Key Points
Question
Is rotating night shift work prospectively associated with healthy aging that simultaneously considers chronic diseases, cognitive and physical function, and mental health?
Findings
In a large cohort study of 46 318 female nurses, long-term rotating night shift work was associated with modestly decreased odds of healthy aging after 24 years of follow-up.
Meaning
In addition to the existing literature suggesting that shift work is associated with increased mortality, the findings of this study further suggest that shift work is also associated with worse overall health among women who survive to older ages.
This cohort study of female nurses examines the association between rotating night shift work and healthy aging after 24 years of follow-up in the Nurses’ Health Study.
Abstract
Importance
Rotating night shift work is associated with higher mortality. Whether it is also associated with overall health among those who survive to older ages remains unclear.
Objective
To examine whether rotating night shift work is associated with healthy aging after 24 years of follow-up in the Nurses’ Health Study, a cohort study among registered female nurses.
Design, Setting, and Participants
For this cohort study, a composite healthy aging phenotype was ascertained among 46 318 participants who were aged 46 to 68 years and free of major chronic diseases in 1988 when the history of night shift work was assessed. In a secondary analysis in which cognitive function decline was considered in the healthy aging definition, 14 273 nurses were involved. Data were analyzed from March 1 to September 30, 2021.
Exposures
Duration of rotating night shift work.
Main Outcomes and Measures
Healthy aging was defined as reaching at least 70 years of age and being free of 11 major chronic diseases, memory impairment, physical limitation, or deteriorated mental health.
Results
Of 46 318 female nurses (mean [SD] age at baseline, 55.4 [6.1] years), 3695 (8.0%) achieved healthy aging after 24 years of follow-up. After adjusting for established and potential confounders, compared with women who never worked rotating night shifts, the odds of achieving healthy aging decreased significantly with increasing duration of night shift work. The odds ratios were 0.96 (95% CI, 0.89-1.03) for 1 to 5 years, 0.92 (95% CI, 0.79-1.07) for 6 to 9 years, and 0.79 (95% CI, 0.69-0.91) for 10 or more years of night shift work (P = .001 for trend). This association did not differ substantially by age and lifestyles and was consistent for 4 individual dimensions of healthy aging. Results were similar in a secondary analysis, with an odds ratio of 0.73 (95% CI, 0.60-0.89; P < .001 for trend) comparing 10 or more years of night shift work vs no night shift work.
Conclusions and Relevance
In this cohort study, rotating night shift work was associated with decreased probability of healthy aging among US female nurses. These data support the notion that excess night shift work is a significant health concern that may also lead to deteriorated overall health among older individuals.
Introduction
Night shift work is becoming increasingly common worldwide, and 15% to 33% of the working population1,2,3 are engaged in night shift work, especially among health care workers.2 Previous studies have suggested that night shift work may result in circadian disruption, sleep disturbances, and other behavioral changes,4 leading to increased risk of chronic diseases,4,5,6,7,8,9,10,11 mental disorders,1,12,13 cognition impairment,14,15 and mortality.14,16 The World Health Organization’s International Agency for Research on Cancer concludes that shift work is probably carcinogenic for humans.17,18
However, although circadian rhythms are considered a universal and fundamental mechanism in essentially every physiologic process across the entire human body,19,20 existing studies7,8,9,10,11,13,15 on rotating night shift work have primarily focused on individual health outcomes, and less is known regarding its association with overall health. Particularly, given the interplay between aging and the circadian clock,19,21 it is critical to understand the association between night shift work and overall health in older populations. As the aging population increases in the US and other countries, it is critical to identify and examine modifiable factors, such as night shift work, that are potentially associated with the overall health status among older individuals. Depending on the definition of healthy aging,22,23,24 an estimated one-third of the population older than 60 years can be considered as healthy agers. In this prospective study, we leveraged the longitudinal follow-up data from the Nurses’ Health Study to examine the association of duration of rotating night shift work with heathy aging (as measured by a full spectrum of health outcomes) among women.
Methods
Study Design and Participants
The Nurses’ Health Study is a prospective cohort study of 121 701 US registered nurses aged 30 to 55 years that was established in 1976. Follow-up questionnaires have been used to update the information every 2 years. The cumulative follow-up rate was greater than 90% in this cohort.25 Women were asked to report their history of rotating night shift work in 1988, which was treated as baseline in the current cohort study. In our primary analysis, the end of follow-up was through 2012,26 when the overall health status, including chronic diseases, physical function, mental health, and memory function, was evaluated (Figure). Of 90 042 women who answered the 1988 questionnaire and were 46 years or older in 1988 (ie, could reach 70 years of age in 2012), we excluded those who had any of 11 main chronic diseases at baseline (n = 17 872), had missing information on rotating night shift work (n = 13 552), or had missing data on healthy aging phenotype in 2012 (n = 12 300), leaving 46 318 women (age range, 46-68 years) in our primary analyses. Participants excluded for missing information on healthy aging did not differ substantially from those included with regard to distributions of major potential confounders (eTable 1 in the Supplement). In our secondary analysis, healthy aging phenotype was defined among 19 415 women who completed a cognitive function test when they reached 70 years of age in 1995 to 2000.25 After excluding women with missing information on rotating night shift work history, any of 11 main chronic diseases at baseline, or healthy aging phenotype, 14 273 women were included (eFigure in the Supplement). The study protocol was approved by the institutional review boards of the Brigham and Women’s Hospital and the Harvard T. H. Chan School of Public Health. Participants provided implied consent by returning the questionnaires. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Figure. Study Design for Rotating Night Shift Work and Healthy Aging in the Nurses’ Health Study.
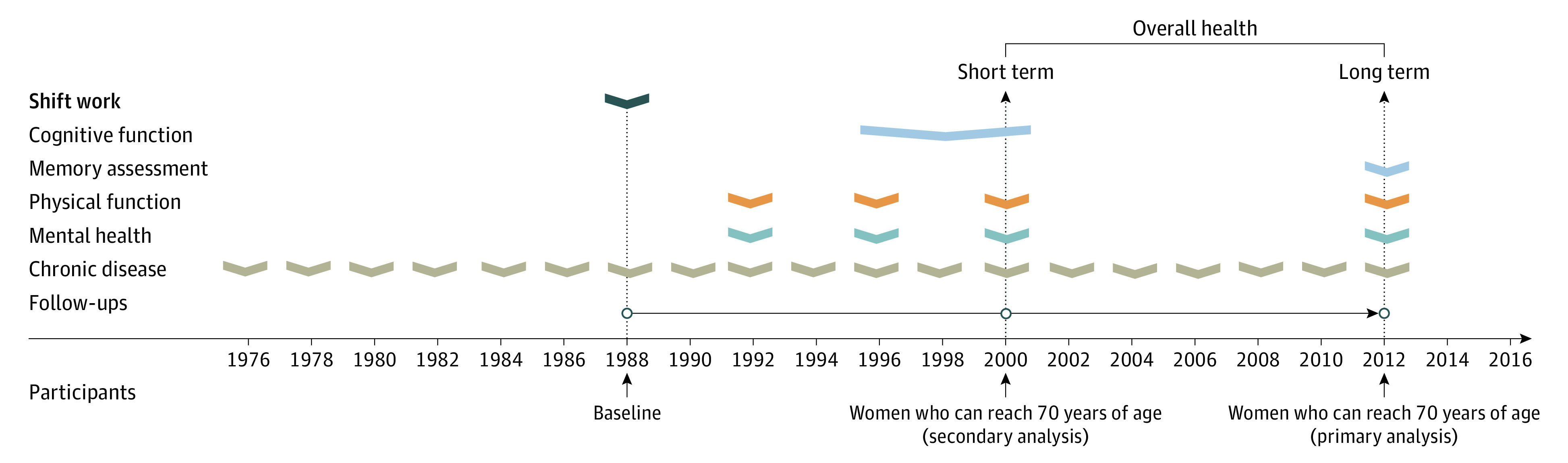
Participants who were free of major chronic diseases in 1988 were followed up for 24 years in the primary analysis (1988-2012; n = 46 319; age range at baseline, 46-68 years) and for 12 years in the secondary analysis (1988-2000; n = 14 273; age range at baseline, 58-68 years).
Assessment of Healthy Aging
On the basis of the concept of successful aging developed by Rowe and Kahn27 and previous literature,25,26,28,29 healthy aging was defined as survival to at least 70 years of age and 4 health domains (no major chronic diseases and no impairment in cognitive function, physical function, or mental health). Participants who did not meet any of these criteria were defined as usual agers. Detailed descriptions of our primary outcome, secondary outcome, and each of the 4 domains are listed in Table 1.30,31,32,33,34,35,36,37,38 Briefly, in the primary analysis, the outcome was evaluated in 2012 based on 46 318 nurses' data on disease (eMethods 1 in the Supplement), physical function, mental health, and memory function, whereas in the secondary analysis, it was evaluated in 1995 to 2000 based on 14 273 nurses' data on disease, physical function, mental health, and cognitive function.
Table 1. Definition and Dimensions of Healthy Aging.
| Dimension | Primary analysis: healthy aging in 2012 | Secondary analysis: healthy aging in 1995-2000 |
|---|---|---|
| Assessment of chronic diseases | Clinical diagnoses of 11 major chronic diseasesa were queried on each biennial questionnaire since 1988, which were then confirmed by professional staff through medical record or pathology report review, telephone interview, or supplementary questionnaire inquiries, and has been shown to be valid in this cohort.25 Women who reported no history of these diseases before the end of follow-up (2000 for short-term and 2012 for long-term follow-up) were considered to be free of chronic diseases. | |
| Assessment of cognitive (or memory) function | In 2012, subjective memory concerns were assessed through the Structured Telephone Interview for Dementia Assessment using 7 questions, which were associated with objective cognitive function in this cohort30 and have previously been used to detect individuals with possible cognitive impairment.31 Research in other cohorts has established that subjective memory correlates well with dementia.32 No impairment in memory was defined as at most 1 memory concern.26,33 | Between 1995 and 2000, we administered the TICS, a telephone version of the MMSE. TICS scores range from 0 to 41, and a score <31 is considered cognitive impairment.34 Studies have shown high test-retest reliability and validity of TICS in assessing cognitive status. A strong correlation (r = 0.97) was found between TICS and MMSE assessments.35 Trained study nurses who were unaware of the study hypothesis performed the assessment, and inter-interviewer reliability was high (>0.95).36 |
| Assessment of physical function | In 2012, physical function was assessed by 10 questionsb in the SF-36. Impairment of physical function was defined as any of the following: limited at least a little on moderate activities or limited a lot on more difficult physical tasks; otherwise, they were defined as no impairment of physical function.26 | In 1996, 1998, and 2000 (the one nearest to cognitive assessment was chosen), physical function was assessed by the same question as in 2012. |
| Assessment of mental health | In 2012, mental health was assessed using the GDS-15) (range, 0-15, with lower scores indicating better mental health).37 Good mental health was defined as a GDS-15 score ≤1 (the median value in the cohort). | In 1996, 1998, and 2000 (the one nearest to cognitive assessment was chosen), mental health was evaluated by 5 questionsc in the SF-36. A score between 1 (worst) and 6 (best) was assigned to each question. We then summed these scores and rescaled them on a range of 0-100. Good mental health was defined as a score >84 (the median value in this cohort).25 |
| Healthy aging | Healthy aging was defined as surviving to the end of follow-up (age ≥70 y), being free of major chronic diseases, and having no impairment of physical function, no mental health limitations, and no impairment of cognition (in 1995-2000) or subjective memory (in 2012).25,26 Participants who did not meet any of these criteria were defined as usual agers. | |
Abbreviations: GDS-15, Geriatric Depression Scale 15; MMSE, Mini-Mental State Examination; SF-36, Medical Outcomes Study Short-Form Health Survey; TICS, Telephone Interview of Cognitive Status.
Major chronic diseases covers most common conditions that would significantly deteriorate human health, including cancer (except for nonmelanoma skin cancers), diabetes, myocardial infarction, coronary artery bypass graft surgery or percutaneous transluminal coronary angioplasty (as a surrogate for coronary artery disease), congestive heart failure, stroke, kidney failure, chronic obstructive pulmonary disease, Parkinson disease, multiple sclerosis, and amyotrophic lateral sclerosis.
The 10 questions inquired about physical limitations in performing the following activities: moderate activities (eg, moving a table, pushing a vacuum cleaner, bowling, or playing golf); bathing and dressing yourself; walking 1 block; walking several blocks; walking more than 1 mile; vigorous activities (eg, running, lifting heavy objects, or strenuous sports); bending, kneeling, or stooping; climbing 1 flight of stairs; climbing several flights of stairs; and lifting or carrying groceries. Each question had 3 response choices: “Yes, limited a lot,” “Yes, limited a little,” or “No, not limited at all.” The validity and reproducibility of the SF-36 and its components have been previously established.38
The 5 questions were as follows: Have you been a very nervous person? Have you felt so down in the dumps nothing could cheer you up? Have you felt calm and peaceful? Have you felt downhearted and blue? and Have you been a happy person? There were 6 possible responses to each question ranging from none of the time to all of the time.
Assessment of Rotating Night Shift Work
In 1988, women were asked to report their total number of years of rotating night shift work (defined as at least 3 nights per month in addition to day and evening shifts) with 8 prespecified categories, including never, 1 to 2 years, 3 to 5 years, 6 to 9 years, 10 to 14 years, 15 to 19 years, 20 to 29 years, and 30 years or more. Duration of rotating night shift work has previously been associated with risk of diabetes,8 coronary heart disease,7 and breast cancer39 in this cohort. Consistent with previous publications,7,8 we categorized the duration of rotating night shift work into 4 categories: never, 1 to 5 years, 6 to 9 years, and 10 years or more.
Assessment of Covariates
Information on a broad range of covariates was obtained, including demographic characteristics,40 such as marital status, race, educational level, and household income; lifestyle factors, such as dietary data,41,42,43 sleep behavior, and physical activity44,45,46 (eMethods 2 in the Supplement); family history of cancer, myocardial infarction, and diabetes; clinical diagnoses of hypertension and high cholesterol; use of supplemental multivitamins and aspirin; and menopausal status and postmenopausal hormone use.
Statistical Analysis
Logistic regression models were used to estimate odds ratios (ORs) and 95% CIs for healthy aging across rotating night shift work categories (none, 1-5 years, 6-9 years, and ≥10 years). Women with no history of rotating night shift work were set as the reference category. An OR smaller than 1 indicates decreased odds of healthy aging. In the base model, we adjusted for age, educational level, marital status, household income, hypertension, high cholesterol, family history (cancer, myocardial infarction, or diabetes), menopausal status and hormone use, and aspirin use. In the multivariate-adjusted model, we additionally adjusted for lifestyle factors, including smoking history, alcohol intake, total energy intake, diet quality (Alternate-Healthy Eating Index), physical activity, standing and sitting time per day, and daily sleep duration. Obesity may be a consequence of night shift work,47,48 and obesity had a strong inverse association with healthy aging.49 By inference, obesity may act as a mediator between night shift work and healthy aging; therefore, we further adjusted for body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) in a separate model. Mediation analysis based on the counterfactual framework50 was also performed. Dummy variables were created to indicate missing covariate values. A P value for trend was obtained by assigning the midpoint value to each rotating night shift work category and modeling it as a continuous variable.
We performed several sensitivity analyses to examine the robustness of observed associations. First, to further control for potential selection bias, we performed a propensity-weighted analysis. In this analysis, the exposure was treated as a binary variable (those who worked the night shift vs those who did not). Second, we restricted our analyses to women without hypertension or hypercholesterolemia. Third, we evaluated potential changes in the association estimates if we additionally adjusted for snoring, waist-hip ratio, or coffee intake or removed sleep duration from the multivariate model (because sleep duration could be an intermediate between rotating night shift work and healthy aging). In addition, to explore the possible influence of age and lifestyle factors51 on the association, we performed stratified analysis (eMethods 3 in the Supplement). Finally, to evaluate the association between years of night shifts and healthy aging among survivors, we excluded women who died before the end of follow-up from the group of usual agers and repeated all analyses.
Data were analyzed from March 1 to September 30, 2021. All analyses were performed with SAS software, version 9.4 (SAS Institute Inc). A 2-sided P < .05 was considered statistically significant.
Results
Of the 46 318 female nurses included in the primary analysis, 17 786 (38.4%) remained free of the 11 chronic diseases, 7150 (15.4%) had no impairment of physical function, 19 654 (42.4%) had good mental health, and 23 169 (50.0%) reported no impairment of memory function. A total of 3695 participants (8.0%) met all criteria of healthy aging; the rest were usual agers.
Baseline Characteristics of Participants
The mean (SD) age of study participants at baseline was 55.4 (6.1) years. A total of 45 300 participants (97.8%) were White, 562 (1.2%) were Black, 98 (0.2%) were American Indian, 347 (0.8%) were Asian, and 11 (0.02%) were Hawaiian. Of the 46 318 women studied, 27 480 (59.3%) reported having ever engaged in rotating night shift work, and 5384 (11.6%) reported at least 10 years of rotating night shift work. Table 2 gives the baseline characteristics of the study participants across categories of duration of rotating night shift work. Compared with women with no history of rotating night shift work, those with more years of rotating night shifts were slightly older (mean [SD] age, 56.7 [6.0] years for those with ≥10 years of shift work vs 55.1 [6.1] for those with no shift work), had less education (master’s or doctorate degree, 341 [7.1%] for those with ≥10 years of shift work vs 1880 [10.8%] for those with no shift work), slept somewhat less (6.8 [1.1] hours per day for those with ≥10 years of shift work vs 7.0 [1.0] hours per day for those with no shift work), were more likely to be current smokers (1347 [25.0%] for those with ≥10 years of shift work vs 3241 [17.2%] for those with no shift work) or regular snorers (538 [11.5%] for those with ≥10 years of shift work vs 1451 [8.7%] for those with no shift work), had higher mean (SD) BMIs (26.4 [5.2] for those with ≥10 years of shift work vs 25.1 [4.5] for those with no shift work), had less median (IQR) sitting time (2.2 [1.1-4.4] hours per day for those with ≥10 years of shift work vs 4.4 [1.1-4.4] hours per day for those with no shift work), and were more likely to have hypertension (983 [18.3%] for those with ≥10 years of shift work vs 2940 [15.6%] for those with no shift work).
Table 2. Age-Adjusted Baseline Characteristics in 1988 by Years of Rotating Night Shift Work in the Nurses’ Health Studya.
| Characteristic | Duration of night shift work | |||
|---|---|---|---|---|
| Never (n = 18 838) | 1-5 y (n = 18 944) | 6-9 y (n = 3152) | ≥10 y (n = 5384) | |
| Length of rotating night shift work, median (IQR), y | 0 | 1.5 (1.5-4.0) | 7.5 (7.5-7.5) | 17.0 (12.0-24.5) |
| Age in 1988,b mean (SD) [range], y | 55.1 (6.1) [46-68] | 55.3 (6) [46-68] | 55.9 (6) [46-68] | 56.7 (6) [46-68] |
| Education, No. (%) | ||||
| Registered nurse | 11 854 (67.9) | 12 146 (68.9) | 2061 (71.2) | 3684 (76.2) |
| Bachelor’s degree | 3712 (21.3) | 3584 (20.3) | 544 (18.8) | 808 (16.7) |
| Master’s or doctorate degree | 1880 (10.8) | 1893 (10.7) | 288 (10.0) | 341 (7.1) |
| Husband’s educational level, No. (%) | ||||
| High school or less | 6710 (44.9) | 6429 (42.7) | 1175 (48.2) | 2271 (56.4) |
| College graduate | 4466 (29.9) | 4519 (30.0) | 714 (29.3) | 1083 (26.9) |
| Graduate school | 3758 (25.2) | 4123 (27.4) | 548 (22.5) | 675 (16.8) |
| Self-reported race, No. (%) | ||||
| American Indian | 30 (0.2) | 43 (0.2) | 5 (0.2) | 20 (0.4) |
| Asian | 155 (0.8) | 131 (0.7) | 22 (0.7) | 39 (0.7) |
| Black | 198 (1.1) | 222 (1.2) | 45 (1.4) | 97 (1.8) |
| Hawaiian | 5 (0.03) | 3 (0.02) | 2 (0.06) | 1 (0.02) |
| White | 18 450 (97.9) | 18 545 (97.9) | 3078 (97.7) | 5227 (97.1) |
| Marital status, No. (%) | ||||
| Married | 16 082 (92.7) | 16 289 (92.9) | 2607 (89.8) | 4443 (89.9) |
| Widowed | 489 (2.8) | 458 (2.6) | 97 (3.3) | 189 (3.8) |
| Separated‚ divorced‚ or never married | 776 (4.5) | 780 (4.5) | 199 (6.8) | 312 (6.3) |
| Family annual income in 1986, median (IQR), $ in 10 000s | 6.0 (4.7-7.8) | 6.1 (4.7-7.9) | 5.8 (4.6-7.5) | 5.6 (4.5-7.2) |
| BMI at baseline, mean (SD) | 25.1 (4.5) | 25.2 (4.5) | 25.7 (4.8) | 26.4 (5.2) |
| Smoking status, No. (%) | ||||
| Never smoker | 8573 (45.5) | 8324 (43.9) | 1305 (41.4) | 2236 (41.5) |
| Past smoker | 7024 (37.3) | 7335 (38.7) | 1167 (37.0) | 1801 (33.5) |
| Current smoker | 3241 (17.2) | 3285 (17.3) | 679 (21.6) | 1347 (25.0) |
| Alcohol intake, No. (%), g/d | ||||
| None | 7173 (40.1) | 6942 (38.5) | 1194 (40.2) | 2239 (44.1) |
| 1-14.9 | 8362 (46.7) | 8637 (47.8) | 1406 (47.3) | 2289 (45.1) |
| ≥15 | 2356 (13.2) | 2475 (13.7) | 373 (12.5) | 547 (10.8) |
| AHEI, mean (SD) | 47.4 (10.9) | 47.8 (10.8) | 47.9 (10.7) | 47.1 (10.6) |
| Total calories, mean (SD), kcal | 1734.2 (519.8) | 1774.6 (527.3) | 1759.8 (539.0) | 1772.8 (553.4) |
| Total coffee, median (IQR), cups per day | 2.5 (1.0-3.5) | 2.5 (1.0-3.5) | 2.5 (1.0-3.5) | 2.5 (1.0-4.5) |
| Physical activity, median (IQR), MET-h/wkc | 8.4 (3.1-20.2) | 9.7 (3.6-21.2) | 9.3 (3.5-21.5) | 8.6 (3.2-21.5) |
| Time, median (IQR), h/d | ||||
| Standing | 4.4 (1.6-7.2) | 4.4 (1.6-7.2) | 4.4 (1.6-7.2) | 4.4 (1.6-7.7) |
| Sitting | 4.4 (1.1-4.4) | 4.4 (1.1-4.4) | 2.2 (1.1-4.4) | 2.2 (1.1-4.4) |
| Family history, No. (%) | ||||
| Diabetes | 5230 (27.8) | 5454 (28.8) | 990 (31.4) | 1677 (31.1) |
| Myocardial infarction | 3421 (18.2) | 3515 (18.6) | 613 (19.5) | 1074 (20.0) |
| Cancer | 2656 (14.1) | 2782 (14.7) | 451 (14.3) | 737 (13.7) |
| History, No. (%) | ||||
| Hypertension | 2940 (15.6) | 2926 (15.4) | 554 (17.6) | 983 (18.3) |
| High cholesterol | 3606 (19.1) | 3624 (19.1) | 583 (18.5) | 1010 (18.8) |
| Use of multivitamin, No. (%) | 7176 (38.6) | 7429 (39.7) | 1197 (38.6) | 2097 (39.6) |
| Menopausal status and hormone use, No. (%) | ||||
| Premenopausal | 4079 (22.3) | 4106 (22.3) | 681 (22.3) | 1027 (19.7) |
| Postmenopausal and never used | 8657 (47.4) | 8637 (46.9) | 1503 (49.3) | 2792 (53.4) |
| Postmenopausal and past user | 560 (3.1) | 553 (3.0) | 98 (3.2) | 145 (2.8) |
| Postmenopausal and current user | 4970 (27.2) | 5116 (27.8) | 767 (25.1) | 1263 (24.2) |
| Regular aspirin use (≥2 tablets per week), No. (%) | 5837 (32.7) | 5988 (33.2) | 1007 (33.4) | 1804 (35.2) |
| Sleep duration, mean (SD), h/d | 7.0 (1.0) | 7.0 (1.0) | 6.9 (1.0) | 6.8 (1.1) |
| Regular snorer, No. (%) | 1451 (8.7) | 1485 (8.8) | 292 (10.5) | 538 (11.5) |
Abbreviations: AHEI, Alternate-Healthy Eating Index; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); MET, metabolic equivalent.
Data are standardized to the age distribution of the study population.
Value was not age adjusted.
MET-h/wk is calculated as the sum of the mean time per week spent in each activity × MET value of each activity.
Primary Analysis: Duration of Rotating Night Shift Work and Healthy Aging in 2012
Table 3 summarizes the ORs of healthy aging in 2012 associated with rotating night shift work. Compared with women without rotating night shift work, the multivariate-adjusted ORs were 0.96 (95% CI, 0.89-1.03) for women with 1-5 years of rotating night shift work, 0.92 (95% CI, 0.79-1.07) for women with 6-9 years of rotating night shift work, and 0.79 (95% CI, 0.69-0.91) for those with 10 years or more of rotating night shift work (P = .001 for trend). Additional adjustment for BMI attenuated the association (adjusted OR, 0.97; 95% CI, 0.90-1.05 for 1-5 years; adjusted OR, 0.98; 95% CI, 0.84-1.15) for 6-9 years; and adjusted OR, 0.88; 95% CI, 0.77-1.01 for ≥10 years; P = .11 for trend). This finding was further confirmed in the formal mediation analysis (eTable 2 in the Supplement): 42.9% to 61.6% of the association was mediated by overweight or BMI in 1988, and the natural direct effects were statistically nonsignificant.
Table 3. Odds Ratios (95% CIs) of Healthy Aging by History of Rotating Night Shift Work in the Nurses’ Health Study (1988-2012).
| Outcome | No. | Healthy aging, No. (%) | Base adjusteda | Multivariate adjustedb | Multivariate and BMI adjustedc |
|---|---|---|---|---|---|
| Healthy aging by duration of shift work, y | |||||
| 0 | 18 838 | 1653 (8.8) | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1-5 | 18 944 | 1547 (8.2) | 0.97 (0.90-1.05) | 0.96 (0.89-1.03) | 0.97 (0.90-1.05) |
| 6-9 | 3152 | 218 (6.9) | 0.92 (0.79-1.07) | 0.92 (0.79-1.07) | 0.98 (0.84-1.15) |
| ≥10 | 5384 | 277 (5.1) | 0.78 (0.68-0.90) | 0.79 (0.69-0.91) | 0.88 (0.77-1.01) |
| P for trend | NA | NA | <.001 | .001 | .11 |
| Free of main chronic diseases by duration of shift work, y | |||||
| 0 | 18 838 | 7565 (40.2) | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1-5 | 18 944 | 7528 (39.7) | 1.01 (0.96-1.05) | 1.01 (0.96-1.05) | 1.01 (0.97-1.06) |
| 6-9 | 3152 | 1063 (33.7) | 0.84 (0.77-0.91) | 0.86 (0.79-0.93) | 0.88 (0.81-0.96) |
| ≥10 | 5384 | 1630 (30.3) | 0.78 (0.73-0.84) | 0.83 (0.77-0.89) | 0.88 (0.82-0.94) |
| P for trend | NA | NA | <.001 | <.001 | <.001 |
| Good physical function by duration of shift work, y | |||||
| 0 | 18 838 | 3135 (16.6) | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1-5 | 18 944 | 2996 (15.8) | 0.99 (0.93-1.05) | 0.97 (0.91-1.03) | 0.98 (0.92-1.04) |
| 6-9 | 3152 | 431 (13.7) | 0.94 (0.84-1.06) | 0.94 (0.83-1.06) | 1.00 (0.89-1.13) |
| ≥10 | 5384 | 588 (10.9) | 0.85 (0.77-0.94) | 0.87 (0.78-0.96) | 0.96 (0.87-1.07) |
| P for trend | NA | NA | .002 | .006 | .56 |
| Good mental health by duration of shift work, y | |||||
| 0 | 18 838 | 8328 (44.2) | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1-5 | 18 944 | 8255 (43.6) | 1.00 (0.96-1.05) | 0.99 (0.95-1.04) | 0.99 (0.95-1.04) |
| 6-9 | 3152 | 1228 (39.0) | 0.91 (0.84-0.99) | 0.92 (0.84-0.998) | 0.94 (0.86-1.02) |
| ≥10 | 5384 | 1843 (34.2) | 0.84 (0.78-0.90) | 0.87 (0.81-0.93) | 0.91 (0.84-0.97) |
| P for trend | NA | NA | <.001 | <.001 | .003 |
| Good memory function by duration of shift work, y | |||||
| 0 | 18 838 | 9748 (51.8) | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1-5 | 18 944 | 9628 (50.8) | 0.98 (0.94-1.03) | 0.98 (0.94-1.03) | 0.98 (0.94-1.03) |
| 6-9 | 3152 | 1468 (46.6) | 0.90 (0.83-0.97) | 0.91 (0.84-0.98) | 0.91 (0.84-0.99) |
| ≥10 | 5384 | 2325 (43.2) | 0.88 (0.82-0.94) | 0.91 (0.85-0.97) | 0.92 (0.86-0.98) |
| P for trend | NA | NA | <.001 | <.001 | .003 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); NA, not applicable.
Base model adjusted for age at baseline (continuous); educational level (registered nurse, bachelor’s, or master’s or doctorate degree); marital status (married, widowed, or separated/divorced/never married); household income (quintiles); baseline hypertension and high cholesterol (yes or no); family history of cancer, myocardial infarction, and diabetes (yes or no); menopausal status and hormone use (premenopausal, postmenopausal never users, postmenopausal past users, or postmenopausal current users); and aspirin use (regular use or not).
Multivariate model additionally adjusted for lifestyle factors, including smoking history (never, former smoker, or current smoker), alcohol intake (none, 1-14.9 g/d, or ≥15 g/d), total energy intake (quintiles), diet quality (Alternate-Healthy Eating Index score, in quintiles), physical activity (metabolic equivalent hours per week, in quintiles); standing and sitting time (in quintiles); and sleep duration (≤5, 6, 7, 8, or ≥9 hours).
Additionally adjusted for BMI at baseline (<18.5, 18.5-24.9, 25-29.9, or ≥30).
Longer years of rotating night shift work were consistently inversely associated with 4 individual dimensions of healthy aging in the multivariate-adjusted model. The multivariate-adjusted ORs comparing women with 10 years or more of rotating night shift work vs women without rotating night shift work were 0.83 (95% CI, 0.77-0.89) for being free of major chronic diseases (P < .001 for trend), 0.87 (95% CI, 0.78-0.96) for having good physical function (P = .006 for trend), 0.87 (95% CI, 0.81-0.93) for having good mental health (P < .001 for trend, and 0.91 (95% CI, 0.85-0.97) for having good memory function (P < .001 for trend).
Secondary Analysis: Duration of Rotating Night Shift Work and Healthy Aging in 1995-2000
Of the 14 273 participants included in the analysis of short-term healthy aging, 8515 women (59.7%) had none of the 11 chronic diseases, 3454 (24.2%) had no impairment of physical function, 5317 (37.3%) had good mental health, and 11 056 (77.5%) reported no impairment of cognitive function. A total of 1386 participants (9.7%) met all criteria of healthy aging in 1995 to 2000; the rest were usual agers.
The associations of rotating night shift work with healthy aging in 1995 to 2000 were consistent with the primary analysis (Table 4). Compared with women without rotating night shift work, the multivariate-adjusted ORs were 1.00 (95% CI, 0.88-1.13) for 1-5 years of shift work, 0.72 (95% CI, 0.56-0.92) for 6-9 years of shift work, and 0.73 (95% CI, 0.60-0.89) for 10 years or more of shift work (P < .001 for trend). The association remained essentially unchanged with additional adjustment for BMI (OR, 1.00; 95% CI, 0.89-1.14 for 1-5 years; OR, 0.75; 95% CI, 0.59-0.97 for 6-9 years; and OR, 0.78; 95% CI, 0.64-0.95 for ≥10 years; P = .003 for trend). Rotating night shift work was also inversely associated with 4 dimensions of healthy aging. The multivariate-adjusted ORs comparing women with 10 years or more of rotating night shift work vs women without rotating night shift work were 0.84 (95% CI, 0.75-0.93) for being free of major chronic diseases (P < .001 for trend), 0.81 (95% CI, 0.71-0.92) for having good physical function (P < .001 for trend), 0.92 (95% CI, 0.82-1.03) for having good mental health (P = .03 for trend), and 0.89 (95% CI, 0.78-1.00) for having good memory function (P = .02 for trend). Additional adjustment for BMI did not change these associations.
Table 4. Odds Ratios (95% CIs) of Healthy Aging by History of Rotating Night Shift Work in the Nurses’ Health Study (1988-2000).
| Outcome | No. | Healthy aging, No. (%) | Base adjusteda | Multivariate adjustedb | Multivariate and BMI adjustedc |
|---|---|---|---|---|---|
| Healthy aging by duration of shift work, y | |||||
| 0 | 5477 | 553 (10.1) | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1-5 | 5722 | 608 (10.6) | 1.03 (0.91-1.17) | 1.00 (0.88-1.13) | 1.00 (0.89-1.14) |
| 6-9 | 1044 | 80 (7.7) | 0.75 (0.59-0.97) | 0.72 (0.56-0.92) | 0.75 (0.59-0.97) |
| ≥10 | 2030 | 145 (7.1) | 0.75 (0.62-0.91) | 0.73 (0.60-0.89) | 0.78 (0.64-0.95) |
| P for trend | NA | NA | <.001 | <.001 | .003 |
| No main chronic diseases by duration of shift work, y | |||||
| 0 | 5477 | 3291 (60.1) | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1-5 | 5722 | 3563 (62.3) | 1.08 (1.00-1.17) | 1.07 (0.99-1.16) | 1.07 (0.99-1.16) |
| 6-9 | 1044 | 572 (54.8) | 0.81 (0.71-0.93) | 0.80 (0.70-0.92) | 0.82 (0.72-0.95) |
| ≥10 | 2030 | 1089 (53.7) | 0.82 (0.74-0.91) | 0.84 (0.75-0.93) | 0.87 (0.78-0.97) |
| P for trend | NA | NA | <.001 | <.001 | <.001 |
| Good physical function by duration of shift work, y | |||||
| 0 | 5477 | 1351 (24.7) | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1-5 | 5722 | 1474 (25.8) | 1.03 (0.94-1.12) | 0.99 (0.90-1.08) | 0.99 (0.91-1.08) |
| 6-9 | 1044 | 216 (20.7) | 0.81 (0.69-0.95) | 0.76 (0.64-0.90) | 0.80 (0.68-0.95) |
| ≥10 | 2030 | 413 (20.3) | 0.85 (0.75-0.96) | 0.81 (0.71-0.92) | 0.88 (0.77-1.00) |
| P for trend | NA | NA | .001 | <.001 | .008 |
| Good mental health by duration of shift work, y | |||||
| 0 | 5477 | 2085 (38.1) | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1-5 | 5722 | 2181 (38.1) | 0.99 (0.92-1.07) | 0.98 (0.91-1.06) | 0.98 (0.91-1.06) |
| 6-9 | 1044 | 356 (34.1) | 0.85 (0.74-0.98) | 0.85 (0.74-0.98) | 0.85 (0.74-0.98) |
| ≥10 | 2030 | 695 (34.2) | 0.90 (0.80-0.99) | 0.92 (0.82-1.03) | 0.92 (0.82-1.03) |
| P for trend | NA | NA | .009 | .03 | .03 |
| Good cognitive function by duration of shift work, y | |||||
| 0 | 5477 | 4266 (77.9) | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1-5 | 5722 | 4514 (78.9) | 1.02 (0.93-1.12) | 1.01 (0.92-1.11) | 1.01 (0.92-1.11) |
| 6-9 | 1044 | 788 (75.5) | 0.87 (0.74-1.02) | 0.88 (0.75-1.03) | 0.88 (0.75-1.04) |
| ≥10 | 2030 | 1488 (73.3) | 0.86 (0.76-0.97) | 0.89 (0.78-1.00) | 0.90 (0.79-1.02) |
| P for trend | NA | NA | .003 | .02 | .03 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); NA, not applicable.
Base model adjusted for age at baseline (continuous); educational level (registered nurse, bachelor’s, or master’s or doctorate degree); marital status (married, widowed, or separated/divorced/never married); household income (quintiles); baseline hypertension and high cholesterol (yes or no); family history of cancer, myocardial infarction, and diabetes (yes or no); menopausal status and hormone use (premenopausal, postmenopausal never users, postmenopausal past users, or postmenopausal current users); and aspirin use (regular use or not).
Multivariate model additionally adjusted for lifestyle factors, including smoking history (never, former smoker, or current smoker), alcohol intake (none, 1-14.9 g/d, or ≥15 g/d), total energy intake (quintiles), diet quality (Alternate-Healthy Eating Index score, in quintiles), physical activity (metabolic equivalent hours per week, in quintiles); standing and sitting time (in quintiles); and sleep duration (≤5, 6, 7, 8, or ≥9 hours).
Additionally adjusted for BMI at baseline (<18.5, 18.5-24.9, 25-29.9, or ≥30).
Sensitivity Analysis
In the propensity-weighted analysis, we found similar associations between rotating night shift work and healthy aging (eTable 3 in the Supplement). We also observed similar results when we restricted our analyses to women who did not report a diagnosis of hypertension or hypercholesterolemia at baseline (eTable 4 in the Supplement). Additional adjustment for snoring, coffee intake, waist-to-hip ratio, or removal of sleep duration from the model did not change these results. In stratified analyses by age and lifestyles, an inverse association between shift work and healthy aging was consistently observed in most of the strata (eTable 5 in the Supplement) except for physical activity. In the analyses excluding 13 352 participants who died during follow-up before 2012 (n = 32 966), the main results remained similar.
Discussion
In this large, prospective cohort study of US female nurses, duration of rotating night shift work was independently associated with healthy aging after 24 years of follow-up. Ten years or more of rotating night shift work was associated with 20% decreased odds of healthy aging. This association was consistently observed for the individual component of healthy aging. Overall, the observed association did not differ substantially by age, BMI, and other lifestyle factors. Results were similar in a secondary analysis in which memory impairment was replaced with cognitive function decline, with an OR of 0.73 comparing 10 or more years vs no night shift work. To the best of our knowledge, this is the first prospective cohort study to investigate the association of night shift work with overall health status.
Comparison With Other Studies and Explanations
In addition to the existing literature suggesting that shift work is associated with increased mortality,14,52,53 our findings further indicate that this reduced lifespan might also be accompanied by worse overall health and functioning. Our results are also consistent with previous findings on the associations between shift work and individual health conditions. Rotating night shift work has previously been linked to chronic diseases, including cardiovascular disease,7,9,10,52 diabetes,6,54 cancers,17,18,55,56 and mental health,13,57 with limited evidence for cognitive function.58 However, some previous studies had relatively short10,54 or unknown59 follow-up duration, prior studies on mental health were mostly cross-sectional,57 and the proportion of shift workers was low.60 Our study provided more concrete evidence on the association of shift work with overall health by simultaneously considering chronic diseases, cognitive health, and mental and physical function and by evaluating outcomes with extended duration of follow-up.
Although mechanisms have not yet been clearly defined, several potential mechanisms underlie this association. Rotating night shift work alters circadian rhythms, which play important roles in daily metabolic function by regulating patterns of energy expenditure and hormones, such as leptin, ghrelin, thyrotropin, insulin, and melatonin61; meanwhile, disruption of circadian rhythms could contribute to insulin resistance, impaired glucose regulation, and development of diseases.4 Besides the effect on physical health, persons working night shifts are more likely to experience chronic sleep deprivation, poor-quality sleep, or sleep disorders,4,62 which can then lead to disruptions in mental health1 and impairment of cognitive function.63 A recent study29 that used Nurses’ Health Study data observed a nonlinear association between sleep duration and the odds of achieving healthy aging; however, the association between rotating night shift work and healthy aging was not explained by sleep duration in our study. Although long-term shift workers had slightly less sleep duration and were more likely to be regular snorers, our results are similar with or without additional adjustment for sleep duration, in different levels of sleep duration, and among regular or nonregular snorers. In addition, other factors, such as disturbed sociotemporal patterns (resulting from atypical work hours leading to family problems, reduced social support, and stress), might also explain the association.12 These findings indicate the potential direct effect of shift work on overall health.
In addition, unfavorable changes in health behaviors (such as obesity) among rotating night shift workers may partly explain the observed association. One meta-analysis48 confirmed the risks of developing overweight and obesity associated with night shift work. Overweight or obesity was also a strong independent risk factor of healthy aging.49 Our analysis confirmed that overweight or obesity might be an important mediator of the association between shift work and healthy aging. This finding suggests the importance of keeping healthy weight among shift workers, although these results warrant replication.
Strengths and Limitations
The strengths of this study included the prospective design; use of an integrated, composite measure for healthy aging; long follow-up; large sample size; and detailed information on a wide range of potential confounders. Several limitations of this study should also be considered. This study is limited to rotating night shift work in predominantly White US female nurses. Although the homogeneity of our study participants improved the response rate and the quality of their self-reported health status and minimized confounding by socioeconomic status, shift work patterns may be different by sex, ethnicity, and socioeconomic status.59 Therefore, our results may not apply to other populations, and future studies in more diverse samples are needed to confirm our findings. In addition, this is an observational study; therefore, we cannot rule out the possibility of unmeasured residual confounding.
Furthermore, health-related selection (eg, healthy worker effect) could lead to an underestimation of the association between rotating night shift work and healthy aging.54,64 It is possible that women who were able to adapt to many years of rotating night shift work were generally healthier than those who only worked on regular daytime schedules or withdrew from work for health reasons. Therefore, the association between rotating night shift work and healthy aging may be underestimated if the reference group included some women who worked on daytime schedules or withdrew from work because of health-related concerns. Another limitation was that we only examined rotating night shift work, a work schedule shown to have the largest impact on sleep, circadian disruption, and chronic disease risk. More research is needed to evaluate the effect of other types of shift work and intensity of shift work on health. In addition, duration of rotating night shift work was only assessed once at baseline, which may lead to misclassification if exposure to night shift work changed after baseline. However, women had a mean age of 55.4 years at baseline, a time when most women no longer performed night shift work and were less likely to start new night shifts.
Conclusions
In this cohort study, among women who worked as registered nurses, longer duration of rotating night shift work was associated with significantly decreased odds of healthy aging after 24 years of follow-up. This association was also present for each of 4 dimensions of healthy aging. Because an increasing proportion of the working population is involved in rotating night shift work, these findings further highlight the importance of understanding the association of night shift work with human health. Additional studies are warranted to confirm our findings in men and other ethnic populations.
eTable 1. Age-Adjusted Baseline Characteristics by Exclusions
eTable 2. Mediation of BMI on the Association Between Rotating Night Shift Work and Healthy Aging, NHS (1988-2012)
eTable 3. Odds Ratios of Healthy Aging by History of Rotating Night Shift Work in the Nurses’ Health Study (1988-2012), Based on Propensity Weighted Analysis, N = 46,318
eTable 4. Sensitivity Analysis on Rotating Night Shift Work and Healthy Aging in 2012 by Restriction or Adjustment of Additional Potential Confounders, NHS (1988-2012)
eTable 5. Stratified Analysis for Rotating Night Shift Work and Healthy Aging in 2012, NHS (1988-2012), N = 46,318
eFigure. Flowchart of Participants’ Selection
eMethods 1. Confirmation of Different Chronic Diseases
eMethods 2. Assessment of Covariates
eMethods 3. Stratified Analysis (Methods and Results)
References:
- 1.Brown JP, Martin D, Nagaria Z, Verceles AC, Jobe SL, Wickwire EM. Mental health consequences of shift work: an updated review. Curr Psychiatry Rep. 2020;22(2):7. doi: 10.1007/s11920-020-1131-z [DOI] [PubMed] [Google Scholar]
- 2.International Agency for Research on Cancer Working Group on the Evaluation of Carcinogenic Risk to Humans. Painting, Firefighting, and Shiftwork. 2010. Accessed November 15, 2020. https://www.ncbi.nlm.nih.gov/books/NBK326814/
- 3.Vyas MV, Garg AX, Iansavichus AV, et al. Shift work and vascular events: systematic review and meta-analysis. BMJ. 2012;345:e4800. doi: 10.1136/bmj.e4800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kervezee L, Kosmadopoulos A, Boivin DB. Metabolic and cardiovascular consequences of shift work: the role of circadian disruption and sleep disturbances. Eur J Neurosci. 2020;51(1):396-412. doi: 10.1111/ejn.14216 [DOI] [PubMed] [Google Scholar]
- 5.Wu QJ, Sun H, Wen ZY, et al. Shift work and health outcomes: an umbrella review of systematic reviews and meta-analyses of epidemiological studies. J Clin Sleep Med. 2022;18(2):653-662. doi: 10.5664/jcsm.9642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kecklund G, Axelsson J. Health consequences of shift work and insufficient sleep. BMJ. 2016;355:i5210. doi: 10.1136/bmj.i5210 [DOI] [PubMed] [Google Scholar]
- 7.Vetter C, Devore EE, Wegrzyn LR, et al. Association between rotating night shift work and risk of coronary heart disease among women. JAMA. 2016;315(16):1726-1734. doi: 10.1001/jama.2016.4454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shan Z, Li Y, Zong G, et al. Rotating night shift work and adherence to unhealthy lifestyle in predicting risk of type 2 diabetes: results from two large US cohorts of female nurses. BMJ. 2018;363:k4641. doi: 10.1136/bmj.k4641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Torquati L, Mielke GI, Brown WJ, Kolbe-Alexander T. Shift work and the risk of cardiovascular disease: a systematic review and meta-analysis including dose-response relationship. Scand J Work Environ Health. 2018;44(3):229-238. doi: 10.5271/sjweh.3700 [DOI] [PubMed] [Google Scholar]
- 10.Kawachi I, Colditz GA, Stampfer MJ, et al. Prospective study of shift work and risk of coronary heart disease in women. Circulation. 1995;92(11):3178-3182. doi: 10.1161/01.CIR.92.11.3178 [DOI] [PubMed] [Google Scholar]
- 11.Gao Y, Gan T, Jiang L, et al. Association between shift work and risk of type 2 diabetes mellitus: a systematic review and dose-response meta-analysis of observational studies. Chronobiol Int. 2020;37(1):29-46. doi: 10.1080/07420528.2019.1683570 [DOI] [PubMed] [Google Scholar]
- 12.Rajaratnam SM, Howard ME, Grunstein RR. Sleep loss and circadian disruption in shift work: health burden and management. Med J Aust. 2013;199(8):S11-S15. doi: 10.5694/mja13.10561 [DOI] [PubMed] [Google Scholar]
- 13.Torquati L, Mielke GI, Brown WJ, Burton NW, Kolbe-Alexander TL. Shift work and poor mental health: a meta-analysis of longitudinal studies. Am J Public Health. 2019;109(11):e13-e20. doi: 10.2105/AJPH.2019.305278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jørgensen JT, Karlsen S, Stayner L, Hansen J, Andersen ZJ. Shift work and overall and cause-specific mortality in the Danish nurse cohort. Scand J Work Environ Health. 2017;43(2):117-126. doi: 10.5271/sjweh.3612 [DOI] [PubMed] [Google Scholar]
- 15.Marquié JC, Tucker P, Folkard S, Gentil C, Ansiau D. Chronic effects of shift work on cognition: findings from the VISAT longitudinal study. Occup Environ Med. 2015;72(4):258-264. doi: 10.1136/oemed-2013-101993 [DOI] [PubMed] [Google Scholar]
- 16.Akerstedt T, Kecklund G, Johansson SE. Shift work and mortality. Chronobiol Int. 2004;21(6):1055-1061. doi: 10.1081/CBI-200038520 [DOI] [PubMed] [Google Scholar]
- 17.IARC Monographs Vol 124 Group . Carcinogenicity of night shift work. Lancet Oncol. 2019;20(8):1058-1059. doi: 10.1016/S1470-2045(19)30455-3 [DOI] [PubMed] [Google Scholar]
- 18.Straif K, Baan R, Grosse Y, et al. ; WHO International Agency for Research on Cancer Monograph Working Group . Carcinogenicity of shift-work, painting, and fire-fighting. Lancet Oncol. 2007;8(12):1065-1066. doi: 10.1016/S1470-2045(07)70373-X [DOI] [PubMed] [Google Scholar]
- 19.Colwell CS. Linking neural activity and molecular oscillations in the SCN. Nat Rev Neurosci. 2011;12(10):553-569. doi: 10.1038/nrn3086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Logan RW, McClung CA. Rhythms of life: circadian disruption and brain disorders across the lifespan. Nat Rev Neurosci. 2019;20(1):49-65. doi: 10.1038/s41583-018-0088-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hood S, Amir S. The aging clock: circadian rhythms and later life. J Clin Invest. 2017;127(2):437-446. doi: 10.1172/JCI90328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Depp CA, Jeste DV. Definitions and predictors of successful aging: a comprehensive review of larger quantitative studies. Am J Geriatr Psychiatry. 2006;14(1):6-20. doi: 10.1097/01.JGP.0000192501.03069.bc [DOI] [PubMed] [Google Scholar]
- 23.Pac A, Tobiasz-Adamczyk B, Błędowski P, et al. Influence of sociodemographic, behavioral and other health-related factors on healthy ageing based on three operative definitions. J Nutr Health Aging. 2019;23(9):862-869. doi: 10.1007/s12603-019-1243-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bosch-Farré C, Garre-Olmo J, Bonmatí-Tomàs A, et al. Prevalence and related factors of Active and Healthy Ageing in Europe according to two models: results from the Survey of Health, Ageing and Retirement in Europe (SHARE). PLoS One. 2018;13(10):e0206353. doi: 10.1371/journal.pone.0206353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sun Q, Townsend MK, Okereke OI, Franco OH, Hu FB, Grodstein F. Physical activity at midlife in relation to successful survival in women at age 70 years or older. Arch Intern Med. 2010;170(2):194-201. doi: 10.1001/archinternmed.2009.503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ma W, Hagan KA, Heianza Y, Sun Q, Rimm EB, Qi L. Adult height, dietary patterns, and healthy aging. Am J Clin Nutr. 2017;106(2):589-596. doi: 10.3945/ajcn.116.147256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rowe JW, Kahn RL. Human aging: usual and successful. Science. 1987;237(4811):143-149. doi: 10.1126/science.3299702 [DOI] [PubMed] [Google Scholar]
- 28.Sun Q, Townsend MK, Okereke OI, et al. Alcohol consumption at midlife and successful ageing in women: a prospective cohort analysis in the nurses’ health study. PLoS Med. 2011;8(9):e1001090. doi: 10.1371/journal.pmed.1001090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shi H, Huang T, Ma Y, Eliassen AH, Sun Q, Wang M. Sleep duration and snoring at midlife in relation to healthy aging in women 70 years of age or older. Nat Sci Sleep. 2021;13:411-422. doi: 10.2147/NSS.S302452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Amariglio RE, Townsend MK, Grodstein F, Sperling RA, Rentz DM. Specific subjective memory complaints in older persons may indicate poor cognitive function. J Am Geriatr Soc. 2011;59(9):1612-1617. doi: 10.1111/j.1532-5415.2011.03543.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Go RC, Duke LW, Harrell LE, et al. Development and validation of a Structured Telephone Interview for Dementia Assessment (STIDA): the NIMH Genetics Initiative. J Geriatr Psychiatry Neurol. 1997;10(4):161-167. doi: 10.1177/089198879701000407 [DOI] [PubMed] [Google Scholar]
- 32.Mitchell AJ, Beaumont H, Ferguson D, Yadegarfar M, Stubbs B. Risk of dementia and mild cognitive impairment in older people with subjective memory complaints: meta-analysis. Acta Psychiatr Scand. 2014;130(6):439-451. doi: 10.1111/acps.12336 [DOI] [PubMed] [Google Scholar]
- 33.James P, Kim ES, Kubzansky LD, Zevon ES, Trudel-Fitzgerald C, Grodstein F. Optimism and healthy aging in women. Am J Prev Med. 2019;56(1):116-124. doi: 10.1016/j.amepre.2018.07.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stampfer MJ, Kang JH, Chen J, Cherry R, Grodstein F. Effects of moderate alcohol consumption on cognitive function in women. N Engl J Med. 2005;352(3):245-253. doi: 10.1056/NEJMoa041152 [DOI] [PubMed] [Google Scholar]
- 35.Brandt J, Spencer M, Folstein M. The telephone interview for cognitive status. Neuropsychol Behav Neurol. 1988;1:111-117. [Google Scholar]
- 36.Lee S, Kawachi I, Berkman LF, Grodstein F. Education, other socioeconomic indicators, and cognitive function. Am J Epidemiol. 2003;157(8):712-720. doi: 10.1093/aje/kwg042 [DOI] [PubMed] [Google Scholar]
- 37.de Craen AJ, Heeren TJ, Gussekloo J. Accuracy of the 15-item geriatric depression scale (GDS-15) in a community sample of the oldest old. Int J Geriatr Psychiatry. 2003;18(1):63-66. doi: 10.1002/gps.773 [DOI] [PubMed] [Google Scholar]
- 38.Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36), I: conceptual framework and item selection. Med Care. 1992;30(6):473-483. doi: 10.1097/00005650-199206000-00002 [DOI] [PubMed] [Google Scholar]
- 39.Wegrzyn LR, Tamimi RM, Rosner BA, et al. Rotating night-shift work and the risk of breast cancer in the Nurses’ Health Studies. Am J Epidemiol. 2017;186(5):532-540. doi: 10.1093/aje/kwx140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Willett W, Stampfer MJ, Bain C, et al. Cigarette smoking, relative weight, and menopause. Am J Epidemiol. 1983;117(6):651-658. doi: 10.1093/oxfordjournals.aje.a113598 [DOI] [PubMed] [Google Scholar]
- 41.Willett WC, Sampson L, Stampfer MJ, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;122(1):51-65. doi: 10.1093/oxfordjournals.aje.a114086 [DOI] [PubMed] [Google Scholar]
- 42.Yuan C, Spiegelman D, Rimm EB, et al. Relative validity of nutrient intakes assessed by questionnaire, 24-hour recalls, and diet records as compared with urinary recovery and plasma concentration biomarkers: findings for women. Am J Epidemiol. 2018;187(5):1051-1063. doi: 10.1093/aje/kwx328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chiuve SE, Fung TT, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142(6):1009-1018. doi: 10.3945/jn.111.157222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41(5):998-1005. doi: 10.1249/MSS.0b013e3181930355 [DOI] [PubMed] [Google Scholar]
- 45.Chasan-Taber S, Rimm EB, Stampfer MJ, et al. Reproducibility and validity of a self-administered physical activity questionnaire for male health professionals. Epidemiology. 1996;7(1):81-86. doi: 10.1097/00001648-199601000-00014 [DOI] [PubMed] [Google Scholar]
- 46.Wolf AM, Hunter DJ, Colditz GA, et al. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol. 1994;23(5):991-999. doi: 10.1093/ije/23.5.991 [DOI] [PubMed] [Google Scholar]
- 47.Zhang Q, Chair SY, Lo SHS, Chau JP, Schwade M, Zhao X. Association between shift work and obesity among nurses: a systematic review and meta-analysis. Int J Nurs Stud. 2020;112:103757. doi: 10.1016/j.ijnurstu.2020.103757 [DOI] [PubMed] [Google Scholar]
- 48.Sun M, Feng W, Wang F, et al. Meta-analysis on shift work and risks of specific obesity types. Obes Rev. 2018;19(1):28-40. doi: 10.1111/obr.12621 [DOI] [PubMed] [Google Scholar]
- 49.Sun Q, Townsend MK, Okereke OI, Franco OH, Hu FB, Grodstein F. Adiposity and weight change in mid-life in relation to healthy survival after age 70 in women: prospective cohort study. BMJ. 2009;339:b3796. doi: 10.1136/bmj.b3796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vanderweele TJ, Vansteelandt S. Odds ratios for mediation analysis for a dichotomous outcome. Am J Epidemiol. 2010;172(12):1339-1348. doi: 10.1093/aje/kwq332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li Y, Pan A, Wang DD, et al. Impact of healthy lifestyle factors on life expectancies in the US population. Circulation. 2018;138(4):345-355. doi: 10.1161/CIRCULATIONAHA.117.032047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang D, Ruan W, Chen Z, Peng Y, Li W. Shift work and risk of cardiovascular disease morbidity and mortality: a dose-response meta-analysis of cohort studies. Eur J Prev Cardiol. 2018;25(12):1293-1302. doi: 10.1177/2047487318783892 [DOI] [PubMed] [Google Scholar]
- 53.Gu F, Han J, Laden F, et al. Total and cause-specific mortality of U.S. nurses working rotating night shifts. Am J Prev Med. 2015;48(3):241-252. doi: 10.1016/j.amepre.2014.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pan A, Schernhammer ES, Sun Q, Hu FB. Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Med. 2011;8(12):e1001141. doi: 10.1371/journal.pmed.1001141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schernhammer ES, Laden F, Speizer FE, et al. Night-shift work and risk of colorectal cancer in the nurses’ health study. J Natl Cancer Inst. 2003;95(11):825-828. doi: 10.1093/jnci/95.11.825 [DOI] [PubMed] [Google Scholar]
- 56.Schernhammer ES, Feskanich D, Liang G, Han J. Rotating night-shift work and lung cancer risk among female nurses in the United States. Am J Epidemiol. 2013;178(9):1434-1441. doi: 10.1093/aje/kwt155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee A, Myung SK, Cho JJ, Jung YJ, Yoon JL, Kim MY. Night shift work and risk of depression: meta-analysis of observational studies. J Korean Med Sci. 2017;32(7):1091-1096. doi: 10.3346/jkms.2017.32.7.1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Devore EE, Grodstein F, Schernhammer ES. Shift work and cognition in the Nurses’ Health Study. Am J Epidemiol. 2013;178(8):1296-1300. doi: 10.1093/aje/kwt214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dun A, Zhao X, Jin X, et al. Association between night-shift work and cancer risk: updated systematic review and meta-analysis. Front Oncol. 2020;10:1006. doi: 10.3389/fonc.2020.01006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Travis RC, Balkwill A, Fensom GK, et al. Night shift work and breast cancer incidence: three prospective studies and meta-analysis of published studies. J Natl Cancer Inst. 2016;108(12):djw169. doi: 10.1093/jnci/djw169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Akerstedt T. Shift work and disturbed sleep/wakefulness. Occup Med (Lond). 2003;53(2):89-94. doi: 10.1093/occmed/kqg046 [DOI] [PubMed] [Google Scholar]
- 62.Shift Work Disorder Symptoms. Accessed October 26, 2020. https://www.sleepfoundation.org/shift-work-disorder/symptoms
- 63.Dula DJ, Dula NL, Hamrick C, Wood GC. The effect of working serial night shifts on the cognitive functioning of emergency physicians. Ann Emerg Med. 2001;38(2):152-155. doi: 10.1067/mem.2001.116024 [DOI] [PubMed] [Google Scholar]
- 64.Carpenter L, Beral V, Fraser P, Booth M. Health related selection and death rates in the United Kingdom Atomic Energy Authority workforce. Br J Ind Med. 1990;47(4):248-258. doi: 10.1136/oem.47.4.248 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Age-Adjusted Baseline Characteristics by Exclusions
eTable 2. Mediation of BMI on the Association Between Rotating Night Shift Work and Healthy Aging, NHS (1988-2012)
eTable 3. Odds Ratios of Healthy Aging by History of Rotating Night Shift Work in the Nurses’ Health Study (1988-2012), Based on Propensity Weighted Analysis, N = 46,318
eTable 4. Sensitivity Analysis on Rotating Night Shift Work and Healthy Aging in 2012 by Restriction or Adjustment of Additional Potential Confounders, NHS (1988-2012)
eTable 5. Stratified Analysis for Rotating Night Shift Work and Healthy Aging in 2012, NHS (1988-2012), N = 46,318
eFigure. Flowchart of Participants’ Selection
eMethods 1. Confirmation of Different Chronic Diseases
eMethods 2. Assessment of Covariates
eMethods 3. Stratified Analysis (Methods and Results)


