Abstract
Purpose:
A phase II multi-institutional clinical trial was conducted to determine overall survival (OS) in patients with recurrent and/or metastatic (R/M) head and neck squamous cell carcinoma (HNSCC) treated with a combination of cetuximab and nivolumab.
Experimental Design:
Patients with R/M HNSCC were treated with cetuximab 500 mg/m2 IV Day (D) −14 as a lead-in followed by cetuximab 500 mg/m2 IV and nivolumab 240 mg IV on D1 and D15 of each 28-D cycle. Expression of p16 and programmed cell death-ligand 1 (PD-L1) in archived tumors were determined. Tumor-tissue-modified human papillomavirus (TTMV) DNA was quantified in plasma.
Results:
Ninety-five patients were enrolled, and 88 patients were evaluable for OS with a median follow-up of 15.9 months. Median OS in the 45 patients who had prior therapy for R/M HNSCC (Cohort A) was 11.4 months, with a 1-year OS 50% (90% CI, 0.43-0.57). Median OS in the 43 patients who had no prior therapy (Cohort B) was 20.2 months, with a 1-year OS 66% (90% CI, 0.59-0.71). In the combined cohorts, the p16-negative immunostaining was associated with higher response rate (RR, p=0.02) but did not impact survival while higher PD-L1 combined positive score was associated with higher RR (p=0.03) and longer OS (log-rank p=0.04). In the p16-positive patients, <median (1,230 copies/mL) TTMV DNA counts were associated with higher RR (p=0.01) and longer OS compared to >median (log-rank p=0.05).
Conclusion:
The combination of cetuximab and nivolumab is effective in patients with both previously treated and untreated R/M HNSCC and warrants further evaluation.
INTRODUCTION
In the United States, approximately 67,000 cases of head and neck squamous cell carcinoma (HNSCC) are diagnosed per year (1). The major risk factors of HNSCC are tobacco use, heavy alcohol use, and human papillomavirus (HPV) infection (2-6). The incidence of HPV-related HNSCC, particularly in the oropharynx, is rapidly increasing (7, 8). While the prognosis of newly diagnosed, HPV-related HNSCC is favorable, with 3-year overall survival (OS) greater than 90%, non-HPV-related HNSCC has poor prognosis, with 3-year OS less than 50% (6, 9-11). Once patients develop recurrent and/or metastatic (R/M) HNSCC, they are mostly incurable.
The current standard of care for the management of previously untreated and incurable R/M HNSCC is a programed cell death 1 (PD-1) inhibitor, pembrolizumab, for patients with a PD ligand 1 (PD-L1) combined positive score (CPS) of ≥1. A combination of pembrolizumab, cisplatin, and 5-fluorouracil (5-FU) followed by pembrolizumab maintenance therapy is recommended for patients with any PD-L1 CPS (12). Although these regimens are highly effective in selected patients, most patients ultimately have disease progression, with a median OS of 11.6-13.6 months and 1-year OS of 49-55% depending upon the PD-L1 expression. In addition, combination chemotherapy with pembrolizumab is relatively toxic compared to monotherapy. There have been attempts to combine two immunotherapy agents to improve efficacy. However, the combination of durvalumab (PD-L1 inhibitor) and tremelimumab [a cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4) inhibitor] did not show an OS benefit in a phase III clinical trial of durvalumab with and without tremelimumab (13). An additional phase III trial comparing a combination of nivolumab (PD-1 inhibitor) and ipilimumab (CTLA-4 inhibitor) to the EXTREME regimen did not meet the primary endpoint goal of OS in the total and PD-L1 CPS ≥20 population.
Cetuximab is a human-mouse chimeric anti-EGFR monoclonal IgG1 antibody with FDA approval in the management of HNSCC. Among the EGFR inhibitors, cetuximab is unique in its ability to activate the antibody-dependent cellular cytotoxicity (ADCC) because it is an IgG1 antibody (14-16). As reviewed in detail by Ferris et al. (14), after cetuximab binds to EGFR on the tumor cells, CD16 on natural killer (NK) cells execute their killing routine on the cetuximab-bound tumor cell. Notably, the killing of tumor cells can result in the cross-priming of cytotoxic CD8+ T cells by activated dendritic cells. Moreover, activated NK cells also secrete interferon (IFN)-gamma, other proinflammatory cytokines, and chemokines, which will mediate changes in the immune contexture that favor immune activation and the recruitment of other immune cells to the tumor microenvironment (TME). However, cetuximab-mediated immune stimulatory activity can also result in immunosuppressive signals through multiple negative feedback loops. For example, cetuximab-mediated immune response can also increase immunosuppressive Treg infiltration and the recruitment of myeloid-derived suppressor cells (MDSC) which can dampen the immune stimulatory activity of cetuximab. Also, IFN-gamma from NK cells can lead to the expression of PD-L1. Given the data that higher expression of PD-L1 is associated with increased clinical benefits (12, 17), there is a strong rationale to combine PD-1/PD-L1 axis inhibitors with cetuximab as a means to synergy in their anti-tumor activities.
The response rate of cetuximab as a monotherapy in R/M HNSCC is 13% and has shown improved OS in combination with radiation or cisplatin and 5-FU (18-20). To determine more effective and less toxic treatments, we evaluated a combination of cetuximab and nivolumab in two R/M HNSCC cohorts: Cohort A for patients with prior exposure to any systemic therapy and persistent or platinum-refractory R/M HNSCC and Cohort B for patients without prior exposure to any systemic therapy for R/M HNSCC. The early results from Cohort A have been published and showed that the combination was very well tolerated (21). In the current manuscript, we report on the updated survival data of Cohort A with a longer follow-up, and the clinical results of Cohort B.
In addition, we report on the biomarker analyses of p16 immunohistochemical (IHC) staining and PD-L1 CPS in the combined Cohort A and B patients. While positive p16 IHC is an established surrogate biomarker of HPV infection in oropharyngeal SCC and a robust prognostic biomarker of favorable outcomes in HNSCC, its predictive role in patients treated with PD-1 inhibitors or immunotherapy-containing regimen is not clearly established (12, 22-24). We also evaluated the role of PD-L1 CPS as a biomarker of response in patients treated with the combination. Furthermore, we quantified circulating tumor-tissue-modified human papillomavirus (TTMV) DNA and determined the HPV strains (25, 26) in patients with p16 positive tumors. While TTMV DNA has been evaluated in newly diagnosed HNSCC patients treated with radiation or concurrent chemoradiotherapy as a tool for response assessment and recurrence surveillance, our study is the first to evaluate this biomarker in R/M HNSCC treated with the combination of cetuximab and nivolumab.
MATERIALS AND METHODS
Study Design and Patient Selection
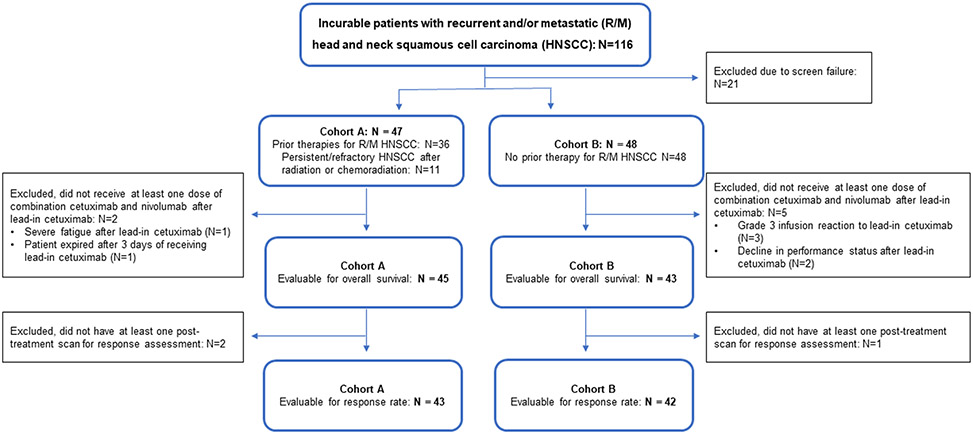
The phase II study was conducted at the Moffitt Cancer Center, The Ohio State University, and Emory University (NCT03370276), and written consents were obtained. Institutional IRB approval was obtained in accordance with the Department of Health and Human Services Federal Policy for the Protection of Human Subjects (US Common Rule) at each participating institution. The study was initiated after the IRB approvals. Patients were eligible for enrollment if they met the following criteria: histologically or cytologically confirmed SCC of oral cavity, oropharynx, paranasal sinuses, nasal cavity, hypopharynx, or larynx; p16-positive SCC of unknown primary in a cervical lymph node; incurable R/M HNSCC by a local therapy (surgery or radiation therapy with or without chemotherapy). Cohort A enrolled patients with prior exposure to any systemic therapy for R/M HNSCC including cetuximab or PD-1 inhibitors and persistent or platinum-refractory disease) (Figure 1) (21). Cohort B enrolled the patients with no prior exposure to any systemic therapy for R/M HNSCC. The detailed eligibility criteria are provided in the protocol (Supplemental File 1).
Figure 1.
Consort diagram of the clinical trial
Patients were treated with lead-in cetuximab 500 mg/m2 alone (Day −14 before Cycle 1 only) followed by nivolumab 240 mg IV + cetuximab 500 mg/m2 every 2 weeks for 24 cycles or discontinuation (Supplementary Figure 1). We chose to have a cetuximab lead-in to exclude patients with cetuximab-related infusion reaction. Patients having a cetuximab-related infusion reaction or who did not receive Cycle 1 Day 1 for any reason were deemed non-evaluable and replaced. The toxicities with possible, probable, and definite attribution were included in treatment-related adverse events (TRAEs) and immune-related adverse events (IRAEs) analyses. Nivolumab dose reduction was not allowed. Cetuximab dose reduction was allowed: Dose −1 (250 mg/m2 every 2 weeks) or Dose −2 (125 mg/m2 every 2 weeks). In cases where one agent was withheld, both were delayed and resumed concurrently.
Radiographical Response Assessment
For response assessment, CT or MRI imaging studies were obtained every 6 weeks for Cycles 1-4, every 2 cycles during Cycles 5-6, and then every 3 cycles during Cycles 7-24 while on study drugs. The same types of scans were used for repeat measurements. Response was assessed by the Response Evaluation Criteria in Solid Tumors (RECIST) 1.1 by the investigators.
Biomarker Studies: p16 and PD-L1 Immunohistochemical Staining and TTMV DNA Quantification
Archived formalin fixed paraffin embedded tumors were collected to assess p16 and PD-L1 expression. The p16 staining was performed using p16 mouse monoclonal antibody predilute, CINtec®, clone E6H4 (Roche Tissue Diagnostics, Tucson, AZ, USA) as previously described and scored following the guidelines for p16 interpretation endorsed by the College of American Pathology. The PD-L1 staining was performed using 22C3 pharmDx assay (Agilent Technologies, Carpinteria, CA, USA), and CPS was determined as previously described (12). Whole blood was collected at 5 time points: 1) pre-treatment, 2) after cetuximab lead-in or 2 weeks after C1D1, 3) C4D1, 4) end of treatment, and 5) end of 2-year follow-up or at the time of disease progression whichever was earlier, and the plasma was separated. TTMV DNA was quantified from cell free DNA isolated from plasma samples (Naveris, Natick, MA, USA), as previously described (25, 26). The lower limit of detection is <5 copies/mL.
Statistical Analysis
For survival analyses, progression-free survival (PFS) time was defined as the time between the date of study enrollment and the date of progressive disease or death whichever happened first or otherwise censored at the last date known alive. Overall survival time was defined as the time between the date of study enrollment and the date of death or censored at the last date known alive. The primary objective of the phase II study Cohort A was to determine the 1-year OS rate of concurrent cetuximab and nivolumab in patients who had any prior treatments and persistent or platinum-refractory R/M HNSCC. The null hypothesis was that the 1-year OS rate with the combination would be no higher than 36% based on the historical data from pembrolizumab and nivolumab monotherapy (24, 27). Forty-five evaluable patients were enrolled to have 90% power to reject the null hypothesis and conclude the true 1-year OS rate was higher than 36% if the true rate was 36% or higher at α=0.05, using the one-sample log-rank test assuming an exponential distribution.
The primary objective of the phase II study Cohort B was to determine the 1-year OS rate of concurrent cetuximab and nivolumab in patients who had not had any prior treatments for their R/M HNSCC. The null hypothesis was that the 1-year OS rate with the combination would be no higher than 46% based on the historical data from pembrolizumab and nivolumab monotherapy (24, 27, 28). Forty-three evaluate patients were enrolled, to achieve 90% power to reject the null hypothesis and conclude the true 1-year OS rate was higher than 46% if the true rate was 46% or higher at α=0.05, using the one-sample log-rank test assuming an exponential distribution. To be considered evaluable, patients must have completed the lead-in period and have received the Cycle 1 Day 1 doses of cetuximab and nivolumab. The exploratory objectives were to identify potential biomarkers related to response to concurrent cetuximab and nivolumab in patients with R/M HNSCC.
For the combined analyses of Cohorts A and B, the clinical features of interest were summarized using descriptive statistics, including median and interquartile range for continuous variables, and proportions and frequencies for categorical variables. In general, Kruskal-Wallis tests for continuous variables and chi-squared tests for categorical variables were conducted to compare the differences among the multiple groups. For 2 × 2 tables, the Barnard unconditional test was applied. The Kaplan-Meier method was used for the PFS and OS analyses, and log-rank tests were adopted to compare survival differences between groups. The univariate Cox proportional hazards model was conducted to evaluate the association of OS with the sequential treatment and individual clinical features. All statistical analyses were performed using SAS (version 9.4, SAS Institute Inc., Cary, NC) or the R 3.6.0 software (https://www.R-project.org).
Data Availability Statement
Data were generated by the authors and included in the article.
RESULTS
Patient Characteristics
A total of 116 patients were screened, and 95 patients were enrolled between December 2017 and September 2020 to the phase II clinical trial assessing the combination of cetuximab and nivolumab (Figure 1). Eighty-eight of 95 patients were evaluable for OS; the other 7 patients did not receive at least one dose of combination cetuximab and nivolumab after lead-in cetuximab (Figure 1). The median follow-up time was 15.9 months [95% confidence interval (CI), 12.2-18.8]. The patient characteristics are detailed in Table 1.
Table 1.
Patient characteristics
| Variables | Cohort A N=45 (%)# |
Cohort B N=43 (%) |
p- value |
|
|---|---|---|---|---|
| Age * | Median | 64.0 (57.0 – 68.0) | 61.0 (56.5 – 68.5) | 0.70 |
| Gender | Male | 37 (82) | 28 (65) | 0.11 |
| Female | 8 (18) | 15 (35) | ||
| Race | White | 40 (89) | 37 (86) | 0.89 |
| Black | 3 (7) | 3 (7) | ||
| Other | 2 (4) | 3 (7) | ||
| ECOG | 0 | 9 (20) | 19 (44) | 0.03 |
| 1 | 33 (73) | 20 (47) | ||
| 2 | 3 (7) | 4 (9) | ||
| Smoking History | Yes | 33 (73) | 27 (63) | 0.41 |
| No | 12 (27) | 16 (37) | ||
| Primary Site | Oral Cavity | 10 (22) | 17 (40) | 0.53 |
| Oropharynx (OP) | 24 (53) | 17 (40) | ||
| Larynx | 6 (13) | 6 (14) | ||
| Hypopharynx | 3 (7) | 2 (5) | ||
| Unknown Primary (UP) | 2 (4) | 1 (2) | ||
| p16 IHC | OP+UP pos | 22 (49) | 14 (33) | 0.14 |
| OP neg | 4 (9) | 4 (9) | ||
| Non-OP pos | 0 (0) | 4 (9) | ||
| Non-OP neg | 19 (42) | 21 (49) | ||
| PD-L1 CPS | <1 | 7 (16) | 7 (16) | 0.84 |
| 1-19 | 13 (29) | 13 (30) | ||
| ≥20 | 19 (42) | 20 (47) | ||
| NA | 6 (13) | 3 (7) | ||
| Line of prior therapy for R/M HNSCC | 0 | 11 (24) | 43 (100) | N/A |
| 1 | 27 (60) | 0 | ||
| 2 | 5 (11) | 0 | ||
| 3 | 2 (4) | 0 |
Median and inter-quartile range is given for age
Reference (21)
N/A – not applicable
R/M HNSCC – recurrent and/or metastatic head and neck squamous cell carcinoma
Efficacy Analyses for Cohort A
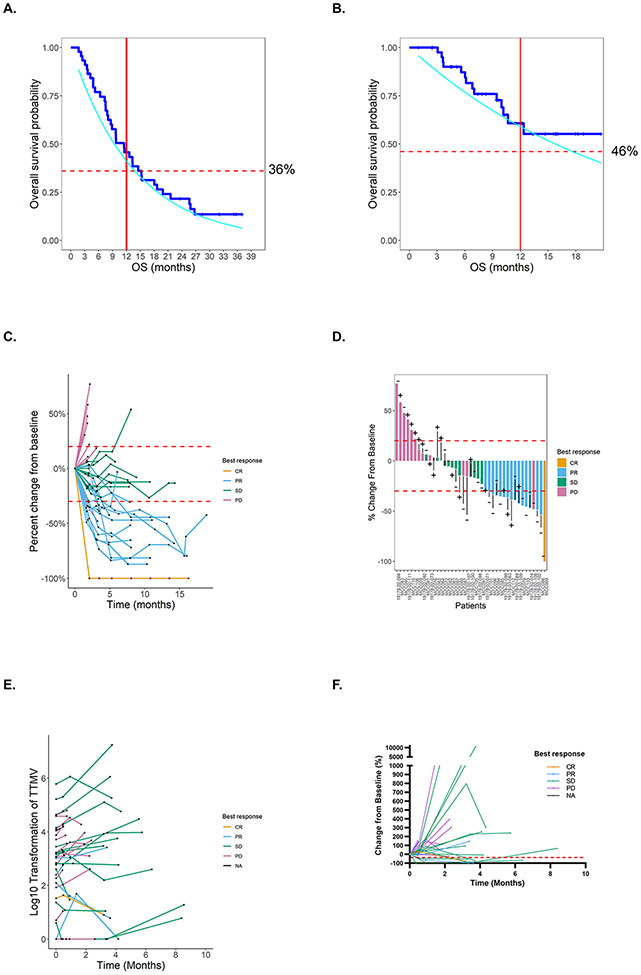
We previously reported the 1-year OS as 44% with a median follow-up for survival analysis of 21.0 months (21). Here, we report the updated survival analyses with a median follow-up of 32.1 months. The median OS was 11.4 months (90% CI 9.4-14.4 months), and the estimated OS was 50% at 12 months (90% CI 43-57%; Figure 2A). A 90% CI was used, as the lower bound is the minimum observed rate to reject the null hypothesis at a one-sided α=0.05 with a true 1-year OS of 0.36; thus, we rejected the null hypothesis for the primary endpoint of the study. We also evaluated the OS and PFS using the Kaplan-Meier method. One-year OS was 46%, and 1-year PFS was 19% (Supplemental Figure 2A and 2B). Median OS was 11.5 months, and median PFS was 3.4 months. The overall response rate (RR) was 22%, with two patients having a complete response (CR) and nine patients having a partial response (PR) in this heavily previously treated cohort. Among the responders, one of two patients with CR and three of nine patients with PR had prior exposure to a PD-1 inhibitor (21).
Figure 2.
A) One-year overall survival (OS) of 50% with a 90% confidence interval (CI, 0.59-0.71), assuming an exponential distribution in patients with prior treatment for incurable RM HNSCC and persistent or platinum-refractory R/M HNSCC (Cohort A). The red dotted line represents 1-year OS assumption of 36%, estimated based on the historical data from programmed cell death 1 (PD-1) inhibitor monotherapy. The cyan line represents the 90% lower bound. The red solid line represents the 1 year time point. B) One-year OS of 66% with a 90% confidence interval (CI, 0.59-0.71), assuming an exponential distribution in patients with no prior treatment for incurable RM HNSCC (Cohort B). The red dotted line represents 1-year OS assumption of 46%, estimated based on the historical data from PD-1 inhibitor monotherapy. The cyan line represents the 90% lower bound. The red solid line represents the 1 year time point. C) Spider plot to illustrate the best response by percent changes in tumor measures over time (Cohort B): CR - complete response, PR - partial response, SD – stable disease, and PD – progressive disease. D) Waterfall plot to illustrate the best response by percent changes in tumor measurement in each patient (Cohort B): “+” - p16-positive HNSCC. “−“ - p16-negative HNSCC. Top 7 patients with the deeper responses are p16-negative HNSCC. E) Spider plot to illustrate the baseline and subsequent changes in the tumor-tissue-modified human papillomavirus (TTMV) DNA levels in p16-positive patients (Cohort A and B): N=105 plasma samples from 36 p16-positive patients. F) Spider plot to illustrate percent changes in TTMV DNA levels in 34 p16-positive patients with available baseline TTMV DNA measurement (Cohort A and B). The best response was determined by the RECIST criteria.
Efficacy Analyses for Cohort B
For the patients enrolled in Cohort B, the median OS was 20.2 months (90% CI 15.7-24.7 months). The estimated OS was 66% at 12 months (90% CI 58-71%; Figure 2B). A 90% CI was used, as the lower bound is the minimum observed rate to reject the null hypothesis at a one-sided α=0.05 with a true 1-year OS of 0.46; thus, we rejected the null hypothesis for the primary endpoint of the study. Using the Kaplan-Meier method, The one-year OS was 61%, and 1-year PFS was 43% (Supplemental Figure 2C and 2D). The median OS was not reached at the time of analyses, and the median PFS was 6.15 months. The PFS and OS evaluation based on the p16 status (Supplemental Figure 2E and 2F) and PD-L1 CPS (Supplemental Figure 2G and 2H) did not show a statistically significant difference.
Of the 43 patients in Cohort B, 42 (98%) patients were evaluated for response assessment while one (2%) patient did not have any response assessment imaging studies. The overall response rate (RR) was 37% (16/43), including complete or partial responses (Figure 2C and 2D). Complete toxicity data of Cohort B are detailed in Table 2 and Supplementary Table 1. The only grade 3 or higher treatment-related adverse events (TRAEs), occurring in ≥2 patients, were hypophosphatemia 2/43 (5%), skin and nail-related 6/43 (14%), and hypomagnesemia 2/43 (5%). Hypomagnesemia was the only grade 4 TRAE (2%). The only grade 3 immune-related adverse event (IRAE) occurring in ≥2 patients was fatigue 2/43 (5%). No grade 4 IRAEs were observed.
Table 2.
Summary of Grade 3 or 4 Toxicities in Cohort B (N=43)
| TREATMENT-RELATED TOXICITIES | GRADE 3 | GRADE 4 | TOTAL |
|---|---|---|---|
| Rash acneiform* | 4 (9) | - | 4 (9) |
| Hypomagnesemia | 1 (2) | 1 (2) | 2 (5) |
| Paronychia* | 1 (2) | - | 1 (2) |
| Fatigue | 1 (2) | - | 1 (2) |
| Diarrhea | 1 (2) | - | 1 (2) |
| Hypophosphatemia | 2 (5) | - | 2(5) |
| Hypokalemia | 1 (2) | - | 1 (2) |
| Lymphocyte count decreased | 1 (2) | - | 1 (2)) |
| Rash maculo-papular* | 1 (2) | - | 1 (2) |
| Nausea | 1 (2) | - | 1 (2) |
| Alanine aminotransferase increased | 1 (2) | - | 1 (2) |
| Aspartate aminotransferase increased | 1 (2) | - | 1 (2) |
| Colitis | 1 (2) | - | 1 (2) |
| Musculoskeletal and connective tissue disorder - Other, specify | 1 (2) | - | 2 (5) |
| Vascular disorders - Other, specify | 1 (2) | - | 1 (2) |
| Overall | 9 (21) | 1 (2) | 42 (98) |
| IMMUNE-RELATED TOXICITIES | GRADE 3 | GRADE 4 | TOTAL |
| Fatigue | 2 (5) | - | 2 (5) |
| Alanine aminotransferase increased | 1 (2) | - | 1 (2) |
| Hypophosphatemia | 1 (2) | - | 1 (2) |
| Aspartate aminotransferase increased | 1 (2) | - | 1 (2) |
| Rash maculo-papular* | 1 (2) | - | 1 (2) |
| Vascular disorders - Other, specify | 1 (2) | - | 1 (2) |
| Overall | 4 (9) | 0 (0.0) | 15 (35) |
Skin and nail-related toxicities
Efficacy Analyses based on p16 and PD-L1 IHC
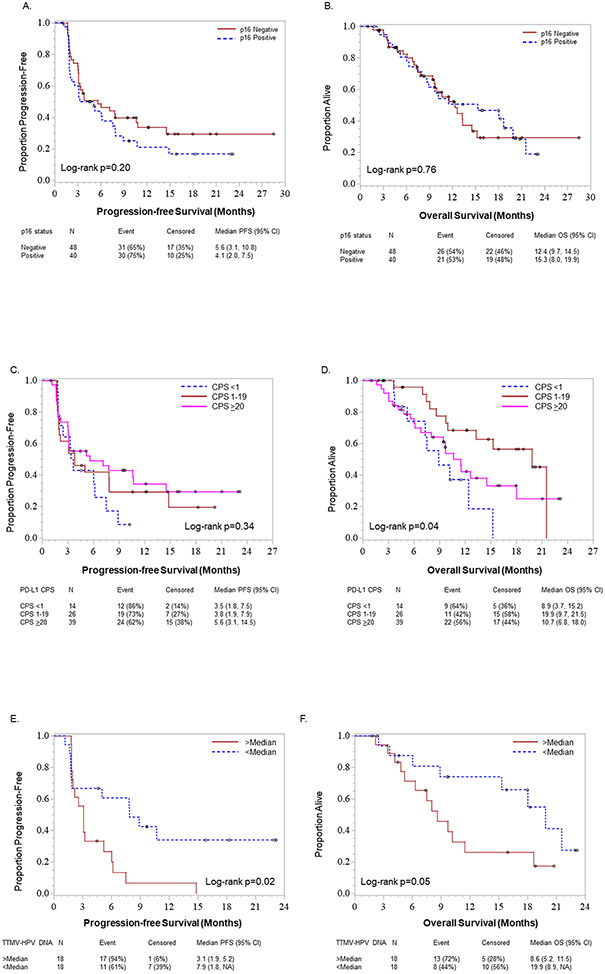
We evaluated data from both Cohorts A and B in the secondary biomarker analyses including p16 (N=88) and PD-L1 IHC (N=79). The patient characteristics based on these biomarkers are detailed in Supplementary Table 2 and Supplementary Table 3. The p16 IHC were positive in 40 (45%) and negative in 48 (55%). The PD-L1 CPS were ≥20 in 39 (49%), 1-19 in 26 (33%), <1 in 14 (18%) of 79 patients, as there were insufficient numbers of tumor cells in 9 patients. The detailed overall response rate (RR) assessments based on these biomarkers are described in Table 3. The RR was statistically signifcantly higher in p16-negative patients compared to p16-positive patients (p=0.02, unconditional test). The RR was also higher in PD-L1 CPS ≥20 and 1-19 compared to CPS <1, with statistical significance (p=0.03, CMH test). There were no statistically significant differences in the RR among patients who had prior cetuximab or immunotherapy exposure or platinum-resistant HNSCC (defined as relapse within 6 months of platinum containing curative therapy). The PFS and OS plots based on the p16 IHC status did not show a statistically significant difference (Figure 3A and 3B). The PFS based on the PD-L1 CPS status also did not show a statistically significant difference (Figure 3C). However, patients with PD-L1 CPS 1-19 had the longest median OS of 19.9 months, compared to CPS <1 with 8.9 months, and compared to CPS ≥20 with 10.7 months (log-rank p-value = 0.04, Figure 3D). No statistically significant differences were found when evaluating PFS and OS using both p16 status and PD-L1 CPS (Supplementary Figure 3A and 3B).
Table 3.
Response rate assessment
| Cohort | CR/PR | SD/PD | p- value# |
||
|---|---|---|---|---|---|
| Cohort B | p16 IHC N=42 (%) | Positive (N=18) | 5 (28) | 13 (72) | 0.27 |
| Negative (N=24) | 11 (46) | 13 (54) | |||
| PD-L1 IHC N=39 (%) | CPS < 1 (N=7) | 1 (14) | 6 (86) | 0.32 | |
| CPS 1-19 (N=13) | 5 (39) | 8 (62) | |||
| CPS >= 1 (N=19) | 9 (47) | 10 (53) | |||
| Cohort A + B | p16 IHC N=85 (%) | Positive (N=39) | 7 (18) | 32 (82) | 0.02 |
| Negative (N=46) | 19 (41) | 27 (59) | |||
| PD-L1 IHC N=76 (%) | CPS < 1 (N=14) | 1 (7) | 13 (93) | 0.03 | |
| CPS 1-19 (N=26) | 7 (27) | 19 (73) | |||
| CPS >=20 (N=36) | 16 (44) | 20 (56) | |||
| Prior cetuximab or immunotherapy exposure* N=85 (%) | Yes (N=29) | 6 (21) | 23 (79) | 0.16 | |
| No (N=56) | 20 (36) | 36 (64) | |||
| Platinum resistant disease+ N=85 (%) | Yes (N=12) | 5 (42) | 7 (58) | 0.46 | |
| No (N=73) | 21 (29) | 52 (71) | |||
| TTMV DNA in plasma N=35 (%) | > median (high, N=17) | 0 (0) | 17 (100) | 0.01 | |
| < median (low, N=18) | 6 (33) | 12 (67) |
CR: completed response, PR: partial response, SD: stable disease, PD: progressive disease, IHC: immunohistochemical staining, PD-L1: Programmed cell death ligand 1, CPS: combined positive score, TTMV: tumor-tissue-modified human papillomavirus.
Exclude cetuximab given with radiation
Relapse within 6 months of platinum containing curative therapy
p value is derived from the Barnard unconditional test for 2 × 2 tables, and CMH test otherwise.
Figure 3.
Survival analyses of patients in both Cohort A and B based on biomarkers. A) Progression-free survival (PFS) and B) Overall survival (OS) comparison between p16-positive and p16-negative patients (N=88). C) PFS and D) OS comparison between patients with programed cell death ligand 1 (PD-L1) combined positive score (CPS) <1, 1-19, and ≥20 (N=79). E) PFS and F) OS comparison between >median and <median 1,230 copies/mL of TTMV DNA in p16-positive patients (N=36).
Efficacy Analyses based on TTMV DNA
For the exploratory analysis of TTMV DNA, 105 plasma samples were available from 37 of 40 (93%) p16-positive patients from Cohorts A and B, although one patient did not have a pre-treatment plasma sample and was thus excluded. All extracted DNA samples passed the quality assurance analysis. The patient characteristics based on these biomarkers are detailed in Supplementary Table 4. Two patients had undetectable TTMV DNA at all time points, one with a larynx SCC and the other with an oropharyngeal SCC. Two patients had undetectable TTMV DNA in the pre-treatment samples, but at least one subsequent sample had detectable levels. The median TTMV DNA was 1,230 copies/mL (range 0-2,850 copies/mL). Among the patients with detectable TTMV DNA at any time point (N=34), HPV strains could be determined in 33 (32 with HPV 16 and one with HPV 18) patients. One patient had indeterminant HPV 16/18/31/33/35, but the TTMV DNA levels were very low (pre-treatment, 3 copies/mL and end of treatment, 5 copies/mL) or undetectable (after lead-in cetuximab, 0 copies/mL and before Cycle 4 Day 1, 0 copies/mL).
Detailed response rate assessments based on the TTMV DNA levels are described in Figure 2E and 2F. When 35 patients with pre-treatment TTMV DNA were evaluated, the RR was higher in patients below the median 1,230 copies/mL compared to those above the median, with a statistical significance (p=0.01, unconditional test; Table 3). Patients with circulating TTMV DNA levels less than the median at baseline had longer median PFS and median OS times (7.9 months and 19.9 months, respectively) compared to patients with TTMV DNA levels higher than the median (3.1 months and 8.6 months, respectively). These differences in PFS and OS were statistically significant (log-rank p=0.02 and p=0.05, respectively; Figure 3E and 3F). In addition, as an exploratory analysis, we evaluated PFS and OS using both TTMV DNA levels and PD-L1 CPS (Supplementary Figure 3C and 3D). There was no statistically significant difference in PFS. However, OS was significanly better in groups; TTMV lower than median and PD-L1 CPS 1-19/CPS ≥20 and TTMV higher than median with PD-L1 CPS 1-19 (log-rank p-value =0.016).
DISCUSSION
In our study, the 1-year OS was 50% in patients with prior exposure to systemic therapy and persistent or platinum-refractory R/M HNSCC and 66% in patients with no prior exposure to systemic therapy for R/M HNSCC treated with combination cetuximab and nivolumab. The safety profile was favorable. Our data suggests that p16-negative patients have comparable OS to p16-positive patients, when previous studies showed that p16-positive patients have overall better prognosis than p16-negative patients with both newly diagnosed and R/M HNSCC (6, 29, 30). The response rate was statistically higher in p16-negative patients than in p16-positive patients.
In a study by Ferris, et al. which studied a similar population with Cohort A, the ORR was 13.3%, and the 1-year OS given nivolumab monotherapy was 36% with median OS of 7.5 months (24). In Cohort A of our study which included patients who failed prior PD-1 inhibitor therapies, the ORR was 22%, and the 1-year OS was 50% with median OS of 11.4 months. In the KeyNote 048 trial which studied the first line R/M HNSCC, the ORR was 17%, and the 1-year OS given pembrolizumab monotherapy was 49% with median OS of 11.5 months in total population with any PD-L1 CPS (12). In the same study for patients treated with combination of pembrolizumab and chemotherapy, the ORR was 36%, and the 1-year OS was 53% with median OS of 13.0 months in total population with any PD-L1 CPS (12). In Cohort B of our study, the ORR was 37%, and the 1-year OS was 61% using the Kaplan-Meier method as in the KeyNote 048. The median OS was not reached at the time of analyses. Even in the selected patients with PD-L1 CPS ≥1 in the KeyNote 048 trial, the 1-year PFS was 20%, and the 1-year OS was 51% with pembrolizumab monotherapy (12). In our study, the 1-year PFS was 45% and the 1-year OS was 58% in patients with PD-L1 CPS ≥1. Our study supports a strong rationale for a larger randomized study.
Our efficacy data are consistent with published results by Sacco, et al. based on the combination of pembrolizumab 200 mg IV every 3 weeks and cetuximab initial loading dose 400 mg/m2 IV followed by 250 mg/m2 IV weekly in each 21-day cycle in R/M HNSCC patients who had no prior exposure to immunotherapy or EGFR inhibition (31). The primary endpoint of that study was overall response rate (ORR) at 6 months. The total sample size was 33 patients with a follow-up time of 7.3 months, and ORR at 6 months was 45%. The median PFS was 6.5 months, and the median OS was 18.4 months. In our study, the 6-month ORR was 23% in Cohort A and 36% in Cohort B. However, we recognized that their study also included platinum-resistant or platinum-ineligible R/M HNSCC. In our study, this population was in Cohort A. Therefore, we combined the 11 patients who failed platinum and enrolled as the first line therapy from Cohort A and 43 patients in Cohort B. Among the 54 patients, 52 were evaluable for response assessment. The 6-month ORR was 37%, the median PFS was 7.8 months, and the median OS was 14.5 months. The differences in the ORR and survival between these studies could be from differences in the clinical characteristics of the study population and the different dosing schedule of cetuximab.
In terms of the toxicities, the combination regimen was very well tolerated. In the first reported study of cetuximab monotherapy in R/M HNSCC by Vermorken, et al. (20), characteristic cetuximab-related toxicities were described in detail including rash (49% for all grades and 1% for grade 3-4) and acne (26% for all grades with no grade 3-4) while hypomagnesemia was not reported. In a more recent study by Adkins, et al. (32), 53% had all grade rash, and 11.7% had all grade hypomagnesemia while none were grade 3-4, in patients treated with cetuximab and placebo. In our study, 84% had rash of all grades including 9% grade 3, and 47% had hypomagnesemia of all grade including 2% grade 3. Furthermore, in Sacco, et al. (31), the most common grade 3-4 TRAE to be oral mucositis (3/33 patients, 9%). We observed 3/45 (7%) grade 1 and 1/45 (2%) grade 2 oral mucositis in Cohort A (21) and 2/43 (5%) grade 1 and 2/43 (5%) grade 2 in Cohort B (Supplementary Table 1). We did not observe any grade 3-4 oral mucositis in both cohorts. However, in Sacco, et al., the grade 3 skin and nail-related toxicity including acneiform rash was only 2/33 (6%). Our study had a numerically higher rate of grade 3 skin and nail-related toxicities with 4/45 (9%) in Cohort A and 6/43 (14%) in Cohort B. Immune-related adverse events included PD-1 inhibitor related grade 3 maculo-papular rash in 1/45 (2%) in Cohort A and in 1/43 (2%) in Cohort B while Sacco, et al did not report IRAE separately. The difference could be from a higher dose of cetuximab 500 mg/m2 given every 2 weeks in our study instead of cetuximab 250 mg/m2 given every week in all previous studies as above. In addition, a significant portion of our patients had prior exposure to cetuximab before enrolling on our study. Compared to the Sacco, et al. study, our study had a much longer follow up potentially allowing cumulative toxicities of cetuximab.
Cetuximab has been extensively studied in both newly diagnosed and R/M HNSCC (10, 18, 19, 33-37). In newly diagnosed HNSCC patients, cetuximab added to concurrent cisplatin and radiation did not show significant survival benefit. Cetuximab was also evaluated for treatment de-intensification compared to cisplatin given concurrently with radiation in p16-positive oropharynx cancer patients but was inferior to cisplatin, without a significantly favorable safety profile compared to cisplatin. However, cetuximab may be more effective in p16-negative R/M HNSCC. When ficlatuzumab and cetuximab combination therapy was evaluated as a part of randomized phase II trial in pan-refractory, advanced HNSCC, the ORR was 19%, and only p16-negative patients had a response suggesting that cetuximab may have a preferential efficacy in HPV-negative patients (38). While our study is unable to answer whether there is a clear synergy between cetuximab and PD-1 inhibitors, considering that it is a single-arm study, it supported a preferential activity of this regimen in p16-negative HNSCC.
It is intriguing to see the longest median OS of 19.9 months in the patients with PD-L1 CPS 1-19 compared to the CPS <1 or CPS ≥20. We considered an imbalance in the clinical characteristics among these 3 groups but did not find any significant characteristics (Supplementary Table 3). We also examined a potential imbalance in patients who presented with distant metastatic disease at diagnosis and received no prior systemic therapy. There were only four patients in this category and received the cetuximab and nivolumab combination as the first line therapy. Two patients had PD-L1 CPS ≥20, one patient had CPS 1-19, and one patient did not have any sufficient tumor to determine the score. The potential biological mechanisms mediating these differences are unknown. CPS represents the ratio between the number of PD-L1 positive cells (tumor, lymphocytes, and macrophages) in relation to the total number of viable tumor cells multiplied by 100. Thus, a simple model can be proposed that can explain the longer PFS and OS in patients with higher CPS. However, this model fails to explain the CPS ≥20 group, as their OS is shorter than in the CPS 1-19 group, as one would expect that a higher CPS would correlate with a longer OS (12). One possible explanation would be that the tumors in the CPS 1-19 group are the ones benefiting from inhibition of the EGFR pathway as the result of subsequent TME remodeling mediated by cetuximab-mediated NK activation, tumor ADCC, antigen cross-presentation, and T cell activation (14, 39). In contrast, cetuximab-induced changes of the immune contexture within the TME in the CPS ≥20 group may be characterized by the immune dampening suppressive cells, such as Tregs and/or MDSC (40). The median OS of pembrolizumab monotherapy and pembrolizumab and chemotherapy combination in the first line R/M HNSCC with any PD-L1 CPS were only 11.5 months and 13 months, respectively (12). The median OS of 19.9 months in the CPS 1-19 group is very promising with a caveat that it is a small subset analysis.
Our data regarding the circulating TTMV DNA levels obtained from cell free DNA extracted from the plasma are also intriguing. Assessing the response to immunotherapies based on the RECIST is known to be challenging with the concern of pseudo-progression (41). The longer PFS and OS in patients with <median TTMV DNA levels at baseline compared to >median are difficult to explain. While it would make an intuitive sense that the higher levels simply reflect higher tumor burdens in our R/M HNSCC patients, the current data in newly diagnosed patients by Chera, et al. suggest that the tumor burden alone does not fully explain the circulating TTMV DNA levels at baseline and the episomal versus integrated HPV genome in the tumors may influence the circulating TTMV DNA levels at baseline (25). However, the potential benefit of this biomarker may be greater in response assessment and surveillance by evaluating the changes over time as an adaptive biomarker demonstrated by patients with no evidence of disease having undetectable TTMV DNA after the definitive treatments when the TTMV DNA was detectable at baseline (26). While our data is preliminary, it warrants further evaluation of the circulating TTMV DNA as a potential surveillance tool. In addition, it may be useful to determine HPV strains in patients without archived tumors for HPV genotyping rather than conducting an invasive biopsy, as there are rapidly increasing developments in HPV-strain specific novel therapeutics such as an HPV16 vaccine.
In summary, our data suggest that the combination of cetuximab and nivolumab is a promising regimen, with significant anti-tumor activity and acceptable toxicity profile in patients with and without prior treatment for incurable R/M HNSCC. Our correlative studies also suggest that p16-negative patients have similar OS and a higher response rate compared to p16-positive patients given the combination.
Supplementary Material
STATEMENT OF TRANSLATIONAL RELEVANCE.
While programmed cell death 1 (PD-1) inhibitors are efficacious in head and neck squamous cell carcinoma (HNSCC), only a limited number of patients gain clinical benefit. To improve the outcomes, we conducted a phase II multi-institutional clinical trial to determine overall survival (OS) in patients with recurrent and/or metastatic (R/M) HNSCC treated with a combination of cetuximab and nivolumab. In addition, to gain insight regarding which patients would benefit the most from the combination therapy, we evaluated the outcomes based on p16 status, PD-Ligand 1 (PD-L1) combined positive score (CPS), and circulating tumor-tissue-modified human papillomavirus (TTMV) DNA copy number. Our data suggest that the combination is safe and effective in patients with previously treated and untreated R/M HNSCC. These findings need further evaluation.
ACKNOWLEDGEMENTS
This work has been supported in part by the James and Esther King Biomedical Research Grant (7JK02; C. Chung). Lilly Oncology provided the clinical trial funding and cetuximab. Bristol-Myers Squibb provided nivolumab. It is also supported in part by the Moffitt’s Biostatistics and Bioinformatics and Tissue Core Facilities at the H. Lee Moffitt Cancer Center & Research Institute, an NCI-designated Comprehensive Cancer Center (P30-CA076292). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Grant Sponsor or the H. Lee Moffitt Cancer Center & Research Institute. We appreciate the staffs at the Moffitt Tissue Core, Biostatistics Shared Resource, and Clinical Trials Office for their support in tissue collection and processing.
Footnotes
Conflict of interest: CHC - honoraria from Bristol-Myers Squibb, CUE, Sanofi, Mirati, Merck, Brooklyn ImmunoTherapuetics, and Exelixis for ad hoc Scientific Advisory Board participation. CS - honoraria from Armo, Bergen Bio, Abbvie, and Lilly Oncology for ad hoc Scientific Advisory Board participation. NFS - honoraria from Pfizer, Merck, Aduro, Rakuten, CUE, and Blupoint for ad hoc Scientific Advisory Board or Data Safety Monitoring Committee and research funding Bristol-Myers Squibb and Exelixis. SK, CK, and PJS are employees of Naveris Inc. and stockholders. The other authors do not have conflict of interest to declare.
REFERENCES
- 1.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71:7–33. [DOI] [PubMed] [Google Scholar]
- 2.Gillison ML, Zhang Q, Jordan R, Xiao W, Westra WH, Trotti A, et al. Tobacco smoking and increased risk of death and progression for patients with p16-positive and p16-negative oropharyngeal cancer. J Clin Oncol. 2012;30:2102–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maier H, Dietz A, Gewelke U, Heller WD, Weidauer H. Tobacco and alcohol and the risk of head and neck cancer. Clin Investig. 1992;70:320–7. [DOI] [PubMed] [Google Scholar]
- 4.Gillison ML, D'Souza G, Westra W, Sugar E, Xiao W, Begum S, et al. Distinct risk factor profiles for human papillomavirus type 16-positive and human papillomavirus type 16-negative head and neck cancers. J Natl Cancer Inst. 2008;100:407–20. [DOI] [PubMed] [Google Scholar]
- 5.D'Souza G, Kreimer AR, Viscidi R, Pawlita M, Fakhry C, Koch WM, et al. Case-control study of human papillomavirus and oropharyngeal cancer. N Engl J Med. 2007;356:1944–56. [DOI] [PubMed] [Google Scholar]
- 6.Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tan PF, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363:24–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chaturvedi AK, Engels EA, Anderson WF, Gillison ML. Incidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United States. J Clin Oncol. 2008;26:612–9. [DOI] [PubMed] [Google Scholar]
- 8.Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011;29:4294–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rischin D, Young RJ, Fisher R, Fox SB, Le QT, Peters LJ, et al. Prognostic significance of p16INK4A and human papillomavirus in patients with oropharyngeal cancer treated on TROG 02.02 phase III trial. J Clin Oncol. 2010;28:4142–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gillison ML, Trotti AM, Harris J, Eisbruch A, Harari PM, Adelstein DJ, et al. Radiotherapy plus cetuximab or cisplatin in human papillomavirus-positive oropharyngeal cancer (NRG Oncology RTOG 1016): a randomised, multicentre, non-inferiority trial. Lancet. 2019;393:40–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mehanna H, Robinson M, Hartley A, Kong A, Foran B, Fulton-Lieuw T, et al. Radiotherapy plus cisplatin or cetuximab in low-risk human papillomavirus-positive oropharyngeal cancer (De-ESCALaTE HPV): an open-label randomised controlled phase 3 trial. Lancet. 2019;393:51–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burtness B, Harrington KJ, Greil R, Soulieres D, Tahara M, de Castro G Jr., et al. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet. 2019;394:1915–28. [DOI] [PubMed] [Google Scholar]
- 13.Ferris RL, Haddad R, Even C, Tahara M, Dvorkin M, Ciuleanu TE, et al. Durvalumab with or without tremelimumab in patients with recurrent or metastatic head and neck squamous cell carcinoma: EAGLE, a randomized, open-label phase III study. Ann Oncol. 2020;31:942–50. [DOI] [PubMed] [Google Scholar]
- 14.Ferris RL, Lenz HJ, Trotta AM, Garcia-Foncillas J, Schulten J, Audhuy F, et al. Rationale for combination of therapeutic antibodies targeting tumor cells and immune checkpoint receptors: Harnessing innate and adaptive immunity through IgG1 isotype immune effector stimulation. Cancer Treat Rev. 2018;63:48–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chow LQM, Morishima C, Eaton KD, Baik CS, Goulart BH, Anderson LN, et al. Phase Ib Trial of the Toll-like Receptor 8 Agonist, Motolimod (VTX-2337), Combined with Cetuximab in Patients with Recurrent or Metastatic SCCHN. Clin Cancer Res. 2017;23:2442–50. [DOI] [PubMed] [Google Scholar]
- 16.Trotta AM, Ottaiano A, Romano C, Nasti G, Nappi A, De Divitiis C, et al. Prospective Evaluation of Cetuximab-Mediated Antibody-Dependent Cell Cytotoxicity in Metastatic Colorectal Cancer Patients Predicts Treatment Efficacy. Cancer Immunol Res. 2016;4:366–74. [DOI] [PubMed] [Google Scholar]
- 17.Cohen EEW, Soulieres D, Le Tourneau C, Dinis J, Licitra L, Ahn MJ, et al. Pembrolizumab versus methotrexate, docetaxel, or cetuximab for recurrent or metastatic head-and-neck squamous cell carcinoma (KEYNOTE-040): a randomised, open-label, phase 3 study. Lancet. 2019;393:156–67. [DOI] [PubMed] [Google Scholar]
- 18.Bonner JA, Harari PM, Giralt J, Azarnia N, Shin DM, Cohen RB, et al. Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. N Engl J Med. 2006;354:567–78. [DOI] [PubMed] [Google Scholar]
- 19.Vermorken JB, Mesia R, Rivera F, Remenar E, Kawecki A, Rottey S, et al. Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med. 2008;359:1116–27. [DOI] [PubMed] [Google Scholar]
- 20.Vermorken JB, Trigo J, Hitt R, Koralewski P, Diaz-Rubio E, Rolland F, et al. Open-label, uncontrolled, multicenter phase II study to evaluate the efficacy and toxicity of cetuximab as a single agent in patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck who failed to respond to platinum-based therapy. J Clin Oncol. 2007;25:2171–7. [DOI] [PubMed] [Google Scholar]
- 21.Chung CH, Bonomi M, Steuer CE, Li J, Bhateja P, Johnson M, et al. Concurrent Cetuximab and Nivolumab as a Second-Line or beyond Treatment of Patients with Recurrent and/or Metastatic Head and Neck Squamous Cell Carcinoma: Results of Phase I/II Study. Cancers. 2021;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chung CH, Zhang Q, Kong CS, Harris J, Fertig EJ, Harari PM, et al. p16 Protein Expression and Human Papillomavirus Status As Prognostic Biomarkers of Nonoropharyngeal Head and Neck Squamous Cell Carcinoma. J Clin Oncol. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McMullen C, Chung CH, Hernandez-Prera JC. Evolving role of human papillomavirus as a clinically significant biomarker in head and neck squamous cell carcinoma. Expert Rev Mol Diagn. 2019;19:63–70. [DOI] [PubMed] [Google Scholar]
- 24.Ferris RL, Blumenschein G Jr., Fayette J, Guigay J, Colevas AD, Licitra L, et al. Nivolumab for Recurrent Squamous-Cell Carcinoma of the Head and Neck. N Engl J Med. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chera BS, Kumar S, Beaty BT, Marron D, Jefferys S, Green R, et al. Rapid Clearance Profile of Plasma Circulating Tumor HPV Type 16 DNA during Chemoradiotherapy Correlates with Disease Control in HPV-Associated Oropharyngeal Cancer. Clin Cancer Res. 2019;25:4682–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chera BS, Kumar S, Shen C, Amdur R, Dagan R, Green R, et al. Plasma Circulating Tumor HPV DNA for the Surveillance of Cancer Recurrence in HPV-Associated Oropharyngeal Cancer. J Clin Oncol. 2020;38:1050–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Seiwert TY, Burtness B, Mehra R, Weiss J, Berger R, Eder JP, et al. Safety and clinical activity of pembrolizumab for treatment of recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-012): an open-label, multicentre, phase 1b trial. Lancet Oncol. 2016;17:956–65. [DOI] [PubMed] [Google Scholar]
- 28.Burtness B, Harrington KJ, Greil R, Soulieres D, Tahara M, de Castro G, et al. KEYNOTE-048: Phase 3 study of first-line pembrolizumab (P) for recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC). . ESMO 2018 Congress. 2018. [Google Scholar]
- 29.Fakhry C, Zhang Q, Nguyen-Tan PF, Rosenthal D, El-Naggar A, Garden AS, et al. Human Papillomavirus and Overall Survival After Progression of Oropharyngeal Squamous Cell Carcinoma. J Clin Oncol. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Galvis MM, Borges GA, Oliveira TB, Toledo IP, Castilho RM, Guerra ENS, et al. Immunotherapy improves efficacy and safety of patients with HPV positive and negative head and neck cancer: A systematic review and meta-analysis. Crit Rev Oncol Hematol. 2020;150:102966. [DOI] [PubMed] [Google Scholar]
- 31.Sacco AG, Chen R, Worden FP, Wong DJL, Adkins D, Swiecicki P, et al. Pembrolizumab plus cetuximab in patients with recurrent or metastatic head and neck squamous cell carcinoma: an open-label, multi-arm, non-randomised, multicentre, phase 2 trial. Lancet Oncol. 2021;22:883–92. [DOI] [PubMed] [Google Scholar]
- 32.Adkins DR, Lin JC, Sacco A, Ley J, Oppelt P, Vanchenko V, et al. Palbociclib and cetuximab compared with placebo and cetuximab in platinum-resistant, cetuximab-naive, human papillomavirus-unrelated recurrent or metastatic head and neck squamous cell carcinoma: A double-blind, randomized, phase 2 trial. Oral Oncol. 2021;115:105192. [DOI] [PubMed] [Google Scholar]
- 33.Ang KK, Zhang Q, Rosenthal DI, Nguyen-Tan PF, Sherman EJ, Weber RS, et al. Randomized Phase III Trial of Concurrent Accelerated Radiation Plus Cisplatin With or Without Cetuximab for Stage III to IV Head and Neck Carcinoma: RTOG 0522. J Clin Oncol. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harari PM, Harris J, Kies MS, Myers JN, Jordan RC, Gillison M, et al. Postoperative Chemoradiotherapy And Cetuximab For High-Risk Squamous Cell Carcinoma of the Head and Neck(RTOG 0234). Journal of Clinical Oncology. 2014;in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rosenthal D, Harari P, Giralt J, Bell D, Raben D, Liu J, et al. Impact of p16 status on the results of the phase III cetuximab (cet)/radiotherapy (RT). J Clin Oncol. 2014;32:suppl; abstr 6001. [Google Scholar]
- 36.Marur S, Li S, Cmelak AJ, Gillison ML, Zhao WJ, Ferris RL, et al. E1308: Phase II Trial of Induction Chemotherapy Followed by Reduced-Dose Radiation and Weekly Cetuximab in Patients With HPV-Associated Resectable Squamous Cell Carcinoma of the Oropharynx- ECOG-ACRIN Cancer Research Group. J Clin Oncol. 2016:JCO2016683300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baselga J, Trigo JM, Bourhis J, Tortochaux J, Cortes-Funes H, Hitt R, et al. Phase II multicenter study of the antiepidermal growth factor receptor monoclonal antibody cetuximab in combination with platinum-based chemotherapy in patients with platinum-refractory metastatic and/or recurrent squamous cell carcinoma of the head and neck. J Clin Oncol. 2005;23:5568–77. [DOI] [PubMed] [Google Scholar]
- 38.Bauman JE, Saba N, Roe D, Bauman JR, Kaczmar J, Bhatia A, et al. Randomized Phase II Trial of Ficlatuzumab with or without Cetuximab in Pan-Refractory, Advanced Head and Neck Squamous Cell Carcinoma (HNSCC). Journal of Clinical Oncology. 2021;39:Suppl. 6015. [DOI] [PubMed] [Google Scholar]
- 39.Yang X, Zhang X, Mortenson ED, Radkevich-Brown O, Wang Y, Fu YX. Cetuximab-mediated tumor regression depends on innate and adaptive immune responses. Mol Ther. 2013;21:91–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jie HB, Schuler PJ, Lee SC, Srivastava RM, Argiris A, Ferrone S, et al. CTLA-4(+) Regulatory T Cells Increased in Cetuximab-Treated Head and Neck Cancer Patients Suppress NK Cell Cytotoxicity and Correlate with Poor Prognosis. Cancer Res. 2015;75:2200–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lauber K, Dunn L. Immunotherapy Mythbusters in Head and Neck Cancer: The Abscopal Effect and Pseudoprogression. American Society of Clinical Oncology educational book American Society of Clinical Oncology Meeting. 2019;39:352–63. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data were generated by the authors and included in the article.