Abstract
Background
Urinary incontinence (UI) is the involuntary loss of urine and can be caused by several different conditions. The common types of UI are stress (SUI), urgency (UUI) and mixed (MUI). A wide range of interventions can be delivered to reduce the symptoms of UI in women. Conservative interventions are generally recommended as the first line of treatment.
Objectives
To summarise Cochrane Reviews that assessed the effects of conservative interventions for treating UI in women.
Methods
We searched the Cochrane Library to January 2021 (CDSR; 2021, Issue 1) and included any Cochrane Review that included studies with women aged 18 years or older with a clinical diagnosis of SUI, UUI or MUI, and investigating a conservative intervention aimed at improving or curing UI. We included reviews that compared a conservative intervention with 'control' (which included placebo, no treatment or usual care), another conservative intervention or another active, but non‐conservative, intervention. A stakeholder group informed the selection and synthesis of evidence.
Two overview authors independently applied the inclusion criteria, extracted data and judged review quality, resolving disagreements through discussion. Primary outcomes of interest were patient‐reported cure or improvement and condition‐specific quality of life. We judged the risk of bias in included reviews using the ROBIS tool. We judged the certainty of evidence within the reviews based on the GRADE approach. Evidence relating to SUI, UUI or all types of UI combined (AUI) were synthesised separately. The AUI group included evidence relating to participants with MUI, as well as from studies that combined women with different diagnoses (i.e. SUI, UUI and MUI) and studies in which the type of UI was unclear.
Main results
We included 29 relevant Cochrane Reviews. Seven focused on physical therapies; five on education, behavioural and lifestyle advice; one on mechanical devices; one on acupuncture and one on yoga. Fourteen focused on non‐conservative interventions but had a comparison with a conservative intervention. No reviews synthesised evidence relating to psychological therapies. There were 112 unique trials (including 8975 women) that had primary outcome data included in at least one analysis.
Stress urinary incontinence (14 reviews)
Conservative intervention versus control: there was moderate or high certainty evidence that pelvic floor muscle training (PFMT), PFMT plus biofeedback and cones were more beneficial than control for curing or improving UI. PFMT and intravaginal devices improved quality of life compared to control.
One conservative intervention versus another conservative intervention: for cure and improvement of UI, there was moderate or high certainty evidence that: continence pessary plus PFMT was more beneficial than continence pessary alone; PFMT plus educational intervention was more beneficial than cones; more‐intensive PFMT was more beneficial than less‐intensive PFMT; and PFMT plus an adherence strategy was more beneficial than PFMT alone. There was no moderate or high certainty evidence for quality of life.
Urgency urinary incontinence (five reviews)
Conservative intervention versus control: there was moderate to high‐certainty evidence demonstrating that PFMT plus feedback, PFMT plus biofeedback, electrical stimulation and bladder training were more beneficial than control for curing or improving UI. Women using electrical stimulation plus PFMT had higher quality of life than women in the control group.
One conservative intervention versus another conservative intervention: for cure or improvement, there was moderate certainty evidence that electrical stimulation was more effective than laseropuncture. There was high or moderate certainty evidence that PFMT resulted in higher quality of life than electrical stimulation and electrical stimulation plus PFMT resulted in better cure or improvement and higher quality of life than PFMT alone.
All types of urinary incontinence (13 reviews)
Conservative intervention versus control: there was moderate to high certainty evidence of better cure or improvement with PFMT, electrical stimulation, weight loss and cones compared to control. There was moderate certainty evidence of improved quality of life with PFMT compared to control.
One conservative intervention versus another conservative intervention: there was moderate or high certainty evidence of better cure or improvement for PFMT with bladder training than bladder training alone. Likewise, PFMT with more individual health professional supervision was more effective than less contact/supervision and more‐intensive PFMT was more beneficial than less‐intensive PFMT. There was moderate certainty evidence that PFMT plus bladder training resulted in higher quality of life than bladder training alone.
Authors' conclusions
There is high certainty that PFMT is more beneficial than control for all types of UI for outcomes of cure or improvement and quality of life. We are moderately certain that, if PFMT is more intense, more frequent, with individual supervision, with/without combined with behavioural interventions with/without an adherence strategy, effectiveness is improved. We are highly certain that, for cure or improvement, cones are more beneficial than control (but not PFMT) for women with SUI, electrical stimulation is beneficial for women with UUI, and weight loss results in more cure and improvement than control for women with AUI.
Most evidence within the included Cochrane Reviews is of low certainty. It is important that future new and updated Cochrane Reviews develop questions that are more clinically useful, avoid multiple overlapping reviews and consult women with UI to further identify outcomes of importance.
Plain language summary
Conservative interventions for urinary incontinence in women: an overview of Cochrane Reviews
What is urinary incontinence?
Bladder problems are common in women. Having to go to the toilet frequently, urgently and sometimes not making it in time is called urgency urinary incontinence. Urgency urinary incontinence occurs when, for some reason, the signals telling women to empty their bladder are much stronger and occur more often than necessary. Leaking when sneezing or exercising is called stress urinary incontinence, and can happen if the muscles controlling the outlet from the bladder are weaker than they should be. Women can also have a mixture of these two conditions, which is called mixed urinary incontinence.
Symptoms of bladder problems can cause a lot of distress. For example, women can often be reluctant to go out and may fear going for walks or taking part in exercise classes. Often these women can feel isolated and their quality of life is significantly poorer compared to women without bladder symptoms.
How is urinary incontinence treated?
Treatment options for urinary incontinence mainly include 'conservative treatment' (avoiding invasive methods), medication and surgery. Conservative treatments should be offered first and these include training of the pelvic floor muscle (muscle between the tail bone (coccyx) and pubic bone that support the bladder, bowel, vagina, and womb) (with and without add‐on treatments such as electrical stimulation), bladder training and devices. These are usually provided by physiotherapists or nurses who have had specialist training.
What did we aim to do?
There are a growing number of Cochrane Reviews relating to conservative management for different types of urinary incontinence, and our aim was to bring together these research findings into one accessible overview document, with input from clinicians and women affected by incontinence.
How up‐to‐date is this overview?
This overview is up‐to‐date to 18 January 2021.
What did we do?
We searched for Cochrane Reviews relating to the conservative management of urinary incontinence in women and found 29 relevant reviews. From these, we collated data regarding the type of intervention (treatment) and what it was compared to in tables. The comparison treatment could have been a control (such as a sham (pretend) treatment or usual care), another conservative intervention or a non‐conservative intervention. We identified two key outcomes that were important to women: if they were cured or improved and if their quality of life had improved. We assessed the quality of the included reviews and the certainty of the data within these reviews (the extent of our confidence that review results are correct in supporting or rejecting a finding).
Key results
There is high certainty evidence that undertaking pelvic floor muscle training can cure symptoms and improve quality of life for all types of urinary incontinence. There is moderate or high certainty evidence that these pelvic floor muscle exercises work better if they are more intense, have more support from a health professional, and are combined with strategies to support continued use. Lifestyle modifications, such as losing weight and trying to control how often you empty your bladder, may also be beneficial for some types of urinary incontinence. The use of adjuncts, such as electrical stimulation, may also be of benefit, especially for those with mixed or urgency urinary incontinence.
Quality of evidence
Approximately half of our findings provided moderate or high certainty evidence. However, 81% of our findings from analyses within the reviews included data only from one trial. These reviews had not been able to pull together the results of several trials. We could not identify any Cochrane Reviews for some commonly used treatments, such as psychological therapies. Generally, long‐term follow‐up was lacking and the use of multiple and diverse outcomes limited the possibility of combining results to give meaningful evidence.
Authors' conclusions
There is a lot of evidence for conservative management of urinary incontinence in women and the use of pelvic floor muscle exercises is strongly supported for most patients, regardless of the type of incontinence. However, there are many limitations with the current evidence for conservative treatment of urinary incontinence and often the evidence does not support clear clinical decisions. More research is urgently required to establish high‐quality evidence addressing questions which matter to women affected by urinary incontinence.
Background
At least one‐quarter of all women have urinary incontinence (UI), with prevalence increasing with age (Sandvik 2000). Around 20% of women with urinary problems seek professional help. This percentage increases with advancing age and is higher among women with other concomitant urogenital problems (Morrill 2007).
Evidence suggests that, for the majority of women affected, UI impacts significantly on daily living. It interferes with women's physical, psychological and social activities, reducing general health, well‐being and quality of life (NICE 2019). It is associated with an increased prevalence of major depression and, in older women, is linked to social isolation and psychological distress (Bogner 2002; Melville 2009). UI can cause several serious medical conditions (such as perineal rash, pressure ulcers and urinary tract infections) and increases the risk of admission to long‐term residential care (Hunskaar 2002).
The annual cost to the UK National Health Service (NHS) of treating clinically significant female UI has been estimated to be GBP 233 million in 1999/2000 (equivalent to approximately GBP 351 million in 2021, using the EPPI‐Centre Cost Converter) (Turner 2004). This does not include the personal costs borne by the women affected, which have been estimated to be GBP 178 million (equivalent to approximately GBP 248 million in 2021 using the EPPI‐Centre Cost Converter) (Turner 2004). Therefore, UI is prevalent and costly to healthcare providers, as well as burdensome to women both financially and in terms of negative impacts on physical and mental well‐being.
UI can result from damage to the neural control of the bladder or the pelvic floor muscles or from direct mechanical trauma to the pelvic floor (Glazener 2017a). The risk is increased by vaginal (particularly assisted) delivery, increasing age and parity, obesity and the menopause (Saraswat 2020). UI may also be caused by trauma or disease to the bladder.
Incidence figures depend on the definition used and the population investigated, with reported annual incidence rates (numbers of new cases) of UI ranging from 1% to 11% and the annual remission rate from 6% to 11% (Hunskaar 2005).
Description of the condition
UI is the involuntary loss of urine and can be caused by a number of different conditions (Blaivas 1997; Haylen 2010).
Continence is achieved through an interplay of the normal anatomical and physiological properties of the bladder, urethra, sphincter and pelvic floor, as well as the nervous system co‐ordinating these areas. The active relaxation of the bladder, coupled with the ability of the urethra and sphincter to contain urine within the bladder by acting as a closure mechanism during filling, allows storage of urine until an appropriate time and place to void is reached. The role of the pelvic floor in providing support to the bladder and urethra and allowing normal abdominal pressure transmission to the proximal urethra is also considered essential in the maintenance of continence. Crucial to the healthy functioning of the bladder, urethra, sphincter and pelvic floor is the co‐ordination between them, facilitated by an intact nervous system control. Incontinence occurs when this normal relationship between the lower urinary tract components is disrupted, resulting from nerve damage or direct mechanical trauma to the pelvic organs. Advancing age, higher parity, vaginal delivery, obesity and menopause are associated with an increase in risk (Saraswat 2020).
There are three main types of UI. Stress urinary incontinence (SUI) is the complaint of involuntary loss of urine on effort or physical exertion (e.g. sporting activities) (Haylen 2010). SUI is a symptom, rather than a condition. Research has shown that about 50% of the women below the age of 65 years with UI had SUI (Milsom 2012). Urgency urinary incontinence (UUI) is the complaint of involuntary loss of urine associated with urgency (Haylen 2010). Isolated UUI is the least common type, accounting for 10% of women who have UI (Milsom 2012). Mixed urinary incontinence (MUI) is the complaint of involuntary loss of urine associated with urgency and also with effort or physical exertion or on sneezing or coughing (Haylen 2010). It occurs in around 30% of women (Milsom 2012).
In addition, loss of urine may occur at night (known as nocturnal enuresis, the complaint of loss of urine occurring during sleep) or the interruption of sleep because of the need to urinate (with loss of urine if the toilet is not reached in time to void) and during intercourse (known as coital incontinence, the complaint of involuntary loss of urine with coitus, occurring with penetration, intromission or at orgasm).
Description of the interventions
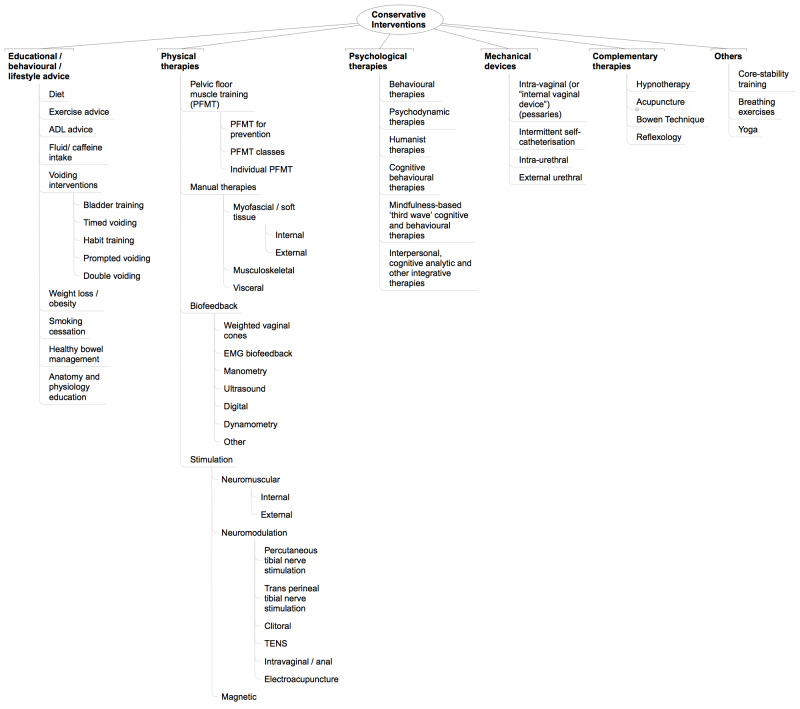
A wide range of interventions can be delivered to reduce the symptoms of UI in women, including conservative, pharmacological and surgical interventions (see Figure 1). The type of intervention selected for an individual woman will depend on an assessment of their symptoms, types of incontinence, factors contributing to UI, associated medical conditions, and clinician and individual choice. Conservative interventions are generally recommended as the first line of treatment for women with UI and are, therefore, the focus of this overview (NICE 2019). These include, but are not limited to, the following.
1.
ADL: activities of daily living; EMG: electromyography; TENS: transcutaneous electrical nerve stimulation.
Mechanical devices to prevent or reduce urinary leakage. These include pessaries (urethral and vaginal inserts) and mechanical plugs/patches (Lipp 2014).
Physical therapies, where for women with SUI, the aim is to improve muscle control. This principally includes pelvic floor muscle training (PFMT), which can be delivered with or without the use of assistive devices such as weighted vaginal cones, biofeedback or electrical stimulation (Dumoulin 2018).
Educational, behavioural and lifestyle advice to enhance management of UI. These commonly include methods of toileting assistance, such as prompted voiding, habit or bladder retraining and timed voiding, and advice about lifestyle factors, such as weight loss, management of fluid intake, caffeine and alcohol intake, and physical activity and exertion (Eustice 2000; Imamura 2015; Ostaszkiewicz 2004a; Ostaszkiewicz 2004b).
Psychological interventions, a range of which can be used to help a woman cope with her UI symptoms and improve her quality of life, based on a number of different philosophical or theoretical approaches. These include the Health Belief Model Theory of Planned Behaviour and the Social Cognitive Theory (self‐efficacy) (Alewijnse 2003a; Alewijnse 2003b; Chiarelli 1999; Whitford 2011).
Complementary therapies, which Cochrane's Complementary Medicine Field defines as "practices and ideas which are outside the domain of conventional medicine in several countries" and which are defined by its users as "preventing or treating illness, or promoting health and wellbeing" (Smith 2006). Therapies that are considered complementary practices in one country or culture may be considered conventional in another. For the purpose of this overview, we defined complementary therapies as complementary interventions (such as acupuncture or electroacupuncture, reflexology) but excluding medicines or consumed remedies (i.e. herbal medicines, traditional Chinese medicines, homeopathic remedies) (Bø 2013).
In addition to these groups of interventions, there are a growing number of digital health interventions that use new technologies and media to support and enhance the delivery of conservative management of UI. In particular, digital health interventions can help support the delivery of behavioural‐based interventions and may be used as part of bladder training or voiding programmes, or both.
The above conservative interventions are the focus of the overview. The following interventions were only included if they were used as comparators in the included evidence.
Pharmacological therapies for treating UI, including oestrogen (Cody 2012), anticholinergic drugs (Rai 2012), adrenergic drugs (Alhasso 2005), and botulinum toxin (Duthie 2011). These interventions may have had local or systemic effects.
Surgical procedures that aimed to treat UI by lifting and supporting the urethrovesical junction. There is disagreement about the precise mechanisms achieved by surgery, and the choice of procedures is often influenced by several different factors, including coexistent problems, a surgeon's specialty, and preference and the physical features of the woman affected (Glazener 2017a). Surgical methods principally include open abdominal retropubic suspension (Lapitan 2016), laparoscopic retropubic suspension (Dean 2017), mid‐urethral sling procedures (Ford 2015), traditional suburethral sling procedures (Saraswat 2020), anterior vaginal repair (Glazener 2017a), bladder neck needle suspensions (Bakali 2019), periurethral injections (Kirchin 2017), and artificial sphincters (Islah 2013).
Specialised products, such as special pads and bedsheets, and catheters, sheaths and bags.
Different techniques for the diagnosis of the cause of UI, including urodynamic investigations, diaries, pad tests, and imaging techniques such as x‐rays and ultrasound (Clement 2013; Groutz 2000).
How the intervention might work
Conservative interventions can work in a variety of ways, and the mechanism of action may be mechanical, physical, behavioural, psychological or a combination of these.
Mechanical devices
These are physical devices designed to stop or control urinary leakage, and work in a number of different ways (Lipp 2014). Intravaginal devices (or 'internal vaginal devices', also known as pessaries) are inserted into the vagina with the aim of supporting the bladder neck to improve SUI. Some devices are shaped with a bump that compresses the urethra, which also helps to reduce SUI. Intraurethral devices are inserted into the urethra, acting like a plug to prevent leakage. They are inserted and removed by the individual as required. External urethral devices are applied like a seal to the outer surface of the urethral opening (external placement) to stop leakage of urine from the urethra.
Physical therapies
Physical therapies are provided by rehabilitation professionals using specially designed exercises, delivered with or without the use of assistive devices, to help individuals regain or improve physical control of their bladder. These include the following.
PFMT involves repetitive selective voluntary contraction and relaxation of specific pelvic floor muscles. PFMT exercises can be taught to women by rehabilitation professionals but are then carried out independently by the woman on a regular basis, with or without supervision. PFMT can improve the strength, endurance and co‐ordination of these muscles (Alves 2015; Dumoulin 2018). For women with UUI, the biological rationale is based on Godec's observation that a detrusor muscle contraction can be inhibited by a pelvic floor muscle contraction induced by electrical stimulations (Godec 1975). Furthermore, de Groat 1997 demonstrated that during urine storage there is an increased pudendal nerve outflow response to the external urethral sphincter increasing intraurethral pressure, representing what he termed a "guarding reflex" for incontinence (de Groat 1997; de Groat 2001). Additionally, Morrison 1995 demonstrated that Barrington's micturition centre excitatory loop switches on when bladder pressures are between 5 mmHg and 25 mmHg, while the inhibitory loop is predominantly active above 25 mmHg. Inhibition involves an automatic, unconscious increase in tone for both the pelvic floor muscle and the urethral striated muscle. Thus, voluntary pelvic floor muscle contractions may be used to control UUI. After inhibiting the urgency to void and the detrusor contraction, the woman can reach the toilet in time to avoid urine leakage.
Biofeedback is used to supplement or enhance PFMT. Information about a normally unconscious physiological process is presented to the individual and the therapist as a visual, auditory or tactile signal (Sandweiss 1985). Such feedback enables a person to identify and modify a bodily function of which they may be unaware. Typically this may involve digital palpation or the use of a device to record the biological signals (e.g. squeeze pressure, electrical activity, pelvic floor morphometry using ultrasound) during a voluntary pelvic floor muscle contraction and presentation of this information back to the woman in auditory or visual form. Examples of this feedback are: verbal encouragement; a louder sound with a stronger squeeze or an increasing number of lights on a visual display as the strength of the squeeze increases; and visual display of levator ani contraction on an ultrasound screen. Thus, for a muscle that cannot be seen, the women receive some type of signal about their ability to use their pelvic floor muscle. Biofeedback may also be provided using weighted vaginal cones, which are small weights placed in the vagina that require contraction of the pelvic floor muscle to prevent them from slipping out. The cones provide a form of biofeedback, as the sensation of one slipping out induces a pelvic floor muscle contraction that may both strengthen muscles and help to synchronise muscle contraction with increases in abdominal pressure (Herbison 2013).
Several different types of stimulation, including electrical and magnetic stimulation, can be delivered either through surface electrodes (transcutaneous) or via direct stimulation (percutaneous), with the aim of stimulating the nerve supply and altering nerve activity. Stimulation of nerve supply is thought to improve muscle tone and sensation of the pelvic floor muscles, enhancing muscle control. It also aims to reduce detrusor contraction in the case of UUI. Electrical stimulation therapy can be used to treat overactive bladder (OAB) via different routes, such as implantable or internal electrodes (sacral neuromodulation) and non‐implantable or external electrodes. The latter can be subclassified as endocavitary electrodes (rectal or intravaginal) or percutaneous electrodes (tibial nerve stimulation). Cadwell 1963 was the first to report the use of intravaginal electrical stimulation (IES) in the treatment of UI. Subsequently, Messelink 1999 also used it with satisfactory results. IES using frequencies below 12 Hz stimulates the pudendal nerve, which may inhibit the detrusor muscle, reduce involuntary contractions and, consequently, reduce the number of micturitions in 24 hours (Messelink 1999). Electrical stimulation also works in passively, helping women to become conscious of the perineal muscle contraction and this may, in turn, help to inhibit detrusor involuntary contractions (Amaro 2003). IES can be used alone or in association with pelvic floor muscle exercises, often indicated in SUI and OAB. Percutaneous tibial nerve stimulation (PTNS) is a form of neuromodulation that delivers retrograde stimulation to the sacral nerve plexus through percutaneous electrical stimulation of the posterior tibial nerve via a needle electrode inserted cephalad to the medial malleolus, an anatomical area recognised as the bladder centre (Hajebrahimi 2015). Magnetic stimulation appears to induce inhibitory effects on detrusor overactivity in a similar manner to electrical stimulation, with the significant clinical advantage of being non‐invasive (Takahashi 2003).
Bladder training encourages people to extend the time between voiding so that continence might be regained. This can take months to achieve but may help people who are physically and mentally able to use this method. For women with UUI, the biological rationale is based on Godec's observation that a detrusor muscle contraction can be inhibited by a pelvic floor muscle contraction induced by electrical stimulation (Godec 1975). Furthermore, de Groat 1997 demonstrated that during urine storage there is an increased pudendal nerve outflow response to the external urethral sphincter increasing intraurethral pressure and representing what he termed a "guarding reflex" for incontinence (de Groat 1997; de Groat 2001). Additionally, Morrison 1995 demonstrated that Barrington's micturition centre excitatory loop switches on when bladder pressures are between 5 mmHg and 25 mmHg, while the inhibitory loop is predominantly active above 25 mmHg. Inhibition involves an automatic, unconscious increase in tone for both the pelvic floor muscle and the urethral striated muscle. Thus, voluntary pelvic floor muscle contractions may be used to control UUI. After inhibiting the urgency to void and the detrusor contraction, the woman can reach the toilet in time to avoid urine leakage (Wallace 2004).
Manual therapy is defined as a clinical physical approach utilising specific hands‐on techniques. It may include massage, soft tissue mobilisation, various connective tissue techniques, myofascial release, mobilisation of joints, joint manipulation or mobilisation of nerve tissue. It is used to diagnose and treat soft tissues and joint structures for the purpose of modulating pain, increasing range of motion, reducing soft tissue oedema, inducing relaxation, improving contractile and non‐contractile tissue extensibility or stability (or both), facilitating movement and improving function (personal communication: Bø 2017).
Educational, behavioural and lifestyle advice
Several lifestyle factors are thought to play a role either in the onset or later in the resolution or management of UI. These include the following.
Diet: many dietary factors are thought to aggravate urinary urgency and may also relate to weight gain or constipation, or both (see below). Therefore, dietary advice can be beneficial to the management of UI (Imamura 2015).
Exercise and activities of daily living (ADL) advice: weakened pelvic floor support structures and raised intra‐abdominal pressure caused by heavy lifting and strenuous activity may result in UI. Strenuous activity alone may also increase incontinence in the short term. Appropriate advice can help women to manage the impact of exercise and daily physical activity on UI, while maintaining a healthy lifestyle (Bø 2013).
Fluid/caffeine intake: worsening of urinary urgency, frequency and incontinence is often reported after consuming caffeine, alcohol, fizzy drinks, sweetened diet drinks or excessive fluids. Caffeine can increase bladder muscle contractility, whereas alcohol or excessive fluids may have a diuretic effect (Imamura 2015).
Voiding interventions: this is a broad term used to describe any type of scheduled toileting intervention, which can include programmes of scheduled bladder voiding and bladder training (aimed at trying to correct faulty habit patterns of frequent urination if present, improve control over bladder urgency, prolong voiding intervals, increase bladder capacity, reduce incontinent episodes and restore women's confidence in controlling bladder function) (Eustice 2000).
Weight loss/obesity: obesity and UI are common problems in women. Obese women have higher intra‐abdominal pressure than non‐obese women and it is thought that this chronically elevated pressure may predispose to incontinence by weakening pelvic floor support structures and by raising intra‐abdominal pressure (Imamura 2015).
Smoking cessation: there is evidence of a relationship between cigarette smoking and UI, although the mechanism is not fully understood (Bump 1992). Chronic coughing among smokers may also contribute to UI by raising intra‐abdominal pressure (Imamura 2015).
Healthy bowel management: constipation can obstruct the bladder, preventing adequate voiding and resulting in urine leakage. Chronic straining may also be a risk factor in the development of UI. Advice that avoids or limits constipation or chronic straining may improve or prevent UI (Imamura 2015).
Anatomy and physiology education: educational interventions to teach women about the causes of their UI may improve understanding of the condition and may therefore help women manage their symptoms (Imamura 2015).
Psychological therapies
There are many different types of psychological therapies, which are based on a range of theoretical and philosophical standpoints. These are often forms of talking therapy with individuals or in groups but may also include interventions such as telephone or internet‐based support. Psychological therapies are generally aimed at helping people change the way they think and behave. Psychological therapies may help women with UI to manage and maintain a sense of well‐being and enhance quality of life. For the purposes of this overview, we considered psychological therapies within the categories proposed and described by Shinohara 2013.
Behavioural therapies include behavioural therapy, behavioural activation, social skills and assertiveness training, and relaxation therapy.
Cognitive‐behavioural therapies include cognitive therapy, rational emotive behavioural therapy, problem‐solving therapy, self‐control therapy and courses aimed at coping with depression.
Mindfulness‐based 'third wave' cognitive and behavioural therapies include acceptance and commitment therapy, compassionate mind training, functional analytical psychotherapy, extended behavioural activation, meta‐cognitive therapy, mindfulness‐based cognitive therapy and dialectical behavioural therapy.
Psychodynamic therapies include interventions based on the Drive/structural model, Relational model and Integrative analytical model (Malan 1963; Mann 1973; Strupp 1984).
Humanist therapies include person‐centred therapy, Gestalt therapy, experiential therapies, transactional analysis, existential therapy, and non‐directive and supportive therapies.
Interpersonal, cognitive analytic and other integrative therapies include interpersonal therapy, cognitive‐analytic therapy, psychodynamic‐interpersonal therapy, cognitive‐behavioural analysis system of psychotherapy, counselling and motivational interviewing.
Complementary therapies
Several alternative therapies, such as hypnotherapy and acupuncture, may be used, often alongside other conservative interventions. These interventions are generally provided to help people feel better and to promote health and well‐being. Complementary therapies used to reduce symptoms and promote well‐being in women with UI may include (but are not limited to) the following.
Acupuncture or electroacupuncture is the practice of inserting a needle or needles into certain points in the body for therapeutic purposes (Wang 2013).
Hypnotherapy is a form of psychotherapy that can be used to create subconscious change in an individual in the form of new responses, thoughts, attitudes, behaviours or feelings (Komesu 2011).
The Bowen Technique is a hands‐on therapy in which very gentle pressure is applied to specific points on the body (Wilks 2007).
Reflexology is a massage used to relieve tension and treat illness, based on the theory that there are reflex points on the feet, hands and head linked to every part of the body (Mak 2007).
Other conservative interventions
There are several other conservative interventions that may be used for women with UI that do not fit within the above categories. These can include (but are not limited to) the following.
Core‐stability training involves specific exercises, comprising stretching and strengthening exercises that are adapted to the condition of the intervention, aimed at improving muscle strength and control around the pelvic area. These exercises may be delivered by an exercise instructor or person who is not a rehabilitation professional. Increased muscle strength and control around the pelvic area may improve the symptoms of UI by changing intra‐abdominal pressure and increasing pelvic floor muscle control (Bø 2013).
Breathing exercises and hypopressive exercises generally aim to complement PFMT by changing the pressure on the abdominal wall and improving the overall quality of PFMT exercises (Bø 2013).
Modern Pilates exercise programmes incorporate exercises that involve breathing and contraction of pelvic floor muscles. The pelvic floor muscles are not specifically trained but they are trained incidentally during exercise and movement. The co‐contraction of pelvic floor muscles that occurs incidentally during Pilates exercises will counteract increases in intra‐abdominal pressure that occur during exercise, preventing leakage and strengthening pelvic floor muscles (Bø 2013).
Yoga is a physical, mental and spiritual practice, which may benefit UI through changes to physical (e.g. muscle stretching, control) and psychological mechanisms (Bø 2013).
In the Paula Method, all sphincters in the body work simultaneously so exercising the ring muscles of the mouth, eyes, or nose may result in co‐contraction and strengthening of the pelvic floor muscles (Bø 2013).
Tai Chi is an ancient exercise regimen originating in China and has widespread use as exercise for general health in China. Chang 1986 describes an exercise called "the deer" involving contraction of the anal sphincter. The exercise is recommended for both men and women for conditions related to the pelvic area (Bø 2013).
Additionally, Carriere 2006 has claimed that "poor posture" can lead to pain and dysfunction in the pelvic floor. It is thought that optimal strategies for transferring loads will balance control of movement while maintaining optimal joint axes, maintain sufficient intra‐abdominal pressure without compromising the organs (preserve continence, prevent prolapse or herniation) and support respiration. Suboptimal strategies for posture, movement and breathing, or combinations thereof, create failed load transfer which can lead to pain, incontinence and breathing disorders (Bø 2013).
Why it is important to do this overview
Conservative management is recommended as a first‐line treatment for women with UI (NICE 2019). However, identifying the most effective rehabilitation interventions is not always easy. Given the importance of curing, improving or managing UI symptoms to allow women to have an active lifestyle and good quality of life, there are a substantive and growing number of randomised controlled trials (RCTs) and systematic reviews relating to the effectiveness of conservative interventions for UI. Despite this growing body of evidence, current clinical practice often does not reflect the available evidence‐base, and this important area of practice receives little attention in undergraduate physiotherapy education (Francis 2012; McClurg 2013). Lack of sufficient time to identify and synthesise evidence is cited as the key barrier to evidence‐utilisation within UI rehabilitation (McClurg 2013).
It has been recognised that a large and growing body of systematic reviews can be overwhelming for decision‐makers, including women and healthcare practitioners, who do not have time to keep up‐to‐date with this evidence‐base (Bastian 2010). In one accessible, comprehensive document, a Cochrane Overview of conservative interventions for women with UI will synthesise all high‐quality evidence about UI conservative interventions, assess the limitations of current best evidence and enable indirect comparisons of the effects of different interventions on UI. This overview will support evidence‐based management of UI among key decision‐makers (such as clinicians, policymakers or informed health service users) and educators of allied health professionals.
Objectives
To summarise Cochrane Reviews that assess the effects of conservative interventions for treating urinary incontinence in women.
Methods
Criteria for considering reviews for inclusion
Types of studies
We included Cochrane Reviews published in the Cochrane Database of Systematic Reviews that assessed conservative interventions for treating UI in women.
Types of participants
We included reviews of studies in which the participants were women aged 18 years or older with a clinical diagnosis of SUI, UUI or MUI, regardless of cause or comorbidities.
Types of interventions
We included reviews of studies that investigated a conservative intervention for which the primary aim was to improve or cure UI. Conservative interventions included those listed in How the interventions might work and are illustrated in Figure 1.
Where the above inclusion criteria were met, we included reviews of studies in which the participants were recruited from any setting, including community, hospital or care home environments. We considered reviews that included both male and female participants but only included reviews in which we could extract data relating specifically to the female participants.
We excluded reviews of surgical or pharmacological interventions, products to manage leakage of urine and investigative techniques unless these were compared with a conservative intervention. We included reviews in which a conservative intervention was considered a control intervention.
We included reviews that compared a conservative intervention with any other intervention. We categorised these comparison interventions as either 'control' (which included placebo, no treatment or usual care), another conservative intervention or another active, but non‐conservative, intervention. We documented the definitions of comparison interventions provided by review authors, and explored and described the comparison interventions according to our prestated taxonomy of interventions.
Stakeholder participation
We convened a stakeholder group comprising 14 purposively selected people, including clinicians, service users and commissioners. Members of this group are listed and acknowledged in the Acknowledgements section. We used formal group consensus methods based on nominal group techniques, as this method enables the pooling of decisions and judgements from a group of informed experts, leading to votes on a range of options until ultimately group consensus is reached (Pollock 2014; Pollock 2016). Stakeholders contributed to the protocol development using consensus methodologies to identify key areas of clinical priority to incorporate into the overview and identified key outcomes for the overview (McClurg 2016). The process of stakeholder group involvement is outlined in Appendix 1.
Types of outcome measures
This overview focussed on two critical (primary) outcomes.
Symptomatic cure or improvement of UI, as reported by the woman (including through self‐report or bladder diaries). This outcome is based on the woman's observations (i.e. is a participant‐reported measure), as described/reported in the review.
Condition‐specific quality of life, as measured by specific instruments designed to assess the impact of UI symptoms on the life of a woman, such as King's Health Questionnaire, Incontinence Quality of Life (I‐QOL) and Bristol Female Lower Urinary Tract Symptoms (BFLUTS) questionnaire (Jackson 1996; Kelleher 1997; Wagner 1996)
See Differences between protocol and review for further information.
Timing of outcome assessment
We considered outcomes at three time periods: the end of treatment, up to one year after end of treatment and more than one year after end of treatment.
We categorised outcomes presented within analyses (forest plots) as either 'immediate' (i.e. at the end of intervention) or 'follow‐up', documenting and reporting within tables the time point of the data pooled, as reported in the included review.
We identified information relating to all outcomes synthesised within the included reviews but only extracted data relating to effect size from relevant analyses of comparisons relating to these stated outcomes of interest.
Search methods for identification of reviews
We identified relevant reviews from Cochrane Incontinence's list of published Cochrane Reviews and searched the Cochrane Library (Cochrane Database of Systematic Reviews; 2021, Issue 1) using the strategy given in Appendix 2 on 18 January 2021.
We also noted titles and protocols registered with Cochrane Incontinence for consideration in future versions of the overview.
Data collection and analysis
During the process of data collection and analysis, evidence relating to SUI, UUI or MUI were separated according to these three subgroups. With the exception of 'Data analysis', the description of methods within subsequent sections refers to synthesis of data as presented within the included reviews and not to any re‐analysis or pooling of data.
Selection of reviews
Two overview authors (two of CH, DM, AP, PC) independently considered the titles and abstracts from the identified reviews and applied the inclusion criteria (see Criteria for considering reviews for inclusion). We resolved disagreements through consideration and discussion of the full paper, involving a third overview author where necessary.
We contacted review authors of any titles or protocols that appeared to meet our selection criteria, identifying those that authors indicated should be completed within three months of our initial search date. We also contacted authors of all completed reviews meeting our selection criteria for which the search date was more than 12 months ago and asked if an update was anticipated within this three‐month period. Initial contact with review authors was made via Cochrane Incontinence. When authors indicated that a review should be finished or updated within this timeframe, we sent a reminder email in advance of this date to check on progress and to gain access to relevant prepublication data where possible.
Data extraction and management
Two overview authors (CH, AP) independently extracted data. We resolved disagreements by discussion, with assistance from a third overview author where necessary. We used a data collection form specifically designed and piloted by the overview author team. Onto this form, we extracted and recorded key features of each review, including details of the aims and rationale, types of studies, participants, interventions, comparisons, outcomes assessed, date of last search and analyses (forest plots) completed.
Using a spreadsheet, we systematically synthesised the studies included within all identified reviews to explore whether any reviews covered the same studies. When there was overlap between reviews, two overview authors discussed the overlap with consideration of each review question and explored comparisons, the date of the last search and key aspects of methodological quality (e.g. types of studies included, risk of bias assessment). We used these details to reach an agreement regarding which data from which review comparisons were to be included within the overview.
Type of urinary incontinence
During the data extraction process, two overview authors independently noted whether each included review reported evidence relating to SUI, UUI, or MUI. We resolved disagreements through discussion, using a third overview author where necessary. We had anticipated that we may identify data relating to combined or unclear populations and had proposed at the protocol stage that, if necessary, we would group data relating to "combined" populations and "unclear" populations (where the population was undefined). However, during the process of categorising type of UI we found that we were unable to distinguish between 'mixed', 'combined' and 'unclear' populations. Therefore, we did not use the planned additional groups of 'combined' and 'unclear' but instead categorised all mixed, combined or unclear data into a group of 'all types of UI'. Thus, we categorised data into three separate populations: SUI, UUI and 'all types of UI' (AUI).
We completed all subsequent stages of the overview in triplicate, for:
conservative interventions for management of SUI;
conservative interventions for management of UUI;
conservative interventions for management of AUI.
Criteria for identifying relevant comparisons
We used extracted data to determine which reviews had analyses (comparisons within forest plots) of relevance to this overview according to the three populations of interest. Relevant comparisons evaluated the effect on the stated primary outcomes of interest to the overview by comparing the effects of:
any conservative intervention versus control, placebo or standard care;
any conservative intervention versus other active intervention (i.e. surgical or pharmacological intervention); or
one conservative intervention versus another conservative intervention.
Originally, we had also planned to extract data relating to analyses comparing different doses, intensities or timing of delivery of conservative intervention. However, due to lack of analyses focused on these comparisons, we extracted no relevant data.
Assessment of methodological quality of included reviews
Quality of included reviews
Two overview authors independently assessed the methodological quality of the included reviews using the ROBIS (Risk of Bias In Systematic Reviews) tool (Whiting 2016), with input from a third overview author (AE) where there were disagreements.
ROBIS is completed in three phases, with the first assessing relevance, identifying concerns with the review process and judging the risk of bias in the review. Phase 2 assesses four domains to help assess specific concerns about potential biases within the review.
Domain one: study eligibility criteria (i.e. review eligibility criteria were clear, appropriate and prespecified).
Domain two: identification and selection of studies (i.e. all relevant primary studies should have been identified and included in the review).
Domain three: data collection and study appraisal (i.e. judgement relating to bias that may have been introduced through the data collection and assessment of risk of bias of included studies).
Domain four: synthesis and findings (i.e. appropriate methods have been used for any meta‐analyses, and syntheses of results).
We completed all signalling questions for the assessment of these domains and used these to help judge overall risk of bias. We used the rating guidance published with the ROBIS tool in answering all signalling questions (Whiting 2016).
Two overview authors carried out assessments for domains one to three independently, discussing any disagreements and reaching consensus on a final judgement of risk of bias for each of these three domains. Due to an initial high level of disagreement between these two overview authors for domain four and lack of clarity relating to how to consistently judge this domain, a third overview author (AE) independently judged this domain for 50% of the reviews. The three overview authors met and discussed their independent judgements and reached consensus on how to judge certain scenarios. Following this, the original two overview authors (CH, AP) discussed and reached consensus over the judgements for this domain for the remaining 50% of the reviews.
Phase 3 involves a judgement of the overall risk of bias of each review, following assessment of three signalling questions. These prompt an answer of 'yes', 'probably yes', 'probably no', 'no' or 'unclear'. Two or three overview authors completed the three signalling questions independently and reached consensus through discussion. The final overall judgement of low, high or unclear risk of bias was not assigned to avoid the possibility of this being used as a summary 'quality score' for each review (Whiting 2016).
Quality of evidence in included reviews
We did not reassess the quality of individual studies included within reviews but reported the quality of individual studies as assessed by the review authors, who all used the Cochrane RoB 1 tool (Higgins 2011). We assessed our certainty in the evidence synthesised within each relevant comparison (i.e. all relevant analyses and forest plots from included reviews which contain data for one of our prestated primary or secondary outcomes of interest) using the GRADE approach (Guyatt 2011a). This includes:
risk of bias due to flawed design or conduct of studies (Guyatt 2011b);
imprecision (e.g. when confidence intervals (CIs) for treatment effect are wide) (Guyatt 2011c);
inconsistency (e.g. when point estimates vary widely, I² statistic is large) (Guyatt 2011d);
indirectness (e.g. variations in participants, interventions, comparisons and outcomes) (Guyatt 2011e);
publication bias (may be explored using funnel plots and classed as not suspected, suspected, strongly suspected or very strongly suspected) (Guyatt 2011f).
The GRADE approach provides a system for rating certainty of evidence and strength of recommendations that is explicit, comprehensive, transparent and pragmatic. It is increasingly being adopted by organisations worldwide. However, difficulties associated with the subjectivity involved in judging grade of evidence have previously been reported, while poor agreement has been found on grading strength of evidence within systematic reviews using GRADE, even among experienced systematic reviewers (Berkman 2013). One Cochrane Overview reported the difficulty in achieving agreement between independent overview authors for GRADE judgements when numerous comparisons needed to be assessed, proposing the use of an objective algorithm to enable transparent, reproducible assignment of GRADE levels of evidence (Pollock 2014; Pollock 2016).
We explored the use of the iterative methods reported by Pollock 2016 to develop a set of objective criteria for exploring the certainty of the specific body of evidence included within this overview. Using the GRADE guidance papers, we assessed the limitations, imprecision, inconsistency, indirectness and publication bias of the comparison in two reviews and all authors assigned a final GRADE rating assigned independently. We discussed these results to determine the key variables to consider and how these could be used to assign a GRADE level.
Overview authors agreed that, for this body of evidence, the algorithm should involve systematic assessment of:
risk of bias of trials contributing participants to the analysis, as reported by the review authors within risk of bias tables, and specifically considering the proportion of participants within the analysis that was judged at high risk of bias for blinding of outcome assessor and allocation concealment;
differential attrition;
publication bias, as assessed by domain 2 of the ROBIS tool;
imprecision, considering both the CIs and sample size;
inconsistency, based on heterogeneity within the analysis, as determined by the I² statistic; and
indirectness, determined by considering important issues of clinical heterogeneity, specifically whether data from participants with SUI and UUI were combined and data from women who were antenatal and postnatal were combined.
Details of all the criteria within the algorithm, the downgrades applied based on the data arising from each relevant analysis within the overview, and justification for the cut‐offs adopted within the algorithm are provided in Appendix 3. There were two reviews for which we did not use the algorithm, and instead we used the GRADE assessments as reported by review authors; reasons for this difference are outlined in Differences between protocol and review.
Data synthesis
Intervention categorisation
We categorised conservative interventions addressed by each review as shown in Figure 1. We categorised the interventions investigated in each included study at three levels, as described in Appendix 4. We categorised all interventions for each study within each relevant comparison using the described levels. Where this related to a primary outcome of interest, this was completed by two overview authors independently (CH, DM), with any differences resolved through discussion. Where this related to a secondary outcome of interest, this was performed by one overview author (DM) and checked by a second (CH). We had planned to use different layers of intervention categorisation to present and describe interventions at various points within analyses and maps but did not complete these (see Differences between protocol and review).
Exploration of subgroups
The objective of this overview was to systematically synthesise the results of data pooled within reviews relating to conservative interventions for different types of UI. As part of this objective, we planned to explore existing data relating to different subgroups of women. We did not plan to carry out any statistical subgroup comparisons ourselves but rather to extract and tabulate results of relevant analyses from the included reviews where these were presented for one or more of our predefined subgroups (see Differences between protocol and review). However, none of the included reviews reported any statistical subgroup analyses based on any of our predefined subgroups and, consequently, no exploration of subgroups is presented within this overview.
Statistical analysis
We planned to analyse available data relating to comparisons within the included reviews for the three populations of interest (SUI, UUI and AUI) and the two primary outcomes (symptomatic cure or improvement of UI and condition‐specific quality of life). We planned to summarise included data within forest plots and network maps but have not included these in the final overview to simplify and enhance accessibility, and promote sustainability, of this overview (see Differences between protocol and review).
Results
Description of included reviews
Results of the search
We considered 1944 titles of Cochrane Reviews and protocols after removal of duplicates and 57 full‐text articles (Figure 2). Sixteen full‐text articles did not meet our inclusion criteria and were excluded (see Appendix 5 for references and further characteristics of these excluded reviews).
2.
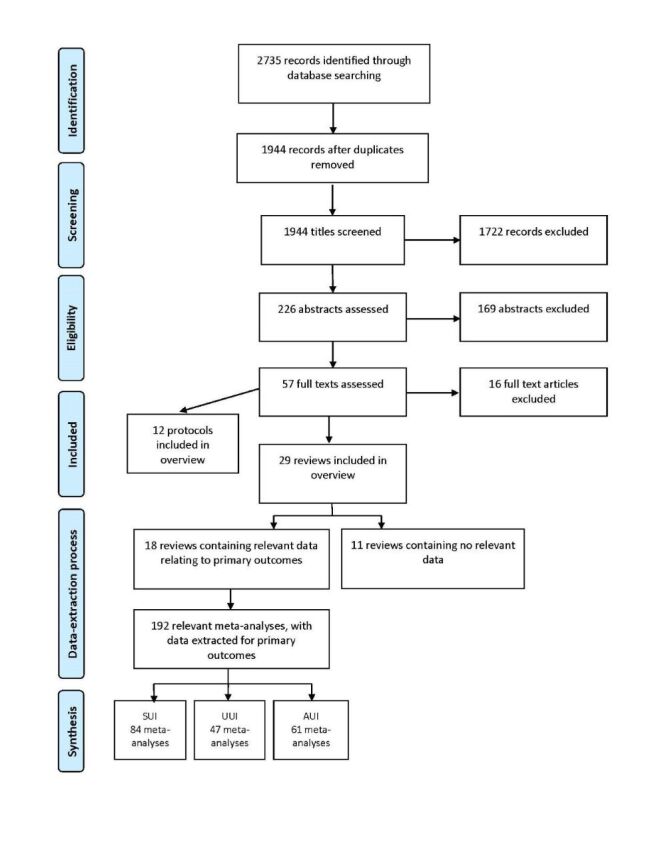
PRISMA study flow diagram. AUI: all types of urinary incontinence; n: number of records; SUI: stress urinary incontinence; UUI: urgency urinary incontinence.
The remaining 41 full texts met our inclusion criteria and were included. Twenty‐nine were completed reviews (Alhasso 2005; Ayeleke 2015; Cody 2012; Dumoulin 2018; Duthie 2011; Eustice 2000; Freites 2019; Glazener 2017a; Glazener 2017b; Hay‐Smith 2011; Herbison 2009; Herbison 2013; Herderschee 2011; Imamura 2015; Kang 2015; Kirchin 2017; Lapitan 2017; Lipp 2014; Mariappan 2005; Nambiar 2017; Ostaszkiewicz 2004a; Ostaszkiewicz 2004b; Rai 2012; Saraswat 2020; Stewart 2016; Stewart 2017; Wallace 2004; Wang 2013; Wieland 2019). Twelve were protocols (Chua 2015; Cotterill 2018; French 2010; Funada 2020; Hajebrahimi 2015; Hargreaves 2020; Khazali 2016; Lane 2020; Lins 2014; Ostaszkiewicz 2013; Reynard 2016; Yi 2014). However, two protocols were withdrawn prior to publication of this overview (Khazali 2016; Reynard 2016; see Appendix 6).
Characteristics of the 29 included reviews are provided in Table 1 (design and conduct) and Table 2 (results).
1. Characteristics of included reviews: design and conduct.
| Study ID | Objective | Inclusion criteria | ||||
| Population | Intervention | Planned comparisons | Study design | Databases searched | ||
| Alhasso 2005 | To determine the effects of adrenergic agonists in the treatment of SUI. | Women with UI Age range 18–90 years |
Adrenergic agonist drug | Adrenergic agonist drug
|
RCT QRCT | Cochrane Incontinence's Specialised Register – 15 September 2010 |
| Ayeleke 2015 | To compare the effects of PFMT plus another active treatment vs the same active treatment alone in the management of women with UI. | Women with SUI, UUI or MUI Age range 18–75 years |
PFMT as a programme of repeated voluntary pelvic floor muscle contractions taught or supervised (or both) by healthcare professionals. All types of PFMT programmes were considered for inclusion. |
A: physical
B: behavioural
C: electrical or magnetic
D: mechanical
E: drugs
F: surgery
G: other
|
RCT QRCT | Cochrane Incontinence's Specialised Register – 5 May 2015 (update)t Embase Classic and Embase 1947 – 7 March 2013 (original) CINAHL – January 1982 and 6 May 2015 (update) ClinicalTrials.gov. – 30 May 2013 (original) WHO ICTRP 3 June 2013 (original) |
| Cody 2012 | To assess the beneficial and harmful effects of oestrogen therapy used for the treatment of UI. | Postmenopausal women with UI and diagnosed as having SUI, UUI or MUI Age not reported |
Oestrogen therapy (different types of oestrogens, different doses and different routes of administration) | Oestrogen therapy
|
— | Cochrane Incontinence's Specialised Register – 21 June 2012 |
| Dumoulin 2018 | To assess the effects of PFMT for women with UI vs no treatment, placebo or sham treatments, or other inactive control treatments. | All women with UI and diagnosed as having SUI, UUI or MUI Overall age not addressed in overview |
PFMT defined as a programme of repeated voluntary pelvic floor muscle contractions taught and supervised by a healthcare professional. All types of PFMT programmes were considered. Trials in which PFMT was combined with a single episode of biofeedback or advice on strategies for symptoms of urgency or frequency were eligible for inclusion. | Comparisons not listed explicitly. However, the objective was to determine the effects of PFMT for women with UI in comparison to no treatment, placebo or sham treatments, or other inactive control treatments. In addition, 1 arm of all eligible trials included use of a PFMT programme to ameliorate symptoms of existing urine leakage, 1 received no treatment, 1 placebo, 1 sham treatment and 1 an inactive control treatment |
RCT QRCT | Cochrane Incontinence's Specialised Register – 12 February 2018 |
| Duthie 2011 | To compare intravesical botulinum toxin injection with other treatments for neurogenic and idiopathic OAB in adults with or without UI | Men and women diagnosed with idiopathic or neurogenic OAB syndrome regardless of whether they also had SUI. | Intravesical botulinum toxin | Intravesical botulinum toxin
|
RCT QRCT | Cochrane Incontinence's Specialised Register – 23 February 2010 |
| Eustice 2000 | To determine the effects of prompted voiding for the management of UI. | Men and women with or without cognitive impairment diagnosed
as having UI Mean age 84 years |
Prompted voiding | Prompted voiding
|
RCT QRCT | Cochrane Incontinence's Specialised Register – 31 January 2006 |
| Freites 2019 | To assess the effects of laparoscopic colposuspension for UI in women and summarise the principal findings of relevant economic evaluations of these interventions. | Women with SUI or MUI | Laparoscopic colposuspension | Laparoscopic colposuspension
|
RCT QRCT |
Cochrane Incontinence's Specialised Register – 22 May 2019 |
| Glazener 2017a | To determine the effects of anterior vaginal repair (anterior colporrhaphy) on SUI or MUI in women | Women with UI diagnosed as having: urodynamic UI (urodynamic diagnosis), SUI (clinical diagnosis) or MUI (any SUI + other urinary symptoms Age not reported |
Anterior vaginal repair (anterior colporrhaphy) | Anterior vaginal repair
|
RCT QRCT | Cochrane Incontinence's Specialised Register – 1 September 2009 |
| Glazener 2017b | To determine the effects of needle suspension on SUI or MUI in comparison with other management options. | Women with SUI MUI | Needle suspension | Needle suspension
|
RCT QRCT |
Cochrane Incontinence's Specialised Register – 12 November 2014 Additional searches conducted for a brief economic commentary in April 2017 |
| Hay‐Smith 2011 | To compare the effects of different approaches to PFMT for women with UI. | Women with UI diagnosed as having SUI, UUI or MUI on the basis of symptoms, signs or urodynamic evaluation, as defined by the study authors. | PFMT defined as any programme of repeated voluntary pelvic floor muscle contractions, or 'indirect' voluntary pelvic floor muscle contraction irrespective of variations in purpose and training parameters |
|
RCT QRCT | Cochrane Incontinence's Specialised Register ‐– 17 May 2011 |
| Herbison 2009 | To determine the effects of implantable ES devices in the treatment of urine storage and voiding problems. | People with
|
An implanted device to provide stimulation to the sacral nerve(s). | Sacral nerve stimulation
|
RCT QRCT | Cochrane Incontinence's Specialised Register (10 February 2009) CENTRAL (March 2008) MEDLINE (March 2008) Embase (March 2008) CINAHL (March 2008) |
| Herbison 2013 | To determine the effectiveness of vaginal cones in the management of female SUI | Women whose predominant complaint was SUI, diagnosed either by symptom classification or urodynamics. Premenopausal, postmenopausal or 3 months' postpartum |
Weighted vaginal cones following a standardised (within trial) protocol. | Vaginal cones
|
RCT QRCT | Cochrane Incontinence's Specialised Register – 19 September 2012 MEDLINE – February 2013 Embase – February 2013 |
| Herderschee 2011 | To determine whether feedback (including biofeedback) provides additional benefit to PFMT in women with UI (SUI, UUI or MUI), regardless of cause. | Women of all ages with SUI, UUI or MUI, diagnosed by symptoms (reported by the woman), signs (as reported or observed by the healthcare professional) or urodynamics, regardless of cause. Age: 20–80 years |
≥ 1 PFMT arm had to include a form of feedback (or biofeedback) to teach, modulate or encourage pelvic floor muscle contractions |
|
RCT QRCT | Cochrane Incontinence's Specialised Register – 13 May 2010 |
| Imamura 2015 | To determine the effectiveness of specific lifestyle interventions (i.e. weight loss; dietary changes; fluid intake; reduction in caffeinated, carbonated and alcoholic drinks; avoidance of constipation; stopping smoking; and physical activity) in the management of adult UI. | Adults with UI, diagnosed either by symptom classification (SUI; UUI; MUI) or by urodynamic investigation (urodynamic SUI where not all participants had UI at baseline Age range (mean) 49–70 years |
A community‐based lifestyle intervention following a standardised (within trial) protocol. | Not clearly stated, but the methods stated: "Comparison interventions included no (active) treatment, other conservative physical therapies such as pelvic floor muscle training (PFMT) or bladder training, or pharmacological therapies." | RCT QRCT | Cochrane Incontinence's Specialised Register – 3 July 2013 Note: a further update was performed on 27 October 2014 but data entered only into 'studies awaiting classification'. |
| Kang 2015 | To evaluate the efficacy of transurethral radiofrequency collagen denaturation, compared with other interventions, in the treatment of women with UI. |
Women with SUI or MUI diagnosed clinically or using urodynamics. | Transurethral radiofrequency collagen denaturation | Transurethral radiofrequency collagen denaturation
|
RCT, QRCT quote: "excluded cluster‐randomised and cross‐over trials." |
Cochrane Incontinence Group Specialised Register Embase and Embase Classic Google scholar Contacted manufacturers US FDA website Current Controlled Trials ClinicalTrials.gov WHO International Clinical Trials Registry Platform Handsearches of relevant conference abstracts – 19 December 2014 |
| Kirchin 2017 | To determine the effects of periurethral and transurethral bulking agents on cure or improvement of UI in women | Women with UI. Classification of diagnoses was as defined by the study authors. Age not reported |
Urethral injection therapy | Urethral injection therapy
|
RCT QRCT | Cochrane Incontinence's Specialised Register – 8 November 2010 MEDLINE – January 1996 to March 2017 Embase – January 1980 to April 2017 NHS EED – April 2017 |
| Lapitan 2017 | To determine the effects of open retropubic colposuspension for the treatment of UI in women. | Women with SUI or MUI | Open retropubic colposuspension | Open retropubic colposuspension
|
RCT QRCT |
Cochrane Incontinence's Specialised Register – 5 May 2015 Additional searches conducted for a brief economic commentary in April 2017 |
| Lipp 2014 | To determine the effects of mechanical devices in the management of adult female UI, particularly SUI. | Women with UI diagnosed as having SUI, UUI or other incontinence either by symptom classification or by urodynamic diagnosis, as defined by the study authors. Age not mentioned under participants. Individual trials reported mean or range (44–73 years) |
Interventions using mechanical devices designed to control urinary leakage by being inserted: within the vagina; within the urethra or applied to the external surface of the urethra. | A mechanical device
|
RCT QRCT | Cochrane Incontinence's Specialised Register – 21 August 2014 Embase – 26 August 2014 CINAHL – 26 August 2014 |
| Mariappan 2005 | To determine the effects of SNRI in the management of SUI and MUI that includes SUI in adults. | Women and men with UI diagnosed as having SUI (clinical diagnosis), urodynamic SUI (urodynamic diagnosis) or MUI Age 49–54 years |
SNRIs | SNRI
|
RCT QRCT | Cochrane Incontinence Specialised Register – 5 March 2007 CENTRAL – the Cochrane Library 2006 – 14 November 2006 MEDLINE – 7 February 2007 MEDLINE In‐Process & Other Non‐Indexed Citations – 7 February 2007 |
| Nambiar 2017 | To assess the effectiveness of mini‐sling procedures in women with urodynamic clinical SUI or MUI in terms of improved continence status, quality of life or adverse events. | Women with SUI, or MUI if women had stress‐predominant symptoms | Single‐incision sling | Single‐incision slings
|
RCT QRT |
Cochrane Incontinence's Specialised Register – 6 February 2013 ClinicalTrials.gov and WHO ICTRP – 20 September 2012 Additional searches conducted for a brief economic commentary in April 2017 |
| Ostaszkiewicz 2004a | To assess the effects of habit retraining for the management of UI in adults |
Men and women with or without cognitive impairment diagnosed either by symptom classification or by urodynamic study as having UI. Women mean age 80.3 years Men mean age 83 years |
Habit retraining | Habit retraining
|
RCT QRCT | Cochrane Incontinence Specialised Register – 2 April 2009 MEDLINE – 15 February 2004 Embase – 9 May 2002 CINAHL – March 2001 PsycINFO – August 2002 Current Contents 2001 |
| Ostaszkiewicz 2004b | To assess the effects of timed voiding for the management of UI in adults. | Men and women with or without cognitive impairment diagnosed either by symptom classification or urodynamic study as having UI. Mean age 86 years |
Timed voiding alone or + other interventions. While acknowledging variability in the definition of timed voiding, this review of timed voiding applied the definitions proposed by Hadley 1986 and by the Agency for Healthcare Research and Quality (Fantl 1991). In this context, timed voiding is distinguished from bladder training, prompted voiding and habit training. |
Timed voiding
|
RCT QRCT | Cochrane Incontinence Specialised Register – 2 April 2009 MEDLINE – January 1966 to November 2003 (performed 15 November 2003) Embase – 1980–2002 week 18 (9 May 2002) PsycINFO – January 1972 to August 2002 (August 2002) CINAHL – January 1982 to February 2001 (performed in March 2001) Biological abstracts – January 1980 to December 2000 (performed March 2001) Current Contents – January 1993–2001 (performed March 2001) DARE – Issue 1, 2001 |
| Rai 2012 | To compare the effects of anticholinergic drugs with various non‐pharmacological therapies for non‐neurogenic OAB syndrome in adults. | Men and women with idiopathic OAB syndrome or UUI (symptomatic or urodynamic diagnosis, or both) Age not provided in review and often not in individual trials |
Anticholinergic drug | Anticholinergic drugs
|
RCT QRCT | Cochrane Incontinence Specialised Register – 4 September 2012 |
| Saraswat 2020 | To assess the effects of traditional suburethral sling procedures for treatment of urodynamic SUI (urodynamic diagnosis), or for symptoms of SUI or MUI (clinical diagnosis) in women. | Women with SUI due to hypermobility or intrinsic sphincter deficiency (or both, diagnosed clinically or with urodynamics, or with MUI. Age not provided in review or often in individual trials |
Traditional suburethral sling procedures to treat SUI or MUI | Traditional suburethral sling operation
|
RCT QRCT | Cochrane Incontinence Specialised Register – 27 February 2017 (quote: "A further updated search was conducted on 23 January 2019, the results of which were not fully incorporated into the review.") |
| Stewart 2016 | To determine the effectiveness of ES | Adults aged ≥ 18 years, or according to study authors' definitions of adult) with:
Age reported in review 46–70 years, though 9 trials did not report participants' ages. Some trials included men and women but majority women. |
Neuromodulation with ES targeting specific nerves in the sacral plexus that control pelvic floor function. Routes were rectal, vaginal and posterior tibial nerve |
ES
|
RCT QRCT |
Cochrane Incontinence Specialised Register – December 2014 |
| Stewart 2017 | To assess the effects of ES with non‐implanted devices, alone or in combination with other treatment, for managing SUI or stress‐predominant MUI in women. | Women with SUI or stress‐predominant MUI on the basis of symptoms, signs or urodynamic diagnosis. | ES with non‐implanted devices | ES
|
RCT QRCT |
Cochrane Incontinence's Specialised Register – 27 February 2017 Additional searches conducted for a brief economic commentary – 10 February 2016 |
| Wallace 2004 | To assess the effects of bladder training on UI, however that diagnosis was made | Men and women with UI Age not reported in review Range from individual trials 19–68 years All participants were women except in 1 trial |
Bladder training; the terms bladder retraining, bladder drill or bladder re‐education were assumed to be synonymous with bladder training. | Bladder training
|
RCT QRCT | Cochrane Incontinence Specialised Register – 15 March 2006 |
| Wang 2013 | To determine the effects and safety of acupuncture for SUI in adults. | People of any age or ethnicity, with a diagnosis of SUI (according to the definition of the International Continence Society) were eligible for inclusion. Mean age 52 years All women |
Scalp acupuncture, body acupuncture, electroacupuncture, warm acupuncture, elongated needle, auricular acupuncture and fire needle. | Acupuncture
|
RCT QRCT | Cochrane Incontinence Specialised Register – 28 January 2013 Embase – 20 February 2013 AMED – 20 February 2013 Chinese Biomedical Literature Database – 20 February 2013 Chinese Acupuncture Trials Register – 20 February 2013 China National Knowledge Infrastructure – 20 February 2013 |
| Wieland 2019 | To assess the effects of yoga for treating UI in women. | Women aged ≥ 18 years diagnosed with UI on the basis of symptoms, signs or urodynamic evaluation. | Yoga (any yoga tradition but excluded studies in which the yoga intervention did not include a physical practice component). | Yoga
|
RCT | Cochrane Incontinence's Specialised Register – 21 June 2018 Cochrane Complementary Medicine Field Specialised Register – 21 June 2018 Additional searches conducted for an economic evaluation – 22 January 2019 |
ES: electrical stimulation; FDA: Food and Drug Administration; MUI: mixed urinary incontinence; OAB: overactive bladder; PFMT: pelvic floor muscle training; QRCT: quasi‐randomised controlled trial; RCT: randomised controlled trial; SNRI: serotonin and noradrenaline reuptake inhibitors; SUI: stress urinary incontinence; UI: urinary incontinence; UUI: urge urinary incontinence; WHO: World Health Organization.
2. Characteristics of included reviews: results.
| Study ID | Intervention focus | Included studies (number that contained a conservative intervention) | Participant details1, for participants within studies containing a conservative intervention | ||||
| n | Age (years) | Sex | Pregnancy as an inclusion or exclusion criteria? | Type of UI | |||
| Alhasso 2005 | To determine the effects of adrenergic agonists in the treatment of SUI | 22 (2) | 218 | Range 30–90 | 100% F | No | SUI |
| Ayeleke 2015 | To compare the effects of pelvic floor muscle training + another active treatment vs the same active treatment alone in the management of women with UI | 13 (13) | 1164 | Range 18–75 | 100% F | No | SUI MUI UUI |
| Cody 2012 | To assess the effects (both beneficial and harmful) of oestrogen therapy used for the treatment of UI | 34 (3) | 192 | Not reported | 100% F | Not reported | AUI |
| Dumoulin 2018 | To determine the effects of PFMT for women with UI vs no treatment, placebo or sham treatments, or other inactive control treatments | 31 (31) | 1871 | 18 trials restricted participation based on ages. Lowest age limit 13 years. No upper age limit in several trials. | 100% F | No | SUI 18 trials MUI 1 trial UUI 1 trial AUI 11 trials |
| Duthie 2011 | To compare intravesical botulinum toxin injection with other treatments for neurogenic and idiopathic OAB in adults with or without incontinence | 19 (0) | 0 | — | — | — | — |
| Eustice 2000 | To determine the effects of prompted voiding for the management of UI | 9 (9) | 674 | Mean age 84 Range 69.3–92.4 |
100% female | No | Unclear |
| Freites 2019 | To assess the effects of laparoscopic colposuspension for UI in women; and summarise the principal findings of relevant economic evaluations of these interventions | 26 (0) | 0 | — | — | — | — |
| Glazener 2017a | To determine the effects of anterior vaginal repair (anterior colporrhaphy) on SUI or mixed UI in women | 10 (1) | 50 | Mean 48 Range 31–66 |
100% female | Not reported | SUI |
| Glazener 2017b | To determine the effects of needle suspension on SUI or MUI in comparison with other management options | 10 (0) | 0 | — | — | — | — |
| Hay‐Smith 2011 | To compare the effects of different approaches to pelvic floor muscle training for women with UI | 21 (1 trial with 3 arms)(21) | 1490 | Mean 35.9–58.4 (SD 10.8) Range 36–80 (possibly) |
100% female | No | SUI UUI MUI |
| Herbison 2009 | To determine the effects of implantable ES devices in the treatment of urine storage and voiding problems | 8 (0) | — | — | — | — | — |
| Herbison 2013 | To determine the effectiveness of vaginal cones in the management of female SUI | 23 studies 7 abstracts only, 1 ongoing (23) |
1806 | Not stated | 100% female | No | SUI 22 Unclear 1 |
| Herderschee 2011 | To determine whether feedback (including biofeedback) provides additional benefit to PFMT in women with UI (SUI, UUI or MUI), regardless of cause | 24 (24) | 1583 | All ages | Assume 100% female | No | SUI MUI UUI |
| Imamura 2015 | To determine the effectiveness of specific lifestyle interventions (i.e. weight loss; dietary changes; fluid intake; reduction in caffeinated, carbonated and alcoholic drinks; avoidance of constipation; stopping smoking; and physical activity) in the management of adult UI | 11 (11) | 5974 | 49–58 (quotes: "unclear if this was a mean or median"), "except for two trials with means of 62.6 and 70.25 years" |
100% female | Not an exclusion criteria | SUI MUI UUI |
| Kang 2015 | To evaluate the efficacy of transurethral radiofrequency collagen denaturation, compared with other interventions, in the treatment of women with UI | 1 (0) | — | — | — | — | — |
| Kirchin 2017 | To determine the effects of periurethral and transurethral bulking agents on cure or improvement of UI in women. | 35 (1) | 47 | Not reported | 100% female | Not reported | SUI |
| Lapitan 2017 | To determine the effects of open retropubic colposuspension for the treatment of UI in women | 55 (2) | 120 | 31–66 years in 1 study; not reported in 1 study | 100% female | Not reported | SUI |
| Lipp 2014 | To determine the effects of mechanical devices in the management of adult female UI, particularly SUI | 8 (8) | 787 | Range 30–75 | 100% female | No | SUI UUI Other |
| Mariappan 2005 | To determine the effects of SNRI in the management of SUI and MUI that includes SUI in adults | 10 (1) | 201 (possibly) | Range 18–75 | 100% female (note: selection criteria included both sexes but data only available for female) |
Exclusion | MUI SUI |
| Nambiar 2017 | To assess the effectiveness of mini‐sling procedures in women with urodynamic clinical stress or MUI in terms of improved continence status, quality of life or adverse events. | 31 (0) | 0 | — | — | — | — |
| Ostaszkiewicz 2004a | To assess the effects of habit retraining for the management of UI in adults | 4 (4) | 378 | Mean 80 | Analysis on females | No | UUI MUI Unclear |
| Ostaszkiewicz 2004b | To assess the effects of timed voiding for the management of urinary incontinence in adults | 2 (2) | 298 | Mean 86.7 | 100% female | No | UUI MUI (possibly) |
| Rai 2012 | To compare the effects of anticholinergic drugs with various non‐pharmacological therapies for non‐neurogenic OAB syndrome in adults | 23 (23) | 3695 | 6 had male and female 17 had only female | Not reported | Not reported | UUI |
| Saraswat 2020 | To assess the effects of traditional suburethral sling procedures for treatment of urodynamic SUI | 34 (0) | 0 | — | — | — | — |
| Stewart 2016 | To determine the effectiveness of ES with non‐implanted electrodes in comparison with placebo or any other active treatment in adults with OAB, with or without UUI | 51 (51) | 3443 | All trials included adults only. 1 trial included only participants aged > 65 years; mean age reported in this trial was 84 years. 9 trials did not report participants' age. Across the remaining trials, mean age ranged from 46 to 70 | 36/51 female only 11/51 male and female 1/51 male only 3/51 not reported |
Not an exclusion criteria | OAB UUI MUI |
| Stewart 2017 | To assess the effects of ES with non‐implanted devices, alone or in combination with other treatment, for managing SUI or stress‐predominant MUI in women | 56 (56) | 3781 | Mean range 41–69 | 100% female | Not reported | SUI MUI AUI |
| Wallace 2004 | To assess the effects of bladder training on UI, however that diagnosis was made | 12 | 1473 | 5 trials no age restriction Remaining trials 35–65 |
11/12 female | No | SUI UUI MUI |
| Wang 2013 | Determine the effects and safety of acupuncture for SUI in adults | 1 | 60 | Mean 53.8 | 100% female | Not reported | SUI |
| Wieland 2019 | To assess the effects of yoga for treating UI in women. | 2 (2) | 49 | Range 22–79 | 100% female | 1 study – pregnancy in last year was an exclusion criterion. 1 study – most were postmenopausal |
UUI AUI |
AUI: all types of urinary incontinence; ES: electrical stimulation; F: female; M: male; MUI: mixed urinary incontinence; n: number of participants; OAB: overactive bladder; PFMT: pelvic floor muscle training; QRCT: quasi‐randomised controlled trial; RCT: randomised controlled trial; SNRI: serotonin and noradrenaline reuptake inhibitors; SUI: stress urinary incontinence; UUI: urgency urinary incontinence. Number of participants are as reported in review text by review authors.1
Fifteen of the 29 included reviews were primarily focused on conservative interventions, while 14 were primarily focused on non‐conservative interventions but contained data (from 'control' groups) that were relevant to the criteria for this overview.
Interventions and comparisons
Physical therapies
Seven reviews focused on interventions categorised as physical therapies. PFMT was the intervention of interest in four reviews (Ayeleke 2015; Dumoulin 2018; Hay‐Smith 2011; Herderschee 2011). Vaginal cones was the intervention in one (Herbison 2013). In Dumoulin 2018, the comparison of interest was PFMT compared to no treatment, placebo or inactive control. In two of the PFMT‐focused reviews, the intervention of interest was different types or ways of delivering PFMT. Hay‐Smith 2011 compared different approaches to the delivery of PFMT, while Herderschee 2011 explored the addition of feedback or biofeedback to PFMT, compared to PFMT alone or PFMT plus a different type of feedback. Ayeleke 2015 compared PFMT combined with another active treatment with the same active treatment. Herbison 2013 explored the effect of vaginal cones delivered alone or in combination with other treatments compared with no treatment or other active interventions (conservative or non‐conservative). Stewart 2016 focused on the effect of electrical stimulation with non‐implanted devices for OAB syndrome and Stewart 2017 focused on electrical stimulation with non‐implanted devices for the management of SUI or predominantly SUI. In both reviews, the electrical stimulation intervention was compared to no active treatment, placebo or sham; to conservative treatments (PFMT); to drug treatments or a combination of these. Herbison 2009 focused on the effects of implantable electrical stimulation for UUI, OAB syndrome and urinary retention.
Thirteen reviews focused on non‐conservative interventions but included (or planned to include) trials in which the comparison comprised physical therapies (Alhasso 2005; Cody 2012; Duthie 2011; Freites 2019; Glazener 2017a; Glazener 2017b; Kang 2015; Kirchin 2017; Lapitan 2017; Mariappan 2005; Nambiar 2017; Rai 2012; Saraswat 2020). Rai 2012 also included trials in which groups received electrical stimulation and combinations of different physical therapies.
Educational, behavioural and lifestyle advice
Five reviews focused on interventions categorised as educational, behavioural or lifestyle advice. Three focused on habit training (Eustice 2000; Ostaszkiewicz 2004a; Wallace 2004). One focused on timed voiding (Ostaszkiewicz 2004b). One focused on lifestyle changes (Imamura 2015). Eustice 2000 compared prompted voiding to no prompting, while Ostaszkiewicz 2004a reported on three trials that tested habit retraining combined with other approaches against usual care and one compared habit retraining alone with habit retraining plus an electronic monitoring device. Wallace 2004 compared bladder training with no bladder training, drugs, PFMT and combinations of these. Ostaszkiewicz 2004a compared timed voiding plus additional interventions with usual care. Imamura 2015 compared weight loss programmes with a control intervention, change in fluid intake with no change and reduction in caffeinated drinks with no change, with one trial comparing a soy‐rich diet with a soy‐free diet.
One review focused on non‐conservative interventions but included some trials in which the comparison was bladder training (Rai 2012).
Mechanical devices
One review focused on the mechanical devices intervention category (Lipp 2014). This review compared a mechanical device with no treatment, one mechanical device with another, and one trial compared three groups: a mechanical device alone, behavioural therapy (PFMT) alone and behavioural therapy combined with a mechanical device.
Complementary interventions
One review focused on an intervention categorised as complementary, where the intervention was acupuncture versus midodrine, a drug for treating hypotension (Wang 2013).
Psychological therapies
None of the reviews focused on an intervention categorised as a psychological therapy.
Other interventions
One reviews focused on yoga (Wieland 2019).
Methodological quality of included reviews
Risk of bias of included reviews
See Table 3 and Figure 3 for a summary of the ROBIS assessments for the included reviews.
3. Risk of bias.
| Reviews | ROBIS Phase 2 | ROBIS Phase 3 signalling questions | ||||||
|
1. Study eligibility criteria |
2. Identification and selection of studies |
3. Data collection and study appraisal |
4. Synthesis and findings | Did the interpretation of findings address all the concerns identified in Domains 1 to 4 | Was the relevance of identified studies to the review's research question appropriately considered? | Did the reviewers avoid emphasising results on the basis of their statistical significance? | Comments relating to Phase 3 signalling questions | |
| Alhasso 2005 | L | L | ?4 | L | PY | PY | PY | — |
| Ayeleke 2015 | L | L | L | H9 | PY | PY | PY | — |
| Cody 2012 | L | L | ?5 | H10 | PN | PY | PY | The concerns relating to domain 4 were not covered in the discussion. |
| Dumoulin 2018 | L | L | L | H11 | PY | PY | PY | — |
| Duthie 2011 | L | L | L | H12 | PN | PY | PY | The concerns relating to study variation have not been adequately discussed. |
| Eustice 2000 | L | ?3 | H6 | H13 | PN | PY | PY | The issues relating to the search (Domain 3) and synthesis (Domain 4) were not addressed in the discussion. |
| Freites 2019 | L | L | L | L | PY | PY | PY | — |
| Glazener 2017a | L | L | L | H14 | PN | PY | PY | Domain 4 concerns were not adequately addressed in the discussion. |
| Glazener 2017b | L | L | L | H15 | PY | PY | PY | — |
| Hay‐Smith 2011 | L | L | L | H16 | PY | PY | PY | — |
| Herbison 2009 | L | L | L | L | PY | PY | PN | The discussion somewhat overemphasises the findings of the review. While authors noted the difficulties in study reporting and the possibility of duplicate publications, the implications of this are not conveyed within the discussion. |
| Herbison 2013 | L | L | L | H17 | PY | PY | PY | — |
| Herderschee 2011 | L | L | L | H18 | PN | PY | PY | Domain 4 concerns were not adequately addressed in the discussion |
| Imamura 2015 | H1 | L | ?7 | L | PN | PY | PY | The concerns relating the data‐driven nature of the review, and the change of criteria noted in Domain 1 were not adequately addressed. |
| Kang 2015 | L | L | L | L | PY | PY | PY | — |
| Kirchin 2017 | L | L | L | H19 | PN | PY | PY | Domain 4 concerns were not addressed in the discussion. |
| Lapitan 2017 | L | L | L | L | PY | PY | PY | — |
| Lipp 2014 | L | L | L | H20 | PY | PY | PY | — |
| Mariappan 2005 | L | L | L | H21 | PY | PY | PY | — |
| Nambiar 2017 | L | L | L | L | PY | PY | PY | — |
| Ostaszkiewicz 2004a | L | L | ?8 | L | PY | PY | PY | — |
| Ostaszkiewicz 2004b | H2 | L | ?8 | L | PY | PY | PY | — |
| Rai 2012 | L | L | L | H22 | PY | PY | PY | — |
| Saraswat 2020 | L | L | L | L | PY | PY | PY | — |
| Stewart 2016 | L | L | L | L | PY | PY | PY | — |
| Stewart 2017 | L | L | L | L | PY | PY | PY | — |
| Wallace 2004 | L | L | L | ?23 | PY | PY | PY | — |
| Wang 2013 | L | L | L | L | PY | PY | PY | — |
| Wieland 2019 | L | L | L | L | PY | PY | PY | — |
| TOTALS | L = 27 H = 2 ? = 0 |
L = 28 H = 0 ? = 1 |
L = 23 H = 1 ? = 5 |
L = 14 H = 14 ? = 1 |
PY = 22 PN = 7 |
PY = 29 PN = 0 |
PY = 28 PN = 1 |
— |
Abbreviations:?: unclear risk of bias; H: high risk of bias; L: low risk of bias; PFMT: pelvic floor muscle training; PN: probably no; PY: probably yes. 1The review authors reported changes to inclusion criteria that were made after the review had started, made because only a low number of studies met the original inclusion criteria. 2Authors identified that the eligibility criteria were difficult to apply: quote: "The review was based on an a priori definition of timed voiding which was developed after an extensive review of the literature; nevertheless we struggled to categorize the interventions used from the descriptions given. Overlap between interventions was found with some interventions having features of more than one approach." 3The process of selection of studies was not fully described. 4There was a lack of clarity about the risk of bias assessment; it was unclear what criteria were used, and only one was reported. 5There was a lack of clarity about the included studies, with poorer details of non‐pharmacological interventions included as comparators. 6Concerns related to the risk of bias assessment – there was a lack of detail, and it appeared to be very limited in nature. 7Only two of the 11 included studies contributed to the analysis. The review authors reported that they tried to obtain the study results but these were not provided for some studies. 8There was a lack of information relating to identification and inclusion of studies (i.e. results of the search), and how risk of bias was assessed and by whom (what criteria were assessed). 9The authors identified trials at high risk of bias, but did not integrate this information into the narrative text describing and supporting the results. 10It appeared that relevant studies had been excluded from synthesis inappropriately – excluded studies appeared to include studies that would have been relevant but which data were unavailable, or outcomes not relevant. There was also a lack of information about how heterogeneity was explored, and no reported sensitivity analyses to explore risk of bias within trials. 11No sensitivity analyses were conducted in this synthesis. GRADE levels did not seem to have been downgraded in response to small sample size; and often only downgraded one level despite more than one identified risk. 12Between‐study variation and study risk of bias were not considered within the findings. 13The analysis that was conducted was correct, but not complete: it failed to address a number of important issues. It contained very little assessment of heterogeneity or risk of bias, and no attempts to ensure robust analyses. 14Between‐study variation and study risk of bias did not appear to have been considered within the findings. 15No GRADE judgements of certainty of evidence, or systematic exploration of study variation. 16The analysis did not fully explore heterogeneity, neither did it ensure the robustness of findings through funnel plots, etc. There also appeared to be some duplication in the subgroup analyses. 17There was high risk of bias due to lack of blinding and high attrition, but these were not addressed. Although authors stated it was not appropriate to perform sensitivity analyses as there were low numbers of included studies, there were analyses containing five trials that were arguably suitable. 18Heterogeneity and study quality did not appear to have been explored systematically within the synthesis and findings. 19The synthesis process did not address the different trial populations, and no sensitivity analyses were performed. 20There were three included studies with high attrition (Cornu 2012; Nielson 1995; Robinson 2003). This appeared to have been dealt with inconsistently and incompletely, with only data from Nielson 1995 being excluded from part of the synthesis. There was no explanation as to why sensitivity analyses to address risk of bias and heterogeneity were not performed. 21Although sensitivity analyses were described within the review methods, these were not conducted, and no rationale was provided. 22Although the grouping of data within the analysis did function as a sensitivity analysis, the quality of studies, especially in relation to attrition bias was not fully explored. 23The authors described a rigorous analysis plan; however, this was not conducted, which may have been an overly conservative approach. Clear information describing and justifying this decision was not provided.
3.
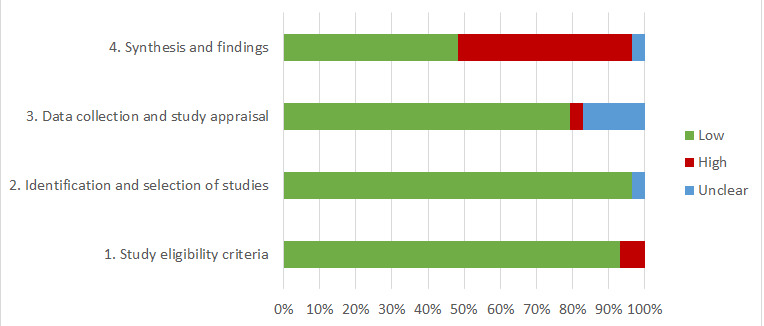
Summary of ROBIS results for Phase 2, identifying concerns about bias in the review process
Risk of bias relating to study eligibility criteria (ROBIS: phase 2, domain 1)
The risk of bias relating to the prespecification and application of study eligibility criteria was low across 27/29 reviews. Only two reviews were judged at high risk of bias in relation to study eligibility criteria (Imamura 2015; Ostaszkiewicz 2004b). Imamura 2015 changed the eligibility criteria after an initial search to increase the number of trials included in the review. In Ostaszkiewicz 2004b, the review authors encountered difficulties applying the eligibility criteria.
Risk of bias relating to identification and selection of studies (ROBIS: phase 2, domain 2)
The risk of bias relating to the identification and selection of studies for inclusion within the review was low across 28/29 reviews. In one review, there was insufficient information about the process with which they selected studies (Eustice 2000).
Risk of bias relating to data collection and study appraisal (ROBIS: phase 2, domain 3)
The risk of bias relating to the method of data collection and study appraisal was low in 23/29 reviews. There were concerns in Eustice 2000 about the comprehensiveness of the assessment of risk of bias of the included trials, and this was judged at high risk of bias. Imamura 2015 reported being unable to obtain all relevant trial data from trial authors, and we judged this at unclear risk of bias. The risk of bias was also unclear for Alhasso 2005, Cody 2012, Ostaszkiewicz 2004a, and Ostaszkiewicz 2004b, with lack of clear details reported in relation to data collection and study appraisal.
Risk of bias relating to synthesis and findings (ROBIS: phase 2, domain 4)
Fourteen reviews were at high risk of bias in relation to the methods and reporting of the syntheses. For the reviews judged at high risk of bias, concerns for 12/14 reviews largely related to lack of exploration of heterogeneity or consideration of risk of bias assessments using subgroup or sensitivity analyses (Ayeleke 2015; Dumoulin 2018; Duthie 2011; Eustice 2000; Glazener 2017a; Glazener 2017b; Hay‐Smith 2011; Herbison 2013; Herderschee 2011; Kirchin 2017; Mariappan 2005; Rai 2012), while concerns for 2/14 reviews related to the studies that were included in (or excluded from) analyses (Cody 2012; Lipp 2014). Of the remaining 15 reviews, 14 were judged at low risk of bias for this domain and, for one, there was insufficient information to make a judgement (Wallace 2004).
Risk of bias of the systematic review (ROBIS phase 3)
As discussed in the Methods, overview authors were unable to reach consensus on judgements relating to the interpretation of the review findings. The agreed responses to the ROBIS phase 3 signalling questions are reported rather than an overall judgement of risk of bias for each review (see Table 3). However, the signalling questions identified that there were no serious concerns for 21 reviews (Alhasso 2005; Ayeleke 2015; Dumoulin 2018; Freites 2019; Glazener 2017b; Hay‐Smith 2011; Herbison 2013; Kang 2015; Lapitan 2017; Lipp 2014; Mariappan 2005; Nambiar 2017; Ostaszkiewicz 2004a; Ostaszkiewicz 2004b; Rai 2012; Saraswat 2020; Stewart 2016; Stewart 2017; Wallace 2004; Wang 2013; Wieland 2019).
There were some concerns relating to the interpretation of the review findings for the remaining eight reviews. Of these, there were concerns in seven reviews that the interpretation of the findings did not address all of the concerns relating to bias in the review process (Cody 2012; Duthie 2011; Eustice 2000; Glazener 2017a; Herderschee 2011; Imamura 2015; Kirchin 2017). In one, there were concerns that the review authors may have emphasised results on the basis of their statistical significance (Herbison 2009; see Table 3).
Quality and quantity of evidence in included reviews
Seven reviews contained no trials with data relevant to the criteria for this overview (Duthie 2011; Freites 2019; Glazener 2017b; Herbison 2009; Kang 2015; Nambiar 2017; Saraswat 2020). Four reviews pooled data from relevant trials within analyses but did not have any analyses relating to the primary outcomes for this overview (Cody 2012; Eustice 2000; Ostaszkiewicz 2004a; Ostaszkiewicz 2004b). From the remaining 18 reviews, we extracted data on every relevant comparison for which there was an analysis relating to one of our primary outcomes of woman's observations of symptomatic cure or improvement of UI or condition‐specific quality of life.
We extracted data from 192 analyses relating to one of our primary outcomes: 134 analyses relating to woman's observation of symptomatic cure or improvement and 58 analyses relating to condition‐specific quality of life. Eighty‐one per cent of these analyses only contained one trial. These analyses contained data from 112 unique trials (which included 8975 women); data from 17 of these trials were included in more than one review (see Table 4).
4. Trials included within reviews.
We assessed the certainty of evidence synthesised for each of these extracted analyses using the GRADE approach, and summarise these results below.
Stress urinary incontinence
Fourteen reviews presented analyses relating to primary outcome data in populations of women with SUI (Alhasso 2005; Ayeleke 2015; Dumoulin 2018; Glazener 2017a; Hay‐Smith 2011; Herbison 2013; Herderschee 2011; Kirchin 2017; Lapitan 2017; Lipp 2014; Mariappan 2005; Stewart 2017; Wallace 2004; Wang 2013). These 14 reviews contained 84 analyses relating to a primary outcome relevant to this overview: 17 compared a conservative intervention with control; 54 compared one conservative intervention with another conservative intervention; and 13 compared a conservative intervention with a non‐conservative intervention.
Table 5 illustrates the number of relevant analyses within these reviews and the judgement of certainty of evidence for each of these analyses. Of the 84 analyses, seven were high‐certainty, 42 were moderate‐certainty, 30 were low‐certainty and one was very low‐certainty. For four of the analyses, the effect was not estimable and we did not assign a certainty of evidence grade.
5. Stress urinary incontinence: quantity and certainty of evidence.
| Comparison | Outcome | Certainty of the evidence | Not estimable | Total analyses | Table | |||
| High | Moderate | Low | Very low | |||||
|
Conservative vs control |
Cure or improvement |
2 | 1 | 2 | 0 | 0 | 5 | Table 8 |
| Quality of life | 1 | 5 | 6 | 0 | 0 | 12 | Table 9 | |
|
Conservative vs conservative |
Cure or improvement |
3 | 22 | 15 | 1 | 2 | 43 | Table 10 |
| Quality of life | 0 | 6 | 4 | 0 | 1 | 11 | Table 11 | |
|
Conservative vs non‐conservative |
Cure or improvement |
0 | 6 | 3 | 0 | 0 | 9 | Table 12 |
| Quality of life | 1 | 2 | 0 | 0 | 1 | 4 | Table 13 | |
| TOTALS | 7 | 42 | 30 | 1 | 4 | 84 | ||
Urgency urinary incontinence
Five reviews presented analyses relating to a primary outcome in populations of women with UUI (Ayeleke 2015; Herderschee 2011; Rai 2012; Stewart 2016; Wallace 2004). However, Stewart 2016 was the only review to present any data relating to quality of life.
These five reviews contained 47 analyses relating to a primary outcome relevant to this overview: eight comparing a conservative intervention with control; 14 comparing one conservative intervention with another conservative intervention; and 25 comparing a conservative intervention with a non‐conservative intervention.
Table 6 illustrates the number of relevant analyses within these reviews and the judgement of certainty of evidence for each of these analyses. Of the 47 analyses, four were high‐certainty evidence, 25 were moderate‐certainty evidence and 18 were low‐certainty evidence.
6. Urgency urinary incontinence: quantity and certainty of evidence.
| Comparison | Outcome | Certainty of the evidence | Not estimable | Total analyses | Table | |||
| High | Moderate | Low | Very low | |||||
|
Conservative vs control |
Cure or improvement |
2 | 4 | 1 | 0 | 0 | 7 | Table 14 |
| Quality of life | 0 | 1 | 0 | 0 | 0 | 1 | Table 15 | |
|
Conservative vs conservative |
Cure or improvement |
0 | 7 | 3 | 0 | 0 | 10 | Table 16 |
| Quality of life | 1 | 2 | 1 | 0 | 0 | 4 | Table 17 | |
|
Conservative vs non‐conservative |
Cure or improvement |
0 | 9 | 13 | 0 | 0 | 22 | Table 18 |
| Quality of life | 1 | 2 | 0 | 0 | 0 | 3 | Table 19 | |
| TOTALS | 4 | 25 | 18 | 0 | 0 | 47 | ||
All types of urinary incontinence
Thirteen reviews presented analyses relating to a primary outcome in populations of women with AUI (Alhasso 2005; Ayeleke 2015; Dumoulin 2018; Hay‐Smith 2011; Herbison 2013; Herderschee 2011; Imamura 2010; Lipp 2014; Rai 2012; Stewart 2016; Stewart 2017; Wallace 2004; Wieland 2019). These 13 reviews contained 61 relevant analyses: 16 comparing a conservative intervention with control; 40 comparing one conservative intervention with another conservative intervention and five comparing a conservative intervention with a non‐conservative intervention.
Table 7 illustrates the number of relevant analyses within these reviews and the judgement of certainty of evidence for each. Of the 61 analyses, six were high‐certainty evidence, 14 were moderate‐certainty evidence, 32 were low‐certainty evidence and nine were very low‐certainty evidence.
7. All types of urinary incontinence: quantity and certainty of evidence.
| Comparison | Outcome | Certainty of the evidence | Not estimable | Total analyses | Table | |||
| High | Moderate | Low | Very low | |||||
|
Conservative vs control |
Cure or improvement |
3 | 4 | 3 | 1 | 0 | 11 | Table 20 |
| Quality of life | 2 | 2 | 0 | 1 | 0 | 5 | Table 21 | |
|
Conservative vs conservative |
Cure or improvement |
1 | 3 | 14 | 6 | 0 | 24 | Table 22 |
| Quality of life | 0 | 3 | 12 | 1 | 0 | 16 | Table 23 | |
|
Conservative vs non‐conservative |
Cure or improvement |
0 | 1 | 2 | 0 | 0 | 3 | Table 24 |
| Quality of life | 0 | 1 | 1 | 0 | 0 | 2 | Table 25 | |
| TOTALS | 6 | 14 | 32 | 9 | 0 | 61 | ||
Effect of interventions
This section reports the analyses identified to provide evidence relating to the effects of interventions for the primary outcomes of patient‐reported cure or improvement and condition‐specific quality of life for different types of UI and different comparators. This presents the results of the extracted data relating to SUI (84 analyses; see Table 5), UUI (47 analyses; see Table 6), and AUI (61 analyses; see Table 7).
For each of the outcome subsections, corresponding data are presented in a table. Where analyses were judged to provide low‐ or very low‐certainty evidence, a narrative description of the intervention comparisons was not provided in the text and readers are directed to the tables for this level of information.
Stress urinary incontinence
Any conservative intervention versus control, placebo or standard care
Symptomatic cure or improvement
For more information, see Table 8.
8. Stress urinary incontinence: primary outcome participant‐reported cure or improvement; conservative versus control.
| Analysis code (in review) | Study ID |
Comparisons included |
Timing of measure |
Included trials (n) |
Effect measure |
Effect estimate (CI) |
Direction of effect | Evidence of beneficial effect? |
Number of downgrades (reason for downgrade) |
| High‐certainty evidence | |||||||||
| 1.1.1 | Herbison 2013 | Cones vs control | IM |
Bø 19991 (n = 57) |
RR | 0.4 (0.2 to 0.6) | > 1 favours control | YES for cones | 0 |
| 1.2.2 | Herderschee 2011 | PFMT + BF vs PFMT alone (control) |
IM |
Goode 2003 (n = 87) |
RR | 0.6 (0.4 to 0.9) | > 1 favours PFMT alone | YES for PFMT and BF | 0 |
| Moderate‐certainty evidence | |||||||||
| 1.2.1 | Dumoulin 2018 | PFMT vs no treatment, placebo or control | IM |
Asklund 2017; Bø 19991; Lagro‐Janssen 1992 (n = 242) |
RR | 6.3 (3.9 to 10.3) |
> 1 favours PFMT | YES for PFMT | 1(H) |
| Low‐certainty evidence | |||||||||
| 3.2.1 | Hay‐Smith 2011 | Direct vs indirect methods of PFMT | IM |
Schagen van Leeuwen 2004; Ramsay 1990 (n = 138) |
RR | 0.7 (0.47 to 1.0) |
> 1 favours indirect | NO | 6(E,F,H×2) |
| 2.2 | Stewart 2017 | ES vs sham treatment | IM | Hofbauer 1990Laycock 1993; Luber 1997; Terlikowski 2013; Whitmore 1995 (n = 236) | RR | 2.03 (1.02 to 4.07) | > 1 favours ES | YES for ES | GRADE as assessed by review authors |
1Bø 1999 was a four‐arm randomised controlled trial in which the groups were: control, PFMT, cones and ES. Data from PFMT and control arms were included in Dumoulin 2018, and data from cones and control arms were included in Herbison 2013. Abbreviations: BF: biofeedback; CI: confidence interval; ES: electrical stimulation; IM: immediate; n: number of participants assessed NOT to have been cured or improved using a variety of different assessment methods; PFMT: pelvic floor muscle training; RR risk ratio. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
Five analyses from five Cochrane Reviews present data on symptomatic cure and improvement in analyses comparing a conservative intervention with a control intervention (Dumoulin 2018; Hay‐Smith 2011; Herbison 2013; Herderschee 2011; Stewart 2017). There were 11 unique trials that compared a conservative intervention with a control intervention, with a cure or improvement outcome, at an immediate time point.
High‐ or moderate‐certainty evidence
Three analyses provided moderate‐ or high‐certainty evidence that PFMT had a beneficial effect on outcome compared to control (moderate‐certainty) and PFMT plus biofeedback had a beneficial effect on outcome compared to control (high‐certainty). Cones had a beneficial effect on outcome compared to control (high‐certainty).
Low‐ or very low‐certainty evidence
Two analyses provided low‐certainty evidence. Hay‐Smith 2011 described this analysis as a comparison of direct and indirect methods of delivering PFMT. Overview authors considered that the indirect methods delivered within the included trials met the criteria for being a control (or no treatment) intervention.
Condition‐specific quality of life
For more information, see Table 9.
9. Stress urinary incontinence: quality of life, conservative versus control.
| Analysis code (in review) | Study ID | Comparisons included | Timing of measure | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| High‐certainty evidence | |||||||||
| 1.12.1 | Dumoulin 2018 | PFMT vs no treatment, placebo or control (I‐QoL) | IM |
Castro 2008 (n = 50) |
MD | −24.6 (−37.7 to −11.4) | > 0 favours control | YES favours PFMT | 0 |
| Moderate‐certainty evidence | |||||||||
| 1.5.1 | Dumoulin 2018 | PFMT vs no treatment, placebo or control | IM |
Beuttenmuller 2010; Carneiro 2010; Nascimento‐Correia 20122 (n = 145) |
MD | −11.89 (−20.5 to −3.2) | > 0 favours control | YES favours PFMT | 2(H×2) |
| 1.5 | Lipp 2014 | Intravaginal mechanical device vs no treatment | UC |
Cornu 20123 (n = 55) |
MD | −2.2 (−3.5 to −0.9) | > 0 favours no treatment | YES favours device | 1(C) |
| 1.6 | Lipp 2014 | Intravaginal mechanical device vs no treatment | UC |
Cornu 20123 (n = 55) |
MD | −1.67 (−2.8 to −0.5) | > 0 favours no treatment | YES favours device | 1(C) |
| 1.7 | Lipp 2014 | Intravaginal mechanical device vs no treatment | UC |
Cornu 20123 (n = 55) |
MD | −0.5 (−0.9 to −0.1) | > 0 favours no treatment | YES favours device | 1(C) |
| 1.3 | Stewart 2017 | ES vs no active treatment | IM | Correia 2013; Correia 2014; Lopès 2014; Pereira 2012 (n = 250) | SMD | −0.72 (−0.99 to −0.45) | < 0 favours ES | YES for ES | GRADE as assessed by review authors |
| Low‐certainty evidence | |||||||||
| 1.3.1 | Dumoulin 2018 | PFMT vs no treatment, placebo or control | IM |
Beuttenmuller 2010; Carneiro 2010; Nascimento‐Correia 20122 (n = 145) |
MD | −13.1 (−21.1 to −5.2) | > 0 favours control | YES favours PFMT | 4(F×2, H×2) |
| 1.4.1 | Dumoulin 2018 | PFMT vs no treatment, placebo or control | IM |
Beuttenmuller 2010; Carneiro 2010; Nascimento‐Correia 20122 (n = 145) |
MD | −11.8 (−20.8 to −2.7) | > 0 favours control | YES favours PFMT | 4(F×2, H×2) |
| 1.8.1 | Dumoulin 2018 | PFMT vs no treatment, placebo or control | IM |
Beuttenmuller 2010; Carneiro 2010; Nascimento‐Correia 20122 (n = 145) |
MD | 1.8 (−3.4 to 7.0) | > 0 favours control | NO | 4(E×2, H×2) |
| 1.6.1 | Dumoulin 2018 | PFMT vs no treatment, placebo or control | IM |
Bø 19991 (n = 55) |
RR | 0.8 (0.6 to 1.1) | > 1 favours PFMT | NO | 3(C, E×2) |
| 1.10.1 | Dumoulin 2018 | PFMT vs no treatment, placebo or control | IM | McLean 2013 (n = 35) | MD | −19.70 (−30.63 to −8.77) | > 0 favours control | YES favours PFMT | 3 (E×2, H) |
| 1.8 | Lipp 2014 | Intravaginal mechanical device vs no treatment | UC |
Cornu 20123 (n = 46) |
MD | −10.3 (−20.77 to 0.17) | > 0 favours no treatment | NO | 3(C, E×2) |
1Bø 1999 used the Bristol Female Lower Urinary Tract Symptoms questionnaire and this was reported as event data within the review (Dumoulin 2018). 2Beuttenmuller 2010; Carneiro 2010; Nascimento‐Correia 2012 – these three trials each present individual subscales for Kings Health Questionnaire (subscales of severity, impact, physical limitation and general health) and these pooled totals are presented in the tables. 3Cornu 2012 – the time point at which outcomes were measured was unclear. Abbreviations: CI: confidence interval; ES: electrical stimulation; I‐QoL: Incontinence Quality of Life; IM: immediate; MD: mean difference; n: number of participants; n: number of participants; PFMT: pelvic floor muscle training; RR: risk ratio; SMD: standardised mean difference; UC: unclear. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
Twelve analyses from three reviews assessed quality of life in analyses comparing a conservative intervention with a control intervention (Dumoulin 2018; Lipp 2014; Stewart 2017). Eight analyses measured the outcome immediately after the intervention. For the remaining four, the timing of outcome assessment was unclear. Across the three reviews, there were 10 unique trials assessing quality of life that compare a conservative intervention with a control intervention.
High‐ or moderate‐certainty evidence
One analysis provided high‐certainty evidence and five analyses provided moderate‐certainty evidence of a beneficial effect.
PFMT was more beneficial than control using the I‐QoL scale (high‐certainty) and the Kings Health Questionnaire (Physical Limitation subscale) (moderate‐certainty).
Intravaginal mechanical device was more beneficial than control using the Urinary Symptoms Profile – SUI subscore, Urinary Symptom Profile Questionnaire OAB subscore and the Urinary Symptom Profile Questionnaire Dysuria subscore (all moderate‐certainty).
Electrical stimulation using non‐implanted electrodes was more beneficial than no active treatment for a pooled measure of incontinence‐specific quality of life (moderate‐certainty).
Low‐ or very low‐certainty evidence
Six analyses provided low‐certainty evidence.
One conservative intervention versus another conservative intervention
Symptomatic cure or improvement
For more information, see Table 10.
10. Stress urinary incontinence: cure or improved, conservative versus conservative.
| Analysis code (in review) | Study ID | Comparisons included | Timing of measure |
Included trials (n) |
Effect measure |
Effect estimate (CI) |
Direction of effect | Evidence of beneficial effect? |
Number of downgrades (reason for downgrade) |
| High‐certainty evidence | |||||||||
| 2.1.1 | Herbison 2013 | Cones vs PFMT | IM |
Bø 19991 (n = 52) |
RR | 4.6 (1.1 to 19.1) | > 1 favours PFMT | YES favours PFMT | 0 |
| 8.1.1 | Lipp 2014 | Intravaginal pessary alone vs pessary + PFMT | IM |
Richter 20071 (n = 299) |
RR | 0.7 (0.6 to 0.9) |
> 1 favours pessary alone | YES favours PFMT + pessary | 0 |
| 7.1.2 | Lipp 2014 | Intravaginal pessary vs behavioural therapy (PFMT) alone | IM |
Richter 20071 (n = 295) |
RR | 0.7 (0.5 to 0.9) |
> 1 favours device | YES favours PFMT | 0 |
| Moderate‐certainty evidence | |||||||||
| 6.1.2 | Ayeleke 2015 | PFMT + continence pessary vs continence pessary alone | FU1 |
Richter 2007 (n = 207) |
RR | 0.9 (0.7 to 1.1) | > 1 favours PFMT | NO | 2(E×2) |
| 6.3.3 | Ayeleke 2015 | PFMT + continence pessary vs continence pessary alone | FU2 | Richter 2007 | RR | 0.9 (0.7 to 1.2) | > 1 favours PFMT | NO | 2(E×2) |
| 11.1.1 | Hay‐Smith 2011 | PFMT and adherence strategy vs PFMT alone | IM |
Sugaya 20032 (n = 41) |
RR | 0.6 (0.38 to 0.9) | > 1 favours PFMT + adherence | YES favours PFMT + adherence | 1(B) |
| 12.2.2 | Hay‐Smith 2011 | More‐intensive vs less‐intensive PFMT programmes | IM |
Diniz Zanetti 20072 (n = 44) |
RR | 0.3 (0.2 to 0.7) | > 1 favours more‐intense PFMT | YES favours more‐intense PFMT | 1(H) |
| 8.2.2 | Hay‐Smith 2011 | Strength and motor learning vs motor learning PFMT alone | IM |
Hay‐Smith 20022 (n = 123) |
RR | 0.6 (0.3 to 1.4) | > 1 favours less intensive | NO | 2(E×2) |
| 2.1.1 | Herbison 2013 | Cones vs PFMT | IM |
Cammu 19983 (n = 60) |
RR | 0.9 (0.5 to 1.6) | > 1 favours PFMT | NO | 2(E×2) |
| 7.1.1 | Lipp 2014 | Intravaginal pessary vs behavioural therapy (PFMT | IM |
Richter 20071 (n = 295) |
RR | 0.8 (0.6 to 1.0) | > 1 favours device | NO | 1(E) |
| 7.1.3 | Lipp 2014 | Intravaginal pessary vs behavioural therapy (PFMT | FU1 |
Richter 2007 (n = 295) |
RR | 1.0 (0.8 to 1.3) | > 1 favours device | NO | 1(E) |
| 7.1.4 | Lipp 2014 | Intravaginal pessary vs behavioural therapy (PFMT | FU2 |
Richter 2007 (n = 295) |
RR | 0.9 (0.7 to 1.3) | > 1 favours device | NO | 1(E) |
| 7.1.6 | Lipp 2014 | Intravaginal pessary vs behavioural therapy (PFMT | FU2 |
Richter 2007 (n = 295) |
RR | 0.9 (0.7 to 1.2) | > 1 favours device | NO | 1(E) |
| 8.1.3 | Lipp 2014 | Intravaginal pessary alone vs pessary + PFMT | FU1 |
Richter 2007 (n = 299) |
RR | 0.9 (0.7 to 1.1) | > 1 favours pessary alone | NO | 1(E) |
| 8.1.4 | Lipp 2014 | Intravaginal pessary alone vs pessary + PFMT, | FU2 |
Richter 2007 (n = 299) |
RR | 0.9 (0.7 to 1.3) | > 1 favours pessary alone | NO | 1(E) |
| 8.1.6 | Lipp 2014 | Intravaginal pessary alone vs pessary + PFMT, | FU2 |
Richter 2007 (n = 299) |
RR | 1.0 (0.7 to 1.3) | > 1 favours pessary alone | NO | 1(E) |
| 9.1.1 | Lipp 2014 | Pessary + PFMT vs behavioural therapy (PFMT) alone | IM |
Richter 20071 (n = 296) |
RR | 1.0 (0.5 to 1.3) | > 1 favours pessary + PFMT | NO | 1(E) |
| 9.1.3 | Lipp 2014 | Pessary + PFMT vs behavioural therapy (PFMT) alone | FU1 |
Richter 2007 (n = 296) |
RR | 1.1 (0.91 to 1.4) | > 1 favours pessary + PFMT | NO | 1(E) |
| 9.1.4 | Lipp 2014 | Pessary + PFMT vs behavioural therapy (PFMT) alone | FU2 |
Richter 2007 (n = 296) |
RR | 1.0 (0.7 to 1.4) | > 1 favours pessary + PFMT | NO | 1(E) |
| 9.1.6 | Lipp 2014 | Pessary + PFMT vs behavioural therapy (PFMT) alone | FU2 |
Richter 2007 (n = 296) |
RR | 0.9 (0.7 to 1.3) | > 1 favours pessary + PFMT | NO | 1(E) |
| 9.1.2 | Lipp 2014 | Pessary + PFMT vs behavioural therapy (PFMT) alone | IM |
Richter 20071 (n = 296) |
RR | 0.9 (0.7 to 1.1) | > 1 favours device | NO | 1(E) |
| 7.1.5 | Lipp 2014 | Intravaginal pessary vs behavioural therapy (PFMT) alone | FU1 |
Richter 2007 (n = 295) |
RR | 0.9 (0.6 to 1.1) | > 1 favours pessary alone | NO | 1(E) |
| 8.1.2 | Lipp 2014 | Intravaginal pessary alone vs pessary + PFMT, | IM |
Richter 20071 (n = 299) |
RR | 0.7 (0.5 to 1.0) | > 1 favours pessary alone | NO | 1(E) |
| 8.1.5 | Lipp 2014 | Intravaginal pessary alone vs pessary + PFMT | FU1 |
Richter 2007 (n = 299) |
RR | 1.1 (0.8 to 1.5) | > 1 favours pessary + PFMT | NO | 1(E) |
| 9.1.5 | Lipp 2014 | Pessary + PFMT vs behavioural therapy (PFMT) alone | FU1 |
Richter 2007 (n = 296) |
RR | 0.8 (0.6 to 1.1) | > 1 favours pessary + PFMT | NO | 1(E) |
| Low‐certainty evidence | |||||||||
| 4.2 | Ayeleke 2015 | PFMT + ES vs ES alone (excluding implanted electrodes) | IM |
Bezerra 20093; Hofbauer 19903 (n = 56) |
RR | 2.1 (0.8 to 5.4) | > 1 favours PFMT + pessary | NO | 4(E×2, H×2) |
| 6.1.1 | Ayeleke 2015 | PFMT + continence pessary vs continence pessary alone | IM |
Richter 20071 (n = 242) |
RR | 1.0 (0.8 to 1.2) | > 1 favours PFMT + pessary | NO | 3(C, E×2) |
| 6.3.1 | Ayeleke 2015 | PFMT + continence pessary vs continence pessary alone | IM |
Richter 20071 (n = 242) |
RR | 1.1 (0.9 to 1.4) | > 1 favours PFMT + pessary | NO | 3(C, E×2) |
| 6.3.2 | Ayeleke 2015 | PFMT + continence pessary vs continence pessary alone | FU1 |
Richter 2007 (n = 225) |
RR | 1.0 (0.8 to 1.3) | > 1 favours PFMT + pessary | NO | 3(C, E×2) |
| 1.2.1 | Hay‐Smith 2011 | More vs less contact with health professionals | IM | Bø 19902; Diniz Zanetti 20072; Felicíssimo 20102; Konstantinidou 20072 (n = 177) |
RR | 0.3 (0.14 to 0.5) | > 1 favours more contact | YES favours more contact | 3(F×2, H) |
| 2.2.1 | Hay‐Smith 2011 | Group vs individual supervision of PFMT | IM | Bø 19902; Felicíssimo 20102; Konstantinidou 20072 (n = 133) |
RR | 0.1 (0.0 to 0.4) | > 1 favours group | YES, favours group | 3(F×2, H) |
| 2.2.2 | Hay‐Smith 2011 | Group vs individual supervision of PFMT | IM |
de Oliveira 20092 (n = 60) |
RR | 1.2 (0.6 to 2.3) | > 1 favours individual | NO | 3(E×2, H) |
| 4.1.1 | Hay‐Smith 2011 | Individualised vs generic PFMT | IM |
de Oliveira 20092 (n = 60) |
RR | 0.8 (0.4 to 1.6) | > 1 favours generic | NO | 3(E×2, H) |
| 2.1.2 | Herbison 2013 | Cones vs PFMT | IM |
Arvonen 20013; Arvonen 20023 (n = 54) |
RR | 0.8 (0.5 to 1.3) | > 1 favours PFMT | NO | 3(E×2, H) |
| 4.1.1 | Herbison 2013 | Cones + PFMT vs PFMT | IM |
Pieber 19953 (n = 46) |
RR | 1.4 (0.8 to 2.4) | > 1 favours PFMT | NO | 3(E×2, H) |
| 4.2.1 | Herbison 2013 | Cones + PFMT vs PFMT | O |
Pieber 1995 (n = 46) |
RR | 0.9 (0.5 to 1.6) | > 1 favours PFMT | NO | 3(E×2, H) |
| 5.1 | Herbison 2013 | Cones + PFMT vs ES | IM | Berglund 19933; Seo 20043 (n = 160) | RR | 1.5 (0.8 to 2.6) | > 1 favours ES | NO | 3(E×2, H) |
| 3.2 | Stewart 2017 | ES vs PFMT | IM | Bø 1999; Castro 2008; Hahn 1991; Henalla 1989; Hofbauer 1990; Laycock 1988; Aaronson 1995 (n = 244) | RR | 0.85 (0.70 to 1.03) | > 1 favours ES | NO | GRADE as assessed by review authors |
| 4.2 | Stewart 2017 | ES vs vaginal cones | IM | Bridges 1988; Bø 1999; Castro 2008; Oláh 1990; Seo 2004 (n = 331) | RR | 1.09 (0.97 to 1.21) | > 1 favours ES | NO | GRADE as assessed by review authors |
| 6.2 | Stewart 2017 | ES + PFMT vs PFMT | IM | Eyjólfsdóttir 2009; Goode 2003; Hofbauer 1990; Knight 1998; Knight 1998; Tapp 1989; Wilson 1987 (n = 308) | RR | 1.10 (0.95 to 1.28) | > 1 favours ES + PFMT | NO | GRADE as assessed by review authors |
| Very low‐certainty evidence | |||||||||
| 5.2 | Stewart 2017 | ES vs PFMT + vaginal cones | IM | Bourcier 1994; Laycock 1993 (n = 68) | RR | 1.53 (1.08 to 2.18) | > 1 favours ES | YES for ES | GRADE as assessed by review authors |
| Other | |||||||||
| 6.2.1 | Hay‐Smith 2011 | Daily vs 3 times per week PFMT | IM | Sriboonreung 20112 (n = 40) | RR | NE | NE | — | — |
| 9.2 | Hay‐Smith 2011 | PFMT and abdominal muscle exercise vs PFMT alone | IM | Sriboonreung 20112 (n = 40) | RR | NE | NE | — | — |
1Trials comparing the effect of conservative interventions from different intervention categories, with an immediate outcome measure. 2Bø 1999, de Oliveira 2009, Diniz Zanetti 2007, Hay‐Smith 2011, Sriboonreung 2011, Sugaya 2003, Felicíssimo 2010, Konstantinidou 2007 compared different ways of delivering the same intervention. 3Arvonen 2001Arvonen 2002, Bezerra 2009, Cammu 1998, Hofbauer 1990, Pieber 1995, Laycock 1993, and Seo 2004 compared the effect of conservative interventions from within the same intervention categories (physical therapy interventions in all cases). Abbreviations: CI: confidence interval; ES: electrical stimulation; FU1: follow‐up one; IM: immediate; PFMT: pelvic floor muscle training; RR: risk ratio; n: number of participants assessed NOT to have been cured or improved using a variety of different assessment methods; NE: not estimable; O: other.
Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
A total of 43 analyses from five reviews assessed symptomatic cure or improvement by comparing one conservative intervention with another conservative intervention (Ayeleke 2015; Hay‐Smith 2011; Herbison 2013; Lipp 2014; Stewart 2017). Of these, 27 related to immediate outcome assessment. Thirty‐two analyses compared two different conservative interventions and nine compared different ways of delivering the same conservative interventions. A total of 31 trials compared different conservative interventions with a measure of cure or improvement.
High‐ or moderate‐certainty evidence
Three analyses provided high‐certainty evidence and 22 analyses provided moderate‐certainty evidence. Five analyses provided moderate‐ or high‐certainty evidence of a difference between treatment groups, at an immediate time point.
Continence pessary plus PFMT was more beneficial compared to continence pessary alone using the PGI‐I, and PFMT was more beneficial than continence pessary alone, as measured by the Urinary Distress Inventory (UDI) subscale of the Pelvic Floor Distress Inventory (PFDI). Two analyses, both high‐certainty (note: analyses used data from same single trial that did not find a difference between other treatment groups, or using other measures or at follow‐up outcomes – see below) (Richter 2007).
PFMT plus educational/behavioural intervention was more beneficial than cones (high‐certainty).
More‐intensive PFMT was beneficial compared to less‐intensive PFMT (moderate‐certainty).
PFMT plus an adherence strategy was beneficial compared to PFMT alone (moderate‐certainty).
Twenty analyses, providing moderate‐certainty evidence, showed no evidence of a difference between groups.
Strength plus motor learning intervention versus motor learning intervention (moderate‐certainty).
PFMT plus continence pessary versus continence pessary alone, and continence pessary versus PFMT for outcomes assessed using a bladder diary, the PGI‐I and UDIS subscale of the PFDI using both immediate and follow‐up data (18 analyses, all with data from the same single trial (Richter 2007)) (moderate‐certainty).
PFMT versus cones (moderate‐certainty).
Low‐ or very low‐certainty evidence
Eighteen analyses provided low‐ or very low‐certainty evidence, or were not estimable.
Condition‐specific quality of life
For more information, see Table 11.
11. Stress urinary incontinence: quality of life, conservative versus conservative.
| Analysis code (in review) | Study ID | Comparisons included | Timing of measure | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| Moderate‐certainty evidence | |||||||||
| 6.2.2 | Ayeleke 2015 | PFMT added to continence pessary vs continence pessary alone, | FU1 |
Richter 2007 (n = 207) |
RR | 0.8 (0.6 to 1.1) | > 1 favours PFMT + pessary | NO | 2(E×2) |
| 7.4 | Lipp 2014 | Intravaginal pessary vs behavioural therapy (PFMT) | IM |
Richter 2007 (n = 295) |
MD | 0.7 (−9.5 to 10.9) | > 0 favours PFMT | NO | 1(E) |
| 7.5 | Lipp 2014 | Intravaginal pessary vs behavioural therapy (PFMT) | FU1 |
Richter 2007 (n = 295) |
MD | −3.2 (−11.4 to 5.0) | > 0 favours PFMT | NO | 1(E) |
| 7.6 | Lipp 2014 | Intravaginal pessary vs behavioural therapy (PFMT) | FU1 |
Richter 2007 (n = 295) |
MD | −0.2 (−1.3 to 0.9) | > 0 favours PFMT | NO | 1(E) |
| 7.7 | Lipp 2014 | Intravaginal pessary vs behavioural therapy (PFMT) | FU1 |
Richter 2007 (n = 295) |
MD | 0.3 (−0.7 to 1.3) | > 0 favours PFMT | NO | 1(E) |
| 2.3 | Mariappan 2005 | SNRI + conservative non‐pharmacological therapy vs conservative non‐pharmacological therapy alone | IM |
Schagen van Leeuwen 20041 (n = 100) |
OR | 1.3 (0.5 to 2.9) | > 1 favours combination | NO | 2(E×2) |
| Low‐certainty evidence | |||||||||
| 6.2.1 | Ayeleke 2015 | PFMT + continence pessary vs continence pessary alone | IM |
Richter 20071 (n = 242) |
RR | 1.1 (0.8 to 1.5) | > 1 favours PFMT + | NO | 3(C, E×2) |
| 4.3 | Stewart 2017 | ES vs vaginal cones | IM | Castro 2008; Santos 2009 (n = 96) | MD | 1.59 (−3.72 to 6.90) | > 1 favours ES | NO | GRADE as assessed by review authors |
| 10.12.3 | Wallace 2004 | Bladder training + non‐pharmacological treatment vs non‐pharmacological treatment alone | IM |
Wyman 19983 (n = 89) |
MD | −18 (−36.6 to 0.6) | > 0 favours control | NO | 4(E×2, G, H) |
| 5.14.3 | Wallace 2004 | Bladder training vs other behavioural/physical/psychological treatments | IM |
Wyman 19983 (n = 92) |
MD | 18 (−1.4 to 37.3) | > 0 favours control | NO | 3(E×2, G) |
| Other | |||||||||
| 9.3 | Mariappan 2005 | SNRI + conservative non‐pharmacological therapy vs conservative non‐pharmacological | IM | Schagen van Leeuwen 2004 (n = 100) | MD | NE | — | NO | NE |
1Data presented as number of events. 2Data for I‐QOL, effect size was not estimable as the standard deviations are provided as 0. 3These Wyman 1998 data comprised a subgroup of the participants from Wyman 1998: Wyman 1998 included participants with combined SUI, UUI and MUI and all data is presented within reviews for the combined group of participants, except for the two subgroups of data here, which related to participants with SUI only. These Wyman 1998 data related to the Urinary Distress Inventory measure of quality of life, for two pairs from this three‐arm trial (the physical therapy treatment (control) group data are the same for both pairs). Abbreviations: CI: confidence interval; FU1: follow‐up one; IM: immediate; I‐QOL: Incontinence Quality of Life; MD: mean difference; MUI: mixed urinary incontinence; n: number of participants; NE: not estimable; O: other; OR: odds ratio; RR: risk ratio; SNRI: serotonin–noradrenaline reuptake inhibitors; SUI: stress urinary incontinence; UUI: urgency urinary incontinence. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
Eleven analyses from five reviews assessed quality of life comparing one conservative intervention with another conservative intervention (Ayeleke 2015; Lipp 2014; Mariappan 2005; Stewart 2017; Wallace 2004). Seven of these analyses related to an immediate assessment and four to a follow‐up outcome. One of these analyses contained data that meant it was not possible to calculate an effect size. Five unique trials contributed data to these analyses.
High‐ or moderate‐certainty evidence
Six analyses provided moderate‐certainty evidence of no evidence of a difference between treatment groups.
PFMT plus serotonin–noradrenaline reuptake inhibitors (SNRI) was no different from PFMT alone (moderate‐certainty).
PFMT plus continence pessary was no different from continence pessary alone at follow‐up assessment (moderate‐certainty).
Continence pessary was no different from PFMT at immediate or follow‐up assessment (four analyses, moderate‐certainty).
Low‐ or very low‐certainty evidence
Four analyses provided low‐certainty evidence and one was not estimable.
Any conservative intervention versus another active intervention (non‐conservative intervention)
Symptomatic cure or improvement
For more information, see Table 12.
12. Stress urinary incontinence: primary outcome participant‐reported cure or improvement; conservative versus non‐conservative.
| Analysis code (in review) | Study ID | Comparisons included | Timing of measure | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| Moderate‐certainty evidence | |||||||||
| 7.2.1 | Ayeleke 2015 | PFMT added to drug therapy vs drug therapy alone | IM |
Schagen van Leeuwen 20041,2 (n = 90) |
RR | 1.1 (0.8 to 1.5) | > 1 favours PFMT + drug | NO | 2(E×2) |
| 7.4.1 | Ayeleke 2015 | PFMT added to drug therapy vs drug therapy alone | IM |
Schagen van Leeuwen 20041,3 (n = 101) |
RR | 1.3 (0.9 to 1.8) | > 1 favours acupuncture | NO | 2(E×2) |
| 2.1 | Alhasso 2005 | Adrenergic agonist vs conservative therapy | UC |
Ishiko 2000 (n = 34) |
RR | 1.3 (0.7 to 2.2) | > 1 favours drug | NO | 2(E×2) |
| 2.1 | Alhasso 2005 | Adrenergic agonist vs conservative therapy | UC |
Ishiko 2000 (n = 37) |
RR | 0.9 (0.6 to 1.3) | > 1 favours drug | NO | 2(E×2) |
| 1.1 | Lapitan 2017 | Open retropubic colposuspension vs conservative interventions | FU1 | Klarskov 19864 (n = 29) | RR | 0.2 (0.1 to 0.7) | < 1 favours surgery | YES favours surgery | 1(H) |
| 2.1 | Wang 2013 | Acupuncture vs any other treatment | IM |
Bi 20071 (n = 60) |
RR | 2.2 (1.3 to 3.8) | > 1 favours acupuncture | YES favours acupuncture | 2(A, B) |
| Low‐certainty evidence | |||||||||
| 2.3 | Glazener 2017a | Anterior repair vs PFMT | FU1 |
Klarskov 19864 (n = 16) |
RR | 0.3 (0.0 to 2.3) | > 1 favours PFMT | NO | 2(E×2) |
| 2.2 | Glazener 2017a | Anterior repair vs PFMT | FU2 |
Klarskov 19864 (n = 16) |
RR | 2.6 (0.6 to 10.2) | > 1 favours PFMT | NO | 2(E×2) |
| 2.2 | Kirchin 2017 | Urethral injection therapy vs conservative management | IM |
ter Meulen 20091 (n = 45) |
RR | 0.2 (0.0 to 1.8) | > 1 favours conservative | NO | 3(E×2, H) |
1Trials with an immediate outcome measure. 2Schagen van Leeuwen 2004 determined cure or improvement using two methods. These data related to data collected via a paper diary. 3Schagen van Leeuwen 2004 determined cure or improvement using two methods. These data are based on the Patient Global Impression scale – Improvement. 4Klarskov 1986 included participants who received different surgical interventions, Lapitan 2017 included all surgical groups, while Glazener 2017a included the subgroup of participants receiving anterior repair – therefore, 16 participants were presented twice. Abbreviations: CI: confidence interval; FU1: follow‐up one; FU2: follow‐up two; IM: immediate; n: number of participants assessed NOT to have been cured or improved using a variety of different assessment methods; PFMT: pelvic floor muscle training; RR: risk ratio; UC: unclear. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
Nine analyses from six reviews assessed symptomatic cure or improvement comparing one conservative intervention with a non‐conservative intervention (Alhasso 2005; Ayeleke 2015; Glazener 2017a; Kirchin 2017; Lapitan 2017; Wang 2013). Of these, four analyses related to immediate outcome assessment. Five trials compared conservative and non‐conservative interventions (Glazener 2017a and Lapitan 2017 both reported data from the same trial).
High‐ or moderate‐certainty evidence
Six analyses provided moderate‐certainty evidence. Two provided moderate‐certainty evidence of a beneficial effect of treatment.
Acupuncture led to high symptomatic cure or improvement compared to 'any other treatment', which comprised a pharmacological intervention.
Open retropubic colposuspension surgery led to higher symptomatic cure or improvement than a conservative intervention within the first year.
Four analyses provided moderate‐certainty evidence of no evidence of a difference between groups.
PFMT plus SNRI versus SNRI alone: two comparisons with different methods of assessing cure or improvement.
Adrenergic agonist versus conservative therapy.
Adrenergic agonist versus conservative therapy plus adrenergic agonist.
Low‐ or very low‐certainty evidence
Three analyses provided low‐certainty evidence.
Condition‐specific quality of life
For more information, see Table 13.
13. Stress urinary incontinence: quality of life, conservative versus non‐conservative.
| Analysis code (in review) | Study ID | Comparisons included | Timing of measure | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| High‐certainty evidence | |||||||||
| 2.2 | Mariappan 2005 | SNRI vs conservative non‐ pharmacological therapies | IM |
Schagen van Leeuwen 20042 (n = 92) |
OR | 2.4 (1.0 to 5.6) | > 1 favours duloxetine | YES favours medication |
1(H) |
| Moderate‐certainty evidence | |||||||||
| 7.3.1 | Ayeleke 2015 | PFMT + drug therapy vs drug therapy alone | IM |
Schagen van Leeuwen 20041 (n = 101) |
MD | 5.8 (−2.1 to 13.7) | > 0 favours PFMT + drug | NO | 2(E×2) |
| 2.3 | Kirchin 2017 | Urethral injection therapy vs conservative management (PFMT) | IM |
ter Meulen 20091 (n = 45) |
MD | 0.5 (0.1 to 0.9) | > 0 Favours PFMT | YES favours PFMT | 1(H) |
| Not estimable | |||||||||
| 2.3 | Mariappan 2005 | SNRI vs conservative non‐ pharmacological therapies | IM |
Schagen van Leeuwen 20042 (n = 99) |
MD | NE | > 0 favours PFMT | NO | 0 |
1Data from the I‐QOL measure of quality of life. 2The review Mariappan 2005 also reported data from Schagen van Leeuwen 2004, reporting the Physical Quality of Life Index (as event data,), and reporting the Incontinence Quality of Life questionnaire (but reporting the standard deviations as 0, and therefore not enabling an effect size estimate). Abbreviations: CI: confidence interval; IM: immediate; MD: mean difference; n: number of participants; NE: not estimable; OR: odds ratio; PFMT: pelvic floor muscle training; RR: risk ratio; SNRI: serotonin–noradrenaline reuptake inhibitor. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
Four analyses from three reviews assessed quality of life comparing one conservative intervention with a non‐conservative intervention (Ayeleke 2015; Kirchin 2017; Mariappan 2005). All four analyses relate to an immediate assessment. One analysis contained data that meant it was not possible to calculate an effect size. Two trials compared a conservative intervention with a non‐conservative intervention at an immediate time point (Schagen van Leeuwen 2004; ter Meulen 2009).
High‐ or moderate‐certainty evidence
One analysis provided high‐certainty evidence and two moderate‐certainty evidence. One analysis provided high‐certainty and one moderate‐certainty evidence of improved quality of life with non‐conservative interventions.
SNRI was more beneficial than conservative intervention (PFMT) (high‐certainty).
Urethral injection was more beneficial than conservative intervention (PFMT) (moderate‐certainty).
One analysis provided moderate‐certainty evidence of no difference between PFMT plus SNRI and SNRI alone.
Urgency urinary incontinence
Any conservative intervention versus control, placebo or standard care
Symptomatic cure or improvement
For more information, see Table 14.
14. Urgency urinary incontinence: primary outcome participant‐reported cure or improvement; conservative versus control.
| Analysis code (in review) | Study ID | Comparisons included | Timing of measure | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| High‐certainty evidence | |||||||||
| 2.2.2 | Herderschee 2011 | PFMT + feedback vs PFMT alone (control) | IM |
Burgio 2002b1 (n = 122) |
RR | 0.5 (0.4 to 0.8) | > 1 favours PFMT | YES favours PFMT + feedback | 0 |
| 1.9 | Stewart 2016 | ES vs no active treatment, placebo or sham treatment | IM |
Finazzi‐Agrò 2010² (n = 35) |
RR | 0.3 (0.1 to 0.6) | < 1 favours ES | YES favours ES | 0 |
| Moderate‐certainty evidence | |||||||||
| 1.2.2 | Herderschee 2011 | PFMT + biofeedback vs PFMT alone | IM |
Burgio 20021 (n = 118) |
RR | 0.5 (0.4 to 0.8) | > 1 favours PFMT alone | YES favours PFMT + BF | 1(C) |
| 1.19.2 | Stewart 2016 | ES vs no active treatment, placebo or sham treatment | IM |
Kosilov 20132 (n = 107) |
MD | −1.1 (−1.8 to −0.4) | < 0 favours ES |
YES favours ES | 1(H) |
| 1.8 | Stewart 2016 | ES vs no active treatment, placebo or sham treatment | IM |
Amaro 2006 (n = 40) |
RR | 0.5 (0.1 to 1.7) | < 1 favours ES |
NO | 2(E×2) |
| 1.4.1 | Wallace 2004 | Bladder training vs no treatment | FU1 |
Lagro‐Janssen 1991 (n = 18) |
RR | 17.0 (1.1 to 256.5) | > 1 favours BT | YES favours BT | 1(H) |
| Low‐certainty evidence | |||||||||
| 5.2 | Stewart 2016 | ES + PFMT vs no active treatment | IM |
Firra 20132 (n = 12) |
MD | −1.6 (−3.6 to 0.4) | < 0 favours ES + PFMT | NO | 3(A, E×2) |
1Burgio 2002 was a three‐arm trial, in which the arms were PFMT (n = 75), PFMT plus feedback (n = 74) and PFMT plus biofeedback (n = 73). Overview authors judged that the PFMT only group met the definition to be classed as a control intervention. Therefore, there were two comparisons categorised within the overview as 'conservative versus control', one that was PFMT plus biofeedback versus control (Burgio 2002), and one that was PFMT plus feedback versus control (Burgio 2002b). 2Data from these trials are presented as 'number of incontinence episodes in 24 hours'. Abbreviations: CI: confidence interval; ES: electrical stimulation; FU1: follow‐up one; IM: immediate; MD: mean difference; n: number of participants assessed NOT to have been cured or improved using a variety of different assessment methods; PFMT: pelvic floor muscle training; RR: risk ratio. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
Seven analyses from three reviews assessed symptomatic cure or improvement and compared a conservative intervention with a control intervention (Herderschee 2011; Stewart 2016; Wallace 2004). Six outcomes were at an immediate time point and one at a follow‐up time point. Six unique trials compared a conservative intervention with a control intervention, with five reporting data on immediate cure or improvement.
High‐ or moderate‐certainty evidence
Two analyses provided high‐certainty and two moderate‐certainty evidence of a beneficial effect demonstrating the following.
PFMT plus feedback had better cure or improvement compared to control (high‐certainty) and PFMT plus biofeedback had a beneficial effect on outcome compared to control (moderate‐certainty). In both these comparisons, the overview authors categorised the 'PFMT' intervention as a no treatment control intervention. This in effect adds a bias against the treatment interventions that make it less likely that any evidence of a difference favouring treatment would be found.
Electrical stimulation had better cure or improvement compared to control (two comparisons, one high‐certainty, one moderate‐certainty).
Bladder training had a beneficial effect compared to no treatment at a follow‐up time point (moderate‐certainty).
One analysis provided moderate‐certainty evidence of no difference when electrical stimulation was compared to control. This was in contrast to the findings of other comparisons, which demonstrated a beneficial effect (see above).
Low‐ or very low‐certainty evidence
One analysis provided low‐certainty evidence.
Condition‐specific quality of life
For more information, see Table 15.
15. Urgency urinary incontinence: quality of life, conservative versus control.
| Analysis code (in review) | Study ID | Comparisons included | Timing of measure | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| Moderate‐certainty evidence | |||||||||
| 5.1.1 | Stewart 2016 | ES + PFMT vs no active treatment | IM |
Firra 2013 (n = 12) |
MD | −12.4 (−20.9 to −3.9) | < 0 favours ES + other | YES favours ES + PFMT | 1(A) |
Abbreviations: CI: confidence interval; ES: electrical stimulation; IM: immediate; MD: mean difference; n: number of participants; PFMT: pelvic floor muscle training. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
One analysis from one review assessed quality of life and compared a conservative intervention with control (Stewart 2016).
High‐ or moderate‐certainty evidence
One analysis provided moderate‐certainty evidence of a beneficial effect. Combined electrical stimulation plus PFMT was more beneficial than control for a measure of quality of life using the York Incontinence Perception Scale score. There was one unique trial.
One conservative intervention versus another conservative intervention
Symptomatic cure or improvement
For more information, see Table 16.
16. Urgency urinary incontinence: cure or improvement, conservative versus conservative.
| Analysis code (in review) | Study ID | Comparisons included | Timing of measure | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| Moderate‐certainty evidence | |||||||||
| 4.2.1 | Herderschee 2011 | PFMT + BF vs PFMT + F | IM |
Burgio 2002c1 (n = 110) |
RR | 1.0 (0.6 to 1.7) | > 1 favours PFMT + feedback | NO | 2(E×2) |
| 2.8.2 | Stewart 2016 | ES vs laseropuncture | IM |
Kosilov 20132 (n = 114) |
MD | −1.8 (−2.3 to −1.3) | < 0 favours ES | YES favours ES | 1(H) |
| 4.2.1 | Stewart 2016 | ES + PFMT vs PFMT alone | IM |
Schreiner 20102 (n = 51) |
RR | 0.56 (0.3 to 0.9) | < 1 favours ES + other | YES favours ES + PFMT | 1(H) |
| 4.3.1 | Stewart 2016 | ES + PFMT vs PFMT alone | IM |
Schreiner 20102 (n = 51) |
RR | 0.3 (0.1 to 0.7) | < 1 favours ES + other | YES favours ES + PFMT | 1(H) |
| 2.3.1 | Stewart 2016 | ES vs PFMT | IM |
Wang 20042 (n = 69) |
RR | 0.8 (0.5 to 1.2) | < 1 favours ES | NO | 2(E×2) |
| 2.3.2 | Stewart 2016 | ES vs PFMT + biofeedback |
IM |
Wang 20042 (n = 69) |
RR | 0.9 (0.6 to 1.6) | < 1 favours ES | NO | 2(E×2) |
| 2.8.1 | Stewart 2016 | ES vs PFMT | IM |
Arruda 20082 (n = 42) |
MD | 0.1 (−8.7 to 8.9) | < 0 favours ES | NO | 2(E×2) |
| Low‐certainty evidence | |||||||||
| 5.2 | Rai 2012 | Anticholinergic drugs + non‐drug therapies vs non‐drug therapies alone | IM |
Park 2002 (n = 50) |
RR | 0.6 (0.3 to 1.3) | < 1 favours anticholinergics + non‐drug therapies | NO | 4(E×2, H×2) |
| 5.2 | Rai 2012 | Anticholinergic drugs + non‐drug therapies vs non‐drug therapies alone | IM |
Song 2006 (n = 57) |
RR | 0.6 (0.3 to 1.2) | < 1 favours anticholinergics + non‐drug therapies | NO | 3(E×2, H) |
| 4.9.2 | Stewart 2016 | ES + PFMT vs PFMT | IM |
Firra 20132 (n = 12) |
MD | 0.2 (−1.2 to 1.6) | < 0 favours ES + other | NO | 3(A, E×2) |
1Burgio 2002 was a three‐arm trial in which two of the groups received PFMT, combined with either feedback or biofeedback. Both groups received active treatment, each comprising a different way of delivering the same intervention. 2These trials compared ES with another conservative intervention. However, in all cases both conservative interventions were categorised as 'physical therapy' interventions. Abbreviation: CI: confidence interval; ES: electrical stimulation; IM: immediate; MD: mean difference; n: number of participants assessed NOT to have been cured or improved using a variety of different assessment methods; RR: risk ratio. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
Ten analyses from three reviews compared one conservative intervention with another conservative intervention for a cure or improvement outcome (Herderschee 2011; Rai 2012; Stewart 2016). All analyses related to immediate outcome assessment. Two analyses compared the effect of anticholinergic drugs plus conservative intervention versus the same conservative intervention, one analysis compared different ways of delivering the same conservative intervention (PFMT) and seven analyses compared different physical therapy interventions. Eight unique trials compared one conservative intervention with another conservative intervention for a measure of cure or improvement with an immediate outcome.
High‐ or moderate‐certainty evidence
Seven analyses provided moderate‐certainty evidence. Three analyses provided evidence of a more beneficial effect.
Electrical stimulation was more effective than laseropuncture (moderate‐certainty).
Electrical stimulation plus PFMT was more effective than PFMT alone (two analyses, moderate‐certainty).
Four analyses provided moderate‐certainty evidence of no difference between groups.
PFMT plus biofeedback versus individualised PFMT (moderate‐certainty).
Electrical stimulation versus PFMT (two analyses, moderate‐certainty).
Electrical stimulation versus PFMT plus biofeedback (one analysis, moderate‐certainty).
Low‐ or very low‐certainty evidence
Three analyses provided low‐certainty evidence.
Condition‐specific quality of life
For more information, see Table 17.
17. Urgency urinary incontinence: quality of life, conservative versus conservative.
| Analysis code (in review) | Study ID | Comparisons included | Timing of measure | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| High‐certainty evidence | |||||||||
| 2.5.1 | Stewart 2016 | ES vs PFMT | IM |
Wang 20041,2 (n = 69) |
MD | 129.8 (47.8 to 211.8) | < 0 favours ES | YES favours PFMT | 0 |
| Moderate‐certainty evidence | |||||||||
| 4.5.1 | Stewart 2016 | ES + PFMT vs PFMT alone | IM | Schreiner 20101 (n = 51) | MD | −2.7 (−5.1 to −0.2) | < 0 favours ES + other | YES favours ES + PFMT | 1(H) |
| 2.5.2 | Stewart 2016 | ES vs PFMT + biofeedback |
IM | Wang 20041,2 (n = 69) | MD | −5.8 (−89.0 to 77.4) | < 0 favours ES | NO | 2(E×2) |
| Low‐certainty evidence | |||||||||
| 4.8.1 | Stewart 2016 | ES + PFMT vs PFMT | IM | Firra 20131 (n = 12) | MD | 5.8 (−3.5 to 15.1) | < 0 favours ES + other | NO | 3(A, E×2) |
1Studies compare two conservative interventions both categorised as 'physical therapy'. 2Wang 2004 was a three‐arm trial comparing PFMT, PFMT plus biofeedback and ES. Abbreviations: CI: confidence interval; ES: electrical stimulation; IM: immediate; MD: mean difference; n: number of participants; PFMT: pelvic floor muscle training. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
Four analyses from one review presented quality of life data from participants with UUI (Stewart 2016). All analyses related to immediate outcome assessment. There were three unique studies.
High‐ or moderate‐certainty evidence
One analysis provided high‐certainty evidence and two moderate‐certainty evidence. Two analyses provided evidence of a difference between groups.
PFMT was more effective than electrical stimulation (high‐certainty).
Electrical stimulation plus PFMT was more effective than PFMT alone (moderate‐certainty).
One analysis provided moderate‐certainty evidence of no difference; there was no evidence that electrical stimulation had a different quality of life to PFMT plus biofeedback.
Low‐ or very low‐certainty evidence
One analysis provided low‐certainty evidence.
Any conservative intervention versus another active intervention (non‐conservative intervention)
Symptomatic cure or improvement
For more information, see Table 18.
18. Urgency urinary incontinence: primary outcome participant‐reported cure or improvement; conservative versus non‐conservative.
| Analysis code (in review) | Study ID | Comparisons included | Timing of measure | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| Moderate‐certainty evidence | |||||||||
| 6.2.3 | Rai 2012 | Anticholinergic drugs + behavioural interventions vs anticholinergic drugs alone | IM |
Burgio 2008; Burgio 20103 (n = 364) |
RR | 0.6 (0.4 to 0.9) | > 1 favours drugs alone | YES favours drugs + behavioural interventions |
2(F×2) |
| 6.2 | Rai 2012 | Anticholinergic drugs + non‐drug therapies vs anticholinergic drugs alone | IM |
Millard 2004 (n = 475) |
RR | 1.3 (0.8 to 1.9) | > 1 favours drugs | NO | 1(H) |
| 3.3 | Rai 2012 | Anticholinergic drugs vs external electrostimulation | IM |
Wang 2006 (n = 47) |
RR | 1.5 (0.8 to 2.6) | > 1 favours ES | NO | 2(E×2) |
| 3.10.3 | Stewart 2016 | ES vs trospium + solifenacin |
IM |
Kosilov 20131 (n = 110) |
MD | 2.2 (1.8 to 2.6) | < 0 favours ES | YES favours drugs | 1(H) |
| 4.9.1 | Stewart 2016 | ES + drugs vs drugs | IM |
Sancaktar 20101 (n = 38) |
MD | −0.9 (−1.1 to −0.7) | < 0 favours ES + other | YES favours ES + drugs | 1(H) |
| 3.10.2 | Stewart 2016 | ES vs oxybutynin | IM |
Arruda 20081 (n = 43) |
MD | 0.9 (−6.4 to 8.2) | < 0 favours ES | NO | 2(E×2) |
| 3.6.1 | Stewart 2016 | ES vs tolterodine | IM |
Franzén 2010 (n = 64) |
RR | 0.9 (0.4 to 2.0) | < 1 favours ES | NO | 2(E×2) |
| 4.9.3 | Stewart 2016 | ES + PFMT + drugs vs drugs | IM |
Kaya 20111 (n = 30) |
MD | −1 (−2.1 to 0.1) | < 0 favours ES + other | NO | 2(E×2) |
| 3.14.1 | Stewart 2016 | ES vs solifenacin succinate | IM |
Vecchioli‐Scaldazza 20131 (n = 30) |
MD | −0.9 (−2.0 to 0.2) | < 0 favours ES | NO | 2(E×2) |
| Low‐certainty evidence | |||||||||
| 7.4.2 | Ayeleke 2015 | PFMT + drug therapy vs drug therapy alone | IM |
Burgio 20103 (n = 58) |
RR | 0.9 (0.7 to 1.1) | > 1 favours PFMT + other | NO | 3(E×2, H) |
| 7.2 | Rai 2012 | Anticholinergic drugs vs combination non‐drug therapies | IM |
Goode 2002 (n = 128) |
RR | 2.4 (1.0 to 5.8) | < 0 favours anticholinergics | NO | 4(C, E×2, H) |
| 1.3 | Rai 2012 | Anticholinergic drugs vs bladder training | IM |
Colombo 19954 (n = 27) |
RR | 0.5 (0.4 to 4.5) | > 1 favours bladder training | NO | 3(E×2, H) |
| 1.3 | Rai 2012 | Anticholinergic drugs vs bladder training | IM |
Milani 1986 (n = 75) |
RR | 0.8 (0.6 to 1.1) | > 1 favours bladder training | NO | 3(E×2, H) |
| 1.3 | Rai 2012 | Anticholinergic drugs vs bladder training | IM |
Park 20022 (n = 48) |
RR | 0.8 (0.4 to 1.5) | > 1 favours bladder training | NO | 4(E×2, H×2) |
| 6.2 | Rai 2012 | Anticholinergic drugs + non‐drug therapies vs anticholinergic drugs alone | IM |
Park 20022 (n = 50) |
RR | 0.7 (0.4 to 1.6) | > 1 favours drugs alone | NO | 4(E×2, H×2) |
| 3.3 | Rai 2012 | Anticholinergic drugs vs external electrostimulation | IM |
Aaronson 1995 (n = 38) |
RR | 1.3 (0.7 to 2.3) | > 1 favours ES | NO | 3(E×2, H) |
| 1.3 | Rai 2012 | Anticholinergic drugs vs bladder training | IM |
Song 20062 (n = 58) |
RR | 0.8 (0.4 to 1.5) | > 1 favours bladder training | NO | 3(E×2, H) |
| 6.2 | Rai 2012 | Anticholinergic drugs + non‐drug therapies vs anticholinergic drugs alone | IM |
Song 20062 (n = 63) |
RR | 0.8 (0.4 to 1.6) | > 1 favours drugs alone | NO | 3(E×2, H) |
| 3.11 | Stewart 2016 | ES vs tolterodine | IM |
Preyer 20071 (n = 31) |
MD | 1.3 (−1.6 to 4.2) | < 0 favours ES | NO | 3(E×2, H) |
| 3.5.1 | Stewart 2016 | ES vs oxybutynin after 12 weeks | IM |
Souto 2014 (n = 37) |
RR | 0.3 (0.1 to 1.5) | < 1 favours ES | NO | 3(E×2, H) |
| 3.5.2 | Stewart 2016 | ES vs oxybutynin after 24 weeks | FU1 |
Souto 2014 (n = 37) |
RR | 0.6 (0.1 to 1.8) | < 1 favours ES | NO | 3(E×2, H) |
| 2.3 | Wallace 2004 | Bladder training vs anticholinergic drugs | IM |
Colombo 19954 (n = 75) |
RR | 1.1 (0.9 to 1.3) | > 1 favours bladder training | NO | 3(E×2, H) |
1Data were presented as mean differences within these trials. 2Song 2006 and Park 2002 were both three‐arm trials, both with groups: bladder training, anticholinergic drug and bladder training plus anticholinergic drug. 3These are the same data for Burgio 2010. This was the same trial, included in two different reviews (the trial name within Ayeleke 2015 was "Burgio 2010a"). 4Data from Colombo 1995 were included within both Kirchin 2017 and Wallace 2004. The methods used to determine number cure or improved differed within the two reviews, resulting with different effect sizes; however, both reviews presented data derived from the same participant groups. Abbreviations: CI: confidence interval; ES: electrical stimulation; FU1: follow‐up one; IM: immediate; MD: mean difference; n: number of participants assessed NOT to have been cured or improved using a variety of different assessment methods; PFMT: pelvic floor muscle training; RR: risk ratio. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
A total of 22 analyses from four reviews presented data on symptomatic cure and improvement comparing one conservative intervention with a non‐conservative intervention (Ayeleke 2015; Rai 2012; Stewart 2016; Wallace 2004). Twenty‐one were at immediate time points. There were 18 unique trials comparing a conservative with a non‐conservative intervention, with an immediate measure of cure of improvement.
High‐ or moderate‐certainty evidence
Nine analyses provided moderate‐certainty evidence. Three of these provided moderate‐certainty evidence of a difference between groups.
Conservative intervention (PFMT plus behavioural interventions) plus anticholinergic drugs had better cure or improvement than anticholinergic drugs alone.
Pharmacological intervention (trospium and solifenacin) was more effective than electrical stimulation.
Electrical stimulation plus drugs was more effective than drugs alone.
Six analyses provided moderate‐certainty evidence of no difference between groups.
Anticholinergic drugs versus external electrical stimulation.
Anticholinergic drugs plus PFMT versus anticholinergic drugs alone.
Electrical stimulation versus drugs (four analyses).
Electrical stimulation plus PFMT plus drugs versus drugs.
Low‐ or very low‐certainty evidence
Thirteen analyses provided low‐certainty evidence.
Condition‐specific quality of life
For more information, see Table 19.
19. Urgency urinary incontinence: quality of life, conservative versus non‐conservative.
| Analysis code (in review) | Study ID | Comparisons included | Timing of measure | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| High‐certainty evidence | |||||||||
| 4.6.1 | Stewart 2016 | ES + PFMT + drugs vs drugs | IM |
Kaya 2011 (n = 30) |
MD | −16.2 (−28.0 to −4.4) | < 0 favours ES + other | YES favours ES + PFMT + drugs | 0 |
| Moderate‐certainty evidence | |||||||||
| 4.4.1 | Stewart 2016 | ES + drugs vs drugs alone | IM |
Sancaktar 2010 (n = 38) |
MD | −2.2 (−3.5 to −0.9) | < 0 favours ES + other | YES favours ES + drugs | 1(H) |
| 3.8.1 | Stewart 2016 | ES vs solifenacin succinate | IM |
Vecchioli‐Scaldazza 2013 (n = 30) |
MD | −0.6 (−1.3 to 0.1) | < 0 favours ES | YES favours ES + drugs | 2(E×2) |
Abbreviation: CI: confidence interval; ES: electrical stimulation; IM: immediate; MD: mean difference; n: number of participants; PFMT: pelvic floor muscle training. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
Three analyses in one review included quality of life data from participants with UUI comparing conservative intervention with a non‐conservative intervention (Stewart 2016). There were three unique studies.
High‐ or moderate‐certainty evidence
One analysis provided high‐certainty evidence of a beneficial effect. Electrical stimulation plus drugs had better quality of life when compared to drugs alone.
Two analyses provided moderate‐certainty evidence of a beneficial effect. Electrical stimulation plus PFMT plus drugs had better quality of life compared to drugs alone.
All type of urinary incontinence
Any conservative intervention versus control, placebo or standard care
Symptomatic cure or improvement
For more information, see Table 20.
20. All types of urinary incontinence: primary outcome participant‐reported cure or improvement; conservative versus control.
| Analysis code (in review) | Study ID | Comparisons included | Timing of measure | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| High‐certainty evidence | |||||||||
| 1.2.4 | Dumoulin 2018 | PFMT vs no treatment, placebo or control | IM | Diokno 2010; Goode 2002 (n = 166) | RR | 2.4 (1.6 to 3.5) | > 1 favours PFMT | YES favours PFMT | 0 |
| 1.6 | Imamura 2015 | Weight loss vs no active intervention | IM | Subak 2005 (n = 40) | RR | 16.5 (1.0 to 270.8) | At 3 months; > 1 favours weight loss | YES favours weight loss | 0 |
| 11.19.1 | Stewart 2016 | ES vs no active treatment, placebo or sham treatment | IM | Barroso 20042 (n = 36) | MD | −1.7 (−2.3 to −1.0) | < 0 favours ES | YES favours ES | 0 |
| Moderate‐certainty evidence | |||||||||
| 1.1 | Herbison 2013 | Cones vs control | IM | Bø 1999; Williams 20061 (n = 215) | RR | 0.7 (0.5 to 1.0) | > 1 favours control | YES favours cones | 2(E×2) |
| 1.1 | Imamura 2015 | Weight loss vs no active intervention | FU1 | Wing 2010 (n = 304) | RR | 1.4 (1.1 to 1.7) | > 1 favours weight loss | YES favours weight loss | 1(C) |
| 1.6 | Imamura 2015 | Weight loss vs no active intervention | FU1 | Wing 2010 (n = 304) | RR | 1.8 (1.2 to 2.8) | At 6 months; > 1 favours weight loss | YES favours weight loss | 1(C) |
| 1.6 | Imamura 2015 | Weight loss vs no active intervention | FU2 | Wing 2010 (n = 287) | RR | 1.1 (0.9 to 1.5) | At 18 months; > 1 favours weight loss | NO | 2(C, E) |
| Low‐certainty evidence | |||||||||
| 1.6 | Imamura 2015 | Weight loss vs no active intervention | O |
Phelan 2012; Wing 2010 (n = 1032) |
RR | 1.2 (1.0 to 1.4) | > 1 favours weight loss | YES favours weight loss | 3(C, E×2) |
| 1.2 | Stewart 2017 | ES vs no active treatment | IM | Bø 1999; Castro 2008; Henalla 1989; Lopès 2014; Oldham 2013 (n = 347) | RR | 1.73 (1.41 to 2.11) | > 1 favours ES | YES for ES | GRADE as assessed by review authors |
| 1.20.4 | Wallace 2004 | Bladder training vs no treatment | IM | Fantl 1991 (n = 123) | RR | 3.1 (2.0 to 5.0) | > 1 favours Bladder Training | YES favours BT | 3(G, H×2) |
| Very low‐certainty evidence | |||||||||
| 1.1 | Wieland 2019 | Yoga vs waiting list control | IM | Huang 2014 (n = 18) | RR | 6.33 (1.44 to 27.88) | > 1 favours yoga | YES for yoga | GRADE as assessed by review authors |
1Bø 1999 contained only participants with SUI, but when pooled with Williams 2006 the pooled total contained a mixed population. Results from Williams 2006 are presented within the forest plot, but the individual study results from Bø 1999 are presented alongside the SUI data. 2Barroso 2004 presented data as a mean difference, rather than number cure or improved, and, therefore, these data are not included in the forest plot. 3Only data relating to immediate outcome measures were considered for inclusion in forest plots. Abbreviations: CI: confidence interval; ES: electrical stimulation; FU1: follow‐up one; FU2: follow‐up two; IM: immediate; MD: mean difference; n: number of participants; O: other; PFMT: pelvic floor muscle training; RR: risk ratio. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
Eleven analyses from seven reviews assessed symptomatic cure and improvement and compared a conservative intervention with a control intervention (Dumoulin 2018; Herbison 2013; Imamura 2015; Stewart 2016; Stewart 2017; Wallace 2004; Wieland 2019). Seven outcomes were assessed at an immediate time point, three at follow‐up time points and one was unclear. There were 13 unique trials contained within the analyses.
High‐ or moderate‐certainty evidence
Three analyses provided high‐certainty and four moderate‐certainty evidence. Six analyses provided high‐ or moderate‐certainty evidence for conservative intervention compared to control, for measures of cure or improvement.
PFMT had better cure or improvement compared to no treatment, control or placebo (high‐certainty).
Electrical stimulation had better cure or improvement compared to no treatment (high‐certainty).
Weight loss interventions had a beneficial effect compared to no active treatment at immediate outcome (high‐certainty) and six‐month follow‐up outcome measured by self‐report and by a seven‐day voiding diary (two analyses, moderate‐certainty).
Cones had better cure or improvement compared to control (moderate‐certainty).
One analysis provided moderate‐certainty evidence of no difference in cure or improvement for weight loss interventions compared to no active treatment at a longer term (18 months) follow‐up (moderate‐certainty).
Low‐ or very low‐certainty evidence
Four analyses provided low‐ or very low‐certainty evidence.
Condition‐specific quality of life
For more information, see Table 21.
21. All types of urinary incontinence: primary outcome quality of life; conservative versus control.
| Analysis code (in review) | Study ID | Comparisons included | Outcome measure (timing of measure) | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| High‐certainty evidence | |||||||||
| 1.11.4 | Dumoulin 2018 | PFMT vs no treatment, placebo or control | Incontinence Impact Questionnaire Long Form (IM) | Sran 2016 (n = 48) | MD | −52.67 (−95.00 to −10.34) | > 0 favours control | YES favours PFMT | 0 |
| 1.16.4 | Dumoulin 2018 | PFMT vs no treatment, placebo or control | Incontinence Impact Questionnaire Long Form (FU) | Sran 2016 (n = 48) | MD | −41.91 (−83.20 to −0.62) | > 0 favours control | YES favours PFMT | 0 |
| Moderate‐certainty evidence | |||||||||
| 1.12.4 | Dumoulin 2018 | PFMT vs no treatment, placebo or control | Incontinence of Quality of Life Questionnaire (IM) |
Sar 2009 (n = 34) |
MD | 28.9 (35.1 to 22.7) | > 0 favours control | YES favours PFMT | 1(A) no change |
| 1.10.4 | Dumoulin 2018 | PFMT vs no treatment, placebo or control | Incontinence Impact Questionnaire Short Form (IM) | Celiker Tosun 2015; Leong 2015 (n = 176) | MD | −7.54 (−14.70 to −0.39) | > 0 favours control | YES favours PFMT | 2(F×2) |
| Very low‐certainty evidence | |||||||||
| 1.2 | Wieland 2019 | Yoga vs waiting list control | IM | Huang 2014 (n = 18) | MD | 1.7 (−33.0 to 36.5) | > 0 favours control | NO | GRADE as assessed by review authors |
Abbreviations: CI: confidence interval; FU: follow‐up; IM: immediate; MD: mean difference; n: number of participants; PFMT: pelvic floor muscle training. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
Five analyses from two reviews presented quality of life data from participants with AUI (Dumoulin 2018; Wieland 2019). These analyses contained data from five unique studies.
High‐ or moderate‐certainty evidence
Two analyses provided high‐certainty and two moderate‐certainty evidence that PFMT was more beneficial than no treatment, control or placebo on measures of quality of life at an immediate time point.
Very low‐certainty evidence
One analysis provided very low‐certainty evidence.
One conservative intervention versus another conservative intervention
Symptomatic cure or improvement
For more information, see Table 22.
22. All types of urinary incontinence: primary outcome participant‐reported cure or improvement; conservative versus conservative.
| Analysis code (in review) | Study ID | Comparisons included | Outcome measure (timing of measure) | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| High‐certainty evidence | |||||||||
| 1.2.31 | Hay‐Smith 2011 | Home PFMT programme (unsupervised) vs PFMT (Sapsford style2) with 8 clinic visits | IM | Hung 2010(n = 64) | RR | 0.1 (0 to 0.7) | > 1 favours less contact/supervision | YES favours more contact/supervision | 0 |
| Moderate‐certainty evidence | |||||||||
| 3.2.1 | Ayeleke 2015 | PFMT + bladder training vs bladder training alone | IM | Wyman 1998(n = 128) | RR | 1.3 (1.0 to 1.8) | > 1 favours PFMT + bladder training | YES favours PFMT + BT | 2(C, H) |
| 12.2.3 | Hay‐Smith 2011 | More‐intensive vs less‐intensive PFMT programmes | IM | de Oliveira 20093; Delgado 2009; Hay‐Smith 20023; Sriboonreung 20113; Sugaya 20033; Wells 1999(n = 405) | RR | 0.7 (0.6 to 0.9) | > 1 favours less intensive | YES favours more intensive | 1(H) |
| 10.3 | Wallace 2004 | Bladder training + non‐pharmacological treatments vs non‐pharmacological treatments (PFMT) | IM | Wyman 1998(n = 124) | RR | 1.2 (1.0 to 1.4) | > 1 favours bladder training + non‐pharmacological | YES favours BT + PFMT | 2(G, H) |
| Low‐certainty evidence | |||||||||
| 3.5.1 | Ayeleke 2015 | PFMT + bladder training vs bladder training alone | IM |
Kaya 2014; Wyman 1998 (n = 235) |
RR | 1.3 (1.1 to 1.4) | > 1 favours PFMT + bladder training | YES favours PFMT + BT | 4(C, E×2, H) |
| 3.2.2 | Ayeleke 2015 | PFMT + bladder training vs bladder training alone | FU1 |
Wyman 1998 (n = 120) |
RR | 1.3 (0.9 to 1.8) | > 1 favours PFMT + bladder training | NO | 3(E×2, H) |
| 3.5.2 | Ayeleke 2015 | PFMT + bladder training vs bladder training alone | FU1 |
Wyman 1998 (n = 119) |
RR | 1.2 (0.9 to 1.5) | > 1 favours PFMT + bladder training | NO | 3(E×2, H) |
| 12.2.1 | Hay‐Smith 2011 | More‐intensive vs less intensive PFMT programmes | IM |
Bø 19903; Felicíssimo 20103; Schagen van Leeuwen 20043; Hung 2010; Konstantinidou 20073; Ramsay 19903 (n = 335) |
RR | 0.4 (0.2 to 0.8) | > 1 favours less intensive | YES more intense | 3(E×2, H) |
| 10.2 | Hay‐Smith 2011 | PFMT with intravaginal resistance device vs PFMT alone | IM | Delgado 2009; Wells 1999(n = 120) | RR | 0.9 (0.6 to 1.2) | > 1 favours no device | NO | 4(A, E×2, H) |
| 1.2.2 | Herderschee 2011 | PFMT + biofeedback vs PFMT alone | IM |
Burgio 20024; Goode 2003; Pages 2001; Wang 20044; Wilson 1987 (n = 343) |
RR | 0.7 (0.6 to 0.8) | > 1 favours PFMT alone | YES favours PFMT + BF | 4(C, E×2, H) |
| 1.2 | Herderschee 2011 | PFMT + biofeedback vs PFMT alone | IM |
Burgio 20024; Goode 20033; Pages 20013; Wang 20044; Wilson 19873; Burns 1993; Morkved 20033 (n = 520) |
RR | 0.7 (0.7 to 0.9) | > 1 favours PFMT alone | YES favours BF | 4(C, E×2, H) |
| 1.2.1 | Herderschee 2011 | PFMT + biofeedback vs PFMT alone | IM |
Burns 1993; Morkved 20033 (n = 177) |
RR | 0.9 (0.7 to 1.0) | > 1 favours PFMT alone | NO | 4(E×2, H×2) |
| 4.2.2 | Herderschee 2011 | PFMT + biofeedback vs PFMT + feedback | IM | Johnson 2000(n = 20) | RR | 1.0 (0.2 to 5.8) | > 1 favours PFMT + feedback | NO | 3(B, E×2) |
| 4.2 | Herderschee 2011 | PFMT + biofeedback vs PFMT + feedback | IM |
Burgio 20024; Johnson 2000 (n = 130) |
RR | 1.0 (0.6 to 1.6) | > 1 favours PFMT + feedback | NO | 4(E×2, H×2) |
| 6.2 | Lipp 2014 | Intraurethral Reliance device vs intraurethral FemAssist device | IM | Boos 1998(n = 101) | RR | 1.0 (0.5 to 2.0) | > 1 favours reliance | NO | 3(B, E×2) |
| 5.3 | Wallace 2004 | Bladder training + behavioural/physical/psychological treatments | IM | Wyman 1998(n = 129) | RR | 0.9 (0.7 to 1.1) | > 1 favours bladder training | NO | 4(C, E×2, G) |
| 5.4 | Wallace 2004 | Bladder training + behavioural/physical/psychological treatments | FU1 | Wyman 1998 (n = 124) | RR | 0.9 (0.7 to 1.1) | > 1 favours bladder training | NO | 4(E×2, G, H) |
| 10.4 | Wallace 2004 | Bladder training + non‐pharmacological treatments vs non‐pharmacological treatments | FU1 | Wyman 1998 (n = 122) | RR | 1.1 (0.9 to 1.3) | > 1 favours bladder training + non‐pharmacological | NO | 4(E×2, G, H) |
| Very low‐certainty evidence | |||||||||
| 2.1 | Herbison 2013 | Cones vs PFMT | IM |
Bø 19993; Cammu 19983; Peattie 1988; Williams 2006; Arvonen 20013; Arvonen 20023 (n = 358) |
RR | 0.9 (0.7 to 1.2) | > 1 favours PFMT | NO | 5(C, F×2, G, H) |
| 3.1 | Herbison 2013 | Cones vs ES | IM | Bø 19993; Oláh 1990; Santos 2009(n = 151) | RR | 1.3 (0.8 to 1.9) | > 1 favours ES | NO | 6(E×2, F×2, G, H) |
| 3.2 | Herbison 2013 | Cones v ES | IM |
Bø 19993; Castro 20083; Oláh 1990 (n = 154) |
RR | 1.2 (0.9 to 1.6) | > 1 favours ES | NO | 6(E×2, F×2, G, H) |
| 2.1 | Wieland 2019 | Yoga vs mindfulness stress reduction | IM | Baker 2014 (n = 24) | RR | 0.09 (0.01 to 1.43) | > 1 favours yoga | NO | GRADE as assessed by review authors |
| 2.2 | Wieland 2019 | Yoga vs mindfulness stress reduction | FU1 | Baker 2014 (n = 20) | RR | 0.2 (0 to 1.4) | > 1 favours yoga | NO | GRADE as assessed by review authors |
| 2.3 | Wieland 2019 | Yoga vs mindfulness stress reduction | FU2 | Baker 2014 (n = 21) | RR | 0.2 (0 to 1.5) | > 1 favours yoga | NO | GRADE as assessed by review authors |
1The data from Hung 2010 for this comparison and outcomes were included in both Analysis 1.2.3 and Analysis 3.2.3 in Hay‐Smith 2011. While the study data were the same in these analyses, the reported risk ratio differed. We are uncertain about the risk ratio presented in Analysis 3.2.3 and, therefore, chose to present the result from Analysis 1.2.3. 2Sapsford‐style PFMT involved diagrammatic and transversus abdominus co‐ordination to 'activate' pelvic floor muscle contraction and no direct pelvic floor muscle contractions. 3Trials with participants who had stress urinary incontinence only, where these were pooled with trials with other populations to give a pooled total relating to a combined participant population. 4Trials with participants who had urgency urinary incontinence only, where these were pooled with trials with other populations to give a pooled total relating to a combined participant population. Abbreviations: CI: confidence interval; ES: electrical stimulation; FU: follow‐up; IM: immediate; n: number of participants assessed NOT to have been cured or improved using a variety of different assessment methods; PFMT: pelvic floor muscle training; RR: risk ratio. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
A total of 25 analyses from seven reviews presented data assessing symptomatic cure or improvement comparing one conservative intervention with another conservative intervention (Ayeleke 2015; Hay‐Smith 2011; Herderschee 2011; Herbison 2013; Lipp 2014; Wallace 2004; Wieland 2019). Of these, 19 related to immediate outcome assessment and six to follow‐up assessment. Eleven analyses compared the effect of different conservative interventions and 11 analyses compared different methods of delivering the same conservative intervention (in 10 analyses this was different ways of delivering PFMT and in one analysis this was different types of IU devices). These analyses pooled data from 32 unique trials. Of these 32 trials, 13 had participants with mixed, combined or unclear types of UI. The remaining 19 trials included participants with either SUI or UUI.
High‐ or moderate‐certainty evidence
Two analyses provided high‐certainty evidence and three moderate‐certainty evidence of a benefit of one conservative intervention compared to another.
Where this was comparing different types of conservative interventions, PFMT plus bladder training had better cure or improvement than bladder training alone or PFMT alone (two analyses, both containing the same single trial, moderate‐certainty).
Where this was comparing different ways of delivering a conservative intervention:
a Sapsord style PFMT programme with eight clinic visits had better cure or improvement than an unsupervised home PFMT programme (high‐certainty). Sapsford‐style PFMT involved diagrammatic and transversus abdominus co‐ordination to 'activate' pelvic floor muscle contraction and no direct pelvic floor muscle contractions;
'more‐intensive' PFMT programmes had better cure or improvement than 'less‐intensive' PFMT programmes (moderate‐certainty).
Low‐ or very low‐certainty evidence
Fourteen analyses provided low‐certainty evidence and six very low‐certainty evidence.
Condition‐specific quality of life
For more information, see Table 23.
23. All types of urinary incontinence: quality of life, conservative versus conservative.
| Analysis code (in review) | Study ID | Comparisons included | Outcome measure (timing of measure) | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| Moderate‐certainty evidence | |||||||||
| 3.3.1 | Ayeleke 2015 | PFMT + bladder training vs bladder training alone | IM |
Wyman 19981 (n = 127) |
MD | −25.5 (−49.9 to −1.0) | > 0 favours bladder training | YES favours PFMT + bladder training | 1(H) |
| 3.4.1 | Ayeleke 2015 | PFMT + bladder training vs bladder training alone | IM |
Wyman 19982 (n = 128) |
MD | −31.1 (−50.0 to −13.2) | > 0 favours bladder training | YES favours PFMT + bladder training |
2(C, H) |
| 10.12 | Wallace 2004 | Bladder training + PFMT + biofeedback vs PFMT + biofeedback | IM |
Wyman 19982 (n = 35) |
MD | −47.2 (−87.0 to −7.4) | > 0 favours control | YES favours bladder training + PFMT + biofeedback |
2(G, H) |
| Low‐certainty evidence | |||||||||
| 3.3.2 | Ayeleke 2015 | PFMT + bladder training vs bladder training alone | FU1 |
Wyman 1998 (n = 118) |
MD | −5.9 (−35.5 to 23.7) | > 0 favours bladder training | NO | 3(E×2, H) |
| 3.4.2 | Ayeleke 2015 | PFMT + bladder training vs bladder training alone | FU1 |
Wyman 1998 (n = 118) |
MD | −18.9 (−38.0 to 0.1) | > 0 favours bladder training | NO | 3(E×2, H) |
| 6.7 | Lipp 2014 | Intraurethral Reliance device vs intraurethral FemAssist device | IM |
Boos 19983 (n = 67) |
MD | −1.0 (−12.6 to 10.6) | > 0 favours FemAssist | NO | 3(B, E×2) |
| 6.7 | Lipp 2014 | Intraurethral Reliance device vs intraurethral FemAssist device | IM |
Boos 19983 (n = 67) |
MD | −6.9 (−15.5 to 1.7) | > 0 favours FemAssist | NO | 3(B, E×2) |
| 6.7 | Lipp 2014 | Intraurethral Reliance device vs intraurethral FemAssist device | IM |
Boos 19983 (n = 67) |
MD | −7.4 (−16.7 to 1.9) | > 0 favours FemAssist | NO | 3(B, E×2) |
| 6.7 | Lipp 2014 | Intraurethral Reliance device vs intraurethral FemAssist device | IM |
Boos 19983 (n = 67) |
MD | 5.2 (−5.0 to 15.4) | > 0 favours FemAssist | NO | 3(B, E×2) |
| 6.7 | Lipp 2014 | Intraurethral Reliance device vs intraurethral FemAssist device | IM |
Boos 19983 (n = 67) |
MD | −1.0 (−12.6 to 10.6) | > 0 favours FemAssist | NO | 3(B, E×2) |
| 6.7 | Lipp 2014 | Intraurethral Reliance device vs intraurethral FemAssist device | IM |
Boos 19983 (n = 67) |
MD | 1.1 (−9.5 to 11.8) | > 0 favours FemAssist | NO | 3(B, E×2) |
| 6.7 | Lipp 2014 | Intraurethral Reliance device vs intraurethral FemAssist device | IM |
Boos 19983 (n = 67) |
MD | 1.9 (−6.9 to 10.7) | > 0 favours FemAssist | NO | 3(B, E×2) |
| 10.13 | Wallace 2004 | Bladder training + non‐pharmacological treatment vs non‐pharmacological treatment | FU1 |
Wyman 1998 (n = 122) |
MD | −12.2 (−30.4 to 6.0) | > 0 favours control | NO | 4(E×2, G, H) |
| 5.14.4 | Wallace 2004 | Bladder training vs other behavioural/physical/psychological treatments | IM |
Wyman 19982 (n = 38) |
MD | −28.0 (−68.4 to 12.4) | > 0 favours control | NO | 4(E×2, G, H) |
| 5.15 | Wallace 2004 | Bladder training vs other behavioural/physical/psychological treatments | FU1 |
Wyman 1998 (n = 124) |
MD | 6.7 (−12.2 to 25.6) | > 0 favours control | NO | 4(E×2, G, H) |
| Very low‐certainty evidence | |||||||||
| 6.3 | Stewart 2017 | ES + PFMT vs PFMT | IM | Beuttenmuller 2010; Haig 1995; Patil 2010; Schmidt 2009 (n = 193) | SMD | −0.35 (−0.64 to −0.05) | < 0 favours ES + PFMT | YES for ES + PFMT | GRADE as assessed by review authors |
1Outcome measured by the Incontinence Impact Questionnaire – Revised. 2Outcome measured by the Urinary Distress Inventory, for different pairs of treatment groups from this three‐arm trial. 3Boos 1998 compared two different types of mechanical devices. Abbreviations: CI: confidence interval; FU1: follow‐up one; IM: immediate; MD: mean difference; n: number of participants; PFMT: pelvic floor muscle training; SMD: standardised mean difference. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
Sixteen analyses from four reviews presented data on quality of life for comparisons of one conservative intervention with another conservative intervention (Ayeleke 2015; Lipp 2014; Stewart 2017; Wallace 2004). Of these, 12 related to an immediate measure of quality of life and four to follow‐up measures. Nine analyses compared the effects of two different types of conservative interventions and seven compared two similar types of interventions. Six unique trials contributed data to these analyses.
High‐ or moderate‐certainty evidence
Three analyses provide moderate‐certainty evidence of higher quality of life with one conservative intervention compared to another conservative intervention.
PFMT plus bladder training resulted in better quality of life than bladder training alone at an immediate time point measured using the IIQ‐R and the UDI (two analyses, moderate‐certainty).
PFMT plus bladder training resulted in better quality of life than PFMT alone at an immediate time point measured using the UDI (moderate‐certainty).
Low‐ or very low‐certainty evidence
Thirteen analyses provide low‐ or very low‐certainty evidence.
Any conservative intervention versus another active intervention (non‐conservative)
Symptomatic cure or improvement
For more information, see Table 24.
24. All types of urinary incontinence: primary outcome participant‐reported cure or improvement; conservative versus non‐conservative.
| Analysis code (in review) | Study ID | Comparisons included | Outcome measure (timing of measure) | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| Moderate‐certainty evidence | |||||||||
| 2.1.2 | Alhasso 2005 | Adrenergic agonist vs conservative therapy | UC |
Wells 1991 (n = 157) |
RR | 1.4 (1.1 to 1.8) | > 1 favours drug | YES favours drugs | 1(H) |
| Low‐certainty evidence | |||||||||
| 2.3.2 | Alhasso 2005 | Adrenergic agonist vs conservative therapy | UC |
Wells 1991 (n = 86) |
RR | 0.9 (0.5 to 1.4) | > 1 favours drug; differential dropout from groups, more from PFMT group (P < 0.01) | NO | 4(C, E×2, H) |
| 1.3.1 | Rai 2012 | Anticholinergic drugs vs bladder training | IM |
Macaulay 1987 (n = 29) |
RR | 1.0 (0.7 to 1.3) | > 1 favours bladder training | NO | 3(E×2, H) |
Abbreviations: CI: confidence interval; IM: immediate; n: number of participants; RR: risk ratio; UC: unclear. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
Three analyses from two reviews assessed symptomatic cure or improvement comparing one conservative intervention with a non‐conservative intervention (Alhasso 2005; Rai 2012). One outcome was at an immediate time point and two were unclear. There were two unique trials comparing a conservative intervention with a non‐conservative intervention but only one with an immediate measure of cure of improvement.
High‐ or moderate‐certainty evidence
One analysis provided moderate‐certainty evidence of better cure or improvement with a non‐conservative compared with conservative intervention. An adrenergic agonist (phenylpropanolamine) was more effective than conservative intervention (PFMT), although the timing of the outcome measure was unclear.
Low‐ or very low‐certainty evidence
Two analyses provided low‐certainty evidence.
Condition‐specific quality of life
For more information, see Table 25.
25. All types of urinary incontinence: quality of life; conservative versus non‐conservative.
| Analysis code (in review) | Study ID | Comparisons included | Outcome measure (timing of measure) | Included trials (n) | Effect measure | Effect estimate (CI) | Direction of effect | Evidence of beneficial effect? | Number of downgrades (reason for downgrade) |
| Moderate‐certainty evidence | |||||||||
| 2.13 | Wallace 2004 | Bladder training vs anticholinergic drugs | IM |
Herbison 20041 (n = 34) |
MD | −8.0 (−18.8 to 2.8) | > 0 favours bladder training | NO | 2(E×2) |
| Low‐certainty evidence | |||||||||
| 9.13 | Wallace 2004 | Bladder training + pharmacological treatments vs pharmacological treatment alone | IM |
Herbison 20041 (n = 28) |
MD | 2.0 (−6.8 to 10.8) | > 0 favours anticholinergic + bladder training | NO | 3(C, E×2) |
1Herbison 2004 was a three‐arm trial, where the groups were: bladder training, anticholinergic drug (oxybutynin) and bladder training + anticholinergic drugs. The anticholinergic drug group data within both analyses are the same. Abbreviations: CI: confidence interval; IM: immediate; MD: mean difference; n: number of participants. Codes for GRADE assessment: A: blinding of outcome assessor; B: allocation concealment; C: differential attrition; D: ROBIS domain 2; E: CIs plus sample size; F: heterogeneity using I2 statistic; G: type of UI was unclear or not reported; H: unclear or not reported for blinding, allocation and differential attrition.
Two analyses from one review compared one conservative intervention with a non‐conservative intervention assessing quality of life (Wallace 2004). Both analyses had outcome measures at an immediate time point. The two analyses included only one unique trial (Herbison 2004).
High‐ or moderate‐certainty evidence
One analysis provided moderate‐certainty evidence of no difference between groups.
Bladder training versus anticholinergic drugs measured using the OAB Questionnaire.
Low‐ or very low‐certainty evidence
One analysis provided low‐certainty evidence.
Discussion
Evidence relating to conservative management of urinary incontinence in women
For summary of findings tables by type of UI, see Table 26, Table 27, and Table 28.
26. Stress urinary incontinence: summary of findings – high‐ or moderate‐certainty evidence of beneficial effect on primary outcomes.
| Comparison group | Intervention of greater benefit | Comparison intervention | High‐ or moderate‐certainty evidence relating to cure or improvement | High‐ or moderate‐certainty evidence relating to quality of life | Review |
| Conservative intervention vs control (see Table 8 and Table 9) |
Cones | Control | ✔ | — | Herbison 2013 |
| PFMT + biofeedback | PFMT alone | ✔ | — | Herderschee 2011 | |
| PFMT | Control | ✔ | ✔ | Dumoulin 2018 | |
| Intravaginal mechanical device | No treatment | — | ✔ | Lipp 2014 | |
| ES | No treatment | — | ✔ | Stewart 2017 | |
| 1 conservative intervention vs another conservative intervention (see Table 10 and Table 11) |
Pessary + PFMT | Pessary alone | ✔ | — | Lipp 2014 |
| PFMT | Cones | ✔ | — | Herbison 2013 | |
| PFMT | Intravaginal pessary | ✔ | — | Lipp 2014 | |
| PFMT + adherence strategy | PFMT alone | ✔ | — | Hay‐Smith 2011 | |
| More‐intensive PFMT | Less‐intensive PFMT | ✔ | — | Hay‐Smith 2011 | |
| Conservative intervention vs non‐conservative intervention (see Table 12 and Table 13) |
Acupuncture | Any other treatment | ✔ | — | Wang 2013 |
| SNRI | Conservative | — | ✔ | Mariappan 2005 | |
| PFMT | Urethral injection therapy | — | ✔ | Kirchin 2017 | |
| Open retropubic colposuspension | Conservative | ✔ | — | Lapitan 2017 |
ES: electrical stimulation; PFMT: pelvic floor muscle training; SNRI: serotonin–noradrenaline reuptake inhibitor.
27. Urgency urinary incontinence: summary of findings – high‐ or moderate‐certainty evidence of beneficial effect on primary outcomes.
| Comparison group | Intervention of greater benefit | Comparison intervention | High‐ or moderate‐certainty evidence relating to cure or improvement | High‐ or moderate‐certainty evidence relating to quality of life | Review |
| Conservative intervention vs control (see Table 14 and Table 15) |
PFMT + feedback/biofeedback | Control | ✔ | — | Herderschee 2011 |
| ES | Control | ✔ | — | Stewart 2016 | |
| Bladder training | Control | ✔ | — | Wallace 2004 | |
| ES + PFMT | No active treatment | — | ✔ | Stewart 2016 | |
| 1 conservative intervention vs another conservative intervention (see Table 16 and Table 17) |
ES | Laseropuncture | ✔ | — | Stewart 2016 |
| ES + PFMT | PFMT alone | ✔ | ✔ | Stewart 2016 | |
| ES | PFMT | — | ✔ | Stewart 2016 | |
| Conservative intervention vs non‐conservative intervention (see Table 18 and Table 19) |
Trospium + solifenacin | ES | ✔ | — | Stewart 2016 |
| ES + drugs | Drugs | ✔ | ✔ | Stewart 2016 | |
| ES + PFMT + drugs | Drugs | — | ✔ | Stewart 2016 | |
| Anticholinergic drugs + behavioural interventions (PFMT) | Anticholinergic drugs | ✔ | — | Rai 2012 |
ES: electrical stimulation; PFMT: pelvic floor muscle training.
28. All types of urinary incontinence: summary of findings – high‐ or moderate‐certainty evidence of beneficial effect on primary outcomes.
| Comparison group | Intervention of greater benefit | Comparison intervention | High‐ or moderate‐certainty evidence relating to cure or improvement | High‐ or moderate‐certainty evidence relating to quality of life | Review |
| Conservative intervention vs control (see Table 20 and Table 21) |
PFMT | Control | ✔ | ✔ | Dumoulin 2018 |
| Weight loss | No active intervention | ✔ | — | Imamura 2015 | |
| ES | Control | ✔ | — | Stewart 2016 | |
| Cones | Control | ✔ | — | Herbison 2013 | |
| 1 conservative intervention vs another conservative intervention (see Table 22 and Table 23) |
Home PFMT programme (no health professional supervision) | Structured programme of 'indirect' PFMT (every 2 weeks, individual, health professional contact) | ✔ | — | Hay‐Smith 2011 |
| PFMT + bladder training | Bladder training | ✔ | ✔ | Ayeleke 2015 | |
| More‐intensive PFMT | Less‐intensive PFMT | ✔ | — | Hay‐Smith 2011 | |
| PFMT + bladder training | PFMT | ✔ | — | Wallace 2004 | |
| PFMT + biofeedback + bladder training | PFMT + biofeedback | — | ✔ | Wallace 2004 | |
| Conservative intervention vs non‐conservative intervention (see Table 24 and Table 25) |
Adrenergic agonist | Conservative interventions | ✔ | — | Alhasso 2005 |
ES: electrical stimulation; PFMT: pelvic floor muscle training.
There are 29 Cochrane Reviews reporting evidence relevant to the conservative management of UI in women (see Table 1). There were 12 Cochrane Protocols relevant to this topic but two have been withdrawn, leaving a further 10 potential reviews (see Appendix 6).
Of the 29 included Cochrane Reviews, 18 contained data and analyses relating to the primary outcomes and comparisons of relevance to this overview (including multiple additional analyses relating to a wide range of secondary outcomes (see Appendix 7), data from which have not been synthesised within this overview). Seventy per cent of the analyses (134/192) related to the effect of conservative management of UI on symptomatic cure or improvement, and 30% (58/192) related to condition‐specific quality of life. Eighty‐one per cent of these analyses included data from only one trial. Therefore, this body of evidence comprises a relatively large number of Cochrane Reviews, synthesising a relatively small number of trials within a relatively large number of analyses.
There was a lack of high‐certainty evidence relating to conservative management of UI. We judged only 9% (17/192) of analyses to provide high‐certainty evidence relating to one of our primary outcomes. Most of the evidence relating to the effect of conservative interventions was low‐ to moderate‐certainty. We found that analyses from populations with UUI were more likely to be of moderate‐certainty, while those from populations with AUI were more likely to be of low‐certainty. However, analyses from populations with UUI were more likely to include data from only one trial.
For SUI, the main focus of research was PFMT. PFMT was primarily compared to a control intervention or to the addition of biofeedback. Further comparisons included adding electrical stimulation or intravaginal devices to a PFMT programme. There was a limited amount reported on mechanical devices, electrical stimulation, Macroplastique injections or drugs. For UUI, pharmaceutical interventions were the most frequently studied and these were primarily compared with electrical stimulation, education, behavioural or lifestyle advice, and PFMT in various combinations. There was a particular lack of evidence relating to quality of life outcomes for women with UUI, with the only analyses relating to this outcome focused on comparisons with electrical stimulation. For AUI, similar to SUI, the main focus of research was PFMT delivered with and without a variety of adjuncts. There was some evidence relating to the effect of educational and lifestyle interventions on quality of life for women with AUI, delivered both with and without PFMT and adjuncts.
Assessment of the quality of the reviews and the certainty of evidence within the Cochrane Reviews highlighted several methodological limitations relating to reporting, quality and definition of key parameters. This arguably presents challenges to clinicians and policymakers, who will have to be familiar with a large number of reviews and aware of the overlapping evidence between reviews in order to make informed evidence‐based clinical decisions. Therefore, this overview has an important role in synthesising the best evidence on conservative interventions for UI into a single, accessible, comprehensive document to signpost clinicians and policymakers towards relevant Cochrane Reviews to support clinical decisions.
Role of the stakeholder group
Conservative interventions of relevance to this overview were identified at the protocol stage by a stakeholder group, using consensus decision‐making techniques based on the nominal group technique. Six broad categories of conservative intervention were identified, each with multiple subcategories (see Figure 1). The Cochrane Reviews included in this overview assessed trials of interventions from four of these categories, with most focusing on physical therapy, educational, behavioural or lifestyle interventions, or mechanical devices (see Table 29). There was no evidence specifically relating to the predefined subcategory of psychological therapies within the included Cochrane Reviews. Moreover, exploration of intervention descriptions revealed that interventions were often delivered in combination, rather than singularly, and that reporting within the trials of the details of the delivered intervention and the 'control' were often poor. This causes significant challenges in the synthesis and interpretation of the available evidence.
29. Identification of relevant reviews mapped to six primary conservative categories.
| Primary conservative intervention (categories) | Review |
| Educational/behavioural/lifestyle | Imamura 2015 – lifestyle intervention Wallace 2004 – bladder training Ostaszkiewicz 2004a – habit training Ostaszkiewicz 2004a – timed voiding Eustice 2000 – prompted voiding |
| Physical therapies | Ayeleke 2015 – pelvic floor muscle training + another active treatment vs the same active treatment alone Dumoulin 2018 – pelvic floor muscle training vs no treatment, or inactive control treatments Hay‐Smith 2011 – comparisons of approaches to pelvic floor muscle training Herderschee 2011 – feedback or biofeedback Herbison 2013 – cones Stewart 2016 and Stewart 2017 – electrical stimulation |
| Psychological therapies | — |
| Mechanical devices | Lipp 2014 – mechanical devices |
| Complementary therapies | Wang 2013 – acupuncture |
| Others | Wieland 2019 – yoga |
The stakeholder group also highlighted the need to present evidence according to populations of women with SUI, MUI or UUI, and we have used these as far as possible following the International Continence Society definitions (Haylen 2010 and, if appropriate, D'Ancona 2019). However, there are substantial inconsistencies within the literature in terms of diagnosis and definition of these conditions and, subsequently, some trials and Cochrane Reviews include mixed populations while others are limited to a population with a specific diagnosis or set of symptoms. In practice, we found that we were often unable to distinguish between 'mixed', 'combined' and 'unclear' populations, and, therefore, brought all data relating to mixed, combined or unclear populations into a group for all types of UI (AUI) (see Differences between protocol and review). These challenges and variations within the current evidence base again highlight the need for an accessible overview that summarises the evidence in a comprehensive, consistent and coherent manner.
Summary of main results
Evidence of effectiveness of conservative interventions
Evidence from the trials in the included Cochrane Reviews has been collated within numerous analyses. Around 25% of the reported analyses related to our first primary outcome of cure or improvement but very few (only around 10%) related to our second primary outcome of participant‐reported quality of life. Interpretation of the results of the high‐certainty and moderate‐certainty evidence was challenging due to a number of factors, in particular the investigation of multimodal (rather than singular) interventions, poorly defined and described interventions and control group interventions, and the wide variety of outcome measures and methods of reporting and analysis.
Based on our assessment of the evidence, we are highly certain that PFMT is more beneficial than control for all types of UI for the primary outcomes of cure or improvement and quality of life. We are moderately certain that if the PFMT is more intense, more frequent, with individual supervision, or combined with behavioural interventions or an adherence strategy effectiveness is improved (or a combination of these) effectiveness is improved. We are also highly certain that for our primary outcome of cure or improvement there was benefit associated with the use of cones compared to a control for women with SUI (but not compared to PFMT), electrical stimulation was beneficial for women with UUI and weight loss reduced symptoms in women with AUI compared to control.
Conservative interventions with little or no evidence
Of the six primary conservative intervention categories identified by our stakeholders, four were covered by relevant Cochrane Reviews (see Table 29). The Cochrane Reviews identified a lack of evidence relating to the use of psychological therapies for the conservative management of UI, despite the fact that these approaches are increasingly used within clinical practice. The only Cochrane Review of complementary therapies in this topic area focused on acupuncture, and identified and included only one trial.
We identified five Cochrane Reviews relating to education, behaviour or lifestyle interventions. There was no high‐ or moderate‐certainty evidence for most lifestyle interventions, despite the fact that anecdotal evidence suggests that interventions such as fluid reduction or change in caffeine, diet, exercise smoking cessation and education are frequently delivered within clinical practice. Although four Cochrane Reviews synthesised evidence relating to voiding interventions, they all had very limited evidence, perhaps highlighting the difficulty in undertaking relevant research in these areas where often there are multicausative factors, multimorbidities and participants may be older and potentially in residential care.
We found a lack of evidence relating to a number of physical therapy interventions, including the use of manual therapies, ultrasound, and dynamometry biofeedback and magnetic stimulation. Evidence relating to the effect of electrical stimulation was only considered in the population of women with OAB.
Summary of evidence of effect of key interventions
Stress urinary incontinence
Fourteen Cochrane Reviews synthesised evidence relating to SUI. These contained 84 analyses relevant to the primary outcomes of this overview.
Most evidence was moderate‐ or low‐certainty.
There was some high‐ or moderate‐certainty evidence relating to cones, PFMT and intravaginal mechanical devices.
There was relatively little evidence relating to primary outcomes, particularly quality of life, and virtually no long‐term follow‐up data.
Table 26 summarises where there was moderate‐ or high‐certainty evidence of a benefit of one intervention, for primary outcomes of cure of improvement or quality of life, and signposts the reviews within which this evidence was synthesised.
Urgency urinary incontinence
Seven Cochrane Reviews synthesised evidence relating to UUI, but only five contained analyses relevant to the primary outcomes of this overview. These contained 47 relevant analyses relevant to the primary outcomes of this overview.
Most evidence was moderate‐ or low‐certainty.
There was some moderate‐ and high‐certainty evidence indicating effectiveness of PFMT, electrical stimulation and bladder training when compared to no treatment or a control treatment.
There was relatively little evidence relating to primary outcomes, particularly quality of life, and virtually no long‐term follow‐up data.
Table 27 summarises where there was moderate‐ or high‐certainty evidence of a benefit of one intervention, for primary outcomes of cure of improvement or quality of life, and signposts the Cochrane Reviews within which this evidence was synthesised.
All types of urinary incontinence
Thirteen Cochrane Reviews synthesised evidence relating to AUI. These contained 61 analyses relevant to the primary outcomes of this overview.
Most evidence was moderate‐ or low‐certainty, but there was some high‐certainty evidence relating to weight loss and PFMT.
There was some moderate‐ or high‐certainty evidence that PFMT, weight loss, electrical stimulation and cones may be more beneficial than control (no treatment or placebo treatment), and that PFMT that was more intense, more frequent, with individual supervision, or combined with behavioural interventions or an adherence strategy effectiveness (or a combination of these) may be more beneficial than less‐intense or frequent PFMT, or PFMT that has no individual supervision, and is not combined with behavioural interventions or adherence strategies.
There was relatively little evidence relating to primary outcomes, particularly quality of life, and virtually no long‐term follow‐up data.
Table 28 summarises where there was moderate‐ or high‐certainty evidence of a benefit of one intervention, for primary outcomes of cure of improvement or quality of life, and signposts the Cochrane Reviews within which this evidence was synthesised.
Overall completeness and applicability of evidence
Interventions covered by Cochrane Reviews
Despite a relatively large number of Cochrane Reviews synthesising evidence relating to interventions for UI (29) and multiple analyses presenting data relating to the effectiveness of conservative interventions, review evidence relating to conservative interventions for UI was not complete.
The trials included within the reviews included 8975 participants with data for one of our primary outcomes, with a mean of about 80 participants per trial (standard deviation 94; range 14 to 738). Given the number and variety of potential conservative interventions for UI, the number of trials and participants is arguably relatively low, while the number of Cochrane Reviews and analyses are high. The high number of Cochrane Reviews is primarily because of 'splitting' of reviews, with many of the included Cochrane Reviews addressing highly specific and narrow research questions (Weir 2012). For example, four included reviews were focused on PFMT, with each review addressed a very narrow question: PFMT versus no treatment, placebo or sham treatment; PFMT combined with other active treatment; PFMT combined with feedback and different approaches to PFMT (Ayeleke 2015; Dumoulin 2018; Hay‐Smith 2011; Herderschee 2011). There is an argument for first demonstrating the effectiveness of an intervention compared to no treatment or placebo treatment, before determining whether reviews comparing different interventions or approaches to an intervention can be justified. While it can be argued that such narrow reviews will have some advantages, such as greater homogeneity of studies, the disadvantage may be that the evidence is less accessible to clinical decision‐makers when split across multiple reviews (Weir 2012). Conversely, Cochrane Reviews addressing broad research questions, which are not supported by network meta‐analyses that explore differences between interventions, may become large and unwieldy and, therefore, also difficult to access. Furthermore, this pattern of splitting reviews results in some trials being included in more than one review, which can potentially mislead readers (who are unlikely to spend time checking the overlap between reviews) into believing that the volume of evidence is greater than it is. Of the 112 unique trials reporting primary outcome data and summarised within analyses relevant to this overview, 17 were included in two or more reviews.
Despite the high number of Cochrane Reviews included in this overview, there were a number of conservative interventions identified as important by our stakeholder group for which no Cochrane Reviews were identified. Our searching identified 10 published protocols, some of which will address conservative interventions or populations for which there is no existing Cochrane Review, which may fill some of the current gaps in evidence (e.g. Khazali 2016; Ostaszkiewicz 2013; Reynard 2016; see Appendix 6). However, some are likely to overlap with existing reviews, including trials that have already been included within reviews. Therefore, it is unclear whether these new reviews will add clarity to this already complex body of synthesised evidence or will instead reduce the accessibility of information further.
Commonly, the planning and publication of Cochrane Reviews is dependent on the drive and enthusiasm of individual review authors, with editorial oversight that aims to ensure coverage without excessive overlap. Despite concerted efforts to focus reviews on distinct pairwise comparisons, issues of lumping, splitting and overlapping have arisen within the topics covered. Systematic reviews can play a key role in the avoidance of research waste, ensuring that there is full knowledge of what is already known but poorly planned, overlapping reviews can contribute to research waste (Berge 2017; Chalmers 2009; Chalmers 2014; Pollock 2014), and Cochrane has an important role in determining how best to achieve optimal accessibility of evidence with minimal overlap.
With our stakeholder group highlighting conservative interventions for which no Cochrane Review evidence exists, there is a clear need for careful consideration of this body of Cochrane Reviews and the introduction of clear strategies for prioritisation of future reviews. Cochrane has identified the need for robust prioritisation methods and processes (Bero 2012), and the Cochrane Knowledge Translation Priority Setting Working Group has defined a set of standards and materials to support priority setting for Cochrane Reviews (Cochrane Priority Setting Guidance). In order to optimise research efficiency and enhance accessibility of evidence, we believe that there is a need to continue to develop and implement clear, strategic plans to ensure that Cochrane Reviews address what is of greatest importance to the end‐users of the reviews in a manner that is easily accessible. It may be beneficial to use enhanced strategies to ensure meaningful involvement of key stakeholders in all aspects of review prioritisation, planning, conduct and reporting (Pollock 2018).
Outcomes within included reviews
The inclusion of relevant outcomes, which matter to people affected by UI, is of key importance to the content of individual reviews.
As well as ensuring that outcomes within trials and reviews are validated and relevant, it is important that the long‐term effect of interventions is investigated and reported. This overview highlights that less than 20% of the analyses reported in the reviews related to follow‐up outcomes for our primary outcomes of interest. Furthermore, the timing of the outcome assessment was often unclear. Clearly it is essential that future trials are designed to incorporate appropriate long‐term follow‐up in order that the clinical and cost‐effectiveness of interventions can be truly understood. Therefore, we would recommend that researchers make plans to follow up participants longer term, both through data linkage and obtaining consent for contact with the participant over several years. Timing of outcome assessment should be clearly reported within trials and Cochrane Reviews. Health economics data, although often identified as an outcome in the reviews, is only briefly reported within four trials, investigating conservative interventions, and one trial exploring surgical interventions. None attempted to identify and summarise cost and cost‐effectiveness data.
There are limitations within the current evidence base in relation to the outcomes that are reported in the trials and pooled within analyses within the Cochrane Reviews. The challenges in pooling data from the completed trials when they have used and reported different measures of outcomes arguably provides an explanation for the fact that we found that 81% of the relevant analyses only included data from one trial. The inability to pool outcome data from trials investigating the same or similar interventions is a key limitation of the current evidence relating to conservative interventions for UI, and we urge trialists to ensure that outcome measures are validated and reflect outcomes of importance. It is also essential that review authors adhere to Cochrane standards by prestating relevant outcomes and measures, clearly stating how these will be incorporated into meta‐analyses (including the structure of comparisons and subgroups, and decisions on combining of measures assessing similar domains).
Our stakeholder group identified that how women feel about and cope with incontinence is of key importance and that consequently patient‐reported quality of life is a high priority outcome. However, there is currently a lack of evidence relating to this outcome, with predominantly objective measures analysed within current Cochrane Reviews. These objective measures do not necessarily correlate with, or reflect, what is of greatest importance to women with UI. Additionally, the stakeholder group identified that a primary outcome for this overview should be "cure or improvement as reported by the woman" (i.e. participant‐reported cure or improvement). We later identified that Cochrane Reviews commonly report outcomes of both participant‐reported cure or improvement and participant‐reported cure. In order to enable comprehensive synthesis of the available Cochrane Review data, we added 'participant‐reported cure' as an additional secondary outcome. However, it is important to note that our focus on 'cure or improvement' as the primary outcome means that data relating to 'cure' only has been incorporated only as a secondary outcome and is therefore omitted from key tables and figures. These key tables and figures focus only on primary outcomes. It is important to note that for outcomes of both participant‐reported 'cure or improvement' (primary outcome) and 'cure' (secondary outcome), we based our categorisation of data on definitions and descriptions included within the Cochrane Reviews. However, there are a range of different definitions used (both within trials and within reviews) and, consequently, measures reported from different reviews, or from different trials within these reviews, may be based on a variety of different definitions.
Furthermore, this overview highlights that there are multiple, diverse secondary outcomes, which are often poorly defined. Initial plans to extract and summarise data from analyses relating to a range of secondary outcomes were not completed due to the number and diversity of secondary outcome data identified (see Differences between protocol and review). In many cases, trials reported the results of unvalidated, poorly defined questionnaires and the results of these have been inputted into several analyses within Cochrane Reviews. Arguably, the production of multiple analyses from one outcome measure, often with only results from a single trial, can mislead readers in relation to the quantity and quality of evidence, creating barriers to the interpretation of evidence.
Quality of the evidence
Assessment of quality of included reviews
Overview authors independently assessed the quality of included reviews using the ROBIS tool (Whiting 2016). The authors involved in the independent assessment of risk of bias using the ROBIS tool all reported challenges in the application of this tool. There were considerable disagreements in the independent assessments. Consensus was reached through discussion between two independent authors for Domains 1 to 3 but could not be reached for Domain 4. Given these challenges, a third independent author (AE) with statistical expertise was involved. After independent assessment and discussion between the three authors to reach a consensus on 50% of the included reviews, many of the original issues that were causing uncertainty and disagreement had been clarified and the original two authors completed the assessments for the remaining 50%. The difficulties in applying and reaching consensus over the ROBIS assessments were a limitation of this overview. However, in order to be transparent about our decision making, wherever a review was judged to have unclear or high risk of bias, we reported our justification for this decision.
Furthermore, we sought clarification around any particular issues that arose relating to the application of the ROBIS tool. For example, initially there was substantial disagreement between independent overview authors in their assessment of risk of bias relating to the search for studies, as many of the included reviews only searched a single database (the Cochrane Incontinence Specialised Register). Guidance was sought from the experts involved in the development of the ROBIS tool through personal communication as to whether a review that only searched this one register should be judged as having a high or low level of concern about the identification of all relevant studies (Whiting 2015 [pers comm]). This led authors to agree that the use of only the Cochrane Incontinence Specialised Register should be judged as a low level of concern as, despite the use of only one database, the register does involve systematic searching of a wide number of databases using comprehensive search strategies.
The ROBIS tool includes a final judgement of overall risk of bias within Phase 3 of the assessment process. We had originally planned to implement this final phase of the ROBIS tool. However, the lack of agreement between independent authors and challenges in reaching consensus between authors within Phase 2 of the ROBIS tool raised concerns among the overview authors in relation to applying one overall judgement. Given the complex discussion and decision‐making involved in reaching consensus over the Phase 2 domains, overview authors considered that it would be challenging to reach one overall judgement and also that this risked implementing a reductionist approach. Overview authors considered that just one overall judgement may fail to recognise subtle differences in the strengths and limitations between the included reviews and may encourage readers of this overview to use this as a summary 'quality score' (Whiting 2016). Rather than report this final judgement, we therefore opted to report the agreed responses to the three signalling questions, believing that this provides a more transparent and open reporting of our judgements. Where we answered a signalling question as 'probably no' or 'unclear', we provided a reason for this answer. We did not use the responses 'yes' or 'no' in our answers to any of the signalling questions, as we did not consider it to be possible for us to be completely certain in our responses.
There clearly are a number of challenges associated with the use of the ROBIS tool to assess risk of bias of reviews included in an overview and further work and guidance to address the issues that we experienced would be beneficial. However, we believe that our transparent reporting of our judgements using this tool, and by avoidance of a final overall, potentially reductionist judgement that may mask differences between reviews, are strengths of our approach.
Quality of included reviews
We have provided a detailed, transparent assessment of the quality of included reviews using the ROBIS tool (Table 3; Figure 3). Notwithstanding our difficulties with using the ROBIS tool, around half of the included reviews were at high risk of bias in relation to the methods and approach to the method and reporting of the syntheses. The concerns related to both limitations in the information provided within trials and the methods of synthesising trials within the reviews. As discussed earlier, methodological limitations in the conduct or reporting (or both) of trials and reviews relating to conservative interventions for UI present challenges to interpretation and the conclusions that can be drawn. This includes paying particular attention to the outcomes used within trials and synthesised within reviews in order that future research is relevant and meaningful to people affected by UI. It is essential that future research in this field addresses these methodological limitations. It is particularly important that future research has adequate reporting and we urge researchers to adhere to relevant reporting guidelines for trials and reviews (Liberati 2009; Moher 2005).
Assessment of certainty of evidence in included reviews
We planned to use an objective algorithm as, despite uncertainty about the appropriateness of this approach to GRADE, we anticipated having a large quantity of analyses to quality assess and considered the use of a transparent, objective process would be beneficial (Pollock 2016). Building on previous work, we developed an objective algorithm to apply GRADE levels of evidence (Pollock 2014; Pollock 2016). The criteria that we used within the objective algorithm were developed within detailed discussions among the overview authors. The agreed criteria are presented in Appendix 3 and our method of applying these criteria outlined in the methods section. However, we do acknowledge the concerns that have been voiced in relation to this approach and recognise that both this approach and the particular cut‐offs and 'weightings' selected for use within the algorithm require systematic exploration (Gionfriddo 2016; Murad 2016). The application of rigid cut‐offs for objective criteria potentially means that two analyses, which may subjectively appear fairly similar in relation to the certainty of evidence synthesised, could result in differing objectively applied GRADEs.
A complex relationship exists between the criteria contributing to our judgement of certainty of evidence. For example, in an attempt to address concerns relating to the use of sample size as the sole criterion to judge imprecision used by Pollock 2014, our algorithm considered both the CIs and the sample size. If the 95% CIs did not include an RR of 1.0 (or MD of 0) then there was no downgrade (regardless of sample size). However, if the 95% CIs did include an RR of 1.0 (or MD of 0) then there was a downgrade if the sample size was fewer than 344 participants. In this way, fewer downgrades are applied to analyses that demonstrate statistical significance and analyses that do not demonstrate statistical significance will be downgraded at least once (twice if the sample size is fewer than 258 participants). Many of the analyses within this overview did have small sample sizes, meaning that analyses with statistically non‐significant findings were downgraded twice. This system may potentially result in us overemphasising and reporting greater certainty in the statistically significant findings. Further exploration into appropriateness of this is important.
The lack of indepth exploration of the impact of the criteria used within this algorithm is clearly a limitation of this overview. For example, our algorithm will also downgrade to low certainty any analyses where the CI rules out a clinically important difference in favour or one or other of the interventions. This is unlikely to be an issue in this overview but may be in others. However, until further guidance is available relating to the use of GRADE within overviews, we believe that this objective application and determination of GRADE levels of evidence enhance the transparency and consistency of this overview. There is a new 'GRADE in overviews' project group, exploring these issues and aiming to develop relevant guidance, and we await the recommendation of this group with interest.
Potential biases in the overview process
One of the limitations of this overview was that we only included Cochrane Reviews. However, we made this decision based on our knowledge of Cochrane methodology and that only RCTs would be included. We are relatively certain that we were able to identify all Cochrane Reviews relevant to the conservative management of UI. However, many of these are now out‐of‐date and consequently, there could be included trials that have not been incorporated in this evidence base (Alhasso 2005; Cody 2012; Duthie 2011; Eustice 2000; Hay‐Smith 2011; Herbison 2009; Herderschee 2011; Kirchin 2017; Mariappan 2005; Ostaszkiewicz 2004a; Ostaszkiewicz 2004b; Saraswat 2020; Wallace 2004).
However, even with our restriction to Cochrane Reviews, the quality of the reviews included in this overview and the quality of the trials included within these reviews, have varied substantially. Additional sources of potential bias includes the fact that there was overlapping trial evidence between reviews, which we systematically explored and included and deleted as relevant. Our decision to exclude analyses that included men also presents a possible source of bias, as does the decision to exclude analyses were the outcomes synthesised were unclear. The methodological limitations within both the reviews and the studies included within the reviews mean that all evidence within this overview should be interpreted with caution, as several biases may exist.
As identified above, there may be bias within our use of ROBIS and GRADE but we have been transparent about our processes and the use of the objective algorithm for GRADE has made it consistent and reproducible. The use of thresholds within our approach to GRADE may have introduced biases to our assessment of certainty of evidence, as there are important limitations relating to thresholds. For example, our algorithm considered the proportion of studies at risk of bias, rather than the impact of studies with a high risk of bias on the size and direction of effect. Also, our algorithm places emphasis on the statistical significance of results, rather than on a judgement of what is clinically important or relevant. We recommend further research to explore the validity and impact of an algorithmic approach to applying GRADE within overviews.
Agreements and disagreements with other studies or reviews
The main finding of this overview was that PFMT is effective for curing or improving the symptoms of most types of UI, with some evidence that more 'intense' training provides an even better outcome. However, there is a particular need to establish evidence related to 'intensity' or the dose of intervention as this has widespread implications for clinical practice, organisation of services and future research, and indeed, adherence to the intervention by women.
These findings are supported by a systematic review and economic modelling of the effectiveness and cost‐effectiveness of non‐surgical treatments for women with SUI, which was a Health Technology Assessment monograph, which synthesised evidence from a range of sources, including Cochrane Reviews (Imamura 2010). It included a survey of 188 women with SUI to identify outcomes of importance to them (activities of daily living, sex, hygiene and lifestyle issues, emotional health and availability of services), as well as a systematic review considering five generic interventions (PFMT, ES, vaginal cones, bladder training and SNRI). This review identified that for women with SUI, there was evidence that more‐intense PFMT appeared to be the most effective treatment in terms of cure, while basic PFMT was better than no treatment in terms of improvement. We agree with these conclusions, although there is little evidence to support an optimal form of more‐intense PFMT (e.g. in the amount of supervision, individual assessment, type of supervision, use of adjuncts or aids de memoir, frequency of exercise) and current data for most comparisons were sparse.
Interpretation needs to be carefully considered, as confounders are frequent. For example, trials comparing biofeedback to no biofeedback often have widely different levels of contact with the clinician. These findings are also supported by the included Hay‐Smith 2011 review, which reported women receiving regular (e.g. weekly) supervision were more likely to report improvement than women doing PFMT with little or no supervision. A more recent review compared individual supervision, group supervision and home unsupervised PFMT (Paiva 2017). Despite considerable heterogeneity between protocols and low methodological quality, it was reported that PFMT was an efficient technique for the improvement of the symptoms of female UI, both in groups and individually with no significant differences between groups. However, group intervention was more efficient than home PFMT.
Other important issues regarding implications
Women need to be consulted about the type of treatment and setting they would like, including whether supported self‐management is an option. What is not in doubt is that, with increasingly ageing demographics, the number of women with UI is set to rise and there may not be sufficient trained clinicians to deliver some treatments to everyone. More specialists need to be trained, which may be costly, but options such as training generalists or the use of apps (applications for smartphones, etc.) need to be explored. Many of the conservative management options described in this overview involve long‐term changes to daily life activities and adherence to long‐term PFMT. Therefore, it is important that we explore how to maintain women's long‐term adherence to therapy.
Authors' conclusions
There is a relatively large number of overlapping Cochrane Reviews with small numbers of trials related to interventions to improve urinary incontinence (UI) in women and this overview serves to signpost clinicians and policymakers toward relevant systematic reviews to support clinical decisions, providing a single, accessible and comprehensive document that brings together all relevant reviews. This overview should also play a key role in research prioritisation, ensuring effective use of resources, promoting collaborative working toward shared priorities and avoiding duplication of effort.
Implications for practice.
A diverse range of conservative interventions are aimed at curing or improving UI in women. In general, evidence is of low‐certainty and does not support clear clinical decisions. However, there is certainty that pelvic floor muscle training (PFMT) is effective for most types of UI, at least in the short‐term. The dose or intensity or the benefits of using adjuncts is less clear. However, clinical application of evidence will depend on specific details of an individual patient or setting, or both, and clinical decisions will require expert clinical reasoning and judgement if available evidence is to be interpreted and applied effectively.
It would also seem that, at present, there are many interventions used routinely with little evidence of effect. Often it is a package of interventions that is offered to the patient. Expert opinion cannot be ignored and clinical reasoning is important when selecting and implementing interventions on the basis of individual patient assessment. However, there may at times be a danger of continuing to do things because it has always been done and they seem to work for some patients, or of starting to use techniques or devices due to anecdotal evidence about how good they are. The conservative interventions, and indeed most of the devices described in the overview, are unlike drugs, which go through rigorous trials before being licensed. However, it is important that we aspire to appropriate evidence‐based and cost‐effective conservative interventions that are attractive to commissioners, policymakers and patients.
Implications for research.
Further research is urgently required to establish high‐certainty evidence related to interventions to cure or improve urinary incontinence in women. This includes new and updated Cochrane Reviews and randomised controlled trials (RCTs). Care should be taken to ensure that both reviews and RCTs are of the highest possible methodological quality, with comprehensive reporting (see EQUATOR 2021 network).
In order to avoid research waste and ensure that evidence relating to the effectiveness of conservative interventions for UI is easily accessible to end‐users, any new and updated Cochrane Reviews should be carefully planned. New reviews should be planned in order to synthesise evidence relating to interventions that have been identified as clinically relevant and important by key stakeholders. For example, there are no reviews on manual therapy techniques as a treatment, or on the use of ultrasound as a biofeedback tool.
Careful consideration should be given to issues of lumping and splitting, ensuring that reviews address questions that are clinically useful and that the same evidence is not synthesised within multiple overlapping reviews. Outcomes should focus on what matters to women: quality of life, health economic outcomes and long‐term benefits. Behavioural change techniques, such as the use of apps, should be explored to improve adherence in the short and long term.
Further research is clearly required to establish high‐certainty evidence of effectiveness and cost‐effectiveness related to interventions to improve UI in women, as is effective collaboration to support large, robust RCTs of interventions currently used routinely within clinical practice. In particular, arising from but not limited to, the results of this overview, we believe that the following research is justified and important.
High‐quality RCTs related to the intensity and dose of PFMT. Dose should always be considered when primary and secondary research is planned and performed.
Full‐scale (Phase 3) RCTs to establish the benefits of electrical stimulation in its various forms and on all populations.
High‐quality RCTs to establish effectiveness of lifestyle advice interventions (e.g. habit training, timed voiding, bladder training and suppression techniques, weight reduction and fluid advice).
High‐quality RCTs on the benefits of behavioural change techniques and the long‐term adherence to PFMT.
High‐quality RCTs on the use of manual therapy techniques for the relief of urinary symptoms.
What's new
| Date | Event | Description |
|---|---|---|
| 9 September 2022 | Amended | 'public bone' amended to 'pubic bone' in the plain language summary |
History
Protocol first published: Issue 9, 2016 Review first published: Issue 9, 2022
Acknowledgements
We would like to thank members of a stakeholder group who contributed to discussions and consensus agreement over definition and categorisation of conservative interventions, relevant subgroups and outcomes of interest to this overview. We are also grateful to David Hill for his contribution to the protocol of this overview.
We would like to thank the following Cochrane Incontinence editorial base staff members for their help and support with this review: Lyn Ajanaku, Chantale Dumoulin, Peter Herbison, Suzanne Macdonald, Muhammad Imran Omar, Luke Vale and Sheila Wallace.
Appendices
Appendix 1. Summary of stakeholder consensus meetings
Stakeholder group
A stakeholder group of 14 clinicians, service users and commissioners was convened and met on two occasions contributing to protocol development. The School of Health & Life and Health Sciences Ethic's Committee of Glasgow Caledonian University (UK) gave ethical approval for the meeting and members of the group were provided with written information before convening and signed a consent form before the meeting to allow us to tape the proceedings and publish the process.
The first occasion was on the 25 June 2015 at Glasgow Caledonian University. The aim of the meeting was to obtain input from key stakeholders to support the planning of the protocol (Conservative interventions for urinary incontinence in women: an Overview of Cochrane systematic reviews) (McClurg 2016).
During the meeting, key issues were explored and group consensus decisions were made using the Nominal Group Technique (NGT) (Pollock 2015). The key issues covered within the first meeting were:
conservative interventions for UI – what should be included in the overview, and how should these be categorised?
how the evidence should be collated within the overview to ensure that it is accessible and clinically relevant.
Decisions reached in relation to these two issues are summarised below (A to D). These decisions informed the protocol for the Cochrane Overview.
The stakeholder group were kept up‐to‐date with the progress of the project by email in March 2016.
A second meeting was held on the 17 May 2016 at Glasgow Caledonian University. Eleven attendees were provided with an update on progress and that 27 possible reviews had been identified that focused on conservative interventions with relevant results. At this meeting, group discussions centred around coding of the intervention at three layers of complexity, and how to present findings and GRADE quality. Decisions reached in relation to these issues are summarised below (E and F).
Stakeholder group decisions
A. Conservative interventions for urinary incontinence
Discussion centred around a mindmap of possible conservative treatments, and table of related definitions, which had been drafted by researchers prior to the meeting. The meeting participants discussed each 'branch' of the mindmap, mapping out modifications and amendments on flipchart paper until agreement was reached. The interventions were broadly categorised into six overarching groups (see Figure 1 in McClurg 2016).
educational/behavioural/lifestyle advice;
physical therapies;
psychological therapies;
mechanical devices;
complementary therapies; and
others.
Each category had multiple subcategories, for example educational/behavioural/lifestyle advice had subcategories of diet, exercise, fluid, voiding interventions, etc.
B. How this evidence should be brought together
There was discussion around the different groups of people who should be included in the overview, including different types of incontinence, other neurological and health‐related disorders, and demographic and clinical variables that were considered important when interpreting evidence.
Using the NGT, the group agreed that the following were key points for inclusion in the protocol for the overview.
-
Type of incontinence
Evidence relating to women with stress urinary incontinence (SUI), urgency urinary incontinence (UUI) or mixed urinary incontinence (MUI) should be presented separately within the overview.
Evidence relating to urge incontinence, data relating to nocturia should be presented as a subgroup.
-
Other health‐related problems
Any evidence from women aged 18 years and older with UI, regardless of cause and comorbidities, should be included in this overview.
Other health‐related problems may include cancer, neurological diseases, chronic respiratory disease, learning difficulties and dementia. People living in care home environments were also included.
C. Subgroups
When discussing how the evidence should be brought together, a number of important subgroups were identified. In order of priority, the following topics (and relevant subgroups) were identified as relevance to this overview:
Severity of symptoms
Pregnancy (pregnancy/no pregnancy, antenatal/postnatal/mode of delivery)
Cause (see health‐related problems, above for relevant subgroups)
Age
Premenopausal/postmenopausal
Comorbidities
Body mass index
Normal/obese/morbidly obese
Ethnicity
Duration of symptoms
Place of living
Living at home/living in care home or nursing home)
Socioeconomic status
D. Outcomes
The stakeholder group generated and prioritised a list of outcomes that they perceived were relevant to the overview.
Primary outcomes should be cure or improvement and condition‐specific quality of life
-
Secondary outcomes should include:
generic quality of life
adverse events
anxiety/depression
amount of leakage (e.g. pad test; pad usage relating to amount (usage per se))
patient‐held diary – incontinence episodes, frequency, number of voids
pelvic floor muscle strength/function
skin integrity
adherence
usability/acceptability
urodynamic
E. Intervention coding
In order to map the evidence or to perform statistical analysis the comparisons required grouping by coding the interventions. The overview authors had attempted to do this at three different levels of detail, but had difficulty in categorising the intervention and control in the same detail in a way that would be meaningful to the end‐user. The members of the stakeholder group were asked to help with coding of three reviews and rules established would then be applied to the other reviews. For example, the use of cones for the treatment of UI compared to a pelvic floor muscle training (PFMT) (Herbison 2013). Cones come under the overarching section of physical therapy (Level 1), cones provide biofeedback (Level 2) and then cones would come under Level 3. The comparison of PFMT, Level 1 would again be physical therapy, Level 2 PFMT and Level 3 would be Individualised or other.
F. How to present findings and grade certainty of evidence?
Discussions on how to present findings and grade certainty of evidence were undertaken using statements that were discussed and reworded accordingly with attendees then completing paper voting slips to note if they agreed or disagreed with the statement (using a five‐point scale).
The following were the statements and the decisions.
-
How results relating to different types of urinary incontinence and different populations should be presented
SUI + MUI should be presented with the combined SUI/UUI/MUI category. Vote result: 8/9 agreed or strongly agreed
Where the type of UI is not reported or unclear explore the impact of adding to the "combined (SUI, UUI, MUI)" category. Vote result: all agreed or strongly agreed
Antenatal and postnatal populations should be presented separately. Vote result: all agreed or strongly agreed
-
How the quality should be graded
Evidence should be downgraded if the type of UI is unclear or unreported. Vote result: 8/9 agreed or strongly agreed
Evidence should be downgraded if the type of UI is combined (SUI, UUI, MUI). Vote result: 6 disagreed, 3 agreed or strongly agreed (so this was not be applied)
Evidence should be downgraded to reflect uncertainty due to unclear or unreported information. Vote result: all agreed or strongly agreed (two attendees had left and did not take part in this vote. Attendees did feel able to state exactly how this downgrading should be carried out.
The outputs from these two meetings fed into our review process and protocol. Following completion of the draft overview the stakeholder group have been involved with facilitating the writing of the clinical guideline and finalising dissemination plans.
Appendix 2. Cochrane Database of Systematic Reviews search strategy
The Cochrane Database of Systematic Reviews (CDSR) was searched from inception to the most recent issue (2021, Issue 1) on 18 January 2021 using the following search strategy:
#1 incontinen*:ti,ab,kw (Word variations have been searched) #2 continen*:ti,ab,kw (Word variations have been searched) #3 MeSH descriptor: [Urinary Bladder, Overactive] explode all trees #4 MeSH descriptor: [Urinary Bladder, Neurogenic] explode all trees #5 MeSH descriptor: [Urinary Incontinence] explode all trees #6 ((bladder or detrusor or vesic*) near/2 (hyper* or overactiv*)).ti,ab,kw. #7 (urin* near/2 (leak* or freq* or urge*)).ti,ab,kw. #8 ((bladder or detrusor or vesic*) near/5 (instab* or stab* or unstab* or irritab* or hyperreflexi* or dys*ynerg* or dyskinesi* or irritat*)).ti,ab,kw. #9 (bladder* near/2 (neuropath* or neurogen* or neurolog*)).ti,ab,kw. #10 (pollakisur* or pollakiur*).ti,ab,kw. #11 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10
Appendix 3. Algorithm for determining GRADE levels of evidence
This table details the objective data used to assign downgrades in order to apply GRADE levels of evidence.
| GRADE criteria | Risk of bias | Publication bias | Imprecision | Inconsistency | Indirectness | ||
| Item assessed for algorithm | Blinding of outcome assessor | Allocation concealment | Differential attrition | ROBIS domain 2 | CIs + sample sizea | Heterogeneity, using I2 statisticb | Clinical heterogeneity |
| No downgrade | < 50% of participants are from trials with high risk of bias for this domain. | < 50% of participants are from trials with high risk of bias for this domain. | Chi2 testc, P ≥ 0.05 OR (if baseline participant numbers not available) < 50% participants are from trials with high risk of bias for differential attrition/loss to follow‐up. |
Low or unclear risk of bias on ROBIS domain 2 | If 95% CI excludes an RR of 1.0, or an MD of 0 | I2 ≤ 50% | Data from participants with SUI and UUI is not combined. AND data from women who are antenatal and postnatal are not combined. |
| 1 downgrade | ≥ 50% of participants are from trials with high risk of bias for this domain. | ≥ 50% of participants are from trials with high risk of bias for this domain. | YES differential attrition – Chi2 testc, P < 0.05 OR (if baseline participant numbers not available) ≥ 50% participants are from trials with high risk of bias for differential attrition/loss to follow‐up. |
High risk of bias on ROBIS domain 2 | If 95% CI includes an RR of 1.0, or an MD of 0 AND sample size < 344 |
I2 > 50% | If data from participants with SUI and participants with UUI are combined OR if data from women who are antenatal and postnatal (as defined by review authors) are combined OR both. |
| 2 downgrades | — | — | — | — | If 95% CI includes an RR of 1.0, or an MD of 0 AND sample size < 258 |
I2 > 75% | — |
| CI: confidence interval; MD: mean difference; ROBIS: Risk of Bias In Systematic Reviews assessment tool; RR: risk ratio; SUI: stress urinary incontinence; UUI: urgency urinary incontinence. | |||||||
Notes relating to the application of the algorithm and justification of key cut‐offs.
Differential attrition
A Chi2 test was used to determine differential attrition. This was based on the number of participants recruited/at baseline as reported in the review (e.g. within the characteristics of included studies table), and the number of participants included in the analysis for that comparison/outcome). A formula was used in Excel to compute the presence (or absence) of differential attrition, based on the formula which Stata uses for two‐sample test of proportions (www.stata.com/manuals13/rprtest.pdf).
Sample size
A downgrade was applied if the combined total sample size was fewer than 344 and two downgrades were applied if the total sample size was fewer than 258.
344 is the sample size required for 90% power to detect a standardised effect size of 0.35 standard deviations (or a difference of 17.5% between two proportions).
258 is the sample size required for 80% power.
Heterogeneity, using the I2 statistic
The Cochrane Handbook for Systematic Reviews of Interventions guidance on I2 values suggests that:
0% to 40% might not be important;
30% to 60% moderate heterogeneity;
50% to 90% substantial heterogeneity;
75% to 100% considerable heterogeneity.
Therefore, within our algorithm we considered that:
unimportant or moderate heterogeneity, i.e. I2 ≤ 50%; no downgrade;
substantial heterogeneity, i.e. I2 > 50% and I2 ≤ 75%; one downgrade;
considerable heterogeneity, i.e. I2 > 75%; two downgrades.
Appendix 4. Intervention categorisation
The interventions investigated in each included study were categorised at three levels:
representing the category of intervention, e.g. physical therapies;
describing the type of intervention, e.g. biofeedback; and
providing the more specific detail, if required, e.g. electromyography (EMG) biofeedback.
Details of these are provided in tables below for both active treatments (Table 15.1) and control treatments (Table 15.2).
This system was introduced as many of the interventions were multimodal or combined. The system was developed in consultation with the stakeholder group to ensure that the level of detail was able to reflect key differences in interventions provided in clinical practice (see Appendix 1; Differences between protocol and review). Where conservative interventions were delivered in combination, they were also categorised at three levels, with the categorisation system amended to ensure that the combined interventions were clearly represented.
Active treatment group codes
| Level 1 | Level 1 abbreviations | Level 2 | Level 2 abbreviations | Level 3 | Level 3 abbreviations |
| Physical therapy | PT | Physical therapy‐biofeedback | PT‐BF | Physical therapy‐PFMT‐individual | PT‐PFMT‐I |
| Educational/behavioural/lifestyle advice | EBL | Physical therapy‐electrical stimulation | PT‐ES | Physical therapy‐PFMT‐other | PT‐PFMT‐O |
| Mechanical devices | MD | Educational/behavioural/lifestyle advice‐voiding intervention | EBL‐VI | Physical therapy‐PFMT‐individual‐individual‐other | PT‐PFMT‐I‐O |
| Complementary | CT | Educational/behavioural/lifestyle advice‐exercise advice | EBL‐EXAD | Physical therapy‐biofeedback‐EMG | PT‐BF‐EMG |
| Psychological | PST | Educational/behavioural/lifestyle advice‐weight loss | EBL‐WTL | Physical therapy‐biofeedback‐manometry/dynomanometry | PT‐BF‐DM |
| Other | O | Mechanical device‐intravaginal | MD‐IV | Physical therapy‐biofeedback‐cones | PT‐BF‐C |
| Pharmacology | PH | Mechanical device‐intraurethral | MD‐IU | Physical therapy‐electrical stimulation‐neuromuscular | PT‐ES‐NM |
| Physical therapy + education | PT+EBL | Complementary therapy‐acupuncture | CT‐ACU | Physical therapy‐electrical stimulation‐neuromodulation | PT‐ES‐ND |
| Physical therapy + mechanical devices | PT+MD | Complementary therapy‐reflexology | CT‐R | Physical therapy‐electrical stimulation‐neuromodulation + complementary‐acupuncture | PT‐ES‐ND+CT‐ACU |
| Physical therapy + complementary | PT+CT | Physical therapy‐PFMT + biofeedback and exercise advice | PT‐PFMT+BF+EBL‐EXAD | Education/behaviour/lifestyle‐voiding interventions‐bladder training | EBL‐VI‐BT |
| Physical therapy + psychological | PT+PST | Physical therapy‐PFMT + electrical stimulation | PT‐PFMT+ES | Education/behaviour/lifestyle‐voiding interventions‐timed voiding | EBL‐VI‐TV |
| Physical therapy + other | PT+O | Complementary therapy‐acupuncture + physical therapy‐ electrical stimulation | PT‐ES+CT‐ACU | Education/behaviour/lifestyle‐voiding interventions‐habit training | EBL‐VI‐HT |
| Physical therapy + pharmacology | PT+PH | Physical therapy‐PFMT + biofeedback | PT‐PFMT+BF | Education/behaviour/lifestyle‐exercise advice | EBL‐EXAD |
| Education/lifestyle/behaviour + pharmacology | EBL+PH | Physical therapy‐PFMT + pharmacology‐drug | PT‐PFMT+Phar‐Dr | Education/behaviour/lifestyle‐weight loss | EBL‐WTL |
| — | — | Education/behaviour/lifestyle‐voiding interventions + pharmacology‐drugs | EBL‐VI+Phar‐drugs | Physical therapy‐PFMT‐other + biofeedback‐EMG + educational/behavioural/lifestyle advice‐exercise advice | PT‐PFMT‐O +BF‐EMG+EBL‐EXAD |
| — | — | Physical therapy‐PFMT + mechanical device‐intravaginal | PT‐PFMT+MD‐IV | Physical therapy‐PFMT‐individual + electrical stimulation‐neuromuscular | PT‐PFMT‐I+ES‐NM |
| — | — | Physical therapy‐PFMT + biofeedback + educational‐voiding interventions | PT‐PFMT+BF+EbL‐VI | Complementary‐acupuncture + electrical stimulation‐neuromodulation | CT‐ACU+ES‐ND |
| — | — | Physical therapy‐electrical stimulation + complementary‐acupuncture | PT‐ES+CT‐ACU | Mechanical devices‐intraurethral | MD‐IU |
| — | — | Physical therapy‐PFMT + complementary‐heat | PF‐PFMT+CT‐Heat | Mechanical device intravaginal | MD‐IV |
| — | — | Education‐voiding intervention‐bladder training | EBL‐VI‐BT | Physical therapy‐PFMT‐I + biofeedback‐EMG | PT‐PFMT‐I+BF‐EMG |
| — | — | Physical therapy‐PFMT obstetric‐prevention | PT‐PFMTO‐PREV | Physical therapy‐PFMT‐I + pharmacology‐drug‐SNRI | PT‐PFMT‐I+Phar‐Dr‐SNRI |
| — | — | Physical therapy‐PFMT obstetric‐treatment | PT‐PFMTO‐TREAT | Physical therapy‐PFMT‐I + pharmacology‐drug‐anticholinergic | PT‐PFMT‐I+Dr‐Anti |
| — | — | — | — | Physical therapy‐PFMT‐individual + biofeedback + voiding intervention‐bladder training | PT‐PFMT‐I+BF+VI+BT |
| — | — | — | — | Physical therapy‐PFMT‐other + biofeedback‐EMG‐ Behavioural/lifestyle/advice‐exercise advice |
PT‐PFMT‐O + BF‐EMG+EBL‐EXAD |
| — | — | — | — | Physical therapy‐PFMT‐I + biofeedback‐cones | PT‐PFMT‐I+BF‐C |
| — | — | — | — | Physical therapy‐PFMT individual and other + biofeedback‐EMG | PT‐PFMT‐I‐O+BF‐EMG |
| — | — | — | — | Physical therapy‐PFMT‐individualised and other + biofeedback‐manometry/dynamometry | PT‐PFMT‐I‐O+BF‐M/D |
| — | — | — | — | Physical therapy‐PFMT‐individual + mechanical devices‐intravaginal‐pessary | PT‐PFMT‐I+MD‐IV‐P |
| — | — | — | — | Physical therapy‐PFMT‐other + mechanical device‐intravaginal | PT‐PFMT‐O+MD‐IV |
| — | — | — | — | Physical therapy‐PFMT‐individual + biofeedback‐ EMG + education/behavioural/advice‐voiding interventions‐bladder training |
PT‐PFMT‐I+BF‐EMG+EBL‐VI‐BT |
| — | — | — | — | Education/behaviour/lifestyle‐voiding interventions‐bladder training + pharmacological‐drug‐anticholinergic | EBL‐VI‐BT+Phar‐Dr‐Anti |
| — | — | — | — | Physical therapy‐PFMT‐individual + biofeedback‐dynamometry/manometry + education/behavioural/advice‐voiding interventions‐bladder training | PT‐PFMT‐I+BF‐DM+EBL‐VI+BT |
| — | — | — | — | Physical therapy‐PFMT‐individual + dynamometry/manometry | PT‐PFMT‐I+BF‐D/M |
| — | — | — | — | Physical therapy‐PFMT‐individual + pharmacological‐drug‐SNRI | PT‐PFMT‐I+Phar‐Dr‐SNRI |
| — | — | — | — | Mechanical devices‐intravaginal‐pessary | MD‐IV‐P |
| — | — | — | — | PT‐PFMT (individualised) + mechanical device‐intravaginal‐pessary | PT‐PFMT‐I+MD‐IV‐P |
| — | — | — | — | Physical therapy‐electrical stimulation‐neuromodulation + complementary‐acupuncture | PT‐ES‐ND+CT‐ACU |
| — | — | — | — | Physical therapy‐PFMT‐other + complementary‐heat | PT‐PFMT‐O+CT‐heat |
| — | — | — | — | Education‐voiding intervention‐prompted voiding | EBL‐VI‐PV |
| — | — | — | — | Physical therapy‐PFMT‐individual + biofeedback‐dynamometry or manometry | PT‐PFMT‐I+BF‐DM |
| — | — | — | — | Education‐voiding intervention‐bladder training‐caffeine reduction | EBL‐VI‐BT‐caff |
| — | — | — | — | Physical therapy‐PFMT‐obstetric‐prevention‐individual | PT‐PFMTO‐Prev‐I |
| — | — | — | — | Physical therapy‐PFMT‐obstetric‐prevention‐other | PT‐PFMTO‐Prev‐O |
| — | — | — | — | Physical therapy‐PFMT‐obstetric‐treatment‐individual | PT‐PFMTO‐Treat‐I |
| — | — | — | — | Physical therapy‐PFMT‐obstetric‐treatment‐other | PT‐PFMTO‐Treat‐O |
Control group codes
| Level 1 | Level 1 abbreviations | Level 2 | Level 2 abbreviations | Level 3 | Level 3 abbreviations |
| Physical therapy | PT | Physical therapy‐biofeedback | PT‐BF | Physical therapy‐pelvic floor muscle training‐individual | PT‐PFMT‐I |
| Educational/behavioural/lifestyle advice | EBL | Physical therapy‐electrical stimulation | PT‐ES | Physical therapy‐pelvic floor muscle training‐other | PT‐PFMT‐O |
| Mechanical Devices | MD | Educational/behavioural/lifestyle advice‐voiding intervention | EBL‐VI | Physical therapy‐pelvic floor muscle training‐individual‐individual‐other | PT‐PFMT‐I‐O |
| Complementary | CT | Educational/behavioural/lifestyle advice‐exercise advice | EBL‐EXAD | Physical therapy‐biofeedback‐EMG | PT‐BF‐EMG |
| Psychological | PST | Educational/behavioural/lifestyle advice‐weight loss | EBL‐WTL | Physical therapy‐biofeedback‐manometry/dynamometry | PT‐BF‐M/D |
| Other | O | Mechanical device‐ intravaginal | MD‐IV | Physical therapy‐biofeedback‐cones | PT‐BF‐C |
| Pharmacology | PH | Mechanical device‐intraurethral | MD‐IU | Physical therapy‐electrical stimulation‐neuromuscular | PT‐ES‐NM |
| Physical therapy + education | PT+EBL | Complementary therapy‐acupuncture | CT‐ACU | Physical therapy‐electrical stimulation‐neuromodulation | PT‐ES‐ND |
| Physical therapy + mechanical devices | PT+MD | Complementary therapy‐reflexology | CT‐R | Physical therapy‐electrical stimulation‐ neuromodulation + complementary‐acupuncture | PT‐ES‐ND+C‐ACU |
| Physical therapy + complementary | PT+CT | Physical therapy‐PFMT + biofeedback and exercise advice | PT‐PFMT+BF‐EXAD | Education/behaviour/lifestyle‐voiding interventions‐bladder training | EBL‐VI‐BT |
| Physical therapy + psychological | PT+PST | Physical therapy‐PFMT + electrical stimulation | PT‐PFMT+ES | Education/behaviour/lifestyle‐voiding interventions‐timed voiding | EBL‐VI‐TV |
| Control | Con | Complementary therapy‐acupuncture + electrical stimulation | CT‐ACU+ES | Education/behaviour/lifestyle‐voiding interventions‐habit training | EBL‐VI‐HT |
| — | — | Physical therapy‐PFMT + biofeedback | PT‐PFMT+BF | Education/behaviour/lifestyle‐exercise advice | EBL‐EXAD |
| — | — | Physical therapy‐PFMT + pharmacology‐drug | PT‐PFMT+pharmacology‐drugs | Education/behaviour/lifestyle‐weight loss | EBL‐WTL |
| — | — | Education/behaviour/lifestyle‐voiding interventions + pharmacology‐drugs | EBL‐VI+pharmacology‐drugs | Physical therapy‐PFMT‐other + biofeedback‐ EMG + educational/behavioural/lifestyle advice‐exercise advice | PT‐PFMT‐O+BF‐EMG+EBL‐EXAD |
| — | — | Physical therapy‐PFMT + mechanical device‐intravaginal | PT‐PFMT+MD‐IV | Physical therapy‐PFMT‐individual + electrical stimulation‐neuromuscular | PT‐PFMT‐I+ES‐NM |
| — | — | Physical therapy‐PFMT + biofeedback + voiding interventions | PT‐PFMT+BF+VI | Complementary‐acupuncture + electrical stimulation‐neuromodulation | CT‐ACU+ES‐ND |
| — | — | Conservative | Con | Mechanical device‐intraurethral | MD‐IU |
| — | — | Pharmacological‐drugs | Ph‐DR | Mechanical devise‐intravaginal | MD‐IV |
| — | — | — | — | Physical therapy‐PFMT‐I + biofeedback‐EMG | PT‐PFMT‐I+BF‐EMG |
| — | — | — | — | Physical therapy‐PFMT‐I + pharmacology‐drug‐SNRI | PT‐PFMT‐I+Phar‐Dr‐SNRI |
| — | — | — | — | Physical therapy‐PFMT‐I + pharmacology‐drug‐anticholinergic | PT‐PFMT‐I+Dr‐Anti |
| — | — | — | — | Physical therapy‐PFMT‐individual + biofeedback + voiding intervention‐bladder training | PT‐PFMT‐I+BF+VI+BT |
| — | — | — | — | Physical therapy‐PFMT‐other + biofeedback‐EMG‐ behavioural/lifestyle/advice‐exercise advice |
PT‐PFMT‐O+BF‐EMG+EXAD |
| — | — | — | — | Physical therapy‐PFMT‐I + biofeedback‐cones | PT‐PFMT‐I+BF‐C |
| — | — | — | — | Physical therapy‐PFMT individual and other + biofeedback‐EMG | PT‐PFMT‐I‐O+BF‐EMG |
| — | — | — | — | Physical therapy‐PFMT‐individualised and other + biofeedback‐manometry / dynamometry | PT‐PFMT‐I‐O+BF‐M/D |
| — | — | — | — | Physical therapy‐PFMT‐individual + mechanical devices‐intravaginal‐pessary | PT‐PFMT‐I+MD‐IV‐P |
| — | — | — | — | Physical therapy‐PFMT‐other + mechanical device‐intravaginal | PT‐PFMT‐O+MD‐IV |
| — | — | — | — | Physical therapy‐PFMT‐Individual + biofeedback‐ EMG + education/behavioural/advice‐voiding interventions‐bladder training |
PT‐PFMT‐I+BF‐EMG+EBL‐VI‐BT |
| — | — | — | — | Conservative | Con |
| — | — | — | — | Mechanical devices‐intravaginal‐pessary | MD‐IV‐P |
| — | — | — | — | Pharmacological‐drugs‐alpha adrenoceptors | Phar‐dr‐alp |
| — | — | — | — | Pharmacological‐drugs‐SNRI | Phar‐dr‐SNRI |
| — | — | — | — | Pharmacological‐drugs‐anticholinergics | Phar‐dr‐anti |
EMG: electromyography; PFMT: pelvic floor muscle training; SNRI: serotonin–noradrenaline reuptake inhibitor.
Appendix 5. Characteristics of excluded reviews
We excluded 16 full‐text reviews.
10 clearly did not meet inclusion criteria (Baessler 2018; Beeckman 2016; Ford 2017; Hagen 2011; Ismail 2010; Jamison 2013; McNaughton Collins 2002; Utomo 2014; Walsh 2015; Woodward 2014).
2 were Cochrane Reviews that would have met our inclusion criteria but they were withdrawn (Hay‐Smith 2007; Hay‐Smith 2008).
4 focused on a specific aetiology or condition, and initially were considered to meet the inclusion criteria; however, discussion among overview authors and editors led to consensus that these reviews should be excluded (Bakali 2019; Farrar 2014; Thomas 2019; Woodley 2020). Further details of these four reviews are provided in the table below.
| Study ID | Objective | Inclusion criteria | Study design | Databases searched | |||
| Population | Intervention | Planned comparisons | Outcome categories | ||||
|
Bakali 2019 (contained no trials) |
To obtain and examine evidence supporting different management strategies for recurrent and persistent SUI in women after failed suburethral tape surgery. | Women of any age with persistent or recurrent SUI after any suburethral tape surgery (failed surgery). |
Any form of previous suburethral tape was included (retropubic, transobturator (either direction), and minimally invasive). |
|
Primary outcomes
Secondary outcomes
|
RCT QRCT | Cochrane Incontinence's Specialised Register |
|
Farrar 2014 (contained no trials) |
To assess the effects of antenatal and intrapartum interventions for women in subsequent pregnancies following a previous obstetric anal sphincter injury to reduce the risk of recurrent injury and associated harms. | Pregnant women who sustained obstetric anal sphincter injury during a previous birth. | Any type of intervention aimed at reducing the risk of harm in a subsequent pregnancy following obstetric anal sphincter injury. | Specific comparisons were not stated, but the aim was to compare any intervention aimed at reducing the risk of harm in a subsequent pregnancy following obstetric anal sphincter injury compared with any other intervention or with routine care, i.e. antenatal interventions such as massage or creams and intrapartum interventions such as vacuum vs selective or routine episiotomy and selective or routine episiotomy with routine care. |
Primary outcomes
Secondary outcomes Perinatal
Long term
Other outcome
|
RCT (not QRCTs or cross‐over studies) | Cochrane Pregnancy and Childbirth Specialised Register – 30 September 2014 |
| Thomas 2019 | To assess the effects of interventions for treating urinary incontinence after stroke in adults ≥ 1‐month poststroke | Adults aged ≥ 18 years with a diagnosis of stroke, including people with incontinence who had had a stroke identified as a subgroup within a larger group for whom relevant data were reported. Not reported in review. Not always reported in trials. Largest age range: 40–96 years. |
An intervention designed to promote urinary continence. Intervention types: behavioural, specialised professional input, complementary, pharmacotherapy and physical therapy. |
|
Primary outcomes
Secondary outcomes
|
RCT QRCT | Cochrane Incontinence's Specialised Register – 30 October 2017 Cochrane Stroke's Specialised Register – 1 November 2017 |
| Woodley 2020 | To determine the effectiveness of PFMT in the prevention or treatment of urinary and faecal incontinence in pregnant or postnatal women. | Antenatal or postnatal women. Women could have urinary, faecal, or both urinary and faecal incontinence symptoms. Note: the review included trials with women who were continent when randomised Age range: 24–42 years |
PFMT – a programme of repeated voluntary pelvic floor muscle contractions taught and supervised by a healthcare professional. All types of PFMT programmes were considered. |
|
Primary outcomes
Secondary outcomes
|
RCT QRCT | Cochrane Incontinence's Specialised Register – 7 August 2019 |
PFMT: pelvic floor muscle training; QRCT: quasi‐randomised controlled trial; RCT: randomised controlled trial.
Appendix 6. Characteristics of included protocols
| Study ID | Objective | Inclusion criteria | ||
| Population | Intervention | Planned comparisons | ||
| Chua 2015 | To assess the overall effects of treatment with beta‐3‐adrenoceptor agonists in adults with OAB | Men and women from any ethnic origin, diagnosed with OAB of either neurogenic or non‐neurogenic aetiology | Any beta‐3‐adrenoceptor agonist |
|
| Cotterill 2018 | To assess the effects of conservative interventions for urinary or faecal incontinence (or both) in adults with multiple sclerosis, compared to no treatment, sham and usual care, any other active treatment, or another conservative treatment. | Men and women aged > 18 years with existing urinary, faecal or anal incontinence (or a combination of these), with a clinical diagnosis of relapsing/remitting, primary or secondary progressive multiple sclerosis | Conservative treatments
|
|
| French 2010 | To determine whether combinations of conservative interventions for UUI, SUI, or MUI reduce the number of people with UI compared with no treatment/usual care, or another intervention | Adults (as defined by study authors) diagnosed either by symptom, sign, or urodynamic study as having any type of UI, excluding people with short‐term incontinence for physiological reasons, e.g. within 1 year of urological surgery or childbirth | Conservative interventions |
|
| Funada 2020 | To assess the effects of bladder training for treating adults with OAB and summarise the principal findings of relevant economic evaluations of this intervention. | Men and women with non‐neurogenic OAB | Bladder training for treating OAB |
|
| Hargreaves 2020 | "To assess the effects of acupuncture for treating OAB in adults; and summarise the principal findings of relevant economic evaluations." | "We will include studies of adults aged over 18 years with a diagnosis of OAB that fits the criteria defined by the International Continence Society…" | "acupuncture interventions intended to treat the symptoms of OAB that involve needle insertion at defined acupuncture points. This includes body acupuncture, scalp acupuncture, auricular acupuncture, and electro‐acupuncture." |
|
| Hajebrahimi 2015 | To determine the effects of non‐drug treatment for LUTS in women with voiding dysfunction. | Women aged > 18 years experiencing LUTS of voiding dysfunction (difficulty voiding), who find them bothersome and seek treatment from voiding dysfunction |
|
|
|
Khazali 2016 (WITHDRAWN) |
To determine the effectiveness of electromagnetic treatment in the management of urinary incontinence in adults. | Men and women with urinary incontinence regardless of type of incontinence or criteria for diagnosis | Electromagnetic treatment. The terms functional extracorporeal magnetic stimulation, functional magnetic stimulation, extracorporeal magnetic innervation, electromagnetic pelvic floor stimulation, extracorporeal magnetic stimulation or any other term used to describe the use of electromagnetic waves to treat incontinence will be assumed to be synonymous with electromagnetic treatment. |
|
| Lane 2020 | To assess the effects of vaginal lasers for treating SUI in women and summarise the principal findings of relevant economic evaluations. | Women with SUI | Vaginal lasers |
|
| Lins 2014 | To determine the effects of PFMT against other single treatment modalities in the management of female SUI, MUI and UUI | Women diagnosed with SUI, UUI or MUI on the basis of symptoms, signs or urodynamic evaluation | PFMT – a programme of repeated voluntary pelvic floor muscle contractions taught or supervised (or both) by a healthcare professional. All types of PFMT programmes are to be considered. PFMT may be combined with biofeedback, if they use biofeedback for the purpose of teaching a pelvic floor muscle contraction or for reinforcement. |
|
| Ostaszkiewicz 2013 | To determine the effectiveness of toileting assistance programmes for managing UI in adults. | Men and women, with or without cognitive impairment, diagnosed as having UI as defined by study authors, either by symptom classification or urodynamic study. | Toileting assistance programme – the intervention must include the presence of a fixed or individualised voiding interval and the use of carers or staff to verbally prompt or physically assist the person to use the toilet |
|
|
Reynard 2016 (WITHDRAWN) |
To determine the effects of conservative (non‐surgical, non‐pharmacological) management of nocturia in adults. | Men and women with nocturia confirmed by questionnaire or frequency/volume chart, or both | Any non‐surgical, non‐pharmacological treatment option that could be used for the treatment of nocturia |
|
| Yi 2014 | To determine the effectiveness and safety of drugs to treat LUTS in women with voiding dysfunction. | Participants with a definite diagnosis of voiding dysfunction according to the International Urogynecological Association or the International Continence Society terminology report (Haylen 2010), or reasonable clinical criteria for the diagnosis of voiding dysfunction. | Any pharmacological treatment |
|
| LUTS: lower urinary tract symptoms; MUI: mixed urinary incontinence; OAB: overactive bladder; PFMT: pelvic floor muscle training; SUI: stress urinary incontinence; UUI: urgency urinary incontinence. | ||||
Appendix 7. Secondary outcome data within reviews
The table below gives an overview of the secondary outcomes included and analysed within each of the included reviews.
| Review | Participant‐reported cure, accepting the definition of participant‐reported cure as used in the review | General quality of life measures (i.e. not condition‐specific), such as Short Form‐36 | Adverse effects (e.g. discomfort, soreness, pain, bleeding) | Measures of anxiety/depression, such as HADS | Other clinician‐measured or observed outcomes (e.g. pad tests, pad weights frequency of UI) | Other participant self‐report not presented as cure or improvement (e.g. data relating to incontinence episodes, frequency, number of voids) | Pelvic muscle floor strength/function (e.g. digital evaluation, pelvic floor muscle dynamometry or electromyography, vaginal squeeze pressure, perineal ultrasound) | Skin integrity | Adherence to intervention (including measures of usability and acceptability) | Urodynamics (urodynamic testing), for example postvoid residual volume, rate of bladder emptying and detrusor pressure | Socioeconomic measures | Any other outcomes |
| Alhasso 2005 | x | p | x | — | p | x | — | — | — | — | p | x |
| Ayeleke 2015 | x | p | x | — | x | x | — | — | — | — | p | x |
| Cody 2012 | x | — | x | — | x | p | x | — | — | — | p | p |
| Dumoulin 2018 | x | p | p | — | x | x | — | — | — | — | p | x |
| Eustice 2000 | — | p | — | — | x | — | — | — | — | — | p | p |
| Glazener 2017a | x | — | — | — | p | p | — | — | — | — | — | p |
| Hay‐Smith 2011 | x | p | — | — | x | p | — | p | — | p | p | |
| Herbison 2013 | x | p | — | — | x | x | x | — | — | — | p | — |
| Herderschee 2011 | x | — | p | — | p | x | — | — | — | — | p | x |
| Imamura 2015 | x | p | p | — | p | x | — | — | — | — | p | p |
| Kirchin 2017 | x | — | x | — | p | p | — | — | — | p | p | p |
| Lapitan 2017 | p | p | p | — | x | x | — | — | — | — | x | x |
| Lipp 2014 | x | x | x | — | x | x | — | — | — | — | p | x |
| Mariappan 2005 | p | p | p | — | p | — | — | — | — | — | p | p |
| Ostaszkiewicz 2004a | — | p | — | — | p | p | — | — | p | — | p | x |
| Ostaszkiewicz 2004b | — | p | — | — | x | p | — | — | p | — | p | — |
| Rai 2012 | x | x | x | — | p | x | — | — | — | — | p | x |
| Stewart 2016 | — | — | x | — | x | x | — | — | — | x | p | x |
| Stewart 2017 | x | p | x | — | x | x | — | — | — | — | x | — |
| Wallace 2004 | x | x | x | — | — | x | — | — | — | — | p | x |
| Wang 2013 | x | p | p | — | p | — | — | — | — | — | p | — |
| Wieland 2019 | p | p | x | — | p | x | — | — | — | — | p | x |
Abbreviations: —: not applicable/reported; HADS: Hospital Anxiety and Depression Scale; p: outcome of interest listed in methods of review; SF‐36: 36‐item Short Form; x: relevant outcome data from trials included within review; UI: urinary incontinence.
Appendix 8. Outcomes for this review
As reported in Appendix 1; first the stakeholder group generated and prioritised the following list of outcomes.
Primary outcomes
Cure or improvement, as reported by the woman
Condition specific quality of life
Secondary outcomes
Generic quality of life
Adverse events
Anxiety/depression
Amount of leakage (e.g. pad test; pad usage relating to amount (usage per se)
Patient‐held diary – incontinence episodes, frequency, number of voids
Pelvic floor muscle strength/function
Skin integrity
Adherence
Usability/acceptability
Urodynamic
The above list was proposed within the protocol for this overview (McClurg 2016). At the stage of peer review, the Cochrane Incontinence editorial group highlighted that within published Cochrane Incontinence reviews it was common for review authors to define, and synthesise/analyse data relating to two separate, but related, outcomes:
symptomatic cure of urinary incontinence (UI);
symptomatic cure or improvement of UI.
Studies included in reviews use a range of different outcome measures to assess participants' perceived response to treatment. For example, Dumoulin 2018 stated that "The studies used many different scales to measure a participant's response to treatment, including Likert scales, visual analogue scales and per cent reduction in symptoms." Data from these scales are commonly used to define participant‐perceived cure or improvement, or both. For example, study authors may define participant‐perceived cure as occurring when "no urine loss" is recorded on a participant‐reported scale; or may define participant perceived cure or improvement as an outcome of "much better" or "somewhat better" on a scale. These definitions may be proposed by study authors or review authors. It is common for Cochrane Incontinence Reviews to use data relating to both "cure" and "cure or improvement", as explained by Dumoulin 2018: "As some trial reports did not differentiate cure from improvement, we used two measures to avoid losing important data ('cure only' or 'cure or improvement')."
While the stakeholder group had defined symptomatic (patient‐reported) cure or improvement as a primary outcome, they had been unaware of the issue that reviews commonly synthesise data for participant‐reported cure, in addition to data for participant‐reported cure or improvement. Consequently, we added 'patient‐reported cure' as an additional secondary outcome for this overview.
In extracting data relating to these outcomes for this overview, we accepted the definitions and categorisation of data presented within the reviews.
As explained in the Differences between protocol and review section, data relating to these secondary outcomes has not been synthesised within this overview.
Differences between protocol and review
Type of urinary incontinence
We anticipated that some reviews may include populations with more than one type of UI. In the protocol, we proposed that we would initially categorise data into three groups (McClurg 2016).
Conservative interventions for management of SUI.
Conservative interventions for management of UUI.
Conservative interventions for management of MUI.
If we identified data relating to combined or unclear populations, we proposed additional groups.
Conservative interventions for management of SUI, UUI or MUI (combined populations).
Unclear (population undefined).
In practice, we were unable to distinguish between 'mixed', 'combined' and 'unclear' populations. Therefore, we did not use the additional groups but instead categorised all mixed, combined or unclear data into a group for 'all types of UI' (AUI).
Types of participants
Our inclusion criteria stated that we would include studies in which participants had a clinical diagnosis of UI regardless of cause or comorbidities. However, these criteria led to identification of four reviews that focused on participants with specific conditions or aetiologies, and discussion among overview authors led to the decision that these reviews should be excluded (see Appendix 5). To avoid future confusion relating to the inclusion of reviews focused on specific conditions or aetiologies we removed the following statement from our inclusion criteria: "… we included reviews of trials in which the participants had other, comorbid, health‐related problems including (but not limited to) pregnancy and delivery, cancer, neurological diseases, chronic respiratory disease, learning difficulties and dementia".
Types of outcome measures
The stakeholder group debated, agreed and prioritised outcomes of interest to this overview (see Appendix 1). These were then refined and finalised for the protocol, with secondary outcomes as listed below. Appendix 8 provides further information about the process of determining this list of outcome measures. However, due to the volume and diversity of data presented within reviews relating to these secondary outcomes (often with multiple analyses relating to each listed secondary outcome), data relating to these secondary outcomes was not synthesised within this overview. Initial drafts of this overview included a synthesis of these secondary outcome data, as per the protocol, but editorial feedback highlighted that the overview was overly lengthy and complex. The large number of analyses relating to secondary analyses was a key contributor to the length and complexity, and subsequently the overview team decided to remove data relating to these outcomes from the overview. A further factor in this decision was the desire to create an overview that could be relatively easily updated, and the large volume of secondary outcome data was considered to be a major barrier to future updates.
Secondary outcomes
Participant‐reported cure, accepting the definition as used in the review.
General quality of life measures (i.e. not condition‐specific), such as the 36‐item Short Form.
Adverse effects (e.g. discomfort, soreness, pain, bleeding).
Measures of anxiety/depression, such as Hospital Anxiety and Depression Scale (HADS).
Other clinician‐measured or observed outcomes (e.g. pad tests, pad weights frequency of UI). Note: even if described within a review as measures of "cure or improvement", clinician‐based measures will be considered under this outcome category (as the primary outcome of symptomatic cure or improvement, is as reported/observed by the woman).
Other participant self‐report not presented as cure or improvement (e.g. data relating to incontinence episodes, frequency, number of voids).
Pelvic muscle floor strength/function (e.g. digital evaluation, pelvic floor muscle dynamometry or electromyography, vaginal squeeze pressure, perineal ultrasound).
Skin integrity.
Adherence to intervention (including measures of usability and acceptability).
Urodynamics (urodynamic testing), for example postvoid residual volume, rate of bladder emptying and detrusor pressure.
Socioeconomic measures (e.g. cost of intervention, economic analysis, resource implications).
Any other outcomes (note: we planned to gather information relating to outcomes that did not fall within our prestated outcomes of interest, in order to provide a comprehensive overview of the outcomes that had been synthesised within the included reviews)
An overview of the secondary outcomes reported in the included reviews is provided in Appendix 7.
Identification of studies included in more than one review
At the protocol stage, we had not anticipated that the same data from some studies may be included in more than one review. We introduced a method based on discussion between overview authors to explore potential duplicate data within reviews and took action to avoid inclusion of duplicate data (see Methods).
Data extraction for relevant comparisons
We extracted more data relating to each relevant analysis than originally stated within our protocol. We were able to do this as, rather than extracting data by manually, we were able to download electronic data relating to each comparison, facilitating comprehensive and accurate data extraction. We originally planned to extract and report comparisons relating to dose, intensity or timing of intervention but did not identify any relevant comparisons within the included reviews.
Intervention categorisation
Within the protocol, we planned to categorise conservative interventions as defined in Figure 1. However, we found that this categorisation failed to adequately distinguish between and categorise different forms of delivering the interventions. The delivery of interventions was often multimodal, where a number of different interventions were combined in a programme, or there were specific differences in the manner in which the intervention was delivered (e.g. the use of individualised assessment and treatment using PFMT, as opposed to group PFMT without any individualised assessment). Therefore, we introduced a three‐layer system that enabled us to group interventions at several different levels (see Appendix 4). The system was developed through discussion and consensus with the stakeholder group, combined with iterative exploration of the interventions included within the reviews (see Appendix 1). The full list of categories is illustrated in Table 1 and Table 2.
Certainty of evidence in included reviews: use of algorithm to assign GRADE rating
As is outlined in the methods, we developed and used an algorithm to determine the certainty of evidence (GRADE) for relevant analyses included in reviews. Our justification for this approach was that use of objective criteria, selected specifically for this body of evidence, enabled a transparent, reproducible assignment of GRADE levels of evidence.
However, the time required to extract, assess and analyse the data required to use the algorithm was substantive. After completion of a first version of this overview, but before publication, we updated our searches. Two new reviews were added at this late stage (Stewart 2017; Wieland 2019). To facilitate timely completion of the overview with limited author time/resources available, we made the pragmatic decision to use the GRADE assessments as reported by the review authors, rather than use our algorithm. The impact of this decision is something that we hope to explore at a later date.
Therefore, except for analyses from Stewart 2017 and Wieland 2019, GRADE levels of evidence have been determined using the approach stated in the protocol. In all relevant tables, we clearly marked where we deviated from this and used the author reported GRADE levels for Stewart 2017 and Wieland 2019.
Statistical analysis
Within our protocol, we stated that we would "discuss the available data and reach consensus on whether any data are suitable for meta‐analysis" in order to determine an estimate of the indirect comparison of different interventions. Exploration of the data included in the reviews and discussion among overview authors led to consensus that the issue of transitivity (where trials cover a wide diversity of conditions and types) would not allow sensible analyses to be made. Rather than carrying out any indirect comparisons, forest plots were created to provide visual illustration of the data relating to different subsets of the data. The methods adopted are fully described in the Data synthesis section.
Exploration of subgroups
Where the included reviews carried out subgroup analyses relating to our predefined subgroups (listed below), using data from one of our primary outcomes, we planned to extract and tabulate the results of these analyses. We then planned to report the pooled data for all the subgroups as defined within the included reviews and the results of the statistical test for subgroup differences.
Our predefined subgroups were:
severity of symptoms (mild, moderate, severe);
pregnancy (pregnancy or no pregnancy and antenatal or postnatal and mode of delivery);
health‐related cause of UI (cancer, neurological diseases, chronic respiratory disease, learning difficulties, dementia);
age (premenopausal, postmenopausal);
comorbidities (i.e. any other conditions);
body mass index (normal, obese, morbidly obese);
ethnicity;
duration of symptoms;
place of living (at home, care home or nursing home);
socioeconomic status.
In addition, where possible, we planned to synthesise data relating to groups of participants with nocturia, nocturnal enuresis and coital incontinence. None of the reviews included in our overview reported any statistical subgroup analyses and subsequently we were unable to report any data relating to, or to explore, subgroups.
Summarising result data tables
We had originally planned to present separate summary of results tables for each of the stated primary and secondary outcomes of interest to this overview (based on a template adapted from a presentation by A Oxman at Cochrane Meeting, Athens, May 2015). However, we found an alternative format that we thought was better given the volume and complexity of information that we had.
Network maps and forest plots
We originally planned to summarise included data by creating network maps of the direct comparisons reported by the individual trials included within the reviews using Stata Version 14 (StataCorp). The network plot mapping function in Stata allows for weighting and colouring of nodes and edges in the map that reveal important characteristics of comparison data. We planned that these summaries would illustrate the quantity and quality of evidence for different comparisons but not the effect sizes for the comparisons. We initially created a series of network maps specifically aimed at summarising the quantity of data available. The size of the nodes were determined by the number of studies including the treatment and the thickness of the edges joining two interventions were determined by the number of studies that included the comparison. If a comparison had the same treatment and control categorisation, the comparison was excluded in the analysis at that level. We created maps for each UI type, at each of the three levels described in the intervention categorisation section above. Level 3 was deemed too detailed and resulted in maps that were illegible and thus consensus was reached between overview authors that maps at Level 1 should be included in this overview. However, subsequent editorial feedback about the size and complexity of this overview, combined with a desire to simplify the overview in order to support ease of future updating, led to a decision to remove all network maps.
We originally planned to described comparisons, using a series of intervention categories (see Appendix 4), and by summarising the data graphically in forest plot format, including estimates from individual comparisons extracted from the reviews but without pooled effect size estimates. We planned to undertake this (for each UI type and for both primary outcomes) for the following three subsets of comparisons: conservative intervention versus control; conservative intervention versus another (possibly same type) conservative intervention and conservative intervention versus non‐conservative intervention. Details of planned statistical analyses were described in the protocol. These were not conducted in order to simplify and enhance accessibility of the overview, and to promote ease of updating of the overview.
Contributions of authors
ATB (previously AP): contributed to methodological decisions. Acted as third review author for disagreements during data extraction and quality assessment. Contributed to decision‐making over assessment of certainty of evidence within reviews. Performed data synthesis. Wrote methods and results. Contributed to writing discussion and conclusion. Read and commented on all drafts. Led amendments to editorial comments.
CH: data extraction and management. Assessed quality of reviews using ROBIS and certainty of evidence within reviews using agreed approach to GRADE. Performed data entry. Contributed to writing of results.
PC: contributed to methodological decisions. Ran searches and managed search results. Assessed quality of reviews using ROBIS and certainty of evidence within reviews using agreed approach to GRADE. Contributed to writing of methods and results.
AE: led discussion and decision relating to completion of statistical analysis. Provided advice relating to extraction of analysis data. Carried out statistical analysis. Read and commented on all drafts.
SH: contributed to methodological and statistical decisions and provided content expertise. Assessed reviews for inclusion. Acted as third overview author for disagreements during data extraction and quality assessment. Contributed to decision‐making over assessment of certainty of evidence within reviews. Read and commented on all drafts.
DMcC: contributed to methodological decisions and provided content expertise. Assessed reviews for inclusion. Acted as third overview author for disagreements during data extraction and quality assessment. Contributed to decision‐making over assessment of certainty of evidence within reviews. Wrote discussion and conclusion. Read and commented on all drafts.
Sources of support
Internal sources
No sources of support provided
External sources
-
Physiotherapy Research Foundation, UK
This overview was supported by a project grant by the Physiotherapy Research Foundation. This covered the salary costs of Christine Hazelton.
-
Chief Scientist Office, UK
The Nursing, Midwifery and Allied Health Professions (NMAHP) Research Unit is supported by the Chief Scientist Office of the Scottish Government.
-
National Institute for Health Research, UK
This project was supported by the National Institute for Health Research, via infrastructure funding to Cochrane Incontinence. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Evidence Synthesis Programme, the NIHR, NHS or the Department of Health and Social Care.
Declarations of interest
ATB: none.
CH: none.
PC: none.
AE: none.
SH: none.
DMcC: none.
Edited (no change to conclusions)
References
References to included reviews
Alhasso 2005
- Alhasso A, Glazener CM, Pickard R, N'Dow JM. Adrenergic drugs for urinary incontinence in adults. Cochrane Database of Systematic Reviews 2005, Issue 3. Art. No: CD001842. [DOI: 10.1002/14651858.CD001842.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ayeleke 2015
- Ayeleke RO, Hay-Smith EJ, Omar MI. Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women. Cochrane Database of Systematic Reviews 2015, Issue 11. Art. No: CD010551. [DOI: 10.1002/14651858.CD010551.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cody 2012
- Cody JD, Jacobs ML, Richardson K, Moehrer B, Hextall A. Oestrogen therapy for urinary incontinence in post-menopausal women. Cochrane Database of Systematic Reviews 2012, Issue 10. Art. No: CD001405. [DOI: 10.1002/14651858.CD001405.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dumoulin 2018
- Dumoulin C, Cacciari LP, Hay-Smith EJ. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews 2018, Issue 10. Art. No: CD005654. [DOI: 10.1002/14651858.CD005654.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Duthie 2011
- Duthie JB, Vincent M, Herbison GP, Wilson DI, Wilson D. Botulinum toxin injections for adults with overactive bladder syndrome. Cochrane Database of Systematic Reviews 2011, Issue 12. Art. No: CD005493. [DOI: 10.1002/14651858.CD005493.pub3] [DOI] [PubMed] [Google Scholar]
Eustice 2000
- Eustice S, Roe B, Paterson J. Prompted voiding for the management of urinary incontinence in adults. Cochrane Database of Systematic Reviews 2000, Issue 2. Art. No: CD002113. [DOI: 10.1002/14651858.CD002113] [DOI] [PMC free article] [PubMed] [Google Scholar]
Freites 2019
- Freites J, Stewart F, Omar MI, Mashayekhi A, Agur WI. Laparoscopic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2019, Issue 12. Art. No: CD002239. [DOI: 10.1002/14651858.CD002239.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Glazener 2017a
- Glazener CM, Cooper K, Mashayekhi A. Anterior vaginal repair for urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No: CD001755. [DOI: 10.1002/14651858.CD001755] [DOI] [PMC free article] [PubMed] [Google Scholar]
Glazener 2017b
- Glazener CM, Cooper K, Mashayekhi A. Bladder neck needle suspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No: CD003636. [DOI: 10.1002/14651858.CD003636.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hay‐Smith 2011
- Hay-Smith EJ, Herderschee R, Dumoulin C, Herbison GP. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women. Cochrane Database of Systematic Reviews 2011, Issue 12. Art. No: CD009508. [DOI: 10.1002/14651858.CD009508] [DOI] [PubMed] [Google Scholar]
Herbison 2009
- Herbison GP, Arnold EP. Sacral neuromodulation with implanted devices for urinary storage and voiding dysfunction in adults. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No: CD004202. [DOI: 10.1002/14651858.CD004202.pub2] [DOI] [PubMed] [Google Scholar]
Herbison 2013
- Herbison GP, Dean N. Weighted vaginal cones for urinary incontinence. Cochrane Database of Systematic Reviews 2013, Issue 7. Art. No: CD002114. [DOI: 10.1002/14651858.CD002114.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Herderschee 2011
- Herderschee R, Hay-Smith EJ, Herbison GP, Roovers JP, Heineman MJ. Feedback or biofeedback to augment pelvic floor muscle training for urinary incontinence in women. Cochrane Database of Systematic Reviews 2011, Issue 7. Art. No: CD009252. [DOI: 10.1002/14651858.CD009252] [DOI] [PubMed] [Google Scholar]
Imamura 2015
- Imamura M, Williams K, Wells M, McGrother C. Lifestyle interventions for the treatment of urinary incontinence in adults. Cochrane Database of Systematic Reviews 2015, Issue 12. Art. No: CD003505. [DOI: 10.1002/14651858.CD003505.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kang 2015
- Kang D, Han J, Neuberger MM, Moy ML, Wallace SA, Alonso-Coello P, et al. Transurethral radiofrequency collagen denaturation for the treatment of women with urinary incontinence. Cochrane Database of Systematic Reviews 2015, Issue 3. Art. No: CD010217. [DOI: 10.1002/14651858.CD010217.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kirchin 2017
- Kirchin V, Page T, Keegan PE, Atiemo KO, Cody JD, McClinton S, et al. Urethral injection therapy for urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No: CD003881. [DOI: 10.1002/14651858.CD003881.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lapitan 2017
- Lapitan MC, Cody JD, Mashayekhi A. Open retropubic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No: CD002912. [DOI: 10.1002/14651858.CD002912.pub7] [DOI] [Google Scholar]
Lipp 2014
- Lipp A, Shaw C, Glavind K. Mechanical devices for urinary incontinence in women. Cochrane Database of Systematic Reviews 2014, Issue 12. Art. No: CD001756. [DOI: 10.1002/14651858.CD001756.pub6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mariappan 2005
- Mariappan P, Alhasso AA, Grant A, N'Dow JM. Serotonin and noradrenaline reuptake inhibitors (SNRI) for stress urinary incontinence in adults. Cochrane Database of Systematic Reviews 2005, Issue 3. Art. No: CD004742. [DOI: 10.1002/14651858.CD004742.pub2] [DOI] [PubMed] [Google Scholar]
Nambiar 2017
- Nambiar A, Cody JD, Jeffery ST, Aluko P. Single-incision sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No: CD008709. [DOI: 10.1002/14651858.CD008709.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ostaszkiewicz 2004a
- Ostaszkiewicz J, Chestney T, Roe B. Habit retraining for the management of urinary incontinence in adults. Cochrane Database of Systematic Reviews 2004, Issue 2. Art. No: CD002801. [DOI: 10.1002/14651858.CD002801.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ostaszkiewicz 2004b
- Ostaszkiewicz J, Johnston L, Roe B. Timed voiding for the management of urinary incontinence in adults. Cochrane Database of Systematic Reviews 2004, Issue 1. Art. No: CD002802. [DOI: 10.1002/14651858.CD002802.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rai 2012
- Rai BP, Cody JD, Alhasso A, Stewart L. Anticholinergic drugs versus non-drug active therapies for non-neurogenic overactive bladder syndrome in adults. Cochrane Database of Systematic Reviews 2012, Issue 12. Art. No: CD003193. [DOI: 10.1002/14651858.CD003193.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Saraswat 2020
- Saraswat L, Rehman H, Omar MI, Cody JD, Aluko P, Glazener CM. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2020, Issue 1. Art. No: CD001754. [DOI: 10.1002/14651858.CD001754.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stewart 2016
- Stewart F, Gameiro LF, El Dib R, Gameiro MO, Kapoor A, Amaro JL. Electrical stimulation with non-implanted electrodes for overactive bladder in adults. Cochrane Database of Systematic Reviews 2016, Issue 12. Art. No: CD010098. [DOI: 10.1002/14651858.CD010098.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stewart 2017
- Stewart F, Berghmans B, Bø K, Glazener CM. Electrical stimulation with non-implanted devices for stress urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 12. Art. No: CD012390. [DOI: 10.1002/14651858.CD012390.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wallace 2004
- Wallace SA, Roe B, Williams K, Palmer M. Bladder training for urinary incontinence in adults. Cochrane Database of Systematic Reviews 2004, Issue 1. Art. No: CD001308. [DOI: 10.1002/14651858.CD001308.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2013
- Wang Y, Zhishun L, Peng W, Zhao J, Liu B. Acupuncture for stress urinary incontinence in adults. Cochrane Database of Systematic Reviews 2013, Issue 7. Art. No: CD009408. [DOI: 10.1002/14651858.CD009408.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wieland 2019
- Wieland LS, Shrestha N, Lassi ZS, Panda S, Chiaramonte D, Skoetz N. Yoga for treating urinary incontinence in women. Cochrane Database of Systematic Reviews 2019, Issue 2. Art. No: CD012668. [DOI: 10.1002/14651858.CD012668.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to excluded reviews
Baessler 2018
- Baessler K, Christmann-Schmid C, Maher C, Haya N, Crawford TJ, Brown J. Surgery for women with pelvic organ prolapse with or without stress urinary incontinence. Cochrane Database of Systematic Reviews 2018, Issue 8. Art. No: CD013108. [DOI: 10.1002/14651858.CD013108] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bakali 2019
- Bakali E, Johnson E, Buckley BS, Hilton P, Walker B, Tincello DG. Interventions for treating recurrent stress urinary incontinence after failed minimally invasive synthetic midurethral tape surgery in women. Cochrane Database of Systematic Reviews 2019, Issue 9. Art. No: CD009407. [DOI: 10.1002/14651858.CD009407.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beeckman 2016
- Beeckman D, Damme N, Schoonhoven L, Lancker A, Kottner J, Beele H, et al. Interventions for preventing and treating incontinence-associated dermatitis in adults. Cochrane Database of Systematic Reviews 2016, Issue 11. Art. No: CD011627. [DOI: 10.1002/14651858.CD011627.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Farrar 2014
- Farrar D, Tuffnell DJ, Ramage C. Interventions for women in subsequent pregnancies following obstetric anal sphincter injury to reduce the risk of recurrent injury and associated harms. Cochrane Database of Systematic Reviews 2014, Issue 11. Art. No: CD010374. [DOI: 10.1002/14651858.CD010374.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ford 2017
- Ford AA, Rogerson L, Cody JD, Aluko P, Ogah JA. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No: CD006375. [DOI: 10.1002/14651858.CD006375.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hagen 2011
- Hagen S, Stark D. Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database of Systematic Reviews 2011, Issue 12. Art. No: CD003882. [DOI: 10.1002/14651858.CD003882.pub4] [DOI] [PubMed] [Google Scholar]
Hay‐Smith 2007
- Hay-Smith J, Mørkved S, Herbison GP. Physical therapies for prevention of urinary and faecal incontinence in adults. Cochrane Database of Systematic Reviews 2007, Issue 4. Art. No: CD003191. [DOI: 10.1002/14651858.CD003191.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hay‐Smith 2008
- Hay-Smith J, Bø K, Berghmans B, Hendriks E, Bie R, Waalwijk van Doorn E. Pelvic floor muscle training for urinary incontinence in women. Cochrane Database of Systematic Reviews 2008, Issue 3. Art. No: CD001407. [DOI: 10.1002/14651858.CD001407.pub3] [DOI] [PubMed] [Google Scholar]
Ismail 2010
- Ismail SI, Bain C, Hagen S. Oestrogens for treatment or prevention of pelvic organ prolapse in postmenopausal women. Cochrane Database of Systematic Reviews 2010, Issue 9. Art. No: CD007063. [DOI: 10.1002/14651858.CD007063.pub2] [DOI] [PubMed] [Google Scholar]
Jamison 2013
- Jamison J, Maguire S, McCann J. Catheter policies for management of long term voiding problems in adults with neurogenic bladder disorders. Cochrane Database of Systematic Reviews 2013, Issue 11. Art. No: CD004375. [DOI: 10.1002/14651858.CD004375.pub4] [DOI] [PubMed] [Google Scholar]
McNaughton Collins 2002
- McNaughton Collins M, Wilt TJ. Allopurinol for chronic prostatitis. Cochrane Database of Systematic Reviews 2002, Issue 4. Art. No: CD001041. [DOI: 10.1002/14651858.CD001041] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2019
- Thomas LH, Coupe J, Cross LD, Tan AL, Watkins CL. Interventions for treating urinary incontinence after stroke in adults. Cochrane Database of Systematic Reviews 2019, Issue 2. Art. No: CD004462. [DOI: 10.1002/14651858.CD004462.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Utomo 2014
- Utomo E, Groen J, Blok BF. Surgical management of functional bladder outlet obstruction in adults with neurogenic bladder dysfunction. Cochrane Database of Systematic Reviews 2014, Issue 5. Art. No: CD004927. [DOI: 10.1002/14651858.CD004927.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Walsh 2015
- Walsh KA, Grivell RM. Use of endoanal ultrasound for reducing the risk of complications related to anal sphincter injury after vaginal birth. Cochrane Database of Systematic Reviews 2015, Issue 10. Art. No: CD010826. [DOI: 10.1002/14651858.CD010826.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Woodley 2020
- Woodley SJ, Lawrenson P, Boyle R, Cody JD, Mørkved S, Kernohan A, et al. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database of Systematic Reviews 2020, Issue 5. Art. No: CD007471. [DOI: 10.1002/14651858.CD007471.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Woodward 2014
- Woodward S, Norton C, Chiarelli P. Biofeedback for treatment of chronic idiopathic constipation in adults. Cochrane Database of Systematic Reviews 2014, Issue 3. Art. No: CD008486. [DOI: 10.1002/14651858.CD008486.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Aaronson 1995
- Aaronson PS, Loehner D, Bingham W, Smith JJ. Intravaginal electrical stimulation in the treatment of genuine stress urinary incontinence and detrusor instability: a controlled study (abstract 1051). Journal of Urology 1995;153(4 Suppl):491A. [Google Scholar]
Alewijnse 2003a
- Alewijnse D, Metsemakers JF, Mesters IE, den Borne B. Effectiveness of pelvic floor muscle exercise therapy supplemented with a health education program to promote long-term adherence among women with urinary incontinence. Neurourology and Urodynamics 2003;22(4):284-95. [DOI] [PubMed] [Google Scholar]
Alewijnse 2003b
- Alewijnse D, Mesters I, Metsemakers J, den Borne B. Predictors of long-term adherence to pelvic floor muscle exercise therapy among women with urinary incontinence. Health Education Research 2003;18(5):511-24. [DOI] [PubMed] [Google Scholar]
Alves 2015
- Alves FK, Riccetto C, Adami DB, Marques J, Pereira LC, Pama P, et al. A pelvic floor muscle training program in postmenopausal women: a randomised controlled trial. Maturitas 2015;81(2):300-5. [DOI] [PubMed] [Google Scholar]
Amaro 2003
- Amaro JL, Gameiro MO, Padovani CR. Treatment of urinary stress incontinence by intravaginal electrical stimulation and pelvic floor physiotherapy. International Urogynecology Journal and Pelvic Floor Dysfunction 2003;14(3):204-8. [DOI] [PubMed] [Google Scholar]
Amaro 2006
- Amaro JL, Gameiro MO, Kawano PR, Padovani CR. Intravaginal electrical stimulation: a randomized, double blind on the treatment of mixed urinary incontinence. Acta Obstetricia et Gynecologica Scandinavia 2006;85(5):619-22. [DOI] [PubMed] [Google Scholar]
Arruda 2008
- Arruda RM, Castro RA, Sousa GC, Sartori MG, Baracat EC, Girão MJ. Prospective randomized comparison of oxybutynin, functional electrostimulation, and pelvic floor training for treatment of detrusor overactivity in women. International Urogynecology Journal and Pelvic Floor Dysfunction 2008;19(8):1055-61. [DOI] [PubMed] [Google Scholar]
Arvonen 2001
- Arvonen T, Fianu-Jonasson A, Tyni-Lenné R. Effectiveness of two conservative modes of physical therapy in women with urinary stress incontinence. Neurourology and Urodynamics 2001;20:591-9. [DOI] [PubMed] [Google Scholar]
Arvonen 2002
- Arvonen T, Jonasson AF, Tyni-Lenné R. A clinical trial comparing conventional pelvic floor training and training with vaginal balls in women with stress urinary incontinence – a pilot study. Nordisk Fysioterapi 2002;6(1):41-6. [Google Scholar]
Asklund 2017
- Asklund I, Nyström E, Sjöström M, Umefjord G, Stenlund H, Samuelsson E. Mobile app for treatment of stress urinary incontinence: a randomized controlled trial. Neurourology and Urodynamics 2017;36(5):1369-76. [DOI: 10.1002/nau.23116] [DOI] [PubMed] [Google Scholar]
Baker 2014
- Baker J, Costa D, Guarino JM, Nygaard I. Comparison of mindfulness-based stress reduction versus yoga on urinary urge incontinence: a randomized pilot study with 6-month and 1-year follow-up visits. Female Pelvic Medicine and Reconstructive Surgery 2014;20(3):141-6. [DOI] [PubMed] [Google Scholar]
Barroso 2004
- Barroso JC, Ramos JG, Martins-Costa S, Sanches PR, Muller AF. Transvaginal electrical stimulation in the treatment of urinary incontinence. BJU International 2004;93(3):319-23. [DOI] [PubMed] [Google Scholar]
Bastian 2010
- Bastian H, Glasziou P, Chalmers I. Seventy-five trials and eleven systematic reviews a day: how will we ever keep up? PLOS Medicine 2010;7(9):e1000326. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berge 2017
- Berge E, Salman RA, Worp HB, Stapf C, Sandercock P, Sprigg N, et al. Increasing value and reducing waste in stroke research. Lancet. Neurology 2017;16(5):399-408. [DOI] [PubMed] [Google Scholar]
Berglund 1993
- Berglund AL, Eisemann M, Lalos A, Lalos O. Predictive factors of the outcome of primary surgical treatment of stress incontinence in women. Scandinavian Journal of Urology and Nephrology 1997;31(1):49-55. [DOI] [PubMed] [Google Scholar]
Berkman 2013
- Berkman ND, Lohr KN, Morgan LC, Kuo T-M, Morton SC. Interrater reliability of grading strength of evidence varies with the complexity of the evidence in systematic reviews. Journal of Clinical Epidemiology 2013;66(10):1105-17. [DOI] [PubMed] [Google Scholar]
Bero 2012
- Bero LA, Binder L. The Cochrane Collaboration review prioritization projects show that a variety of approaches successfully identify high-priority topics. Journal of Clinical Epidemiology 2012;66(5):472-3. [DOI: 10.1016/j.jclinepi.2012.03.015] [DOI] [PubMed] [Google Scholar]
Bertotto 2017
- Bertotto A, Schvartzman R, Wender MC. Effect of electromyographic biofeedback as an add-on to pelvic floor muscle exercises on neuromuscular outcomes and quality of life in postmenopausal women with stress urinary incontinence: a randomized controlled trial. Neurourology and Urodynamics 2017;36(8):2142-7. [DOI] [PubMed] [Google Scholar]
Beuttenmuller 2010
- Beuttenmuller L, Cader SA, Macena RH, Araujo ND, Nunes EF, Dantas EH. Muscle contraction of the pelvic floor and quality of life of women with stress urinary incontinence who underwent kinesitherapy. Fizjoterapia 2010;18(1):35-41. [SR-INCONT43326] [Google Scholar]
Bezerra 2009
- Bezerra CA, Wroclawski ER, Rodrigues AO, Tristao R, Borrelli M. Randomized clinical trial do not show that PFMT plus vaginal electrical stimulation is better than electrical stimulation alone for SUI in women (Abstract number 1561). Journal of Urology 2009;181(4 Suppl):561. [sr-incont62404] [Google Scholar]
Bi 2007
- Bi W. Clinical study on electroacupuncture treatment of female stress incontinence [电针治疗女性压力性尿失禁]. Chinese Archives of Traditional Chinese Medicine 2007;25(6):1284-5. [Google Scholar]
Blaivas 1997
- Blaivas JG, Appell RA, Fantl JA, Leach G, McGuire EJ, Resnick NM, et al. Definition and classification of urinary incontinence: recommendations of the Urodynamic Society. Neurourology and Urodynamics 1997;16(3):149-51. [DOI] [PubMed] [Google Scholar]
Bogner 2002
- Bogner HR, Gallo JJ, Sammel MD, Ford DE, Armenian HK, Eaton WW. Urinary incontinence and psychological distress in community-dwelling older adults. Journal of the American Geriatrics Society 2002;50(3):489-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boos 1998
- Boos K, Anders K, Hextall A, Toozs-Hobson P, Cardozo L. Randomised trial of reliance versus femassist devices in the management of genuine stress incontinence. Neurourology and Urodynamics 1998;17(4):455. [Google Scholar]
Bourcier 1994
- Bourcier A, Juras J. Randomised study comparing physiotherapy and pelvic floor rehabilitation. In: International Continence Society (ICS), 24th Annual Meeting; 1994 Aug 30–Sep 2; Prague (Czech Republic). 1994:146.
Bridges 1988
- Bridges N, Denning J, Olah KS, Farrar DJ. A prospective trial comparing interferential therapy and treatment using cones in patients with symptoms of stress incontinence. Neurourology and Urodynamics 1988;7(3):267-8. [Google Scholar]
Bump 1992
- Bump RC, McClish DK. Cigarette smoking and urinary incontinence in women. American Journal of Obstetrics and Gynecology 1992;167(5):1213-8. [DOI] [PubMed] [Google Scholar]
Burgio 2002
- Burgio KL, Goode PS, Locher JL, Richter HE, Roth DL, Wright KC, et al. Predictors of outcome in the behavioral treatment of urinary incontinence in women. Obstetrics and Gynecology 2003;102(5 Pt 1):940-7. [DOI] [PubMed] [Google Scholar]
Burgio 2008
- Burgio KL, Kraus SR, Menefee S, Borello-France D, Corton M, Johnson HW, et al. Behavioral therapy to enable women with urge incontinence to discontinue drug treatment: a randomized trial. Annals of Internal Medicine 2008;149(3):161-9. [srincont27584] [DOI] [PMC free article] [PubMed] [Google Scholar]
Burgio 2010
- Burgio KL, Goode PS, Richter HE, Markland AD, Johnson TM, Redden DT. Combined behavioral and individualized drug therapy versus individualized drug therapy alone for urge urinary incontinence in women. Journal of Urology 2010;184(2):598-603. [sr-incont39902] [DOI] [PubMed] [Google Scholar]
Burns 1993
- Burns PA, Pranikoff K, Nochajski TH, Hadley EC, Levy KJ, Ory MG. A comparison of effectiveness of biofeedback and pelvic muscle exercise treatment of stress incontinence in older community-dwelling women. Journal of Gerontology 1993;48(4):M167-74. [DOI] [PubMed] [Google Scholar]
Bø 1990
- Bø K, Hagen RH, Kvarstein B, Jørgensen J, Larsen S. Pelvic floor muscle exercise for the treatment of female stress urinary incontinence: III. Effects of two different degrees of pelvic floor muscle exercises. Neurourology and Urodynamics 1990;9(5):489-502. [sr-incont2625] [Google Scholar]
Bø 1999
- Bø K, Talseth T, Home I. Single blind, randomised controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones, and no treatment in management of genuine stress incontinence in women. BMJ 1999;318(7182):487-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bø 2013
- Bø K, Herbert RD. There is not yet strong evidence that exercise regimens other than pelvic floor muscle training can reduce stress urinary incontinence in women: a systematic review. Journal of Physiotherapy 2013;59(3):159-68. [DOI] [PubMed] [Google Scholar]
Bø 2017
- Bø K, Frawley HC, Haylen BT, Abramov Y, Almeida FG, Berghmans B, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Neurourology and Urodynamics 2017;36(2):221-44. [DOI] [PubMed] [Google Scholar]
Cadwell 1963
- Cadwell KP. The electrical control of the sphincter incompetence. Lancet 1963;2(7300):174-5. [DOI] [PubMed] [Google Scholar]
Cammu 1998
- Cammu H, Nylen M. Pelvic floor exercises versus vaginal weight cones in genuine stress incontinence. European Journal of Obstetrics, Gynecology, and Reproductive Biology 1998;77(1):89-93. [DOI] [PubMed] [Google Scholar]
Carneiro 2010
- Carneiro EF, Araujo NS, Beuttenmüll L, Vieira PC, Cader SA, Rett M, et al. The anatomical-functional characteristics of the pelvic floor and quality of life of women with stress urinary incontinence subjected to perineal exercises [Las características anatomofuncionales del suelo pélvico y la calidad de vida de mujeres con incontinencia urinaria de esfuerzo sometidas a ejercicios perineales]. Actas Urologicas Espanolas 2010;34(9):788-93. [SR-INCONT40377] [PubMed] [Google Scholar]
Carriere 2006
- Carriere B. Interdependence of posture and the pelvic floor. In: Carriere B, Feldt CM, editors(s). The Pelvic Floor. New York (NY): Thieme, 2006:68-81. [Print ISBN 9781588903259] [Google Scholar]
Castro 2008
- Castro RA, Arruda RM, Zanetti MR, Santos PD, Sartori MG, Girao MJ. Single-blind, randomized, controlled trial of pelvic floor muscle training, electrical stimulation, vaginal cones, and no active treatment in the management of stress urinary incontinence. Clinics (Sao Paulo, Brazil) 2008;63(4):465-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Celiker Tosun 2015
- Celiker Tosun O, Mutlu EK, Ergenoglu AM, Yeniel AO, Tosun G, Malkoc M, et al. Does pelvic floor muscle training abolish symptoms of urinary incontinence? A randomized controlled trial. Clinical Rehabilitation 2015;29(6):525-37. [DOI: 10.1177/0269215514546768] [DOI] [PubMed] [Google Scholar]
Chalmers 2009
- Chalmers I, Glasziou P. Avoidable waste in the production and reporting of research evidence. Lancet 2009;374(9683):86-9. [DOI] [PubMed] [Google Scholar]
Chalmers 2014
- Chalmers I, Bracken MB, Djulbegovic B, Garattini S, Grant J, Gülmezoglu AM, et al. How to increase value and reduce waste when research priorities are set. Lancet 2014;383(9912):156-65. [DOI] [PubMed] [Google Scholar]
Chang 1986
- Chang ST. The Complete System of Self-healing: Internal Exercises. Mumbai (India): Tao Publishing, 1986. [ISBN 0942196066] [Google Scholar]
Chiarelli 1999
- Chiarelli P, Cockburn J. The development of a physiotherapy continence promotion program using a customer focus. Australian Journal of Physiotherapy 1999;45(2):111-9. [DOI] [PubMed] [Google Scholar]
Chua 2015
- Chua ME, Lapitan MC, Silangcruz JM, Luna S Jr, Morales ML Jr. Beta-3 adrenergic receptor agonist for adult with overactive bladder. Cochrane Database of Systematic Reviews 2015, Issue 3. Art. No: CD011593. [DOI: 10.1002/14651858.CD011593] [DOI] [Google Scholar]
Clement 2013
- Clement KD, Lapitan MC, Omar MI, Glazener CM. Urodynamic studies for management of urinary incontinence in children and adults. Cochrane Database of Systematic Reviews 2013, Issue 10. Art. No: CD003195. [DOI: 10.1002/14651858.CD003195.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cochrane Priority Setting Guidance
- Cochrane Knowledge Translation Priority Setting Working Group. Guidance for Cochrane Review priority setting; 2019. training.cochrane.org/online-learning/knowledge-translation/priority-setting/guidance-cochrane-review-priority-setting (accessed 22 July 2021).
Colombo 1995
- Colombo M, Zanetta G, Scalambrino S, Milani R. Oxybutynin and bladder training in the management of female urinary urge incontinence: a randomized study. International Urogynecology Journal and Pelvic Floor Dysfunction 1995;6:63-7. [Google Scholar]
Cornu 2012
- Cornu JN, Mouly S, Amerenco G, Jacquetin B, Ciofu C, Haab F, et al. 75NC007 device for noninvasive stress urinary incontinence management in women: a randomized controlled trial. International Urogynecology Journal 2012;23(12):1727-34. [DOI] [PubMed] [Google Scholar]
Correia 2013
- Correia GN, Pereira VS, Bastos AM, Hirakawa HS, Driusso P. Surface and intravaginal electrical stimulation versus no treatment in severity of stress urinary incontinence: randomized controlled study (Abstract number 23). International Urogynecology Journal and Pelvic Floor Dysfunction 2013;24(Suppl 1):S23-4. [Google Scholar]
Correia 2014
- Correia GN, Pereira VS, Hirakawa HS, Driusso P. Effects of surface and intravaginal electrical stimulation in the treatment of women with stress urinary incontinence: randomized controlled trial. European Journal of Obstetrics, Gynecology, and Reproductive Biology 2014;173(1):113-8. [DOI] [PubMed] [Google Scholar]
Cotterill 2018
- Cotterill N, Sullivan A, Norton C, Wilkins A, Weir I, Kilonzo M, et al. Conservative interventions for urinary or faecal incontinence, or both, in adults with multiple sclerosis. Cochrane Database of Systematic Reviews 2018, Issue 10. Art. No: CD013150. [DOI: 10.1002/14651858.CD013150] [DOI] [Google Scholar]
D'Ancona 2019
- D'Ancona C, Haylen B, Oelke M, Abranches-Monteiro L, Arnold E, Goldman H, et al, on behalf of the Standardisation Steering Committee ICS and the ICS Working Group on Terminology for Male Lower Urinary Tract & Pelvic Floor Symptoms and Dysfunction. The International Continence Society (ICS) report on the terminology for adult male lower urinary tract and pelvic floor symptoms and dysfunction. Neurourology and Urodynamics 2019;38(2):433-77. [DOI] [PubMed] [Google Scholar]
Dean 2017
- Dean N, Ellis G, Herbison GP, Wilson D, Mashayekhi A. Laparoscopic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No: CD002239. [DOI: 10.1002/14651858.CD002239.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
de Groat 1997
- Groat WC. A neurologic basis for the overactive bladder. Urology 1997;50(6A Suppl):36-52. [DOI] [PubMed] [Google Scholar]
de Groat 2001
- Groat WC, Fraser MO, Yoshiyama M, Smerin S, Tai C, Chancellor MB, et al. Neural control of the urethra. Scandinavian Journal of Urology and Nephrology 2001;35(207):35-43. [DOI] [PubMed] [Google Scholar]
Delgado 2009
- Delgado D, Drake M. A randomised study to compare the PelvicToner device against standard pelvic floor exercises in the treatment of stress urinary incontinence in women. In: International Continence Society (ICS), 39th Annual Meeting; 2009 Sep 29–Oct 3; San Francisco (CA). 2009.
de Oliveira 2009
- Oliveira Camargo F, Rodrigues AM, Arruda RM, Ferreira Sartori MG, Girao MJ, Castro RA. Pelvic floor muscle training in female stress urinary incontinence: comparison between group training and individual treatment using PERFECT assessment scheme. International Urogynecology Journal and Pelvic Floor Dysfunction 2009;20(12):1455-62. [DOI] [PubMed] [Google Scholar]
Diniz Zanetti 2007
- Diniz Zanetti MR, Aquino Castro R, Lyvio Rotta A, Diniz dos Santos P, Sartori M, Castello Girão MJ. Impact of supervised physiotherapeutic pelvic floor exercises for treating female stress incontinence. Sao Paulo Medical Journal 2007;125(5):265-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Diokno 2010
- Diokno AC, Ocampo MS Jr, Ibrahim IA, Karl CR, Lajiness MJ, Hall SA. Group session teaching of behavioral modification program (BMP) for urinary incontinence: a randomized controlled trial among incontinent women. International Urology and Nephrology 2010;42(2):375-81. [DOI] [PubMed] [Google Scholar]
EPPI‐Centre Cost Converter
- Shemilt I, Thomas J, Morciano M. A web-based tool for adjusting costs to a specific target currency and price year. Evidence & Policy 2010;6(1):51-9. [Google Scholar]
EQUATOR 2021
- EQUATOR Network. Enhancing the QUAlity and Transparency Of health Research (EQUATOR). www.equator-network.org (accessed 9 September 2021).
Eyjólfsdóttir 2009
- Eyjólfsdóttir H, Ragnarsdóttir M, Geirsson G. Pelvic floor muscle training with and without functional electrical stimulation as treatment for stress urinary incontinence [Samanburdur á grindarbotnsthjálfun med og án raförvunar sem medferd vid áreynsluthvagleka]. Laeknabladid 2009;95(9):575-80. [PubMed] [Google Scholar]
Fantl 1991
- Fantl A, Wyman JF, McClish DK, Harkins SW, Elswick RK, Taylor JR, et al. Efficacy of bladder training in older women with urinary incontinence. JAMA 1991;265(5):609-13. [PMID: ] [PubMed] [Google Scholar]
Felicíssimo 2010
- Felicíssimo MF, Carneiro MM, Saleme CS, Pinto RZ, da Fonseca AM, da Silva-Filho AL. Intensive supervised versus unsupervised pelvic floor muscle training for the treatment of stress urinary incontinence: a randomized comparative trial. International Urogynecology Journal 2010;21(7):835-40. [DOI] [PubMed] [Google Scholar]
Finazzi‐Agrò 2010
- Finazzi-Agrò E, Petta F, Sciobica F, Pasqualetti P, Musco S, Bove P. Percutaneous tibial nerve stimulation effects on detrusor overactivity incontinence are not due to a placebo effect: a randomized double-blind, placebo controlled trial. Journal of Urology 2010;184(5):2001-6. [DOI] [PubMed] [Google Scholar]
Firra 2013
- Firra J, Thompson M, Smith SS. Paradoxical findings in the treatment of predominant stress and urge incontinence: a pilot study with exercise and electrical stimulation. Journal of Women's Health Physical Therapy 2013;37(3):113-23. [Google Scholar]
Ford 2015
- Ford AA, Rogerson L, Cody JD, Ogah J. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database of Systematic Reviews 2015, Issue 7. Art. No: CD006375. [DOI: 10.1002/14651858.CD006375.pub3] [DOI] [PubMed] [Google Scholar]
Francis 2012
- Francis AM, Madill SJ, Gentilcore-Saulnier E, McLean L. Survey of Canadian physiotherapists: entry-level and post-professional education in women's health. Physiotherapy Canada 2012;64(3):271-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Franzén 2010
- Franzén K, Johansson J-E, Lauridsen I, Canelid J, Heiwall B, Nilsson K. Electrical stimulation compared with tolterodine for treatment of urge/urge incontinence amongst women: a randomized controlled trial. International Urogynecology Journal 2010;21(12):1517-24. [DOI] [PubMed] [Google Scholar]
French 2010
- French B, Thomas LH, Leathley MJ, Sutton CJ, Booth J, Brittain K, et al. Combined conservative interventions for urge, stress or mixed incontinence in adults. Cochrane Database of Systematic Reviews 2010, Issue 12. Art. No: CD008910. [DOI: 10.1002/14651858.CD008910] [DOI] [Google Scholar]
Funada 2020
- Funada S, Yoshioka T, Luo Y, Sato A, Akamatsu S, Watanabe N. Bladder training for treating overactive bladder in adults. Cochrane Database of Systematic Reviews 2020, Issue 4. Art. No: CD013571. [DOI: 10.1002/14651858.CD013571] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gionfriddo 2016
- Gionfriddo MR. Subjectivity is a strength: a comment on "an algorithm was developed to assign GRADE levels of evidence to comparisons within systematic reviews" [letter]. Journal of Clinical Epidemiology 2016;74:237. [DOI] [PubMed] [Google Scholar]
Godec 1975
- Godec C, Cass AS, Ayala GF. Bladder inhibition with functional electrical stimulation. Urology 1975;6(6):663-6. [DOI] [PubMed] [Google Scholar]
Goode 2002
- Goode PS, Burgio KL, Locher JL, Umlauf MG, LLoyd KL, Roth DL. Urodynamic changes associated with behavioural and drug treatment of urge incontinence in older women. Journal of the American Geriatrics Society 2002;50(5):808-16. [DOI] [PubMed] [Google Scholar]
Goode 2003
- Goode PS, Burgio KL, Locher JL, Roth DL, Umlauf MG, Richter HE, et al. Effect of behavioral training with or without pelvic floor electrical stimulation on stress incontinence in women: a randomized controlled trial. JAMA 2003;290(3):345-52. [DOI] [PubMed] [Google Scholar]
Groutz 2000
- Groutz A, Blaivas JG, Chaikin DC, Resnick NM, Engleman K, Anzalone D, et al. Noninvasive outcome measures of urinary incontinence and lower urinary tract symptoms: a multicenter study of micturition diary and pad tests. Journal of Urology 2000;164(3):698-701. [DOI] [PubMed] [Google Scholar]
Guyatt 2011a
- Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knotterus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. Journal of Clinical Epidemiology 2011;64(4):380-2. [DOI] [PubMed] [Google Scholar]
Guyatt 2011b
- Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, et al. GRADE guidelines: 4. Rating the quality of evidence – study limitations (risk of bias). Journal of Clinical Epidemiology 2011;64(4):407-15. [DOI] [PubMed] [Google Scholar]
Guyatt 2011c
- Guyatt G, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines: 6. Rating the quality of evidence – imprecision. Journal of Clinical Epidemiology 2011;12:1283-93. [DOI] [PubMed] [Google Scholar]
Guyatt 2011d
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al, the GRADE Working Group. GRADE guidelines: 7. Rating the quality of evidence – inconsistency. Journal of Clinical Epidemiology 2011;64(12):1294-302. [DOI] [PubMed] [Google Scholar]
Guyatt 2011e
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al, the GRADE Working Group. GRADE guidelines: 8. Rating the quality of evidence – indirectness. Journal of Clinical Epidemiology 2011;64(12):1303-10. [DOI] [PubMed] [Google Scholar]
Guyatt 2011f
- Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J, et al. GRADE guidelines: 5. Rating the quality of evidence – publication bias. Journal of Clinical Epidemiology 2011;64(12):1277-82. [DOI] [PubMed] [Google Scholar]
Hadley 1986
- Hadley EC. Bladder training and related therapies for urinary incontinence in older people. JAMA 1986;256(3):372-9. [PMID: ] [PubMed] [Google Scholar]
Hahn 1991
- Hahn I, Sommar S, Fall M. A comparative study of pelvic floor training and electrical stimulation for the treatment of genuine female stress urinary incontinence. Neurourology and Urodynamics 1991;10(6):545-54. [Google Scholar]
Haig 1995
- Haig L, Mantle J, Versi E. Does interferential therapy (IFT) confer added benefit over a pelvic floor muscle exercise programme (PFMEP) for genuine stress incontinence (GSI)? (Abstract number 111). In: International Continence Society (ICS), 25th Annual Meeting; 1995 Oct 17-20; Sydney (Australia). 1995:36-7.
Hajebrahimi 2015
- Hajebrahimi S, Sadeghi-Bazargani H, Taleschian Tabrizi N, Farhadi F, Sadeghi Ghyassi F. Non-drug treatment for lower urinary tract symptoms in women with voiding dysfunction. Cochrane Database of Systematic Reviews 2015, Issue 1. Art. No: CD011470. [DOI: 10.1002/14651858.CD011470] [DOI] [Google Scholar]
Hargreaves 2020
- Hargreaves E, Baker K, Barry G, Harding C, Zhang Y, Kandala NB, et al. Acupuncture for treating overactive bladder in adults. Cochrane Database of Systematic Reviews 2020, Issue 1. Art. No: CD013519. [DOI: 10.1002/14651858.CD013519] [DOI] [PMC free article] [PubMed] [Google Scholar]
Haylen 2010
- Haylen BT, Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourology and Urodynamics 2010;29(1):4-20. [DOI] [PubMed] [Google Scholar]
Hay‐Smith 2002
- Hay-Smith EJ, Herbison GP, Wilson PD. Pelvic floor muscle training for women with symptoms of stress urinary incontinence: a randomised trial comparing strengthening and motor relearning approaches (Abstract). Neurourology and Urodynamics 2002;21(4):371-2. [sr-incont14538] [Google Scholar]
Henalla 1989
- Henalla SM, Hutchins CJ, Robinson P, MacVicar J. Non-operative methods in the treatment of female genuine stress incontinence of urine. Journal of Obstetrics and Gynaecology 1989;9(3):222-5. [Google Scholar]
Herbison 2004
- Herbison GP, Lauti M, Hay-Smith J, Wilson D. Three month results from the urgent pilot study: a randomised controlled trial comparing drug therapy, bladder retraining and their combination in patients with urge urinary incontinence (Abstract number 174). In: International Continence Society (34th Annual Meeting) and the International UroGynecological Association; 2004 Aug 23–27; Paris (France). 2004. [sr-incont19033]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Hofbauer 1990
- Hofbauer J, Preisinger F, Nürnberger N. The value of physical therapy in genuine female stress incontinence [Der stellenwert der physiokotherapie bei der wieblichen genuinen seb-inkontinenz]. Zeitschrift fur Urologie und Nephrologie 1990;83(5):249-54. [SR-INCONT350] [PubMed] [Google Scholar]
Huang 2014
- Huang AJ, Jenny HE, Chesney MA, Schembri M, Subak LL. A group-based yoga therapy intervention for urinary incontinence in women: a pilot randomized trial. Female Pelvic Medicine and Reconstructive Surgery 2014;20(3):147-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hung 2010
- Hung HC, Hsiao SM, Chih SY, Lin HH, Tsauo JY. An alternative intervention for urinary incontinence: retraining diaphragmatic, deep abdominal and pelvic floor muscle coordinated function. Manual Therapy 2010;15(3):273-9. [DOI] [PubMed] [Google Scholar]
Hunskaar 2002
- Hunskaar S, Burgio K, Diokno AC, Herzog AR, Hjalmas K, Lapitan MC. Epidemiology and natural history of urinary incontinence (UI). In: Abrams P, Cardozo L, Khoury S, Wein A, editors(s). Incontinence: 2nd International Consultation on Incontinence. Recommendations of the International Scientific Committee: the evaluation and treatment of urinary incontinence. Paris, 1–3 July 2001. 2nd edition. Plymouth, UK: Health Publication Ltd, 2002:165-201. [Google Scholar]
Hunskaar 2005
- Hunskaar S, Burgio K, Clark A, Lapitan MC, Nelson R, Sillén U, et al. Epidemiology of urinary (UI) and faecal (FI) incontinence and pelvic organ prolapse (POP). In: Abrams P, Cardozo L, Khoury R, Wein A, editors(s). Incontinence. 3rd International Consultation on Incontinence. Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence; 2004 Jun 26–29; Monte Carlo, Monaco. Plymouth, UK: Health Publication Ltd, 2005:255-312. [Google Scholar]
Imamura 2010
- Imamura M, Abrams P, Bain C, Buckley B, Cardozo L, Cody J, et al. Systematic review and economic modelling of the effectiveness and cost-effectiveness of non-surgical treatments for women with stress urinary incontinence. Health Technology Assessment (Winchester, England) 2010;14(40):1-506. [DOI: 10.3320/hta14400] [DOI] [PubMed] [Google Scholar]
Ishiko 2000
- Ishiko O, Ushiroyama T, Saji F, Mitsuhashi Y, Tamura T, Yamamoto K, et al. Beta(2)-adrenergic agonists and pelvic floor exercises for female stress incontinence. International Journal of Gynaecology and Obstetrics 2000;71(1):39-44. [DOI] [PubMed] [Google Scholar]
Islah 2013
- Islah M, Cho SY, Son H. The current role of the artificial urinary sphincter in male and female urinary incontinence. World Journal of Men's Health 2013;31(1):21-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jackson 1996
- Jackson S, Donovan J, Brookes S, Eckford S, Swithinbank L, Abrams P. The Bristol Female Lower Urinary Tract Symptoms questionnaire: development and psychometric testing. British Journal of Urology 1996;77(6):805-12. [DOI] [PubMed] [Google Scholar]
Johnson 2000
- Johnson JL, King Baker T. Biofeedback versus verbal instruction for pelvic floor training in the treatment of urinary incontinence. Journal of Women's Health Physical Therapy 2000;24(3):7-13. [Google Scholar]
Kargar Jahromi 2015
- Kargar Jahromi M, Talebizadeh M, Mirzaei M. The effect of pelvic muscle exercises on urinary incontinency and self-esteem of elderly females with stress urinary incontinency, 2013. Global Journal of Health Science 2015;72(2):71-9. [DOI: 10.5539/gjhs.v7n2p71] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaya 2011
- Kaya S, Akbayrak T, Beksaç S. Comparison of different treatment protocols in the treatment of idiopathic detrusor overactivity: a randomized controlled trial. Clinical Rehabilitation 2011;25(4):327-38. [DOI] [PubMed] [Google Scholar]
Kaya 2014
- Kaya S, Akbayrak T, Gürsen C, Beksaç S. Pelvic floor muscle training added to bladder training versus bladder training alone for female urinary incontinence: a randomized controlled trial. Neurourology and Urodynamics 2014;33(6):864-6. [sr-incont64341] [Google Scholar]
Kelleher 1997
- Kelleher CJ, Cardozo LD, Khullar V, Salvatore S. A new questionnaire to assess the quality of life of urinary incontinent women. British Journal of Obstetrics and Gynaecology 1997;104(12):1374-9. [DOI] [PubMed] [Google Scholar]
Khazali 2016
- Khazali S, Jackson S, Balmforth J. Electromagnetic treatment for urinary incontinence in adults (Protocol). Cochrane Database of Systematic Reviews 2016, Issue 5. Art. No: CD006711. [DOI: 10.1002/14651858.CD006711.pub2] [DOI] [Google Scholar]
Klarskov 1986
- Klarskov P, Belving D, Bischoff N, Dorph S, Gerstenberg T, Hald T, et al. Pelvic floor exercise versus surgery for female urinary stress incontinence: preliminary results. In: International Continence Society (ICS), 14th Annual Meeting; 1984 Sep 13–15; Innsbruck (Austria). 1984:159-61.
Knight 1998
- Knight S, Laycock J, Naylor D. Evaluation of neuromuscular electrical stimulation in the treatment of genuine stress incontinence. Physiotherapy 1998;84(2):61-71. [Google Scholar]
Komesu 2011
- Komesu YM, Sapien RE, Rogers RG, Ketai LH. Hypnotherapy for treatment of overactive bladder: a randomized controlled trial pilot study. Female Pelvic Medicine and Reconstructive Surgery 2011;17(6):308-13. [DOI: 10.1097/SPV.0b013e31823a08d9] [DOI] [PMC free article] [PubMed] [Google Scholar]
Konstantinidou 2007
- Konstantinidou E, Apostolidis A, Kondelisis N, Tsimtsiou Z, Hatzchristou D, Ioannides E. Short-term efficacy of group pelvic floor training under intensive supervision versus unsupervised home training for female stress urinary incontinence: a randomized pilot study. Neurology and Urodynamics 2007;26:486-91. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kosilov 2013
- Kosilov KV, Loparev SA, Ivanovskaya MA, Kosilova LV. Therapeutic effect consolidation in overactive bladder treatment in elderly women by the use of increased antimuscarinic dosages. Sovremennye Tehnologii v Medicine 2013;5(4):78-82. [Google Scholar]
Lagro‐Janssen 1991
- Lagro-Janssen TL, Debruyne FM, Smits AJ, Weel C. Controlled trial of pelvic floor exercises in the treatment of urinary stress incontinence in general practice. British Journal of General Practice 1991;41(352):445-9. [PMC free article] [PubMed] [Google Scholar]
Lagro‐Janssen 1992
- Lagro-Janssen AL, Debruyne FM, Smits AJ, Weel C. The effects of treatment of urinary incontinence in general practice. Family Practice 1992;9(3):284-9. [DOI] [PubMed] [Google Scholar]
Lane 2020
- Lane GI, Barboglio-Romo P, Crescenze I, Raza D, Clemens JQ, Dahm P, et al. Vaginal lasers for treating stress urinary incontinence in women. Cochrane Database of Systematic Reviews 2020, Issue 6. Art. No: CD013643. [DOI: 10.1002/14651858.CD013643] [DOI] [Google Scholar]
Lapitan 2016
- Lapitan MC, Cody JD. Open retropubic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2016, Issue 2. Art. No: CD002912. [DOI: 10.1002/14651858.CD002912.pub6] [DOI] [PubMed] [Google Scholar]
Laycock 1988
- Laycock J. Interferential therapy in the treatment of genuine stress incontinence. Neurourology and Urodynamics 1988;7(3):268-9. [Google Scholar]
Laycock 1993
- Laycock J, Jerwood D. Does pre-modulated interferential therapy cure genuine stress incontinence? Physiotherapy 1993;79(8):553-60. [Google Scholar]
Leong 2015
- Leong BS, Mok NW. Effectiveness of a new standardised Urinary Continence Physiotherapy Programme for community-dwelling older women in Hong Kong. Hong Kong Medical Journal 2015;21(1):30-7. [DOI: 10.12809/hkmj134185] [DOI] [PubMed] [Google Scholar]
Liberati 2009
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLOS Medicine 2009;6(7):e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lins 2014
- Lins S, Hayder-Beichel D, Kunath F, Cartwright R, Motschall E, Antes G, et al. Pelvic floor muscle training versus other active treatments for urinary incontinence in women. Cochrane Database of Systematic Reviews 2014, Issue 6. Art. No: CD007173. [DOI: 10.1002/14651858.CD007173.pub3] [DOI] [Google Scholar]
Lopès 2014
- Lopès P, Rimbault F, Scheffler M, André C, Cappelletti MC, Marès P. Multicentric prospective randomized and controlled study assessing effectiveness of intravaginal electrostimulation at home compared to usual care in female patients with urinary incontinence and prior perineal reeducation. Gynecologie, Obstetrique and Fertilite 2014;42(11):779-86. [DOI] [PubMed] [Google Scholar]
Luber 1997
- Luber KM, Wolde-Tsadik G. Efficacy of functional electrical stimulation in treating genuine stress incontinence: a randomized clinical trial. Neurourology and Urodynamics 1997;16(6):543-51. [DOI] [PubMed] [Google Scholar]
Macaulay 1987
- Macaulay AJ, Stern RS, Holmes DS, Stanton SL. Micturition and the mind: psychological factors in the aetiology and the treatment of urinary symptoms in women. BMJ (Clinical Research Ed.) 1987;294(6571):540-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mak 2007
- Mak HL, Cheon WC, Wong T, Liu YS, Tong WM. Randomized controlled trial of foot reflexology on patients with symptomatic idiopathic detrusor overactivity. International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(6):653-8. [DOI] [PubMed] [Google Scholar]
Malan 1963
- Malan DH. A Study of Brief Psychotherapy. London (UK): Tavistock, 1963. [Google Scholar]
Mann 1973
- Mann J. Time-Limited Psychotherapy. Cambridge (MA): Harvard University Press, 1973. [Google Scholar]
McClurg 2013
- McClurg D, Cheater FM, Eustice S, Burke J, Jamieson K, Hagen S. A multi-professional UK wide survey of undergraduate continence education. Neurourology and Urodynamics 2013;32(3):224-9. [DOI] [PubMed] [Google Scholar]
McLean 2013
- McLean L, Varette K, Gentilcore-Saulnier E, Harvey MA, Baker K, Sauerbrei E. Pelvic floor muscle training in women with stress urinary incontinence causes hypertrophy of the urethral sphincters and reduces bladder neck mobility during coughing. Neurourology and Urodynamics 2013;32(8):1096-102. [DOI: 10.1002/nau.22343] [DOI] [PMC free article] [PubMed] [Google Scholar]
Melville 2009
- Melville JL, Fan MY, Rau H, Nygaard IE, Katon WJ. Major depression and urinary incontinence in women: temporal associations in an epidemiologic sample. American Journal of Obstetrics and Gynecology 2009;201(5):490, e1-7. [DOI] [PubMed] [Google Scholar]
Messelink 1999
- Messelink EJ. The overactive bladder and the role of pelvic floor muscles. British Journal of Urology 1999;83(Suppl 2):31-5. [DOI] [PubMed] [Google Scholar]
Milani 1986
- Milani R, Scalambrino S, Carrera S, Quadri G, Riva D, Casolati E. A randomized trial of bladder retraining versus oxybutynin in the treatment of idiopathic urge syndrome, early results. In: International Continence Society (ICS), 16th Annual Meeting; 1986 Sept 17–19; Boston (MA). 1986:488-90.
Millard 2004
- Millard RJ. Clinical efficacy of tolterodine with or without a simplified pelvic floor exercise regimen. Neurourology and Urodynamics 2004;23:48-53. [DOI] [PubMed] [Google Scholar]
Milsom 2012
- Milsom I, Altman D, Cartwright R, Lapitan MC, Nelson R, Sillén U, et al. Epidemiology of urinary incontinence (UI) and other lower urinary tract symptoms (LUTS), pelvic organ prolapse (POP) and anal incontinence (AI). In: Incontinence. London (UK): ICUD-EAU, 2013:15-107. [Google Scholar]
Moher 2005
- Moher D, Schulz KF, Altman D, Group C. The CONSORT Statement: revised recommendations for improving the quality of reports of parallel-group randomized trials 2001. Explore (NY) 2005;1(1):40-5. [DOI] [PubMed] [Google Scholar]
Morkved 2003
- Morkved S, Bø K, Fjortoft T. Continence status one year after cessation of organised pelvic floor muscle training. In: International Continence Society (ICS), 33rd Annual Meeting; 2003 Oct 5–9; Florence Italy. 2003:260-1.
Morrill 2007
- Morrill M, Lukacz ES, Lawrence JM, Nager CW, Contreras R, Luber KM. Seeking healthcare for pelvic floor disorders: a population-based study. American Journal of Obstetrics and Gynecology 2007;197(1):86. [DOI] [PubMed] [Google Scholar]
Morrison 1995
- Morrison JF. The excitability of the micturition reflex. Scandinavian Journal of Urology and Nephrology Supplementum 1995;175:21-5. [PubMed] [Google Scholar]
Murad 2016
- Murad MH, Mustafa R, Morgan R, Sultan S, Falck-Ytter Y, Dahm P. Rating the quality of evidence is by necessity a matter of judgment. Journal of Clinical Epidemiology 2016;74:237-8. [DOI] [PubMed] [Google Scholar]
Nascimento‐Correia 2012
- Nascimento-Correia G, Santos-Pereira V, Tahara N, Driusso P. Effects of pelvic floor muscle training on quality of life of a group of women with urinary incontinence: randomized controlled trial. Actas Urologicas Espanolas 2012;36(4):216-21. [sr-incont44721] [DOI] [PubMed] [Google Scholar]
NICE 2019
- National Institute for Health and Care Excellence (NICE), National Guideline Alliance. Urinary incontinence and pelvic organ prolapse in women: management. NICE guideline [NG123], 2019. www.nice.org.uk/guidance/ng123 (accessed 30 May 2022).
Nielson 1995
- Nielsen KK, Walter S, Maegaard E, Kromann-Andersen B. The urethral plug – an alternative treatment of women with urinary stress incontinence. Ugeskrift for Laeger 1995;157(22):3194-7. [PubMed] [Google Scholar]
Oláh 1990
- Oláh KS, Bridges N, Denning J, Farrar DJ. The conservative management of patients with symptoms of stress incontinence: a randomized prospective study comparing weighted vaginal cones and interferential therapy. American Journal of Obstetrics and Gynecology 1990;162(1):87-92. [DOI] [PubMed] [Google Scholar]
Oldham 2013
- Oldham J, Herbert J, McBride K. Evaluation of a new disposable "tampon like" electrostimulation technology (Pelviva®) for the treatment of urinary incontinence in women: a 12-week single blind randomized controlled trial. Neurourology and Urodynamics 2013;32(5):460-6. [DOI] [PubMed] [Google Scholar]
Ostaszkiewicz 2013
- Ostaszkiewicz J, Eustice S, Roe B, Thomas LH, French B, Islam T, et al. Toileting assistance programmes for the management of urinary incontinence in adults. Cochrane Database of Systematic Reviews 2013, Issue 6. Art. No: CD010589. [DOI: 10.1002/14651858.CD010589] [DOI] [Google Scholar]
Pages 2001
- Pages IH, Jahr S, Schaufele MK, Conradi E. Comparative analysis of biofeedback and physical therapy for treatment of urinary stress incontinence in women. American Journal of Physical Medicine and Rehabilitation 2001;80(7):494-502. [DOI] [PubMed] [Google Scholar]
Paiva 2017
- Paiva L, Ferla L, Darski C, Catarino B, Ramos J. Pelvic floor muscle training in groups versus individual or home treatment of women with urinary incontinence: systematic review and meta-analysis. International Urogynecology Journal 2017;28(3):351-9. [DOI] [PubMed] [Google Scholar]
Park 2002
- Park JT, Song C, Choo M. The effects of bladder retraining, tolterodine, and bladder retraining with tolterodine in female patients with overactive bladder; prospective, randomized study. Neurourology and Urodynamics 2002;21(4):434-5. [Google Scholar]
Patil 2010
- Patil SP, Nagrale AV, Ganvir SD. Additive effect of interferential therapy over pelvic floor exercises. International Journal of Therapy and Rehabilitation 2010;17(11):596-602. [Google Scholar]
Peattie 1988
- Peattie AB, Plevnik S. Cones versus physiotherapy as conservative management of genuine stress incontinence. Neurourology and Urodynamics 1988;7(3):265-6. [Google Scholar]
Pereira 2012
- Pereira VS, Melo MV, Correia GN, Driusso P. Long-term effects of pelvic floor muscle training with vaginal cone in post-menopausal women with urinary incontinence: a randomized controlled trial. Neurourology and Urodynamics 2013;32(1):48-52. [DOI] [PubMed] [Google Scholar]
Phelan 2012
- Phelan S, Kanaya AM, Subak LL, Hogan PE, Espeland MA, Wing RR, et al. Weight loss prevents urinary incontinence in women with type 2 diabetes: results from the Look AHEAD trial. Journal of Urology 2012;187(3):939-44. [sr-incont44588] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pieber 1995
- Pieber D, Zivkovic F, Tamussino K, Ralph G, Lippitt G, Fauland B. Pelvic floor exercise alone or with vaginal cones for the treatment of mild to moderate stress urinary incontinence in premenopausal women. International Urogynecology Journal 1995;6(1):14-7. [Google Scholar]
Pollock 2014
- Pollock A, Farmer SE, Brady MC, Langhorne P, Mead GE, Mehrholz J, et al. Interventions for improving upper limb function after stroke. Cochrane Database of Systematic Reviews 2014, Issue 11. Art. No: CD010820. [DOI: 10.1002/14651858.CD010820.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pollock 2015
- Pollock A, Campbell P, Baer G, Choo PL, Morris J, Forster A. User involvement in a Cochrane systematic review: using structured methods to enhance the clinical relevance, usefulness and usability of a systematic review update. Systematic Reviews 2015;4:55. [DOI] [PMC free article] [PubMed]
Pollock 2016
- Pollock A, Farmer SE, Brady MC, Langhorne P, Mead GE, Mehrholz J, et al. An algorithm was developed to assign GRADE levels of evidence to comparisons within systematic reviews. Journal of Clinical Epidemiology 2016;70:106-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pollock 2018
- Pollock A, Campbell P, Struthers C, Synnot A, Nunn J, Hill S, et al. Stakeholder involvement in systematic reviews: a scoping review. Systematic Reviews 2018;7(1):208. [DOI: 10.1186/s13643-018-0852-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Preyer 2007
- Preyer O, Gabriel B, Mailath-Porkorny M, Doerfler D, Laml T, Umek W, et al. Peripheral tibial neurostimulation (PTNS) versus tolterodine in the treatment of women with urge urinary incontinence and urge symptoms. International Urogynecology Journal 2007;18(Suppl 1):S139-40. [Google Scholar]
Ramsay 1990
- Ramsay IN, Thow M. A randomised, double blind, placebo controlled trial of pelvic floor exercises in the treatment of genuine stress incontinence. Neurourology and Urodynamics 1990;9(4):398-9. [Google Scholar]
Reynard 2016
- Reynard J, Cannon A, Abrams P. Conservative management of nocturia in adults. Cochrane Database of Systematic Reviews 2016, Issue 9. Art. No: CD004669. [DOI: 10.1002/14651858.CD004669.pub2] [DOI] [Google Scholar]
Richter 2007
- Richter HE, Burgio KL, Goode PS, Borello-France D, Bradley CS, Brubaker L, et al. Non-surgical management of stress urinary incontinence: ambulatory treatments for leakage associated with stress (ATLAS) trial. Clinical Trials 2007;4(1):92-101. [DOI] [PubMed] [Google Scholar]
Robinson 2003
- Robinson H, Schulz J, Flood C, Hansen L. A randomized controlled trial of the NEAT expandable tip continence device. International Urogynecology Journal and Pelvic Floor Dysfunction 2003;14(3):199-203. [DOI] [PubMed] [Google Scholar]
Sancaktar 2010
- Sancaktar M, Ceyhan ST, Akyol I, Muhcu M, Alanbay I, Mutlu Ercan CM, et al. The outcome of adding peripheral neuromodulation (Stoller afferent neuro-stimulation) to anti-muscarinic therapy in women with severe overactive bladder. Gynecological Endocrinology 2010;26(10):729-32. [DOI] [PubMed] [Google Scholar]
Sandvik 2000
- Sandvik H, Seim A, Vanvik A, Hunskaar S. A severity index for epidemiological surveys of female urinary incontinence: comparison with 48-hour pad-weighing tests. Neurourology and Urodynamics 2000;19(2):137-45. [DOI] [PubMed] [Google Scholar]
Sandweiss 1985
- Sandweiss JH, Wolf SL, editor(s). Biofeedback and Sports Science. New York (NY): Plenum Press, 1985. [Google Scholar]
Santos 2009
- Santos PF, Oliveira E, Zanetti MR, Arruda RM, Sartori MG, Girão MJ, et al. Electrical stimulation of the pelvic floor versus vaginal cone therapy for the treatment of stress urinary incontinence [Eletroestimulação funcional do assoalho pélvico versus terapia com os cones vaginais para o tratamento de incontinência urinária de esforço]. Revista Brasileira de Ginecologia e Obstetríca 2009;31(9):447-52. [DOI] [PubMed] [Google Scholar]
Sar 2009
- Sar D, Khorshid L. The effects of pelvic floor muscle training on stress and mixed urinary incontinence and quality of life. Journal of Wound, Ostomy, and Continence Nursing 2009;36(4):429-35. [sr-incont32103] [DOI] [PubMed] [Google Scholar]
Schagen van Leeuwen 2004
- Schagen van Leeuwen JH, Elser D, Freeman R, Ghoniem G, Zhao Y, Yalcin I, et al. Controlled trial of duloxetine alone, pelvic floor muscle training alone, combined treatment, and no treatment in women with stress urinary incontinence (SUI). European Urology Supplements 2004;3(2):52. [DOI] [PubMed] [Google Scholar]
Schmidt 2009
- Schmidt AP, Sanches PR, Silva DP, Ramos JG, Nohama P. A new pelvic muscle trainer for the treatment of urinary incontinence. International Journal of Gynaecology and Obstetrics 2009;105(3):218-22. [DOI] [PubMed] [Google Scholar]
Schreiner 2010
- Schreiner L, dos Santos TG, Knorst MR, Silva Filho IG. Randomized trial of transcutaneous tibial nerve stimulation to treat urge urinary incontinence in older women. International Urogynecology Journal 2010;21(9):1065-70. [DOI] [PubMed] [Google Scholar]
Seo 2004
- Seo JT, Yoon H, Kim YH. A randomized prospective study comparing new vaginal cone and FES-Biofeedback. Yonsei Medical Journal 2004;45(5):879-84. [DOI] [PubMed] [Google Scholar]
Shinohara 2013
- Shinohara K, Honyashiki M, Imai H, Hunot V, Caldwell DM, Davies P, et al. Behavioural therapies versus other psychological therapies for depression. Cochrane Database of Systematic Reviews 2013, Issue 10. Art. No: CD008696. [DOI: 10.1002/14651858.CD008696.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2006
- Smith CA, Collins CT, Cyna AM, Crowther CA. Complementary and alternative therapies for pain management in labour. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No: CD003521. [DOI: 10.1002/14651858.CD003521.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Solberg 2016
- Solberg M, Alraek T, Mdala I, Klovning A. A pilot study on the use of acupuncture or pelvic floor muscle training for mixed urinary incontinence. Acupuncture in Medicine 2016;34(1):7-13. [DOI: 10.1136/acupmed-2015-010828] [DOI] [PMC free article] [PubMed] [Google Scholar]
Song 2006
- Song C, Park JT, Heo KO, Lee KS, Choo MS. Effects of bladder training and/or tolterodine in female patients with overactive bladder syndrome: a prospective, randomized study. Journal of Korean Medical Science 2006;21(6):1060-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Souto 2014
- Souto SC, Reis LO, Palma T, Palma P, Denardi F. Prospective and randomized comparison of electrical stimulation of the posterior tibial nerve versus oxybutynin versus their combination for treatment of women with overactive bladder syndrome. World Journal of Urology 2014;32(1):179-84. [DOI] [PubMed] [Google Scholar]
Sran 2016
- Sran M, Mercier J, Wilson P, Lieblich P, Dumoulin C. Physical therapy for urinary incontinence in postmenopausal women with osteoporosis or low bone density: a randomized controlled trial. Menopause 2016;23(3):286-93. [DOI: 10.1097/GME.0000000000000594] [DOI] [PubMed] [Google Scholar]
Sriboonreung 2011
- Sriboonreung T, Wongtra-Ngan S, Eungpinichpong W, Laopaiboon M. Effectiveness of pelvic floor muscle training in incontinent women at Maharaj Nakorn Chiang Mai Hospital: a randomized controlled trial. Journal of the Medical Association of Thailand 2011;94(1):1-7. [PubMed] [Google Scholar]
Strupp 1984
- Strupp H, Binder J. Psychotherapy in a New Key: a Guide to Time-Limited Dynamic Psychotherapy. New York (NY): Basic Books, 1984. [Google Scholar]
Subak 2005
- Subak LL, Whitcomb E, Shen H, Saxton J, Vittinghoff E, Brown JS. Weight loss: a novel and effective treatment for urinary incontinence. Journal of Urology 2005;174(1):190-5. [sr-incont20655] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sugaya 2003
- Sugaya K, Owan T, Hatano T, Nishijima S, Miyazato M, Mukouyama H, et al. Device to promote pelvic floor muscle training for stress incontinence. International Journal of Urology 2003;10(8):416-22. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Takahashi 2003
- Takahashi S, Kitamura T. Overactive bladder: magnetic versus electrical stimulation. Current Opinion in Obstetrics and Gynecology 2003;15(5):429-33. [DOI] [PubMed] [Google Scholar]
Tapp 1989
- Tapp AJ, Hills B, Cardozo L. Randomised study comparing pelvic floor physiotherapy with the Burch colposuspension. Neurourology and Urodynamics 1989;8(4):356-7. [Google Scholar]
Terlikowski 2013
- Terlikowski R, Dobrzycka B, Kinalski M, Kuryliszyn-Moskal A, Terlikowski SJ. Transvaginal electrical stimulation with surface-EMG biofeedback in managing stress urinary incontinence in women of premenopausal age: a double-blind, placebo-controlled, randomized clinical trial. International Urogynecology Journal 2013;24(10):1631-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
ter Meulen 2009
- ter Meulen PH, Berghmans LC, Nieman FH, Kerrebroeck PE. Effects of Macroplastique Implantation System for stress urinary incontinence and urethral hypermobility in women. International Urogynecology Journal and Pelvic Floor Dysfunction 2009;20(2):177-83. [DOI] [PubMed] [Google Scholar]
Turner 2004
- Turner DA, Shaw C, McGrother CW, Dallosso HM, Cooper NJ, MRC Incontinence Team. The cost of clinically significant urinary storage symptoms for community dwelling adults in the UK. BJU International 2004;93(9):1246-52. [DOI] [PubMed] [Google Scholar]
Vecchioli‐Scaldazza 2013
- Vecchioli-Scaldazza C, Morosetti C, Berouz A, Giannubilo W, Ferrara V. Solifenacin succinate versus percutaneous tibial nerve stimulation in women with overactive bladder syndrome: results of a randomized controlled crossover study. Gynecology and Obstetric Investigation 2013;75(4):230-4. [DOI] [PubMed] [Google Scholar]
Wagner 1996
- Wagner TH, Patrick DL, Bavendam TG, Martin ML, Buesching DP. Quality of life of persons with urinary incontinence: development of a new measure. Urology 1996;47(1):67-71. [DOI] [PubMed] [Google Scholar]
Wang 2004
- Wang A, Wang Y. Single blind, randomized trial of pelvic floor muscle training (PFMT), biofeedback assisted pelvic floor muscle training (BAPFMT) and electrical stimulation (ES) in the management of overactive bladder (OAB). Neurourology and Urodynamics 2004;22(5):519-20. [Google Scholar]
Wang 2006
- Wang AC, Chih SY, Chen MC. Comparison of electric stimulation and oxybutynin chloride in management of overactive bladder with special reference to urinary urgency: a randomized placebo-controlled trial. Urology 2006;68(5):999-1004. [DOI] [PubMed] [Google Scholar]
Weir 2012
- Weir MC, Grimshaw JM, Mayhew A, Fergusson D. Decisions about lumping vs. splitting of the scope of systematic reviews of complex interventions are not well justified: a case study in systematic reviews of health care professional reminders. Journal of Clinical Epidemiology 2012;65(7):756-63. [DOI] [PubMed] [Google Scholar]
Wells 1991
- Wells TJ, Brink CA, Diokno AC, Wolfe R, Gillis GL. Pelvic muscle exercise for stress urinary incontinence in elderly women. Journal of the American Geriatrics Society 1991;39(8):785-91. [DOI] [PubMed] [Google Scholar]
Wells 1999
- Wells T, Major R, Brink C, Brown R. Pelvic muscle exercise: a controlled clinical trial. Unpublished manuscript (written in 1999, as supplied 3 November 2008).
Whitford 2011
- Whitford HM, Jones M. An exploration of the motivation of pregnant women to perform pelvic floor exercises using the revised theory of planned behavior. British Journal of Health Psychology Internet 2011;16(4):761-78. [DOI] [PubMed] [Google Scholar]
Whiting 2015 [pers comm]
- Whiting P. ROBIS tool: search strategy query [personal communication]. Email to: A Pollock 16 December 2015.
Whiting 2016
- Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, et al, ROBIS group. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. Journal of Clinical Epidemiology 2016;69:225-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Whitmore 1995
- Whitmore KE, Staskin DR, Grigoriev VE, Appell RA, Sand PK, Ostergaard DR. Pelvic floor stimulation in the treatment of genuine stress incontinence: a multicenter placebo controlled trial. Journal of Urology 1995;153(4 Suppl):491A. [DOI] [PubMed] [Google Scholar]
Wilks 2007
- Wilks J. The Bowen Technique: the Inside Story. Sherborne (UK): CYMA Ltd, 2007. [ISBN: 9780955706301] [Google Scholar]
Williams 2006
- Williams KS, Assassa RP, Gillies CL, Abrams KR, Turner DA, Shaw C, et al. A randomized controlled trial of the effectiveness of pelvic floor therapies for urodynamic stress and mixed incontinence. BJU International 2006;98(5):1043-50. [DOI] [PubMed] [Google Scholar]
Wilson 1987
- Wilson PD, Faragher B, Butler B, Bu'lock D, Robinson EL, Brown AD. Treatment with oral piperazine oestrone sulphate for genuine stress incontinence in postmenopausal women. British Journal of Obstetrics and Gynaecology 1987;94(6):568-74. [sr-incont513] [DOI] [PubMed] [Google Scholar]
Wing 2010
- Wing RR, West DS, Grady D, Creasman JM, Richter HE, Myers D, et al. Effect of weight loss on urinary incontinence in overweight and obese women: results at 12 and 18 months. Journal of Urology 2010;184(3):1005-10. [sr-incont40041] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wyman 1998
- Wyman JF, Fantl JA, McClish DK, Bump RC, Continence Program for Women Research Group. Comparative efficacy of behavioral interventions in the management of female urinary incontinence. American Journal of Obstetrics and Gynecology 1998;179(4):999-1007. [PMID: ] [DOI] [PubMed] [Google Scholar]
Yi 2014
- Yi ZM, Zhao RS, Zhai SD, Wang GL. Drug treatment for lower urinary tract symptoms in women with voiding dysfunction. Cochrane Database of Systematic Reviews 2014, Issue 8. Art. No: CD011264. [DOI: 10.1002/14651858.CD011264] [DOI] [Google Scholar]
Yoon 2003
- Yoon HS, Song HH, Ro YJ. A comparison of effectiveness of bladder training and pelvic muscle exercise on female urinary incontinence. International Journal of Nursing Studies 2003;40(1):45-50. [sr-incont15700] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
McClurg 2016
- McClurg D, Pollock A, Campbell P, Hazelton C, Elders A, Hagen S, et al. Conservative interventions for urinary incontinence in women: an overview of Cochrane systematic reviews. Cochrane Database of Systematic Reviews 2016, Issue 9. Art. No: CD012337. [DOI: 10.1002/14651858.CD012337] [DOI] [PMC free article] [PubMed] [Google Scholar]