Background:
Femoral nerve block is a widely accepted nerve block method with evident reduction in consumption of opioid painkiller and minimization of the duration of hospital stay but may cause weakness of quadriceps muscle strength. Adductor canal block is another nerve block technique that attracts the attention of scientific community nowadays because of its possible superiority over Femoral nerve block regarding mobility and muscle strength.
Methods:
This is a systematic review and meta-analysis of 33 studies, aiming to compare femoral nerve block with adductor canal block following total knee arthroplasty regarding pain control and mobilization.
Results:
Adductor canal block showed better preservation of quadriceps muscle strength (MD = 0.28, 95% CI [0.11, 0.46], P = .002), and better mobilization up to 2 days postoperatively. However, no significant difference was found between the 2 interventions regarding pain control (MD = 0.06, 95% CI [−0.06, 0.17], P = .33) or opioid consumption (SMD = 0.08, 95% CI [−0.06, 0.22], P = .28) up to 2 days postoperatively. The better mobilization results of adductor canal block did not translate into a significant difference in the risk of falls or patients’ satisfaction; however, adductor canal block patients had less mean length of hospital stay than the patients with femoral nerve block.
Conclusion:
Both femoral nerve block and adductor canal block provide similar results regarding pain control and opioid consumption, however adductor canal block provides better preservation of quadriceps strength and mobilization, giving it more advantage over femoral nerve block.
Keywords: adductor canal block, femoral nerve block, postoperative analgesia, total knee arthroplasty
1. Introduction
Total knee arthroplasty (TKA) is a popular and effective surgical intervention for the treatment of knee osteoarthritis.[1] The number of TKA operations has prominently increased over the last decade to be the most frequent surgical operation done in the developed world.[2] However, TKA is known to cause moderate to severe postoperative pain that delays the recovery process.[3] The pain following TKA increases the patients’ risk to various postoperative complications including infections, loosening of the joint, reflex sympathetic dystrophy and immobility-related complications as deep venous thrombosis (DVT).[3,4]
Peripheral nerve blocks (PNBs) are analgesic techniques used after TKA primarily for pain control. In addition to pain reduction, nerve blocks significantly enhance recovery and reduce both hospital length of stay (LOS) and risk of re-admission.[5] Femoral nerve block (FNB) is a widely accepted nerve block technique after TKA with high success rates in reduction of opioid consumption and minimization of the length of hospital stay.[3,6] However, (FNB) may cause reduction of the quadriceps muscle strength impairing postoperative ambulation which increases the patients’ risk of falls after the surgery.[7,8] Adductor canal block (ACB) is another nerve block technique that attracts the attention of the scientific community nowadays because of its possible superiority over (FNB).[9] Several studies have documented that (ACB) is better than (FNB) regarding postoperative quadriceps muscle strength preservation, postoperative ambulation and functional recovery without any alteration of pain control.[10–13] But on the contrary, 2 recent studies concluded that there is no statistically significant difference between ACB and FNB regarding the analgesic effect, quadriceps strength or functional recovery postoperatively.[14,15]
This systematic review aims to investigate the clinical efficacy of (ACB) compared to (FNB) and draw conclusions on whether or not ACB is superior to FNB regarding functional recovery without alteration of postoperative pain control following TKA.
2. Methods and Materials
We conducted this systematic review according to the Cochrane handbook for systematic reviews of interventions.[16] Also, we reported this study using the preferred reporting items for systematic review and meta-analysis (PRISMA statement).[17] This current review tests the hypothesis that patients with ACB will have better postoperative functional recovery, and muscle strength with–at least- same level of pain control as FNB. Ethical approval was not necessary for this study; because all data were obtained from previous published studies.
2.1. Search strategy
We searched PubMed, SCOPUS, web of science and Cochrane databases by using the keywords (Adductor canal block OR motor sparing knee blocks) AND (Femoral nerve block) AND (total knee arthroplasty OR total knee replacement) from conception till March 2021.
2.2. Eligibility criteria and study selection
We included only original papers (Randomized controlled trials or Cohort studies) which compare Adductor canal block with femoral nerve block in total knee arthroplasty patients and excluded any review, case report, systemic review, meta-analysis, or animal studies as well as studies with data that cannot be extracted. Reviewers independently screened the retrieved citations in 2 steps; title and abstract screening followed by full text screening.
2.3. Data extraction
Authors extracted the following data from the included studies:
Baseline characters of the studies’ participants and summary of the included studies,
Study outcomes: pain control measured by visual analog scale (VAS) at rest and at motion—Quadriceps muscle strength (knee extensors strength) by Isometric measurement or manual muscle testing (MMT)–Mobilization after the operation measured by timed up and Go test and ambulation distance—the amount of Opioid consumption - length of hospital stay—Risk of falls - patient satisfaction.
2.4. Quality Assessment
We assessed the Quality of included trials using Cochrane Risk of Bias tool provided in Cochrane handbook for systematic reviews of interventions (version 5.1.0).[16] The domains included were: (1) Random sequence generation (selection bias). (2) Allocation concealment (selection bias). (3) Blinding of participants and personnel (performance bias). (4) Outcomes assessment (detection bias). (5) Incomplete outcome data (attrition bias). (6) Other potential sources of bias. The reviewers judged the domains as: “ low risk,” “high risk,” or “ unclear”. The quality assessment table used was provided in (part 2, chapter 2.5) of the same book.[16] The quality of the included cohort studies was assessed by the quality assessment tool of the National Heart, Lung, and Blood Institute (NHLBI).[18] We used the tool for observational cohort studies and cross-sectional studies. This tool is composed of 14 questions to assess the risk of bias and confounders. These questions were answered by “yes,” “no,” “cannot determine, ” “not applicable,” or “not reported” then each study was given a score to guide the overall rating of the quality as “good,” “fair,” or “poor” quality.
2.5. Data analysis
In the analysis, we presented the dichotomous data as risk ratio (RR) and continuous data as mean difference (MD) or standard mean difference (SMD), in a random-effects meta-analysis model using the inverse-variance method for continuous data and Mantel-Haenzel method for dichotomous data. Missing SD was calculated from standard error or 95% confidence interval (CI) according to Altman.[19] In this analysis, we used review manager 5.3 for windows.
2.6. Assessment of heterogeneity
The heterogeneity of the pooled data was assessed by I square and chi-square tests presented in the forest plots. The chi-square test measures the presence of significant heterogeneity. And the I-square test quantifies the size of the heterogeneity in the pooled data. Interpretation of the results followed the recommendations of the Cochrane handbook for systematic reviews and meta-analysis. The chi-square test was considered significant with a P value less than (.1) and the I-square test was interpreted as follows: ((0–40 %): might not be important; (30–60%): may represent moderate heterogeneity; (50–90 %): may represent substantial heterogeneity).
3. Results
3.1. Literature search
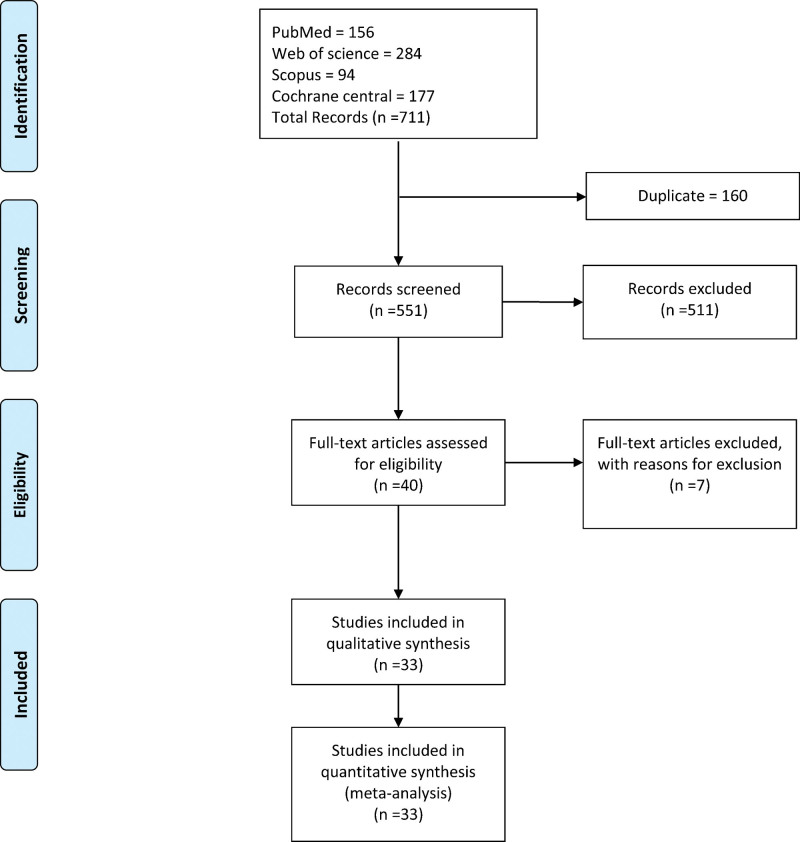
The literature search retrieved 711 citations. After title and abstract screening, 40 articles were selected. We evaluated the full text of the selected studies. Finally, 33 studies were eligible to be included in our review and quantitative analysis (PRISMA flow diagram; Fig. 1).
Figure 1.
PRISMA flow chart.
3.2. Characteristics of the included studies and quality assessment
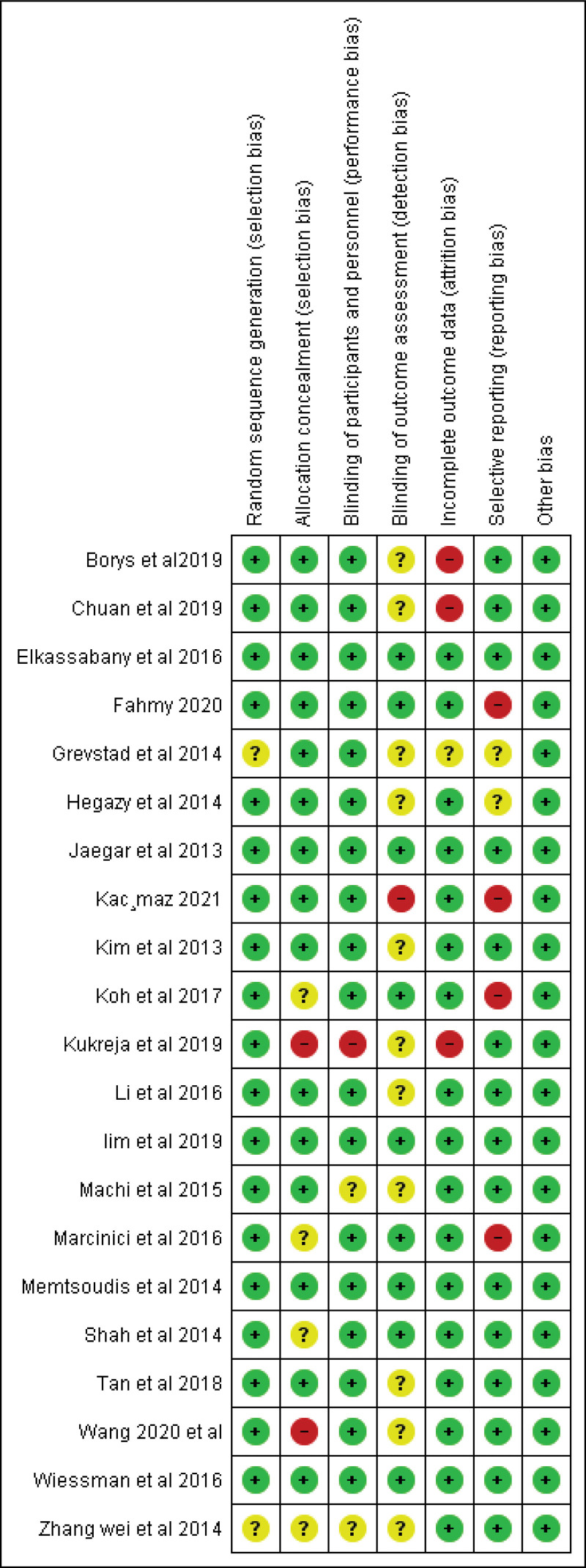
The baseline characteristics of the studies’ participants are shown in (Table 1) and the summary of all the included studies is present in (Supplementary table 1, http://links.lww.com/MD/G1000). A summary of the quality assessment for the included randomized trials is shown in (Fig. 2), All the included randomized controlled trials showed moderate to high quality. Eleven cohort studies[24,25,27,28,34–38,40,41] were fair in quality according to NIH (national institute of health) quality assessment tool for Observational Cohort. One study[42] had good quality. For more details and answers to all assessment questions in each study, see Supplementary table 2, http://links.lww.com/MD/H2.
Table 1.
Baseline characters of the studies’ participants.
| Study ID | Groups | No of patients | Age (yr) | Male (%) | Body mass index | Duration of surgery (min) |
|---|---|---|---|---|---|---|
| Fahmy et al 2020.[20] | ACB | 40 | 59.5 ± 4.6 | 14 | 24.4 ± 4.6 | 100.1 ± 2.9 |
| FNB | 40 | 60.1 ± 1.1 | 13 | 23.5 ± 2.9 | 100.4 ± 3.1 | |
| Kac¸maz et al 2021.[21] | ACB | 43 | 64.4 ± 1.7 | 20 | – | – |
| FNB | 43 | 66.0 ± 1.4 | 25 | – | – | |
| Jaegar et al 2013[22] | ACB | 23 | 70 ± 8 | 21.7 | – | 82 ± 20 |
| FNB | 27 | 66 ± 9 | 51.8 | – | 75 ± 15 | |
| Kim et al 2013[23] | ACB | 46 | 68 ± 9.4 | 47.8 | 29.9 ± 6.4 | – |
| FNB | 47 | 67.6 ± 11.3 | 38.3 | 30.3 ± 5.8 | – | |
| Elkassabany et al 2016[11] | ACB | 31 | 63 ± 8 | 29 | 31 ± 5 | – |
| FNB | 31 | 65 ± 8 | 38.7 | 32 ± 6 | – | |
| Tan et al 2018[13] | ACB | 100 | 64.2 ± 7.5 | 44 | 26.12 ± 3.6 | 71.5 ± 8.1 |
| FNB | 100 | 63.5 ± 6.7 | 42 | 25.67 ± 2.88 | 72.6 ± 8.1 | |
| Ludwigson et al 2015[24] | ACB | 148 | 64.09 ± 112 | 45.95 | 31.29 ± 75 | – |
| FNB | 149 | 64.74 ± 112 | 44..97 | 31.48 ± 71 | – | |
| Seo et al 2017[25] | ACB | 19 | 72.2 ± 5.3 | 21 | – | – |
| FNB | 24 | 74.3 ± 6.81 | 16.67 | – | – | |
| Weissman et al 2016[26] | ACB | 21 | 86.67 ± 11 | 42.85 | 29 ± 5.9 | 60 ± 18.5 |
| FNB | 21 | 67.3 ± 8.89 | 43.85 | 31.3 ± 5.9 | 56.67 ± 11.1 | |
| Klement et al 2018[27] | ACB | 118 | 65.5 ± 9.3 | 43.2 | – | – |
| FNB | 146 | 66.8 ± 9.4 | 43.8 | – | – | |
| Mudumbai et al 2013[28] | ACB | 66 | 65 ± 9 | 92.4 | 33 ± 6 | 105 ± 18 |
| FNB | 102 | 66 ± 10 | 96 | 33 ± 7 | 105 ± 27 | |
| Machi et al 2015[29] | ACB | 39 | 67 ± 8 | 41 | 30 ± 5 | 113 ± 32 |
| FNB | 41 | 66 ± 7 | 34 | 29 ± 5 | 115 ± 21 | |
| Koh et al 2017[30] | ACB | 50 | 64.3 ± 17.7 | – | 27.2 ± 10.14 | – |
| FNB | 50 | – | ||||
| Grevstad et al 2014[31] | ACB | 25 | 65.33 ± 28.88 | 28 | – | 71.6 ± 23.7 |
| FNB | 25 | 63.33 ± 31.11 | 32 | – | 81 ± 45.92 | |
| Shah et al 2014[32] | ACB | 48 | 68.31 ± 7.56 | 27.1 | 29.54 ± 5.46 | 68.85 ± 4.57 |
| FNB | 50 | 65.94 ± 7.22 | 28 | 30.52 ± 5.3 | 68.30 ± 4.42 | |
| Marcinici et al 2016[12] | ACB | 49 | 67 ± 8 | 39 | 31.5 ± 6 | – |
| FNB | 49 | 67 ± 8 | 37 | 31.7 ± 5.4 | – | |
| Lim et al 2019[15] | ACB | 15 | 63 ± 7 | 33 | 26.6 ± 4.3 | – |
| FNB | 15 | 65 ± 8 | 47 | 28.0 ± 3.5 | – | |
| Hegazy et al 2014[33] | ACB | 53 | 62 ± 12 | 47.2 | 31.3 ± 2.7 | – |
| FNB | 54 | 63 ± 11 | 48.1 | 31.1 ± 2.8 | – | |
| Patterson et al 2015[34] | ACB | 35 | 65.7 ± 8.9 | 31 | 35.3 ± 5.92 | – |
| FNB | 41 | 65 ± 13.3 | 27 | 34.3 ± 9.6 | – | |
| Mudumbai et al 2015[35] | ACB | 48 | 66.7 ± 13.3 | 100 | 33 ± 11.1 | – |
| FNB | 46 | 67.3 ± 20 | 91 | 34.3 ± 12.6 | – | |
| Thacher et al 2017[36] | ACB | 150 | 68.4 ± 31.1 | 21 | 33.8 ± 24.6 | – |
| FNB | 129 | 68.8 ± 28.9 | 21 | 35.1 ± 28.4 | – | |
| Rassmussen et al 2014[37] | ACB | 23 | 63.3 ± 11.9 | 20 | 34 ± 16.3 | – |
| FNB | 22 | 62 ± 11.9 | 20 | 32.7 ± 10.4 | – | |
| Thobhani et al 2017[38] | ACB | 22 | 64.3 ± 7.4 | 36.4 | 35.7 ± 9.6 | – |
| FNB | 23 | 68.7 ± 6.7 | 39.1 | 33.3 ± 7.4 | – | |
| Memtsoudis et al 2014[39] | ACB | 30 | – | – | – | – |
| FNB | 29 | – | – | – | – | |
| Brennan et al 2018[40] | ACB | 141 | 73.21 + 0.55 | – | 30.58 + 0.46 | – |
| FNB | 104 | 72.28 + 0.78 | – | 31.47 + 0.57 | – | |
| Bolarinwa et al 2018[41] | ACB | 791 | – | – | – | – |
| FNB | 834 | – | – | – | – | |
| Ardon et al 2015[42] | ACB | 45 | 64.86 | 31.1 | – | 93.31 |
| FNB | 45 | 67.71 | 31.1 | – | 90.29 | |
| Li et al 2016[43] | ACB | 24 | 62.3 ± 6.5 | 46 | – | 77.6 ± 8.2 |
| FNB | 27 | 61.4 ± 6.8 | 48 | – | 76.6 ± 8.4 | |
| Zhang wei et al 2014[44] | ACB | 30 | 63.7 ± 5.8 | 25 | – | 98.4 ± 10.3 |
| FNB | 30 | 61.9 ± 6.7 | 36 | – | 97.1 ± 8.2 | |
| Kukreja et al 2019[45] | ACB | 45 | 63.4 | 46.5 | 31.4 | – |
| FNB | 45 | 65.4 | 46.3 | 32.3 | – | |
| Borys et al 2019[10] | ACB | 43 | 67.33 ± 2.59 | 18.6 | 31.56 ± 1.85 | – |
| FNB | 42 | 68.8 ± 2.37 | 19 | 30.8 ± 1.92 | – | |
| Chuan et al 2019[14] | ACB | 75 | 66.66 ± 10.37 | 53 | 32.3 ± 4.37 | 91 ± 18.51 |
| FNB | 76 | 68 ± 7.4 | 49 | 33.46 ± 7.03 | 96 ± 31.11 | |
| Wang et al 2020[46] | FTB | 31 | 61.77 ± 3.66 | 50 | – | 87.77 ± 6.55 |
| ACB | 32 | 61.67 ± 4.49 | 53 | – | 84.20 ± 6.10 |
ACB = adductor canal block, FNB = femoral nerve block, FTB = femoral triangle block.
Figure 2.
Risk of bias summary.
3.3. Main outcomes of the study
A. Pain control measured by pain scores (VAS):
i. Pain scores at 6-8 hours at rest
The pooled effect estimate showed no statistically significant difference between the 2 techniques at 6-8 hours (MD = -0.06, 95% CI [-0.45, 0.33], P = .77). (Supplementary figure 1, http://links.lww.com/MD/H3) Pooled results were heterogeneous (P < .00001, I² = 87%) and the detected heterogeneity could not be solved.
ii. Pain scores at 6-8 hours at motion
The overall effect showed no statistically significant difference between the 2 interventions at motion (MD = -0.08, 95% CI [-0.47, 0.31], P = .70). (Supplementary figure 1, http://links.lww.com/MD/H3) Pooled results were heterogeneous (P < .0002, I² = 80%) and the detected heterogeneity was best resolved after excluding Wang et al (P = .78, I² = 0%) and the effect estimate remained nonsignificant (MD = 0.14, 95% CI [-0.03, 0.32], P < .11).
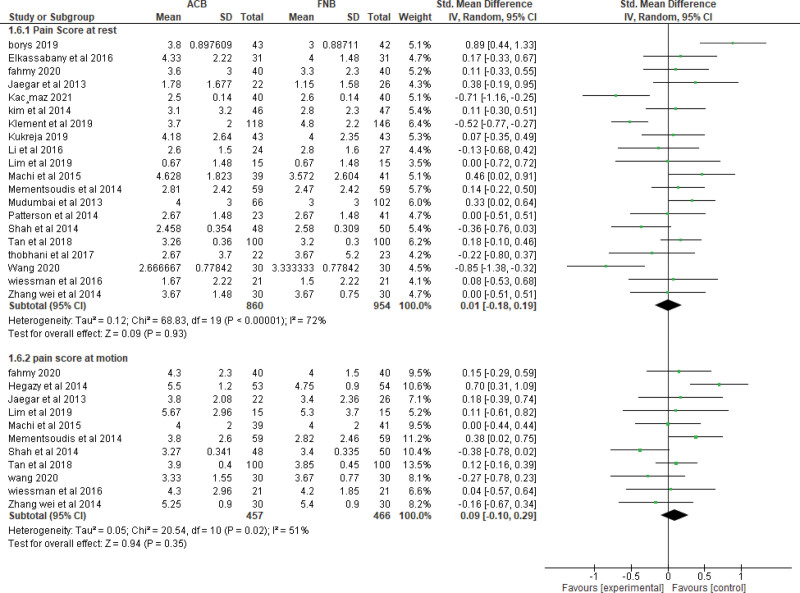
iii. Pain scores at 24 hours at rest.
The pooled effect estimate showed no statistically significant difference between the 2 techniques at 24 hours postoperatively (MD = 0.01, 95% CI [-0.18, 0.19], P = .93). (Fig. 3). The pooled results were heterogeneous (P < .00001, I² = 72%), and heterogeneity could not be solved.
iv. Pain score at 24 hours at motion.
The pooled studies showed no significant difference between the 2 interventions at motion (MD = 0.09, 95% CI [−0.10, 0.29], P = .35). The pooled results were heterogeneous (P = .02, I² = 51%) (Fig. 3). The detected heterogeneity could be solved by excluding Hegazy et al (P = .30, I² = 15%) and the effect estimate remained nonsignificant (MD = 0.03, 95% CI [−0.12, 0.18], P = .69).
v. Pain score at 48 hours at rest.
The pooled effect estimate showed no statistically significant difference between adductor canal and femoral nerve block (MD = 0.06, 95% CI [−0.06, 0.17], P = .33). The studies were homogenous (P = .90, I² = 0%) (Supplementary figure 2, http://links.lww.com/MD/H4).
vi. Pain score at 48 hours at motion.
The pooled studies showed no statistically significant difference between adductor canal and femoral nerve block (MD = 0.00, 95% CI [-0.13, 0.13], P = .99) (Supplementary figure 2, http://links.lww.com/MD/H4). The studies were heterogenous (P = .02, I² = 54%) and the detected heterogeneity was best solved by excluding Wang et al (P = .26, I² = 20%). Results remained nonsignificant (P = .42).
B. Quadriceps muscle strength:
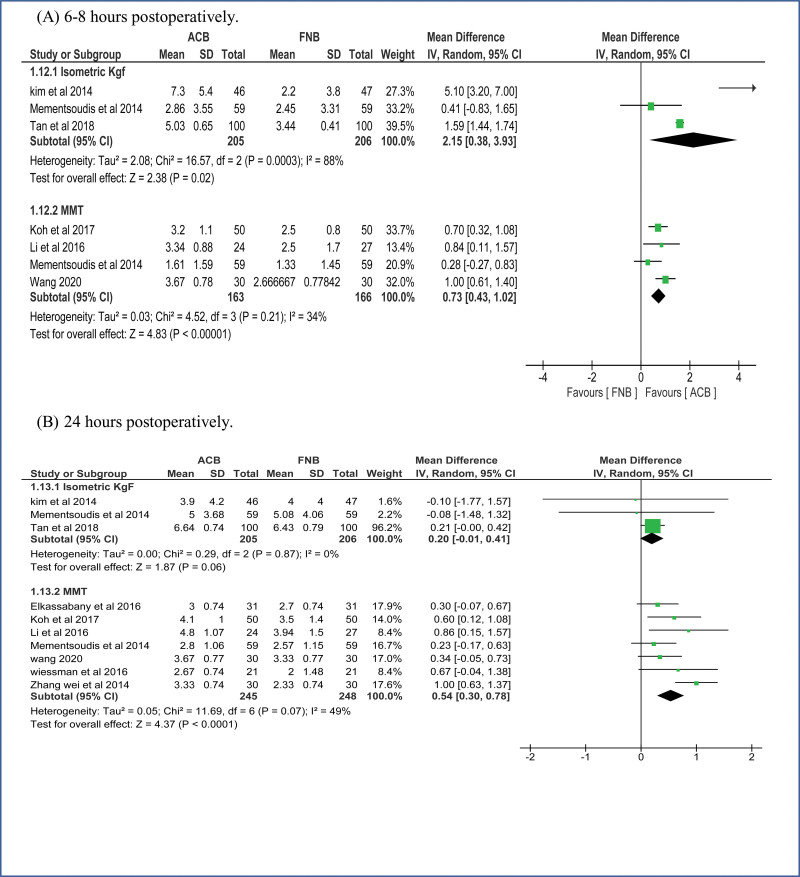
i. Quadriceps muscle strength 6–8 hours postoperatively.
Isometric measurement: ACB showed higher values of muscle strength over FNB on pooling means from included studies (MD = 2.15, 95% CI [0.38, 3.93], P = .02) (Fig. 4A). The pooled studies were heterogeneous (P = .0003, I² = 88%).
MMT: Pooled results showed that the ACB group has higher values of muscle strength (MD = 0.73, 95% CI [0.43, 1.02], P < .00001) (Fig. 4A). The pooled studies were homogenous (P = .21, I² = 34%).
ii. Quadriceps muscle strength 1 day postoperatively.
Isometric measurement: pooled studies showed no statistically significant difference between the 2 interventions (MD = 0.20, 95% CI [-0.01, 0.41], P = .06) (Fig. 4B). The pooled studies were homogeneous (P = .87, I² = 0%).
MMT: Pooled results showed that the ACB group has higher mean values of muscle strength (MD = 0.54, 95% CI [0.30, 0.78], P < .0001) (Fig. 4B). The pooled studies were heterogonous (P = .07, I² = 49%).
iii. Quadriceps muscle strength 2 days postoperatively.
Isometric measurement: pooled studies showed no statistically significant difference between the 2 interventions (MD = 0.05, 95% CI [-0.18, 0.28], P = .66) (Supplementary figure 3, http://links.lww.com/MD/H5). The pooled studies were homogeneous (P = .39, I² = 0%).
MMT: Pooled results showed that the ACB group has significantly higher mean values of muscle strength (MD = 0.28, 95% CI [0.11, 0.46], P = .002) (Supplementary figure 3, http://links.lww.com/MD/H5). The pooled studies were homogenous (P = .12, I² = 45%).
C. Mobilization after the operation
i. Mobilization by ambulation and walking distance at 24 hours.
The pooled mean difference showed that ACB significantly increases walking distance at 24 hours compared to femoral nerve block (MD = 46.32, 95% CI [13.77, 78.87], P = .005) (Supplementary figure 4, http://links.lww.com/MD/H6). The pooled studies were heterogeneous (P < .00001, I² = 99%) and the detected heterogeneity could not be solved by excluding a study.
ii. Mobilization by ambulation and walking distance at 48 hours.
The pooled mean difference showed that ACB significantly increases the walking distance at 48 hours compared to FNB (MD = 17.97, 95% CI [3.08, 32.86], P = .02). The pooled studies were heterogeneous (P = .002, I² = 68%) (Supplementary figure 4, http://links.lww.com/MD/H6).
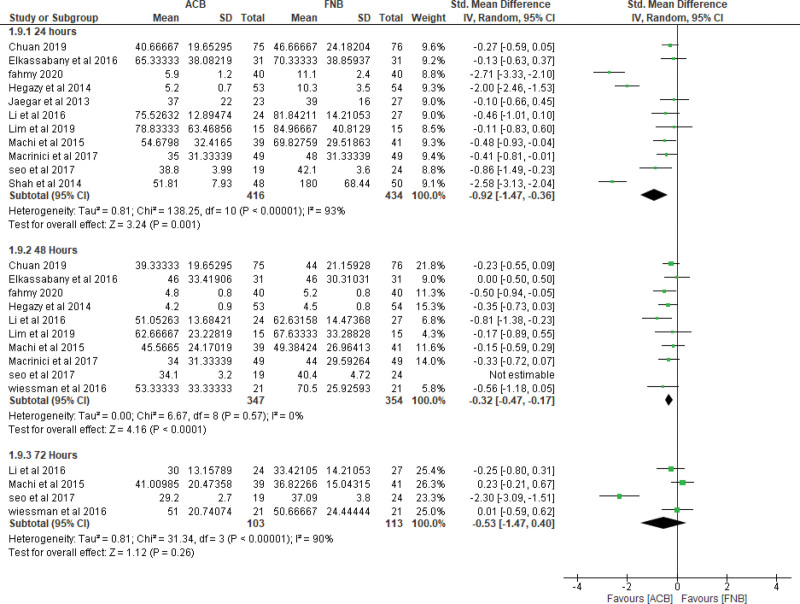
iii. Mobilization by timed up and GO test (TUG) at 24 hours.
The pooled mean difference showed that ACB technique significantly decreases the test duration at 24 hours compared to FNB (SMD = −0.92, 95% CI [−1.47, −0.36], P = .001) (Fig. 5). The pooled studies were heterogeneous (P < .00001, I² = 93%). The detected heterogeneity could not be solved by excluding single study.
iv. Mobilization by timed up and GO test (TUG) at 48 hours.
The pooled mean difference showed that ACB technique significantly decreases the test duration at 48 hours compared to FNB (SMD = −0.41, 95% CI [−0.62, −0.20], P = .003) (Fig. 5). The pooled studies were heterogeneous (P = .04, I² = 49%). The detected heterogeneity could be solved by excluding Seo et al (P = .57, I² = 0%) and the effect estimate would remain significant (P = .0002).
v. Mobilization by timed up and GO test (TUG) at 72 hours.
The pooled mean difference showed no statistically significant difference between the 2 interventions at 72 hours (SMD = -0.53, 95% CI [-1.47, 0.40], P = .26) (Fig. 5). The pooled studies were heterogeneous (P < .00001, I² = 90%). The detected heterogeneity could be solved by excluding Seo et al (I² = 0%) and the effect estimate would remain nonsignificant (P = .80)
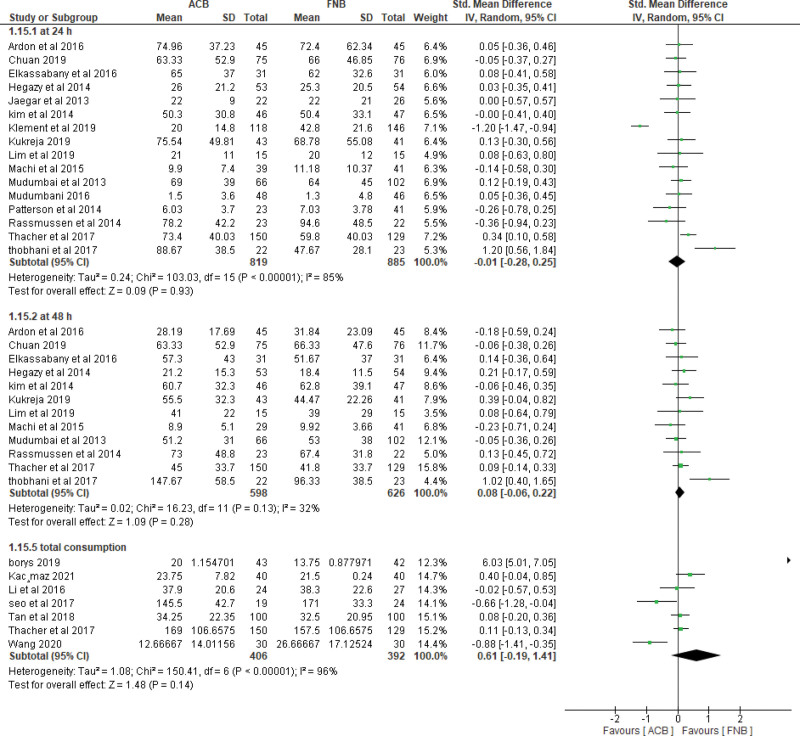
D. Opioid consumption
i. At 24 Hours.
The pooled effect estimate showed no statistically significant difference between the 2 intervention groups (SMD = -0.01, 95% CI [-0.28, 0.25], P = .93) (Fig. 6). Pooled results were heterogeneous (P < .00001, I² = 85%) and the detected heterogeneity could be best solved by excluding klement et al 2019 (P = .08, I² = 37%). The pooled results would remain nonsignificant.
ii. At 48 Hours.
The pooled effect estimate showed no statistically significant difference between the 2 intervention groups (SMD = 0.08, 95% CI [-0.06, 0.22], P = .28) (Fig. 6). Pooled results were homogenous (P = .13, I² = 32%).
iii. Total opioid consumption.
Results showed no statistically significant difference between the 2 intervention groups (SMD = 0.61, 95% CI [-0.19, 1.41], P = .14) (Fig. 6). Pooled results were heterogenous (P < .00001, I² = 96%) and it could not be solved.
E. Recovery After the operation:
i. Length of hospital stay.
Pooled results showed that ACB was associated with significantly lower period of hospital stay when compared to FNB (MD = −0.25, 95% CI [-0.48, −0.02], P = .04) (Supplementary figure 5, http://links.lww.com/MD/H7). Pooled results were heterogeneous (P < .00001, I² = 92%) and the detected heterogeneity could not be solved by excluding any study.
ii. Risk of falls
The pooled results showed no statistically significant difference between ACB and FNB regarding the risk of postoperative falls (MD = 1.09, 95% CI [0.77, 1.53], P = .64) (Supplementary figure 6, http://links.lww.com/MD/H8). Pooled results were heterogeneous (P = .03, I² = 67%) and the detected heterogeneity could be solved by excluding Bolarina et al (I² = 18%). And the effect estimate would remain nonsignificant.
iii. Mean patient satisfaction
The pooled results showed no statistically significant difference between ACB and FNB (MD = 0.08, 95% CI [-0.06, 0.22], P = .28) regarding the patients’ satisfaction (Supplementary figure 7, http://links.lww.com/MD/H9). Pooled results were homogeneous (P = .21, I² = 27%).
Figure 3.
Pain Score at 24 hours.
Figure 4.
Quadriceps muscle strength: (A) at 6–8 hours postoperatively. (B) at 1 day postoperatively.
Figure 5.
Mobilization by timed up and GO test TUG.
Figure 6.
Opioid consumption.
4. Discussion
The pooled results of the studies included in this meta-analysis showed that both ACB and FNB exhibit equal pain control and opioid consumption after 24 and 48 hours of total knee arthroplasty operation both in rest and in motion; however, ACB showed superiority to FNB regarding quadriceps muscle strength up to 2 days postoperation specially when assessing the muscle strength using manual muscle testing. ACB also showed better mobilization results than FNB up to 2 days postoperation but equal results after 3 days, the better mobilization results did not translate into any difference in the risk of falls or patients’ satisfaction about the procedure.
Total Knee arthroplasty is a successful surgical procedure with excellent long-term survival rates.[47–49] The main aim of patients undergoing TKA is to alleviate pain and improve their functional mobility, thus no leniency is allowed in handling such aspect of the patient complaint.[50] Besides suffering and discomfort, severe unrelieved postoperative pain delays rehabilitation and lengthens the hospital-stay period, and may lead to persistent postsurgical pain.[51] Previous studies reported poor management and a higher percentage of patients with severe pain after TKA procedure.[52,53] Almost 44–57% of the patients who have undergone the surgery are woken up by pain during the first 3 days after TKA.[53] The developed sleep deprivation reduces pain threshold generating a vicious cycle and causing dissatisfaction in about 19% of the patients undergoing TKA.[54,55] Therefore, sleep disturbance and persistent postoperative pain appear to be crucial predictors of persistent functional limitations at 1 and 3 months after TKA.[54,56]
Our nonsuperiority results between both modalities of anesthesia in TKA in terms of pain control and opioid consumption are in line with the results of many other studies.[14,15,57,58] A recent meta-analysis showed an equivalent effect of ACB and FNB in patients with TKA.[59] Lim et al found that the perioperative morphine consumption and pain scores at 1, 24, and 48 hours postoperatively were similar between the groups.[15] Likewise, both Kim et al and Jaeger et al showed that pain scores and opioid consumption were similar in both ACB and FNB groups.[22,23] Moreover, the superiority of ACB over FNB in terms of mobility and muscle strength is also consistent with the results reported in previous trials.[11,31,60] ACB is proposed to have a quadriceps-sparing effect, as it blocks distally to where most of the motor fibers of the femoral nerve branch off.[61] Both Jaeger et al and Kwofie et al showed preservation of quadriceps strength with ACB as opposed to FNB.[8,62] Jaeger et al reported quadriceps strength of 52% of the baseline value in patients with continuous ACB and 18% only in patients with continuous FNB.[22]
Regarding the risk of falls, we found no statistical difference between both interventions in the meta-analysis model. nevertheless, Kwofie et al (using the Berg Balance Scale) demonstrated a higher incidence of quadriceps muscle weakness and risk of falls after administration of FNB.[62] Elkassabany et al used the Tinetti Scale for gait and balance to report a higher incidence of falls in the FNB group after 48 hours.[11] The weakness of quadriceps with FNB was also demonstrated by Thacher et al who reported a statistically significant difference in episodes of near fall (knee-buckling) in about 13% of patients with FNB vs 2% with ACB during physiotherapy.[36]
Despite all the aforementioned advantages of the 2 peripheral nerve blockade techniques being investigated in this study, various limitations and disadvantages may exist. Patients undergoing peripheral nerve blockades carry the risk for a possible nerve injury during the procedure, in addition to possible local and systemic toxicities from the large volume of local anesthetic used in the procedure.[63,64] Despite its advantage in preservation of muscle strength postoperatively, ACB carries an increased risk for neuropathy, myositis, and infection due to perioperative injection of local anesthetic in the adductor canal close to the operative site, in addition to ischemia resulting from possible tourniquet compression.[65] Another major challenge in the use of ultra-sound guided peripheral nerve blockade techniques, is the requirement of a highly skilled physician to perform the procedure specifically in cases of smaller and deeper nerves, or in individuals with higher body mass index, edematous tissues or subcutaneous emphysema, which are known conditions that limit the visualization by the ultra-sound and consequently make the nerve blockade difficult.[63,64]
The knowledge from this study is a statistical confirmation of the previously reported literature that points out the superiority of ACB over FNB in preservation of muscle strength postoperatively, with both the techniques being equally effective in pain control. Physicians can use this piece of knowledge to make evidence based decisions on which peripheral nerve block modality to use with different types of patients undergoing TKA, bearing in mind that pain is a complex multi-dimensional perception that is influenced by several factors above and beyond the pain control method being applied on the patient. These factors include but are not limited to the patient gender, age, length of hospital stay in addition to the familial, psychological, social and cultural variables.[66,67]
5. Strengths and Limitations
The main strength point of the current systematic review is the high number of included studies in the analysis compared to previous systematic reviews.[59,68] The available data from the included studies allowed for assessment of different outcomes at various time points enriching the analysis.
However, Heterogeneity of the pooled data in different outcomes is a major limitation to this study; this heterogeneity may be explained by the variations in ACB protocols (continuous infusion or single shot) and the different types of anesthesia used in the TKA operation (general or spinal) among the included studies. Variations among patients in pain tolerance may be another source of heterogeneity.[69]
6. Conclusion
ACB has the advantage of preserving the quadriceps muscle strength and better mobilization after the operation over the FNB, but both the interventions are equal regarding pain control and opioid consumption.
Author contributions
AA: idea conception, search strategy, screening and extraction conflict resolution and study supervision. EAH, MMM, HAA, EAI, MAH: Screening, data extraction, and writing. AKE, YHA, AAA, ASA: Statistical analysis, manuscript writing and study revision. All authors reviewed the manuscript and approved it for publication.
Supplementary Material
Abbreviations:
- ACB =
- adductor canal block
- CI =
- confidence interval
- DVT =
- deep venous thrombosis
- FNB =
- femoral nerve block
- LOS =
- length of stay
- MD
- : mean difference
- MMT =
- manual muscle testing
- NHLBI =
- National Heart, Lung, and Blood Institute
- NIH =
- National Institute of Health
- PNBs =
- peripheral nerve blocks
- PRISMA =
- preferred reporting items for systematic review and meta-analysis
- RR =
- risk ratio
- SMD =
- standard mean difference
- TKA =
- total knee arthroplasty
- TUG =
- timed up and GO test
- VAS =
- visual analog scale.
How to cite this article: Hasabo EA, Assar A, Mahmoud MM, Abdalrahman HA, Ibrahim EA, Hasanin MA, Emam AK, Abdelqadir YH, Abdelazim AA, Ali AS. Adductor canal block versus femoral nerve block for pain control after total knee arthroplasty: a systematic review and Meta-analysis. Medicine 2022;101:34(e30110).
Supplemental Digital Content is available for this article.
Ethics approval and consent to participate: nonapplicable.
Consent for publication: nonapplicable.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interest: The authors declare that they have no competing interests.
Funding: This study received no funding.
References
- [1].Gao F, Ma J, Sun W, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty. Clin J Pain. 2017;33:356–68. [DOI] [PubMed] [Google Scholar]
- [2].National Center for Health Statistics. Health, United States, 2016: With Chartbook on Long-term Trends in Health. Hyattsville, MD: US Government Printing Office; 2017. [PubMed] [Google Scholar]
- [3].Grosu I, Lavand’homme P, Thienpont E. Pain after knee arthroplasty: an unresolved issue. Knee Surg. Sports Traumatol. Arthrosc. 2013;22:1744–58. [DOI] [PubMed] [Google Scholar]
- [4].Czurda T, Fennema P, Baumgartner M, et al. The association between component malalignment and post-operative pain following navigation-assisted total knee arthroplasty: results of a cohort/nested case–control study. Knee Surg. Sports Traumatol. Arthrosc. 2009;18:863–9. [DOI] [PubMed] [Google Scholar]
- [5].Kapoor M, Karkhur Y, Mahajan R, et al. A comparative analysis of femoral nerve block with adductor canal block following total knee arthroplasty: a systematic literature review. J Anaesthesiol Clin Pharmacol. 2018;34:433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Chelly JE, Greger J, Gebhard R, et al. Continuous femoral blocks improve recovery and outcome of patients undergoing total knee arthroplasty. J Arthroplasty. 2001;16:436–45. [DOI] [PubMed] [Google Scholar]
- [7].Sharma S, Iorio R, Specht LM, et al. Complications of femoral nerve block for total knee arthroplasty. Clin Orthop Relat Res. 2010;468:135–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Jæger P, Nielsen ZJK, Henningsen MH, et al. Adductor canal block versus femoral nerve block and quadriceps strength. Anesthesiology. 2013;118:409–15. [DOI] [PubMed] [Google Scholar]
- [9].Hussain N, Ferreri TG, Prusick PJ, et al. Adductor canal block versus femoral canal block for total knee arthroplasty. Reg Anesth Pain Med. 2016;41:314–20. [DOI] [PubMed] [Google Scholar]
- [10].Borys M, Domagała M, Wencław K, et al. Continuous femoral nerve block is more effective than continuous adductor canal block for treating pain after total knee arthroplasty. Medicine. 2019;98:e17358e17358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Elkassabany NM, Antosh S, Ahmed M, et al. The risk of falls after total knee arthroplasty with the use of a femoral nerve block versus an adductor canal block. Anesth Analg. 2016;122:1696–703. [DOI] [PubMed] [Google Scholar]
- [12].Macrinici GI, Murphy C, Christman L, et al. Prospective, double-blind, randomized study to evaluate single-injection adductor canal nerve block versus femoral nerve block. Reg Anesth Pain Med. 2017;42:10–6. [DOI] [PubMed] [Google Scholar]
- [13].Tan Z, Kang P, Pei F, et al. A comparison of adductor canal block and femoral nerve block after total-knee arthroplasty regarding analgesic effect, effectiveness of early rehabilitation, and lateral knee pain relief in the early stage. Medicine. 2018;97:e13391e13391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Chuan A, Lansdown A, Brick KL, et al. Adductor canal versus femoral triangle anatomical locations for continuous catheter analgesia after total knee arthroplasty: a multicentre randomised controlled study. Br J Anaesth. 2019;123:360–7. [DOI] [PubMed] [Google Scholar]
- [15].Lim YC, Quek HYK, Phoo WHJ, et al. A randomised controlled trial comparing adductor canal block and femoral nerve block for knee arthroplasty. Singapore Med J. 2019;60:145–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. Chichester, UK: John Wiley & Sons; 2019. [Google Scholar]
- [17].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Study Quality Assessment Tools | NHLBI, NIH [Internet]. Nhlbi.nih.gov. 2022 [cited 13 December 2021]. Available at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- [19].Altman DG, Bland JM. Standard deviations and standard errors. BMJ. 2005;331:903903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Fahmy M. Early postoperative quadriceps power, motion range, and analgesia evaluation following knee replacement after femoral or adductor block: randomized controlled study. J Musculoskeletal Res. 2020;23:20500062050006. [Google Scholar]
- [21].Kaçmaz M, Turhan ZY. The effect of femoral nerve block and adductor canal block methods on patient satisfaction in unilateral knee arthroplasty: randomized non-inferiority trial. Geriatr Orthop Surg Rehabil. 2021;12:215145932199663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Jæger P, Zaric D, Fomsgaard JS, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty. Reg Anesth Pain Med. 2013;38:526–32. [DOI] [PubMed] [Google Scholar]
- [23].Kim DH, Lin Y, Goytizolo EA, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a prospective, randomized, controlled trial. Anesthesiology. 2014;120:540–50. [DOI] [PubMed] [Google Scholar]
- [24].Ludwigson JL, Tillmans SD, Galgon RE, et al. A comparison of single shot adductor canal block versus femoral nerve catheter for total knee arthroplasty. J Arthroplasty. 2015;30:68–71. [DOI] [PubMed] [Google Scholar]
- [25].Seo SS, Kim OG, Seo JH, et al. Comparison of the effect of continuous femoral nerve block and adductor canal block after primary total knee arthroplasty. Clin Orthop Surg. 2017;9:303–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Wiesmann T, Piechowiak K, Duderstadt S, et al. Continuous adductor canal block versus continuous femoral nerve block after total knee arthroplasty for mobilisation capability and pain treatment: a randomised and blinded clinical trial. Arch Orthop Trauma Surg. 2016;136:397–406. [DOI] [PubMed] [Google Scholar]
- [27].Klement MR, Bullock WM, Nickel BT, et al. The knee continuous adductor canal blockade facilitates increased home discharge and decreased opioid consumption after total knee arthroplasty. Knee. 2019;26:679–86. [DOI] [PubMed] [Google Scholar]
- [28].Mudumbai SC, Kim TE, Howard SK, et al. Continuous adductor canal blocks are superior to continuous femoral nerve blocks in promoting early ambulation after TKA. Clin Orthop Relat Res. 2014;472:1377–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Machi AT, Sztain JF, Kormylo NJ, et al. Discharge readiness after tricompartment knee arthroplasty: Adductor canal versus femoral continuous nerve blocks-a dual-center, randomized trial. Anesthesiology. 2015;123:444–56. [DOI] [PubMed] [Google Scholar]
- [30].Koh HJ, Koh IJ, Kim MS, et al. does patient perception differ following adductor canal block and femoral nerve block in total knee arthroplasty? A simultaneous bilateral randomized study. J Arthroplasty. 2017;32:1856–61. [DOI] [PubMed] [Google Scholar]
- [31].Grevstad U, Mathiesen O, Valentiner LS, et al. Effect of adductor canal block versus femoral nerve block on quadriceps strength, mobilization, and pain after total knee arthroplasty. Reg Anesth Pain Med. 2015;40:3–10. [DOI] [PubMed] [Google Scholar]
- [32].Shah NA, Jain NP. Is continuous adductor canal block better than continuous femoral nerve block after total knee arthroplasty? Effect on ambulation ability, early functional recovery and pain control: a randomized controlled trial. J Arthroplasty. 2014;29:2224–9. [DOI] [PubMed] [Google Scholar]
- [33].Hegazy N, Sultan S. Comparison between effects of adductor canal block and femoral nerve block on early postoperative course in total knee arthroplasty: a prospective double-blind, randomized controlled study. Ain-Shams J Anaesthesiol. 2015;8:124. [Google Scholar]
- [34].Patterson ME, Bland KS, Thomas LC, et al. The adductor canal block provides effective analgesia similar to a femoral nerve block in patients undergoing total knee arthroplasty — a retrospective study. J Clin Anesth. 2015;27:39–44. [DOI] [PubMed] [Google Scholar]
- [35].Mudumbai SC, Ganaway T, Kim TE, et al. Can bedside patient-reported numbness predict postoperative ambulation ability for total knee arthroplasty patients with nerve block catheters? Korean J Anesthesiol. 2016;69:32–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Thacher RR, Hickernell TR, Grosso MJ, et al. Decreased risk of knee buckling with adductor canal block versus femoral nerve block in total knee arthroplasty: a retrospective cohort study. Arthroplasty Today. 2017;3:281–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Rasmussen M, Kim E, Kim TE, et al. A retrospective comparative provider workload analysis for femoral nerve and adductor canal catheters following knee arthroplasty. J Anesth. 2015;29:303–7. [DOI] [PubMed] [Google Scholar]
- [38].Thobhani S, Scalercio L, Elliott CE, et al. Novel regional techniques for total knee arthroplasty promote reduced hospital length of stay: an analysis of 106 patients. Ochsner J. 2017;17:233–8. [PMC free article] [PubMed] [Google Scholar]
- [39].Memtsoudis SG, Yoo D, Stundner O, et al. Subsartorial adductor canal vs femoral nerve block for analgesia after total knee replacement. Int Orthop. 2015;39:673–80. [DOI] [PubMed] [Google Scholar]
- [40].Brennan PT, Villa JM, Rossi MD, et al. Rehabilitation outcomes for total knee arthroplasties: continuous adductor canal block versus continuous femoral nerve block. Geriatr Orthop Surg Rehabil. 2018;9:215145851875619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Bolarinwa SA, Novicoff W, Cui Q. Reducing costly falls after total knee arthroplasty. World J Orthop. 2018;9:198–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Ardon AE, Clendenen SR, Porter SB, et al. Opioid consumption in total knee arthroplasty patients: a retrospective comparison of adductor canal and femoral nerve continuous infusions in the presence of a sciatic nerve catheter. J Clin Anesth. 2016;31:19–26. [DOI] [PubMed] [Google Scholar]
- [43].Li D, Tan Z, Kang P, et al. Effects of multi-site infiltration analgesia on pain management and early rehabilitation compared with femoral nerve or adductor canal block for patients undergoing total knee arthroplasty: a prospective randomized controlled trial. Int Orthop. 2017;41:75–83. [DOI] [PubMed] [Google Scholar]
- [44].Zhang W, Hu Y, Tao Y, et al. Ultrasound-guided continuous adductor canal block for analgesia after total knee replacement. Chin Med J (Engl). 2014;127:4077–81. [PubMed] [Google Scholar]
- [45].Kukreja P, Bevinetto C, Brooks B, et al. Comparison of adductor canal block and femoral nerve block for early ambulation after primary total knee arthroplasty: a randomized controlled trial. Cureus. 2019;11:e6331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Wang C-G, Ding Y-L, Wang Y-Y, et al. Comparison of adductor canal block and femoral triangle block for total knee arthroplasty. Clin J Pain. 2020;36:558–61. [DOI] [PubMed] [Google Scholar]
- [47].Knutson K, Lindstrand A, Lidgren L. Survival of knee arthroplasties. A nation-wide multicentre investigation of 8000 cases. J Bone Joint Surg Br. 1986;68-B:795–803. [DOI] [PubMed] [Google Scholar]
- [48].Nafei A, Kristensen O, Moustgaard Knudsen H, et al. Survivorship analysis of cemented total condylar knee arthroplasty. J Arthroplasty. 1996;11:7–10. [DOI] [PubMed] [Google Scholar]
- [49].Sharkey PF, Hozack WJ, Rothman RH, et al. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. [DOI] [PubMed] [Google Scholar]
- [50].Terkawi AS, Mavridis D, Sessler DI, et al. Pain management modalities after total knee arthroplasty. Anesthesiology. 2017;126:923–37. [DOI] [PubMed] [Google Scholar]
- [51].Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367:1618–25. [DOI] [PubMed] [Google Scholar]
- [52].Thomas T, Robinson C, Champion D, et al. Prediction and assessment of the severity of post-operative pain and of satisfaction with management. Pain. 1998;75:177–85. [DOI] [PubMed] [Google Scholar]
- [53].Wylde V, Rooker J, Halliday L, et al. Acute postoperative pain at rest after hip and knee arthroplasty: Severity, sensory qualities and impact on sleep. Orthop Traumatol Surg Res. 2011;97:139–44. [DOI] [PubMed] [Google Scholar]
- [54].Cremeans-Smith JK, Millington K, Sledjeski E, et al. Sleep disruptions mediate the relationship between early postoperative pain and later functioning following total knee replacement surgery. J Behav Med. 2006;29:215–22. [DOI] [PubMed] [Google Scholar]
- [55].Bourne RB, Chesworth BM, Davis AM, et al. Patient Satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Scott CEH, Howie CR, MacDonald D, et al. Predicting dissatisfaction following total knee replacement. J Bone Joint Surg Br. 2010;92-B:1253–8. [DOI] [PubMed] [Google Scholar]
- [57].Sztain JF, Khatibi B, Monahan AM, et al. Proximal versus distal continuous adductor canal blocks. Anesth Analg. 2018;127:240–6. [DOI] [PubMed] [Google Scholar]
- [58].Meier AW, Auyong DB, Yuan SC, et al. Comparison of continuous proximal versus distal adductor canal blocks for total knee arthroplasty. Reg Anesth Pain Med. 2018;43:36–42. [DOI] [PubMed] [Google Scholar]
- [59].Zhang Z, Wang Y, Liu Y. Effectiveness of continuous adductor canal block versus continuous femoral nerve block in patients with total knee arthroplasty: a PRISMA guided systematic review and meta-analysis. Medicine. 2019;98:e18056–e18056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Charous MT, Madison SJ, Suresh PJ, et al. Continuous femoral nerve blocks: varying local anesthetic delivery method (bolus versus basal) to minimize quadriceps motor block while maintaining sensory block. Anesthesiology. 2011;115:774–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Lund J, Jenstrup MT, Jaeger P, et al. Continuous adductor-canal-blockade for adjuvant post-operative analgesia after major knee surgery: preliminary results. Acta Anaesthesiol Scand. 2010;55:14–9. [DOI] [PubMed] [Google Scholar]
- [62].Kwofie MK, Shastri UD, Gadsden JC, et al. The effects of ultrasound-guided adductor canal block versus femoral nerve block on quadriceps strength and fall risk. Reg Anesth Pain Med. 2013;38:321–5. [DOI] [PubMed] [Google Scholar]
- [63].Sakura S. Pitfalls of ultrasound-guided nerve blocks. Mausi. 2008;57:596–604. [PubMed] [Google Scholar]
- [64].Saranteas T, Karatitsos D, Alevizou A, et al. Limitations and technical considerations of ultrasound-guided peripheral nerve blocks: edema and subcutaneous air. Reg Anesth Pain Med. 2008;33:353–6. [DOI] [PubMed] [Google Scholar]
- [65].Neal JM, Salinas FV, Choi DS. Local anesthetic-induced myotoxicity after continuous adductor canal block. Reg Anesth Pain Med. 2016;41:723–7. [DOI] [PubMed] [Google Scholar]
- [66].Lin L-Y, Hung T-C, Lai Y-H. Pain control and related factors in hospitalized patients. Medicine (Baltim). 2021;100:e26768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].McGrath PA. Psychological aspects of pain perception. Arch Oral Biol. 1994;39(Suppl):55S–62S. [DOI] [PubMed] [Google Scholar]
- [68].Yu R, Wang H, Zhuo Y, et al. Continuous adductor canal block provides better performance after total knee arthroplasty compared with the single-shot adductor canal block?: an updated meta-analysis of randomized controlled trials. Medicine. 2020;99:e22762–e22762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Barrington JW, Lovald ST, Ong KL, et al. Postoperative pain after primary total knee arthroplasty: comparison of local injection analgesic cocktails and the role of demographic and surgical factors. J Arthroplasty. 2016;31(9 Suppl):288–92. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.