Abstract
Background
Physical activity and a healthy diet are important in helping to maintain mobility with aging. This umbrella review aims to identify group-based physical activity and/or nutrition interventions for community-dwelling older adults that improve mobility-related outcomes.
Methods
Five electronic databases (MEDLINE, Embase, CINAHL, Cochrane CENTRAL, Sociological Abstracts) were searched from inception to December 2021. Eligibility criteria included systematic reviews exploring the effectiveness of physical activity or structured exercise, alone or combined with nutrition interventions on mobility-related outcomes (aerobic capacity, physical function, balance, falls/safety, muscle strength, health-related quality of life/wellbeing). Interventions must have been delivered in a group setting to community-dwelling older adults aged 55+. Two reviewers independently performed eligibility screening, critical appraisal (using AMSTAR 2) and data extraction. The GRADE approach was used to reflect the certainty of evidence based on the size of the effect within each mobility-related outcome category. Older adult/provider research partners informed data synthesis and results presentation.
Results
In total, 62 systematic reviews (1 high, 21 moderate, 40 low/critically low quality) were identified; 53 included physical activity only, and nine included both physical activity and nutritional supplements. No reviews included nutrition interventions alone. Combined aerobic/resistance, general physical activity, and mind-body exercise all improved physical function and balance (moderate-high certainty). Aerobic/resistance training improved aerobic capacity (high certainty). Resistance training and general physical activity improved muscle strength (moderate certainty). Aerobic/resistance training and general physical activity are likely to reduce falls among older adults (moderate certainty). There was no evidence of benefit for nutritional supplementation with physical activity.
Conclusions
Group-based physical activity interventions that combine aerobic and resistance, general PA and mind-body exercise can improve measures of mobility in community-dwelling older adults. We found no reviews focused on nutrition only, highlighting a gap in the literature.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-022-03170-9.
Keywords: Mobility, Nutrition, Older adults, Physical activity, Umbrella review
Background
Mobility is a multifaceted construct, influenced by a range of modifiable (e.g., physical, cognitive, psychosocial, financial) and non-modifiable (e.g., environmental, gender, cultural, and biographical) factors [1]. A comprehensive view of mobility reflects one’s ability to move within their immediate home environment and the broader community [1]. Reductions in mobility and the ability to carry out activities of daily living are common with aging and are recognized precursors to frailty, falls, hospitalization, and death [2–4]. Although some factors influencing mobility among older adults are non-modifiable, several modifiable risk factors have been identified, including physical function, balance, muscular strength, aerobic endurance, and psychosocial wellbeing [5, 6]. Nutritional risk factors (e.g., inadequate food/fluid intake to support optimal physical functioning) are also predictive of reduced mobility in older adults [5, 7].
The beneficial effect of physical activity (PA) and improved diet quality on modifiable mobility-related outcomes has been widely demonstrated; however, inactivity and malnutrition continue to affect the well-being and mobility of older adults [8–12]. Community-based physical activity and nutrition programs delivered in group settings can address both the physical and psychosocial aspects of mobility, promoting a sense of belonging which aids in long-term adherence [13, 14]. The Enhancing physical and community MoBility in OLDEr adults with health inequities using commuNity co-design (EMBOLDEN) trial is a multi-year program of research from XX University in [City, Country] (Trial ID: NCT05008159) [15]. The transdisciplinary team of EMBOLDEN researchers, older adults and community partners have used community-based co-design to integrate local community needs, preferences, and resources with high-quality scientific evidence to develop a mobility-enhancing program that supports physical activity, healthy eating, and social participation among older adults.
Several systematic reviews have been published exploring a broad range of PA and/or nutrition interventions for older adults, making it challenging to bring together the best scientific evidence to inform program design. Umbrella reviews provide a rigorous methodology for synthesizing evidence from multiple existing systematic reviews [16], and may be particularly useful for a phenomenon such as mobility given the wide variety of interventions and uncertainty as to which interventions are more effective when delivered individually or in combination and within different populations and/or settings. To date, two umbrella reviews have reported the effectiveness of exercise interventions in pre-frail, frail, or sarcopenic older adults [17, 18], and one umbrella review has described the impact of nutritional interventions for community-dwelling older adults on body composition [19]. Given the lack of recent, relevant synthesized evidence to meet our needs, our team undertook this umbrella review to help inform intervention design and provide a foundation for the EMBOLDEN research program. This umbrella review aims to synthesize evidence from existing systematic reviews regarding the effectiveness of group-based PA and/or nutrition interventions to improve measures of mobility in community-dwelling older adults.
Methods
This review was conducted following the Joanna Briggs Institute (JBI) guidance for umbrella reviews [16], and was registered with PROSPERO (CRD42020141352). Although originally conceptualized as a systematic review, upon initiation of screening it was determined that many systematic reviews existed, and an umbrella review was most appropriate.
Search strategy
A trained librarian conducted a search of MEDLINE, Embase, CINAHL, Cochrane CENTRAL, and Sociological Abstracts from inception to December 2021 (Additional file 1). Searches were limited to systematic reviews/meta-analyses and randomized controlled trials (RCTs) published in English.
Study selection
Citations were imported into DistillerSR (Evidence Partners, Ottawa, Canada) and duplicates were removed. Citations were reviewed by two independent reviewers using pre-determined criteria. At the title/abstract level, a study must have been selected by one reviewer for inclusion, while exclusion required two reviewers to agree. At the full-text level, disagreements were resolved through discussion by two reviewers, with input from a third team member as needed.
Eligibility criteria
Types of studies
Systematic reviews (narrative summary, meta-analysis, or network meta-analysis) of interventions were eligible. Scoping or narrative reviews that did not include critical appraisal of primary studies were excluded. Eligible reviews could include RCTs and non-randomized intervention studies, however, at least 80% of single studies included must have been interventions (i.e., not descriptive, qualitative, or observational). To balance feasibility, while ensuring we captured the most recent and relevant intervention data, we chose to include only reviews that were published in 2010 or later; although eligible reviews did include single studies that were conducted prior to 2010.
Types of participants
Eligible systematic reviews included studies involving community-dwelling older adults. Reviews were included if the pooled mean age or inclusion criteria identified an age of ≥ 55 years. If this information was not available, at least 70% of included studies must have reported a mean sample age of ≥ 55 years. Reviews in which studies were selected based on a specific health or disease status (e.g., cancer, sarcopenia) were excluded. In reviews that did not restrict by disease status, 70% of included studies must have been conducted in a general sample of older adults. The choice of 70% was intended to include reviews in which the majority of included studies were relevant to the general population; most studies were either well above or well below this threshold.
Interventions
Eligible reviews must have included single studies of any PA (any movement resulting in energy expenditure), structured exercise (planned and repetitive movements), and/or nutrition intervention (e.g., education, counselling, dietary changes and/or supplementation) that could reasonably be delivered in a group-based setting [20]. Exercise or PA interventions were categorized as: aerobic exercise, resistance exercise, combined aerobic and resistance exercise, general physical activity (reviews in which a variety of types of physical activity and/or exercise were synthesized together), mind-body exercise (e.g., Tai Chi, yoga, Pilates), and dance.
Context
Single studies within eligible reviews must have been delivered in a community setting. Reviews that focused exclusively on interventions delivered in hospitals, rehabilitation centers, long-term care homes, or clinics were excluded. When the reviews did not set inclusion criteria by setting, at least 70% of included single studies were required to be community-based.
Outcomes
Reviews must have synthesized (narratively or via meta-analysis) outcomes related to physical or community mobility. These outcomes were broadly classified into six domains based on modifiable risk factors related to mobility that could be reasonably addressed through PA and/or nutrition interventions, as described above. The mobility-related outcomes explored include aerobic capacity, physical function, balance, falls/safety, muscular strength, and self-reported mental wellbeing/quality of life. Reviews that focused exclusively on cognitive function or body composition were excluded. These criteria were not part of our original protocol as registered in PROSPERO but added at the full text screening level as the goals of these interventions and associated outcomes were quite distinct.
Assessment of methodological quality
Eligible reviews were critically appraised using A MeaSurement Tool to Assess systematic Reviews (AMSTAR 2) [21]. AMSTAR 2 was completed independently by two reviewers, with conflicts resolved through discussion or the input of a third reviewer, as needed. Following consensus, results were entered into the online AMSTAR checklist, which provides an assessment of overall quality as critically low, low, moderate, or high based on seven critical domains [22].
Data extraction
Data were extracted by two independent reviewers using a standardized form. Disagreements were resolved through discussion or by a third reviewer. Data were extracted related to review methodology (e.g., sources searched, publication date range, methodological quality of included studies, noted limitations) and details of included studies (e.g., study designs, participant characteristics, intervention descriptions, setting). To explore issues of equity, diversity and inclusion, any data regarding material deprivation, and the percentage of low-income and/or immigrant populations were also extracted. Results from both narrative syntheses and meta-analyses were extracted within the six outcome categories described above. Any outcomes within these categories or composite outcomes in these areas (e.g., when multiple outcome measures were grouped and reported as standardized mean difference in a meta-analysis) were extracted, as reported. Data collection forms and full extracted data are available upon request.
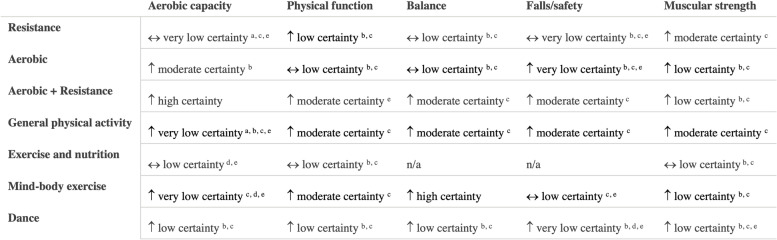
Data synthesis and certainty of evidence
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used to assess the overall certainty of the evidence [23]. The GRADE process was adapted to accommodate the umbrella review by considering both the findings across included reviews and across single studies within reviews by intervention type and outcome. Following the GRADE approach, reviews including primarily RCTs start at ‘high’ certainty, while reviews primarily including non-randomized studies start at ‘low’ certainty. The level of certainty was further downgraded based on the risk of bias, inconsistency of findings, indirectness of interventions/outcomes, imprecision of effect measures, and/or publication bias, and were upgraded based on the magnitude of effect size, dose-response relationship, and accounting for confounding. A narrative approach to data synthesis was used, with results presented in supporting tables and figures. Informative statements reflecting both the certainty of evidence and importance of the size of the effect are presented to communicate overall findings within each intervention type and outcome category, in line with published recommendations [24]. Only results that compared an intervention group to a control group were included in GRADE, although subgroup analyses are presented in accompanying tables.
The review team synthesized data with feedback and input from the larger research team and key stakeholders. After an initial draft, preliminary results and categories were presented to four older adult citizen and service provider partners from an established stakeholder group within the EMBOLDEN research program who were consulted via a one-time, virtual meeting. The aim of this engagement was to allow for feedback and discussion about the appropriateness of intervention/outcome groupings and to identify priority outcome measures (e.g., prioritize general physical function outcomes over measures such as body composition). Our older adult and service provider partners also contributed to developing public-facing documents, including a plain-language summary and infographic.
Results
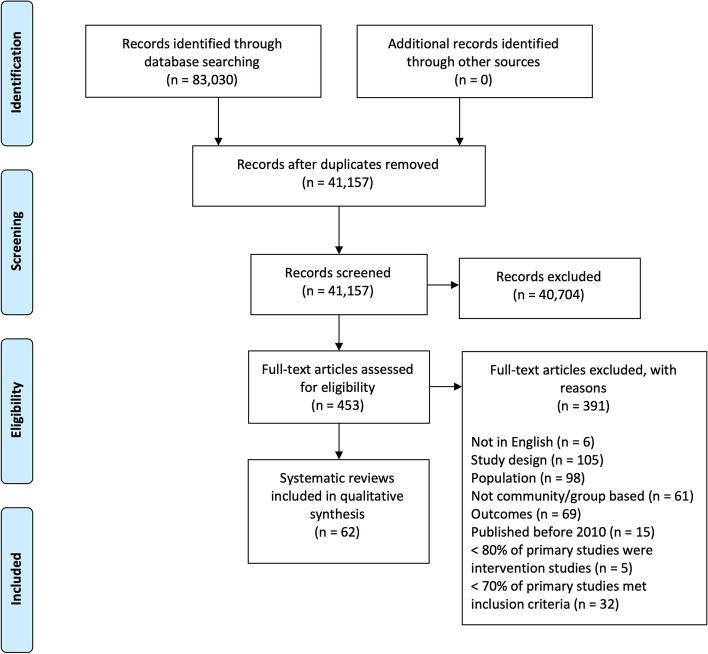
The search identified 41,157 unique citations, of which 1547 were potentially relevant; at this point, the team elected to limit to systematic reviews (Fig. 1). A second screen identified 453 citations for full-text review, of which 62 were included (Table 1). A list of excluded studies with reasons is provided in Additional file 2.
Fig. 1.
PRISMA Flow Diagram
Table 1.
Characteristics of Included Reviews
| Study | Objectives | Search | Years included | Description of intervention and comparator | Number and type of studies | Age (years) | N | % F | Study Quality (Tool) |
|---|---|---|---|---|---|---|---|---|---|
| Antoniak 2017 [25] | To assess effectiveness of RT + vitamin D3 on musculoskeletal health in older adults. | ScienceDirect, MEDLINE, PubMed, Google Scholar, Cochrane CENTRAL to Mar 2016 | 2003–2015 |
I: RT and vitamin D3 supplementation with or without calcium C: inactive, usual care without vitamin D3 supplementation |
7 RCTs |
Inclusion: ≥65 Mean: 72.8 |
792 | 82 |
RT + vitamin D: moderate RT + vitamin D + calcium: moderate-high (GRADE) |
| Borde 2015 [26] | To determine effects of RT on muscle strength and morphology and explore any dose–response relationships. | PubMed, Web of Science, Cochrane Library to May 2015 | 1991–2014 |
I: Machine-based RT of low, moderate, or high intensity C: inactive |
25 RCTs |
Inclusion: ≥60 Mean: 70.4 Range: 60–90 |
819 | NR; 16% F only, 16% M only |
Low (PEDro) |
| Bouaziz 2016 [27] | To evaluate the evidence of the health benefits of MCT training in adults > 65. | CINAHL, Embase, SPORTDiscus, Web of Science, Scopus, PubMed, MEDLINE, ScienceDirect, Jan 2000-Apr 2015 | 2000–2015 |
I: MCT including AT, RT, balance, stability, flexibility, and/or coordination training C: NR |
27 total; 19 RCTs |
Inclusion: ≥65 Range: 65–83 |
NR | NR |
Low quality studies excluded (Tool NR) |
| Bouaziz 2017 [28] | To review effect of AT in adults > 70 on cardiovascular, metabolic, functional, cognitive, and QoL outcomes. | CINAHL Plus, Embase, MEDLINE, PubMed, Scopus, Web of Science, SPORTDiscus, ScienceDirect, to Jan 31, 2016 | 1984–2013 |
I: Supervised (class or small group) AT C: NR |
53 total; 36 RCTs |
Inclusion: ≥70 Range: 70.0–87 |
2051 | NR | Low-moderate (Cochrane) |
| Bouaziz 2018 [29] | To determine the benefits of AT on VO2peak among those ≥70. | MEDLINE, PubMed Central, Scopus ScienceDirect, Embase to Mar 31, 2017 | 1989–2013 |
I: AT, any activity that uses large muscle groups, can be maintained continuously, and is rhythmic C: usual care or other exercise |
10 RCTs |
Inclusion: ≥70 Range: 70–79 |
348 | NR; 20% F only, 10% M only | Moderate (Cochrane) |
| Bruderer-Hofstetter 2018 [30] | To identify effective MCT interventions for physical capacity and/or cognitive function. | MEDLINE, CENTRAL, CINAHL, PsycINFO, Scopus, Date NR | 2002–2017 |
I: Combined cognitive training (exergames, dancing or Tai Chi) and physical exercise (planned, structured) C: attention controls or no intervention |
17 RCTs |
Inclusion ≥55 Mean: 71.37 ± 4.89 |
1758 Range: 32–555 |
67 |
Very low certainty (GRADE) |
| Bueno de Souza 2018 [31] | To determine the effects of mat Pilates on physical function in older persons. | MEDLINE, Scopus, Scielo, PEDro, Jan 2011-Mar 2017 | 2011–2017 |
I: Mat Pilates with or without accessories C: inactive control |
9 RCTs |
Inclusion ≥60 Mean: 68.5 ± 5.1 |
Range: 45–88 | NR; 56% F only |
56% high 44% low (PEDro) |
| Bullo 2015 [32] | To summarize the benefits of Pilates on physical fitness and QoL in the elderly. | MEDLINE, Embase, SPORTDiscus, PubMed, Scopus, PsycINFO, Date NR | 2009–2014 |
I: Pilates-identified exercise training intervention C: inactive control |
10; 6 RCTs |
Inclusion: ≥60 Range: 60–80 |
349 Range: 9–60 |
NR; 50% F only |
40% high 60% low (Cochrane) |
| Bullo 2018 [33] | To determine the effects of Nordic walking on physical fitness, QoL and body composition in the elderly. | MEDLINE, Embase, PubMed, Scopus, SPORTDiscus, PsycINFO, Date NR | 2012–2017 |
I: Supervised or unsupervised Nordic walking C: sedentary, walking, or resistance exercise |
15; 8 RCTs |
Inclusion ≥60 Range: 60–92 |
Range: 18–95 | “Majority female” |
27% high 73% low (Cochrane) |
| Chase 2017 [34] | To determine the effects of supervised RT and/or AT on physical function among community-dwelling older adults | MEDLINE, PubMed, CINAHL, Cochrane Library, Proquest, SPORTDiscus, PEDro, Ageline, Dissertation Abstracts International, 1960–2015 | 1999–2015 |
I: Supervised intervention involving RT and/or AT. 18 studies used RT only, the remainder employed combination RT and AT C: NR |
28 (designs NR) |
Inclusion: > 65 Mean: 70 Range: 65–85 |
2608 | 71 | NR; lower quality studies had stronger findings (PEDro) |
| da Rosa Orssatto 2019 [35] | To compare change in functional capacity following fast- vs. moderate-velocity lower limb RT in older adults | PubMed, Scopus, Web of Science to Jan 2019 | 2003–2019 |
I: Fast-velocity lower limb RT C: moderate-velocity lower limb RT |
15 RCTs |
Inclusion: ≥60 Range: 64.4–81.6 |
593 | NR |
Fair (PEDro) |
| Devries 2014 [36] | To determine whether the addition of creatine to RT increased gains in muscle mass, strength, and function in older adults over RT alone. | MEDLINE, HealthStar to June 2013 | 1998–2013 |
I: RT and Creatine supplementation C: RT and placebo |
10 RCTs |
Inclusion: > 45 Range: 55–71 |
357 | NR; 20% F only, 40% M only | Low-moderate (Jadad) |
| Ebner 2021 [37] | To determine the effects of mind-body interventions on physical fitness in healthy community dwelling older adults. | Web of Knowledge, PubMed, SPORTDiscus to Nov 2019 | 2005–2019 |
I: Yoga, Qi Gong, Tai Chi, Pilates C: Active and inactive controls |
30 RCTs |
Inclusion: ≥65 Mean: 71.2 |
2792 | 37 |
3% poor 17% fair 63% good 17% excellent (PEDro) |
| Elboim-Gabyzon 2021 [38] | To explore the effectiveness of high-intensity interval training for reducing fall risk factors in older adults. | PubMed, CINAHL, Cochrane, APA PsycInfo, Web of Science, Scopus, PEDro, AgeLine, ClinicalTrials.gov, Google Scholar to July 2021 | 2015–2020 |
I: High-intensity exercise (90–95% peak heart rate, 90% maximal oxygen uptake, at least 75% peak work rate) separated by periods of low to moderate-intensity or rest (e.g., walking/running, cycling). C: No treatment or other exercise |
11 (8 RCTs) |
Inclusion: Average ≥ 60 Range: 50–81 |
328 | 9% F only, 36% M only |
45% high 36% moderate 9% low 1 not assessed (PEDro) |
| Fernandez-Arguelles 2015 [39] | To know the effects of dancing as a physical exercise modality on balance, flexibility, gait and muscle strength in older adults. | PubMed, Cochrane Library Plus, PEDro, ScienceDirect, Dialnet, Academic Search Complete, Jan 2000-Jan 2013 | 2002–2012 |
I: Dance-based AT, dance and foot tapping or squatting, Turkish folk dance, low impact aerobic dance, Greek traditional dance, ballroom dance, and salsa dancing C: other types of exercise |
7 RCTs |
Inclusion: > 60 Range: 63.1–82.2 |
354 Range: 26–97 |
NR; 43% F only |
29% good 71% fair (PEDro) |
| Fernández-Rodríguez 2021 [40] | To estimate the effectiveness of Pilates on physical performance and risk of falls in older adults. | MEDLINE, Scopus, Web of Science, Physiotherapy Evidence Database, Cochrane Central Register of Controlled Trials to April 2021 | 2010–2021 |
I: At least one exercise intervention described as “Pilates” (Mat, machine, or both) C: Habitual or non-exercise |
39 RCTs |
Inclusion: ≥60 Range: 60–80 |
1650 | 62 |
64% high 36% unclear (Cochrane) |
| Finger 2015 [41] | To determine whether protein supplements can optimize the effects of RT on muscle mass and strength in an aged population. | MEDLINE, Cochrane Central, EMBASE, LILACS to January 2014 | 1995–2013 |
I: RT and protein for ≥6 weeks. Protein supplements ranged from 0.3 to 0.8 g/kg/day (mean 0.46 g/kg/day) or 6 to 40 g/day (mean = 20.7 g/day) or high protein diet C: RT with placebo or no supplement |
9 RCTs |
Inclusion: ≥60 Range: 61.2–79.2 |
462 Range: 12–87 |
NR; 11% F only, 33% M only | Low-moderate risk of bias (PRISMA statement) |
| Frost 2017 [42] | To evaluate effectiveness of home- and community-based health promotion interventions on functioning and frailty in older people with mild or pre-frailty. | MEDLINE, EMBASE, Scopus, Social Science Citation Index, Science Citation Index Expanded, Cochrane (library, CENTRAL, EPOC), NHS Health Economic Evaluations, DARE, PsycINFO, CINAHL, Bibliomap, Social Care Online, Sociological Abstracts, Applied Social Sciences Index, Jan 1990-May 2016 | 2000–2015 |
I: Home- or community-based health promotion interventions (i.e., interventions that enable people to improve or increase control over their health) C: usual care or health education or flexibility training |
10 (7 RCTs) |
Inclusion: > 60 Range: 72–83 |
485 | NR | Low or unclear risk of bias (Cochrane) |
| Gade 2018 [43] | To determine the effect of protein or essential amino acid supplementation during RT in older adults. | PubMed, SCOPUS, EMBASE, Cochrane databases to 2017 | 1994–2016 |
I: RT plus protein or essential amino acid supplementation or a modified diet with increased protein content for > 5 weeks C: RT with/without non-protein placebo |
16 RCTs |
Inclusion: > 60 Range: 61–85 |
1107 Range: 16–179 |
NR; 13% F only, 25% M only |
Good to excellent (PEDro) |
| Garcia-Hermoso 2020 [44] | To analyze the safety and effectiveness of long-term exercise interventions in older adults. | PubMed, Cochrane CENTRAL, SPORTDiscus to Sept 16, 2019 | 1991–2019 |
I: MCT (n =45), RT (n=24), AT (n=19), and Tai Chi (n=4). Most used group-based supervised exercise alone (n=46) or combined with home-based unsupervised training (n=21) C: usual care with or without non-exercise intervention |
99 (93 RCTs; 90 RCTs in meta-analysis) |
Inclusion: ≥65 Mean: 74.2 |
28,523 | NR; 19% F only, 4% M only |
Good (PEDro) |
| Grässler 2021 [45] | To summarize the effects of endurance, resistance, coordinative, and multimodal exercise interventions on resting heart rate variability and secondary health factors in healthy older adults. | PubMed, Scopus, SPORTDiscus, Ovid, Cochrane Jan 2005-Sept 2020 | 2005–2020 |
I: Physical training intervention (endurance, resistance, coordinative, or multimodal training) with a minimum of 4 weeks and 8 training sessions C: NR |
13 RCTs and non-RCTs (designs NR) |
Inclusion: ≥60 Mean: 67.8 |
422 | 31% F only, 8% M only |
Mean: 8.88 (SD 2.47)/15 (Tool for the Assessment of Study Quality and reporting in Exercise) Mean: 20 (SD 1.56)/25 (STARDHRV) |
| Hanach 2019 [46] | To evaluate the effectiveness of dairy proteins on functions associated with sarcopenia in middle-aged and older adults. | PubMed, CINAHL, Web of Science to May 10, 2017 | 2009–2016 |
I: Dairy protein supplementation (e.g., whey protein, milk-protein concentrate, casein) or a protein-based dairy product (e.g., ricotta cheese) for ≥12 weeks with/out RT C: usual care, placebo, or regular dairy |
14 RCTs |
Inclusion: 45–65 Range: 61–81 |
1424 | NR; 7% F only | Moderate-High (Cochrane) |
| Hortobagyi 2015 [47] | To determine the effects of strength, power, coordination, and MCT on healthy older adults’ gait speed. | PubMed, Web of Knowledge, Cochrane, Jan 1984 to Dec 2014 | 1993–2014 |
I: RT or interventions that included 2+ types of exercise in any combination or functional or coordination training C: no exercise |
42 (designs NR) |
Inclusion ≥65 Mean: 74.2 Range: 64.4–82.7 |
2495 | 63 | Low (PEDro) |
| Hou 2019 [48] | To explore whether a combination of protein supplementation with RT is effective in enhancing muscle mass, strength and function in the elderly. | PubMed, MEDLINE, Embase, Jan 2004-May 2018 | 2004–2018 |
I: Protein supplements containing leucine, whey protein, casein, lean meat, low-fat milk or related mixture and RT 1–4 times/week C: RT alone |
21 RCTs |
Inclusion: > 50 Range: 50–91 |
1249 | NR; 38% F only, 14% M only | Moderate certainty (Cochrane) |
| Howe 2011 [49] | To examine the effects of exercise interventions on balance in older people, ≥60 y, living in the community or institutional care. | Cochrane Specialized Register, CENTRAL, MEDLINE, EMBASE, PEDro, CINAHL, AMED to Feb 2011 | 1989–2010 |
I: Interventions designed to improve balance, or RT or MCT or Tai Chi, qi gong, dance and yoga or gait, coordination, and functional exercises C: attention control |
94 RCTs and quasi-experimental |
Inclusion: ≥60 Range: 60–75 |
9821 | NR; 27% F only, 5% M only | Most unclear risk of bias (Cochrane) |
| Hurst 2019 [50] | To assess the effects of same session combined exercise on measures of fitness in adults ≥50 y. | PubMed, MEDLINE, Scopus, BIOSIS, Web of Science to July 2018 | 1991–2018 |
I: At least one AT and RT group C: no exercise, AT only, or RT only |
27 (22 RCTs) |
Inclusion: > 50 Mean: 68.8 Range: 54–85 |
1346 | NR; 44% F only, 18% M only | Low or unclear risk of bias (Cochrane) |
| Hwang 2015 [51] | To examine the benefits to physical health of dance among older adults. | PubMed, Date NR | 2004–2013 |
I: Dance defined as a form of artistic expression through rhythmic movement to music, not including aerobic fitness classes taught to music C: other activity or no activity |
18 (10 RCTs) |
Inclusion: NR Range: 52–87 |
Range: 13–97 | NR; 44 > 50% F, 28% F only |
Moderate (Sackett, Megens and Harris) |
| Katsoulis 2019 [52] | To investigate the effect of high- vs. low-intensity RT on muscular power in older, healthy, untrained adults. | MEDLINE, Embase, CINAHL, AgeLine, SPORTDiscus, Scopus to Apr 2017 | 2001–2017 |
I: Low (≤50% 1RM), moderate or high (≥70% 1RM) intensity power training C: post-intervention vs. pre-intervention |
27 RCTs |
Inclusion: > 60 Mean: 74.5 Range: 62.7–81.8 |
549 Range: 5–59 |
NR; 22% F only, 7% M only | 52% high (> 6); remaining fair-good (PEDro) |
| King 2016 [53] | To synthesize research that tests the effects of aquatic exercise in healthy older adults on functional balance. | Academic Search Complete, AMED, CINHAL, MEDLINE, SPORTDiscus, Date NR | 1996–2013 |
I: Exercise programs in water, with no restriction on depth or temperature of the aquatic environment. Swimming programs were not included C: land exercise or no exercise |
13 (6 RCTs) |
Inclusion > 60 Mean: 71 Range: 68–80 |
545 Range: 20–79 |
NR; 31% F only, 8% M only |
46% good; 54% poor-fair (Downs and Black) |
| Labott 2019 [54] | To examine the effects of exercise training on handgrip strength in healthy community-dwelling older adults ≥60 y. | PubMed, Web of Science, SPORTDiscus to Nov 25, 2018 | 1995–2018 |
I: aquatic exercise, walking, flexibility, TRX-training, home-trainer exercise, RT, vibration platform, dance, Tai Chi, exergames, balance training, calisthenics, and MCT C: NR |
24 RCTs |
Inclusion: ≥60 Mean: 73.3 ± 6.0 |
3018 Range: 22–1635 |
NR; 50% F only 4% M only | Fair (PEDro) |
| Lesinski 2015 [55] | To quantify effects of balance training on balance outcomes and to characterize dose–response in healthy community-dwelling older adults. | PubMed, Web of Science, Jan 1985 to Jan 2015 | 1994–2014 |
I: Balance training protocol comprising static/dynamic postural stabilization exercises (combined training was excluded) C: no intervention |
23 RCTs |
Inclusion: ≥65 Range: 66–83 |
1220 Range: 11–75 |
NR; 9% F only | 74% weak (PEDro) |
| Leung 2011 [56] | To assess the usefulness of tai chi to improve balance reduce falls in older adults. | CINAHL, Science citation index, social science citation index, MEDLINE, Cochrane Central, ScienceDirect, PubMed, Allied & Complementary medicine, China journals, eCAM, Jan 1, 1998-Jan 31, 2008 | 2000–2007 |
I: Various styles of Tai Chi C: no treatment or other exercise |
13 RCTs |
Inclusion: ≥60 Range: 45–98 |
2151 | NR; 23% mostly F, 8% mostly M, 8% M only |
Good to excellent (PEDro) |
| Levin 2017 [57] | To examine the dual effects of different types of physical training on cognitive and motor tasks in older adults with no known cognitive or motor disabilities or disease | PubMed, Jan 2007-Dec 2016 | 2008–2016 |
I: physical training (e.g., balance training, AT, strength training, group sports, etc.) or combined physical and cognitive intervention (dual-task) C: passive control or health education classes and lesser training |
19 (17 RCTs) |
Inclusion: > 65 Range: 65.5 ± 6.3–81.9 ± 6.3 |
1226 | 52 |
Mostly low (Jadad) |
| Liberman 2017 [58] | To assess the effects of exercise on muscle strength, body composition, physical function and inflammatory profile in older adults. | PubMed, 2015–2016 | 2015–2016 |
I: Any exercise; included RT (n=16), AT (n=8), AT/RT (n=6) and other types (n=10) C: no intervention |
34 RCTs |
Inclusion: > 65 Range: 54.5–92.3 |
1747 | NR | Unclear risk of bias across domains (NICE) |
| Liu 2010 [59] | To determine whether Tai Chi has an effect on static and dynamic balance, functional performance, muscle strength and flexibility, and subjective measures. | MEDLINE, PubMed; Jan 2000-July 2007 | 2000–2007 |
I: Tai Chi C: NR |
18 (15 RCTs) |
Inclusion: ≥60 Mean: NR |
3741 Range: 17–1200 |
NR | NR; lower-quality studies screened out |
| Liu 2017 [60] | To compare RT or MCT to no intervention or attentional controls, on muscle strength, physical functioning, ADL, and falls in community- dwelling older adults with reduced physical capacity. | MEDLINE, Embase, Cochrane Library Central, Date NR | 1996–2015 |
I: Progressive RT, strength training in which one exerts an effort against an external resistance or MCT combines > 2 types of exercise RT, balance, stretching, and AT C: no intervention or attention control |
23 RCTs |
Inclusion: ≥60 Mean: 75 Range: 69–84 |
2018 | NR; 22% F only, 4% M only | Low risk of bias (Cochrane) |
| Liu 2020 [61] | To evaluate the effects of dance on physical function performance in healthy older adults. | Cochrane Library, PsycINFO, PubMed, Scopus, Web of Science to June 2018 | 2008–2017 |
I: Dance interventions of at least 6 weeks duration C: usual care with no intervention or other exercise |
13 RCTs |
Inclusion: ≥65 Mean: NR |
1029 Range: 23–510 |
85 | Low-moderate risk of bias (Cochrane) |
| Loureiro 2021 [62] | To determine the effects of multifactorial programs including physical activity based on individual assessment of fall risk factors on rate of falls and physical performance in older adults. | PubMed, Cochrane Plus, Web of Science, SCOPUS, 2009–2020 | 2009–2017 |
I: Multi-component interventions including strength and balance training, flexibility, endurance, gait, and/or functional exercises, treatment of sensory impairments, health education, medical management and/or in home falls risk assessment C: Usual care, delayed intervention, health education |
6 RCTs |
Inclusion: ≥60 years Mean: 77.62 |
2012 Range: 19–616 |
54.4 |
50% good 50% fair (PEDro) |
| Martin 2013 [63] | To compare physical therapist–administered group-based exercise with individual or no exercise control. | PubMed, CINAHL, Dec 1, 2001-June 7, 2012 | 2002–2010 |
I: Physical therapist led or supervised group exercise C: individual physical therapy or no exercise control |
10 RCTs |
Inclusion: ≥65 Mean: 76.21 Range: 72–81 |
2293 Range: 32–1090 |
NR |
Good (PEDro) |
| Martins 2018 [64] | To identify modified Otago Exercise Program delivering methods and analyze their effects on balance, functional ability and self-reported falls. | PubMed, PEDro, ScienceDirect, Scopus, Date NR | 2011–2016 |
I: Modified Otago Exercise program (RT, balance and walking) C: original Otago program, non-intervention, or other exercise |
8 (5 RCTs) |
Inclusion: NR Mean: 76.75 ± 5.5 |
604 | NR; 13% F only |
Fair-Good (PEDro) |
| Meereis-Lemos 2019 [65] | To determine the effectiveness of RT and MCT on functionality of healthy older patients. | PubMed, Web of Science, PEDro, Cochrane, Lilacs databases, Date NR | 2007–2016 |
I: Supervised RT or RT combined with another modality at least twice a week for a minimum of 8 weeks C: no exercise |
28 RCTs |
Inclusion: ≥60 Range: 62.2 ± 4.3–83.4 ± 2.8 |
NR | NR; 36% F only, 14% M only |
Good (PEDro) |
| Montero 2016 [66] | To explore the effects of AT on VO2max, Qmax and Ca-VO2max in healthy middle-aged and older subjects. | MEDLINE, Scopus and Web of Science to May 2015 | 1989–2014 |
I: Dynamic exercise involving a large muscle mass (e.g., running, cycling), 3 weeks or more C: post-intervention vs. pre-intervention |
16 (designs NR) |
Inclusion: > 40 Range: 42–71 |
153 | NR; 19% F only, 63% M only |
Moderate-high (SAQOR) |
| Moore 2016 [67] | To assess the effectiveness of community-based interventions to increase physical activity in older people (≥ 65 y) living rural or regional areas. | CINHAL, Ageline, ProQuest Central, PubMed, Informit Complete, Google Scholar to Aug 2014 | 1997–2014 |
I: Community-based PA intervention of six weeks or more (from start to follow-up) C: NR |
7 (3 RCTs) |
Inclusion: ≥65 Mean: NR |
Range: 37–1200 | NR; 14% F only |
High risk of bias (Cochrane) |
| Moran 2018 [68] | To determine the effect of jump training on muscular power in older adults (≥ 50 y). | Google Scholar, PubMed, Microsoft Academic, Date NR | 1998–2018 |
I: Jump training, defined as lower body unilateral and bilateral bounds, jumps and hops C: NR |
9 (designs NR) |
Inclusion: ≥50 Range: 53.0–72.4 |
467 | NR; 56% F only, 11% M only |
Good (PEDro) |
| Nicolson 2021 [69] | To evaluate the effects of therapeutic exercise interventions on physical function, health-related quality of life and psychosocial outcomes in community-dwelling adults. | MEDLINE, EMBASE, CINAHL to July 2020 | 1997–2020 |
I: Therapeutic exercise including AT, RT, functional training, balance training, gait training, flexibility, or 3D (constant movement in a controlled, fluid, repetitive way through all three spatial dimensions, e.g., Tai Chi) C: Usual care, no treatment, other exercise, pharmacotherapy, or health education |
16 RCTs |
Inclusion: ≥80 Median: 84.2 (interquartile range: 83.4–86.1) |
1660 | 19% F only, 6% M only |
6% low 63% moderate 31% high (Cochrane) |
| Plummer 2015 [70] | To examine the effects of physical exercise on dual-task performance during walking in older adults. | PubMed, CINAHL, EMBASE, Web of Science, PsycINFO up to Sept 19, 2014 | 2006–2014 |
I: Any physical exercise intervention C: active, education, or inactive no treatment/delayed treatment |
21 (15 RCTs) |
Inclusion: ≥60 Range: 71.1–91.1 |
Range: 10–134 | ≥70% in all but 2 studies |
Good (Downs and Black) |
| Qi 2020 [71] | To evaluate the effects of Tai Chi with RT on health outcomes in adults ≥50 y. | PubMed, Scopus, Web of Science, CINAHL, MEDLINE, PEDro, Cochrane library to Jan 2018 | 2005–2016 |
I: Tai Chi combined with RT C: any control or comparison |
7 (6 RCTs) |
Inclusion: ≥50 Range: 58.5–74.0 |
703 | NR; 14% F only |
Fair (PEDro) |
| Raymond 2013 [72] | To examine the effect of high intensity RT on strength, function, mood, QoL, and adverse events in older adults. | Cochrane Central, MEDLINE, Embase, CINAHL, AMED, AgeLine, PEDro to July 2012 | 1995–2007 |
I: Lower limb high intensity progressive RT with or without upper limb or trunk strengthening C: other intensity RT |
21 RCTs |
Inclusion: ≥65 Range: 60–95 |
724 | NR; 14% F only, 24% M only | Poor to fair (PEDro) |
| Rodrigues-Krause 2019 [73] | To review the literature on the use of dance to promote functional and metabolic health in older adults. | MEDLINE, Cochrane Wiley, ClinicalTrials.gov; PEDRO, LILACS, Nov 1980 to Mar 2016 | 1984–2016 |
I: Regular dance classes of any style for at least 2 weeks. Dance environments included dance studios and stage and/or dance ballrooms C: inactive control or other exercise |
50 (31 RCTs) |
Inclusion: > 55 Range: 50–94 |
Range: 10–700 | NR; 34% F only, 4% M only |
Majority high risk of bias (PRISMA) |
| Roland 2011 [74] | To investigate whether physical fitness and function benefits are engendered through the practice of yoga in older adults. | PubMed, Scholars Portal, AgeLine, CINAHL, EBSCO, MEDLINE, SPORTDiscus, PsycINFO, EMBASE, 1970–2009 | 1989–2009 |
I: Yoga C: other exercise, no exercise, or pre/post yoga groups |
10 (5 RCTs) |
Inclusion: ≥65 or 55–64 Mean: 69.6 ± 6.3 |
544 Range: 13–176 |
71 |
Moderate-high (Modified Downs and Black) |
| Sivaramakrishnan 2019 [75] | To synthesize existing evidence on the effects of yoga on physical function and QoL in older adults not characterized by any specific clinical condition. | MEDLINE, PsycINFO, CINAHL Plus, Scopus, Web of Science, Cochrane Library, Embase, SPORTDiscus, AMED, ProQuest Dissertations & Theses Global to Sept 2017 | 1983–2017 |
I: Yoga C: inactive or active controls |
22 RCTs |
Inclusion: ≥60 Range: 61.0–83.8 |
Range: 18–410 | > 70 | Moderate risk of bias (Cochrane) |
| Stares 2020 [76] | To assess whether creatine combined with exercise results improves indices of skeletal muscle, bone, and mental health over exercise alone in healthy older adults. | PubMed, CINAHL, Web of Science, 1998–2018 | 1998–2016 |
I: A physical training program and creatine supplementation C: placebo |
17 RCTs |
Inclusion: ≥48 Mean age: NR Range: 48–84 |
583 | 39 |
Overall good (PEDro) |
| Stathokostas 2012 [77] | To assess the effects of flexibility training on functional outcomes in healthy older adults > 65 y. | PubMed, Embase, CINAHL, Scopus, and SPORTDiscus to Jan 2011 | 1988–2011 |
I: Flexibility training (excluding Tai Chi or yoga) C: NR |
22 (13 RCTs) |
Inclusion: ≥65 Mean: 74.1 Range: 64–88.8 |
1127 Range: 7–132 |
75 |
RCTs: good Non-RCTs: low-moderate (Modified Downs and Black) |
| Straight 2016 [78] | To estimate the effect of RT on lower-extremity muscle power in middle-aged and older adults. | Google Scholar to Nov 1, 2014 | 1995–2013 |
I: RT, defined as muscle-strengthening activities that use major muscle groups and could include free weights, machines, and resistance bands C: usual care or sham exercise |
12 RCTs |
Inclusion: ≥50 Range: 56.3–93 (intervention), 56.7–93 (control) |
810 | NR; 17% F only, 8% M only | NR |
| Ten Haaf 2018 [79] | To assess the effect of protein on lean body mass, muscle strength, and/or physical performance, in non-frail community-dwelling older adults. | PubMed, Embase, Web of Science to May 15, 2018 | 1992–2018 |
I: Multi-nutrient protein or essential amino acid supplementation added to or replacing normal diet with or without RT. Supplements were consumed ≥3 times/week for at least 4 weeks C: placebo control or RT |
36 RCTs |
Inclusion: ≥50 Range: 55–85 |
1682 | NR; 19% F only, 31% M only |
50% Moderate, 42% Good, 8% Excellent (Downs and Black) |
| Tschopp 2011 [80] | To determine the effects of power training with high movement velocity for older community-dwelling people. | PubMed (MEDLINE), EMBASE, CINAHL, PEDro, Cochrane Central and Google Scholar to April 2010 | 2002–2009 |
I: Power training (training with moderate resistance and an ‘as fast as possible’ movement speed for at least the concentric phase of an exercise) C: Conventional RT (high or moderate resistance and slow concentric movement) |
11 RCTs | Inclusion: > 60 | 377 | NR | Moderate risk of bias (Tool NR) |
| Van Abbema 2015 [81] | To determine the effects of different types or combinations of exercise to improve preferred gait speed. | PubMed, EMBASE, AMED, CINAHL, ERIC, MEDLINE, PsycINFO, SocINDEX, and Cochrane Library 1990 -Dec 9, 2013 | 1994–2013 |
I: Progressive RT or RT, balance and AT with or without additional training components, exercise interventions with a dance/rhythmic component or stretching exercises C: usual care or attention control |
25 RCTs |
Inclusion: ≥65 Mean: 75.8 Range: 61.4 ± 5.5–87.1 ± 0.6 |
2389 | NR; 32% F only |
Low-quality studies excluded Moderate-high (PEDro) |
| Vetrovsky 2019 [82] | To evaluate the safety and efficacy of plyometric training in older adults regarding various performance, functional, and health related outcomes. | PubMed, SPORTDiscus, Scopus, and EMBASE to 2017 | 2007–2017 |
I: Plyometric training (eccentric loading followed by a concentric contraction, e.g., repetitive jumping, hopping, bounding, and skipping) or MCT with plyometrics C: non-exercising control or other exercise |
12 RCTs |
Inclusion: ≥60 Range: 58.4–79.4 |
289 Range: 8–36 |
61 |
75% high (PEDro) |
| Waller 2016 [83] | To investigate the effect of aquatic exercise on physical functioning in healthy older adults. | MEDLINE, Embase, CINAHL, PEDro, SPORTDiscus, Web of Science, Cochrane Library to Dec 31, 2015 | 1994–2015 |
I: Exercise in an aquatic environment with no limitation on the type of exercise C: land exercise or no exercise |
28 RCTs |
Inclusion: ≥55 Mean: 66.4 Range: 55.4–82.0 |
1456 | 89 | High risk of bias (Cochrane) |
| Wang 2021 [84] | To examine the impact of Traditional Chinese medicine-based exercises on physical performance, balance, and muscle strength in the elderly. | PubMed, EMBASE, Scopus, Cochrane Central Register of Controlled Trials, China National Knowledge Infrastructure, Wan Fang, manual search of Soochow University and Nanjing University of Chinese Medicine libraries to March 2021 | 2003–2020 |
I: Traditional Chinese medicine-based exercises including but not limited to Tai Chi, Ba Duan Jin, and Qigong C: Placebo, AT, routine care, or educational programs |
27 RCTs |
Inclusion: ≥55 Range: 59.7–88.8 |
2580 | 68 |
Moderate (Cochrane) |
| Wirth 2020 [85] | To investigate the effect of protein supplementation on body composition and muscle function in healthy adults. | PubMed, Web of Science, CINAHL, Embase to March 2019 | 2001–2019 |
I: Oral protein intake, 2wk minimal duration, including energy-restriction or not, and including exercise or not C: Low-protein diet, no protein supplementation, or non-protein placebo |
23 RCTs |
Inclusion: > 55 Range: 55–81 |
1290 | 62 |
Moderate certainty (GRADE) |
| Yang 2019 [86] | To determine intensity and interval of effective interventions in improving physical function in community-dwelling older adults. | PubMed, EBSCO, and Cochrane Trials, Jan 1, 2013-Dec 31, 2017. | 2013–2017 |
I: Any types of MCT interventions that were conducted in the community, delivered by any kinds of providers C: no exercise control |
5 RCTs |
Inclusion: > 60 Mean: 70 (intervention) 69 (control) |
272 | “Majority female” | Moderate (Cochrane) |
F Female, M Male, NR Not reported, RCT Randomized controlled trial, PEDro Physiotherapy Evidence Database, GRADE Grading of Recommendations, Assessment, Development and Evaluations, MCT Multicomponent interventions, AT Aerobic exercise training, RT Resistance training, QoL Quality of life, ADL Activities of daily living, VO2 max Maximal oxygen consumption, Qmax Maximal cardiac output, Ca-VO2max Arteriovenous oxygen difference at maximal exercise
Included reviews reported on several types of interventions, with some reporting separate results for more than one intervention type. Most reviews focused on exercise or PA only (n = 53) [26–35, 37–40, 42, 44, 45, 47, 49–75, 77, 78, 80–84, 86], while others included exercise with nutritional supplements (n = 9) [25, 36, 41, 43, 46, 48, 76, 79, 85]. No reviews included group-based nutrition interventions alone. Exercise or PA interventions were categorized as resistance exercise (n = 12) [26, 35, 47, 49, 52, 60, 65, 69, 72, 78, 80, 81], aerobic exercise (n = 5) [28, 29, 33, 38, 66], combined aerobic and resistance exercise (n = 9) [27, 34, 47, 50, 57, 60, 64, 65, 81], general PA (n = 12) [42, 44, 45, 49, 54, 58, 62, 63, 67, 69, 70, 86], mind-body exercise (e.g., Tai Chi, yoga, Pilates) (n = 11) [31, 32, 37, 40, 49, 56, 59, 71, 74, 75, 84], dance (n = 5) [39, 51, 61, 73, 81], and other (e.g., aquatics, stretching) (n = 10) [30, 47, 49, 53, 55, 68, 77, 81–83]. Nutritional supplements included protein (n = 5) [41, 43, 48, 79, 85], creatine (n = 2) [36, 76], vitamin D (n = 1) [25], or dairy (n = 1) [46]. Meta-analyses were undertaken in 39 reviews [25, 26, 29, 31–37, 40–42, 44, 46–50, 54–56, 60, 61, 65, 66, 68–70, 72, 75, 78–81, 83–86], 22 reviews presented findings narratively [27, 28, 38, 39, 43, 45, 51–53, 57–59, 62–64, 67, 71, 73, 74, 76, 77, 82], and one performed a network meta-analysis [30]. Total sample sizes ranged from 153 to 28,523 when reported. Participants ranged from 42 to 98 years old, with most reviews only including studies with participants aged 60 and older. No reviews extracted data on material deprivation, low income, or immigrant populations.
Eligible reviews included 1339 primary studies, of which 962 were unique (28.2% overlap across reviews, although some duplicates were included in reviews focused on different intervention types). Reviews with the most overlap by intervention type were exercise with nutritional supplements (36.2% overlap), dance (31.9% overlap), and resistance exercise (26.3% overlap). Single studies were published between 1983 and 2021 (range 5 to 99 studies per review). Of these, 83% were randomized controlled trials and 17% were quasi-experimental, observational, or not reported.
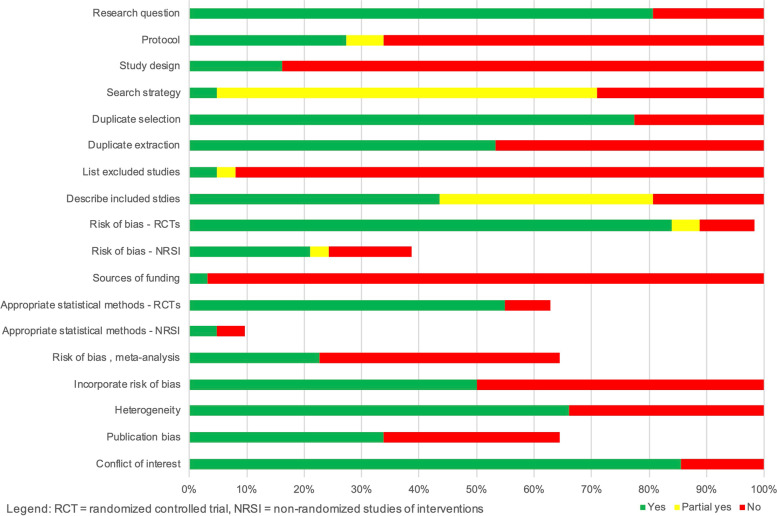
Methodological quality of included reviews
Methodological quality of the reviews was variable (summary in Fig. 2, full assessment in Additional file 3), with one review [49] rated as having high confidence in findings. The confidence for the remaining reviews were moderate (n = 21) [25, 28, 30, 35, 36, 42–44, 46, 50, 53, 66, 67, 71, 72, 75, 77, 80–83], low (n = 17) [31, 34, 39, 40, 48, 54–56, 60, 63, 69, 70, 73, 74, 76, 85, 86], and critically low (n = 23) [26, 27, 29, 32, 33, 37, 38, 41, 45, 47, 51, 52, 57–59, 61, 62, 64, 65, 68, 78, 79, 84]. Most reviews did not report protocol registration, describe an adequate search strategy, justify excluded studies, or incorporate risk of bias in interpreting review findings.
Fig. 2.
AMSTAR 2 Summary of Systematic Review Quality. Legend: RCT = randomized controlled trial, NRSI = non-randomized studies of interventions
Findings of reviews
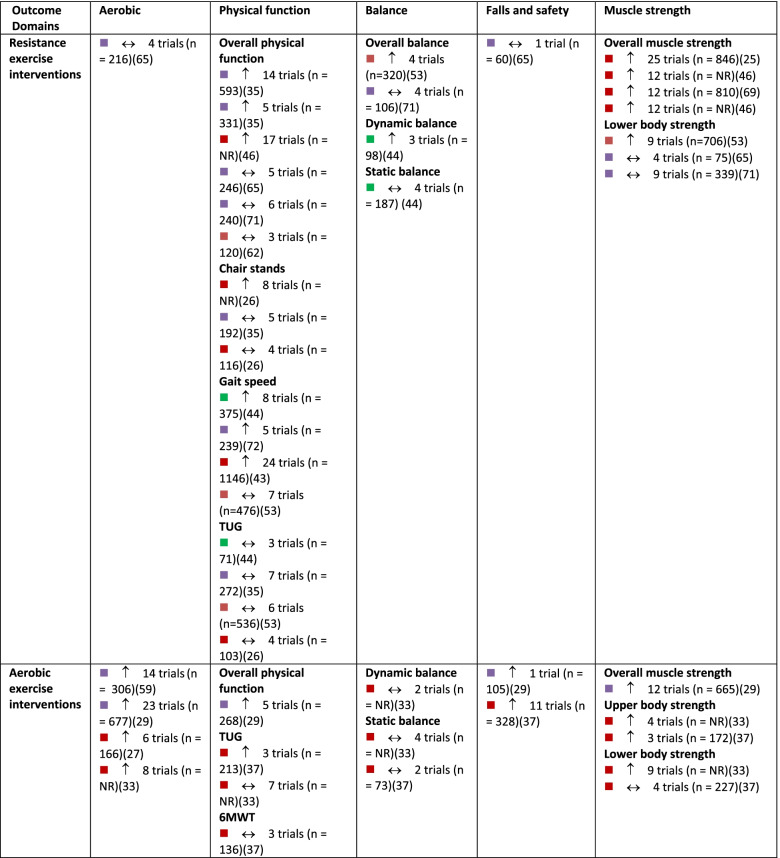
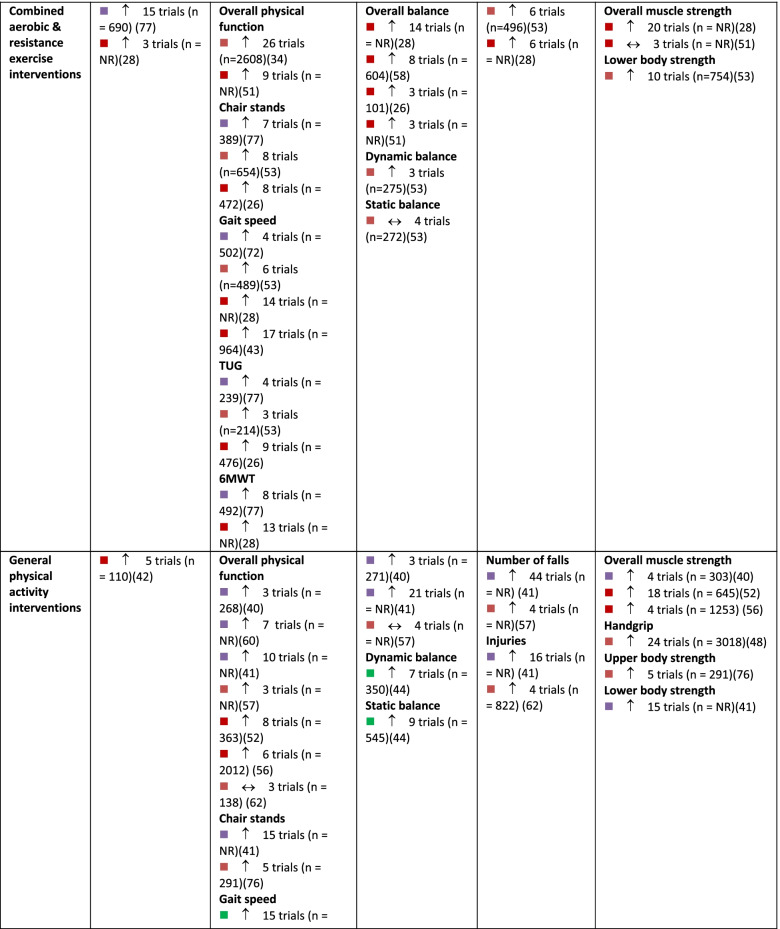
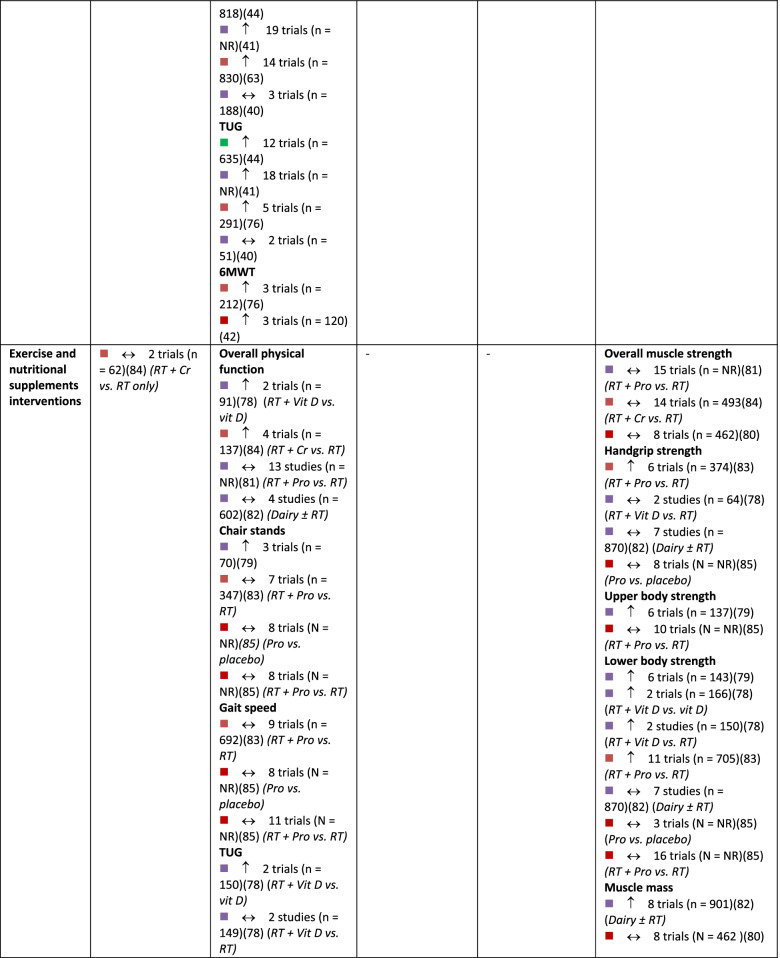
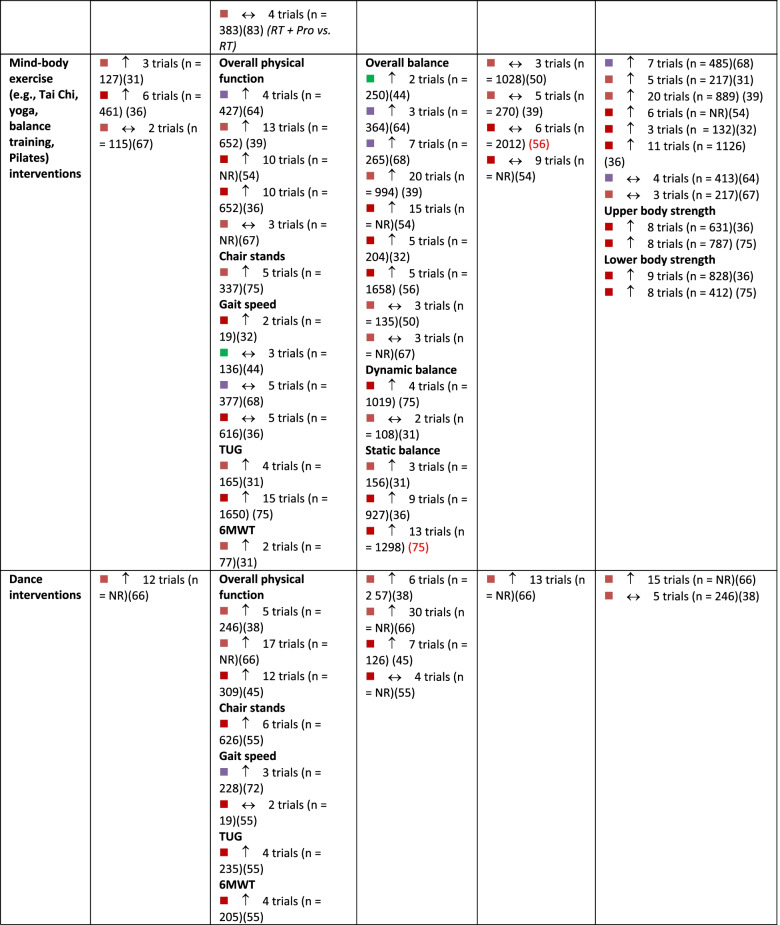
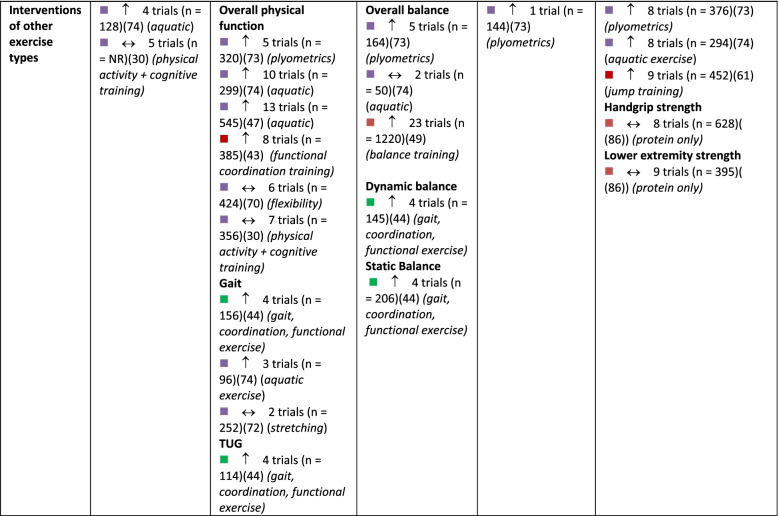
A summary of findings by intervention type and outcome category, alongside review quality is listed in Table 2, with a summary of the certainty of evidence (GRADE) in Fig. 3.
Table 2.
Summary of results across included systematic reviews by outcome domain and intervention type, alongside methodological quality of the review, number of trials included in the relevant analysis and sample size
Note:
 = critically low quality;
= critically low quality;
 = low quality;
= low quality;
 = moderate quality;
= moderate quality;
 = high quality (as determined by AMSTAR 2).
= high quality (as determined by AMSTAR 2).
 = compared to a control group, intervention demonstrates statistically significant beneficial effect on outcome;
= compared to a control group, intervention demonstrates statistically significant beneficial effect on outcome;
 = intervention demonstrates no significant change in outcome when compared to a control group.
= intervention demonstrates no significant change in outcome when compared to a control group.
6MWT six-minute walking test, CR creatine supplementation, NR not reported, Pro protein supplementation, RT resistance training, TUG Timed Up and Go test, Vit D vitamin D supplementation
Fig. 3.
GRADE Summary of Certainty of Evidence. Legend: a start at low certainty due to non-randomized study designs. b downgraded due to risk of bias. c downgraded due to inconsistency in effects. d downgraded due to indirectness of interventions/outcomes. e downgraded due to imprecision in effect estimate. f downgraded due to publication bias. g upgraded due to large effect. h upgraded due to dose-response relationship. i upgraded due to accounting for confounding
Aerobic capacity
The effect of interventions on aerobic capacity was reported in 15 reviews [27–31, 33, 37, 45, 50, 66, 72–74, 76, 83] (Additional file 4). Across reviews, 109 studies were reported, of which 104 were unique (overlap, 4.6% across intervention types). Aerobic capacity was most often assessed using measured or predicted maximal or peak oxygen consumption (VO2 peak). Based on high-certainty evidence, a combination of aerobic and resistance training results in meaningful improvements in aerobic capacity in older adults. Based on moderate certainty evidence, aerobic exercise probably results in improvements in aerobic capacity. Dance interventions may result in increased aerobic capacity, although this is based on low-certainty evidence and findings may change as more information becomes available. Interventions that combined exercise with nutritional supplements may make little to no difference in aerobic capacity of older adults, although this is based on low-certainty evidence. The evidence is very uncertain about the effect of mind-body exercise, general physical activity, or resistance exercise alone on aerobic capacity in older adults (very low certainty evidence). Other exercise types, including aquatic exercise and a combination of PA and cognitive training, were also examined for their effect on aerobic capacity.
Physical function
In total, 51 reviews [25, 27, 28, 30–40, 42–53, 57–63, 65, 67, 69–77, 79–84, 86] reported on 596 single studies, of which 434 were unique (27.2% overlap across intervention types). Physical function was typically assessed using the Timed Up and Go test, chair stands, gait speed, and six-minute walk test; often findings from single studies were compiled into a composite score for self-reported and/or measured physical function within meta-analyses (Additional file 5). Based on moderate certainty evidence, interventions that included a combination of aerobic and resistance exercise, interventions focused on general PA, and mind-body exercise interventions are all likely to result in improvements in physical function in older adults. Resistance training and dance interventions may also increase physical function (low certainty evidence). Low certainty evidence suggests that aerobic exercise interventions and exercise combined with nutritional supplements may have little to no impact on physical function.
Balance
In total, 30 reviews [27, 31–33, 37–40, 42, 44, 49, 51, 55–57, 59, 60, 62–65, 71, 73–75, 80, 82–84] reported on 275 single studies, of which 226 were unique (17.8% overlap). Static and dynamic balance tests (e.g., single-leg stance, Berg Balance Scale) and composite balance measures were used across reviews (Additional file 6). High certainty evidence suggests that participation in mind-body exercise interventions increases balance in older adults. General PA interventions and interventions that combined aerobic and resistance training are also likely to result in improvements in balance in older adults, based on moderate-certainty evidence. Dance interventions may improve balance; however, this is based on low certainty evidence. Also based on low certainty evidence, resistance training and aerobic exercise alone may result in little to no change in balance. No included reviews explored the effects of exercise and nutritional supplements on balance.
Falls and safety
Number of falls, risk of falling, and fall-related injuries were measured across 14 reviews [27, 28, 38, 40, 44, 56, 59, 60, 62, 63, 69, 72, 73, 82] including 108 single studies, 98 of which were unique (9.3% overlap). Interventions that combine aerobic and resistance exercise and interventions focused on general PA are likely to result in a small reduction in the risk of falls or fall-related injuries in older adults, based on moderate certainty evidence (Additional file 7). Based on low-certainty evidence, mind-body exercises may have little to no meaningful effect on fall risk, although these findings may change as more data are available. Dance interventions and aerobic exercise only may reduce falls, but the evidence is of very low certainty. Also based on very low certainty evidence, resistance training alone may have little to no effect on falls risk. No reviews reported the risk of falls within interventions that combined exercise and nutrition.
Muscle strength
Within reviews reporting muscle strength outcomes, 40 reviews [25–28, 31–33, 36–44, 46, 48, 52, 54, 58–60, 62, 65, 68, 71–76, 78–80, 82–86] reported on 452 single studies, of which 349 were unique (22.8% overlap). Various measures were reported, including handgrip strength, upper body strength, lower body strength, muscle mass, and overall muscle strength (Additional file 8). Both resistance exercise interventions and general PA interventions likely increase upper and lower body strength (moderate certainty evidence). Aerobic exercise alone, combined aerobic and resistance exercise, mind-body exercise, and dance interventions may result in improvements in muscle strength, however, this is based on low certainty evidence and findings may change as more data become available. Also based on low certainty evidence, interventions that combined exercise with nutritional supplements may not improve muscle strength.
Health-related quality of life and self-reported wellbeing
In total, 14 reviews [27, 28, 32, 33, 38, 42, 44, 60, 61, 63, 72, 73, 75, 82] reported health-related quality of life and self-reported wellbeing outcomes (Additional file 9). Given the variation in constructs measured within this domain (e.g., activities of daily living, quality of life (SF-36), perceived mental health) and limited number of reviews for each outcome type, these results were not incorporated into the overall summary of findings using GRADE.
Discussion
We provide a high-level comprehensive synthesis regarding the overall effectiveness of group-based PA and/or nutrition interventions to improve mobility among community-dwelling older adults. Within this review, we take a broad view of mobility, which captures several modifiable risk factors that influence older adults’ ability to move within and beyond their immediate environments [1, 5]. Interventions that combined aerobic and resistance exercise, and general PA interventions were found to result in meaningful improvements in physical function, balance, and muscle strength in older adults and are also likely to reduce falls and fall-related injuries. Mind-body exercise is also effective at improving physical function and balance, as is combined aerobic and resistance exercise for aerobic capacity.
Our findings support a multifaceted approach to health and wellbeing among community-dwelling older adults. Similar findings are reflected in two overviews of reviews focused on all adults over the age of 18, including older adults [87, 88], which informed the recent Canadian 24-Hour Movement Guidelines [89]. These guidelines also recommend a combination of aerobic, resistance, and balance exercises for adults aged 65+. Recent evidence has found that older adults face unique barriers and hesitancy to engage in certain types of exercise, such as resistance training [90]. It is encouraging that benefits for each of our outcome domains were seen across a range of intervention types. This suggests that effective interventions for older adults can incorporate a variety of types of exercises or physical activities that are most likely to foster enjoyment. This notion is consistent with emerging literature regarding the role of intrinsic motivation (i.e., enjoyment in physical activity) as an important predictor of physical activity engagement among older adults [91]. This approach can also improve accessibility to PA within this population by building upon existing community services and group-based PA programs that provide the additional benefit of social participation, which enhances enjoyment, adherence, and sustainability of PA [92]. The importance of social participation for older adults is supported by recent research informed by social-cognitive and socio-emotional theories, suggesting that older adults experiencing social isolation may derive meaningful social benefits from interactions with other participants in group-based exercise programs [93].
Our findings did not provide any convincing evidence for the addition of protein, creatine, vitamin D, or dairy supplementation to PA interventions to improve mobility-related outcomes within community-dwelling older adults. However, the overall quality of the systematic reviews and single studies was low to moderate, and numerous distinct comparator groups were used to test intervention effectiveness. These reviews typically synthesized highly heterogeneous single studies, including a wide range in “dose” of both exercise and dietary supplement components of the interventions; this may have limited the ability to see effects of specific combinations of interventions when synthesized together. Future high-quality studies with similar intervention and comparator groups may provide a better understanding of the role of combined diet and nutrition interventions on mobility-related outcomes in older adults. No reviews focused on group-based nutrition interventions alone, nor did any explore or report on domains of equity, diversity, and inclusion, highlighting priorities for future research.
There are several inherent limitations of this umbrella review that should be considered in interpreting results. Included reviews were limited to those in English, published since 2010. Considering the redundancy in single studies across the reviews dating back as early as 1983, we feel our strategy is robust, captures relevant data from much earlier than 2010, and conclusions are highly unlikely to be changed by older studies that employed less relevant methodologies and practices compared to those used today. Given the large number of included reviews, the overlap in single studies across reviews is unsurprising. The highest amount of overlap of studies evaluating physical function outcomes is attributable to our broad characterization of this outcome and the overlap in single studies among reviews focused on resistance, exercise and nutrition, and dance interventions. Although 28.2% overlap in single studies exists, each review contributing to these results focused on specific outcomes (e.g., gait speed alone, composite physical function measures), and we do not anticipate this greatly influenced our overall certainty of evidence. At the systematic review level, it was not possible to extract specific intervention “doses” and we did not examine single studies to collect this data. Although we would expect targeted aerobic, resistance, or combined aerobic and resistance exercise to be more effective than general PA interventions, certainty in the evidence was influenced by higher risk of bias and heterogeneity across both single studies and reviews of aerobic, resistance, and combined interventions, reflective of variation in types of interventions and tools used to assess outcomes. Finally, changing behaviour is a necessary precursor to changes in mobility-related health outcomes. For example, if an intervention fails to increase physical activity levels of older adults, an improvement in cardiovascular fitness or muscular strength will not occur. An understanding of interventions or techniques that are most effective to change older adults’ physical activity and/or nutrition-related behaviour is an important area of study, particularly when considering sustainability of change beyond the research study. A synthesis of the literature to answer this question is warranted but is outside of the scope of this review.
A strength of this umbrella review was the collaboration with older adults and service provider partners to inform the protocol and identify relevant outcomes. Specifically, the older adult partners involved in this project prioritized the inclusion of quality of life and wellbeing as outcomes of primary importance. The partners voiced that older adults’ self-reported functional measures were likely more meaningful to older adults than measures designed to capture physiology or function. We recognize that objective measures are important as benchmarks; however, we propose that subjective ratings represent a personal participant-relevant domain that could be as, or more, important when considering intervention effectiveness. However, very few reviews reported these outcomes separately as they were commonly combined within meta-analyses, thus we are unable to distinguish between self-reported and objectively measured function.
Conclusion
Group and community-based PA interventions that combine aerobic and resistance, general PA, and mind-body exercise can improve mobility measures in older adults. There was no evidence of benefit for nutritional supplementation with physical activity. No reviews focused on group-based nutrition interventions alone, and very few identified quality of life outcomes, highlighting a need for future synthesis work. The results of this umbrella review will be used to inform the co-design of a community-based, mobility-enhancing intervention.
Supplementary Information
Additional file 2. List of Excluded Studies.
Additional file 3. AMSTAR 2 Critical Appraisal Results.
Additional file 5. Physical Function Outcomes.
Additional file 7. Falls and Safety Outcomes.
Additional file 8. Muscle Strength Outcomes.
Additional file 9. Health-Related Quality of Life and Wellbeing Outcomes.
Additional file 10. PRISMA Systematic Reviews and Meta-Analyses Checklist.
Acknowledgments
Not applicable.
Abbreviations
- AMSTAR 2
A MeaSurement Tool to Assess systematic Reviews
- EMBOLDEN
Enhancing physical and community MoBility in OLDEr adults with health inequities using commuNity co-design trial
- GRADE
Grading of Recommendations Assessment, Development and Evaluation
- JBI
Joanna Briggs Institute
- PA
Physical activity
- RCT
Randomized controlled trial
Authors’ contributions
SNS, CM, DS, DFL, SMP, KBN, EA, AK, CCK, PLS, and RG conceptualized and designed the study. SNS, KT, CM, DS, DFL, GC, and RG acquired, analyzed, and interpreted the data. SNS, KT, and RG drafted the manuscript. All authors substantively revised the manuscript and have approved the submitted version.
Funding
Funding received from the Labarge Centre for Mobility in Aging within the McMaster Institute for Research on Aging at McMaster University, Canada Research Chairs Program, the Canadian Institutes of Health Research, and in-kind support from the Aging, Community and Health Research Unit at McMaster University. The funders had no role in the study design, conduct, or decision to publish.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article and its additional files.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
SMP declares that he is a named inventor on a patent held by Exerkine, but receives no fees/payment, and is an unpaid member of the Scientific Advisory Board for Enhanced Recovery.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Webber SC, Porter MM, Menec VH. Mobility in older adults: a comprehensive framework. Gerontologist. 2010;50(4):443–450. doi: 10.1093/geront/gnq013. [DOI] [PubMed] [Google Scholar]
- 2.Tuscany Regional Health Council. Frailty in elderly people 2013 [cited 2021 May]. Available from: https://www.regione.toscana.it/documents/10180/320308/Frailty+in+elderly+people/9327bb85-6d3c-4e1b-a398-669e76ce5b01?version=1.0.
- 3.Wen YC, Chen LK, Hsiao FY. Predicting mortality and hospitalization of older adults by the multimorbidity frailty index. PLoS One. 2017;12(11):e0187825. doi: 10.1371/journal.pone.0187825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lo AX, Rundle AG, Buys D, Kennedy RE, Sawyer P, Allman RM, et al. Neighborhood disadvantage and life-space mobility are associated with incident falls in community-dwelling older adults. J Am Geriatr Soc. 2016;64(11):2218–2225. doi: 10.1111/jgs.14353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuspinar A, Verschoor CP, Beauchamp MK, Dushoff J, Ma J, Amster E, et al. Modifiable factors related to life-space mobility in community-dwelling older adults: results from the Canadian longitudinal study on aging. BMC Geriatr. 2020;20(1):35. doi: 10.1186/s12877-020-1431-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rikli RE, Jones CJ. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical Independence in later years. Gerontologist. 2013;53(2):255–267. doi: 10.1093/geront/gns071. [DOI] [PubMed] [Google Scholar]
- 7.Milaneschi Y, Tanaka T, Ferrucci L. Nutritional determinants of mobility. Curr Opin Clin Nutr Metab Care. 2010;13(6):625–629. doi: 10.1097/MCO.0b013e32833e337d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization . World Report on Ageing and Health. Geneva: World Health Organization; 2015. [Google Scholar]
- 9.Ramage-Morin PL, Garriguet D. Nutritional risk among older Canadians. Health Rep. 2013;24(3):3–13. [PubMed] [Google Scholar]
- 10.Bandayrel K, Wong S. Systematic literature review of randomized control trials assessing the effectiveness of nutrition interventions in community-dwelling older adults. J Nutr Educ Behav. 2011;43(4):251–262. doi: 10.1016/j.jneb.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 11.Pahor M, Guralnik JM, Ambrosius WT, Blair S, Bonds DE, Church TS, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. 2014;311(23):2387–2396. doi: 10.1001/jama.2014.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young K, Bunn F, Trivedi D, Dickinson A. Nutritional education for community dwelling older people: a systematic review of randomised controlled trials. Int J Nurs Stud. 2011;48(6):751–780. doi: 10.1016/j.ijnurstu.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 13.Landi F, Cesari M, Calvani R, Cherubini A, Di Bari M, Bejuit R, et al. The “sarcopenia and physical fRailty IN older people: multi-componenT treatment strategies” (SPRINTT) randomized controlled trial: design and methods. Aging Clin Exp Res. 2017;29(1):89–100. doi: 10.1007/s40520-016-0715-2. [DOI] [PubMed] [Google Scholar]
- 14.Farrance C, Tsofliou F, Clark C. Adherence to community based group exercise interventions for older people: A mixed-methods systematic review. Prev Med. 2016;87:155–166. doi: 10.1016/j.ypmed.2016.02.037. [DOI] [PubMed] [Google Scholar]
- 15.Neil-Sztramko SE, Teggart K, Phillips S, Sherifali D, Fitzpatrick-Lewis D, Newbold B, et al. An evidence-informed and stakeholder co-designed physical activity and community mobility intervention for older adults facing health inequities: the EMBOLDEN study. Advances in evidence synthesis: special issue. Cochrane Database Syst Rev. 2020;9:21. [Google Scholar]
- 16.Aromataris E, Fernandez R, Godfrey C, Holly C, Khalil H, Tungpunkom P. Chapter 10: Umbrella Reviews. JBI Manual for Evidence Synthesis. 2020. [Google Scholar]
- 17.Jadczak AD, Makwana N, Luscombe-Marsh N, Visvanathan R, Schultz TJ. Effectiveness of exercise interventions on physical function in community-dwelling frail older people: an umbrella review of systematic reviews. JBI Database System Rev Implement Rep. 2018;16(3):752–775. doi: 10.11124/JBISRIR-2017-003551. [DOI] [PubMed] [Google Scholar]
- 18.Moore SA, Hrisos N, Errington L, Rochester L, Rodgers H, Witham M, et al. Exercise as a treatment for sarcopenia: an umbrella review of systematic review evidence. Physiotherapy. 2020;107:189–201. doi: 10.1016/j.physio.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Schultz TJ, Roupas P, Wiechula R, Krause D, Gravier S, Tuckett A, et al. Nutritional interventions for optimizing healthy body composition in older adults in the community: an umbrella review of systematic reviews. JBI Database System Rev Implement Rep. 2016;14(8):257–308. doi: 10.11124/JBISRIR-2016-003063. [DOI] [PubMed] [Google Scholar]
- 20.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–131. [PMC free article] [PubMed] [Google Scholar]
- 21.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR checklist. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Santesso N, Glenton C, Dahm P, Garner P, Akl EA, Alper B, et al. GRADE guidelines 26: informative statements to communicate the findings of systematic reviews of interventions. J Clin Epidemiol. 2020;119:126–135. doi: 10.1016/j.jclinepi.2019.10.014. [DOI] [PubMed] [Google Scholar]
- 25.Antoniak AE, Greig CA. The effect of combined resistance exercise training and vitamin D3 supplementation on musculoskeletal health and function in older adults: a systematic review and meta-analysis. BMJ Open. 2017;7(7):e014619. doi: 10.1136/bmjopen-2016-014619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Borde R, Hortobagyi T, Granacher U. Dose-response relationships of resistance training in healthy old adults: A systematic review and Meta-analysis. Sports Med. 2015;45(12):1693–1720. doi: 10.1007/s40279-015-0385-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bouaziz W, Lang PO, Schmitt E, Kaltenbach G, Geny B, Vogel T. Health benefits of multicomponent training programmes in seniors: a systematic review. Int J Clin Pract. 2016;70(7):520–536. doi: 10.1111/ijcp.12822. [DOI] [PubMed] [Google Scholar]
- 28.Bouaziz W, Vogel T, Schmitt E, Kaltenbach G, Geny B, Lang PO. Health benefits of aerobic training programs in adults aged 70 and over: a systematic review. Arch Gerontol Geriatr. 2017;69:110–127. doi: 10.1016/j.archger.2016.10.012. [DOI] [PubMed] [Google Scholar]
- 29.Bouaziz W, Kanagaratnam L, Vogel T, Schmitt E, Drame M, Kaltenbach G, et al. Effect of aerobic training on peak oxygen uptake among seniors aged 70 or older: A Meta-analysis of randomized controlled trials. Rejuvenation Res. 2018;21(4):341–349. doi: 10.1089/rej.2017.1988. [DOI] [PubMed] [Google Scholar]
- 30.Bruderer-Hofstetter M, Rausch-Osthoff AK, Meichtry A, Munzer T, Niedermann K. Effective multicomponent interventions in comparison to active control and no interventions on physical capacity, cognitive function and instrumental activities of daily living in elderly people with and without mild impaired cognition - A systematic review and network meta-analysis. Ageing Res Rev. 2018;45:1–14. doi: 10.1016/j.arr.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 31.Bueno de Souza RO, Marcon LF, Arruda ASF, Pontes Junior FL, Melo RC. Effects of mat Pilates on physical functional performance of older adults: A Meta-analysis of randomized controlled trials. Am J Phys Med Rehabil. 2018;97(6):414–425. doi: 10.1097/PHM.0000000000000883. [DOI] [PubMed] [Google Scholar]
- 32.Bullo V, Bergamin M, Gobbo S, Sieverdes JC, Zaccaria M, Neunhaeuserer D, et al. The effects of Pilates exercise training on physical fitness and wellbeing in the elderly: A systematic review for future exercise prescription. Prev Med. 2015;75:1–11. doi: 10.1016/j.ypmed.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 33.Bullo V, Gobbo S, Vendramin B, Duregon F, Cugusi L, Di Blasio A, et al. Nordic walking can be incorporated in the exercise prescription to increase aerobic capacity, strength, and quality of life for elderly: A systematic review and Meta-analysis. Rejuvenation Res. 2018;21(2):141–161. doi: 10.1089/rej.2017.1921. [DOI] [PubMed] [Google Scholar]
- 34.Chase JD, Phillips LJ, Brown M. Physical activity intervention effects on physical function among community-dwelling older adults: A systematic review and Meta-analysis. J Aging Phys Act. 2017;25(1):149–170. doi: 10.1123/japa.2016-0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.da Rosa Orssatto LB, de la Rocha FC, Shield AJ, Silveira Pinto R, Trajano GS. Effects of resistance training concentric velocity on older adults’ functional capacity: A systematic review and meta-analysis of randomised trials. Exp Gerontol. 2019;127:110731. doi: 10.1016/j.exger.2019.110731. [DOI] [PubMed] [Google Scholar]
- 36.Devries MC, Phillips SM. Creatine supplementation during resistance training in older adults-a meta-analysis. Med Sci Sports Exerc. 2014;46(6):1194–1203. doi: 10.1249/MSS.0000000000000220. [DOI] [PubMed] [Google Scholar]
- 37.Ebner SA, Meikis L, Morat M, Held S, Morat T, Donath L. Effects of movement-based mind-body interventions on physical fitness in healthy older adults: A Meta-analytical review. Gerontology. 2021;67(2):125–143. doi: 10.1159/000512675. [DOI] [PubMed] [Google Scholar]
- 38.Elboim-Gabyzon M, Buxbaum R, Klein R. The effects of high-intensity interval training (HIIT) on fall risk factors in healthy older adults: A systematic review. Int J Environ Res Public Health. 2021;18(22):11809. doi: 10.3390/ijerph182211809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fernandez-Arguelles EL, Rodriguez-Mansilla J, Antunez LE, Garrido-Ardila EM, Munoz RP. Effects of dancing on the risk of falling related factors of healthy older adults: a systematic review. Arch Gerontol Geriatr. 2015;60(1):1–8. doi: 10.1016/j.archger.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 40.Fernandez-Rodriguez R, Alvarez-Bueno C, Ferri-Morales A, Torres-Costoso A, Pozuelo-Carrascosa DP, Martinez-Vizcaino V. Pilates improves physical performance and decreases risk of falls in older adults: a systematic review and meta-analysis. Physiotherapy. 2021;112:163–177. doi: 10.1016/j.physio.2021.05.008. [DOI] [PubMed] [Google Scholar]
- 41.Finger D, Goltz FR, Umpierre D, Meyer E, Rosa LH, Schneider CD. Effects of protein supplementation in older adults undergoing resistance training: a systematic review and meta-analysis. Sports Med. 2015;45(2):245–255. doi: 10.1007/s40279-014-0269-4. [DOI] [PubMed] [Google Scholar]
- 42.Frost R, Belk C, Jovicic A, Ricciardi F, Kharicha K, Gardner B, et al. Health promotion interventions for community-dwelling older people with mild or pre-frailty: a systematic review and meta-analysis. BMC Geriatr. 2017;17(1):157. doi: 10.1186/s12877-017-0547-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gade J, Pedersen RJ, Beck AM. Effect of protein or essential amino acid supplementation during prolonged resistance exercise training in older adults on body composition, muscle strength, and physical performance parameters: A Systematic Review. Rehabilitation Process Outcome. 2018;7(7):1–12. [Google Scholar]
- 44.Garcia-Hermoso A, Ramirez-Velez R, Saez de Asteasu ML, Martinez-Velilla N, Zambom-Ferraresi F, Valenzuela PL, et al. Safety and effectiveness of long-term exercise interventions in older adults: A systematic review and Meta-analysis of randomized controlled trials. Sports Med. 2020;50(6):1095–1106. doi: 10.1007/s40279-020-01259-y. [DOI] [PubMed] [Google Scholar]
- 45.Grassler B, Thielmann B, Bockelmann I, Hokelmann A. Effects of different exercise interventions on heart rate variability and cardiovascular health factors in older adults: a systematic review. Eur Rev Aging Phys Act. 2021;18(1):24. doi: 10.1186/s11556-021-00278-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hanach NI, McCullough F, Avery A. The impact of dairy protein intake on muscle mass, muscle strength, and physical performance in middle-aged to older adults with or without existing sarcopenia: A systematic review and Meta-analysis. Adv Nutr. 2019;10(1):59–69. doi: 10.1093/advances/nmy065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hortobagyi T, Lesinski M, Gabler M, VanSwearingen JM, Malatesta D, Granacher U. Effects of three types of exercise interventions on healthy old Adults’ gait speed: A systematic review and Meta-analysis. Sports Med. 2015;45(12):1627–1643. doi: 10.1007/s40279-015-0371-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hou L, Lei Y, Li X, Huo C, Jia X, Yang J, et al. Effect of protein supplementation combined with resistance training on muscle mass, strength and function in the elderly: A systematic review and Meta-analysis. J Nutr Health Aging. 2019;23(5):451–458. doi: 10.1007/s12603-019-1181-2. [DOI] [PubMed] [Google Scholar]
- 49.Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C. Exercise for improving balance in older people. Cochrane Database Syst Rev. 2011;(11):CD004963. [DOI] [PMC free article] [PubMed]
- 50.Hurst C, Weston KL, McLaren SJ, Weston M. The effects of same-session combined exercise training on cardiorespiratory and functional fitness in older adults: a systematic review and meta-analysis. Aging Clin Exp Res. 2019;31(12):1701–1717. doi: 10.1007/s40520-019-01124-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hwang PW, Braun KL. The effectiveness of dance interventions to improve older Adults’ health: A systematic literature review. Altern Ther Health Med. 2015;21(5):64–70. [PMC free article] [PubMed] [Google Scholar]
- 52.Katsoulis K, Stathokostas L, Amara CE. The effects of high- versus low-intensity power training on muscle power outcomes in healthy, older adults: A systematic review. J Aging Phys Act. 2019;27(3):422–439. doi: 10.1123/japa.2018-0054. [DOI] [PubMed] [Google Scholar]
- 53.King A, Eitivipart C. Systematic review of published research on aquatic exercise for balance in the elderly. J Aquatic Physical Ther. 2016;24(1):9–21. [Google Scholar]
- 54.Labott BK, Bucht H, Morat M, Morat T, Donath L. Effects of exercise training on handgrip strength in older adults: A Meta-analytical review. Gerontology. 2019;65(6):686–698. doi: 10.1159/000501203. [DOI] [PubMed] [Google Scholar]
- 55.Lesinski M, Hortobagyi T, Muehlbauer T, Gollhofer A, Granacher U. Effects of balance training on balance performance in healthy older adults: A systematic review and Meta-analysis. Sports Med. 2015;45(12):1721–1738. doi: 10.1007/s40279-015-0375-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Leung DP, Chan CK, Tsang HW, Tsang WW, Jones A. Tai chi as an intervention to improve balance and reduce falls in older adults: A systematic and meta-analytical review. Altern Ther Health Med. 2011;17(1):40–48. [PubMed] [Google Scholar]
- 57.Levin O, Netz Y, Ziv G. The beneficial effects of different types of exercise interventions on motor and cognitive functions in older age: a systematic review. Eur Rev Aging Phys Act. 2017;14:20. doi: 10.1186/s11556-017-0189-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liberman K, Forti LN, Beyer I, Bautmans I. The effects of exercise on muscle strength, body composition, physical functioning and the inflammatory profile of older adults: a systematic review. Curr Opin Clin Nutr Metab Care. 2017;20(1):30–53. doi: 10.1097/MCO.0000000000000335. [DOI] [PubMed] [Google Scholar]
- 59.Liu H, A. F. Tai chi as a balance improvement exercise for older adults: a systematic review. J Geriatr Phys Ther. 2010;33(3):103–109. [PubMed] [Google Scholar]
- 60.Liu CJ, Chang WP, Araujo de Carvalho I, Savage KEL, Radford LW, Amuthavalli TJ. Effects of physical exercise in older adults with reduced physical capacity: meta-analysis of resistance exercise and multimodal exercise. Int J Rehabil Res. 2017;40(4):303–314. doi: 10.1097/MRR.0000000000000249. [DOI] [PubMed] [Google Scholar]
- 61.Liu X, Shen PL, Tsai YS. Dance intervention effects on physical function in healthy older adults: a systematic review and meta-analysis. Aging Clin Exp Res. 2021;33(2):253–263. doi: 10.1007/s40520-019-01440-y. [DOI] [PubMed] [Google Scholar]
- 62.Loureiro V, Gomes M, Loureiro N, Aibar-Almazan A, Hita-Contreras F. Multifactorial programs for healthy older adults to reduce falls and improve physical performance: systematic review. Int J Environ Res Public Health. 2021;18(20):10842. doi: 10.3390/ijerph182010842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Martin JT, Wolf A, Moore JL, Rolenz E, DiNinno A, Reneker JC. The effectiveness of physical therapist-administered group-based exercise on fall prevention: a systematic review of randomized controlled trials. J Geriatr Phys Ther. 2013;36(4):182–193. doi: 10.1519/JPT.0b013e3182816045. [DOI] [PubMed] [Google Scholar]
- 64.Martins AC, Santos C, Silva C, Baltazar D, Moreira J, Tavares N. Does modified Otago exercise program improves balance in older people? A systematic review Prev Med Rep. 2018;11:231–239. doi: 10.1016/j.pmedr.2018.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Meereis-Lemos ECW, Guadagnin EC, CB M. Influence of strength training and multicomponent training on the functionality of older adults: systematic review and meta-analysis. Rev Bras de Cineantropometria & Desempenho Humano. 2020;22:e60707. doi: 10.1590/1980-0037.2020v22e6070. [DOI] [Google Scholar]
- 66.Montero D, Diaz-Canestro C. Endurance training and maximal oxygen consumption with ageing: role of maximal cardiac output and oxygen extraction. Eur J Prev Cardiol. 2016;23(7):733–743. doi: 10.1177/2047487315617118. [DOI] [PubMed] [Google Scholar]
- 67.Moore M, Warburton J, O'Halloran PD, Shields N, Kingsley M. Effective community-based physical activity interventions for older adults living in rural and regional areas: A systematic review. J Aging Phys Act. 2016;24(1):158–167. doi: 10.1123/japa.2014-0218. [DOI] [PubMed] [Google Scholar]
- 68.Moran J, Ramirez-Campillo R, Granacher U. Effects of jumping exercise on muscular power in older adults: A Meta-analysis. Sports Med. 2018;48(12):2843–2857. doi: 10.1007/s40279-018-1002-5. [DOI] [PubMed] [Google Scholar]
- 69.Nicolson PJA, Duong V, Williamson E, Hopewell S, Lamb SE. The effect of therapeutic exercise interventions on physical and psychosocial outcomes in adults aged 80 years and older: A systematic review and Meta-analysis. J Aging Phys Act. 2022;30(3):517–34. [DOI] [PubMed]
- 70.Plummer P, Zukowski LA, Giuliani C, Hall AM, Zurakowski D. Effects of physical exercise interventions on gait-related dual-task interference in older adults: A systematic review and Meta-analysis. Gerontology. 2015;62(1):94–117. doi: 10.1159/000371577. [DOI] [PubMed] [Google Scholar]
- 71.Qi M, Moyle W, Jones C, Weeks B. Tai chi combined with resistance training for adults aged 50 years and older: A systematic review. J Geriatr Phys Ther. 2020;43(1):32–41. doi: 10.1519/JPT.0000000000000218. [DOI] [PubMed] [Google Scholar]
- 72.Raymond MJ, Bramley-Tzerefos RE, Jeffs KJ, Winter A, Holland AE. Systematic review of high-intensity progressive resistance strength training of the lower limb compared with other intensities of strength training in older adults. Arch Phys Med Rehabil. 2013;94(8):1458–1472. doi: 10.1016/j.apmr.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 73.Rodrigues-Krause J, Krause M, Reischak-Oliveira A. Dancing for healthy aging: functional and metabolic perspectives. Altern Ther Health Med. 2019;25(1):44–63. [PubMed] [Google Scholar]
- 74.Roland KP, Jakobi JM, GR. J. Does yoga engender fitness in older adults? A critical review. J Aging Phys Act. 2011;19(1):62–79. doi: 10.1123/japa.19.1.62. [DOI] [PubMed] [Google Scholar]
- 75.Sivaramakrishnan D, Fitzsimons C, Kelly P, Ludwig K, Mutrie N, Saunders DH, et al. The effects of yoga compared to active and inactive controls on physical function and health related quality of life in older adults- systematic review and meta-analysis of randomised controlled trials. Int J Behav Nutr Phys Act. 2019;16(1):33. doi: 10.1186/s12966-019-0789-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Stares A, Bains M. The additive effects of Creatine supplementation and exercise training in an aging population: A systematic review of randomized controlled trials. J Geriatr Phys Ther. 2020;43(2):99–112. doi: 10.1519/JPT.0000000000000222. [DOI] [PubMed] [Google Scholar]
- 77.Stathokostas L, Little RM, Vandervoort AA, Paterson DH. Flexibility training and functional ability in older adults: a systematic review. J Aging Res. 2012;2012(306818):1–13. doi: 10.1155/2012/306818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Straight CR, Lindheimer JB, Brady AO, Dishman RK, Evans EM. Effects of resistance training on lower-extremity muscle power in middle-aged and older adults: A systematic review and Meta-analysis of randomized controlled trials. Sports Med. 2016;46(3):353–364. doi: 10.1007/s40279-015-0418-4. [DOI] [PubMed] [Google Scholar]
- 79.Ten Haaf DSM, Nuijten MAH, Maessen MFH, Horstman AMH, Eijsvogels TMH, Hopman MTE. Effects of protein supplementation on lean body mass, muscle strength, and physical performance in nonfrail community-dwelling older adults: a systematic review and meta-analysis. Am J Clin Nutr. 2018;108(5):1043–1059. doi: 10.1093/ajcn/nqy192. [DOI] [PubMed] [Google Scholar]
- 80.Tschopp M, Sattelmayer MK, Hilfiker R. Is power training or conventional resistance training better for function in elderly persons? A meta-analysis. Age Ageing. 2011;40(5):549–556. doi: 10.1093/ageing/afr005. [DOI] [PubMed] [Google Scholar]
- 81.Van Abbema R, De Greef M, Craje C, Krijnen W, Hobbelen H, Van Der Schans C. What type, or combination of exercise can improve preferred gait speed in older adults? A meta-analysis BMC Geriatr. 2015;15:72. doi: 10.1186/s12877-015-0061-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Vetrovsky T, Steffl M, Stastny P, Tufano JJ. The efficacy and safety of lower-limb plyometric training in older adults: A systematic review. Sports Med. 2019;49(1):113–131. doi: 10.1007/s40279-018-1018-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Waller B, Ogonowska-Słodownik A, Vitor M, Rodionova K, Lambeck J, Heinonen A, et al. The effect of aquatic exercise on physical functioning in the older adult: a systematic review with meta-analysis. Age Ageing. 2016;45(5):593–601. doi: 10.1093/ageing/afw102. [DOI] [PubMed] [Google Scholar]
- 84.Wang C, Liang J, Si Y, Li Z, Lu A. The effectiveness of traditional Chinese medicine-based exercise on physical performance, balance and muscle strength among older adults: a systematic review with meta-analysis. Aging Clin Exp Res. 2022;34(4):25–740. [DOI] [PubMed]
- 85.Wirth J, Hillesheim E, Brennan L. The role of protein intake and its timing on body composition and muscle function in healthy adults: A systematic review and Meta-analysis of randomized controlled trials. J Nutr. 2020;150(6):1443–1460. doi: 10.1093/jn/nxaa049. [DOI] [PubMed] [Google Scholar]
- 86.Yang Y-P, Lin H-C, Chen K-M. Functional fitness in older adults. Topics Geriatric Rehabilitation. 2019;35(4):238–247. doi: 10.1097/TGR.0000000000000241. [DOI] [Google Scholar]
- 87.McLaughlin EC, El-Kotob R, Chaput JP, Janssen I, Kho ME, Poitras VJ, et al. Balance and functional training and health in adults: an overview of systematic reviews. Appl Physiol Nutr Metab. 2020;45(10 (Suppl. 2)):S180–SS96. doi: 10.1139/apnm-2020-0279. [DOI] [PubMed] [Google Scholar]
- 88.El-Kotob R, Ponzano M, Chaput JP, Janssen I, Kho ME, Poitras VJ, et al. Resistance training and health in adults: an overview of systematic reviews. Appl Physiol Nutr Metab. 2020;45(10 (Suppl. 2)):S165–SS79. doi: 10.1139/apnm-2020-0245. [DOI] [PubMed] [Google Scholar]
- 89.Ross R, Chaput JP, Giangregorio LM, Janssen I, Saunders TJ, Kho ME, et al. Canadian 24-hour movement guidelines for adults aged 18-64 years and adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2020;45(10 (Suppl. 2)):S57–S102. doi: 10.1139/apnm-2020-0467. [DOI] [PubMed] [Google Scholar]
- 90.Burton E, Farrier K, Lewin G, Pettigrew S, Hill AM, Airey P, et al. Motivators and barriers for older people participating in resistance training: A systematic review. J Aging Phys Act. 2017;25(2):311–324. doi: 10.1123/japa.2015-0289. [DOI] [PubMed] [Google Scholar]
- 91.Labudek S, Fleig L, Jansen CP, Kramer-Gmeiner F, Nerz C, Becker C, et al. Applying social cognition models to explain walking duration in older adults: the role of intrinsic motivation. J Aging Phys Act. 2021;29(5):744–752. doi: 10.1123/japa.2020-0296. [DOI] [PubMed] [Google Scholar]
- 92.Devereux-Fitzgerald A, Powell R, Dewhurst A, French DP. The acceptability of physical activity interventions to older adults: A systematic review and meta-synthesis. Soc Sci Med. 2016;158:14–23. doi: 10.1016/j.socscimed.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 93.Steckhan GMA, Warner LM, Fleig L. Preventing falls together: social identification matters for engaging older adults in a group-based exercise program. Act Adapt Aging. 2022;46(1):31–45. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 2. List of Excluded Studies.
Additional file 3. AMSTAR 2 Critical Appraisal Results.
Additional file 5. Physical Function Outcomes.
Additional file 7. Falls and Safety Outcomes.
Additional file 8. Muscle Strength Outcomes.
Additional file 9. Health-Related Quality of Life and Wellbeing Outcomes.
Additional file 10. PRISMA Systematic Reviews and Meta-Analyses Checklist.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article and its additional files.