Abstract
Purpose
To assess the impact of Visual Field Loss (VFL) on Vision-Specific Quality of Life (VSQOL) by race, ethnicity and age
Design
Pooled analysis of cross-sectional data from three population-based, prospective cohort studies
Participants
The Multiethnic Ophthalmology Cohorts of California Study (MOCCaS) participants included 6,142 Latinos, 4,582 Chinese Americans, and 6,347 African Americans from Los Angeles County.
Methods
17,071 adults 40 years and older completed comprehensive interviews and ophthalmic examinations from 2000 to 2018. VFL was measured using the Humphrey SITA Standard 24–2 test as decibels (dB) of mean deviation (MD). Multivariable linear regression was used to evaluate the impact of VFL in the better-seeing eye on self-reported VSQOL scores, adjusting for sociodemographic and clinical covariables. Hierarchical modeling was performed to determine the best-fit model after considering main effects and interactions by race, ethnicity and age.
Main Outcome Measures
VSQOL scores were measured using the 25 Item National Eye Institute Visual Functioning Questionnaire (NEI-VFQ-25). Item response theory (IRT) was used to model vision-related task and well-being composite scores, while classical test theory (CTT) was used to calculate 11 vision subscales.
Results
The impact of VFL on VSQOL varied by race and ethnicity. 5-point reductions in task and well-being scores were reached after mild-to-moderate VFL for Latinos (6.7 dB and 7.5 dB), mild-to-moderate VFL for Chinese Americans (7.0 dB and 8.7 dB), and moderate-to-severe VFL for African Americans (10.1 dB and 12.9 dB), respectively. Differences met statistical significance when comparing Latinos and African Americans (P < 0.01). VFL had the largest effect on driving among all participants. Driving difficulties was the only VSQOL outcome modified by age; participants 65 years and older scored 0.487 lower points per MD of VFL (P < 0.01). Subscales most affected by VFL included role function, mental health, and dependency.
Conclusions
Race and ethnicity modified the impact of VFL on VSQOL, even after adjusting for sociodemographic covariates. In MOCCaS, Latinos and Chinese Americans reported a greater change in VSQOL than African Americans for the same level of VFL. Future work should assess whether findings were due to socioeconomic or cultural differences in perception of visual function.
Précis
Visual field loss affected person-reported vision-specific quality of life differently in different racial and ethnic groups. Driving was more affected among participants 65 years and older.
Introduction
The prevalence of chronic eye disease is expected to increase as the US population ages over the next 30 years. The financial burden of visual impairment (VI) and blindness is projected to double by 2050 as demographics in the US shift from younger to older ages.1 Vision specific quality of life (VSQOL) will also decrease as people are limited in their ability to complete daily tasks in their homes and as their emotional well-being diminishes due to restricted social interaction. In addition, the prevalence of eye disease varies by race and ethnicity, sex, and age.2,3 For example, Latinos and African Americans experience a higher burden of both diabetic retinopathy4 and open-angle glaucoma,5,6 while Chinese Americans have a greater prevalence of myopic degeneration.7 These health disparities may contribute to racial and ethnic differences in visual function, including visual acuity (VA), visual field loss (VFL) and VSQOL.
VSQOL is a patient-reported outcome measure of visual function that has been used to inform clinical decisions and facilitate communication with patients. VSQOL has also been used in clinical trials to test the efficacy of rehabilitation programs8 and to identify appropriate interventions for public use.9,10 It is essential to obtain contextual clinical data from diverse populations to assess the generalizability of findings.11 Ophthalmic research must also prioritize the vision-related concerns of multiethnic communities to improve eyecare services for the diverse US population.
We conducted the first population-based study of the relationship between VI and VSQOL in a multiethnic cohort of US adults. Several population-based studies have been conducted on VFL and VSQOL, however the number of participants from minority groups has been limited, cohorts were dedicated to a single racial or ethnic group, or data were based on definitions and clinical protocols from more than 20 years prior.12–15 The Multiethnic Ophthalmology Cohorts of California Study (MOCCaS) is a pooled cohort of adults age 40 years and older from three population-based studies of Latinos, Chinese Americans, and African Americans living in Los Angeles County. In this study, we take advantage of the large sample size in the MOCCaS to assess the interaction of race and ethnicity on the associations between VFL and self-reported VSQOL, emphasizing domains of ability to complete vision-related tasks and socioemotional well-being. We hypothesized that age is an effect modifier of this relationship given the greater incidence of eye disease and comorbidities among patients aged 65 years and older.
Methods
The MOCCaS is a pooled analysis of 17,071 subjects residing in Los Angeles County who were studied during three population-based, cross-sectional, prospective cohort studies: the Los Angeles Latino Eye Study (LALES),16 the Chinese American Eye Study (CHES),17 and the African American Eye Disease Study (AFEDS).18 In brief, LALES participants were studied from 2000 to 2003 and resided in the city of La Puente; CHES participants were studied from 2010 to 2013 and resided in Monterey Park; AFEDS participants were studied from 2014 to 2018 and resided in Inglewood. Participants were asked to report all racial and ethnic descriptors relevant to their identity, and this information was used for cohort recruitment. LALES and AFEDS participants were age 40 years and older, and CHES participants were age 50 years and older. Data were collected from standardized interviews and comprehensive clinical eye examinations. Participants who preferred languages other than English were interviewed and examined in Spanish during the LALES and Mandarin or Cantonese during the CHES. Demographics of MOCCaS participants were comparable to their respective racial or ethnic populations in Los Angeles County, California, and the United States. Approval was obtained by the University of Southern California Medical Center Institutional Review Board. All study procedures adhered to the Declaration of Helsinki.
Sociodemographic Assessment
Eligible residents were identified by door-to-door census. Participants were interviewed in their homes after providing informed consent to gather demographic factors, history of medical conditions, and access to ocular and medical care. A comorbidity score was calculated as a summation of thirteen self-reported medical conditions, including diabetes mellitus, arthritis, stroke or brain hemorrhage, hypertension, angina, heart attack, heart failure, asthma, skin cancer, other cancers, back problems, deafness or hearing problems, and other comorbidities. Participants who completed the in-home questionnaire were invited to attend the clinical eye examination.
Visual Function Assessment
VA measures high acuity, central vision. Binocular VA was measured with presenting correction at 4 meters using standard Early Treatment Diabetic Retinopathy protocols with a modified distance chart illuminator (Precision Vision).19 An automated refraction was performed as needed using the Humphrey Automatic Refractor (Carl Zeiss Meditec, Dublin, CA) followed by subjective refraction. Visual Impairment was defined as VA of 20/40 or worse based on the U.S. definition of VI. LogMAR score is a common transformation of VA that was used in regression models.
Visual field (VF) testing was conducted to assess participants’ ability to detect objects in both their central and peripheral vision. VF for each eye was assessed using the Swedish Interactive Threshold Algorithm (SITA) Standard C24–2 test (Carl Zeiss Humphrey Field Analyzer II 750 Dublin, CA). VF was measured as decibels (dB) of total mean deviation (MD) from the age-adjusted standard population. VF testing was repeated up to 2 times if the measurement was unreliable. Measurements with 15% or more false negatives or false positives were considered unreliable and were excluded from analyses; we have demonstrated that using 15% limits leads to minimal differences in associations between VSQOL and VFL in the AFEDS.15 Fixation losses were not used to determine reliability of VF measurements.20 Continuous VFL was stratified into the worse- and better-seeing eye (BSE); results are presented only for the BSE, which is strongly related to binocular VFL.21 We used the Hodapp-Parrish-Anderson method to classify the severity of VFL as mild [−2 dB to −6 dB), moderate [−6 dB to −12 dB), and severe [≤ −12 dB).22
Vision-Specific Quality of Life
VSQOL was measured using the National Eye Institute Visual Functioning Questionnaire-25 (NEI-VFQ-25) survey instrument,23 which was administered by a trained interviewer prior to the clinical examination. Classical test theory (CTT) is a traditional method for scoring the NEI-VFQ-25 that yields 11 subscales and an overall composite for VSQOL. The primary concern is that several assumptions of CTT are unmet including equal differences between response categories, less than 5% missing data, and a constant standard error across the distribution of respondents.24 Item response theory (IRT) has been favored in the recent ophthalmic literature24 as it relies on fewer statistical assumptions and is amenable to validation of latent domains of VSQOL. Therefore, we report IRT composite domains as the primary outcomes for the current analysis and additionally report CTT subscales as secondary outcomes to identify subdomains of VSQOL associated with VFL. IRT domains and CTT subscales were standardized from 0 to 100, with higher scores indicating greater VSQOL.
NEI-VFQ-25: Item Response Theory (Graded Response Model)
IRT models were used to classify participants with varying magnitude of VSQOL latent scores along a linear continuum of NEI-VFQ-25 item difficulty.25 The graded response model (GRM) is a 2-parameter IRT model for ordinal items on a Likert scale, which was used to produce two unidimensional composites for completing vision task and vision-related socioemotional well-being. The task composite domain was calculated from 12 items, and the well-being domain from 12 items (Table S1 available at http://www.aaojournal.org); the general health item was not included in either domain. IRT composite domains were calculated using the ltm package for R software.26
NEI-VFQ-25: Classical Test Theory
CTT subscales were scored as the mean of related NEI-VFQ-25 items.23 CTT subscales related to the IRT task domain included driving difficulties, vision-related role function, near vision, peripheral vision, distance vision, and color vision; subscales related to the well-being domain included vision-related mental health, dependency, social functioning, general vision, ocular pain.
Statistical Analysis
Data were restricted to participants with complete and reliable VFL measurements and VSQOL outcomes. Tests for equal means in a one-way layout and Pearson’s χ2 tests were conducted to compare continuous and categorical sociodemographic variables, respectively, across racial and ethnic cohorts.
Hierarchical, multivariable linear regression was performed to investigate the impact of VFL on VSQOL among all participants in the MOCCaS. The duplication method was used to assess for subgroup heterogeneity by race, ethnicity and age categories.27 Models for each VSQOL outcome were nested as (1) a main effects model on VFL adjusted for covariates, (2) an interaction model where associations with VFL varied by each racial and ethnic cohort, and (3) a subsequent interaction model where associations with VFL also varied by age categorized as 65 years or older. The Multivariate Wald test for multiply imputed data was used to compare nested hierarchical models and to determine the best fitting, most parsimonious model for each VSQOL outcome.27,28 For interaction models, beta coefficients between VSQOL on VFL were obtained for each racial and ethnic group or age strata by reassigning the baseline group. Models for each VSQOL outcome on VFL were ranked in descending order by the strength of association.
Potential covariates relating to perceived VSQOL and VFL included age (years), highest grade of education completed, number of comorbidities, sex (female), born in the US (yes), employment status (working), household annual income (≥ $20,000), health insurance (yes), depression measured by the 12-Item Short-Form Health Survey item “Have you felt downhearted or blue a good bit of the time or more during the past 4 weeks?”, and presenting binocular LogMAR VA. US birth was a proxy for acculturation available in all cohorts. Unbiased regression coefficients were obtained from missing covariate data using 10 data sets multiply imputed with chained equations (MICE) via the mice package for R.28
Statistical models were interpreted using procedures that we have previously reported.15 Predicted VSQOL outcomes regressed on VFL were illustrated using locally weighted scatterplot smoothing (LOWESS) with 95% confidence limits. Forest plots were used to compare VSQOL and VFL associations for both IRT composites and the top 4 CTT subscales. A 5-unit change in NEI-VFQ-25 was interpretated as a clinically meaningful because it has been associated with a 2-line deficit in VA29; beta coefficients were transformed by 5 points of VSQOL to obtain a meaningful difference in VFL. Sensitivity analyses were conducted in subgroups of MOCCaS participants to assess whether the relationships between VFL and VSQOL for IRT task and well-being outcomes were biased by age, sex, socioeconomic status (SES),30 immigration,31 depression,32 or VI. All analyses were performed using R statistical software, version 3.6.1.33 Statistical tests were performed with a 0.05 type 1 error rate. The Holm method was used to adjust for multiple comparisons.34 The study was reported according to STROBE guidelines.35
Results
Participants and Descriptive Data
The MOCCaS included 17,071 participants from the LALES, the CHES, and the AFEDS (Figure S1 available at http://www.aaojournal.org). 14,570 (85.3%) participants had complete outcome and exposure data and were included in the analytic cohort. 6.3% of participants were excluded due to missing VSQOL outcomes and were mostly missing from the LALES. 8.6% of participants had missing or unreliable VF measurements and were mostly missing from the AFEDS. Finally, the quarter of participants with missing data for the driving difficulties subscale were not excluded because the questionnaire was designed to skip these items when the person was a non-driver or had stopped driving for reasons other than vision loss.23
Most sociodemographic variables were significantly different across cohorts of the MOCCaS (p < 0.001). Exceptions included no differences in age, sex, or self-reported depression between Chinese Americans and African Americans. Participants were 59 years old on average; Latinos tended to be younger (55.0 years) compared to Chinese and African Americans (61.2 years). Most participants were female (61%), and Latinos were slightly more likely to be male. The mean highest grade of education completed was 11.5 years; African Americans completed more education (14.3 years) than Chinese Americans (12.2 years) or Latinos (8.2 years). African Americans had the greatest number of self-reported comorbidities (2.0) followed by Latinos (1.5) and Chinese Americans (1.2). The majority of African Americans were born in the US (91.0%) while only a quarter of Latinos (24.5%) and few Chinese Americans (1.3%). The cohort most likely to be employed was Chinese Americans (53.0%) followed by Latinos (48.7%), and African Americans (44.7%). The reverse pattern was observed for health insurance coverage; African Americans were most likely to be insured (89.7%), then Latinos (64.9%), and Chinese Americans (53.0%). Latinos reported being depressed (16.0%) more than twice as often as Chinese (6.6%) and African Americans (6.0%). Chinese Americans were most likely to have visual impairment (8.9%), followed by Latinos (6.2%), and African Americans (4.4%).
Among the MOCCaS analytic cohort (n = 14,570), 12,469 (85.6%) of participants had complete sociodemographic information. Income was the largest incomplete variable, with 1,868 (12.8%) missing. Less than 5% of participants were missing data for all other covariables, including 182 (1.2%) for education, 10 (0.1%) for sex, 118 (0.8%) for US born, 182 (1.2%) for employment, 306 (2.1%) for insurance, 12 (0.1%) for depression, and 2 (0.0%) for VA loss.
NEI-VFQ-25 Outcome Data
Many participants reported the maximum possible VSQOL response for NEI-VFQ-25 items, especially for completing vision-related tasks (Figure S2 available at http://www.aaojournal.org). This resulted in ceiling effects with skewed response distributions.24 The average IRT score for the task composite was 83.1 out of 100 points maximum (standard deviation [SD] = 16.7), and for the well-being composite was 71.8 points (SD = 16.6). Test information curves revealed the NEI-VFQ-25 instrument was most informative for VSQOL ranging between the mean and 3–4 standard deviations below. High measures of internal consistency were observed for the IRT graded response models for both the task and well-being composites. High inter-item correlations were observed for each composite score; Cronbach’s alpha was 0.888 for task (12 items) and 0.872 for well-being (12 items). Factor analysis suggested IRT task and well-being model latent traits were unidimensional, as evidenced by the Scree plots and Chi-Square tests for unidimensionality (P < 0.001); a single factor explained 68.3% of the observed variance for the task composite and 64.7% for the well-being composite.
Selecting Hierarchical Linear Regression Models
We observed significant inverse associations between VFL main effects and VSQOL outcomes for all three hierarchical models (Table S2 available at http://www.aaojournal.org). In model 2, there were significant interactions by racial and ethnic cohorts for VFL and all VSQOL outcomes. In Model 3, there was a significant interaction by age strata and VFL for the vision-specific driving difficulties outcome only. Furthermore, all Wald tests were significant after adjusting for multiple comparisons, indicating the three models were statistically different. For each outcome we selected the most parsimonious regression model with significant VFL terms; therefore, we used Model 3 for the association between VFL and driving difficulties and Model 2 for all remaining VSQOL outcomes.
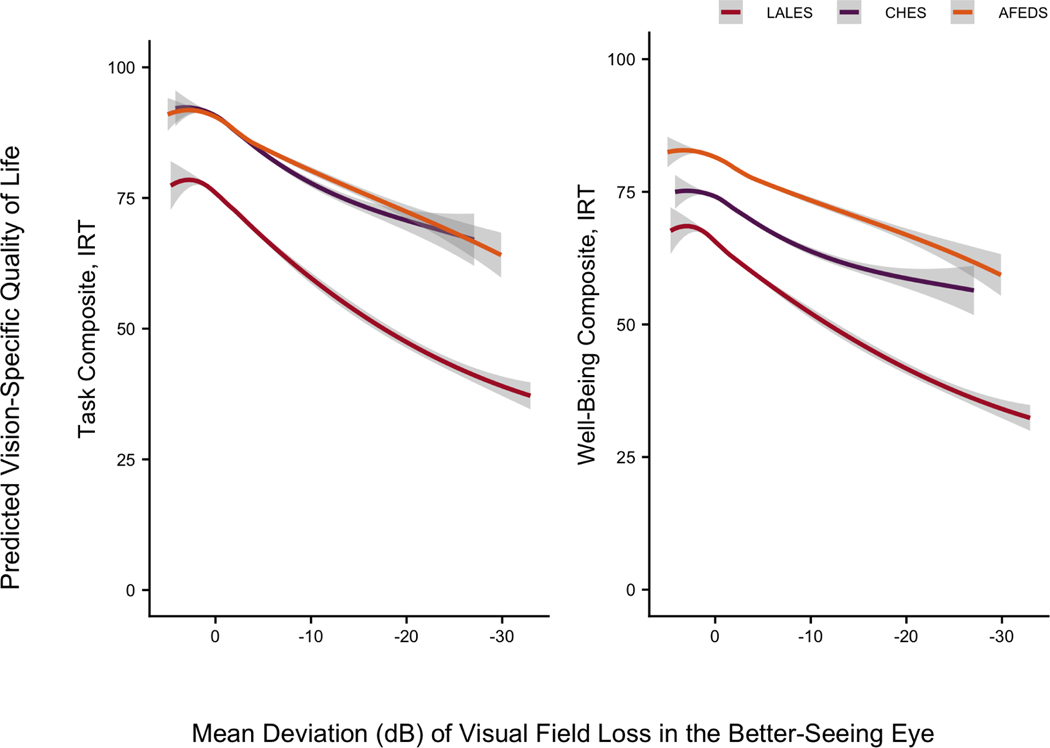
VSQOL Item Response Theory Composites and VFL Varied by Race and Ethnicity
Variations by race and ethnicity were observed in associations between IRT domains of VSQOL and VFL in the BSE (Table 2). LOWESS plots of predicted IRT task and well-being scores on VFL were used to illustrate associations by cohorts (Figure 1). The intercept for VSQOL outcomes were larger for task compared to wellbeing for all racial and ethnic cohorts; baseline differences in VSQOL were greatest for Chinese Americans (18.5 points) and smaller for African Americans (13.7) and Latinos (12.2 points). VFL had the greatest impact on IRT composite scores among Latinos and the least impact among African Americans; differences in associations between cohorts were statistically significant for both task (P = 0.004) and well-being (P = 0.002). Intermediate effects were seen among Chinese Americans, where associations of VFL and VSQOL were not statistically different from either Latinos or African Americans.
Table 2:
Linear Regression β Coefficients for the Association of VSQOL IRT Composite Scores and VFL in the MOCCaS (n = 14,570)*
| Vision-Specific Quality of Life Item Response Theory | ßMD | (95% CI) | MD (dB) of VFL for 5-point of VSQOL† | P-Valuei‡ | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Latinos | Chinese Americans | African Americans | ||||
|
| ||||||
| Task Composite, IRT§ | ||||||
| Latinos | 0.750 | (0.646, 0.854) | 6.7 | < 0.001 | ||
| Chinese Americans | 0.719 | (0.567, 0.872) | 7.0 | 1.000 | < 0.001 | |
| African Americans | 0.496 | (0.374, 0.617) | 10.1 | 0.004 | 0.172 | <0.001 |
| Well-Being Composite, IRT|| | ||||||
| Latinos | 0.666 | (0.560, 0.772) | 7.5 | < 0.001 | ||
| Chinese Americans | 0.575 | (0.419, 0.731) | 8.7 | 0.990 | < 0.001 | |
| African Americans | 0.387 | (0.263, 0.511) | 12.9 | 0.002 | 0.420 | < 0.001 |
VSQOL = Vision-Specific Quality of Life; VFL = Visual Field Loss in the better seeing eye;
MOCCaS = Multiethnic Ophthalmology Cohorts of California Study; 95% CI = 95% confidence interval; NEI-VFQ-25 = National Eye Institute Visual Function Questionnaire 25-Item; MD = Mean Deviation; IRT = Item Response Theory
VFL is presented as mean deviation score in decibels; VSQOL is assessed by IRT analysis of the NEI-VFQ-25. Linear regression models of VSQOL on VFL were adjusted for race/ethnicity, age, number of comorbidities, sex (female), born in USA (yes), education highest grade obtained), working status (unemployed), income (≤ $20,000), has health insurance (yes), presenting binocular visual acuity (LogMAR score), depression (a good bit of the time or more in the last 4 weeks), and an interaction between VFL and race/ethnicity.
Regression coefficients were transformed per 5-point difference in HRQOL score, a clinically significant difference in VSQOL score.
P-values along the diagonal represent main effects for associations between VSQOL and VFL within each racial/ethnic cohort; P-values off the diagonal indicate interactions across cohorts. The Holm method was used to adjust for multiple comparisons for 15 VSQOL outcomes.
IRT Task Composite was calculated from a graded response theory model of 12 items from near vision, distance vision, driving, color vision, peripheral vision, and role difficulties subscales.
IRT Well-Being Composite was calculated from a graded response model of 12 items from general vision, dependency on others, mental health, ocular pain, and social functioning subscales.
Figure 1:
LOWESS plot of predicted NEI-VFQ-25 IRT composite scores from linear regression on VFL (MD in dB) in the BSE by cohort LOWESS = Locally Weighted Scatterplot Smoothing; NEI-VFQ-25 = National Eye Institute Visual Function Questionnaire 25-ltem; IRT = Item Response Theory; VFL = Visual Field Loss; MD = Mean Deviation; dB = Decibels; BSE = Better-Seeing Eye The LOWESS smoothing parameter is 0.6. Gray bars represent 95% confidence limits of the predicted NEI-VFQ-25 IRT composite scores. Linear regression models were adjusted for race and ethnicity, age, number of comorbidities, sex (female), born in USA (yes), education highest grade obtained), working status (unemployed), income (≤ $20,000), has health insurance (yes), presenting binocular visual acuity (LogMAR score), depression (a good bit of the time or more in the last 4 weeks), and an interaction between VFL and race, ethnicity.
For the IRT task model, a 1 dB lower value of MD for VFL was associated with 0.750 (95% CI: 0.646, 0.854) lower VSQOL score for Latinos, 0.719 (95% CI: 0.567, 0.872) for Chinese Americans, and 0.496 (95% CI: 0.374, 0.617) for African Americans. A minimum difference in VFL of 6.7 dB for Latinos (mild-to-moderate), 7.0 dB for Chinese Americans (mild-to-moderate), and 10.1 dB for African Americans (moderate-to-severe) was necessary to observe a clinically meaningful, 5-point lower score in task composite VSQOL.
For the IRT well-being model, a 1 dB lower value of MD for VFL was associated with 0.666 (95% CI: 0.560, 0.772) lower VSQOL score for Latinos, 0.575 (95% CI: 0.419, 0.731) for Chinese Americans, and 0.387 (95% CI: 0.263, 0.511) for African Americans. A minimum difference in VFL of 7.5 dB for Latinos (moderate), 8.7 dB for Chinese Americans (moderate), and 12.9 dB for African Americans (moderate-to-severe) was necessary to observe a clinically meaningful, 5-point lower score in well-being composite VSQOL.
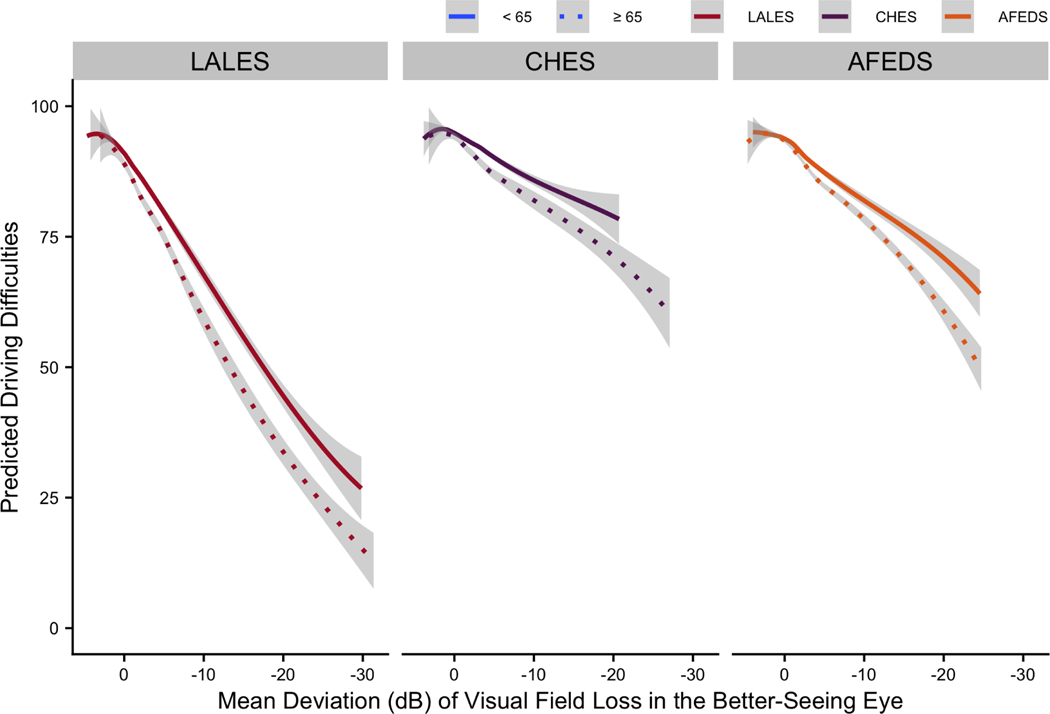
VSQOL Driving Difficulties and VFL Varied by Age Strata and Race and Ethnicity
Variation by age as well as race and ethnicity was observed in the association between the CTT driving difficulties subscale and VFL in the BSE (Table 3). Among participants aged 65 years and older, there was a 0.487 point (95% CI: 0.278, 0.695) greater loss in VSQOL scores for driving difficulties with every 1 dB of MD in VFL compared to younger participants (P for interaction < 0.001). Predicted VSQOL stratified by race and ethnicity and age categories were used to visualize how older participants from all three cohorts were more sensitive to VFL (Figure 2). Among both age groups, driving difficulties was the CTT subscale most impacted by VFL for Latinos and African Americans, as well as for Chinese Americans greater than 65 years old. However, driving difficulties was the third most affected CTT subscale for younger Chinese Americans, following vision-related role function and mental health (Figure 3). Across racial and ethnic cohorts, driving difficulties VSQOL was more sensitive to VFL in Latinos compared to African Americans or Chinese Americans; there was no significant difference in this association for the two latter groups.
Table 3:
Linear Regression β Coefficients for the Association of VSQOL CTT Driving Difficulties and VFL in MOCCaS, Age Stratified by 65 years (n = 11,473)*
| Vision-Specific Quality of Life Classical Test Theory | ßMD | (95% CI) | MD (dB) of VFL for 5-point of VSQOL‡ | P-Value§ | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Latinos | Chinese Americans | African Americans | Age-MD Interaction | ||||
|
| |||||||
| Driving Difficulties, Age ≥ 65 Years† | −0.487 | (−0.695, −0.278) | < 0.001 | ||||
| Latinos | 1.989 | (1.779, 2.198) | 2.5 | < 0.001 | |||
| Chinese Americans | 1.141 | (0.878, 1.404) | 4.4 | < 0.001 | < 0.001 | ||
| African Americans | 1.117 | (0.932, 1.303) | 4.5 | < 0.001 | 0.865 | < 0.001 | |
| Driving Difficulties, Age < 65 Years† | 0.487 | (0.278, 0.695) | < 0.001 | ||||
| Latinos | 1.502 | (1.306, 1.698) | 3.3 | < 0.001 | |||
| Chinese Americans | 0.654 | (0.422, 0.887) | 7.6 | < 0.001 | < 0.001 | ||
| African Americans | 0.631 | (0.435, 0.827) | 7.9 | < 0.001 | 0.865 | < 0.001 | |
| Vision-Related Role Function | |||||||
| Latinos | 1.071 | (0.932, 1.210) | 4.7 | < 0.001 | |||
| Chinese Americans | 1.039 | (0.835, 1.243) | 4.8 | 1.000 | < 0.001 | ||
| African Americans | 0.191 | (0.029, 0.353) | < 0.001 | < 0.001 | 0.084 | ||
| Vision-Related Mental Health | |||||||
| Latinos | 1.142 | (1.000, 1.283) | 4.4 | < 0.001 | |||
| Chinese Americans | 0.881 | (0.673, 1.088) | 5.7 | 0.257 | < 0.001 | ||
| African Americans | 0.263 | (0.098, 0.428) | 19.0 | < 0.001 | < 0.001 | 0.012 | |
| Vision-Related Dependency | |||||||
| Latinos | 1.382 | (1.263, 1.502) | 3.6 | < 0.001 | |||
| Chinese Americans | 0.516 | (0.341, 0.691) | 9.7 | < 0.001 | < 0.001 | ||
| African Americans | 0.112 | (−0.027, 0.251) | < 0.001 | 0.004 | 0.227 | ||
VSQOL = Vision-Specific Quality of Life; VFL = Visual Field Loss in the better seeing eye;
MOCCaS = Multiethnic Ophthalmology Cohorts of California Study; 95% CI = 95% confidence interval; NEI-VFQ-25 = National Eye Institute Visual Function Questionnaire 25-Item; MD = Mean Deviation; IRT = Item Response Theory; CTT = Classical Test Theory
VFL is presented as mean deviation score in decibels; VSQOL is assessed by the NEI-VFQ-25. Data are presented as coefficient (95% CI). The CTT Driving Difficulties subscale of the NEI-VFQ-25 scores are adjusted for age, gender, education, employment status, income, acculturation, co-morbidities, health insurance, vision insurance, and visual acuity impairment. There was an interaction term for race/ethnicity and VFL, and for age and VFL.
Scores could be generated for only 11,473 of participants who reported that they were currently driving or had driven in the past.
Regression coefficients were transformed per 5-point difference in HRQOL score, a clinically significant difference in VSQOL score.
The P-value for age ≥ 65 years indicates the interaction between age strata and VFL. P-values along the diagonal represent main effects for associations between VSQOL and VFL within each racial/ethnic cohort; P-values off the diagonal indicate interactions across cohorts. The Holm method was used to adjust for multiple comparisons for 15 VSQOL outcomes.
Figure 2:
LOWESS plot of predicted NEI-VFQ-25 CTT driving difficulties scores from linear regression on VFL (MD in dB) in the BSE by cohort LOWESS = Locally Weighted Scatterplot Smoothing; NEI-VFQ-25 = National Eye Institute Visual Function Questionnaire 25-ltem; CTT = Classical Test Theory; VFL = Visual Field Loss; MD = Mean Deviation; dB = Decibels; BSE = Better-Seeing Eye The LOWESS smoothing parameter is 0.6. Gray bars represent 95% confidence limits of the predicted NEI-VFQ-25 IRT composite scores. Linear regression models were adjusted for race and ethnicity, age, number of comorbidities, sex (female), born in USA (yes), education highest grade obtained), working status (unemployed), income (≤ $20,000), has health insurance (yes), presenting binocular visual acuity (LogMAR score), depression (a good bit of the time or more in the last 4 weeks), and an interaction between VFL and race, ethnicity. LOWESS curves are shown stratified by age < 65 and ≥ 65 to illustrate effect modification of VSQOL on VFL by age.
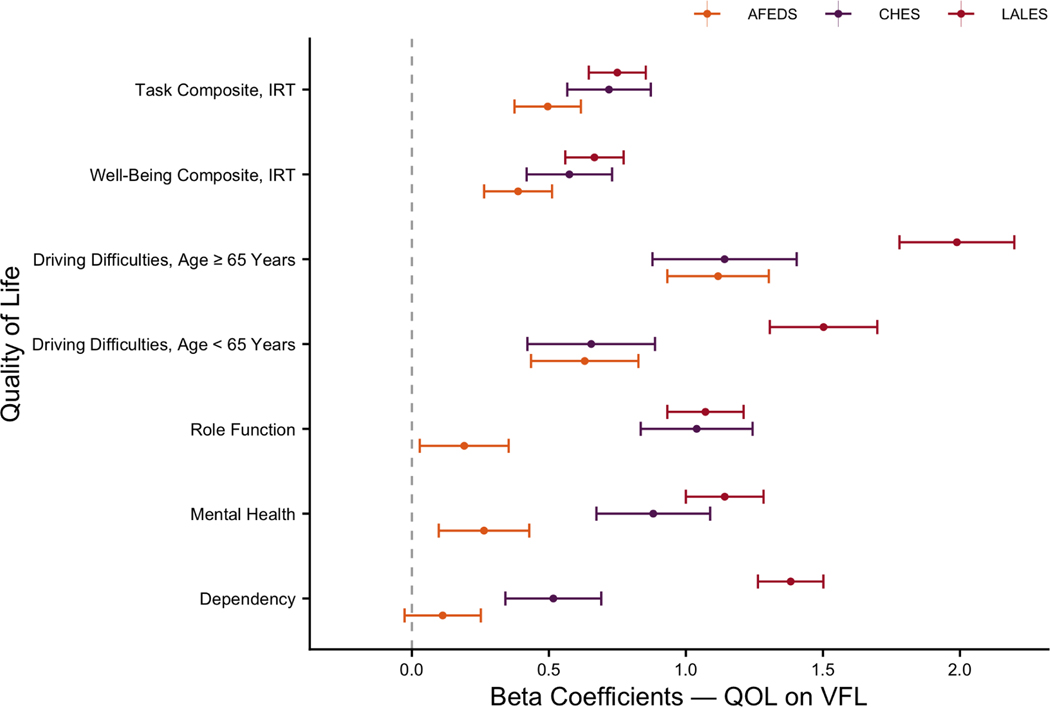
Figure 3:
Linear regression beta coefficients of NEI-VFQ-25 IRT and CTT on VFL (MD in dB) in the BSE by cohort LOWESS = Locally Weighted Scatterplot Smoothing; NEI-VFQ-25 = National Eye Institute Visual Function Questionnaire 25-ltem; IRT = Item Response Theory; CTT = Classical Test Theory; VFL = Visual Field Loss; MD = Mean Deviation; dB = Decibels; BSE = Better-Seeing Eye Linear regression models were adjusted for race and ethnicity, age, number of comorbidities, sex (female), born in USA (yes), education highest grade obtained), working status (unemployed), income (≤ $20,000), has health insurance (yes), presenting binocular visual acuity (LogMAR score), depression (a good bit of the time or more in the last 4 weeks), and an interaction between VFL and race, ethnicity.
VSQOL Classical Test Theory Subscales and VFL Varied by Race and Ethnicity
Variations by race and ethnicity were observed in associations between VFL and CTT subscales of VSQOL. Subscales with the largest relationships included vision-related driving difficulties, role function, mental health, and dependency (Figure 3). Beta coefficients for VSQOL on VFL were tabulated for Latinos (Table S3), Chinese Americans (Table S4), and African Americans (Table S5 available at http://www.aaojournal.org).
After driving difficulties, the CTT subscale with the second largest association with VFL overall was vision-related role function (Figure S3 available at http://www.aaojournal.org). It was the strongest inverse association in Chinese Americans at 1.039 (95% CI: 0.835, 1.243) points of VSQOL per dB of VFL; role function was the fifth strongest association in both Latinos at 1.071 (95% CI: 0.932, 1.210) and African Americans at 0.191 (95% CI: 0.029, 0.353), but was not significant in the latter group after adjusting for multiple comparisons. The associations were significantly larger in Chinese Americans and Latinos compared to African Americans. Vision-related mental health was the third largest association with VFL overall (Figure S4 available at http://www.aaojournal.org). It was the second largest association in Chinese Americans at 0.881 (95% CI: 0.673, 1.088) points of VSQOL per dB of VFL; mental health was the fourth largest association in both Latinos at 1.142 (95% CI: 1.000, 1.283) and African Americans at 0.263 (95% CI: 0.098, 0.428). The associations were also significantly larger in Latinos and Chinese Americans compared to African Americans. Vision-related dependency was the fourth largest association with VFL overall (Figure S5 available at http://www.aaojournal.org). It was the second strongest association in Latinos at 1.382 (95% CI: 1.263, 1.502) points of VSQOL per dB of VFL; dependency was the fifth largest association in Chinese Americans 0.516 (95% CI: 0.341, 0.691), and was not significantly associated with VFL in African Americans at 0.112 (95% CI: −0.027, 0.251). Associations between dependency and VFL were significantly different among all three cohorts.
Several CTT subscales were uniquely associated with VFL in specific racial and ethnic groups (Figure S6 available at http://www.aaojournal.org). Near vision was the third largest association with VFL in African Americans at 0.397 (95% CI: 0.269, 0.525) and the fourth largest in Chinese Americans at 0.565 (95% CI: 0.404, 0.726). Peripheral vision was the third strongest association for Latinos at 1.151 (95% CI: 1.046, 1.257) and the fourth in African Americans at 0.313 (95% CI: 0.190, 0.436).
Sensitivity Analyses
Racial and ethnic differences in associations between VFL and VSQOL IRT outcomes from the primary analysis were compared to sensitivity analyses in subgroups of the MOCCaS population (Figure S7 available at http://www.aaojournal.org). There was greater variation by race and ethnicity among participants who were younger than 65 years, male, born in the US, graduated high school, employed, insured, not depressed, and not visually impaired. Conversely, racial and ethnic differences were unobserved among participants who were 65 years and older, women, and foreign born; there were no differences among high income earners only for the socioemotional well-being outcome.
Discussion
Race and ethnicity significantly modified the relationship between VFL and VSQOL. An inverse relationship was observed between VFL and VSQOL for all racial and ethnic groups; associations were larger for vision-related tasks yet varied more by race and ethnicity for well-being. In MOCCaS, Latinos and Chinese Americans reported a greater change in VSQOL than African Americans for the same level of VFL. A 5-point reduction in the task and well-being composite scores were associated with mild-to-moderate VFL for Latinos and Chinese Americans and with moderate-to-severe VFL for African Americans. These differences reached statistical significance when comparing Latinos and African Americans, but not Chinese Americans. Disparities in health outcomes have been attributed to differences in SES and barriers to healthcare.36 However, meaningful differences in VSQOL persisted across self-identified racial and ethnic groups after controlling SES and clinical variables. Unmeasured social or cultural factors could explain enduring effects by race and ethnicity.
Sensitivity analyses were conducted to further address whether the interaction by race and ethnicity in the association of VSQOL and VFL could be explained by measured sociodemographics. Racial and ethnic differences were diminished when restricting models to participants aged 65 years and older, suggesting that underlying differences associated with race and ethnicity have less influence on older populations with worse VFL. A survivor bias may contribute to older participants from all races and ethnicities having similar VSQOL responses to VFL. However, most differences persisted when restricting by sex, SES factors, immigration status, depression, and central VI, suggesting that race and ethnicity have an enduring differential effect on the associations between VFL and VSQOL among specific subgroups (see Appendix 1 available at http://www.aaojournal.org).
We hypothesized that age would modify the association of VFL and all VSQOL outcomes due to the complex processes that limit autonomy during the final decades of life. However, most models that included an additional interaction term by age greater than 65 years provided no better explanation than nested models with an interaction term by race and ethnicity alone. This finding suggests that the impact of VFL on VSQOL was similar for both age groups. In contrast, age was an important modifier of VI and VSQOL in a cross-sectional analyses of a Singaporean Chinese community.37
Driving is a complex activity affected by reduced VF, VA, cognition, and reaction time. The association of VFL with driving difficulties was the only outcome with a significant interaction by age stratified at 65 years; moderate VFL (10.3 dB) was associated with a meaningful 5-point reduction in driving difficulties between age groups. Unmeasured comorbidities such as cognitive function and hearing loss may contribute to age-specific interactions of VFL on driving difficulties.38 Such factors could be involved in the mechanism by which older participants with VI experience greater reductions to VSQOL.
The driving VSQOL subscale was most affected by VFL, which was consistent with existing literature.12,13,15 This was true for older participants of all racial and ethnic groups as well as for younger adults who self-identified as Latino or African American. Vision-related role function and mental health, however, were more impacted by VFL among younger Chinese Americans. This difference may be related to barriers to care in Chinese Americans;39 only 53% of Chinese Americans had health insurance, which was lower than both 64.9% of Latinos and 89.7% of African Americans. VFL may have a greater relative impact on younger Chinese American’s self-efficacy and mental health if they lack health insurance; Medicare may lessen worries about vision loss for older Chinese Americans, while age-related vision loss could impact their driving ability. Following driving difficulties, the VSQOL subscales most impacted by VFL included vision-related role function, mental health, and dependency. Differences by race and ethnicity were larger for the granular CTT subscales than for the more robust IRT domains.
Sociodemographic differences may exacerbate challenges in navigating a healthcare system and accomplishing vision-dependent tasks for less acculturated participants with VI. VFL had the second-largest effect on vision-related role function, which indicates how vision inhibits participants from accomplishing as much as they would like and from working for longer periods of time. Latinos and Chinese Americans reported significantly lower role function scores with VFL as well as lower educational attainment, annual income, and health insurance. These cohorts were also predominantly immigrant populations (24.5% of the LALES were US-born; 1.3% of the CHES) compared to the African American cohort (91.0% of the AFEDS). Differences in how VFL affects the ability to complete visual tasks may be due to differences by race and ethnicity, but perhaps is more likely due to differences in sociodemographics that persist even when adjusting for SES and immigration.
Vision-related mental health may be one aspect of socioemotional well-being that is most affected by VFL across races and ethnicities. Mental health includes worry, frustration, loss of control and embarrassment due to vision loss. Previous studies have suggested the psychosocial impact of VI is driven by changes in identity and self-esteem.40 VFL may reduce mental health through these mechanisms regardless of race and ethnicity, as mental health was among the VSQOL subscales with the least impact by cohort. Both treatments and rehabilitation programs aimed at preventing vision loss may prioritize vision-specific mental health as outcome measures. Furthermore, associations of VFL with well-being outcomes tended towards greater variation by cohort compared to task outcomes.
Vision-related dependency was the second most sensitive subscale to VFL among Latinos in the MOCCaS. The magnitude of dependency on VFL was twice as large as that of Chinese Americans and was not significant among African Americans. Vision-related dependency measured whether participants’ vision caused them to stay at home most of the time and to rely on others more than they desired. The disproportionate burden of diabetic retinopathy among Latinos4,41 could be related to the greater reporting of dependency on others.
Strengths of the present analysis include the use of population-based cohort studies to minimize selection bias and detect interactions of associations among the most populous US racial and ethnic groups. Standard approaches were used to measure VF, central VA, VSQOL and covariates over diverse populations. In addition, the baseline methods papers of all three cohorts provide evidence that the study populations in the MOCCaS were generally representative of Latino, Chinese American, and African American populations in the State of California and the US overall.16–18
Our study has several limitations. Overadjustment of completely separated covariates may limit our ability to capture the true associations of VSQOL and VFL by race and ethnicity. For example, African American participants were almost all born in the US while Chinese Americans were almost all born abroad. Adjusting on birthplace may limit our ability to detect differences between these two groups. However, birth country was included as an important proxy of acculturation that was available in all three cohorts. Additionally, a fraction of participants were both Latino and African American; genetic modeling in the LALES cohort indicated the average admixture was of 4.0–5.2% African American ancestry,42 and 1.5% of AFEDS participants self-reported Hispanic ethnicity. Although potential bias could be reduced by reclassifying the subset of participants with mixed races and ethnicities, this was opted against to avoid introducing additional bias from potential unmeasured confounders specific to the distinct cohorts. Furthermore, there was a large difference in the SES of African Americans compared to Latinos and Chinese Americans. Future work should study the relationship of VSQOL and VI in diverse populations across a larger spectrum of SES. This work should also include a broader sampling of individuals in rural environments experiencing risk factors different from those in the urban populations of the MOCCaS.
We relied on the epidemiological literature to propose multiple mechanisms of how race and ethnicity may modify the relationships between VSQOL and VFL. Follow-up studies employing qualitative methods may be used to investigate how associations of VI and self-perceived VSQOL differ across cohorts in the MOCCaS. In addition, focus groups could be designed to elucidate why Latinos were more sensitive to VFL compared to African Americans.
Preserving VSQOL is a priority when caring for patients with eye disease, conducting public health prevention programs, and designing clinical trials for novel ophthalmic interventions. Preventing VFL may protect patients’ ability to complete visual tasks and their socioemotional well-being. In the MOCCaS we found evidence that race and ethnicity are important modifiers of the relationship between VFL and VSQOL even after controlling for education, employment, and income. Therefore, the perception of VFL on self-reported VSQOL could be influenced by additional contextual SES factors that remain to be studied. Nevertheless, providers may advise patients with VFL regardless of race and ethnicity that their ability to drive may be affected as early as mild VFL (< −6 dB) or even earlier in those age 65 years and older. Furthermore, it is essential that clinical trials include multiethnic samples to ensure findings apply to the increasingly diverse US population with respect to race, ethnicity, age, and SES. VSQOL will continue to be an important outcome in determining clinical treatments for the public and ensuring patient satisfaction with clinical care.
Supplementary Material
Table 1:
Sociodemographic and Clinical Characteristics of Participants in MOCCaS (n = 14,570)*
| MOCCaS | LALES | CHES | AFEDS | P-Value† | |||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Race/Ethnicity | |||||||||
| Latino | 5,248 | (36.0%) | 5,248 | (100.0%) | |||||
| Chinese American | 4,151 | (28.5%) | 4,151 | (100.0%) | |||||
| African American | 5,171 | (35.5%) | 5,171 | (100.0%) | |||||
| Age | 59.0 | (10.7) | 55.0 | (10.7) a | 61.2 | (8.5) b | 61.2 | (11.0) b | < 0.001 |
| Education‡ | 11.5 | (4.5) | 8.2 | (4.4) a | 12.2 | (3.8) b | 14.3 | (2.4) c | < 0.001 |
| Number of Comorbidities§ | 1.6 | (1.5) | 1.5 | (1.5) a | 1.2 | (1.4) b | 2.0 | (1.5) c | < 0.001 |
| Sex (Female) | 8903 | (61.1%) | 3069 | (58.5%) a | 2599 | (62.6%) b | 3235 | (62.6%) b | < 0.001 |
| US Born | 6048 | (41.5%) | 1284 | (24.5%) a | 56 | (1.3%) b | 4708 | (91.0%) c | < 0.001 |
| Employment (Working) | 7066 | (48.5%) | 2555 | (48.7%) a | 2202 | (53.0%) b | 2309 | (44.7%) c | < 0.001 |
| Annual Income ≥ $20,000 | 6997 | (48.0%) | 2285 | (43.5%) a | 1716 | (41.3%) b | 2996 | (57.9%) c | < 0.001 |
| Health Insurance | 10243 | (70.3%) | 3407 | (64.9%) a | 2199 | (53.0%) b | 4637 | (89.7%) c | < 0.001 |
| Depression|| | 1424 | (9.8%) | 840 | (16.0%) a | 274 | (6.6%) b | 310 | (6.0%) b | < 0.001 |
| Visual Impairment¶ | 905 | (6.2%) | 310 | (5.9%) a | 369 | (8.9%) b | 226 | (4.4%) c | < 0.001 |
MOCCaS = Multiethnic Ophthalmology Cohorts of California Study; LALES = Los Angeles Latino Eye Study; CHES = Chinese American Eye Study; AFEDS = African American Eye Disease Study; SD = Standard Deviation; VFL = Visual Field Loss
Data are presented as mean (SD) for continuous variables (age, education, comorbidities); categorical variables are presented as frequency counts with percentages (%) of participants for each category of visual field loss (VFL) severity; percentages exclude participants with missing responses); the number missing is 182 (1.2%) for education; 10 (0.1%) for sex, 118 (0.8%) for US born; 182 (1.2%) for employment; 1,868 (12.8%) for income; 306 (2.1%) for insurance; 12 (0.1%) for depression; and 2 ( 0.0%) for visual acuity loss.
P-values for continuous variables are from the test for equal means in a one-way layout, and for categorical variables are from the Pearson’s χ2 test. Superscripts indicate Holm-adjusted pairwise comparisons across cohorts.
Highest educational grade completed
Number of self-reported comorbidities (diabetes, arthritis, stroke/brain hemorrhage, high blood pressure, angina, heart attack, heart failure, asthma, skin cancer, other cancer, back problems, hearing problems and other major health problems).
Depression was scored using the SF-12 item “Have you felt downhearted or blue a good bit of the time or more during the past 4 weeks?” Participants were considered depressed if they reported “A good bit of the time”, “Most of the time”, or “All of the time”.
Visual Impairment was defined as binocular presenting visual acuity 20/40 or worse.
Acknowledgements
The authors would like to thank the Multiethnic Ophthalmology Cohorts of California Study Group External Advisory Committees for their advice and contributions. The authors would also like to acknowledge support of the analysis for this project from Wendy J. Mack, PhD; Lourdes A. Baezconde-Garbanati, PhD, MPH; Trevor Pickering, PhD; and Eileen M. Crimmins, PhD. Department of Ophthalmology, Battelle Survey Research Center, St. Louis, MO: Lisa John, PhD; Nicole Weinstein, MSW; Natasha Van Leeuwen; James Clark; Sandra Ramirez. Singapore National Eye Centre, Ocular Reading Center: Tien Wong, MD, PhD; Soundaram Jaganathan; Haslina Hamzah.
Financial Support: NIH National Institute of Environmental Health Sciences T32 ES-013678, NIH National Institute on Aging Grant T32 AG-000037, NIH National Eye Institute Grant U10 EY-023575, and an unrestricted grant from the Research to Prevent Blindness, New York, New York. The sponsor or funding organization had no role in the design or conduct of this research.
Abbreviations/Acronyms
- (AFEDS)
African American Eye Disease Study
- (BSE)
Better Seeing Eye
- (CTT)
Classical Test Theory
- (IRT)
Item Response Theory
- (LOWESS)
Locally Weighted Scatterplot Smoothing
- (LALES)
Los Angeles Latino Eye Study
- (NEI-VFQ-25)
National Eye Institute Visual Functioning Questionnaire-25
- (SES)
Socioeconomic Status
- (VA)
Visual Acuity
- (VF)
Visual Field
- (VFL)
Visual Field Loss
- (VI)
Visual Impairment
- (VSQOL)
Vision-Specific Quality of Life
Footnotes
This article contains additional online-only material. The following should appear online-only: Figures S1 to S6, Tables S1 to S5, and Appendix 1, which includes Figure S7.
Meeting Presentation: This abstract was communicated as a paper presentation for the ARVO Annual Meeting held virtually during May 2020.
This is an original article submission. This article has not been published anywhere previously, has not been submitted for publication anywhere previously, and it is not simultaneously being considered for any other publication.
Conflict of Interest: No conflict of interest exists for any author.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Varma R, Vajaranant TS, Burkemper B, et al. Visual Impairment and Blindness in Adults in the United States: Demographic and Geographic Variations from 2015 to 2050. JAMA Ophthalmol. 2016;134(7):802–809. doi: 10.1001/jamaophthalmol.2016.1284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klein R, Klein BEK. The prevalence of age-related eye diseases and visual impairment in aging: current estimates. Invest Ophthalmol Vis Sci. 2013;54(14):ORSF5-ORSF13. doi: 10.1167/iovs.13-12789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fisher DE, Shrager S, Shea SJ, et al. Visual Impairment in White, Chinese, Black, and Hispanic Participants from the Multi-Ethnic Study of Atherosclerosis Cohort. Ophthalmic Epidemiol. 2015;22(5):321–332. doi: 10.3109/09286586.2015.1066395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varma R, Torres M, Pena F, Klein R, Azen SP, Los Angeles Latino Eye Study G. Prevalence of diabetic retinopathy in adult Latinos: the Los Angeles Latino eye study. Ophthalmology. 2004;111(7):1298–1306. doi: 10.1016/j.ophtha.2004.03.002 [DOI] [PubMed] [Google Scholar]
- 5.Friedman DS, Jampel HD, Muñoz B, West SK. The prevalence of open-angle glaucoma among blacks and whites 73 years and older: the Salisbury Eye Evaluation Glaucoma Study. Arch Ophthalmol. 2006;124(11):1625–1630. doi: 10.1001/archopht.124.11.1625 [DOI] [PubMed] [Google Scholar]
- 6.Gupta P, Zhao D, Guallar E, Ko F, Boland MV, Friedman DS. Prevalence of Glaucoma in the United States: The 2005–2008 National Health and Nutrition Examination Survey. Invest Ophthalmol Vis Sci. 2016;57(6):2905–2913. doi: 10.1167/iovs.15-18469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choudhury F, Meuer SM, Klein R, et al. Prevalence and Characteristics of Myopic Degeneration in an Adult Chinese American Population: The Chinese American Eye Study. American journal of ophthalmology. 2018;187:34–42. doi: 10.1016/j.ajo.2017.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fayers P, Machin D. Quality of Life: The Assessment, Analysis and Reporting of Patient-Reported Outcomes. Third. John Wiley & Sons, Ltd; 2016. https://www.wiley.com/en-us/Quality+of+Life%3A+The+Assessment%2C+Analysis+and+Reporting+of+Patient+reported+Outcomes%2C+3rd+Edition-p-9781444337952 [Google Scholar]
- 9.Leyland M, Zinicola E. Multifocal versus monofocal intraocular lenses in cataract surgery: a systematic review. Ophthalmology. 2003;110(9):1789–1798. doi: 10.1016/S0161-6420(03)00722-X [DOI] [PubMed] [Google Scholar]
- 10.van Nispen RM, Virgili G, Hoeben M, et al. Low vision rehabilitation for better quality of life in visually impaired adults. Cochrane Database Syst Rev. 2020;1:CD006543. doi: 10.1002/14651858.CD006543.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.George S, Duran N, Norris K. A Systematic Review of Barriers and Facilitators to Minority Research Participation Among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health. 2014;104(2):e16–e31. doi: 10.2105/AJPH.2013.301706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qiu M, Wang SY, Singh K, Lin SC. Association between visual field defects and quality of life in the United States. Ophthalmology. 2014;121(3):733–740. doi: 10.1016/j.ophtha.2013.09.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McKean-Cowdin R, Varma R, Wu J, Hays RD, Azen SP. Severity of visual field loss and health-related quality of life. American journal of ophthalmology. 2007;143(6):1013–1023. doi: 10.1016/j.ajo.2007.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rubin GS, Bandeen-Roche K, Huang GH, et al. The association of multiple visual impairments with self-reported visual disability: SEE project. Invest Ophthalmol Vis Sci. 2001;42(1):64–72. [PubMed] [Google Scholar]
- 15.Grisafe II DJ, Varma R, Burkemper BS, et al. Impact of Visual Field Loss on Vision-Specific Quality of Life in African Americans: The African American Eye Disease Study. Am J Ophthalmol. Published online February 8, 2021. doi: 10.1016/j.ajo.2021.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Varma R, Paz SH, Azen SP, et al. The Los Angeles Latino Eye Study: design, methods, and baseline data. Ophthalmology. 2004;111(6):1121–1131. doi: 10.1016/j.ophtha.2004.02.001 [DOI] [PubMed] [Google Scholar]
- 17.Varma R, Hsu C, Wang D, Torres M, Azen SP. The Chinese American Eye Study: Design and Methods. Ophthalmic epidemiology. 2013;20(6):335–347. doi: 10.3109/09286586.2013.823505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McKean-Cowdin R, Fairbrother-Crisp A, Torres M, et al. The African American Eye Disease Study: Design and Methods. Ophthalmic epidemiology. 2018;25(4):306–314. doi: 10.1080/09286586.2018.1454965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferris FL 3rd, Bailey I. Standardizing the measurement of visual acuity for clinical research studies: Guidelines from the Eye Care Technology Forum. Ophthalmology. 1996;103(1):181–182. [DOI] [PubMed] [Google Scholar]
- 20.Yohannan J, Wang J, Brown J, et al. Evidence-based Criteria for Assessment of Visual Field Reliability. Ophthalmology. 2017;124(11):1612–1620. doi: 10.1016/j.ophtha.2017.04.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arora KS, Boland MV, Friedman DS, Jefferys JL, West SK, Ramulu PY. The Relationship between Better-Eye and Integrated Visual Field Mean Deviation and Visual Disability. Ophthalmology. 2013;120(12):2476–2484. doi: 10.1016/j.ophtha.2013.07.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hodapp E, Parrish RK, Anderson DR. Clinical Decisions in Glaucoma. Mosby; 1993. [Google Scholar]
- 23.Mangione CM, Lee PP, Pitts J, Gutierrez P, Berry S, Hays RD. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ). NEI-VFQ Field Test Investigators. Archives of ophthalmology (Chicago, Ill : 1960). 1998;116(11):1496–1504. [DOI] [PubMed] [Google Scholar]
- 24.Petrillo J, Cano SJ, McLeod LD, Coon CD. Using classical test theory, item response theory, and Rasch measurement theory to evaluate patient-reported outcome measures: a comparison of worked examples. Value in health : the journal of the International Society for Pharmacoeconomics and Outcomes Research. 2015;18(1):25–34. doi: 10.1016/j.jval.2014.10.005 [DOI] [PubMed] [Google Scholar]
- 25.Andrich D. Rating scales and Rasch measurement. http://dx.doi.org/101586/erp1159. Published online January 9, 2014. doi: 10.1586/erp.11.59 [DOI] [Google Scholar]
- 26.Rizopoulos D. Latent Trait Models under Item Response Theory; 2018. https://github.com/drizopoulos/ltm [Google Scholar]
- 27.Wang M, Spiegelman D, Kuchiba A, et al. Statistical methods for studying disease subtype heterogeneity. Stat Med. 2016;35(5):782–800. doi: 10.1002/sim.6793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in r. Journal of Statistical Software. 2011;45(3):1–67. [Google Scholar]
- 29.Globe DR, Wu J, Azen SP, Varma R, Los Angeles Latino Eye Study G. The impact of visual impairment on self-reported visual functioning in Latinos: The Los Angeles Latino Eye Study. Ophthalmology. 2004;111(6):1141–1149. doi: 10.1016/j.ophtha.2004.02.003 [DOI] [PubMed] [Google Scholar]
- 30.Friedman DS, West SK, Munoz B, et al. Racial variations in causes of vision loss in nursing homes: The Salisbury Eye Evaluation in Nursing Home Groups (SEEING) Study. Arch Ophthalmol. 2004;122(7):1019–1024. doi: 10.1001/archopht.122.7.1019 [DOI] [PubMed] [Google Scholar]
- 31.Wilson FA, Wang Y, Stimpson JP, Kessler AS, Do DV, Britigan DH. Disparities in Visual Impairment by Immigrant Status in the United States. American Journal of Ophthalmology. 2014;158(4):800–807.e5. doi: 10.1016/j.ajo.2014.07.007 [DOI] [PubMed] [Google Scholar]
- 32.Owsley C, McGwin G. Depression and the 25-item National Eye Institute Visual Function Questionnaire in older adults. Ophthalmology. 2004;111(12):2259–2264. doi: 10.1016/j.ophtha.2004.06.026 [DOI] [PubMed] [Google Scholar]
- 33.R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; 2019. http://www.R-project.org/ [Google Scholar]
- 34.Holm S. A Simple Sequentially Rejective Multiple Test Procedure. Scandinavian Journal of Statistics. 1979;6(2):65–70. [Google Scholar]
- 35.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Journal of Clinical Epidemiology. 2008;61(4):344–349. doi: 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 36.Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health. 2010;100 Suppl 1:S186–196. doi: 10.2105/AJPH.2009.166082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Man REK, Gan ATL, Fenwick EK, et al. The Differential Impact of Age on Vision-Related Quality of Life across the Visual Impairment Spectrum. Ophthalmology. 2021;128(3):354–363. doi: 10.1016/j.ophtha.2020.07.046 [DOI] [PubMed] [Google Scholar]
- 38.Schubert CR, Cruickshanks KJ, Fischer ME, et al. Sensory Impairments and Cognitive Function in Middle-Aged Adults. J Gerontol A Biol Sci Med Sci. 2017;72(8):1087–1090. doi: 10.1093/gerona/glx067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jiang X, Varma R, Torres M, Hsu C, McKean-Cowdin R, Chinese American Eye Study Group. Self-reported Use of Eye Care Among Adult Chinese Americans: The Chinese American Eye Study. Am J Ophthalmol. 2017;176:183–193. doi: 10.1016/j.ajo.2017.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Senra H, Barbosa F, Ferreira P, et al. Psychologic adjustment to irreversible vision loss in adults: a systematic review. Ophthalmology. 2015;122(4):851–861. doi: 10.1016/j.ophtha.2014.10.022 [DOI] [PubMed] [Google Scholar]
- 41.Mazhar K, Varma R, Choudhury F, et al. Severity of diabetic retinopathy and health-related quality of life: the Los Angeles Latino Eye Study. Ophthalmology. 2011;118(4):649–655. doi: 10.1016/j.ophtha.2010.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shtir CJ, Marjoram P, Azen S, et al. Variation in genetic admixture and population structure among Latinos: the Los Angeles Latino eye study (LALES). BMC Genet. 2009;10:71. doi: 10.1186/1471-2156-10-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.