Abstract
Objectives
To understand how and why participation in quality circles (QCs) improves general practitioners’ (GPs) psychological well-being and the quality of their clinical practice. To provide evidence-informed and practical guidance to maintain QCs at local and policy levels.
Design
A theory-driven mixed method.
Setting
Primary healthcare.
Method
We collected data in four stages to develop and refine the programme theory of QCs: (1) coinquiry with Swiss and European expert stakeholders to develop a preliminary programme theory; (2) realist review with systematic searches in MEDLINE, Embase, PsycINFO and CINHAL (1980–2020) to inform the preliminary programme theory; (3) programme refinement through interviews with participants, facilitators, tutors and managers of QCs and (4) consolidation of theory through interviews with QC experts across Europe and examining existing theories.
Sources of data
The coinquiry comprised 4 interviews and 3 focus groups with 50 European experts. From the literature search, we included 108 papers to develop the literature-based programme theory. In stage 3, we used data from 40 participants gathered in 6 interviews and 2 focus groups to refine the programme theory. In stage 4, five interviewees from different healthcare systems consolidated our programme theory.
Result
Requirements for successful QCs are governmental trust in GPs’ abilities to deliver quality improvement, training, access to educational material and performance data, protected time and financial resources. Group dynamics strongly influence success; facilitators should ensure participants exchange knowledge and generate new concepts in a safe environment. Peer interaction promotes professional development and psychological well-being. With repetition, participants gain confidence to put their new concepts into practice.
Conclusion
With expert facilitation, clinical review and practice opportunities, QCs can improve the quality of standard practice, enhance professional development and increase psychological well-being in the context of adequate professional and administrative support.
PROSPERO registration number
CRD42013004826.
Keywords: Quality in health care, EDUCATION & TRAINING (see Medical Education & Training), GENERAL MEDICINE (see Internal Medicine), Change management, MEDICAL EDUCATION & TRAINING, AUDIT
Strengths and limitations of this study.
This study synthesised over 100 academic papers published in English, German, French and Scandinavian languages, and data from 90 experts and participants from different European countries and healthcare systems.
The resulting programme theory reflects and explains the complex process in quality circles in the current context of European primary healthcare, and may need to be adapted in response to future changes.
The recommendations rely on the detail and depth of the reports we identified in our literature review and on the veracity and adequacy of the information gathered in interviews.
We were only able to test a limited set of existing theories to gain insights into how the programme theory’s mechanisms work and interrelate.
Introduction
Quality circles (QCs) are made up of 6–12 primary healthcare (PHC) professionals who regularly meet to reflect on and improve their standard practice. The terms Practice Based Small Group Work, Peer Review Group, Problem Based Small Group Learning, Practice Based Research Group, QC, Continuous Medical Education (CME) Group and Continuous Professional Development (CPD) Group were used interchangeably and varied among countries. The labels suggest the basic, original intent of the group. We decided to use the umbrella term QC to describe all of them.1 In the UK and Europe, QCs are commonly used by general practitioners (GPs) for CPD. The focus of discussion is usually a critical evaluation of an aspect of quality which participants themselves identify as important to them. GPs seek to improve the quality of their care by linking evidence to practice, learning to deal with uncertainty, discussing and reflecting on practice issues.2 Participation in QCs can raise self-esteem, create a sense of belonging and improve psychological well-being in GPs.1 QCs may be especially helpful in crisis situations like the current COVID-19 pandemic, where working continuously under high pressure can undermine the professionalism and mental health of GPs.3
QCs can improve standard practice like prescription patterns and diagnostic habits, enhance professional development and psychological well-being, but the results of randomised controlled trials are inconsistent and offer only limited behavioural explanations for these positive effects. As a complex social intervention, QCs combine didactic methods like brainstorming and reflective thinking with quality improvement (QI) techniques like audit and feedback or purposeful use of local experts. Their activities must be tailored to address local problems in PHC that participants want to solve.4 5 Our understanding of QCs is incomplete, and we need to learn more about these complex social interventions and their context-dependent outcomes and effects. This study seeks to clarify the contexts in which QCs are conducted, when they change GP behaviour and improve psychological well-being and why. We intended to develop a programme theory for QCs that explains how and why they work, with the aim of creating a common language and understanding,6 7 to engage stakeholders in discussions about improving QC processes in a participatory way and prepare the ground for further empirical testing.8 9 Our end goal was to develop an initial set of policy recommendations for setting up optimal QC processes and maintaining them.10–12
Methods
A project protocol was registered with PROSPERO (CRD42013004826) and published in 2013.5
We answered our research question in four stages with details to follow. In stage 1, we conducted a coinquiry with stakeholders on QCs from Switzerland and other European countries, in which we narrowed the research question and provided a preliminary programme theory. In stage 2, we synthesised evidence from a literature review and built a literature-informed programme theory. In stage 3, we collected evidence from interviews and focus groups with QC participants, facilitators, tutors and managers and refined the programme theory. In stage 4, we consolidated the programme theory, integrating interview data with participants across Europe and examining existing theories.
We conducted this research between 2013 and 2020, when the first author (AR) was completing his DPhil (PhD) project at the University of Oxford. AR’s thesis research engaged key Swiss and European expert stakeholders, including QC participants, facilitators, tutors, managers and policy-makers. The different players shared their perspectives when we developed the research questions, methods and analysis, and when we considered the implications of the results.
Pawson and Tilley’s realist logic was used to analyse the collected data in order to provide an in-depth explanation of QCs that showed how mutual learning in a social context improves standard practice, enhances professional development and increases well-being. The realist approach examines causal explanations of outcomes and then expresses them in their simplest form: context (C) ‘triggers’ or ‘activates’ a mechanism (M) that produces an outcome (O). The idea of mechanisms as being the generative power of how and why change occurs is central to realism. In the case of QCs, we looked for mechanisms at the level of human reasoning, because it is individuals who take an action or not, as a result of participating in QCs.13 When these mechanisms are activated in their context, it can be an immediate or delayed response. The context–mechanism–outcome (CMO) configurations are ‘mini’ explanatory theories situated within a programme theory.14 As we develop CMO configurations, we can more clearly see the contexts and mechanisms that produce desired outcomes. Once we identify these contexts, we can more easily select QC activities to change a given context to match our desired outcome.
Patient and public involvement
No patient involved.
Stage 1: the coinquiry
From May to December 2013, we consulted with 50 expert stakeholders, tutors, facilitators, QC participants and policy-makers, from Switzerland and 23 countries within the European Society of Quality and Safety in Family Medicine (EQuiP). They shared their perspectives on our research questions and helped us construct a mental model of QC function. For characteristics of participants, see online supplemental file 1. Stakeholders provided access to detailed and local information about QC aims, objectives and roles from professional websites, local publications and confidential training material and manuals across different European regions. We codesigned the preliminary conceptualisation of the programme theory, in short, preliminary programme theory, in discussion with the stakeholders, supported by local programme documentation and training material.
bmjopen-2021-058453supp001.pdf (58.9KB, pdf)
Stage 2: realist review
We performed iterative searches: to become familiar with existing literature; to find possible candidate theories to be tested; to find empirical evidence to refine, refute or confirm CMOs of the emerging programme theory and to look for further empirical evidence or theories to consolidate the programme theory.
Searching for theories
In principle, any theory that explained QCs was a candidate for our realist review, including those from psychology, social or economic sciences. We first identified key components of QCs; these were theories that described group dynamics, the role of the facilitator and their interaction with organisations. We searched for theories about motivation, learning, behaviour change, psychological well-being and QI in PHC. After this search we had identified 52 threads of theories across several levels. Since the theories overlapped considerably in a complex way, they did not allow empirical testing. Therefore, we deviated from the original protocol and used the preliminary programme theory (stage 1) as a starting point for the emerging programme theory. However, we benefitted from these findings in stage 4.
Searching for evidence for QC outcomes
Our search strategy was informed by an earlier scoping review that reported on the intentions and benefits, historical development and spread of QCs.1 In collaboration with a librarian, we refined our search strategy, combining terminology like ‘Programme’, ‘Quality Improvement’ and ‘Group’ terms with a PHC search filter.15 We ran the search in Medline, EMBASE, PsycINFO and CINHAL, without language restrictions (online supplemental file 2) from 1974, to reflect the emergence of QCs in 1974, at McMaster, Canada, and in 1979 at the University of Nijmegen, the Netherlands. We conducted the search in October 2013 and updated it in December 2020. Some full-text papers retrieved seemed closely related so we used cluster searching, a sampling strategy, to search for and complete clusters of closely related (kinship) papers.16 These kinship papers had common contextual features or theoretical backgrounds to the referring studies. We categorised these papers into kinship networks based on common themes, common contexts like geographical area, and common methods of organising QCs (eg, papers that tested similar didactic methods or similar QI tools in QCs). We broadened the search by examining citations in reference lists and Web of Science and searched manually for closely related papers (kinship papers)5 16
bmjopen-2021-058453supp002.pdf (69.9KB, pdf)
Selecting articles
Criteria for inclusion were: (1) the studies focused on small group work, (2) took place in the PHC setting and (3) had a quantitative or qualitative outcome. We managed search results in Endnote X7. SM and JH each assessed half of the retrieved papers and AR examined them all. The authors resolved disagreements through discussion. AR updated the search and included papers published from November 2013 to December 2020. GW checked the process paper selection and interpretation of the new data.
We appraised the relevance and rigour of each paper’s contribution. Data were relevant if they helped us understand a specific element or thread of theory in the emerging programme theory. Threads of theory were rigorous if they met three explanatory criteria: consilience (the theory accounts for most of the data), simplicity (the theory is straightforward, without exceptions) and analogy (the theory relates to already known principles).14 17 18
Analysis and synthesis of the data
We created a data extraction framework based on the preliminary programme theory and implemented it in Microsoft Excel. For each study, we extracted data on mechanisms, contexts, and outcomes (table 1).10 At least two authors (AR, SM or JH) reviewed extracted data and all authors reviewed the analysis and interpretation.
Table 1.
Data analysis process throughout the study
| Step | Description of the analytical step |
| One | We collected data on the following key elements of QCs:
|
| Two | Outcomes: each intermediate outcome, or final outcome received a new code. |
| Three | To identify the components of CMO configurations, we linked what was done in the QCs with intermediate outcomes, or final outcomes, and noted any corresponding contextual features and mechanisms that were mentioned. |
| Four | We sought explanations for when and why they had these outcomes (if the source mentioned context or underlying reasoning or mechanism) and then built CMO configurations. |
| Five | We categorised and ordered the CMO configurations to create a chain of outcomes and explained how CMO configurations related to each other. |
| Six | We compared and contrasted CMO patterns identified in different sources. |
| Seven | We consolidated the programme theory foundation of QCs. |
CMO, context–mechanism–outcome; QC, quality circle.
Initially, for each paper, we extracted components of context along with descriptions of mechanisms that led to an outcome. We summarised these configurations into descriptions of interaction between context and mechanisms that either facilitate or hinder QCs to reach their outcomes. Since papers were often closely related, we grouped them based on their kinship, which helped us look for and confirm CMO configurations between papers within the same (family) study. We iteratively arranged and rearranged the CMO configurations, moving between the papers, their data and families, and built patterns of outcomes (demiregularities) to develop the programme theory (see online supplemental file 3).
bmjopen-2021-058453supp003.pdf (69.1KB, pdf)
Stage 3: Refining the programme theory
AR conducted interviews and focus groups, and collected data from 40 participants to refine and test the configuration, interpretation and underlying mechanisms of each CMO configuration and its relative position/contribution to the programme theory.19
We invited a broad range of participants (including QC facilitators, GPs participating in QCs, tutors and QC managers) to participate in interviews, including the expert stakeholders from stage 1, so we could capture a range of professional backgrounds and roles.20 21 We applied the concepts of data saturation and stopped collecting data when additional information added no further relevant evidence. None of the invited participants declined. Throughout the process, we reflected critically on assumptions that AR or participants might have made during the interviews or focus groups.20
AR conducted six 30–60 min interviews in Swiss German between March and May 2015. After explaining the literature-based programme theory in plain words, AR offered contrasting options for participants to discuss. Then, he asked them to share their understanding of the underlying mechanisms and explain QC outcomes.
In April 2015, during an EQuiP conference, we held two focus group sessions with 33 GPs from over 19 European countries. Participants were given written descriptions of the emerging programme theory, phrased as conditional clauses that did not suggest mechanisms. During the focus group, participants were asked if and how much they agreed with the statements, and then the group discussed whether and why parts of the programme would or would not work in certain contexts. We summarise the characteristics of interview and focus group participants in online supplemental file 4.
bmjopen-2021-058453supp004.pdf (59.4KB, pdf)
Stage 4: consolidating the programme theory
Interviews with QC experts across healthcare systems
The literature, the interviews and focus groups contained little data about how the national contextual level or how national organisations or reimbursement of PHC affect QCs. Therefore, to consolidate the programme theory at a national and policy level, AR invited five representatives with expertise in QCs from five countries with different PHC provision systems to a 1-hour online interview to discuss the ways that different professional associations, institutional settings and other contexts affect QC outcomes.21 Participant characteristics are summarised in online supplemental file 5.
bmjopen-2021-058453supp005.pdf (68.7KB, pdf)
Existing theories and their relationships to CMO configurations in the programme theory
We then compared and contrasted this programme theory with formal theories to explain intermediate and final QC outcomes. Formal theories explain how mechanisms interrelate and how they may work across different disciplines. Programme theories that are based on formal, existing, theories may provide better explanations of phenomena than those that are not.7 Our candidate formal theories came from four sources: the scoping review5; the realist review; theories described by interviewees; and theories identified during iterative searches when we were looking for and testing possible mechanisms. We chose theories with the highest level of explanatory coherence, based on the three criteria of consilience, simplicity and analogy.17 18
Results
Stage 1: the coinquiry
This coinquiry along with programme documentation resulted in the following preliminary programme theory: GPs want to meet with their peers, share their problems and exchange ideas. CME credits or requirements from health insurance companies seem to be additional drivers to participate in QCs. Skilled facilitators are key to establish a safe environment where GPs share local data, and exchange experiences and knowledge. Reflection on personal experiences, successes and failures, helps in identifying learning needs. A goal-oriented facilitator helps members to choose the method they want to use to approach an issue and helps them build a learning environment where they adapt or create new knowledge which they then put into practice in a repetitive process. We described the CMO configurations we developed in this stage in online supplemental file 6.
bmjopen-2021-058453supp006.pdf (66.2KB, pdf)
Stage 2: realist review
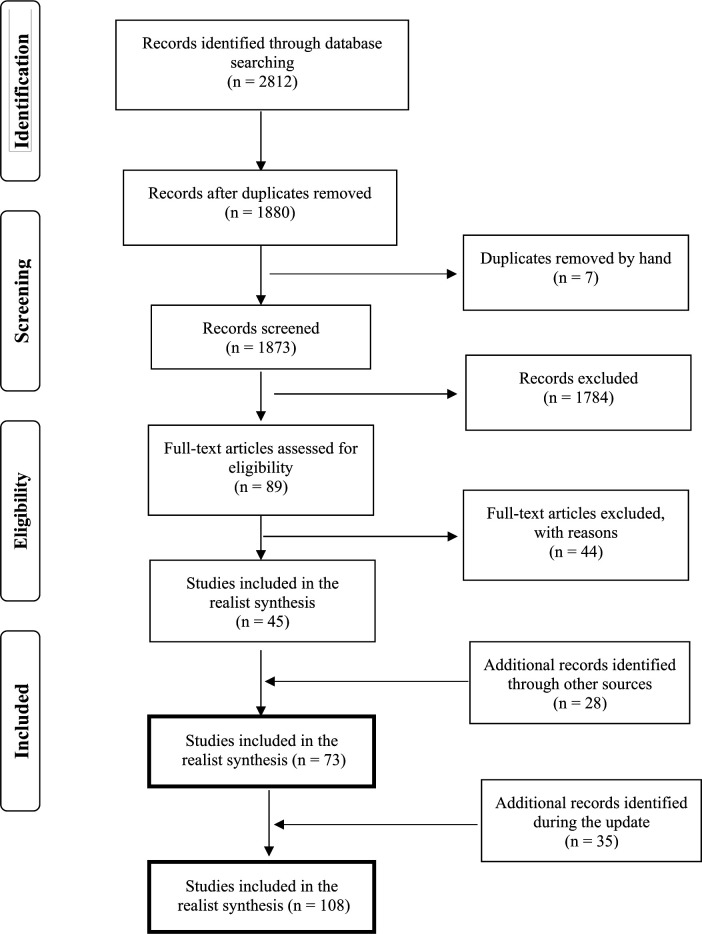
Our search strategy returned 2812 results (figure 1), out of which AR, JH and SM assessed 73 papers. An update in December 2020 yielded 35 more papers.
Figure 1.
Paper flow realist review.
The literature mainly covered QCs in which GPs participated. We found 24 relevant articles about German QCs, 12 about Dutch QCs and 2 about Swiss QC; 10 papers were about CME groups in Canada and Scotland, 6 about a QC research project in Norway, 3 about QCs on osteoporosis in Canada and 5 about the Drug Education Project in Sweden, Norway, the Netherlands and Slovakia; 6 papers covered QC projects in England, Austria, Belgium and France; 5 other relevant papers were from South Africa, the US (Hawaii and California), New Zealand and Australia. We categorised these papers into groups to clarify their kinship network.
Study designs varied by research question. Our search returned 5 study protocols, 2 case series, 14 before-and-after studies, 13 controlled before-and-after studies, 9 randomised controlled trials, 9 cluster randomised controlled trials, 12 surveys and 9 qualitative research papers that used data from interviews or focus groups. Few papers studied the performance of well-established QCs; data were often limited to interventions in newly formed groups. In pre-existing QCs (German, Dutch or Norwegian trials), researchers introduced their own interventions on prescription or test-ordering patterns rather than studying interventions chosen and designed by the QC group. For full details of study characteristics, see online supplemental file 7. The resulting literature-informed programme theory gave details about necessary preconditions, group processes, learning environment, how and why participants adapt, create and test new knowledge and that repetition is necessary for sustainable changes. We present the literature-based programme theory and supporting quotations from the literature in online supplemental file 8). The data we retrieved from the update search did not change our CMO configurations or programme theory.
bmjopen-2021-058453supp007.pdf (593.1KB, pdf)
bmjopen-2021-058453supp008.pdf (495.4KB, pdf)
Stage 3: the refined programme theory
Data from interviews and focus group helped us refine the wording of six CMO configurations and added three new configurations that linked the chains of outcomes. Participants emphasised that the national bodies should entrust QC with QI, but national organisations or professional association should be sufficiently flexible to allow local QCs to implement their plans, giving them a feeling that they had a say and a job to do. At the level of the group, they pointed out that individual character traits and different professional experiences along with differing opinions provide a necessary tension to stimulate lively discussions as long as mutual respect exists. However, there are (a few) individuals who experience critical feedback as threat to self-image and, as a consequence, withdraw or disturb the group process. See online supplemental file 9 for the resulting intermediate programme theory and supporting quotations and data from focus group sessions.
bmjopen-2021-058453supp009.pdf (425KB, pdf)
Stage 4: consolidating the programme theory
Interviews with stakeholders across healthcare systems
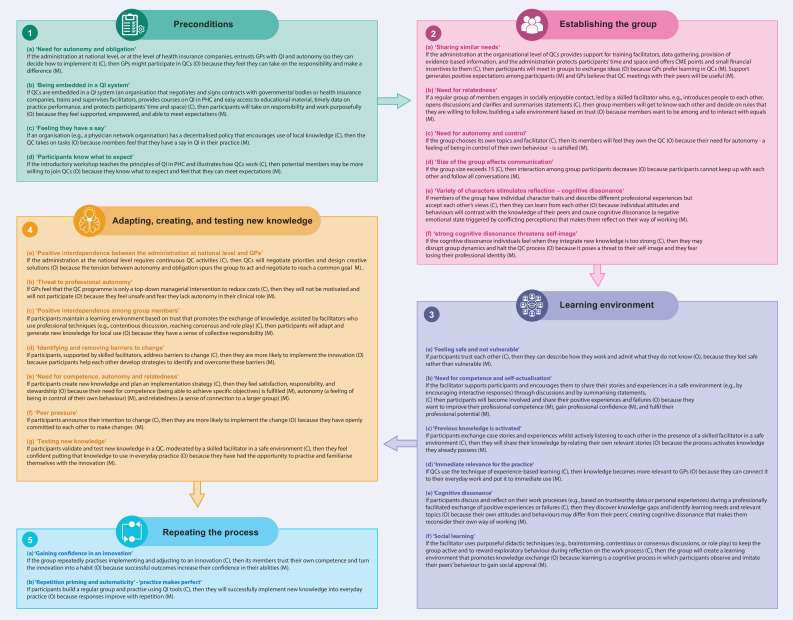
In addition to supporting existing CMO configurations, these interview data suggested that QCs can only succeed if they are embedded in a wider system that helps participants to negotiate and sign contracts with governmental bodies or health insurance companies, organises training and supervises facilitators, offers courses on QI in PHC, and facilitates access to educational material and timely data on practice performance (CMO configuration 1b ‘being embedded in a QI system’). For supporting quotations during these interviews, see online supplemental file 10. Figure 2 shows the final CMO configurations of the consolidated programme theory that was iteratively developed from stages 1–4.
Figure 2.
Consolidated programme theory on quality circles. GP, general practitioner; PHC, primary healthcare; QC, quality circle; QI, quality improvement.
bmjopen-2021-058453supp010.pdf (232.7KB, pdf)
Existing theories and their relationships to CMO configurations in the programme theory
Some theories about organisational context, groups, learning, knowledge exchange, development of innovations and their implementation were relevant. Some CMO configurations fit well with, or are directly supported by, existing theories, while others seem to clarify how existing theories work when they are applied to QCs. Table 2 summarises the theories and their corresponding CMO configurations.
Table 2.
Existing theories and their relationships to CMO configurations in the programme theory
| Theory | Explanation of relationships | CMO configurations in the programme theory (figure 2) |
| Receptive capacity of an organisation 22 24 58 | Theories about the organisational setting elucidate the mechanisms by which organisations help or hinder quality circles in their work. Quality circles should be embedded in a system that provides training in QI and promotes it by providing explicit knowledge, valuing tacit knowledge, and ensuring that groups have competent facilitators. These features are part of an organisation’s receptive capacity: how well it values, integrates, and uses new external knowledge. | CMO configuration 1 b-c |
| Self-determination theory59 | Self-determination theory suggests that GPs are motivated to participate in quality circles if they feel that the quality circle will satisfy their basic needs for competence, social bonding and autonomy. | CMO configurations 1 a, 1 c, 2 a-c, 3 b, 4 b and 4 e |
| Theories about groups 29 33 60–62 | Theories about groups and facilitation describe how groups form and norm their rules, a prerequisite for building an environment of trust in which participants can exchange ideas and thoughts. The knowledge and capacity of the group may be greater than the sum of the average of each individual’s capacity. When participants share their knowledge and incorporate all perspectives, they can collectively solve problems more efficiently than they could alone. | CMO configurations 2 b-d, 3 a-c, 4 c and 4 g |
| Social learning theory 63 64 | Social learning theory frames learning as an active cognitive process of perception and thinking in a social context. Participants in quality circles learn by observing and imitating peers. They also learn from the responses they receive, or expect to receive, when they try something new or avoid unrewarding actions. Learning depends much on individual expectations and feelings of competence to carry tasks. Organisational factors that lend support to learners, for example, by giving access to learning material, incentives or rewards, improve the process. | CMO configuration 3 f |
| Adult-learning theories65 | Adult-learning theories suggest that adults are highly motivated: they learn things that are immediately useful to them, and prefer to do so in a self-directed, task-oriented, experience-based manner. | CMO configurations 1 c, 2 b and 3 b-d |
| Experience-based learning66 67 | GPs prefer experiential learning, in which experience is the starting point. Reflecting on an experience enables GPs to restructure their knowledge. They turn insights gained from experience into knowledge and transfer them to other situations. They actively experiment with the new knowledge, and then report their experiences back to the group. | CMO configurations 3 b- e |
| Transformative learning theory 35 44 | Transformative learning begins with cognitive dissonance, a negative emotional state triggered by conflicting perceptions. Generally, people want to reduce discordant feelings. In the safe environment of a quality circle, cognitive dissonance prompts GPs to reflect on and accept new arguments or revise their old ones to resolve their internal conflict. | CMO configurations 3 e and 4 g |
| Social interdependence theory 45 68 | Social interdependence theory explains why groups may work together towards a common goal. When quality circle participants realise that they will only achieve their own goals if their peers achieve theirs, this creates a positive interdependence, which encourages participants to reassure and support each other in pursuit of those goals. Positive interdependence improves psychological well-being and raises self-esteem through cooperation and mutual appreciation. | CMO configurations 4 a and 4 c |
| Knowledge-creation theory 49–51 | Knowledge-creation theories describe the process by which implicit knowledge becomes explicit when participants relate and combine their experiences with other explicit knowledge like evidence-based information, generating new concepts that participants integrate into their everyday clinical practice. | CMO configurations 1 b, 3 c, 4 c, e, g |
| Theory of planned behaviour69 70 | The theory of planned behaviour describes how intentions can change behaviour: if the new behaviour makes sense, others approve and it feels easy enough to change. | CMO configuration 4 f |
| Automaticity 71 | There are theories that support the argument that quality circles are much more successful when they repeatedly implement new knowledge, giving participants the opportunity to build confidence in innovation and their quality circle skills. | CMO configurations 5 a-b |
CMO, context–mechanism–outcome; GP, general practitioner; QI, quality improvement.
Discussion
The consolidated programme theory
The most important contextual requirements for successful QCs are governmental trust in the ability of GPs to deliver QI and appropriate professional and administrative support for QC work. Professional support includes training in QI techniques, easy access to teaching materials and trustworthy personalised performance data. Administrative support includes providing protected time, an appropriate venue, and financial resources for meetings. If QC groups are to be successful, participants must feel that they have a say in their CPD and QI work, but the additional workload from participating in QCs must be manageable.
Several factors in QCs influence practitioner performance. QC members and their group dynamics are at the core of the process. Facilitators help participants build social bonds and mutual trust so that the QC becomes a safe environment that fosters open discussions and where participants link insights to everyday practice, manage uncertainty and develop their professional role. Members reflect on personal experiences, add information from relevant sources, including evidence-based information and personal performance data, and then develop new ideas and concepts to improve their practice. With skilful facilitation, participants work towards a common goal and test their new ideas in the group, knowing that success depends on the individual member contributions. The QC process raises self-esteem and fosters psychological well-being. QI is cyclical, so putting innovations into practice is a continuous and repetitive process that increases participants’ confidence in their innovation and QI skills with each repetition.
How the programme theory contributes to our understanding of QCs and relates to existing QC literature
Our understanding that QCs should be embedded in a system of QI that values, integrates and uses new external knowledge aligns with the existing literature.22 23 Health systems should provide training in QI tools and give access to trustworthy data (explicit knowledge) that help participants identify their own learning needs (CMO configuration 1 b-c and 3 e in figure 2.24–28
Our research confirmed that well-functioning groups are essential to the QC process. The group’s capacity for problem-solving surpasses the ability of the individual when members share and pool their experiences and views.26 29 Supportive facilitation in a non-threatening environment of mutual trust eases learning in the group and opens possibilities for sharing, creating and integrating new knowledge.22 26 30–32 Trust implies that participants operate on the basis of equality and mutual respect, according to the principle of benevolence, when they take risks and participate actively in the group (CMO configurations 1 c, 2 b 3 a-c, 4 c and 4 g in figure 2).33 34
Literature and interview data provided us with mechanisms that had not been reported in current QC literature. Cognitive dissonance, like conflicting attitudes, beliefs or behaviours that create unease, is a mechanism that compels GPs to reflect on, accept, and adopt new reasoning to resolve inner conflict. This is the starting point of transformative learning.35According to our interview data, GPs can risk doing this in a QC group where they feel safe and confident, a process described in educational literature (CMO configurations 3 e and 4 g in figure 2).36–40
Our data show that reflecting on an experience enables GPs to restructure their knowledge for transfer to other situations. When they share knowledge and experience, they can validate their clinical reasoning and thus integrate tacit and explicit knowledge and develop professional values like integrity and empathy; this process is recognised in the literature on psychology of learning as important to professional development.41 42 Explicit knowledge can be easily expressed through language or in writing because it is factual, for example, evidence-based information, or a measurement of practice performance; whereas implicit or tacit knowledge is embodied in the knowledge or skills that a GP accumulates through experience but may find difficult to communicate.43 GPs need tangible experiences and opportunities for repeated attempts to absorb new knowledge (CMO configurations 3 b-e, 4 g, and 5 a in figure 2).44
According to our data, the mechanism of positive interdependence explained how and why collective or social learning can flourish and create a sense of ownership in QCs. When QC participants realise that they will only achieve their own goals if their peers achieve theirs, they are encouraged to reassure and support each other. Peers create new ideas and the cooperation and mutual appreciation that results improve their psychological well-being, increase their self-esteem, and may reduce their risk of burnout (CMO configurations 4 a and 4 c, e in figure 2).1 45–48
Participants relate and combine their experiences with other, explicit knowledge and generate new concepts or improve quality of care—a process described in business literature as knowledge creation.41 49–54 A key function of QCs is to merge familiar knowledge, local context and personal experience with evidence-based knowledge and extend this from the micro view of single-patient care to a wider view of the whole system (CMO configurations 3 c, 4 e, 4 g and 5 g in figure 2).
Participants may change their behaviour if it makes sense to do so, if others approve, and if change is not too demanding.55 But to embed these behaviour changes in everyday practice, the QC processes must be repeated until they become habitual, especially during the phase when GPs are implementing new knowledge,56 57 (CMO configurations 4 f, 5 a and 5 b in figure 2).
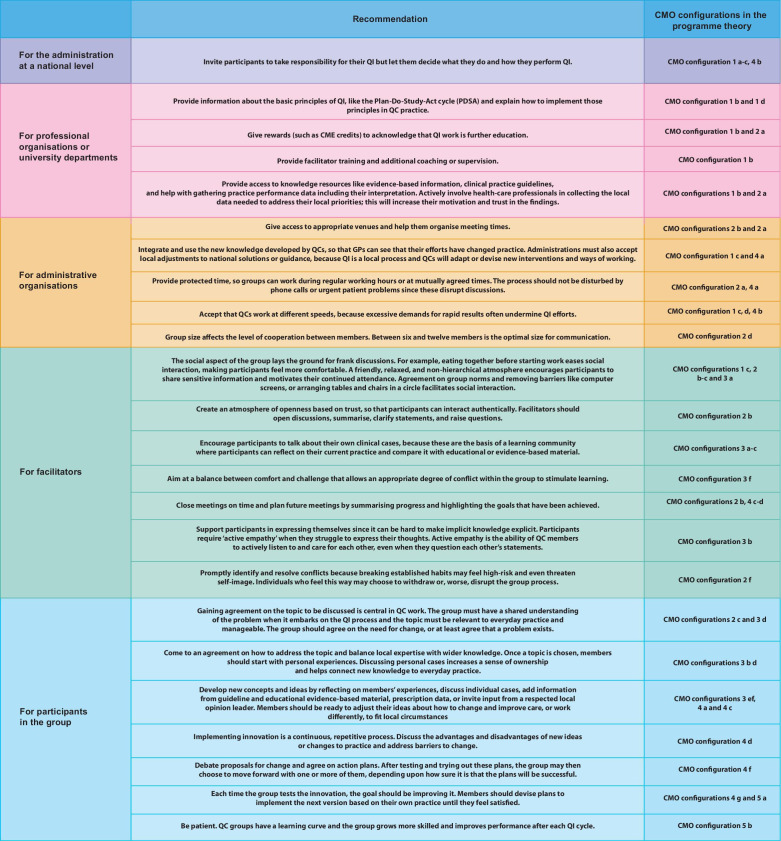
Implications for policy and practice
Based on our findings, we summarised the recommendations for organising and performing QCs to increase the likelihood that GPs successfully improve the quality of their work (figure 3). Each recommendation is based on one or more CMO configurations. These recommendations should be considered as a form of decision support that QCs can draw on to determine if action is needed in their specific circumstances.
Figure 3.
Recommendations and principles for organising successful quality circles. CME, Continuous Medical Education; CMO, context–mechanism–outcome; GP, general practitioner; QC, quality circle; QI, quality improvement.
The QC process and its implications are summarised as an infographic in online supplemental file 11).
bmjopen-2021-058453supp011.pdf (2.3MB, pdf)
Limitations
Our study has some limitations The resulting theory relies on the detail and depth of the reports we identified in our literature review and on the veracity and adequacy of the information stakeholders revealed during 2015–2020 in Europe. CMO configurations reflect and explain the complex process in QCs in the current context of European PHC, and may need to be adapted in response to future changes.
Quality appraisal of relevance and rigour of data that contributed to the emerging programme theory may depend on research team judgements. Another team might have taken differing decisions.
We could not include all theories found during iterative searches but had to make choices of the ones that fitted best. Finally, we could not relate all aspects of the theories in table 2 to the CMO configurations to explain how the programme theory’s mechanisms interrelate.
Future research
Future researchers can build on this programme theory to design, implement and evaluate new QC interventions. We encourage researchers to test our programme theory to confirm, refute or refine it for specific settings and/or professional groups.
Conclusion
Our consolidated programme theory explains how participation in QCs can improve standard practice, enhance professional development and increase psychological well-being. Group dynamics are at the core of the process. Facilitators help participants exchange knowledge in a safe environment where they generate new concepts to improve their practice. With repetition, QC participants gain confidence in their QI skills and put their innovations into practice. The most important contextual requirements for successful QCs are (1) governmental trust in GPs’ abilities to deliver QI and appropriate support like professional facilitation, (2) training in QI techniques, (3) access to educational material and personal performance data; (4) granting protected time, appropriate venues and financial resources for QC group members.
Supplementary Material
Footnotes
Twitter: @Smickan
Contributors: AR performed the research as part of formal postgraduate studies (DPhil Programme in Evidence-Based Health Care, University of Oxford, Oxford, UK). SM and JH supervised the development of the research and actively participated in the review process (eligibility, selection, data extraction followed by discussions). GW as AR’s main supervisor, provided important input regarding the methodology and supervised the whole research process. All authors critically reviewed the text, assisted with editing read and approved the final manuscript. GW, SM and JH contributed independently to this project from their academic and methodological experience. The guarantor AR accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The project was approved by the Central University Research Ethics Committee in Oxford (MSD-IDREC-C1-2015-002); it fulfilled the requirements of informed consent: handling of personal information and confidentiality conformed to the operational principles of the Declaration of Helsinki and adhered to the Belmont Report principles mandating respect for persons, beneficence and justice.
References
- 1.Rohrbasser A, Harris J, Mickan S, et al. Quality circles for quality improvement in primary health care: their origins, spread, effectiveness and lacunae- a scoping review. PLoS One 2018;13:e0202616. 10.1371/journal.pone.0202616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rohrbasser A, Kirk UB, Arvidsson E. Use of quality circles for primary care providers in 24 European countries: an online survey of European Society for quality and safety in family practice delegates. Scand J Prim Health Care 2019;37:302–11. 10.1080/02813432.2019.1639902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carrieri D, Mattick K, Pearson M, et al. Optimising strategies to address mental ill-health in doctors and medical students: 'Care Under Pressure' realist review and implementation guidance. BMC Med 2020;18:76. 10.1186/s12916-020-01532-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plsek PE, Greenhalgh T. The challenge of complexity in health care. BMJ 2001;323:625–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rohrbasser A, Mickan S, Harris J. Exploring why quality circles work in primary health care: a realist review protocol. Syst Rev 2013;2:1–7. 10.1186/2046-4053-2-110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davidoff F, Dixon-Woods M, Leviton L, et al. Demystifying theory and its use in improvement. BMJ Qual Saf 2015;24:228–38. 10.1136/bmjqs-2014-003627 [DOI] [Google Scholar]
- 7.Wong G, Greenhalgh T, Westhorp G. RAMESES II Project: “Theory” in realist evaluation 2017 [cited 2019 27/04]. Available: http://www.ramesesproject.org/media/RAMESES_II_Theory_in_realist_evaluation.pdf [Accessed 28 April 2019].
- 8.Macaulay AC, Commanda LE, Freeman WL, et al. Participatory research maximises community and lay involvement. BMJ 1999;319:774–8. 10.1136/bmj.319.7212.774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jagosh J, Macaulay AC, Pluye P, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311–46. 10.1111/j.1468-0009.2012.00665.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Funnel SC, Rogers PI. Purposeful program theory: effective use of theories of change and logic models. San Francisco: Wiley, 2011: 550. [Google Scholar]
- 11.Leeuw FL. Reconstructing program theories: methods available and problems to be solved. Am J Eval 2003;24:5–20. 10.1177/109821400302400102 [DOI] [Google Scholar]
- 12.Astbury B, Leeuw FL. Unpacking black boxes: mechanisms and theory building in evaluation. Am J Eval 2010;31:363–81. 10.1177/1098214010371972 [DOI] [Google Scholar]
- 13.Dalkin SM, Greenhalgh J, Jones D, et al. What’s in a mechanism? Development of a key concept in realist evaluation. Implementation Science 2015;10:1–5. 10.1186/s13012-015-0237-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Emmel N, Greenhalgh J, Manzano A. Doing Realist Research. London: SAGE, 2018. [Google Scholar]
- 15.Gill PJ, Roberts NW, Wang KY, et al. Development of a search filter for identifying studies completed in primary care. Fam Pract 2014;31:739-45. 10.1093/fampra/cmu066 [DOI] [PubMed] [Google Scholar]
- 16.Booth A, Harris J, Croot E, et al. Towards a methodology for cluster searching to provide conceptual and contextual “richness” for systematic reviews of complex interventions: case study (CLUSTER). BMC Med Res Methodol 2013;13:1–13. 10.1186/1471-2288-13-118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thagard P. Explanatory coherence. Behav Brain Sci 1989;12:435–67. 10.1017/S0140525X00057046 [DOI] [Google Scholar]
- 18.Haig BD, Evers CW. Realist inquiry in social science. London: SAGE, 2016. [Google Scholar]
- 19.Edwards PK, O'Mahoney J, Vincent S, eds. Studying Organizations Using Critical Realism: A Practical Guide. Oxford University Press, 2014. [Google Scholar]
- 20.Pawson R. Theorizing the interview. Br J Sociol 1996;47:295–314. 10.2307/591728 [DOI] [Google Scholar]
- 21.Manzano A. The craft of interviewing in realist evaluation. Evaluation 2016;22:342–60. 10.1177/1356389016638615 [DOI] [Google Scholar]
- 22.Berta W, Cranley L, Dearing JW, et al. Why (we think) facilitation works: insights from organizational learning theory. Implement Sci 2015;10:141. 10.1186/s13012-015-0323-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kilo CM. A framework for collaborative improvement: lessons from the Institute for healthcare improvement's breakthrough series. Qual Manag Health Care 1998;6:1–13. 10.1097/00019514-199806040-00001 [DOI] [Google Scholar]
- 24.Lane PJ, Lubatkin M. Relative absorptive capacity and interorganizational learning. Strategic Management Journal 1998;19:461–77. [Google Scholar]
- 25.Kelly DR, Cunningham DE, McCalister P. Applying evidence in practice through small-group learning: a qualitative exploration of success. Quality in Primary Care 2007;15:93–9. [Google Scholar]
- 26.Brennan SE, Bosch M, Buchan H, et al. Measuring organizational and individual factors thought to influence the success of quality improvement in primary care: a systematic review of instruments. Implement Sci 2012;7:1–19. 10.1186/1748-5908-7-121 [DOI] [Google Scholar]
- 27.Brennan SE, Bosch M, Buchan H, et al. Measuring team factors thought to influence the success of quality improvement in primary care: a systematic review of instruments. Implementation Science 2013;8:1–20. 10.1186/1748-5908-8-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang H, Jefferson ER, Gotink M, et al. Collaborative improvement in Scottish GP clusters after the quality and outcomes framework: a qualitative study. British Journal of General Practice 2021;71:e719–27. 10.3399/BJGP.2020.1101 [DOI] [Google Scholar]
- 29.Kozlowski SWJ, Ilgen DR. Enhancing the effectiveness of work groups and teams. Psychol Sci Public Interest 2006;7:77–124. 10.1111/j.1529-1006.2006.00030.x [DOI] [PubMed] [Google Scholar]
- 30.Rhydderch M, Edwards A, Marshall M, et al. Developing a facilitation model to promote organisational development in primary care practices. BMC Fam Pract 2006;7:38. 10.1186/1471-2296-7-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dogherty EJ, Harrison MB, Graham ID. Facilitation as a role and process in achieving evidence-based practice in nursing: a focused review of concept and meaning. Worldviews Evid Based Nurs 2010;7:76–89. 10.1111/j.1741-6787.2010.00186.x [DOI] [PubMed] [Google Scholar]
- 32.Elwyn G, Greenhalg T, Macfarlane F, eds. Groups a guide to small group work in healthcare, management, education and research. Radcliffe Medical Press, 2004. [Google Scholar]
- 33.Cross R, Rice RE, Parker A. Information seeking in social context: structural influences and receipt of information benefits. IEEE Transactions on Systems, Man and Cybernetics, Part C 2001;31:438–48. 10.1109/5326.983927 [DOI] [Google Scholar]
- 34.Gubbins C, MacCurtain S. Understanding the dynamics of collective learning: the role of trust and social capital. Adv Dev Hum Resour 2008;10:578–99. 10.1177/1523422308320372 [DOI] [Google Scholar]
- 35.Mezirow J. Transformative learning: theory to practice. New Directions for Adult and Continuing Education 1997;1997:5–12. 10.1002/ace.7401 [DOI] [Google Scholar]
- 36.Newton J, Hutchinson A, Steen N, et al. Educational potential of medical audit: observations from a study of small groups setting standards. Qual Health Care 1992;1:256–9. 10.1136/qshc.1.4.256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Payne VL, Hysong SJ. Model depicting aspects of audit and feedback that impact physicians’ acceptance of clinical performance feedback. BMC Health Serv Res 2016;16:1–12. 10.1186/s12913-016-1486-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Braak M, Visser M, Holtrop M, et al. What motivates general practitioners to change practice behaviour? A qualitative study of audit and feedback group sessions in Dutch general practice. BMJ Open 2019;9:e025286–8. 10.1136/bmjopen-2018-025286 [DOI] [Google Scholar]
- 39.Brennan N, Bryce M, Pearson M, et al. Towards an understanding of how appraisal of doctors produces its effects: a realist review. Med Educ 2017;51:1002–13. 10.1111/medu.13348 [DOI] [PubMed] [Google Scholar]
- 40.Eva KW, Regehr G. Effective feedback for maintenance of competence: from data delivery to trusting dialogues. CMAJ 2013;185:463–4. 10.1503/cmaj.121772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Eraut M. Non-formal learning and tacit knowledge in professional work. Br J Educ Psychol 2000;70 (Pt 1:113–36. 10.1348/000709900158001 [DOI] [PubMed] [Google Scholar]
- 42.Oborn E, Barrett M, Racko G. Knowledge translation in healthcare: incorporating theories of learning and knowledge from the management literature. J Health Organ Manag 2013;27:412–31. 10.1108/JHOM-01-2012-0004 [DOI] [PubMed] [Google Scholar]
- 43.Hildreth PM, Kimble C. The duality of knowledge. Information research 2002;8. [Google Scholar]
- 44.Sandars J. Transformative learning: the challenge for reflective practice. Work Based Learning in Primary Care 2006;4:6–10. [Google Scholar]
- 45.Johnson DW, Johnson RT. An educational psychology success story: social interdependence theory and cooperative learning. Educational Researcher 2009;38:365–79. 10.3102/0013189X09339057 [DOI] [Google Scholar]
- 46.Eliasson G, Mattsson B. From teaching to learning. experiences of small CME group work in general practice in Sweden. Scand J Prim Health Care 1999;17:196–200. 10.1080/028134399750002403 [DOI] [PubMed] [Google Scholar]
- 47.Zaher E, Ratnapalan S. Practice-Based small group learning programs: systematic review. Can Fam Physician 2012;58:637–42. [PMC free article] [PubMed] [Google Scholar]
- 48.Lancaster J, Prager S, Nash L, et al. Psychiatry peer review groups in Australia: a mixed-methods exploration of structure and function. BMJ Open 2020;10:e040039. 10.1136/bmjopen-2020-040039 [DOI] [Google Scholar]
- 49.Nonaka I, Byosiere P, Borucki CC, et al. Organizational knowledge creation theory: a first comprehensive test. Int Bus Rev 1994;3:337–51. 10.1016/0969-5931(94)90027-2 [DOI] [Google Scholar]
- 50.Von Krogh G, Ichijo K, Nonaka I. Enabling knowledge creation: how to unlock the mystery of tacit knowledge and release the power of innovation. Oxford university press, 2000. [Google Scholar]
- 51.Nonaka I, von Krogh G, Knowledge Perspective—Tacit. Perspective—Tacit knowledge and knowledge conversion: controversy and advancement in organizational knowledge creation theory. Organization Science 2009;20:635–52. 10.1287/orsc.1080.0412 [DOI] [Google Scholar]
- 52.Gabbay J, May Ale, le May A. Evidence based guidelines or collectively constructed “mindlines?” Ethnographic study of knowledge management in primary care. BMJ 2004;329:1013–4. 10.1136/bmj.329.7473.1013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Eraut M. Learning from other people in the workplace. Oxf Rev Educ 2007;33:403–22. 10.1080/03054980701425706 [DOI] [Google Scholar]
- 54.Orzano AJ, McInerney CR, Scharf D, et al. A knowledge management model: implications for enhancing quality in health care. Journal of the American Society for Information Science and Technology 2008;59:489–505. 10.1002/asi.20763 [DOI] [Google Scholar]
- 55.Armson H, Elmslie T, Roder S, et al. Is the cognitive complexity of Commitment-to-Change statements associated with change in clinical practice? an application of Bloom's taxonomy. J Contin Educ Health Prof 2015;35:166–75. 10.1002/chp.21303 [DOI] [PubMed] [Google Scholar]
- 56.Poldrack RA, Gabrieli JD. Characterizing the neural mechanisms of skill learning and repetition priming: evidence from mirror reading. Brain 2001;124:67–82. 10.1093/brain/124.1.67 [DOI] [PubMed] [Google Scholar]
- 57.Hauptmann B, Karni A. From primed to learn: the saturation of repetition priming and the induction of long-term memory. Brain Res Cogn Brain Res 2002;13:313–22. 10.1016/s0926-6410(01)00124-0 [DOI] [PubMed] [Google Scholar]
- 58.Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. Qual Health Care 1998;7:149–58. 10.1136/qshc.7.3.149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000;55:68–78. 10.1037//0003-066x.55.1.68 [DOI] [PubMed] [Google Scholar]
- 60.Dirks KT, Ferrin DL. The role of trust in organizational settings. Organization Science 2001;12:450–67. 10.1287/orsc.12.4.450.10640 [DOI] [Google Scholar]
- 61.Pereles L, Lockyer J, Fidler H. Permanent small groups: group dynamics, learning, and change. J Contin Educ Health Prof 2002;22:205–13. 10.1002/chp.1340220404 [DOI] [PubMed] [Google Scholar]
- 62.Baumeister RF, Ainsworth SE, Vohs KD. Are groups more or less than the sum of their members? the moderating role of individual identification. Behavioral and Brain Sciences 2016;39:1–38. [Google Scholar]
- 63.Bandura A, McClelland DC. Social learning theory, 1977. [Google Scholar]
- 64.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol 2001;52:1–26. 10.1146/annurev.psych.52.1.1 [DOI] [PubMed] [Google Scholar]
- 65.Mukhalalati BA, Taylor A. Adult learning theories in context: a quick guide for healthcare professional educators. J Med Educ Curric Dev 2019;6:1–10. 10.1177/2382120519840332 [DOI] [Google Scholar]
- 66.Kolb D, ed. Experiential Learning: Experience as the Source of Learning and development. Prentice Hall, 1984. [Google Scholar]
- 67.Kolb DA, Boyatzis RE, Mainemelis C. Experiential learning theory: previous research and new directions. Perspectives on Thinking, Learning, and Cognitive Styles 2001;1:227–47. [Google Scholar]
- 68.Johnson DW, Johnson RT. New developments in social interdependence theory. Genet Soc Gen Psychol Monogr 2005;131:285–358. 10.3200/MONO.131.4.285-358 [DOI] [PubMed] [Google Scholar]
- 69.Ajzen I. The theory of planned behavior. Organizational behavior and human decision processes 1991;50:179–211. [Google Scholar]
- 70.Eccles MP, Hrisos S, Francis J, et al. Do self- reported intentions predict clinicians' behaviour: a systematic review. Implement Sci 2006;1:28. 10.1186/1748-5908-1-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Logan GD. Repetition priming and automaticity: common underlying mechanisms? Cogn Psychol 1990;22:1–35. 10.1016/0010-0285(90)90002-L [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-058453supp001.pdf (58.9KB, pdf)
bmjopen-2021-058453supp002.pdf (69.9KB, pdf)
bmjopen-2021-058453supp003.pdf (69.1KB, pdf)
bmjopen-2021-058453supp004.pdf (59.4KB, pdf)
bmjopen-2021-058453supp005.pdf (68.7KB, pdf)
bmjopen-2021-058453supp006.pdf (66.2KB, pdf)
bmjopen-2021-058453supp007.pdf (593.1KB, pdf)
bmjopen-2021-058453supp008.pdf (495.4KB, pdf)
bmjopen-2021-058453supp009.pdf (425KB, pdf)
bmjopen-2021-058453supp010.pdf (232.7KB, pdf)
bmjopen-2021-058453supp011.pdf (2.3MB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.