Abstract
Background
There are limited data on large-scale, multi-level implementation research studies to improve hypertension diagnosis, treatment, and control rates at the primary health care (PHC) level in Africa. We describe the characteristics, treatment, and control rates of patients with hypertension in public PHC centers in the Hypertension Treatment in Nigeria Program.
Methods
Data were collected from adults ≥18 years at 60 public PHC centers between January 2020 and November 2020. Hypertension treatment rates were calculated at registration and upon completion of the initial visit. Hypertension control rates were calculated based on systolic and diastolic blood pressures <140/90 mmHg. Regression models were created to evaluate factors associated with hypertension treatment and control status.
Results
4,927 individuals (66.7% female, mean [SD] age = 48.2 [12.9] years) were included. Mean (SD) systolic blood pressure was higher in males compared with females (152.9 [20.0] mm Hg versus 150.8 [21.0] mm Hg, p = 0.001). Most (58.3%) patients were on treatment at the time of registration, and by the end of the baseline visit, 89.2% of patients were on treatment. The baseline hypertension control rate was 13.1%, and control was more common among patients who were older (adjusted OR [95% CI]: 1.01 [1.01, 1.02]), female (adjusted OR [95% CI]: 1.30 [1.05, 1.62]), who used fixed dose combination therapy (adjusted OR [95% CI]: 1.83 [1.49, 2.26]), and had higher education levels.
Conclusions
This baseline report of the largest facility-based hypertension study in Africa demonstrates high hypertension treatment rates but low control rates.
Keywords: hypertension, global health, implementation research
INTRODUCTION
In low- and middle-income countries, community-based studies demonstrate that less than 3 out of every 10 patients are on treatment, and only 1 out of every 10 patients have their blood pressure controlled.(1) In Nigeria, which is the most populous country in Africa, the most recent nationally-representative data demonstrate an age-standardized hypertension prevalence of 38%, with suboptimal hypertension awareness (60%), treatment (34%), and control (12%) rates.(2) Reasons for these low rates are myriad and include: weak health systems, including lack of standardized protocols and health information systems for longitudinal hypertension management; few qualified, trained, and empowered health personnel to provide team-based care; limited access to quality equipment and medicines; low health literacy; and direct and indirect costs of evaluation and management.(3–5)
Evidence-based, multi-level implementation strategies to improve hypertension treatment and control rates through health behaviors and pharmacotherapy are recommended to overcome multi-level barriers.(6,7) These strategies have been demonstrated to improve hypertension control rates from 44% to 90% in unselected patients in the Kaiser Permanente Northern California health system.(8) Based on this evidence and experience, the World Health Organization (WHO) published its HEARTS technical package in 2016 to improve cardiovascular care, including hypertension care, by implementing these strategies at the primary health care level.(9)
However, despite the large burden of hypertension and its consequences, as well as the potential benefits of implementing evidence-based interventions, there are very limited number of reports of large-scale, multi-level implementation research studies to improve hypertension diagnosis, treatment, and control rates at the primary health care level in Africa,(9) and none in Nigeria. Furthermore, hypertension diagnostic and management services have not been available in public, primary health care settings in Nigeria, despite the perceived fit, acceptability, appropriateness, relative advantage, and demonstrated feasibility. We therefore created the Hypertension Treatment in Nigeria Program to implement and evaluate a culturally- and contextually-adapted, large-scale, evidence-based implementation package to improve the cascade of hypertension care in public, primary health care centers in the Federal Capital Territory of Nigeria.
The primary objective of this baseline report was to describe the clinical characteristics, treatment, and control rates of patients with hypertension in public, primary health centers in the Federal Capital Territory of Nigeria that are part of the Hypertension Treatment in Nigeria Program. Secondary objectives were to compare baseline rates of blood pressure control by age, sex, level of education, area council and to evaluate short-term retention, or follow-up rates, in care during the baseline study period as recommended by Nigeria’s national hypertension treatment protocol (10).
METHODS
Study Design and Population
The Hypertension Treatment in Nigeria Program is a prospective, longitudinal type 2 hybrid implementation research study that is evaluating implementation and effectiveness of a multi-level, evidence-based implementation package using an interrupted time series design (NCT04158154).(11) Formative work, including site readiness assessment and sampling methods of primary health care centers, has been published.(12) Briefly, at the study initiation, the Federal Capital Territory of Nigeria had 243 primary health care centers across 62 wards in 6 local government area councils. To be eligible, study sites needed to have 2 full-time staff and be operational, accessible, and safe for the research team to visit and work. A multi-stage probability sampling frame was used to select sites based on geographic representation and population size, with additional sites selected after consultation with the Nigerian Federal Ministry of Health and the Federal Capital Territory’s Primary Health Care Board. All 60 selected primary health care centers agreed to participate and were included in the program.
The first 11 months of the program (January 2020 to November 2020) represented the pre-intervention, control period, and the remaining 37 months represent the post-intervention period (December 2020 to December 2023). The multi-level implementation package was based on the WHO HEARTS technical package(9) and Kaiser Permanente Northern California model(8) of hypertension control and includes: 1) patient registration and empanelment (health system level), 2) standard treatment protocol (national policy level), 3) encouragement of fixed-dose combination therapy (health system level), 4) team-based care (health worker level), and 5) home blood pressure monitoring and health coaching (patient-level). During the control phase, the only component of the implementation package used was a registry for patient registration and empanelment. Prior to initiation of the registry, physicians, nurses, community health extension workers, and community health officers received in-person, 2-day case-based training from the research team on blood pressure measurement and principles of hypertension diagnosis and management based on materials in the WHO HEARTS technical package.(9) On-site training of the same staff as well as record information officers preceded initiation at each site, which was indexed by registration of the sites’ first patient with hypertension. Initiation of all 60 primary health care centers occurred between 20 January 2020 and 13 March 2020.
Study Population
Sites were instructed to measure blood pressures among all adults (18 years and older) who presented to the participating primary health care center using a standard approach. Two blood pressure measurements were taken in each patient by a trained physician, nurse, community health extension worker, or community health officer using an automated blood pressure monitor (Omron M3; HEM-7131-E, Kyoto, Japan) provided by the study team. Blood pressures were measured after a 5-minute rest period, and patients were seated with their back, arms, and feet supported. The research team performed periodic site monitoring and supportive supervision to ensure that blood pressures were measured accurately with additional, on-site training provided as needed.
Consecutive adults with hypertension, defined as: 1) a history of hypertension, 2) persistently elevated SBP of 140 mm Hg or above, 3) persistently elevated diastolic blood pressure (DBP) of 90 mm Hg or above, or 4) use of blood pressure lowering medications, including those in the 2019 Nigeria Hypertension Treatment Protocol,(10) were registered at their respective primary health care centers. Persistently elevated blood pressures were defined based on two or more measurements taken at least one week apart at respective health centers. Documentation of patient registration comprised addition to a site-based ledger and inclusion of a paper case report form within the patients’ file at the site. Registered patients were given a diagnosis and treatment card and were asked to return to the primary health care center for monthly follow-up for usual care during the program’s baseline period.
Medical history, medications, and anthropometry data were collected for each registered patient on paper case report forms using a standardized protocol and methods by trained study staff. Trained record information officers at each study site performed electronic data entry using the REDCap (Research Electronic Data Capture) mobile application hosted at the University of Abuja. REDCap is a secure, web-based software platform designed to support data capture for research studies, providing: 1) an intuitive interface for validated data capture; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for data integration and interoperability with external sources.(13)
Staff from the 60 primary health care centers were provided with personal protective equipment and hand sanitizer by the study team at the beginning of the COVID-19 pandemic in Nigeria to promote health care worker and patient safety.
Statistical Analysis
Bi-weekly data status and quality reports were created to identify missing and low-quality data, including outliers and data entry errors. The research team reviewed sites’ reports with respective record information officers to verify or correct data based on review of source documents.
De-identified descriptive data were reported as means (standard deviation) and medians (interquartile ranges, IQR) for continuous variables if data were skewed, and as proportions (95% CI) for categorical variables. Baseline hypertension treatment rates were calculated by dividing the number of patients taking 1 or more blood pressure lowering medication at the time of first visit by the total number of patients with hypertension. Treatment rates using any (two- or three-drug) fixed-dose combination were similarly calculated. Baseline hypertension control rates were calculated by dividing the number of patients with systolic and diastolic blood pressures less than 140/90 mm Hg by the total number of patients with hypertension. The proportion of treated patients who were controlled was also calculated. Data were analyzed overall and by key subgroups, including by sex, primary health care center, area council, and calendar month. We calculated the rate of retention, or follow-up rate, based on return to clinic within 31 days of the baseline visit. We also calculated follow-up at 37 days as a sensitivity analysis. Follow-up clinical data will be reported in future reports.
A complete case analysis was performed. Hierarchical mixed-effect multivariable logistic regression models were created to evaluate associations between patient, site, and area council-level factors and baseline hypertension treatment and control. Unadjusted and adjusted models are reported. Models were adjusted for age, sex, and patients’ level of education as a marker of socioeconomic position as well as factors previously demonstrated to be associated with hypertension awareness (as a proxy for health system access), baseline treatment (i.e., fixed dose combination therapy), and blood pressure as a proxy for baseline control (i.e., body mass index, alcohol use).(1, 2) Random effects modeling was used to account for within-site clustering. A two-sided p value <0.05 was used to detect statistical significance, and no adjustments were made for multiple comparisons. SAS version 9.4 (SAS, Cary, NC, USA) and R version 4.0.5 (R Foundation, Vienna, Austria) were used for statistical analyses.
Ethics Review and Informed Consent
The study protocol was reviewed and approved by the ethics boards of University of Abuja Teaching Hospital, Federal Capital Territory of Nigeria, and Northwestern University, as well as the program’s Data and Safety Monitoring Board. Patient informed consent was waived based on the Common Rule.
RESULTS
Study Population
From January 2020 to November 2020, 5,103 unique patients were recruited and registered from 60 primary health care centers in six area councils. After excluding individuals with missing or erroneous data on age, sex, or blood pressure or without meeting diagnostic criteria for hypertension, there were 4,927 individuals included in the current analysis (Figure 1) and who had 13,256 unique visits (Supplemental Table 1). The median (IQR) number of registered patients at each primary health center per month was 7 (Supplemental Figure 1)
Figure 1.
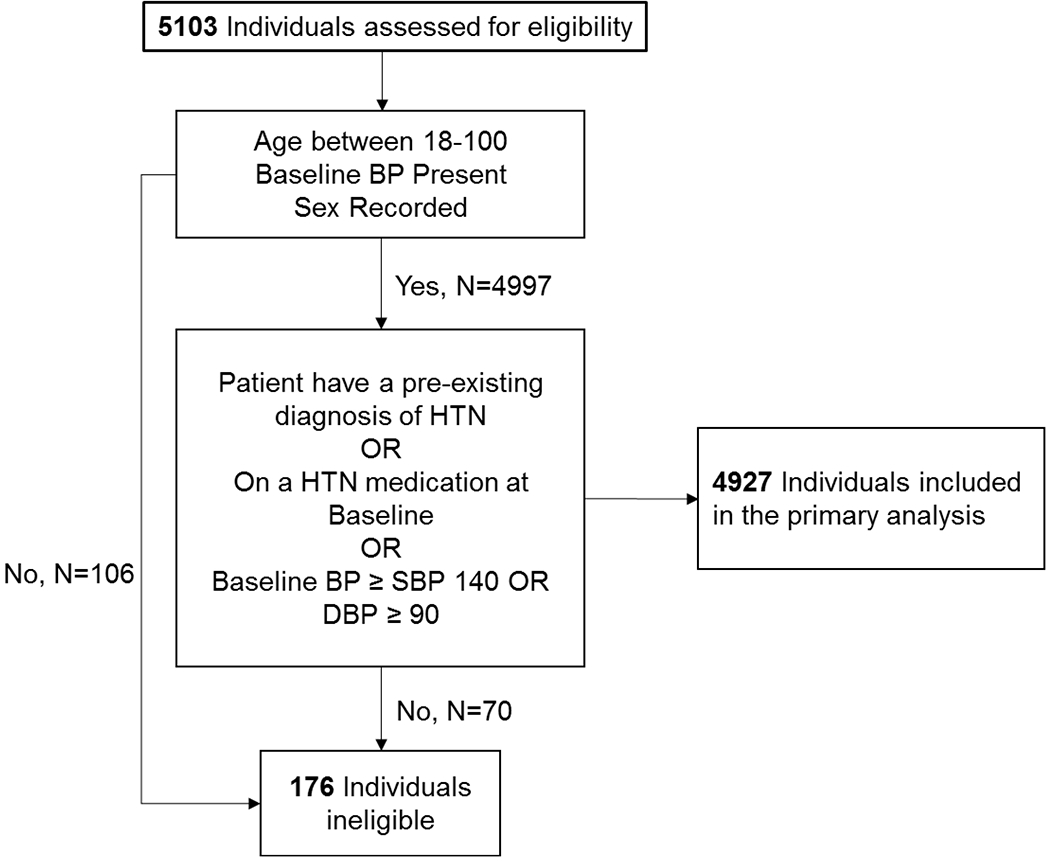
Flow diagram of study participants.
Table 1 reports patients’ demographics and clinical characteristics, overall and by sex. Mean (standard deviation, SD) age was 48.2 (12.9) years, 66.7% were female, and 27.2% never attended school. Most (56.2%) patients had a prior history of hypertension, but self-reported history of comorbid factors was uncommon, including diabetes mellitus (5.9%), stroke, (1.1%), heart attack (0.4%), and heart failure (0.4%). Smoking was reported in 1.3% of patients, with a higher smoking rate in males compared with females (3.3% versus 0.3%, p<0.001). Mean (SD) body mass index was higher in females compared with males (27.8 [6.2] kg/m2 versus 26.2 [4.9] kg/m2, p<0.001). The mean (SD) of the second SBP measured was higher in males compared with females (152.9 [20.0] mm Hg versus 150.8 [21.0] mm Hg, p = 0.001), but mean DBP levels were similar between males and females.
Table 1.
Patients’ baseline sociodemographics, clinical characteristics, and blood pressure overall and by sex.
| Variables | Total (N=4927) |
Male (N=1642) |
Female (N=3285) |
P-Value |
|---|---|---|---|---|
| Age, Mean (SD), years | 48.2 (12.9) | 51.5 (12.3) | 46.6 (12.8) | < 0.001 |
| Pregnant, No. (%) | -- | 75 (2.3) | NE | |
| Body mass index, Mean (SD), kg/m2 | 27.3 (5.9) | 26.2 (4.9) | 27.8 (6.2) | < 0.001 |
| Education, No. (%) | < 0.001 | |||
| Never attended school | 1338 (27.2) | 287 (17.5) | 1051 (32.1) | |
| Primary school | 952 (19.4) | 287 (17.5) | 665 (20.3) | |
| Secondary school | 1198 (24.4) | 395 (24.1) | 803 (24.5) | |
| High school | 193 (3.9) | 88 (5.4) | 105 (3.2) | |
| College/University | 1030 (21.0) | 478 (29.2) | 552 (16.9) | |
| Professional Degree | 146 (3.0) | 73 (4.5) | 73 (2.2) | |
| Other* | 56 (1.1) | 30 (1.8) | 26 (0.8) | |
| History of hypertension, No. (%) | 2767 (56.2) | 895 (54.9) | 1872 (57.7) | 0.07 |
| History of diabetes, No. (%) | 292 (5.9) | 96 (5.9) | 196 (6.0) | 0.51 |
| History of heart failure, No. (%) | 18 (0.4) | 3 (0.2) | 15 (0.5) | 0.19 |
| History of chronic kidney disease, No. (%) | 14 (0.3) | 6 (0.4) | 8(0.2) | 0.64 |
| History of stroke, No. (%) | 56 (1.1) | 31 (1.9) | 25 (0.8) | 0.003 |
| History of heart attack, No. (%) | 19 (0.4) | 8 (0.5) | 11 (0.3) | 0.49 |
| Current smoker, No. (%) | 51 (1.0) | 39 (2.4) | 12 (0.4) | < 0.001 |
| Former smoker, No. (%) | 63 (1.3) | 54 (3.3) | 9 (0.3) | < 0.001 |
| Current alcohol user, No. (%) | 216 (4.4) | 154 (9.4) | 62 (1.9) | < 0.001 |
| Former alcohol user, No. (%) | 112 (2.3) | 72 (4.4) | 40 (1.2) | < 0.001 |
| First systolic blood pressure, Mean (SD), mm Hg | 156.8 (21.1) | 157.8 (20.7) | 156.4 (21.3) | 0.07 |
| Second systolic blood pressure, Mean (SD), mm Hg | 151.5 (20.8) | 152.9 (20.0) | 150.8 (21.0) | 0.001 |
| First diastolic blood pressure, Mean (SD), mm Hg | 96.7 (14.1) | 96.4 (14.1) | 96.8 (14.2) | 0.20 |
| Second diastolic blood pressure, Mean (SD), mm Hg | 94.7 (14.0) | 94.4 (13.8) | 94.9 (14.0) | 0.11 |
| Heart rate, Mean (SD), bpm | 84.0 (17.8) | 82.4 (14.1) | 84.8 (19.3) | < 0.001 |
Including Arabic school, Islamic school, Bible school, or Technical/Vocational school. NE=non-estimable.
Table 2 outlines blood pressure medication type and class at the time of registration, during the baseline visit, and at the end of the baseline visit. More than half (58.3%) of patients were on treatment at the time of registration with single dose, or free pill, medications (57.3%) being the most used drug type among treated patients, compared with two-drug (35.7%) and three-drug (7.0%) fixed dose combinations. Calcium channel blockers (82.7%) were the most used drug class at the time of registration, followed by diuretics (25.3%) and angiotensin converting enzyme inhibitors (19.4%). During the baseline visit, 2,876 (58.4%) patients received a renewed or newly prescribed medication, which was most commonly a calcium channel blocker (83.8%). By the end of the baseline visit, 4,395 (89.2%) patients were on treatment, and the median (interquartile range) number of blood pressure lowering medications prescribed per patient was 1 (1–2).
Table 2.
Number, type, and class of blood pressure lowering medication at the time of registration, during the baseline visit, and at the end of the baseline visit.
| Blood Pressure Lowering Medications at Baseline | At the Time of Registration (N=4927) |
Prescribed during Baseline Visit (N=4927) |
Medications at End of Baseline Visit (N=4927) |
|---|---|---|---|
| Number of medications per person, Median (IQR) | 1 (0-2) | 1 (0-1) | 1 (1-2) |
| Any medication, No. (%) | 2871 (58.3) | 2876 (58.4) | 4395 (89.2) |
| Type of blood pressure lower medication*† | |||
| Single dose (free pill) medication, No. (%) | 1644 (57.3) | 1921 (66.8) | 2503 (57.0) |
| Fixed dose combination with two medication, No. (%) | 1025 (35.7) | 800 (27.8) | 1565 (35.6) |
| Fixed dose combination with three medication, No. (%) | 202 (7.0) | 155 (5.4) | 327 (7.4) |
| Class of blood pressure lowering medication† | |||
| Angiotensin converting enzyme inhibitor, No. (%) | 558 (19.4) | 296 (10.3) | 769 (17.5) |
| Angiotensin receptor blocker, No. (%) | 367 (12.8) | 602 (20.9) | 803 (18.3) |
| Beta blocker, No. (%) | 18 (0.6) | 8 (0.3) | 24 (0.5) |
| Calcium channel blocker, No. (%) | 2374 (82.7) | 2410 (83.8) | 3881 (88.3) |
| Central acting agent, No. (%) | 346 (12.1) | 169 (5.9) | 454 (10.3) |
| Diuretic, ‡ No. (%) | 727 (25.3) | 275 (9.6) | 918 (20.9) |
| Vasodilator, No. (%) | 21 (0.7) | 3 (0.1) | 22 (0.5) |
| Undefined, § No. (%) | 8 (0.3) | 4 (0.1) | 10 (0.2) |
Type of medication is based on most complex type of medication taken. If the patient is on both a fixed dose medication with two agents, and a single dose medication, then they are reported here in the fixed dose with two medications row.
Some patients are prescribed multiple drugs or fixed dose medications, so the column percentages may add to more than 100%.
Including furosemide, spironolactone, thiazide, or other diuretic.
Drug name or class were unspecified.
Figure 2 demonstrates the treatment and control rates with corresponding 95% CI by sex from January 2020 to November 2020 with proportions reported in Supplemental Table 2. Overall, treatment rates at the baseline visit modestly increased over the baseline period, reaching 94% (95% CI, 91%, 98%) in males and 93% (95% CI: 90%, 95%) in females (p = 0.40 for between sex group differences; ptrend <0.001 for both sex groups). Over the same time, control rates at the baseline visit declined modestly, reaching 8% (95% CI: 4%, 11%) in males and 9% (95% CI: 6%, 13%) in females (p = 0.46 for between sex group differences; ptrend <0.001 for both sex groups). Females had a higher overall control rate at the baseline visit compared with males (14% [95% CI: 13%, 15%] versus 11% [95% CI: 10%, 13%]).
Figure 2.
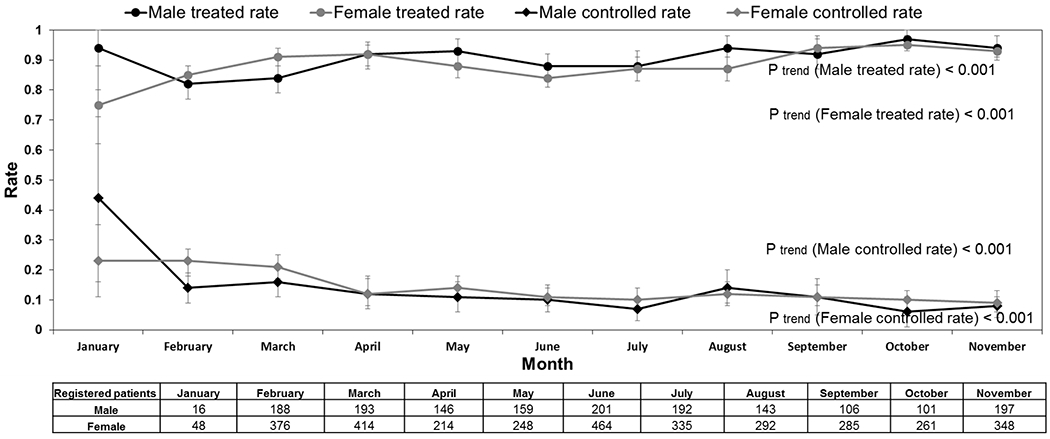
Treatment and control rate (95% CI) at patients’ baseline visit by calendar month.
Sex-stratified treatment and control rates at the baseline visit by area council are shown in Supplemental Table 3. Treatment and control rates by area council were more variable among females than among males. Females in Kwali had the highest treatment rate (95%, 95% CI: 93%, 97%), and females in Gwagwalada had the lowest treatment rate (84%, 95% CI: 81%, 87%). On the other hand, females in Abaji had the highest control rate (30%, 95% CI: 26%, 34%), and males in Bwari had the lowest control rate (4%, 95% CI: 1%, 6%).
The cascade of hypertension care is reported in Figure 3. All patients with hypertension, whether they had been previously diagnosed or undiagnosed, are represented as 100%. From this total, 58.3% had been treated prior to the start of the baseline visit, and 13.1% had controlled hypertension at their baseline visit. Among those who were treated prior to the start of the baseline visit, the control rate was 19.2%. Monthly treatment and control rates varied substantially by primary health care center, which are shown in Supplemental Figures 3 and 4, respectively.
Figure 3.
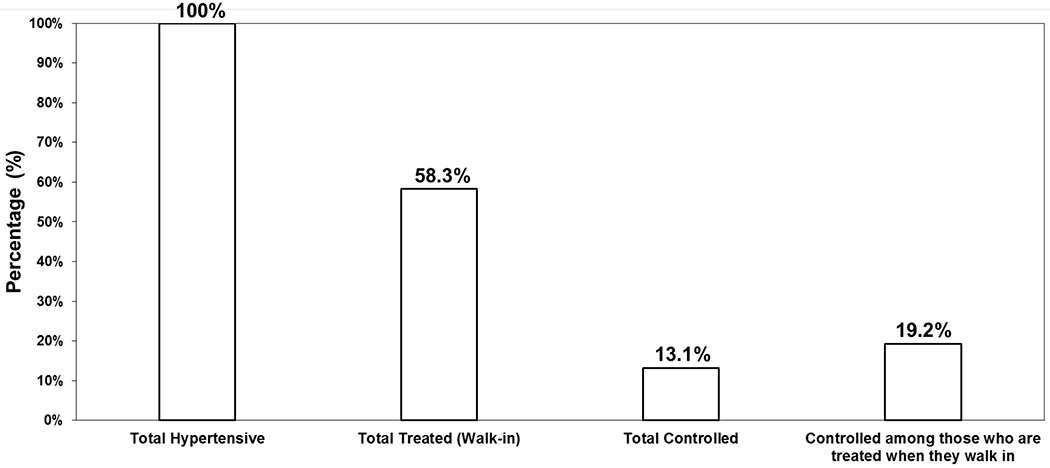
Hypertension cascade of care for baseline visits. The walk-in treatment rate can be considered the rate at the start of a patient’s baseline visit.
Supplemental Table 4 demonstrates the logistic regression results. After multivariable adjustment, older patients were more likely to have their hypertension treated (adjusted Odds Ratio, OR [95% CI] 1.02 [1.01, 1.03] per year), as were individuals with some education compared with never having attended school. Hypertension control was more common among individuals who were older (adjusted OR [95% CI]: 1.014 [1.01, 1.02]), were female (adjusted OR [95% CI]: 1.30 [1.05, 1.62]), used fixed dose combination therapy (adjusted OR [95% CI]: 1.83 [1.49, 2.26]), and had high school education and above. Patients in Abuja Municipal Area Council (adjusted OR [95% CI]: 0.41 [0.18, 0.92]), Bwari (adjusted OR [95% CI]: 0.24 [0.09, 0.64]), and Kwali (adjusted OR [95% CI]: 0.13 [0.05, 0.38]) had lower odds of hypertension control compared with Abaji.
Supplemental Figures 2a and 2b show the mean retention rates at 31 and 37 days, respectively, by primary health care center. The mean 31-day retention rate was 25% (95% CI: 20%, 31%), and the mean 37-day retention rate was 39% (95% CI: 32%, 45%) with wide variability among sites.
DISCUSSSION
Summary of Results
This report represents the largest facility-based study of hypertension care in Nigeria and in sub-Saharan Africa, demonstrating the cascade of hypertension care from 60 public, primary health care centers in the Federal Capital Territory. Patients in this registry had relatively low levels of education and low self-reported rates of smoking and co-morbid diseases. At the time of patient registration, rates of hypertension treatment and control were 58.3% and 13.1%, respectively. The hypertension treatment rate increased to 89.2% at the end of the study baseline visit, which can be likely attributed to the influence of registration, health worker training, and study participation. There was wide variability across primary health care centers in terms of number of patients recruited and hypertension treatment and control rates with higher rates among patients who were older, female, and with higher levels of education. Hypertension control was more common among individuals who used fixed-dose combination therapy but was less common in Abuja Municipal Area Council, Bwari, and Kwali compared with Abaji.
Baseline treatment rates at the time of registration increased over the study period, which may have resulted from a combination of sites’ study participation, including health worker training, temporal trends, and the Hawthorne effect. Monotherapy with calcium channel blockers or angiotensin receptor blockers were the most frequently newly prescribed blood pressure lowering medications in accordance with the 2019 national hypertension protocol.(10) Retention rates were 25% and 39% at 31 days and 37 days, respectively.
Results in Context
The baseline hypertension treatment rate (58.3%) in the current study was higher than previous community-based reports in Nigeria and other low- and middle-income countries, including in countries in Africa.(1,2,14) Differences in treatment can be likely attributed to differences in sampling between facility- and community-based studies and corresponding health-seeking behavior, as well as availability of hypertension services at the primary health care level. In addition, these may also be partly attributed to the Nigeria Hypertension Control Initiative, which was announced by the Federal Ministry of Health, WHO Nigeria, and Resolve to Save Lives in August 2019(15) with publication of a national hypertension treatment protocol in June 2020.(10) Nevertheless, the reported hypertension control rate (13.1%) is comparable to and complements the latest national, community-based estimate in Nigeria (12%), albeit with variation among area councils.(2) Follow-up hypertension control rates may be higher than baseline given the relatively high rate of blood pressure lowering treatment prescribed during the registration visit and time needed for these medications to take full effect, even with variable medication adherence rates. The Federal Ministry of Health and WHO Nigeria plan to collect demographic health surveillance data for non-communicable diseases in the second half of 2021 using the WHO STEPwise approach to Surveillance for non-communicable diseases (STEPS), which will further complement these results.
The higher recruitment and hypertension control rates of female participants in hypertension studies in Africa has been shown in large population hypertension registries in Africa.(16, 17) Potential reasons for these differences between sexes include earlier detection of hypertension in females at both antenatal and postnatal cares, and higher health seeking behaviors in African females compared to males. Similar to the current study results, previous research has demonstrated that individuals who are older, female, and with higher education were more likely to have hypertension treated and controlled in other low- and middle-income countries.(1,2) Fixed-dose combination therapy has been also demonstrated to increase hypertension control.(18)
Both the current study and aforementioned reports use point prevalence estimates, which may overestimate the true hypertension control rate. The WHO HEARTS technical package recommends using a 6-month hypertension control rate, which is generally considered to be a more rigorous and reliable method and will be incorporated in future analyses. However, while this method may more accurately estimate sustained hypertension control, patients need to be retained in care to calculate these estimates. In the current study, less than 40% of patients were retained in care at 37 days. Thus, defining hypertension control over 6 months may similarly overestimate the true rate of hypertension control in a health facility’s catchment area because of a healthy user bias.(19) Nevertheless, among 18 countries that have implemented the WHO HEARTS technical package, 6-month hypertension control rates ranged from 18% (Dominican Republic) to 79% (Ecuador).(5) Ethiopia was the only African country that has reported results in this program and showed a higher hypertension control rate (42%). Nigeria also participates in this program through Kano and Ogun states but has not reported results to date.
In addition to multi-level implementation strategies to improve the cascade of care,(5) strategies will need to be contextualized and implemented to improve coverage and retention across sociodemographic groups that were less likely to be represented in the current study, including patients who are younger, male, and with less education. Lower baseline treatment rates at the time of registration among some of these groups suggest that availability of services at the primary health care level may help to address these coverage gaps.
Specific treatment strategies may also be effective at improving treatment coverage. Further, the Nigeria national hypertension treatment protocol encourages the early use of 2-drug and 3-drug fixed-dose combination therapy based on high-quality evidence demonstrating greater effectiveness and efficiency with similar tolerability compared with monotherapy.(18,20) However, despite fixed-dose combination blood pressure lowering therapy being listed on the WHO Model List of Essential Medicines,(21) fixed-dose combination use in the current study was used in the minority of patients at baseline (38.4%) and was infrequently available (7%) among primary health care centers in the Federal Capital Territory prior to study initiation.(13) To address this gap, the study team embedded a cluster randomized trial within the Hypertension Treatment in Nigeria Program in January 2021 to evaluate the effect of a strategy that uses initial fixed-dose combination therapy compared with monotherapy (NCT04158154).
Strengths and Limitations
This study has several strengths, including using a prospective study design, recruitment of a large sample of patients from 60 public, primary health care centers, training and retraining of PHC staff, and rigorous data monitoring and analysis. The study also safely recruited patients and collected high-quality data from settings that had not previously conducted research and during the COVID-19 pandemic, demonstrating the feasibility of research in challenging conditions. On the other hand, this study also had limitations. First, the study setting was in 1 state in Nigeria; thus, these results may not necessarily be generalizable to other states in Nigeria. However, the study team collaborates with researchers and stakeholders in Kano and Ogun states to harmonize study procedures, including the same national treatment protocol,(10) which will allow for comparisons among different regions in Nigeria. Second, while the trained study staff were instructed to measure blood pressure on every patient who came to the primary health care center, it is possible that some patients’ blood pressures were not measured. Nevertheless, the study team performed regular site-level monitoring and supportive supervision visits to directly observe study procedures, including registration and blood pressure measurement, with real-time feedback to maximize adherence to study procedures. Third, treatment and control rates only represent data from patients’ baseline visits and may differ over time. Longitudinal analyses will be an area of future study within this program. Fourth, despite efforts to optimize data quality, including bi-weekly data status and quality reporting, there were some missing or low-quality data that needed to be excluded, even after source document review. However, the proportion of patients excluded was small (3.4%) and thus not likely to influence the validity of this report. Fifth, we did not collect self-reported measures of medication adherence, which have limitations related to recall and social desirability bias. Longitudinal measures of blood pressure, and subsequent hypertension control rates, provides an objective and feasible method for monitoring adherence compared with other approaches, such as pill counts and pharmacy data.
CONCLUSION
The current report describes the largest facility-based study of the hypertension cascade of care in Nigeria and in Africa. This report serves as the baseline for a prospective, longitudinal type 2 hybrid implementation study that tests the effectiveness and implementation of a multi-level, evidence-based implementation package using an interrupted time series design. Contextualization, implementation, sustainment, and spread of evidence-based strategies for better hypertension treatment and control at the primary health care level are needed to reduce the burden of cardiovascular diseases in Nigeria.
Supplementary Material
Acknowledgements
Hypertension Treatment in Nigeria Investigators and Staff: Regina Asuku, Elizabeth Ngadda, Joel Abu, Alice Osuji, Blessing Akor, Charity Akor, Christine Archibong, Abubakar Haruna, Confidence Joseph-Alo, Emmanuel Odo, Douglas Okoye, Grace Afolabi, Emmanuel Okpetu, Nana Ripiye, Dorothy Ihegazie, Christian Ukeh, Vivian Chukwuma, Nicholas Baamlong, Sani Mohammed, Deborah Joshua, Saleh Ashafa, Hope Omeiza, Mercy Ikechukwu-Orji.
Primary health care center investigators: All health care workers including facility managers of all the 60 primary health care centres.
Data and Safety Monitoring Board: Dr. Brian Rayner, University of Cape Town; Dr. Adeloye Davies, University of Edinburgh; Dr. Justine Davies, University of Birmingham; Dr. Amam Mbakwem, University of Lagos; Dr. Patricia Ojiah, University of Abuja; Dr. James Sheppard, University of Oxford; Dr. Amanda Thrift, Monash Health
Additional stakeholders: Non-Communicable Disease Unit of Federal Ministry of Health of Nigeria, World Health Organization, Nigeria Office, Federal Capital Territory Public Health Department, Federal Capital Territory Primary Health Care Board, Resolve To Save Lives, Directors of Primary Health Care of the 6 Local Government Area Councils in the Federal Capital Territory.
Disclosures:
In the last 3 years, MDH has received support from the World Heart Federation through unrestricted education grants from Boehringer Ingelheim, Novartis, and Bupa and from the American Heart Association, Verily, and AstraZeneca for work unrelated to this research. MDH has also received salary support from the American Medical Association for his role as an associate editor for JAMA Cardiology. MDH has planned patents for combination therapy for the treatment of heart failure. The George Institute for Global Health has a patent, license, and has received investment funding with intent to commercialize fixed-dose combination therapy through its social enterprise business, George Medicines. The other authors do not report any disclosures.
Funding:
This study was sponsored by the National Heart, Lung, and Blood Institute (R01HL144708) with additional support from the Northwestern University Clinical and Translational Science Institute (UL1TR00422). The funders had no role in the design, conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Abbreviations
- CI
confidence interval
- DBP
diastolic blood pressure
- HEARTS
Healthy-lifestyle counselling; Evidence-based treatment protocols; Access to essential medicines and technology; Risk-based CVD management; Team-based care; Systems for monitoring
- kg
kilogram
- m
meter
- REDCap
Research Electronic Data Capture
- SBP
systolic blood pressure
- SD
standard deviation
- STEPS
STEPwise approach to Surveillance for non-communicable diseases
- WHO
World Health Organization
Footnotes
Trial registration: NCT04158154
Data Sharing
In accordance with National Institutes of Health policies, data, data dictionaries, statistical code, protocols, and informed consent will be shared 12 months after completion of the Hypertension Treatment in Nigeria program (expected December 2024) through the National Heart, Lung, and Blood Institute Biological Specimen and Data Repository.
REFERENCES
- 1.Geldsetzer P, Manne-Goehler J, Marcus M-E, et al. The state of hypertension care in 44 low-income and middle-income countries: a cross-sectional study of nationally representative individual-level data from 1·1 million adults. Lancet 2019;394:652–662. [DOI] [PubMed] [Google Scholar]
- 2.Odili AN, Chori BS, Danladi B, et al. Prevalence, Awareness, Treatment and Control of Hypertension in Nigeria: Data from a Nationwide Survey 2017. Global Hear 2020;15:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iwelunmor J, Plange-Rhule J, Airhihenbuwa CO, Ezepue C, Ogedegbe O. A Narrative Synthesis of the Health Systems Factors Influencing Optimal Hypertension Control in Sub-Saharan Africa Thielman NM, editor. Plos One 2015;10:e0130193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khatib R, Schwalm J-D, Yusuf S, et al. Patient and Healthcare Provider Barriers to Hypertension Awareness, Treatment and Follow Up: A Systematic Review and Meta-Analysis of Qualitative and Quantitative Studies Barengo NC, editor. Plos One 2014;9:e84238–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Improving hypertension control in 3 million people. Geneva, Switzerland; 2021. [Google Scholar]
- 6.Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Db Syst Rev 2010:CD005182. [DOI] [PubMed] [Google Scholar]
- 7.Mills KT, Obst KM, Shen W, et al. Comparative Effectiveness of Implementation Strategies for Blood Pressure Control in Hypertensive Patients. Ann Intern Med 2018;168:110–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jaffe MG, Young JD. The Kaiser Permanente Northern California Story: Improving Hypertension Control From 44% to 90% in 13 Years (2000 to 2013). J Clin Hypertens 2016;18:260–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. WHO HEARTS technical package for cardiovascular disease management in primary health care. WHO: Geneva, Switzerland; 2016. Available at: https://apps.who.int/iris/bitstream/handle/10665/252661/9789241511377-eng.pdf?sequence=1. [Google Scholar]
- 10.Federal Ministry of Health. Nigeria hypertension treatment protocol for the primary care level. Available at: https://linkscommunity.org/assets/PDFs/nigeria-hypertension-protocol-04.pdf.
- 11.Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation Hybrid Designs. Med Care 2012;50:217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Orji IA, Baldridge AS, Omitiran K, et al. Capacity and site readiness for hypertension control program implementation in the Federal Capital Territory of Nigeria: a cross-sectional study. Bmc Health Serv Res 2021;21:322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harris PA, Taylor R, Minor BL, et al. The REDCap Consortium: Building an International Community of Software Platform Partners. J Biomed Inform 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ogah OS. Blood pressure, prevalence of hypertension and hypertension related complications in Nigerian Africans: A review. World J Cardiol 2012;4:327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. Nigeria collaborates with WHO to curb hypertension, introduces control initiative. Available at: https://www.afro.who.int/news/nigeria-collaborates-who-curb-hypertension-introduces-control-initiative.
- 16.Ojji DB, Libhaber E, Atherton JJ, Abdullahi B, Nwankwo A, Sliwa K. Risk-Factor Profile and Comorbidities in 2398 Patients With Newly Diagnosed Hypertension From the Abuja Heart Study. Medicine 2015;94:e1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stewart S, Libhaber E, Carrington M, et al. The clinical consequences and challenges of hypertension in urban-dwelling black Africans: Insights from the Heart of Soweto Study. Int J Cardiol 2011;146:22–27. [DOI] [PubMed] [Google Scholar]
- 18.Salam A, Kanukula R, Atkins E, et al. Efficacy and safety of dual combination therapy of blood pressure-lowering drugs as initial treatment for hypertension. J Hypertens 2019; 37:1768–1774. [DOI] [PubMed] [Google Scholar]
- 19.Shrank WH, Patrick AR, Brookhart MA. Healthy User and Related Biases in Observational Studies of Preventive Interventions: A Primer for Physicians. J Gen Intern Med 2011;26:546–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salam A, Atkins ER, Hsu B, Webster R, Patel A, Rodgers A. Efficacy and safety of triple versus dual combination blood pressure-lowering drug therapy. J Hypertens 2019:1. [DOI] [PubMed] [Google Scholar]
- 21.Salam A, Huffman MD, Kanukula R, et al. Two-drug fixed-dose combinations of blood pressure-lowering drugs as WHO essential medicines: An overview of efficacy, safety, and cost. J Clin Hypertens 2020;22:1769–1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


