Abstract
Anxiety disorders form the most common group of mental disorders and generally start before or in early adulthood. Core features include excessive fear and anxiety or avoidance of perceived threats that are persistent and impairing. Anxiety disorders involve dysfunction in brain circuits that respond to danger. Risk for anxiety disorders is influenced by genetic factors, environmental factors, and their epigenetic relations. Anxiety disorders are often comorbid with one another and with other mental disorders, especially depression, as well as with somatic disorders. Such comorbidity generally signifies more severe symptoms, greater clinical burden, and greater treatment difficulty. Reducing the large burden of disease from anxiety disorders in individuals and worldwide can be best achieved by timely, accurate disease detection and adequate treatment administration, scaling up of treatments when needed. Evidence-based psychotherapy (particularly cognitive behavioural therapy) and psychoactive medications (particularly serotonergic compounds) are both effective, facilitating patients’ choices in therapeutic decisions. Although promising, no enduring preventive measures are available, and, along with frequent therapy resistance, clinical needs remain unaddressed. Ongoing research efforts tackle these problems, and future efforts should seek individualised, more effective approaches for treatment with precision medicine.
Introduction
Anxiety disorders form the most common type of mental illness. Anxiety disorders comprise separation anxiety and selective mutism (occurring primarily in childhood; between the ages of 4 years and 18 years), specific phobias, social anxiety disorder, and generalised anxiety disorder (occurring in childhood as well as in adulthood), as well as panic disorder and agoraphobia (occurring primarily in adulthood; from the age of 18 years and older). High prevalence, chronicity, and comorbidity led WHO to rank anxiety disorders as the ninth most health-related cause of disability.1 Worldwide, anxiety disorders heavily affect patients and society, accounting for 3·3% of the global burden of disease and costing approximately €74 billion for 30 European countries.2 Globally, the use of treatment for anxiety disorders is low, which is most problematic in low-income countries but is also an issue in high-income countries.3
Clinical presentation
Fear is a conscious feeling evoked by threat or impending danger, whereas anxiety involves anticipation of real or imagined future threat or danger. Both fear and anxiety facilitate survival and are often adaptive. As such, many fears and anxieties represent normative occurrences in childhood (eg, stranger or performance anxiety) or in adulthood (eg, anxiety during life stress or transitions).
Fears and anxieties can require clinical attention when they are disproportionate to a threat, are severe and enduring, or disrupt normal functioning. Perceived threats include environmental stimuli (eg, a social situation or health risk), signalling to the individual that they might be in danger. This signalling also includes interoceptive stimuli (eg, palpitations or shortness of breath). The main classification schemes, the fifth edition of Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the 11th edition of International Classification of Diseases (ICD-11), define anxiety disorders on the basis of similar key symptoms (table 1).
Table 1:
Core diagnostic features and characteristics for anxiety disorders
| Selective mutism | Separation anxiety | Specific phobia | Social anxiety disorder | Agoraphobia | Panic disorder | Generalised anxiety disorder | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Core emotions or cognitions | Consistent failure to speak in situations for which there is an expectation to speak, despite language competence | Unrealistic, persistent fear or anxiety about separation from, or loss of, attachment figure, or adverse events occurring to them | Marked, excessive, and unreasonable fear or anxiety of circumscribed objects or situations (eg, animals, natural forces, blood injection, or places) | Marked, excessive, and unreasonable fear or anxiety of scrutiny or negative judgement by other people | Marked, excessive, and concerning fear of leaving home, entering closed or open public places, crowds, or transportation | Recurrent, unexpected panic attacks with sustained mental (eg, fear, fear of losing control, or feeling of alienation) manifestations | Marked, uncontrollable, and anxious worry and fears about everyday events and problems |
| Physical symptoms | No physical symptoms | Nightmares and symptoms of distress | No physical symptoms | Blushing, fear of vomiting, urgency or fear of micturition or defaecation | No physical symptoms | Multiple symptoms (eg, palpitations, dyspnoea, diaphoresis, chest pain, dizziness, paraesthesia, or nausea) | Restlessness, fatigue, irritability, difficulty concentrating, muscle tension, sleep disturbance, or autonomic arousal |
| Behaviour | Disturbance interferes with (educational) achievement or social communication | Reluctance to leave attachment figure; disturbance impairs social, school, or other functioning | Avoidance of circumscribed objects or situations; disturbance impairs social, school, work, or other functioning | Avoidance of social interactions and situations; disturbance impairs social, school, work, or other functioning | Avoidance of fear-inducing situations; disturbance impairs social, school, work, or other functioning | Changed behaviour in maladaptive ways related to the attacks; disturbance impairs social, school, work or other functioning | Disturbance impairs social, school, work, or other functioning |
| Required symptom duration | >1 month (beyond first school month) | >1 month (childhood; 4–18 years); >6 months (adulthood; 18 years or older) | >6 months | >6 months | >6 months | >1 month | >6 months |
| Median age of onset | Childhood (<5 years) | Childhood ( around 6 years) | Childhood (around 8 years) | Early adolescence (around 13 years) | Late adolescence (around 20 years) | Adulthood (around 25 years) | Adulthood (around 30 years) |
Characteristics and features for anxiety disorders were based on criteria from the Diagnostic and Statistical Manual of Mental Disorders (fifth edition) and International Classification of Diseases (11th edition).
Categorical diagnostic criteria are clinically useful, but boundaries between anxiety disorders and normative anxiety are often ill-defined. Recognition of distinctions requires clinical judgement of severity, duration, persistence, and, importantly, degree of distress and impairment. Symptoms can occur without distress and impairment, including cases of specific phobias for which people never encounter their feared objects (eg, snakes). In this instance, medical attention is generally not needed. Conversely, anxiety symptoms and panic attacks commonly occur in attenuated forms, supporting dimensional over categorical approaches for diagnoses. For example, isolated panic attacks do not meet the criteria (DSM-5 or ICD-11) for a panic disorder; however, these attacks have been shown to impair functioning and increase the risk for various other mental disorders.4 Consequently, panic attacks deserve attention as a separate dimension across mental disorders.
Symptoms are generally not pathognomonic of individual anxiety disorders, and anxiety disorder comorbidity is substantial: 48–68% of adults with one anxiety disorder fulfil the criteria for another concurrent anxiety disorder.5 Comorbidity is higher in clinical settings than in community settings because individuals with concomitant disorders are more likely to seek treatment. Also, longitudinal diagnostic instability within anxiety disorders is high,6 showing frequent sequential comorbidity as well as possible shared causes.
Anxiety disorders, which are the most common type of mental disorders in children, represent the earliest of all forms of mental illness. Mostly due to separation anxiety, a specific phobia, or social anxiety disorder, the onset of any anxiety disorder is usually in childhood, and thus considerably earlier than, for example, depressive or substance use disorders. Generalised anxiety disorder, agoraphobia, and panic disorder exhibit more age-of-onset heterogeneity and sometimes present later in life.
Clarification of anxiety-associated cognitions and behaviours could show prevailing diagnoses. Avoidance of social interaction could suggest separation anxiety (if the predominant fear is for losing attachment; figure 1), panic disorder (if fear is for panic attacks), social anxiety disorder (if fear is for scrutiny by others), or agoraphobia (if fear is for entrapment). Fulfilling multiple anxiety disorder diagnoses could partly reflect artefacts of classification systems, but it also holds prognostic importance because people with multiple disorders have higher severity, disability, and a poorer disease course compared with people who have a single anxiety disorder.7,8 A full clinical assessment is paramount as it guides treatment selection.
Figure 1: Visual representation of components of the brain’s threat-responsive circuitry.
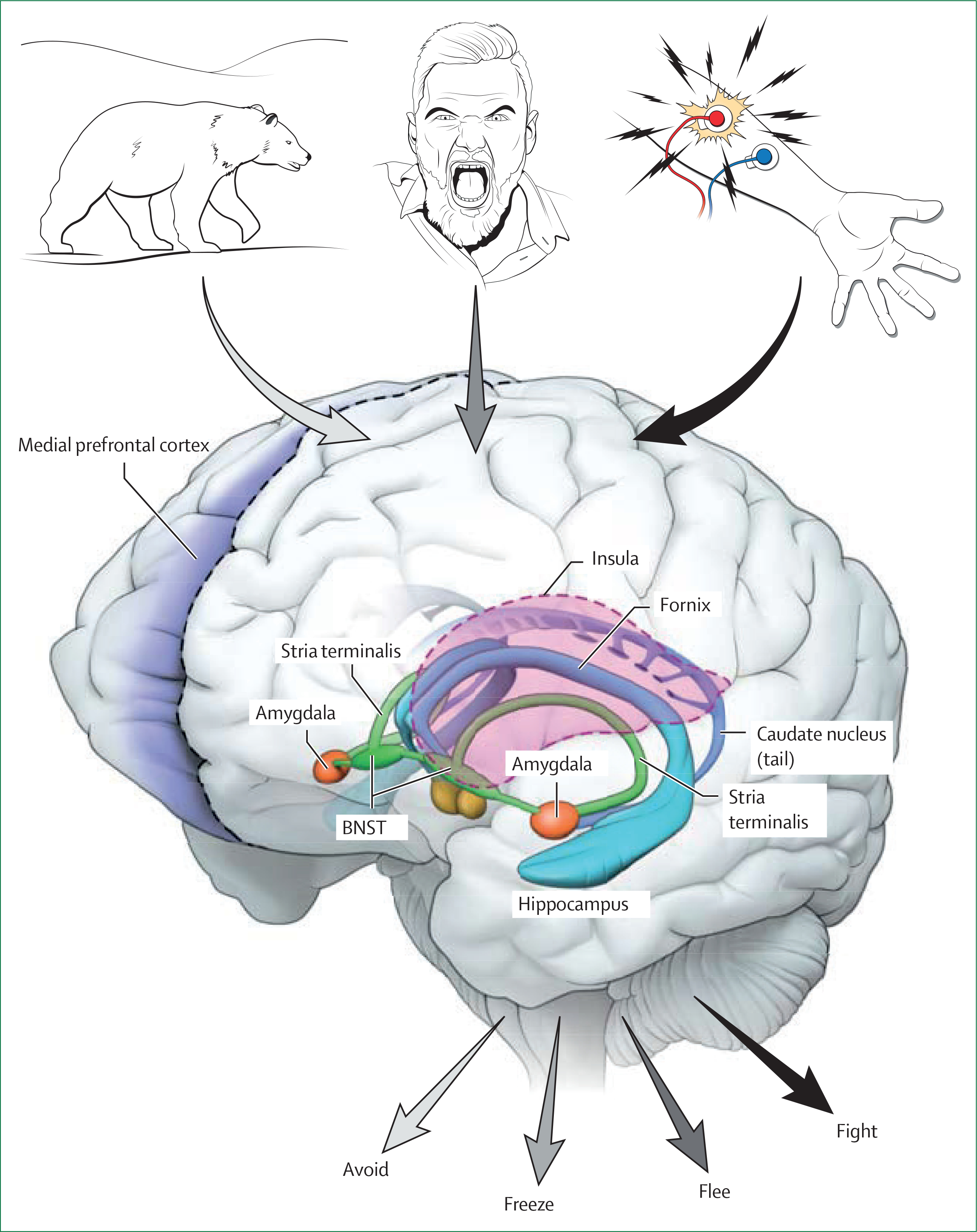
Threats are classified on the basis of proximity, with the top of the figure showing a threat continuum, including distant predators, an approaching threatening person, or a direct encounter with painful stimuli. Components of the brain’s circuitry involved in threat responses appear in distinct colours, with the hippocampus in blue, stria terminalis and its bed nucleus in green, amygdala in red, and frontal regions, including the medial prefrontal cortex and insula, in purple. These circuitry components interact in unique ways depending on the nature of threats, thereby generating adaptive defensive responses shown at the bottom of the figure, including avoidance, freezing, fleeing, and fighting. BNST=bed nucleus of the stria terminalis.
Detection and diagnostic methods
Because anxiety disorders are underdiagnosed in all care settings,3 clinicians should monitor their occurrence. Monitoring is particularly important because patients who have anxiety disorders often present symptoms other than clear anxiety symptoms: for instance, patients who have panic disorder could present in general care settings or emergency care settings with presumed cardiac or respiratory problems. Given that patients who have anxiety disorders are mostly seen in primary care, clinicians should be aware of these conditions to initiate proper treatment or refer to a specialist, if needed. Because no blood, genetic, or imaging biomarkers exist, diagnosis rests on mental-state history and examinations, which should therefore be sufficiently monitored by every primary care practitioner. Validated, structured, or semi-structured clinical interviews, such as the DSM-5-based or ICD-11-based composite international diagnostic interview9 or structured clinical interview for DSM disorders,10 can assist in correct diagnostics. In children, interviews such as the Kiddie-SADS11 require additional assessment of parents or caregivers. To determine the severity of anxiety disorders and monitor treatment, continuous clinician-rated scales include, for example, the Hamilton Anxiety Scale.12 Validated self-report scales exist for relevant dimensional anxiety disorder aspects: examples include the Beck Anxiety Inventory for panic symptoms,13 the Fear Questionnaire for phobia symptoms,14 the Penn State Worry Questionnaire for generalised anxiety disorder symptoms,15 and the Anxiety Sensitivity Index for general fear and arousal-related sensations.16 Standardised diagnostics and assessments for outcome monitoring are part of evidence-based care, could prevent underdiagnosis, and lead to effective treatments. However, these diagnostics and assessments are still not widely used in clinical practice.
Screeners comprising only a few items, such as the Generalised Anxiety Disorder-7 scale, have adequate sensitivity and specificity for detecting generalised anxiety disorder but also other anxiety disorders.17 However, structural implementation of anxiety screeners in various settings anxiety screening in various settings has yet to be proven efficacious and cost-effective.
Comorbidity and differential diagnosis
Pathological anxiety occurs in many mental and somatic disorders along with anxiety disorders. For any patient presenting with increased pathological anxiety, a thorough psychiatric and somatic evaluation should consider whether symptoms reflect other health conditions or effects of substance or medication use. The most common psychiatric comorbidity is major depressive disorder: half to two-thirds of adults with anxiety disorders also suffer from this diagnosis.5 Among more than 3 million Danish people, anxiety disorder increased the incidence of depression by three to five times.18 Anxiety and depression share clinical symptoms and causes due to genetic pleiotropy and share psychological, social, and neurobiological risk mechanisms. Anxiety and depression comorbidity signifies higher disorder severity, burden, and chronicity compared with individual disorders.19 Consequently, it is often less a matter of identifying a differential diagnosis, but rather assigning multiple diagnoses and prioritising more intensive management for the patient with comorbidities. Anxiety disorder also co-occurs with bipolar disorder or substance dependence disorder, and obsessive-compulsive disorder and post-traumatic stress disorder, which in previous, but not current, ICD and DSM classifications were considered anxiety disorders (table 2). Anxiety disorder comorbidity often signals severity. In such patients, anxiety should be treated in its own right, with the understanding that additional interventions will be needed to address the specific comorbidity.
Table 2:
Mental and somatic disorders that are frequently comorbid or difficult to distinguish in anxiety disorder
| Examples of overlapping symptoms | Key clinical insights to recognise | |
|---|---|---|
|
| ||
| Mental disorders | ||
| Major depressive disorder | Fatigue, anxiety, worry, or agitation | Major depressive disorder is the highest comorbidity in anxiety disorder and associated with higher severity, suicidality, disability and chronicity;19 clinicians must comprehensively assess because major depressive disorder comorbidity requires more intensive pharmacological treatment and a different form of psychotherapy treatment (eg, cognitive behavioural therapy for depression rather than for anxiety disorder) |
| Bipolar disorder | Agitation, irritability, or racing thoughts | Anxiety is often present in bipolar disorder and is associated with rapid cycling;20 targeting anxiety could aid in mood stabilisation; bipolar disorder requires focus on mood stabilisation and considerate use of medication, which could induce mania (especially antidepressants) |
| Obsessive-compulsive disorder* | Extreme worry or inability to relax | People who have obsessive-compulsive disorder engage in ritualistic, repetitive behaviour to deal with their fears, which is absent in anxiety disorder; these people often realise that their behaviour is irrational and inappropriate |
| Post-traumatic stress disorder* | Avoidance, hyperarousal, or anxiety-laden intrusive memories | The intense experience of anxiety in post-traumatic stress disorder is specifically in response to a psychological trauma (eg, abuse, war, or accident); specific psychotherapies focused on the trauma associated with the post-traumatic stress disorder should be used |
| Health anxiety* (hypochondriasis) | Anxiety or worry from bodily responses | Anxiety is specifically related to preoccupation with having or acquiring a serious, undiagnosed medical illness |
| Substance use (eg, illicit drugs, alcohol, or benzodiazepines) disorder | Tremor, sweating, palpitations, or panic attacks (during withdrawal or in some cases intoxication) | When suspected, clinicians should conduct a psychiatric interview of substance use disorders, with potential breath, urine, or plasma drug screening; comorbidity of alcohol or benzodiazepine abuse with anxiety disorder is considerable |
| Somatic disorders | ||
| Cardiac disease | Chest pain or palpitations (which is also common in panic disorder) | Clinical evaluation, including electrocardiogram, assessment of plasma troponin concentration, or Holter monitoring |
| Thyroid disease (eg, hyperthyroidism) | Palpitations, tremor, panic attacks, or persistent anxiety | Laboratory assessment of plasma thyroid-stimulating hormone |
| Respiratory disease (eg, asthma) | Shortness of breath | Clinical evaluation with a pulmonary function test |
| Phaeochromocytoma or other disorders that result in a sudden blood pressure increase | Panic attacks or bodily sensations | Blood pressure monitoring over 24 h or hormone assessment (eg, in blood or urine) |
| Epilepsy | Anxiety symptoms as part of aura or start of seizure | Clinical evaluation or neurological referral when the causes of symptoms are unclear |
In previous classifications of the Diagnostic and Statistical Manual of Mental Disorders and International Classification of Diseases, these disorders were included in the classification of anxiety disorders. In current classifications (eg, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders and the 11th edition of the International Classification of Diseases), they are integrated in different classifications.
Patients with diverse somatic illnesses, including cardiovascular, respiratory, or musculoskeletal disease, have an increased risk of comorbid anxiety. Because certain symptoms are overlapping between an anxiety and somatic diagnosis, there is a risk of diagnostic confusion and potential under or over diagnosis and mismanagement (table 2). The value of distinguishing between primary and secondary anxiety is unclear because there is growing evidence that the link between somatic illness and anxiety is bidirectional, and anxiety treatment is needed regardless. The presence of anxiety in cardiac disease,21 cancer,22 or pulmonary disease23 has been shown to negatively affect quality of life, adherence to treatment, prognosis, and treatment costs. These findings indicate that proper detection and management of anxiety disorder comorbidity is also imperative for patients with somatic illnesses.
Epidemiology
Due to methodological differences, estimates of anxiety disorder prevalence in populations vary widely across large-scale studies (table 3).33 At late adolescence and early adulthood (aged 15–25 years), the cumulative prevalence of all anxiety disorders combined ranges between 20% and 30%.24,25 This finding suggests that one out of three to five children and adolescents have an anxiety disorder at some point in their childhood, although not always severe or requiring medical attention. In adulthood, 10%–14% of the population fulfil the DSM criteria for anxiety disorder within a year (table 3), most commonly specific phobia, followed by social anxiety disorder and panic disorder or agoraphobia. The 1-year prevalence of anxiety disorders is highest in people aged between 18 years and 25 years. The few methodologically sound studies of time trends show no evidence of increased anxiety prevalence over the past two decades.32,34 However, awareness, seeking of, and provision of treatment has increased,32,34 possibly explaining views of the growing effect of anxiety disorders.
Table 3:
Prevalence estimates of anxiety disorder in large-scale studies across age groups
| GSMS of children followed up through to early adulthood, cumulatively over 3 waves (26 years; n=1420)24 | TRAILS of adolescents (19 years; n=1584)25* |
WMH Surveys of adults (≥18 years; n=around 150 000)26–31*† |
Meta-analysis of adults (≥18 years)32‡ |
|||||
|---|---|---|---|---|---|---|---|---|
| 1 year | Cumulative | 1 year | Lifetime | Prevalence ratio of female : male | 1 year | Prevalence ratio of female : male | ||
| Selective mutism | ··§ | ··§ | ··§ | ··§ | ··§ | ·· | ··§ | ·· |
| Separation anxiety | 5·0 | 0·3 | 3·1 | 1·0 | 4·8 | 1·4 | ·· | ·· |
| Specific phobia | 2·2 | 9·0 | 11·5 | 5·5 | 7·4 | 2·0 | 6·4 | 2·4 |
| Social anxiety disorder | 4·2 | 7·5 | 12·4 | 2·4 | 4·0 | 1·3 | 2·3 | 2·1 |
| Agoraphobia | 6·1 | 0·7 | 1·0 | 1·0 | 1·5 | 1·9 | 2·0 | 3·1 |
| Panic disorder | 4·8 | 1·3 | 1·6 | 1·0 | 1·7 | 2·0 | 1·8 | 1·8 |
| Generalised anxiety disorder | 9·7 | 1·8 | 2·9 | 1·8 | 3·7 | 1·8 | 1·7 | 2·1 |
| All anxiety disorders | 27·0 | 18·4 | 28·0 | 9·8 | ·· | ·· | 14·0 | 2·1 |
··=not examined or reported.
Diagnostic and Statistical Manual of Mental Disorders (fifth edition) Composite International Diagnostic Interview.
From 25 countries.
Including 12–18 European studies.
Expected prevalence is <1·0%.
In large-scale World Mental Health Surveys done in 27 countries, anxiety disorder prevalence was highest in high-income countries.26–29 Whether this finding reflects true regional or cultural differences, problems with diagnostic criteria, or differences in symptom reporting is unclear.35 However, stable sociodemographic correlates exist across nations. Importantly, anxiety disorders are 1·3–2·4 times more prevalent in women than in men,26–31,33 which is accentuated during development and evident after adolescence. Anxiety disorders are also more common in people with unmarried status, low education, low income, and those who are unemployed.26–31
Epidemiological studies show a relatively high ratio of 1 year to lifetime prevalence for anxiety disorders, indicative of a chronic recurrent nature. Prospective studies,7,19,36 show that patients who have anxiety disorders could have symptoms for years. Among patients with only one anxiety disorder, 2 year remission rates were around 70% for panic disorder without agoraphobia and generalised anxiety disorder, decreasing to 50–55% for social anxiety disorder and panic disorder with agoraphobia and 43% for those with multiple anxiety disorders.7 A previous study showed that symptoms of anxiety and avoidance improved in only 309 (44%) of 703 patients over 6 years.36Beyond the adverse mental health effects, anxiety disorders can predict unstable relationships, poorer functioning, and higher work absenteeism than in people who do not have these disorders,37,38 with major economic costs and effects on somatic health. Risk of death has been shown to be increased by 1·4 times by natural causes and increased by 2·5 times by unnatural causes.39 Anxiety has consistently been linked with an increased risk of subsequent cardiovascular disease (hazard ratio 1·5),40 with emerging evidence of increased onset risk of other somatic conditions, including stroke, diabetes, arthritis, and lung disease than in the general population.41 Suggested mechanisms of higher comorbid anxiety in persons with somatic illnesses comprise unhealthy lifestyles, low treatment adherence, and dys-regulations of psychobiological stress systems. Therefore, attention to somatic health should be optimally integrated early on in the treatment of anxiety disorders.
Pathophysiology
Genetics
Heritability of anxiety disorders can vary, but heritability estimates converge to rates of between around 35% for generalised anxiety disorder and around 50% for social anxiety disorder, panic disorder, and agoraphobia.42 The mode of inheritance is complex, with many genetic variants of small effect interacting with, or adding to, other (presumably non-shared environmental) risk factors. The genetic basis of anxiety disorders overlaps not only within the different disorders but also with the non-pathological anxiety dimension, suggesting at least a partial continuum from normal to pathological anxiety. However, the substantial heritability and thus familial aggregation of anxiety disorders suggests that thorough recording of family history during the diagnostic process is required.
Until 2010, molecular genetic research has focused on candidate genes, especially genes relevant in monoaminergic neurotransmission or stress axis function. However, a meta-analysis of candidate genes43 only showed an association of panic disorder with TMEM132D gene variants and, in subsamples, with HTR2A, NPSR1, and MAOA genes.
The advent of low-cost genotyping has shifted research towards genome-wide association studies. The first and underpowered genome-wide association studies yielded none or only few genome-wide significant loci.44–47 When anxiety was examined as a dimension with the use of the Generalised Anxiety Disorder 2-item scale in 2 million people,48 only five genome-wide significant loci were identified. Another genome-wide association study49 used a dimensional agoraphobic symptom score and related the top hit, in the gene encoding the potentially druggable GLRB, to panic disorder and intermediate phenotypes. Few studies have examined copy number variants (ie, larger parts of the genome that are duplicated or deleted). A recent study in children50 suggested that the presence of copy number variants associated with a high risk for neurodevelopmental disorders increases the risk of anxiety disorders by three times. Overall, no converging pathways can yet be derived from these initial genome-wide association studies. However, genome-wide association studies showed a high genetic correlation (rG>0·6) among people with anxiety, depression, and neuroticism,44–46,51 which suggests shared genetic risks and supports the existence of a general genetic risk factor for mental disorders (p factor) that could explain the high comorbidity between most mental disorders.52
Epigenetic mechanisms involve modification of DNA and chromatin regulating gene expression, which might mediate gene–environment interactions and could be modified by intervention. The inaccessibility of neuronal cells poses methodological problems in human studies. Hence, data examining peripheral biomarkers require validation via model systems. Hypothesis-driven studies suggest differential methylation of genes like MAOA,53 CRHR1,54 and OXTR55 to be associated with panic disorder, social anxiety disorder, and treatment response. However, epigenome-wide screenings have also not yet included large enough samples to allow definitive conclusions. Taken together, epigenetic and genetic testing cannot yet be recommended for clinical practice; rather, respective studies might provide mechanistic insights and hence avenues for new treatments.
Basic neuroscience
Basic neuroscience informs attempts to improve treatment and outcome prediction in people with anxiety disorders. Relative to many mental illnesses, neuroscience research regarding anxiety appears more clinically relevant because there is strong cross-species conservation in the mammalian responses to danger and the associated brain circuitry (figure 1).56–62 This research suggests that perturbed threat responding in anxiety disorders involves dysfunction in the circuitry that supports core psychological processes, such as attention, emotion, learning, and memory.59
Neuroscience research examines how brain circuitry supports learning about threats.56,59,61–63 This learning includes forms of conditioning, extinction, and reconsolidation, a memory updating mechanism.64 By defining plasticity-related factors underlying learning, this research has already identified promising novel therapies to treat anxiety disorders.56,61 Moreover, other research defines molecular processes, through which genetic risk might manifest, and environmentally sensitive processes (such as hippocampal neurogenesis),61 through which stress might increase the risk for anxiety disorders.
Translational research
Many brain imaging studies have examined the structure of regions that basic neuroscience implicates in threat responding, showing structural alterations in anxiety disorders within medial temporal, prefrontal cortex, and cingulate regions.65,66 Because small effect sizes are expected on the basis of data in other mental disorders (eg, for depressive or obsessive-compulsive disorders; pooled Cohen’s d of 0·10–0·30),67–69 structural imaging in anxiety disorders is minimally clinically relevant.
More clinically promising findings are arising in functional MRI studies when, for example, evoking threat response. With functional MRI, patients who are anxious have an altered response in temporal and prefrontal brain regions, which has also been shown in functional MRI research regarding attention.65,70,71 Such functional MRI studies connect anxiety-related perturbations at psychological and neurophysiological levels, with effect sizes of typically 0·50–1·00.72 Treatment trials have already extended such translational work in ways that are relevant to clinicians by targeting attention with the goal of reducing the risk and expression of anxiety disorders.73 Other functional MRI studies have isolated responding on threat-learning, extinction, and uncontrollable-stress frameworks,57,62,63,65 for which anxiety disorder-related hyper-responding was shown to manifest in temporal and prefrontal cortex regions, with relatively large effects.
Decision making research finds a robust anxiety disorder correlate on tasks for which patients make errors. Such errors, particularly when they are highly salient, evoke a midline encephalography response called the error-related negativity, which is larger in individuals with anxiety disorders than is in individuals who do not have anxiety disorders (Cohen’s d 0·20–0·60).74 Increased error-related negativity could reflect alterations in decision making, although people with anxiety disorders show few other consistent signs of altered decision making. Increased error-related negativity could also be viewed as a form of threat hypersensitivity, evoked by the potential adverse consequences of error commission.
To study immediate threat responses, other research has examined behavioural, physiological, or psychological responses to danger. Specifically, patients with anxiety disorders have been shown to manifest heightened sensitivity to threats, including attention bias to threat.59,72,75,76 Such hypersensitivity can manifest in reaction-time, ocular, and multiple psychophysiological measures.59 Other research has focused on prolonged defensive stress-system responding. When people are exposed to stressors, such as public speaking, scary pictures, or painful stimulation, studies generally report increased stress responses in people with anxiety disorders versus controls across many measures.63,70–72,77 These measures include peripheral autonomic, neurochemical, and hormonal measures, as well as startle response, for which relevant circuitry has been isolated in basic research.59 For some measures, including blood inflammatory indicators, differences between persons with and without anxiety disorders occur even without laboratory stress tests, suggesting chronically increased responsivity is present in normal life.78,79 For peripheral measures, rarely do effect sizes exceed a Cohen’s d of 0·50, indicating that these are not useful biomarkers that currently guide diagnosis.
Developmental perspectives
Overall, developmental cascades into chronic anxiety begin with preclinical signs, followed by (childhood) anxiety symptoms, culminating in persistent anxiety and comorbid conditions.
Studies in non-human primates and human infants younger than 4 years have detected developmental risk markers related to anxiety symptoms.60 Temperaments linked to anxiety involve heightened emotional sensitivity, as well as defensive responding to threat exposure.60 Strong findings exist for the temperament of behavioural inhibition, expressed as reduced movement and vocalisation in the presence of novelty.73
Although unique combinations of genes and environmental factors can operate selectively at specific timepoints across development, others might operate more consistently at many points throughout development.73 Environmental factors that influence the risk for anxiety disorders at multiple timepoints include various stressful life experiences and parenting practices, including childhood trauma, separation from attachment figures, and forms of overprotective parenting that limit children’s opportunities to encounter frightening circumstances in ways that facilitate mastery.
Part of the pathophysiology of anxiety is shared with other mental disorders. Heightened stress responsivity represents a cross-disorder risk that is initially associated with anxiety in childhood.57,62,65,71,77 Ultimately, research in this area will help clinicians to predict transitions from anxiety disorders to other problems. Other markers, such as perturbed memory, reward processing, and executive functioning occur more prominently in conditions other than anxiety disorders (eg, depressive disorders).57 Conversely, anxiety-specific pathophysiology markers could include the error-related negativity and certain varieties of attention bias.58,72,74,76
Prevention
Universal, selective, and indicated prevention strategies for children or young people might prevent the onset of anxiety disorders. A meta-analysis80 of 47 randomised controlled trials of prevention in people aged between 5 years and 18 years, mainly concerning psychological strategies, showed reduced risks for internalising disorder onset with the use of prevention strategies versus control. However, only nine studies focused on anxiety onset, and effects do not sustain beyond 9 months. In university students, psychoeducation, relaxation, or cognitive restructuring programmes have showed moderate symptom reduction (hedges’ g=0·65),81 regardless of delivery format or prevention level. By contrast, a network meta-analysis82 of 137 studies among 56 620 participants examining school-based interventions showed a high risk of bias and no clear evidence that interventions might reduce anxiety. Young offspring (aged 4–25 years) of parents with anxiety disorders form a group who are at high risk, with a 78% increased risk of anxiety disorders.83 In this group, a brief family-based psychosocial prevention programme has been reported to reduce the 1 year incidence of anxiety.84
In adults, anxiety prevention has been evaluated in a few trials of selective or indicated prevention.85–88 eHealth interventions (involving the delivery of psychotherapy through the internet) have been shown to be effective in improving anxiety symptoms (standardised mean difference 0·31);85 however, it is unclear whether this improvement translates into reduced anxiety disorder onset. Behavioural lifestyle interventions (eg, stimulating exercise86 or sleep hygiene87) have shown efficacy in depression prevention, but have barely been tested for anxiety. Supplementation of omega-3 fatty acids in five trials showed no effect in preventing anxiety.88
In summary, prevention interventions, mainly concerning cognitive behavioural therapy (CBT) or educational interventions, or both, have a small benefit for anxiety prevention (standardised mean difference 0·31) when meta-analysed across the entire life span (29 studies, 10430 people).89 Future well-designed randomised controlled trials (including adequate sample size and active comparators) are needed to determine to what extent, which components, and under what conditions anxiety prevention programmes can be cost-effective, efficacious, and long lasting.
Clinical management
Globally, anxiety disorders are underdiagnosed and undertreated.3 Most people who have anxiety disorders will present to, and are managed in, primary care. However, effective treatments do exist; these treatments not only reduce anxiety symptoms but also improve quality of life and functioning. Randomised studies concerning medication and psychotherapy cannot easily be compared due to methodological reasons, especially regarding the effect sizes of the respective control condition (eg, placebo, sham therapies, or waiting list controls: placebo can also can have an effect on anxiety reduction90). The most parsimonious current conclusion is that medication and psychotherapy produce benefits with similar effect sizes90 when given as a first-line treatment, such as in primary care. Therefore, potential side-effects, ecological factors (such as treatment availability), and patient preference should be discussed in a shared decision making process between the clinician and patient. Psychoeducation needs to be included as soon as a diagnosis has been made.
Psychotherapy
Evidence-based psychotherapies91 (as pharmacotherapies) are considered first-line treatments for anxiety disorders. These range from low-intensity interventions incorporating self-help approaches (eg, bibliotherapy) to high-intensity therapies with a specialised therapist according to disorder severity. Most evidence exists for the use of CBT as a treatment for anxiety disorders. However, the evidence base is not as strong for the use of other psychotherapies, such as psychodynamic-based, interpersonal-based, or acceptance-based psychotherapies, for treating anxiety disorders. CBT is a short-term therapy (consisting of eight to 20 sessions) derived from principles of behavioural and cognitive psychology. Practical considerations are shown in panel 1. A key CBT component for most forms of anxiety disorder involves exposure to the feared stimuli, either in vivo or imaginal. Exposure is used to break a vicious circle of avoidance behaviour and enable new, so-called safety learning so that the expected aversive outcome does not occur or is manageable. Cognitive restructuring can be used for verbal thoughts or the anxiety-provoking mental imagery that is highly common in anxiety disorders.92 Meta-analyses93 have concluded that effect sizes of CBT on anxiety are large when the control is waiting list placement but small to moderate when the control is care-as-usual or pill placebo (figure 2). Due to the small number of high quality trials, effect estimates should be considered with caution, and future improvements should be encouraged in psychological treatment trial methodology, including active controls and blinding.102
Panel 1: Practical psychotherapy treatment considerations.
Patients should receive education about what anxiety is and what symptoms belong to their particular anxiety disorder. They should be informed that most anxiety disorders can be effectively treated with evidence-based psychotherapy, or by pharmacotherapy, and patient choice should be discussed. Patients should be made aware that not all forms of psychotherapy are effective and that most substantial evidence exists for a form called cognitive behavioural therapy (CBT; patients can be signposted to the national CBT association website—eg, Association of Behavioral and Cognitive Therapies, USA and British Association for Behavioural and Cognitive Psychotherapies, UK). CBT is a short-term therapy, typically consisting of eight to 20 sessions, and involves setting goals and learning skills to reduce anxiety and perception of threat. Rather than avoiding feared situations or seeking reassurance, patients will learn to approach fearful situations and cope with them, use techniques to stay calmer, and develop skills to maintain gains longer term. CBT should be delivered by trained therapists who adhere closely to (anxiety disorder-specific) empirically grounded treatment protocols. Therapists should explain what is being used and why, and work collaboratively with patients (eg, give a rationale for the use of techniques such as exposure or cognitive restructuring, explain how effective these can be, and tailor these treatments to the patients’ specific anxiety). What is important in the treatment is what the patient learns, not the format. Learning can be done either face to face with a therapist or remotely by a therapy delivered via the internet. Patients should be encouraged to attend all therapy sessions to receive adequate treatment. Long-term management could include booster sessions. Because the presence of more than one anxiety disorder is common, patients could choose which to target and can receive different therapy packages for each anxiety disorder accordingly. Almost per definition, people with anxiety disorders can have anxiety about starting therapy. Therefore, access to information and encouragement is important, to give patients the confidence to start treatment and the optimism that anxiety can be effectively treated, benefiting their lives in terms of improved functioning.
Figure 2: Effect sizes of different treatments in reducing anxiety symptoms based on meta-analytic evidence.
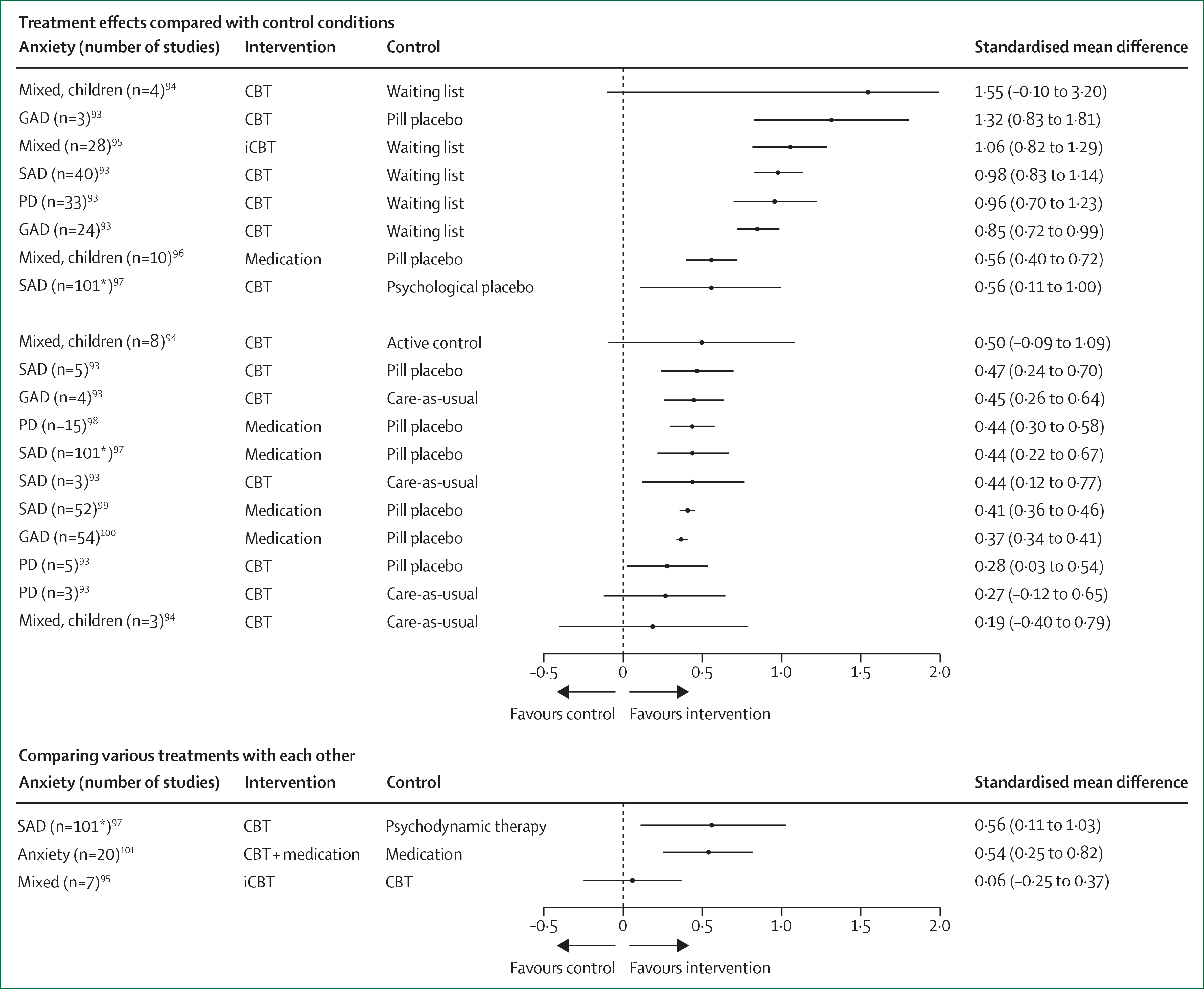
CBT=cognitive behavioural therapy. GAD=generalised anxiety disorder. iCBT=therapist-assisted internet cognitive behavioural therapy. PD=panic disorder. SAD=social anxiety disorder. *Based on network meta-analysis; therefore, sample size reflects all studies included, not just for the specific contrast.
CBT is an umbrella term. CBT protocols and studies have largely been specific to disorders and delivered by trained individuals who adhere closely to empirically grounded treatment protocols. A unified protocol for the transdiagnostic treatment of anxiety disorders has been developed. Unified protocol treatment has been shown to yield equivalent symptom reductions to single-disorder protocols for anxiety disorders (eg, panic disorder, generalised anxiety disorder, and social anxiety disorder), but also increased session completion.103 Internet-based CBT has greatly expanded over the past decade, and provides an important way to improve access to therapy where services are limited or where geographical location makes it hard to reach a therapist. Compared with face-to-face CBT, similar effectiveness on anxiety reduction has been reported for internet-based CBT.95 Another innovation is CBT via telephone.104 Furthermore, digital technologies (such as virtual reality) are alternative approaches to provide exposure to avoided stimuli. For example, compared with usual care, use of a virtual reality display of an avatar alongside a great vertical drop resulted in reduced fear of heights.105 Compared with invivo exposure, virtual reality exposure to social situations with CBT seems an effective treatment for social anxiety disorder.106 Overall, more rigorous, well-controlled studies are needed to test alternative forms of CBT delivery.
There is less evidence about the use of CBT in children and adolescents than in adults. More strong evidence in children and adolescents is needed, given the unknown risks from the use of medication to treat anxiety disorders in this age group. CBT is considered effective compared with waiting list control, but only mildly so when compared with active control in children and adolescents (figure 2).94 Additionally, CBT has similar efficacy from school age (4–12 years) through to adolescence (15–25 years). The internet offers a promising mode of treatment delivery for young children with anxiety disorders (eg, a parenting programme for the prevention and early intervention of anxiety problems in young children aged 3–6 years).107 Effective innovations also include parent-delivered CBT for children.108,109
Pharmacotherapy
Pharmacotherapy is also a first-line treatment for anxiety disorders. There are several factors, such as non-response to psychotherapy, chronic courses or complex conditions, and depression comorbidity, that might prioritise treatment with medication. Different classes of selective serotonin reuptake inhibitors (SSRIs) and serotonin–noradrenaline reuptake inhibitors (SNRIs) have been shown to be mildly to moderately efficacious in social anxiety disorder, panic disorder, and agoraphobia and generalised anxiety disorder (effect sizes 0·37–0·44, figure 2).98–100 Efficacy of SSRIs and SNRIs has also been shown in children and adolescents.96 A placebo-controlled trial110 of people with mild depression in primary care showed that the SSRI sertraline improved anxious symptoms but not depressive symptoms. Although approval status can vary by country, in general, all SSRIs, SNRIs, MAO inhibitors, and the serotonergic tricyclic compound clomipramine are superior to placebo in reducing anxiety symptoms in adults. However, SSRIs (and, to a lesser extent, SNRIs) are preferred due to their favourable risk–benefit ratio at all ages, and particularly in children and adolescents (panel 2). A network meta-analysis112 of generalised anxiety disorder showed superior efficacy of duloxetine, venlafaxine, escitalopram, pregabalin, and quetiapine, although quetiapine exhibited increased discontinuation rates. Initial disease severity moderates the effect size of drug treatment both in panic disorder and generalised anxiety disorder: a meta-analysis113 showed that effect sizes increased from Cohen’s d 0·2 in mild generalised anxiety disorder to 0·5 in severe generalised anxiety disorder; similar effects were shown for panic disorder. These findings call for caution regarding the use of medication in patients who are mildly symptomatic.
Panel 2: Practical psychopharmacology treatment considerations.
In terms of efficacy, there is no clear superiority of any selective serotonin reuptake inhibitor or serotonin–noradrenaline reuptake inhibitor compound; therefore, medication selection should be based on interactions and side-effect profile. Because the risk–benefit ratio seems best for newer medications, such as venlafaxine, escitalopram, or sertraline, these medications should be given as first-line treatment. Patients need to be informed about possible side-effects, the general harmlessness of these side-effects, and the 2–4 week latency of effect. Almost per definition, people with anxiety disorders have a greater sensitivity to medication side-effects and, therefore, treatment should start at the lowest dose and only cautiously be increased following the so-called rule of start low, go slow. As is true for all medication treatments, comorbid somatic disorders and polypharmacy call especially for cautious treatment initiation and careful evaluation of drug interactions in older patients aged 65 years or older. On response, drug therapy should be continued for at least 12 months, given that placebo-controlled studies have shown an increased risk of relapse on discontinuation.111 If discontinued, these compounds should be tapered slowly over several weeks to avoid withdrawal effects. Benzodiazepines should be given very cautiously and never as monotherapy; their use should be limited to the first few weeks of specific substances until these treatments start to be effective. Also, benzodiazepines should be given at a fixed-dose regimen but not as needed, to avoid the development of dependency.
Benzodiazepines are anxiolytic and therefore efficacious in most anxiety disorders.100,114 However, these drugs only act acutely, lead to relapse after discontinuation, and are associated with dependency. These compounds therefore require strict monitoring. A few other drugs are used in the treatment of anxiety disorders. Pregabalin, which blocks voltage-gated calcium channels, is licensed for generalised anxiety disorder in many countries and shows a moderate effect size of Cohen’s d 0·37 and a favourable safety profile,115 although cases of misuse of the drug have been reported. Buspirone and opipramol are prescribed for generalised anxiety disorder, but evidence is insufficient; these substances should therefore be limited to second-line use. An extended release formulation of quetiapine is similar to SSRI with regard to response;116 but this drug is off-label for generalised anxiety disorder and the associated side-effects, such as weight gain and sedation, limit its use.
Combination treatment and treatment non-response
Combination treatments are used by many patients in clinical reality (eg, when there is treatment resistance, comorbidity, and complicated courses), although research is underdeveloped.102 Meta-analytic evidence101 has shown that combined psychotherapy plus pharmacotherapy outperforms pharmacotherapy alone in standard settings. However, resistance to first-line treatments poses a major clinical challenge. Generally, a patient should only be considered resistant to treatment if both pharmacotherapy and psychotherapy are ineffective. A systematic review117 on augmentation strategies in patients with SSRI-resistant anxiety disorders could identify only six medication studies and no psychotherapy augmentation studies. Although a small positive effect on symptom reduction was noted, none of the augmentation strategies resulted in increased response rate.
Beyond more conventional designs, experimental research has investigated the use of combinations of medication and psychotherapy118 or other neuroscience-informed treatment combinations. For example, attention bias modification might improve outcome over placebo attention bias modification when added to CBT in children who have anxiety disorders (Cohen’s d=0·45).119 Pharmacological manipulation of memory reconsolidation appears a promising direction that combines exposure and various pharmacotherapies, aiming to create integrated treatments.120 Finally, a meta-analysis suggests a small effect (Cohen’s d=0·25) for d-cycloserine, a partial N-methyl-d-aspartate agonist, when added to augment exposure-based CBT.121 Findings on transcranial brain stimulation techniques in anxiety disorders are sparse. Two randomised controlled trials of generalised anxiety disorder122 have shown a positive effect of transcranial brain stimulation, but these trials were not done in patients who were resistant to treatment and data for other anxiety disorders are less conclusive or have not yet been obtained. Future work should investigate mechanisms to inform the innovation of synergistic combination treatments102 and how to improve long-term effects for relapse prevention.
Controversies, uncertainties, and outstanding research questions
COVID-19: understanding and treating anxiety at scale under pandemic conditions
This Seminar has been written during the COVID-19 pandemic—a pandemic associated with sequelae, such as challenging economic consequences. An outstanding uncertainty is how to help manage anxiety related to the pandemic and to consider how this anxiety will be managed from a global mental health perspective.123 Repeated media exposure to information about (infectious) disease can exacerbate anxieties and associated maladaptive behaviours in susceptible populations.124 Strategies to manage anxiety-provoking media consumption and to promote successful adherence to health behavioural advice while minimising anxiety require research.123 Approaches for investigating populationlevel interventions will require rapid evaluation and modification; for example, testing whether existing digital interventions (eg, for sleep or stress management) can be repurposed. Treatments need to be tailored for what is possible to deliver under pandemic conditions, that is, remotely via digital clinics.
Anxiety-changing mechanisms operate across many levels: from the molecular, neurobiological, and cognitive, to the behavioural or social.102 Although knowledge at each level is known, cross-level work insufficiently connects molecular and system levels to support precision medicine approaches. Such insights would inform new approaches to diagnosis and classification with improved representation of the underlying disturbances in brain function. Effective anxiety disorder treatments seem to be targeting mechanisms identified through neurobiological studies,125 but insufficient research connects clinical outcomes to changes in mechanisms. Better cross-level understanding of the routes to disease and recovery offers promising ways to improve existing anxiety treatments, such as with extinction126 or reinforcement learning algorithms.127 The integration of detailed cross-level knowledge of how pathological fear and defensive reactions develop will provide suggestions for best applying existing treatments and identifying novel ones.128,129 Overall, better theoretical models are needed to link processes within treatment to those observed in outcomes or to dismantle the mechanisms of change in more detail (eg, for specific symptoms or treatment components).102
Extending treatment opportunities
Effectiveness of currently available treatments vary for people at different stages of anxiety severity, and a major challenge is finding meaningful ways of sequencing and combining treatments. Particularly, further research of escalated therapies to treat treatment-resistant anxiety is called for. Given the global prevalence and burden of anxiety disorders, it is surprising that the current medication pipeline is rather empty. A 2019 overview130 has not listed a single compound in the current medication pipeline, although preclinical studies have suggested a wide range of molecular targets beyond serotonin and GABA receptors or transporters (eg, corticotropin-releasing hormone receptors, translocator protein, or the endocannabinoid system). Also glutamatergic compounds hold future promise; small proofof-concept studies of intravenous ketamine showed beneficial results in generalised anxiety disorder and social anxiety disorder.131,132 The question of how to selectively target neuronal subpopulations that build pathological defensive responses within the fear network will be the focus of novel therapies in coming years.
Integrating patient’s choice and functioning in treatment
Given that pharmacotherapy and psychotherapy are similarly effective first-line treatments (figure 2), the patient’s choice deserves further consideration in treatment decisions. A 2019 review133 showed that people with mental disorders who received their preferred treatment had lower dropout rates and higher therapeutic alliance than those who received their non-preferred treatment or who were not given a choice. Research should examine what determines patient preferences and how to accommodate patient preference in mental health services to maximise treatment uptake and reduce financial costs of premature dropout and disengagement. Future developments should also focus more on improvements in patients’ social and occupational functioning.134 A growing area is workplace mental health, which focuses on interventions that a workplace could initiate or facilitate, aiming to prevent, treat, or rehabilitate a worker.135
Reducing the anxiety treatment gap
Of all people with anxiety disorders worldwide, less than 25% are estimated to receive any form of treatment, and even among those with an explicitly expressed need for care, less than 25% are estimated to receive potentially adequate treatment.3 Adequate detection and management is necessary in primary care, in which most people with anxiety disorders do present, but also in specialised (somatic) clinical settings. Especially when there is minimal access to health-care providers, eHealth interventions could considerably help to prevent and treat anxiety disorders. Generally, health-care systems need to adopt stepped care approaches that provide cost-effective, low-intensity treatments and self-help aids for patients with mild disorders, as well as implementing more intensive interventions for patients who are severely ill early from symptom onset, to avoid chronic and disabling courses. Such developments call for measurement-based and guided care systems rather than user-driven service provision. Only a combined effort in which we better prevent, better recognise, and more effectively treat anxiety disorders can ultimately reduce the burden that anxiety disorders place on our society.
Search strategy and selection criteria.
We searched articles in PubMed and Cochrane databases using major medical subject headings and title or key words for “anxiety disorder”, “separation anxiety”, “selective mutism”, “specific phobia”, “social phobia”, “social anxiety disorder”, “panic disorder”, “agoraphobia”, or “generalized anxiety disorder” published in English between Jan 1, 2015, and March 1, 2020. From the identified papers, we selectively prioritised reviews, meta-analyses, and strong, influential (experimental) studies within maximum reference criteria. We focused on the most recent papers unless evidence was sparse or if older papers were particularly important.
Acknowledgments
Declaration of interests
BWJHP has received unrestricted research funding from Jansen Research and Boehringer Ingelheim (not related to the contents of this Seminar). DSP received research funding from the National Institute of Mental Health Intramural Research Program through project ZIAMH002781. EAH has received grants from the OAK Foundation, the Lupina Foundation, and the Swedish Research Council (not related to the contents of this Seminar). AR has received honoraria for talks or advisory boards from Jansen, Servier, Neuroaxpharm, Medice, Shire (Takeda), and SAGE (not related to the contents of this Seminar).
Contributor Information
Brenda W J H Penninx, Department of Psychiatry, Amsterdam University Medical Center, Vrije Universiteit, Amsterdam, Netherlands; GGZ inGeest, Amsterdam, Netherlands.
Daniel S Pine, Emotion and Development Branch, National Institute of Mental Health, Bethesda, MD, USA.
Emily A Holmes, Department of Psychology, Uppsala University, Uppsala, Sweden.
Andreas Reif, Department of Psychiatry, Psychosomatic Medicine and Psychotherapy, University Hospital Frankfurt–Goethe University, Frankfurt, Germany.
References
- 1.Vos T, Abajobir AA, Abbafati C, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017; 390: 1211–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gustavsson A, Svensson M, Jacobi F, et al. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 2011; 21: 718–79. [DOI] [PubMed] [Google Scholar]
- 3.Alonso J, Liu Z, Evans-Lacko S, et al. Treatment gap for anxiety disorders is global: results of the World Mental Health Surveys in 21 countries. Depress Anxiety 2018; 35: 195–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Batelaan NM, Rhebergen D, de Graaf R, Spijker J, Beekman ATF, Penninx BWJH. Panic attacks as a dimension of psychopathology. J Clin Psychiatry 2012; 73: 1195–202. [DOI] [PubMed] [Google Scholar]
- 5.Lamers F, van Oppen P, Comijs HC, et al. Comorbidity patterns of anxiety and depressive disorders in a large cohort study: the Netherlands Study of Depression and Anxiety (NESDA). J Clin Psychiatry 2011; 72: 341–48. [DOI] [PubMed] [Google Scholar]
- 6.Scholten WD, Batelaan NM, Penninx BWJH, et al. Diagnostic instability of recurrence and the impact on recurrence rates in depressive and anxiety disorders. J Affect Disord 2016; 195: 185–90. [DOI] [PubMed] [Google Scholar]
- 7.Hendriks SM, Spijker J, Licht CMM, Beekman ATF, Penninx BWJH. Two-year course of anxiety disorders: different across disorders or dimensions? Acta Psychiatr Scand 2013; 128: 212–21. [DOI] [PubMed] [Google Scholar]
- 8.Hendriks SM, Spijker J, Licht CMM, et al. Long-term disability in anxiety disorders. BMC Psychiatry 2016; 16: 248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robins LN, Wing J, Wittchen HU, et al. The composite international diagnostic interview. Arch Gen Psychiatry 1988; 45: 1069. [DOI] [PubMed] [Google Scholar]
- 10.Spitzer RL, Williams JBW, Gibbon M, First MB. The structured clinical interview for DSM-III-R (SCID). Arch Gen Psychiatry 1992; 49: 624. [DOI] [PubMed] [Google Scholar]
- 11.Ambrosini PJ. Historical development and present status of the schedule for affective disorders and schizophrenia for school-age children (K-SADS). J Am Acad Child Adolesc Psychiatry 2000; 39: 49–58. [DOI] [PubMed] [Google Scholar]
- 12.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361–70. [DOI] [PubMed] [Google Scholar]
- 13.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988; 56: 893–97. [DOI] [PubMed] [Google Scholar]
- 14.Van Zuuren FJ. The fear questionnaire. Br J Psychiatry 1988; 153: 659–62. [DOI] [PubMed] [Google Scholar]
- 15.Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther 1990; 28: 487–95. [DOI] [PubMed] [Google Scholar]
- 16.Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav Res Ther 1986; 24: 1–8. [DOI] [PubMed] [Google Scholar]
- 17.Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry 2016; 39: 24–31. [DOI] [PubMed] [Google Scholar]
- 18.Meier SM, Petersen L, Mattheisen M, Mors O, Mortensen PB, Laursen TM. Secondary depression in severe anxiety disorders: a population-based cohort study in Denmark. Lancet Psychiatry 2015; 2: 515–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Penninx BWJH Nolen WA, Lamers F, et al. Two-year course of depressive and anxiety disorders: results from the Netherlands Study of Depression and Anxiety (NESDA). J Affect Disord 2011; 133: 76–85. [DOI] [PubMed] [Google Scholar]
- 20.Spoorthy MS, Chakrabarti S, Grover S. Comorbidity of bipolar and anxiety disorders: an overview of trends in research. World J Psychiatry 2019; 9: 7–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smaardijk VR, Maas AHEM, Lodder P, Kop WJ, Mommersteeg PMC. Sex and gender-stratified risks of psychological factors for adverse clinical outcomes in patients with ischemic heart disease: a systematic review and meta-analysis. Int J Cardiol 2020; 302: 21–29. [DOI] [PubMed] [Google Scholar]
- 22.Pitman A, Suleman S, Hyde N, Hodgkiss A. Depression and anxiety in patients with cancer. BMJ 2018; 361: k1415. [DOI] [PubMed] [Google Scholar]
- 23.Eisner MD, Blanc PD, Yelin EH, et al. Influence of anxiety on health outcomes in COPD. Thorax 2010; 65: 229–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Copeland WE, Angold A, Shanahan L, Costello EJ. Longitudinal patterns of anxiety from childhood to adulthood: the great smoky mountains study. J Am Acad Child Adolesc Psychiatry 2014; 53: 21–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ormel J, Raven D, van Oort F, et al. Mental health in Dutch adolescents: a TRAILS report on prevalence, severity, age of onset, continuity and co-morbidity of DSM disorders. Psychol Med 2015; 45: 345–60. [DOI] [PubMed] [Google Scholar]
- 26.de Jonge P, Roest AM, Lim CC, et al. Cross-national epidemiology of panic disorder and panic attacks in the world mental health surveys. Depress Anxiety 2016; 33: 1155–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wardenaar KJ, Lim CCW, Al-Hamzawi AO, et al. The cross-national epidemiology of specific phobia in the World Mental Health Surveys. Psychol Med 2017; 47: 1744–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ruscio AM, Hallion LS, Lim CCW, et al. Cross-sectional comparison of the epidemiology of DSM-5 generalized anxiety disorder across the globe. JAMA Psychiatry 2017; 74: 465–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stein DJ, Lim CCW, Roest AM, et al. The cross-national epidemiology of social anxiety disorder: data from the World Mental Health Survey Initiative. BMC Med 2017; 15: 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roest AM, de Vries YA, Lim CCW, et al. A comparison of DSM-5 and DSM-IV agoraphobia in the World Mental Health Surveys. Depress Anxiety 2019; 36: 499–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Silove DM, Tay AK, Tol WA, et al. Patterns of separation anxiety symptoms amongst pregnant women in conflict-affected Timor-Leste: associations with traumatic loss, family conflict, and intimate partner violence. J Affect Disord 2016; 205: 292–300. [DOI] [PubMed] [Google Scholar]
- 32.Wittchen HU, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 2011; 21: 655–79. [DOI] [PubMed] [Google Scholar]
- 33.Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci 2015; 17: 327–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kessler RC, Demler O, Frank RG, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med 2005; 352: 2515–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baxter AJ, Scott KM, Vos T, Whiteford HA. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol Med 2013; 43: 897–910. [DOI] [PubMed] [Google Scholar]
- 36.Spinhoven P, Batelaan N, Rhebergen D, van Balkom A, Schoevers R, Penninx BW. Prediction of 6-yr symptom course trajectories of anxiety disorders by diagnostic, clinical and psychological variables. J Anxiety Disord 2016; 44: 92–101. [DOI] [PubMed] [Google Scholar]
- 37.Plaisier I, Beekman ATF, de Graaf R, Smit JH, van Dyck R, Penninx BWJH. Work functioning in persons with depressive and anxiety disorders: the role of specific psychopathological characteristics. J Affect Disord 2010; 125: 198–206. [DOI] [PubMed] [Google Scholar]
- 38.Iancu SC, Batelaan NM, Zweekhorst MBM, et al. Trajectories of functioning after remission from anxiety disorders: 2-year course and outcome predictors. Psychol Med 2014; 44: 593–605. [DOI] [PubMed] [Google Scholar]
- 39.Meier SM, Mattheisen M, Mors O, Mortensen PB, Laursen TM, Penninx BW. Increased mortality among people with anxiety disorders: total population study. Br J Psychiatry 2016; 209: 216–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Batelaan NM, Seldenrijk A, Bot M, van Balkom AJLM, Penninx BWJH. Anxiety and new onset of cardiovascular disease: critical review and meta-analysis. Br J Psychiatry 2016; 208: 223–31. [DOI] [PubMed] [Google Scholar]
- 41.Momen N, Plana-Ripoll O, Agerbo E, et al. Association between mental disorders and subsequent medical conditions. N Engl J Med 2020; 382: 1721–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Meier SM, Deckert J. Genetics of anxiety disorders. Curr Psychiatry Rep 2019; 21: 16. [DOI] [PubMed] [Google Scholar]
- 43.Howe AS, Buttenschon HN, Bani-Fatemi A, et al. Candidate genes in panic disorder: meta-analyses of 23 common variants in major anxiogenic pathways. Mol Psychiatry 2016; 21: 665–79. [DOI] [PubMed] [Google Scholar]
- 44.Meier SM, Trontti K, Purves KL, et al. Genetic variants associated with anxiety and stress-related disorders: a genome-wide association study and mouse-model study. JAMA Psychiatry 2019; 76: 924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Purves KL, Coleman JRI, Meier SM, et al. A major role for common genetic variation in anxiety disorders. Mol Psychiatry 2019; published online Nov 20. 10.1038/s41380-019-0559-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Forstner AJ, Awasthi S, Wolf C, et al. Genome-wide association study of panic disorder reveals genetic overlap with neuroticism and depression. Mol Psychiatry 2019; published online Nov 20. 10.1038/s41380-019-0590-2. [DOI] [PubMed] [Google Scholar]
- 47.Otowa T, Hek K, Lee M, et al. Meta-analysis of genome-wide association studies of anxiety disorders. Mol Psychiatry 2016; 21: 1391–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Levey DF, Gelernter J, Polimanti R, et al. Reproducible genetic risk loci for anxiety: results from approximately 200,000 participants in the million veteran program. Am J Psychiatry 2020; 177: 223–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Deckert J, Weber H, Villmann C, et al. GLRB allelic variation associated with agoraphobic cognitions, increased startle response and fear network activation: a potential neurogenetic pathway to panic disorder. Mol Psychiatry 2017; 22: 1431–39. [DOI] [PubMed] [Google Scholar]
- 50.Chawner S, Owen MJ, Holmans P, et al. Genotype-phenotype associations in children with copy number variants associated with high neuropsychiatric risk in the UK (IMAGINE-ID): a case-control cohort study. Lancet Psychiatry 2019; 6: 493–505. [DOI] [PubMed] [Google Scholar]
- 51.Nagel M, Jansen PR, Stringer S, et al. Meta-analysis of genome-wide association studies for neuroticism in 449,484 individuals identifies novel genetic loci and pathways. Nat Genet 2018; 50: 920–27. [DOI] [PubMed] [Google Scholar]
- 52.Caspi A, Moffitt TE. All for one and one for all: mental disorders in one dimension. Am J Psychiatry 2018; 175: 831–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ziegler C, Richter J, Mahr M, et al. MAOA gene hypomethylation in panic disorder-reversibility of an epigenetic risk pattern by psychotherapy. Transl Psychiatry 2016; 6: e773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schartner C, Ziegler C, Schiele MA, et al. CRHR1 promoter hypomethylation: an epigenetic readout of panic disorder? Eur Neuropsychopharmacol 2017; 27: 360–71. [DOI] [PubMed] [Google Scholar]
- 55.Ziegler C, Dannlowski U, Brauer D, et al. Oxytocin receptor gene methylation: converging multilevel evidence for a role in social anxiety. Neuropsychopharmacology 2015; 40: 1528–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pittig A, Treanor M, LeBeau RT, Craske MG. The role of associative fear and avoidance learning in anxiety disorders: gaps and directions for future research. Neurosci Biobehav Rev 2018; 88: 117–40. [DOI] [PubMed] [Google Scholar]
- 57.Otte C, Gold SM, Penninx BW, et al. Major depressive disorder. Nat Rev Dis Primers 2016; 2: 16065. [DOI] [PubMed] [Google Scholar]
- 58.Moser JS, Moran TP, Schroder HS, Donnellan MB, Yeung N. On the relationship between anxiety and error monitoring: a meta-analysis and conceptual framework. Front Hum Neurosci 2013; 7: 466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.LeDoux J, Daw ND. Surviving threats: neural circuit and computational implications of a new taxonomy of defensive behaviour. Nat Rev Neurosci 2018; 19: 269–82. [DOI] [PubMed] [Google Scholar]
- 60.Fox AS, Kalin NH. A translational neuroscience approach to understanding the development of social anxiety disorder and its pathophysiology. Am J Psychiatry 2014; 171: 1162–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Anacker C, Hen R. Adult hippocampal neurogenesis and cognitive flexibility—linking memory and mood. Nat Rev Neurosci 2017; 18: 335–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.de Quervain D, Schwabe L, Roozendaal B. Stress, glucocorticoids and memory: implications for treating fear-related disorders. Nat Rev Neurosci 2017; 18: 7–19. [DOI] [PubMed] [Google Scholar]
- 63.Duits P, Cath DC, Lissek S, et al. Updated meta-analysis of classical fear conditioning in the anxiety disorders. Depress Anxiety 2015; 32: 239–53. [DOI] [PubMed] [Google Scholar]
- 64.Monfils MH, Holmes EA. Memory boundaries: opening a window inspired by reconsolidation to treat anxiety, trauma-related, and addiction disorders. Lancet Psychiatry 2018; 5: 1032–42. [DOI] [PubMed] [Google Scholar]
- 65.Fonzo GA, Etkin A. Affective neuroimaging in generalized anxiety disorder: an integrated review. Dialogues Clin Neurosci 2017; 19: 169–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wu Y, Zhong Y, Ma Z, et al. Gray matter changes in panic disorder: a voxel-based meta-analysis and meta-analytic connectivity modeling. Psychiatry Res Neuroimaging 2018; 282: 82–89. [DOI] [PubMed] [Google Scholar]
- 67.Boedhoe PSW, Schmaal L, Abe Y, et al. Cortical abnormalities associated with pediatric and adult obsessive-compulsive disorder: findings from the ENIGMA obsessive-compulsive disorder working group. Am J Psychiatry 2018; 175: 453–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schmaal L, Veltman DJ, van Erp TGM, et al. Subcortical brain alterations in major depressive disorder: findings from the ENIGMA major depressive disorder working group. Mol Psychiatry 2016; 21: 806–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Schmaal L, Hibar DP, Sämann PG, et al. Cortical abnormalities in adults and adolescents with major depression based on brain scans from 20 cohorts worldwide in the ENIGMA major depressive disorder working group. Mol Psychiatry 2017; 22: 900–09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Marin M-F, Hammoud MZ, Klumpp H, Simon NM, Milad MR. Multimodal categorical and dimensional approaches to understanding threat conditioning and its extinction in individuals with anxiety disorders. JAMA Psychiatry 2020; 77: 618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Janiri D, Moser DA, Doucet GE, et al. Shared neural phenotypes for mood and anxiety disorders: a meta-analysis of 226 task-related functional imaging studies. JAMA Psychiatry 2019; 77: 172–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kircanski K, White LK, Tseng W-L, et al. A latent variable approach to differentiating neural mechanisms of irritability and anxiety in youth. JAMA Psychiatry 2018; 75: 631–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pine DS, Fox NA. Childhood antecedents and risk for adult mental disorders. Annu Rev Psychol 2015; 66: 459–85. [DOI] [PubMed] [Google Scholar]
- 74.Pasion R, Barbosa F. ERN as a transdiagnostic marker of the internalizing-externalizing spectrum: a dissociable meta-analytic effect. Neurosci Biobehav Rev 2019; 103: 133–49. [DOI] [PubMed] [Google Scholar]
- 75.Joyal M, Wensing T, Levasseur-Moreau J, Leblond J, Sack AT, Fecteau S. Characterizing emotional Stroop interference in posttraumatic stress disorder, major depression and anxiety disorders: a systematic review and meta-analysis. PLoS One 2019; 14: e0214998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pergamin-Hight L, Naim R, Bakermans-Kranenburg MJ, van IJzendoorn MH, Bar-Haim Y. Content specificity of attention bias to threat in anxiety disorders: a meta-analysis. Clin Psychol Rev 2015; 35: 10–18. [DOI] [PubMed] [Google Scholar]
- 77.McTeague LM, Lang PJ. The anxiety spectrum and the reflex physiology of defense: from circumscribed fear to broad distress. Depress Anxiety 2012; 29: 264–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Costello H, Gould RL, Abrol E, Howard R. Systematic review and meta-analysis of the association between peripheral inflammatory cytokines and generalised anxiety disorder. BMJ Open 2019; 9: e027925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Vogelzangs N, de Jonge P, Smit JH, Bahn S, Penninx BW. Cytokine production capacity in depression and anxiety. Transl Psychiatry 2016; 6: e825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Stockings EA, Degenhardt L, Dobbins T, et al. Preventing depression and anxiety in young people: a review of the joint efficacy of universal, selective and indicated prevention. Psychol Med 2016; 46: 11–26. [DOI] [PubMed] [Google Scholar]
- 81.Rith-Najarian LR, Boustani MM, Chorpita BF. A systematic review of prevention programs targeting depression, anxiety, and stress in university students. J Affect Disord 2019; 257: 568–84. [DOI] [PubMed] [Google Scholar]
- 82.Caldwell DM, Davies SR, Hetrick SE, et al. School-based interventions to prevent anxiety and depression in children and young people: a systematic review and network meta-analysis. Lancet Psychiatry 2019; 6: 1011–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lawrence PJ, Murayama K, Creswell C. Systematic review and meta-analysis: anxiety and depressive disorders in offspring of parents with anxiety disorders. J Am Acad Child Adolesc Psychiatry 2019; 58: 46–60. [DOI] [PubMed] [Google Scholar]
- 84.Ginsburg GS, Drake KL, Tein JY, Teetsel R, Riddle MA. Preventing onset of anxiety disorders in offspring of anxious parents: a randomized controlled trial of a family-based intervention. Am J Psychiatry 2015; 172: 1207–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Deady M, Choi I, Calvo RA, Glozier N, Christensen H, Harvey SB. eHealth interventions for the prevention of depression and anxiety in the general population: a systematic review and meta-analysis. BMC Psychiatry 2017; 17: 310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, Vandelanotte C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev 2015; 9: 366–78. [DOI] [PubMed] [Google Scholar]
- 87.Christensen H, Batterham PJ, Gosling JA, et al. Effectiveness of an online insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight Study): a randomised controlled trial. Lancet Psychiatry 2016; 3: 333–41. [DOI] [PubMed] [Google Scholar]
- 88.Deane KHO, Jimoh OF, Biswas P, et al. Omega-3 and polyunsaturated fat for prevention of depression and anxiety symptoms: systematic review and meta-analysis of randomised trials. Br J Psychiatry 2019; published online Oct 24. 10.1192/bjp.2019.234. [DOI] [PubMed] [Google Scholar]
- 89.Moreno-Peral P, Conejo-Cerón S, Rubio-Valera M, et al. Effectiveness of psychological and/or educational interventions in the prevention of anxiety: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry 2017; 74: 1021–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bandelow B, Reitt M, Rover C, Michaelis S, Gorlich Y, Wedekind D. Efficacy of treatments for anxiety disorders: a meta-analysis. Int Clin Psychopharmacol 2015; 30: 183–92 [DOI] [PubMed] [Google Scholar]
- 91.National Institute for Health and Care Excellence. Anxiety disorders. 2014. https://www.nice.org.uk/guidance/qs53 (accessed Jan 13, 2021).
- 92.Ji JL, Kavanagh DJ, Holmes EA, MacLeod C, Di Simplicio M. Mental imagery in psychiatry: conceptual & clinical implications. CNS Spectr 2019; 24: 114–26. [DOI] [PubMed] [Google Scholar]
- 93.Cuijpers P, Cristea IA, Karyotaki E, Reijnders M, Huibers MJ. How effective are cognitive behavior therapies for major depression and anxiety disorders? A meta-analytic update of the evidence. World Psychiatry 2016; 15: 245–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.James AC, James G, Cowdrey FA, Soler A, Choke A. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Syst Rev 2015; 2015: CD004690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Olthuis JV, Watt MC, Bailey K, Hayden JA, Stewart SH. Therapist-supported Internet cognitive behavioural therapy for anxiety disorders in adults. Cochrane Database Syst Rev 2016; 3: CD011565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Locher C, Koechlin H, Zion SR, et al. Efficacy and safety of selective serotonin reuptake inhibitors, serotoninnorepinephrine reuptake inhibitors, and placebo for common psychiatric disorders among children and adolescents: a systematic review and meta-analysis. JAMA Psychiatry 2017; 74: 1011–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mayo-Wilson E, Dias S, Mavranezouli I, et al. Psychological and pharmacological interventions for social anxiety disorder in adults: a systematic review and network meta-analysis. Lancet Psychiatry 2014; 1: 368–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bighelli I, Castellazzi M, Cipriani A, et al. Antidepressants versus placebo for panic disorder in adults. Cochrane Database Syst Rev 2018; 4: CD010676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Curtiss J, Andrews L, Davis M, Smits J, Hofmann SG. A meta-analysis of pharmacotherapy for social anxiety disorder: an examination of efficacy, moderators, and mediators. Expert Opin Pharmacother 2017; 18: 243–51. [DOI] [PubMed] [Google Scholar]
- 100.Gomez AF, Barthel AL, Hofmann SG. Comparing the efficacy of benzodiazepines and serotonergic anti-depressants for adults with generalized anxiety disorder: a meta-analytic review. Expert Opin Pharmacother 2018; 19: 883–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Cuijpers P, Sijbrandij M, Koole SL, Andersson G, Beekman AT, Reynolds CF 3rd. Adding psychotherapy to antidepressant medication in depression and anxiety disorders: a meta-analysis. World Psychiatry 2014; 13: 56–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Holmes EA, Ghaderi A, Harmer CJ, et al. The Lancet Psychiatry Commission on psychological treatments research in tomorrow’s science. Lancet Psychiatry 2018; 5: 237–86. [DOI] [PubMed] [Google Scholar]
- 103.Barlow DH, Farchione TJ, Bullis JR, et al. The unified protocol for transdiagnostic treatment of emotional disorders compared with diagnosis-specific protocols for anxiety disorders: a randomized clinical trial. JAMA Psychiatry 2017; 74: 875–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Brenes GA, Danhauer SC, Lyles MF, Hogan PE, Miller ME. Telephone-delivered cognitive behavioral therapy and telephone-delivered nondirective supportive therapy for rural older adults with generalized anxiety disorder: a randomized clinical trial. JAMA Psychiatry 2015; 72: 1012–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Freeman D, Haselton P, Freeman J, et al. Automated psychological therapy using immersive virtual reality for treatment of fear of heights: a single-blind, parallel-group, randomised controlled trial. Lancet Psychiatry 2018; 5: 625–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bouchard S, Dumoulin S, Robillard G, et al. Virtual reality compared with in vivo exposure in the treatment of social anxiety disorder: a three-arm randomised controlled trial. Br J Psychiatry 2017; 210: 276–83. [DOI] [PubMed] [Google Scholar]
- 107.Morgan AJ, Rapee RM, Salim A, et al. Internet-delivered parenting program for prevention and early intervention of anxiety problems in young children: randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2017; 56: 417–25. [DOI] [PubMed] [Google Scholar]
- 108.Creswell C, Violato M, Fairbanks H, et al. Clinical outcomes and cost-effectiveness of brief guided parent-delivered cognitive behavioural therapy and solution-focused brief therapy for treatment of childhood anxiety disorders: a randomised controlled trial. Lancet Psychiatry 2017; 4: 529–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lebowitz ER, Marin C, Martino A, Shimshoni Y, Silverman WK. Parent-based treatment as efficacious as cognitive-behavioral therapy for childhood anxiety: a randomized noninferiority study of supportive parenting for anxious childhood emotions. J Am Acad Child Adolesc Psychiatry 2019; 59: 362–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Fernandez RL, Morcillo C, Wang S, et al. Acculturation dimensions and 12-month mood and anxiety disorders across US Latino subgroups in the National Epidemiologic Survey of Alcohol and Related Conditions. Psychol Med 2016; 46: 1987–2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Batelaan NM, Bosman RC, Muntingh A, Scholten WD, Huijbregts KM, van Balkom A. Risk of relapse after antidepressant discontinuation in anxiety disorders, obsessive-compulsive disorder, and post-traumatic stress disorder: systematic review and meta-analysis of relapse prevention trials. BMJ 2017; 358: j3927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Slee A, Nazareth I, Bondaronek P, Liu Y, Cheng Z, Freemantle N. Pharmacological treatments for generalised anxiety disorder: a systematic review and network meta-analysis. Lancet 2019; 393: 768–77. [DOI] [PubMed] [Google Scholar]
- 113.de Vries YA, Roest AM, Burgerhof JGM, de Jonge P. Initial severity and antidepressant efficacy for anxiety disorders, obsessive-compulsive disorder, and posttraumatic stress disorder: an individual patient data meta-analysis. Depress Anxiety 2018; 35: 515–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Breilmann J, Girlanda F, Guaiana G, et al. Benzodiazepines versus placebo for panic disorder in adults. Cochrane Database Syst Rev 2019; 3: CD010677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Generoso MB, Trevizol AP, Kasper S, Cho HJ, Cordeiro Q, Shiozawa P. Pregabalin for generalized anxiety disorder: an updated systematic review and meta-analysis. Int Clin Psychopharmacol 2017; 32: 49–55. [DOI] [PubMed] [Google Scholar]
- 116.Maneeton N, Maneeton B, Woottiluk P, et al. Quetiapine monotherapy in acute treatment of generalized anxiety disorder: a systematic review and meta-analysis of randomized controlled trials. Drug Des Devel Ther 2016; 10: 259–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Patterson B, Van Ameringen M. Augmentation strategies for treatment-resistant anxiety disorders: a systematic review and meta-analysis. Depress Anxiety 2016; 33: 728–36. [DOI] [PubMed] [Google Scholar]
- 118.Gingnell M, Frick A, Engman J, et al. Combining escitalopram and cognitive-behavioural therapy for social anxiety disorder: randomised controlled fMRI trial. Br J Psychiatry 2016; 209: 229–35. [DOI] [PubMed] [Google Scholar]
- 119.White LK, Sequeira S, Britton JC, et al. Complementary features of attention bias modification therapy and cognitive-behavioral therapy in pediatric anxiety disorders. Am J Psychiatry 2017; 174: 775–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Soeter M, Kindt M. An abrupt transformation of phobic behavior after a post-retrieval amnesic agent. Biol Psychiatry 2015; 78: 880–86. [DOI] [PubMed] [Google Scholar]
- 121.Mataix-Cols D, Fernandez de la Cruz L, Monzani B, et al. D-Cycloserine augmentation of exposure-based cognitive behavior therapy for anxiety, obsessive-compulsive, and posttraumatic stress disorders: a systematic review and meta-analysis of individual participant data. JAMA Psychiatry 2017; 74: 501–10. [DOI] [PubMed] [Google Scholar]
- 122.Cirillo P, Gold AK, Nardi AE, et al. Transcranial magnetic stimulation in anxiety and trauma-related disorders: a systematic review and meta-analysis. Brain Behav 2019; 9: e01284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 2020; 7: 547–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Garfin D, Silver R, Holman E. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Health Psychol 2020; 39: 355–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Marwood L, Wise T, Perkins AM, Cleare AJ. Meta-analyses of the neural mechanisms and predictors of response to psychotherapy in depression and anxiety. Neurosci Biobehav Rev 2018; 95: 61–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Pittig A, van den Berg L, Vervliet B. The key role of extinction learning in anxiety disorders: behavioral strategies to enhance exposure-based treatments. Curr Opin Psychiatry 2016; 29: 39–47. [DOI] [PubMed] [Google Scholar]
- 127.Mkrtchian A, Aylward J, Dayan P, Roiser JP, Robinson OJ. modeling avoidance in mood and anxiety disorders using reinforcement learning. Biol Psychiatry 2017; 82: 532–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Craske MG, Hermans D, Vervliet B. State-of-the-art and future directions for extinction as a translational model for fear and anxiety. Philos Trans R Soc L B Biol Sci 2018; 373: 20170025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kindt M The surprising subtleties of changing fear memory: a challenge for translational science. Philos Trans R Soc Lond B Biol Sci 2018; 373: 20170033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Brady LS, Potter WZ, Gordon JA. Redirecting the revolution: new developments in drug development for psychiatry. Expert Opin Drug Discov 2019; 14: 1213–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Taylor JH, Landeros-Weisenberger A, Coughlin C, et al. Ketamine for social anxiety disorder: a randomized, placebo-controlled crossover trial. Neuropsychopharmacology 2018; 43: 325–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Glue P, Neehoff S, Sabadel A, et al. Effects of ketamine in patients with treatment-refractory generalized anxiety and social anxiety disorders: exploratory double-blind psychoactive-controlled replication study. J Psychopharmacol 2020; 34: 267–72. [DOI] [PubMed] [Google Scholar]
- 133.Windle E, Tee H, Sabitova A, Jovanovic N, Priebe S, Carr C. Association of patient treatment preference with dropout and clinical outcomes in adult psychosocial mental health interventions: a systematic review and meta-analysis. JAMA Psychiatry 2019; 77: 294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Brown LA, Krull JL, Roy-Byrne P, et al. An examination of the bidirectional relationship between functioning and symptom levels in patients with anxiety disorders in the CALM study. Psychol Med 2015; 45: 647–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Joyce S, Modini M, Christensen H, et al. Workplace interventions for common mental disorders: a systematic meta-review. Psychol Med 2016; 46: 683–97. [DOI] [PubMed] [Google Scholar]


