Abstract
The experience of stigma by autistic people is relatively understudied, despite contributing to a range of poor outcomes and having an overarching impact on well-being. The current review of the literature synthesizes research to determine what is currently known and presents a theoretical model of autism stigma. Autism stigma is primarily influenced by a public and professional understanding of autism in combination with interpretation of visible autistic traits. Moderating factors include the quality and quantity of contact with autistic people, cultural factors, sex and gender, individual differences, and diagnostic disclosure. Stigma can reduce well-being as well as increase the presence of camouflaging behaviors, which mask autistic traits. Caregivers of autistic people can experience stigma by association, that is, affiliate stigma, which can impact their own well-being. A variety of interventions and approaches to reduce stigma are discussed, including “autism friendly” spaces, positive media representation, educational and psychosocial training for the public and professionals, as well as cultural and systemic shifts that foster inclusivity and recognize neurodiversity.
Keywords: autism, stigma, attitudes, neurodiversity, discrimination, well-being
Community brief
Why is this topic important?
Autistic people are known to experience stigma. This means that they can face ignorance, prejudice, and discrimination.
What was the purpose of this article?
The purpose of the article was to review research on autism stigma. We wanted to better understand autism stigma. We looked at why autistic people and their families experienced stigma. We also looked at what factors influenced stigma and the impact of stigma. Last, we discussed how to reduce stigma for autistic people and their families.
What do the authors conclude?
We summarized the research findings into a model. Autism stigma is affected by people's understanding of autism and by visible autistic traits. Poor understanding of autism means that visible autistic traits may be viewed negatively. Certain factors influence the amount of stigma. One factor was the quality and quantity of contact that autistic people have with others. Another factor was cultural differences, such as specific beliefs about autism. Sex and gender were important, as were other differences such as education and age. Last, whether an autistic person had shared their diagnosis affected stigma. Autism stigma had a negative impact on well-being. This included poor mental and physical health, as well as reduced social connections. Autism stigma also led to increased “camouflaging” of autistic traits. Family members also experienced stigma, which can affect their own well-being. Reducing autism stigma is important. To reduce stigma people should create more “autism friendly” spaces. They should include more positive representations of autistic people in the media. They should also improve the autism education of the public and professionals. Last, they should support neurodiversity.
What do the authors recommend for future research on this topic?
We need to better understand the factors that lead to autism stigma. We also need more effective ways to reduce stigma for autistic people and their families. Including the autistic community in this research process is very important.
How will this review help autistic adults now and in the future?
The review shows how stigma affects the autistic community. Autistic adults may find that the model helps them understand their own experiences of stigma. We hope the review will help develop more research into how to reduce autism stigma. Reducing autism stigma will improve the lives of autistic adults.
Introduction
The experience of stigma for minority groups is well recognized,1,2 with autism considered an identity-based minority.3 However, the specific experience of stigma for autistic people has been relatively understudied, with a bias toward the experiences of family members rather than autistic people themselves.4 The term stigma dates back to the ancient Greek practice of cutting or burning a mark into a person to brand them a slave, traitor, or criminal, the mark of someone to be avoided.5 In modern usage, stigma is considered an attribute that is unfavorable and that seemingly discredits an individual, leaving them to be viewed as less valuable than the rest of society.1,5,6 Notably, this definition depends on a collective understanding of what is unfavorable, thus stigma is inherently socially constructed.1
Stigma can be seen as an overarching term for problems of knowledge (i.e., ignorance), problems of attitudes (i.e., prejudice), and problems of behaviors (i.e., discrimination).7 Definitions of the interconnecting processes that contribute to or reflect stigma are varied, underlining the challenge of capturing this complex process. This review draws on Link and Phelan's seminal conceptualization of stigma.8 They argue that the development of stigma derives from the culturally driven detection and labeling of a difference (e.g., labeling people with a particular set of behavioral characteristics as autistic), which converges with other interrelated components to form stigma.
Link and Phelan's8 second component of stigma is the attribution of unfavorable stereotypes to the label (e.g., autistic people are unfriendly). From a social-cognitive perspective, this linking between a label and its stereotypes is key to the development of stigma, as stereotypes can implicitly affect how an individual perceives other people.9 The next component is the use of the label to cause a separation between “them” and “us” (e.g., autistic people vs. everyone else). The final component is loss of status and the experience of discrimination (e.g., not being hired or promoted because of being autistic).
Status loss and discrimination can be perceived as behavioral outcomes of stigma; a consequence of being labeled, being classified as other, and being linked to undesirable characteristics. Experiencing status loss and discrimination lies at the heart of the inequality that a stigmatized person faces and contributes to negative treatment at both personal and structural levels.7,8 Limited knowledge and understanding has a critical role in the presence of stigmatized views, as an individual is more likely to rely on reductionist labels and stereotypes, dichotomize into them versus us, and ultimately behave in a discriminatory way.
Attitudes and beliefs can be conceptualized as the deeply held cognitions that lead to the labeling, stereotyping, setting apart, and discriminating that contribute to stigma.8 Attitudes are often measured by directly asking people to state how much they endorse positive and negative attitudes toward autism.10 Alternatively, openness toward a fictional autistic adult or child can be explored, for example, by asking participants to rate whether they would feel afraid of the autistic person.11,12 Stigma is traditionally measured by using a measure of social distance, which is seen as a consequence of stigmatized views and conceptualized as the deliberate avoidance or exclusion of another person from social interactions.13,14
Stigma can be categorized into different types. Most commonly, the discussion of stigma refers to enacted or public stigma, which is the overt discrimination of stigmatized individuals.15 However, this review will also consider self-stigma, or felt stigma, which is when the stigmatized person turns the prejudice they experience onto themselves.16 This can include feeling shame in relation to stigmatized characteristic(s), and fear of enacted stigma.16,17 Affiliate, or courtesy, stigma will also be discussed, which is stigma experienced by people associated with the stigmatized person, e.g., family members (Table 1).5,15
Table 1.
A Summary of the Definitions of Stigma
| Term | Definition |
|---|---|
| Stigma | A socially constructed concept; any attribute that is seen as unfavorable and that seemingly discredits an individual, leaving them to be viewed as less valuable than the rest of society. |
| Public/Enacted Stigma | Discrimination or rejection experienced by a stigmatized person. |
| Felt/Self Stigma | The internalized prejudice experienced by a stigmatized person, including shame and fear of enacted stigma. |
| Affiliate/Courtesy Stigma | Stigma experienced through association with a stigmatized person (e.g., parents/caregivers and other family members). |
Autistic people can experience loneliness and fewer friendships compared with neurotypical peers,18–20 fewer friendships in adolescence compared with peers with other special educational needs,21 have more difficulties with education22 and employment,23,24 experience poor social integration,25,26 and face high rates of bullying.21 These factors are associated with a reduced quality of life.27 While these experiences have been attributed to autistic traits, more recent thinking has also considered the impact of negative societal responses to autistic people in contributing to these outcomes.28,29 Reflecting this, interviews with neurotypical people have found that autism is perceived by some as violating “accepted societal norms.”30
Autistic people encounter negative experiences in their everyday lives that likely reflect autism stigma. For example, neurotypical people are less likely to want to live in the same building as autistic people or to spend time together as friends,11 and they are also less likely to want an intimate relationship with an autistic person.31 At the extreme, autistic people can be dehumanized by neurotypical people.32 Autistic people describe autism stigma as destructive and at odds with their own conception of autism as a value-neutral category, such as handedness and eye color.33
Accordingly, 15.4% of a recent sample of 149 autistic adults report moderate to severe felt stigma,4 with the experience of stigma being reported by autistic adolescents and adults across a range of qualitative accounts.33–35 Alongside this, there is consistent evidence that affiliate stigma is experienced by the families of autistic people.36–45
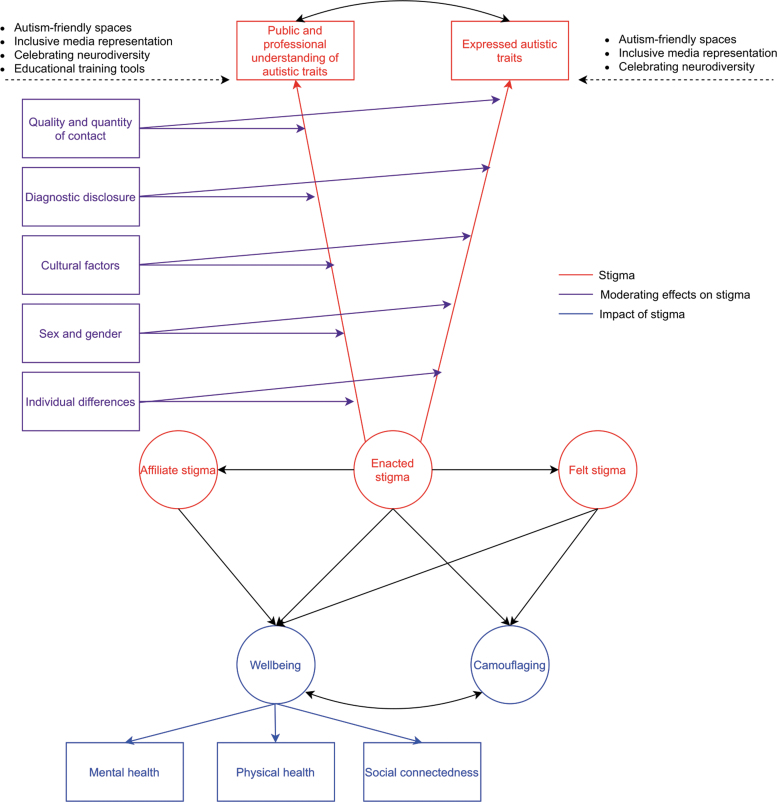
The breadth of psychological and social issues relevant to autism stigma and the limited synthesis of this work drew us to a narrative review. The broad remit of a narrative review enabled us to consider a wide range of pertinent issues: factors that contribute to autism stigma, the impact of stigma for autistic people and their families, and possible interventions to reduce stigma. These findings will be conceptualized in a theoretical model of autism stigma (Fig. 1).
FIG. 1.
Theoretical model of causes and impact of autism stigma. Red circles indicate stigma, with Enacted stigma represented by the convergence of public and professional understanding of autism and expressed autistic traits (observed variables). Felt stigma and Affiliate stigma are experienced through Enacted stigma (black arrows). Purple rectangles indicate factors that have a moderating effect on the observed variables. Blue circles indicate the impact of stigma, including Well-being, measured by three observed variables, and camouflaging. Black arrows indicate the direct effects between Enacted stigma and Well-being and Camouflaging, as well as the indirect effects through the effects of Affiliate and Felt stigma. The curved black double- headed arrow illustrates covariance between public and professional understanding of autistic traits and expressed autistic traits, and between Well-being and Camouflaging. The bullet points above the dashed lines indicate interventions that may reduce stigma.
The model provides an overview for researchers interested in exploring the many facets of autism stigma and supports autistic people wanting to map their own experiences onto existing evidence. Importantly, when developing the model, we considered the definition of stigma broadly and also incorporated relevant research on attitudes and acceptance, which are correlates of stigma and theoretically tightly coupled.8,46 Our narrative approach was underpinned by a thorough PubMed review of articles on autism (autis*) paired systematically with each of the following terms stigma, attitude, understanding, and knowledge.
We followed up relevant citations enabling our search to snowball and reach saturation. The model has been shaped by the findings, theory, and critical analysis within the references, as well as by additional areas of research flagged as important by our initial search and included as part of our snowballing strategy (e.g., neurodiversity in autism).
Factors Influencing Stigma in Autism
As detailed in Figure 1, the variables that contribute to autism stigma are public and professional understanding of autistic traits and expressed autistic traits. As previously mentioned, understanding has an overarching effect on the development of stigma. We also include expressed autistic traits, as stigma is fundamentally driven by a culturally driven detection and labeling of a difference.8 We argue that it is from this intersection of understanding of and observation of autism that other components of stigma occur.
Moderating factors that influence the strength or direction of the relationship between these variables and stigma include: the quality and quantity of contact, diagnostic disclosure, culture, sex and gender, and individual differences. Note that our model only includes the direct moderating effects on enacted stigma. These moderators are likely to have direct effects on both felt and affiliate stigma, but this is beyond the scope of the review.
Public and professional understanding of autistic traits
When discussing understanding we are referring to a holistic conception and comprehension of autism that goes beyond factual or “book” knowledge. For example, knowing that autism is diagnosed more in males would not be useful when wanting to support an autistic person struggling with sensory overload. However, studies have focused on measures that probe knowledge, for example, discrete facts about etiology, treatment, or selected symptoms.13,47 Poorer public and professional knowledge of autism is often correlated with less positive attitudes48 and more stigma,29,48–51 although null results also occur.52–56 Knowledge is also recognized by carers of autistic children as contributing toward stigmatized views.44
Some surveys have shown encouraging levels of autism knowledge among the public.48,57,58 However, incorrect knowledge is present in the public and the impact of incorrect knowledge, even in the context of dominantly correct knowledge, is not understood. Some areas of misinformation include that autism is characterized by symptoms of other conditions,58 that all autistic children show poor eye contact,57 and that autistic people do not show affection or attachments.50
Undergraduate students who incorrectly attributed unfavorable traits to autism were likely to have less positive attitudes toward autism regardless of the number of correct traits they identified.53 This suggests certain misconceptions may dominate, even in the face of some correct knowledge. Another important consideration is the valence of the knowledge that is associated with autism. Eight of the 10 characteristics that undergraduate students most commonly associated with autism had negative valence, with negative stereotyping likely to contribute to stigma.59
There are also misconceptions and inadequate knowledge about autism among health care professionals.52,56,60–65 UK general practitioners displayed good knowledge of autism but only modest confidence in their ability to work with autistic people,66 which arguably highlights the limitations of factual knowledge in equipping professionals to engage effectively with autistic people. Teachers and childcare providers may also have poor knowledge and outdated beliefs about autism, particularly relating to etiology,58,67–71 although teachers with more experience of autism have more knowledge.72,73
Some autistic pupils reported feeling stigmatized by their teachers and attributed this to being judged based on previous experiences with other autistic pupils.74 These limitations have been partly attributed to insufficient training,64–66,75 with professionals with better knowledge and experiences less likely to stigmatize autistic children.44,49
To fully explore the effect of autism understanding on autism stigma, fine-grained analysis is needed to disentangle what types of knowledge and understanding are most predictive of better attitudes and lower stigma. We argue that nuanced understanding, which critically recognises the heterogeneity and complexity within the autism spectrum, would be a better predictor than discrete facts. To this end, measuring understanding through identifying autistic people in vignettes or a video, which relies on consideration of patterns of behaviours, may be a more sensitive measure than fact endorsement.
It would also be meaningful to extend understanding of autism to knowing how to best support autistic people. Consideration should also be given to what the autistic community think others should understand about autism. Reflecting this, a recent autism knowledge questionnaire that was co-produced by the autistic community found that the subsections around societal views and the experience of being autistic were predictors of autism attitudes in Australian adults.48
Expressed autistic traits
Autistic people's difficulties in social communication are often physically expressed; examples include unusual patterns of eye contact, reduced facial expression and sharing of emotions, and limited gesture use.76 Restricted and repetitive behaviors can include motor mannerisms and unusual responses to sensory stimuli.76 Sensory behaviors can be particularly prevalent outside the home in unfamiliar spaces,77 and overwhelming sensory experiences can induce significant distress.78
These visible autistic traits may lead to negative attitudes during first impression formation.28,79,80 When assessing first impressions using video clips, neurotypical people have perceived autistic people as less attractive, more submissive, and more awkward than matched neurotypical counterparts.28 However, first impressions were not negative when the speech transcript was presented without visual stimuli, suggesting that the bias was driven by expressive differences.28
Some of these expressed differences can be particularly negatively perceived by the neurotypical population. Stereotyped or repetitive motor mannerisms, or “stimming,” were recognized by autistic people as being negatively judged by neurotypical people, making them feel devalued or “weird.”81 Autistic people have also reported that some autistic differences can be perceived as frightening to neurotypical people82 and that people sometimes associate autism with violent acts.33 Relatedly, students in the United States and Lebanon perceived disruptive autistic behaviors as more “dangerous” than withdrawn behaviors, which prompted greater stigmatization.14
Within our model (Fig. 1), we have indicated a covariance between public and professional understanding of autistic traits and expressed autistic traits. This is because the social model of disability recognizes the social construction within which autistic people exist, with poor understanding and attitudes from professionals and the public likely to affect expressed traits and possibly lead to elevated distress or discomfort for autistic people.83 Similarly, the way that an autistic person behaves will inform public and professional insights into autism.
Moderating factors
The quality and quantity of contact that autistic and neurotypical people have with one another is an important consideration. Knowing and spending time with an autistic person is associated with more positive attitudes toward autistic adults and children.11,48,53,84,85 It is important to consider the distinct contributions of both the quantity and quality of contact, with both dimensions associated with more positive attitudes54 and decreased stigma.86 However, quality of contact appears to be a more robust predictor of attitudes than quantity.54,86 This pattern of findings is congruent with data showing that people with autistic immediate family members have more positive attitudes,11 and less stigma toward autism.13,29
For neurotypical people, high-quality interactions may lead to decreased anxiety and increased comfort around autistic people, which lays the foundation for better understanding and, consequently, better attitudes toward autism.54 Similarly, high-quality interactions also support autistic people in feeling comfortable, which create better conditions for autistic people to be accurately understood. Conversely, lack of understanding and unfavorable attitudes about autism from neurotypical people may lead to negative social interactions (e.g., being unwelcoming) that impact the interactions of autistic people (e.g., displaying wariness), limiting opportunities for quality social connections and potentially exacerbating stigmatized views.28,87
The quality of contact may be influenced by the issue of “double empathy,” whereby autistic and neurotypical people are mutually challenged in their understanding of one another due to fundamental differences in how each understand the world.88,89 Autism is not associated with distinctive physical features; therefore, autistic people's “typical” appearance coupled with their unusual behaviors may elevate stigma, with autistic behaviors understood as social deviance rather than reflecting an underlying difference or difficulty.30,90 Overall, although more direct comparisons are required, existing research suggests that quality of contact has more impact than quantity.
Another important consideration is whether diagnostic disclosure may moderate how autistic people are perceived. The attribution model of stigma proposes that if a behavior is perceived as controllable, then negative reactions to a stigmatized individual will be greater as responsibility for their actions will be assumed.91 Related to this, the label of autism leads to more favorable first impressions of autistic people presented in video clips than when this label is not provided80,92 There is growing evidence that diagnostic disclosure can lead to more positive attitudes,55,93,94 more positive affective responses,95 greater acceptance of inappropriate social behaviors,96 as well as reduced stigma.97
However, these findings are not universal. For example, knowledge of diagnosis can have a negative impact on first impressions of autistic people for those with high autism stigma,98 whereas school children and adolescents do not modify their social distancing toward a fictional autistic peer when diagnosis is disclosed.99 A recent scoping review concluded that the fear of stigma was tied to the reluctance of autistic people to share their diagnosis,100 although concerns about judgment and misunderstanding have been attributed to both disclosing and not disclosing an autism diagnosis.33,101
The disconnect between experimental evidence of the positive impact of diagnostic disclosure and the lived experiences of autistic people warrants further exploration. One possible source of variance is the impact of preexisting autism knowledge or understanding on the effect of diagnostic disclosure, with findings currently mixed.92,95 It is also relevant that diagnostic disclosure may also affect how autistic people express themselves. A stronger autistic identity has been linked to a more open expression of autistic behaviors in everyday life, mediated by the extent to which the autistic person is open about their diagnosis.102 Further, autistic people may choose not to share their diagnosis in certain contexts,103 which means they may behave differently across environments.
Another possible moderator is cultural factors. People in the United States have been found to hold less stigma toward autistic people than those in Lebanon, Japan, and China. However, whereas people in China and Lebanon had a lower understanding of autism, people in Japan had a similar level of knowledge to the United States.50,104,105 This aligns with the idea that dominantly collectivist cultures, where group cohesion is biased over the needs of the individual, may be more susceptible to stigma due to more ready adoption of culturally defined norms.104 However, it is notable that an investigation of autism stigma in college students in Lebanon and the United States found that individual characteristics (e.g., previous contacts with autistic people) exerted a stronger influence on autism stigma than the country of residence.106
Cultural differences can clearly exert significant influence. In South Korea, the lay classification of “border children” recognizes children in mainstream schools who would be described as autistic by Western-trained clinicians.107 This label is partly driven by parental desire to avoid autism stigma, with the cultural importance of academic success supporting their child's “normalcy.”107 Parents in China have described that the cultural belief that respect for the father is related to the prospects of the son, can mean that parents do not want to disclose their son's autism.108
In other countries, the conceptualization of autism as something other than a developmental disorder can leave communities vulnerable to stigma. For example, in Vietnam, autism has been variously conceptualized as a disease, a “family problem,” and karmic demerit.109 In parts of Africa, autism has been attributed to supernatural phenomenon.110,111 These types of beliefs not only lead to significant stigma, such as autistic children being asked to leave public transport or families being unable to rent accommodation,112 but can also lead to inappropriate and sometimes dangerous “cures” by traditional healers.110,111
Cultural differences can also be perceived within a country among minority immigrant or indigenous communities. Somalian families in the United Kingdom report high levels of stigma toward their autistic children, leading to families hiding their child and delaying seeking support because challenging behaviors are not tolerated within their communities.113–116 There is prevalent autism stigma within Black American communities from diverse socioeconomic backgrounds, particularly related to denial and shame,117,118 as well as lower levels of autism acceptance in Asian American communities.119
Aboriginal and Torres Strait Island community members in Australia that have autistic family members also report a high degree of stigma.120 The experience of shame, which has strong cultural relevance, was commonly identified and linked with a reluctance to share the diagnosis. An additional challenge for minority groups is that autism stigma, which may have community-specific manifestations, is likely to interact with other stigma, such as those relating to religion, race, and ethnicity. Indeed, the starkest accounts of stigma by the Aboriginal and Torres Strait Island communities were related to interactions with non-Aboriginal people.120
In addition, Black American parents have reported experiencing racism, including negative assumptions about their autism knowledge and family circumstances, within the diagnostic process.117 More nuanced investigation is needed to better understand the impact of culture and community, both within and across countries, on the experience of stigma for autistic people and their families. This could include a direct exploration of whether there are contrasting experiences of autism stigma for families and autistic individuals within and outside of different community groups, and the extent to which additional forms of “otherness” may compound stigma.
Although cultural factors are more easily associated with their possible impact on public or professional perceptions and understanding, it is also true they may influence the expression of autistic traits. Reflecting this, there is modest evidence that the severity of some autistic traits may vary across some cultures.121
It is also important to consider the moderating effects of the sex and gender of autistic people. Though sometimes used interchangeably, sex focuses on the biological differences between males and females, whereas gender focuses on socially constructed roles, behaviors, and attributes.122 There is growing interest in delineating differences in the expression of autism based on sex and gender,122 but gender and sex norms may also affect the perceptions of autistic people by neurotypical people.
One qualitative study suggested that autistic females recognized pressure to fulfil gender stereotypes, including expected social skills, and that female groups were less forgiving of social “faux pas.”123 Similarly, in a mixed-methods study, autistic girls were more likely to feel like victims in friendship groups than autistic boys and neurotypical girls and boys, and felt punished for not “getting it” socially.124 These studies predict that autistic females would experience more stigma based on greater difficulty in aligning with gender norms.
From the parent perspective, mothers of autistic children may be more vulnerable to experiencing autism stigma than fathers, including avoidance, hostile staring, and rude remarks from the public.15 Again, this may relate to gender stereotypes, with a higher threshold of expectation set on mothers' parenting. Typically, studies that include gender do not consider the broader spectrum of gender presentations, including transgender and nonbinary, who are overrepresented in autistic populations,125,126 which is an important consideration for future research.
Consideration should also be given to wider individual differences beyond an autistic person's sex or gender. Individual differences related to the expression of autism are also relevant. For example, disruptive autistic behaviors lead to more stigma than withdrawn behaviors,14 and parents of violent or aggressive autistic children are more likely to encounter stigma.15 From a different perspective, the autism stigma experienced by families may be greater if their child's autism is less visible compared with children with more obvious additional needs, such as intellectual disability.15
In terms of individual differences among the public, there is converging evidence that females are less likely to have stigmatized views about autism,13,48,119 have higher levels of acceptance of autistic people,119 more positive attitudes,48 and greater willingness for social closeness with autistic people.13,50 Higher educational levels are also associated with higher levels of acceptance119 and lower levels of stigmatized views.127 However, education level is not a predictor in all studies.29,48 Age is generally not predictive of autism-related attitudes and stigma.29,48,119,127 Other relevant individual differences predictive of lower autism stigma include openness to experience, and decreased acceptance of inequality.106
The Impact of Stigma
The potential effect of stigma on autistic people and their families is wide ranging and has an overarching impact on well-being.3 Well-being is a multidimensional construct, with stable well-being occurring when individuals have the psychological, social, and physical resources to meet a particular psychological, social, and/or physical challenge.128 The insidious effects of stigma may erode at some of these resources, with deleterious consequences for well-being. As illustrated in Figure 1, stigma can affect well-being by influencing a range of factors, including mental health, physical health, and social connectedness.129–131 In addition, we consider the impact of stigma on behaviors adopted by autistic people to camouflage their behaviors, typically driven by a desire to “fit in.”132,133
Well-being
Recent research identified that greater awareness of stigmatized status was related to lower levels of psychological well-being in autistic adults.134 The lower social standing of stigmatized minority groups is believed to lead to exposure to more stressful life events, alongside fewer resources to manage these events.3 Autistic people have reported a wide range of stressors common to minority groups, including victimization, violence, discrimination, rejection, and felt stigma,3,35,135 which predicted heightened psychological distress, reduced well-being,3 and reduced quality of life.135 Relatedly, only 7% of autistic adults felt accepted as an autistic person within society, with feelings of acceptance protecting against depression.136 These findings are particularly relevant given the high prevalence of co-occurring mental health conditions in autistic people.137
Felt and enacted stigma can lead to reduced access to health care, with implications for both mental and physical health.138,139 For example, there is a suggestion that negative attitudes at university could stop autistic students from approaching support services.53 Stigma can also lead to a reluctance to disclose an autism diagnosis in health care settings,140–142 as well as in the workplace,143 despite disclosure often being necessary for appropriate care or support.142,143 Similarly, stigma can lead parents to resist a diagnosis for their child.144 Autistic people and family members have identified stigma and negative perceptions among health care professionals, alongside a lack of flexibility and unwillingness to make autism-specific adjustments.142 Therefore, stigma can affect the quality and appropriateness of health and social care received, with consequences for well-being.
The caregivers of autistic people are also adversely affected, with affiliate stigma correlated with anxiety and depression,37,145 poorer physical health,42 lower subjective well-being,146 and fewer working hours.39 A recent theoretical framework of the relationship between autism stigma and caregiver mental health suggests that there are both changeable factors (e.g., caregiver burden, self-blame, social isolation) and nonchangeable factors (e.g., culture, financial burden), both of which contribute to mental ill health and stigma.145
Aside from mental and physical health, the social connectedness that someone feels to their local and wider communities is also an important dimension of well-being.147 The stigma and misconceptions of the neurotypical majority can lead to autistic people becoming socially isolated.148 A dominant perception of autistic people is that they are not interested in social relationships.148 However, many autistic people have a desire for meaningful friendships and relationships but struggle to obtain them.149–151
Dissatisfaction with social support,19 less social contact,152 and less social connectedness153 have all been associated with the experience of loneliness for autistic people. In turn, loneliness has been associated with depression and anxiety for autistic people across multiple studies,131,152–154 as well as with poorer life satisfaction and self-esteem.131 In contrast, feelings of greater social connectedness, more time spent with friends, and greater levels of perceived social support have all been associated with better well-being among autistic college students.155 However, the heterogeneity of autism means that assumptions should not be made about the desire for social connectedness.
Those who want more social connectedness are arguably more likely or able to voice their social preferences, so it is easy to forget those who are more passive and retiring, including those who prefer aloneness and do not want intrusion. There should be understanding and acceptance of autistic people regardless of their social style or preferences.156
For family members, parents report friends asking them not to bring their autistic children to social gatherings or judging their parenting.157 More generally, parents can find reactions from members of the public difficult and have reported feeling embarrassed in public when their autistic child does not behave in a socially acceptable way.78 These experiences may partly explain why the degree of affiliate stigma associates negatively with participation in community events for parents of autistic children,158 as well as lead to social disconnection from family and friends.39 In summary, autism stigma can have negative effects on the mental and physical health of autistic people and their families, as well as leading to reduced social connectedness. These factors all contribute to reducing well-being within autistic communities.
Camouflaging
Stigma may also be a driver of the behaviors that autistic people choose to present to society, with a consequential impact on mental health and identity. Defined as “camouflaging,” some autistic people dampen down or mask their autistic traits to try and appear more neurotypical and better manage social situations.132,133 This relates to the concept of “compensation” in autism, whereby some autistic people show more “typical” social skills than their underlying social cognitive difficulties would predict.159–161
Compensating for underlying difficulties and camouflaging certain behaviors is mentally taxing and may result in fatigue,132,160,162 poorer mental health,130,133,140,162–164 educational underachievement,162 and suicidality.165 The drive to behave neurotypically can also delay diagnosis, not only delaying access to support but also making the autistic person vulnerable to stigma through being less well understood.92,95,96,157,166 Some motivations for camouflaging appear to reflect the pursuit of fulfilment, such as the desire for meaningful relationships.130,132,160 However, other behaviors often relate to societal norms, including the fear of rejection or bullying, a pressure to conform,160 and awareness of being in a “social minority.”167
Camouflaging has resonance with the concept of “concealment,” which is a way that stigmatized groups have protected themselves from discrimination.168 Recently, autistic people have described the camouflaging of their autism as a direct response to concerns about experiencing stigma,33,169 as well as feelings of shame, which reflects felt stigma.130 In this context, camouflaging behaviors have been described as a “normalising artifice” in which the stigma of autism is transformed into the mask of autism.170
Reflecting this, a greater perception of autism stigma was associated with greater camouflaging in a sample of autistic adults, which has been interpreted through Social Identity Theory as a way of associating with the higher-status neurotypical majority.134 However, although there is a relationship between a stronger autistic identity and reduced camouflaging, some autistic people experience an inconsistency; being proud of and strongly identifying as autistic while also camouflaging to fit in.130,134,162 Better understanding of this apparent paradox could be an important avenue for future research. In summary, there is converging evidence that camouflaging behaviors can have a deleterious effect on mental health, and they are tightly coupled with protecting the self from the negative consequences of autism stigma.
Reducing Stigma
There are various approaches that may reduce the stigma experienced by autistic people and their families, although there has been relatively little investigation into their effectiveness. In Figure 1, we have included examples of interventions that may bring positive change for the autistic community. For ease of illustration, we have focused the impact of the interventions on contributors to enacted stigma: public and professional understanding of autism and expressed autistic traits. However, these interventions are likely to have a wider impact on, and interact with, other components of the model.
Autism-friendly spaces
Autism-friendly spaces are ones in which the “person-environment” fit is enhanced,171–173 including making a space more socially comfortable (e.g., availability of a quiet room; agreed expectations about social interaction) or physically comfortable (e.g., appropriate lighting) alongside more generic adaptations such as improving the predictability of an environment. A relevant overarching approach is Universal Design, in which environments are developed as inclusive for all at their earliest conception, rather than being subsequently modified.174
Autistic people have reported that socializing can be particularly difficult when neurotypical family and friends do not consider their preferences, with some activities being inaccessible due to environmental challenges.167 Further, the inappropriateness of many school environments has been described as a barrier to inclusivity, including issues relating to unpredictability, sensory experiences, and social pressures.74,175
Adaptations to environments give more opportunities for neurotypical and autistic people to share spaces. Although yet to be empirically tested, we argue that autism-friendly spaces can improve understanding of and attitudes toward autism by enabling autistic people to better integrate with the wider community. Further, autism-friendly spaces are less likely to invoke distress, thus enabling autistic people to be their true selves. We argue that this will enhance the quality of interactions with autistic people, and consequently reduce stigma.54,106 Thus, although the driver of autism-friendly environments is to make spaces more comfortable for autistic people, there may be wider benefits relating to inclusivity and stigma reduction.
Increased inclusive media representation
Knowing someone with autism is associated with more positive attitudes toward autism11,48,53 and less stigma.11,13,29 This “knowing” of autistic people could be partly achieved by greater and better media representation. Negative reporting of autism is correlated with negative attitudes,176 but the media representation of autistic people is often negative.177–180 There has a been a call for more accuracy in portrayals of autism in the media, although achieving a balanced message is difficult given the heterogeneity of autism.181 Positive portrayals are also beneficial for autistic people and their families.144 Therefore, positive autistic role models and representation of the diversity of autistic experience are likely to improve understanding and reduce negative attitudes, ultimately reducing autism stigma. In addition, positive media representations may support autistic people in expressing themselves and reduce the need for camouflaging.
Educational and psychosocial training tools
Another approach is to formally educate the public and professionals about autism. Online training using PowerPoint has significantly increased knowledge and decreased stigma in students.13,50,182,183 However, it is unknown whether these positive changes would be sustained over time, nor whether the training would translate to real-life behaviors.
With respect to the impact of training on real life, a recent study investigated the effect of an autism acceptance training video on young adult males who subsequently engaged in a conversation with an autistic social partner.184 Both partners reported more interest in spending time with each other compared with dyads where the neurotypical partner had not had the training, suggesting that training had a relational effect. This supports a previous study where the video had a positive effect on reducing self-reported autism stigma in undergraduates.185 However, the positive effects of the video on real-life interactions did not extend to all measures of interaction quality,184 and the video did not affect an implicit bias toward associating autism with stigma-related attributes.185
For children, the “Understanding Our Peers with Pablo” program encompasses story books and animations to teach about autism and reduce autism stigma. It improved attitudes toward unfamiliar autistic peers but did not enhance attitudes toward familiar autistic peers compared with a control group.186 In addition, behavioral intentions were not improved and thus stigma still prevailed, which is consistent with previous research that has used a similar intervention with adolescents.187,188 Therefore, although studies addressing stigma can bring positive change, the outcome measure is an important consideration. An explicit shift in attitudes may not be a sufficient determinant of a more embedded change in implicit beliefs or behaviors.
A recent survey of neurotypical people found that knowledge of what it could be like to have autism predicated more positive attitudes toward autism.48 First-hand experience of an autistic perspective may help neurotypical people understand that their actions may align with an autistic person when they have similar experiences,189 reflecting the issue of double empathy. Technological innovations offer opportunities for providing this perspective. “Auti-Sim” is a simulation of sensory overload designed to give neurotypical people a first-person experience of the challenges that autistic people face.189
Using the simulation increased perspective taking compared with watching a simulated experience or reading a vignette, and heightened perspective taking was associated with greater emotional concern and helping intentions. However, there was no difference in explicit attitudes toward autism. Similar approaches include videos designed to illustrate the first-hand experiences of autistic people in their everyday lives, e.g., during a short walk.190
Looking forward, there may be mileage in drawing on existing resources that target the implicit, or unconscious, bias that individuals can hold toward marginalized groups.191,192 Further, comprehensive programs that include whole organizations, such as the Welsh Government's Learning with Autism whole-school training program,193 may engender greater attitude change due to the enhanced capacity for a cultural shift. Importantly, participatory input from autistic people in adapting an online training tool has led to the tool being more effective at changing autism knowledge, autism stigma, and attitudes toward inclusion, compared with a version of the training where there was no participation.182 This underlines the value of including autistic people in the development of training tools.
Neurodiversity
Arguably, autism stigma may be best reduced by a fundamental shift in the way autism is perceived by society. The neurodiversity movement celebrates autism for the differences it brings to society and for being an integral part of autistic people's identities, similar to race, sexuality, or nationality.29,194 The term “neurodiversity,” initially adopted by members of the autistic community,195 is now recognized by many other neurodivergent groups.196,197
Neurodiversity is encapsulated within the minority model of disability, which emerged as a direct challenge to the biomedical model of disability, with its focus on pathology and cure.3,194,198 A central tenant of the minority model is that society's restricted conceptualization of “normal” creates disability.3 It has close ties with a social-developmental account of autism that argues the development and well-being of autistic individuals is significantly shaped by misperceptions of the neurotypical majority.87 In essence, neurodiversity is the recognition of the range of natural diversity that is found within human development.199
Adopters of neurodiversity reject the medical model of autism as “deficit” in favor of autism as “difference,” which contributes positive diversity to society.29,194 Importantly, the onus on embracing neurodiversity should not be placed solely with autistic people and their families. Autistic people may feel more positive self-identification through identifying with neurodiversity, but the power of neurodiversity to engender meaningful societal change depends on its wide adoption. Recently, there has been a call to members of the autism research community to engage with the tenants of neurodiversity and bring about a paradigm shift in autism research.199
Having views aligned with the neurodiversity model is associated with lower stigma toward autistic people.29 Autistic identification is positively related to positive self-esteem, as well as lower levels of depression and anxiety.200 The neurodiversity movement aligns with the ownership that many autistic people have taken of language used to describe them, with endorsement of identity-first language.194,201,202 Identity-first language (e.g., autistic person) is considered less stigmatizing, partially because person-first language (e.g., person with autism) could imply the identity is shameful and partially because person-first language is not used in contexts outside of disability.33,202,203 However, not all autistic people or their families prefer identity-first language201 and differences in preference should be considered.
Alongside adoption of identity-first language, there has also been a call for researchers to avoid ableist language, which carries an implicit assumption that disabled people are inferior to others,204 and to adopt the term “autism spectrum condition” over the potentially more stigmatizing “autism spectrum disorder.”
It is important to note that identity with the autistic community can be ambivalent for some, with the benefit of finding a sense of belonging existing alongside internalization of the autism stigma.101,170 The visibility of positive autism messages is, therefore, key and the embracing of neurodiversity can be seen in narratives in which autistic people call for acceptance of autistic behaviors, such as stimming.81 Other activities to support neurodiversity include events that showcase the achievements of autistic people, particularly when designed by autistic people.190
The neurodiversity movement, therefore, has potential to improve public and professional understanding of autism, while also creating a culture where autistic people feel more able to express their true selves. It may also reduce the need to camouflage autistic behaviors, bringing co-occurring improvements in mental health.
Conclusion
Our synthesis of the literature has presented a model of autism stigma designed to promote understanding and further research of the difficulties people within the autistic community may face in finding acceptance. A truly nuanced exploration of autism stigma should take an intersectional approach, in which the wider social and cultural context and other forms of stigma can be accommodated.205 It is imperative that future autism sigma research includes participation from those with lived experience,29,199,206,207 not least because to leave the autistic community out of the research process perpetuates a “them” and “us” culture that reinforces stigma. Consideration must be given to including a diverse range of autistic community contributors, including those who may not typically engage with research.208
Importantly, we are not assigning responsibility to the autistic community for their stigma. Rather, we are reflecting theoretical understanding that the development of stigma is driven by the cultural framing of difference and the insidious effects of labeling this difference.8 For autism, decades of converging research support the reality of patterns of social communication differences and restricted and repetitive behaviors, which can cause challenges in everyday life. However, when we refer to a label as a “condition” or “disorder,” we are locating the referent in the stigmatized person, rather than recognizing that the label has evolved because of its social significance and as a product of social processes.8
There is clearly a value to labeling, not least because it creates a shorthand for society to recognize and address an individual's needs. However, by labeling a “difference,” ostensibly to provide support, we are creating challenges for the labeled. There is no easy solution to this conundrum.
An interesting counterpoint to this has been the neurodiversity movement and the reclaiming of identity by autistic people. Many autistic people are communicating that their autism “is” them and not something separate,202 which at face value is counter to approaches that advocate distancing from a stigmatized label.8 The neurodiversity movement may, therefore, support a shift in both the power and value of autism labels, with the potential to reduce autism stigma. In addition, neurodiversity may provide an important framework in which to develop a novel program to challenge and reduce felt stigma in autistic people.
Authorship Confirmation Statement
C.R.G.J. and A.T. were involved in the conceptualization of the article and wrote the original draft. C.R.G.J. led on the development of the model. K.L. reviewed and edited drafts of the article. All co-authors have reviewed and approved of the article before submission. The article has been submitted solely to this journal and is not published, in press, or submitted elsewhere.
Acknowledgments
Thank you to Professor Sue Leekam for helpful comments on an earlier draft.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
The authors did not receive any funding for this review.
References
- 1. Major B, Dovidio JF, Link BG, Calabrese SK. Stigma and its implications for health: Introduction and overview. In: Major B, Dovidio JF, Link BG, eds. The Oxford Handbook of Stigma, Discrimination, and Health, New York: Oxford University Press; 2018;3–28. [Google Scholar]
- 2. Oyserman D, Swim JK. Stigma: An insider's view. J Soc Issues. 2001;57(1):1–14. [Google Scholar]
- 3. Botha M, Frost DM. Extending the minority stress model to understand mental health problems experienced by the autistic population. Soc Ment Health. 2020;10(1):20–34. [Google Scholar]
- 4. Bachmann CJ, Höfer J, Kamp-Becker I, et al. . Internalised stigma in adults with autism: A German multi-center survey. Psychiatry Res. 2019;276:94–99. [DOI] [PubMed] [Google Scholar]
- 5. Goffman E. Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs, NJ: Prentice Hall; 1963. [Google Scholar]
- 6. Shtayermman O. An exploratory study of the stigma associated with a diagnosis of Asperger's syndrome: The mental health impact on the adolescents and young adults diagnosed with a disability with a social nature. J Hum Behav Soc Environ. 2009;19(3):298–313. [Google Scholar]
- 7. Thornicroft G, Rose D, Kassam A, Sartorius N. Stigma: Ignorance, prejudice or discrimination? Br J Psychiatry. 2007;190(3):192–193. [DOI] [PubMed] [Google Scholar]
- 8. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27(1):363–385. [Google Scholar]
- 9. Greenwald AG, Banaji MR. Implicit social cognition: Attitudes, self-esteem, and stereotypes. Psychol Rev. 1995;102(1):4–27. [DOI] [PubMed] [Google Scholar]
- 10. Flood LN, Bulgrin A, Morgan BL. Piecing together the puzzle: Development of the societal attitudes towards autism (SATA) scale. J Res Spec Educ Needs. 2013;13(2):121–128. [Google Scholar]
- 11. Nevill REA, White SW. College students' openness toward autism spectrum disorders: Improving peer acceptance. J Autism Dev Disord. 2011;41(12):1619–1628. [DOI] [PubMed] [Google Scholar]
- 12. Harnum M, Duffy J, Ferguson DA. Adults' versus children's perceptions of a child with autism or attention deficit hyperactivity disorder. J Autism Dev Disord. 2007;37(7):1337–1343. [DOI] [PubMed] [Google Scholar]
- 13. Gillespie-Lynch K, Brooks PJ, Someki F, et al. . Changing college students' conceptions of autism: An online training to increase knowledge and decrease stigma. J Autism Dev Disord. 2015;45(8):2553–2566. [DOI] [PubMed] [Google Scholar]
- 14. Gillespie-Lynch K, Daou N, Obeid R, Reardon S, Khan S, Goldknopf EJ. What contributes to stigma towards autistic university students and students with other diagnoses? J Autism Dev Disord. 2021(51):459–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gray DE. ‘Everybody just freezes. Everybody is just embarrassed’: Felt and enacted stigma among parents of children with high functioning autism. Sociol Health Illn. 2002;24(6):734–749. [Google Scholar]
- 16. Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. 2002;1(1):16. [PMC free article] [PubMed] [Google Scholar]
- 17. Jacoby A. Felt versus enacted stigma—A concept revisited—Evidence from a study of people with epilepsy in remission. Soc Sci Med. 1994;38(2):269–274. [DOI] [PubMed] [Google Scholar]
- 18. Bauminger N, Kasari C. Loneliness and friendship in high-functioning children with autism. Child Dev. 2000;71(2):447–456. [DOI] [PubMed] [Google Scholar]
- 19. Ee D, Hwang YI, Reppermund S, et al. . Loneliness in adults on the autism spectrum. Autism Adulthood. 2019;1:182–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Petrina N, Carter M, Stephenson J. The nature of friendship in children with autism spectrum disorders: A systematic review. Res Autism Spectr Disord. 2014;8(2):111–126. [Google Scholar]
- 21. Rowley E, Chandler S, Baird G, et al. . The experience of friendship, victimization and bullying in children with an autism spectrum disorder: Associations with child characteristics and school placement. Res Autism Spectr Disord. 2012;6(3):1126–1134. [Google Scholar]
- 22. Brede J, Remington A, Kenny L, Warren K, Pellicano E. Excluded from school: Autistic students' experiences of school exclusion and subsequent re-integration into school. Autism Dev Lang Impair. 2017;2:1–20. [Google Scholar]
- 23. Shattuck PT, Narendorf SC, Cooper B, Sterzing PR, Wagner M, Taylor JL. Postsecondary education and employment among youth with an autism spectrum disorder. Pediatrics. 2012;129(6):1042–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Black MH, Mahdi S, Milbourn B, et al. . Multi-informant international perspectives on the facilitators and barriers to employment for autistic adults. Autism Res. 2020;13(7):1195–1214. [DOI] [PubMed] [Google Scholar]
- 25. Billstedt E, Gillberg C, Gillberg C. Autism after adolescence: Population-based 13-to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. J Autism Dev Disord. 2005;35(3):351–360. [DOI] [PubMed] [Google Scholar]
- 26. Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. J Child Psychol Psychiatry. 2004;45(2):212–229. [DOI] [PubMed] [Google Scholar]
- 27. Tobin MC, Drager KDR, Richardson LF. A systematic review of social participation for adults with autism spectrum disorders: Support, social functioning, and quality of life. Res Autism Spectr Disord. 2014;8(3):214–229. [Google Scholar]
- 28. Sasson NJ, Faso DJ, Nugent J, Lovell S, Kennedy DP, Grossman RB. Neurotypical peers are less willing to interact with those with autism based on thin slice judgments. Sci Rep. 2017;7:40700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gillespie-Lynch K, Kapp SK, Brooks PJ, Pickens J, Schwartzman B. Whose expertise is it? Evidence for autistic adults as critical autism experts. Front Psychol. 2017;8:438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Huws JC, Jones RSP. ‘They just seem to live their lives in their own little world’: Lay perceptions of autism. Disabil Soc. 2010;25(3):331–344. [Google Scholar]
- 31. Jensen CM, Martens CS, Nikolajsen ND, et al. . What do the general population know, believe and feel about individuals with autism and schizophrenia: Results from a comparative survey in Denmark. Autism. 2016;20(4):496–508. [DOI] [PubMed] [Google Scholar]
- 32. Cage E, Di Monaco J, Newell V. Understanding, attitudes and dehumanisation towards autistic people. Autism. 2018;23(6):1373–1383. [DOI] [PubMed] [Google Scholar]
- 33. Botha M, Dibb B, Frost DM. “Autism is me”: An investigation of how autistic individuals make sense of autism and stigma. Disabil Soc. 2020:1–27. 10.1080/09687599.2020.1822782. [DOI] [Google Scholar]
- 34. Brownlow C, Lawson W, Pillay Y, Mahony J, Abawi D. “Just ask me”: The importance of respectful relationships within schools. Front Psychol. 2021;12:678264. 10.3389/fpsyg.2021.678264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mantzalas J, Richdale AL, Adikari A, Lowe J, Dissanayake C.. What is autistic burnout? A thematic analysis of posts on two online platforms. Autism Adulthood. 2021. 10.1089/aut.2021.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Oti-Boadi M, Dankyi E, Kwakye-Nuako CO. Stigma and forgiveness in ghanaian mothers of children with autism spectrum disorders (ASD). J Autism Dev Disord. 2020;50(4):1391–1400. [DOI] [PubMed] [Google Scholar]
- 37. Öz B, Yüksel T, Nasiroğlu S. Depression-anxiety symptoms and stigma perception in mothers of children with autism spectrum disorder. Arch Neuropsychiatry. 2020;57(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zuckerman KE, Lindly OJ, Reyes NM, et al. . Parent perceptions of community autism spectrum disorder stigma: Measure validation and associations in a multi-site sample. J Autism Dev Disord. 2018;48(9):3199–3209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kinnear SH, Link BG, Ballan MS, Fischbach RL. Understanding the experience of stigma for parents of children with autism spectrum disorder and the role stigma plays in families' lives. J Autism Dev Disord. 2016;46(3):942–953. [DOI] [PubMed] [Google Scholar]
- 40. Liao X, Lei X, Li Y. Stigma among parents of children with autism: A literature review. Asian J Psychiatr. 2019;45:88–94. [DOI] [PubMed] [Google Scholar]
- 41. Mitter N, Ali A, Scior K. Stigma experienced by families of individuals with intellectual disabilities and autism: A systematic review. Res Dev Disabil. 2019;89:10–21. [DOI] [PubMed] [Google Scholar]
- 42. Song J, Mailick MR, Greenberg JS. Health of parents of individuals with developmental disorders or mental health problems: Impacts of stigma. Soc Sci Med. 2018;217:152–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lovell B, Wetherell MA. Affiliate stigma, perceived social support and perceived stress in caregivers of children with autism spectrum disorder: A multiple mediation study. Arch Psychiatr Nurs. 2019;33(5):31–35. [DOI] [PubMed] [Google Scholar]
- 44. Broady TR, Stoyles GJ, Morse C. Understanding carers' lived experience of stigma: The voice of families with a child on the autism spectrum. Health Soc Care Community. 2017;25(1):224–233. [DOI] [PubMed] [Google Scholar]
- 45. Lovell B, Wetherell MA. Caregivers' characteristics and family constellation variables as predictors of affiliate stigma in caregivers of children with ASD. Psychiatry Res. 2018;270:426–429. [DOI] [PubMed] [Google Scholar]
- 46. Jansen-van Vuuren J, Aldersey HM. Stigma, acceptance and belonging for people with IDD across cultures. Curr Dev Disord Rep. 2020;7(3):163–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Harrison AJ, Bradshaw LP, Naqvi NC, Paff ML, Campbell JM. Development and psychometric evaluation of the Autism Stigma and Knowledge Questionnaire (ASK-Q). J Autism Dev Disord. 2017;47(10):3281–3295. [DOI] [PubMed] [Google Scholar]
- 48. Kuzminski R, Netto J, Wilson J, Falkmer T, Chamberlain A, Falkmer M. Linking knowledge and attitudes: Determining neurotypical knowledge about and attitudes towards autism. PLoS One. 2019;14(7):e0220197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ling CYM, Mak WWS, Cheng JNS. Attribution model of stigma towards children with autism in Hong Kong. J Appl Res Intellect Disabil. 2010;23(3):237–249. [Google Scholar]
- 50. Obeid R, Daou N, DeNigris D, Shane-Simpson C, Brooks PJ, Gillespie-Lynch K. A cross-cultural comparison of knowledge and stigma associated with autism spectrum disorder among college students in Lebanon and the United States. J Autism Dev Disord. 2015;45(11):3520–3536. [DOI] [PubMed] [Google Scholar]
- 51. Kitchin JL, Karlin NJ. Awareness and stigma of autism spectrum disorders in undergraduate students. Psychol Rep. 2021. [Epub ahead of print]; DOI: 10.1177/00332941211014144. [DOI] [PubMed] [Google Scholar]
- 52. Mac Cárthaigh S, López B. Factually based autism awareness campaigns may not always be effective in changing attitudes towards autism: Evidence from British and South Korean nursing students. Autism. 2020;24(5):1177–1190. [DOI] [PubMed] [Google Scholar]
- 53. White D, Hillier A, Frye A, Makrez E. College students' knowledge and attitudes towards students on the autism spectrum. J Autism Dev Disord. 2019;49(7):2699–2705. [DOI] [PubMed] [Google Scholar]
- 54. Gardiner E, Iarocci G. Students with autism spectrum disorder in the university context: Peer acceptance predicts intention to volunteer. J Autism Dev Disord. 2014;44(5):1008–1017. [DOI] [PubMed] [Google Scholar]
- 55. Matthews NL, Ly AR, Goldberg WA. College students' perceptions of peers with autism spectrum disorder. J Autism Dev Disord. 2015;45(1):90–99. [DOI] [PubMed] [Google Scholar]
- 56. van ‘t Hof M, van Berckelaer-Onnes I, Deen M, et al. . Novel insights into autism knowledge and stigmatizing attitudes toward mental illness in Dutch youth and family center physicians. Community Ment Health J. 2020;56(7):1318–1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Tipton LA, Blacher J. Brief report: Autism awareness: Views from a campus community. J Autism Dev Disord. 2014;44(2):477–483. [DOI] [PubMed] [Google Scholar]
- 58. Mitchell GE, Locke KD. Lay beliefs about autism spectrum disorder among the general public and childcare providers. Autism. 2015;19(5):553–561. [DOI] [PubMed] [Google Scholar]
- 59. Wood C, Freeth M. Students' stereotypes of autism. J Educ Issues. 2016;2:131. [Google Scholar]
- 60. Heidgerken AD, Geffken G, Modi A, Frakey L. A survey of autism knowledge in a health care setting. J Autism Dev Disord. 2005;35(3):323–330. [DOI] [PubMed] [Google Scholar]
- 61. Plumb AM, Plexico LW. Autism spectrum disorders: Experience, training, and confidence levels of school-based speech-language pathologists. Lang Speech Hear Serv Sch. 2013;44(1):89–104. [DOI] [PubMed] [Google Scholar]
- 62. Khanna R, Jariwala K, Holmes ER, Ramachandran S. Autism familiarity and knowledge among pharmacy students. Curr Pharm Teach Learn. 2014;6(1):150–157. [Google Scholar]
- 63. Zerbo O, Massolo ML, Qian Y, Croen LA. A study of physician knowledge and experience with autism in adults in a large integrated healthcare system. J Autism Dev Disord. 2015;45(12):4002–4014. [DOI] [PubMed] [Google Scholar]
- 64. Crane L, Davidson I, Prosser R, Pellicano E. Understanding psychiatrists' knowledge, attitudes and experiences in identifying and supporting their patients on the autism spectrum: Online survey. BJPsych Open. 2019;5(3):e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Bono LK, Haverkamp CR, Lindsey RA, Freedman RN, McClain MB, Simonsmeier V. Assessing interdisciplinary trainees' objective and self-reported knowledge of autism spectrum disorder and confidence in providing services. J Autism Dev Disord. 2022;52(1):376–391. [DOI] [PubMed] [Google Scholar]
- 66. Unigwe S, Buckley C, Crane L, Kenny L, Remington A, Pellicano E. GPs' confidence in caring for their patients on the autism spectrum: An online self-report study. Br J Gen Pract. 2017;67(659):e445–e452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Al-Sharbati MM, Al-Farsi YM, Ouhtit A, et al. . Awareness about autism among school teachers in Oman: A cross-sectional study. Autism. 2015;19(1):6–13. [DOI] [PubMed] [Google Scholar]
- 68. Haimour AI, Obaidat YF. School teachers' knowledge about autism in Saudi Arabia. World J Educ. 2013;3(5):45–56. [Google Scholar]
- 69. Sanz-Cervera P, Fernández-Andrés M-I, Pastor-Cerezuela G, Tárraga-Mínguez R. Pre-service teachers' knowledge, misconceptions and gaps about autism spectrum disorder. Teach Educ Spec Educ. 2017;40(3):212–224. [Google Scholar]
- 70. Schwartz H, Drager KDR. Training and knowledge in autism among speech-language pathologists: A survey. Lang Speech Hear Serv Sch. 2008;39(1):66–77. [DOI] [PubMed] [Google Scholar]
- 71. Young K, Mannix McNamara P, Coughlan B. Post-primary school teachers' knowledge and understanding of autism spectrum disorders. Irish Educ Stud. 2017;36(3):399–422. [Google Scholar]
- 72. Ballantyne C, Gillespie-Smith K, Wilson C. A comparison of knowledge and experience of autism spectrum disorder among teachers in the United Kingdom and China. Intl J Disabil Dev Educ. 2019;68(8):1–12. [Google Scholar]
- 73. Segall MJ, Campbell JM. Factors relating to education professionals' classroom practices for the inclusion of students with autism spectrum disorders. Res Autism Spectr Disord. 2012;6(3):1156–1167. [Google Scholar]
- 74. Goodall C. ‘I felt closed in and like I couldn't breathe’: A qualitative study exploring the mainstream educational experiences of autistic young people. Autism Dev Lang Impair. 2018;3:2396941518804407. [Google Scholar]
- 75. Dillenburger K, McKerr L, Jordan J-A, Keenan M. Staff training in autism: The one-eyed wo/man…. Int J Environ Res Public Health. 2016;13(7):716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM-5). Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 77. Schaaf RC, Toth-Cohen S, Johnson SL, Outten G, Benevides TW. The everyday routines of families of children with autism: Examining the impact of sensory processing difficulties on the family. Autism. 2011;15(3):373–389. [DOI] [PubMed] [Google Scholar]
- 78. Ryan S. ‘Meltdowns’, surveillance and managing emotions; going out with children with autism. Health Place. 2010;16(5):868–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Grossman RB. Judgments of social awkwardness from brief exposure to children with and without high-functioning autism. Autism. 2015;19(5):580–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. DeBrabander KM, Morrison KE, Jones DR, Faso DJ, Chmielewski M, Sasson NJ. Do first impressions of autistic adults differ between autistic and nonautistic observers? Autism Adulthood. 2019;1(4):250–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Kapp SK, Steward R, Crane L, et al. . ‘People should be allowed to do what they like’: Autistic adults' views and experiences of stimming. Autism. 2019;23(7):1782–1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Jones R, Quigney C, Huws J. First-hand accounts of sensory perceptual experiences in autism: A qualitative analysis. J Autism Dev Disord. 2003;28(2):112–121. [Google Scholar]
- 83. Barnes C. Understanding the social model of disability: Past, present and future. In: Watson N, Vehmas S, eds. Routledge Handbook of Disability Studies. London: Routledge; 2019;14–31. [Google Scholar]
- 84. Dachez J, Ndobo A, Ameline A. French validation of the multidimensional attitude scale toward persons with disabilities (MAS): The case of attitudes toward autism and their moderating factors. J Autism Dev Disord. 2015;45(8):2508–2518. [DOI] [PubMed] [Google Scholar]
- 85. Cook A, Ogden J, Winstone N. The effect of school exposure and personal contact on attitudes towards bullying and autism in schools: A cohort study with a control group. Autism. 2020;24(8):2178–2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Kim SY. College disability service office staff members' autism attitudes and knowledge. Remedial Spec Educ. 2021;43(1):15–26. [Google Scholar]
- 87. Mitchell P, Sheppard E, Cassidy S. Autism and the double empathy problem: Implications for development and mental health. Br J Dev Psychol. 2021;39(1):1–18. [DOI] [PubMed] [Google Scholar]
- 88. Milton DEM. On the ontological status of autism: The ‘double empathy problem’. Disabil Soc. 2012;27(6):883–887. [Google Scholar]
- 89. Crompton CJ, Sharp M, Axbey H, Fletcher-Watson S, Flynn EG, Ropar D. Neurotype-matching, but not being autistic, influences self and observer ratings of interpersonal rapport. Front Psychol. 2020;11:586171. 10.3389/fpsyg.2020.586171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Gray DE. Perceptions of stigma: The parents of autistic children. Sociol Health Illn. 1993;15(1):102–120. [Google Scholar]
- 91. Corrigan P, Markowitz FE, Watson A, Rowan D, Kubiak MA. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. 2003;44(2):162–179. [PubMed] [Google Scholar]
- 92. Sasson NJ, Morrison KE. First impressions of adults with autism improve with diagnostic disclosure and increased autism knowledge of peers. Autism. 2019;23(1):50–59. [DOI] [PubMed] [Google Scholar]
- 93. Austin JE, Zinke VL, Davies WH. Influencing perception about children with autism and their parents using disclosure cards. J Autism Dev Disord. 2016;46(8):2764–2769. [DOI] [PubMed] [Google Scholar]
- 94. Austin JE, Galijot R, Davies WH. Evaluating parental Autism disclosure strategies. J Autism Dev Disord. 2018;48(1):103–109. [DOI] [PubMed] [Google Scholar]
- 95. Brosnan M, Mills E. The effect of diagnostic labels on the affective responses of college students towards peers with ‘Asperger's Syndrome'and ‘Autism Spectrum Disorder’. Autism. 2016;20(4):388–394. [DOI] [PubMed] [Google Scholar]
- 96. Mogavero MC, Hsu K-H. Autism spectrum disorder and harassment: An application of attribution theory. Int J Criminol Sociol. 2018;7:260–274. [Google Scholar]
- 97. O'Connor C, Burke J, Rooney B. Diagnostic disclosure and social marginalisation of adults with ASD: Is there a relationship and what mediates it? J Autism Dev Disord. 2020;50(9):3367–3379. [DOI] [PubMed] [Google Scholar]
- 98. Morrison KE, DeBrabander KM, Faso DJ, Sasson NJ. Variability in first impressions of autistic adults made by neurotypical raters is driven more by characteristics of the rater than by characteristics of autistic adults. Autism. 2019;23(7):1817–1829. [DOI] [PubMed] [Google Scholar]
- 99. White R, Barreto M, Harrington J, Kapp SK, Hayes J, Russell G. Is disclosing an autism spectrum disorder in school associated with reduced stigmatization? Autism. 2020;24(3):744–754. [DOI] [PubMed] [Google Scholar]
- 100. Thompson-Hodgetts S, Labonte C, Mazumder R, Phelan S. Helpful or harmful? A scoping review of perceptions and outcomes of autism diagnostic disclosure to others. Res Autism Spectr Disord. 2020;77:101598. [Google Scholar]
- 101. Frost KM, Bailey KM, Ingersoll BR. “I just want them to see me as…me”: Identity, community, and disclosure practices among college students on the autism spectrum. Autism Adulthood. 2020;1(4):268–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Cage E, Troxell-Whitman Z. Understanding the relationships between autistic identity, disclosure, and camouflaging. Autism Adulthood. 2020;2:334–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Johnson TD, Joshi A. Dark clouds or silver linings? A stigma threat perspective on the implications of an autism diagnosis for workplace well-being. J Appl Psychol. 2016;101(3):430–449. [DOI] [PubMed] [Google Scholar]
- 104. Someki F, Torii M, Brooks PJ, Koeda T, Gillespie-Lynch K. Stigma associated with autism among college students in Japan and the United States: An online training study. Res Dev Disabil. 2018;76:88–98. [DOI] [PubMed] [Google Scholar]
- 105. Yu L, Stronach S, Harrison AJ. Public knowledge and stigma of autism spectrum disorder: Comparing China with the United States. Autism. 2020;24(6):1531–1545. [DOI] [PubMed] [Google Scholar]
- 106. Gillespie-Lynch K, Daou N, Sanchez-Ruiz M-J, et al. . Factors underlying cross-cultural differences in stigma toward autism among college students in Lebanon and the United States. Autism. 2019;23(8):1993–2006. [DOI] [PubMed] [Google Scholar]
- 107. Grinker RR, Cho K. Border children: Interpreting autism spectrum disorder in South Korea. Ethos. 2013;41(1):46–74. [Google Scholar]
- 108. McCabe H. Parent advocacy in the face of adversity: Autism and families in the People's Republic of China. Focus Autism Other Dev Disabl. 2007;22(1):39–50. [Google Scholar]
- 109. Ha VS, Whittaker A, Whittaker M, Rodger S. Living with autism spectrum disorder in Hanoi, Vietnam. Soc Sci Med. 2014;120:278–285. [DOI] [PubMed] [Google Scholar]
- 110. Sangare M, Dembele B, Toure A, et al. . Autism seminary for public engagement: Evaluation of knowledge and attitudes of traditional medical practitioners in Mali [version 1; peer review: 1 approved, 1 approved with reservations, 1 not approved]. AAS Open Res. 2019;2(21). 10.12688/aasopenres.12955.1. [DOI] [Google Scholar]
- 111. Tilahun D, Hanlon C, Fekadu A, Tekola B, Baheretibeb Y, Hoekstra RA. Stigma, explanatory models and unmet needs of caregivers of children with developmental disorders in a low-income African country: A cross-sectional facility-based survey. BMC Health Serv Res. 2016;16:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Tekola B, Baheretibeb Y, Roth I, et al. . Challenges and opportunities to improve autism services in low-income countries: Lessons from a situational analysis in Ethiopia. Glob Ment Health. 2016;3:e21., 1–11. 10.1017/gmh.2016.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Ellen Selman L, Fox F, Aabe N, Turner K, Rai D, Redwood S. ‘You are labelled by your children's disability’—A community-based, participatory study of stigma among Somali parents of children with autism living in the United Kingdom. Ethn Health. 2018;23(7):781–796. [DOI] [PubMed] [Google Scholar]
- 114. Sritharan B, Koola MM. Barriers faced by immigrant families of children with autism: A program to address the challenges. Asian J Psychiatr. 2019;39:53–57. [DOI] [PubMed] [Google Scholar]
- 115. Hussein AM, Pellicano E, Crane L. Understanding and awareness of autism among Somali parents living in the United Kingdom. Autism. 2019;23(6):1408–1418. [DOI] [PubMed] [Google Scholar]
- 116. Fox F, Aabe N, Turner K, Redwood S, Rai D. “It was like walking without knowing where I was going”: A qualitative study of autism in a UK Somali Migrant Community. J Autism Dev Disord. 2017;47(2):305–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Dababnah S, Shaia WE, Campion K, Nichols HM. “We had to keep pushing”: Caregivers' perspectives on autism screening and referral practices of black children in primary care. Intellect Dev Disabil. 2018;56(5):321–336. [DOI] [PubMed] [Google Scholar]
- 118. Burkett K, Morris E, Manning-Courtney P, Anthony J, Shambley-Ebron D. African American families on autism diagnosis and treatment: The influence of culture. J Autism Dev Disord. 2015;45(10):3244–3254. [DOI] [PubMed] [Google Scholar]
- 119. Kim SY. The Development and pilot-testing of the autism attitude acceptance scale: An instrument measuring autism acceptance. Autism Adulthood. 2020;2:204–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Lilley R, Sedgwick M, Pellicano E. Inclusion, acceptance, shame and isolation: Attitudes to autism in aboriginal and Torres Strait islander communities in Australia. Autism. 2020;24(7):1860–1873. [DOI] [PubMed] [Google Scholar]
- 121. de Leeuw A, Happé F, Hoekstra RA. A conceptual framework for understanding the cultural and contextual factors on autism across the globe. Autism Res. 2020;13(7):1029–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Lai MC, Lombardo MV, Auyeung B, Chakrabarti B, Baron-Cohen S. Sex/gender differences and autism: Setting the scene for future research. J Am Acad Child Adolesc Psychiatry. 2015;54(1):11–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Bargiela S, Steward R, Mandy W. The experiences of late-diagnosed women with autism spectrum conditions: An investigation of the female autism phenotype. J Autism Dev Disord. 2016;46(10):3281–3294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Sedgewick F, Hill V, Pellicano E. ‘It's different for girls’: Gender differences in the friendships and conflict of autistic and neurotypical adolescents. Autism. 2018;23(5):1119–1132. [DOI] [PubMed] [Google Scholar]
- 125. Van Der Miesen AIR, Hurley H, De Vries ALC. Gender dysphoria and autism spectrum disorder: A narrative review. Int Rev Psychiatry. 2016;28(1):70–80. [DOI] [PubMed] [Google Scholar]
- 126. Glidden D, Bouman WP, Jones BA, Arcelus J. Gender dysphoria and autism spectrum disorder: A systematic review of the literature. Sex Med Rev. 2016;4(1):3–14. [DOI] [PubMed] [Google Scholar]
- 127. Stronach S, Wiegand S, Mentz E. Brief report: Autism knowledge and stigma in university and community samples. J Autism Dev Disord. 2019;49(3):1298–1302. [DOI] [PubMed] [Google Scholar]
- 128. Dodge R, Daly AP, Huyton J, Sanders LD. The challenge of defining wellbeing. Int J Wellbeing. 2012;2(3):222–235. [Google Scholar]
- 129. Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet. 2015;385(9968):640–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Cage E, Troxell-Whitman Z. Understanding the reasons, contexts and costs of camouflaging for autistic adults. J Autism Dev Disord. 2019;49(5):1899–1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Mazurek MO. Loneliness, friendship, and well-being in adults with autism spectrum disorders. Autism. 2014;18(3):223–232. [DOI] [PubMed] [Google Scholar]
- 132. Hull L, Petrides KV, Allison C, et al. . “Putting on my best normal”: Social camouflaging in adults with autism spectrum conditions. J Autism Dev Disord. 2017;47(8):2519–2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Lai M-C, Lombardo MV, Ruigrok ANV, et al. . Quantifying and exploring camouflaging in men and women with autism. Autism. 2017;21(6):690–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Perry E, Mandy W, Hull L, Cage E. Understanding camouflaging as a response to autism-related stigma: A social identity theory approach. J Autism Dev Disord. 2021;52:800–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Caron V, Jeanneret N, Giroux M, et al. . Sociocultural context and autistics' quality of life: A comparison between Québec and France. Autism. 2021. [Epub ahead of print]; DOI: 10.1177/13623613211035229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Cage E, Di Monaco J, Newell V. Experiences of autism acceptance and mental health in autistic adults. J Autism Dev Disord. 2018;48(2):473–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Lai M-C, Kassee C, Besney R, et al. . Prevalence of co-occurring mental health diagnoses in the autism population: A systematic review and meta-analysis. Lancet Psychiatry. 2019;6(10):819–829. [DOI] [PubMed] [Google Scholar]
- 138. Earnshaw VA, Quinn DM. The impact of stigma in healthcare on people living with chronic illnesses. J Health Psychol. 2012;17(2):157–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry. 2010;10:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Crane L, Adams F, Harper G, Welch J, Pellicano E. ‘Something needs to change’: Mental health experiences of young autistic adults in England. Autism. 2019;23(2):477–493. [DOI] [PubMed] [Google Scholar]
- 141. Nicolaidis C, Raymaker D, McDonald K, et al. . Comparison of healthcare experiences in autistic and non-autistic adults: A cross-sectional online survey facilitated by an academic-community partnership. J Gen Intern Med. 2013;28(6):761–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Walsh C, Lydon S, O'Dowd E, O'Connor P. Barriers to healthcare for persons with autism: A systematic review of the literature and development of a taxonomy. Dev Neurorehabil. 2020;23(7):413–430. [DOI] [PubMed] [Google Scholar]
- 143. Romualdez AM, Heasman B, Walker Z, Davies J, Remington A. “People might understand me better”: Diagnostic disclosure experiences of autistic individuals in the workplace. Autism Adulthood. 2021;3(2):157–167. [Google Scholar]
- 144. Russell G, Norwich B. Dilemmas, diagnosis and de-stigmatization: Parental perspectives on the diagnosis of autism spectrum disorders. Clin Child Psychol Psychiatry. 2012;17(2):229–245. [DOI] [PubMed] [Google Scholar]
- 145. Papadopoulos C, Lodder A, Constantinou G, Randhawa G. Systematic review of the relationship between autism stigma and informal caregiver mental health. J Autism Dev Disord. 2019;49(4):1665–1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Werner S, Shulman C. Subjective well-being among family caregivers of individuals with developmental disabilities: The role of affiliate stigma and psychosocial moderating variables. Res Dev Disabil. 2013;34(11):4103–4114. [DOI] [PubMed] [Google Scholar]
- 147. Linton M-J, Dieppe P, Medina-Lara A. Review of 99 self-report measures for assessing well-being in adults: Exploring dimensions of well-being and developments over time. BMJ Open. 2016;6(7):e010641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. John RPS, Knott FJ, Harvey KN. Myths about autism: An exploratory study using focus groups. Autism. 2018;22(7):845–854. [DOI] [PubMed] [Google Scholar]
- 149. Jaswal VK, Akhtar N. Being versus appearing socially uninterested: Challenging assumptions about social motivation in autism. Behav Brain Sci. 2019;42:e82., 1–73. 10.1017/S0140525X18001826. [DOI] [PubMed] [Google Scholar]
- 150. Müller E, Schuler A, Yates GB. Social challenges and supports from the perspective of individuals with Asperger syndrome and other autism spectrum disabilities. Autism. 2008;12(2):173–190. [DOI] [PubMed] [Google Scholar]
- 151. Skafle I, Nordahl-Hansen A, Øien RA. Short report: Social perception of high school students with ASD in Norway. J Autism Dev Disord. 2020;50(2):670–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Schiltz HK, McVey AJ, Dolan Wozniak B, et al. . The role of loneliness as a mediator between autism features and mental health among autistic young adults. Autism. 2021;25(2):545–555. [DOI] [PubMed] [Google Scholar]
- 153. Stice LV, Lavner JA. Social connectedness and loneliness mediate the association between autistic traits and internalizing symptoms among young adults. J Autism Dev Disord. 2019;49(3):1096–1110. [DOI] [PubMed] [Google Scholar]
- 154. Han GT, Tomarken AJ, Gotham KO. Social and nonsocial reward moderate the relation between autism symptoms and loneliness in adults with ASD, depression, and controls. Autism Res. 2019;12(6):884–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Bailey KM, Frost KM, Casagrande K, Ingersoll B. The relationship between social experience and subjective well-being in autistic college students: A mixed methods study. Autism. 2020;24(5):1081–1092. [DOI] [PubMed] [Google Scholar]
- 156. Scheeren AM, Koot HM, Begeer S. Stability and change in social interaction style of children with autism spectrum disorder: A 4-year follow-up study. Autism Res. 2020;13(1):74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Farrugia D. Exploring stigma: Medical knowledge and the stigmatisation of parents of children diagnosed with autism spectrum disorder. Sociol Health Illn. 2009;31(7):1011–1027. [DOI] [PubMed] [Google Scholar]
- 158. Ng CKM, Lam SHF, Tsang STK, Yuen C, Chien C-W. The relationship between affiliate stigma in parents of children with autism spectrum disorder and their children's activity participation. Int J Environ Res Public Health. 2020;17(5):1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Livingston LA, Colvert E, Social Relationships Study T, Bolton P, Happé F. Good social skills despite poor theory of mind: Exploring compensation in autism spectrum disorder. J Child Psychol Psychiatry. 2019;60(1):102–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Livingston LA, Shah P, Happé F. Compensatory strategies below the behavioural surface in autism: A qualitative study. Lancet Psychiatry. 2019;6(9):766–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Livingston LA, Happé F. Conceptualising compensation in neurodevelopmental disorders: Reflections from autism spectrum disorder. Neurosci Biobehav Rev. 2017;80:729–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Halsall J, Clarke C, Crane L. “Camouflaging” by adolescent autistic girls who attend both mainstream and specialist resource classes: Perspectives of girls, their mothers and their educators. Autism. 2021;25(7):2074–2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Bernardin CJ, Lewis T, Bell D, Kanne S. Associations between social camouflaging and internalizing symptoms in autistic and non-autistic adolescents. Autism. 2021;25(6):1580–1591. [DOI] [PubMed] [Google Scholar]
- 164. Hull L, Levy L, Lai MC, et al. . Is social camouflaging associated with anxiety and depression in autistic adults? Mol Autism. 2021;12(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Cassidy S, Bradley L, Shaw R, Baron-Cohen S. Risk markers for suicidality in autistic adults. Mol Autism. 2018;9:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. O'Connor C, Burke J, Rooney B. Diagnostic disclosure and social marginalisation of adults with ASD: Is There a relationship and what mediates it? J Autism Dev Disord. 2020;50(9):3367–3379. [DOI] [PubMed] [Google Scholar]
- 167. Crompton CJ, Hallett S, Ropar D, Flynn E, Fletcher-Watson S. ‘I never realised everybody felt as happy as I do when I am around autistic people’: A thematic analysis of autistic adults' relationships with autistic and neurotypical friends and family. Autism. 2020;24(6):1438–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Miller D, Rees J, Pearson A. “Masking is life”: Experiences of masking in autistic and nonautistic adults. Autism Adulthood. 2021;3(4):330–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Schneid I, Raz AE. The mask of autism: Social camouflaging and impression management as coping/normalization from the perspectives of autistic adults. Soc Sci Med. 2020;248:112826. [DOI] [PubMed] [Google Scholar]
- 171. Lai MC, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015;2(11):1013–1027. [DOI] [PubMed] [Google Scholar]
- 172. Lai M-C, Anagnostou E, Wiznitzer M, Allison C, Baron-Cohen S. Evidence-based support for autistic people across the lifespan: Maximising potential, minimising barriers, and optimising the person–environment fit. Lancet Neurol. 2020;19(5):434–451. [DOI] [PubMed] [Google Scholar]
- 173. Tola G, Talu V, Congiu T, Bain P, Lindert J. Built environment design and people with autism spectrum disorder (ASD): A scoping review. Int J Environ Res Public Health. 2021;18(6):3203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Milton D, Martin N, Melham P. Beyond reasonable adjustment: autistic-friendly spaces and Universal Design. In: Milton D, Martin N, eds. Autism and Intellectual Disabilities in Adults Vol. 1. Hove: Pavilion Publishing and Media; 2016;81–85. [Google Scholar]
- 175. Pellicano L, Bölte S, Stahmer A. The current illusion of educational inclusion. Autism. 2018;22(4):386–387. [DOI] [PubMed] [Google Scholar]
- 176. Brewer N, Zoanetti J, Young RL. The influence of media suggestions about links between criminality and autism spectrum disorder. Autism. 2017;21(1):117–121. [DOI] [PubMed] [Google Scholar]
- 177. Tang L, Bie B. The stigma of autism in china: An analysis of newspaper portrayals of autism between 2003 and 2012. Health Commun. 2016;31(4):445–452. [DOI] [PubMed] [Google Scholar]
- 178. Holton AE, Farrell LC, Fudge JL. A threatening space?: Stigmatization and the framing of autism in the news. Commun Stud. 2014;65(2):189–207. [Google Scholar]
- 179. Bie B, Tang L. Representation of autism in leading newspapers in China: A content analysis. Health Commun. 2015;30(9):884–893. [DOI] [PubMed] [Google Scholar]
- 180. Baeyens D, Moniquet A, Danckaerts M, van der Oord S. A comparative study of the structural stigmatisation of ADHD and autism spectrum disorder in Flemish newspapers. Tijdschr Psychiatr. 2017;59(5):269–277. [PubMed] [Google Scholar]
- 181. Nordahl-Hansen A, Øien RA, Fletcher-Watson S. Pros and cons of character portrayals of autism on TV and film. J Autism Dev Disord. 2018;48(2):635–636. [DOI] [PubMed] [Google Scholar]
- 182. Gillespie-Lynch K, Bisson J, Saade S, et al. . If you want to develop an effective autism training, ask autistic students to help you. Autism. 2021 [Epub ahead of print]; DOI: 10.1177/13623613211041006. [DOI] [PubMed] [Google Scholar]
- 183. Saade S, Bean YF, Gillespie-Lynch K, Poirier N, Harrison AJ. Can participation in an online ASD training enhance attitudes toward inclusion, teaching self-Efficacy and ASD knowledge among preservice educators in diverse cultural contexts? Int J Inclusive Educ. 2021:1–16. 10.1080/13603116.2021.1931716. [DOI] [Google Scholar]
- 184. Jones DR, Morrison KE, DeBrabander KM, Ackerman RA, Pinkham AE, Sasson NJ. Greater social interest between autistic and non-autistic conversation partners following autism acceptance training for non-autistic people. Front Psychol. 2021;12:739147. 10.3389/fpsyg.2021.739147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Jones DR, DeBrabander KM, Sasson NJ. Effects of autism acceptance training on explicit and implicit biases toward autism. Autism. 2021;25(5):1246–1261. [DOI] [PubMed] [Google Scholar]
- 186. Morris S, O'Reilly G, Byrne MK. Understanding our peers with Pablo: Exploring the merit of an autism spectrum disorder de-stigmatisation programme targeting peers in Irish early education mainstream settings. J Autism Dev Disord. 2020;50(12):4385–4400. [DOI] [PubMed] [Google Scholar]
- 187. Staniland JJ, Byrne MK. The effects of a multi-component higher-functioning autism anti-stigma program on adolescent boys. J Autism Dev Disord. 2013;43(12):2816–2829. [DOI] [PubMed] [Google Scholar]
- 188. Ranson NJ, Byrne MK. Promoting peer acceptance of females with higher-functioning autism in a mainstream education setting: A replication and extension of the effects of an autism anti-stigma program. J Autism Dev Disord. 2014;44(11):2778–2796. [DOI] [PubMed] [Google Scholar]
- 189. Sarge MA, Kim H-S, Velez JA. An auti-sim intervention: The role of perspective taking in combating public stigma with virtual simulations. Cyberpsychol Behav Soc Netw. 2020;23(1):41–51. [DOI] [PubMed] [Google Scholar]
- 190. Bonsu A. Keeping an open mind about autism. Lancet Neurol. 2017;16(12):963. [Google Scholar]
- 191. Como DH, Floríndez LI, Tran CF, Cermak SA, Stein Duker LI. Examining unconscious bias embedded in provider language regarding children with autism. Nurs Health Sci. 2020;22(2):197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Teal CR, Gill AC, Green AR, Crandall S. Helping medical learners recognise and manage unconscious bias toward certain patient groups. Med Educ. 2012;46(1):80–88. [DOI] [PubMed] [Google Scholar]
- 193. Government W. Refreshed Autistic Spectrum Disorder Strategic Action Plan. In. Wales, United Kingdom; 2020. [Google Scholar]
- 194. Kapp SK, Gillespie-Lynch K, Sherman LE, Hutman T. Deficit, difference, or both? Autism and neurodiversity. Dev Psychol. 2013;49(1):59. [DOI] [PubMed] [Google Scholar]
- 195. Jaarsma P, Welin S. Autism as a natural human variation: Reflections on the claims of the neurodiversity movement. Health Care Anal. 2012;20(1):20–30. [DOI] [PubMed] [Google Scholar]
- 196. Griffin E, Pollak D. Student experiences of neurodiversity in higher education: Insights from the BRAINHE project. Dyslexia. 2009;15(1):23–41. [DOI] [PubMed] [Google Scholar]
- 197. Armstrong T. The myth of the normal brain: embracing neurodiversity. AMA J Ethics. 2015;17(4):348–352. [DOI] [PubMed] [Google Scholar]
- 198. Smart J. Challenges to the Biomedical Model of Disability. Advan Medical Psychother Psychodiag. 2006;12:1–4. [Google Scholar]
- 199. Pellicano E, den Houting J.. Annual Research Review: Shifting from ‘normal science’ to neurodiversity in autism science. J Child Psychol Psychiatry. 2021. [Epub ahead of print]; DOI: 10.1111/jcpp.13534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Cooper K, Smith LGE, Russell A. Social identity, self-esteem, and mental health in autism. Eur J Soc Psychol. 2017;47(7):844–854. [Google Scholar]
- 201. Kenny L, Hattersley C, Molins B, Buckley C, Povey C, Pellicano E. Which terms should be used to describe autism? Perspectives from the UK autism community. Autism. 2016;20(4):442–462. [DOI] [PubMed] [Google Scholar]
- 202. Bury SM, Jellett R, Spoor JR, Hedley D.. “It defines who i am” or “it's something i have”: What language do [autistic] Australian adults [on the autism spectrum] prefer? J Autism Dev Disord. 2020. [Epub ahead of print]; DOI: 10.1007/s10803-020-04425-3. [DOI] [PubMed] [Google Scholar]
- 203. Gernsbacher MA. Editorial perspective: The use of person-first language in scholarly writing may accentuate stigma. J Child Psychol Psychiatry. 2017;58(7):859–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Bottema-Beutel K, Kapp SK, Lester JN, Sasson NJ, Hand BN. Avoiding ableist language: suggestions for autism researchers. Autism Adulthood. 2021;3(1):18–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Singh JS, Bunyak G. Autism disparities: A systematic review and meta-ethnography of qualitative research. Qual Health Res. 2019;29(6):796–808. [DOI] [PubMed] [Google Scholar]
- 206. Corrigan PW, Shapiro JR. Measuring the impact of programs that challenge the public stigma of mental illness. Clin Psychol Rev. 2010;30(8):907–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Fletcher-Watson S, Adams J, Brook K, et al. . Making the future together: Shaping autism research through meaningful participation. Autism. 2019;23(4):943–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Pickard H, Pellicano E, den Houting J, Crane L. Participatory autism research: Early career and established researchers' views and experiences. Autism. 2022;26(1):75–87. [DOI] [PMC free article] [PubMed] [Google Scholar]