Abstract
The eye is a sensory organ exposed to the environment and protected by a mucosal tissue barrier. While it shares a number of features with other mucosal tissues, the ocular mucosal system, composed of the conjunctiva, Meibomian glands, and lacrimal glands, is specialized to address the unique needs of (a) lubrication and (b) host defense of the ocular surface. Not surprisingly, most challenges, physical and immunological, to the homeostasis of the eye fall into those two categories. Dry eye, a dysfunction of the lacrimal glands and/or Meibomian glands, which can both cause, or arise from, sensory defects, including those caused by corneal herpes virus infection, serve as examples of these perturbations and will be discussed ahead. To preserve vision, dense neuronal and immune networks sense various stimuli and orchestrate responses, which must be tightly controlled to provide protection, while simultaneously minimizing collateral damage. All this happens against the backdrop of, and can be modified by, the microorganisms that colonize the ocular mucosa long term, or that are simply transient passengers introduced from the environment. This review will attempt to synthesize the existing knowledge and develop trends in the study of the unique mucosal and immune elements of the ocular surface.
The ocular mucosal immune system
The eye is a specialized organ with a sensory function to transmit impulses that later are transduced into vision in the brain. While specialized neurons are located at the back of the eye in the retina, the front of the eye, composed of cornea, conjunctiva, and its adnexae, including Meibomian glands, together with the lens and anterior chamber, is responsible for 2/3 of the refractive power of the eye1. Therefore, a transparent and smooth optical surface is critical for optimum vision.
The tear film, which covers the eye, is only a few microns thick, but it maintains a moist and smooth ocular surface. It is a complex fluid composed of three different layers: aqueous, mucous, and lipid, that are constantly being produced and replenished. The tear film prevents drying of the ocular surface and functions as a lubricant between the conjunctiva and the eyelids. Also, the tear film harbors many growth factors, antimicrobial peptides, secretory IgA and vitamins, that are critical for ocular surface health by promoting immune homeostasis and host defense (Fig. 1). The conjunctival goblet cells produce mucins to moisturize and protect the ocular surface, as well as immunomodulatory factors, such as TGF-β and retinoic acid, which have been implicated in dampening immune activation of conjunctival antigen-presenting cells (APCs)2,3. Muc5ac is considered the prototypic mucin on the ocular surface and goblet-cell secreted mucous is an important part of the tear film. Goblet cells will be discussed later since they are key cells maintaining an uninflamed ocular surface. Meibomian glands, which are holocrine glands located at the lid margin of the conjunctiva, produce the lipid portion of the tear film. When these glands are affected by physical or inflammatory stressors, gland dropout and keratinization might lead to Meibomian gland dysfunction and contribute to ocular surface disease. Finally, the lacrimal gland produces the aqueous part of the tear film. This tubuloacinar gland continuously secretes water and soluble factors into the tear film. The lacrimal gland also secretes tears secondary to a foreign body on the ocular surface (reflex tears) or emotions (emotional tears). Rodents also have an extra gland called Harderian gland that also participates in tear secretion4.
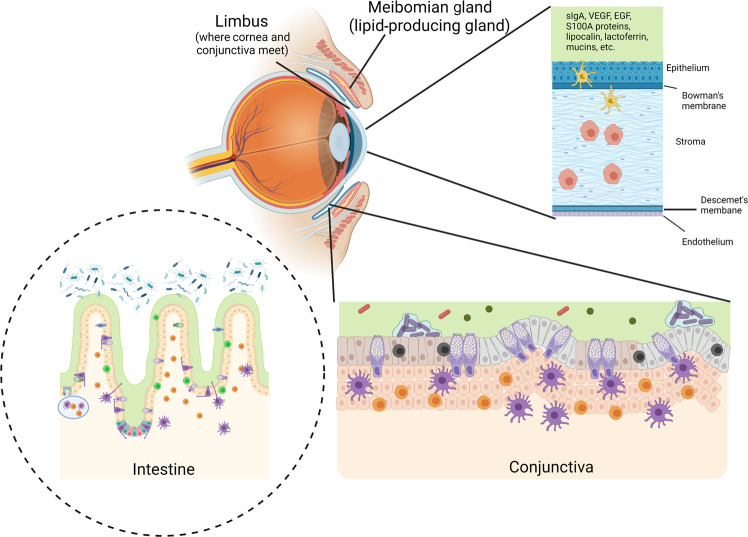
Fig. 1. Similarities and differences between intestinal and ocular surface mucosal immune tissues.
Similarities between the intestinal and ocular surface mucosal immune tissues include being continually bathed in mucus, harboring a diverse array of immune cells, the presence of goblet cells, and associations with bacteria. Differences include the presence of Peyer’s patches (light blue oval) in the intestines, which are not found in the conjunctiva. Also, the types, amount, and diversity of bacteria associated with the tissues is vastly different. Goblet cells (purple cells in the epithelial layer of the conjunctiva and intestines) are more concentrated in the conjunctiva as compared to the intestines. The meibomian glands associated with the eyelid supply the lipid fraction of the tears that coat the ocular surface. While both tissues are bathed in mucus, MUC5A is the tear associated mucin while MUC2 is associated with intestinal mucus. Tears contain a diverse array of factors that prevent microbes from adhering and infecting the ocular surface including: secretory IgA (sIgA), VEGF, EGF, S100A proteins, lipocalin, lactoferrin, and other miscellaneous factors.
After the tear film, the corneal epithelium is the first cellular line of defense against the environment and pathogens. The cornea is the avascular, transparent tissue whose homeostasis is dependent on trophic factors contained in fluids, such as the tear film produced by the lacrimal gland, and by the aqueous humor produced by the ciliary body. Anatomically, the most anterior portion of the cornea is a stratified epithelial cell layer with a strong barrier function, followed by the stroma composed of tightly packed collagen fibers, and finally, by organized single columnar endothelium. The function of this single columnar endothelium is to maintain corneal hydration and preserve corneal transparency.
The conjunctiva is spatially varied in structure. Close to the eyelid margin, the conjunctiva is composed of a non-keratinized stratified squamous epithelium, while close to the eye (bulbar conjunctiva) is a columnar epithelium. In mucosal tissues, lymphoid organization into follicles where APCs, T and B cells localize is thought to be important for local antigen presentation and induction of immune tolerance. (24) Peyer’s patches in the intestine are the most well-characterized mucosal-associated lymphoid tissue (MALT). In the conjunctiva, in addition to intraepithelial lymphocytes, loosely organized immune cells are present underneath the lamina propria. More structured organized tissues forming follicles have been described as conjunctival-associate lymphoid tissue (CALT) and lacrimal drainage associated lymphoid tissues (LDALT)5,6. No M cells were found in CALTs in a comparative analysis of 14 mammal species7. CALT and LDALT are thought to provide immune surveillance as immunoreactivity for IgA and secretoglobulins have been shown in lacrimal gland acinar cells and conjunctiva8,9. CALT and LDALT are frequent findings in histology investigations in cadavers, often of advanced age. Some authors have suggested that lymphoid aggregates with B and T cells accompanying aging are pathological findings. However, a consensus on whether they are LDALTs or pathological tertiary lymphoid structures has not been achieved10–18. In mice, CALTs are present in the nictating membrane and are easily missed in histological sections that include this tissue19. Intravital confocal microscopy techniques have identified CALTs in mice20 that can be induced by antigen instillation19,21. The number of CALTs has been shown to decrease in experimental DED but increase in allergic conjunctivitis models22.
The human and murine conjunctivae also harbor many immune cells, such as CD8+ T cells, innate lymphoid cells, natural killer (NK) cells, and γδ T cells23–36. In rodents, these intraepithelial lymphocytes are thought to participate in immune surveillance and development of conjunctival immune tolerance in homeostasis. This is borne out by functional consequences of eliminating these cells by subconjunctival injection of antibodies29,30. Additionally, antibody depletion of CD8 cells during desiccation worsens dry eye phenotypes by augmenting IL-17 production by ocular surface cells and CD4+T cells30. The role of γδ T cells in host defense of the ocular surface in relation to the commensal microbiome has been discussed. γδ T cells have also been implicated in preventing microbial keratitis, initiating corneal wound healing, and in maintaining corneal clarity27,28,37,38. Some of these functions are mediated by IL-17 production26,38,39. It is possible that functions performed by γδ T cells in mice, may be taken on by other immune cells in the conjunctiva of humans. The functional aspects of these interactions remain to be elucidated.
APCs are widely dispersed in the lamina propria and among the epithelial cell layer in the conjunctiva. These cells express CD103, CD8, CD11b and CD11c markers and have been easily identified in human and rodent tissues31,40–42. Ocular APCs have a diverse origin; macrophages, monocytes cells and plasmacytoid dendritic cells are widely present in normal conjunctiva and cornea and are important cells in dry eye, allergy, corneal transplantation and Herpes Simplex infection (which will be discussed later)31,41,43–47. While expression of MHC II is an important feature of APCs, the APCs in the central cornea are MHC II negative while the cells in the peripheral cornea are MHC II+40,43. Some of these APCs localize in close proximity to goblet cells and this will be discussed later in this review.
Innate lymphoid cell (ILCs) are an innate-like cell. ILCs can be subdivided into different subsets depending on the transcription factors and cytokines that they produce. In the gut, ILC3s have been implicated in goblet-cell hyperplasia after Listeria infection48. while ILC2 cells have also been implicated in homeostatic goblet cell through secretion of IL-1336. Recently, single-cell RNAseq of murine conjunctiva35 demonstrated the presence of ILC2 subsets that secrete IL-13, a critical cytokine for conjunctival goblet cells. Conjunctival ILCs have also been shown to produce IL-2249, a critical cytokine for epithelial barrier function in mucosal sites50.
The conjunctiva is second only to the gut in density of the goblet cells that it harbors51. Although the predominant mucin produced by conjunctival goblet cells differs from the mucin produced by intestinal goblet cells (Muc5ac vs. Muc2)52, conjunctival goblet cells also produce retinoic acid and TGF-β2,3,53, which together can modulate APCs that reside underneath goblet cells in the conjunctiva and can promote differentiation of T regulatory cells29,54,55. Goblet cells in the gut and the conjunctiva form goblet-cell associated passages, that are critical for the sampling of antigens and establishment of mucosal tolerance54–57.
Conjunctival goblet cells are exquisitely sensitive to the cytokine milieu; studies have shown that, similar to the lung, the Th-2 cytokine, IL-13, participates in homeostatic control of conjunctival goblet cells, whereas even minute quantities of IFN-γ can cause goblet cell metaplasia or cell death, and interrupt mucin secretion3,51,58–63. Treatment of bone marrow-derived cells with conjunctival goblet cell supernatant alters the differentiation of dendritic cells and myeloid cells, decreases secretion of IL-12, blunts the inflammatory response to LPS and decreases APC-dependent priming of OVA-specific Th1 cells. In fact, goblet cell-conditioned medium was as efficacious as exogenous retinoic acid, a classical immunomodulatory factor also elaborated by gut APCs2. Mice devoid of goblet cells due to genetic deletion of the goblet-cell associated transcription factor SPDEF, display intense conjunctival lymphocytic and myeloid infiltration and develop spontaneous dry eye disease55,64. SPDEF−/− mice have a higher frequency of IL-12-producing cells. In vivo administration of goblet cell-conditioned media decreases IL-12 mean fluorescence intensity in conjunctival CD11b+CD11c+ cells55. Critical cells in conjunctival mucosal tolerance are CD11c+APC+65 and conjunctival goblet cells54,55. For more details about conjunctival tolerance, see the review by Galletti and de Paiva57.
Together, the cornea, conjunctiva, lacrimal gland, meibomian gland, and its nerves are referred to as “lacrimal functional unit”66, as alterations in any of these components can affect the homeostasis and the correct functioning of the others. Examples of these are dry eye disease (DED) and infection by Herpes Simplex Virus (HSV), both of which will be discussed later in this review.
Unique and shared mucosal defenses
One unique defense of the ocular surface is the constant blinking and removal of any debris. This function is shared by eyelids and tear film. While peristaltic movements advance the intestinal contents along the relatively protected lumen of the gastrointestinal tract, the eye is exposed to the environment and subject to insults such as foreign bodies. A normal blink rate is around 15–20 times per minute, but this frequency can be increased if needed (for example, a foreign body in the eye). Interestingly, a decreased blink rate is found in humans who work at video displays or computers for a prolonged time. This has been associated with an increased prevalence of DED in relatively young subjects67–69.
Unlike the gut, which is literally packed with microorganisms, the conjunctival ocular surface microbiome is highly paucibacterial38,70–74, but the skin of the eyelids, adjacent to the eye, is rich in microbes75,76. There has been an augmented interest in microbes and their modulation of the physiology of mucosal surfaces, including the eye. The relationship between the microbiome and its effects on the eye will be discussed in the next section.
As a sensory organ, the eye is exposed to the environment and is subject to potentially harmful and inflammatory stimuli that can adversely affect vision. Because vision constitutes a strong evolutionary pressure, the eye has evolved mechanisms to limit inflammation in order to protect vision. An antigen injected into the anterior chamber in the eye is treated differently by the body than antigen injected into other organs or tissues, which illustrates a complex physiological phenomenon known as “ocular immune privilege”77. Immune privilege of the eye involves active as well as passive immune mechanisms that limit inflammation and minimize collateral damage to the eye. Multiple molecules and systems within the ocular fluids and on the surface of ocular cells maintain immune privilege, including, among others, TGF-β, retinoic acid, vasoactive intestinal peptide (VIP), substance P (SP), and the Fas-Fas Ligand pathway77–82. Fas Ligand interacts with Fas, and leads to cell death by activating the caspase pathway83. The Fas-Fas ligand signaling is well studied in the immune system, where it controls the proliferation of autoreactive T cells in the thymus (establishing central tolerance) or in the tissues (promoting peripheral tolerance)84,85. Fas ligand expression on T cells after T cell receptor engagement is upregulated by TNF-α and IL-286–90. However, signaling via Fas-Fas ligand is not restricted to immune cells. Constitutive expression of Fas ligand on corneal epithelium, corneal endothelium, iris, and retina are important for maintaining immune privilege in the eye82,91. Mice deficient in the Fas or FasL signaling pathway (MRLlpr or gld/gld, respectively) develop lupus and Sjögren syndrome (SS)-like disease, and accumulate T cells in lacrimal glands, eyes, and conjunctiva92–94.
However, unlike the inside of the eye, the ocular surface is not immune privileged and has to decide when to mount defenses or ignore (i.e., tolerate) insults. Mechanisms of tolerance on the ocular surface are of paramount importance, as uncontrolled ocular inflammation can lead to blindness. For example, corneal scarring and fibrosis after corneal insult can result in an opaque cornea that prevents light transmission, often requiring surgery to improve vision clarity. Inflammation inside the eye, also known as uveitis, can lead to retinal detachment, degeneration, and intra-vitreal hemorrhages. Studies have shown that up to 70% of patients with uveitis have permanent visual damage and meet legal criteria for blindness95. Mucosal tolerance mechanisms have been described in all mucosal tissues, including the gut, airways and the eye57. Conjunctival mucosal tolerance is similar to oral tolerance; an antigen administered topically into the eye prior to immunization will lead to an active immune response that generates CD4+Foxp3+ regulatory T cells or T cell anergy96–98.
The ocular mucosal immune system shares some defenses with other mucosal tissues, while also displaying unique properties (Fig. 1). Examples of similar defenses to other mucosal sites are the presence of an efficient epithelial barrier composed of tight junction proteins and desmosomes, that are present in the lateral membrane of the corneal cells, maintaining a tight contact between cells. In the gut, disruption of the epithelial barrier can lead to diarrhea, bacterial translocation, and eventually sepsis. In the cornea, disruption of the corneal epithelial barrier is a hallmark of DED, and it is used clinically as both a diagnostic criterion and severity endpoint in clinical trials. In allergic conjunctivitis and DED, the production of matrix metalloproteinases such as matrix-metalloproteinase (MMP)-9 and cytokines such as IL-33 have been implicated in corneal barrier disruption by disturbing tight junction protein networks99,100. Recently, barrier disruption in epithelial cells has been implicated in allergic, autoimmune, and inflammatory diseases101.
Thus, the ocular immune system has evolved mechanisms to maintain an optimal reflecting surface for vision while also minimizing inflammation and scarring.
Microbiome and disease
A host’s microbiome includes bacteria, fungi, and viruses; however, this section of the review will focus on the bacterial members of the microbiome, which are the most well-characterized. It has become evident that the microbiome can dictate the status between health and disease. While this concept has been primarily investigated within the context of the intestine, there is clear evidence at other tissues where dysbiosis of the microbiome is associated with disease and pathology.
To fully understand the nature of the microbiome across various mucosal sites, one must consider the environment where bacteria may live. For example, the lumen of the small intestine (S.I.) is largely devoid of oxygen102, so the microbial components there consist largely of anaerobic bacteria and facultative anaerobes103–105. Similarly to the intestinal environment, the oral cavity harbors a diverse microbiome in an environment with large amounts of mucus. At this site, the microbiome is made up of over 700 species of bacteria of which 99% come from the phyla, Firmicutes, Actinobacteria, Proteobacteria, Fusobacteria, Bacteroidetes, and Spirochaetes106–108. Conversely, other sites in the host offer different environments, which allow for varying consortia of bacteria to thrive. For example, the skin is much drier and has fewer nutrients than the intestine and is continually exposed to a drier environment and has a low abundance of nutrients compared to other mucosal surfaces. That being said, the composition of the skin microbiome is largely dependent on how oily or moist an area is109–111. While the intestine and skin have higher densities of bacteria, areas like the lungs also appear to harbor a resident microbiome, albeit in much lower quantities. The lungs are still exposed to the environment; however, the resources for bacteria are much less abundant due to a relative lack of nutrients. While many agree that commensal bacteria are present within the lungs, a consensus on what constitutes a healthy microbiome in that location still lacks resolution112–115.
The ocular mucosal environment brings together characteristics shared with each of the aforementioned areas. The eye is bathed in mucus like the intestines and oral cavity; however, nutrients are quite limited similar to the skin and lung habitats. Moreover, the eye microbiome is considered low biomass like the lungs, and it has been calculated that there is about 1 bacterium for every 20 ocular epithelial cells116. Notably, the eye is a relatively hostile environment for potential colonizing microbes due to the continual flow of tears that wash the ocular surface, and the elevated levels of salt, antimicrobial peptides, antibodies, and other antimicrobial factors like lysozyme. Further, the action of blinking helps to prevent bacteria and other pathogens from adhering to the corneal surface. These mechanisms are relatively effective at preventing colonization of the central cornea, which is normally devoid of bacteria, even under desiccating conditions that lead to dry eye117,118. However, the environment appears more hospitable to bacteria underneath the eyelids. Here, the impact of moving eyelids is felt much less and there is less disruption of colonization by physical force. Underneath the eyelid on conjunctival epithelia is where the first identifications of eye-colonizing microbes were found38,118.
Forming a consensus on defining the “core” ocular microbiome has been difficult, largely due to the paucibacterial nature of the eye116. Studies dating back to the 70 s using traditional culture techniques have shown that up to 50% of conjunctival swabs do not yield culturable bacteria75. However, the development of next generation sequencing has provided an opportunity to sample larger cohorts of patients and establish appropriate pipelines of analyses to eliminate contaminating genomic reads that could dramatically disrupt the true identities of ocular microbes. Corynebacterium, Propionibacterium, and coagulase-negative Staphylococci are all routinely sampled from the conjunctiva76,118–122. Intriguingly, torque teno virus is a human virus linked to cancers and other diseases that is found in a high frequency of sampled individuals116. This constituent of the virome may influence ocular health and disease; however, the development of models centered around torque teno virus remains elusive.
Ocular microbiome studies have compared the constituents of the ocular microbiome between healthy individuals and contact lens wearers, or patients with pathologies like keratitis, DED, conjunctivitis, and ocular surface allergy70,119,121,122. Information acquired from these studies shows that the composition of the microbiome changes with the health status of the eye; however, true mechanistic and causative studies have yet to be performed. Our recent study showed the immune effects of the local microbiome at the ocular surface. Specifically, the eye-colonizing Corynebacterium mastitidis (C. mast), induced the recruitment of IL-17-producing γδ T cells to the conjunctiva where they play a direct role in enhancing the ability of the ocular surface to resist infection by pathogens38. While C. mastitidis and other Corynebacterium spp. have been detected on the ocular surface of humans119,123–125, the role that these microbes play in local ocular surface immunity in humans has not been investigated.
The local microbiome is not the only consortium of microbes that affect the eye. The intestinal microbiome is also closely linked to ocular immunity. Germ-free mice, which are devoid of all microbes, do not generate a sufficient level of secretory IgA (sIgA) antibodies11,126, which bind and facilitate the washing away of potential pathogens and allergens. Similarly, a series of studies, which combined observations from humans and mouse models, investigated the critical role that intestinal microbes play in the development and severity of DED, illustrating the far-reaching effects of intestinal dysbiosis70,127,128. Intriguingly, a correlative study showed this may not only apply to DED, as intestinal dysbiosis was also linked to development and severity of keratitis129,130.
The intestinal microbiome not only affects the ocular surface, where it is difficult to exclude direct transfer of gut bacteria onto the eye as a result of poor hygiene, it also can modulate intraocular disease. Microbes within the intestine can activate autoreactive T cells that target the retina and trigger autoimmune uveitis in a genetically predisposed model105,131. In addition, microbes can provide antigen-independent stimuli through their immunoregulatory metabolites in an immunization-induced model132. In humans, dysregulated microbiome signatures correlate to disease in glaucoma and age-related macular degeneration133–137. While immunological mechanisms for intraocular diseases have been defined in animal models of uveitis, mechanisms of disease in models such as glaucoma and age-related macular degeneration are still much less well understood.
Understanding the influence that the microbiome has on ocular disease, opens up the potential for modulating the microbiome to limit pathogenesis. In models of Sjögren Syndrome (SS), fecal transplants were successful at reducing disease severity127,128. Similarly, antibiotic treatment that eliminates bacteria which may, directly or indirectly, activate autoreactive uveitogenic T cells, cells, ameliorated experimental uveitis131,132.
Bacteria that can colonize the eye could be genetically modified to produce and secrete factors that can modulate local host immunity to encourage ocular health. Because these bacteria would be continuously delivering the therapeutic substance to the eye, the need for frequent and laborious application of eye drops could become unnecessary. Of course, more details like biological “switches” within the bacteria would need to be defined so that there would be optimal control over drug delivery. Overall, these studies and hypotheses reveal a potential for using the microbiome to revolutionize the way eye diseases are treated.
Neuroimmune axis and the modulation of mucosal immunity
Despite its small size, the cornea is the most densely innervated tissue in the body138,139 (Fig. 2). Uniquely, it is primarily innervated by sensory nerves140. Evidence shows that sympathetic and parasympathetic nerves reach the ocular surface; however, these “non-sensing” nerves do not pass the limbus—where the mucosal conjunctival tissue meets the optically clear cornea—and do not enter the cornea during homeostasis141. In other, more well-studied, mucosal tissues like the intestines, the nature of the interplay between the host immunity and neurons is becoming more apparent. Moreover, this relationship contributes in a major way to the balance between tissue homeostasis and pathology.
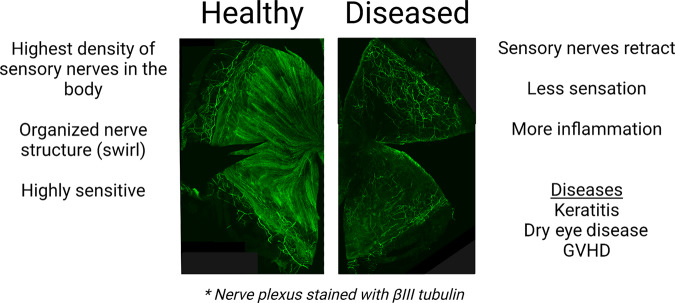
Fig. 2. Ocular surface diseases can lead to a loss of sensory nerves in the cornea.
In a normal corneal, thick sensory nerve trunk begin at the limbus (peripheral to the cornea) and innervate the cornea eventually thinning to become fine sensory nerve endings which terminate in the corneal epithelium. Fine sensory nerve endings become more concentrated and begin to swirl as they reach the central cornea (left). During ocular surface disease, sensory nerve endings can retract (right) and this results in a loss of blink reflex that can be temporary or permanent. Loss of blink reflex can leave the eye susceptible to infection, dry eye phenotypes and excessive inflammation. Nerves in the figure were stained with βIII tubulin.
As already mentioned, unlike the intestines, the cornea is an extremely sensitive tissue. The reason for that is that the eye is continually exposed to the external environment, and sensation is a means to prevent injury. During steady state, corneal nerves express the transient receptor potential (TRP) channels, TRPV1, TRPA1, TRPM1, and TRPM8, which can respond to heat (TRPV1), pain (TRPV1), cold (TRPA1/TRPM1/TRPM8), and chemical stimuli (TRPM1/TRPM8)142–146. Notably, TRPV4 is also expressed at the cornea; however, it is more closely associated with the apical domain of corneal epithelial cells, where TRPV4 is essential in forming tight junctions146,147. In addition to TRP channels, the ocular surface also expresses acid sensing ion channels (ASIC), which detect changes in pH due to noxious stimuli and/or damage associated with inflammation or trauma144,148. Generally, upon activation of these channels, the eye responds by blinking and/or tearing which allows the movement of tears across the eye. This response to stimuli is meant to dislodge and wash away potential pathogens, allergens, or irritants, which drain into the tear duct and are removed from the eye. The process of blinking is critical for the maintenance of mucosal homeostasis at the ocular surface, and it is documented that the loss of blink reflex results in ocular surface drying, increased susceptibility to infection, and potentially blinding pathology149. Corneal nerves do not only mediate the physical act of blinking, they also appear to contribute to the appropriate production of tears. Recently, lacrimal gland organoids from mice and humans were created from lacrimal gland biopsies and revealed that the release of the aqueous portion of the tears was mediated by neurotransmitters like norepinephrine, VIP and pilocarpine150. Similarly, in humans, the loss of corneal nerves correlates with atrophy of the meibomian gland, which, as mentioned above, supplies the lipid fraction of the tears151.
Neuropeptides contribute to maintaining ocular immune homeostasis and, when dysregulated, can exacerbate disease. For example, sensory nerves in the cornea express substance P (SP) and SP promotes vascularization and inflammation152,153. Calcitonin gene-related peptide (CGRP) is another factor that influences corneal homeostasis by increasing wound healing and promoting tissue healing phenotypes in macrophages (M2)154,155. Conversely, CGRP is also known to play a role in photophobia and may limit the ability of the cornea to resist infection156,157. Vasoactive intestinal peptide (VIP) is another neuropeptide produced at the ocular surface, and this factor has been shown to aid in limiting disease in diabetic keratopathy, bacterial keratitis, and allergic conjunctivitis158–161. Other neuropeptides like neuropeptide Y (NPY) are present at the ocular surface162; however, their roles in ocular surface disease and homeostasis are less clear.
A tissue with similar mechanisms at play is the lung, which is another mucosal tissue directly exposed to environmental stimuli. TRPV1 neurons have been extensively studied in this tissue and have been shown to greatly modulate the immune response. Activation of TRPV1 channels in lung neurons by noxious elements, allergens, or other factors can lead to lung irritation and coughing163. Specifically, activation of TRPV1 neurons during lung infection dampens immunity to Staph aureus, leading to morbidity in mice. Ablation of this neuronal subset increased survival164. Conversely, TRPV1 expression is increased in models of extended lung pathology165–167 leading to the conclusion that TRPV1 neurons can be both anti-inflammatory and pro-inflammatory, depending on the context. At the ocular surface, TRPV1 expression is upregulated after corneal injury168. Furthermore, activation of the nociceptive receptor, TRPV1, resulted in increased susceptibility to Pseudomonas aeruginosa infection157; however, TRPV1 signaling also appears to appear to prevent the adhesion of environmental bacteria169.
The skin also harbors neurons with nociceptors; however, skin is not exclusively innervated with sensory nerves like the eye. Instead, the skin is innervated by a pool of sensory, sympathetic, and parasympathetic nerves. In this tissue, TRPV1-expressing neurons have also been demonstrated to modulate immunity170. Specifically, stimulation of these neurons, through sensing of bacterial or fungal infections, leads to the development of “anticipatory” immunity, which enhances anti-microbial immunity at sites that are peripheral to the site of infection. This mechanism relies on successful transfer of neuronal signals from the periphery to the neuronal cell bodies, and back down other branches of the ganglia171. Another recently described mechanism of neuronal control of skin immunity focuses on sensory nonpeptidergic neurons, which express the Mas-related G-protein-coupled receptor D (MrgprD). These nerves suppress mast cell responses and limit excessive mast cell-centric immunity172. Under pathological conditions like dermatitis, the direct sensing of cytokines and pathogens can lead to itch and disease173,174. Notably, MrgprD and MrgprA3 nerves exist within the conjunctiva, suggesting that these nerves play an active role maintaining ocular homeostasis through sensing “itch” signals leading to blinking and tearing175. The roles that these and similar receptors play in ocular homeostasis and disease have yet to be fully investigated.
The enteric nervous system governs the control of smooth muscle throughout the intestinal tract. The enteric nervous system mostly consists of autonomic sympathetic and parasympathetic nerves. Due to the extensive number of immune cells within the intestinal tract and their close proximity to enteric nerves, there are ample opportunities for the neuroimmune axis to function to maintain tissue homeostasis and prevent infection and disease. The enteric nervous system secretes various neurotransmitters and neuropeptides that are known to modulate immunity such as acetylcholine (Ach), NE, VIP, and SP176. Through feedback mechanisms with immune cells, these transmitters and peptides can modulate cytokine production within innate and adaptive immune cells. Some of these factors have been studied in relation to the maintenance of corneal nerves and immune response; however, not all have been thoroughly investigated. Intestinal-resident immune cells also can regulate neuronal survival after infection. Specifically, muscularis macrophages can protect neurons from death through an arginase 1-polyamine axis that depends on β2-adrenergic receptor stimulation177. In addition to the enteric nervous system, enteric glial cells assist in regulating intestinal barrier permeability178. This could have implications for the eye, in that intestinal bacteria have been identified in the eye and have been posited to play a role in pathologies like age-related macular degeneration and other intraocular diseases135,179; however, these claims require more substantiated support before definitive conclusions can be made.
Corneal herpes infection and Herpes Stromal Keratitis
Common infectious agents of the eye are herpesviruses, which include varicella zoster virus (VZV) and HSV type 1 and 2. For the purposes of this part of the review, we will focus on HSV-1, which is the leading cause of blindness due to infectious disease in developed countries180,181. HSV-1 and other herpesviruses can initiate lasting pathology due to their ability to cause corneal scarring, which necessitates a corneal transplant or will lead to blindness. At the periphery, HSV-1 normally infects sub-clinically and replicates within corneal epithelial cells. This allows the virus to gain access to sensory neurons, which are supplied by the trigeminal ganglion. The virus can then enter a latent state within the trigeminal ganglion and will remain in the trigeminal ganglion for the life of the host. Under the influence of various stimuli, the virus can reactivate from latency and produce live, infectious virions, which are delivered to and induce immune responses at, distal sites (cornea)182–188. These immune responses, rather than viral replication, are the primary reasons for pathology and disease. While the blinding effects of corneal herpesvirus infections are clear, herpesviruses can infect and cause disease at an array of barrier and mucosal interfaces. Therefore, a thorough understanding of the immune responses directed against herpesviruses is critical for the development of better therapies to alleviate pathology in the eye as well as other sites of infection like the genital tract and skin.
The prevailing consensus is that the cornea lacks lymphatics and is largely devoid of immune cells, which reduces the chances of developing excessive inflammation that leads to immunopathology. Especially in mice, the tears are effective at washing away viruses and preventing infection, and most mouse models of ocular HSV-1 rely on scarifying the cornea to facilitate infection. Upon infection with HSV-1, corneal dendritic cells (DCs) and macrophages become activated and respond to the virus by producing type I interferons (IFNα and IFNβ) and inflammatory cytokines/chemokines, IL-6 and CXCL1/9/10189,190. Similarly, epithelial cells respond to HSV by producing inflammatory cytokines, which recruit other immune cells, like neutrophils and inflammatory monocytes to the cornea, which likely migrate from the conjunctiva191.
As the virus enters latency days after primary infection, migratory DCs begin priming the adaptive CD4+ and CD8+ T cell responses. Within days of primary infection, HSV-specific CD8+ T cells infiltrate the trigeminal ganglion and assist natural killer (NK) cells in pushing HSV-1 into a latent state by producing IFN-γ and lytic granules containing granzyme B192–195. This process results in a life-long battle between HSV-specific CD8+ T cells and HSV-harboring neurons. When CD8+ T cell functionality is compromised through immune suppression, HSV-1 can exit latency, travel back to the cornea and cause disease196–198.
Unlike CD8+ T cells, which largely traffic to the trigeminal ganglion from draining lymph nodes, CD4+ T cells expand after primary infection and traffic to the trigeminal ganglion and cornea. In the trigeminal ganglia, CD4+ T cells support CD8+ T cell functionality and may help limit viral spread199. However, CD4+ T cells that migrate to the cornea play the opposite role200,201. Specifically, in concert with inflammatory monocytes, cornea CD4+ T cells can produce vascular endothelial growth factor-A (VEGF-A). Additionally, the HSV-1 protein, infected cell polypeptide (ICP)4, can directly activate transcription of VEGF-A, suggesting that HSV-1 itself can induce the production and release of VEGF-A202. Since VEGF-A can stimulate vascularization of the cornea, this factor plays a direct role in the infiltration of neutrophils and inflammatory monocytes that disrupt the clear, organized collagen network within the cornea, leading to corneal scarring. Depletion of CD4+ T cells during this process can mitigate subsequent waves of leukocyte recruitment to the cornea, reducing pathology and disease203. In mice, pathology occurs after acute primary infection, and does not necessarily rely on viral reactivation from latency. In humans, however, this process is progressive, taking years to develop after numerous rounds of viral reactivation from latency.
Conventionally, the cause of corneal pathology was thought to be restricted to the immune response directed against reactivated virus that was deposited in the cornea. More recently, this line of thought has been challenged by observations that corneal hypoesthesia (loss of sensation) accompanied pathology, suggesting a role for the nervous system in disease. Indeed, after HSV-1 infection, sensory nerves retract; however, this is not unique to HSV-1 as DED, ocular manifestations of Graft versus Host Disease (GVHD), and corneal wounds, also result in the retraction of sensory nerves (Fig. 3)204–208.
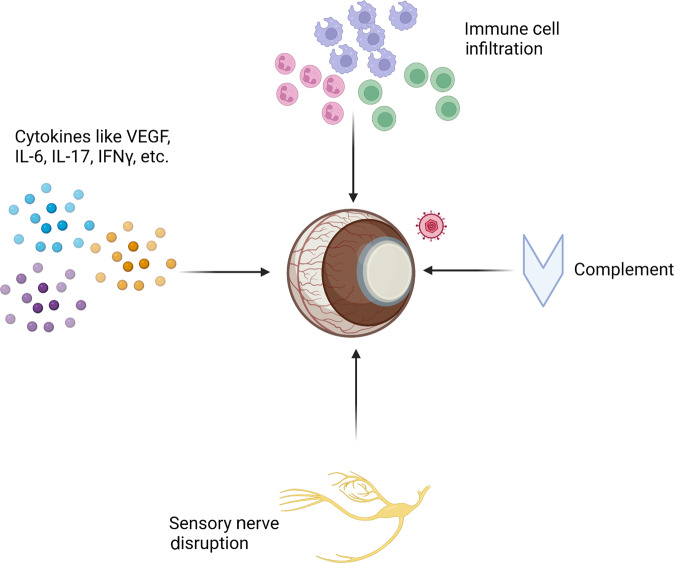
Fig. 3. Factors that contribute to Herpes Stromal Keratitis (HSK).
After a predominantly sub-clinical primary infection, HSV-1 gains access to sensory neurons and enters a latent state within trigeminal ganglion neurons indefinitely. Spontaneously or during times of immune suppression, HSV-1 can reactivate and virions can be deposited at the cornea resulting in an inflammatory response. Repeated reactivation events result in: (1) increased recruitment of inflammatory immune cells, (2) the production of inflammatory cytokines/chemokines, (3) disruption of sensory nerves, and (4) the initiation of complement, which preferentially targets sensory nerves. Because HSK is a multi-factoral disease, these processes all contribute to disease and ultimately result in tissue damage, fibrosis, and eventual blindness.
In other models of disease sensory nerves can grow back, albeit sometimes in reduced numbers. However, in HSV infection, sensory nerves are replaced by “non-sensing” sympathetic nerves that perpetuate the loss of sensation indefinitely140. Loss of sensation results in an inhibited blink reflex and desiccation stress, which acts to further enhance inflammation in a feed-forward manner causing more severe disease. The well-established procedure of tarsorrhaphy (sewing the eyelid shut) can prevent the desiccation and alleviate disease.
Nerve disruption is common during infectious diseases and has been observed in models of intestinal disease where disruption of nerves can result in reduced motility and symptoms associated with “irritable bowel syndrome”. At the ocular surface, the contribution of corneal nerve disruption during HSV pathogenesis is beginning to gain interest and understanding. CD4+ T cells recruited to the cornea produce complement factor C3, which contributes to sensory nerve retraction and loss, and inhibition of this factor using cobra snake venom alleviates disease. This mechanism is not only functional during HSV infection, but it likely extends to other ocular surface diseases, as ocular manifestations of GVHD is known to be mediated through this pathway as well207. Additionally, VEGF-A, produced by monocyte-derived cells and CD4+ T cells, and is better known to induce blood vessel formation, was shown to act directly on corneal nerves to disrupt sensory nerves and induce the ingrowth of sympathetic nerves203. Macrophages and monocyte-derived cells have the potential to cause pathology in the cornea due to their production of inflammatory cytokines and disruption of corneal nerves; however, macrophages can act to prevent neuronal loss in the intestine177, which highlights an interesting difference between these two mucosal tissues. The mechanisms that lead to the production of VEGF-A in each of these immune cell populations has yet to be elucidated; however, both monocyte-derived cells and CD4+ T cells closely localize to sympathetic nerves during pathogenicity, suggesting that a tripartite relationship exists to perpetuate inflammation.
Antimicrobial components of tears have an ability to target all potential pathogens. For example, beta defensins—produced by corneal epithelial cells209—can inactivate bacteria, fungi, and viruses210,211. Similarly, lactoferrin is known to sequester iron, which can impede growth of bacteria and fungi212. Additionally, lactoferrin can degrade RNA and acts as an antiviral. Most recently, it has been shown to limit SARS-CoV2 infection213. Lipocalin is another factor present in tears that possesses robust anti-microbial activity. Its endonuclease activity can act as an antiviral, and it can bind siderophores to prevent bacterial and fungal infection214,215. Antibodies can bind and neutralize HSV-1 to limit its ability to infect the eye and persist there. Antibody responses are generated after primary HSV infection, and these antibodies do confer protection against disease. In the skin, IgM that binds HSV innately, can protect the host from skin lesions and death216. In the eye, however, B cell deficiency leads to longer viral persistence after primary infection that can increase viral spread to areas like the brain217. After primary infection, induced antibodies play a larger role in neutralization of infectious virus. Others have shown that antibodies generated in response to an HSV-1 vaccine can reduce the need for functional adaptive T cells in preventing viral reactivation197. Also, in models of HSV-1 reactivation, neutralizing antibodies can lead to the under-reporting of viral reactivation from latency. Specifically, we have observed that only 30% of mice that are reactivating HSV-1 actively shed infectious virus, while the remaining 70% of mice have HSV-1 antigens deposited in the cornea that are detectable by fluorescence microscopy. Further, antibodies from HSV-infected dams can be passively transferred to pups through nursing218,219. Those antibodies have been shown to prevent HSV-1 infection and dissemination to the brain, which can lead to cognitive disorders.
Dry eye disease
A disease that often affects the ocular surface is DED, which affects millions of people worldwide and is the most common reason to seek eye care. DED is a chronic disease that, in extreme cases, can lead to blindness secondary to corneal melting/perforation. Patients complain of burning, itching, grittiness and ocular pain to various degrees of intensity, from mild discomfort to debilitating pain. However, it is well established that a disconnect between clinical symptoms and clinical signs happens in dry eye and some of these effects might be secondary to nerve alterations in severe cases. Female sex, increased age, presence of systemic autoimmunity, use of contact lenses are all risk factors that have been associated with dry eye. In addition, any disturbance in the lacrimal functional unit can lead to DED.
DED is a heterogeneous disease. For example, SS, an autoimmune disease that primarily affects the exocrine glands such as lacrimal and salivary glands, is the prototypic aqueous-tear-deficient DED. Patients with SS tend to have more severe forms of dry eye. Meibomian gland disease, which is also another form of DED, happens when the Meibomian glands are involved and have an unstable or a decreased lipid layer that leads to tear instability and increased evaporation. Alterations in eyelids and incomplete closing at night can also lead to dry eye. Another contributing factor is reduced blinking while staring at computer displays and smartphone devices for extended periods of time and use of systemic medications that have secondary drying effects.
Despite its low frequency, evidence has shown that commensal bacteria can have a protective role on the ocular surface38. Studies have indicated that topical antibiotics administered as eye drops into the conjunctival sac can modulate the ocular microbiome differently from systemic antibiotics220,221. The body of evidence identifying the protective role of the microbiome during dry eye comes from experiments in mice using either germ-free animals or evaluating their ocular surface after oral antibiotic-induced dysbiosis (see recent reviews222,223. Naive germ-free mice have low levels of IL-1β, lower levels of sIgA, extremely decreased number of conjunctival goblet cells, and increased frequency of APCs and IL-12-producing dendritic cells11,70,126,128,220,224. This is accompanied by corneal barrier disruption that is more prevalent in the C57BL/6 germ-free female mice, and can be reverted by fecal microbiota transplant from conventional, specific pathogen-free mice128. Administration of oral antibiotics worsens the dry eye phenotype in mice subjected to desiccation stress and also increases the production of inflammatory transcripts such as IL-1β, IL-12, TNF-α in corneas subjected to topical LPS challenge70,224. Further evidence of the protective effect of the microbiome was observed in the CD25−/− SS model, where germ-free CD25−/− mice had more accelerated eye and worse lacrimal inflammation than CD25−/− mice with a conventional microbiome. IL-12, MHC II and IFN-γ were identified as key players in the lacrimal gland in this model127. IL-12 antibody depletion in germ-free CD25−/− mice ameliorated the lacrimal gland inflammation, confirming the role of Th1 cells in this model127. Interestingly, and in contrast to most other autoimmune and inflammatory disease models, where depletion of microbiota protects from disease, germ free or MyD88−/− non-obese diabetic (NOD) mice develop worse Type I diabetes than their counterparts with a conventional microbiome225,226. Conversely, administration of antibiotics to NOD mice, which also develop salivary gland inflammation, ameliorates this inflammation227,228, indicating that context dictates the role that the microbiome plays in disease.
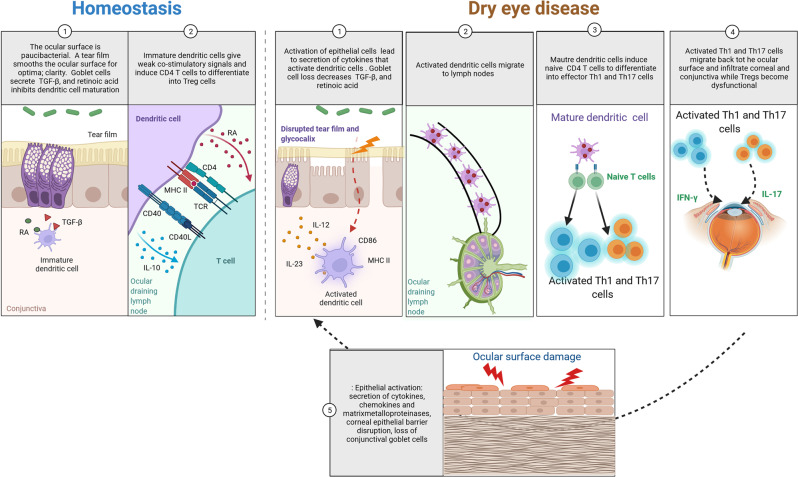
It is also well established that dry eye is accompanied by a vicious cycle of inflammation, activation of innate and adaptive immune responses and damage to the epithelium, which further causes inflammation (Fig. 4). The exact source of the initiating event(s) in dry eye have not been identified, although it is clear that there are multiple entry points (autoimmunity, aging, low humidity exposure, video display, use of contact lenses, dysbiosis) that can combine to constitute “multiple hits.” An insult on the ocular surface (desiccation, surgery) can lead to epithelial activation, which increased production of inflammatory cytokines and MMPs, activation of inflammasome and oxidative stress pathways, altering the local environment. Clinical signs are altered corneal barrier function and loss of conjunctival goblet cells. Activation of APCs, migration to eye-draining lymph nodes, priming of Th1 and Th17 cells that migrate to the ocular surface epithelium and secretion of IFN-γ and IL-17, causing further insult to the ocular surface, breaking the corneal barrier, and activating the epithelium, reinitiating the vicious circle and becoming self-perpetuating (Fig. 4) 229,230. Interruption of APC migration, achieved by subconjunctival administration of liposome-encapsulated clodronate (which depletes APCs), or lymphadenectomy of eye-draining nodes will decrease the generation of eye-pathogenic T cells231,232. The subject has recently been extensively reviewed—the interested reader is referred to reference233 for a comprehensive review of dry eye pathophysiology.
Fig. 4. The immune response in dry eye disease and the vicious cycle of inflammation.
Homeostasis: 1-In homeostasis, the ocular surface is paucibacterial and has innumerous anti-microbial defenses, including a healthy tear film rich in anti-microbial proteins (SA100s, lysozyme). In the conjunctiva, goblet cells secrete retinoic acid (RA) and TGF-beta that maintain the resident dendritic cells in an immature state. 2- Immature dendritic cells provide ocular surveillance and migrate constantly to the ocular draining nodes where regulatory T cells (Tregs) are preferentially primed. dry eye disease: 1-Insults to the ocular surface cause activation of epithelial cells, disrupted tear film and glycocalyx which in turn lead to secretion of chemokines, secretion of T helper (Th) polarizing cytokines such as IL-12 and IL-23 and upregulation of CD86 and MHC II, leading to activated dendritic cells. Loss of goblet cells and squamous metaplasia of the conjunctival epithelium lead to goblet cells that do not properly secrete at the ocular surface. Secondary to loss of goblet cells, there is less RA and TGF-β, leading to further APC activation. 2-Activated dendritic cells migrate to ocular lymph nodes. 3-Mature dendritic cells primer naïve T cells into Th1 and Th17 cells. 4-Activated Th1 and Th17 cells migrate back to the eye, where they secrete IFN-γ and IL-17, which cause goblet cell loss, corneal barrier disruption and activation of innate immunity. Dysfunctional Tregs also participate in the immune response of dry eye disease (not despicted). 5- Insults to the ocular surface reinitiate the vicious cycle of dry eye activating epithelial cells, disrupting the tear film and glycocalyx which in turn lead to secretion of chemokines, secretion of Th polarizing cytokines such as IL-12 and IL-23 and upregulation of CD86 and MHC II, leading to activated dendritic cells. Loss of goblet cells and squamous metaplasia of the conjunctival epithelium lead to goblet cells that do not properly secrete at the ocular surface. Secondary to loss of goblet cells, there is less RA and TGF-β, leading to further APC activation.
Unifying events in the vicious circle of dry eye are disturbances in the tear film (quantity, quality, mechanical spread), hyperosmolarity and epithelial activation. As such, a hyperosmolar tear initiates a cascade of pro-inflammatory cytokine secretion by the cornea and conjunctival epithelium230,234–236 and activation of inflammasome and oxidative pathways. Defects in autophagy, endoplasmic reticulum stress and the unfolded protein response have all been implicated in dry eye, and are supported by the increased expression of the chaperone GPR78 in animal models and in culture systems62,237. Increased expression of the chaperone GPR78 in epithelial cells is also noted in minor salivary gland biopsies in SS patients and in impression cytology conjunctival imprints62,238.
Epithelial cells that line either the conjunctiva and cornea, or acinar and epithelial ducts from SS and dry eye patients, are active players in dry eye. They suffer bystander damage by immune cells that become activated and secrete cytokines such as IFN-γ and IL-1758,62,239–244. Corneal and conjunctival epithelial cells express low levels of MHC II, but can upregulate it after stimulation with IFN-γ60,239,245. A similar phenomenon246 is seen in the lacrimal and salivary glands and also by intestinal epithelial cells247. It has been proposed that these epithelial cells can function as non-professional APCs245,247,248 although a consensus regarding their signaling pathways and the type of CD4+ T cells that are modulated by these MHC II+ cells, has not been reached247. SS and non-SS patients have increased levels of HLA-DR in their conjunctiva239,249–252 and this has been used as a biomarker in clinical trials249,253. Experimentally, constitutive expression of major inflammatory nuclear factor kappa-light-chain-enhancer of activated B cells (NFκB) pathway due to genetic deletion of its transcriptional regulator IκB-ζ, induces an SS-like disease with both ocular and glandular involvement254. Further evidence of epithelial cells being initiators of dry eye is provided by experimental dry eye models where epithelial disturbance through either desiccation or topical application of benzalkonium chloride elicits an innate response, which is followed by an adaptive immune response30,58,97,255. Other inflammatory pathways that have been implicated in dry eye are MAPK (JNK, ERK and p38)236,256,257. For example, studies have shown that JNK2−/− mice are resistant to dry eye-induced corneal changes258. Activation of innate pathways such as Toll-Like receptors, NOD, MyD88, and NLRP3 in corneal epithelial cells has also been implicated in dry eye259–263, further supporting the crucial role of epithelial activation in DED.
There is a complex relationship between APCs and conjunctival goblet cells264. Goblet cells and their products not only act to mechanically lubricate the eye, but also actively contribute to immune homeostasis at the ocular surface by secreting TGF-β and retinoic acid, as mentioned before29,30,58,62,231–233,240,243,265,266. Studies have shown that experimental dry eye changes the polarization of conjunctival macrophages from M2 to M1267,268. Desiccating stress was also associated with disappearance of immature monocytes in the conjunctiva and their replacement with MHC II+ macrophages, suggesting active recruitment of these cells to the conjunctiva268. This was also accompanied by elevated expression of genes involved in antigen presentation and inflammation like NLRP3268. Furthermore, at least five of the differentially expressed genes (Icam1, Batf, S100a9, Mx1, and Irf7) evaluated by a NanoString® panel from murine conjunctivae subjected to desiccating stress were also upregulated in the conjunctiva of SS patients269. Some of these genes have been implicated in the SS and dry eye before270–279. Of particular interest is BATF. Although not causally implicated in SS or dry eye, BATF is a transcription factor involved in differentiation of Th17 cells280 whose signature cytokine, IL-17, promotes corneal barrier disruption240,243.
It is therefore not surprising that the only four FDA-approved drugs to treat dry eye are immunomodulatory agents that interfere with the vicious cycle of dry eye by modulating T cell activation and by decreasing immune synapse (cyclosporine [in two different formulations], lifitegrast and loteprednol etabonate)281–284. While much has been learned about dry eye disease in the last 20 years, effective therapies that can be used by a large number of patients remain elusive.
Conclusions
In summary, the ocular surface is a complex mucosal system that is highly specialized to perform the functions of maintaining ocular physical and immunological integrity. The component cells, immune as well as structural, interact with each other and with the environment, including physical, chemical and microbial stimuli. Any defect in one of the cellular or secretory components in this complex interacting network can trigger, or can contribute to, ocular surface pathology. Research during the past decade, employing state-of-the-art approaches, has revealed much of these critical networks and interactions and has opened new therapeutic perspectives, but much remains to be learned. The microbial and neuroimmune aspects controlling ocular surface health and disease have been foci of intense interest and promise to yield novel clinical approaches to treatment of ocular surface disease.
Author contributions
R.R.C. conceptualized and edited the manuscript, C.S.d.P. and A.J.St.L. wrote the manuscript, all authors refined and approved the final manuscript.
Funding
This work was supported by NEI/NIH Intramural funding, Project EY000184 (R.R.C.), NIH EY026893 (C.S.d.P.), EY030447 (C.S.d.P.), EY025761 (A.J.St.L.), EY026891 (A.J.St.L.), EY032482 (A.J.St.L.); NIH/NEI EY002520 (Core Grant for Vision Research Department of Ophthalmology, Baylor College of Medicine), EY08098 (Core Grant for Vision Research Department of Ophthalmology University of Pittsburgh); NIH Pathology Core (P30CA125123), Research to Prevent Blindness (unrestricted grant to the Dept. Of Ophthalmology), The Hamill Foundation, The Sid Richardson Foundation, and the Eye and Ear Foundation of Pittsburgh.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Cintia S. de Paiva, Anthony J. St. Leger.
References
- 1.Sridhar MS. Anatomy of cornea and ocular surface. Indian J. Ophthalmol. 2018;66:190–194. doi: 10.4103/ijo.IJO_646_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xiao Y, et al. Goblet cell-produced retinoic acid suppresses CD86 expression and IL-12 production in bone marrow-derived cells. Int. Immunol. 2018;30:457–470. doi: 10.1093/intimm/dxy045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Contreras-Ruiz L, Ghosh-Mitra A, Shatos MA, Dartt DA, Masli S. Modulation of conjunctival goblet cell function by inflammatory cytokines. Mediators Inflamm. 2013;2013:636812. doi: 10.1155/2013/636812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Payne AP. The harderian gland: a tercentennial review. J. Anat. 1994;185:1–49. [PMC free article] [PubMed] [Google Scholar]
- 5.Knop E, Knop N. Lacrimal drainage-associated lymphoid tissue (LDALT): a part of the human mucosal immune system. Invest Ophthalmol. Vis. Sci. 2001;42:566–574. [PubMed] [Google Scholar]
- 6.Knop N, Knop E. Conjunctiva-associated lymphoid tissue in the human eye. Investig. Ophthalmol. Vis. Sci. 2000;41:1270–1279. [PubMed] [Google Scholar]
- 7.Chodosh J, Nordquist RE, Kennedy RC. Comparative anatomy of mammalian conjunctival lymphoid tissue: a putative mucosal immune site. Dev. Comp. Immunol. 1998;22:621–630. doi: 10.1016/S0145-305X(98)00022-6. [DOI] [PubMed] [Google Scholar]
- 8.Knop E, Knop N. The role of eye-associated lymphoid tissue in corneal immune protection. J. Anat. 2005;206:271–285. doi: 10.1111/j.1469-7580.2005.00394.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knop E, Knop N, Claus P. Local production of secretory IgA in the eye-associated lymphoid tissue (EALT) of the normal human ocular surface. Investig. Ophthalmol. Vis. Sci. 2008;49:2322–2329. doi: 10.1167/iovs.07-0691. [DOI] [PubMed] [Google Scholar]
- 10.Schuh JCL. Mucosa-Associated Lymphoid Tissue and Tertiary Lymphoid Structures of the Eye and Ear in Laboratory Animals. Toxicol. Pathol. 2021;49:472–482. doi: 10.1177/0192623320970448. [DOI] [PubMed] [Google Scholar]
- 11.Allansmith MR, et al. The immune response of the lacrimal gland to antigenic exposure. Curr. Eye Res. 1987;6:921–927. doi: 10.3109/02713688709034860. [DOI] [PubMed] [Google Scholar]
- 12.Gudmundsson OG, Benediktsson H, Olafsdottir K. T-lymphocyte subsets in the human lacrimal gland. Acta Ophthalmologica. 1988;66:19–23. doi: 10.1111/j.1755-3768.1988.tb08528.x. [DOI] [PubMed] [Google Scholar]
- 13.Gudmundsson OG, et al. T cell populations in the lacrimal gland during aging. Acta Ophthalmologica. 1988;66:490–497. doi: 10.1111/j.1755-3768.1988.tb04369.x. [DOI] [PubMed] [Google Scholar]
- 14.Nasu M, Matsubara O, Yamamoto H. Post-mortem prevalence of lymphocytic infiltration of the lacrymal gland: a comparative study in autoimmune and non-autoimmune diseases. J. Pathol. 1984;143:11–15. doi: 10.1002/path.1711430104. [DOI] [PubMed] [Google Scholar]
- 15.Damato BE, Allan D, Murray SB, Lee WR. Senile atrophy of the human lacrimal gland: the contribution of chronic inflammatory disease. Br. J. Ophthalmol. 1984;68:674–680. doi: 10.1136/bjo.68.9.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Obata H. Anatomy and histopathology of the human lacrimal gland. Cornea. 2006;25:S82–S89. doi: 10.1097/01.ico.0000247220.18295.d3. [DOI] [PubMed] [Google Scholar]
- 17.Obata H, Yamamoto S, Horiuchi H, Machinami R. Histopathologic study of human lacrimal gland. Stat. Anal. Spec. Ref. aging Ophthalmol. 1995;102:678–686. doi: 10.1016/s0161-6420(95)30971-2. [DOI] [PubMed] [Google Scholar]
- 18.Trujillo-Vargas, C. M. et al. Immune phenotype of the CD4 + T cells in the aged lymphoid organs and lacrimal glands. GeroScience, 10.1007/s11357-022-00529-z (2022). [DOI] [PMC free article] [PubMed]
- 19.Steven P, et al. Experimental induction and three-dimensional two-photon imaging of conjunctiva-associated lymphoid tissue. Investig. Ophthalmol. Vis. Sci. 2008;49:1512–1517. doi: 10.1167/iovs.07-0809. [DOI] [PubMed] [Google Scholar]
- 20.Siebelmann S, et al. Development, alteration and real time dynamics of conjunctiva-associated lymphoid tissue. PloS One. 2013;8:e82355–e82355. doi: 10.1371/journal.pone.0082355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Steven P, Gebert A. Conjunctiva-associated lymphoid tissue - current knowledge, animal models and experimental prospects. Ophthalmic Res. 2009;42:2–8. doi: 10.1159/000219678. [DOI] [PubMed] [Google Scholar]
- 22.Steven, P. et al. Disease-Specific Expression of Conjunctiva Associated Lymphoid Tissue (CALT) in Mouse Models of Dry Eye Disease and Ocular Allergy. Int. J. Mol. Sci.21, 10.3390/ijms21207514 (2020). [DOI] [PMC free article] [PubMed]
- 23.Hingorani M, Metz D, Lightman SL. Characterisation of the normal conjunctival leukocyte population. Exp. Eye Res. 1997;64:905–912. doi: 10.1006/exer.1996.0280. [DOI] [PubMed] [Google Scholar]
- 24.Hingorani M, Calder VL, Buckley RJ, Lightman SL. The role of conjunctival epithelial cells in chronic ocular allergic disease. Exp. Eye Res. 1998;67:491–500. doi: 10.1006/exer.1998.0528. [DOI] [PubMed] [Google Scholar]
- 25.Dua HS, Gomes JA, Donoso LA, Laibson PR. The ocular surface as part of the mucosal immune system: conjunctival mucosa-specific lymphocytes in ocular surface pathology. Eye. 1995;9:261–267. doi: 10.1038/eye.1995.51. [DOI] [PubMed] [Google Scholar]
- 26.Coursey TG, et al. Age-related spontaneous lacrimal keratoconjunctivitis is accompanied by dysfunctional T regulatory cells. Mucosal Immunol. 2017;10:743–756. doi: 10.1038/mi.2016.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Brien RL, et al. αβ TCR+ T cells, but not B cells, promote autoimmune keratitis in b10 mice lacking γδ T cells. Investig. Ophthalmol. Vis. Sci. 2012;53:301–308. doi: 10.1167/iovs.11-8855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O’Brien RL, et al. Protective role of gammadelta T cells in spontaneous ocular inflammation. Investig. Ophthalmol. Vis. Sci. 2009;50:3266–3274. doi: 10.1167/iovs.08-2982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang X, et al. NK cells promote Th-17 mediated corneal barrier disruption in dry eye. PLoS. One. 2012;7:e36822. doi: 10.1371/journal.pone.0036822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang X, et al. CD8( + ) cells regulate the T helper-17 response in an experimental murine model of Sjogren syndrome. Mucosal. Immunol. 2014;7:417–427. doi: 10.1038/mi.2013.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khandelwal P, et al. Ocular mucosal CD11b + and CD103 + mouse dendritic cells under normal conditions and in allergic immune responses. PloS One. 2013;8:e64193. doi: 10.1371/journal.pone.0064193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu Q, Smith CW, Zhang W, Burns AR, Li Z. NK cells modulate the inflammatory response to corneal epithelial abrasion and thereby support wound healing. Am. J. Pathol. 2012;181:452–462. doi: 10.1016/j.ajpath.2012.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bialasiewicz AA, Schaudig U, Ma JX, Vieth S, Richard G. Alpha/beta- and gamma/delta-T-cell-receptor-positive lymphocytes in healthy and inflamed human conjunctiva. Graefes Arch. Clin. Exp. Ophthalmol. 1996;234:467–471. doi: 10.1007/BF02539415. [DOI] [PubMed] [Google Scholar]
- 34.Arnous R, et al. Tissue resident memory T cells inhabit the deep human conjunctiva. Sci. Rep. 2022;12:6077. doi: 10.1038/s41598-022-09886-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alam, J. et al. Single-cell transcriptional profiling of murine conjunctival immune cells reveals distinct populations expressing homeostatic and regulatory genes. Mucosal Immunol.10.1038/s41385-022-00507-w (2022). [DOI] [PMC free article] [PubMed]
- 36.Waddell A, Vallance JE, Hummel A, Alenghat T, Rosen MJ. IL-33 Induces Murine Intestinal Goblet Cell Differentiation Indirectly via Innate Lymphoid Cell IL-13 Secretion. J. Immunol. 2019;202:598–607. doi: 10.4049/jimmunol.1800292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li Z, Burns AR, Rumbaut RE, Smith C. W. gamma delta T cells are necessary for platelet and neutrophil accumulation in limbal vessels and efficient epithelial repair after corneal abrasion. Am. J. Pathol. 2007;171:838–845. doi: 10.2353/ajpath.2007.070008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.St Leger AJ, et al. An Ocular Commensal Protects against Corneal Infection by Driving an Interleukin-17 Response from Mucosal gammadelta T Cells. Immunity. 2017;47:148–158.e145. doi: 10.1016/j.immuni.2017.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alam J, et al. IL-17 Producing Lymphocytes Cause Dry Eye and Corneal Disease With Aging in RXRα Mutant Mouse. Front Med. 2022;9:849990. doi: 10.3389/fmed.2022.849990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shen L, Barabino S, Taylor AW, Dana MR. Effect of the ocular microenvironment in regulating corneal dendritic cell maturation. Arch. Ophthalmol. 2007;125:908–915. doi: 10.1001/archopht.125.7.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ahadome, S. D. et al. Classical dendritic cells mediate fibrosis directly via the retinoic acid pathway in severe eye allergy. JCI insight1, 10.1172/jci.insight.87012 (2016). [DOI] [PMC free article] [PubMed]
- 42.Saban, D. R. et al. Deletion of Thrombospondin (TSP)-1 in Dendritic Cells (DC) of the Conjunctiva Exacerbates Allergic Conjunctivitis (AC). ARVO Meeting Abstracts 53, 1241 (2012).
- 43.Hamrah P, Huq SO, Liu Y, Zhang Q, Dana MR. Corneal immunity is mediated by heterogeneous population of antigen-presenting cells. J. Leukoc. Biol. 2003;74:172–178. doi: 10.1189/jlb.1102544. [DOI] [PubMed] [Google Scholar]
- 44.Jamali A, et al. Characterization of Resident Corneal Plasmacytoid Dendritic Cells and Their Pivotal Role in Herpes Simplex Keratitis. Cell Rep. 2020;32:108099. doi: 10.1016/j.celrep.2020.108099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jamali, A. et al. Plasmacytoid dendritic cells in the eye. Review. Prog Retin Eye Res80, 100877 (2021). [DOI] [PMC free article] [PubMed]
- 46.Foulsham, W., Coco, G., Amouzegar, A., Chauhan, S. K. & Dana, R. When Clarity Is Crucial: Regulating Ocular Surface Immunity. Trend Immunol.10.1016/j.it.2017.11.007 (2017). [DOI] [PMC free article] [PubMed]
- 47.Lee, H. S., Amouzegar, A. & Dana, R. Kinetics of Corneal Antigen Presenting Cells in Experimental Dry Eye Disease. BMJ Open Ophthalmol.1, 10.1136/bmjophth-2017-000078 (2017). [DOI] [PMC free article] [PubMed]
- 48.Pian Y, et al. Type 3 Innate Lymphoid Cells Direct Goblet Cell Differentiation via the LT-LTβR Pathway during Listeria Infection. J. Immunol. 2020;205:853–863. doi: 10.4049/jimmunol.2000197. [DOI] [PubMed] [Google Scholar]
- 49.Yoon CH, Lee D, Jeong HJ, Ryu JS, Kim MK. Distribution of Interleukin-22-secreting Immune Cells in Conjunctival Associated Lymphoid Tissue. Korean J. Ophthalmol.: KJO. 2018;32:147–153. doi: 10.3341/kjo.2017.0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ji, Y. W. et al. Lacrimal gland-derived IL-22 regulates IL-17-mediated ocular mucosal inflammation. Mucosal Immunol.10.1038/mi.2016.119 (2017). [DOI] [PMC free article] [PubMed]
- 51.de Paiva CS, et al. Homeostatic control of conjunctival mucosal goblet cells by NKT-derived IL-13. Mucosal. Immunol. 2011;4:397–408. doi: 10.1038/mi.2010.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McCauley HA, Guasch G. Three cheers for the goblet cell: maintaining homeostasis in mucosal epithelia. Trends Mol. Med. 2015;21:492–503. doi: 10.1016/j.molmed.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 53.Pflugfelder SC, de Paiva CS, Villarreal AL, Stern ME. Effects of sequential artificial tear and cyclosporine emulsion therapy on conjunctival goblet cell density and transforming growth factor-beta2 production. Cornea. 2008;27:64–69. doi: 10.1097/ICO.0b013e318158f6dc. [DOI] [PubMed] [Google Scholar]
- 54.Barbosa FL, et al. Goblet Cells Contribute to Ocular Surface Immune Tolerance-Implications for Dry Eye Disease. Int. J. Mol. Sci. 2017;18:1–13. doi: 10.3390/ijms18050978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ko BY, Xiao Y, Barbosa FL, de Paiva CS, Pflugfelder SC. Goblet cell loss abrogates ocular surface immune tolerance. JCI Insight. 2018;3:98222. doi: 10.1172/jci.insight.98222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kulkarni DH, et al. Goblet cell associated antigen passages support the induction and maintenance of oral tolerance. Mucosal Immunol. 2020;13:271–282. doi: 10.1038/s41385-019-0240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Galletti, J. G. & de Paiva, C. S. Age-related changes in ocular mucosal tolerance: Lessons learned from gut and respiratory tract immunity. Immunology, 10.1111/imm.13338 (2021). [DOI] [PMC free article] [PubMed]
- 58.de Paiva CS, et al. Dry Eye-Induced Conjunctival Epithelial Squamous Metaplasia Is Modulated by Interferon-{gamma} Investig. Ophthalmol. Vis. Sci. 2007;48:2553–2560. doi: 10.1167/iovs.07-0069. [DOI] [PubMed] [Google Scholar]
- 59.Garcia-Posadas L, et al. Interaction of IFN-gamma with cholinergic agonists to modulate rat and human goblet cell function. Mucosal Immunol. 2016;9:206–217. doi: 10.1038/mi.2015.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang X, et al. Topical interferon-gamma neutralization prevents conjunctival goblet cell loss in experimental murine dry eye. Exp. Eye Res. 2014;118:117–124. doi: 10.1016/j.exer.2013.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Puro DG. Role of ion channels in the functional response of conjunctival goblet cells to dry eye. Am. J. Physiol. Cell Physiol. 2018;315:C236–C246. doi: 10.1152/ajpcell.00077.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Coursey TG, Henriksson JT, Barbosa FL, de Paiva CS, Pflugfelder SC. Interferon-gamma-Induced Unfolded Protein Response in Conjunctival Goblet Cells as a Cause of Mucin Deficiency in Sjogren Syndrome. Am. J. Pathol. 2016;186:1547–1558. doi: 10.1016/j.ajpath.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tukler Henriksson J, Coursey TG, Corry DB, De Paiva CS, Pflugfelder SC. IL-13 Stimulates Proliferation and Expression of Mucin and Immunomodulatory Genes in Cultured Conjunctival Goblet Cells. Investig. Ophthalmol. Vis. Sci. 2015;56:4186–4197. doi: 10.1167/iovs.14-15496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Marko CK, et al. Spdef null mice lack conjunctival goblet cells and provide a model of dry eye. Am. J. Pathol. 2013;183:35–48. doi: 10.1016/j.ajpath.2013.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dang Z, Kuffová L, Liu L, Forrester JV. Soluble antigen traffics rapidly and selectively from the corneal surface to the eye draining lymph node and activates T cells when codelivered with CpG oligonucleotides. J. Leukoc. Biol. 2014;95:431–440. doi: 10.1189/jlb.0612294. [DOI] [PubMed] [Google Scholar]
- 66.Stern ME, Gao J, Siemasko KF, Beuerman RW, Pflugfelder SC. The role of the lacrimal functional unit in the pathophysiology of dry eye. Exp. Eye Res. 2004;78:409–416. doi: 10.1016/j.exer.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 67.Tsubota K, et al. Quantitative videographic analysis of blinking in normal subjects and patients with dry eye. Arch. Ophthalmol. 1996;114:715–720. doi: 10.1001/archopht.1996.01100130707012. [DOI] [PubMed] [Google Scholar]
- 68.Tsubota K, Nakamori K. Dry eyes and video display terminals. N. Eng. J. Med. 1993;328:584–584. doi: 10.1056/NEJM199302253280817. [DOI] [PubMed] [Google Scholar]
- 69.Loebis R, Subakti Zulkarnain B, Zahra N. Correlation between the exposure time to mobile devices and the prevalence of evaporative dry eyes as one of the symptoms of computer vision syndrome among Senior High School students in East Java, Indonesia. J. Basic Clin. Physiol. Pharmacol. 2021;32:541–545. doi: 10.1515/jbcpp-2020-0478. [DOI] [PubMed] [Google Scholar]
- 70.de Paiva CS, et al. Altered Mucosal Microbiome Diversity and Disease Severity in Sjogren Syndrome. Sci. Rep. 2016;6:23561–23571. doi: 10.1038/srep23561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ozkan J, Coroneo M, Willcox M, Wemheuer B, Thomas T. Identification and Visualization of a Distinct Microbiome in Ocular Surface Conjunctival Tissue. Investig. Ophthalmol. Vis. Sci. 2018;59:4268–4276. doi: 10.1167/iovs.18-24651. [DOI] [PubMed] [Google Scholar]
- 72.Ozkan J, Willcox MD. The Ocular Microbiome: Molecular Characterization of a Unique and Low Microbial Environment. Curr. Eye Res. 2019;44:685–694. doi: 10.1080/02713683.2019.1570526. [DOI] [PubMed] [Google Scholar]
- 73.Ozkan, J. et al. The Temporal Stability of the Ocular Surface Microbiome. ARVO Abstracts,2017, 5615 (2017).
- 74.Nolan J. Evaluation of conjunctival and nasal bacterial cultures before intra-ocular operations. Br. J. Ophthalmol. 1967;51:483–485. doi: 10.1136/bjo.51.7.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Willcox MD. Characterization of the normal microbiota of the ocular surface. Exp. Eye Res. 2013;117:99–105. doi: 10.1016/j.exer.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 76.Dong Q, et al. Diversity of bacteria at healthy human conjunctiva. Investig. Ophthalmol. Vis. Sci. 2011;52:5408–5413. doi: 10.1167/iovs.10-6939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wilbanks GA, Mammolenti M, Streilein JW. Studies on the induction of anterior chamber-associated immune deviation (ACAID). III. Induction of ACAID depends upon intraocular transforming growth factor-beta. Eur. J. Immunol. 1992;22:165–173. doi: 10.1002/eji.1830220125. [DOI] [PubMed] [Google Scholar]
- 78.Zhou R, Horai R, Mattapallil MJ, Caspi RR. A new look at immune privilege of the eye: dual role for the vision-related molecule retinoic acid. J. Immunol. 2011;187:4170–4177. doi: 10.4049/jimmunol.1101634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhou R, et al. The living eye “disarms” uncommitted autoreactive T cells by converting them to Foxp3(+) regulatory cells following local antigen recognition. J. Immunol. 2012;188:1742–1750. doi: 10.4049/jimmunol.1102415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Taylor AW, Streilein JW, Cousins SW. Immunoreactive vasoactive intestinal peptide contributes to the immunosuppressive activity of normal aqueous humor. J. Immunol. 1994;153:1080–1086. [PubMed] [Google Scholar]
- 81.Ferguson TA, Fletcher S, Herndon J, Griffith TS. Neuropeptides modulate immune deviation induced via the anterior chamber of the eye. J. Immunol. 1995;155:1746–1756. [PubMed] [Google Scholar]
- 82.Griffith TS, Yu X, Herndon JM, Green DR, Ferguson TA. CD95-induced apoptosis of lymphocytes in an immune privileged site induces immunological tolerance. Immunity. 1996;5:7–16. doi: 10.1016/S1074-7613(00)80305-2. [DOI] [PubMed] [Google Scholar]
- 83.Volpe, E., Sambucci, M., Battistini, L. & Borsellino, G. Fas–Fas Ligand: Checkpoint of T Cell Functions in Multiple Sclerosis. Front Immunol.7, 10.3389/fimmu.2016.00382 (2016). [DOI] [PMC free article] [PubMed]
- 84.Bouillet P, O’Reilly LA. CD95, BIM and T cell homeostasis. Nat. Rev. Immunol. 2009;9:514–519. doi: 10.1038/nri2570. [DOI] [PubMed] [Google Scholar]
- 85.Castro JE, et al. Fas modulation of apoptosis during negative selection of thymocytes. Immunity. 1996;5:617–627. doi: 10.1016/S1074-7613(00)80275-7. [DOI] [PubMed] [Google Scholar]
- 86.Refaeli Y, Van Parijs L, London CA, Tschopp J, Abbas AK. Biochemical mechanisms of IL-2-regulated Fas-mediated T cell apoptosis. Immunity. 1998;8:615–623. doi: 10.1016/S1074-7613(00)80566-X. [DOI] [PubMed] [Google Scholar]
- 87.Choi C, Benveniste EN. Fas ligand/Fas system in the brain: regulator of immune and apoptotic responses. Brain Res Brain Res Rev. 2004;44:65–81. doi: 10.1016/j.brainresrev.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 88.Zheng L, Sharma R, Gaskin F, Fu SM, Ju ST. A novel role of IL-2 in organ-specific autoimmune inflammation beyond regulatory T cell checkpoint: both IL-2 knockout and Fas mutation prolong lifespan of Scurfy mice but by different mechanisms. J. Immunol. 2007;179:8035–8041. doi: 10.4049/jimmunol.179.12.8035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Esser MT, et al. IL-2 induces Fas ligand/Fas (CD95L/CD95) cytotoxicity in CD8 + and CD4 + T lymphocyte clones. J. Immunol. 1997;158:5612–5618. [PubMed] [Google Scholar]
- 90.Elzey BD, et al. Regulation of Fas ligand-induced apoptosis by TNF. J. Immunol. 2001;167:3049–3056. doi: 10.4049/jimmunol.167.6.3049. [DOI] [PubMed] [Google Scholar]
- 91.Griffith TS, Brunner T, Fletcher SM, Green DR, Ferguson TA. Fas ligand-induced apoptosis as a mechanism of immune privilege. Science. 1995;270:1189–1192. doi: 10.1126/science.270.5239.1189. [DOI] [PubMed] [Google Scholar]
- 92.Jabs DA, Lee B, Whittum-Hudson JA, Prendergast RA. Th1 versus Th2 immune responses in autoimmune lacrimal gland disease in MRL/Mp mice. Investig. Ophthalmol. Vis. Sci. 2000;41:826–831. [PubMed] [Google Scholar]
- 93.Jabs DA, et al. Autoimmune Th2-mediated dacryoadenitis in MRL/MpJ mice becomes Th1-mediated in IL-4 deficient MRL/MpJ mice. Investig. Ophthalmol. Vis. Sci. 2007;48:5624–5629. doi: 10.1167/iovs.07-0237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Jie G, Jiang Q, Rui Z, Yifei Y. Expression of interleukin-17 in autoimmune dacryoadenitis in MRL/lpr mice. Curr. Eye Res. 2010;35:865–871. doi: 10.3109/02713683.2010.497600. [DOI] [PubMed] [Google Scholar]
- 95.Durrani OM, et al. Degree, duration, and causes of visual loss in uveitis. Br. J. Ophthalmol. 2004;88:1159–1162. doi: 10.1136/bjo.2003.037226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Egan RM, et al. In vivo behavior of peptide-specific T cells during mucosal tolerance induction: antigen introduced through the mucosa of the conjunctiva elicits prolonged antigen-specific T cell priming followed by anergy. J. Immunol. 2000;164:4543–4550. doi: 10.4049/jimmunol.164.9.4543. [DOI] [PubMed] [Google Scholar]
- 97.Galletti JG, et al. Benzalkonium chloride breaks down conjunctival immunological tolerance in a murine model. Mucosal Immunol. 2013;6:24–34. doi: 10.1038/mi.2012.44. [DOI] [PubMed] [Google Scholar]
- 98.Galletti JG, Guzman M, Giordano MN. Mucosal immune tolerance at the ocular surface in health and disease. Immunology. 2017;150:397–407. doi: 10.1111/imm.12716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Pflugfelder SC, et al. Matrix metalloproteinase-9 knockout confers resistance to corneal epithelial barrier disruption in experimental dry eye. Am. J. Pathol. 2005;166:61–71. doi: 10.1016/S0002-9440(10)62232-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hu J, et al. IL-33/ST2/IL-9/IL-9R signaling disrupts ocular surface barrier in allergic inflammation. Mucosal Immunol. 2020;13:919–930. doi: 10.1038/s41385-020-0288-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Akdis, C. A. Does the epithelial barrier hypothesis explain the increase in allergy, autoimmunity and other chronic conditions? Nat. Rev. Immunol.10.1038/s41577-021-00538-7 (2021). [DOI] [PubMed]
- 102.Friedman ES, et al. Microbes vs. chemistry in the origin of the anaerobic gut lumen. Proc. Natl Acad. Sci. USA. 2018;115:4170–4175. doi: 10.1073/pnas.1718635115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Thursby E, Juge N. Introduction to the human gut microbiota. Biochemical J. 2017;474:1823–1836. doi: 10.1042/BCJ20160510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Goodrich JK, et al. Genetic Determinants of the Gut Microbiome in UK Twins. Cell host microbe. 2016;19:731–743. doi: 10.1016/j.chom.2016.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zarate-Blades CR, et al. Gut microbiota as a source of a surrogate antigen that triggers autoimmunity in an immune privileged site. Gut microbes. 2017;8:59–66. doi: 10.1080/19490976.2016.1273996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Dewhirst FE, et al. The human oral microbiome. J. Bacteriol. 2010;192:5002–5017. doi: 10.1128/JB.00542-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Deo PN, Deshmukh R. Oral microbiome: Unveiling the fundamentals. J. Oral. Maxillofac. Pathol. 2019;23:122–128. doi: 10.4103/jomfp.JOMFP_304_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Dutzan, N. et al. A dysbiotic microbiome triggers TH17 cells to mediate oral mucosal immunopathology in mice and humans. Sci. Transl. Med.10, 10.1126/scitranslmed.aat0797 (2018). [DOI] [PMC free article] [PubMed]
- 109.Byrd AL, Belkaid Y, Segre JA. The human skin microbiome. Nat. Rev. Microbiol. 2018;16:143–155. doi: 10.1038/nrmicro.2017.157. [DOI] [PubMed] [Google Scholar]
- 110.Harrison, O. J. et al. Commensal-specific T cell plasticity promotes rapid tissue adaptation to injury. Science363, 10.1126/science.aat6280 (2019). [DOI] [PMC free article] [PubMed]
- 111.Grice EA, Segre JA. The skin microbiome. Nat. Rev. Microbiol. 2011;9:244–253. doi: 10.1038/nrmicro2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Dickson RP, Huffnagle GB. The Lung Microbiome: New Principles for Respiratory Bacteriology in Health and Disease. PLoS Pathog. 2015;11:e1004923. doi: 10.1371/journal.ppat.1004923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kitsios, G. D. Translating Lung Microbiome Profiles into the Next-Generation Diagnostic Gold Standard for Pneumonia: a Clinical Investigator’s Perspective. mSystems3, 10.1128/mSystems.00153-17 (2018). [DOI] [PMC free article] [PubMed]
- 114.Kitsios GD, et al. Respiratory Tract Dysbiosis Is Associated with Worse Outcomes in Mechanically Ventilated Patients. Am. J. Respir. Crit. Care Med. 2020;202:1666–1677. doi: 10.1164/rccm.201912-2441OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zhao CY, et al. Microbiome Data Enhances Predictive Models of Lung Function in People With Cystic Fibrosis. J. Infect. Dis. 2021;223:S246–S256. doi: 10.1093/infdis/jiaa655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Doan T, et al. Paucibacterial Microbiome and Resident DNA Virome of the Healthy Conjunctiva. Invest Ophthalmol. Vis. Sci. 2016;57:5116–5126. doi: 10.1167/iovs.16-19803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.McDermott AM. Antimicrobial compounds in tears. Exp. Eye Res. 2013;117:53–61. doi: 10.1016/j.exer.2013.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wan SJ, Ma S, Evans DJ, Fleiszig SMJ. Resistance of the murine cornea to bacterial colonization during experimental dry eye. PloS one. 2020;15:e0234013. doi: 10.1371/journal.pone.0234013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Shin H, et al. Changes in the Eye Microbiota Associated with Contact Lens Wearing. mBio. 2016;7:e00198. doi: 10.1128/mBio.00198-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Cavuoto, K. M., Banerjee, S. & Galor, A. Relationship between the microbiome and ocular health. Ocul Surf, 10.1016/j.jtos.2019.05.006 (2019). [DOI] [PubMed]
- 121.Prashanthi, G. S. et al. Alterations in the Ocular Surface Fungal Microbiome in Fungal Keratitis Patients. Microorganisms7, 10.3390/microorganisms7090309 (2019). [DOI] [PMC free article] [PubMed]
- 122.Ozkan J, Majzoub ME, Coroneo M, Thomas T, Willcox M. Comparative analysis of ocular surface tissue microbiome in human, mouse, rabbit, and guinea pig. Exp. Eye Res. 2021;207:108609. doi: 10.1016/j.exer.2021.108609. [DOI] [PubMed] [Google Scholar]
- 123.Shanbhag SS, et al. Diphtheroids as Corneal Pathogens in Chronic Ocular Surface Disease in Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis. Cornea. 2021;40:774–779. doi: 10.1097/ICO.0000000000002696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Suzuki T, Sutani T, Nakai H, Shirahige K, Kinoshita S. The Microbiome of the Meibum and Ocular Surface in Healthy Subjects. Investigative Ophthalmol. Vis. Sci. 2020;61:18–18. doi: 10.1167/iovs.61.2.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bernard KA, et al. Corynebacterium lowii sp. nov. and Corynebacterium oculi sp. nov., derived from human clinical disease and an emended description of Corynebacterium mastitidis. Int J. Syst. Evol. Microbiol. 2016;66:2803–2812. doi: 10.1099/ijsem.0.001059. [DOI] [PubMed] [Google Scholar]
- 126.Kugadas A, Wright Q, Geddes-McAlister J, Gadjeva M. Role of Microbiota in Strengthening Ocular Mucosal Barrier Function Through Secretory IgA. Investig. Ophthalmol. Vis. Sci. 2017;58:4593–4600. doi: 10.1167/iovs.17-22119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Zaheer, M. et al. Protective role of commensal bacteria in Sjogren Syndrome. J. Autoimmun. 45–56, 10.1016/j.jaut.2018.06.004 (2018). [DOI] [PMC free article] [PubMed]
- 128.Wang, C. et al. Sjogren-Like Lacrimal Keratoconjunctivitis in Germ-Free Mice. Int. J. Mol. Sci.19, pii: E565, 10.3390/ijms19020565 (2018). [DOI] [PMC free article] [PubMed]
- 129.Jayasudha R, et al. Alterations in gut bacterial and fungal microbiomes are associated with bacterial Keratitis, an inflammatory disease of the human eye. J. Biosci. 2018;43:835–856. doi: 10.1007/s12038-018-9798-6. [DOI] [PubMed] [Google Scholar]
- 130.Kalyana Chakravarthy S, et al. Alterations in the gut bacterial microbiome in fungal Keratitis patients. PloS one. 2018;13:e0199640. doi: 10.1371/journal.pone.0199640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Horai R, et al. Microbiota-Dependent Activation of an Autoreactive T Cell Receptor Provokes Autoimmunity in an Immunologically Privileged Site. Immunity. 2015;43:343–353. doi: 10.1016/j.immuni.2015.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Nakamura YK, et al. Gut Microbial Alterations Associated With Protection From Autoimmune Uveitis. Investig. Ophthalmol. Vis. Sci. 2016;57:3747–3758. doi: 10.1167/iovs.16-19733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Tang J, Tang Y, Yi I, Chen DF. The role of commensal microflora-induced T cell responses in glaucoma neurodegeneration. Prog. Brain Res. 2020;256:79–97. doi: 10.1016/bs.pbr.2020.06.002. [DOI] [PubMed] [Google Scholar]
- 134.Skrzypecki J, et al. Glaucoma patients have an increased level of trimethylamine, a toxic product of gut bacteria, in the aqueous humor: a pilot study. Int Ophthalmol. 2021;41:341–347. doi: 10.1007/s10792-020-01587-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zinkernagel MS, et al. Association of the Intestinal Microbiome with the Development of Neovascular Age-Related Macular Degeneration. Sci. Rep. 2017;7:40826. doi: 10.1038/srep40826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Rinninella, E. et al. The Role of Diet, Micronutrients and the Gut Microbiota in Age-Related Macular Degeneration: New Perspectives from the Gut(-)Retina Axis. Nutrients10, 10.3390/nu10111677 (2018). [DOI] [PMC free article] [PubMed]
- 137.Rowan S, Taylor A. The Role of Microbiota in Retinal Disease. Adv. Exp. Med. Biol. 2018;1074:429–435. doi: 10.1007/978-3-319-75402-4_53. [DOI] [PubMed] [Google Scholar]
- 138.Marfurt CF, Cox J, Deek S, Dvorscak L. Anatomy of the human corneal innervation. Exp. Eye Res. 2010;90:478–492. doi: 10.1016/j.exer.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 139.Muller LJ, Marfurt CF, Kruse F, Tervo TM. Corneal nerves: structure, contents and function. Exp. Eye Res. 2003;76:521–542. doi: 10.1016/S0014-4835(03)00050-2. [DOI] [PubMed] [Google Scholar]
- 140.Yun H, Lathrop KL, Hendricks RL. A Central Role for Sympathetic Nerves in Herpes Stromal Keratitis in Mice. Investig. Ophthalmol. Vis. Sci. 2016;57:1749–1756. doi: 10.1167/iovs.16-19183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Xue Y, et al. The mouse autonomic nervous system modulates inflammation and epithelial renewal after corneal abrasion through the activation of distinct local macrophages. Mucosal Immunol. 2018;11:1496–1511. doi: 10.1038/s41385-018-0031-6. [DOI] [PubMed] [Google Scholar]
- 142.Mergler S, et al. TRPV channels mediate temperature-sensing in human corneal endothelial cells. Exp. Eye Res. 2010;90:758–770. doi: 10.1016/j.exer.2010.03.010. [DOI] [PubMed] [Google Scholar]
- 143.Okada Y, et al. Transient Receptor Potential Channels and Corneal Stromal Inflammation. Cornea. 2015;34:S136–S141. doi: 10.1097/ICO.0000000000000602. [DOI] [PubMed] [Google Scholar]
- 144.Eguchi H, Hiura A, Nakagawa H, Kusaka S, Shimomura Y. Corneal Nerve Fiber Structure, Its Role in Corneal Function, and Its Changes in Corneal Diseases. BioMed. Res. Int. 2017;2017:3242649. doi: 10.1155/2017/3242649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Yang, J. M., Wei, E. T., Kim, S. J. & Yoon, K. C. TRPM8 Channels and Dry Eye. Pharmaceuticals (Basel)11, 10.3390/ph11040125 (2018). [DOI] [PMC free article] [PubMed]
- 146.Yoon, H. J. et al. Topical TRPM8 Agonist for Relieving Neuropathic Ocular Pain in Patients with Dry Eye: A Pilot Study. J. Clin. Med.10, 10.3390/jcm10020250 (2021). [DOI] [PMC free article] [PubMed]
- 147.Guarino BD, Paruchuri S, Thodeti CK. The role of TRPV4 channels in ocular function and pathologies. Exp. Eye Res. 2020;201:108257. doi: 10.1016/j.exer.2020.108257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Callejo G, et al. Acid-sensing ion channels detect moderate acidifications to induce ocular pain. Pain. 2015;156:483–495. doi: 10.1097/01.j.pain.0000460335.49525.17. [DOI] [PubMed] [Google Scholar]
- 149.McMonnies CW. Diagnosis and remediation of blink inefficiency. Contact Lens anterior eye: J. Br. Contact Lens Assoc. 2021;44:101331. doi: 10.1016/j.clae.2020.04.015. [DOI] [PubMed] [Google Scholar]
- 150.Bannier-Helaouet M, et al. Exploring the human lacrimal gland using organoids and single-cell sequencing. Cell Stem Cell. 2021;28:1221–1232 e1227. doi: 10.1016/j.stem.2021.02.024. [DOI] [PubMed] [Google Scholar]
- 151.Dikmetas O, Kocabeyoglu S, Mocan MC. The Association between Meibomian Gland Atrophy and Corneal Subbasal Nerve Loss in Patients with Chronic Ocular Graft-versus-host Disease. Curr. eye Res. 2021;46:796–801. doi: 10.1080/02713683.2020.1846754. [DOI] [PubMed] [Google Scholar]
- 152.Lee SJ, et al. Corneal lymphangiogenesis in dry eye disease is regulated by substance P/neurokinin-1 receptor system through controlling expression of vascular endothelial growth factor receptor 3. Ocul. Surf. 2021;22:72–79. doi: 10.1016/j.jtos.2021.07.003. [DOI] [PubMed] [Google Scholar]
- 153.Yu M, et al. Neurokinin-1 Receptor Antagonism Ameliorates Dry Eye Disease by Inhibiting Antigen-Presenting Cell Maturation and T Helper 17 Cell Activation. Am. J. Pathol. 2020;190:125–133. doi: 10.1016/j.ajpath.2019.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Yuan K, et al. Sensory nerves promote corneal inflammation resolution via CGRP mediated transformation of macrophages to the M2 phenotype through the PI3K/AKT signaling pathway. Int. Immunopharmacol. 2022;102:108426. doi: 10.1016/j.intimp.2021.108426. [DOI] [PubMed] [Google Scholar]
- 155.Mikulec AA, Tanelian DL. CGRP increases the rate of corneal re-epithelialization in an in vitro whole mount preparation. J. Ocul. Pharm. Ther. 1996;12:417–423. doi: 10.1089/jop.1996.12.417. [DOI] [PubMed] [Google Scholar]
- 156.Diel RJ, et al. Photophobia: shared pathophysiology underlying dry eye disease, migraine and traumatic brain injury leading to central neuroplasticity of the trigeminothalamic pathway. Br. J. Ophthalmol. 2021;105:751–760. doi: 10.1136/bjophthalmol-2020-316417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Lin T, et al. Pseudomonas aeruginosa-induced nociceptor activation increases susceptibility to infection. PLoS Pathog. 2021;17:e1009557. doi: 10.1371/journal.ppat.1009557. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 158.Sacchetti M, et al. Tear levels of neuropeptides increase after specific allergen challenge in allergic conjunctivitis. Mol. Vis. 2011;17:47–52. [PMC free article] [PubMed] [Google Scholar]
- 159.Berger EA, Vistisen KS, Barrett RP, Hazlett LD. Effects of VIP on corneal reconstitution and homeostasis following Pseudomonas aeruginosa induced keratitis. Investig. Ophthalmol. Vis. Sci. 2012;53:7432–7439. doi: 10.1167/iovs.12-9894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Jiang X, McClellan SA, Barrett RP, Zhang Y, Hazlett LD. Vasoactive intestinal peptide downregulates proinflammatory TLRs while upregulating anti-inflammatory TLRs in the infected cornea. J. Immunol. 2012;189:269–278. doi: 10.4049/jimmunol.1200365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Zhang Y, et al. Role of VIP and Sonic Hedgehog Signaling Pathways in Mediating Epithelial Wound Healing, Sensory Nerve Regeneration, and Their Defects in Diabetic Corneas. Diabetes. 2020;69:1549–1561. doi: 10.2337/db19-0870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Hwang, D. D., Lee, S. J., Kim, J. H. & Lee, S. M. The Role of Neuropeptides in Pathogenesis of Dry Dye. J. Clin. Med.10, 10.3390/jcm10184248 (2021). [DOI] [PMC free article] [PubMed]
- 163.Geppetti P, Materazzi S, Nicoletti P. The transient receptor potential vanilloid 1: role in airway inflammation and disease. Eur. J. Pharmacol. 2006;533:207–214. doi: 10.1016/j.ejphar.2005.12.063. [DOI] [PubMed] [Google Scholar]
- 164.Baral P, et al. Nociceptor sensory neurons suppress neutrophil and gammadelta T cell responses in bacterial lung infections and lethal pneumonia. Nat. Med. 2018;24:417–426. doi: 10.1038/nm.4501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Guo Y, Ying S, Zhao X, Liu J, Wang Y. Increased expression of lung TRPV1/TRPA1 in a cough model of bleomycin-induced pulmonary fibrosis in Guinea pigs. BMC Pulm. Med. 2019;19:27. doi: 10.1186/s12890-019-0792-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Sadofsky LR, et al. Inflammatory stimuli up-regulate transient receptor potential vanilloid-1 expression in human bronchial fibroblasts. Exp. Lung Res. 2012;38:75–81. doi: 10.3109/01902148.2011.644027. [DOI] [PubMed] [Google Scholar]
- 167.Zhang G, Lin RL, Wiggers M, Snow DM, Lee LY. Altered expression of TRPV1 and sensitivity to capsaicin in pulmonary myelinated afferents following chronic airway inflammation in the rat. J. Physiol. 2008;586:5771–5786. doi: 10.1113/jphysiol.2008.161042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Jiao H, Ivanusic JJ, McMenamin PG, Chinnery HR. Distribution of Corneal TRPV1 and Its Association With Immune Cells During Homeostasis and Injury. Investig. Ophthalmol. Vis. Sci. 2021;62:6. doi: 10.1167/iovs.62.9.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Wan SJ, et al. Nerve-associated transient receptor potential ion channels can contribute to intrinsic resistance to bacterial adhesion in vivo. FASEB J. 2021;35:e21899. doi: 10.1096/fj.202100874R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Trier AM, Mack MR, Kim BS. The Neuroimmune Axis in Skin Sensation, Inflammation, and Immunity. J. Immunol. 2019;202:2829–2835. doi: 10.4049/jimmunol.1801473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Cohen JA, et al. Cutaneous TRPV1( + ) Neurons Trigger Protective Innate Type 17 Anticipatory Immunity. Cell. 2019;178:919–932 e914. doi: 10.1016/j.cell.2019.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Zhang S, et al. Nonpeptidergic neurons suppress mast cells via glutamate to maintain skin homeostasis. Cell. 2021;184:2151–2166 e2116. doi: 10.1016/j.cell.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wang F, et al. A basophil-neuronal axis promotes itch. Cell. 2021;184:422–440 e417. doi: 10.1016/j.cell.2020.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Oetjen LK, et al. Sensory Neurons Co-opt Classical Immune Signaling Pathways to Mediate Chronic Itch. Cell. 2017;171:217–228 e213. doi: 10.1016/j.cell.2017.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Huang CC, et al. Anatomical and functional dichotomy of ocular itch and pain. Nat. Med. 2018;24:1268–1276. doi: 10.1038/s41591-018-0083-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.You XY, et al. Intestinal Mucosal Barrier Is Regulated by Intestinal Tract Neuro-Immune Interplay. Front. Pharmacol. 2021;12:659716. doi: 10.3389/fphar.2021.659716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Matheis F, et al. Adrenergic Signaling in Muscularis Macrophages Limits Infection-Induced Neuronal Loss. Cell. 2020;180:64–78 e16. doi: 10.1016/j.cell.2019.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Yu YB, Li YQ. Enteric glial cells and their role in the intestinal epithelial barrier. World J. gastroenterology: WJG. 2014;20:11273–11280. doi: 10.3748/wjg.v20.i32.11273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Deng Y, et al. Identification of an intraocular microbiota. Cell Discov. 2021;7:13. doi: 10.1038/s41421-021-00245-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Lairson DR, Begley CE, Reynolds TF, Wilhelmus KR. Prevention of herpes simplex virus eye disease: a cost-effectiveness analysis. Arch. Ophthalmol. 2003;121:108–112. doi: 10.1001/archopht.121.1.108. [DOI] [PubMed] [Google Scholar]
- 181.Farooq AV, Shukla D. Herpes simplex epithelial and stromal keratitis: an epidemiologic update. Surv. Ophthalmol. 2012;57:448–462. doi: 10.1016/j.survophthal.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Grinde, B. Herpesviruses: latency and reactivation - viral strategies and host response. J. Oral Microbiol5, 10.3402/jom.v5i0.22766 (2013). [DOI] [PMC free article] [PubMed]
- 183.Freeman ML, Sheridan BS, Bonneau RH, Hendricks RL. Psychological stress compromises CD8 + T cell control of latent herpes simplex virus type 1 infections. J. Immunol. 2007;179:322–328. doi: 10.4049/jimmunol.179.1.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Doll JR, Hoebe K, Thompson RL, Sawtell NM. Resolution of herpes simplex virus reactivation in vivo results in neuronal destruction. PLoS Pathog. 2020;16:e1008296. doi: 10.1371/journal.ppat.1008296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Doll, J. R., Thompson, R. L. & Sawtell, N. M. Infectious Herpes Simplex Virus in the Brain Stem Is Correlated with Reactivation in the Trigeminal Ganglia. J. Virol.93, 10.1128/JVI.02209-18 (2019). [DOI] [PMC free article] [PubMed]
- 186.Yin, X. T. et al. CD28 Costimulation Is Required for Development of Herpetic Stromal Keratitis but Does Not Prevent Establishment of Latency. J. Virol.93, 10.1128/JVI.00659-19 (2019). [DOI] [PMC free article] [PubMed]
- 187.Tajfirouz D, et al. CXCL9 compensates for the absence of CXCL10 during recurrent Herpetic stromal keratitis. Virology. 2017;506:7–13. doi: 10.1016/j.virol.2017.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Rogge M, et al. Therapeutic Use of Soluble Fas Ligand Ameliorates Acute and Recurrent Herpetic Stromal Keratitis in Mice. Investig. Ophthalmol. Vis. Sci. 2015;56:6377–6386. doi: 10.1167/iovs.15-16588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Donaghy H, et al. Role for plasmacytoid dendritic cells in the immune control of recurrent human herpes simplex virus infection. J. Virol. 2009;83:1952–1961. doi: 10.1128/JVI.01578-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Moss NJ, et al. Peripheral blood CD4 T-cell and plasmacytoid dendritic cell (pDC) reactivity to herpes simplex virus 2 and pDC number do not correlate with the clinical or virologic severity of recurrent genital herpes. J. Virol. 2012;86:9952–9963. doi: 10.1128/JVI.00829-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Li H, et al. Herpes simplex virus 1 infection induces the expression of proinflammatory cytokines, interferons and TLR7 in human corneal epithelial cells. Immunology. 2006;117:167–176. doi: 10.1111/j.1365-2567.2005.02275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Liu T, Tang Q, Hendricks RL. Inflammatory infiltration of the trigeminal ganglion after herpes simplex virus type 1 corneal infection. J. Virol. 1996;70:264–271. doi: 10.1128/jvi.70.1.264-271.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.St Leger AJ, Jeon S, Hendricks RL. Broadening the repertoire of functional herpes simplex virus type 1-specific CD8 + T cells reduces viral reactivation from latency in sensory ganglia. J. Immunol. 2013;191:2258–2265. doi: 10.4049/jimmunol.1300585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Sheridan BS, Cherpes TL, Urban J, Kalinski P, Hendricks RL. Reevaluating the CD8 T-cell response to herpes simplex virus type 1: involvement of CD8 T cells reactive to subdominant epitopes. J. Virol. 2009;83:2237–2245. doi: 10.1128/JVI.01699-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Knickelbein JE, et al. Noncytotoxic lytic granule-mediated CD8 + T cell inhibition of HSV-1 reactivation from neuronal latency. Science. 2008;322:268–271. doi: 10.1126/science.1164164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Himmelein S, et al. Circulating herpes simplex type 1 (HSV-1)-specific CD8 + T cells do not access HSV-1 latently infected trigeminal ganglia. Herpesviridae. 2011;2:5. doi: 10.1186/2042-4280-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Gmyrek, G. B. et al. Herpes Simplex Virus 1 (HSV-1) 0DeltaNLS Live-Attenuated Vaccine Protects against Ocular HSV-1 Infection in the Absence of Neutralizing Antibody in HSV-1 gB T Cell Receptor-Specific Transgenic Mice. J. Virol.94, 10.1128/JVI.01000-20 (2020). [DOI] [PMC free article] [PubMed]
- 198.Decman V, Kinchington PR, Harvey SA, Hendricks RL. Gamma interferon can block herpes simplex virus type 1 reactivation from latency, even in the presence of late gene expression. J. Virol. 2005;79:10339–10347. doi: 10.1128/JVI.79.16.10339-10347.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Frank GM, et al. Early CD4( + ) T cell help prevents partial CD8( + ) T cell exhaustion and promotes maintenance of Herpes Simplex Virus 1 latency. J. Immunol. 2010;184:277–286. doi: 10.4049/jimmunol.0902373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Lepisto AJ, Frank GM, Xu M, Stuart PM, Hendricks RL. CD8 T cells mediate transient herpes stromal keratitis in CD4-deficient mice. Investig. Ophthalmol. Vis. Sci. 2006;47:3400–3409. doi: 10.1167/iovs.05-0898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Doymaz MZ, Rouse BT. Herpetic stromal keratitis: an immunopathologic disease mediated by CD4 + T lymphocytes. Investig. Ophthalmol. Vis. Sci. 1992;33:2165–2173. [PubMed] [Google Scholar]
- 202.Wuest T, Zheng M, Efstathiou S, Halford WP, Carr DJ. The herpes simplex virus-1 transactivator infected cell protein-4 drives VEGF-A dependent neovascularization. PLoS Pathog. 2011;7:e1002278. doi: 10.1371/journal.ppat.1002278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Yun H, et al. Production of the Cytokine VEGF-A by CD4( + ) T and Myeloid Cells Disrupts the Corneal Nerve Landscape and Promotes Herpes Stromal Keratitis. Immunity. 2020;53:1050–1062.e1055. doi: 10.1016/j.immuni.2020.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Stepp MA, et al. Reduced intraepithelial corneal nerve density and sensitivity accompany desiccating stress and aging in C57BL/6 mice. Exp. Eye Res. 2018;169:91–98. doi: 10.1016/j.exer.2018.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Chucair-Elliott AJ, Gurung HR, Carr MM, Carr DJJ. Colony Stimulating Factor-1 Receptor Expressing Cells Infiltrating the Cornea Control Corneal Nerve Degeneration in Response to HSV-1 Infection. Investig. Ophthalmol. Vis. Sci. 2017;58:4670–4682. doi: 10.1167/iovs.17-22159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Chucair-Elliott AJ, Jinkins J, Carr MM, Carr DJ. IL-6 Contributes to Corneal Nerve Degeneration after Herpes Simplex Virus Type I Infection. Am. J. Pathol. 2016;186:2665–2678. doi: 10.1016/j.ajpath.2016.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Royer DJ, et al. Complement and CD4( + ) T cells drive context-specific corneal sensory neuropathy. eLife. 2019;8:e48378. doi: 10.7554/eLife.48378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Paunicka KJ, et al. Severing corneal nerves in one eye induces sympathetic loss of immune privilege and promotes rejection of future corneal allografts placed in either eye. Am. J. Transplant.: Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2015;15:1490–1501. doi: 10.1111/ajt.13240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Narayanan S, Manning J, Proske R, McDermott AM. Effect of hyperosmolality on beta-defensin gene expression by human corneal epithelial cells. Cornea. 2006;25:1063–1068. doi: 10.1097/01.ico.0000228785.84581.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.McDermott AM. The role of antimicrobial peptides at the ocular surface. Ophthalmic. Res. 2009;41:60–75. doi: 10.1159/000187622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Garreis F, Gottschalt M, Paulsen FP. Antimicrobial peptides as a major part of the innate immune defense at the ocular surface. Dev. Ophthalmol. 2010;45:16–22. doi: 10.1159/000315016. [DOI] [PubMed] [Google Scholar]
- 212.Lu J, et al. Lactoferrin: A Critical Mediator of Both Host Immune Response and Antimicrobial Activity in Response to Streptococcal Infections. ACS Infect. Dis. 2020;6:1615–1623. doi: 10.1021/acsinfecdis.0c00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Lai X, et al. Identified human breast milk compositions effectively inhibit SARS-CoV-2 and variants infection and replication. iScience. 2022;25:104136. doi: 10.1016/j.isci.2022.104136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Dartt DA. Tear lipocalin: structure and function. Ocul. Surf. 2011;9:126–138. doi: 10.1016/S1542-0124(11)70022-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Fluckinger M, Haas H, Merschak P, Glasgow BJ, Redl B. Human tear lipocalin exhibits antimicrobial activity by scavenging microbial siderophores. Antimicrob. Agents Chemother. 2004;48:3367–3372. doi: 10.1128/AAC.48.9.3367-3372.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Deshpande SP, Kumaraguru U, Rouse BT. Dual role of B cells in mediating innate and acquired immunity to herpes simplex virus infections. Cell. Immunol. 2000;202:79–87. doi: 10.1006/cimm.2000.1666. [DOI] [PubMed] [Google Scholar]
- 217.Deshpande SP, Zheng M, Daheshia M, Rouse BT. Pathogenesis of herpes simplex virus-induced ocular immunoinflammatory lesions in B-cell-deficient mice. J. Virol. 2000;74:3517–3524. doi: 10.1128/JVI.74.8.3517-3524.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Patel, C. D. et al. Trivalent Glycoprotein Subunit Vaccine Prevents Neonatal Herpes Simplex Virus Mortality and Morbidity. J. Virol.94, 10.1128/JVI.02163-19 (2020). [DOI] [PMC free article] [PubMed]
- 219.Patel, C. D. et al. Maternal immunization confers protection against neonatal herpes simplex mortality and behavioral morbidity. Sci. Transl. Med.11, 10.1126/scitranslmed.aau6039 (2019). [DOI] [PMC free article] [PubMed]
- 220.Kugadas A, et al. Impact of Microbiota on Resistance to Ocular Pseudomonas aeruginosa-Induced Keratitis. PLoS Pathog. 2016;12:e1005855. doi: 10.1371/journal.ppat.1005855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Kugadas, A. & Gadjeva, M. Impact of Microbiome on Ocular Health. Ocul. Surf, 10.1016/j.jtos.2016.04.004 (2016). [DOI] [PMC free article] [PubMed]
- 222.Trujillo-Vargas CM, et al. The gut-eye-lacrimal gland-microbiome axis in Sjogren Syndrome. Ocul. Surf. 2020;18:335–344. doi: 10.1016/j.jtos.2019.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Moon J, Choi SH, Yoon CH, Kim MK. Gut dysbiosis is prevailing in Sjogren’s syndrome and is related to dry eye severity. PloS one. 2020;15:e0229029. doi: 10.1371/journal.pone.0229029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Wang C, et al. Dysbiosis Modulates Ocular Surface Inflammatory Response to Liposaccharide. Investig. Ophthalmol. Vis. Sci. 2019;60:4224–4233. doi: 10.1167/iovs.19-27939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Markle JG, et al. Sex differences in the gut microbiome drive hormone-dependent regulation of autoimmunity. Science. 2013;339:1084–1088. doi: 10.1126/science.1233521. [DOI] [PubMed] [Google Scholar]
- 226.Wen L, et al. Innate immunity and intestinal microbiota in the development of Type 1 diabetes. Nature. 2008;455:1109–1113. doi: 10.1038/nature07336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Hansen CH, Yurkovetskiy LA, Chervonsky AV. Cutting Edge: Commensal Microbiota Has Disparate Effects on Manifestations of Polyglandular Autoimmune Inflammation. J. Immunol. 2016;197:701–705. doi: 10.4049/jimmunol.1502465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Hansen CHF, et al. Targeting gut microbiota and barrier function with prebiotics to alleviate autoimmune manifestations in NOD mice. Diabetologia. 2019;62:1689–1700. doi: 10.1007/s00125-019-4910-5. [DOI] [PubMed] [Google Scholar]
- 229.Pflugfelder SC, de Paiva CS. The Pathophysiology of Dry Eye Disease: What We Know and Future Directions for Research. Ophthalmology. 2017;124:S4–s13. doi: 10.1016/j.ophtha.2017.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Baudouin C, et al. Role of hyperosmolarity in the pathogenesis and management of dry eye disease: proceedings of the OCEAN group meeting. Ocul. Surf. 2013;11:246–258. doi: 10.1016/j.jtos.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 231.Zhou D, et al. Critical involvement of macrophage infiltration in the development of Sjogren’s syndrome-associated dry eye. Am. J. Pathol. 2012;181:753–760. doi: 10.1016/j.ajpath.2012.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Schaumburg CS, et al. Ocular surface APCs are necessary for autoreactive T cell-mediated experimental autoimmune lacrimal keratoconjunctivitis. J. Immunol. 2011;187:3653–3662. doi: 10.4049/jimmunol.1101442. [DOI] [PubMed] [Google Scholar]
- 233.Bron, A. J. et al. TFOS DEWS II pathophysiology report. Ocul. Surf, 10.1016/j.jtos.2017.05.011 (2017). [DOI] [PubMed]
- 234.Li DQ, Chen Z, Song XJ, Luo L, Pflugfelder SC. Stimulation of matrix metalloproteinases by hyperosmolarity via a JNK pathway in human corneal epithelial cells. Investig. Ophthalmol. Vis. Sci. 2004;45:4302–4311. doi: 10.1167/iovs.04-0299. [DOI] [PubMed] [Google Scholar]
- 235.Julio G, Lluch S, Pujol P, Merindano MD. Effects of tear hyperosmolarity on conjunctival cells in mild to moderate dry eye. Ophthalmic Physiol. Opt. 2012;32:317–323. doi: 10.1111/j.1475-1313.2012.00915.x. [DOI] [PubMed] [Google Scholar]
- 236.Luo L, Li DQ, Corrales RM, Pflugfelder SC. Hyperosmolar saline is a proinflammatory stress on the mouse ocular surface. Eye Contact Lens. 2005;31:186–193. doi: 10.1097/01.ICL.0000162759.79740.46. [DOI] [PubMed] [Google Scholar]
- 237.Wang B, et al. Melatonin ameliorates oxidative stress-mediated injuries through induction of HO-1 and restores autophagic flux in dry eye. Exp. Eye Res. 2021;205:108491. doi: 10.1016/j.exer.2021.108491. [DOI] [PubMed] [Google Scholar]
- 238.Katsiougiannis S, Tenta R, Skopouli FN. Endoplasmic reticulum stress causes autophagy and apoptosis leading to cellular redistribution of the autoantigens Ro/Sjögren’s syndrome-related antigen A (SSA) and La/SSB in salivary gland epithelial cells. Clin. Exp. Immunol. 2015;181:244–252. doi: 10.1111/cei.12638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Tsubota K, Fujihara T, Saito K, Takeuchi T. Conjunctival epithelium expression of HLA-DR in dry eye patients. Ophthalmologica. 1999;213:16–19. doi: 10.1159/000027387. [DOI] [PubMed] [Google Scholar]
- 240.Chauhan SK, et al. Autoimmunity in dry eye is due to resistance of Th17 to Treg suppression. J. Immunol. 2009;182:1247–1252. doi: 10.4049/jimmunol.182.3.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Pelegrino FS, Pflugfelder SC, de Paiva CS. Low humidity environmental challenge causes barrier disruption and cornification of the mouse corneal epithelium via a c-jun N-terminal kinase 2 (JNK2) pathway. Exp. Eye Res. 2012;94:150–156. doi: 10.1016/j.exer.2011.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Zhang X, Wu Z, Hayashi Y, Okada R, Nakanishi H. Peripheral role of cathepsin S in Th1 cell-dependent transition of nerve injury-induced acute pain to a chronic pain state. J. Neurosci.: Off. J. Soc. Neurosci. 2014;34:3013–3022. doi: 10.1523/JNEUROSCI.3681-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.de Paiva CS, et al. IL-17 disrupts corneal barrier following desiccating stress. Mucosal. Immunol. 2009;2:243–253. doi: 10.1038/mi.2009.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Cha S, et al. A dual role for interferon-gamma in the pathogenesis of Sjogren’s syndrome-like autoimmune exocrinopathy in the nonobese diabetic mouse. Scand. J. Immunol. 2004;60:552–565. doi: 10.1111/j.0300-9475.2004.01508.x. [DOI] [PubMed] [Google Scholar]
- 245.Tsunawaki S, et al. Possible function of salivary gland epithelial cells as nonprofessional antigen-presenting cells in the development of Sjogren’s syndrome. J. Rheumatol. 2002;29:1884–1896. [PubMed] [Google Scholar]
- 246.Meng Z, Klinngam W, Edman MC, Hamm-Alvarez SF. Interferon-gamma treatment in vitro elicits some of the changes in cathepsin S and antigen presentation characteristic of lacrimal glands and corneas from the NOD mouse model of Sjogren’s Syndrome. PloS one. 2017;12:e0184781. doi: 10.1371/journal.pone.0184781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Heuberger C, Pott J, Maloy KJ. Why do intestinal epithelial cells express MHC class II. Immunology. 2021;162:357–367. doi: 10.1111/imm.13270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Royer DJ, Elliott MH, Le YZ, Carr DJJ. Corneal Epithelial Cells Exhibit Myeloid Characteristics and Present Antigen via MHC Class II. Investigative Ophthalmol. Vis. Sci. 2018;59:1512–1522. doi: 10.1167/iovs.17-23279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Epstein SP, Gadaria-Rathod N, Wei Y, Maguire MG, Asbell PA. HLA-DR expression as a biomarker of inflammation for multicenter clinical trials of ocular surface disease. Exp. Eye Res. 2013;111:95–104. doi: 10.1016/j.exer.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Versura P, Profazio V, Schiavi C, Campos EC. Hyperosmolar stress upregulates HLA-DR expression in human conjunctival epithelium in dry eye patients and in vitro models. Investig. Ophthalmol. Vis. Sci. 2011;52:5488–5496. doi: 10.1167/iovs.11-7215. [DOI] [PubMed] [Google Scholar]
- 251.Rolando M, et al. Distribution of Conjunctival HLA-DR Expression and the Pathogenesis of Damage in Early Dry Eyes. Cornea. 2005;24:951–954. doi: 10.1097/01.ico.0000157421.93522.00. [DOI] [PubMed] [Google Scholar]
- 252.Jirsova K, et al. Aberrant HLA-DR expression in the conjunctival epithelium after autologous serum treatment in patients with graft-versus-host disease or Sjögren’s syndrome. PloS one. 2020;15:e0231473. doi: 10.1371/journal.pone.0231473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Pisella PJ, et al. Flow cytometric analysis of conjunctival epithelium in ocular rosacea and keratoconjunctivitis sicca. Ophthalmology. 2000;107:1841–1849. doi: 10.1016/S0161-6420(00)00347-X. [DOI] [PubMed] [Google Scholar]
- 254.Okuma A, et al. Enhanced apoptosis by disruption of the STAT3-IkappaB-zeta signaling pathway in epithelial cells induces Sjogren’s syndrome-like autoimmune disease. Immunity. 2013;38:450–460. doi: 10.1016/j.immuni.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 255.Niederkorn JY, et al. Desiccating Stress Induces T Cell-Mediated Sjogren’s Syndrome-Like Lacrimal Keratoconjunctivitis. J. Immunol. 2006;176:3950–3957. doi: 10.4049/jimmunol.176.7.3950. [DOI] [PubMed] [Google Scholar]
- 256.de Paiva CS, et al. Corticosteroid and doxycycline suppress MMP-9 and inflammatory cytokine expression, MAPK activation in the corneal epithelium in experimental dry eye. Exp. Eye Res. 2006;83:526–535. doi: 10.1016/j.exer.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 257.Luo L, et al. Experimental dry eye stimulates production of inflammatory cytokines and MMP-9 and activates MAPK signaling pathways on the ocular surface. Investig. Ophthalmol. Vis. Sci. 2004;45:4293–4301. doi: 10.1167/iovs.03-1145. [DOI] [PubMed] [Google Scholar]
- 258.de Paiva CS, et al. Essential role for c-Jun N-terminal kinase 2 in corneal epithelial response to desiccating stress. Arch. Ophthalmol. 2009;127:1625–1631. doi: 10.1001/archophthalmol.2009.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Redfern RL, et al. Toll-like receptor expression and activation in mice with experimental dry eye. Investig. Ophthalmol. Vis. Sci. 2013;54:1554–1563. doi: 10.1167/iovs.12-10739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Chi, W. et al. Mitochondrial DNA oxidation induces imbalanced activity of NLRP3/NLRP6 inflammasomes by activation of caspase-8 and BRCC36 in dry eye. J. Autoimmun.80, 65–76 (2017). [DOI] [PMC free article] [PubMed]
- 261.Reins RY, Lema C, Courson J, Kunnen CME, Redfern RL. MyD88 Deficiency Protects Against Dry Eye-Induced Damage. Investig. Ophthalmol. Vis. Sci. 2018;59:2967–2976. doi: 10.1167/iovs.17-23397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Li Y, et al. Expression and Role of Nucleotide-Binding Oligomerization Domain 2 (NOD2) in the Ocular Surface of Murine Dry Eye. Investig. Ophthalmol. Vis. Sci. 2019;60:2641–2649. doi: 10.1167/iovs.19-27144. [DOI] [PubMed] [Google Scholar]
- 263.Kiripolsky J, McCabe LG, Gaile DP, Kramer JM. Myd88 is required for disease development in a primary Sjogren’s syndrome mouse model. J. Leukoc. Biol. 2017;102:1411–1420. doi: 10.1189/jlb.3A0717-311R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Alam J, de Paiva CS, Pflugfelder SC. Immune - Goblet cell interaction in the conjunctiva. Ocul. Surf. 2020;18:326–334. doi: 10.1016/j.jtos.2019.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Chen, Y. et al. IFN-gamma-Expressing Th17 Cells Are Required for Development of Severe Ocular Surface Autoimmunity. J. Immunol.10.4049/jimmunol.1602144 (2017). [DOI] [PMC free article] [PubMed]
- 266.Foulsham W, et al. Severe dry eye disease in aged mice is associated with an expanded memory Th17 cell response and higher frequencies of IFN-γ-expressing Th17 Cells. Investigative Ophthalmol. Vis. Sci. 2018;59:3286–3286. [Google Scholar]
- 267.You IC, et al. Macrophage Phenotype in the Ocular Surface of Experimental Murine Dry Eye Disease. Archivum Immunol. et. therapiae experimentalis. 2015;63:299–304. doi: 10.1007/s00005-015-0335-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Alam, J., de Paiva, C. S. & Pflugfelder, S. C. Desiccation Induced Conjunctival Monocyte Recruitment and Activation - Implications for Keratoconjunctivitis. Front. Immunol.12, 10.3389/fimmu.2021.701415 (2021). [DOI] [PMC free article] [PubMed]
- 269.de Paiva CS, et al. Differentially expressed gene pathways in the conjunctiva of Sjogren Syndrome Keratoconjunctivitis Sicca. Front. Immunol. 2021;12:702755. doi: 10.3389/fimmu.2021.702755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Gao J, et al. ICAM-1 expression predisposes ocular tissues to immune-based inflammation in dry eye patients and Sjogrens syndrome-like MRL/lpr mice. Exp. Eye Res. 2004;78:823–835. doi: 10.1016/j.exer.2003.10.024. [DOI] [PubMed] [Google Scholar]
- 271.Roescher N, et al. Effect of soluble ICAM-1 on a Sjögren’s syndrome-like phenotype in NOD mice is disease stage dependent. PloS one. 2011;6:e19962. doi: 10.1371/journal.pone.0019962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Emamian ES, et al. Peripheral blood gene expression profiling in Sjögren’s syndrome. Genes Immun. 2009;10:285–296. doi: 10.1038/gene.2009.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Peck AB, Nguyen CQ. Transcriptome analysis of the interferon-signature defining the autoimmune process of Sjogren’s syndrome. Scand. J. Immunol. 2012;76:237–245. doi: 10.1111/j.1365-3083.2012.02749.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Hall JC, et al. Precise probes of type II interferon activity define the origin of interferon signatures in target tissues in rheumatic diseases. Proc. Natl Acad. Sci. USA. 2012;109:17609–17614. doi: 10.1073/pnas.1209724109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Mavragani CP, Crow MK. Activation of the type I interferon pathway in primary Sjogren’s syndrome. J. Autoimmun. 2010;35:225–231. doi: 10.1016/j.jaut.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 276.Oyelakin A, et al. Transcriptomic and Network Analysis of Minor Salivary Glands of Patients With Primary Sjögren’s Syndrome. Front. Immunol. 2020;11:606268. doi: 10.3389/fimmu.2020.606268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Guzmán, M. et al. Transient tear hyperosmolarity disrupts the neuroimmune homeostasis of the ocular surface and facilitates dry eye onset. Immunology, 10.1111/imm.13243 (2020). [DOI] [PMC free article] [PubMed]
- 278.Gestermann N, et al. STAT4 is a confirmed genetic risk factor for Sjögren’s syndrome and could be involved in type 1 interferon pathway signaling. Genes Immun. 2010;11:432–438. doi: 10.1038/gene.2010.29. [DOI] [PubMed] [Google Scholar]
- 279.Aydemir YG, Kocakusak A. The evaluation of the Myxovirus Resistance 1 protein in serum and saliva to monitor disease activation in primary Sjögren’s syndrome. Clin. (Sao Paulo) 2019;74:e631–e631. doi: 10.6061/clinics/2019/e631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Schraml BU, et al. The AP-1 transcription factor Batf controls T(H)17 differentiation. Nature. 2009;460:405–409. doi: 10.1038/nature08114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Perez VL, Pflugfelder SC, Zhang S, Shojaei A, Haque R. Lifitegrast, a Novel Integrin Antagonist for Treatment of Dry Eye Disease. Ocul. Surf. 2016;14:207–215. doi: 10.1016/j.jtos.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 282.Coursey TG, Wassel RA, Quiambao AB, Farjo RA. Once-Daily Cyclosporine-A-MiDROPS for Treatment of Dry Eye Disease. Transl. Vis. Sci. Technol. 2018;7:24–24. doi: 10.1167/tvst.7.5.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.de Paiva CS, Pflugfelder SC, Ng SM, Akpek EK. Topical cyclosporine A therapy for dry eye syndrome. Cochrane database Syst. Rev. 2019;9:Cd010051. doi: 10.1002/14651858.CD010051.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Chighizola, C. B., Ong, V. H. & Meroni, P. L. The Use of Cyclosporine A in Rheumatology: a 2016 Comprehensive Review. Clin. Rev. Allerg. Immunol.10.1007/s12016-016-8582-3 (2016). [DOI] [PubMed]