Introduction
Resilience as one of the pillars of successful aging has received increasing attention from the scientific community in recent years and has become even more important post-Covid-19 pandemic where countries worldwide are trying to build individual, community and system resilience (1, 2). Successful aging was first introduced by Rowe and Kahn emphasizing on illness avoidance, high physical and mental functioning, and active life engagement (3); and subsequently expanded to include multidimensional factors such as social functioning, psychological factors and resilience (4). The fastest growing segment worldwide is above 80 years old where the numbers are expected to triple between 2020 and 2050 to 426 million (5). Age is a risk factor for chronic disease, cancer, frailty, dementia and associated with declining resilience (6). With advances in public health and medical treatment, there is widening gap between lifespan and healthspan. Health systems across the world are challenged to find effective means of reducing prevalence of disability and promote solutions to successful aging. Most of the scientific literature in the past decade has been on prevention of chronic disease, frailty, and dementia.
The term “resilience” is not new and defined as the ability to bounce back after a stressful encounter or adversity in life (6). Older adults are a heterogenous group and demonstrate variable response to stressors despite similar clinical status or chronological age possibly explained by differences at the molecular, cellular and system level. Medium and high-level resilience is prevalent in 73% of the population and identifying resilience is of utmost importance (7). The challenge lies in its measurement as while there are many resilience measurement tools (Table 1), they rely on the concept that measurements can be generalised across the population, but studies have shown that adaptations to adversity is influenced by gender, ethnicity, generation differences, cultural variation, type and intensity of stressor and outcome (8–10). Decline in resistance with aging is possibly explained by decline in homeostasis and elevated stress response, and there is no mechanism in place to predict dose-response and tipping point for adverse outcomes. In addition, a single stressor can result in multiple adverse outcomes, e.g., bedrest causing muscle wasting, delirium or multiple stressors in combination, e.g., osteoarthritis, sedatives and antihypertensives causing falls and fracture.
Table 1.
Resilience Scale
| Resilience Scale | Description |
|---|---|
| Ego Resiliency Scale (44, 45) | The ego resiliency scale was developed initially for young adults and subsequently applied to older adults. |
| The 25- and 14-item Resilience Scale (46) | Developed as a measure of resilience for adults across the life span. |
| Hardy-Gill Resilience Scale (47) | Nine questions based on most stressful life event they experienced in the past five years. |
| Dispositional Resilience Scale (48) | The DRS is a 45-item questionnaire that includes 15 commitment, 15 control, and 15 challenge items. The original DRS was modified to be appropriate for older adults |
| Connor-Davidson Resilience Scale (49) | This measure consists of 25 items, each of which is rated on a 5-point scale. |
| Brief Resilient Coping Scale (50) | Short unidimensional scale that aims to assess ability to cope with stress adaptively |
| Making it CLEAR (MiC) (51) | 34 items questionnaire which assess the “individual determinants of resilience” (IDoR) and the “environmental determinants of resilience” (EDoR). Validated in older patients discharged from hospital. |
| Multidimensional Individual and Interpersonal Resilience Measure (MIIRM) (52) | Eight-factor structure that appeared clinically relevant for measuring the multidimensional nature of resilience. |
| Resilience Scale for Adults (RSA) (53) | Self-report scale targeting adults with five scoring items that examine both the intrapersonal and interpersonal protective factors that promote adaptation to adversity. |
There is emerging evidence on the role of genetics, dysregulated immune system, insulin resistance and alterations in metabolic pathways on resilience (Figure 1) (11–13). Eissmann et al. has recently shown that 30% of older adults are cognitively intact despite meeting Alzheimer’s disease (AD) pathological criteria at autopsy (14). They demonstrated sex differences in clinical manifestation despite similar neuropathological AD burden and identified female-specific resilience locus, and numerous sex specific metabolic pathways (14). Resilience is a multifaceted and difficult construct to measure with two main categories, physical resilience and psychological (mental and/or cognitive) resilience (15, 16). Physical resilience has become a topic of interest in recent years and defined as “the ability to recover or optimize function in the face of age-related losses or disease” (17).
Figure 1.
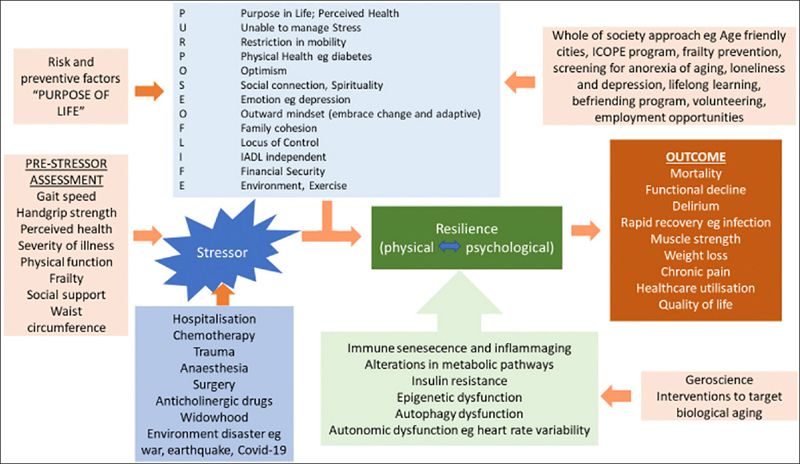
Resilience: Risk and Protective Factors, Pre-stressor Assessment, Outcomes and Possible Interventions
ICOPE: Integrated Care for Older People
Resilience is a dynamic construct with multiple risk and protective factors described with mnemonic “PURPOSE OF LIFE” listed in Figure 1. Protective factors include having a purpose in life, a better perceived health, optimism, locus of control, social connectivity, spirituality, functioning independently, exercise practice, type of environment, male sex, and age < 80 years old (18). Risk factors include difficulty managing stress, depression, mobility limitation, physical illness such as diabetes and personality disorders (7). Increasing resilience has been associated with positive mental health, quality of life, increased physical activity, improved pain threshold, better physical and rehabilitative outcomes (7).
Physical Resilience in Acute Care
Aging is a complex process with multiple interacting factors. Clinicians and surgeons dealing with older patients are often faced with difficulties in predicting adverse outcomes in older adults. Most of the work in the acute care setting has been based on frailty and not resilience. Frailty is the underlying physiologic state while resilience is the speed and process of recovery after a stress event which can have an impact on overall length of stay, healthcare resource utilisation and institutionalisation (19). Static tests of physiological reserve have been shown to be better predictors of clinical recovery compared with multidimensional (physical, psychological, social) assessments (20). Comprehensive geriatric assessment has proven to be useful in predicting outcomes in frail older adults, but it requires special skill and is resource intensive (21). Automated frailty assessment tools such as Hospital Frailty Risk Score and Rapid Geriatric Assessment with assisted management pathway requires further validation in predicting recovery in hospitalised patients exposed to different stressors (22–24). In a group of patients with hip fracture, a panel of biomarkers explained 27% of the differences in physical resilience or expected differential recovery (25). Future studies are needed to validate the correlation of various pre-stress provocative tests (physical function, cognition, psychological) (Figure 1) and biomarkers with recovery post-surgery and/or other medical illness such as infections and stroke (26).
Resilience, Frailty, and Intrinsic Capacity
Frailty, intrinsic capacity (IC) and physical resilience should be regarded as separate, but highly intertwined entities. IC and physical resilience are positive attributes while frailty is a negative attribute. IC and resilience can be applied to all stages of life course, and frailty to later stages of life (27). Frailty expresses deficit whereas resilience is the coping and/or recovery aspect (27). Frailty is a state of declining physiological reserve which increases vulnerability to adverse outcomes (19). Physical resilience can be described as ability to mobilise the reserve and can co-exist with frailty in the same older adult but to date, there are limited studies on physical resilience trajectory in frail older adult (16, 27). IC framework was first proposed by the World Health Organization (WHO) and includes cognition, vitality, mobility, psychological and sensory functions (5). IC domains have shown to predict functional recovery after exposure to adversity (28). Woo initially described IC as a determinant of physical resilience through the physiologic reserve concept and later supported by Chhetri et al. (27, 29). Although IC is only one of the determinants of physical resilience besides genetic, environment and other factors shown in Figure 1, it may be reversible with interventions (30). We need more studies to measure longitudinal impact of interventions to reverse frailty and managing declines in IC on improving physical resilience (25).
Geroscience and Resilience
The geroscience approach assumes all diseases affecting older adults are major cause of function and resilience decline possibly mediated through proinflammatory cytokines, persistent inflammation, and immune senescence (11). An intact and responsive immune system is a pre-requisite for resilience and dysregulation of the immune system is thought to mediate the adverse outcomes in older adults from acute illness, chemotherapy, post-surgery, trauma, etc (12). Aging and resilience trajectories are also determined by multiple interacting factors such as genetic, environment, exposure to microorganisms and toxins across lifespan, comorbidities, polypharmacy, and lifestyle factors such as exercise, obesity, nutrition, smoking, and stress, which also contributes to immune senescence and overall decline in immunologic capability (12). Other risk factors for aging and disease, which can have an impact on resilience, include impaired autophagy and endoplasmic reticulum stress, insulin resistance, epigenetic, autonomic, and vascular dysfunction (Figure 1), which are all interrelated, and possibly mediated through dysregulated immune system and cytokine production (11, 31). Future studies need to focus on understanding the relationship between resilience, chronic diseases at molecular level and biological aging.
Interventions
Interventions to build and/or maintain resilience needs to include whole of societal approach, multisectoral collaborations and “ensure that communities foster the abilities of older people” as described in the WHO Decade of Healthy Aging report (32). IC is one of the determinant of physical resilience, and the WHO released the “Integrated care for older people: guidelines on community-level interventions to manage declines in intrinsic capacity” in 2017 (33) and the “Handbook: Guidance on person-centred assessment and pathways in primary care” in 2019 with digital app for community level screening and intervention (34).
The WHO Global Age-Friendly Cities Project also aims to promote active aging by optimizing environment (transportation, housing, outdoor spaces and buildings), social (participation, respect and inclusion), employment, community support and health services (35). Many countries are implementing various programs at individual, community, and city level to prevent or delay decline in physiological reserve which may possibly improve resilience in longer term (36–41) (Table 2). There is currently limited literature on geroscience interventions in improving resilience outcomes.
Table 2.
Country specific programs which may help in resilience building
| USA | Age-Friendly Health System with screening for geriatric syndromes and intervention utilizing the 4M’s (“what Matters”; “Medication”; “Mentation”; and “Mobility”) (38) |
| Europe | INSPIRE ICOPE-CARE program in the Occitania region (40) |
| Hong Kong | The Integrated Health and Social Care Model with Personalised Care Plan (41) |
| Japan | “Work For Purpose” and “Second Life Platform Project” in Kashiwa City which links older adult with volunteer activities, life-long learning, hobbies, and health promotion activities (54) |
| Taiwan | Taiwan Integrated Geriatric Care (TIGER) Multidomain Intervention (55) |
| South Korea | Integrated Care of Older Patients with Frailty in Primary Care (ICOOP_Frail) (56) |
| Singapore | Peer-led Healthy Aging Promotion Program for You (39); Health District @ Queenstown (36) |
Gaps and Future Opportunities
To date, most publications on resilience are on broad concept and epidemiology without targeting specific stressors, organ systems, biological aging, and outcomes. Resilience scales need to be validated in different regions, ethnic groups, gender, specific stress, and outcome measures. There is lack of data on the role of genetic predisposition and biomarkers on resilience to specific stressors although GDF-15 shows some promising results (13, 42). We need future prospective studies on the role of geroscience interventions targeting specific biological pathways personalised to stressors and impact on desired resilience outcome. While decline or tipping point in resilience is often attributed to aging, disease and stressors such as hospitalisation, we need more data on the role of P4 medicine (prevention, predictive, personalised and participatory) in building lifelong resilience and impact of psychosocial, physical and cognitive reserve on modifying the tipping point (43). Effect of immune modulation through diet e.g. Mediterranean diet, exercise types and intensity, social interventions and pharmacologic interventions on effect of resilience requires further evaluation (12).
Conclusion
Resilience is increasingly being considered as a pillar of successful aging. Due to its contextual nature, measuring resilience has become a challenge with downstream impact on providing appropriate interventions to promote resilience. There are still significant gaps in research from a geroscience perspective and future studies need to focus on understanding the relationship between resilience, chronic diseases at molecular level, functional reserve, and biological aging.
Conflicts of interest: The authors declare no conflicts of interest for this work.
References
- 1.Yip W, Ge L, Ho AHY, Heng BH, Tan WS. Building community resilience beyond COVID-19: The Singapore way. Lancet Reg Health West Pac. 2021;7:100091. doi: 10.1016/j.lanwpc.2020.100091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Majnarić LT, Bosnić Z, Guljaš S, Vučić D, Kurevija T, Volarić M, et al. Low Psychological Resilience in Older Individuals: An Association with Increased Inflammation, Oxidative Stress and the Presence of Chronic Medical Conditions. Int J Mol Sci. 2021;22(16)10.3390/ijms221689710 [DOI] [PMC free article] [PubMed]
- 3.Rowe JW, Kahn RL. Successful Aging1. The Gerontologist. 1997;37(4):433–40. doi: 10.1093/geront/37.4.433. [DOI] [PubMed] [Google Scholar]
- 4.Bowling A. Aspirations for Older Age in the 21st Century: What is Successful Aging? The International Journal of Aging and Human Development. 2007;64(3):263–97. doi: 10.2190/L0K1-87W4-9R01-7127. [DOI] [PubMed] [Google Scholar]
- 5.WHO: Ageing and Health 2021 [Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
- 6.Hadley EC, Kuchel GA, Newman AB, Allore HG, Bartley JM, Bergeman CS, et al. Report: NIA Workshop on Measures of Physiologic Resiliencies in Human Aging. The Journals of Gerontology: Series A. 2017;72(7):980–90. doi: 10.1093/gerona/glx015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Musich S, Wang SS, Schaeffer JA, Kraemer S, Wicker E, Yeh CS. The association of increasing resilience with positive health outcomes among older adults. Geriatr Nurs. 2022;44:97–104. doi: 10.1016/j.gerinurse.2022.01.007. [DOI] [PubMed] [Google Scholar]
- 8.Cosco TD, Kaushal A, Hardy R, Richards M, Kuh D, Stafford M. Operationalising resilience in longitudinal studies: a systematic review of methodological approaches. J Epidemiol Community Health. 2017;71(1):98–104. doi: 10.1136/jech-2015-206980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hirani S, Lasiuk G, Hegadoren K. The intersection of gender and resilience. Journal of psychiatric and mental health nursing. 2016;23(6–7):455–67. doi: 10.1111/jpm.12313. [DOI] [PubMed] [Google Scholar]
- 10.Cosco TD, Kaushal A, Richards M, Kuh D, Stafford M. Resilience measurement in later life: a systematic review and psychometric analysis. Health Qual Life Outcomes. 2016;14:16. doi: 10.1186/s12955-016-0418-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrucci L, Gonzalez-Freire M, Fabbri E, Simonsick E, Tanaka T, Moore Z, et al. Measuring biological aging in humans: A quest. Aging Cell. 2020;19(2):e13080. doi: 10.1111/acel.13080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Banić M, Pleško S, Urek M, Babić Ž, Kardum D. Immunosenescence, Inflammaging and Resilience: An Evolutionary Perspective of Adaptation in the Light of COVID-19 Pandemic. Psychiatr Danub. 2021;33(Suppl 4):427–31. [PubMed] [Google Scholar]
- 13.Ryan M, Ryznar R. The Molecular Basis of Resilience: A Narrative Review. Frontiers in Psychiatry. 2022;13 10.3389/fpsyt.2022.856998 [DOI] [PMC free article] [PubMed]
- 14.Eissman JM, Dumitrescu L, Mahoney ER, Smith AN, Mukherjee S, Lee ML, et al. Sex differences in the genetic architecture of cognitive resilience to Alzheimer’s disease. Brain. 2022 10.1093/brain/awac177 [DOI] [PMC free article] [PubMed]
- 15.Windle G, Markland DA, Woods RT. Examination of a theoretical model of psychological resilience in older age. Aging Ment Health. 2008;12(3):285–92. doi: 10.1080/13607860802120763. [DOI] [PubMed] [Google Scholar]
- 16.Whitson HE, Cohen HJ, Schmader KE, Morey MC, Kuchel G, Colon-Emeric CS. Physical Resilience: Not Simply the Opposite of Frailty. Journal of the American Geriatrics Society. 2018;66(8):1459–61. doi: 10.1111/jgs.15233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whitson HE, Duan-Porter W, Schmader KE, Morey MC, Cohen HJ, Colón-Emeric CS. Physical resilience in older adults: systematic review and development of an emerging construct. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences. 2016;71(4):489–95. doi: 10.1093/gerona/glv202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rea JNM, Broczek KM, Cevenini E, Celani L, Rea SAJ, Sikora E, et al. Insights Into Sibling Relationships and Longevity From Genetics of Healthy Ageing Nonagenarians: The Importance of Optimisation, Resilience and Social Networks. Front Psychol. 2022;13:722286. doi: 10.3389/fpsyg.2022.722286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dent E, Morley JE, Cruz-Jentoft AJ, Woodhouse L, Rodriguez-Manas L, Fried LP, et al. Physical Frailty: ICFSR International Clinical Practice Guidelines for Identification and Management. J Nutr Health Aging. 2019;23(9):771–87. doi: 10.1007/s12603-019-1273-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gijzel SMW, Whitson HE, Leemput IA, Scheffer M, Asselt D, Rector JL, et al. Resilience in Clinical Care: Getting a Grip on the Recovery Potential of Older Adults. Journal of the American Geriatrics Society. 2019;67(12):2650–7. doi: 10.1111/jgs.16149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ellis G, Gardner M, Tsiachristas A, Langhorne P, Burke O, Harwood RH, et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database of Systematic Reviews. 2017;2017(9) 10.1002/14651858.cd006211.pub3 [DOI] [PMC free article] [PubMed]
- 22.Merchant RA, Hui RJY, Kwek SC, Sundram M, Tay A, Jayasundram J, et al. Rapid Geriatric Assessment Using Mobile App in Primary Care: Prevalence of Geriatric Syndromes and Review of Its Feasibility. Frontiers in Medicine. 2020;7 10.3389/fmed.2020.00261 [DOI] [PMC free article] [PubMed]
- 23.Gilbert T, Neuburger J, Kraindler J, Keeble E, Smith P, Ariti C, et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet. 2018;391(10132):1775–82. doi: 10.1016/S0140-6736(18)30668-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Merchant RA, Ho VWT, Chen MZ, Wong BLL, Lim Z, Chan YH, et al. Outcomes of Care by Geriatricians and Non-geriatricians in an Academic Hospital. Frontiers in Medicine. 2022;9 10.3389/fmed.2022.908100 [DOI] [PMC free article] [PubMed]
- 25.Parker DC, Colón-Emeric C, Huebner JL, Chou C-H, Kraus VB, Pieper CF, et al. Biomarkers Associated with Physical Resilience After Hip Fracture. The Journals of Gerontology: Series A. 2020;75(10):e166–e72. doi: 10.1093/gerona/glaa119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Whitson HE, Crabtree D, Pieper CF, Ha C, Au S, Berger M, et al. A template for physical resilience research in older adults: Methods of the PRIME-KNEE study. J Am Geriatr Soc. 2021;69(11):3232–41. doi: 10.1111/jgs.17384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Woo J. Frailty, Successful Aging, Resilience, and Intrinsic Capacity: a Cross-disciplinary Discourse of the Aging Process. Current Geriatrics Reports. 2019;8(2):67–71. doi: 10.1007/s13670-019-0276-2. [DOI] [Google Scholar]
- 28.Gijzel SMW, Rector J, van Meulen FB, van der Loeff RS, van de Leemput IA, Scheffer M, et al. Measurement of Dynamical Resilience Indicators Improves the Prediction of Recovery Following Hospitalization in Older Adults. J Am Med Dir Assoc. 2020;21(4):525–30.e4. doi: 10.1016/j.jamda.2019.10.011. [DOI] [PubMed] [Google Scholar]
- 29.Chhetri JK, Xue QL, Ma L, Chan P, Varadhan R. Intrinsic Capacity as a Determinant of Physical Resilience in Older Adults. J Nutr Health Aging. 2021;25(8):1006–11. doi: 10.1007/s12603-021-1629-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Qualls C, Waters DL, Vellas B, Villareal DT, Garry PJ, Gallini A, et al. Reversible States of Physical and/or Cognitive Dysfunction: A 9-Year Longitudinal Study. J Nutr Health Aging. 2017;21(3):271–5. doi: 10.1007/s12603-017-0878-3. [DOI] [PubMed] [Google Scholar]
- 31.Dou Y, Fatemi S, Darvas M, Gale M, Ladiges W. A geroscience approach to preventing pathologic consequences of COVID-19. Journal of Interferon & Cytokine Research. 2020;40(9):433–7. doi: 10.1089/jir.2020.29018.dou. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.WHO. Decade of healthy ageing: baseline report 2020 [Available from: https://www.who.int/publications/m/item/decade-of-healthy-ageing-plan-of-action.
- 33.WHO. Integrated care for older people: guidelines on community-level interventions to manage declines in intrinsic capacity 2017 [Available from: https://apps.who.int/iris/handle/10665/258981. [PubMed]
- 34.Organization WH . Handbook: guidance for person-centred assessment and pathways in primary care [Internet] Geneva: WHO; 2019. [Google Scholar]
- 35.WHO. Global Age-friendly Cities: A Guide [Available from: https://apps.who.int/iris/bitstream/handle/10665/43755/9789241547307_eng.pdf?sequence=1&isAllowed=y.
- 36.Pilot Health District in Queenstown to focus on residents’ holistic well-being 2021 [Available from: https://news.nus.edu.sg/pilot-health-district-in-queenstown-to-focus-on-residents-holistic-well-being/.
- 37.I Feel Young In My Singapore 2016 [Available from: https://www.moh.gov.sg/docs/librariesprovider3/action-plan/action-plan.pdf.
- 38.Lundy J, Hayden D, Pyland S, Berg-Weger M, Malmstrom TK, Morley JE. An Age-Friendly Health System. J Am Geriatr Soc. 2021;69(3):806–12. doi: 10.1111/jgs.16959. [DOI] [PubMed] [Google Scholar]
- 39.Merchant RA, Tsoi CT, Tan WM, Lau W, Sandrasageran S, Arai H. Community-Based Peer-Led Intervention for Healthy Ageing and Evaluation of the ‘HAPPY’ Program. J Nutr Health Aging. 2021;25(4):520–7. doi: 10.1007/s12603-021-1606-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tavassoli N, Piau A, Berbon C, De Kerimel J, Lafont C, De Souto Barreto P, et al. Framework Implementation of the INSPIRE ICOPE-CARE Program in Collaboration with the World Health Organization (WHO) in the Occitania Region. J Frailty Aging. 2021;10(2):103–9. doi: 10.14283/jfa.2020.26. [DOI] [PubMed] [Google Scholar]
- 41.Yu R, Tong C, Woo J. Effect of an integrated care model for pre-frail and frail older people living in community. Age and Ageing. 2020;49(6):1048–55. doi: 10.1093/ageing/afaa087. [DOI] [PubMed] [Google Scholar]
- 42.Tavenier J, Rasmussen LJH, Andersen AL, Houlind MB, Langkilde A, Andersen O, et al. Association of GDF15 With Inflammation and Physical Function During Aging and Recovery After Acute Hospitalization: A Longitudinal Study of Older Patients and Age-Matched Controls. J Gerontol A Biol Sci Med Sci. 2021;76(6):964–74. doi: 10.1093/gerona/glab011. [DOI] [PubMed] [Google Scholar]
- 43.Morley JE, Anker SD. Myopenia and precision (P4) medicine. Journal of Cachexia, Sarcopenia and Muscle. 2017;8(6):857–63. doi: 10.1002/jcsm.12231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cha KS, Lee HS. The effects of ego-resilience, social support, and depression on suicidal ideation among the elderly in South Korea. J Women Aging. 2018;30(5):444–59. doi: 10.1080/08952841.2017.1313023. [DOI] [PubMed] [Google Scholar]
- 45.Block J, Kremen AM. IQ and ego-resiliency: conceptual and empirical connections and separateness. J Pers Soc Psychol. 1996;70(2):349–61. doi: 10.1037/0022-3514.70.2.349. [DOI] [PubMed] [Google Scholar]
- 46.Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas. 1993;1(2):165–78. [PubMed] [Google Scholar]
- 47.Hardy SE, Concato J, Gill TM. Resilience of community-dwelling older persons. J Am Geriatr Soc. 2004;52(2):257–62. doi: 10.1111/j.1532-5415.2004.52065.x. [DOI] [PubMed] [Google Scholar]
- 48.Rossi NE, Bisconti TL, Bergeman CS. The Role of Dispositional Resilience in Regaining Life Satisfaction after the Loss of a Spouse. Death Studies. 2007;31(10):863–83. doi: 10.1080/07481180701603246. [DOI] [PubMed] [Google Scholar]
- 49.Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 50.Resnick BA, Inguito PL. The Resilience Scale: Psychometric properties and clinical applicability in older adults. Archives of psychiatric nursing. 2011;25(1):11–20. doi: 10.1016/j.apnu.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 51.Whitehall L, Górska S, Rush R, Singh Roy A, Irvine Fitzpatrick L, Forsyth K. Psychometric Evaluation of the Making it CLEAR Questionnaire: A Resilience Measure for Older Adults. Innovation in Aging. 2021;5(3) 10.1093/geroni/igab030 [DOI] [PMC free article] [PubMed]
- 52.Martin AS, Distelberg B, Palmer BW, Jeste DV. Development of a new multidimensional individual and interpersonal resilience measure for older adults. Aging Ment Health. 2015;19(1):32–45. doi: 10.1080/13607863.2014.909383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Friborg O, Hjemdal O, Rosenvinge JH, Martinussen M. A new rating scale for adult resilience: what are the central protective resources behind healthy adjustment? International Journal of Methods in Psychiatric Research. 2003;12(2):65–76. doi: 10.1002/mpr.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kashiwa-Toyoshikidai Projects for Enabling Age-friendly Communities: Achievements and Future Challenge 2018 [Available from: http://www.glafs.u-tokyo.ac.jp/wp-content/uploads/2018/07/35222084446b30b77df3f23690141037.pdf.
- 55.Lee W-J, Peng L-N, Lin C-H, Chen R-C, Lin S-Z, Loh C-H, et al. Effects of incorporating multidomain interventions into integrated primary care on quality of life: a randomised controlled trial. The Lancet Healthy Longevity. 2021;2(11):e712–e23. doi: 10.1016/S2666-7568(21)00248-8. [DOI] [PubMed] [Google Scholar]
- 56.Won CW, Ha E, Jeong E, Kim M, Park J, Baek JE, et al. World Health Organization Integrated Care for Older People (ICOPE) and the Integrated Care of Older Patients with Frailty in Primary Care (ICOOP_Frail) Study in Korea. Annals of geriatric medicine and research. 2021;25(1):10–6. doi: 10.4235/agmr.21.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]


