Abstract
OBJECTIVE:
The aim of this study was to describe the relationships between intent to leave, reasons nurses intend to leave, and the nursing work environment in military hospitals.
BACKGROUND:
Intention to leave is a precursor of nurse turnover. The reasons nurses intend to leave may be influenced by leader interventions and potentially preventable.
METHODS:
This descriptive, correlational secondary analysis included 724 nurse survey responses from 23 US Army hospitals. Bivariate correlations and predictive modeling techniques were used.
RESULTS:
Forty-nine percent of nurses indicated they intended to leave, 44% for potentially preventable reasons. Dissatisfaction with management and the nursing work environment were the top potentially preventable reasons to leave. Nurses who intended to leave for potentially preventable reasons scored aspects of the nursing work environment significantly lower than those intending to leave for nonpreventable reasons.
CONCLUSIONS:
Identifying potentially preventable reasons in conjunction with intent to leave can provide leaders opportunities to intervene and influence turnover intention.
The COVID-19 pandemic has placed exponential demand on a nursing workforce already facing global staffing shortages and increased workloads.1,2 In the United States, nurse turnover rates continue to average 19.1%, costing hospitals an average of $6.5 million annually.3 The consequences of nurse turnover are associated with adverse patient outcomes.4 Nurse turnover is complex, and definitions in the literature are multifaceted.5 Nurse turnover occurs when nurses voluntarily or involuntarily leave their current nursing job for a different position either within or outside of their current organization.6 Nurse turnover and intent to leave are often presented as related concepts.7 Intent to leave is a nurse’s self-reported plan to leave his or her job.8 Intention to leave is influenced by individual and work-related factors.9 Examples of individual factors include pursuing higher education, career advancement,10 and burnout.11 Examples of work-related factors include organizational climate12 and the nursing work environment.13 The nursing work environment is the context in which nurses provide care.14 Research shows that unfavorable nursing work environments are associated with increased intention to leave the job or the nursing profession.15,16 Very little research examines the relationship between the nursing work environment and the reasons nurses intend to leave.17,18
Nurse leaders have a crucial role in influencing the factors or reasons that lead nurses to leave their jobs.19–21 Researchers posit that effective nurse leaders develop comprehensive strategies and facilitate positive work environments that retain experienced nursing staff.22 It is imperative that nurse leaders identify the preventable reasons nurses intend to leave, which generates an opportunity for nurse leaders to proactively engage with nurses and intervene before turnover happens. The purpose of this study was to examine the relationship between the nursing work environment, intent to leave, and reasons nurses intend to leave, as well as identify which reasons may be potentially preventable by leader interventions. We also discuss how leaders may positively influence preventable reasons.
Conceptual Model
Donabedian’s23 conceptual framework of structure, process, and outcome underpins this work and offers a systematic way to identify factors affecting healthcare quality. US Army hospitals were the overall clinical setting. Nursing staff and unit type were the primary structural components of the analysis. The nursing work environment, categorized by the Practice Environment Scale of the Nursing Work Index’s (PES-NWI) 5 subscales, was the process.24 Intent to leave was the initial dichotomous outcome. We further analyzed the reasons for those respondents intending to leave and categorized them as preventable, nonpreventable, and other reasons for leaving. This study aimed to describe the relationships between intent to leave, reasons nurses intend to leave, and the nursing work environment in US Army hospitals (Figure 1).
Figure 1.
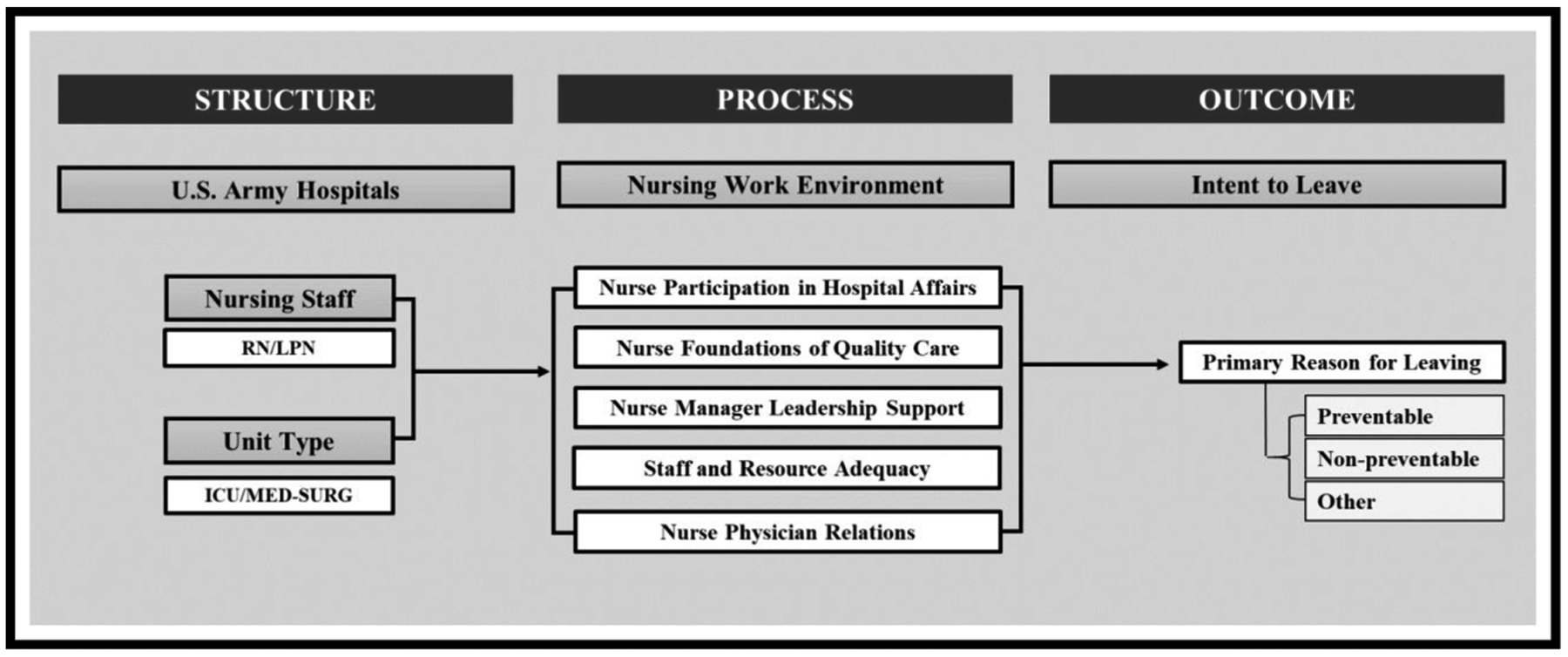
Conceptual framework. The conceptual framework, adapted from Donabedian’s structure, process, and outcomes, depicts evaluated associations. Med-Surg indicates medical-surgical unit; RN, registered nurse; LPN, licensed practical nurse; ICU, intensive care unit.
Methods
Sample and Setting
This study used survey data from 23 US Army hospitals, part of a larger Military Health System, which provides healthcare services to over 9.5 million beneficiaries.25 These military hospitals range in size from 24 to 200 beds. Some are similar to teaching hospitals in that they contain graduate medical education programs; others do not. Turnover in staff and leadership is organically high in these military hospitals as military service members move approximately every 3 years.
Nurses sampled included active duty and reserve service members and federal government service civilian nursing personnel working in adult medical-surgical and intensive care inpatient units. Unlicensed nursing personnel and contract nurse responses were excluded. Our sample included survey responses from 633 registered nurses (RNs) and 91 licensed practical nurses (LPNs) (N = 724) to describe the relationship between intent to leave and the nursing work environment. A subset of 222 RNs and 24 LPNs (n = 246) was used to describe the relationship between reasons nurses intend to leave and the nursing work environment. The minimum required sample size of 115 was calculated using G-Power 3.1 software,26 as categorized by Cohen,27 for 80% power and a significant level of 0.05.
Data Source
Data were extracted from a parent study that examined the impact of professional nursing work environments and nurse staffing on readmissions, failure to rescue, and mortality in military hospitals.28 The use of secondary survey data was appropriate for answering the research question. Potential respondents (eg, all nursing staff) received electronic survey invitations via e-mail, which included a cover letter describing the voluntary nature of the survey and confidentiality of their survey responses.28
Measures
Intent to leave was operationally defined as a nurse’s desire to leave their current position within a specified timeframe.10 Service members and federal government service civilians are often obligated to work specific commitment terms; therefore, the survey asked: “If you COULD, regardless of military obligation (yours or your spouse’s), WOULD you leave your current job?” When answering “yes,” respondents also indicated the timeframe they intended to leave: 3, 6, or 12 months. Responses were dichotomized into 2 categories, “yes,” corresponding to any of the 3 timeframes, or “no,” indicating that the respondent would not leave their current job. Previous studies have deemed this single-item measure appropriate for measuring this global construct.29,30
The primary reason for leaving was categorized as potentially preventable or nonpreventable and assessed by asking nurses who responded “yes” to the intent to leave survey item to select 1 primary reason from 20 choices (Table 1). When respondents selected “other,” they could enter a free-text comment. Preventable reasons are factors that can be influenced by leader actions, for example, dissatisfaction with management, team-work, and scheduling.10 Nonpreventable reasons are individual factors that include a personal desire to further one’s education, moves directed by the military, planned retirement, or promotion.10 “Personal reasons” for leaving and the “other” responses could not be categorized as either preventable or nonpreventable and were considered a separate category. This measure has been described and used in a previous study that analyzed the nursing work environment in military hospitals.10
Table 1.
Primary Reasons for Leaving
| n | % | |
|---|---|---|
| Preventable reasons | 109 | 44 |
| Dissatisfied with management | 45 | 41 |
| Dissatisfied with nursing work environment | 21 | 19 |
| Leaving before retirement | 13 | 12 |
| Taking a position elsewhere within healthcare | 10 | 9 |
| Dissatisfied with schedule | 7 | 6 |
| Dissatisfied with compensation | 5 | 5 |
| Dissatisfied with team members | 6 | 6 |
| Taking a position elsewhere outside of healthcare | 2 | 2 |
| Nonpreventable reasons | 99 | 40 |
| Permanent change of station (military move) | 48 | 49 |
| Pursue further education | 27 | 27 |
| Retiring | 11 | 11 |
| Transferring within the hospital | 7 | 7 |
| Promoted out of position—within hospital system | 3 | 3 |
| Military deployment | 1 | 1 |
| Medical discharge or disability | 1 | 1 |
| Cutbacks or reduction in force | 1 | 1 |
| Other | 38 | 15 |
| Personal reasons | 14 | 37 |
| Other | 24 | 63 |
The nursing work environment was measured by the PES-NWI, an empirically developed instrument that evaluates nursing work environment characteristics that facilitate or detract from nurses’ ability to practice professionally.14 The PES-NWI has 5 subscales: Nurse Participation in Hospital Affairs; Nursing Foundations for Quality Care; Nurse Manager Ability, Leadership, and Support of Nurses; Staffing and Resource Adequacy; and Collegial Nurse-Physician Relations. Composite scores are calculated by averaging subscale scores.14 Respondents’ perception of their work environment was assessed by determining the presence of the individual items, such as “enough staff to get the work done,” in their work environment using a 4-point Likert scale, where 1 = “strongly disagree,” 2 = “disagree,” 3 = “agree,” and 4 = “strongly agree.” An average composite score of 3.0 or higher is considered favorable.31 Psychometric assessments of the PES-NWI’s reliability and validity are acceptable for nurses working in civilian14 and military32 hospitals.
Data Analysis
Data were analyzed at the individual level. Descriptive statistics and bivariate correlations were used to evaluate the relationships between intent to leave and the nursing work environment. Descriptive statistics, analysis of variance (ANOVA), multivariate logistic regression, and 2 different data mining techniques, decision tree and random forest analyses,33 were used to evaluate relationships between the primary reason for leaving and the nursing work environment. Predictive models were compared using receiver operating characteristics curves.34 χ2 was calculated for categorical predictor variables and t tests or ANOVA for continuous predictor variables. Cramer V, Cohen d, and η2 were used to determine effect sizes for the χ2 and Fisher exact, t statistics, and ANOVA, respectively. All statistical analyses were performed using R statistical software.35 The rattle package was used to run the predictive models. Missing data were deleted listwise (Figure 2).
Figure 2.
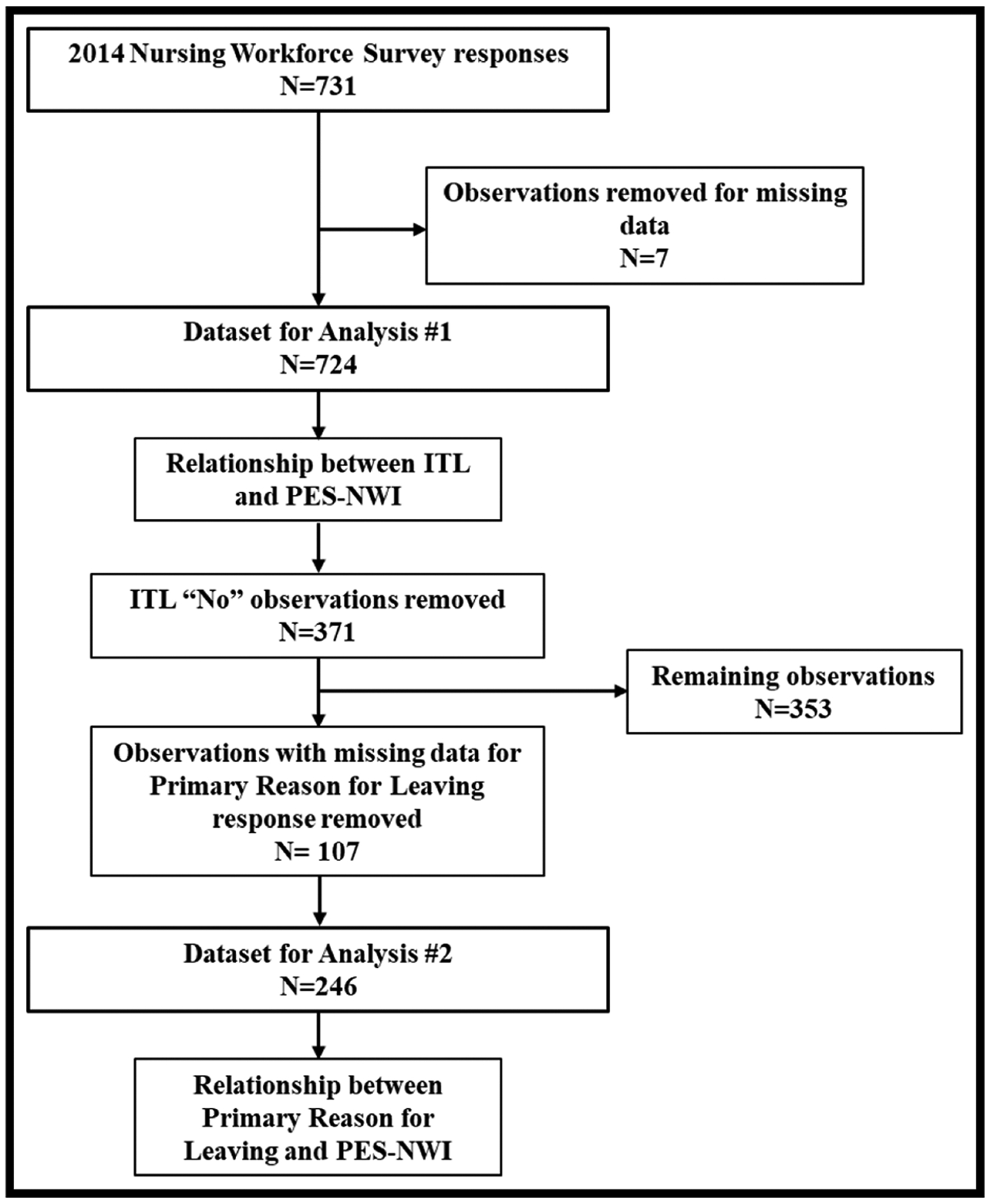
Data cleaning process. This figure depicts the process of cleaning the datasets used for analysis. ITL, intent to leave.
Ethical Approval
This study was approved by the University of Alabama at Birmingham and Uniformed Services University of the Health Sciences institutional review boards.
Results
Means and standard deviations for continuous variables and frequencies and percentages for categorical variables are summarized in Table 2. Of the 724 respondents, 49% (n = 353) indicated intent to leave their current position within 3 to 12 months. There were significant associations (P < 0.0001) between all 5 subscales of the PES-NWI and intent to leave. Respondents who intended to leave their jobs scored each of the 5 PES-NWI subscales significantly lower (P < 0.0001) than those who intended to stay. An ANOVA on the PES-NWI subscale and composite scores yielded significant variation among respondents who indicated they were leaving for potentially preventable, nonpreventable, and other reasons for all PES-NWI subscales and the subscale composite score, except Staffing and Resource Adequacy and Collegial Nurse-Physician Relations (P < 0.0001). Effect sizes ranged from small (η2 = 0.02) to medium (η 2= 0.13).
Table 2.
Descriptive Summary
| Variable | Intent to Leave | Primary Reason for Leaving | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N = 724 | n = 246 | |||||||||||
| Yes n = 353 (49%) | No n = 371 (51%) | Nonpreventable n = 99 (40%) | Preventable n = 109 (44%) | Other n = 38 (15%) | Pairwise Post Hoc Comparison | |||||||
| Mean ± SD | Mean ± SD | P | Cohen d Effect Size | Mean ± SD | Mean ± SD | Mean ± SD | P | η2 Effect Size | Preventable vs Nonpreventa ble | Preventable vs Other | Other vs Nonpreventable | |
| NPHA | 2.53 ± 0.66 | 2.94 ± 0.62 | <0.0001 | 0.64 | 2.79 ± 0.60 | 2.27 ± 0.63 | 2.62 ± 0.67 | <0.0001 | 0.13 | 0.0000a | 0.0210a | 0.4820 |
| NFQC | 2.94 ± 0.53 | 3.26 ± 0.48 | <0.0001 | 0.64 | 3.12 ± 0.45 | 2.76 ± 0.57 | 3.07 ± 0.55 | <0.0001 | 0.10 | 0.0002a | 0.0120a | 1.0000 |
| NMLS | 2.56 ± 0.87 | 3.18 ± 0.69 | <0.0001 | 0.79 | 2.88 ± 0.74 | 2.21 ± 0.86 | 2.48 ± 0.91 | <0.0001 | 0.12 | 0.0000a | 0.2900 | 0.0500a |
| SRA | 2.59 ± 0.74 | 3.07 ± 0.66 | <0.0001 | 0.69 | 2.70 ± 0.71 | 2.47 ± 0.75 | 2.68 ± 0.80 | 0.1020 | 0.02 | 0.1200 | 0.5400 | 1.0000 |
| CNPR | 2.98 ± 0.64 | 3.27 ± 0.61 | 0.0000 | 0.47 | 3.08 ± 0.61 | 2.86 ± 0.68 | 3.04 ± 0.70 | 0.0721 | 0.02 | 0.0770 | 0.5570 | 1.0000 |
| Composite | 2.72 ± 0.54 | 3.14 ± 0.49 | <0.0001 | 0.82 | 2.92 ± 0.47 | 2.52 ± 0.54 | 2.78 ± 0.57 | <0.0001 | 0.11 | 0.0000a | 0.0420a | 0.5430 |
| n (%) | n (%) | P | Cramer V | n (%) | n (%) | n (%) | P | Cramer V | Preventable vs Nonpreventable | Preventable vs Other | Other vs Nonpreventable | |
| Unit type | ||||||||||||
| Adult ICU | 41 (52) | 44 (48) | 1.000 | <0.01 | 6 (33) | 10 (56) | 2 (11) | 0.7134 | 0.06 | 1.0000 | 1.0000 | 1.0000 |
| Adult Med-Surg | 312 (49) | 327 (51) | 93 (41) | 99 (43) | 36 (16) | |||||||
| Position | ||||||||||||
| RN | 325 (51) | 308 (49) | 0.0003 | 0.13 | 99 (45) | 85 (38) | 38 (17) | <0.0001 | 0.37 | <0.0001a | 0.0011a | 1.0000 |
| LPN | 28 (31) | 63 (69) | 0 (0) | 24 (100) | 0 (0) | |||||||
Effect size is Cramer V for binary variables: small, ~0.1; medium, ~0.3; large, ~0.5 or greater; Cohen d correlation for continuous variables: small, ~0.2; medium, ~0.5; large, ~0.8, and η2 for ANOVA: ~0.01, small; ~0.06, medium, and >0.14, large. P values are reported for the pairwise post hoc comparison.
Abbreviations: CNPR, Collegial Nurse-Physician Relationships; Med-Surg, medical, surgical or combined medical surgical units; NFQC, Nursing Foundations of Quality Care; NMLS, Nurse Manager Ability, Leadership, and Support for Nurses; NPHA, Nurse Participation in Hospital Affairs; SRA, Staffing and Resource Adequacy.
Significant variation.
Table 1 shows a summary of the potentially preventable and nonpreventable reasons respondents intended to leave their jobs. Dissatisfaction with management and the work environment were the most frequently reported potentially preventable reasons. Military moves (expected for this population) and pursuit of higher education were the top 2 nonpreventable reasons respondents intended to leave. Personal reasons and other, which could not be categorized as preventable or nonpreventable, accounted for 15% of all reasons for leaving.
Logistic Regression, Decision Tree, and Random Forest Modeling
Logistic regression, decision tree, and random forest modeling were used to predict potentially preventable reasons nurses intend to leave based on the 5 PES-NWI subscales. The logistic regression model showed that the Nurse Manager Ability, Leadership, and Support of Nurses subscale was a significant predictor of a nurse selecting a potentially preventable reason for intending to leave (F6, −106 = 35.89, P < 0.001; adjusted R2 = 0.43) (Supplemental Digital Content #1, http://links.lww.com/JONA/A856). The root node of the decision tree model indicated the Nurse Participation in Hospital Affairs and Nurse Manager Ability, Leadership, and Support of Nurses subscales were the most influential predictors of potentially preventable reasons (Supplemental Digital Content #2, http://links.lww.com/JONA/A857). The random forest model indicated Nurse Manager Ability, Leadership, and Support of Nurses and Nurse Participation in Hospital Affairs were the 1st and 2nd most important predictors of potentially preventable reasons, respectively (Supplemental Digital Content #3, http://links.lww.com/JONA/A858).
Discussion
In this study, 49% of nurses intended to leave their positions within 3 to 12 months. However, the intent to leave measure alone is insufficient for determining appropriate leader interventions. Forty-four percent of respondents reported a potentially preventable reason for their intention to leave, with the most common reasons being dissatisfaction with management and the nursing work environment. Like previous studies, these findings validate that nurses intending to leave their positions report lower PES-NWI subscales scores,36 thus highlighting the importance of a favorable nursing work environment in preventing nurse turnover. Although personal reasons are subjective and cannot be exclusively categorized as preventable, selecting this response option presents leaders an opportunity to engage their nursing staff to learn more about what exactly may be motivating them to leave.
Analysis using 3 different modeling techniques revealed similar results: aspects of the work environment appear to be predictors of leaving for potentially preventable reasons. In all 3 models, the Nurse Manager Ability, Leadership, and Support of Nurses subscale was an important predictor. The effects of nurse managers on the work environment are well established.37 A systematic review of healthy work environments underscores the nurse manager as a significant factor in nurses’ decisions to leave or stay in a job.38 Previous studies also found that better leadership would likely prompt nurses to reconsider leaving.22 Nurse managers perceived by staff to be caring, flexible, and authentic leaders are critical to nurse retention.39 Strategies to mentor and develop nurse managers are vital to improving the nursing work environment. These strategies could decrease nurses wanting to leave their jobs for potentially preventable reasons, reducing intent to leave and potentially decreasing turnover.
The other PES-NWI subscale that was a strong predictor of potentially preventable reasons for intending to leave was Nurse Participation in Hospital Affairs. These findings bolster the abundance of evidence that nurses need a voice in decisions about their work and work environments.40 Leadership interventions that target Nurse Participation in Hospital Affairs include engaging with and maximizing nurse practice councils and active performance improvement programs.41 These interventions together positively influence nursing work environments and reduce potentially preventable reasons for intending to leave.
Limitations and Strengths
We used 3 complementary statistical techniques34; however, secondary data use has potential data quality limitations.42 Beyond the limits of this study, there is a rich opportunity within the free-text response options of “other” to understand this category more fully and explore if these reasons are preventable or not preventable or simply do not lend themselves to this type of categorization. This study provides a strong start for this work. Combining RN and LPN survey responses for this analysis could have affected the results. Educational preparation, role, autonomy, and level of control over practice could affect how nurses respond to survey items. The military sample may present a limitation as the potential effect of nursing commitment within the military setting may differ from the civilian setting. However, concepts and leader actions are applicable across civilian and military settings.
Recommendations for Further Research
Further exploration into the relationship between nursing work environment variables and potentially preventable reasons nurses intend to leave is vital. Future research may lead to targeted interventions to improve nursing work environments and reduce preventable intent to leave. Determining and validating a standardized list of objective reasons for intent to leave are required for comparison across settings and appreciating organizational and leader influences. Measuring the effectiveness of interventions to improve nurse manager performance on preventable reasons nurses intend to leave is essential. Lastly, considering the significant impact of the COVID-19 pandemic on the reasons nurses intend to leave is yet another area for future exploration.
Implications for Nurse Executives
The effect of the nursing work environment on nurses’ intent to leave is well established. More recent studies have confirmed how poor working conditions and ineffective nurse managers during a global pandemic have further challenged the ability to retain experienced nurses. Asking nurses if they intend to leave is not enough. Based on our findings, nurse executives should identify potentially preventable reasons nurses intend to leave and proactively intervene. Furthermore, leaders should consider interventions to improve nurse manager competency and performance. These interventions must focus on education in principles such as leadership style,43 receiving and giving feedback,39 talent management, mentorship, coaching,44 award and recognition,45 conflict management, financial management, human resources, quality, and safety.46 It is common practice to replace nurse manager vacancies with staff nurses promoted on the same unit who are excellent clinicians but lack formal management training. Unfortunately, this practice ignores that clinical nursing and nurse management are very distinct roles.47 Nurse executives should also consider interventions that allow nurses to be more engaged in decisions that affect their practice. The goal of these interventions is to make nurses feel valued and respected.41 Proactively engaging nursing staff with interventions that target identified preventable reasons for intending to leave may contribute to the retention of experienced nursing staff.
Conclusions
Nurse turnover is common, expensive, and strongly associated with adverse patient outcomes. Healthcare organizations struggle with the inability to retain top-quality nursing personnel. Considering intent to leave is a dichotomous variable that does not get to “why” nurses depart, and we explored the underlying reasons of their intent and identified opportunities for leaders to intervene. Identifying potentially preventable reasons is a more informative and actionable nursing-sensitive indicator in conjunction with intent to leave.
Supplementary Material
Acknowledgments
The authors would like to thank Carla Dickenson, PhD, RN, Chief, Center for Nursing Science and Clinical Inquiry, Brooke Army Medical Center, Fort Sam Houston, Texas, and Dan Wood, AN, FACHE, NE-BC, Chief clinical instructor Army-Baylor MHA/MBA Graduate Program, Fort Sam Houston, Texas, for assistance with data collection and general support for the parent study. In addition, we would like to acknowledge the nurses who took the survey and the nurse leaders who are committed to improving the work environment.
The parent study, “The Impact of Nursing on Readmissions, Failure to Rescue, and Mortality in Department of Defense Hospitals,” was supported by the TriService Nursing Research Program (grant number HU0001-16-1-TS12/project number N16-P08). The parent study for this project was approved by the University of Alabama at Birmingham, protocol N170113001 (February 6, 2017), and the Uniformed Services University (March 17, 2017) institutional review boards.
Footnotes
Publisher's Disclaimer: Disclaimer: The views expressed are solely those of the authors and do not reflect the official policy or position of the US Army, US Navy, US Air Force, the Department of Defense, or the US Government. Approved by the US Army Medical Center of Excellence Public Affairs Office.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.jonajournal.com).
The authors declare no conflicts of interest.
References
- 1.Varasteh S, Esmaeili M, Mazaheri M. Factors affecting Iranian nurses’ intention to leave or stay in the profession during the COVID-19 pandemic [published online ahead of print September 25, 2021]. Int Nurs Rev. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ali H, Cole A, Ahmed A, Hamasha S, Panos G. Major stressors and coping strategies of frontline nursing staff during the out-break of coronavirus disease 2020 (COVID-19) in Alabama. J Multidiscip Healthc. 2020;13:2057–2068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.NSI Nursing Solutions, Inc. 2021 NSI National Healthcare Retention & RN Staffing Report. East Petersburg, PA: NSI Nursing Solutions, Inc.; 2021. [Google Scholar]
- 4.Kim Y, Han K. Longitudinal associations of nursing staff turnover with patient outcomes in long-term care hospitals in Korea. J Nurs Manag. 2018;26(5):518–524. [DOI] [PubMed] [Google Scholar]
- 5.Hayes LJ, O’Brien-Pallas L, Duffield C, et al. Nurse turnover: a literature review—an update. Int J Nurs Stud. 2012;49(7):887–905. [DOI] [PubMed] [Google Scholar]
- 6.O’Brien-Pallas L, Murphy GT, Shamian J, Li X, Hayes LJ. Impact and determinants of nurse turnover: a pan-Canadian study. J Nurs Manag. 2010;18(8):1073–1086. [DOI] [PubMed] [Google Scholar]
- 7.Brewer CS, Kovner CT, Greene W, Tukov-Shuser M, Djukic M. Predictors of actual turnover in a national sample of newly licensed registered nurses employed in hospitals. J Adv Nurs. 2012;68(3):521–538. [DOI] [PubMed] [Google Scholar]
- 8.Koehler T, Olds D. Generational differences in nurses’ intention to leave [published online ahead of print March 20, 2021]. West J Nurs Res. doi: 10.1177/0193945921999608. [DOI] [PubMed] [Google Scholar]
- 9.Takase M A concept analysis of turnover intention: implications for nursing management. Collegian. 2010;17(1):3–12. [DOI] [PubMed] [Google Scholar]
- 10.Breckenridge-Sproat ST, Swiger PA, Belew DL, Raju D, Patrician PA, Loan LA. A program evaluation of the patient CaringTouch System: a pre- and postimplementation assessment. Nurs Out-look. 2017;65(5S):S109–S119. [DOI] [PubMed] [Google Scholar]
- 11.Labrague LJ, De Los Santos JAA, Falguera CC, et al. Predictors of nurses’ turnover intention at one and five years’ time. Int Nurs Rev. 2020;67(2):191–198. [DOI] [PubMed] [Google Scholar]
- 12.Van den Heede K, Florquin M, Bruyneel L, et al. Effective strategies for nurse retention in acute hospitals: a mixed method study. Int J Nurs Stud. 2013;50(2):185–194. [DOI] [PubMed] [Google Scholar]
- 13.Patrician PA, Shang J, Lake ET. Organizational determinants of work outcomes and quality care ratings among Army medical department registered nurses. Res Nurs Health. 2010;33(2):99–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lake ET. Development of the Practice Environment Scale of the Nursing Work Index. Res Nurs Health. 2002;25(3):176–188. [DOI] [PubMed] [Google Scholar]
- 15.Choi SP, Cheung K, Pang SM. Attributes of nursing work environment as predictors of registered nurses’ job satisfaction and intention to leave. J Nurs Manag. 2013;21(3):429–439. [DOI] [PubMed] [Google Scholar]
- 16.Lasater KB, Aiken LH, Sloane DM, et al. Chronic hospital nurse understaffing meets COVID-19: an observational study. BMJ Qual Saf. 2021;30(8):639–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tummers LG, Groeneveld SM, Lankhaar M. Why do nurses intend to leave their organization? A large-scale analysis in long-term care. J Adv Nurs. 2013;69(12):2826–2838. [DOI] [PubMed] [Google Scholar]
- 18.Valizadeh L, Zamanzadeh V, Habibzadeh H, Alilu L, Gillespie M, Shakibi A. Experiences of Iranian nurses that intent to leave the clinical nursing: a content analysis. J Caring Sci. 2016. Jun 1; 5(2):169–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dewanto A, Wardhani V. Nurse turnover and perceived causes and consequences: a preliminary study at private hospitals in Indonesia. BMC Nurs. 2018;17(suppl 2):52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roche MR, Duffield CM, Dimitrelis S, Frew B. Leadership skills for nursing unit managers to decrease intention to leave. Nurs Res Rev. 2015;5:57–64. [Google Scholar]
- 21.Suliman M, Aljezawi M, Almansi S, Musa A, Alazam M, Ta’an WF. Effect of nurse managers’ leadership styles on predicted nurse turnover. Nurs Manag (Harrow). 2020. Sep 24;27(5): 20–25. [DOI] [PubMed] [Google Scholar]
- 22.Labrague LJ, Nwafor CE, Tsaras K. Influence of toxic and transformational leadership practices on nurses’ job satisfaction, job stress, absenteeism and turnover intention: a cross-sectional study. J Nurs Manag. 2020;28(5):1104–1113. [DOI] [PubMed] [Google Scholar]
- 23.Donabedian A Evaluating the quality of medical care. Milbank Mem Fund Q. 1966;44(suppl 3):166–206. [PubMed] [Google Scholar]
- 24.Swiger PA, Patrician PA, Miltner RSS, Raju D, Breckenridge-Sproat S, Loan LA. The Practice Environment Scale of the Nursing Work Index: an updated review and recommendations for use. Int J Nurs Stud. 2017;74:76–84. [DOI] [PubMed] [Google Scholar]
- 25.Defense Health Agency. 2018 Stakeholder Report. Washington, DC: Defense Health Agency; 2020. [Google Scholar]
- 26.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. [DOI] [PubMed] [Google Scholar]
- 27.Cohen J Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1988. [Google Scholar]
- 28.Patrician PA. Final Report: Grant HU0001-16-1-TS12. The Impact of Nursing on Readmissions, Failure to Rescue, and Mortality in Department of Defense Hospitals. Bethesda, MD: TriService Nursing Res Program; 2019. [Google Scholar]
- 29.Patrician PA. Single-item graphic representational scales. Nurs Res. 2004;53(5):347–352. [DOI] [PubMed] [Google Scholar]
- 30.Aiken LH, Clarke SP, Sloane DM, et al. Nurses’ reports on hospital care in five countries. Health Aff (Millwood). 2001;20(3): 43–53. [DOI] [PubMed] [Google Scholar]
- 31.Smith JG, Morin KH, Lake ET. Association of the nurse work environment with nurse incivility in hospitals. J Nurs Manag. 2018;26(2):219–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Swiger PA, Raju D, Breckenridge-Sproat S, Patrician PA. Adaptation of the Practice Environment Scale for military nurses: a psychometric analysis. J Adv Nurs. 2017;73(9):2219–2236. [DOI] [PubMed] [Google Scholar]
- 33.Raju D, Su X, Patrician PA, Loan LA, McCarthy MS. Exploring factors associated with pressure ulcers: a data mining approach. Int J Nurs Stud. 2015;52(1):102–111. [DOI] [PubMed] [Google Scholar]
- 34.Wasserstein RL, Schirm AL, Lazar NA. Moving to a world beyond “P<0.05”. Am Stat. 2019;73(suppl 1):1–19. [Google Scholar]
- 35.R Core Team. R:A Language and Environment for Statistical Computing [Internet]. Vienna, Austria: R Foundation for Statistical Computing; 2019. https://www.R-project.org/. Accessed March 11, 2020. [Google Scholar]
- 36.Nantsupawat A, Kunaviktikul W, Nantsupawat R, Wichaikhum OA, Thienthong H, Poghosyan L. Effects of nurse work environment on job dissatisfaction, burnout, intention to leave. Int Nurs Rev. 2017;64(1):91–98. [DOI] [PubMed] [Google Scholar]
- 37.Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm. 2008;38(5):223–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wei H, Sewell KA, Woody G, Rose MA. The state of the science of nurse work environments in the United States: a systematic review. Int J Nurs Sci. 2018;5(3):287–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Duffield CM, Roche MA, Blay N, Stasa H. Nursing unit managers, staff retention and the work environment. J Clin Nurs. 2011;20(1–2):23–33. [DOI] [PubMed] [Google Scholar]
- 40.Kutney-Lee A, Germack H, Hatfield L, et al. Nurse engagement in shared governance and patient and nurse outcomes. J Nurs Adm. 2016;46(11):605–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bieber P, Joachim H. Shared governance: a success story. Nurse Lead. 2016;14(1):62–66. [Google Scholar]
- 42.Dunn SL, Arslanian-Engoren C, DeKoekkoek T, Jadack R, Scott LD. Secondary data analysis as an efficient and effective approach to nursing research. West J Nurs Res. 2015;37(10): 1295–1307. [DOI] [PubMed] [Google Scholar]
- 43.Abraham PJ. Developing nurse leaders: a program enhancing staff nurse leadership skills and professionalism. Nurs Adm Q. 2011;35(4):306–312. [DOI] [PubMed] [Google Scholar]
- 44.Goodyear C, Goodyear M. Career development for nurse managers. Nurs Manage. 2018;49(3):49–53. [DOI] [PubMed] [Google Scholar]
- 45.Barnes B, Barnes M, Sweeney CD. Putting the “meaning” in meaningful recognition of nurses: the DAISY award™. J Nurs Adm. 2016;46(10):508–512. [DOI] [PubMed] [Google Scholar]
- 46.Miltner RS, Jukkala A, Dawson MA, Patrician PA. Professional development needs of nurse managers. J Contin Educ Nurs. 2015;46(6):252–258; quiz 259. [DOI] [PubMed] [Google Scholar]
- 47.Westphal JA. Characteristics of nurse leaders in hospitals in the U.S.A. from 1992 to 2008. J Nurs Manag. 2012;20(7): 928–937. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


