Abstract
Background
There is a multitude of systematic reviews of interventions for children and adolescents with autism spectrum disorder (ASD). However, most reviews seem to be based on research conducted in High-Income Countries (HIC). Thus, summary findings may not directly apply to Lower Middle-Income Countries (LMIC). Therefore, we conducted a Meta-Review analyzing systematic reviews on the effectiveness of interventions for target outcomes in children and adolescents with ASD to find out whether there are differences in effectiveness between HIC and LMIC and which interventions can be considered evidence-based in LMIC.
Methods
Electronic databases (PsycINFO, PubMed, Cochrane database of systematic reviews) were searched for reviews on interventions for ASD in children and adolescents from January 2011 through December 2021, which included studies not coming from HIC. Systematic reviews with qualitative and quantitative syntheses of findings were included. Two investigators independently assessed studies against predetermined inclusion/exclusion criteria and extracted relevant data including quality and evidence assessments. Evidence for different types of interventions in HIC vs. LMIC was planned to be compared, but none of the reviews assessed potential differences. Therefore, a narrative review of the studies from LMIC was conducted including an assessment of quality and evidence.
Results
Thirty-five reviews fulfilled the inclusion criteria. Eleven considered findings from HIC and LMIC. Sixty-nine percent included studies with various research designs; 63% provided a qualitative synthesis of findings; 77% percent assessed the quality of studies; 43% systematically assessed the level of evidence across studies. No review compared evidence from HIC and LMIC. A review of the studies from LMIC found some promising results, but the evidence was not sufficient due to a small number of studies, sometimes poor quality, and small sample sizes.
Conclusion
Systematic reviews on interventions for children and adolescents with ASD did not look for potential differences in the effectiveness of interventions in HIC and LMIC. Overall, there is very little evidence from LMIC. None of the interventions can be considered evidence-based in LMIC. Hence, additional research and mutually agreed methodological standards are needed to provide a more secure basis for evidence-based treatments in LMIC trying to establish evidence-based practices.
Keywords: interventions, autism spectrum disorder, high-income countries, lower middle-income countries, meta-review
Introduction
Autism Spectrum Disorder (ASD) is characterized by persistent deficits in social communication and social interaction across multiple contexts, including deficits in social reciprocity, in non-verbal communicative behaviors, and in skills required for developing, maintaining, and understanding relationships. In addition, restricted, repetitive patterns of behavior, interests, or activities have to be present for a diagnosis (1). Symptoms emerge during the first 3 years of life (2, 3). The symptoms of ASD vary in severity and may present differently in children with a mixture of cognitive abilities (4). The extreme variability of behavioral and communicative problems and coexisting conditions make it difficult for mental health professionals and non-specialists to identify ASD as early as possible (5, 6), although respective diagnostic tools exist for children as young as 18 months. The American Academy of Pediatrics (AAP), for example, recommends standardized screening for ASD at 18 and 24 months of age with ongoing developmental surveillance in primary care.
Worldwide, there is an increasing number of children, who meet the diagnostic criteria for ASD (7, 8). The estimated number of cases is 52 million worldwide, which means that 1–2% of children are affected (9–12). The prevalence rate for children was one in 44 in the U.S, based on a sample of 8-year-old children (13) and one in 100 in the UK (14). In Europe (Germany, Poland, France, Belgium, Denmark, Iceland, Sweden, Ireland), China, and North America the reported prevalence of ASD is close to 1.5%, but varies considerably between regions and populations (11, 15–22). The majority of the epidemiological studies were conducted in HIC. According to the World Bank (23), HIC are defined as countries with an average income of more than 12,353 U.S. dollars per year, upper middle-income countries (UMIC) by an average income between 4,046 and 12,535 dollars, and LMIC by an average income between 1,036 and 4,045 dollars per year. The prevalence rate in LMIC is rather uncertain due to a lack of research (24). A systematic review on the prevalence of ASD in Asia revealed that it was around 1.9/10,000 before 1980 and 14.8/10,000 from 1980 to 2008 (25). For South Asia, a systematic review estimated the prevalence as 0.09% in India, 1.07% in Sri Lanka, and 3% in Bangladesh (26).
ASD is considered an emerging public health issue by the World Health Organization (27). Still, research, public awareness, and mental health services are mostly concentrated in HIC. In these countries, large efforts have been made to bridge the gap between evidence and practice. By contrast, a large gap exists in LMIC due to a lack of public awareness, professional knowledge, and well-conducted scientific studies (28). International studies found that 75–85% of individuals with mental disorders including autism do not receive particular treatment services in LMIC (29), which prevents children from realizing a healthy life (30). Major barriers to increasing services for childhood mental disorders in these countries include financial constraints, absence of government initiatives, inadequately trained healthcare professionals, and an overcentralized health system (31–37). In addition, there might be limited knowledge about effective evidence-based treatments and a lack of competencies required for their implementation (38).
Many different types of treatments for children and adolescents with ASD have been developed and investigated [cf. (39)]. With respect to cognitive and/or behavioral interventions, it is important to delineate comprehensive treatment models and focused interventions. Comprehensive treatment models (CTM) are conceptually organized sets of practices, which address the core deficits of ASD over a lengthy period of time (e.g., 1–2 years). Multiple developmental domains (e.g., social communication, daily living skills, and repetitive behaviors) are targeted by using multiple interventions (e.g., The UCLA Young Autism Program by Lovaas (40), the TEACCH program developed by Lord and Schopler (41), the LEAP model, the Early Start Denver model). Many comprehensive programs aim at young children, which underlines the importance of an early diagnosis. By contrast, focused interventions are a set of individual instructional strategies that are designed to address a specific behavioral or developmental problem, for instance, joint attention or repetitive behaviors. Further examples are social skills training or visual support in academic instruction.
A special sub-group of treatments is psychosocial interventions delivered by non-specialists (parents or caregivers, peers, and teachers). In many LMIC, interventions for children and adolescents with ASD have to be delivered by these non-specialists due to a lack of other resources. Therefore, we considered these treatments separately, although the interventions themselves overlap with focussed interventions. In community settings, these interventions have been found to produce benefits in development, social-communication skills, daily living skills, comprehension or academic performance, behavior, or family outcomes (42, 43).
In recent years, technological devices have been used more often to deliver treatments, train, and support health care professionals as well as parents. Technology-based interventions make use of a broad range of devices such as speech-generating devices or robots, and software applications like computer-assisted instructional programs, or mobile- and tablet-based applications (44–47). Educational computer games (e.g., EmotionTrainer, FaceMaze, FaceSay, Squizzy, TeachTown) were designed for enhancing a broader set of skills, including social, emotional, as well as cognitive, and academic skills (48–53). As technological devices and software programs require substantial financial resources to acquire and maintain them, we decided to treat respective treatments as a separate sub-group to provide respective information for readers coming from LMIC.
In addition to cognitive and behaviorally oriented treatments, medical and alternative treatments have been developed and tested (47, 54). The use of medical treatments to address behavioral problems in children and youth with ASD has increased significantly since the publication of the AAP's clinical report in 2007 [cf. (55, 56)]. The U.S. Food and Drug Administration (FDA) has approved the use of some antipsychotic drugs, such as aripiprazole and risperidone, for the treatment of irritability/ aggression and repetitive behaviors in children and youth with ASD.
Complementary and alternative medicine (CAM) treatments refer to a broad set of health care practices that are not part of that country's own tradition and are not integrated into the dominant health care system (57). These encompass diets (e.g., gluten-free diet, ketogenic diet), nutritional supplements (e.g., omega 3 fatty acids, vitamins, melatonin), traditional alternative medicine (e.g., acupuncture), exercise (e.g., yoga), body therapies (e.g., massage, touch therapy). CAM treatments are frequently used to treat behavioral problems (e.g., aggression, irritability, hyperactivity). Some interventions classified as CAM were found to be ineffective, some potentially harmful (58, 59).
The research on the effectiveness of the different types of treatments looked at various outcomes, including language development, interpersonal skills, behavior, and academic achievement. Systematic reviews often summarize the findings for a specific type of treatment and/or for a specific type of outcome. Very few try to collate the evidence across all types of treatments [see (47, 54, 60), for exceptions]. Based on the findings, some treatments have been identified as evidence-based practices, that is, as treatments for which sufficient evidence is available that they are beneficial for the outcome under investigation. The latest review of the National Standards Project (NSP) and the National Professional Development Center (NPDC) identified 27 evidence-based practices (61, 62).
Research has shown that clinical features of ASD present the same in HIC and LMIC (63–65). However, the significant contextual differences between HIC and LMIC may result in very different consequences (66). HIC provide treatment facilities and comprehensive care for children and adolescents with ASD. A rather large number of mental health professionals with a specific focus on developmental disorders (psychiatrists as well as clinical psychologists) are available. The awareness of ASD is generally high. The situation in LMIC is rather different. In many aspects, it is quite the opposite. In most LMIC, there are very few trained professionals, who have expertise with respect to ASD-related interventions. In addition to insufficient training, there are financial constraints and limited resources within health care systems, which are much less elaborated than in HIC (33, 36, 37). Finally, there are substantial cultural differences and medical traditions in LMIC than in the mostly Western HIC. Therefore, interventions designed and tested in HIC may turn out to be less applicable and less effective in LMIC (43, 67–71). Hence, it is important to look for potential differences.
In the past two decades, many reviews (systematic and unsystematic) on treatments for children and adolescents with ASD and other developmental disorders have been published. Most of these come from researchers in HIC, although ~95% of individuals with ASD do not live in these countries (64, 72, 73). There are very few reviews that come from and focus on evidence from LMIC, although some studies have been conducted (see Table 2 for on overview). Hence, there is a need for conducting a systematic review of reviews to summarize and compare the results from HIC and/or LMIC. This is the aim of the present meta-review. It provides an overview of the existing systematic reviews published from the beginning of 2011 up to the end of 2021, analyzes potential differences in findings from HIC and LMIC, summarizes the effectiveness of the different types of interventions, and describes the quality and findings of the studies coming from LMIC.
The following research questions were addressed:
Do systematic reviews of treatments for children and adolescents with ASD consider research findings from LMIC?
Are there differences in the effectiveness of interventions in HIC and LMIC?
Which types of treatments can be considered evidence-based in LMIC?
Methods
Search strategy
A systematic review of reviews was carried out in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses guidelines [PRISMA, (74)]. Eligible review articles were obtained by searching three electronic databases: PsycINFO, PubMed and Cochrane Database of Systematic Reviews. The research team developed a series of search terms appropriate for each database using medical subject headings (MeSH). These terms included “Review” OR “Review as literature” AND “Autism” OR “Autism spectrum disorders” AND “Evidence based practice” OR “Evidence based treatment” OR “Treatment program” OR “Interventions” AND “High- income countries” OR “Lower middle-income countries.” A manual search of the reference lists of all included reviews was conducted to identify additional reviews.
Eligibility criteria
Criteria for inclusion were defined in advance. To be included, the review had to be systematic (i.e., a clear objective and research questions had to be specified and the methodology including a search and data extraction strategy had to be described in enough detail to be replicable). Reviews had to be published between January 2011 and December 2021 in English. The population had to be children and adolescents (up to 18 years of age) diagnosed with ASD. There were no restrictions with respect to treatment, treatment setting, or outcome. Reviews had to include studies coming not only from HIC. Following the classification of countries from the World Bank, this includes studies from LMIC and UMIC, although we were interested in LMIC. Note that we decided to be overinclusive at this point to provide a good overview on how research not coming from HIC is taken into account in systematic reviews. Reviews with a qualitative and/or quantitative synthesis of findings were included. Reviews not meeting these inclusion criteria were excluded.
Study selection
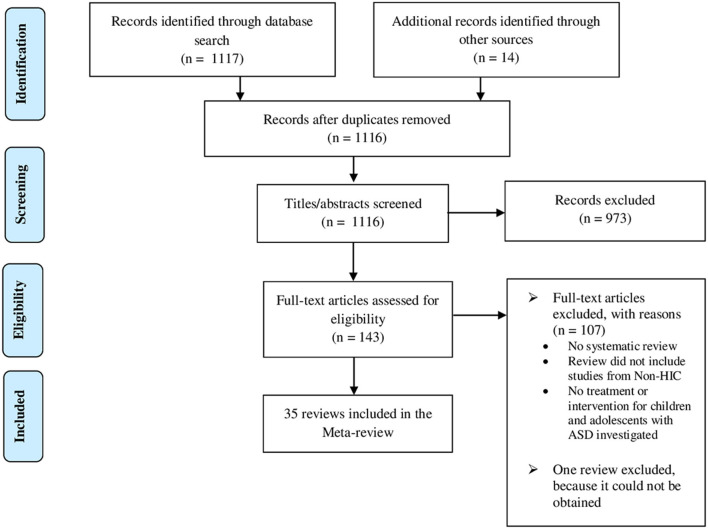
The first author screened all review papers, initially on the basis of title and abstract to identify potentially eligible reviews. All titles and abstracts were screened independently by the third author. Following this, full articles were assessed independently by the first author and third author with respect to the inclusion criterion. Initial agreement was 92%. Disagreements were resolved through discussion. Reviews not meeting the inclusion criteria were excluded. The flow of studies is presented in the respective PRISMA diagram shown in Figure 1.
Figure 1.
PRISMA flow diagram [modified from Moher et al. (74)].
Data extraction and management
Data were extracted from all eligible reviews and tabulated by the first reviewer using a set of data extraction forms, which were developed for the present meta-review. The following information were collected: name of the first author, year of publication, age group, countries of included studies [HIC, LMIC, or UMIC, as defined by the (23)], number of included studies, study designs, data synthesis method, quality assessment method for individual studies, method for evidence rating across studies, types of treatments, types of outcomes, evidence for each type of treatment according to the authors of the review. Treatments and outcomes were classified following the categories proposed by the National Autism Center (61, 62, 75). To provide a better overview, we organized treatments into the seven major groups outlined in the introduction: Comprehensive treatment programs (e.g., Early Start Denver Model, UCLA/Lovaas-based interventions), Focused interventions (e.g., social skill training), Treatments delivered by non-specialists (e.g., parent-mediated interventions), Technology-assisted interventions (e.g., video modeling), Medical treatments (e.g., risperidone), Complementary and Alternative Medicine (e.g., acupuncture), and Other (e.g., weighted vests). We selected these groups of treatments, as they might be most informative for LMIC. With respect to outcomes, we differentiated between communication and language skills, social behavior, joint attention, play, cognitive/intellectual functioning, academic performance/comprehension skills, restricted/repetitive/stereotyped behavior, challenging/problematic behaviors/irritability, hyperactivity, adaptive behavior, emotion regulation, ASD symptoms, daily living skills, sensory-motor skills, and others, respectively. Adverse effects were reported for medical as well as CAM treatments.
Narrative summary of individual studies from LMIC
It turned out that none of the reviews addressed potential differences between HIC and LMIC even when studies from both classes of countries were considered. Therefore, we further analyzed the studies coming from LMIC, which were included in the reviews to find out which types of interventions are effective in LMIC and can be considered evidence-based. All empirical studies investigating outcomes of children and adolescents were analyzed in detail. Information on study design, number of participants, interventions investigated, and major findings were extracted. Findings were summarized in a qualitative way because research designs varied widely. In addition, the quality of the studies and evidence across studies was assessed. We used the What Works Clearinghouse standards (version 4.1, https://ies.ed.gov/ncee/wwc/Resources/ResourcesForReviewers) (76), as they are applicable to group-based and single-subject designs. Data extraction and rating of studies were performed by the first and last author independently. Initial agreement was 93 and 92%, respectively (see Table 2).
Results
Review selection
Electronic database search identified a total of 1,117 review papers. Fourteen additional reviews were found by manually searching reference lists. From a total of 1,131 review papers, 15 duplicate reviews were removed. One thousand one hundred sixteen review papers were assessed for eligibility, 973 of which were excluded based on abstract and title. The full text of the remaining 143 reviews was examined against the inclusion criteria. One hundred seven reviews were excluded because they failed to meet inclusion criteria, 46 reviews because they considered only studies from HIC. One review was not considered, because it could not be obtained (77). Finally, 35 reviews were included in the current meta-review (see Figure 1).
Description of reviews
An overview of included reviews can be found in Table 1. Eight out of 35 reviews considered findings from HIC, UMIC, and LMIC, 21 from HIC and UMIC, three from HIC and LMIC, and three only from LMIC. Considering also the 46 reviews, which only included studies from HIC but met all other inclusion criteria (see Online Appendix for full list), this means that 32 of 81 reviews (40%) included research from HIC and other countries.
Table 1.
Overview of systematic reviews including studies from high-income countries (HIC), lower middle-income countries (LMIC), and upper middle-income countries (UMIC).
| References | Year |
Abbre- viated title |
Age group | Countries of studies | Studies | Synthesis method | Systematic assessment of quality and/or evidence | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Under 3 years |
Pre- school (up to 6/7) |
Up to 12 |
Adoles- cents 13-18 |
HIC | UMIC | LMIC | Total number | Single case studies | RCT |
Quali- tative |
Quanti- tative |
Quality or evidence of individual studies | Evidence across studies | |||
| Ameis et al. (78) | 2018 | Management of core and psychiatric symptoms | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ (Brazil, Iran) | ✓ (India, Pakistan) | 44 | 0 | 40 | ✓ | ✓ | Cochrane's risk of bias tool (79) |
Review specific |
| Bond et al. (80) | 2016 | Educational interventions | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ (South Africa) | 85 | 54 | 30 | ✓ | (81, 82) | Review specific [based on Wong et al. (47)] | ||
| Cheuk et al. (83) | 2011 | Acupuncture | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ (China) | ✓ (Egypt) | 10 | 0 | 10 | ✓ | Cochrane's risk of bias tool (79) |
No | |
| Dababnah et al. (67) | 2018 | Autism interventions in India |
✓ | ✓ | ✓ | ✓ | ✓ (India) | 13 | 3 | 1 | ✓ | No | No | |||
| Dawson-Squibb et al. (84) | 2020 | Parent education and training | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ (China, Turkey, Iran, Jordan) | ✓ (India, Bangladesh, Tanzania) | 37 | 0 | 5 | ✓ | Mixed methods appraisal tool (85) | No | |
| Dean and Chang (86) | 2021 | School-based social skills interventions | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ (China) | 18 | 7 | 10 | ✓ | (81, 87, 88) | No | ||
| Deb et al. (89) | 2020 | Parent training for Children with ASD | ✓ | ✓ | ✓ | ✓ | ✓(Thailand) | 17 | 0 | 15 | ✓ | ✓ | Cochrane's risk of bias tool (90) |
No | ||
| Dijkstra-de Neijs et al. (91) | 2021 | Play-based interventions | ✓ | ✓ | ✓ | ✓ | ✓ (Iran) | 32 | 0 | 32 | ✓ | ✓ | Cochrane's risk of bias tool (92) |
No | ||
| Ferguson et al. (93) | 2019 | Telehealth with behavior analytic interventions | ✓ | ✓ | ✓ | ✓ | ✓ | ✓(Georgia) | 28 | 18 | 4 | ✓ | (81) | (81, 82) | ||
| Geretsegger et al. (94) | 2016 | Music therapy | ✓ | ✓ | ✓ | ✓ | ✓ (Brazil) | 10 | 0 | 10 | ✓ | Cochrane's risk of bias tool (79) |
GRADE system (95) | |||
| Harrop (96) | 2015 | Parent-mediated interventions |
✓ | ✓ | ✓ | ✓ (Thailand) | 29 | 2 | 19 | ✓ | (81) | No | ||||
| Koly et al. (97) | 2021 | Parent-mediated intervention programs | ✓ | ✓ | ✓ | ✓ | ✓ (South Asian countries) | 9 | 0 | 5 | ✓ | The Kmet appraisal checklist (98) | No | |||
| Lee et al. (99) | 2016 | Movement-based interventions | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ (Iran) | 14 | 9 | 5 | ✓ | Mixed methods appraisal Tool (100) | No | ||
| Lee and Meadan (101) | 2020 | Parent-mediated interventions | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ (Albania, Brazil, China, Jordan, Macedonia) | ✓ (India, Pakistan, Nigeria, Tanzania) | 12 | 1 | 1 | ✓ | No | No | |
| Liu et al. (69) | 2020 | Parent-mediated interventions | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ (China) | 21 | 0 | 16 | ✓ | ✓ | Cochrane's risk of bias tool (90). QualSyst (98) |
GRADE system (102) | |
| Logan et al. (103) | 2016 | Augmentative and alternative communication interventions to increase communication | ✓ | ✓ | ✓ | ✓ | ✓ (South Africa) | 30 | 24 | 0 | ✓ | Review specific [based on (104, 105)] | No | |||
| Mazon et al. (106) | 2019 | Technology-based interventions | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ (Brazil, Thailand, Romania) | 31 | 0 | 13 | ✓ | ✓ | (107) | No | |
| McPheeters et al. (108) | 2011 | Medical treatments | ✓ | ✓ | ✓ | ✓ | ✓ (Iran) | 18 | 0 | 10 | ✓ | Review specific | AHQR standards (109) | |||
| Mercer (110) | 2017 | DIR/Floortime™ | ✓ | ✓ | ✓ | ✓ | ✓ (Thailand) | ✓ (India) | 10 | 1 | 5 | ✓ | No | No | ||
| Naveed et al. (111) | 2019 | Non-specialist mediated interventions |
✓ | ✓ | ✓ | ✓ | ✓ | ✓ (India, Pakistan) | 24 | 0 | 24 | ✓ | Cochrane's Risk of Bias Tool (79) |
GRADE system (112) | ||
| Under 3 years |
Pre- school (up to 6/7) |
Up to 12 |
Adoles-
cents 13-18 |
HIC | UMIC | LMIC | Total number | Single case studies | RCT |
Quali-
tative |
Quanti-
tative |
Quality or evidence of individual studies | Evidence across studies | |||
| Ona et al. (113) | 2020 | Pivotal response treatment | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ (Iran) | 7 | 0 | 7 | ✓ | ✓ | Cochrane's risk of bias tool (114) |
GRADE system, (115, 116) | |
| Oono et al. (117) | 2013 | Parent-mediated early interventions | ✓ | ✓ | ✓ | ✓ (Thailand) | 17 | 0 | 17 | ✓ | Cochrane's risk of bias tool (79) |
GRADE system (118) | ||||
| Patra and Kar (119) | 2020 | Autism spectrum disorder in India | ✓ | ✓ | ✓ | ✓ | ✓ (India) | 26 | 4 | 3 | ✓ | No | No | |||
| Pi et al. (120) | 2021 | Technology-assisted parent-mediated interventions | ✓ | ✓ | ✓ | ✓ | ✓ (Macedonia) | 16 | 0 | 16 | ✓ | ✓ | (81, 82) | GRADE system | ||
| Piwowarczyk et al. (121) | 2017 | Gluten- and casein-free diet |
✓ | ✓ | ✓ | ✓ | ✓ | ✓(Indonesia) | 6 | 0 | 6 | ✓ | Cochrane's risk of bias tool (122) |
No | ||
| Sathe et al. (123) | 2017 | Nutritional and dietary interventions | ✓ | ✓ | ✓ | ✓ | ✓ (Iran) | ✓ (Egypt, Indonesia) | 22 | 0 | 19 | ✓ | (124) | Review specific (based on AHQR, 2014) | ||
| Siegel and Beaulieu (125) | 2012 | Psychotropic medications | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ (Iran) | 33 | 0 | 33 | ✓ | (81) | (81) | ||
| Smith and Iadarola (126) | 2015 | Psychological and behavioral interventions |
✓ | ✓ | ✓ | ✓ (Thailand) | 29 | 0 | 23 | ✓ | ✓ | JCCAP criteria (127) | JCCAP criteria (127) | |||
| Spector (128) | 2011 | Sight word instruction | ✓ | ✓ | ✓ | ✓ | ✓ (Turkey) | 9 | 9 | 0 | ✓ | (81) | (81) | |||
| Sullivan and Wang (129) | 2020 | Autism spectrum disorder interventions | ✓ | ✓ | ✓ | ✓ | ✓ (China) | 33 | 14 | 9 | ✓ | No | No | |||
| Syriopoulou-Delli and Gkiolnta (130) | 2020 | Assistive technology | ✓ | ✓ | ✓ | ✓ | ✓ (Malaysia, Romania) | 13 | 1 | 1 | ✓ | No | No | |||
| Tan et al. (131) | 2021 | Probiotics, prebiotics, synbiotics, and fecal microbiota transplantation | ✓ | ✓ | ✓ | ✓ | ✓ (China, Thailand) | ✓ (Egypt) | 13 | 0 | 7 | ✓ | Cochrane's risk of bias tool (132) |
No | ||
| Tseng et al. (133) | 2020 | Social cognitive interventions | ✓ | ✓ | ✓ (China) | ✓ (Kenya) | 18 | 0 | 18 | ✓ | No | No | ||||
| Vetter (134) | 2018 | Parent-child interaction therapy |
✓ | ✓ | ✓ | ✓ | ✓ (Iran) | 9 | 2 | 0 | ✓ | No | No | |||
| Weitlauf et al. (124) | 2017 | Interventions targeting sensory challenges | ✓ | ✓ | ✓ | ✓ | ✓ (Brazil, Iran, Thailand Turkey) | 24 | 0 | 20 | ✓ | Review specific | Review specific [based on (135)] | |||
Reviews included between 6 and 85 different studies (M = 21.3, SD = 14.1). Reviews included either none or only very few studies from LMIC. Across all reviews, only 29 studies from LMIC investigating children's and adolescents' outcomes could be identified (see Table 2).
Table 2.
Studies from LMIC included in systematic reviews from 2011 to 2021 investigating the effectiveness of treatments.
| Type of treatment | References | Year | Age group (Years) | Country | Study design | N | Inter- vention | Control if applicable | Primary outcome | Major findings | Group-designs | Single case designs | Overall quality rating | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quality assessment | Randomized assignment | Acceptable attrition | Baseline equilvalence | Eligible outcome | No confounding | Data available |
Experimental manipulation
independent variable |
Interassessor agreement | No residual treatment effects | Enough data points | Eligible outcome | No confounding | ||||||||||||
| Comprehensive treatment programs | Gupta (136) | 2015 | 5 | India | Single case | 1 | Program based on theory of mind | Social behavior, ASD symptoms | Improved theory of mind and ASD symptoms | Yes | No | No | NA | Yes | Yes | Yes | Does not meet standards | |||||||
| Comprehensive treatment programs | Karanth et al. (137) | 2010 | 2–6 | India | Uncontrolled group design (pre vs. post) | 30 | Program based on ABA: “Communication DEALL” | Social-communication skills, adaptive skills, problematic behavior | Significantly improved communication skills, undesirable behavior reduced post intervention | No | Yes | NA | Yes | No | Does not meet standards | |||||||||
| Focused interventions | Banerjee and Ray (138)* | 2013 | 4–14 | India | Controlled group design | 20 | Play therapy plus other regular management program | Other regular management program | Communication, problematic behavior, cognition, social behavior | According to abstract: improvements in communication and social skills given play therapy | ||||||||||||||
| Focused interventions | Lal (139) | 2010 | 9–12 | India | Uncontrolled group design (pre vs. post) | 8 | Alternative and augment. Communication program | Communication and language skills, social behavior | Significantly improved language and communication skills, improved social behavior | No | Yes | NA | Yes | No | Does not meet standards | |||||||||
| Focused interventions | Lal and Chhabria (140) | 2013 | 3–6 | India | RCT | 26 | Floor time intervention based on DIR model | Usual early intervention | Social behavior | Significant improvement of the treatment group, treatment group superior to control group at post test | Yes | Yes | Yes | Yes | Yes | Meets standards without reservations | ||||||||
| Focused interventions | Malhotra et al. (141) | 2010 | 7 | India | Single case | 1 | Picture exchange communication system (PECS) | Communication and language skills | Improvements in communication skills and repetitive behavior | No | No | No | NA | Un- clear | Yes | Un-clear | Does not meet standards | |||||||
| Focused interventions | Rai et al. (142) | 2015 | 9 | India | Single case | 1 | Social stories | Problematic behavior | Improvement of undesirable behavior | Yes | No | No | No | Yes | Yes | Yes | Does not meet standards | |||||||
| Non-specialist mediated interventions | Bello-Mojeed et al. (143) | 2016 | 3–17 | Nigeria | Uncontrolled group design (Pre vs. Post) | 20 | Parent mediated behavioral intervention | Problematic behavior | Significantly reduced aggressive and self-injurious behaviors | No | Yes | NA | Yes | No | Does not meet standards | |||||||||
| Non-specialist mediated interventions | Divan et al. (144) |
2019 | 2–7 | India | RCT | 40 | Community health-workers mediated intervention | Usual care | Autism symptom severity, Dyadic social communication, Adaptive behavior |
Significantly improved autism severity scores and dyadic social communication skills with large effect size | Yes | Yes | Yes | Yes | Yes | Meets standards without reservations | ||||||||
| Non-specialist mediated interventions | Juneja et al. (145) |
2012 | 1.5–6 | India | Uncontrolled group design (Pre vs. Post) | 16 | Individualized parent mediated behavioral intervention | ASD symptoms | Significant improvements in ASD symptom severity, social and language skills | No | Un- clear | NA | Yes | No | Does not meet standards | |||||||||
| Non-specialist mediated interventions | Krishnan et al. (146) |
2016 | 4 | India | Uncontrolled group design (Pre vs. Post) | 77 | Parent-mediated multi-component, early intervention | Sensory, motor, and adaptive skills | Significant improvement of developmental age, motor skills, and cognitive performance | No | Un- clear | NA | Yes | Un- clear | Does not meet standards | |||||||||
| Non-specialist mediated interventions | Louis and Kumar (147) | 2015 | 2.5–5 | India | RCT | 30 | Home-based program with additional training for fathers | Home-based program | Language, adaptive skills, and problematic behaviors | Significant improvement in social-communication skills, adaptive behaviors, and repetitive behaviors | Yes | Un- clear | Yes | Yes | Yes | Meets standards with reservations | ||||||||
| Non-specialist mediated interventions | Manohar et al. (148) | 2019 | 2–6 | India | RCT | 50 | Brief parent-mediated intervention | Treatment as usual | Joint attention, imitation, social and adaptive skills | Significant improvement in autism severity, joint attention, dyadic interaction, language and communication skills, adaptive and intellectual functions | Yes | Yes | Yes | Yes | Yes | Meets standards without reservations | ||||||||
| Non-specialist mediated interventions | Nair et al. (149) | 2014 | 2–6 | India | Uncontrolled group design (Pre vs. Post) | 52 | Low-intensity, parent-mediated early intervention | ASD symptoms, social behavior, communication and language skills | Significant improvements in ASD symptom severity, social and language skills | No | Un- clear | NA | Yes | No | Does not meet standards | |||||||||
| Non-specialist mediated interventions | Rahman et al. (71) | 2016 | 2–9 | India and Pakistan | RCT single blind | 65 | Parent-mediated intervention for ASD in South Asia (PASS) + treatment as usual |
Treatment as usual | Parent child interaction | Significantly better parent-child interaction after PASS with large effect size, no differences with respect to problematic behavior and communication skills | Yes | Yes | Yes | Yes | Yes | Meets standards without reservations | ||||||||
| Technology assisted interventions | Barkaia et al. (150) | 2017 | 4–6 | Georgia | Single-case experiment design: multiple baseline | 3 | Telehealth coaching of therapists | Communi-cation and language skills |
Some effects on language in all three children | Yes | Yes | Yes | NA | Yes | Yes | Yes | Meets standards without reservations | |||||||
| Technology assisted interventions | Lahiri et al. (151) |
2015 | 13–18 | India | Single case | 8 | Virtual reality technology (computer assisted) | Social-communication skills | Improvements in socio-communication skills and language in individuals with ASD | Yes | No | No | No | Yes | Yes | Yes | Does not meet standards | |||||||
| Technology assisted interventions | Lal and Bali (152)* | 2007 | 5–10 | India | Controlled trial | 30 | Visual strategy training | unclear | Communication and language skills | According to abstract: improvements in communication skills | ||||||||||||||
| Technology assisted interventions | Padmanabha et al. (153) | 2019 | 3–12 | India | RCT | 40 | Home-based sensory interventions+ speech therapy and ABA |
Speech therapy and ABA | Sensory skills | Significant reduction in sensory abnormalities and improvement in overall wellbeing and health-related quality of life | Yes | Yes | Yes | Yes | Yes | Meets standards without reservations | ||||||||
| Technology assisted interventions | Paul et al. (154) | 2015 | 3–4 | India | Single case design: alternating treatment | 3 | Music-based intervention | Social-communication skills | Sung instructions were more effective for improving socio-communicative responsiveness than spoken language | Yes | Yes | Yes | NA | Yes | Yes | Yes | Meets standards without reservations | |||||||
| Medical treatments | Nagaraj et al. (155) | 2006 | 2–9 | India | RCT double blind | 40 | Risperidone | Placebo | Problematic behaviors | Significant reductions in problematic behaviors given risperidone, improvement in social- communication skills, weight gain, and increased sedation | Yes | Yes | Yes | Yes | Yes | Meets standards without reservations | ||||||||
| Medical treatments | Desousa (156) | 2010 | 5–16 | India | Controlled group design | 40 | Risperidone | Fluoxetine | Problematic behaviors | Improvement in irritability and hyperactivity given risperidone, improvement of speech and stereotypy behavior given fluoxetine | No | Un- clear | Yes | Yes | No | Does not meet standards | ||||||||
| Complemen -tary and alternative medicine |
Allam et al. (157) |
2008 | 4–7 | Egypt | RCT single blind | 20 | Scalp acupuncture plus language therapy | Language therapy alone | Communication and language skills | Significant improvement in some aspects in both groups, more improvement in attention and receptive semantics given additional acupuncture | Yes | Yes | Yes | Yes | Yes | Meets standards without reservations | ||||||||
| Complemen -tary and alternative medicine |
Fahmy et al. (158) |
2013 | 2.5–8.5 | Egypt | RCT double blind | 30 | L-Carnitine | Placebo | ASD symptoms | Significantly stronger improvement given L-Carnitine therapy (but less severe symptoms in Placebo-group at baseline) | Yes | Yes | No | Yes | Yes | Meets standards without reservations | ||||||||
| Complemen -tary and alternative medicine |
Narasingharao et al. (159) | 2017 | 5–16 | India | Controlled trial | 64 | Yoga | School curriculum | Sleep, gastro -intestinal, behavior problems |
Improvement in all three areas in yoga group but not in control group | No | Yes | Yes | Yes | Un- clear | Does not meet standards | ||||||||
| Complemen -tary and alternative medicine |
Pusponegoro et al. (160) | 2015 | 4–7 | Indonesia | RCT double blind | 74 | Diet with gluten and casein supplement |
Diet without supplement | Problematic behaviors | Significant decrease of maladaptive behavior in both groups. No difference between groups. | Yes | Yes | Yes | Yes | Yes | Meets standards without reservations | ||||||||
| Complemen -tary and alternative medicine |
Radhakrishna (161) | 2010 | 8–14 | India | Single case | 6 | Yoga | Imitation skills | Improvement in children's non-verbal communication skills, cognitive skills, and social behavior | No | No | No | NA | Un- clear |
Yes | Un- clear |
Does not meet standards | |||||||
| Complemen -tary and alternative medicine |
Saad et al. (162) | 2015 | 3–9 | Egypt | RCT double blind | 101 | Digestive enzymes | Placebo | ASD symptoms | Significantly better improvement in emotional response, ASD symptoms, and behavior given digestive enzyme treatment | Yes | Yes | Yes | Yes | Yes | Meets standards without reservations | ||||||||
| Complemen -tary and alternative medicine |
Shaaban et al. (163) | 2018 | 5–9 | Egypt | Uncontrolled group design (Pre vs. Post) | 30 | Probiotics | ASD symptoms and gastrointestinal symptoms | Significant improvements in the severity of ASD and gastrointestinal symptoms | No | No | NA | Yes | No | Does not meet standards | |||||||||
*Only abstract could be obtained.
Only randomized control trials (RCTs) were considered in 10 reviews, one considered only single case studies, the remaining included studies with various research designs. To integrate the findings, 22 (63%) provided only a qualitative synthesis, 5 (14%) only a quantitative synthesis, and 8 (23%) reported both. None of the reviews analyzed potential differences in the effectiveness of treatments for different classes of countries. This is also true for the eleven reviews, which included studies from HIC and LMIC.
Twenty-seven reviews (77%) assessed the quality or evidence provided by each individual study using a specific methodology. These methodologies varied considerably between studies. Most often Cochrane's risk of bias tool (79, 164) and the criteria proposed by Reichow et al. (81) were used. Fifteen (43%) assessed the evidence for types of treatments across studies using a specific methodology. Again, methodologies varied substantially. The Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) system (95, 112) and the criteria by Reichow et al. (81) were most frequently utilized.
Evidence for different types of treatment
Although most of the thirty-five reviews focused on a particular topic [e.g., parent-mediated early interventions, (117), see Table 1], many of the thirty-five reviews addressed more than one type of treatment according to our classification [e.g., comprehensive treatment programs, focused interventions, and parent-mediated interventions in the case of (117)]. Six reviews including 36 studies (two from LMIC) addressed comprehensive treatment programs; 14 reviews including 191 studies (five from LMIC) addressed various focused interventions; 15 reviews including 203 studies (eight from LMIC) addressed non-specialist mediated interventions; 15 reviews including 171 studies (five from LMIC) technology-assisted interventions, four reviews including 65 studies (two from LMIC) medical interventions, and 11 reviews including 67 studies (seven from LMIC) complementary and alternative medicine interventions. Hence the percentage of studies from LMIC ranged from 2.6% for focused interventions to 10% for complementary and alternative medicine. In the individual reviews only very few studies came from LMIC (0–4). This was true even for the three reviews that focused on research from LMIC (67, 97, 119). Many of the cited studies in these reviews did not investigate the ASD-related outcomes for children or adolescents.
The following sections first briefly describe which types of treatments are judged evidence-based in systematic reviews which only consider research from HIC (see Online Appendix for more detailed information on these reviews and their findings). Second, the results of the individual studies from LMIC for the respective type of treatment are summarized and their quality as well as the quality of the evidence is evaluated. Details on the studies can be found in Table 2.
Comprehensive treatment programs
As described above, comprehensive treatment programs integrate various types of interventions (i.e., applied behavior analysis, early intensive behavioral interventions, the UCLA young autism program by Lovaas and colleagues, ESDM, ToM, LEAP, TEACCH as well) over a prolonged period and are usually designed for preschoolers. The specific interventions differ between programs (60, 165).
There was consensus across reviews from HIC that comprehensive Applied Behavior Analysis (ABA) programs are evidence-based (126, 166, 167) as are Lovaas-based programs [UCLA Early Autism Project; (167, 168)].
With respect to LMIC, one single case study from India was cited in the reviews (136). It reported a positive effect of a comprehensive program on ASD symptoms and theory of mind. Another study investigated DEALL (Developmental Eclectic Approach to Language Learning), an indigenous early intervention program for children with autism, using an uncontrolled pre-post group design (137). Significant improvements in social-communication skills, motor skills, adaptive behaviors, language, and reduced behavioral problems were found.
The quality of the studies was low. The single case study did not meet the standards due to the absence of an experimental manipulation of the independent variable (136). The other study (137) did not meet the standards for group designs due to missing controls (see Table 2).
Focused interventions
Overall, focused interventions addressing social behavior (e.g., social skill training, play-based interventions, social stories) were considered established evidence-based treatments [(80, 91, 111, 169, 170); see also (171–173)]. The same was true for educational interventions aiming to improve academic performance by discrete skills teaching, response prompting strategies, and self-determination instructions (80, 169, 174). In addition, reviews judged joint attention-based interventions as evidence-based (80, 111, 167, 175).
Regarding LMIC, two reviews (67, 119) summarized studies from India on various focused interventions. One uncontrolled study investigated a vocabulary language program and reported significant improvement in language and social-communication skills at posttest (139). One single case study reported a positive effect of PECS on communication and repetitive behaviors while another single case study found that social stories reduced problematic behavior (141, 142). One RCT (140) found that a Developmental, Individual-Difference, Relationship-Based (DIR)/Floortime™ intervention improved social behavior. A second controlled study (138) reported a positive effect of play therapy in addition to the regular treatment (see Table 2 for details).
According to the WWC Procedures and Standards Handbook, one RCT met all basic design standards (140). The other controlled trial could not be evaluated because only the abstract could be obtained (138). The uncontrolled trial failed to meet standards (139) as did the two single case studies [(141, 142); see Table 2 for details].
Non-specialist mediated interventions
Most reviews focused on parent-mediated interventions, rather few considered peer-mediated interventions or teacher-mediated interventions (cf. Table 1). Several reviews judged parent training or parent-mediated interventions as evidence-based [(43, 117, 126, 167, 175, 176); see also (173)]. There was a consensus among two reviews on peer-mediated interventions (80, 111) that these interventions are effective and can be considered evidence-based. There is also some evidence for the effectiveness of teacher-implemented interventions (43, 126).
Regarding LMIC, four recent reviews looked into parent-mediated interventions for children with ASD (84, 97, 101, 119). However, most of the cited studies did not investigate the outcomes for children but looked into outcomes for parents (e.g., gain in knowledge, perceived helpfulness of intervention). Eight studies did assess ASD-related outcomes in children. Three uncontrolled studies from India (145, 146, 149) found that parent-mediated interventions improved ASD symptoms as well as social and language skills, sensory-motor and adaptive skills. One RCT from India and Pakistan (71) investigated the effectiveness of the Parent-mediated intervention for Autism Spectrum Disorder in South Asia (PASS), which is a program adapted from a program developed in the UK. They found that adding the program to a treatment as usual resulted in better parent-child interaction, but no further improvement in other outcomes. A second RCT from India by Manohar et al. (148) reported significant improvements in child-related measures such as autism severity, joint attention, social-communication skills, and adaptive behavior after a parent-mediated intervention. A third Indian RCT by Divan et al. (144) found positive effects of a community health worker-mediated communication intervention on autism severity scores and dyadic social communication skills. Louis and Kumar (147) found a positive effect of an intensive training for fathers added to a home-based program on social-communication skills, adaptive behaviors, and repetitive behaviors. One uncontrolled trial from Nigeria reported a significant effect of a parent-mediated behavioral intervention on challenging behaviors (143).
By WWC criteria, three RCTs were of good quality because they fulfilled the standards without reservations (71, 144, 148). One RCT (147) fulfilled the standards with reservations due to missing information on the randomization procedure and attrition. Four uncontrolled studies (pre-post design) did not meet the standards due to a lack of a control group (143, 145, 146, 149). According to the WWC standards at least two studies meeting standards without reservations are required for an intervention to be eligible for being considered evidence-based. There were three well-conducted RCTs. However, only one of the two studies investigating parent-mediated interventions (71, 148) reported positive effects on ASD symptoms. The third study (144) concerned community-health worker mediated interventions. In addition, <50% of the evidence comes from studies meeting standards without reservations. Hence there is not sufficient evidence.
Technology-assisted interventions
In line with previous research, we considered technology-assisted interventions to be interventions in which technology is the central feature supporting the acquisition of a goal of the learner such as social or academic skills, challenging behaviors, or daily living activities (44–47). Interventions include computer-based interventions, video-modeling music therapy, visual strategies training, video modeling, neurofeedback, Ayres Sensory Integration, and Augmented Auditory Integration. Overall, there was no consensus among reviews that technology-based interventions can be considered evidence-based, although promising results have been reported in quite a number of studies [see the reviews by (106, 120, 130, 177); for more information].
Regarding LMIC, one single case experimental study from Georgia investigating the effect of distance coaching of therapists found some effects of the intervention on the language skills of three children (150). A single case experimental study from India (154) found that sung instructions, as compared to spoken directives, were more effective in improving socio-communicative responsiveness in children. A non-experimental single case study from India on virtual reality-based interventions reported positive effects on social-communication skills [(151); see Table 2]. One controlled trial from India reported a significant effect of technology-based visual strategy training on communication skills (152). One RCT from India on home-based sensory interventions reported significant improvement in sensory abnormalities as well as overall wellbeing and health-related quality of life (153).
According to WWC Procedures and Standard Handbook, the two studies with single-case experimental designs met the standards (150, 154), while the other single case study did not (151). One RCT met all basic design standards (153). Unfortunately, the quality of one controlled trial could not be assessed as the full article could not be acquired (152).
Medical treatments
Overall, quite a number of reviews based on research from HIC considered aripiprazole and risperidone as evidence-based treatments for irritability, hyperactivity, repetitive behaviors, and inappropriate speech. However, significant side effects including marked weight gain and sedation were found for these medications (78, 108, 125, 178–180). Two Cochrane reviews pointed out lacking evidence for a long-term use of aripiprazole and risperidone (178, 180). The cited reviews also addressed other pharmacological treatments (including SSRIs, stimulants, sympatholytic agents, and chelating agents), none of which were considered evidence-based.
No evidence from LMIC was mentioned in the reviews until 2019. A more recent review (119), cites one RCT from India, which found risperidone to be effective in reducing behavioral problems (aggressiveness, hyperactivity, and irritability) and in improving social responsiveness and non-verbal communication skills (155). The same review also considers a non-randomized trial from India, which compared the efficacy and safety of risperidone and fluoxetine (156). A significant positive effect of risperidone on irritability and hyperactivity was found, while fluoxetine reduced speech deviance, social withdrawal, and stereotypic behavior. While the RCT met the standards of the WWC without reservations, the non-randomized trial did not. In addition, sample sizes were rather small.
Complementary and alternative medicine
In general, none of the treatments in this category have been considered evidence-based [see (78, 83, 111, 123, 124, 131)].
Regarding LMIC, one RCT from Indonesia found inconclusive results with respect to gluten and casein supplementation (160). One RCT from Egypt (162) investigated the effect of digestive enzymes and found significant improvement in emotional response and autistic behaviors. Another RCT from Egypt (158) showed an effect of L-Carnitine therapy in improving autistic behaviors. An RCT on acupuncture from Egypt (157) found that acupuncture in conjunction with language therapy may have an additional positive effect on some aspects of communication and language [see Cochrane review from (83), for more findings on acupuncture mostly coming from China a UMIC). A recent review from India (119) cited two studies on yoga. A controlled trial found that structured yoga improved gastrointestinal symptoms, sleep problems, and behavioral problems (159). A small uncontrolled study reported that integrated yoga therapy (IAYT) increased imitation skills (161). Another recent review by Tan et al. (131) cited one study from Egypt on probiotics and reported significant improvements in the severity of ASD and gastrointestinal symptoms (163). The four RCTs met the WWC standards without reservations, while the three other studies did not meet the standards (see Table 2 for more details).
Summary of evidence
Comprehensive treatment programs are well-investigated in HIC and some are considered evidence-based [see (47)]. Evidence from LMIC is lacking apart from two low-quality studies from India (136, 137), which entails that none of these programs can be considered evidence-based for LMIC.
Research on focused interventions also comes mostly from HIC [(61, 62); see (173), for a recent summary]. There are a few isolated studies on different types of focused interventions from LMIC, not providing sufficient evidence to consider them evidence-based. There were, however, two controlled studies looking into interventions addressing social-communication skills (a DIR/Floortime intervention and a play-based intervention) with reported positive findings (138, 140).
Non-specialist mediated interventions are particularly interesting for LMIC, as they require less resources and may be used to provide care for a larger number of children and adolescents. Reviews judged parent training or parent-mediated interventions as effective with good evidence, especially for preschoolers in HIC [(42, 43, 176); see also (173)]. In LMIC, however, the evidence is still insufficient to judged parent-mediated interventions as evidence-based. Two reviews from India and one review from Bangladesh judged parent-mediated interventions as effective (67, 97, 119). It is important to note, however, that in the review by Dababnah et al. (67) the total number of studies with respect to ASD was low. Two recent reviews by Patra and Kar (119) and Koly et al. (97) reported only three RCTs with good quality, while the other studies were mostly low-quality. Three other reviews also looked into parent-mediated interventions and/or parent training citing studies from LMIC (69, 84, 101). However, most of these studies did not look into children's outcomes in LMIC.
Many technology-based interventions have been tried for children and adolescents in HIC. For most interventions, high-quality evidence is still lacking. Recently, Steinbrenner et al. (173) judged video modeling and technology-aided instruction and intervention as evidence-based. Concerning LMIC, there is a lack of studies exploring the effect of technology-based interventions.
With respect to medical interventions, most studies were conducted in HIC focusing on the effect of pharmacological agents on behavioral problems. A new review from India [LMIC, (119)] included two studies on risperidone and found this medical agent to be effective for reducing behavioral problems (155, 156). These findings on antipsychotic medication conform to the findings in HIC.
Research on complementary and alternative medical treatments comes from HIC, UMIC, and LMIC. The existing evidence base is still too limited for the various types of CAM treatments. Again, evidence from LMIC is scarce and scattered across different treatments. Hence, none can be considered evidence-based.
Discussion
In line with the significant increase in the prevalence of ASD in children and adolescents over the past two decades worldwide, a lot of research on different types of treatments for many different types of outcomes has been completed. Many systematic reviews have been published summarizing the respective research and more are published every year. We conducted a meta-review analyzing systematic reviews on the effectiveness of treatments and interventions in children and adolescents with ASD from 2011 until the end of 2021, which also considered research not coming from HIC. Our aims were to find out whether there are differences in the effectiveness of treatments in HIC vs. LMIC and which types of treatments can be considered evidence-based in LMIC.
Summary of key findings
In this systematic review of reviews, we identified 35 systematic reviews that included research from LMIC and/or UMIC. Thirty-one of these considered also research from HIC. In the same time span (2011–2021) another 46 reviews on interventions for children and adolescents with ASD were published only including studies from HIC. There are many potential reasons why research studies from LMIC (and UMIC) may not be included in a systematic review. One is that these studies may be difficult to find and/or obtain. Another is that many of the studies were not RCTs and many not of high quality. Thus, these studies may have been excluded due to the inclusion criteria of the respective review.
Although eleven of the identified reviews included research from HIC and LMIC, none of the reviews looked for potential differences in effectiveness for a particular type of intervention. One obvious reason was the low number of studies from LMIC, which precluded any meaningful statistical comparison. Another seems to be lack of awareness that there may be relevant differences.
When we went back to the original studies from LMIC, which were cited in the reviews, we found studies with many different research questions, various research designs, and often a rather low quality. Nevertheless, we analyzed these studies and provided a narrative synthesis. Because of their heterogeneity, it did not make sense to integrate their findings statistically and compare them to the average findings from HIC. Thus, we were unable to determine, whether there are differences in the effectiveness of treatments in HIC and LMIC.
Finally, we evaluated the studies from LMIC for quality and evidence. Due to the low number of high-quality studies, no type of treatment fulfilled the criteria for being evidence-based according to the What Works Clearinghouse standards (version 4.1, https://ies.ed.gov/ncee/wwc/Resources/ResourcesForReviewers). One reason, why research from LMIC is still scarce, is probably the limited amount of funding available [cf. (33, 36, 37)]. Another reason may be that the awareness of the importance of research and knowledge about respective research methodologies is still moderate in some LMICs. A final reason might be that international publication fees are often prohibitively expensive, despite the price reductions for researchers from LMIC. This may reduce the international visibility of existing research.
Limitations
Because of the many choices that have to be made when conducting a review of reviews with many methodological differences, some limitations exist. First, we decided to include only reviews that were published in English. Despite English being the common language of science, some reviews especially from LMIC might have been published in other languages. Therefore, some reviews and the findings summarized in them may be missing.
Second, we decided to include reviews being published between 2011 and the end of 2021 that consider research from HIC and LMIC and/or UMIC by searching only three electronic databases (PsycINFO, PubMed, Cochrane Database of Systematic Reviews). An updated version of this meta-review in the future should use more databases including databases collating research papers published in the languages of LMIC.
The third important decision, which limits our findings, was to consider only reviews that systematically reviewed the literature on interventions. While assessing the full texts we found some interesting unsystematic reviews of research from LMIC [e.g., (181)]. Following our inclusion criteria, we excluded these reviews. If the results from these unsystematic collections of research studies had been included, more research from LMIC might have been taken in account.
Fourth, we used the classification scheme of high-income, upper middle-income, and lower middle-income countries provided by the World Bank, which is the commonly used standard (e.g., by the WHO). This classification scheme is based on average income. As it does not specifically consider the health care system, some researchers have criticized using this classification scheme for making comparisons between countries [e.g., (101)]. They suggest to compare low-resource settings in health care to high resource settings instead.
Implications for practice and future research
Although we were able to identify 35 systematic reviews summarizing the results from many empirical studies, there was very little evidence from LMIC. The eleven reviews including research from LMIC ran no analyses comparing results from HIC and LMIC. This finding has two important implications. First, more research needs to be conducted in LMIC on the effectiveness of different treatments and interventions for children and adolescents with ASD. The research should be of high quality no matter whether single case experimental designs or randomized group-based designs are used. Second, findings for HIC and LMIC need to be compared systematically. HIC and LMIC countries differ in many respects, including differences in health care systems but also in cultural and medical traditions. Hence, findings from HIC on specific treatments cannot be easily transferred to LMIC. There is no alternative to conducting the respective studies and to comparing the findings.
Nevertheless, there are some tentative implications for practice in LMIC. Many of the treatments that have been established as evidence-based by previous research, have to be considered as evidence-based only for HIC (see https://mn.gov/mnddc/asd-employment/pdf/09-NSR-NAC.pdf and https://www.nationalautismcenter.org/national-standards-project/phase-2/ for a good overview of these treatments). As shown in the present meta-review, there is currently not sufficient evidence for these interventions and treatments in LMIC to consider them evidence-based. There seems to be one notable exception: parent-mediated interventions. The reviews by Dababnah et al. (67), Koly et al. (97), Lee and Meadan (101), and Patra and Kar (119) concluded that these interventions are effective in LMIC. The evidence, however, was mostly indirect showing that parents acquire more knowledge and skills through these interventions. As shown here, direct evidence with respect to children's outcomes is still limited and studies were often of low quality. The review by Reichow et al. (43), however, supports the conclusion of the four reviews by showing that educating parents to deliver behavioral interventions is effective to address developmental disorders in LMIC. Thus, parent-mediated interventions can be considered at least promising and probably effective.
Another interesting option for LMIC might be the delivery of interventions by paraprofessionals, e.g., nurses, teaching assistants, social workers [cf. (182)]. At present respective research is almost completely lacking, but it might be interesting to explore this option in the future [see (144) for a first trial]. It also important to note that other evidence-based treatments and interventions from HIC might be promising for LMIC when being adapted to the respective context. Given the biological basis of ASD and the similar presentation of ASD in LMIC and HIC, treatments could work in both contexts.
Conclusion
Treatments for children and adolescents with ASD, which are considered evidence-based in HIC, are still rarely investigated in LMIC. The findings presented here may still support mental health researchers, government organizations, and NGOs that seek to improve an uptake of effective treatments for children with autism in LMIC by summarizing the present state of research and pointing out, what evidence is still missing. It also shows that parent-mediated interventions at present have the best evidence for being effective, although the evidence is not sufficient when high standards are applied. We hope that the overview of reviews considering studies from LMIC and/or UMIC provides an easy access to mental health professionals (both specialists and non-specialists) in LMIC to the respective research. We recommended mental healthcare providers, clinicians, and other caregivers to look into these reviews and maybe even individual studies for more details on the specific treatments and interventions. This information along with their personal experience may allow them to engage in evidence-based practice when delivering treatments to children and adolescents with ASD.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MP, HA, and YH contributed to the conception and design of the meta-review. MP organized the database, wrote the first draft of the manuscript, and extracted the data. MP and YH made the bibliographic search and selected papers for the meta-review. HA contributed with comments to the draft, especially the introduction and the LMIC context. All authors contributed to the revision of the first draft, read, and approved the submitted version of the manuscript.
Funding
This work was supported by a grant from the University of Goettingen, Germany and Ministry of Science and Technology, Government of Bangladesh.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.834783/full#supplementary-material
References
- 1.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th edition. Washington, DC: American Psychiatric Association; (2013). 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- 2.Lai MC, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. (2015) 2:1013–27. 10.1016/S2215-0366(15)00277-1 [DOI] [PubMed] [Google Scholar]
- 3.Varcin KJ, Jeste SS. The emergence of autism spectrum disorder (ASD): insights gained from studies of brain and behaviour in high-risk infants. Curr Opin Psychiatry. (2017) 30:85. 10.1097/YCO.0000000000000312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.King M, Bearman P. Diagnostic change and the increased prevalence of autism. Int J Epidemiol. (2009) 38:1224–34. 10.1093/ije/dyp261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hyman SL, Levy SE, Myers SM, Kuo DZ, Apkon S, Davidson LF, et al. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics. (2020) 145:e20193447. 10.1542/peds.2019-3447 [DOI] [PubMed] [Google Scholar]
- 6.Noterdaeme M, Hutzelmeyer-Nickels A. Early symptoms and recognition of pervasive developmental disorders in Germany. Autism. (2010) 14:575–88. 10.1177/1362361310371951 [DOI] [PubMed] [Google Scholar]
- 7.Fombonne E. Epidemiology of pervasive developmental disorders. Pediatr Res. (2009) 65:591–8. 10.1203/PDR.0b013e31819e7203 [DOI] [PubMed] [Google Scholar]
- 8.Williams JG, Higgins JP, Brayne CE. Systematic review of prevalence studies of autism spectrum disorders. Arch Dis Child. (2006) 91:8–15. 10.1136/adc.2004.062083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baxter AJ, Brugha TS, Erskine HE, Scheurer RW, Vos T, Scott JG. The epidemiology and global burden of autism spectrum disorders. Psychol Med. (2015) 45:601–13. 10.1017/S003329171400172X [DOI] [PubMed] [Google Scholar]
- 10.Hahler EM, Elsabbagh M. Autism: a global perspective. Curr Dev Disord Rep. (2015) 2:58–64. 10.1007/s40474-014-0033-3 [DOI] [Google Scholar]
- 11.Lyall K, Croen L, Daniels J, Fallin MD, Ladd-Acosta C, Lee BK, et al. The changing epidemiology of autism spectrum disorders. Annu Rev Public Health. (2017) 38:81–102. 10.1146/annurev-publhealth-031816-044318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Narzisi A, Posada M, Barbieri F, Chericoni N, Ciuffolini D, Pinzino M, et al. Prevalence of autism spectrum disorder in a large Italian catchment area: a school-based population study within the ASDEU project. Epidemiol Psychiatr Sci. (2020) 29:e5. 10.1017/S2045796018000483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maenner MJ, Shaw KA, Bakian AV, Bilder DA, Durkin MS, Esler A, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2018. MMWR Surveill Summ. (2021) 70:1. 10.15585/mmwr.ss7011a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.British Medical Association. Autism Spectrum Disorder. (2020). Retrieved on https://www.bma.org.uk/what-we-do/population-health/child-health/autism-spectrum-disorder (accessed September 7, 2020).
- 15.Bachmann CJ, Gerste B, Hoffmann F. Diagnoses of autism spectrum disorders in Germany: time trends in administrative prevalence and diagnostic stability. Autism. (2018) 22:283–90. 10.1177/1362361316673977 [DOI] [PubMed] [Google Scholar]
- 16.Boilson AM, Staines A, Ramirez A, Posada M, Sweeney MR. Operationalisation of the European protocol for autism prevalence (EPAP) for autism spectrum disorder prevalence measurement in Ireland. J Autism Dev Disord. (2016) 46:3054–67. 10.1007/s10803-016-2837-y [DOI] [PubMed] [Google Scholar]
- 17.Dereu M, Warreyn P, Raymaekers R, Meirsschaut M, Pattyn G, Schietecatte I, et al. Screening for autism spectrum disorders in flemish day-care centres with the checklist for early signs of developmental disorders. J Autism Dev Disord. (2010) 40:1247–58. 10.1007/s10803-010-0984-0 [DOI] [PubMed] [Google Scholar]
- 18.Idring S, Lundberg M, Sturm H, Dalman C, Gumpert C, Rai D, et al. Changes in prevalence of autism spectrum disorders in 2001–2011: findings from the Stockholm youth cohort. J Autism Dev Disord. (2015) 45:1766–73. 10.1007/s10803-014-2336-y [DOI] [PubMed] [Google Scholar]
- 19.Parner ET, Thorsen P, Dixon G, De Klerk N, Leonard H, Nassar N, et al. A comparison of autism prevalence trends in Denmark and Western Australia. J. Autism Dev Disord. (2011) 41:1601–8. 10.1007/s10803-011-1186-0 [DOI] [PubMed] [Google Scholar]
- 20.Saemundsen E, Magnússon P, Georgsdóttir I, Egilsson E, Rafnsson V. Prevalence of autism spectrum disorders in an Icelandic birth cohort. BMJ Open. (2013) 3:e002748. 10.1136/bmjopen-2013-002748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Skonieczna-Zydecka K, Gorzkowska I, Pierzak-Sominka J, Adler G. The prevalence of autism spectrum disorders in West Pomeranian and Pomeranian regions of Poland. J Appl Res Intellect Disabil. (2017) 30:283–9. 10.1111/jar.12238 [DOI] [PubMed] [Google Scholar]
- 22.van Bakel MME, Delobel-Ayoub M, Cans C, Assouline B, Jouk PS, Raynaud JP, et al. Low but increasing prevalence of autism spectrum disorders in a French area from register-based data. J Autism Dev Disord. (2015) 45:3255–61. 10.1007/s10803-015-2486-6 [DOI] [PubMed] [Google Scholar]
- 23.World Bank. Historical Classification by Income. World Bank (2020). Available online at: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519
- 24.Elsabbagh M, Divan G, Koh YJ, Kim YS, Kauchali S, Marcín C, et al. Global prevalence of autism and other pervasive developmental disorders. Autism Res. (2012) 5:160–79. 10.1002/aur.239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sun X, Allison C. A review of the prevalence of autism spectrum disorder in Asia. Res Autism Spectr Disord. (2010) 4:156–67. 10.1016/j.rasd.2009.10.00331735373 [DOI] [Google Scholar]
- 26.Hossain MD, Ahmed HU, Uddin MJ, Chowdhury WA, Iqbal MS, Kabir RI, et al. Autism spectrum disorders (ASD) in South Asia: a systematic review. BMC Psychiatry. (2017) 17:281. 10.1186/s12888-017-1440-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization . Meeting Report: Autism Spectrum Disorders and Other Developmental Disorders: From Raising Awareness to Building Capacity. Geneva: World Health Organization; (2013). [Google Scholar]
- 28.Dua T, Barbui C, Clark N, Fleischmann A, Poznyak V. Evidence-based guidelines for mental, neurological, and substance use disorders in low- and middle-income countries: summary of WHO recommendations. PLoS Med. (2011) 8:e1001122. 10.1371/journal.pmed.1001122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the world health organization world mental health surveys. JAMA. (2004) 291:2581–90. 10.1001/jama.291.21.2581 [DOI] [PubMed] [Google Scholar]
- 30.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2197–223. 10.1016/S0140-6736(12)61689-4 [DOI] [PubMed] [Google Scholar]
- 31.Adugna MB, Nabbouh F, Shehata S, Ghahari S. Barriers and facilitators to healthcare access for children with disabilities in low and middle income sub-Saharan African countries: a scoping review. BMC Health Serv Res. (2020) 20:15. 10.1186/s12913-019-4822-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Blake JM, Rubenstein E, Tsai PC, Rahman H, Rieth SR, Ali H, et al. Lessons learned while developing, adapting and implementing a pilot parent-mediated behavioural intervention for children with autism spectrum disorder in rural Bangladesh. Autism. (2017) 21:611–21. 10.1177/1362361316683890 [DOI] [PubMed] [Google Scholar]
- 33.Dababnah S, Bulson K. “On the sidelines”: access to autism-related services in the West Bank. J Autism Dev Disord. (2015) 45:4124–34. 10.1007/s10803-015-2538-y [DOI] [PubMed] [Google Scholar]
- 34.Eid AM, Aljaser SM, AlSaud AN, Asfahani SM, Alhaqbani OA, Mohtasib RS, et al. Training parents in Saudi Arabia to implement discrete trial teaching with their children with autism spectrum disorder. Behav Anal Pract. (2017) 10:402–6. 10.1007/s40617-016-0167-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harrison AJ, Long KA, Manji KP, Blane KK. Development of a brief intervention to improve knowledge of autism and behavioral strategies among parents in Tanzania. Intellect Dev Disabil. (2016) 54:187–201. 10.1352/1934-9556-54.3.187 [DOI] [PubMed] [Google Scholar]
- 36.Saraceno B, van Ommeren M, Batniji R, Cohen A, Gureje O, Mahoney J, et al. Barriers to improvement of mental health services in low-income and middle-income countries. Lancet. (2007) 370:1164–74. 10.1016/S0140-6736(07)61263-X [DOI] [PubMed] [Google Scholar]
- 37.Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. (2007) 370:878–89. 10.1016/S0140-6736(07)61239-2 [DOI] [PubMed] [Google Scholar]
- 38.Mannan M. Autism in Bangladesh: current scenario and future prospects. Eur J Paediatr Neurol. (2017) 21:e207. 10.1016/j.ejpn.2017.04.1087 [DOI] [Google Scholar]
- 39.Odom SL, Duda MA, Kucharczyk S, Cox AW, Stabel A. Applying an implementation science framework for adoption of a comprehensive program for high school students with autism spectrum disorder. Remedial Spec Educ. (2014) 35:123–32. 10.1177/0741932513519826 [DOI] [Google Scholar]
- 40.Lovaas OI. Behavioral treatment and normal educational and intellectual functioning in young autistic children. J Consult Clin Psychol. (1987) 55:3–9. [DOI] [PubMed] [Google Scholar]
- 41.Lord C, Schopler E. TEACCH services for preschool children. In Harris SL, Handleman JS, editors. Preschool Education Programsfor Children with Autism. Austin, TX: Pro-Ed; (1994). p. 87–106. [Google Scholar]
- 42.Parsons D, Cordier R, Vaz S, Lee HC. Parent-mediated intervention training delivered remotely for children with autism spectrum disorder living outside of urban areas: systematic review. J Med Internet Res. (2017) 19:e198. 10.2196/jmir.6651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Reichow B, Servili C, Yasamy MT, Barbui C, Saxena S. Non-specialist psychosocial interventions for children and adolescents with intellectual disability or lower-functioning autism spectrum disorders: a systematic review. PLoS Med. (2013) 10:e1001572. 10.1371/journal.pmed.1001572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Begum M, Serna RW, Yanco HA. Are robots ready to deliver autism interventions? A comprehensive review. Int J Soc Robot. (2016) 8:157–81. 10.1007/s12369-016-0346-y [DOI] [Google Scholar]
- 45.Grynszpan O, Weiss PL, Perez-Diaz F, Gal E. Innovative technology-based interventions for autism spectrum disorders: a meta-analysis. Autism. (2014) 18:346–61. 10.1177/1362361313476767 [DOI] [PubMed] [Google Scholar]
- 46.Odom SL, Thompson JL, Hedges S, Boyd BA, Dykstra JR, Duda MA, et al. Technology-aided interventions and instruction for adolescents with autism spectrum disorder. J Autism Dev Disord. (2015) 45:3805–19. 10.1007/s10803-014-2320-6 [DOI] [PubMed] [Google Scholar]
- 47.Wong C, Odom SL, Hume KA, Cox AW, Fettig A, Kucharczyk S, et al. Evidence-based practices for children, youth, and young adults with autism spectrum disorder: a comprehensive review. J Autism Dev Disord. (2015) 45:1951–66. 10.1007/s10803-014-2351-z [DOI] [PubMed] [Google Scholar]
- 48.Gordon I, Pierce MD, Bartlett MS, Tanaka JW. Training facial expression production in children on the autism spectrum. J Autism Dev Disord. (2014) 44:2486–98. 10.1007/s10803-014-2118-6 [DOI] [PubMed] [Google Scholar]
- 49.Hopkins IM, Gower MW, Perez TA, Smith DS, Amthor FR, Casey Wimsatt F, et al. Avatar assistant: improving social skills in students with an ASD through a computer-based intervention. J Autism Dev Disord. (2011) 41:1543–55. 10.1007/s10803-011-1179-z [DOI] [PubMed] [Google Scholar]
- 50.Purnama Y, Herman FA, Hartono J, Suryani D, Sanjaya G. Educational software as assistive technologies for children with autism spectrum disorder. Proc Comput Sci. (2021) 179:6–16. 10.1016/j.procs.2020.12.002 [DOI] [Google Scholar]
- 51.Rice LM, Wall CA, Fogel A, Shic F. Computer-assisted face processing instruction improves emotion recognition, mentalizing, and social skills in students with ASD. J Autism Dev Disord. (2015) 45:2176–86. 10.1007/s10803-015-2380-2 [DOI] [PubMed] [Google Scholar]
- 52.Silver M, Oakes P. Evaluation of a new computer intervention to teach people with autism or asperger syndrome to recognize and predict emotions in others. Autism. (2001) 5:299–316. 10.1177/1362361301005003007 [DOI] [PubMed] [Google Scholar]
- 53.Whalen C, Moss D, Ilan AB, Vaupel M, Fielding P, Macdonald K, et al. Efficacy of teachtown: basics computer-assisted intervention for the intensive comprehensive autism program in Los Angeles unified school district. Autism. (2010) 14:179–97. 10.1177/1362361310363282 [DOI] [PubMed] [Google Scholar]
- 54.Wong C, Odom SL, Hume KA, Cox AW, Fettig A, Kucharczyk S, et al. Evidence-Based Practices for Children, Youth, Young Adults With Autism Spectrum Disorder. Chapel Hill, NC: Frank Porter Graham Child Development Institute; (2014). Retrieved from https://autismpdc.fpg.unc.edu/how-do-i-find-out-more-about-ebps [Google Scholar]
- 55.Jobski K, Höfer J, Hoffmann F, Bachmann C. Use of psychotropic drugs in patients with autism spectrum disorders: a systematic review. Acta Psychiatr Scand. (2017) 135:8–28. 10.1111/acps.12644 [DOI] [PubMed] [Google Scholar]
- 56.Schubart JR, Camacho F, Leslie D. Psychotropic medication trends among children and adolescents with autism spectrum disorder in the medicaid program. Autism. (2014) 18:631–7. 10.1177/1362361313497537 [DOI] [PubMed] [Google Scholar]
- 57.World Health Organization . WHO Global Report on Traditional and Complementary Medicine 2019. Geneva: World Health Organization; (2019). [Google Scholar]
- 58.Höfer J, Hoffmann F, Bachmann C. Use of complementary and alternative medicine in children and adolescents with autism spectrum disorder: a systematic review. Autism. (2017) 21:387–402. 10.1177/1362361316646559 [DOI] [PubMed] [Google Scholar]
- 59.Levy SE, Hyman SL. Complementary and alternative medicine treatments for children with autism spectrum disorders. Child Adolesc Psychiatr Clin N Am. (2015) 24:117–43. 10.1016/j.chc.2014.09.004 [DOI] [PubMed] [Google Scholar]
- 60.Odom SL, Boyd BA, Hall LJ, Hume K. Evaluation of comprehensive treatment models for individuals with autism spectrum disorders. J Autism Dev Disord. (2010) 40:425–36. 10.1007/s10803-009-0825-1 [DOI] [PubMed] [Google Scholar]
- 61.National Professional Development Center on Autism Spectrum Disorder. Matrix of Evidence-Based Practices by Outcome and Age. Chapel Hill, NC: The University of North Carolina, Frank Porter Graham Child Development Institute (2017). Retrieved from https://autismpdc.fpg.unc.edu/implementation
- 62.National Professional Development Center on Autism Spectrum Disorder. Comparison of NPDC and NSP EBPs. Chapel Hill, NC: The University of North Carolina, Frank Porter Graham Child Development Institute (2017). Retrieved from https://autismpdc.fpg.unc.edu/evidence-based-practices
- 63.Abubakar A, Ssewanyana D, de Vries PJ, Newton CR. Autism spectrum disorders in sub-Saharan Africa. Lancet Psychiatry. (2016) 3:800–2. 10.1016/S2215-0366(16)30138-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.de Vries PJ. Thinking globally to meet local needs: autism spectrum disorders in Africa and other low-resource environments. Curr Opin Neurol. (2016) 29:130–6. 10.1097/WCO.0000000000000297 [DOI] [PubMed] [Google Scholar]
- 65.Newton CR, Chugani DC. The continuing role of ICNA in Africa: how to tackle autism? Dev Med Child Neurol. (2013) 55:488–9. 10.1111/dmcn.12150 [DOI] [PubMed] [Google Scholar]
- 66.Daley TC. The need for cross-cultural research on the pervasive developmental disorders. Transcult Psychiatry. (2002) 39:531–50. 10.1177/13634615020390040922495912 [DOI] [Google Scholar]
- 67.Dababnah S, Ghosh S, Campion K, Hussein D, Downton KD. Autism interventions in India: a systematic review. Rev J Autism Dev Disord. (2018) 5:260–7. 10.1007/s40489-018-0137-5 [DOI] [Google Scholar]
- 68.Davenport M, Mazurek M, Brown A, McCollom E. A systematic review of cultural considerations and adaptation of social skills interventions for individuals with autism spectrum disorder. Res Autism Spectr Disord. (2018) 52:23–33. 10.1016/j.rasd.2018.05.003 [DOI] [Google Scholar]
- 69.Liu Q, Hsieh WY, Chen G. A systematic review and meta-analysis of parent-mediated intervention for children and adolescents with autism spectrum disorder in mainland China, Hong Kong, and Taiwan. Autism. (2020) 24:1960–79. 10.1177/1362361320943380 [DOI] [PubMed] [Google Scholar]
- 70.Maulik PK, Darmstadt GL. Childhood disability in low-and middle-income countries: overview of screening, prevention, services, legislation, and epidemiology. Pediatrics. (2007) 120 (Supplement_1):S1–55. 10.1542/peds.2007-0043B [DOI] [PubMed] [Google Scholar]
- 71.Rahman A, Divan G, Hamdani SU, Vajaratkar V, Taylor C, Leadbitter K, et al. Effectiveness of the parent-mediated intervention for children with autism spectrum disorder in south Asia in India and Pakistan (PASS): a randomised controlled trial. Lancet Psychiatry. (2016) 3:128–36. 10.1016/S2215-0366(15)00388-0 [DOI] [PubMed] [Google Scholar]
- 72.Franz L, Chambers N, von Isenburg M, de Vries PJ. Autism spectrum disorder in sub-saharan africa: a comprehensive scoping review. Autism Res. (2017) 10:723–49. 10.1002/aur.1766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Olusanya BO, Davis AC, Wertlieb D, Boo NY, Nair MKC, Halpern R, et al. Developmental disabilities among children younger than 5 years in 195 countries and territories, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Glob. Health. (2018) 6:e1100–21. 10.1016/S2214-109X(18)30309-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. (2009) 151:264–9. 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- 75.National Autism Center . Findings and Conclusions: National Standards Project. Phase 2. New York, NY: National Autism Center; (2015). [Google Scholar]
- 76.Clearinghouse WW . What Works Clearinghouse Standards Handbook, Version 4.1. US Department of Education, Institute of Education Sciences. National Center for Education Evaluation Regional Assistance (2020). Available online at: https://ies.ed.gov/ncee/wwc/handbooks
- 77.Denizli-Gulboy H, Genc-Tosun D, Gulboy E. Evaluating augmented reality as evidence-based practice for individuals with autism spectrum disorder: a meta-analysis of single-case design studies. Int J Dev Disabil. (2021) 2021:1972741. 10.1080/20473869.2021.1972741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ameis SH, Kassee C, Corbett DP, Cole L, Dadhwal S, Lai MC, et al. Systematic review and guide to management of core and psychiatric symptoms in youth with autism. Acta Psychiatr Scand. (2018) 138:379–400. 10.1111/acps.12918 [DOI] [PubMed] [Google Scholar]
- 79.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1. 0. The Cochrane Collaboration (2011). Available online at: www.handbook.cochrane.org (accessed March 28, 2016).
- 80.Bond C, Symes W, Hebron J, Humphrey N, Morewood G, Woods K. Educational interventions for children with ASD: a systematic literature review 2008–2013. Sch Psychol Int. (2016) 37:303–20. 10.1177/0143034316639638 [DOI] [Google Scholar]
- 81.Reichow B, Volkmar FR, Cicchetti DV. Development of the evaluative method for evaluating and determining evidence-based practices in autism. J Autism Dev Disord. (2008) 38:1311–9. 10.1007/s10803-007-0517-7 [DOI] [PubMed] [Google Scholar]
- 82.Reichow B. Development, procedures, and application of the evaluative method for determining evidence-based practices in autism. In: Rashikj-Canevska O, editors. Evidence-Based Practices and Treatments for Children With Autism. Boston, MA: Springer; (2011). p. 25–39. 10.1007/978-1-4419-6975-0_2 [DOI] [Google Scholar]
- 83.Cheuk DKL, Wong V, Chen WX. Acupuncture for autistic spectrum disorder. Cochrane Database Syst Rev. (2011) 2011:CD007849. 10.1002/14651858.CD007849.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dawson-Squibb JJ, Davids EL, Harrison AJ, Molony MA, de Vries PJ. Parent education and training for autism spectrum disorders: scoping the evidence. Autism. (2020) 24:7–25. 10.1177/1362361319841739 [DOI] [PubMed] [Google Scholar]
- 85.Pluye P, Robert E, Cargo M, Bartlett G, O'cathain A, Griffiths F, et al. Proposal: A Mixed Methods Appraisal Tool for Systematic Mixed Studies Reviews. Montréal, QC: McGill University; (2011). [Google Scholar]
- 86.Dean M, Chang YC. A systematic review of school-based social skills interventions and observed social outcomes for students with autism spectrum disorder in inclusive settings. Autism. (2021) 25:1828–43. 10.1177/13623613211012886 [DOI] [PubMed] [Google Scholar]
- 87.Horner RH, Carr EG, Halle J, McGee G, Odom S, Wolery M. The use of single-subject research to identify evidence-based practice in special education. Except Child. (2005) 71:165–79. 10.1177/00144029050710020320421615 [DOI] [Google Scholar]
- 88.Kratochwill TR, Hitchcock JH, Horner RH, Levin JR, Odom SL, Rindskopf DM, et al. Single-case intervention research design standards. Remedial Spec Educ. (2013) 34:26–38. 10.1177/0741932512452794 [DOI] [Google Scholar]
- 89.Deb SS, Retzer A, Roy M, Acharya R, Limbu B, Roy A. The effectiveness of parent training for children with autism spectrum disorder: a systematic review and meta-analyses. BMC Psychiatry. (2020) 20:583. 10.1186/s12888-020-02973-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions Versions 6.0. (2019). Available online at: https://training.cochrane.org/handbook [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dijkstra-de Neijs L, Tisseur C, Kluwen LA, van Berckelaer-Onnes IA, Swaab H, Ester WA. Effectivity of play-based interventions in children with autism spectrum disorder and their parents: a systematic review. J Autism Dev Disord. (2021) 2:1–30. 10.1007/s10803-021-05357-2 [DOI] [PubMed] [Google Scholar]
- 92.Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions: The Cochrane Collaboration. Toronto, ON: Wiley; (2008). 10.1002/9780470712184 [DOI] [Google Scholar]
- 93.Ferguson J, Craig EA, Dounavi K. Telehealth as a model for providing behaviour analytic interventions to individuals with autism spectrum disorder: a systematic review. J Autism Dev Disord. (2019) 49:582–616. 10.1007/s10803-018-3724-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Geretsegger M, Elefant C, Mössler KA, Gold C. Music therapy for people with autism spectrum disorder. Cochrane Database Syst Rev. (2014) 6:CD004381. 10.1002/14651858.CD004381.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. (2008) 336:924–6. 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Harrop C. Evidence-based, parent-mediated interventions for young children with autism spectrum disorder: the case of restricted and repetitive behaviors. Autism. (2015) 19:662–72. 10.1177/1362361314545685 [DOI] [PubMed] [Google Scholar]
- 97.Koly KN, Martin-Herz SP, Islam MS, Sharmin N, Blencowe H, Naheed A. Parent mediated intervention programmes for children and adolescents with neurodevelopmental disorders in South Asia: a systematic review. PLoS ONE. (2021) 16:e0247432. 10.1371/journal.pone.0247432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kmet LM, Cook LS, Lee RC. Standard Quality Assessment Criteria for Evaluating Primary Research Papers From a Variety of Fields. Edmonton, AB: AHFMR; (2004). [Google Scholar]
- 99.Lee K, Lambert H, Wittich W, Kehayia E, Park M. The use of movement-based interventions with children diagnosed with autism for psychosocial outcomes—a scoping review. Res Autism Spectr Disord. (2016) 24:52–67. 10.1016/j.rasd.2015.12.011 [DOI] [Google Scholar]
- 100.Pluye P, Gagnon MP, Griffiths F, Johnson-Lafleur J. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in mixed studies reviews. Int J Nurs Stud. (2009) 46:529–46. 10.1016/j.ijnurstu.2009.01.009 [DOI] [PubMed] [Google Scholar]
- 101.Lee JD, Meadan H. Parent-mediated interventions for children with ASD in low-resource settings: a scoping review. Rev J Autism Dev Disord. 8:285–98. 10.1007/s40489-020-00218-735845443 [DOI] [Google Scholar]
- 102.GRADE Working Group . GRADE Handbook for Grading Quality of Evidence Strength of Recommendations. GRADE Working Group (2013). Available online at: https://gdt.gradepro.org/app/handbook/handbook.html#h.hnedbo8gqjqk
- 103.Logan K, Iacono T, Trembath D. A systematic review of research into aided AAC to increase social-communication functions in children with autism spectrum disorder. Augment Altern Commun. (2017) 33:51–64. 10.1080/07434618.2016.1267795 [DOI] [PubMed] [Google Scholar]
- 104.Millar DC, Light JC, Schlosser RW. The impact of augmentative and alternative communication intervention on the speech production of individuals with developmental disabilities: a research review. J Speech Lang Hear Res. (2006) 49:248–64. 10.1044/1092-4388(2006/021) [DOI] [PubMed] [Google Scholar]
- 105.Odom SL, Brown WH, Frey T, Karasu N, Smith-Canter LL, Strain PS. Evidence-based practices for young children with autism contributions for single-subject design research. Focus Autism Other Dev Disabl. (2003) 18:166–75. 10.1177/10883576030180030401 [DOI] [Google Scholar]
- 106.Mazon C, Fage C, Sauzéon Sauzéon H . Effectiveness and usability of technology-based interventions for children and adolescents with ASD: a systematic review of reliability, consistency, generalization and durability related to the effects of intervention. Comput Hum Behav. (2019) 93:235–51. 10.1016/j.chb.2018.12.001 [DOI] [Google Scholar]
- 107.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. (1996) 17:1–12. 10.1016/0197-2456(95)00134-4 [DOI] [PubMed] [Google Scholar]
- 108.McPheeters ML, Warren Z, Sathe N, Bruzek JL, Krishnaswami S, Jerome RN, et al. A systematic review of medical treatments for children with autism spectrum disorders. Pediatrics. (2011) 127:e1312–21. 10.1542/peds.2011-0427 [DOI] [PubMed] [Google Scholar]
- 109.Owens DK, Lohr KN, Atkins D, Treadwell JR, Reston JT, Bass EB, et al. AHRQ series paper 5: grading the strength of a body of evidence when comparing medical interventions—agency for healthcare research and quality and the effective health-care program. J Clin Epidemiol. (2010) 63:513–23. 10.1016/j.jclinepi.2009.03.009 [DOI] [PubMed] [Google Scholar]
- 110.Mercer J. Examining DIR/Floortime™ as a treatment for children with autism spectrum disorders: a review of research and theory. Res Soc Work Pract. (2017) 27:625–35. 10.1177/1049731515583062 [DOI] [Google Scholar]
- 111.Naveed S, Waqas A, Amray AN, Memon RI, Javed N, Tahir MA, et al. Implementation and effectiveness of non-specialist mediated interventions for children with autism spectrum disorder: a systematic review and meta-analysis. PLoS ONE. (2019) 14:e0224362. 10.1371/journal.pone.0224362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. (2011) 64:383–94. 10.1016/j.jclinepi.2010.04.026 [DOI] [PubMed] [Google Scholar]
- 113.Ona HN, Larsen K, Nordheim LV, Brurberg KG. Effects of pivotal response treatment (PRT) for children with autism spectrum disorders (ASD): a systematic review. Rev J Autism Dev Disord. (2020) 7:78–90. 10.1007/s40489-019-00180-z33821200 [DOI] [Google Scholar]
- 114.Higgins JP, Altman DG. Assessing risk of bias in included studies. In: Pullen PC, editor. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series. Boston, MA: Taylor and Francis Online; (2008). [Google Scholar]
- 115.Schünemann HJ, Oxman AD, Vist GE, Higgins JP, Deeks JJ, Glasziou P, et al. Interpreting results and drawing conclusions. In: Ayres KM, Lowrey KA, editors. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series. Albuquerque, NM: Sage; (2008). p. 359–87. 10.1002/9780470712184.ch12 [DOI] [Google Scholar]
- 116.GRADEpro . GRADEpro (Version 29.04.15). Hamilton, ON: McMaster University; (2014). [Google Scholar]
- 117.Oono IP, Honey EJ, McConachie H. Parent-mediated early intervention for young children with autism spectrum disorders (ASD). Evid Based Child Health Cochrane Database Syst Rev. (2013) 8:2380–479. 10.1002/ebch.1952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Brozek J, Oxman A, Schünemann H. GRADEpro. 3.2 for Windows. Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group (2008). [Google Scholar]
- 119.Patra S, Kar SK. Autism spectrum disorder in India: a scoping review. Int Rev Psychiatry. (2020) 33:1761136. 10.1080/09540261.2020.1761136 [DOI] [PubMed] [Google Scholar]
- 120.Pi HJ, Kallapiran K, Munivenkatappa S, Kandasamy P, Kirubakaran R, Russell P, et al. Meta-Analysis of RCTs of technology-assisted parent-mediated interventions for children with ASD. J Autism Dev Disord. (2021) 1–19. 10.1007/s10803-021-05206-2 [DOI] [PubMed] [Google Scholar]
- 121.Piwowarczyk A, Horvath A, Łukasik J, Pisula E, Szajewska H. Gluten-and casein-free diet and autism spectrum disorders in children: a systematic review. Eur J Nutr. (2017) 57:433–40. 10.1007/s00394-017-1483-2 [DOI] [PubMed] [Google Scholar]
- 122.Schünemann H, Brozek J, Guyatt G, Oxman A. GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. (2016). Available online at: www.gradepro.org/
- 123.Sathe N, Andrews JC, McPheeters ML, Warren ZE. Nutritional and dietary interventions for autism spectrum disorder: a systematic review. Pediatrics. (2017) 139:e20170346. 10.1542/peds.2017-0346 [DOI] [PubMed] [Google Scholar]
- 124.Weitlauf AS, Sathe N, McPheeters ML, Warren ZE. Interventions targeting sensory challenges in autism spectrum disorder: a systematic review. Pediatrics. (2017) 139:e20170347. 10.1542/peds.2017-0347 [DOI] [PubMed] [Google Scholar]
- 125.Siegel M, Beaulieu AA. Psychotropic medications in children with autism spectrum disorders: a systematic review and synthesis for evidence-based practice. J Autism Dev Disord. (2012) 42:1592–605. 10.1007/s10803-011-1399-2 [DOI] [PubMed] [Google Scholar]
- 126.Smith T, Iadarola S. Evidence base update for autism spectrum disorder. J Clin Child Adolesc Psychol. (2015) 44:897–922. 10.1080/15374416.2015.1077448 [DOI] [PubMed] [Google Scholar]
- 127.Silverman WK, Hinshaw SP. The second special issue on evidence-based psychosocial treatments for children and adolescents: a 10-year update. J Clin Child Adolesc. (2008) 37:1–7. 10.1080/15374410701817725 [DOI] [Google Scholar]
- 128.Spector JE. Sight word instruction for students with autism: an evaluation of the evidence base. J Autism Dev Disord. (2011) 41:1411–22. 10.1007/s10803-010-1165-x [DOI] [PubMed] [Google Scholar]
- 129.Sullivan OA, Wang C. Autism spectrum disorder interventions in mainland China: a systematic review. Rev J Autism Dev Disord. (2020) 7:263–77. 10.1007/s40489-019-00191-w [DOI] [Google Scholar]
- 130.Syriopoulou-Delli CK, Gkiolnta E. Review of assistive technology in the training of children with autism spectrum disorders. Int J Dev Disabil. (2020) 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Tan Q, Orsso CE, Deehan EC, Kung JY, Tun HM, Wine E, et al. Probiotics, prebiotics, synbiotics, and fecal microbiota transplantation in the treatment of behavioral symptoms of autism spectrum disorder: a systematic review. Autism Res. (2021) 14:1820–36. 10.1002/aur.2560 [DOI] [PubMed] [Google Scholar]
- 132.Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 133.Tseng A, Biagianti B, Francis SM, Conelea CA, Jacob S. Social cognitive interventions for adolescents with autism spectrum disorders: a systematic review. J Affect Disord. (2020) 274:199–204. 10.1016/j.jad.2020.05.134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Vetter JA. Parent-child interaction therapy for autism spectrum and attention-deficit/hyperactivity disorders: a review of the literature. Child Fam Behav Ther. (2018) 40:204–32. 10.1080/07317107.2018.1487740 [DOI] [Google Scholar]
- 135.Weitlauf AS, McPheeters ML, Peters B, Sathe N, Travis R, Aiello R, et al. Vanderbilt Evidence-Based Practice Center. Therapies for Children With Autism Spectrum Disorder: Behavioral Interventions Update. Comparative Effectiveness Review No. 137. Rockville, MD: Agency for Healthcare Research and Quality. AHRQ Publication No. 14-EHC036-EF (2014). [PubMed] [Google Scholar]
- 136.Gupta B. Theory of mind in autism: a case study. Psychol Stud. (2015) 60:339–45. 10.1007/s12646-015-0316-8 [DOI] [Google Scholar]
- 137.Karanth P, Shaista S, Srikanth N. Efficacy of communication DEALL-an indigenous early intervention program for children with autism spectrum disorders. Indian J Pediatr. (2010) 77:957–62. 10.1007/s12098-010-0144-8 [DOI] [PubMed] [Google Scholar]
- 138.Banerjee M, Ray SG. Development of play therapy module for children with autism. J Indian Acad Appl Psychol. (2013) 39:245–53.24695121 [Google Scholar]
- 139.Lal R. Effect of alternative and augmentative communication on language and social behavior of children with autism. Educ Res Rev. (2010) 5:119–25.30198333 [Google Scholar]
- 140.Lal R, Chhabria R. Early intervention of autism: a case for floor time approach. In: Guitton M, editors. Recent Advances in Autism Spectrum Disorders. France: IntechOpen; (2013). 10.5772/54378 [DOI] [Google Scholar]
- 141.Malhotra S, Rajender G, Bhatia MS, Singh TB. Effects of picture exchange communication system on communication and behavioral anomalies in autism. Indian J Psychol Med. (2010) 32:141–3. 10.4103/0253-7176.78513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Rai S, Haque Nizamie S, Nizamie A. Social story in improving problem behavior in moderate autism – a case study. J Indian Assoc Child Adolesc Ment Health. (2015) 11:246–55. [Google Scholar]
- 143.Bello-Mojeed M, Ani C, Lagunju I, Omigbodun O. Feasibility of parent-mediated behavioral intervention for behavioral problems in children with autism spectrum disorder in Nigeria: a pilot study. Child Adolesc Psychiatry Ment Health. (2016) 10:1–8. 10.1186/s13034-016-0117-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Divan G, Vajaratkar V, Cardozo P, Huzurbazar S, Verma M, Howarth E, et al. The feasibility and effectiveness of PASS plus, lay health worker delivered comprehensive intervention for autism spectrum disorders: pilot RCT in a rural low and middle income country setting. Autism Res. (2019) 12:328–39. 10.1002/aur.1978 [DOI] [PubMed] [Google Scholar]
- 145.Juneja M, Mukherjee SB, Sharma S, Jain R, Das B, Sabu P. Evaluation of a parent-based behavioral intervention program for children with autism in a low-resource setting. J Pediatr Neurosci. (2012) 7:16–8. 10.4103/1817-1745.97612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Krishnan R, Nesh MTJA, Russell PSS, Russell S, Mammen P. The effectiveness of an intensive, parent mediated, multi-component, early intervention for children with autism. J Indian Assoc Child Adolesc Ment Health. (2016) 12:230–52. [Google Scholar]
- 147.Louis PT, Kumar N. Does father involvement influence the affect, language acquisition, social engagement and behavior in young autistic children? An early intervention study. J Spec Educ Rehabil. (2015) 16:e7. 10.1515/jser-2015-0007 [DOI] [Google Scholar]
- 148.Manohar H, Kandasamy P, Chandrasekaran V, Rajkumar RP. Brief parent-mediated intervention for children with autism spectrum disorder: a feasibility study from South India. J Autism Dev Disord. (2019) 49:3146–58. 10.1007/s10803-019-04032-x [DOI] [PubMed] [Google Scholar]
- 149.Nair MK, Russell PS, George B, Prasanna GL, Bhaskaran D, Leena ML, et al. CDC Kerala 9: effectiveness of low intensity home based early intervention for autism spectrum disorder in India. Indian J Pediatr. (2014) 81:S115–9. 10.1007/s12098-014-1474-8 [DOI] [PubMed] [Google Scholar]
- 150.Barkaia A, Stokes TF, Mikiashvili T. Intercontinental telehealth coaching of therapists to improve verbalizations by children with autism. J Appl Behav Anal. (2017) 50:582–9. 10.1002/jaba.391 [DOI] [PubMed] [Google Scholar]
- 151.Lahiri U, Bekele E, Dohrmann E, Warren Z, Sarkar N. A physiologically informed virtual reality based social communication system for individuals with autism. J Autism Dev Disord. (2015) 45:919–31. 10.1007/s10803-014-2240-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Lal R, Bali M. Effect of visual strategies on development of communication skills in children with autism. Asia Pac Disabil Rehabil J. (2007) 18:120–30. [Google Scholar]
- 153.Padmanabha H, Singhi P, Sahu JK, Malhi P. Home-based sensory interventions in children with autism spectrum disorder: a randomized controlled trial. Indian J Pediatr. (2019) 86:18–25. 10.1007/s12098-018-2747-4 [DOI] [PubMed] [Google Scholar]
- 154.Paul A, Sharda M, Menon S, Arora I, Kansal N, Arora K, et al. The effect of sung speech on socio-communicative responsiveness in children with autism spectrum disorders. Front Hum Neurosci. (2015) 9:555. 10.3389/fnhum.2015.00555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Nagaraj R, Singhi P, Malhi P. Risperidone in children with autism: randomized, placebo-controlled, double-blind study. J Child Neurol. (2006) 21:450–5. 10.1177/08830738060210060801 [DOI] [PubMed] [Google Scholar]
- 156.Desousa A. An open-label trial of risperidone and fluoxetine in children with autistic disorder. Indian J Psychol Med. (2010) 32:17–21. 10.4103/0253-7176.70522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Allam H, Eldine NG, Helmy G. Scalp acupuncture effect on language development in children with autism: a pilot study. J Altern Complement Med. (2008) 14:109–14. 10.1089/acm.2007.0508 [DOI] [PubMed] [Google Scholar]
- 158.Fahmy SF, El-Hamamsy MH, Zaki OK, Badary OA. L-Carnitine supplementation improves the behavioral symptoms in autistic children. Res Autism Spectr Disord. (2013) 7:159–66. 10.1016/j.rasd.2012.07.006 [DOI] [Google Scholar]
- 159.Narasingharao K, Pradhan B, Navaneetham J. Efficacy of structured yoga intervention for sleep, gastrointestinal and behavior problems of ASD children: an exploratory study. J Clin Diagn Res. (2017) 11:VC01–6. 10.7860/JCDR/2017/25894.9502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Pusponegoro HD, Ismael S, Firmansyah A, Sastroasmoro S, Vandenplas Y. Gluten and casein supplementation does not increase symptoms in children with autism spectrum disorder. Acta Paediatr. (2015) 104:e500–5. 10.1111/apa.13108 [DOI] [PubMed] [Google Scholar]
- 161.Radhakrishna S. Application of integrated yoga therapy to increase imitation skills in children with autism spectrum disorder. Int J Yoga. (2010) 3:26–30. 10.4103/0973-6131.66775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Saad K, Eltayeb AA, Mohamad IL, Al-Atram AA, Elserogy Y, Bjørklund G, et al. A randomized, placebo-controlled trial of digestive enzymes in children with autism spectrum disorders. Clin Psychopharmacol Neurosci. (2015) 13:188–93. 10.9758/cpn.2015.13.2.188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Shaaban SY, El Gendy YG, Mehanna NS, El-Senousy WM, El-Feki HSA, Saad K, et al. The role of probiotics in children with autism spectrum disorder: a prospective, open-label study. Nutr Neurosci. (2018) 21:676–81. 10.1080/1028415X.2017.1347746 [DOI] [PubMed] [Google Scholar]
- 164.Higgins JPT . Cochrane Handbook for Systematic Reviews of Interventions Version 5.0. 1. The Cochrane Collaboration (2008). Available online at: https://training.cochrane.org/handbook
- 165.National Research Council . Educating Children With Autism. Washington, DC: National Academies Press; (2001). [Google Scholar]
- 166.Tachibana Y, Miyazaki C, Ota E, Mori R, Hwang Y, Kobayashi E, et al. A systematic review and meta-analysis of comprehensive interventions for pre-school children with autism spectrum disorder (ASD). PLoS ONE. (2017) 12:e0186502. 10.1371/journal.pone.0186502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Zwaigenbaum L, Bauman ML, Choueiri R, Kasari C, Carter A, Granpeesheh D, et al. Early intervention for children with autism spectrum disorder under 3 years of age: recommendations for practice and research. Pediatrics. (2015) 136:S60–81. 10.1542/peds.2014-3667E [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Warren Z, McPheeters ML, Sathe N, Foss-Feig JH, Glasser A, Veenstra-VanderWeele J. A systematic review of early intensive intervention for autism spectrum disorders. Pediatrics. (2011) 127, e1303–11. 10.1542/peds.2011-0426 [DOI] [PubMed] [Google Scholar]
- 169.Munsell EG, Coster WJ. Scoping review of interventions supporting self-management of life tasks for youth with high functioning ASD. Exceptionality. (2018) 29:81–94. 10.1080/09362835.2018.1480949 [DOI] [Google Scholar]
- 170.Qi CH, Barton EE, Collier M, Lin YL, Montoya C. A systematic review of effects of social stories interventions for individuals with autism spectrum disorder. Focus Autism Other Dev Disabl. (2018) 33:25–34. 10.1177/1088357615613516 [DOI] [Google Scholar]
- 171.Parsons L, Cordier R, Munro N, Joosten A, Speyer R. A systematic review of pragmatic language interventions for children with autism spectrum disorder. PLoS ONE. (2017) 12:e0172242. 10.1371/journal.pone.0172242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Stary AK, Everett GE, Sears KB, Fujiki M, Hupp SD. Social stories for children with autism spectrum disorders: updated review of the literature from 2004 to 2010. J Evid Based Pract Sch. (2013)13:123–41. [Google Scholar]
- 173.Steinbrenner JR, Hume K, Odom SL, Morin KL, Nowell SW, Tomaszewski B, et al. Evidence-Based Practices for Children, Youth, and Young Adults WITH AUTISM. Chapel Hill, NC: The University of North Carolina at Chapel Hill, Frank Porter Graham Child Development Institute, National Clearinghouse on Autism Evidence and Practice Review Team; (2020). [Google Scholar]
- 174.Knight VF, Sartini E. A comprehensive literature review of comprehension strategies in core content areas for students with autism spectrum disorder. J Autism Dev Disord. (2015) 45:1213–29. 10.1007/s10803-014-2280-x [DOI] [PubMed] [Google Scholar]
- 175.Maw SS, Haga C. Effectiveness of cognitive, developmental, and behavioural interventions for autism spectrum disorder in preschool-aged children: a systematic review and meta-analysis. Heliyon. (2018) 4:e00763. 10.1016/j.heliyon.2018.e00763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Ratliff-Black M, Therrien W. Parent-mediated interventions for school-age children with ASD: a meta-analysis. Focus Autism Other Dev Disabil. (2021) 36:3–13. 10.1177/1088357620956904 [DOI] [Google Scholar]
- 177.Lorah ER, Holyfield C, Miller J, Griffen B, Lindbloom C. A systematic review of research comparing mobile technology speech-generating devices to other AAC modes with individuals with autism spectrum disorder. J Dev Phys Disabil. (2021) 34:187–210. 10.1007/s10882-021-09803-y [DOI] [Google Scholar]
- 178.Ching H, Pringsheim T. Aripiprazole for autism spectrum disorders (ASD). Cochrane Database Syst Rev. (2012) 5:CD009043. 10.1002/14651858.CD009043.pub2 [DOI] [PubMed] [Google Scholar]
- 179.Fung LK, Mahajan R, Nozzolillo A, Bernal P, Krasner A, Jo B, et al. Pharmacologic treatment of severe irritability and problem behaviors in autism: a systematic review and meta-analysis. Pediatrics. (2016) 137:124–35. 10.1542/peds.2015-2851K [DOI] [PubMed] [Google Scholar]
- 180.Hirsch LE, Pringsheim T. Aripiprazole for autism spectrum disorders (ASD). Cochrane Database Syst Rev. (2016) 6:CD009043. 10.1002/14651858.CD009043.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Kandasamy P, Manohar H. Early intervention of autism spectrum disorder: translating research into practice. Indian J Ment Health Neurosci. (2018) 1:1–7. 10.32746/ijmhns.2018.v1.i1.3 [DOI] [Google Scholar]
- 182.Mrachko AA, Kaczmarek LA. Examining paraprofessional interventions to increase social communication for young children with ASD. Topics Early Child Spec Educ. (2017) 37:4–15. 10.1177/0271121416662870 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.