Abstract
Gain-of-function point mutations in the receptor tyrosine kinase RET, a driver oncogene in medullary thyroid carcinoma (MTC), prevent apoptosis through inhibition of ATF4, a critical transcriptional regulator of endoplasmic reticulum stress. However, the critical regulatory mechanisms driving RET-dependent oncogenesis remain elusive, and there is a clinical need to identify a transcriptional RET inhibitor. Here, we found that RET depletion decreased IGFBP2 and VEGFR2 mRNA and protein expression in MTC cells. IGFBP2 knockdown decreased cell survival and migration of MTC cells. In patients, IGFBP2 expression increased in metastatic MTC, and high IGFBP2 associated with poor overall survival. VEGFR2 protein levels were positively associated with RET expression in primary tumors, and VEGF-mediated increased cell viability was RET dependent. The small molecule ONC201 treatment of MTC cells caused apoptotic cell death, decreased transcription of RET, VEGFR2, IGFBP2, increased mRNA levels of ATF4, and ATF4 target genes including DDIT3, BBC3, DUSP8, MKNK2, KLF9, LZTFL1, SESN2. Moreover, IGFBP2 depletion increased ONC201-induced cell death. ONC201 inhibited tumor growth at a well-tolerated dose of 120 mg/kg/week administered by oral gavage and decreased MTC xenografts cell proliferation and angiogenesis. The protein levels of RET, IGFBP2, and VEGFR2 were decreased in ONC201-treated xenografts. Our study uncovered a novel ONC201 mechanism of action through regulation of RET and its targets, VEGFR2 and IGFBP2; this mechanism could be translated into the clinic and represent a promising strategy for the treatment of all MTC patients, including those with TKI-refractory disease and other cancer with RET abnormalities.
Keywords: RET, ATF4, VEGFR2, IGFBP2
Introduction
Medullary thyroid carcinoma (MTC) originates from the calcitonin-producing thyroid parafollicular cells (1). Seventy-five percent of patients have lymph node metastasis at diagnosis, and 10–15% have distant metastasis (2). The RET (rearranged during transfection) gene encodes a transmembrane tyrosine kinase receptor, mutated in 43–70% of sporadic cases (3). The most frequent RET mutation is M918T alteration, which is associated with worse overall survival of MTC patients (4). In recent years, there has been a paradigm shift in the treatment of MTC, with the U.S. Food and Drug Administration (FDA) approval of multi-kinase inhibitors (TKIs), vandetanib (inhibits multiple receptors: RET, epidermal growth factor receptor and vascular endothelial growth factor 2) and cabozantinib (inhibits RET, C-Met, VEGFR2, and AXL) for the treatment of MTC (5, 6). To date, TKIs have not been curative, and the adverse effects often limit their use, leaving room for improvement (7). Selpercatinib, a specific RET inhibitor, was recently approved by the US FDA to treat RET-mutant MTC (8). Selpercatinib showed durable efficacy with mainly low-grade toxicity effects with or without previous vandetanib or cabozantinib treatment (8, 9).
Prior studies from our laboratory demonstrated that activated RET prevents cell death by promoting degradation of ATF4 via direct phosphorylation, thereby circumventing stress-induced apoptosis (10). While these observations are important in tumorigenesis, the critical regulatory mechanisms driving RET-dependent oncogenesis remain elusive. We hypothesize that RET regulates the expression of proteins involved in MTC’s pathogenesis, such as insulin-like growth factor binding 2 (IGFBP2) and vascular endothelial growth factor receptor 2 (VEGFR2, also known as KDR). IGFBP2, a secreted protein, is elevated in the serum of patients with advanced cancers such as glioblastoma and gastric, prostate, and breast cancer and is associated with progression and metastasis (11–15). IGFBP2 exerts autocrine and paracrine growth modulation of tumor cells and transcriptional regulation of the mesenchymal markers vimentin and Snail and the epithelial marker E-cadherin, promoting an invasive phenotype (16). Furthermore, IGFBP2 mediates resistance to MAPK inhibitors in melanoma (17).
MTC cell lines and tumors have shown dysregulation of receptor tyrosine kinases other than RET and their ligands, including EGFR, VEGFR2, and c-MET (18, 19). Therefore, despite a prominent role for RET in MTC tumorigenesis, it seems possible that cross-talk and direct interactions with other members of the receptor tyrosine kinase network also contribute to tumor development and TKI efficacy.
ONC201 is a first-in-class anti-cancer small molecule (imipridone) in phase II clinical trials in select advanced cancers (20, 21). ONC201 is first identified from an NCI chemical library screen describes as an imidazo[1,2-a]pyrido[4,3-d]pyrimine derivative and possesses an angular [3,4-e] structure (22). ONC201 triggers cell death in various tumor types through an integrated stress response (ISR) involving the transcription factor ATF4, the transactivator DDIT3(CHOP), and the pro-apoptotic protein TRAIL encoded by TNFSF10 and TRAIL receptor, DR5 encoded by TNFSF10B (23, 24). This report demonstrates that RET promotes IGFBP2 and VEGFR2 expression, drivers of tumor growth in MTC xenografts. ONC201 induces cell death by inhibiting RET, IGFBP2, and VEGF2 at the transcriptional level and represents a novel therapeutic option that may benefit all MTC patients, including those with TKI-refractory disease.
Materials and Methods
Reagents and antibodies.
Antibodies specific to RET(D3D8R), IGFBP2(Cat#3922), VEGFR2 (55B11), BBC3(D30C10), and MCL1(D35A5), DDIT3(D46F1), and vinculin were purchased from Cell Signaling Technology. ATF4 antibody(D4B8) was purchased from Abcam. Anti–active caspase 3(clone 10–1-62) and anti–cleaved PARP(ASP214) were purchased from BD Biosciences. ONC201 was obtained from Onceutics (22).
We purchased TT, and 293T cells from ATCC and MZCRC1 cells are from Dr. Alex Knuth (Switzerland) and were previously described (25, 26). TT cells carry a codon 634 cysteine to tryptophan (C634W) exon 11 RET mutation, and MZCRC1 cells have a codon 918 methionine to threonine (M918T) exon 16 RET mutation verified by sequencing. All cell lines were authenticated by Short Tandem Repeat DNA profiling and tested negative for Mycoplasma using the core facility’s core service at the MD Anderson Cancer Center (MDACC). Cells used for the experiments were between 2 and 5 passages from thawing.
Reverse-phase protein array analysis.
RPPA analyses were performed cell lysates from TT parental cells, and TT cells were stably transfected with non-target shRNA and two individual RET shRNA and analyzed in the RPPA core at MDACC. Each sample has two biological replicates that were two-fold-serial diluted for five dilutions and arrayed on nitrocellulose and probed with antibodies and visualized by the colorimetric reaction. Relative protein levels for each sample were determined by interpolation to each dilution curves from the standard curve. All the data points were normalized for protein loading and transformed into linear value and used in the bar graph. Linear after normalization values were transformed to log2 values and the median-centered for Hierarchical Cluster analysis for Heatmap. We stained 168 slides for 152 antibodies. The data for 152 antibodies with quality control scores higher than 0.8 is included in the Heatmap. Heatmap was generated using Cluster3.0 and Java TreeView1.1.1 (27).
Plasmid construction and lentiviral transduction.
Lentiviral vectors (pLKO.1) containing RET and IGFBP2-specific shRNAs or pLK0.1-puro non-target shRNA control (shRNA insert) do not target any known genes from any species) were purchased from Sigma-Aldrich. Lentiviral control shRNA or RET-shRNAs or IGFBP2-shRNA plasmids were co-transfected into 293T cells along with packaging (VPR8.9) and envelope (VSV-G) plasmids for two days. The virus particles containing RET-shRNA, IGFBP2-shRNA, or control shRNA were used to infect TT or MZCRC1 cells. Transfected cells were selected in media containing 2 μg/ml of puromycin (Takara Bio).
Cell viability, cell cycle, apoptosis, and migration assays.
Cell viability was measured using an MTT assay with 20,000 cells in a 96-well plate, as previously described (28). For cell cycle analysis, cells were fixed in ice-cold 70% ethanol, stained with propidium iodide, and analyzed using a Beckman Coulters Gallios flow cytometer. Apoptotic cell death was measured by staining with antibodies against cleaved caspase 3 and cleaved PARP and analyzed using a flow cytometer. The migration assay was performed in 24-well transwell migration chambers with an 8.0-μM pore size (BD Biosciences) as previously described (29).
Real-time PCR.
RNA and cDNA were prepared from cells using a Cells-to-CT kit (Invitrogen). Quantitative PCR was performed as previously described (28). Gene expression values were normalized to HPRT mRNA. According to the manufacturer’s instructions, patient-derived samples were used to isolate RNA using an RNeasy kit (Qiagen). The normal thyroid control was purchased from Newcomer Supply (Middleton, WI). RNA was reverse transcribed into cDNA by using SuperScript III Reverse Transcriptase kit (Invitrogen). Gene expression values were normalized to GAPDH mRNA. All real-time RT-PCR assays were performed in triplicate in at least two independent experiments.
Chromatin immunoprecipitation assay.
MZCRC1 cells were treated with ONC201 (3 μM) for 24 h, and the chromatin immunoprecipitation assays were performed as described previously (28). Formaldehyde-fixed cells were immunoprecipitated overnight with anti-ATF4 antibody, H3K9ac antibody, or rabbit immunoglobulin G. Quantitative real-time PCR SYBR Green was used to determine the fold enrichment of immunoprecipitated material relative to immunoglobulin G with gene-specific primers at the specified regions.
Primers used for ChIP assay: Forward-240bp-ACCCGCGAGTTATCCGTATTC; Reverse-240bp-CCGTCCCTCCGCACTCTT; Forward 1.3Kb-CTTCAATTTCAGCTCCGACTCA; Reverse 1.3Kb-GGTAGAGAGGTGATGTGGTGGTT; Forward 2Kb GCCACAGTCAACTGGATTTCC; Reverse-2Kb- CAGAGTGCAGGATGCTTGCA.
Immunohistochemistry.
The study group consisted of 52 patients diagnosed with MTC who underwent surgery at MDACC. Primary tumors were stained with IGFBP2, as previously described (30). The fraction of IGFBP2-positive tumor cells, as well as the staining intensity, were assessed. IGFBP2 score (H-score) was calculated by multiplying the percentage of stained tumor cells by the staining intensity (1–4), obtaining a range of 1–400 (30). An H score of less than 20 was considered low, and above 20 was considered high. Clinical and histopathologic characteristics of the study population are shown in Supplementary Table S1.
In vivo studies.
Five-week-old male NOD-SCID gamma mice (Jackson laboratory) are maintained under pathogen-free conditions. A total of 5×106 TT and MZCRC1 cells in 100 μl of phosphate-buffered saline/50% Matrigel were subcutaneously injected into the rear flanks of mice. When tumors reached 100 mm3, the mice were randomly divided into two groups (eight mice per group) and treated to either control vehicle or ONC201 (120 mg/kg/week) by oral gavage. Every week, tumor volumes were measured with a caliper and calculated as 𝑉=𝐴×𝐵2×0.5326 (A=long axis, B=short axis), and mice were weighed. At the end of the experiments, the mice were euthanized, and the tumors were harvested and weighed. The animal protocol was approved by the Institutional Animal Care and Use Committee at MDACC.
MTC Patients and clinical data.
This study is a retrospective study of 52 patients who underwent surgery between 1986 to 2016 at MDACC with approval from the Institutional Review Board. TNM staging was based on the American Joint Committee on Cancer 7th edition staging criteria (31). Overall survival was measured from the date of diagnosis until death from any cause. RET germline mutation (exon 16) status was determined by sequencing. Nineteen of the 52 sporadic MTCs (36%) in this cohort showed a somatic RETM918T mutation. Disease status was censored at the last evaluation or time of death. Overall survival was measured from the date of diagnosis, defined as the date of initial surgery, until death from any cause.
Statistical analysis.
All data were expressed as mean ± standard deviation. Data were analyzed with GraphPad Prism 7 software using the indicated tests. Statistical significance was indicated as follows: *, P<0.05; **, P<0.01; ***, P<0.001; and ****, P<0.0001. For patient-related data, unadjusted survival distributions were estimated by the Kaplan-Meier method and compared using the log-rank test. Firth’s penalized Cox regression models were fitted when there was no observed event (i.e., death) for a covariate-defined subgroup. All statistical analyses were performed using R version 3.5.1.
Results
RET depletion decreases IGFBP2 and VEGFR2 transcription in MTC cells.
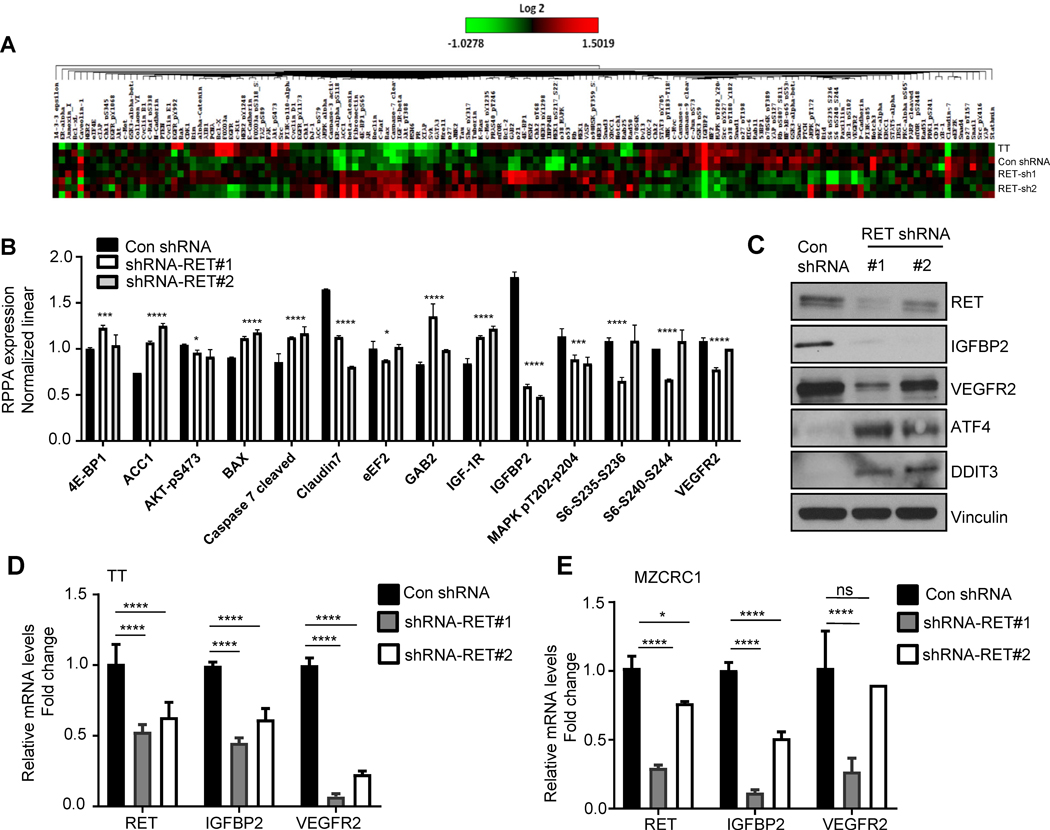
To uncover additional signaling molecules regulated by RET, we performed a reverse-phase protein array analysis of TT cells subjected to stable RET knockdown using independent short hairpins. This antibody-based array included 152 antibodies to detect total protein levels or specific post-translational modifications of protein. We identified subsets of proteins with differential expression between control shRNA and two shRNA-RET cell lines. We observed downregulation od AKT-p473, Claudin 7, IGFBP2, MAPK-T202-Y204, S6-S240-S244, S6-S235-S236, and VEGFR2 and upregulation of 4E-BP1, ACC1, BAX, Cleaved Caspase 7, IGF-1R (Fig. 1A, B). We chose to study IGFBP2 and VEGFR2 that showed a substantial difference in expression profiles between RET knockdown and con shRNA. The validation of RPPA by western blot demonstrated that RET depletion reduced the protein levels of IGFBP2 and VEGFR2 (Fig. 1C). As expected from earlier studies (10), RET-depleted cells showed the upregulated expression of ATF4 in RET-shRNA cells as well as the ATF4 target DDIT3 (CHOP) (Fig. 1C). To examine whether RET regulates IGFBP2 and VEGFR2 at the transcriptional level, we examined the VEGFR2 and IGFBP2 mRNA levels in RET-depleted cells. In two independently selected TT and MZCRC1 cell pools, we found that RET depletion was associated with the downregulation of IGFBP2 and VEGFR2 at the mRNA level (P<0.0001, 2 way ANOVA, Dunnet’s multiple comparison test) (Fig. 1D, E).
Figure 1.
RET knockdown decreased IGFBP2 and VEGFR2 expression. A) Heatmap from reverse-phase protein array analysis showing proteins or phosphoproteins differentially expressed in TT parental cells, control (con) non-target shRNA cells, and two RET-shRNA stable cell lines. Red indicates higher protein levels, and green indicates lower protein levels. B) Differentially expressed proteins in RET-shRNA stable cells using normalized linear values. C) Western blot analysis of indicated proteins in RET-depleted TT cells. D-E) Levels of RET, IGFBP2, and VEGFR2 mRNA in TT RET-shRNA cells in TT and MZCRC1 RET-shRNA cells. Error bars, ±SD (n=3). *p<0.05, ****p<0.0001 (Dunnett’s multiple comparison, unpaired two-tailed t-test).
IGFBP2 promotes cell survival and migration of MTC cells.
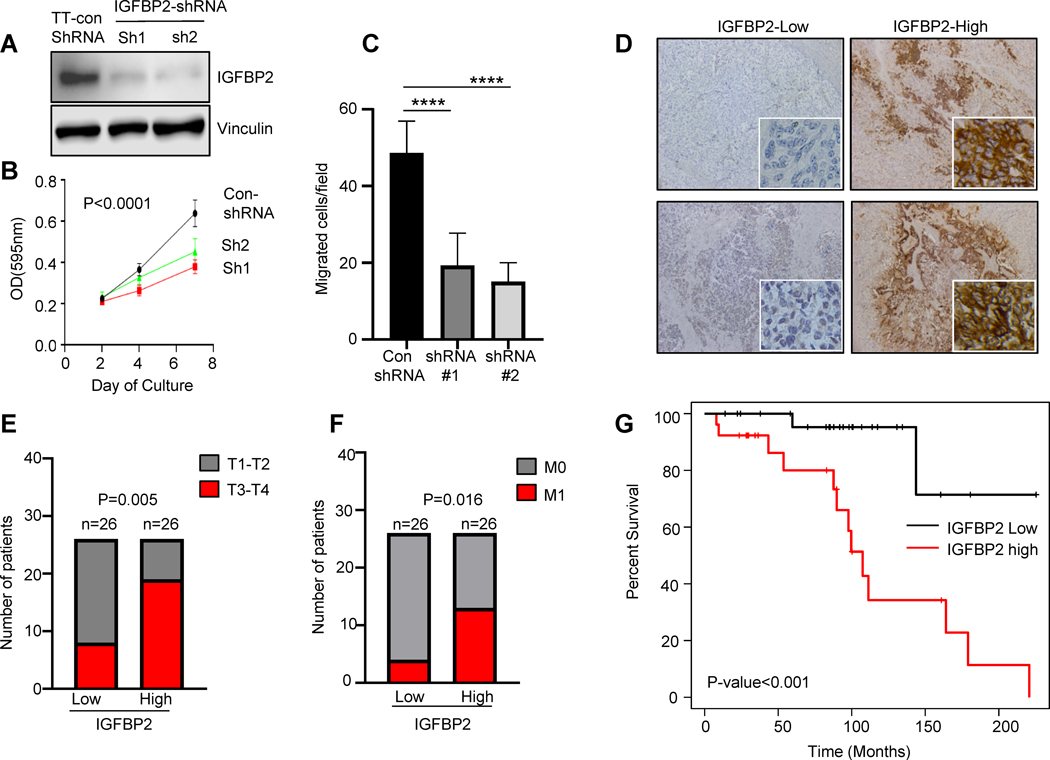
IGFBP2 is elevated in the serum of patients with advanced cancers such as glioblastoma, gastric, prostate, and breast cancer and is associated with progression and metastasis (11–14). To determine the role of endogenous IGFBP2 in the pathogenesis of MTC, we generated stable IGFBP2 knockdown cells using independent short hairpins in both TT and MZCRC1 cell lines. We observed that IGFBP2 knockdown decreased cell survival and migration of TT cells (Fig. 2A, B, C) (P<0.0001, two way ANOVA, Dunnet’s multiple comparison test) and decreased cell survival of MZCRC cells (Supplementary Fig. S1 A, B)
Figure 2.
High IGFBP2 expression is associated with an aggressive phenotype in MTC. A) TT cells were stably transduced with lentiviral shRNA vectors targeting IGFBP2 (sh1 and sh2) or non-target shRNA, and knockdown efficiency was determined by western blot analysis. B) IGFBP2 knockdown decreased the survival of MTC cells. The cell viability of two stable shRNA-IGFBP2 clones was analyzed by MTT assay. Data are representative of three independent experiments: error bars, ±SD (n=3) OD, optical density. C) IGFBP2 knockdown decreased the migration of MTC cells. Data are representative of three independent experiments. Error bars, ±SD (n=3). D) Representative immunohistochemical analysis of IGFBP2 in primary MTC tumors (n=52). Magnification, 20x. E) Association of high IGFBP2 expression with high tumor category (n=52). F) Association of high IGFBP2 expression with metastasis of MTC (n=52). G) High IGFBP2 expression is associated with poor overall survival. Kaplan-Meier survival analysis of 52 MTC primary tumors (P=0.0004, log-rank test). *P<0.05, ***P<0.001,****P<0.0001.
High expression of IGFBP2 is associated with lymph node metastasis and poor prognosis in MTC patients.
A role for IGFBP2 in MTC has not been identified. To investigate the clinical significance of IGFBP2 in MTC, we examined the expression of IGFBP2 in a cohort of 52 MTC tumor tissues by immunohistochemistry (Fig. 2D). The median follow up time was 98.2 (Interquartile range(IQR): 37.9–134.4) months. High IGFBP2 expression ( Hscore>20) was detected in 26 of 52 MTC specimens (50%), of which 7 had a concurrent RET M918T mutation. (Supplementary Table 1). The expression levels of IGFBP2 were increased in patients with pT3 and pT4 primary tumors relative to those with pT1 and pT2 tumors (P=0.005) and increased in M1 (P=0.016) (Fig. 2E, F). The elevated IGFBP2 expression in primary tumors was associated with shorter survival in patients with MTC (HR: 0.12, 95%CI: 0.03–0.53, P=0.005) (Fig. 2G). The median overall survival was 107 months (95% CI: 87.7-not reached ) in patients whose tumors had high levels of IGFBP2 but was undefined in patients whose tumors had low IGFBP2 protein expression. These findings validate the clinical importance of IGFBP2 in MTC and make a compelling argument for future studies to understand the regulation of IGFBP2 expression and the function.
VEGF-mediated cell proliferation is RET-dependent.
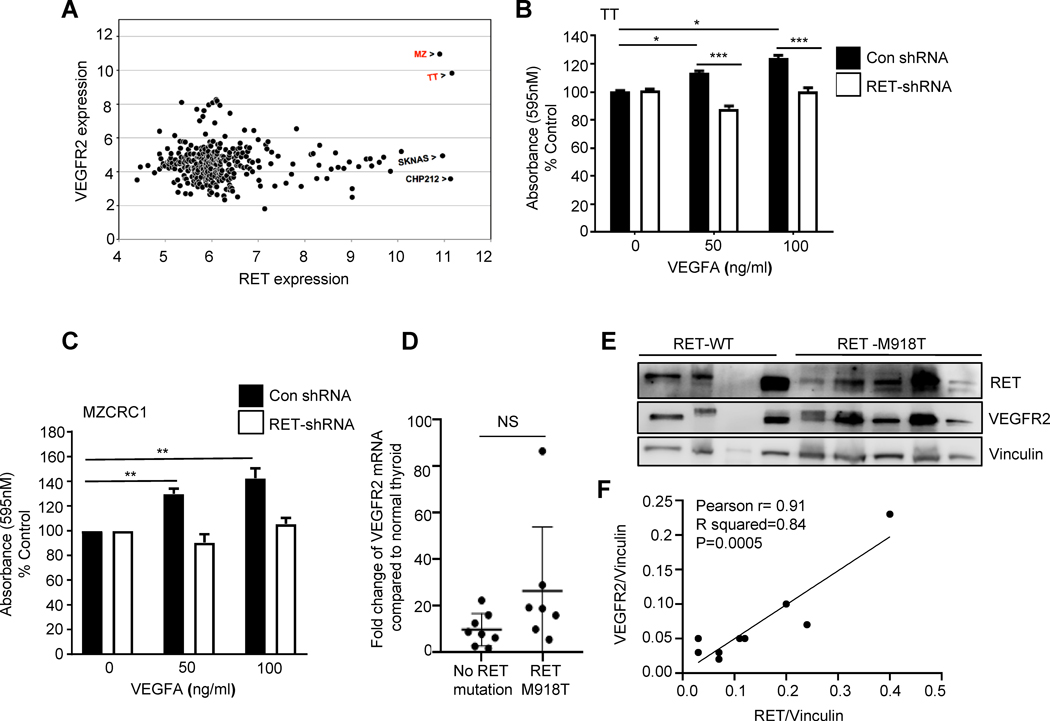
The analysis of VEGFR2 expression levels in the 318 cell lines representing various cancers in the GlaxoSmithKline data set (E-MTAB-37) showed higher expression of VEGFR2 in both MTC cell lines than in any other cell line (Fig. 3A). The RET-mediated upregulation of VEGFR2 suggests that the VEGF signaling pathway plays a biologically relevant role in MTC cell survival. Therefore, we examined the possible existence of an autocrine loop involving VEGFR2 in MTC cells. To this end, control shRNA or RET-shRNA TT and MZCRC1 cells were serum-starved and then treated with an increasing dose of recombinant VEGFA for 72 h. Using the MTT viability assay, we found that VEGF stimulates MTC cell survival by 20–40%, and RET depleted cells did not respond to VEGFA while control cells did (Fig. 3B, C).
Figure 3.
High VEGFR2 expression in MTC tumors is associated with RET expression. A) Analysis of VEGFR2 and RET mRNA expression in the 318 cell lines in the GlaxoSmithKline data set (E-MTAB-37). MZ, MZCRC1. B, C) VEGFA-associated increase in TT and MZCRC1 cell viability was dependent on RET expression. MTT assay was performed in TT and MZCRC1 cells expressing RET- shRNA or control shRNA after VEGFA treatment. TT and MZCRC1cells were serum-starved for 48 h, treated with VEGFA in serum-free media for 72 h at indicated concentrations, and analyzed by MTT assay. The results are the average of two independent experiments performed in six replicates. D) Quantitative real-time PCR was performed using total RNA isolated from 15 primary MTC tumors, with the relative quantities normalized to a normal thyroid sample using a VEGFR2-specific TaqMan probe and GAPDH mRNA as an internal control. Error bars, ±SD (n=3). E) Western blot analysis of MTC tumors with the indicated antibodies (n=9). Vinculin served as a loading control. F) Positive association of RET and VEGFR2 protein levels. Densitometric quantification of RET and VEGFR2 relative to vinculin (Pearson r=0.91, r2=0.84, P=0.0005).
Then, to investigate a potential association between RET and VEGFR2 mRNA levels in primary tumors, we examined the mRNA expression of VEGFR2 in 15 MTC tumor tissues (7 MTC with RET-M918T mutation and 8 MTC without RET-M918T mutation). The range of VEGFR2 mRNA increase was 1.13 −105 fold compared to the normal thyroid, and the mean of VEGFR2 mRNA expression was higher in MTCs with a RET M918T mutation compared with MTC tumors without a RET M918T mutation but did not reach significance (P=0.09) (Fig. 3D).
We analyzed the protein levels of RET and VEGFR2 in 9 primary MTCs with or without RET-M918T mutation. Western blot analysis showed a positive association of RET and VEGFR2 protein levels across the primary tumors regardless of RET mutational status (Pearson r=0.91, r2=0.84, P=0.0005) (Fig. 3E, F); these results suggest that RET promotes VEGFR2 expression in MTC.
ONC201 promotes cell death through inhibition of RET and RET downstream targets IGFBP2 and VEGFR2.
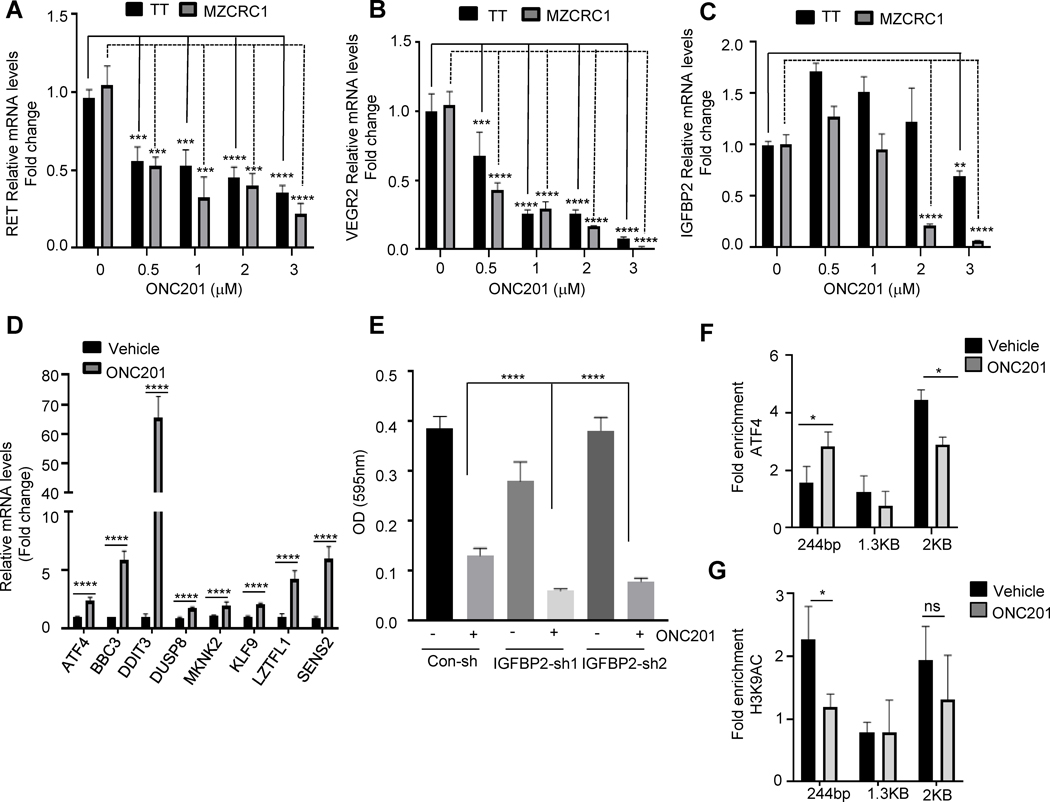
ONC201 is a small-molecule, p53-independent inducer of TRAIL and the integrated stress response pathway, involving ATF4, the transactivator DDIT3, and the TRAIL receptor DR5 with anti-proliferative and pro-apoptotic properties against a wide range of malignant but not normal cells (23). Our laboratory previously identified a crucial role of RET in preventing apoptotic cell death through direct interaction to facilitate degradation of ATF4, a universal stress-responsive gene, and an essential effector of the integrated stress response pathway (10). Therefore, we hypothesized that a small-molecule inducer of ATF4 could re-sensitize cancer cells to stress-induced apoptosis in MTC. ONC201 treatment at various concentrations led to a dose-dependent reduction of TT and MZCRC1 MTC cells’ cell viability as assessed by MTT assay (EC50 5μM) (Fig. 4A). Cell cycle analysis showed a dose-dependent increase in the subG1 population in ONC201-treated TT and MZCRC1 cells (Fig. 4B, Supplementary Fig. S2). ONC201 treatment of MTC cells for 72 h increased cell death, as demonstrated by quantification of cleaved caspase 3 and cleaved PARP (Fig. 4C). As expected, ONC201 increased the protein levels of ATF4 and ATF4 targets, including BBC3 and DDIT3, but decreased RET protein levels and survival factor MCL1, all in a dose-dependent manner in MTC cells (Fig. 4D, E). ONC201 also decreased the expression of IGFBP2 and VEGFR2 in these cells (Fig. 4D, E). To determine whether ONC201 regulates the expression of RET and its targets at the transcriptional level, we examined the effect of this compound on mRNA levels of these genes by quantitative real-time polymerase chain reaction (PCR). We observed that ONC201 decreased the mRNA levels of RET, IGFBP2, and VEGFR2 in a dose-dependent manner, more efficiently in MZCRC1 cells than in TT cells (Fig. 5A-C). Moreover, MZCRC1 cells treated with ONC201 (3 μM) for 72 h had 2.4 fold increased ATF4 mRNA levels (Fig. 5D). The treatment also increased the expression of reported ATF4 target genes (28), including BBC3 (5.9-fold), DDIT3 (65-fold), DUSP8 (1.7-fold), MKNK2 (2-fold), KLF9 (2-fold), LZTFL1 (4-fold), and SESN2 (6-fold).
Figure 4.
ONC201 induces cancer cell death in MTC. A) MTC cells were treated with increasing concentrations (1–5 μM) of ONC201 for 72h, and cell viability was measured by an MTT assay. Data presented are the mean of three independent experiments. Percentage inhibition at each concentration of the ONC201 in TT and MZCRC1 cells is shown. Error bars, ±SD (n=3). B) Cell cycle analysis of MZCRC1 cells treated with increasing concentrations of ONC201 for 72 h. C) TT and MZCRC1 cells treated with ONC201 (3–5 μM) for 72 h, stained with cleaved caspase 3 and cleaved PARP, and analyzed by flow cytometry. D, E) TT cells (D) and MZCRC1 cells (E) treated with ONC201 at indicated concentrations for 72 h and analyzed by western blot with the indicated antibodies.
Figure 5.
ONC201 inhibits RET, IGFBP2, and VEGFR2 transcription. A-C) TT and MZCRC1 cells were treated with ONC201 (0.5–3 μM) for 72 h, and gene expression was measured by quantitative real-time PCR using indicated probes and HPRT as an internal control. Error bars, ±SD (n=3). D) MZCRC1 cells were treated with ONC201 (3 μM) for 72 h and analyzed by quantitative real-time PCR using indicated probes and HPRT as an internal control. Error bars, ±SD (n=3). *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001 by Sidak’s multiple comparison test. Data are representative of three independent experiments. E) IGFBP2 knockdown increased response to ONC201. Stable shRNA-IGFBP2 TT cells were treated with ONC201 (3 μM) and subjected to MTT assay after 72 h. Error bars, ±SD (n=6) OD, optical density. F-G) MZCRC1 cells were treated with ONC201 at 3 μM for 24 h. The chromatin was prepared and precipitated using control (immunoglobulin IgG) or ATF4-specific (F) or H3K9ac-specific antibody (G), and analyzed by quantitative PCR with the indicated primers.
IGFBP2 depletion enhances ONC201-induced apoptosis.
To determine whether IGFBP2 expression was functionally crucial for sensitivity to ONC201, we treated IGFBP2-depleted MTC cells with ONC201 and measured cell survival. IGFBP2 knockdown increased cell sensitivity to ONC201 (Fig.5E). Thus, these results suggest that high expression of IGFBP2 may cause resistance to ONC201-induced cell death.
ATF4 mediates RET regulation of IGFBP2 expression.
The ConTra V3 web server (32) has predicted several binding sites of ATF4 in the IGFBP2 promoter (– 219, –396, –1318, –1433, –1652) (ATF4 binding sequence: GTGACGT[AC][AG]-3’) (Supplementary Fig. S3); we therefore examined whether ATF4 mediates RET regulation of IGFBP2 transcription. To test whether IGFBP2 is a direct target of ATF4, we examined the binding of ATF4 to the IGFBP2 promoter. As shown by chromatin immunoprecipitation assay, using specific primers for several sub-regions covering promoter and enhancer regions of the IGFBP2 promoter showed that ATF4 bound the IGFBP2 promoter and enhancer regions in MTC cells (Fig. 5F). ATF4 occupancy was significantly increased at the IGFBP2 promoter but decreased at the enhancer regions in MZCRC1 cells treated with ONC201 compared with untreated cells (Fig. 5F). The recruitment of H3K9ac to the IGFBP2 promoter was decreased in cells treated with ONC201, suggesting repression of IGFBP2 (Fig. 5G). Therefore, RET may promote IGFBP2 expression through repression of ATF4 transcriptional activity.
ONC201 inhibits tumor growth in mice.
To evaluate the anti-cancer activity of ONC201, we administered ONC201 orally to male Nod-SCID gamma mice bearing TT and MZCRC1 xenograft tumors. TT and MZCRC1 cell xenografts were treated with ONC201 weekly by oral gavage at 120 mg/kg for eight weeks. ONC201 decreased tumor growth by 80%−90% (P<0.0001) (Fig. 6A, B). At the end of treatment, tumors were significantly smaller in ONC201-treated mice compared with control vehicle-treated mice. (Supplementary, Fig. 4A, 4C). We observed no overt toxicity of treatment or significant weight changes during the treatment period (Supplementary Fig. 4B, D). In ONC201-treated tumors, the protein levels of RET, IGFBP2, and VEGFR2 were decreased compared with untreated mice (Fig. 6C, D). The proliferation index, Ki67, was decreased by 30% in ONC201-treated tumors compared with untreated tumors, indicating decreased cell proliferation (Fig. 6E). Immunohistochemistry analysis showed an 80% decrease in IGFBP2 expression in ONC201-treated compared to control tumors (Fig. 6F). CD31 tumor staining showed that the number of vessels was decreased by 63% in ONC201-treated compared with untreated mice (Fig. 6G). These results demonstrate preclinical single-agent efficacy of ONC201 in MTC and downregulation of a key driver of MTC, RET, along with its molecular targets VEGFR2 and IGFBP2.
Figure 6.
ONC201 inhibits tumor growth. A, B) TT and MZCRC1 cells were injected into nude mice (n=8) and were treated with ONC201 (120 mg/kg/week, oral gavage) or vehicle for 8 weeks, and tumor growth was measured every week for 8 weeks. *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001 by the Holm-Sidak method. C) Western blot analysis of the MTC xenograft tumor tissues from the vehicle-treated or ONC201-treated mice with the indicated antibodies. D) Densitometric quantification of RET and VEGFR2 and IGFBP2 relative to vinculin in control and ONC201 treated tumors (unpaired t-test). E) Immunohistologic analysis of the expression of proliferation marker Ki67 quantified as a percentage of Ki67-positive cells for each xenograft tumor (n=6), magnification 20x. F) Immunohistologic analysis of the expression of IGFBP2, quantified as H-score (% staining × intensity) for each xenograft tumor (n=6), magnification 20x. G) Immunohistologic analysis of the expression of angiogenesis marker CD31, quantified as the number of vessels per field in each xenograft tumor (n=6), magnification 20x.
Discussion
In the present study, our results indicate that RET protooncogene promotes the expression of VEGFR2 and IGFBP2 in medullary thyroid cancer. We demonstrate that IGFBP2 promotes cell survival and migration of MTC cells and that high IGFBP2 expression is associated with poor overall survival, higher T category, and distant metastasis, suggesting a central role in the pathogenesis of MTC. Also, our findings demonstrate that small-molecule ONC201 inhibits RET, VEGFR2, and IGFBP2 expression leading to increased apoptotic cell death and inhibition of tumor growth.
Increasing evidence suggests that IGFBP2 promotes cell survival and an aggressive phenotype in many malignancies (33). Our data show that RET promotes IGFBP2 expression, which, in turn, contributes to increased cell survival, progression, and resistance to therapy. These results suggest that IGFBP2, known to be elevated in patients with advanced cancers and associated with progression, may serve as a novel biomarker of aggressive MTC that could be quantified in serum or tumor tissues. IGFBP2 may act in other ways, as it is translocated into the nucleus and binds to the VEGF gene’s promoter region, leading to increased VEGF mRNA expression (34). Das et al. reported that secreted IGFBP2 activated the PI3K/AKT pathway, leading to the upregulation of the proangiogenic factor VEGFA thereby triggering angiogenesis (35). Moreover, IGFBP2 promotes vasculogenic mimicry formation, i.e., the fluid-conducting channels formed by aggressive gliomas (36). We found that VEGFA increased the survival of MTC cells and that this increase was abrogated by depletion of RET, suggesting the involvement of an autocrine loop with VEGFA and VEGFR2, leading to increased cell survival, cell proliferation, and angiogenesis in MTC tumors.
As noted earlier, EGFR and VEGFR2 are upregulated in metastatic MTC compared with primary tumors (19). Our studies showed a positive association between RET protein levels and VEGFR2 protein levels in MTC tumors, confirming our data in MTC cell lines showing RET depletion in both TT(RET-W634T) and MZCRC1(RET-M918T) downregulates VEGFR2 mRNA levels suggesting that RET activation promotes VEGFR2 transcription.
The current standard of care for MTC is a combination of surgery and multi tyrosine kinase inhibitors. These TKIs tend to be static rather than cidal, leading to secondary RET mutations (such as RET V804) that confer resistance (37). While there is clear evidence that both first and second generations of TKIs cause tumor size reduction with increased MTC cell death, these effects are invariably incomplete leading to tumor regrowth after TKI discontinuation. Thus, a novel compound that strongly downregulates RET expression could be beneficial for refractory MTC. Furthermore, TKIs that target VEGFR2 selectively with little RET activity (e.g., axitinib) have significant efficacy in MTC, suggesting that inhibition of VEGF receptor signaling contributes to anti-MTC response (38). Our results establish a link between RET activity and expression of VEGFR2, identifying a regulatory loop between RET and VEGFR2 expression. To date, all multi-kinase inhibitors, including cabozantinib, vandetanib, mostenib, nintedanib, inhibit RET, or VEGFR2 activity without affecting RET or VEGFR2 protein levels (39–41). However, dinaciclib, a CDK1/2/5/9 inhibitor that reduces CDK9, is shown to reduce RET protein and RET mRNA levels and induce apoptosis in MTC cells (42).
ONC201 is currently in early-phase clinical trials for several cancers, including leukemia, lymphoma, glioblastoma, and prostate cancer, without severe toxicity reported to date (20). ONC201 has many favorable characteristics for an anti-cancer drug, including oral, infrequent administration, and an excellent safety profile. ONC201 activates the integrated stress response pathway through ATF4 and its target DDIT3 (23, 43, 44). We have previously shown that RET promotes cell survival through phosphorylation-dependent degradation of ATF4 and that overexpression of ATF4 leads to RET ubiquitination (30, 45). Here, we showed that ONC201 strongly increased the transcription of ATF4 and ATF4 targets, including DDIT3, BBC3, DUSP8, MKNK2, KLF9, LZTFL1, and SESN2 with known pro-apoptotic and tumor suppressor function (46–48). We showed that ATF4 recruits to the promoter and enhancer region of the IGFBP2 gene and ATF4 occupancy at the IGFBP2 promoter are enhanced in MTC cells treated with ONC201 compared to untreated cells, whereas H3K9Ac recruitment was significantly decreased, suggesting that ATF4 may repress IGFBP2 transcription. Thus, RET may promote IGFBP2 transcription through repression of ATF4 transcriptional activity.
Moreover, targeting RET and VEGFR2 at the transcriptional level by ONC201 may represent a novel, and potent therapeutic approach in both RET mutated or non-mutated tumors. MTC is a highly vascular tumor in a growth factor–rich microenvironment, and RET inhibition may have profound effects on VEGF-dependent biological processes. Moreover, ONC201 may decrease blood vessels’ growth in MTC by inhibiting VEGFR2 expression and disturbing a VEGF/VEGFR2 autocrine loop. In summary, our results identified a novel ONC201 mechanism of action through regulation of RET and its targets, VEGFR2 and IGFBP2; this mechanism can be translated directly into the clinical research goals and provide a promising strategy for treatment in MTC.
Supplementary Material
Acknowledgments
We thank Krishna Sinha for the helpful discussion. We thank Sarah Bronson in Scientific Publications, Research Medical Library, at The University of Texas MD Anderson Cancer Center for editing the manuscript.
Financial Support:
This work was supported by the National Institutes of Health thrxough grants P50CA168505/DRP (to R.B.Y.) and a Cancer Center Support Grant (CA016672).
Footnotes
Conflict of interest statement: Rohinton Tarapore and Joshua E. Allen have employment relationships with Oncoceutics. Steven Sherman is a consultant to LOXO Oncology. All other authors have declared that no conflicts of interest exist.
References
- 1.Cote GJ, Grubbs EG, Hofmann MC. Thyroid C-Cell Biology and Oncogenic Transformation. Recent Results Cancer Res. 2015;204:1–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ball DW. Medullary thyroid cancer: monitoring and therapy. Endocrinol Metab Clin North Am. 2007;36(3):823–37, viii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Santoro M, Carlomagno F. Central role of RET in thyroid cancer. Cold Spring Harb Perspect Biol. 2013;5(12):a009233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cote GJ, Evers C, Hu MI, Grubbs EG, Williams MD, Hai T, et al. Prognostic Significance of Circulating RET M918T Mutated Tumor DNA in Patients With Advanced Medullary Thyroid Carcinoma. J Clin Endocrinol Metab. 2017;102(9):3591–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wells SA Jr., Robinson BG, Gagel RF, Dralle H, JA Fagin, M Santoro, et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol. 2012;30(2):134–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kurzrock R, Sherman SI, Ball DW, Forastiere AA, Cohen RB, Mehra R, et al. Activity of XL184 (Cabozantinib), an oral tyrosine kinase inhibitor, in patients with medullary thyroid cancer. J Clin Oncol. 2011;29(19):2660–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Resteghini C, Cavalieri S, Galbiati D, Granata R, Alfieri S, Bergamini C, et al. Management of tyrosine kinase inhibitors (TKI) side effects in differentiated and medullary thyroid cancer patients. Best Pract Res Clin Endocrinol Metab. 2017;31(3):349–61. [DOI] [PubMed] [Google Scholar]
- 8.Wirth LJ, Sherman E, Robinson B, Solomon B, Kang H, Lorch J, et al. Efficacy of Selpercatinib in RET-Altered Thyroid Cancers. N Engl J Med. 2020;383(9):825–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Subbiah V, Yang D, Velcheti V, Drilon A, Meric-Bernstam F. State-of-the-Art Strategies for Targeting RET-Dependent Cancers. J Clin Oncol. 2020;38(11):1209–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bagheri-Yarmand R, Sinha KM, Gururaj AE, Ahmed Z, Rizvi YQ, Huang SC, et al. A novel dual kinase function of the RET protooncogene negatively regulates activating transcription factor 4-mediated apoptosis. J Biol Chem. 2015;290(18):11749–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hur H, Yu EJ, Ham IH, Jin HJ, Lee D. Preoperative serum levels of insulin-like growth factor-binding protein 2 predict prognosis of gastric cancer patients. Oncotarget. 2017;8(7):10994–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mehrian-Shai R, Chen CD, Shi T, Horvath S, Nelson SF, Reichardt JK, et al. Insulin growth factor-binding protein 2 is a candidate biomarker for PTEN status and PI3K/Akt pathway activation in glioblastoma and prostate cancer. Proc Natl Acad Sci U S A. 2007;104(13):5563–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Das SK, Pradhan AK, Bhoopathi P, Talukdar S, Shen XN, Sarkar D, et al. The MDA-9/Syntenin/IGF1R/STAT3 Axis Directs Prostate Cancer Invasion. Cancer research. 2018;78(11):2852–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abdolhoseinpour H, Mehrabi F, Shahraki K, Khoshnood RJ, Masoumi B, Yahaghi E, et al. Investigation of serum levels and tissue expression of two genes IGFBP-2 and IGFBP-3 act as a potential biomarker for predicting the progression and survival in patients with glioblastoma multiforme. J Neurol Sci. 2016;366:202–6. [DOI] [PubMed] [Google Scholar]
- 15.Holmes KM, Annala M, Chua CY, Dunlap SM, Liu Y, Hugen N, et al. Insulin-like growth factor-binding protein 2-driven glioma progression is prevented by blocking a clinically significant integrin, integrin-linked kinase, and NF-kappaB network. Proceedings of the National Academy of Sciences of the United States of America. 2012;109(9):3475–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gao S, Sun Y, Zhang X, Hu L, Liu Y, Chua CY, et al. IGFBP2 Activates the NF-kappaB Pathway to Drive Epithelial-Mesenchymal Transition and Invasive Character in Pancreatic Ductal Adenocarcinoma. Cancer research. 2016;76(22):6543–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Strub T, Ghiraldini FG, Carcamo S, Li M, Wroblewska A, Singh R, et al. SIRT6 haploinsufficiency induces BRAF(V600E) melanoma cell resistance to MAPK inhibitors via IGF signalling. Nat Commun. 2018;9(1):3440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Papotti M, Olivero M, Volante M, Negro F, Prat M, Comoglio PM, et al. Expression of Hepatocyte Growth Factor (HGF) and its Receptor (MET) in Medullary Carcinoma of the Thyroid. Endocr Pathol. 2000;11(1):19–30. [DOI] [PubMed] [Google Scholar]
- 19.Rodriguez-Antona C, Pallares J, Montero-Conde C, Inglada-Perez L, Castelblanco E, Landa I, et al. Overexpression and activation of EGFR and VEGFR2 in medullary thyroid carcinomas is related to metastasis. Endocr Relat Cancer. 2010;17(1):7–16. [DOI] [PubMed] [Google Scholar]
- 20.Allen JE, Kline CL, Prabhu VV, Wagner J, Ishizawa J, Madhukar N, et al. Discovery and clinical introduction of first-in-class imipridone ONC201. Oncotarget. 2016;7(45):74380–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chi AS, Tarapore RS, Hall MD, Shonka N, Gardner S, Umemura Y, et al. Pediatric and adult H3 K27M-mutant diffuse midline glioma treated with the selective DRD2 antagonist ONC201. J Neurooncol. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wagner J, Kline CL, Pottorf RS, Nallaganchu BR, Olson GL, Dicker DT, et al. The angular structure of ONC201, a TRAIL pathway-inducing compound, determines its potent anti-cancer activity. Oncotarget. 2014;5(24):12728–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kline CL, Van den Heuvel AP, Allen JE, Prabhu VV, Dicker DT, El-Deiry WS. ONC201 kills solid tumor cells by triggering an integrated stress response dependent on ATF4 activation by specific eIF2alpha kinases. Sci Signal. 2016;9(415):ra18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Allen JE, Krigsfeld G, Mayes PA, Patel L, Dicker DT, Patel AS, et al. Dual inactivation of Akt and ERK by TIC10 signals Foxo3a nuclear translocation, TRAIL gene induction, and potent antitumor effects. Science translational medicine. 2013;5(171):171ra17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhu W, Hai T, Ye L, Cote GJ. Medullary thyroid carcinoma cell lines contain a self-renewing CD133+ population that is dependent on ret protooncogene activity. J Clin Endocrinol Metab. 2010;95(1):439–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cooley LD, Elder FF, Knuth A, Gagel RF. Cytogenetic characterization of three human and three rat medullary thyroid carcinoma cell lines. Cancer Genet Cytogenet. 1995;80(2):138–49. [DOI] [PubMed] [Google Scholar]
- 27.Siwak DR, Li J, Akbani R, Liang H, Lu Y. Analytical Platforms 3: Processing Samples via the RPPA Pipeline to Generate Large-Scale Data for Clinical Studies. Adv Exp Med Biol. 2019;1188:113–47. [DOI] [PubMed] [Google Scholar]
- 28.Bagheri-Yarmand R, Sinha KM, Li L, Lu Y, Cote GJ, Sherman SI, et al. Combinations of Tyrosine Kinase Inhibitor and ERAD Inhibitor Promote Oxidative Stress-Induced Apoptosis through ATF4 and KLF9 in Medullary Thyroid Cancer. Mol Cancer Res. 2019;17(3):751–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sinha KM, Bagheri-Yarmand R, Lahiri S, Lu Y, Zhang M, Amra S, et al. Oncogenic and osteolytic functions of histone demethylase NO66 in castration-resistant prostate cancer. Oncogene. 2019. [DOI] [PubMed] [Google Scholar]
- 30.Bagheri-Yarmand R, Williams MD, Grubbs EG, Gagel RF. ATF4 Targets RET for Degradation and Is a Candidate Tumor Suppressor Gene in Medullary Thyroid Cancer. J Clin Endocrinol Metab. 2017;102(3):933–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Annals of surgical oncology. 2010;17(6):1471–4. [DOI] [PubMed] [Google Scholar]
- 32.Kreft L, Soete A, Hulpiau P, Botzki A, Saeys Y, De Bleser P. ConTra v3: a tool to identify transcription factor binding sites across species, update 2017. Nucleic acids research. 2017;45(W1):W490–W4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yao X, Sun S, Zhou X, Guo W, Zhang L. IGF-binding protein 2 is a candidate target of therapeutic potential in cancer. Tumour biology : the journal of the International Society for Oncodevelopmental Biology and Medicine. 2016;37(2):1451–9. [DOI] [PubMed] [Google Scholar]
- 34.Azar WJ, Azar SH, Higgins S, Hu JF, Hoffman AR, Newgreen DF, et al. IGFBP-2 enhances VEGF gene promoter activity and consequent promotion of angiogenesis by neuroblastoma cells. Endocrinology. 2011;152(9):3332–42. [DOI] [PubMed] [Google Scholar]
- 35.Das SK, Bhutia SK, Azab B, Kegelman TP, Peachy L, Santhekadur PK, et al. MDA-9/syntenin and IGFBP-2 promote angiogenesis in human melanoma. Cancer Res. 2013;73(2):844–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu Y, Li F, Yang YT, Xu XD, Chen JS, Chen TL, et al. IGFBP2 promotes vasculogenic mimicry formation via regulating CD144 and MMP2 expression in glioma. Oncogene. 2019;38(11):1815–31. [DOI] [PubMed] [Google Scholar]
- 37.Liu X, Shen T, Mooers BHM, Hilberg F, Wu J. Drug resistance profiles of mutations in the RET kinase domain. Br J Pharmacol. 2018;175(17):3504–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cohen EE, Rosen LS, Vokes EE, Kies MS, Forastiere AA, Worden FP, et al. Axitinib is an active treatment for all histologic subtypes of advanced thyroid cancer: results from a phase II study. J Clin Oncol. 2008;26(29):4708–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pozo K, Zahler S, Ishimatsu K, Carter AM, Telange R, Tan C, et al. Preclinical characterization of tyrosine kinase inhibitor-based targeted therapies for neuroendocrine thyroid cancer. Oncotarget. 2018;9(102):37662–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Coxon A, Bready J, Kaufman S, Estrada J, Osgood T, Canon J, et al. Anti-tumor activity of motesanib in a medullary thyroid cancer model. J Endocrinol Invest. 2012;35(2):181–90. [DOI] [PubMed] [Google Scholar]
- 41.Bentzien F, Zuzow M, Heald N, Gibson A, Shi Y, Goon L, et al. In vitro and in vivo activity of cabozantinib (XL184), an inhibitor of RET, MET, and VEGFR2, in a model of medullary thyroid cancer. Thyroid. 2013;23(12):1569–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Valenciaga A, Saji M, Yu L, Zhang X, Bumrah C, Yilmaz AS, et al. Transcriptional targeting of oncogene addiction in medullary thyroid cancer. JCI insight. 2018;3(16). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kline CLB, Ralff MD, Lulla AR, Wagner JM, Abbosh PH, Dicker DT, et al. Role of Dopamine Receptors in the Anticancer Activity of ONC201. Neoplasia. 2018;20(1):80–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ishizawa J, Zarabi SF, Davis RE, Halgas O, Nii T, Jitkova Y, et al. Mitochondrial ClpP-Mediated Proteolysis Induces Selective Cancer Cell Lethality. Cancer Cell. 2019;35(5):721–37 e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Luo J, Xia Y, Yin Y, Luo J, Liu M, Zhang H, et al. ATF4 destabilizes RET through nonclassical GRP78 inhibition to enhance chemosensitivity to bortezomib in human osteosarcoma. Theranostics. 2019;9(21):6334–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wei Q, Chen ZH, Wang L, Zhang T, Duan L, Behrens C, et al. LZTFL1 suppresses lung tumorigenesis by maintaining differentiation of lung epithelial cells. Oncogene. 2016;35(20):2655–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maimon A, Mogilevsky M, Shilo A, Golan-Gerstl R, Obiedat A, Ben-Hur V, et al. Mnk2 alternative splicing modulates the p38-MAPK pathway and impacts Ras-induced transformation. Cell Rep. 2014;7(2):501–13. [DOI] [PubMed] [Google Scholar]
- 48.Mannava S, Zhuang D, Nair JR, Bansal R, Wawrzyniak JA, Zucker SN, et al. KLF9 is a novel transcriptional regulator of bortezomib- and LBH589-induced apoptosis in multiple myeloma cells. Blood. 2012;119(6):1450–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.