morbidity, mortality, and survival.1 The Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database has robust objective clinical data that supports accurate risk algorithms and important quality metrics, but is lacking in health-related quality of life (HR-QOL) data.2 The Institute of Medicine and many other national organizations, such as the American Heart Association, National Cancer Institute, Food and Drug Administration, and National Institutes of Health (NIH), have recognized the importance of PROs and advocate for their inclusion in future research studies.1,3–5 Providing patients with long-term HR-QOL data may allow for more informed decision making and an alignment of patient and clinician expectations. Delivery of high-value, patient-centered cardiac care will require a better understanding of long-term patient-reported QOL after cardiac surgery.
The NIH Patient Reported Outcomes Measurement Information System (PROMIS) is a validated set of questionnaires that was designed to allow for efficient collection of HR-QOL data across many domains, including mental health, physical functioning, and social well-being.6–8 The questionnaires are publicly available and can easily be administered through various forms of communication, allowing for inclusion in clinical workflows without causing major disruptions. Khullar and colleagues9 demonstrated the feasibility of integrating longitudinal PROMIS data collection into their institutional STS database in a pilot study of patients undergoing surgery for lung cancer. Likewise, our group assessed 1-year postoperative PRO in a cohort of 782 eligible patients who underwent cardiac surgery at a tertiary care institution.10 Follow-up at 1 year was quite successful, with a lost to follow-up rate of only 4.5%. The study demonstrated that long-term PRO data collection was feasible and yielded meaningful, patient-centered results; however, the findings were limited by the lack of enrolment and PROMIS data collection during the preoperative period.
Given that our prior study did not enroll patients in the preoperative period and follow them to 1-year postoperatively, we have designed and executed the present study as a longitudinal pilot study assessing the effect of cardiac surgery on HR-QOL. The objective was to assess the change in patient-reported QOL from the preoperative period to 1 year postoperatively. We hypothesized that cardiac surgery would improve PROs at 1 year postoperatively.
Patients and Methods
Study Population
All adult patients (aged 18 years or more) being considered for cardiac surgery at a single tertiary care academic medical center between June 2016 and January 2017 were eligible for enrollment. Exclusion criteria included prisoners, non-English speaking patients, patients being considered for transcatheter valve therapies or other procedures not captured in the STS Database, and patients who did not ultimately undergo cardiac surgery after enrollment. Both inpatient consultations to the cardiac surgery service and outpatient clinic visits were screened for eligibility by certified research coordinators. Enrollment was not limited by day of the week, time of day, or attending on call. Target analysis for this pilot study was 100 patients; therefore, goal enrollment was 110 patients to allow for an estimated 10% exclusion rate. The Institutional Review Board for Human Subjects Research at the University of Virginia (protocol #19091) approved this study. Written informed consent was obtained from all patients at the time of enrollment.
Data Collection
After enrollment, baseline patient-reported QOL was obtained from all patients using four NIH PROMIS short-form questionnaires: global health, 10 questions (Supplemental File 1); physical function, 10 questions (Supplemental File 2); satisfaction with social roles and activities, 8 questions (Supplemental File 3); and applied cognition, 8 questions (Supplemental File 4). The global health questionnaire yields two separate PROMIS scores: global mental health and global physical health; therefore, five total PROMIS domains were assessed in this study. To be successfully enrolled, patients were required to answer all 36 PROMIS questions. After all patients had been operated on (or excluded if it was determined that they would not undergo an operation), our institutional STS database was queried to obtain demographics, preoperative predicted risk scores, procedure details, and perioperative outcomes. At 1 year after their operation, all patients were contacted by telephone to reassess patient-reported QOL using the same four NIH PROMIS questionnaires. Phone calls were made at different times of the day and different days of the week to increase the likelihood of successfully reaching each patient, with a minimum of three attempts made to all patients.
National Institutes of Health PROMIS
The NIH PROMIS contains more than 300 measures of mental, physical, and social well-being that are universally relevant and can be used in the general population or in specific subgroups, such as cardiac surgery patients.11 All PROMIS questionnaires provide a T-score, normalized to a mean of 50 with a standard deviation of 10, which is the mean in the US general population for most measures. The global health short form evaluates physical function, emotional distress, social health, pain, and fatigue, and results in two separate scores, one for global mental health and one for global physical health. The physical function short form evaluates a patient’s ability to complete activities of daily living, as well as assesses their strength, mobility, and endurance. The satisfaction with social roles and activities short form measures a patient’s ability to complete daily and work-related tasks, as well as provide for their friends and family. The applied cognition short form evaluates a patient’s assessment of their memory, concentration, and thought formation.6,11 The PROMIS questionnaires were chosen for this study as they provide a general assessment of a patient’s mental, physical, and social health, and are aligned with the goals of the STS PRO Taskforce and the American Heart Association.2,12
Primary and Secondary Outcomes
The primary endpoint of this study was change in PROs at 1 year assessed using NIH PROMIS. For secondary endpoints, we analyzed the impact of discharge to a facility and the occurrence of a postoperative major morbidity (stroke, prolonged ventilation, reoperation, renal failure, deep sternal wound infection) on change in PROs from the preoperative period to 1 year postoperatively.
Statistical Analysis
Summary data for demographics, intraoperative characteristics, and postoperative outcomes are presented as mean ± SD or median and interquartile range (IQR) as determined by normality of the data for continuous variables. Percentage of the total and number were reported for categoric variables. Preoperative and 1-year postoperative PROMIS scores were collected, reported, and analyzed in accordance with guidelines provided by the NIH.11 They are presented as mean ± SD and compared using the Mann-Whitney U test. The Kruskal-Wallis test was used to evaluate the effect of discharge to facility and postoperative morbidity on change in PROMIS scores from the preoperative period to 1 year after cardiac surgery. All analyses were completed using SAS 9.4 (SAS Institute, Cary, NC). Alpha level for statistical significance was 0.05. Distributions of preoperative and 1-year postoperative PROMIS scores were modeled using Prism 7 (GraphPad Software, La Jolla, CA).
Results
Enrollment and Eligibility
During the study period from June 2016 to January 2017, 110 patients were enrolled (Figure 1). A total of 98 patients underwent cardiac surgery and satisfied the eligibility criteria for inclusion in the final analysis. One-year mortality was 5.1% (5 of 98). Of eligible patients who were alive at 1 year after their cardiac operation, 92.5% (86 of 93) were successfully contacted by telephone. Four patients declined to participate further, resulting in 83.7% of eligible patients (82 of 98) who ultimately completed the 1-year postoperative PROMIS questionnaires. Lost to follow-up rate due to inability to contact the patient by telephone was 5.1% (5 of 98).
Figure 1.
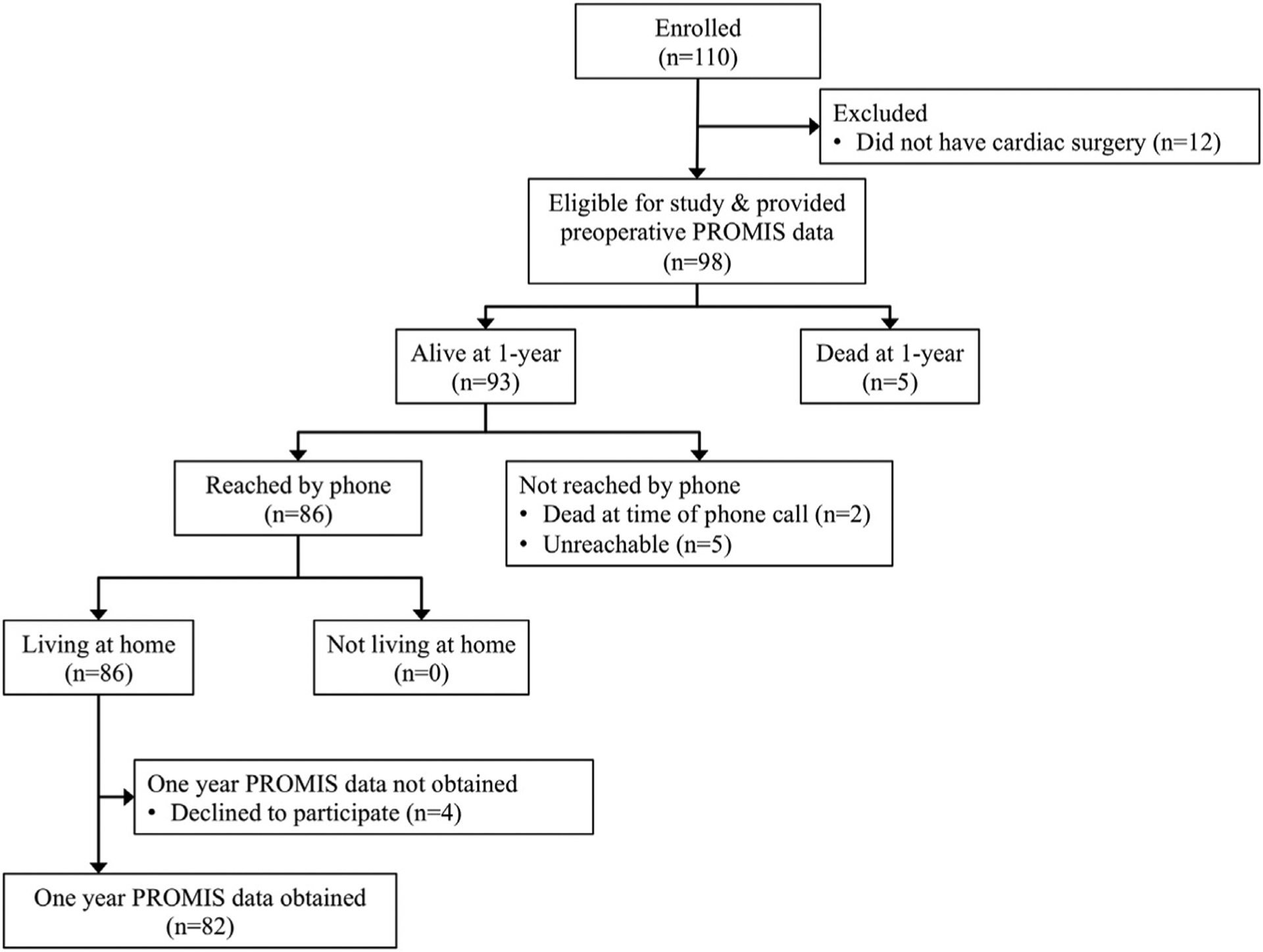
Participant flow diagram for all patients enrolled in the study. (PROMIS, Patient-Reported Outcomes Measurement Information System.)
Demographics and Intraoperative Characteristics
Baseline demographics and intraoperative characteristics for all eligible patients (n = 98) are shown in Table 1. Median age was 69 years (IQR, 61 to 75), with 40.8% (40 of 98) being female. Hypertension (68.4% [67 of 98]) and heart failure (48% [47 of 98]) were the two most common comorbidities. Coronary artery bypass graft surgery (63.3% [62 of 98]) and aortic valve replacement (33.7% [33 of 98]) were the two most common operations, with 60.2% (59 of 98) undergoing an elective operation.
Table 1.
Baseline Demographics and Intraoperative Characteristics for All Eligible Patients
| Characteristics | Eligible Patients (n = 98) |
|---|---|
| Baseline demographics | |
| Age, years | 69 (61–75) |
| Female | 40.8 (40) |
| White | 95.9 (94) |
| Heart failure | 48 (47) |
| Hypertension | 68.4 (67) |
| Peripheral artery disease | 14.3 (14) |
| Prior cerebrovascular accident | 7.1 (7) |
| Prior myocardial infarction | 41.8 (41) |
| Dialysis-dependent renal failure | 3.1 (3) |
| Diabetes mellitus | 32.7 (32) |
| Pulmonary disease | 10.2 (10) |
| Ejection fraction, % | 52.7 ± 13.9 |
| Intraoperative characteristics | |
| Case status | |
| Elective | 60.2 (59) |
| Urgent | 39.8 (39) |
| Emergent or emergent salvage | 0 (0) |
| Atrial fibrillation procedure | 4.1 (4) |
| Aortic procedure | 7.1 (7) |
| Coronary artery bypass graft | 63.3 (62) |
| Isolated coronary artery bypass graft | 39.8 (39) |
| Aortic valve repair | 1 (1) |
| Aortic valve replacement | 33.7 (33) |
| Mitral valve repair | 11.2 (11) |
| Mitral valve replacement | 5.1 (5) |
| Tricuspid valve repair | 5.1 (5) |
| Tricuspid valve replacement | 1 (1) |
| Pulmonary valve repair | 0 (0) |
| Ventricular assist device | 0 (0) |
| Heart transplantation | 0 (0) |
| Cardiopulmonary bypass time, min | 109 ± 36 |
Values are median (interquartile range), percent (n), or mean ± SD.
Postoperative STS Outcomes
Postoperative outcomes for all eligible patients are shown in Table 2. Atrial fibrillation was the most common postoperative occurrence (25.5% [25 of 98]). Rate of major morbidity was 11.2% (11 of 98) and operative mortality was 2% (2 of 98). Approximately 1 of every 5 patients was discharged to a facility (22.5% [22 of 98]).
Table 2.
The Society of Thoracic Surgeons Postoperative Outcomes for All Eligible Patients
| Postoperative Outcomes | Eligible Patients (n = 98) |
|---|---|
| Stroke | 2 (2) |
| Atrial fibrillation | 25.5 (25) |
| Cardiac arrest | 0 (0) |
| Pneumonia | 1 (1) |
| Renal failure | 4.1 (4) |
| Prolonged ventilation, >24 hours | 7.1 (7) |
| Deep sternal wound infection | 0 (0) |
| Reoperation | 1 (1) |
| Intensive care unit length of stay, h | 61 (38–114) |
| Hospital length of stay, d | 6 (5–8) |
| Discharge to facility | 22.5 (22) |
| Major morbidity | 11.2 (11) |
| Operative mortality | 2 (2) |
| One-year mortality | 5.1 (5) |
Values are percent (n) or median (interquartile range).
One-Year Patient-reported Outcomes
Cardiac surgery significantly improved patient-reported outcomes at 1 year across four NIH PROMIS domains: global mental health, global physical health, physical functioning, and satisfaction with social roles and activities (Table 3). Applied cognition was not significantly different at 1 year compared with preoperative scores. Graphical distributions of preoperative and 1-year postoperative PROMIS scores are shown in Figure 2.
Table 3.
Comparison of Preoperative and One-Year Postoperative National Institutes of Health Patient-Reported Outcomes Measurement Information System Scores for Eligible Patients Undergoing Cardiac Surgery
| NIH PROMIS Domain | Preop Score (n = 98) | 1-Year Postop Score (n = 82) | P Value |
|---|---|---|---|
| Global mental health | 47.3 ± 7.7 | 51.1 ± 8.9 | <.001 |
| Global physical health | 41.2 ± 8.2 | 46.3 ± 9.3 | <.001 |
| Physical functioning | 39.8 ± 8.6 | 44.8 ± 8.5 | <.001 |
| Satisfaction with social roles and activities | 46.8 ± 10.9 | 50.7 ± 10.8 | .023 |
| Applied cognition | 33.8 ± 7.8 | 33.3 ± 7.5 | .666 |
Values are mean ± SD.
NIH PROMIS, National Institutes of Health Patient-Reported Outcomes Measurement Information System; Postop, postoperative.
Figure 2.
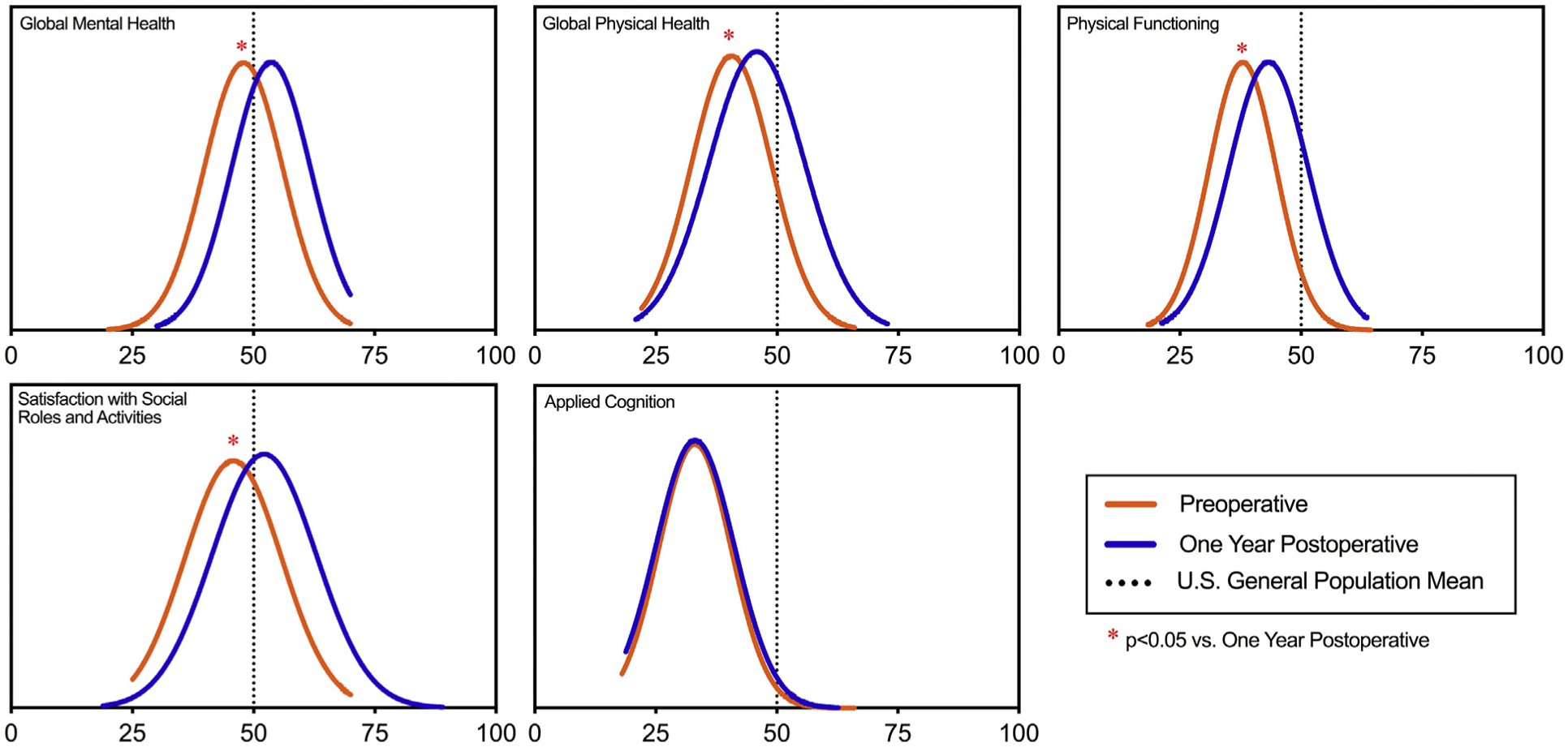
Distributions of National Institutes of Health Patient-Reported Outcomes Measurement Information System scores—global mental health, global physical health, physical functioning, satisfaction with social roles and activities, and applied cognition—for all eligible patients preoperatively (orange lines) and 1 year postoperatively (blue lines). The vertical dotted line indicates US general population mean; red asterisk (*) indicates P < .05 vs 1 year postoperative.
Discharge to a facility did not affect 1-year PROs across all five domains (Table 4). Changes in NIH PROMIS scores from the preoperative period to 1-year after cardiac surgery were not different when patients were stratified by occurrence of a major morbidity across four domains (global mental health, global physical health, physical functioning, and satisfaction with social roles and activities). However, applied cognition showed a significant difference (Table 5).
Table 4.
Change in National Institutes of Health Patient-Reported Outcomes Measurement Information System Scores From Preoperative Period to 1 Year After Cardiac Surgery Stratified by Discharge Location
| NIH PROMIS Domain | Discharge to Home (n = 65) | Discharge to Facility (n = 17) | P Value |
|---|---|---|---|
| Global mental health | 4.1 ± 8.7 | 1.8 ± 10.9 | .595 |
| Global physical health | 5 ± 10.2 | 3.1 ± 9.8 | .496 |
| Physical functioning | 5.6 ± 8.6 | 1.2 ± 9.2 | .073 |
| Satisfaction with social roles and activities | 4.8 ± 13.3 | −1.7 ± 14.4 | .107 |
| Applied cognition | −0.4 ± 9.6 | 0.4 ± 6.5 | .611 |
Values are mean ± SD.
NIH PROMIS, National Institutes of Health Patient-Reported Outcomes Measurement Information System.
Table 5.
Change in National Institutes of Health Patient-Reported Outcomes Measurement Information System Scores From Preoperative Period to 1 Year After Cardiac Surgery Stratified by Major Morbiditya
| NIH PROMIS Domain | No Major Morbidity (n = 74) | Major Morbidity (n = 8) | P Value |
|---|---|---|---|
| Global mental health | 3.6 ± 9.5 | 3.7 ± 6.5 | .969 |
| Global physical health | 4.2 ± 10.3 | 8 ± 8.2 | .208 |
| Physical functioning | 4.4 ± 9.2 | 7.2 ± 4.6 | .352 |
| Satisfaction with social roles and activities | 3.7 ± 14 | 1.6 ± 11.9 | .79 |
| Applied cognition | −0.9 ± 9 | 5.3 ±7 | .028 |
Values are mean ± SD.
Major morbidity includes stroke, prolonged ventilation, reoperation, renal failure, and deep sternal wound infection.
NIH PROMIS, National Institutes of Health Patient-Reported Outcomes Measurement Information System.
Comment
The present study evaluated PROs 1 year after cardiac surgery using a validated and generalizable set of NIH PROMIS short-form questionnaires. Global mental health, global physical health, physical functioning, satisfaction with social roles and activities, and applied cognition were successfully measured at 1 year in 88.2% of alive and eligible patients (82 of 93). Cardiac surgery resulted in significant improvements across four NIH PROMIS domains at 1 year compared with preoperative values. Hospital discharge to a facility and occurrence of a postoperative major morbidity did not negatively affect 1-year PROs.
The lost to follow-up rate was only 5.1% at 1 year in this longitudinal pilot study of long-term PROs. Figure 1 highlights the patient flow from enrollment to attainment of the primary endpoint. Our successful follow-up rate in the present study mirrors the results presented in our prior publication.10 In a postoperative cohort of 782 patients who underwent cardiac surgery, more than 95% of patients were successfully contacted by telephone at 1 year after their operation. Feasibility of data collection is one obstacle that must be navigated; however, there are other burdens associated with collecting long-term PROs. These hurdles include but are not limited to choosing which measures to use, deciding how to collect the data, and designing an efficient methodology for incorporating the data into the electronic medical record.13,14 As more studies incorporate PROs, it is expected that best practices will evolve that can be generalized across different clinical settings. The STS PRO Taskforce is once such organization that is already testing methods for the design and implementation of collecting meaningful, patient-reported QOL data.9
In the present study, HR-QOL improved significantly at 1 year after cardiac surgery compared with preoperative values across four NIH PROMIS domains. Collecting objective outcomes data is more convenient than PROs, but studies have found that PROs better define treatment success for patients compared with short-term perioperative outcomes.15–18 As we shift toward patient-centered care models that focus on quality rather than volume, presenting patients with meaningful HR-QOL in the preoperative setting will become a necessity.19 Being able to present patients with accurate estimates of their mental, physical, and social well-being at 1 year after surgery would be remarkably empowering for patients and their families, allowing them to make well-informed medical decisions. As collection of HR-QOL measures becomes standard practice, we anticipate combining traditional clinical outcome metrics (ie, morbidity, mortality) with PROs into a complete risk assessment model that can be used to advise patients and perform indepth comparative effectiveness analyses between treatment options. In addition, the expansion of PRO data collection over time and its inclusion in the STS Database will allow us to better correlate effect size of NIH PROMIS score differences with clinical significance.
We chose to use NIH PROMIS short-form questionnaires to obtain preoperative and 1-year postoperative PROs in the current study. The PROMIS questionnaires have been well validated in the general public and in patients with different medical conditions, allowing scores to be obtained and compared easily across various populations.6,11,20 This flexibility is well suited for comparative effectiveness studies evaluating different treatment options on long-term PRO. Nonetheless, there are multiple different HR-QOL measures that can be used to obtain PROs. To determine QOL in patients with heart failure, options include but are not limited to the Minnesota Living With Heart Failure Questionnaire, the Quality of Life in Severe Heart Failure Questionnaire, and the Kansas City Cardiomyopathy Questionnaire.21–23 Although most of these measures have been used for quite some time, it still remains to be answered which questionnaire provides the appropriate balance of efficiency, precision, and utility. The same questions exist for assessing patient-reported QOL and clinical success after cardiac surgery. Our experience collecting 1-year PROs with NIH PROMIS measures has been positive. The questionnaires are easy to administer either in person, electronically on a tablet, or through the mail. Enrolling patients preoperatively and collecting their responses took on average 15 minutes. Telephone calls made 1 year after cardiac surgery took less time, as patients were already enrolled and familiar with the questions being asked.
In addition to evaluating the overall effect of cardiac surgery on patient-reported QOL, the present study assessed the impact of discharge to a facility and the occurrence of a postoperative morbidity on PROs. There is a perception that patients discharged to a facility and patients with a postoperative morbidity have worse overall outcomes. However, results from this pilot study indicate that discharge to a facility does not impact PROs at 1 year after surgery, nor does a postoperative morbidity. Our previous study found that a surprising 82% of patients discharged to a facility were alive and living at home at 1 year, but discharge to a facility was found to correlate with worse long-term PROs.10 The discordance between these two studies may be attributed to the difference in study design (postoperative enrollment and data collection versus preoperative enrollment with preoperative and postoperative data collection) or sample size (782 versus 98 patients). The findings from both studies are of significant interest but will require further investigation with future studies before definitive conclusions can be made.
The present study has several important limitations. It was designed as a longitudinal pilot study, so the overall sample size is small (110 patients enrolled, 98 ultimately eligible for participation). One important objective was assessing the feasibility of obtaining preoperative and postoperative PROs for patients undergoing various cardiac surgery procedures while ensuring a low lost to follow-up rate. Future studies are needed with larger sample sizes to allow for procedure-specific subgroup analyses, which will limit potential bias and account for the fact that PROs can vary significantly depending on the presenting clinical picture (ie, congestive heart failure exacerbation versus stable angina).
In addition, our research protocol utilized clinical research coordinators and a few dedicated surgical residents for screening, enrollment, data acquisition, and analysis. This methodology for collecting and analysing PROs is most likely not scalable for all patients undergoing cardiac surgery across multiple different institutions. For PROs to become a routine data field in the STS Database, an efficient, low-cost process for obtaining and analyzing the data will need to be designed. Future studies should compare different PROs measures and explore other domains within the NIH PROMIS system to help identify the most meaningful outcomes to collect. Some measures used in this study assess patients’ temporal well being (ie, “within the last 7 days”), which may be a source of bias due to non-health-related life events occurring during that timeframe. A multiinstitutional prospective study that evaluates long-term PROs based on treatment modality, coronary artery bypass graft surgery versus percutaneous coronary intervention or surgical versus transcatheter aortic valve replacement, will be another important next step. These data will allow us to determine whether PROs can improve our ability to counsel patients regarding which therapies align most with their values and expectations.
In conclusion, this longitudinal pilot study found that cardiac surgery positively affects long-term patient-reported quality of life. Mental, physical, and social well-being scores as measured by NIH PROMIS questionnaires were significantly higher 1 year postoperatively compared with preoperative values. Obtaining long-term PROs in this study was feasible and yielded meaningful, quantifiable results. As numerous national organizations now encourage or require the collection of PROs in research studies and clinical practice, it is prudent for cardiothoracic surgeons and the STS to be at the forefront of this endeavor. Incorporating PROs in clinical trials, registries, and databases will allow us to continue setting the example for the delivery of high quality, patient-centered health care.
Supplementary Material
Acknowledgments
This work was supported by the National Heart, Lung, and Blood Institute grant numbers UM1 HL088925 and T32 HL007849. The authors wish to thank the Surgical Therapeutic Advancement Center at the University of Virginia for the assistance with screening, enrollment, and data collection.
Footnotes
Presented at the Sixty-sixth Annual Meeting of the Southern Thoracic Surgical Association, Marco Island, FL, Nov6–9, 2019.
The Supplemental Material can be viewed in the online version of this article [10.1016/j.athoracsur.2020.09.061] on http://www.annalsthoracicsurgery.org.
References
- 1.Khullar OV, Fernandez FG. Patient-reported outcomes in thoracic surgery. Thorac Surg Clin. 2017;27:279–290. [DOI] [PubMed] [Google Scholar]
- 2.D’Agostino RS, Jacobs JP, Badhwar V, et al. The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2018 update on outcomes and quality. Ann Thorac Surg. 2018;105: 15–23. [DOI] [PubMed] [Google Scholar]
- 3.Lipscomb J, Gotay CC, Snyder CF. Patient-reported outcomes in cancer: a review of recent research and policy initiatives. CA Cancer J Clin. 2007;57:278–300. [DOI] [PubMed] [Google Scholar]
- 4.Institute of Medicine (US). Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Available at: https://www.ncbi.nlm.nih.gov/pubmed/25057539. Accessed November 1, 2019.
- 5.Rumsfeld JS, Alexander KP, Goff DC, et al. Cardiovascular health: the importance of measuring patient-reported health status: a scientific statement from the American Heart Association. Circulation. 2013;127:2233–2249. [DOI] [PubMed] [Google Scholar]
- 6.Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63: 1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones RS, Stukenborg GJ. Patient-Reported Outcomes Measurement Information System (PROMIS) use in surgical care: a scoping study. J Am Coll Surg. 2017;224:245–254. e241. [DOI] [PubMed] [Google Scholar]
- 8.Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of physical and mental health summary scores from the Patient-Reported Outcomes Measurement Information System (PROMIS) global items. Qual Life Res. 2009;18: 873–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khullar OV, Rajaei MH, Force SD, et al. Pilot study to integrate patient reported outcomes after lung cancer operations into The Society of Thoracic Surgeons Database. Ann Thorac Surg. 2017;104:245–253. [DOI] [PubMed] [Google Scholar]
- 10.Charles EJ, Mehaffey JH, Hawkins RB, et al. Meaningful patient-centered outcomes 1 year following cardiac surgery. Ann Surg. 2021;273:e247–e254. [DOI] [PubMed] [Google Scholar]
- 11.National Institutes of Health. HealthMeasures: Patient-Reported Outcomes Measurement Information System. Available at: http://www.nihpromis.org. Accessed November 1, 2019.
- 12.Rumsfeld JS, Magid DJ, O’Brien M, et al. Changes in health-related quality of life following coronary artery bypass graft surgery. Ann Thorac Surg. 2001;72:2026–2032. [DOI] [PubMed] [Google Scholar]
- 13.Basch E Patient-reported outcomes—harnessing patients’ voices to improve clinical care. N Engl J Med. 2017;376:105–108. [DOI] [PubMed] [Google Scholar]
- 14.Snyder CF, Aaronson NK, Choucair AK, et al. Implementing patient-reported outcomes assessment in clinical practice: a review of the options and considerations. Qual Life Res. 2012;21:1305–1314. [DOI] [PubMed] [Google Scholar]
- 15.Amemiya T, Oda K, Ando M, et al. Activities of daily living and quality of life of elderly patients after elective surgery for gastric and colorectal cancers. Ann Surg. 2007;246:222–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garcia SF, Cella D, Clauser SB, et al. Standardizing patient-reported outcomes assessment in cancer clinical trials: a patient-reported outcomes measurement information system initiative. J Clin Oncol. 2007;25:5106–5112. [DOI] [PubMed] [Google Scholar]
- 17.Kelkar AA, Spertus J, Pang P, et al. Utility of patient-reported outcome instruments in heart failure. JACC Heart Fail. 2016;4: 165–175. [DOI] [PubMed] [Google Scholar]
- 18.Makhni EC, Meadows M, Hamamoto JT, Higgins JD, Romeo AA, Verma NN. Patient Reported Outcomes Measurement Information System (PROMIS) in the upper extremity: the future of outcomes reporting? J Shoulder Elbow Surg. 2017;26:352–357. [DOI] [PubMed] [Google Scholar]
- 19.Birkmeyer JD, Dimick JB, Birkmeyer NJ. Measuring the quality of surgical care: structure, process, or outcomes? J Am Coll Surg. 2004;198:626–632. [DOI] [PubMed] [Google Scholar]
- 20.Ranganathan K, Shapiro D, Carlozzi NE, et al. The feasibility and validity of PROMIS: a novel measure of quality of life among children with cleft lip and palate. Plast Reconstr Surg. 2016;138:675e–681e. [DOI] [PubMed] [Google Scholar]
- 21.Garin O, Herdman M, Vilagut G, et al. Assessing health-related quality of life in patients with heart failure: a systematic, standardized comparison of available measures. Heart Fail Rev. 2014;19:359–367. [DOI] [PubMed] [Google Scholar]
- 22.Rector TS, Cohn JN. Assessment of patient outcome with the Minnesota Living with Heart Failure Questionnaire: reliability and validity during a randomized, double-blind, placebo-controlled trial of pimobendan. Pimobendan Multicenter Research Group. Am Heart J. 1992;124:1017–1025. [DOI] [PubMed] [Google Scholar]
- 23.Yee D, Novak E, Platts A, Nassif ME, LaRue SJ, Vader JM. Comparison of the Kansas City Cardiomyopathy Questionnaire and Minnesota Living With Heart Failure Questionnaire in predicting heart failure outcomes. Am J Cardiol. 2019;123:807–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


