Abstract
Background:
Globally, nonpharmaceutical interventions for COVID-19, including stay-at-home policies, limitations on gatherings and closure of public spaces, are being lifted. We explored the effect of lifting a stay-at-home policy on virus resurgence under different conditions.
Methods:
Using confirmed case data from Toronto, Canada, between Feb. 24 and June 24, 2020, we ran a compartmental model with household structure to simulate the impact of the stay-at-home policy considering different levels of compliance. We estimated threshold values for the maximum number of contacts, probability of transmission and testing rates required for the safe reopening of the community.
Results:
After the implementation of the stay-at-home policy, the contact rate outside the household fell by 39% (from 11.58 daily contacts to 7.11). The effective reproductive number decreased from 3.56 (95% confidence interval [CI] 3.02–4.14) on Mar. 12 to 0.84 (95% CI 0.79–0.89) on May 6. Strong adherence to stay-at-home policies appeared to prevent SARS-CoV-2 resurgence, but extending the duration of stay-at-home policies beyond 2 months had little added effect on cumulative cases (25 958 for 65 days of a stay-at-home policy and 23 461 for 95 days, by July 2, 2020) and deaths (1404 for 65 days and 1353 for 95 days). To avoid a resurgence, the average number of contacts per person per day should be kept below 9, with strict nonpharmaceutical interventions in place.
Interpretation:
Our study demonstrates that the stay-at-home policy implemented in Toronto in March 2020 had a substantial impact on mitigating the spread of SARS-CoV-2. In the context of the early pandemic, before the emergence of variants of concern, reopening schools and workplaces was possible only with other nonpharmaceutical interventions in place.
Nonpharmaceutical interventions for COVID-19, including stay-at-home policies, isolation of cases and contact tracing, as well as physical distancing, handwashing and use of protective equipment such as face masks, are effective mitigation strategies for preventing virus spread.1–4 Many studies investigating SARS-CoV-2 transmission and nonpharmaceutical interventions point to the importance of within- and between-household transmission. 5–8 Although stay-at-home policies can help curb spread of SARS-CoV-2 in the community by reducing contacts outside the household,8 they can increase contacts among family members, leading to higher risk within the household, 9 with secondary infection rates in households shown to be as high as 30%–52.7%.5,10 Furthermore, prolonged periods of stay-at-home policies may not be practical because of the essential operations of society, and may directly or indirectly harm the economy and the physical and mental health of individuals.11,12 Therefore, it is important to assess the optimal length of policy implementation for preventing virus resurgence.
During the epidemic, stay-at-home policies have been used to mitigate virus spread. The proportion of people staying at home is a paramount factor for evaluating the effectiveness of this policy implementation. For example, symptomatic individuals, those who tested positive for SARS-CoV-2 infection, and traced contacts are more likely to remain in the home through self-isolation or quarantine than uninfected or asymptomatic individuals. 13 Hence, rates of testing, diagnosis, isolation of cases, contact tracing and quarantine of contacts, as well as public compliance with stay-at-home policies, are essential factors for determining virus transmission and the likelihood of epidemic resurgence after the lifting of restrictive closures.1 To allow for this level of complexity, we developed a household-based transmission model to capture differences in policy uptake behaviour using confirmed case data from Toronto, Canada.
Throughout the pandemic, Canadian provinces and territories have implemented restrictive closures of businesses, schools, workplaces and public spaces to reduce the number of contacts in the population and prevent further virus spread, with these restrictions lifted and reinstituted at various times.14 On Mar. 17, 2020, Ontario declared a state of emergency, with directives including stay-at-home policies.15
We aimed to evaluate the effect of the stay-at-home policy issued in March 2020 on the transmission of SARS-CoV-2 in Toronto, accounting for average household size, the degree of adherence to the stay-at-home policy, and the length of policy implementation. Additionally, on the basis of the average family size and local epidemic data, we estimated the basic reproduction number (R0) and effective reproduction number (Rt) and investigated potential thresholds for the number of contacts, testing rates and use of nonpharmaceutical interventions that would be optimal for mitigating the epidemic. Hence, we conducted simulations of dynamic population behaviour under different reopening and adherence scenarios, to compare different public health strategies in hopes of adding those evaluations to the scientific literature.
Methods
Study design
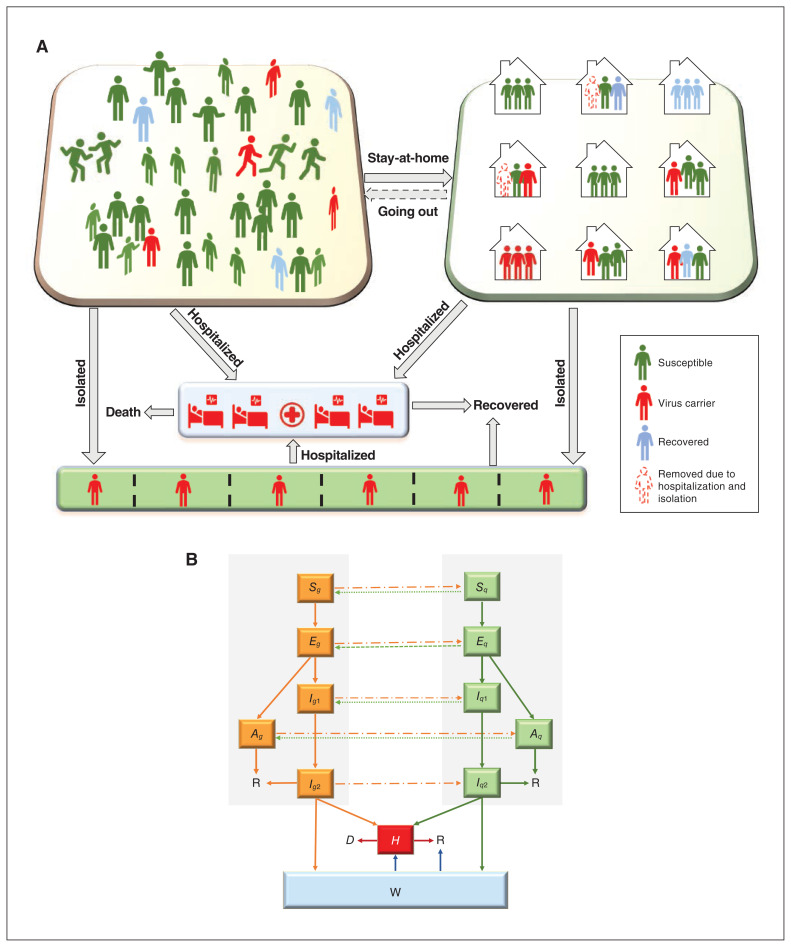
We developed a household-based compartmental model of SARS-CoV-2 transmission dynamics. The model assigns all individuals in the population to different disease states, including susceptible, exposed, infected (subclinical, prodromal or with symptoms), recovered or deceased (Figure 1). Given the importance of asymptomatic and presymptomatic infection in COVID-19,16 both stages are included. We simulated how individuals move between these compartments, including individuals in self-isolation (through hospitalization for the more severe cases, or through testing or contact tracing — in either case, the model assumed they were no longer transmitting the virus). To reflect the local context better, the model incorporated additional complexity by including household structure (i.e., average household size). Demographic changes in the population (i.e., births, deaths) were ignored.
Figure 1:
Transmission model with household structure. Panel A shows the activity and response of different populations. Panel B shows a schematic diagram of the dynamics of COVID-19 in Toronto. Solid lines indicate movement between classes. Dashed lines represent the virus transmission routes. All individuals from groups noncompliant (nq) and compliant (q) with stay-at-home policies are in different disease states, susceptible (Si), exposed (Ei), infected (subclinical [Ai], prodromal [Ii1] or with symptoms [Ii2]), hospitalized (H), isolated (W), recovered (R) or deceased (D) (i = nq, q).
We used the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist to report the findings of our study.17
Study setting and sources
The city of Toronto is the most populous city in Canada, with a recorded population of 2 956 024.18 Its first COVID-19 case was identified in January 2020.19 Toronto activated the Emergency Operations Centre on Mar. 12, 2020, in response to the COVID-19 pandemic, and the stay-at-home policy was enacted.19 The public health response gradually relaxed starting on May 6, 2020,19 after Ontario released the document “A Framework for Reopening our Province” on Apr. 27, 2020.20 The province gradually reopened all workplaces and public spaces. Stage 1 of reopening, which began on May 19, 2020, allowed the opening of select workplaces and some small gatherings. On June 24, 2020, the city of Toronto entered Stage 2 of reopening, opening more workplaces and outdoor spaces, allowing gatherings of up to 10 people.19
To estimate the dynamics of transmission before and after implementation of the stay-at-home policy in Toronto, our deterministic transmission model was calibrated using publicly available data between Feb. 24 and June 24, 2020. We used data on daily new and cumulative confirmed cases by episode date from the open data of the City of Toronto21 and daily new confirmed cases and cumulative deaths by report date from open access epidemiologic data.22 We also used Census data to determine that the average household in Toronto has 2.4 individuals.23
Model assumptions, variables and parameters
Model assumptions, variables and parameters are presented in Tables 1 and 2. Additional details on the model structure and its equations are provided in Appendix 1, Section A, available at www.cmajopen.ca/content/10/2/E367/suppl/DC1.
Table 1:
Model assumptions
| General |
| 1. No birth, death or immigration. |
| 2. We divide the population into 2 groups: one consisting of individuals who follow stay-at-home policies (marked by subscript q) and another consisting of individuals who do not opt for this intervention (marked by subscript nq). Owing to influences of self-protection consciousness and severity of the epidemic, people are assumed to move from one group to another with stay-at-home rate (denoted by q(t)) or going out rate (denoted by g(t)). |
| 3. Each subpopulation is further divided into susceptible (Si(t)), exposed (Ei(t)), asymptomatic (subclinical) infection (Ai(t)), infectious presymptomatic (will eventually show symptoms) (I1 i (t)) and infectious symptomatic (I2 i (t)). |
| 4. Both Ai(t) and I1 i (t) are infectious virus carriers. Individuals in Ai(t) will never show symptoms, while individuals in I1 i (t) develop into symptomatic classes (I2 i (t)) after a specified period. |
| 5. Mild symptomatic infections (I2 i (t)) are a source of infection until recovery. However, they may choose to isolate themselves either at home or other places. If the quarantine is respected well enough, these infections will be fully isolated (W(t)). |
| 6. The fully isolated (W(t)), and the hospitalized (H(t)) who are severely affected do not contribute to infection transmission. |
| Household structure |
| 7. All households contain n (n = 3) individuals, and family members are homogeneously mixing (i.e., contacting each other randomly). |
| 8. The infection rate of the asymptomatic and symptomatic infectious individuals to the susceptible is the same among the household. |
| 9. Every family except for those with symptomatic members has an equal opportunity to be released from quarantine after the stay-at-home policy is relaxed. |
| 10. Households with infected symptomatic individuals will continue to be quarantined after the stay-at-home policy is relaxed. |
| 11. For family members following stay-at-home policies, susceptible Sq(t) will be infected only by infectious individuals in the home Aq(t), Iq1(t) or Iq2(t). |
| 12. When no infections are in a household, the family will be safe and will no longer be involved in the transmission of COVID-19. |
Table 2:
Model variables and parameters*
| Notation | Description | Value | Sources |
|---|---|---|---|
| Variables and their initial values | |||
| Inq2(t) | The number of stay-at-home policy–noncompliant infected individuals with symptoms at day t | 10 | Data21 |
| Sq(t) | The number of stay-at-home policy–compliant susceptible individuals at day t | (n – 1) * 3 | Calculated |
| Eq(t) | The number of stay-at-home policy–compliant exposed individuals at day t | 0 | Assumed |
| Aq(t) | The number of stay-at-home policy–compliant subclinical infected individuals at day t | 0 | Assumed |
| Iq1(t) | The number of stay-at-home policy–compliant prodromal infected individuals at day t | 0 | Assumed |
| Iq2(t) | The number of stay-at-home policy–compliant infected individuals with symptoms at day t | 3 | Data21 |
| H(t) | The number of severe infected individuals in hospitals at day t | 0 | Data21 |
| W(t) | The number of isolated individuals at day t | 0 | Assumed |
| R(t) | The number of recovered individuals at day t | 13 | Data21 |
| D(t) | The number of deaths at day t | 0 | Data21 |
| P | Total population in Toronto | 2 956 024 | Data18 |
| Snq(t) | The number of stay-at-home policy–noncompliant susceptible individuals at day t | 2 955 988 | Estimated |
| Enq(t) | The number of stay-at-home policy–noncompliant exposed individuals at day t | 20 | Estimated |
| Anq(t) | The number of stay-at-home policy–noncompliant subclinical infected individuals at day t | 1 | Estimated |
| Inq1(t) | The number of stay-at-home policy–noncompliant prodromal infected individuals at day t | 2 | Estimated |
| Parameter estimation for COVID-19 in Toronto | |||
| τ1 | Average time spent in the exposed state, Enq, Eq, d | 4 | Refs.24,25 |
| τ2 | Average time spent in prodromal infected state Inq1, Iq1, d | 3 | Ref.25 |
| a | Proportion of infected with prodromal infection | 0.9530 | Ref.2 |
| γa | Recovery rate of subclinical infected | 0.0700 | Ref.2 |
| γm | Recovery rate of infections with mild symptoms | 1/14 | Ref.26 |
| γ | Recovery rate of hospitalized infections | 0.0357 | Ref.26 |
| c 0 | Contact rate before stay-at-home policy implemented, 1/day | 11.58 | Ref.27 |
| T 1 | Time when the stay-at-home policy is implemented | Mar. 12 | Ref.19 |
| T 2 | Time when the preopening begins | May 6 | Ref.19 |
| T 3 | Time when the reopening of stage 1 begins | May 19 | Ref.19 |
| T 4 | Time of reopening of stage 2 begins | June 24 | Ref.19 |
| n | Average number of household population | 2–3 | Ref.23 |
| q(t) | Stay-at-home rate of Snq, Enq, Anq and Inq1 | – | |
| dc(t) | Completion ratio of diagnosis of all symptomatic infections | – | Refs.21,22 |
| g(t) | Going out rate of Sq, Eq, Aq and Iq1 | – | |
| qnq2(t) | Quarantined rate of Inq2 | – | |
| Q(t) | The proportion of population in stay-at-home state to the total population at time t | – | |
| Estimated parameters | |||
| βnq | Probability of transmission per contact outside household | Feb. 24–May 18: 3.2984e-02 May 19–June 24: 1.9000e-02† |
|
| μ | Exponential decreasing rate of contact rate due to stay-at-home policy | 7.5000e-01 | |
| βq | Infection rate of stay-at-home policy–compliant susceptible within household | 1.5030e-02 | |
| Q | Stay-at-home rate of Snq, Enq, Anq and Inq1 before stay-at-home policy implemented | 3.0001e-04 | |
| ɛ | Adjust parameter | 7.0000e-01 | |
| G | Going out rate of Sq, Eq, Aq and Iq1 during the period of stay-at-home policy implementation | 1.0000e-04 | |
| Φh | Hospitalization rate of Inq2, Iq2 | 0.0152 | |
| Φi | Isolation rate of Inq2, Iq2 | 3.9978e-02 | |
| d | Disease-induced death rate in hospitals | 3.4000e-02 | |
| Q | Maximum compliance proportion of stay-at-home policy | 6.5058e-01 | |
| 1/ΔTQ | The average transition rate of stay-at-home policy compliance | 1/9 | |
| G 0 | Maximum going out proportion in the period of May 6 to May 19 | 1.5000e-01 | |
| G 1 | Maximum going out proportion in the period of May 20 to June 24 | 3.0000e-01 | |
| G 2 | Maximum going out proportion in the period of reopening Stage 2 starting June 24 | 3.0000e-01 (assumed) | |
| ΔTG | The average time from stay-at-home policy relaxed to individuals going out | 3 (assumed) | |
n is the average household size.
e-0x denotes the 10 to the power of –x.
Compliance with the stay-at-home policy
To capture differences in policy uptake, we divided the population into 2 subgroups: individuals following the stay-at-home policy, indicated by a subscript q, and those not following it, indicated by a subscript nq. To describe the process of policy implementation, there are some common simplification methods: introducing different parameters before and after policy implementation,3 or considering them as either evenly distributed or dynamic.28 However, because of the influence of a variety of factors including individual preferences, as well as different socioeconomic and occupational characteristics, not all people will fully adhere to the stay-at-home policy. Hence, we assumed compliance to be a gradual process for individuals in different disease states once the stay-at-home policy was enacted on Mar. 12, 2020.19 The reaction time to compliance of individuals in the susceptible, exposed and infected groups is a random variable that follows a Γ distribution, describing the enforcement process of stay-at-home policies. We derived the daily stay-at-home rate, which is described in Appendix 1, Section A2. The movement between groups compliant and noncompliant with the stay-at-home policy was modelled as the policy and time varied.
Symptomatic testing
In Toronto at the beginning of the pandemic, testing was mainly provided to individuals showing symptoms.13 It takes time for infection to cause symptoms, for an individual to get tested for SARS-CoV-2 infection, and for a positive test to return and ultimately enter the case data. With limited testing resources and wait times, there is a time lag between the episode (onset) date and the reporting date. A delay in case diagnosis results in a delay in implementing control measures, increasing the risk of transmission.
To capture the effects of this lag in the model, we defined the ratio of symptomatic diagnosis completion (dc), calculated as the ratio of the cumulative number of confirmed cases by reported date on day t to that by episode date on day t. We examined the trend of dc in Toronto from Feb. 24 to June 24, 2020 (Appendix 1, Section C1). This quantity was used to inform the stay-at-home rate of detected infectious people (i.e., the rate at which they follow isolation recommendations).
Statistical analysis
Parameter values including the per-contact transmission probability, the maximum compliance proportion of the stay-at-home policy, and the transition rate for compliance with the stay-at-home policy listed in Table 2 were estimated by minimizing the sum of squared differences29 between the model’s estimates of the cumulative confirmed cases and cumulative deaths and data on these 2 indicators.
We compared the total infections with or without a stay-at-home policy, and the change of transmission risk over time with implementation of the stay-at-home policy under the assumption of different average household sizes, ranging from 2 to 3, to make our model more applicable to a variety of jurisdictions. We also explored the effect of the stay-at-home policy on the epidemic for different degrees of compliance and the length of the stay-at-home policy. We then reported the trajectories of different reopening scenarios and the threshold for safe opening. Analyses were carried out using Matlab (R2020a) and R (version 4.0.1).
Risk indices and reproduction numbers
We calculated the model-free and model-based basic reproduction number R0, based on the Toronto case data by episode date21,22 and total infection data (including symptomatic and asymptomatic infections) generated by the model, respectively, using an exponential growth method.30,31 The effective reproduction number Rt was estimated by using the method shown elsewhere,32,33 assuming a Γ distributed serial interval of 7.5 (standard deviation 3.4) days.24 We then defined a novel risk index after reopening (Rreopen) to evaluate the risk of reopening by calculating the reproduction number applying a next generation matrix34 when the stay-at-home policy is weakened (Appendix 1, Section B).
Ethics approval
This study is exempt from research ethics approval, as it uses publicly available data.
Results
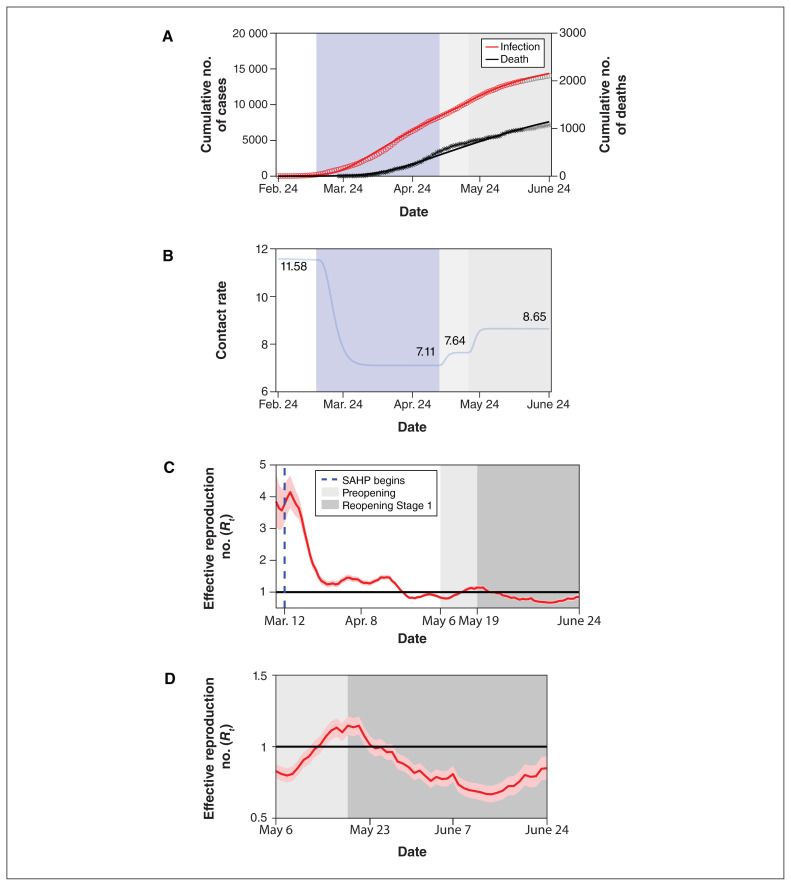
Parameter estimation indicated that, at most, 65.1% of Toronto residents stayed at home because of the stay-at-home policy, after which the contact rate declined by 39%. After Stage 1 reopening of the city on May 19, 2020, the contact rate gradually increased to 8.65 daily contacts, corresponding to a 22% increase compared with the contact rate during the period of the stay-at-home policy (Figure 2).
Figure 2:
SARS-CoV-2 cumulative incidence and deaths, and transmission over time. (A) Data fitting of SARS-CoV-2 infection in Toronto from Feb. 24 to June 13, 2020. The red circles (infection) and black asterisks (death) represent observed data. The grey circles (infection) and grey asterisks (death) represent data validation from June 14 to June 24. The solid curves are model simulations. (B) Changes in contact rates over time. Panels C and D show estimates of the daily effective reproduction number (Rt) of SARS-CoV-2 over time based on the episode date (C) from Mar. 8 to May 6 and (D) from May 6 to June 24, with 95% confidence intervals represented by the pink shaded area. The dark solid line indicates the critical threshold of Rt = 1. The blue dashed line represents the start of the stay-at-home policy. Shaded bars show the dates of implementation of the stay-at-home policy (light blue), preopening (light grey) and reopening Stage 1 (medium grey). The white in panels A and B represent the time period without any public health control measures. The white in panel C represents the time period before and after the implementation of stay-at-home policy. All dates are in 2020. Note: SAHP = stay-at-home policy.
Estimation of reproduction numbers
The estimation result of the model-free R0 in Toronto was 1.45 (95% confidence interval [CI] 1.43–1.48), and the model-based R0 was 2.36 (95% CI 2.28–2.45). The Rt was calculated by using episode data varied before and after the implementation of the stay-at-home policy, and it gradually decreased from 3.56 (95% CI 3.02–4.14) on Mar. 12, 2020, to below 1.00 on Apr. 22, 2020, and to 0.84 (95% CI 0.79–0.89) on May 6, 2020, corresponding to a 76% (95% CI 71%–81%) reduction in transmissibility (Figure 2). After entering the Stage 1 reopening on May 19, 2020, with the strengthened use of face coverings, the Rt showed a clear downward trend initially and gradually decreased to 0.67 (95% CI 0.61–0.73) on June 14, 2020, although the contact rate was expected to be higher. By the end of reopening Stage 1, the Rt had increased to 0.85 (95% CI 0.77–0.93).
Effect of the stay-at-home policy
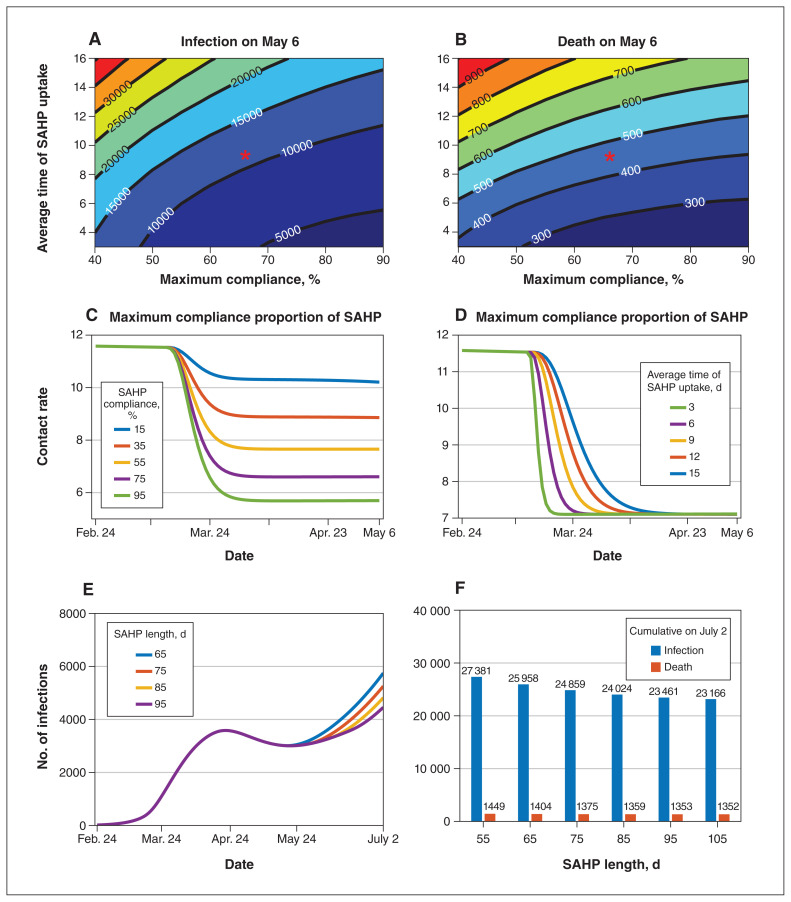
Overall, the stay-at-home policy reduced the average contact rate outside the household (Figures 2, 3 and 4), which affected overall transmission. A large reduction in infections and deaths by May 6, 2020, when the stay-at-home policy ended, was visible if a large proportion of individuals complied with the stay-at-home policy within a short period (Figure 3). If 75% of the population were compliant within 56 days, we could expect to see 5167 cases and 215 deaths by May 6, 2020, decreased by 63.2% and 57.4%, respectively, compared with 55% compliance. The mitigation effect on the epidemic could also be seen if the average transition rate of compliance with the stay-at-home policy was increased. The length of implementation of the stay-at-home policy did not affect the spread of the infection significantly when it was increased from 65 days to 95 days, where the cumulative number of infections and cumulative deaths by July 2 decreased by 9.6% and 3.6%, respectively.
Figure 3:
Effect of the stay-at-home policy with different maximum compliance proportion, average time and length of the stay-at-home policy. Contour plot of cumulative infections (A) and deaths (B) on May 6, 2020, with different average duration of stay-at-home policy uptake and maximum compliance proportions. Red asterisks represent the parameter values estimated from data and are used in simulations. The contact rate changes over time (C) under different compliance proportions of the stay-at-home policy when the average time of the stay-at-home policy uptake is 9 days (this is the inverse of the average transition rate of the stay-at-home policy compliance) and (D) under different average durations of stay-at-home policy uptake when the maximum compliance proportion is 65%. (E) The number of daily infections and (F) cumulative number of infections (blue bars) and deaths (orange bars) on July 2, 2020, with different lengths of the stay-at-home policy duration: 55 days, 65 days, 75 days, 85 days, 95 days, 105 days. All dates are in 2020. Note: SAHP = stay-at-home policy.
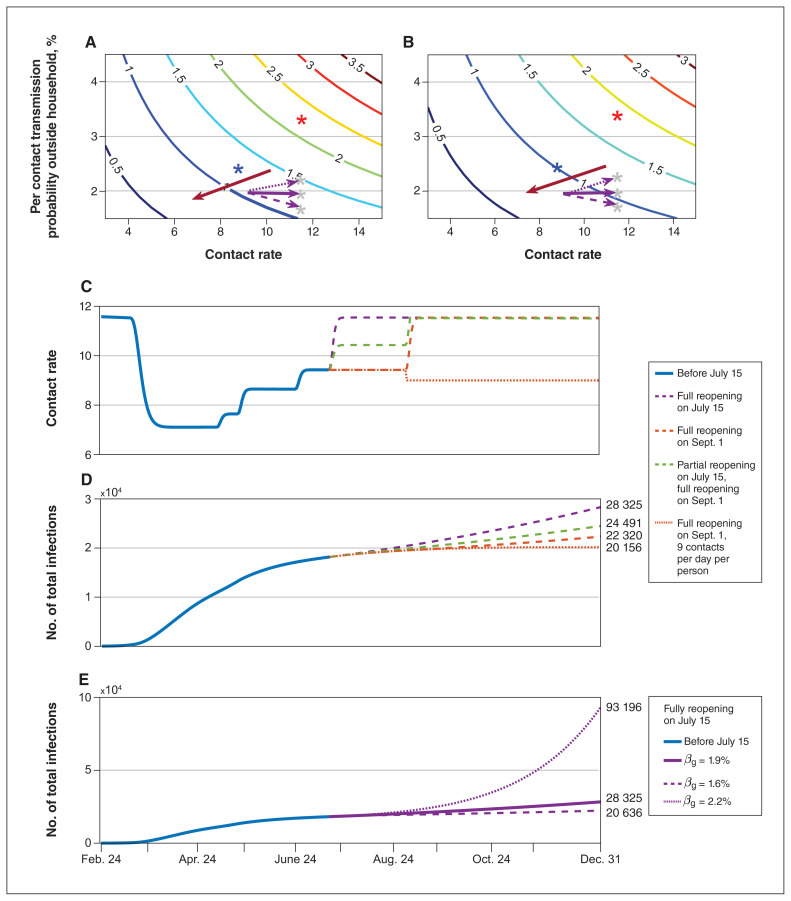
Figure 4:
Risk of reopening under different reopening scenarios. Contour plot of Rreopen with different per-contact transmission probability outside the household (βnq) and contact rate under completion ratio of symptomatic diagnosis is (A) 40%; (B) 97%. The red asterisk is the initial status of βnq and contact rate, and the blue asterisk is the state on June 24. The grey asterisk is the possible state after completely reopening in simulation E. The red arrow shows the low-risk direction with the safe reopening. (C) The change in contact rates and (D) cumulative infections over time with different reopening scenarios: fully reopening on July 15 (purple dashed line), partially reopening on July 15 and then fully reopening on Sept. 1 (green dashed line), fully reopening on Sept. 1 (orange dashed line), fully reopening on Sept. 1 while maintaining a contact rate of 9 (orange dotted line), while βnq is 1.9%. (E) The number of cumulative infections over time with βnq = 1.6% (dashed line), 1.9% (solid line, current state), 2.2% (dotted line) when fully reopening on July 15. Rreopen = the transmission risk after fully reopening. All dates are in 2020.
The cumulative number of infections dropped significantly compared with that without the stay-at-home policy (Appendix 1, Section C2). To make our model more applicable to other jurisdictions, we examined the stay-at-home policy scenario for average household sizes of 3 and 2 individuals, whereby the number of infections was 12.5 and 25.9 times greater without the stay-at-home policy compared to with the stay-at-home policy, respectively. For an average household of 3 individuals, the stay-at-home policy resulted in 11 people infected per 1000 households by May 6, 2020, compared with 4 per 1000 for a household size of 2. However, in early phases of implementation of the stay-at-home policy, owing to the higher risk of transmission within families, the number of infections was higher than when there was no stay-at-home policy. The number of infections was even higher for larger household sizes, where the Rt increased as the maximum compliance proportion increased after 1 day of the implementation of the stay-at-home policy, but decreased after 10 days.
Threshold of contact rate and safe reopening
To avoid an epidemic resurgence after the city’s reopening, it is necessary to reduce the contact rate and probability of transmission per contact outside of the household. With a 1.9% transmission risk, the contact rate needs to be reduced to 11 when the symptomatic diagnosis completion ratio is 97% (Figure 4). However, if the symptomatic diagnosis completion ratio declines to 40%, the contact rate should be maintained below 9. In general, with increased risk of transmission, the contact rate must remain low.
Different reopening strategies can result in different epidemic trajectories, including a resurgence as we observed in the second wave in Toronto after August 2020. Using the Toronto stay-at-home policy issued in 2020 as an example, our model indicates that a safe reopening of public spaces could be achieved when the contact rate is reduced to 9, while maintaining strict physical distancing (Figure 4). With a 97% diagnosis completion ratio and 11.58 daily contacts, if the probability of transmission per contact was 2.2%, Rreopen was 1.2. This suggests that under full reopening conditions, the city still faced the risk of epidemic resurgence. On the other hand, if the per-contact transmission probability decreased to 1.6%, Rreopen was 0.87, and reopening was safe. Here, the claim is based on the situation in 2020.
Interpretation
Using our compartmental model with household structure, we analyzed the effect of the stay-at-home policy on SARS-CoV-2 transmission using Toronto as a case study. Stay-at-home policies have helped to control the epidemic and prevent the collapse of the health care system. However, in cities such as Wuhan, China, the stay-at-home policy was not effective in early stages of the lockdown.2 This phenomenon could be related to the average household size of 3.5 in Wuhan,35 larger than the household size of 2.4 in Toronto.23 Hence, the implementation of a stay-at-home policy needs to be adapted to local conditions. For areas with large average family size, additional measures, such as establishing temporary shelter hospitals, may be needed to reduce transmission.2 Moreover, a lower probability of transmission, provided by keeping mandatory or highly recommended use of nonpharmaceutical interventions such as physical distancing and mask-wearing,36 particularly in indoor public places,37 contributes substantially to epidemic control.
Our model-based R0 estimation captured asymptomatic transmission, which was higher than the estimate derived by case data, which underestimated R0. After Toronto reopened to Stage 1 on May 19, 2020,19 the Rt gradually declined, possibly owing to the strengthening of government regulations on personal protective equipment (PPE) use, as well as public messaging around mask-wearing, hand hygiene and physical distancing.19 Although the contact rate increased after reopening, the enhancement of PPE appears to have reduced the probability of infection, thereby reducing the risk of epidemic resurgence.
We constructed a new indicator, symptomatic diagnosis completion ratio (dc), which reflects the increased efficiency of public health response as the pandemic unfolded. We also observed that the diagnosis completion ratio affected transmission, as measured by the Rt being below 1 at reopening. Indeed, with a small ratio, public health agencies need to strengthen nonpharmaceutical interventions and work to decrease the number of contacts to avoid resurgence.
We found that full reopening without other strengthened nonpharmaceutical interventions leads to resurgence. When the average number of contacts in the population exceeded the threshold found in our analysis after reopening, the number of cases rapidly increased, explaining the second wave in Toronto. Such model-driven thresholds can act as early triggers for policy-makers and allow for dynamic intervention to mitigate the spread of SARS-CoV-2. Our model structure further allows for the generation of long-term projections to support decision-making. Though our analysis is a case study of Toronto, it is applicable to regions where the demographic characteristics are similar to those of this city and can also provide some information to any possible new emerging infections. Our simulation analysis is retrospective, however, and the results should be interpreted as reflecting the 2020 situation in Toronto.
Limitations
Household size and composition vary greatly within Toronto and in other regions. The mitigating effect of stay-at-home policies should be re-examined when applying to other areas with varying household sizes. The real-time serial interval may change with policy implementation, 38 which was not considered in our Rt calculation. In addition, age structure was not incorporated, as we aimed to unpack the impact of the stay-at-home policy on transmission considering the household as a whole, even though there is emerging evidence suggesting different transmission among adults and children, with children being less likely to acquire and transmit the infection.39 Moreover, the higher transmissibility of emerging variants of concern is concerning.40 We have considered school and community reopening with age structure;41 therefore, as a further work, we will consider the variant of concern and its impact on school opening to support public health decision-making.
Conclusion
We explored the mitigating effect of a stay-at-home policy on the spread of SARS-CoV-2 by using a compartmental model that incorporates household structure and nonpharmaceutical interventions, with Toronto as a case study. Our results reflect the 2020 situation in Toronto and have no current relevance to decision-making. We found that the effect of the stay-at-home policy was almost wholly evident after 2 months from implementation. Our study demonstrated that to control outbreaks, a stay-at-home policy, combined with physical distancing, PPE, and effective case diagnosis, contact tracing and isolation, is an effective strategy. Our results show that to reduce the risk of infection and transmission, if one of the control measures is relaxed, others may need to be strengthened. Our analysis of thresholds, including contact rates, can be applied to a variety of settings and can provide early triggers for dynamic public health response.
Supplementary Material
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: Huaiping Zhu, Pei Yuan, Juan Li, Iain Moyles, Nicholas Ogden, Jacques Bélair and Jane Heffernan contributed to the research design. Qi Li, Elena Aruffo, Pei Yuan, Juan Li, Tingting Zheng and Yi Tan contributed to the literature search. Evgenia Gatov, Sarah Collier, Tingting Zheng, Qi Li, Yi Tan, Pei Yuan and Juan Li contributed to data collection. Huaiping Zhu and all other authors contributed to the modelling. Jun Li, Pei Yuan, Juan Li, Elena Aruffo and Huaiping Zhu contributed to the model analysis. Pei Yuan, Juan Li, Elena Aruffo, Tingting Zheng, Yi Tan and Jun Li contributed to the simulations. Pei Yuan, Juan Li, Elena Aruffo, Qi Li, Tingting Zheng, Yi Tan and Huaiping Zhu prepared the draft. Pei Yuan, Juan Li, Elena Aruffo, Iain Moyles, Evgenia Gatov, Huaiping Zhu, Nicholas Ogden, Beate Sander, Jane Heffernan, Sarah Collier, Julien Arino, Jacques Bélair, James Watmough and Jude Dzevela Kong contributed to writing and revising the article. Huaiping Zhu supervised the study. Pei Yuan, Juan Li, Elena Aruffo contributed equally as co–first authors. All authors gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Funding: This research was supported by the Canadian Institutes of Health Research, the Canadian COVID-19 Math Modelling Task Force (Huaiping Zhu, Nicholas Ogden, Beate Sander, Jane Heffernan, Julien Arino, Jacques Bélair, James Watmough and Jude Dzevela Kong), the Natural Sciences and Engineering Research Council of Canada (Huaiping Zhu, Jane Heffernan, Julien Arino, Jacques Bélair, James Watmough, Jude Dzevela Kong and Iain Moyles), the York University Research Chairs program (Huaiping Zhu) and the Chinese Scholarship Council (Pei Yuan, Qi Li, Tingting Zheng and Yi Tan).
Data sharing: The data used for this study are published by Toronto Public Health and Berry et al., and are publicly available at the following links: https://open.toronto.ca/dataset/covid-19-cases-in-toronto/ (accessed 2021 Mar. 24) and https://github.com/ishaberry/Covid19Canada (accessed 2021 Mar. 24).
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/10/2/E367/suppl/DC1.
References
- 1.Ng V, Fazil A, Waddell LA, et al. Projected effects of nonpharmaceutical public health interventions to prevent resurgence of SARS-CoV-2 transmission in Canada. CMAJ. 2020;192:E1053–64. doi: 10.1503/cmaj.200990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li J, Yuan P, Heffernan J, et al. Fangcang shelter hospitals during the COVID-19 epidemic, Wuhan, China. Bull World Health Organ. 2020;98:830–41D. doi: 10.2471/BLT.20.258152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tang B, Xia F, Tang SY, et al. The effectiveness of quarantine and isolation determine the trend of the COVID-19 epidemics in the final phase of the current outbreak in China. Int J Infect Dis. 2020;95:288–93. doi: 10.1016/j.ijid.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ludwig A, Berthiaume P, Orpana H, et al. Assessing the impact of varying levels of case detection and contact tracing on COVID-19 transmission in Canada during lifting of restrictive closures using a dynamic compartmental model. Can Commun Dis Rep. 2020;46:409–21. doi: 10.14745/ccdr.v46i1112a08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Z, Ma W, Zheng X, et al. Household transmission of SARS-CoV-2. J Infect. 2020;81:179–82. doi: 10.1016/j.jinf.2020.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pellis L, Ferguson NM, Fraser C. Epidemic growth rate and household reproduction number in communities of households, schools and workplaces. J Math Biol. 2011;63:691–734. doi: 10.1007/s00285-010-0386-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.House T, Keeling MJ. Deterministic epidemic models with explicit household structure. Math Biosci. 2008;213:29–39. doi: 10.1016/j.mbs.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Sjödin H, Wilder-Smith A, Osman S, et al. Only strict quarantine measures can curb the coronavirus disease (COVID-19) outbreak in Italy, 2020. Euro Surveill. 2020;25:2000280. doi: 10.2807/1560-7917.ES.2020.25.13.2000280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prem K, Liu Y, Russell TW, et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261–70. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baker JM, Nakayama JY, O’Hegarty M, et al. SARS-CoV-2 B.1.1.529 (Omicron) variant transmission within households — four U.S. jurisdictions, November 2021–February 2022. MMWR Morb Mortal Wkly Rep. 2022;71:341–346. doi: 10.15585/mmwr.mm7109e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–20. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mandel A, Veetil V. The economic cost of COVID lockdowns: an out-of-equilibrium analysis. Econ Disaster Clim Chang. 2020 June 19; doi: 10.1007/s41885-020-00066-z. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.COVID-19. Toronto: City of Toronto; [accessed 2021 Mar. 24]. updated 2021 Dec. 28. Available: https://www.toronto.ca/home/covid-19/ [Google Scholar]
- 14.Coronavirus disease (COVID-19) Ottawa: Public Health Agency of Canada; [accessed 2020 May 31]. modified 2021 Dec. 23. Available: https://www.canada.ca/en/public-health/services/diseases/coronavirus-disease-covid-19.html. [Google Scholar]
- 15.Ontario enacts declaration of emergency to protect the public [news release] Toronto: Ontario Ministry of Health; 2020. Mar 17, [accessed 2020 Apr. 8]. Available: https://news.ontario.ca/en/release/56356/ontario-enacts-declaration-of-emergency-to-protect-the-public. [Google Scholar]
- 16.Zou L, Ruan F, Huang M, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–9. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Husereau D, Drummond M, Petrou S, et al. ISPOR Health Economic Evaluation Publication Guidelines-CHEERS Good Reporting Practices Task Force. Consolidated health economic evaluation reporting standards (CHEERS): explanation and elaboration — a report of the ISPOR health economic evaluations publication guidelines good reporting practices task force. Value Health. 2013;16:231–50. doi: 10.1016/j.jval.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 18.Toronto at a glance. Toronto: City of Toronto; [accessed 2020 Apr. 22]. Available: https://www.toronto.ca/city-government/data-research-maps/toronto-at-a-glance/ [Google Scholar]
- 19.News releases & other resources. Toronto: City of Toronto; [accessed 2020 July 30]. Available: https://www.toronto.ca/news/ [Google Scholar]
- 20.A plan to safely reopen Ontario and manage COVID-19 for the long-term. Toronto: Ontario Ministry of Health; [accessed 2020 June 28]. Available: https://www.ontario.ca/page/reopening-ontario-whats-each-stage. [Google Scholar]
- 21.Open data catalogue: COVID-19 cases in Toronto. Toronto: City of Toronto; [accessed 2021 Mar. 24]. Available: https://open.toronto.ca/dataset/covid-19-cases-in-toronto/ [Google Scholar]
- 22.Berry I, Soucy J-PR, Tuite A, et al. Open access epidemiologic data and an interactive dashboard to monitor the COVID-19 outbreak in Canada [letter] CMAJ. 2020;192:E420. doi: 10.1503/cmaj.75262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Census Profile, 2016 Census. Ottawa: Statistics Canada; [accessed 2020 Mar. 20]. modified 2021 Oct 27. Available https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/Page.cfm?Lang=E&Geo1=CSD&Code1=3520005&Geo2=PR&Data=Count&B1=All. [Google Scholar]
- 24.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan,8 China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2) Science. 2020;368:489–93. doi: 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coronavirus disease 2019 (COVID-19) situation report – 170. Geneva: World Health Organization; 2020. [accessed 2020 July 15]. Available https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200708-covid-19-sitrep-170.pdf?sfvrsn=bca86036_2. [Google Scholar]
- 27.Tang B, Scarabel F, Bragazzi NL, et al. De-escalation by reversing the escalation with a stronger synergistic package of contact tracing, quarantine, isolation and personal protection: feasibility of preventing a COVID-19 rebound in Ontario, Canada, as a case study. Biology (Basel) 2020;9:100. doi: 10.3390/biology9050100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moyles IR, Heffernan JM, Kong JD. Cost and social distancing dynamics in a mathematical model of COVID-19 with application to Ontario, Canada. R Soc Open Sci. 2021;8:201770. doi: 10.1098/rsos.201770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lagarias JC, Reeds JA, Wright MH, et al. Convergence properties of the Nelder–Mead simplex method in low dimensions. SIAM J Optim. 1998;9:112–47. [Google Scholar]
- 30.Wallinga J, Lipsitch M. How generation intervals shape the relationship between growth rates and reproductive numbers. Proc Biol Sci. 2007;274:599–604. doi: 10.1098/rspb.2006.3754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Obadia T, Haneef R, Boëlle P-Y. The R0 package: a toolbox to estimate reproduction numbers for epidemic outbreaks. BMC Med Inform Decis Mak. 2012;12:147. doi: 10.1186/1472-6947-12-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wallinga J, Teunis P. Different epidemic curves for severe acute respiratory syndrome reveal similar impacts of control measures. Am J Epidemiol. 2004;160:509–16. doi: 10.1093/aje/kwh255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cori A, Ferguson NM, Fraser C, et al. A new framework and software to estimate time-varying reproduction numbers during epidemics. Am J Epidemiol. 2013;178:1505–12. doi: 10.1093/aje/kwt133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van den Driessche P, Watmough J. Reproduction numbers and sub-threshold endemic equilibria for compartmental models of disease transmission. Math Biosci. 2002;180:29–48. doi: 10.1016/s0025-5564(02)00108-6. [DOI] [PubMed] [Google Scholar]
- 35.2018 Wuhan Statistic Yearbook. Hubei Provincial Bureau of Statistics; 2019. [accessed 2020 July 20]. Available: http://tjj.hubei.gov.cn/tjsj/sjkscx/tjnj/gsztj/whs/ [Google Scholar]
- 36.Leung NHL, Chu DKW, Shiu EYC, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26:676–80. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Your guide to masks. Atlanta: Centers for Disease Control and Prevention; [accessed 2020 Apr. 8]. updated 2021 Oct 25. Available https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/about-face-coverings.html. [Google Scholar]
- 38.Ali ST, Wang L, Lau EHY, et al. Serial interval of SARS-CoV-2 was shortened over time by nonpharmaceutical interventions. Science. 2020;369:1106–9. doi: 10.1126/science.abc9004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Viner RM, Mytton OT, Bonell C, et al. Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: a systematic review and meta-analysis. JAMA Pediatr. 2021;175:143–56. doi: 10.1001/jamapediatrics.2020.4573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tracking SARS-CoV-2 variants. Geneva: World Health Organization; [accessed 2021 Apr. 20]. updated 2022 Jan 10. Available https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/ [Google Scholar]
- 41.Pei Y, Elena A, Evgenia G, et al. School and community reopening during the COVID-19 pandemic: a mathematical modelling study. Royal Society Open Science. 2022;9:211883. doi: 10.1098/rsos.211883. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.