Abstract
Background:
Obesity is increasingly prevalent worldwide and is becoming an epidemic in many countries, including Canada. We sought to describe and analyze temporal obesity trends in the Canadian adult population from 2005 through 2018 at the national and provincial or territorial levels.
Methods:
We conducted a consecutive, cross-sectional study using data from 7 sequential Canadian Community Health Survey (CCHS) cycles (2005 to 2017/18). We included data from Canadian adults (age ≥ 18 yr) who participated in at least 1 of the 7 consecutive CCHS cycles and who had body mass index values (calculated by Statistics Canada based on respondents’ self-reported weight and height). Obesity prevalence (adjusted body mass index ≥ 30) was a primary outcome variable. We analyzed temporal trends in obesity prevalence using Pearson χ2 tests with Bonferroni adjustment, and the Cochran–Armitage test of trend.
Results:
We included data from 746 408 (403 582 female and 342 826 male) CCHS participants. Across Canada, the prevalence of obesity increased significantly between 2005 and 2017/18, from 22.2% to 27.2% (p < 0.001). We observed increases across both sexes, all age groups and all Canadian provinces and territories (p < 0.001). In 2017/18, the prevalence of obesity was higher among males than females (28.9% v. 25.4%; p < 0.001); the prevalence among adults aged 40–69 years exceeded 30%. In 2017/18, Newfoundland and Labrador had the highest prevalence (39.4%), and British Columbia had the lowest (22.8%) prevalence of obesity. Over the 14-year study period, Quebec and Alberta exhibited the largest relative increases in obesity.
Interpretation:
In 2017/18, more than 1 in 4 adult Canadians lived with obesity, and from 2005 to 2017/18, the prevalence of obesity among adults in Canada increased substantially across sexes, age groups and all Canadian provinces and territories to 27.2%. Our findings call for urgent actions to identify, implement and evaluate solutions for obesity prevention and management in all Canadian provinces and territories.
According to the World Health Organization (WHO), obesity continues to advance across every region, pervading all socioeconomic classes and becoming a global epidemic, with over 13% of adults worldwide affected.1 Obesity is a progressive, multifactorial, chronic disease with high risks of relapse, recurrence2 and multiple comorbidities, including type 2 diabetes, cardiovascular diseases, nonalcoholic fatty liver disease, osteoarthritis, chronic kidney disease, chronic back pain and many types of cancer.3–9 All-cause mortality and premature mortality from adiposity-related complications are also substantially higher in people living with obesity and, as shown in many large population-based studies, increase linearly with body mass index (BMI) in this population.4,10–13 From an economic standpoint, up to 12.0% of Canadian health expenditures are attributed to obesity, with aggregated annual costs exceeding $11 billion.14
Population-wide studies of temporal obesity trends in Canadian adults using multiple sequential cross-sectional surveys at national and provincial or territorial levels are lacking, are outdated or do not include trend analyses.15–20 Exploring the prevalence of obesity and its temporal trends may assist in identifying current priorities for obesity prevention and management in Canada, including targeting geographic areas exhibiting the largest increases in obesity.
In this study, our aim was to describe and analyze temporal trends in obesity prevalence at the national and provincial or territorial levels in the adult Canadian population from 2005 through 2017/18.
Methods
Study design and data source
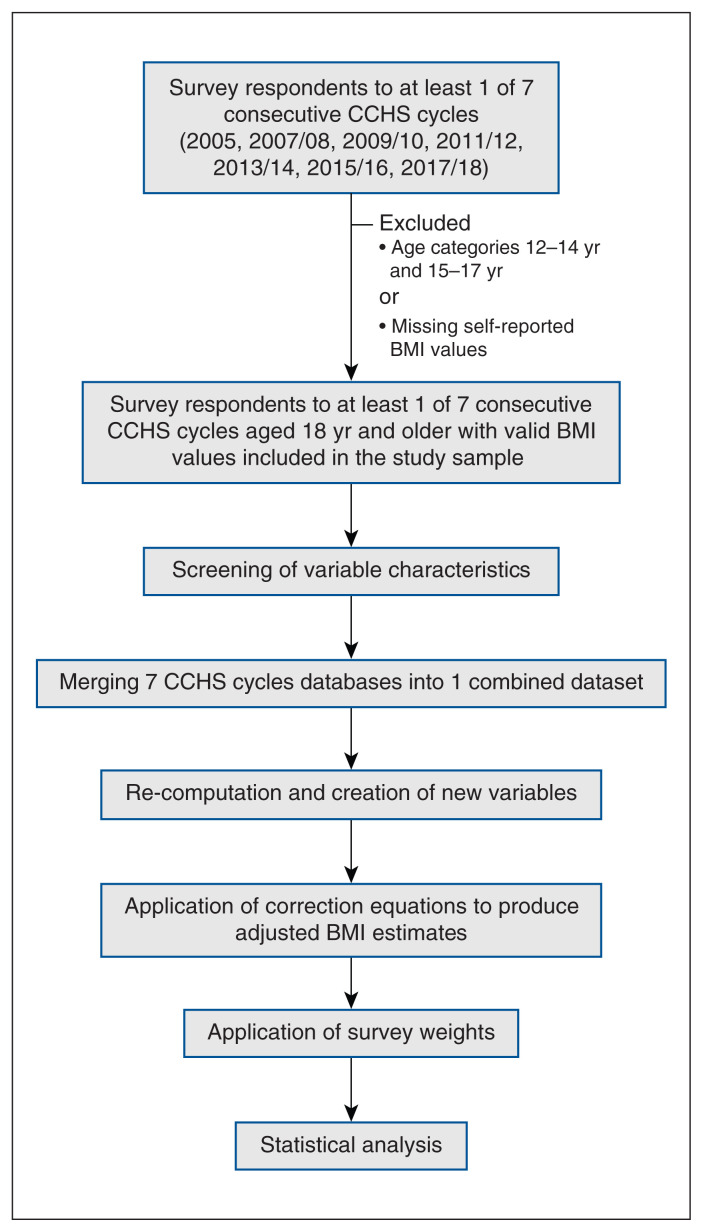
We conducted a consecutive cross-sectional study using data collected by Statistics Canada and obtained from 7 sequential cycles of the Canadian Community Health Survey (CCHS) from 2005 to 2017/18.21–27 The CCHS is a Canada-wide, cross-sectional survey designed and conducted by Statistics Canada. The survey uses a complex, multistage, multiframe, stratified sampling design that collects information related to health status, health care use and health determinants from a large national sample of survey respondents to provide estimates for the whole Canadian population.28 Estimates from Yukon, the Northwest Territories and Nunavut are combined. Surveys are conducted using computer-assisted telephone interviews, and responses are collected directly from participants. Further details about CCHS methodology and sampling strategy can be found elsewhere.28 Our step-by-step methodological approach to the study is presented in Figure 1.
Figure 1:
Flow chart outlining the data sources and step-wise methodological approach to the study. Note: BMI = body mass index, CCHS = Canadian Community Health Survey. Self-reported BMI refers to the BMI values precalculated by Statistics Canada based on self-reported weight and height.
Study population
Eligibility criteria for our study participants included being an adult (age ≥ 18 yr) participant in at least 1 of the 7 CCHS cycles, with self-reported BMI values available (i.e., BMI values precalculated by Statistics Canada based on self-reported weight and height). Exclusion criteria were driven by CCHS coverage.28 The CCHS sampling frame covers the Canadian population 12 years and older living in the 10 provinces and the 3 territorial capitals, representing about 98% of the Canadian population. The survey focuses on the population residing in private households; therefore, people who live on reserves and other Indigenous settlements, full-time members of the Canadian Armed Forces, institutionalized populations and those living in some remote areas are excluded. Self-reported BMI was not derived for pregnant people.
Variables and outcomes
The variables used in our study consisted of self-reported sex, age, province of residence and BMI. Large international and Canadian studies have consistently shown the tendency of survey participants to overestimate self-reported height and underestimate self-reported weight, leading to a systematic underestimation of obesity prevalence and its relation with adiposity-related outcomes.29–31 Therefore, to improve the estimation of obesity, we applied sex-specific correction equations developed by Gorber and colleagues (reduced Model 4) to self-reported BMI. This produces adjusted BMI estimates that yield estimates maximally in line with the measured ones.31–33
We used adjusted BMI (a number with 2 decimals) to categorize respondents into corresponding weight status categories.34–36 We defined individuals with an adjusted BMI of 30.00 or higher as obese.35 The prevalence of obesity was the primary outcome variable. A full list of CCHS questionnaire items and answer categories that were analyzed in our study can be found in Appendix 1, Supplementary Table S1, available at www.cmajopen.ca/content/10/2/E439/suppl/DC1.
Statistical analysis
For statistical estimates produced from the CCHS data to be accurate and representative of the Canadian population and not just the sample, we incorporated standardized survey weights in calculations before statistical analyses were performed.37 Categorical data were presented as proportions (weighted) and counts (unweighted).
We compared the prevalence of obesity across CCHS cycles using the 2-tailed Pearson χ2 test and adjusted the p values of posthoc paired comparisons on each pair of CCHS cycles according to the Bonferroni method for multiple pairwise comparisons. We analyzed trends in obesity prevalence over time using the Cochran–Armitage test of trend. We performed all statistical analyses and data visualization using SPSS 23.0, GraphPad Prism 6.0, and Tableau Public 2020.3, with a p value 0.05 or less indicating statistical significance.
Ethics approval
Our study was exempt from need for review by the University of Alberta Research Ethics Board as CCHS public use microdata files produced by Statistics Canada are publicly accessible via the Data Liberation Initiative.
Results
The initial sample size in the 2005–2017/18 CCHS cycles was 862 810 survey respondents. We excluded 72 469 respondents who were younger than 18 years and 43 933 who were missing BMI values. This resulted in a final sample of 746 408 CCHS survey respondents, more than half of whom were female (n = 403 582, 54.1%).
The main demographic characteristics of study participants are presented in Table 1. Respondents aged 50–59 years had the largest share in the study population compared with other age categories for the first 3 CCHS cycles, shifting to people aged 60–69 years in more recent years. Geographic area distributions were consistent throughout cycles.
Table 1:
Demographic characteristics of survey respondents by cycle of the Canadian Community Health Survey
| Characteristic | No. (%) of survey respondents | ||||||
|---|---|---|---|---|---|---|---|
| 2005 n = 115 787 |
2007/08 n = 113 322 |
2009/10 n = 106 950 |
2011/12 n = 107 691 |
2013/14 n = 110 349 |
2015/16 n = 94 316 |
2017/18 n = 97 993 |
|
| Sex | |||||||
| Female | 61 970 (49.7) | 61 492 (50.0) | 57 993 (49.7) | 59 078 (49.9) | 60 648 (49.8) | 50 158 (49.7) | 52 243 (49.8) |
| Male | 53 817 (50.3) | 51 830 (50.0) | 48 957 (50.3) | 48 613 (50.1) | 49 701 (50.2) | 44 158 (50.3) | 45 750 (50.2) |
| Age category, yr | |||||||
| 18–19 | 3840 (3.3) | 3223 (3.2) | 3319 (3.2) | 3084 (3.0) | 2973 (3.0) | 1976 (3.1) | 1756 (3.0) |
| 20–29 | 15 961 (17.4) | 13 851 (17.4) | 13 934 (17.4) | 13 653 (17.5) | 12 703 (17.1) | 10 818 (16.1) | 11 174 (16.1) |
| 30–39 | 19 321 (17.4) | 17 856 (17.5) | 15 438 (16.6) | 14 304 (16.6) | 13 752 (16.7) | 14 235 (17.5) | 14 802 (17.9) |
| 40–49 | 19 756 (21.8) | 18 688 (20.8) | 15 680 (20.2) | 14 539 (18.4) | 13 116 (17.6) | 13 739 (17.4) | 13 757 (16.6) |
| 50–59 | 20 487 (17.4) | 21 638 (18.5) | 20 124 (18.9) | 20 309 (19.1) | 20 835 (19.5) | 17 388 (18.8) | 17 250 (18.0) |
| 60–69 | 16 788 (11.5) | 18 227 (12.0) | 18 927 (13.0) | 21 186 (14.3) | 23 596 (14.7) | 18 579 (15.5) | 19 877 (15.8) |
| 70–79 | 12 758 (7.6) | 12 879 (7.4) | 12 521 (7.2) | 13 079 (7.4) | 15 186 (8.0) | 11 829 (8.3) | 13 069 (9.0) |
| ≥ 80 | 6876 (3.5) | 6960 (3.2) | 7007 (3.4) | 7537 (3.6) | 8188 (3.6) | 5752 (3.3) | 6308 (3.6) |
| Province or territory | |||||||
| Alberta | 10 151 (9.7) | 10 215 (10.3) | 9924 (10.5) | 9760 (10.9) | 10 434 (11.3) | 11 381 (11.6) | 11 732 (11.5) |
| British Columbia | 13 570 (13.3) | 13 718 (13.3) | 12 995 (13.4) | 13 418 (13.5) | 13 387 (13.3) | 12 419 (13.2) | 13 338 (13.2) |
| Manitoba | 6353 (3.4) | 6433 (3.3) | 5837 (3.3) | 5905 (3.4) | 6337 (3.3) | 4631 (3.3) | 4719 (3.4) |
| New Brunswick | 4512 (2.4) | 4746 (2.3) | 4215 (2.2) | 4207 (2.2) | 4279 (2.1) | 2841 (2.1) | 3182 (2.1) |
| Newfoundland and Labrador | 3587 (1.7) | 3481 (1.6) | 3243 (1.5) | 3074 (1.5) | 3410 (1.5) | 2729 (1.5) | 2804 (1.5) |
| Nova Scotia | 4442 (2.9) | 4486 (2.9) | 4048 (2.8) | 4011 (2.8) | 4548 (2.7) | 4105 (2.7) | 4174 (2.6) |
| Ontario | 36 578 (38.8) | 38 137 (39.0) | 36 418 (38.9) | 36 640 (38.7) | 36 566 (38.4) | 28 024 (38.3) | 28 585 (38.5) |
| Prince Edward Island | 1751 (0.4) | 2029 (0.4) | 1612 (0.4) | 1513 (0.4) | 1695 (0.4) | 1511 (0.4) | 1653 (0.4) |
| Quebec | 25 980 (24.2) | 20 742 (23.9) | 19 862 (23.7) | 20 495 (23.6) | 20 675 (23.7) | 20 487 (23.8) | 21 447 (23.5) |
| Saskatchewan | 6706 (2.9) | 6633 (2.8) | 6328 (2.8) | 6132 (2.8) | 6338 (2.9) | 3970 (2.9) | 4172 (2.9) |
| Yukon, Northwest Territories or Nunavut | 2157 (0.3) | 2702 (0.3) | 2468 (0.3) | 2536 (0.3) | 2680 (0.3) | 2218 (0.3) | 2187 (0.3) |
Prevalence and temporal trends
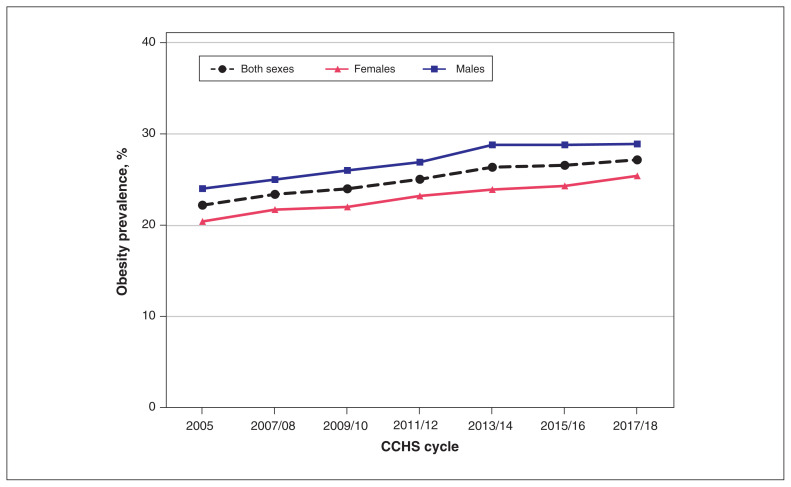
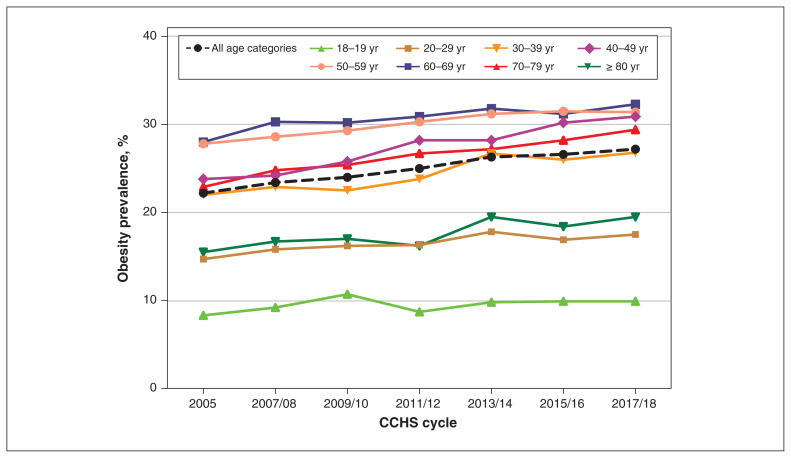
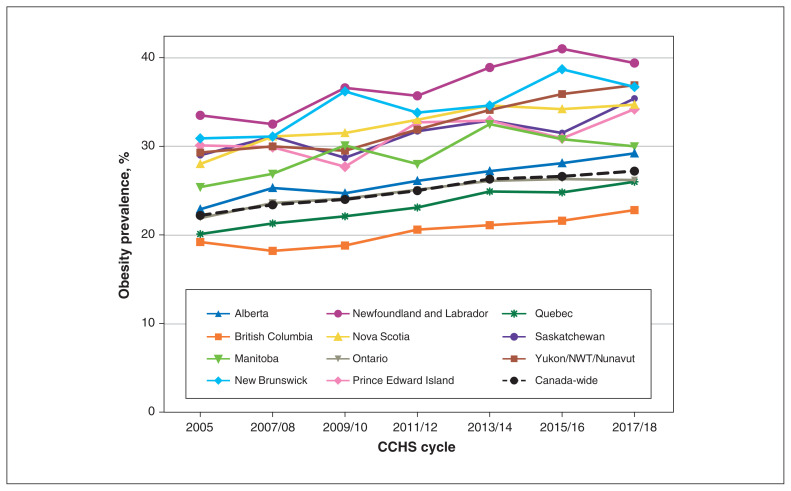
In 2005, the prevalence of obesity across Canada was 22.2% and increased significantly over 14 years, reaching the highest level of 27.2% in 2017/18 (p < 0.001), and showing a gradually rising temporal pattern (Table 2, Figure 2, Figure 3, Figure 4).
Table 2:
Temporal dynamics in prevalence of obesity across Canada and by province or territory by cycle of the Canadian Community Health Survey
| Parameter | Prevalence, % (95% CI)* | p value | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| 2005 | 2007/08 | 2009/10 | 2011/12 | 2013/14 | 2015/16 | 2017/18 | Pearson χ2 test† | Cochran–Armitage test of trend | |
| Canada, all sexes and ages | 22.2 (22.2–22.2) | 23.4 (23.4–23.4) | 24.0 (24.0–24.0) | 25.0 (25.0–25.1) | 26.3 (26.3–26.4) | 26.6 (26.5–26.6) | 27.2 (27.1–27.2) | < 0.001 | < 0.001 |
|
| |||||||||
| Sex-specific estimates | |||||||||
|
| |||||||||
| Females | 20.4 (20.4–20.4) | 21.7 (21.7–27.8) | 22.0 (21.9–22.0) | 23.2 (23.2–23.2) | 23.9 (23.9–23.9) | 24.3 (24.3–24.3) | 25.4 (25.4–25.5) | < 0.001 | < 0.001 |
|
| |||||||||
| Males | 24.0 (23.9–24.0) | 25.0 (25.0–25.1) | 26.0 (25.9–26.0) | 26.9 (26.8–26.9) | 28.8 (28.8–28.8) | 28.8 (28.8–28.8) | 28.9 (28.8–28.9) | < 0.001 | < 0.001 |
|
| |||||||||
| Age-specific estimates, yr | |||||||||
|
| |||||||||
| 18–19 | 8.3 (8.3–8.4) | 9.2 (9.1–9.2) | 10.7 (10.6–10.7) | 8.7 (8.6–8.7) | 9.8 (9.8–9.9) | 9.9a (9.9–10.0) | 9.9a (9.9–10.0) | < 0.001 | < 0.001 |
|
| |||||||||
| 20–29 | 14.7 (14.7–14.7) | 15.8 (15.7–15.8) | 16.2 (16.2–16.2) | 16.3 (16.3–16.3) | 17.8 (17.8–17.8) | 16.9 (16.9–17.0) | 17.5 (17.5–17.6) | < 0.001 | < 0.001 |
|
| |||||||||
| 30–39 | 22.0 (21.9–22.0) | 22.9 (22.9–23.0) | 22.5 (22.4–22.5) | 23.8 (23.8–23.9) | 26.7 (26.6–26.7) | 26.0 (26.0–26.0) | 26.8 (26.8–26.9) | < 0.001 | < 0.001 |
|
| |||||||||
| 40–49 | 23.8 (23.7–23.8) | 24.2 (24.2–24.3) | 25.8 (25.8–25.8) | 28.2b (28.1–28.2) | 28.2b (28.1–28.2) | 30.2 (30.2–30.3) | 30.9 (30.8–30.9) | < 0.001 | < 0.001 |
|
| |||||||||
| 50–59 | 27.8 (27.7–27.8) | 28.6 (28.6–28.7) | 29.3 (29.2–29.3) | 30.3 (30.2–30.3) | 31.2 (31.2–31.3) | 31.5 (31.5–31.6) | 31.4 (31.4–31.4) | < 0.001 | < 0.001 |
|
| |||||||||
| 60–69 | 28.0 (28.0–28.1) | 30.3 (30.3–30.4) | 30.2 (30.1–30.2) | 30.9 (30.8–30.9) | 31.8 (31.7–31.8) | 31.2 (31.2–31.3) | 32.3 (32.3–32.3) | < 0.001 | < 0.001 |
|
| |||||||||
| 70–79 | 22.9 (22.8–22.9) | 24.8 (24.8–24.9) | 25.4 (25.3–25.4) | 26.7 (26.7–26.8) | 27.2 (27.2–27.3) | 28.1 (28.1–28.2) | 29.4 (29.4–29.5) | < 0.001 | < 0.001 |
|
| |||||||||
| ≥ 80 | 15.5 (15.4–15.5) | 16.7 (16.6–16.7) | 17.0 (16.9–17.1) | 16.2 (16.1–16.3) | 19.5c (19.4–19.6) | 18.4 (18.3–18.5) | 19.5c (19.4–19.6) | < 0.001 | < 0.001 |
|
| |||||||||
| Province-specific estimates | |||||||||
|
| |||||||||
| Newfoundland and Labrador | 33.5 (33.4–33.7) | 32.5 (32.3–32.6) | 36.6 (36.5–36.8) | 35.7 (35.5–35.8) | 38.9 (38.8–39.1) | 41.0 (40.8–41.2) | 39.4 (39.2–39.5) | < 0.001 | < 0.001 |
|
| |||||||||
| Prince Edward Island | 30.1d (29.9–30.4) | 29.9d (29.6–30.2) | 27.7 (27.4–27.9) | 32.7e (32.4–33.0) | 32.9e (32.6–33.2) | 30.9 (30.6–31.2) | 34.2 (34.0–34.5) | < 0.001 | < 0.001 |
|
| |||||||||
| Nova Scotia | 28.0 (27.9–28.1) | 31.1 (31.0–31.2) | 31.5 (31.4–31.7) | 33.0 (32.9–33.1) | 34.6f (34.5–34.7) | 34.2 (34.1–34.4) | 34.7f (34.6–34.8) | < 0.001 | < 0.001 |
|
| |||||||||
| New Brunswick | 30.9g (30.8–31.1) | 31.1g (31.0–31.2) | 36.2 (36.1–36.3) | 33.8 (33.7–34.0) | 34.6 (34.4–34.7) | 38.7 (38.6–38.9) | 36.7 (36.5–36.8) | < 0.001 | < 0.001 |
|
| |||||||||
| Quebec | 20.1 (20.1–20.2) | 21.3 (21.3–21.4) | 22.1 (22.0–22.1) | 23.1 (23.1–23.1) | 24.9 (24.9–24.9) | 24.8 (24.7–24.8) | 26.0 (26.0–26.1) | < 0.001 | < 0.001 |
|
| |||||||||
| Ontario | 21.9 (21.9–22.0) | 23.6 (23.5–23.6) | 24.1 (24.1–24.1) | 25.1 (25.1–25.1) | 26.1h (26.1–26.12) | 26.3 (26.3–26.3) | 26.2h (26.2–26.2) | < 0.001 | < 0.001 |
|
| |||||||||
| Manitoba | 25.4 (25.3–25.5) | 26.9 (26.8–27.0) | 30.1 (30.0–30.2) | 28.0 (27.9–28.1) | 32.5 (32.4–32.6) | 30.8 (30.7–30.9) | 30.0 (29.9–30.1) | < 0.001 | < 0.001 |
|
| |||||||||
| Saskatchewan | 29.0 (28.9–29.1) | 31.1 (31.0–31.3) | 28.7 (28.6–28.8) | 31.7 (31.6–31.8) | 32.9 (32.8–33.0) | 31.5 (31.4–31.6) | 35.4 (35.3–35.5) | < 0.001 | < 0.001 |
|
| |||||||||
| Alberta | 22.9 (22.9–23.0) | 25.3 (25.2–25.3) | 24.7 (24.6–24.7) | 26.1 (26.0–26.1) | 27.2 (27.2–27.3) | 28.1 (28.0–28.1) | 29.2 (29.2–29.3) | < 0.001 | < 0.001 |
|
| |||||||||
| British Columbia | 19.2 (19.1–19.2) | 18.2 (18.1–18.2) | 18.8 (18.7–18.8) | 20.6 (20.6–20.7) | 21.1 (21.0–21.1) | 21.6 (21.6–21.7) | 22.8 (22.8–22.9) | < 0.001 | < 0.001 |
|
| |||||||||
| Yukon, Northwest Territories or Nunavut | 29.3i (28.9–29.6) | 30.0 (29.6–30.4) | 29.5i (29.1–29.8) | 31.9 (31.5–32.2) | 34.1 (33.8–34.5) | 35.9 (35.6–36.3) | 36.9 (36.6–37.2) | < 0.001 | < 0.001 |
Note: CCHS = Canadian Community Health Survey, CI = confidence interval.
Data are based on adjusted and weighted estimates.
Proportions compared across CCHS cycles using a 2-tailed Pearson χ2 test, with subsequent cycle-to-cycle pairwise comparisons using a 2-tailed Pearson χ2 test with p-value adjustment for multiple testing, according to the Bonferroni method. All pairwise comparisons between CCHS cycles show a statistically significant difference in proportions (p < 0.05), except for those cycles indicated by paired tags with superscript letters (a, b, c, etc.).
Figure 2:
Trends in obesity prevalence among adults in Canada, by sex, from 2005 through 2017/18. All groups showed a significantly increasing trend (p < 0.001).
Figure 3:
Trends in obesity prevalence among adults in Canada, by age category, from 2005 through 2017/18. All groups showed a significantly increasing trend (p < 0.001).
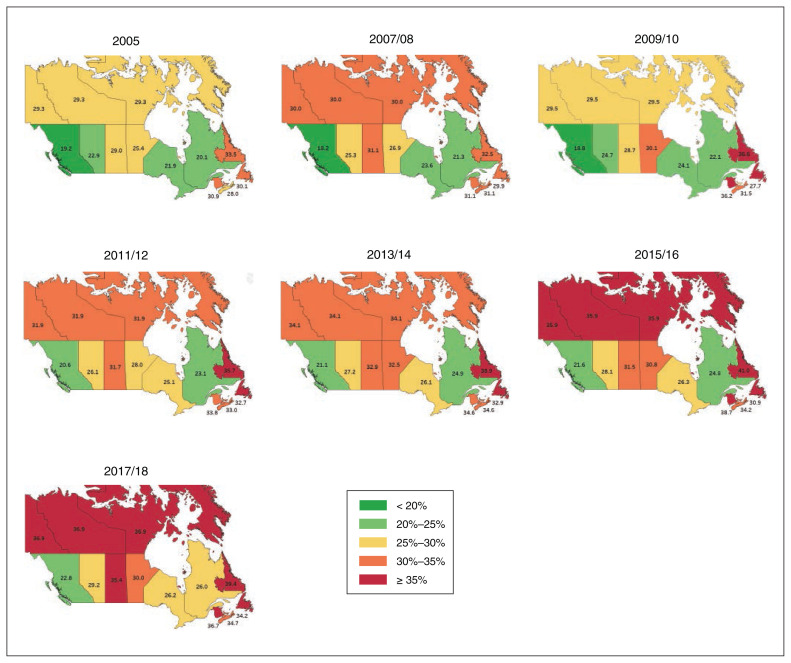
Figure 4:
Trends in obesity prevalence among adults in Canada, by province or territory, from 2005 through 2017/18. All groups showed a significantly increasing trend (p < 0.001).
In 2005, the prevalence of obesity among males was substantially higher than among females (24.0% v. 20.4%, p < 0.001). Over the subsequent 14 years, the prevalence increased in both sexes, with larger increases among females. By 2017/18, the prevalence of obesity among males continued to be significantly higher than among females (28.9% v. 25.4%, p < 0.001) (Table 2, Figure 2).
Adults aged 50–59 and 60–69 years had the highest prevalence of obesity in 2005, followed by adults aged 40–49 years (28.0%, 27.8% and 23.8%, respectively). Over the next 14 years, the prevalence increased significantly in all age groups, with the largest increase among people aged 40–49 years (p < 0.001). By 2017/18, the prevalence of obesity among adults aged 60–69, 50–59 and 40–49 years was 32.3%, 31.4% and 30.9%, respectively (Table 2, Figure 3).
In 2005, British Columbia and Quebec had the lowest prevalence of obesity (19.2% and 20.1%, respectively), while Newfoundland and Labrador, New Brunswick and Prince Edward Island had the highest prevalence (33.5%, 30.9% and 30.1%, respectively). All provinces and territories had increases in obesity prevalence from 2005 to 2017/18 (p < 0.001), with the highest prevalence remaining in Newfoundland and Labrador at 39.4% and the lowest prevalence in BC at 22.8%. Over the 14-year study period, Quebec and Alberta had the largest relative increases in obesity prevalence (Table 2, Figure 4, Figure 5).
Figure 5:
Prevalence of obesity among adults in Canada, from 2005 through 2017/18.
There were statistically significant differences in obesity prevalence across CCHS cycles for both sexes, all age categories, and at the national and provincial or territorial levels (p < 0.001). Findings of pairwise comparisons were consistent, with a significant increase in obesity prevalence across Canada with each subsequent CCHS cycle (p < 0.001). In 2017/18, sex-specific, age-specific, national and provincial or territorial prevalences were significantly higher than those in 2005 (p < 0.001). Furthermore, from 2005 through 2017/18, there was a statistically significant increasing linear trend in obesity prevalence in both sexes, and across all age groups, across Canada and in all provinces or territories (Cochran–Armitage test of trend, p < 0.001) (Table 2, Figure 2, Figure 3, Figure 4).
Interpretation
Our study findings show that the prevalence of obesity among adults in Canada increased from 22.2% in 2005 to 27.2% in 2017/18. We observed this trend across sexes, in all studied age categories and in all provinces and territories. In 2017/18, the prevalence of obesity among males was substantially higher than among females; this pattern remained unchanged over the 14-year study period. Adults aged 40–69 years had the highest obesity prevalence, exceeding 30%; those aged 40–49 years had the largest increase. Almost 4 out of 10 residents of Newfoundland and Labrador lived with obesity in 2017/18; BC had the lowest prevalence of obesity in Canada, but nevertheless, at least every fifth person was affected in that province. Quebec and Alberta exhibited the largest relative increases in obesity prevalence from 2005 to 2017/18.
We analyzed data from 7 consecutive CCHS cycles, with large sample sizes and complete data that allowed for comprehensive trend analyses. In addition, we applied well-defined and robust methodological processes as we defined explicit inclusion and exclusion criteria, included the 18–19 year age category and excluded the underweight category from analyses, rederived weight categories based on 2-decimal point BMI values to improve precision and used correction equations. A previous study comparing obesity prevalence between nonconsecutive CCHS cycles was based on data up to 2013.20 Therefore, it is challenging to compare our findings with those of other studies directly.
Based on data from the WHO Global Health Observatory data repository, the prevalence of obesity in Canada was 23.3% in 2005 and increased to 29.4% by 2016, higher than the prevalence reported in our study.38 Other high-income, English-speaking countries had similar increases, including Australia (from 22.9% to 29.0%), Ireland (from 18.7% to 25.3%), New Zealand (from 24.4% to 30.8%), the United Kingdom (from 21.4% to 27.8%) and the United States (from 29.0% to 36.2%). Global relative increases for obesity were even higher (from 9.9% to 13.1%).38 Overall, the trends identified in our study are comparable with global data, reflecting the consistently increasing prevalence of obesity worldwide.39–41
In multiple studies across the world, obesity has been identified as a major risk factor for cardiovascular diseases, different types of cancer and type 2 diabetes, along with their sequelae.3,4,8 Over the last 20 years, cardiovascular diseases and cancers have been the leading causes of death in Canada, and type 2 diabetes carries the heaviest health care cost burden.42–44 In addition, high BMI and adiposity-associated conditions, such as hypertension, hyperglycemia and hypercholesterolemia, are responsible for 27.1% of all-cause disability-adjusted life years in Canada, and high BMI is the top risk factor contributing to years lived with disability.45 The economic burden of cardiovascular diseases, cancer and type 2 diabetes combined exceeds $23 billion in direct health care costs.46
Recent meta-analyses suggest that obesity is a key risk factor for SARS-CoV-2 infection and a strong predictor of its adverse outcomes. Obesity was associated with up to a 2.1-fold higher risk for severe COVID-19, a 2.4-fold higher risk for hospital admission, a 5.3-fold higher risk for ICU admission, a 7.4-fold higher risk for invasive mechanical ventilation support and a 2.7-fold higher risk for death.47–56
The trajectory of obesity trends in Canada and across provinces and territories is increasing alarmingly and poses a substantial concern that cannot be disregarded. To understand the Canadian subpopulations most affected, it would be essential to evaluate temporal obesity patterns by sociodemographic and behavioural factors, and trends in severe obesity. Addressing obesity and its associated comorbidities will require joint efforts from many sectors, including physicians (in primary care, those specializing in obesity medicine and specialists treating comorbidities) and other health care providers; public health professionals; various stakeholders at the municipal, provincial and federal levels (including policymakers, urban planners and developers shaping community environments); community organizations; the pharmaceutical industry; employers; academia; and those living with obesity.
More recently, newly introduced medications for obesity and bariatric surgery are changing the overall approach to obesity management at an individual level.57 At the population and community levels, many interventions aimed at behavioural modification and large-scale changes in policies, in built or human-made environments, and in social support systems in various settings show evidence of meaningful weight reduction and improvement in dietary patterns and physical activity levels.58
In 2017, the Chief Public Health Officer of Canada released the Designing Healthy Living report in a call to action to improve our community environments in support of healthy living.59 Implementing and evaluating innovative interventions that have already shown reversals in longstanding obesity trends and increasing life expectancies from improvement in comorbidities at a population level should be a priority for all Canadian provinces and territories.59–74 For example, policy and environmental approaches that successfully reversed childhood obesity trends and increased life expectancies from chronic diseases in New York in 2002–2013 are being developed and evaluated in Canada through the Housing for Health initiative, funded by the Public Health Agency of Canada.75–77 Learning from the US experience, the University of Alberta’s Public Health and Preventive Medicine Residency Program and patient care partners are also developing and piloting an adult Obesity Medicine Fellowship Program in Canada for approval by the Obesity Medicine Fellowship Council.78
Limitations
Analyzing a series of cross-sectional studies does not assess for a definitive trend over time, given the lack of a clear longitudinal component. Recall, observer and social acceptability biases could also not be ruled out. Individuals living on reserves and other Indigenous settlements are excluded from CCHS coverage and, therefore, were excluded from our study; however, Indigenous populations living off reserve were included in the study population. A higher prevalence of obesity among Indigenous people in Canada living on reserve, reaching 51% in some Indigenous populations, may have contributed to the underestimation of obesity prevalence.79
Use of BMI as a proxy of weight status does not take into consideration ethnicity, sex and body composition and can be an inaccurate marker of adiposity, with high specificity but low- to-moderate sensitivity.80,81 Nevertheless, BMI has been shown to be a reliable standardized weight status measure at the population level.80–85 The robustness of relationships between BMI, obesity-related comorbidities and mortality also reflects its high utility and reliability.86 Tendency to under-report weight and over-report height, especially among people living with obesity, youth and females, can lead to underestimation of obesity prevalence but helps to avoid overestimation.29,87–90 However, unless the tendency to under-report and over-report varies over time, this should not affect temporal trends. Self-reported anthropometric measurements correlate strongly with objective measures and can be used in epidemiological studies.91–93 To overcome potential divergence, we applied correction equations developed and used by Statistics Canada to self-reported BMI estimates to produce adjusted BMI estimates that are maximally in line with measured ones.31–33
Conclusion
Our study findings suggest that more than 1 in 4 adults in Canada lived with obesity in 2017/18. From 2005 to 2017/18, the prevalence of obesity increased substantially across sexes and age groups, and in all Canadian provinces and territories. We cannot afford to ignore the increasing prevalence of obesity and obesity-related comorbidities and their negative impact on health and well-being of the current Canadian population and our future generations. Our findings highlight the urgent need to identify, develop, implement and evaluate solutions for obesity prevention and management in Canada as well as funding for such efforts.
Supplementary Material
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: Ellina Lytvyak and Karen Lee conceptualized and designed the study. Ellina Lytvyak collected the data and performed the statistical analysis. Ellina Lytvyak and Karen Lee interpreted results. Ellina Lytvyak drafted the manuscript. All authors revised it critically for important intellectual content, gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Funding: This project was funded in part by Karen Lee’s research funds through the University of Alberta Faculty of Medicine and Dentistry.
Data sharing: The public use microdata files of the Canadian Community Health Survey are produced by Statistics Canada and are publicly accessible via the Data Liberation Initiative.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/10/2/E439/suppl/DC1.
References
- 1.Obesity and overweight [fact sheet] Geneva: World Health Organization; pp. 2561–65. updated 2020 Apr. 1. [Google Scholar]
- 2.Obesity: preventing and managing the global epidemic. Geneva: World Health Organization; 2000. (WHO Technical Report Series 894). [PubMed] [Google Scholar]
- 3.Bellou V, Belbasis L, Tzoulaki I, et al. Risk factors for type 2 diabetes mellitus: an exposure-wide umbrella review of meta-analyses. PLoS One. 2018;13:e0194127. doi: 10.1371/journal.pone.0194127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schmidt M, Johannesdottir SA, Lemeshow S, et al. Obesity in young men, and individual and combined risks of type 2 diabetes, cardiovascular morbidity and death before 55 years of age: a Danish 33-year follow-up study. BMJ Open. 2013;3:e002698. doi: 10.1136/bmjopen-2013-002698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li L, Liu D-W, Yan H-Y, et al. Obesity is an independent risk factor for non-alcoholic fatty liver disease: evidence from a meta-analysis of 21 cohort studies. Obes Rev. 2016;17:510–9. doi: 10.1111/obr.12407. [DOI] [PubMed] [Google Scholar]
- 6.Plotnikoff R, Karunamuni N, Lytvyak E, et al. Osteoarthritis prevalence and modifiable factors: a population study. BMC Public Health. 2015;15:1195. doi: 10.1186/s12889-015-2529-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pinto KRD, Feckinghaus CM, Hirakata VN. Obesity as a predictive factor for chronic kidney disease in adults: systematic review and meta-analysis. Braz J Med Biol Res. 2021;54:e10022. doi: 10.1590/1414-431X202010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guh DP, Zhang W, Bansback N, et al. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88. doi: 10.1186/1471-2458-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shiri R, Karppinen J, Leino-Arjas P, et al. The association between obesity and low back pain: a meta-analysis. Am J Epidemiol. 2010;171:135–54. doi: 10.1093/aje/kwp356. [DOI] [PubMed] [Google Scholar]
- 10.Global BMI, Mortality Collaboration, Di Angelantonio E, Bhupathiraju S, Wormser D, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388:776–86. doi: 10.1016/S0140-6736(16)30175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McGee DL Diverse Populations Collaboration. Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann Epidemiol. 2005;15:87–97. doi: 10.1016/j.annepidem.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 12.Calle EE, Thun MJ, Petrelli JM, et al. Body-mass index and mortality in a prospective cohort of U.S. Adults. N Engl J Med. 1999;341:1097–105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 13.Bhaskaran K, dos-Santos-Silva I, Leon DA, et al. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3.6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6:944–53. doi: 10.1016/S2213-8587(18)30288-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tran BX, Nair AV, Kuhle S, et al. Cost analyses of obesity in Canada: scope, quality, and implications. Cost Eff Resour Alloc. 2013;11:3. doi: 10.1186/1478-7547-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vanasse A, Demers M, Hemiari A, et al. Obesity in Canada: Where and how many? Int J Obes (Lond) 2006;30:677–83. doi: 10.1038/sj.ijo.0803168. [DOI] [PubMed] [Google Scholar]
- 16.Bélanger-Ducharme F, Tremblay A. Prevalence of obesity in Canada. Obes Rev. 2005;6:183–6. doi: 10.1111/j.1467-789X.2005.00179.x. [DOI] [PubMed] [Google Scholar]
- 17.Janssen I. The public health burden of obesity in Canada. Can J Diabetes. 2013;37:90–6. doi: 10.1016/j.jcjd.2013.02.059. [DOI] [PubMed] [Google Scholar]
- 18.Luo W, Morrison H, de Groh M, et al. The burden of adult obesity in Canada. Chronic Dis Can. 2007;27:135–44. [PubMed] [Google Scholar]
- 19.Overweight and obese adults, 2018 [health fact sheets]. Cat no 82-625-X. Ottawa: Statistics Canada; 2019. [accessed 2022 May 3]. Available https://www150.statcan.gc.ca/n1/pub/82-625-x/2019001/article/00005-eng.htm. [Google Scholar]
- 20.Lebenbaum M, Zaric GS, Thind A, et al. Trends in obesity and multimorbidity in Canada. Prev Med. 2018;116:173–9. doi: 10.1016/j.ypmed.2018.08.025. [DOI] [PubMed] [Google Scholar]
- 21.Canadian Community Health Survey, 2005 public use microdata file. Ottawa: Statistics Canada; 2006. [Google Scholar]
- 22.Canadian Community Health Survey, 2007–2008 public use microdata file. Ottawa: Statistics Canada; 2009. [Google Scholar]
- 23.Canadian Community Health Survey, 2009–2010 public use microdata file. Ottawa: Statistics Canada; 2011. [Google Scholar]
- 24.Canadian Community Health Survey, 2011–2012 annual component — public use microdata file. Ottawa: Statistics Canada; 2013. [Google Scholar]
- 25.Canadian Community Health Survey, 2013–2014 annual component — public use microdata file. Ottawa: Statistics Canada; [Google Scholar]
- 26.Canadian Community Health Survey, 2015–2016 annual component — public use microdata file. Ottawa: Statistics Canada; [Google Scholar]
- 27.Canadian Community Health Survey, 2017–2018 annual component — public use microdata file. Ottawa: Statistics Canada; [Google Scholar]
- 28.Canadian Community Health Survey. Statistics Canada; [accessed 2022 May 3]. Available https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3226. [Google Scholar]
- 29.Connor Gorber S, Tremblay M, Moher D, et al. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev. 2007;8:307–26. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 30.Shields M, Connor Gorber S, Tremblay MS. Estimates of obesity based on self-report versus direct measures. Health Rep. 2008;19:61–76. [PubMed] [Google Scholar]
- 31.Connor Gorber S, Shields M, Tremblay MS, et al. The feasibility of establishing correction factors to adjust self-reported estimates of obesity. Health Rep. 2008;19:71–82. [PubMed] [Google Scholar]
- 32.Shields M, Connor Gorber S, Janssen I, et al. Bias in self-reported estimates of obesity in Canadian health surveys: an update on correction equations for adults. Health Rep. 2011;22:35–45. [PubMed] [Google Scholar]
- 33.Navaneelan T, Janz T. Adjusting the scales: obesity in the Canadian population after correcting for respondent bias. Ottawa: Statistics Canada; 2014. [Google Scholar]
- 34.Garrow JS, Webster J. Quetelet’s index (W/H2) as a measure of fatness. Int J Obes. 1985;9:147–53. [PubMed] [Google Scholar]
- 35.Canadian guidelines for body weight classification in adults. Cat no H49-179/2003E-IN. Ottawa: Health Canada; 2003. pp. 1–40. [Google Scholar]
- 36.Obesity and overweight. Geneva: World Health Organization; 2021. [accessed 2022 May 3]. Available https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. [Google Scholar]
- 37.Canadian Community Health Survey (CCHS): household weights documentation. Ottawa: Statistics Canada; [accessed 2022 May 3]. modified 2010 June 14. Available: https://www23.statcan.gc.ca/imdb-bmdi/pub/document/3226_D57_T9_V1-eng.htm. [Google Scholar]
- 38.Prevalence of obesity among adults, BMI ≥ 30 age-standardized: estimates by country. Geneva: World Health Organization; 2017. [accessed 2022 May 3]. Available https://apps.who.int/gho/data/node.main.A900A?lang=en. [Google Scholar]
- 39.Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ford ES, Li C, Zhao G, et al. Trends in obesity and abdominal obesity among adults in the United States from 1999–2008. Int J Obes (Lond) 2011;35:736–43. doi: 10.1038/ijo.2010.186. [DOI] [PubMed] [Google Scholar]
- 41.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity in the United States, 2009–2010. NCHS Data Brief. 2012;82:1–8. [PubMed] [Google Scholar]
- 42.Table 13-1: Leading causes of death, total population, by age group. Ottawa: Statistics Canada; 2020. [accessed 2022 May 3]. Available https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310039401. [Google Scholar]
- 43.Bilandzic A, Rosella L. The cost of diabetes in Canada over 10 years: applying attributable health care costs to a diabetes incidence prediction model. Health Promot Chronic Dis Prev Can. 2017;37:49–53. doi: 10.24095/hpcdp.37.2.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Braffett BH, Gubitosi-Klug RA, Albers JW, et al. DCCT/EDIC Research Group. Risk factors for diabetic peripheral neuropathy and cardiovascular autonomic neuropathy in the Diabetes Control and Complications Trial/ Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) study. Diabetes. 2020;69:1000–10. doi: 10.2337/db19-1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alam S, Lang JJ, Drucker AM, et al. Assessment of the burden of diseases and injuries attributable to risk factors in Canada from 1990 to 2016: an analysis of the Global Burden of Disease Study. CMAJ Open. 2019;7:E140–8. doi: 10.9778/cmajo.20180137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Economic burden of illness in Canada custom report. Public Health Agency of Canada; 2010. [accessed 2022 May 3]. Available: https://cost-illness.canada.ca/custom-personnalise/results-national-resultats.php. [Google Scholar]
- 47.Yang J, Tian C, Chen Y, et al. Obesity aggravates COVID-19: an updated systematic review and meta-analysis. J Med Virol. 2021;93:2662–74. doi: 10.1002/jmv.26677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Soeroto AY, Soetedjo NN, Purwiga A, et al. Effect of increased BMI and obesity on the outcome of COVID-19 adult patients: A systematic review and meta-analysis. Diabetes Metab Syndr. 2020;14:1897–904. doi: 10.1016/j.dsx.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.de Carvalho Sales-Peres SH, de Azevedo-Silva LJ, Bonato RCS, et al. Coronavirus (SARS-CoV-2) and the risk of obesity for critically illness and ICU admitted: meta-analysis of the epidemiological evidence. Obes Res Clin Pract. 2020;14:389–97. doi: 10.1016/j.orcp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Du Y, Lv Y, Zha W, et al. Association of body mass index (BMI) with critical COVID-19 and in-hospital mortality: a dose-response meta-analysis. Metabolism. 2021;117:154373. doi: 10.1016/j.metabol.2020.154373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kalligeros M, Shehadeh F, Mylona EK, et al. Association of obesity with disease severity among patients with coronavirus disease 2019. Obesity (Silver Spring) 2020;28:1200–4. doi: 10.1002/oby.22859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Földi M, Farkas N, Kiss S, et al. KETLAK Study Group. Obesity is a risk factor for developing critical condition in COVID-19 patients: a systematic review and meta-analysis. Obes Rev. 2020;21:e13095. doi: 10.1111/obr.13095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yang J, Tian C, Chen Y, et al. Obesity aggravates COVID-19: an updated systematic review and meta-analysis. J Med Virol. 2021;93:2662–74. doi: 10.1002/jmv.26677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huang Y, Lu Y, Huang Y-M, et al. Obesity in patients with COVID-19: a systematic review and meta-analysis. Metabolism. 2020;113:154378. doi: 10.1016/j.metabol.2020.154378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tamara A, Tahapary DL. Obesity as a predictor for a poor prognosis of COVID-19: a systematic review. Diabetes Metab Syndr. 2020;14:655–9. doi: 10.1016/j.dsx.2020.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhou Y, Yang Q, Chi J, et al. Comorbidities and the risk of severe or fatal outcomes associated with coronavirus disease 2019: a systematic review and meta-analysis. Int J Infect Dis. 2020;99:47–56. doi: 10.1016/j.ijid.2020.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wharton S, Lau DCW, Vallis M, et al. Obesity in adults: a clinical practice guideline. CMAJ. 2020;192:E875–91. doi: 10.1503/cmaj.191707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Obesity. Atlanta: The Community Guide. [accessed 2022 May 3]. https://www.thecommunityguide.org/topic/obesity .
- 59.The Chief Public Health Officer’s report on the state of public health in Canada 2017: designing healthy living. Ottawa: Public Health Agency of Canada; 2018. [accessed 2022 May 3]. Available: https://www.canada.ca/en/public-health/services/publications/chief-public-health-officer-reports-state-public-health-canada/2017-designing-healthy-living.html. [Google Scholar]
- 60.Puska P, Vartiainen E, Nissinen A, et al. Background, principles, implementation, and general experiences of the North Karelia Project. Glob Heart. 2016;11:173–8. doi: 10.1016/j.gheart.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 61.Rube K, Veatch M, Huang K, et al. Developing built environment programs in local health departments: lessons learned from a nationwide mentoring program. Am J Public Health. 2014;104:e10–8. doi: 10.2105/AJPH.2013.301863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Centers for Disease Control and Prevention (CDC) Obesity prevalence among low-income, preschool-aged children: New York City and Los Angeles County, 2003–2011. MMWR Morb Mortal Wkly Rep. 2013;62:17–22. [PMC free article] [PubMed] [Google Scholar]
- 63.Harris KW, Briss PA, Zaza S, editors. Task Force on Community Preventive Services. The guide to community preventive services: What works to promote health? Oxford University Press; 2005. [Google Scholar]
- 64.Lee KK. Planning and public health: the need to work together — again! PLAN Can (Centenary Ed) 2019;59:202–8. [Google Scholar]
- 65.Kelly PM, Davies A, Greig AJM, et al. Obesity prevention in a city state: lessons from New York City during the Bloomberg administration. Front Public Health. 2016;4:60. doi: 10.3389/fpubh.2016.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.World Health Organization. Metropolis Cities for health. Kobe: World Health Organization; 2014. [accessed 2022 May 3]. pp. 26–33. Available: www.drkarenlee.com/resources/who-citiesforhealth. [Google Scholar]
- 67.Vartiainen E, Laatikainen T, Peltonen M, et al. Thirty-five-year trends in cardiovascular risk factors in Finland. Int J Epidemiol. 2010;39:504–18. doi: 10.1093/ije/dyp330. [DOI] [PubMed] [Google Scholar]
- 68.Farquhar JW, Fortmann SP, Flora JA, et al. Effects of communitywide education on cardiovascular disease risk factors. The Stanford Five-City Project. JAMA. 1990;264:359–65. [PubMed] [Google Scholar]
- 69.Luepker RV, Murray DM, Jacobs DR, Jr, et al. Community education for cardiovascular disease prevention: risk factor changes in the Minnesota Heart Health Program. Am J Public Health. 1994;84:1383–93. doi: 10.2105/ajph.84.9.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Carleton RA, Lasater TM, Assaf AR, et al. The Pawtucket Heart Health Program: community changes in cardiovascular risk factors and projected disease risk. Am J Public Health. 1995;85:777–85. doi: 10.2105/ajph.85.6.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lytvyak E, Olstad DL, Schopflocher DP, et al. Impact of a 3-year multicentre community-based intervention on risk factors for chronic disease and obesity among free-living adults: the Healthy Alberta Communities study. BMC Public Health. 2016;16:344. doi: 10.1186/s12889-016-3021-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Raine KD, Plotnikoff R, Schopflocher D, et al. Healthy Alberta communities: impact of a three-year community-based obesity and chronic disease prevention intervention. Prev Med. 2013;57:955–62. doi: 10.1016/j.ypmed.2013.08.024. [DOI] [PubMed] [Google Scholar]
- 73.Lee K, Jones KS. The path well traveled: using mammalian retroviruses to guide research on XMRV. Mol Interv. 2010;10:20–4. doi: 10.1124/mi.10.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Li W, Maduro GA, Begier EM. Increased life expectancy in New York City, 2001–2010: an exploration by cause of death and demographic characteristics. J Public Health Manag Pract. 2016;22:255–64. doi: 10.1097/PHH.0000000000000265. [DOI] [PubMed] [Google Scholar]
- 75.O’Byrne R. New housing projects aim to promote healthier living by design. Edmonton: University of Alberta; 2019. [accessed 2022 May 3]. Available: https://www.folio.ca/new-housing-projects-aim-to-promote-healthier-living-by-design/ [Google Scholar]
- 76.Lee KK. Fit cities: my quest to improve the world’s health and wellness — including yours. Toronto: Doubleday Canada; 2020. [accessed 2022 May 3]. Available https://books.google.ca/books?id=n-eTDwAAQBAJ. [Google Scholar]
- 77.Housing for Health. Edmonton: University of Alberta; [accessed 2022 May 3]. Available: https://www.ualberta.ca/department-of-medicine/divisions/preventive-medicine/housing-for-health/index.html. [Google Scholar]
- 78.Obesity Medicine Fellowship Council. Denver (CO): Obesity Medicine Fellowship Council; [accessed 2022 May 3]. Available: https://omfellowship.org/ [Google Scholar]
- 79.Batal M, Decelles S. A scoping review of obesity among Indigenous peoples in Canada. J Obes. 2019;2019:9741090. doi: 10.1155/2019/9741090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chandrasekaran A. Body mass index: Is it reliable indicator of obesity. J Nutr Weight Loss. 2018;3:111–2. [Google Scholar]
- 81.Okorodudu DO, Jumean MF, Montori VM, et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: a systematic review and meta-analysis. Int J Obes (Lond) 2010;34:791–9. doi: 10.1038/ijo.2010.5. [DOI] [PubMed] [Google Scholar]
- 82.Keys A, Fidanza F, Karvonen MJ, et al. Indices of relative weight and obesity. Int J Epidemiol. 2014;43:655–65. doi: 10.1093/ije/dyu058. [DOI] [PubMed] [Google Scholar]
- 83.Romero-Corral A, Somers VK, Sierra-Johnson J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond) 2008;32:959–66. doi: 10.1038/ijo.2008.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nicholls SG. Standards and classification: a perspective on the ‘obesity epidemic’. Soc Sci Med. 2013;87:9–15. doi: 10.1016/j.socscimed.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 85.Palta M, Prineas RJ, Berman R, et al. Comparison of self-reported and measured height and weight. Am J Epidemiol. 1982;115:223–30. doi: 10.1093/oxfordjournals.aje.a113294. [DOI] [PubMed] [Google Scholar]
- 86.Abramowitz MK, Hall CB, Amodu A, et al. Muscle mass, BMI, and mortality among adults in the United States: a population-based cohort study. PLoS One. 2018;13:e0194697. doi: 10.1371/journal.pone.0194697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wilson OWA, Bopp CM, Papalia Z, et al. Objective vs self-report assessment of height, weight and body mass index: relationships with adiposity, aerobic fitness and physical activity. Clin Obes. 2019;9:e12331. doi: 10.1111/cob.12331. [DOI] [PubMed] [Google Scholar]
- 88.Chau N, Chau K, Mayet A, et al. Self-reporting and measurement of body mass index in adolescents: refusals and validity, and the possible role of socioeconomic and health-related factors. BMC Public Health. 2013;13:815. doi: 10.1186/1471-2458-13-815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Connor Gorber S, Tremblay MS. The bias in self-reported obesity from 1976 to 2005: a Canada-US comparison. Obesity (Silver Spring) 2010;18:354–61. doi: 10.1038/oby.2009.206. [DOI] [PubMed] [Google Scholar]
- 90.Engstrom JL, Paterson SA, Doherty A, et al. Accuracy of self-reported height and weight in women: an integrative review of the literature. J Midwifery Womens Health. 2003;48:338–45. doi: 10.1016/s1526-9523(03)00281-2. [DOI] [PubMed] [Google Scholar]
- 91.Olfert MD, Barr ML, Charlier CM, et al. Self-reported vs. measured height, weight, and BMI in young adults. Int J Environ Res Public Health. 2018;15:2216. doi: 10.3390/ijerph15102216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Seijo M, Minckas N, Cormick G, et al. Comparison of self-reported and directly measured weight and height among women of reproductive age: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2018;97:429–39. doi: 10.1111/aogs.13326. [DOI] [PubMed] [Google Scholar]
- 93.McAdams MA, Van Dam RM, Hu FB. Comparison of self-reported and measured BMI as correlates of disease markers in US adults. Obesity (Silver Spring) 2007;15:188–96. doi: 10.1038/oby.2007.504. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.