Abstract
PURPOSE:
To review students’ perceived symptom-based computer vision syndrome (CVS) and its determinants and to suggest preventive measures.
METHODS:
This cross-sectional survey was conducted in 2021 at a university in Central Saudi Arabia. The presence and severity of symptoms related to CVS were investigated. The total CVS symptom score was the outcome variable. The CVS score was correlated to participants’ demographics, visual habits when using digital devices, and knowledge about CVS. Due to skewed distribution, a nonparametric method was used for analysis.
RESULTS:
Overall, 521 students were surveyed. The prevalence of CVS based on at least one symptom was 96% (95% confidence interval 94.3–97.7). The median score was 8.0 (interquartile range 4.0–12.0). Of the 24 possible CVS scores, 42 students (8%) had scores of 18 or more (severe CVS). Being female (Mann–Whitney [MW] P < 0.001), being older (Spearman P < 0.001), refractive error (MW P < 0.001), the presence of dry eye (MW P < 0.001), using devices other than a desktop computer (KruskalWallis) P = 0.03), and more than 6 h constantly working with a device (MW P = 0.001) were correlated with a higher CVS score. Older age, female, refractive error, and using digital devices for more than 6 h were the independent and significant predictors of CVS in college students.
CONCLUSION:
Most of the students suffered from mild-to-moderate CVS symptoms. Health promotion for prevention and periodic ophthalmic consultations are recommended. Identified predictors should be the focus when implementing strategies to combat CVS in the adolescent Saudi population.
Keywords: Adolescent health, computer vision syndrome, digital devices, eye strain
Introduction
Computer vision syndrome (CVS) or digital eye strain is a combination of eye and vision problems linked to near-vision activities and resulting from prolonged use of digital devices.[1] The trend shows a rapid rise of CVS in the eye and subsequent musculoskeletal problems in the younger population.[2,3,4] Working for a longer time on digital devices, having uncorrected refractive errors, being female, having poor posture for the viewing device, and using ambient illumination are some of the known risk factors of CVS.[5,6,7]
Several studies have reviewed the extent of CVS in the adult population and professional groups at high risk.[8,9,10,11,12] However, few studies cover the adolescent population. The COVID-19 pandemic resulted in lockdown, and when educational institutions were closed and outdoor activities were minimized, exposure to digital devices increased for education, communication, and entertainment purposes.[13,14]
Our institute is in the semiurban area of the Riyadh province of Saudi Arabia.[15] During the pandemic, the university was closed, and indoor classes were canceled. Most educational activities resumed in September 2020 but with remote teaching.
We present the magnitude and determinants of students’ perceived symptom-based CVS. On this basis, we recommend strategies to minimize its impact on ocular health and improve quality of life.
Methods
The ethical and research committee of the institute approved this study. It was conducted from June 2020 to December 2020. The tenets of the Helsinki declaration were strictly followed during the various stages of the research. All students at our university were the prospective study population. They were approached and encouraged to participate in this study through their student E-mail and social media groups. Those agreeing to participate by written informed consent were included in the study. Those who declined or had incomplete responses regarding CVS symptoms were excluded.
To calculate the appropriate sample size for the survey from 25,000 students, we assumed that leading CVS symptoms would be present in 82.5% of participants.[11] To achieve a 95% CI and 5% acceptable error margin with a study design effect factor of two, we needed 440 participants. To compensate for the unevenness of the web-based participants, we added 20% to the sample. Thus, the final sample size was 528. We used OpenEpi (This is free software by Emory university, USA) software to calculate the sample size.[16]
A Google platform-based questionnaire was used with closed-ended responses. The demographic information included age, gender, and the student's department. Information on ocular health included refractive error, visual aids, dry eye history, duration of work with digital devices, purpose, position, distance, and viewing angle. There were eight questions related to CVS symptoms. The participants were to select one option from “none,” “mild,” “moderate,” and “severe.”[17] Participants were also informed about the need for medical intervention for CVS symptoms. The questions related to knowledge about CVS included an explanation of CVS and the 20-20-20 rule.
The outcome variable was the total CVS score. A response to each CVS symptom of none (0), mild (1), moderate (2), or severe (3) score was given. Thus for eight questions, the total possible maximum score was 24, and the minimum was 0. The presence of any one symptom of at least a mild nature determined the presence of CVS. Its number, percentage, and 95% confidence interval (CI) were estimated. If the CVS score sum was one to seven, we deemed it a mild grade. If the score sum was 8–16, it was graded as moderate, and for a score of 17 or more, we considered the student to have severe CVS.
The data were transferred into the spreadsheet of Statistical Package for Social Studies (SPSS 25) (IBM, NY, USA). The reliability of 521 participants’ responses to eight symptom scores was tested, and the Cronbach's alpha value was 0.839. The qualitative data were presented as numbers and percentages. The quantitative data were plotted to study distribution. For nonnormal distribution, we calculated the median and interquartile ranges. We performed the Mann–Whitney (MW) U-test to compare the outcome variables in two subgroups of an independent variable, and we estimated the P value. We estimated a KruskalWallis P value for more than two subgroups. To correlate two quantitative variables, we estimated Spearman's P value. A two-sided P < 0.05 was considered to have a statistically significant correlation. Using the step-out method, the determinants that significantly correlated to the CVS score were inserted into the linear regression model. The variables with P < 0.05 were considered the independent predictors of CVS.
Results
We surveyed 521 students. Their mean age was 21.8 (standard deviation 2.7) years. There were 293 (56.2%) males and 228 (43.8%) females. Of the participants, 167 (32.1%) students were in health-related fields, and 354 (67.9%) were in other fields. Visual aids were used by 172 (33%) students. Of those, 130 (25%) were using glasses, 4 (0.8%) were using contact lens (CL), six (1.2%) were using both glasses and CL, and 32 (6.1%) were not using any visual aids while working with the digital device. The prevalence of CVS based on at least one symptom was 96% (95% CI 94.3; 97.7).
The median CVS score of participants was 8.0 (interquartile range 4.0; 12.0). Based on the minimum and maximum possible CVS scores, the distribution of students by grade of CVS is presented in Figure 1. Only 21 (4%) students had no CVS symptoms, and 42 (8%) had severe CVS.
Figure 1.
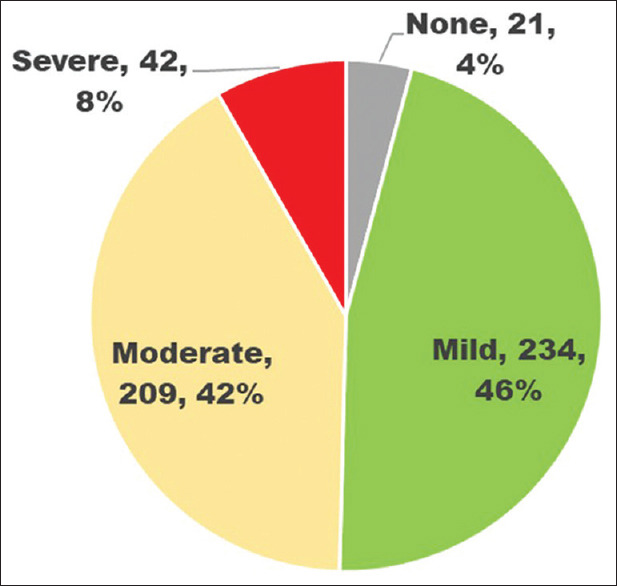
Distribution of college students by symptom based computer vision syndrome grades. None = no perceived symptom of computer vision syndrome, Mild grade = <33% of total score of participant perceived computer vision syndrome, Moderate grade = 33%–66% of the total score of participant perceived computer vision syndrome, Severe grade = more than 66% of the total score of participant perceived computer vision syndrome
The CVS score was correlated with the different determinants shown in Table 1. Being female (MW P < 0.001), age (Spearman P < 0.001), refractive error (MW P < 0.001), presence of dry eye (MW P < 0.001), devices other than desktop computers (KruskalWallis P = 0.03), and more than 6 h continuous work with a device (MW P = 0.001) correlated to a higher CVS score. On regression analysis, being younger (P = 0.039), being female (P < 0.001), having refractive errors (P < 0.001), and working for more than 6 h in front of a digital device (P = 0.042) were independent and significant predictors of CVS symptoms in college students.
Table 1.
Determinants of computer vision syndrome score among college students of central Saudi Arabia
| Number | CVS score median | IQR | Validation | |
|---|---|---|---|---|
| Total | 521 | 8.0 | 4.0-12.0 | - |
| Gender | ||||
| Male | 293 | 6.0 | 3.0-9.0 | MW U P<0.001 |
| Female | 228 | 11.0 | 6.3-14.0 | |
| Faculty | ||||
| Health | 167 | 6.0 | 3.0-9.0 | MW U P<0.001 |
| Other | 354 | 9.0 | 5.0-13.0 | |
| Refractive error | ||||
| Present | 172 | 10.0 | 6.0-13.0 | MW U P<0.001 |
| Absent | 349 | 7.0 | 4.0-11.0 | |
| Dry eye | ||||
| Yes | 134 | 12.0 | 9.0-16.0 | KW P<0.001 |
| No | 283 | 6.0 | 3.0-10.0 | |
| Don’t know | 104 | 7.0 | 5.0-12.0 | |
| Type of digital device | ||||
| Smartphone | 438 | 8.0 | 4.75-12.0 | KW P=0.03 |
| Tablet | 24 | 8.0 | 4.0-15.5 | |
| Laptop | 46 | 8.0 | 3.75-13.25 | |
| Desktop | 13 | 3.0 | 0.0-7.5 | |
| Duration of using devices per day (h) | ||||
| <6 | 223 | 7.0 | 4.0-11.0 | MW U P=0.001 |
| >6 | 296 | 8.0 | 5.0-12.0 | |
| Frequency of break from computer work (h) | ||||
| <2 | 326 | 7.0 | 4.0-12.0 | MW U P=0.16 |
| 2 or more | 195 | 8.0 | 5.0-12.0 | |
| CVS knowledge | ||||
| Yes | 38 | 6.0 | 3.0-10.0 | MW U P=0.137 |
| No | 483 | 8.0 | 4.0-10.0 | |
| 20-20 20 rule | ||||
| Yes | 84 | 7.0 | 4.0-10.0 | MW U P=0.154 |
| No | 437 | 8.0 | 4.0-12.0 | |
| Age | Spearman rho=−0.253 | P<0.001 | ||
CVS: Computer vision syndrome, IQR: Inter quartile range, KW: Kruskal-Wallis, MW: Mann-Whitney
The CVS symptoms by grade of severity as perceived by college students are presented in Figure 2. Eye strain (75.6%), neck pain (78.9%), and shoulder pain (73.7%) were leading symptoms reported by participants. Symptoms of dry eye (10.4%), neck pain (14%), and shoulder pain (15.7%) were reported as severe CVS symptoms.
Figure 2.
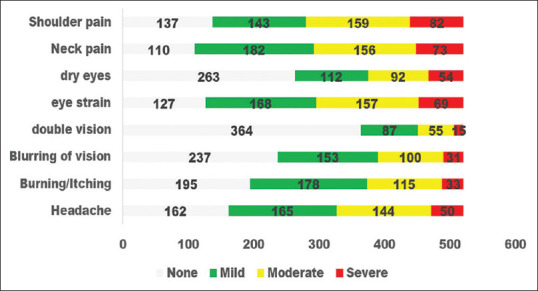
Severity of symptoms related to asthenopia and musculoskeletal fatigue among colleges students in relation to abuse of digital devices. X axis shows the number of students, Y axis shows different symptoms as perceived by participants, Gray color depicts students with no complaint, Green depicts students with mild grade of symptom, Yellow color depicts students with moderate grade of symptom, Red color depicts students with severe grade of symptom
Discussion
The extent of CVS among university students in a semiurban area of Saudi Arabia was high. One in 12 students reported severe CVS symptoms. Neck pain, shoulder pain, and eye strain were the leading complaints. Younger students, females, those with refractive errors, and those working for more than 6 h in front of digital devices had higher CVS risk. Students in health-related studies and students from other departments had a similar risk of CVS.
The present study is unique because it generated baseline information on the adolescent population's perceived symptoms of CVS in the modern era of the COVID-19 pandemic and extensive use of digital devices. Our results strongly suggest undertaking remedial measures to educate students on preventive measures, perform periodic eye check-ups, and focus more on identified risk factors. A large sample and the reliability of the tool used to generate information on CVS enable us to extrapolate the findings to the university's entire student population.
For 96% of students to have CVS is unusually high and cause for concern. In a study in western Saudi Arabia, Turkistani et al. noted a 76% prevalence of CVS; and in Riyadh, 82% of students had neck and shoulder pain, both CVS symptoms.[10,11] In India, 50% of school students had symptoms of dry eye disease (DED) in the period of intense e-learning during the COVID-19 pandemic.[13] One should be careful about comparing the CVS and DED of the Saudi population with other countries because climatic conditions vary and could influence the severity of dry eye.
Females had a significantly higher risk of CVS in our study. This has been noted in many other studies.[6,17,18] Saudi women have only recently been granted permission to drive and may now travel unescorted by a male relative.[19] However, this is slow process and most of the ladies stay indoors, use of digital devices more than males, resulting in more symptoms of CVS.
Working with digital devices for more than 6 h posed a significant risk for CVS among our students. Al Tawil et al. noted that more than 5 h of working with digital devices increases the risk of CVS by 50%.[11] Workers in information technology who work with a computer for a mean of 7.7 h had a higher risk of CVS.[20] Forgetting to blink while doing work that requires concentration, continuous convergence, and the additional load on the ocular muscle to maintain binocularity could contribute to CVS symptoms in this group.[21]
Students with refractive errors in our study had a higher risk of CVS. Although refractive error is a risk factor for eye strain in professionals working with a computer, its correction did little to reduce CVS.[22,23]
In our study, the risk of CVS was not different in medical students than in other students. This contrasts with the Riyadh, Saudi Arabia, study in which business students had a 1.6 times higher CVS risk than medical students.[11] Thus, similar e-education habits in medical students and other students could be the reason for a lack of differential CVS rate in our study.
The nation's eye health care and adolescent health programs should note that this highly prevalent ocular morbidity is an important issue and should be addressed through health promotion, early detection through screening and periodic clinical assessments, and proactive treatment of moderate and severe CVS in this young population. It will be interesting to study the awareness and practice of using digital devices of this adolescent population. Symptom-based diagnosis of CVS has been documented to be a reliable tool; however, it may be complemented by objective indicators to review individual bias in reporting symptoms.
Promotion of more outdoor activities as part of education system could be one of the strategies to address CVS. Less outdoor activities were risk factor for CVS in school children of China.[24] Restricted use of mobile, tabs and encouraging using books and desktops in school has been proposed to reduce CVS and dry eye syndrome.[22] Usage of devices to increase blinking rate have been claimed to reduce CVS and they could be tried in adolescent with severe CVS.[25] The World Health Organization is conscious and recommends member countries to adopt public health strategies to reduce excessive use of internet and related digital devices and resultant physical and mental health issues.[26]
There were few limitations of our study. The extent of CVS was symptom-based. Objective parameters should complement to subjective measurements to confirm the high prevalence noted. This being a cross-sectional study, the correlation of risk factors to CVS should be performed with caution because the lack of a special relationship could influence it. The purpose of the study sample was to assess the overall magnitude of CVS. With a large sample, however comparison of subgroups should be considered a trend and be confirmed through other longitudinal studies.
Conclusion
CVS seems to be associated with several digital devices in adolescent population. Most popular among them are smartphones. Norms to reduce adverse health effects, especially eye strain and musculoskeletal problems need to be included in health promotion through influential channels to reach this vulnerable population, and vision habits could be improved.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank the administrators as well as faculty members for their support in mobilizing the college students to participate in this study.
References
- 1.Randolph SA. Computer vision syndrome. Workplace Health Saf. 2017;65:328. doi: 10.1177/2165079917712727. [DOI] [PubMed] [Google Scholar]
- 2.Mylona I, Deres ES, Dere GS, Tsinopoulos I, Glynatsis M. The impact of internet and videogaming addiction on adolescent vision: A review of the literature. Front Public Health. 2020;8:63. doi: 10.3389/fpubh.2020.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenfield M. Computer vision syndrome (aka digital eye strain) Optometry. 2016;17:1–10. [Google Scholar]
- 4.Altalhi A, Khayyat W, Khojah O, Alsalmi M, Almarzouki H. Computer vision syndrome among health sciences students in Saudi Arabia: Prevalence and risk factors. Cureus. 2020;12:e7060. doi: 10.7759/cureus.7060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gowrisankaran S, Sheedy JE. Computer vision syndrome: A review. Work. 2015;52:303–14. doi: 10.3233/WOR-152162. [DOI] [PubMed] [Google Scholar]
- 6.Ranasinghe P, Wathurapatha WS, Perera YS, Lamabadusuriya DA, Kulatunga S, Jayawardana N, et al. Computer vision syndrome among computer office workers in a developing country: An evaluation of prevalence and risk factors. BMC Res Notes. 2016;9:150. doi: 10.1186/s13104-016-1962-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Portello JK, Rosenfield M, Bababekova Y, Estrada JM, Leon A. Computer-related visual symptoms in office workers. Ophthalmic Physiol Opt. 2012;32:375–82. doi: 10.1111/j.1475-1313.2012.00925.x. [DOI] [PubMed] [Google Scholar]
- 8.Kushali R, Brundha MP. Prevalence and awareness on computer vision syndrome among individuals in information technology. Drug Invent Today. 2020;14:416–9. [Google Scholar]
- 9.Boadi-Kusi SB, Adueming PO, Hammond FA, Antiri EO. 1 Computer vision syndrome and its associated ergonomic factors 2 among bank workers. Int J Occup Saf Ergon. 2021;28:2,1219–26. doi: 10.1080/10803548.2021.1897260. [DOI] [PubMed] [Google Scholar]
- 10.Turkistani AN, Al-Romaih A, Alrayes MM, Al Ojan A, Al-Issawi W. Computer vision syndrome among Saudi population: An evaluation of prevalence and risk factors. J Family Med Prim Care. 2021;10:2313–8. doi: 10.4103/jfmpc.jfmpc_2466_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al Tawil L, Aldokhayel S, Zeitouni L, Qadoumi T, Hussein S, Ahamed SS. Prevalence of self-reported computer vision syndrome symptoms and its associated factors among university students. Eur J Ophthalmol. 2020;30:189–95. doi: 10.1177/1120672118815110. [DOI] [PubMed] [Google Scholar]
- 12.Chawla A, Lim TC, Shikhare SN, Munk PL, Peh WC. Computer vision syndrome: Darkness under the shadow of light. Can Assoc Radiol J. 2019;70:5–9. doi: 10.1016/j.carj.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 13.Mohan A, Sen P, Shah C, Jain E, Jain S. Prevalence and risk factor assessment of digital eye strain among children using online e-learning during the COVID-19 pandemic: Digital eye strain among kids (DESK study-1) Indian J Ophthalmol. 2021;69:140–4. doi: 10.4103/ijo.IJO_2535_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alabdulkader B. Effect of digital device use during COVID-19 on digital eye strain. Clin Exp Optom. 2021;104:698–704. doi: 10.1080/08164622.2021.1878843. [DOI] [PubMed] [Google Scholar]
- 15.Prince Sattam bin Abdulaziz University. [Last accessed on 2021 Sep 17]. Available from: https:// www.psau.edu.sa/en .
- 16.Dean AG, Sullivan KM, Soe MM. OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version. [Last accessed on 2021 Sep 17; Last updated on 2013 Apr 06]. Available from: https://www.OpenEpi.com .
- 17.Abudawood GA, Ashi HM, Almarzouki NK. "Computer Vision Syndrome among Undergraduate Medical Students in King Abdulaziz University, Jeddah, Saudi Arabia". Journal of Ophthalmology. 2020;2020:7. Article ID 2789376. https://doi.org/10.1155/2020/2789376. [Google Scholar]
- 18.Mowatt L, Gordon C, Santosh AB, Jones T. Computer vision syndrome and ergonomic practices among undergraduate university students. International journal of clinical practice. 2018;72:e13035. doi: 10.1111/ijcp.13035. [DOI] [PubMed] [Google Scholar]
- 19.Krane J, Majid F. Women driving in Saudi Arabia: Ban lifted, what are the economic and health effects? Issue Brief. 2018;6:1–7. [Google Scholar]
- 20.Poudel S, Khanal SP. Magnitude and determinants of computer vision syndrome (CVS) among IT workers in Kathmandu, Nepal. Nepal J Ophthalmol. 2020;12:245–51. doi: 10.3126/nepjoph.v12i2.29387. [DOI] [PubMed] [Google Scholar]
- 21.Sheppard AL, Wolffsohn JS. Digital eye strain: Prevalence, measurement and amelioration. BMJ Open Ophthalmol. 2018;3:e000146. doi: 10.1136/bmjophth-2018-000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosenfield M. Computer vision syndrome: A review of ocular causes and potential treatments. Ophthalmic Physiol Opt. 2011;31:502–15. doi: 10.1111/j.1475-1313.2011.00834.x. [DOI] [PubMed] [Google Scholar]
- 23.Heus P, Verbeek JH, Tikka C. Optical correction of refractive error for preventing and treating eye symptoms in computer users. Cochrane Database Syst Rev. 2018;4:CD009877. doi: 10.1002/14651858.CD009877.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li R, Ying B, Qian Y, Chen D, Li X, Zhu H, et al. Prevalence of Self-Reported Symptoms of Computer Vision Syndrome and Associated Risk Factors among School Students in China during the COVID-19 Pandemic. Ophthalmic Epidemiol. 2021:1–11. doi: 10.1080/09286586.2021.1963786. [DOI] [PubMed] [Google Scholar]
- 25.Dementyev A, Holz C. DualBlink: A wearable device to continuously detect, track, and actuate blinking for alleviating dry eyes and computer vision syndrome. Proc ACM Interact Mob Wearable Ubiquitous Technol. 2017;1:1–9. [Google Scholar]
- 26.World Health Organization. Public Health Implications of Excessive Use of the Internet, Computers, Smartphones and Similar Electronic Devices: Meeting Report, Main Meeting Hall, Foundation for Promotion of Cancer Research, National Cancer Research Centre, Tokyo, Japan, 27-29 August 2014. World Health Organization. 2015. [Last accessed on 2022 Apr 04]. Available from: https://apps.who.int/iris/ handle/10665/184264 .


