Abstract
The growing increase in antibiotic-resistant bacteria has led to the search for new antibacterial agents capable of overcoming the resistance problem. In recent years, nanoparticles (NPs) have been increasingly used to target bacteria as an alternative to antibiotics. The most promising nanomaterials for biomedical applications are metal and metal oxide NPs, due to their intrinsic antibacterial activity. Although NPs show interesting antibacterial properties, the mechanisms underlying their action are still poorly understood, limiting their use in clinical applications. In this review, an overview of the mechanisms underlying the antibacterial activity of metal and metal oxide NPs will be provided, relating their efficacy to: (i) bacterial strain; (ii) higher microbial organizations (biofilm); (iii) and physico-chemical properties of NPs. In addition, bacterial resistance strategies will be also discussed to better evaluate the feasibility of the different treatments adopted in the clinical safety fields. Finally, a wide analysis on recent biomedical applications of metal and metal oxide NPs with antibacterial activity will be provided.
Keywords: antibacterial mechanisms, bacterial resistance, biofilm, metal and metal oxide nanoparticles, nanotechnology, nanomedicine
1. Introduction
The excessive and improper use of antibiotics, causing antimicrobial resistance, has become one of the most significant problems in the clinical field in recent years [1].
From the first documented case [2] to date, we are observing a growing increase in bacteria resistant to common antibiotics, with the consequent spread of so-called multi-drug-resistant (MDR) strains [3]. The Centers for Disease Control and Prevention (CDC) have estimated that over 2 million infections and 23,000 deaths associated with MDR bacteria occur annually [1]. These pathogenic strains belong to the group named ESKAPE and include Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacter species [4].
Antibiotic resistance is probably due to the misuse and overuse of antibiotics, as well as poor infection prevention and control [5]. In the literature, several antimicrobial resistance mechanisms are reported, including: (i) limiting the uptake of a drug; (ii) modifying a drug target; (iii) inactivating a drug; and (iv) active drug efflux [6]. These mechanisms, that may be native or acquired, allow the survival of the resistant strains and their spread, with the consequent failure of antibacterial therapies.
Gram-negative and Gram-positive bacterial strains exhibit different mechanisms of antimicrobial resistance, mainly due to differences in cell wall structure. Specifically, while Gram-negative bacteria limit the uptake of a drug, Gram-positive bacteria, missing LPS in the outer membrane, inactivate the drug [7,8].
In recent years, several strategies to overcome antimicrobial resistance have been developed in order to obtain new broad-spectrum drugs with a better half-life [9]. Among these approaches, the possibility of using nanomaterials as new non-traditional antimicrobials agents has been investigated. In vitro studies have demonstrated that nanomaterials exhibit toxic effects against several bacterial strains, suggesting their feasibility for biomedical applications, including drug delivery and tissue engineering [10,11,12]. Among the most promising nanomaterials are metal and metal oxide nanoparticles (NPs).
The antibacterial activity associated with metal NPs has long been known; however, their mechanisms are still poorly understood. In recent years, several antibacterial mechanisms, ascribable to both physical damage and chemical interactions, have been proposed, including ion leaching, ion dissolution, and/or reactive oxygen species (ROS) production, involving the loss of cell wall and cell membrane integrity and, consequently, the interference with some metabolic pathways essential for bacterial viability [13,14].
Furthermore, some requirements are crucial for the antibacterial activity of metal NPs, such as size, shape, surface/volume ratio and surface functionalization, mainly affecting the biocompatibility and bactericidal properties. In this context, nanotechnology represents a powerful tool to design NPs with appropriate physico-chemical properties in order to reduce their cytotoxic effect and the risk related to their use in biomedical applications [15,16,17,18].
This review aims to provide an overview of metal NP antibacterial mechanisms related to different bacterial species, higher microbial organizations (biofilm), and the physico-chemical properties of NPs themselves. In addition, bacterial resistance strategies are also discussed to better evaluate the feasibility of different treatments adopted in the clinical and human safety fields. Finally, a wide analysis of recent biomedical applications of antibacterial NPs will be provided.
2. Gram-Positive and Gram-Negative Bacteria and Biofilm
Although metallic NPs have demonstrated broad-spectrum antibacterial properties, the composition and organization of the bacterial cell wall can influence their bactericidal efficiency. In addition, higher microbial organizations such as biofilm can hinder the diffusion, subsequently increasing the lethal dose compared to planktonic cells.
2.1. Gram-Positive and Gram-Negative Bacteria
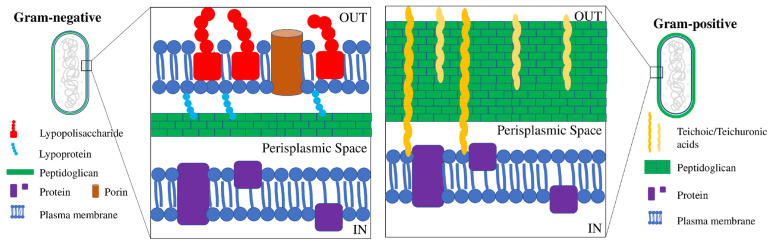
Except for a few species, most bacteria have an outer protective cell wall and membrane and, depending on the cell wall composition, they can be classified as “Gram-positive” or “Gram-negative”. Gram-positive and Gram-negative bacteria can be differentiated by Gram-staining (Figure 1).
Figure 1.
Schematic structure of Gram-negative and Gram-positive cell walls. Gram-negative bacteria have an inner and an outer cell membrane (double lipid bilayer) and only a thin layer of peptidoglycan in the periplasmic space, whereas Gram-positive bacteria show only one lipid plasma membrane and a thick peptidoglycan layer interlinked with teichoic and lipoteichoic acids.
Gram-positive bacteria contain a uniform and relatively thick (20–80 nm) wall, consisting of numerous layers of peptidoglycan, crisscrossed by teichoic and teichuronic acids (polymers of alcohols and phosphates). As a result, they have a very polar structure that only allows the permeation of hydrophilic compounds. On the other hand, Gram-negative bacteria contain a very thin (<10 nm) and complex wall, in which peptidoglycan is surrounded by an outer membrane containing an internal phospholipid sheet and an external lipopolysaccharide (LPS). The presence of the outer membrane makes the wall highly selective, also hindering the passage of small hydrophilic molecules, including water [19,20]. Since Gram-negative and Gram-positive bacteria display a different structural organization, they respond differently to antimicrobial agents, including metal NPs. Several studies, in fact, have demonstrated that Gram-positive bacteria are more resistant to NPs than Gram-negative bacteria, because their different arrangement and structure facilitate the entrance of released ions [21,22,23,24,25,26]. Furthermore, it has also been demonstrated that metal NPs can interact with the repeated units of amino acids and carbohydrates of the peptidoglycan layer. Therefore, since Gram-positive walls contain a greater amount of peptidoglycan than Gram-negative walls, Gram-positive bacteria have a higher resistance to damage [27,28]. For the same reasons, Gram-positive bacteria are considerably more resistant to damage by metal ions, due to their trapping by negatively charged peptidoglycan [24]. In addition, it has been reported that the different susceptibility of Gram-negative bacteria to NPs could also be due to the presence of LPS molecules, which increase the negative charge of the cell membrane compared to Gram-positive bacteria [29].
Recent evidence has also suggested that the mosaic structure of LPS molecules in Gram-negative bacteria make some regions more negatively charged, and thus NPs (positively charged) tend to aggregate in these areas, leading to a localized toxic effect [30]. Differently, ROS produced outside the bacterial cell induce the same antibacterial activity in both Gram-positive and Gram-negative bacteria. This can be attributed to the fact that these radicals, mainly hydroxyl radicals, are negatively charged and so can hardly penetrate into the cell membrane [31].
2.2. Biofilm
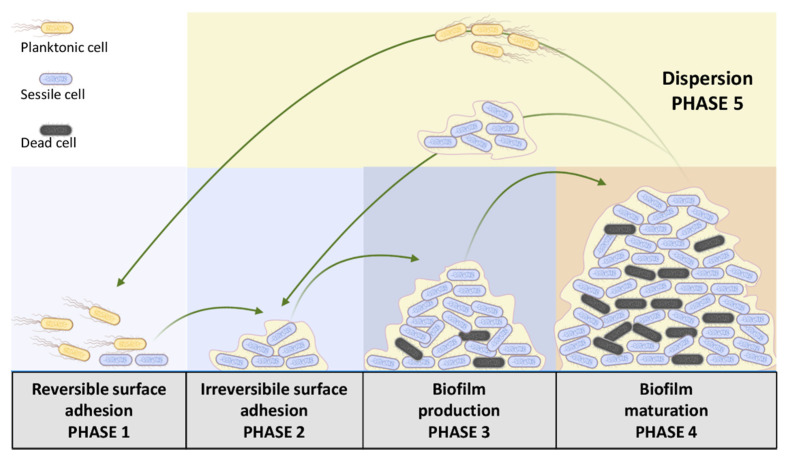
Microorganisms are able to organize themselves into a higher life structure and grow adhered to almost every surface, forming architecturally complex communities, termed biofilms [32]. These structures consist of bacteria incorporated in an extracellular polymer matrix (polysaccharides, proteins, glycopeptides, nucleic acids, and lipids) whose primary function is to protect bacteria from all unfavorable chemical–physical agents, including antibiotics [33]. Figure 2 reports the several steps of biofilm synthesis and maturation [34].
Figure 2.
Schematic representation of cyclic biofilm formation, from reversible adhesion of bacteria to biofilm dispersion, consisting of the evacuation of matrix–bacteria aggregates.
The process starts with the transition from reversible surface adhesion (phase 1) to the irreversible one (phase 2). In this transition, some genetic pathways are blocked and replaced with those related to the production of the main components of the biofilm matrix (phase 3) and its subsequent maturation (phase 4). The final step of the cyclic biofilm formation includes the dispersion of both planktonic cells and full bacteria–matrix aggregates (phase 5). Recent evidence has shown that biofilm-like aggregates can also form in the absence of surfaces and attach at a later time [35]. Since the extracellular matrix acts as a filter, the antibacterial success of NPs depends almost exclusively on their interactions with this polymeric matrix. In this context, NP–matrix interactions include three consequential phases that lead to the destruction of the extracellular matrix and bacteria killing: (i) NPs’ adhesion to the matrix, (ii) NPs’ inclusion within it, and (iii) lethal interaction between bacteria and NPs. Although antibacterial mechanisms of metal NPs are identical to those on planktonic ones, biofilms offer greater resistance by limiting the diffusion of NPs and their contact with biofilm cells [36,37,38]. Surface-covering strategies using NPs can act on the initial stages of bacterial adhesion, effectively providing an excellent biofilm inhibition strategy. An example is represented in the surface coating of AgNPs, which is able to prevent biofilm formation from both Gram-negative and Gram-positive bacteria [39,40]. Similar results were also obtained with the zinc oxide (ZnO) NP coating [41,42].
3. Influence of Metal NPs’ Physico-Chemical Properties on Antibacterial Activity
Physico-chemical features of metal NPs are critical factors for their antimicrobial and antibiofilm activity. Heavy metals, with densities greater than 5 g/cm3, have excellent antimicrobial activity [43]. At the nanoscale, the physical and chemical properties of metals change dramatically from that of the bulk material due to size and shape effects, as well as the high surface area to volume ratio of nanomaterials [44]. Consequently, several properties such as ion release, hardness, plasmon and super-paramagnetism are affected [45,46,47]. Moreover, the response to external stimuli—such as light in the case of photocatalytic and photothermal activity [48,49], and magnetism in the case of magnetically induced hyperthermia activity [50,51]—is modified compared to the bulk metal.
3.1. Size
Typically, smaller NPs have higher antibacterial activity due to their ability to penetrate a cell and to inhibit bacteria growth [52,53,54,55,56,57,58]. Moreover, smaller NPs have a relatively large surface area/volume ratio compared to larger NPs, favoring ROS production. Skomorokhova et al. tested the antibacterial activity of AgNPs of three different sizes against Escherichia coli in their study, demonstrating that larger particles were less effective as antibacterial agents than smaller NPs, and that the antibacterial activity for particles of the same size was strictly dose- and time-dependent [59]. Similarly, Korshed et al. found that the bactericidal effects were inversely correlated to the NPs’ size [60]. Furthermore, they showed that smaller AgNPs induced more ROS production than larger AgNPs. In another study, it was shown that AgNPs of 18 nm in size were more toxic than those of 80 nm in water, but their toxicity declined to a similar level in the PBS buffer [52]. Zare et al. synthesized ZnONPs of various sizes and morphologies and found that these NPs displayed very good antibacterial and antioxidant activity that was size- and morphology-dependent [61]. Adams et al. found that palladium NPs (PdNPs) with smaller diameter, i.e., 2.0 ± 0.1 nm, exhibited higher toxicity relative to the 2.5 ± 0.2 nm and 3.1 ± 0.2 nm NPs. Furthermore, they demonstrated that Gram-negative E. coli required higher concentrations and longer exposure times of PdNPs to inhibit bacteria growth compared to the Gram-positive S. aureus [62].
3.2. Shape
NPs can exhibit different shapes, including spherical, dots, wires, rods, stars, flowers and 2D materials, affecting their antibacterial activity [16,63,64,65,66]. Although NPs’ spherical shape is the most common, nanocubes and nanorods are more effective than other shapes, possibly due to the exposed planes and to the oxidation levels of the metals. Specifically, it has been suggested that less stable planes require less energy to form oxygen vacancies, linking the bactericidal activity of the NPs to the stability of the planes [14]. Wang et al. evaluated CeO2 and Ag/CeO2 NPs with different shapes and demonstrated that nanocubes and nanorods displayed higher bactericidal activities than other shapes due to their exposed crystal planes and oxidation ability [14]. Hong et al. showed that Ag nanowires displayed a lower antibacterial activity compared to Ag nanocubes and nanospheres, due to their lower interaction with bacterial cells [63]. The same authors found that silver nanocubes had better antimicrobial properties than nanospheres, due to the larger contact areas and higher reactive facets. In their paper, Franco et al. developed a magnesium–hydroxyapatite (Mg-HA) scaffold functionalized with Au nanorods (AuNr) and showed that the presence of AuNr induced 100% bacteria reduction after 24 h for both S. aureus and E. coli [16].
Furthermore, it has been also observed that the presence of corners, edges or defects increases NPs’ toxicity, probably due to the increased surface area, affecting their adsorption, binding, or ROS production. Huynh et al. found that gold nanostars can be used instead of antibiotics in acne treatment due to their strong bactericidal activity against Propionibacterium acne [64]. Silver nanoflowers coupled with a low dose of antibiotics led to the complete eradication of drug-resistant bacteria, probably due to the release of ROS and antibiotic uptake induction mainly mediated by NPs [65]. This evidence suggests that the shape of NPs has a crucial role in affecting antimicrobial properties.
3.3. Surface Charge
Another important factor for NPs’ antibacterial activity is given from their surface charge. It has been shown that NPs with positive charge display higher toxicity due to their electrostatic interaction with the negative charge of the bacterial cell wall [29,55,67,68,69]. Li et al. showed that magnetic NPs with a positive charge (NP+) efficiently attracted over 90% of E. coli, while negatively charged magnetic NPs (NP−) did not show any affinities. These results suggest that NPs+ have good potential to capture bacteria via electrostatic attraction [68]. Abbaszadegan et al. compared the antibacterial efficiency of three different AgNPs that were positively, negatively, and neutrally charged. They found that positively charged NPs showed the highest bactericidal activity, while the negative ones showed the lowest [29]. El Badawy et al. evaluated the toxicity of four AgNPs with several surface charges, ranging from highly negative to highly positive. Their results showed that AgNPs exhibited surface charge-dependent toxicity on the bacterial species investigated [52,70]. In another study, it was demonstrated that positively charged Ag–polyethylenimine (BPEI) NPs tightly adhered to the bacterial surface, while no attachment was observed for negatively charged citrate–Ag NPs [55]. In contrast, Agnihotri et al. found that negatively charged AgNPs (citrate-stabilized) exhibited a strong antibacterial activity against E. coli and S. aureus. Their results also indicated that the antibacterial efficacy increased with lowering particle size [71].
4. Antibacterial Mechanisms
In this section, the antibacterial mechanisms of metal NPs including (i) physical interactions, (ii) ion leaching and dissolution, and (iii) ROS production will be analyzed.
4.1. Physical Interactions
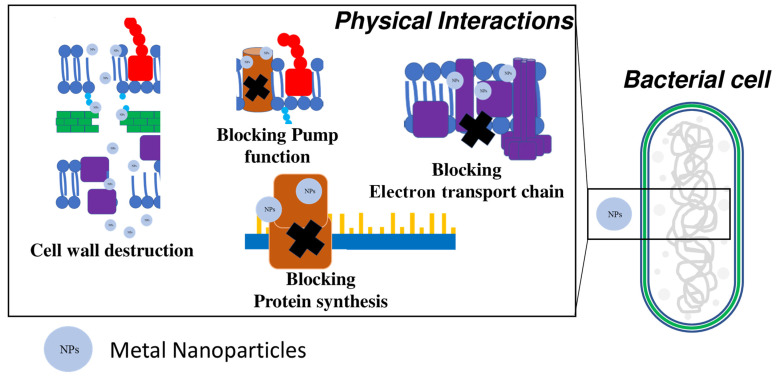
It has been already demonstrated that metal nanomaterials can interact physically with the cell membrane/wall or with intracellular components [72] (Figure 3).
Figure 3.
Schematic description and targets of antibacterial mechanisms due to a physical interaction mediated by metal nanoparticles (NPs).
The cell wall has an important role in isolating cytoplasmic inclusions from the external environment and in hosting important metabolic pathways (e.g., the electron transport chain and controlled passage of molecules to and from the outside), so its destruction is fatal for bacterial cells [73]. Since the cell wall of both Gram-positive and Gram-negative bacteria is negatively charged, electrostatic interactions with positively charged NPs are favored.
The contact of bacteria with NPs lead to membrane damage due to their adsorption and penetration into the cell [56]. NPs’ adsorption causes cell wall depolarization, modifying the negative charge of the wall and making it more penetrable. Consequently, the cell wall is destroyed, and ROS are produced [74].
Several studies have shown that AgNPs adhere to the cell wall, degrading it and increasing ion passage towards the cytosol [54,75]. Ninganagouda et al. demonstrated that AgNPs are able to anchor on bacterial surfaces, causing death via ruptured cell membranes and the leakage of intracellular components [76]. Other researchers have demonstrated that MgONPs and Mg(OH)2NPs can cause cell death by electrostatic adsorption onto the cell wall without entering the cell [77,78].
The cellular uptake of NPs is another mechanism associated with physical interaction, and occurs when NPs are small enough to cross the cell membrane [79]. Mukha et al. showed that the antibacterial activity of AgNPs smaller than 10 nm is due to membrane damage and their penetration into the cell [80]. Similarly, Dong et al. evaluated NPs with different sizes and concluded that AgNPs with smaller size are more effective because they are able to cross the cell membrane [81]. Oves et al. synthesized AgNPs with bacterial exopolysaccharides, spherical shape, and a size of about 35 nm. They demonstrated that the antimicrobial activity of these NPs against B. subtilis and methicillin-resistant Staphylococcus aureus (MRSA) is due to ROS production inside bacterial cells. Furthermore, they showed that NPs also had excellent properties against biofilm formation [82].
In another study, it was demonstrated that the bactericidal activity of gold (Au) NPs against E. coli was due to the inhibition of ribosome subunits, in addition to the alteration of membrane and ATPase activities [83].
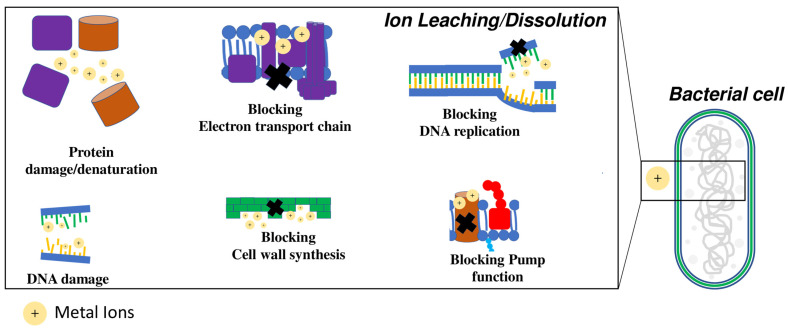
4.2. Ion Leaching and Dissolution
The antibacterial activity of NPs can be also attributed to ion leaching; these ions can diffuse inside the cell and interact with the cellular membrane and wall, as well as cell macromolecules such as proteins and nucleic acids [84,85,86,87] (Figure 4). Several studies have demonstrated that environmental conditions, including pH and NP dissolution rate, can significantly affect the antimicrobial activity of NPs themselves. Saliani et al. showed that the inhibition of bacterial growth due to ZnONPs increased when pH decreased from 7 to acidic pH [88]. Analogously, Moreau et al. observed an increased dissolution of ZnONPs under acidic conditions, suggesting a higher release of Zn2+ ions [89]. Pereziazhko et al. suggested that once released into the aquatic system, AgNPs undergo oxidative dissolution which results in the release of Ag + ions and the induction of antibacterial activity [90]. In addition, they observed that the size-dependent dissolution of AgNPs was larger in acetic acid than in water.
Figure 4.
Schematic description and targets of antibacterial mechanisms due to the release of metal ions (+) by nanoparticles (NPs).
Wigginton et al. showed that over 50% of bacterial proteins have a strong binding affinity for NPs and metal ions, including enzymatic and non-enzymatic proteins [91]. Therefore, bacterial cells undergo damage both at the metabolic level and at the structural level, due to the loss of cellular integrity and the energy transport chain.
The NPs’ interaction with nucleic acids is certainly the main antibacterial mechanism due to the ion diffusion in the cells. Chatterjee et al. reported that E. coli and S. aureus after AgNP treatment showed DNA condensation. Furthermore, their results indicated that the DNA of E. coli was more susceptible compared to S. aureus [92]. Another study indicated that the accumulation of high concentrations of metal ions can lead to double-stranded DNA breakdown [93].
Ions released from metal NPs can be significantly influenced by the medium in which they are dispersed [94]. Levard et al. found that chloride present in seawater or culture medium can favor ion release from AgNPs [95]. This release, despite leading to an initial increase in bactericidal activity, reduces the NPs’ life and, consequently, their antimicrobial activity overtime. The same effect of bactericidal activity reduction is also due to oxidation and the interaction of zero-valent iron NPs with natural organic matter in aerobic conditions [96].
4.3. Production of Reactive Oxygen Species
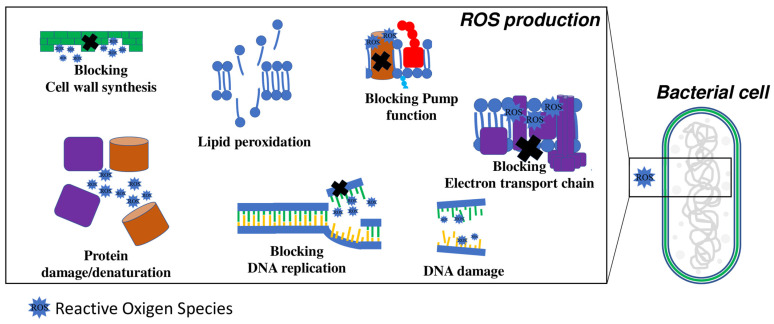
The production of ROS is another important mechanism involved in metal NP-mediated antibacterial activity (Figure 5).
Figure 5.
Schematic description and targets of antibacterial mechanisms due to the ROS produced by nanoparticles (NPs).
ROS can disrupt bacterial cells if they are produced either inside or outside the cell [14,97]. High ROS concentrations can damage the cellular membrane [98,99] by oxidative stress and lipid peroxidation, and the wall by the breakdown of the peptidoglycan structure [55,100,101], degrading proteins and nucleic acids [102] and thus leading to cell death. Metal nanomaterials increase ROS production in bacterial cells that cause DNA denaturation by intercalation between the purine and pyrimidine bases [99]. Consequently, metabolic and transduction signals are altered, and the cell growth is inhibited. The most common metal nanomaterials that produce antibacterial activity mediated by ROS production are silver, zinc oxide, and titanium dioxide [98,103,104,105]. The ROS amount induced by metal nanomaterials depends on the size and chemistry, while the effect of shape is unknown. Mujeeb et al. found that silver–copper nanocomposites (Ag-CuNCs), synthetized using an Olax scandens leaf extract showed a greater antimicrobial activity than monometallic AgNPs with an increase in ROS production [106]. Wang et al. found that the bactericidal activity of Ag/CeO2 NPs in E. coli is mainly due to intracellular ROS production as well as cell wall and membrane disruption [14], and not due to the ion silver release.
4.4. Bacterial Resistance Strategy against NPs
Bacteria can regulate their electrical surface charge to repel NPs with different charges, modifying the structure of the phospholipidic membrane or cell wall [107]. Gram-positive bacteria can reduce their negative surface charge by the incorporation of D-alanine into the cell wall [108]. Otherwise, Gram-negative bacteria modify their LPS in the outer membrane by adding phosphoethanolamine to lipid A [109].
The activity of bacterial cells on NPs can modify their physico-chemical properties, including aggregation and ligation, redox reactions, biomacromolecule adsorption altering ion release and, consequently, antibacterial activity.
It is known that resistance to ion release can be favored by bacterial efflux systems. These systems involve several protein families belonging to resistance-nodulation-cell division proteins (membrane fusion protein family or outer membrane factors), cation diffusion facilitators, and members of P-type ATPases [110,111]. Otherwise, metal ions can be intra- and extracellular-sequestered, or reduced by species-specific pigments [112,113]. Ellis et al. observed that phenazine pigments, including pyocyanin, pyochelin, and pyoverdine, can induce resistance by reducing Ag+ in Ag0 in P. aeruginosa and its biofilm [113]. These systems are controlled by a metal regulatory and homeostasis system and can be codified by specific operons present in bacterial DNA, or plasmids [114,115]. It has recently been observed that exposure to sub-lethal doses of metal NPs increases the conjugative transfer rate, favoring the co-selection and co-expression of antibiotic resistance genes [116,117].
Recently, it has been shown that Gram-negative bacteria, such as E. coli and P. aeruginosa, produce extracellular molecules, such as flagellin, able to favor AgNPs’ aggregation and, consequently, to reduce antibacterial activity on both planktonic and biofilm cells [118,119]. NPs’ size is also important for their diffusion in biofilm through existing pores and water channels [15,120]. Choi et al. demonstrated that biofilms are more resistant to nanosilver inhibition than planktonic cells, suggesting that this resistance could be at least partially due to NPs aggregation and retarded Ag ion/particle diffusion [36].
5. Antimicrobial Application of Metal NPs
5.1. Biomedical Application
Due to increasing drug-resistant bacteria, metal NPs have attracted growing interest in several biomedical applications as antibacterial agents. NPs exhibit several advantages such as easy production and the possibility to modulate their antibacterial effects by changing physical parameters.
One of the most common uses of NPs is in implantable devices. Implantable devices must possess specific requirements, including good biocompatibility, tissue affinity, corrosion resistance and, in particular, antibacterial property [121].
Recently, several approaches have been proposed to improve the antibacterial effects of implants by coating with several metal and metal oxide NPs [122,123,124,125,126,127]. Poly(methyl methacrylate) (PMMA)-based bone cement with AgNPs showed a significant reduction in surface colonization and biofilm formation [128]. Similarly, Kose et al. used titanium nails coated with silver-doped hydroxyapatite for arthroplasty surgery, observing good antibacterial activity, the absence of inflammation around the prostheses, and no cytotoxic effect due to the silver ions [129].
Significant antibacterial results have also been found in other medical devices, such as catheters and dental implants. Some researchers found that functionalization with NPs reduced bacterial growth and biofilm production after catheter implantation [130,131]. Chen et al. optimized a AgNP-coated collagen membrane for dental implants, showing excellent antibacterial effects both against S. aureus and against P. aeruginosa, with low cytotoxicity [132]. Ramazanzadeh et al. coated dental plaque chalk with copper and zinc oxide, showing significant antibacterial activity against Streptococcus mutans from 6 to 24 h [133].
NPs are used also as antibacterial additives in dressings for the treatment of skin wounds. Both Gram-positive and Gram-negative pathogenic bacteria can lead to chronic infections associated with skin wounds. AgNPs significantly inhibited bacterial growth and increased the rate of wound healing when used in combination with poly(vinyl alcohol) and chitosan [134].
Finally, NPs also find application in the agro-food field, especially in food packaging, where their use in the detection and killing of pathogens is closely linked to human health [135,136].
5.2. Recent Application of Metal NPs
The following sections will discuss the latest evidence on the antimicrobial activity of some metal NPs in several applications.
Silver-based nanoparticles: AgNPs and Ag2ONPs are used in a wide range of applications, such as dentistry, scaffolds for tissue engineering, wound healing materials, food packaging, drinking water disinfection, and textile manufacturing, due to their high antibacterial, antifungal and antiviral activities [137,138,139,140,141,142,143,144,145].
It has been observed that AgNPs incorporated into crystallized hydroxyapatite (HA) or titanium scaffolds have significant antibacterial activity against both Gram-positive and Gram-negative bacteria [18,146,147], and show improvement to bone healing [148]. Shimazaki et al. implanted, in rat models, Ag-HA-coated titanium plates to test their activity against methicillin-resistant Staphylococcus aureus (MRSA) compared with HA-coated plates. Their results showed a lower number of MRSA colony-forming units (CFUs) on the Ag-HA-coated plates, suggesting the promising use of the coating in clinical applications [149]. Similarly, Saravanan et al. reported that chitosan/nanohydroxyapatite-containing AgNPs exhibited antimicrobial activities against Gram-positive and Gram-negative bacteria, with negligible cytotoxicity versus rat osteoprogenitor cells and human osteosarcoma cells [150].
Alt et al. performed an in vitro study comparing nanosilver-loaded bone cement with gentamicin-loaded and plain cement against S. epidermidis, methicillin-resistant Staphylococcus epidermidis (MRSE), and MRSA. Their results showed that only the nanosilver cement had good antibacterial efficacy against both bacterial strains [151].
In vitro and in vivo studies have evaluated the utility of nano-Ag as an additive to prevent infection with Porphyromonas gingivalis [152,153,154] or to improve antibacterial surface coating against S. aureus and E. coli [155]. AgNPs have also been used in the preparation of catheters to improve their inhibitory effects against infection [156,157,158], especially due to MRSA, and are able to form biofilms and bacterial dispersion [159]. Wilkinson et al. reported that dressings containing AgNPs exhibited a higher antimicrobial effect than bulk silver due to the sustained release of silver ions on the exudate released from the wound [160]. AgNPs’ antibacterial activity is due to their physical interaction with the peptidoglycan cell wall of bacteria, causing structural changes that increase membrane permeability and subsequently cell death [161]. AgNPs also interact with exposed sulfhydryl groups of bacterial proteins to prevent DNA replication [162]. Silver oxide NPs (Ag2O) interact with the DNA of bacteria causing the loss of their replication ability. The cell cycle halts at the G2/M phase due to DNA damage, and the cells are subsequently killed by oxidative stress [72]. Moreover, AgNPs with a size smaller than 6 nm can penetrate the entire depth of biofilm [163].
Gold-based nanoparticles: The incorporation of AuNPs in PMMA-based bone cement improves the mechanical properties of the polymeric matrix and reduces the formation of S. aureus biofilms [164]. The decrease in size of AuNPs to the nanocluster (NC) range (1–2 nm in diameter) has been found to enhance antimicrobial activity against Gram-positive and Gram-negative bacteria, mainly due to increasing ROS levels, maintaining a low cytotoxic and genotoxic effect on the host cells [165].
In addition, it has been suggested that alteration of the shape (from NPs to nanospikes or nanorods) leads the expansion of the absorption wavelength to the near-infrared region, enhancing light-to-heat conversion [166]. Such nanostructures have potential applications in biomimetic scaffolds [16,167], water sterilization, and photothermal/photodynamic therapy [168,169]. In vivo studies have shown that both AuNPs and AuNCs exhibit toxicity by decreasing red blood cell count and damaging organs such as the spleen, liver and kidney [170].
The main advantages related to gold-based nanostructures are rapid and simple preparation and their use as a bio-conjugable platform. In addition, the ability to absorb, scatter, and enhance the electromagnetic field of light makes them particularly versatile in both diagnostic and therapeutic systems.
Copper-based nanoparticles: The antimicrobial activity of copper NPs (CuNPs) is comparable to that of AgNPs, although bactericidal efficacy against Gram-negative strains is lower [171,172]. Similar to other metal NPs, smaller sizes exhibit a greater bactericidal effect, due to an increase in surface/volume ratio and a closer interaction with membrane and bacterial wall structures [173]. CuNPs are used in several medical applications, such as burn treatment, antibacterial prostheses, catheters, vascular grafts and teeth [174]. CuNPs have been embedded within dendritic polyglycerol to form coatings with a high antibacterial efficacy against both Gram-negative and Gram-positive strains, as well as antibiotic-resistant ones [175].
The antibacterial mechanism has been described as “attract–kill–release” by both ROS production and Cu2+ release, with long-term and good biocompatibility properties. Other applications of CuNPs involve their encapsulation in alginate beads, or their use as a coating for polyurethane foam for the development and design of antibacterial water filters [176]. The advantage of using CuNPs compared to other metal NPs, such as AgNPs and AuNPs, is the low production cost. Furthermore, NPs with high antibacterial and anticancer power have been obtained by green technology, reducing cytotoxic side effects [177].
Iron-based nanoparticles: Zero-valent iron NPs without polymeric coatings have been widely used for environmental remediation due to their ability to detoxify many contaminants by redox reactions. However, in vitro studies found toxicity toward terrestrial and aquatic biota, probably due to the oxidative stress and Fe2+-mediated cell membrane disruption [178,179]. The antibacterial mechanism of iron oxide is mainly due to the production of ROS, chlorosis, and hypoxia [179,180]. Iron oxides consist of magnetite (Fe3O4) and its oxidized forms, maghemite (γ-Fe2O3), and hematite (α-Fe2O3) [181], which are easily obtainable by both chemical–physical and green methods. Fe3O4 NPs penetrate the Gram-negative bacteria through the siderophore channels on the outer membrane. These NPs may be utilized as “Trojan horses” for transferring antibiotics coupled to them, and are usually blocked by the outer membrane into the Gram-negative bacteria [182]. Significant results were also obtained against biofilm. Ali et al. showed that α-Fe2O3 NPs interact with biofilm extracellular polymeric substances (EPS) and penetrate into cell, inhibiting growth by intracellular ROS formation [183]. Similarly, Ikuma et al. displayed that the deposition of α-Fe2O3 NPs on the polysaccharides of EPS is governed by electrostatic forces, so antibiofilm activity is mainly due to the direct contact between NPs and bacteria surface (contact-killing) [181]. Iron oxide NPs have been used as dental irrigants for the antibacterial treatment of the root canal, showing a significant reduction in Entercoccus faecalis, which is particularly resistant to treatment mediated by the activation of H2O2 [184]. α-Fe2O3 with bactericidal ability against Gram-negative and Gram-positive bacteria has been synthetized by pulsed laser ablation and coprecipitation methods [185]; γ-Fe2O3 has been also proved to be effective in bactericide activity [119], while similar results have been obtained from Fe2O3 obtained by an eco-friendly method on biopolymer templates via thermal decomposition [186]. Like other NPs, for iron oxide, coupling to other metals, such as silver [187], cobalt [188], copper [189,190], and bismuth [191], allows the obtainment of properties that can be used in different applications. Crystal hybrid structures based on ferrite NPs with Co or Cu showed a high bactericidal and fungicide activity [190,192]. Similar results against S. aureus have been found with bismuth, in hybrid nanorod-like structures [191]. On the other hand, peculiar characteristics of iron, such as magnetic properties, increase the possibility of its use in bacterial detection [193].
Titanium-based nanoparticles: Titanium NPs (TiNPs) are extensively used as additives in oral drugs, and are mixed with commercial and non-commercial dental resins and food-related products [194,195]. TiO2 NPs have also been used for the nanofunctionalization of titanium biomimetic scaffolds for bone tissue engineering. Calabrese et al., in their in vitro study, showed that titanium scaffold nanofunctionalized with TiO2 (Ti_TiO2) exhibited a good antibacterial activity towards S. aureus, reducing the number of CFUs by 99.4%. Furthermore, they showed that Ti_TiO2 increased the cell proliferation of human adipose-derived mesenchymal stem cells by 4.3-fold compared to the control titanium scaffold [125]. As a wide-bandgap semiconductor, TiO2 NPs have been incorporated into antibacterial paints or coatings for hospital touch surfaces. The excitation of TiO2 NPs by ultraviolet light produces ROS that can destroy many organic molecules [196]. This photocatalytic process can kill many classes of microorganisms. For antibacterial activity, photocatalysis triggers the downregulation of bacteria genes/proteins associated with regulatory, signaling, and growth functions [197]. Additionally, hybrid silver and TiO2 nanotubes activated by ultraviolet light or visible light range have been demonstrated to develop ROS in the form of hydroxyl radicals (OH•) and superoxide anions (•O2−) [198]. Under ultraviolet light, the photocatalytic activity of the TiO2 nanotubes could cause the movement of electrons in the valence band to the conduction band, which reduces O2 in the AgNPs to create •O2− and OH• free radicals. Under visible light, the electrons on the surface of the AgNPs are excited by the surface plasmon resonance effect and move to the conduction band of the TiO2 nanotubes. At a concentration of 20 ppm, the TiO2 nanotubes alone kill S. aureus by 95.9% after 60 min of sunlight exposure. When AgNPs are loaded onto the TiO2 nanotubes, antimicrobial activity against S. aureus further increases to 99.99% after 60 min of sunlight irradiation. TiO2 NPs are capable of binding to the hydroxyl groups in the polysaccharide matrix of synthetic biofilms, resulting in irreversible adsorption [199].
Zinc-based nanoparticles: Similar to TiO2, ZnONPs exhibit broad-spectrum antimicrobial activity, mainly due to their susceptibility to ultraviolet light [200,201]. ZnO has been used as an additive in cosmetic nonprescription drug products and/or sunscreens in which the antibacterial activity is also associated with UV protection [202,203]. Other applications of ZnO include use as an antibacterial agent in food packaging [204,205,206] and in restorative dentistry tissue regeneration, where antibacterial activity is coupled to an enhancement in mechanical properties [207,208,209].
The antibacterial mechanism of ZnONPs is due to the physical damage of membrane and intracellular ROS production. Specifically, ZnONPs with an isoelectric point usually higher than 9 exhibit strong positive surface charges under physiologic conditions, which promotes electrostatic interactions with the negatively charged surface of the bacteria [210]. Some researchers have reported a higher bactericidal activity of ZnONPs than AgNPs against S. mutans [133,211]. Other studies have reported the use of Zn nanostructured with other metal NPs, such as AgNPs, or titanium porous scaffolds for bone regeneration [212,213,214]. For the latter, a proliferative increase in osteoblastic cells and an inhibitory activity towards osteoclastic bone resorption has been highlighted, in addition to bactericidal action towards both Gram-positive and Gram-negative strains [215,216].
6. Discussion and Final Remarks
In the field of new antibacterial materials, NPs represent a concrete alternative to antibiotics. These nanomaterials address multimolecular biotic targets, resulting in a broad spectrum of antibacterial activity, including drug-resistant bacterial variants [217]. While a high dosage could also induce toxicity for eukaryotic cells, a low dosage, sublethal for bacteria, increases the permeability of the bacteria cell membranes and, consequently, promotes the horizontal transfer of resistance genes. Several metal (Ag, Zn, and Cu) and metal oxide (ZnO, CuO, MgO, and TiO2) NPs have been widely utilized in several biomedical applications due to their bactericidal abilities [218,219,220,221]. AgNPs are the most used for the antibacterial coating of medical devices [222], but their accumulation in the body and toxicity limited their use. Unlike silver, copper-based nanoparticles showed a more rapid and higher microbicidal efficacy against different types of microorganisms, such as E. coli, V. cholera, P. aeruginosa, S. typhus, S. aureus, E. faecalis, B. subtilis and S. faecalis, enhancing their range of applicability [223]. Similarly, AuNPs have been used in a wide range of antibacterial applications due to their lesser toxicity to mammalian cells, even though they have considerably lower antibacterial activity than AgNPs [224]. ZnONPs possess antimicrobial activity against numerous Gram-positive (S. aureus, S. epidermis, B. subtilis, B. cereus, L. monocytogenes, E. faecium) and Gram-negative (P. aeruginosa, E. coli, K. pneumoniae, Salmonella sp.) bacteria, stimulating a considerable range of antimicrobial applications, including the food packaging industry [225].
These above-reported studies suggest that NPs are paving way as probable alternatives to antibiotics for future therapies in nanomedicine.
Advancements in this area involve the chemical functionalization of NPs with biomolecules such as peptides, oligomers, oligonucleotide fragments, and engineered phages to address the pharmacokinetics of a given nanomaterial towards a designated target.
Author Contributions
D.F., writing—original draft preparation; G.C. and S.C., conceptualization, writing—review and editing; S.P.P.G., writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.CDC The Biggest Antibiotic-Resistant Threats in the U.S. [(accessed on 5 April 2022)]; Available online: https://www.cdc.gov/drugresistance/biggest-threats.html.
- 2.Abraham E.P., Chain E. An Enzyme from Bacteria Able to Destroy Penicillin. Nature. 1940;146:837. doi: 10.1038/146837a0. [DOI] [PubMed] [Google Scholar]
- 3.Khan A.A., Manzoor K.N., Sultan A., Saeed M., Rafique M., Noushad S., Talib A., Rentschler S., Deigner H.-P. Pulling the Brakes on Fast and Furious Multiple Drug-Resistant (MDR) Bacteria. Int. J. Mol. Sci. 2021;22:859. doi: 10.3390/ijms22020859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Santajit S., Indrawattana N. Mechanisms of Antimicrobial Resistance in ESKAPE Pathogens. BioMed Res. Int. 2016;2016:2475067. doi: 10.1155/2016/2475067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosini R., Nicchi S., Pizza M., Rappuoli R. Vaccines Against Antimicrobial Resistance. Front. Immunol. 2020;11:1048. doi: 10.3389/fimmu.2020.01048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reygaert W.C. An Overview of the Antimicrobial Resistance Mechanisms of Bacteria. AIMS Microbiol. 2018;4:482–501. doi: 10.3934/microbiol.2018.3.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chancey S.T., Zähner D., Stephens D.S. Acquired Inducible Antimicrobial Resistance in Gram-Positive Bacteria. Future Microbiol. 2012;7:959–978. doi: 10.2217/fmb.12.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kapoor G., Saigal S., Elongavan A. Action and Resistance Mechanisms of Antibiotics: A Guide for Clinicians. J. Anaesthesiol. Clin. Pharmacol. 2017;33:300–305. doi: 10.4103/joacp.JOACP_349_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pacios O., Blasco L., Bleriot I., Fernandez-Garcia L., González Bardanca M., Ambroa A., López M., Bou G., Tomás M. Strategies to Combat Multidrug-Resistant and Persistent Infectious Diseases. Antibiotics. 2020;9:65. doi: 10.3390/antibiotics9020065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vimbela G.V., Ngo S.M., Fraze C., Yang L., Stout D.A. Antibacterial Properties and Toxicity from Metallic Nanomaterials. Int. J. Nanomed. 2017;12:3941–3965. doi: 10.2147/IJN.S134526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nocito G., Sciuto E.L., Franco D., Nastasi F., Pulvirenti L., Petralia S., Spinella C., Calabrese G., Guglielmino S., Conoci S. Physicochemical Characterization and Antibacterial Properties of Carbon Dots from Two Mediterranean Olive Solid Waste Cultivars. Nanomaterials. 2022;12:885. doi: 10.3390/nano12050885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agnihotri S., Dhiman N.K. Development of Nano-Antimicrobial Biomaterials for Biomedical Applications. In: Tripathi A., Melo J.S., editors. Advances in Biomaterials for Biomedical Applications. Springer; Singapore: 2017. pp. 479–545. Advanced Structured Materials. [Google Scholar]
- 13.Kittler S., Greulich C., Diendorf J., Köller M., Epple M. Toxicity of Silver Nanoparticles Increases during Storage Because of Slow Dissolution under Release of Silver Ions. [(accessed on 9 April 2022)]. Available online: https://pubs.acs.org/doi/pdf/10.1021/cm100023p.
- 14.Wang L., He H., Yu Y., Sun L., Liu S., Zhang C., He L. Morphology-Dependent Bactericidal Activities of Ag/CeO2 Catalysts against Escherichia Coli. J. Inorg. Biochem. 2014;135:45–53. doi: 10.1016/j.jinorgbio.2014.02.016. [DOI] [PubMed] [Google Scholar]
- 15.Shkodenko L., Kassirov I., Koshel E. Metal Oxide Nanoparticles Against Bacterial Biofilms: Perspectives and Limitations. Microorganisms. 2020;8:1545. doi: 10.3390/microorganisms8101545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Franco D., Calabrese G., Petralia S., Neri G., Corsaro C., Forte L., Squarzoni S., Guglielmino S., Traina F., Fazio E., et al. Antimicrobial Effect and Cytotoxic Evaluation of Mg-Doped Hydroxyapatite Functionalized with Au-Nano Rods. Molecules. 2021;26:1099. doi: 10.3390/molecules26041099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang W., Liu X., Bao S., Xiao B., Fang T. Evaluation of Nano-Specific Toxicity of Zinc Oxide, Copper Oxide, and Silver Nanoparticles through Toxic Ratio. J. Nanopart. Res. 2016;18:372. doi: 10.1007/s11051-016-3689-2. [DOI] [Google Scholar]
- 18.Calabrese G., Petralia S., Franco D., Nocito G., Fabbi C., Forte L., Guglielmino S., Squarzoni S., Traina F., Conoci S. A New Ag-Nanostructured Hydroxyapatite Porous Scaffold: Antibacterial Effect and Cytotoxicity Study. Mater. Sci. Eng. C. 2021;118:111394. doi: 10.1016/j.msec.2020.111394. [DOI] [PubMed] [Google Scholar]
- 19.Malanovic N., Lohner K. Gram-Positive Bacterial Cell Envelopes: The Impact on the Activity of Antimicrobial Peptides. Biochim. Biophys. Acta Biomembr. 2016;1858:936–946. doi: 10.1016/j.bbamem.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 20.Huang K.C., Mukhopadhyay R., Wen B., Gitai Z., Wingreen N.S. Cell Shape and Cell-Wall Organization in Gram-Negative Bacteria. Proc. Natl. Acad. Sci. USA. 2008;105:19282–19287. doi: 10.1073/pnas.0805309105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dorobantu L.S., Fallone C., Noble A.J., Veinot J., Ma G., Goss G.G., Burrell R.E. Toxicity of Silver Nanoparticles against Bacteria, Yeast, and Algae. J. Nanopart. Res. 2015;17:172. doi: 10.1007/s11051-015-2984-7. [DOI] [Google Scholar]
- 22.Tamayo L., Azócar M., Kogan M., Riveros A., Páez M. Copper-Polymer Nanocomposites: An Excellent and Cost-Effective Biocide for Use on Antibacterial Surfaces. Mater. Sci. Eng. C. 2016;69:1391–1409. doi: 10.1016/j.msec.2016.08.041. [DOI] [PubMed] [Google Scholar]
- 23.Morones-Ramirez J.R., Winkler J.A., Spina C.S., Collins J.J. Silver Enhances Antibiotic Activity Against Gram-Negative Bacteria. Sci. Transl. Med. 2013;5:190ra81. doi: 10.1126/scitranslmed.3006276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feng Q.L., Wu J., Chen G.Q., Cui F.Z., Kim T.N., Kim J.O. A Mechanistic Study of the Antibacterial Effect of Silver Ions on Escherichia Coli and Staphylococcus Aureus. J. Biomed. Mater. Res. 2000;52:662–668. doi: 10.1002/1097-4636(20001215)52:4<662::AID-JBM10>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 25.Cavassin E.D., de Figueiredo L.F.P., Otoch J.P., Seckler M.M., de Oliveira R.A., Franco F.F., Marangoni V.S., Zucolotto V., Levin A.S.S., Costa S.F. Comparison of Methods to Detect the in Vitro Activity of Silver Nanoparticles (AgNP) against Multidrug Resistant Bacteria. J. Nanobiotechnology. 2015;13:64. doi: 10.1186/s12951-015-0120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The Effects of Interfacial Potential on Antimicrobial Propensity of ZnO Nanoparticle|Scientific Reports. [(accessed on 5 April 2022)]. Available online: https://www.nature.com/articles/srep09578. [DOI] [PMC free article] [PubMed]
- 27.Shinde V.V., Dalavi D.S., Mali S.S., Hong C.K., Kim J.H., Patil P.S. Surfactant Free Microwave Assisted Synthesis of ZnO Microspheres: Study of Their Antibacterial Activity. Appl. Surf. Sci. 2014;307:495–502. doi: 10.1016/j.apsusc.2014.04.064. [DOI] [Google Scholar]
- 28.Rai M., Kon K., Ingle A., Duran N., Galdiero S., Galdiero M. Broad-Spectrum Bioactivities of Silver Nanoparticles: The Emerging Trends and Future Prospects. Appl. Microbiol. Biotechnol. 2014;98:1951–1961. doi: 10.1007/s00253-013-5473-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abbaszadegan A., Ghahramani Y., Gholami A., Hemmateenejad B., Dorostkar S., Nabavizadeh M., Sharghi H. The Effect of Charge at the Surface of Silver Nanoparticles on Antimicrobial Activity against Gram-Positive and Gram-Negative Bacteria: A Preliminary Study. J. Nanomater. 2015;2015:e720654. doi: 10.1155/2015/720654. [DOI] [Google Scholar]
- 30.Slavin Y.N., Asnis J., Häfeli U.O., Bach H. Metal Nanoparticles: Understanding the Mechanisms behind Antibacterial Activity. J. Nanobiotechnol. 2017;15:65. doi: 10.1186/s12951-017-0308-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Padmavathy N., Vijayaraghavan R. Enhanced Bioactivity of ZnO Nanoparticles-an Antimicrobial Study. Sci. Technol. Adv. Mater. 2008;9:035004. doi: 10.1088/1468-6996/9/3/035004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Penesyan A., Paulsen I.T., Kjelleberg S., Gillings M.R. Three Faces of Biofilms: A Microbial Lifestyle, a Nascent Multicellular Organism, and an Incubator for Diversity. NPJ Biofilms Microbiomes. 2021;7:80. doi: 10.1038/s41522-021-00251-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zheng S., Bawazir M., Dhall A., Kim H.-E., He L., Heo J., Hwang G. Implication of Surface Properties, Bacterial Motility, and Hydrodynamic Conditions on Bacterial Surface Sensing and Their Initial Adhesion. Front. Bioeng. Biotechnol. 2021;9:643722. doi: 10.3389/fbioe.2021.643722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rumbaugh K.P., Sauer K. Biofilm Dispersion. Nat. Rev. Microbiol. 2020;18:571–586. doi: 10.1038/s41579-020-0385-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kragh K.N., Hutchison J.B., Melaugh G., Rodesney C., Roberts A.E.L., Irie Y., Jensen P.Ø., Diggle S.P., Allen R.J., Gordon V., et al. Role of Multicellular Aggregates in Biofilm Formation. mBio. 2016;7:e00237-16. doi: 10.1128/mBio.00237-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choi O., Yu C.-P., Esteban Fernández G., Hu Z. Interactions of Nanosilver with Escherichia Coli Cells in Planktonic and Biofilm Cultures. Water Res. 2010;44:6095–6103. doi: 10.1016/j.watres.2010.06.069. [DOI] [PubMed] [Google Scholar]
- 37.Wang Q., Kang F., Gao Y., Mao X., Hu X. Sequestration of Nanoparticles by an EPS Matrix Reduces the Particle-Specific Bactericidal Activity. Sci. Rep. 2016;6:21379. doi: 10.1038/srep21379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gomes I.B., Simões M., Simões L.C. Copper Surfaces in Biofilm Control. Nanomaterials. 2020;10:2491. doi: 10.3390/nano10122491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Roe D., Karandikar B., Bonn-Savage N., Gibbins B., Roullet J.-B. Antimicrobial Surface Functionalization of Plastic Catheters by Silver Nanoparticles. J. Antimicrob. Chemother. 2008;61:869–876. doi: 10.1093/jac/dkn034. [DOI] [PubMed] [Google Scholar]
- 40.Gomez-Carretero S., Nybom R., Richter-Dahlfors A. Electroenhanced Antimicrobial Coating Based on Conjugated Polymers with Covalently Coupled Silver Nanoparticles Prevents Staphylococcus Aureus Biofilm Formation. Adv. Healthc. Mater. 2017;6:1700435. doi: 10.1002/adhm.201700435. [DOI] [PubMed] [Google Scholar]
- 41.Spirescu V.A., Șuhan R., Niculescu A.-G., Grumezescu V., Negut I., Holban A.M., Oprea O.-C., Bîrcă A.C., Vasile B.Ș., Grumezescu A.M., et al. Biofilm-Resistant Nanocoatings Based on ZnO Nanoparticles and Linalool. Nanomaterials. 2021;11:2564. doi: 10.3390/nano11102564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Applerot G., Lellouche J., Perkas N., Nitzan Y., Gedanken A., Banin E. ZnO Nanoparticle-Coated Surfaces Inhibit Bacterial Biofilm Formation and Increase Antibiotic Susceptibility. RSC Adv. 2012;2:2314–2321. doi: 10.1039/c2ra00602b. [DOI] [Google Scholar]
- 43.Bazzi W., Abou Fayad A.G., Nasser A., Haraoui L.-P., Dewachi O., Abou-Sitta G., Nguyen V.-K., Abara A., Karah N., Landecker H., et al. Heavy Metal Toxicity in Armed Conflicts Potentiates AMR in A. Baumannii by Selecting for Antibiotic and Heavy Metal Co-Resistance Mechanisms. Front. Microbiol. 2020;11:68. doi: 10.3389/fmicb.2020.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thambirajoo M., Maarof M., Lokanathan Y., Katas H., Ghazalli N.F., Tabata Y., Fauzi M.B. Potential of Nanoparticles Integrated with Antibacterial Properties in Preventing Biofilm and Antibiotic Resistance. Antibiotics. 2021;10:1338. doi: 10.3390/antibiotics10111338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chernousova S., Epple M. Silver as Antibacterial Agent: Ion, Nanoparticle, and Metal. Angew. Chem. Int. Ed. 2013;52:1636–1653. doi: 10.1002/anie.201205923. [DOI] [PubMed] [Google Scholar]
- 46.Guo D., Xie G., Luo J. Mechanical Properties of Nanoparticles: Basics and Applications. J. Phys. D Appl. Phys. 2013;47:013001. doi: 10.1088/0022-3727/47/1/013001. [DOI] [Google Scholar]
- 47.Lue J.-T. A Review of Characterization and Physical Property Studies of Metallic Nanoparticles. J. Phys. Chem. Solids. 2001;62:1599–1612. doi: 10.1016/S0022-3697(01)00099-3. [DOI] [Google Scholar]
- 48.Khan A.U., Yuan Q., Wei Y., Khan G.M., Khan Z.U.H., Khan S., Ali F., Tahir K., Ahmad A., Khan F.U. Photocatalytic and Antibacterial Response of Biosynthesized Gold Nanoparticles. J. Photochem. Photobiol. B Biol. 2016;162:273–277. doi: 10.1016/j.jphotobiol.2016.06.055. [DOI] [PubMed] [Google Scholar]
- 49.Liu L., Zhang X., Yang L., Ren L., Wang D., Ye J. Metal Nanoparticles Induced Photocatalysis. Natl. Sci. Rev. 2017;4:761–780. doi: 10.1093/nsr/nwx019. [DOI] [Google Scholar]
- 50.Grazú V., Silber A., Moros M., Asín L., Torres T., Marquina C., Ibarra M., Goya G. Application of Magnetically Induced Hyperthermia in the Model Protozoan Crithidia Fasciculata as a Potential Therapy against Parasitic Infections. Int. J. Nanomed. 2012;7:5351–5360. doi: 10.2147/IJN.S35510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu X., Zhang Y., Wang Y., Zhu W., Li G., Ma X., Zhang Y., Chen S., Tiwari S., Shi K., et al. Comprehensive Understanding of Magnetic Hyperthermia for Improving Antitumor Therapeutic Efficacy. Theranostics. 2020;10:3793–3815. doi: 10.7150/thno.40805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cui L., Chen P., Chen S., Yuan Z., Yu C., Ren B., Zhang K. In Situ Study of the Antibacterial Activity and Mechanism of Action of Silver Nanoparticles by Surface-Enhanced Raman Spectroscopy. Anal. Chem. 2013;85:5436–5443. doi: 10.1021/ac400245j. [DOI] [PubMed] [Google Scholar]
- 53.Pérez-Díaz M.A., Boegli L., James G., Velasquillo C., Sánchez-Sánchez R., Martínez-Martínez R.-E., Martínez-Castañón G.A., Martinez-Gutierrez F. Silver Nanoparticles with Antimicrobial Activities against Streptococcus Mutans and Their Cytotoxic Effect. Mater. Sci. Eng. C. 2015;55:360–366. doi: 10.1016/j.msec.2015.05.036. [DOI] [PubMed] [Google Scholar]
- 54.Wang L., Hu C., Shao L. The Antimicrobial Activity of Nanoparticles: Present Situation and Prospects for the Future. Int. J. Nanomed. 2017;12:1227–1249. doi: 10.2147/IJN.S121956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ivask A., ElBadawy A., Kaweeteerawat C., Boren D., Fischer H., Ji Z., Chang C.H., Liu R., Tolaymat T., Telesca D., et al. Toxicity Mechanisms in Escherichia Coli Vary for Silver Nanoparticles and Differ from Ionic Silver. ACS Nano. 2014;8:374–386. doi: 10.1021/nn4044047. [DOI] [PubMed] [Google Scholar]
- 56.Thill A., Zeyons O., Spalla O., Chauvat F., Rose J., Auffan M., Flank A.M. Cytotoxicity of CeO2 Nanoparticles for Escherichia Coli. Physico-Chemical Insight of the Cytotoxicity Mechanism. Environ. Sci. Technol. 2006;40:6151–6156. doi: 10.1021/es060999b. [DOI] [PubMed] [Google Scholar]
- 57.Wang E.C., Wang A.Z. Nanoparticles and Their Applications in Cell and Molecular Biology. Integr. Biol. 2014;6:9–26. doi: 10.1039/c3ib40165k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shang L., Nienhaus K., Nienhaus G.U. Engineered Nanoparticles Interacting with Cells: Size Matters. J. Nanobiotechnol. 2014;12:5. doi: 10.1186/1477-3155-12-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Skomorokhova E.A., Sankova T.P., Orlov I.A., Savelev A.N., Magazenkova D.N., Pliss M.G., Skvortsov A.N., Sosnin I.M., Kirilenko D.A., Grishchuk I.V., et al. Size-Dependent Bioactivity of Silver Nanoparticles: Antibacterial Properties, Influence on Copper Status in Mice, and Whole-Body Turnover. Nanotechnol. Sci. Appl. 2020;13:137–157. doi: 10.2147/NSA.S287658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Korshed P., Li L., Liu Z., Mironov A., Wang T. Size-Dependent Antibacterial Activity for Laser-Generated Silver Nanoparticles. J. Interdiscip. Nanomed. 2019;4:24–33. doi: 10.1002/jin2.54. [DOI] [Google Scholar]
- 61.Zare M., Namratha K., Byrappa K., Surendra D.M., Yallappa S., Hungund B. Surfactant Assisted Solvothermal Synthesis of ZnO Nanoparticles and Study of Their Antimicrobial and Antioxidant Properties. J. Mater. Sci. Technol. 2018;34:1035–1043. doi: 10.1016/j.jmst.2017.09.014. [DOI] [Google Scholar]
- 62.Adams C.P., Walker K.A., Obare S.O., Docherty K.M. Size-Dependent Antimicrobial Effects of Novel Palladium Nanoparticles. PLoS ONE. 2014;9:e85981. doi: 10.1371/journal.pone.0085981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hong X., Wen J., Xiong X., Hu Y. Shape Effect on the Antibacterial Activity of Silver Nanoparticles Synthesized via a Microwave-Assisted Method. Environ. Sci. Pollut. Res. Int. 2016;23:4489–4497. doi: 10.1007/s11356-015-5668-z. [DOI] [PubMed] [Google Scholar]
- 64.Huynh P.T., Nguyen G.D., Tran K.T.L., Ho T.M., Duong B.T., Lam V.Q., Ngo T.V.K. One-Pot, Surfactant-Free Synthesis of Gold Nanostars and Evaluation of Their Antibacterial Effects against Propionibacterium Acnes. J. Nanomater. 2021;2021:e6650661. doi: 10.1155/2021/6650661. [DOI] [Google Scholar]
- 65.Li X., Ahmad K.Z., He J., Li H., Wang X., Feng Z., Wang X., Shen G., Ding X. Silver Nanoflowers Coupled with Low Dose Antibiotics Enable the Highly Effective Eradication of Drug-Resistant Bacteria. J. Mater. Chem. B. 2021;9:9839–9851. doi: 10.1039/D1TB01773J. [DOI] [PubMed] [Google Scholar]
- 66.Guo B.-L., Han P., Guo L.-C., Cao Y.-Q., Li A.-D., Kong J.-Z., Zhai H.-F., Wu D. The Antibacterial Activity of Ta-Doped ZnO Nanoparticles. Nanoscale Res. Lett. 2015;10:336. doi: 10.1186/s11671-015-1047-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.López-Heras M., Theodorou I.G., Leo B.F., Ryan M.P., Porter A.E. Towards Understanding the Antibacterial Activity of Ag Nanoparticles: Electron Microscopy in the Analysis of the Materials-Biology Interface in the Lung. Environ. Sci. Nano. 2015;2:312–326. doi: 10.1039/C5EN00051C. [DOI] [Google Scholar]
- 68.Li Z., Ma J., Ruan J., Zhuang X. Using Positively Charged Magnetic Nanoparticles to Capture Bacteria at Ultralow Concentration. Nanoscale Res. Lett. 2019;14:195. doi: 10.1186/s11671-019-3005-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mammari N., Lamouroux E., Boudier A., Duval R.E. Current Knowledge on the Oxidative-Stress-Mediated Antimicrobial Properties of Metal-Based Nanoparticles. Microorganisms. 2022;10:437. doi: 10.3390/microorganisms10020437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.El Badawy A.M., Silva R.G., Morris B., Scheckel K.G., Suidan M.T., Tolaymat T.M. Surface Charge-Dependent Toxicity of Silver Nanoparticles. Environ. Sci. Technol. 2011;45:283–287. doi: 10.1021/es1034188. [DOI] [PubMed] [Google Scholar]
- 71.Agnihotri S., Mukherji S., Mukherji S. Size-Controlled Silver Nanoparticles Synthesized over the Range 5–100 Nm Using the Same Protocol and Their Antibacterial Efficacy. RSC Adv. 2013;4:3974–3983. doi: 10.1039/C3RA44507K. [DOI] [Google Scholar]
- 72.Dizaj S.M., Lotfipour F., Barzegar-Jalali M., Zarrintan M.H., Adibkia K. Antimicrobial Activity of the Metals and Metal Oxide Nanoparticles. Mater. Sci. Eng. C. 2014;44:278–284. doi: 10.1016/j.msec.2014.08.031. [DOI] [PubMed] [Google Scholar]
- 73.Rice K.C., Bayles K.W. Molecular Control of Bacterial Death and Lysis. Microbiol. Mol. Biol. Rev. 2008;72:85–109. doi: 10.1128/MMBR.00030-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ramalingam B., Parandhaman T., Das S.K. Antibacterial Effects of Biosynthesized Silver Nanoparticles on Surface Ultrastructure and Nanomechanical Properties of Gram-Negative Bacteria Viz. Escherichia Coli and Pseudomonas Aeruginosa. ACS Appl. Mater. Interfaces. 2016;8:4963–4976. doi: 10.1021/acsami.6b00161. [DOI] [PubMed] [Google Scholar]
- 75.Sukhanova A., Bozrova S., Sokolov P., Berestovoy M., Karaulov A., Nabiev I. Dependence of Nanoparticle Toxicity on Their Physical and Chemical Properties. Nanoscale Res. Lett. 2018;13:44. doi: 10.1186/s11671-018-2457-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ninganagouda S., Rathod V., Singh D., Hiremath J., Singh A.K., Mathew J., ul-Haq M. Growth Kinetics and Mechanistic Action of Reactive Oxygen Species Released by Silver Nanoparticles from Aspergillus Niger on Escherichia Coli. BioMed Res. Int. 2014;2014:753419. doi: 10.1155/2014/753419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Leung Y.H., Ng A.M.C., Xu X., Shen Z., Gethings L.A., Wong M.T., Chan C.M.N., Guo M.Y., Ng Y.H., Djurišić A.B., et al. Mechanisms of Antibacterial Activity of MgO: Non-ROS Mediated Toxicity of MgO Nanoparticles towards Escherichia Coli. Small. 2014;10:1171–1183. doi: 10.1002/smll.201302434. [DOI] [PubMed] [Google Scholar]
- 78.Pan X., Wang Y., Chen Z., Pan D., Cheng Y., Liu Z., Lin Z., Guan X. Investigation of Antibacterial Activity and Related Mechanism of a Series of Nano-Mg(OH)2. ACS Appl. Mater. Interfaces. 2013;5:1137–1142. doi: 10.1021/am302910q. [DOI] [PubMed] [Google Scholar]
- 79.McQuillan J.S., Shaw A.M. Differential Gene Regulation in the Ag Nanoparticle and Ag(+)-Induced Silver Stress Response in Escherichia Coli: A Full Transcriptomic Profile. Nanotoxicology. 2014;8((Suppl. 1)):177–184. doi: 10.3109/17435390.2013.870243. [DOI] [PubMed] [Google Scholar]
- 80.Mukha I.P., Eremenko A.M., Smirnova N.P., Mikhienkova A.I., Korchak G.I., Gorchev V.F., Chunikhin A.Y. Antimicrobial Activity of Stable Silver Nanoparticles of a Certain Size. Appl. Biochem. Microbiol. 2013;49:199–206. doi: 10.1134/S0003683813020117. [DOI] [PubMed] [Google Scholar]
- 81.Dong Y., Zhu H., Shen Y., Zhang W., Zhang L. Antibacterial Activity of Silver Nanoparticles of Different Particle Size against Vibrio Natriegens. PLoS ONE. 2019;14:e0222322. doi: 10.1371/journal.pone.0222322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Oves M., Rauf M.A., Hussain A., Qari H.A., Khan A.A.P., Muhammad P., Rehman M.T., Alajmi M.F., Ismail I.I.M. Antibacterial Silver Nanomaterial Synthesis From Mesoflavibacter Zeaxanthinifaciens and Targeting Biofilm Formation. Front. Pharmacol. 2019;10:801. doi: 10.3389/fphar.2019.00801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cui Y., Zhao Y., Tian Y., Zhang W., Lü X., Jiang X. The Molecular Mechanism of Action of Bactericidal Gold Nanoparticles on Escherichia Coli. Biomaterials. 2012;33:2327–2333. doi: 10.1016/j.biomaterials.2011.11.057. [DOI] [PubMed] [Google Scholar]
- 84.Lemire J.A., Harrison J.J., Turner R.J. Antimicrobial Activity of Metals: Mechanisms, Molecular Targets and Applications. Nat. Rev. Microbiol. 2013;11:371–384. doi: 10.1038/nrmicro3028. [DOI] [PubMed] [Google Scholar]
- 85.Chatterjee A.K., Chakraborty R., Basu T. Mechanism of Antibacterial Activity of Copper Nanoparticles. Nanotechnology. 2014;25:135101. doi: 10.1088/0957-4484/25/13/135101. [DOI] [PubMed] [Google Scholar]
- 86.Godoy-Gallardo M., Eckhard U., Delgado L.M., de Roo Puente Y.J.D., Hoyos-Nogués M., Gil F.J., Perez R.A. Antibacterial Approaches in Tissue Engineering Using Metal Ions and Nanoparticles: From Mechanisms to Applications. Bioact. Mater. 2021;6:4470–4490. doi: 10.1016/j.bioactmat.2021.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ishida T. Antibacterial Mechanism of Ag+ Ions for Bacteriolyses of Bacterial Cell Walls via Peptidoglycan Autolysins, and DNA Damages. MOJ Toxicol. 2018;4:345–350. doi: 10.15406/mojt.2018.04.00125. [DOI] [Google Scholar]
- 88.Saliani M., Jalal R., Goharshadi E.K. Effects of PH and Temperature on Antibacterial Activity of Zinc Oxide Nanofluid Against Escherichia Coli O157: H7 and Staphylococcus Aureus. Jundishapur J. Microbiol. 2015;8:e17115. doi: 10.5812/jjm.17115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Moreau J.W., Weber P.K., Martin M.C., Gilbert B., Hutcheon I.D., Banfield J.F. Extracellular Proteins Limit the Dispersal of Biogenic Nanoparticles. Science. 2007;316:1600–1603. doi: 10.1126/science.1141064. [DOI] [PubMed] [Google Scholar]
- 90.Peretyazhko T.S., Zhang Q., Colvin V.L. Size-Controlled Dissolution of Silver Nanoparticles at Neutral and Acidic PH Conditions: Kinetics and Size Changes. Environ. Sci. Technol. 2014;48:11954–11961. doi: 10.1021/es5023202. [DOI] [PubMed] [Google Scholar]
- 91.Wigginton N.S., de Titta A., Piccapietra F., Dobias J., Nesatyy V.J., Suter M.J.F., Bernier-Latmani R. Binding of Silver Nanoparticles to Bacterial Proteins Depends on Surface Modifications and Inhibits Enzymatic Activity. Environ. Sci. Technol. 2010;44:2163–2168. doi: 10.1021/es903187s. [DOI] [PubMed] [Google Scholar]
- 92.Chatterjee T., Chatterjee B.K., Majumdar D., Chakrabarti P. Antibacterial Effect of Silver Nanoparticles and the Modeling of Bacterial Growth Kinetics Using a Modified Gompertz Model. Biochim. Biophys. Acta Biomembr. 2015;1850:299–306. doi: 10.1016/j.bbagen.2014.10.022. [DOI] [PubMed] [Google Scholar]
- 93.Qiu T.A., Guidolin V., Hoang K.N.L., Pho T., Carra’ A., Villalta P.W., He J., Yao X., Hamers R.J., Balbo S., et al. Nanoscale Battery Cathode Materials Induce DNA Damage in Bacteria. Chem. Sci. 2020;11:11244–11258. doi: 10.1039/D0SC02987D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sharma V.K., Sayes C.M., Guo B., Pillai S., Parsons J.G., Wang C., Yan B., Ma X. Interactions between Silver Nanoparticles and Other Metal Nanoparticles under Environmentally Relevant Conditions: A Review. Sci. Total Environ. 2019;653:1042–1051. doi: 10.1016/j.scitotenv.2018.10.411. [DOI] [PubMed] [Google Scholar]
- 95.Levard C., Mitra S., Yang T., Jew A.D., Badireddy A.R., Lowry G.V., Brown G.E. Effect of Chloride on the Dissolution Rate of Silver Nanoparticles and Toxicity to E. Coli. Environ. Sci. Technol. 2013;47:5738–5745. doi: 10.1021/es400396f. [DOI] [PubMed] [Google Scholar]
- 96.Li Z., Greden K., Alvarez P.J.J., Gregory K.B., Lowry G.V. Adsorbed Polymer and NOM Limits Adhesion and Toxicity of Nano Scale Zerovalent Iron to E. Coli. Environ. Sci. Technol. 2010;44:3462–3467. doi: 10.1021/es9031198. [DOI] [PubMed] [Google Scholar]
- 97.Kim J.S., Kuk E., Yu K.N., Kim J.-H., Park S.J., Lee H.J., Kim S.H., Park Y.K., Park Y.H., Hwang C.-Y., et al. Antimicrobial Effects of Silver Nanoparticles. Nanomedicine. 2007;3:95–101. doi: 10.1016/j.nano.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 98.Ranjan S., Ramalingam C. Titanium Dioxide Nanoparticles Induce Bacterial Membrane Rupture by Reactive Oxygen Species Generation. Environ. Chem. Lett. 2016;14:487–494. doi: 10.1007/s10311-016-0586-y. [DOI] [Google Scholar]
- 99.Sirelkhatim A., Mahmud S., Seeni A., Kaus N.H.M., Ann L.C., Bakhori S.K.M., Hasan H., Mohamad D. Review on Zinc Oxide Nanoparticles: Antibacterial Activity and Toxicity Mechanism. Nano Micro Lett. 2015;7:219–242. doi: 10.1007/s40820-015-0040-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jung W.K., Koo H.C., Kim K.W., Shin S., Kim S.H., Park Y.H. Antibacterial Activity and Mechanism of Action of the Silver Ion in Staphylococcus Aureus and Escherichia Coli. Appl. Environ. Microbiol. 2008;74:2171–2178. doi: 10.1128/AEM.02001-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jahnke J.P., Cornejo J.A., Sumner J.J., Schuler A.J., Atanassov P., Ista L.K. Conjugated Gold Nanoparticles as a Tool for Probing the Bacterial Cell Envelope: The Case of Shewanella Oneidensis MR-1. Biointerphases. 2016;11:011003. doi: 10.1116/1.4939244. [DOI] [PubMed] [Google Scholar]
- 102.Ezraty B., Gennaris A., Barras F., Collet J.-F. Oxidative Stress, Protein Damage and Repair in Bacteria. Nat. Rev. Microbiol. 2017;15:385–396. doi: 10.1038/nrmicro.2017.26. [DOI] [PubMed] [Google Scholar]
- 103.Xu H., Qu F., Xu H., Lai W., Andrew Wang Y., Aguilar Z.P., Wei H. Role of Reactive Oxygen Species in the Antibacterial Mechanism of Silver Nanoparticles on Escherichia Coli O157:H7. Biometals. 2012;25:45–53. doi: 10.1007/s10534-011-9482-x. [DOI] [PubMed] [Google Scholar]
- 104.Choi O., Hu Z. Size Dependent and Reactive Oxygen Species Related Nanosilver Toxicity to Nitrifying Bacteria. Environ. Sci. Technol. 2008;42:4583–4588. doi: 10.1021/es703238h. [DOI] [PubMed] [Google Scholar]
- 105.Xie Y., He Y., Irwin P.L., Jin T., Shi X. Antibacterial Activity and Mechanism of Action of Zinc Oxide Nanoparticles against Campylobacter Jejuni. Appl. Environ. Microbiol. 2011;77:2325–2331. doi: 10.1128/AEM.02149-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mujeeb A.A., Khan N.A., Jamal F., Badre Alam K.F., Saeed H., Kazmi S., Alshameri A.W.F., Kashif M., Ghazi I., Owais M. Olax Scandens Mediated Biogenic Synthesis of Ag-Cu Nanocomposites: Potential Against Inhibition of Drug-Resistant Microbes. Front. Chem. 2020;8:103. doi: 10.3389/fchem.2020.00103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kumariya R., Sood S.K., Rajput Y.S., Saini N., Garsa A.K. Increased Membrane Surface Positive Charge and Altered Membrane Fluidity Leads to Cationic Antimicrobial Peptide Resistance in Enterococcus Faecalis. Biochim. Biophys. Acta Biomembr. 2015;1848:1367–1375. doi: 10.1016/j.bbamem.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 108.Jordan S., Hutchings M.I., Mascher T. Cell Envelope Stress Response in Gram-Positive Bacteria. FEMS Microbiol. Rev. 2008;32:107–146. doi: 10.1111/j.1574-6976.2007.00091.x. [DOI] [PubMed] [Google Scholar]
- 109.Tzeng Y.-L., Ambrose K.D., Zughaier S., Zhou X., Miller Y.K., Shafer W.M., Stephens D.S. Cationic Antimicrobial Peptide Resistance in Neisseria Meningitidis. J. Bacteriol. 2005;187:5387–5396. doi: 10.1128/JB.187.15.5387-5396.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Salusso A., Raimunda D. Defining the Roles of the Cation Diffusion Facilitators in Fe2+/Zn2+ Homeostasis and Establishment of Their Participation in Virulence in Pseudomonas Aeruginosa. Front. Cell. Infect. Microbiol. 2017;7:84. doi: 10.3389/fcimb.2017.00084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Niño-Martínez N., Salas Orozco M.F., Martínez-Castañón G.-A., Torres Méndez F., Ruiz F. Molecular Mechanisms of Bacterial Resistance to Metal and Metal Oxide Nanoparticles. Int. J. Mol. Sci. 2019;20:2808. doi: 10.3390/ijms20112808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Imran M., Das K.R., Naik M.M. Co-Selection of Multi-Antibiotic Resistance in Bacterial Pathogens in Metal and Microplastic Contaminated Environments: An Emerging Health Threat. Chemosphere. 2019;215:846–857. doi: 10.1016/j.chemosphere.2018.10.114. [DOI] [PubMed] [Google Scholar]
- 113.Ellis D.H., Maurer-Gardner E.I., Sulentic C.E.W., Hussain S.M. Silver Nanoparticle Antibacterial Efficacy and Resistance Development in Key Bacterial Species. Biomed. Phys. Eng. Express. 2018;5:015013. doi: 10.1088/2057-1976/aad5a7. [DOI] [Google Scholar]
- 114.Randall C.P., Gupta A., Jackson N., Busse D., O’Neill A.J. Silver Resistance in Gram-Negative Bacteria: A Dissection of Endogenous and Exogenous Mechanisms. J. Antimicrob. Chemother. 2015;70:1037–1046. doi: 10.1093/jac/dku523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Chandrangsu P., Rensing C., Helmann J.D. Metal Homeostasis and Resistance in Bacteria. Nat. Rev. Microbiol. 2017;15:338–350. doi: 10.1038/nrmicro.2017.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wang X., Yang F., Zhao J., Xu Y., Mao D., Zhu X., Luo Y., Alvarez P.J.J. Bacterial Exposure to ZnO Nanoparticles Facilitates Horizontal Transfer of Antibiotic Resistance Genes. NanoImpact. 2018;10:61–67. doi: 10.1016/j.impact.2017.11.006. [DOI] [Google Scholar]
- 117.Qiu Z., Shen Z., Qian D., Jin M., Yang D., Wang J., Zhang B., Yang Z., Chen Z., Wang X., et al. Effects of Nano-TiO2 on Antibiotic Resistance Transfer Mediated by RP4 Plasmid. Nanotoxicology. 2015;9:895–904. doi: 10.3109/17435390.2014.991429. [DOI] [PubMed] [Google Scholar]
- 118.Panáček A., Kvítek L., Smékalová M., Večeřová R., Kolář M., Röderová M., Dyčka F., Šebela M., Prucek R., Tomanec O., et al. Bacterial Resistance to Silver Nanoparticles and How to Overcome It. Nat. Nanotech. 2018;13:65–71. doi: 10.1038/s41565-017-0013-y. [DOI] [PubMed] [Google Scholar]
- 119.Faghihzadeh F., Anaya N.M., Astudillo-Castro C., Oyanedel-Craver V. Kinetic, Metabolic and Macromolecular Response of Bacteria to Chronic Nanoparticle Exposure in Continuous Culture. Environ. Sci. Nano. 2018;5:1386–1396. doi: 10.1039/C8EN00325D. [DOI] [Google Scholar]
- 120.Sohm B., Immel F., Bauda P., Pagnout C. Insight into the Primary Mode of Action of TiO2 Nanoparticles on Escherichia Coli in the Dark. Proteomics. 2015;15:98–113. doi: 10.1002/pmic.201400101. [DOI] [PubMed] [Google Scholar]
- 121.Liu J., Liu J., Attarilar S., Wang C., Tamaddon M., Yang C., Xie K., Yao J., Wang L., Liu C., et al. Nano-Modified Titanium Implant Materials: A Way Toward Improved Antibacterial Properties. Front. Bioeng. Biotechnol. 2020;8:576969. doi: 10.3389/fbioe.2020.576969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Chen M., Yang L., Zhang L., Han Y., Lu Z., Qin G., Zhang E. Effect of Nano/Micro-Ag Compound Particles on the Bio-Corrosion, Antibacterial Properties and Cell Biocompatibility of Ti-Ag Alloys. Mater. Sci. Eng. C. 2017;75:906–917. doi: 10.1016/j.msec.2017.02.142. [DOI] [PubMed] [Google Scholar]
- 123.Bakhsheshi-Rad H.R., Hamzah E., Low H.T., Kasiri-Asgarani M., Farahany S., Akbari E., Cho M.H. Fabrication of Biodegradable Zn-Al-Mg Alloy: Mechanical Properties, Corrosion Behavior, Cytotoxicity and Antibacterial Activities. Mater. Sci. Eng. C. 2017;73:215–219. doi: 10.1016/j.msec.2016.11.138. [DOI] [PubMed] [Google Scholar]
- 124.Cao H., Zhang W., Meng F., Guo J., Wang D., Qian S., Jiang X., Liu X., Chu P.K. Osteogenesis Catalyzed by Titanium-Supported Silver Nanoparticles. ACS Appl. Mater. Interfaces. 2017;9:5149–5157. doi: 10.1021/acsami.6b15448. [DOI] [PubMed] [Google Scholar]
- 125.Calabrese G., Franco D., Petralia S., Monforte F., Condorelli G.G., Squarzoni S., Traina F., Conoci S. Dual-Functional Nano-Functionalized Titanium Scaffolds to Inhibit Bacterial Growth and Enhance Osteointegration. Nanomaterials. 2021;11:2634. doi: 10.3390/nano11102634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Shahid A., Aslam B., Muzammil S., Aslam N., Shahid M., Almatroudi A., Allemailem K.S., Saqalein M., Nisar M.A., Rasool M.H., et al. The Prospects of Antimicrobial Coated Medical Implants. J. Appl. Biomater. Funct. Mater. 2021;19:22808000211040304. doi: 10.1177/22808000211040304. [DOI] [PubMed] [Google Scholar]
- 127.Dube T., Freckmann D., Conoci S., Gambarotta S., Yap G.P.A. Monomeric and Octameric Divalent Ytterbium Complexes of Diphenylmethyl Dipyrrolyl Dianion. Organometallics. 2000;19:209–211. doi: 10.1021/om990798z. [DOI] [Google Scholar]
- 128.Miola M., Bruno M., Maina G., Fucale G., Lucchetta G., Vernè E. Antibiotic-Free Composite Bone Cements with Antibacterial and Bioactive Properties. A Preliminary Study. Mater. Sci. Eng. C. 2014;43:65–75. doi: 10.1016/j.msec.2014.06.026. [DOI] [PubMed] [Google Scholar]
- 129.Kose N., Çaylak R., Pekşen C., Kiremitçi A., Burukoglu D., Koparal S., Doğan A. Silver Ion Doped Ceramic Nano-Powder Coated Nails Prevent Infection in Open Fractures: In Vivo Study. Injury. 2016;47:320–324. doi: 10.1016/j.injury.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 130.Samuel U., Guggenbichler J.P. Prevention of Catheter-Related Infections: The Potential of a New Nano-Silver Impregnated Catheter. Int. J. Antimicrob. Agents. 2004;23((Suppl. 1)):75–78. doi: 10.1016/j.ijantimicag.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 131.Galiano K., Pleifer C., Engelhardt K., Brössner G., Lackner P., Huck C., Lass-Flörl C., Obwegeser A. Silver Segregation and Bacterial Growth of Intraventricular Catheters Impregnated with Silver Nanoparticles in Cerebrospinal Fluid Drainages. Neurol. Res. 2008;30:285–287. doi: 10.1179/016164107X229902. [DOI] [PubMed] [Google Scholar]
- 132.Chen P., Wu Z., Leung A., Chen X., Landao-Bassonga E., Gao J., Chen L., Zheng M., Yao F., Yang H., et al. Fabrication of a Silver Nanoparticle-Coated Collagen Membrane with Anti-Bacterial and Anti-Inflammatory Activities for Guided Bone Regeneration. Biomed. Mater. 2018;13:065014. doi: 10.1088/1748-605X/aae15b. [DOI] [PubMed] [Google Scholar]
- 133.Ramazanzadeh B., Jahanbin A., Yaghoubi M., Shahtahmassbi N., Ghazvini K., Shakeri M., Shafaee H. Comparison of Antibacterial Effects of ZnO and CuO Nanoparticles Coated Brackets against Streptococcus Mutans. J. Dent. 2015;16:200–205. [PMC free article] [PubMed] [Google Scholar]
- 134.Li C., Fu R., Yu C., Li Z., Guan H., Hu D., Zhao D., Lu L. Silver Nanoparticle/Chitosan Oligosaccharide/Poly(Vinyl Alcohol) Nanofibers as Wound Dressings: A Preclinical Study. Int. J. Nanomed. 2013;8:4131–4145. doi: 10.2147/IJN.S51679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.dos Santos C.A., Ingle A.P., Rai M. The Emerging Role of Metallic Nanoparticles in Food. Appl. Microbiol. Biotechnol. 2020;104:2373–2383. doi: 10.1007/s00253-020-10372-x. [DOI] [PubMed] [Google Scholar]
- 136.Couto C., Almeida A. Metallic Nanoparticles in the Food Sector: A Mini-Review. Foods. 2022;11:402. doi: 10.3390/foods11030402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Singh S.P., Bhargava C.S., Dubey V., Mishra A., Singh Y. Silver Nanoparticles: Biomedical Applications, Toxicity, and Safety Issues. Int. J. Res. Pharm. Pharm. Sci. 2017;4:1–10. [Google Scholar]
- 138.Alsammarraie F.K., Wang W., Zhou P., Mustapha A., Lin M. Green Synthesis of Silver Nanoparticles Using Turmeric Extracts and Investigation of Their Antibacterial Activities. Colloids Surf. B Biointerfaces. 2018;171:398–405. doi: 10.1016/j.colsurfb.2018.07.059. [DOI] [PubMed] [Google Scholar]
- 139.Makvandi P., Ashrafizadeh M., Ghomi M., Najafi M., Hossein H.H.S., Zarrabi A., Mattoli V., Varma R.S. Injectable Hyaluronic Acid-Based Antibacterial Hydrogel Adorned with Biogenically Synthesized AgNPs-Decorated Multi-Walled Carbon Nanotubes. Prog. Biomater. 2021;10:77–89. doi: 10.1007/s40204-021-00155-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Makvandi P., Ali G.W., Della Sala F., Abdel-Fattah W.I., Borzacchiello A. Hyaluronic Acid/Corn Silk Extract Based Injectable Nanocomposite: A Biomimetic Antibacterial Scaffold for Bone Tissue Regeneration. Mater. Sci. Eng. C. 2020;107:110195. doi: 10.1016/j.msec.2019.110195. [DOI] [PubMed] [Google Scholar]
- 141.Ravindran D., Ramanathan S., Arunachalam K., Jeyaraj G.P., Shunmugiah K.P., Arumugam V.R. Phytosynthesized Silver Nanoparticles as Antiquorum Sensing and Antibiofilm Agent against the Nosocomial Pathogen Serratia Marcescens: An in Vitro Study. J. Appl. Microbiol. 2018;124:1425–1440. doi: 10.1111/jam.13728. [DOI] [PubMed] [Google Scholar]
- 142.Thomas R., Snigdha S., Bhavitha K.B., Babu S., Ajith A., Radhakrishnan E.K. Biofabricated Silver Nanoparticles Incorporated Polymethyl Methacrylate as a Dental Adhesive Material with Antibacterial and Antibiofilm Activity against Streptococcus Mutans. 3 Biotech. 2018;8:404. doi: 10.1007/s13205-018-1420-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kim M.H., Park H., Nam H.C., Park S.R., Jung J.-Y., Park W.H. Injectable Methylcellulose Hydrogel Containing Silver Oxide Nanoparticles for Burn Wound Healing. Carbohydr. Polym. 2018;181:579–586. doi: 10.1016/j.carbpol.2017.11.109. [DOI] [PubMed] [Google Scholar]
- 144.Hasan A., Morshed M., Memic A., Hassan S., Webster T.J., Marei H.E.-S. Nanoparticles in Tissue Engineering: Applications, Challenges and Prospects. Int. J. Nanomed. 2018;13:5637–5655. doi: 10.2147/IJN.S153758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Jamróz E., Cabaj A., Juszczak L., Tkaczewska J., Zimowska M., Cholewa-Wójcik A., Krzyściak P., Kopel P. Active Double-Layered Films Enriched with AgNPs in Great Water Dock Root and Pu-Erh Extracts. Materials. 2021;14:6925. doi: 10.3390/ma14226925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Myakinin A., Turlybekuly A., Pogrebnjak A., Mirek A., Bechelany M., Liubchak I., Oleshko O., Husak Y., Korniienko V., Leśniak-Ziółkowska K., et al. In Vitro Evaluation of Electrochemically Bioactivated Ti6Al4V 3D Porous Scaffolds. Mater. Sci. Eng. C. 2021;121:111870. doi: 10.1016/j.msec.2021.111870. [DOI] [PubMed] [Google Scholar]
- 147.Cochis A., Azzimonti B., Della Valle C., De Giglio E., Bloise N., Visai L., Cometa S., Rimondini L., Chiesa R. The Effect of Silver or Gallium Doped Titanium against the Multidrug Resistant Acinetobacter Baumannii. Biomaterials. 2016;80:80–95. doi: 10.1016/j.biomaterials.2015.11.042. [DOI] [PubMed] [Google Scholar]
- 148.Felix W.P., Muthu P. Bioscaffolds Impregnated with Ormocarpum Cochinchinense Mediated Ag Nanoparticles; Proceedings of the 2016 International Conference on Electrical, Electronics, and Optimization Techniques (ICEEOT); Chennai, India. 3–5 March 2016; pp. 3533–3535. [Google Scholar]
- 149.Shimazaki T., Miyamoto H., Ando Y., Noda I., Yonekura Y., Kawano S., Miyazaki M., Mawatari M., Hotokebuchi T. In Vivo Antibacterial and Silver-Releasing Properties of Novel Thermal Sprayed Silver-Containing Hydroxyapatite Coating. J. Biomed. Mater. Res. B Appl. Biomater. 2010;92:386–389. doi: 10.1002/jbm.b.31526. [DOI] [PubMed] [Google Scholar]
- 150.Saravanan S., Nethala S., Pattnaik S., Tripathi A., Moorthi A., Selvamurugan N. Preparation, Characterization and Antimicrobial Activity of a Bio-Composite Scaffold Containing Chitosan/Nano-Hydroxyapatite/Nano-Silver for Bone Tissue Engineering. Int. J. Biol. Macromol. 2011;49:188–193. doi: 10.1016/j.ijbiomac.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 151.Alt V., Bechert T., Steinrücke P., Wagener M., Seidel P., Dingeldein E., Domann E., Schnettler R. An in Vitro Assessment of the Antibacterial Properties and Cytotoxicity of Nanoparticulate Silver Bone Cement. Biomaterials. 2004;25:4383–4391. doi: 10.1016/j.biomaterials.2003.10.078. [DOI] [PubMed] [Google Scholar]
- 152.Halkai K.R., Mudda J.A., Shivanna V., Rathod V., Halkai R.S. Biosynthesis, Characterization and Antibacterial Efficacy of Silver Nanoparticles Derived from Endophytic Fungi against P. Gingivalis. J. Clin. Diagn. Res. 2017;11:ZC92–ZC96. doi: 10.7860/JCDR/2017/29434.10681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Halkai K.R., Mudda J.A., Shivanna V., Rathod V., Halkai R.S. Evaluation of Antibacterial Efficacy of Biosynthesized Silver Nanoparticles Derived from Fungi against Endo-Perio Pathogens Porphyromonas Gingivalis, Bacillus Pumilus, and Enterococcus Faecalis. J. Conserv. Dent. 2017;20:398–404. doi: 10.4103/JCD.JCD_173_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Science (IJDOS) Effectiveness of a Novel Nano-Silver Fluoride with Green Tea Extract Compared with Silver Diamine Fluoride: A Randomized, Controlled, Non-Inferiority Trial. SciDoc Publishers; Lewes, DE, USA: 2020. Research Article. [Google Scholar]
- 155.Sundeep D., Vijaya Kumar T., Rao P.S.S., Ravikumar R.V.S.S.N., Gopala Krishna A. Green Synthesis and Characterization of Ag Nanoparticles from Mangifera Indica Leaves for Dental Restoration and Antibacterial Applications. Prog. Biomater. 2017;6:57–66. doi: 10.1007/s40204-017-0067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Mala R., Annie Aglin A., Ruby Celsia A.S., Geerthika S., Kiruthika N., VazagaPriya C., Srinivasa Kumar K. Foley Catheters Functionalised with a Synergistic Combination of Antibiotics and Silver Nanoparticles Resist Biofilm Formation. IET Nanobiotechnol. 2017;11:612–620. doi: 10.1049/iet-nbt.2016.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Wu K., Yang Y., Zhang Y., Deng J., Lin C. Antimicrobial Activity and Cytocompatibility of Silver Nanoparticles Coated Catheters via a Biomimetic Surface Functionalization Strategy. Int. J. Nanomed. 2015;10:7241–7252. doi: 10.2147/IJN.S92307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Fufă O., Andronescu E., Grumezescu V., Holban A., Mogoanta L., Mogoșanu G., Socol G., Iordache F., Chifiriuc M., Grumezescu A. Silver Nanostructurated Surfaces Prepared by MAPLE for Biofilm Prevention. Biointerface Res. Appl. Chem. 2015;5:1011–1017. [Google Scholar]
- 159.Walker J.N., Flores-Mireles A.L., Pinkner C.L., Schreiber H.L., Joens M.S., Park A.M., Potretzke A.M., Bauman T.M., Pinkner J.S., Fitzpatrick J.A.J., et al. Catheterization Alters Bladder Ecology to Potentiate Staphylococcus Aureus Infection of the Urinary Tract. Proc. Natl. Acad. Sci. USA. 2017;114:E8721–E8730. doi: 10.1073/pnas.1707572114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Wilkinson L.J., White R.J., Chipman J.K. Silver and Nanoparticles of Silver in Wound Dressings: A Review of Efficacy and Safety. J. Wound Care. 2011;20:543–549. doi: 10.12968/jowc.2011.20.11.543. [DOI] [PubMed] [Google Scholar]
- 161.Thomas R., Nair A.P., Kr S., Mathew J., Ek R. Antibacterial Activity and Synergistic Effect of Biosynthesized AgNPs with Antibiotics against Multidrug-Resistant Biofilm-Forming Coagulase-Negative Staphylococci Isolated from Clinical Samples. Appl. Biochem. Biotechnol. 2014;173:449–460. doi: 10.1007/s12010-014-0852-z. [DOI] [PubMed] [Google Scholar]
- 162.Seth D., Choudhury S.R., Pradhan S., Gupta S., Palit D., Das S., Debnath N., Goswami A. Nature-Inspired Novel Drug Design Paradigm Using Nanosilver: Efficacy on Multi-Drug-Resistant Clinical Isolates of Tuberculosis. Curr. Microbiol. 2010;62:715–726. doi: 10.1007/s00284-010-9770-7. [DOI] [PubMed] [Google Scholar]
- 163.Zhang M., Zhang K., De Gusseme B., Verstraete W., Field R. The Antibacterial and Anti-Biofouling Performance of Biogenic Silver Nanoparticles by Lactobacillus Fermentum. Biofouling. 2014;30:347–357. doi: 10.1080/08927014.2013.873419. [DOI] [PubMed] [Google Scholar]
- 164.Russo T., Gloria A., De Santis R., D’Amora U., Balato G., Vollaro A., Oliviero O., Improta G., Triassi M., Ambrosio L. Preliminary Focus on the Mechanical and Antibacterial Activity of a PMMA-Based Bone Cement Loaded with Gold Nanoparticles. Bioact. Mater. 2017;2:156–161. doi: 10.1016/j.bioactmat.2017.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Zheng K., Setyawati M.I., Leong D.T., Xie J. Antimicrobial Gold Nanoclusters. ACS Nano. 2017;11:6904–6910. doi: 10.1021/acsnano.7b02035. [DOI] [PubMed] [Google Scholar]
- 166.Han S., Han K., Hong J., Yoon D.-Y., Park C., Kim Y. Photothermal Cellulose-Patch with Gold-Spiked Silica Microrods Based on Escherichia Coli. ACS Omega. 2018;3:5244–5251. doi: 10.1021/acsomega.8b00639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Calabrese G., Petralia S., Fabbi C., Forte S., Franco D., Guglielmino S., Esposito E., Cuzzocrea S., Traina F., Conoci S. Au, Pd and Maghemite Nanofunctionalized Hydroxyapatite Scaffolds for Bone Regeneration. Regen. Biomater. 2020;7:461–469. doi: 10.1093/rb/rbaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Bucharskaya A., Maslyakova G., Terentyuk G., Yakunin A., Avetisyan Y., Bibikova O., Tuchina E., Khlebtsov B., Khlebtsov N., Tuchin V. Towards Effective Photothermal/Photodynamic Treatment Using Plasmonic Gold Nanoparticles. Int. J. Mol. Sci. 2016;17:1295. doi: 10.3390/ijms17081295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Ma H., Li Z., Xue N., Cheng Z., Miao X. A Gold Nanoparticle Based Fluorescent Probe for Simultaneous Recognition of Single-Stranded DNA and Double-Stranded DNA. Mikrochim. Acta. 2018;185:93. doi: 10.1007/s00604-017-2633-1. [DOI] [PubMed] [Google Scholar]
- 170.Zhang Y., Zhang C., Xu C., Wang X., Liu C., Waterhouse G.I.N., Wang Y., Yin H. Ultrasmall Au Nanoclusters for Biomedical and Biosensing Applications: A Mini-Review. Talanta. 2019;200:432–442. doi: 10.1016/j.talanta.2019.03.068. [DOI] [PubMed] [Google Scholar]
- 171.Kailasa S.K., Park T.-J., Rohit J.V., Koduru J.R. Chapter 14—Antimicrobial Activity of Silver Nanoparticles. In: Grumezescu A.M., editor. Nanoparticles in Pharmacotherapy. William Andrew Publishing; Norwich, NY, USA: 2019. pp. 461–484. [Google Scholar]
- 172.Salah I., Parkin I.P., Allan E. Copper as an Antimicrobial Agent: Recent Advances. RSC Adv. 2021;11:18179–18186. doi: 10.1039/D1RA02149D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Müller D.W., Lößlein S., Terriac E., Brix K., Siems K., Moeller R., Kautenburger R., Mücklich F. Increasing Antibacterial Efficiency of Cu Surfaces by Targeted Surface Functionalization via Ultrashort Pulsed Direct Laser Interference Patterning. Adv. Mater. Interfaces. 2021;8:2001656. doi: 10.1002/admi.202001656. [DOI] [Google Scholar]
- 174.Wang P., Yuan Y., Xu K., Zhong H., Yang Y., Jin S., Yang K., Qi X. Biological Applications of Copper-Containing Materials. Bioact. Mater. 2020;6:916–927. doi: 10.1016/j.bioactmat.2020.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Li M., Gao L., Schlaich C., Zhang J., Donskyi I.S., Yu G., Li W., Tu Z., Rolff J., Schwerdtle T., et al. Construction of Functional Coatings with Durable and Broad-Spectrum Antibacterial Potential Based on Mussel-Inspired Dendritic Polyglycerol and in Situ-Formed Copper Nanoparticles. ACS Appl. Mater. Interfaces. 2017;9:35411–35418. doi: 10.1021/acsami.7b10541. [DOI] [PubMed] [Google Scholar]
- 176.Harikumar P.S., Aravind A. Antibacterial Activity of Copper Nanoparticles and Copper Nanocomposites against Escherichia Coli Bacteria. Int. J. Sci. 2016;5:83–90. doi: 10.18483/ijSci.957. [DOI] [Google Scholar]
- 177.Dadi R., Azouani R., Traore M., Mielcarek C., Kanaev A. Antibacterial Activity of ZnO and CuO Nanoparticles against Gram Positive and Gram Negative Strains. Mater. Sci. Eng. C. 2019;104:109968. doi: 10.1016/j.msec.2019.109968. [DOI] [PubMed] [Google Scholar]
- 178.Khan Z., Al-Thabaiti S.A. Green Synthesis of Zero-Valent Fe-Nanoparticles: Catalytic Degradation of Rhodamine B, Interactions with Bovine Serum Albumin and Their Enhanced Antimicrobial Activities. J. Photochem. Photobiol. B Biol. 2018;180:259–267. doi: 10.1016/j.jphotobiol.2018.02.017. [DOI] [PubMed] [Google Scholar]
- 179.Yoon H., Kang Y.-G., Chang Y.-S., Kim J.-H. Effects of Zerovalent Iron Nanoparticles on Photosynthesis and Biochemical Adaptation of Soil-Grown Arabidopsis Thaliana. Nanomaterials. 2019;9:1543. doi: 10.3390/nano9111543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Nehra P., Chauhan R.P., Garg N., Verma K. Antibacterial and Antifungal Activity of Chitosan Coated Iron Oxide Nanoparticles. Br. J. Biomed. Sci. 2018;75:13–18. doi: 10.1080/09674845.2017.1347362. [DOI] [PubMed] [Google Scholar]
- 181.Wu W., Jiang C.Z., Roy V.A.L. Designed Synthesis and Surface Engineering Strategies of Magnetic Iron Oxide Nanoparticles for Biomedical Applications. Nanoscale. 2016;8:19421–19474. doi: 10.1039/C6NR07542H. [DOI] [PubMed] [Google Scholar]
- 182.Hasanova U., Ramazanov M., Maharramov A., Eyvazova Q., Aghamaliyev Z., Parfyonova Y., Hajiyeva S., Hajiyeva F., Veliyeva S. Nano-Coupling of Cephalosporin Antibiotics with Fe3O4 Nanoparticles: Trojan Horse Approach in Antimicrobial Chemotherapy of Infections Caused by Klebsiella spp. J. Biomater. Nanobiotechnol. 2015;06:225–235. doi: 10.4236/jbnb.2015.63021. [DOI] [Google Scholar]
- 183.Ali K., Ahmed B., Khan M.S., Musarrat J. Differential Surface Contact Killing of Pristine and Low EPS Pseudomonas Aeruginosa with Aloe Vera Capped Hematite (α-Fe2O3) Nanoparticles. J. Photochem. Photobiol. B Biol. 2018;188:146–158. doi: 10.1016/j.jphotobiol.2018.09.017. [DOI] [PubMed] [Google Scholar]
- 184.Bukhari S., Kim D., Liu Y., Karabucak B., Koo H. Novel Endodontic Disinfection Approach Using Catalytic Nanoparticles. J. Endod. 2018;44:806–812. doi: 10.1016/j.joen.2017.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Parveen S., Wani A.H., Shah M.A., Devi H.S., Bhat M.Y., Koka J.A. Preparation, Characterization and Antifungal Activity of Iron Oxide Nanoparticles. Microb. Pathog. 2018;115:287–292. doi: 10.1016/j.micpath.2017.12.068. [DOI] [PubMed] [Google Scholar]
- 186.Rafi M.M., Ahmed K.S.Z., Premnazeer K., Kumar D.S. Antibacterial Activity of Iron Oxide Nanoparticles on Polysaccharide Templates: Synthesis, Characterization and Magnetic Studies. Malays. Polym. J. 2015;10:16–22. [Google Scholar]
- 187.Ranmadugala D., Ebrahiminezhad A., Manley-Harris M., Ghasemi Y., Berenjian A. Impact of 3–Aminopropyltriethoxysilane-Coated Iron Oxide Nanoparticles on Menaquinone-7 Production Using B. Subtilis. Nanomaterials. 2017;7:350. doi: 10.3390/nano7110350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.El Nahrawy A.M., Abou Hammad A.B., Mansour A.M. Preparation and Characterization of Transparent Semiconducting Silica Nanocomposites Doped with P2O5 and Al2O3. Silicon. 2021;13:3733–3739. doi: 10.1007/s12633-021-00962-3. [DOI] [Google Scholar]
- 189.Liakos I.L., Abdellatif M.H., Innocenti C., Scarpellini A., Carzino R., Brunetti V., Marras S., Brescia R., Drago F., Pompa P.P. Antimicrobial Lemongrass Essential Oil—Copper Ferrite Cellulose Acetate Nanocapsules. Molecules. 2016;21:520. doi: 10.3390/molecules21040520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Samavati A., Ismail A.F. Antibacterial Properties of Copper-Substituted Cobalt Ferrite Nanoparticles Synthesized by Co-Precipitation Method. Particuology. 2017;30:158–163. doi: 10.1016/j.partic.2016.06.003. [DOI] [Google Scholar]
- 191.Biswas K., De D., Bandyopadhyay J., Dutta N., Rana S., Sen P., Bandyopadhyay S.K., Chakraborty P.K. Enhanced Polarization, Magnetic Response and Pronounced Antibacterial Activity of Bismuth Ferrite Nanorods. Mater. Chem. Phys. 2017;195:207–212. doi: 10.1016/j.matchemphys.2017.04.020. [DOI] [Google Scholar]
- 192.Žalnėravičius R., Paškevičius A., Mažeika K., Jagminas A. Fe(II)-Substituted Cobalt Ferrite Nanoparticles against Multidrug Resistant Microorganisms. Appl. Surf. Sci. 2018;435:141–148. doi: 10.1016/j.apsusc.2017.11.028. [DOI] [Google Scholar]
- 193.Wang C., Gu B., Liu Q., Pang Y., Xiao R., Wang S. Combined Use of Vancomycin-Modified Ag-Coated Magnetic Nanoparticles and Secondary Enhanced Nanoparticles for Rapid Surface-Enhanced Raman Scattering Detection of Bacteria. Int. J. Nanomed. 2018;13:1159–1178. doi: 10.2147/IJN.S150336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Esteban Florez F.L., Hiers R.D., Larson P., Johnson M., O’Rear E., Rondinone A.J., Khajotia S.S. Antibacterial Dental Adhesive Resins Containing Nitrogen-Doped Titanium Dioxide Nanoparticles. Mater. Sci. Eng. C. 2018;93:931–943. doi: 10.1016/j.msec.2018.08.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Chen R., Han Z., Huang Z., Karki J., Wang C., Zhu B., Zhang X. Antibacterial Activity, Cytotoxicity and Mechanical Behavior of Nano-Enhanced Denture Base Resin with Different Kinds of Inorganic Antibacterial Agents. Dent. Mater. J. 2017;36:693–699. doi: 10.4012/dmj.2016-301. [DOI] [PubMed] [Google Scholar]
- 196.Ono Y., Iwahashi H. Titanium Dioxide Nanoparticles Impart Protection from Ultraviolet Irradiation to Fermenting Yeast Cells. Biochem. Biophys. Rep. 2022;30:101221. doi: 10.1016/j.bbrep.2022.101221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Rodríguez-González V., Obregón S., Patrón-Soberano O.A., Terashima C., Fujishima A. An Approach to the Photocatalytic Mechanism in the TiO2-Nanomaterials Microorganism Interface for the Control of Infectious Processes. Appl. Catal. B Environ. 2020;270:118853. doi: 10.1016/j.apcatb.2020.118853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Viet P.V., Phan B.T., Mott D., Maenosono S., Sang T.T., Thi C.M., Hieu L.V. Silver Nanoparticle Loaded TiO2 Nanotubes with High Photocatalytic and Antibacterial Activity Synthesized by Photoreduction Method. J. Photochem. Photobiol. A Chem. 2018;352:106–112. doi: 10.1016/j.jphotochem.2017.10.051. [DOI] [Google Scholar]
- 199.Anaya-Esparza L.M., Villagrán-de la Mora Z., Ruvalcaba-Gómez J.M., Romero-Toledo R., Sandoval-Contreras T., Aguilera-Aguirre S., Montalvo-González E., Pérez-Larios A. Use of Titanium Dioxide (TiO2) Nanoparticles as Reinforcement Agent of Polysaccharide-Based Materials. Processes. 2020;8:1395. doi: 10.3390/pr8111395. [DOI] [Google Scholar]
- 200.Jin S.-E., Jin J.E., Hwang W., Hong S.W. Photocatalytic Antibacterial Application of Zinc Oxide Nanoparticles and Self-Assembled Networks under Dual UV Irradiation for Enhanced Disinfection. Int. J. Nanomed. 2019;14:1737–1751. doi: 10.2147/IJN.S192277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Lu P.-J., Huang S.-C., Chen Y.-P., Chiueh L.-C., Shih D.Y.-C. Analysis of Titanium Dioxide and Zinc Oxide Nanoparticles in Cosmetics. J. Food Drug Anal. 2015;23:587–594. doi: 10.1016/j.jfda.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Baek S., Joo S.H., Kumar N., Toborek M. Antibacterial Effect and Toxicity Pathways of Industrial and Sunscreen ZnO Nanoparticles on Escherichia Coli. J. Environ. Chem. Eng. 2017;5:3024–3032. doi: 10.1016/j.jece.2017.06.009. [DOI] [Google Scholar]
- 203.Lu P.J., Fang S.W., Cheng W.L., Huang S.C., Huang M.C., Cheng H.F. Characterization of Titanium Dioxide and Zinc Oxide Nanoparticles in Sunscreen Powder by Comparing Different Measurement Methods. J. Food Drug Anal. 2018;26:1192–1200. doi: 10.1016/j.jfda.2018.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Kumar S., Mudai A., Roy B., Basumatary I.B., Mukherjee A., Dutta J. Biodegradable Hybrid Nanocomposite of Chitosan/Gelatin and Green Synthesized Zinc Oxide Nanoparticles for Food Packaging. Foods. 2020;9:1143. doi: 10.3390/foods9091143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Valencia G.A., Zare E.N., Makvandi P., Gutiérrez T.J. Self-Assembled Carbohydrate Polymers for Food Applications: A Review. Compr. Rev. Food Sci. Food Saf. 2019;18:2009–2024. doi: 10.1111/1541-4337.12499. [DOI] [PubMed] [Google Scholar]
- 206.Zare E.N., Makvandi P., Borzacchiello A., Tay F.R., Ashtari B., Padil V.V.T. Antimicrobial Gum Bio-Based Nanocomposites and Their Industrial and Biomedical Applications. Chem. Commun. 2019;55:14871–14885. doi: 10.1039/C9CC08207G. [DOI] [PubMed] [Google Scholar]
- 207.Tüzüner T., Güçlü Z.A., Hurt A., Coleman N., Nicholson J. Release of Antimicrobial Compounds from a Zinc Oxide-Chelate Cement. J. Oral Sci. 2018;60:24–28. doi: 10.2334/josnusd.16-0791. [DOI] [PubMed] [Google Scholar]
- 208.Andrade V., Martínez A., Rojas N., Bello-Toledo H., Flores P., Sánchez-Sanhueza G., Catalán A. Antibacterial Activity against Streptococcus Mutans and Diametrical Tensile Strength of an Interim Cement Modified with Zinc Oxide Nanoparticles and Terpenes: An in Vitro Study. J. Prosthet. Dent. 2018;119:862.e1–862.e7. doi: 10.1016/j.prosdent.2017.09.015. [DOI] [PubMed] [Google Scholar]
- 209.Garcia I.M., Balhaddad A.A., Ibrahim M.S., Weir M.D., Xu H.H.K., Collares F.M., Melo M.A.S. Antibacterial Response of Oral Microcosm Biofilm to Nano-Zinc Oxide in Adhesive Resin. Dent. Mater. 2021;37:e182–e193. doi: 10.1016/j.dental.2020.11.022. [DOI] [PubMed] [Google Scholar]
- 210.Mishra P.K., Mishra H., Ekielski A., Talegaonkar S., Vaidya B. Zinc Oxide Nanoparticles: A Promising Nanomaterial for Biomedical Applications. Drug Discov. Today. 2017;22:1825–1834. doi: 10.1016/j.drudis.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 211.Barma M.D., Muthupandiyan I., Samuel S.R., Amaechi B.T. Inhibition of Streptococcus Mutans, Antioxidant Property and Cytotoxicity of Novel Nano-Zinc Oxide Varnish. Arch. Oral Biol. 2021;126:105132. doi: 10.1016/j.archoralbio.2021.105132. [DOI] [PubMed] [Google Scholar]
- 212.Kachoei M., Divband B., Rahbar M., Esmaeilzadeh M., Ghanizadeh M., Alam M. A Novel Developed Bioactive Composite Resin Containing Silver/Zinc Oxide (Ag/ZnO) Nanoparticles as an Antimicrobial Material against Streptococcus Mutans, Lactobacillus, and Candida Albicans. Evid. Based Complement. Alternat. Med. 2021;2021:4743411. doi: 10.1155/2021/4743411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Shimabukuro M., Tsutsumi Y., Nozaki K., Chen P., Yamada R., Ashida M., Doi H., Nagai A., Hanawa T. Chemical and Biological Roles of Zinc in a Porous Titanium Dioxide Layer Formed by Micro-Arc Oxidation. Coatings. 2019;9:705. doi: 10.3390/coatings9110705. [DOI] [Google Scholar]
- 214.Chouirfa H., Bouloussa H., Migonney V., Falentin-Daudré C. Review of Titanium Surface Modification Techniques and Coatings for Antibacterial Applications. Acta Biomater. 2019;83:37–54. doi: 10.1016/j.actbio.2018.10.036. [DOI] [PubMed] [Google Scholar]
- 215.Maleki-Ghaleh H., Siadati M.H., Fallah A., Koc B., Kavanlouei M., Khademi-Azandehi P., Moradpur-Tari E., Omidi Y., Barar J., Beygi-Khosrowshahi Y., et al. Antibacterial and Cellular Behaviors of Novel Zinc-Doped Hydroxyapatite/Graphene Nanocomposite for Bone Tissue Engineering. Int. J. Mol. Sci. 2021;22:9564. doi: 10.3390/ijms22179564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.He J., Feng W., Zhao B.-H., Zhang W., Lin Z. In Vivo Effect of Titanium Implants with Porous Zinc-Containing Coatings Prepared by Plasma Electrolytic Oxidation Method on Osseointegration in Rabbits. Int. J. Oral Maxillofac. Implants. 2018;33:298–310. doi: 10.11607/jomi.5764. [DOI] [PubMed] [Google Scholar]
- 217.Hemeg H.A. Nanomaterials for Alternative Antibacterial Therapy. Int. J. Nanomed. 2017;12:8211–8225. doi: 10.2147/IJN.S132163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Spirescu V.A., Chircov C., Grumezescu A.M., Vasile B.Ș., Andronescu E. Inorganic Nanoparticles and Composite Films for Antimicrobial Therapies. Int. J. Mol. Sci. 2021;22:4595. doi: 10.3390/ijms22094595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Maliszewska I., Sadowski Z. Synthesis and Antibacterial Activity of of Silver Nanoparticles. J. Phys. Conf. Ser. 2009;146:012024. doi: 10.1088/1742-6596/146/1/012024. [DOI] [Google Scholar]
- 220.AlMasoud N., Alhaik H., Almutairi M., Houjak A., Hazazi K., Alhayek F., Aljanoubi S., Alkhaibari A., Alghamdi A., Soliman D.A., et al. Green Nanotechnology Synthesized Silver Nanoparticles: Characterization and Testing Its Antibacterial Activity. Green Process. Synth. 2021;10:518–528. doi: 10.1515/gps-2021-0048. [DOI] [Google Scholar]
- 221.Huh A.J., Kwon Y.J. “Nanoantibiotics”: A New Paradigm for Treating Infectious Diseases Using Nanomaterials in the Antibiotics Resistant Era. J. Control. Release. 2011;156:128–145. doi: 10.1016/j.jconrel.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 222.Zhang X.-F., Liu Z.-G., Shen W., Gurunathan S. Silver Nanoparticles: Synthesis, Characterization, Properties, Applications, and Therapeutic Approaches. Int. J. Mol. Sci. 2016;17:1534. doi: 10.3390/ijms17091534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Mitra D., Kang E.-T., Neoh K.G. Antimicrobial Copper-Based Materials and Coatings: Potential Multifaceted Biomedical Applications. ACS Appl. Mater. Interfaces. 2020;12:21159–21182. doi: 10.1021/acsami.9b17815. [DOI] [PubMed] [Google Scholar]
- 224.Abdel-Kareem M.M., Zohri A.A. Extracellular Mycosynthesis of Gold Nanoparticles Using Trichoderma Hamatum: Optimization, Characterization and Antimicrobial Activity. Lett. Appl. Microbiol. 2018;67:465–475. doi: 10.1111/lam.13055. [DOI] [PubMed] [Google Scholar]
- 225.Vijayakumar S., Krishnakumar C., Arulmozhi P., Mahadevan S., Parameswari N. Biosynthesis, Characterization and Antimicrobial Activities of Zinc Oxide Nanoparticles from Leaf Extract of Glycosmis Pentaphylla (Retz.) DC. Microb. Pathog. 2018;116:44–48. doi: 10.1016/j.micpath.2018.01.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.