Abstract
Objective
The American Heart Association (AHA) proposed the concept of ideal cardiovascular health (CVH) to reduce the risk of cardiovascular mortality. We attempted to broaden the impact of CVH and further contribute to AHA 2030 goals by identifying the relationship between CVH and non-cardiovascular diseases such as sarcopenia.
Design
Cross-sectional survey
Setting
National Health and Nutrition Examination Survey conducted in the USA from 2011 to 2018.
Participants
This study included participants with reliable first 24-hour dietary recall and ≥20 years of age and excluded those who could not diagnose sarcopenia or insufficient data to calculate the CVH scores.
Primary and secondary outcome measures
The prevalence of sarcopenia as measured by dual-energy X-ray absorptiometry.
Results
This cohort study involving 9326 adults≥20 years comprised 4733 females (50.0%). The number of intermediate or ideal and poor CVH participants was 5654 and 3672 with mean CVH score of 9.70±0.03 and 5.66±0.04, respectively. After adjusting for related confounding factors, intermediate or ideal CVH was associated with an odds reduction of sarcopenia than poor CVH (adjusted OR (aOR): 0.36, 95% CI 0.26 to 0.50, p<0.001) and the odds of sarcopenia was significantly lower for each incremental increase of 1 in CVH metrics (aOR: 0.75, 95% CI 0.71 to 0.79, p<0.001). Moreover, if the number of ideal CVH metrics was>5, the odds of sarcopenia decreased by up to 84% (aOR: 0.16, 95% CI 0.08 to 0.30).
Conclusions
Our findings suggest a relationship between the CVH and the prevalence of sarcopenia in adults. The results of our study can contribute to achieving the 2030 public health goal of achieving CVH for all, which may be supported by efforts to reduce the prevalence of sarcopenia.
Keywords: Cardiology, Adult cardiology, Public health
Strengths and limitations of this study.
The main strength of this study is the large sample representative of the adult population of the USA.
Use of a validated survey instrument and standardised data collection methods allows for comparison with other studies.
The limitations of this study were that data were derived from cross-sectional studies and that the relationship was not necessarily identified as causal.
Use of self-reported data might result in recall bias.
A half of initial cohort has been excluded in this study, which will increase the variance of the OR estimates.
Introduction
Life expectancy in the USA has been stagnant since 2010 which has been attributed to a lack of progress in cardiovascular disease (CVD) mortality.1 Indeed, CVD remains the primary cause of mortality globally and a huge burden on public health expenditure.2 Previous investigators have used the Framingham and SCORE risk estimation systems to assess a patient’s risk for CVD.3 4 These risk scores are primarily derived from the development and establishment of effective primary and secondary prevention interventions for high-risk populations. However, individuals with significantly elevated levels of risk factors are relatively uncommon in the population. Most CVD and stroke events occur in individuals with average or only slightly unfavourable levels of risk factors. Therefore, the concept of cardiovascular health (CVH) was introduced to reduce the risk of cardiovascular mortality in 2010.5 CVH includes seven metrics, including body mass index (BMI), cigarette smoking, physical activity, dietary intake, total cholesterol level, blood pressure, and fasting glucose level.5 The beneficial effects of ideal CVH metrics are widely supported by mounts of scientific research.6 However, a recent study showed that the prevalence of ideal CVH status is low on some metrics, such as dietary pattern.7 Moreover, a study involving the offspring of Framingham participants showed that the decreasing presence of ideal CVH metrics over the past 20 years has resulted in increasing risks of subclinical diseases, CVDs and death.8 Therefore, there is a long way to go regarding the ‘Strategic Impact Goals for 2030 and Beyond’ issued by the American Heart Association (AHA).
Previous studies have suggested that an ideal CVH is negatively associated with age-related diseases.9 Sarcopenia, marked by the age-related loss of muscle mass, strength and function, has become a severe medical problem in the current ageing society. A meta-analysis indicated that patients with sarcopenia have decreased function, and higher rates of falls and hospitalisation.10 Sarcopenia shares many common pathogenic mechanisms with CVDs, such as hormonal changes, inflammation and oxidative stress.11 Studies have confirmed that sarcopenia is significantly associated with increased cardiovascular events or mortality,12 and patients with CVDs are also more likely to develop sarcopenia than age-matched controls.13
Although several studies have explored the relationship between cardiovascular risk factors and sarcopenia,14 it remains unclear whether ideal CVH metrics are beneficial in sarcopenic populations.
This study aimed to determine the relationship between CVH and sarcopenia by using the 2011–2018 National Health and Nutrition Examination Survey (NHANES) data to contribute to the accomplishment of the AHA 2030 goals.
Methods
Patient and public involvement
NHANES is a nationally representative health survey designed and administered by the National Center for Health Statistics (NCHS) at the Centers for Disease Control and Prevention and was approved by the NCHS Research Ethics Review Board (protocols Numbers: NHANES Protocol #2011-17 and NHANES Protocol #2018-01). The NHANES was designed to represent the civilian non-institutionalised US population using a complex multistage probability sampling methodology. We conducted a retrospective analysis of a cohort of US population of the NHANES from 2011 to 2018. Written informed consent was acquired from each NHANES participant. The NHANES includes extensive demographic data, physical examinations, laboratory tests, health-related questionnaires and lists of prescription medications, which were measured at the start of the study. Further details on the data collection procedure and analytical guidelines are publicly available on the NHANES website.15 As shown in online supplemental figure S1, this study included participants with reliable first 24 hours dietary recall and ≥20 years of age during NHANES 2011–2018 (n=21 128). Of these participants, 11 802 were excluded based on the following: (1) no reliable dual-energy X-ray absorptiometry (DXA) and BMI data; and (2) insufficient data to calculate the CVH scores. Thus, 9326 participants were enrolled in the present study.
bmjopen-2022-061789supp001.pdf (108.2KB, pdf)
DXA, appendicular skeletal muscle mass, and the definition of sarcopenia
DXA whole-body scans were performed on participants 8–59 years of age using Hologic Discovery model A densitometers (Hologic, Bedford, Massachusetts, USA). DXA exclusion criteria included pregnancy, weight>300 pounds (136 kg, because of the weight limit of the scanner), height>6’5” (DXA table limitations), history of radiographic contrast material (barium) used in the past 7 days, or nuclear medicine studies in the past 3 days. Hologic software (V.8.26: a3*) was used to administer all scans.
Appendicular skeletal muscle mass was measured using DXA. The sarcopenia index was calculated as follows: sarcopenia index=total appendicular skeletal muscle mass (in kg)/BMI (kg/m2).
Sarcopenia was defined as the lowest for sex-specific sarcopenia index cut-off values (0.789 for men and 0.512 for women), based on the National Institutes of Health (FNIH).
CVH metrics
CVH metrics include four health behaviours (cigarette smoking, physical activity, healthy dietary scores, and BMI) and three health factors (total cholesterol level, blood pressure, and fasting plasma glucose level).5 The definitions of ideal, intermediate, and poor CVH metrics for adults are presented in table 1. We used the Healthy Eating Index 2010 (HEI-2010) scores as a proxy of healthy dietary scores, which were calculated using first-day 24-hour dietary recall. HEI-2010 scores were based on a 12-component index, with total scores ranging from 0 to 100, and a higher score indicating a healthier diet: total fruit; whole fruit; total vegetables; grains and beans; whole grains; dairy; total protein foods; seafood and plant protein; fatty acids; refined grains; sodium; and empty calories. Participants with an HEI-2010 score<50 were assigned to poor health, those with a score of 51–80 to intermediate health, and those with a score>81 to ideal health.
Table 1.
Distribution of ideal, intermediate and poor CVH for each metric for adults free of CVD, NHANES 2011–20185
| AHA definitions of CVH for each metric | Total sample (n=9326) | |
| Smoking status, n (%) | ||
| Ideal | Never or quit>12 mo | 7003 (75.2) |
| Intermediate | Former≤12 mo | 216 (2.9) |
| Poor | Yes | 2107 (22.0) |
| Body mass index, n (%) | ||
| Ideal | < 25 kg/m2 | 2890 (31.1) |
| Intermediate | 25–29.9 kg/m2 | 2937 (32.6) |
| Poor | ≥ 30 kg/m2 | 3499 (36.3) |
| Physical activity, n (%) | ||
| Ideal | ≥150 min/week moderate intensity or≥75 min/week vigorous intensity or≥150 min/week moderate+vigorous | 3660 (41.9) |
| Intermediate | 1–149 min/week moderate intensity or 1–74 min/week vigorous intensity or 1–149 min/week moderate+vigorous | 625 (7.6) |
| Poor | None | 5041 (50.5) |
| Healthy diet score *, n (%) | ||
| Ideal | 4–5 components | 201 (2.2) |
| Intermediate | 2–3 components | 4046 (44.3) |
| Poor | 0–1 components | 5079 (53.5) |
| Total cholesterol, n (%) | ||
| Ideal | < 200 mg/dL | 5213 (54.1) |
| Intermediate | 200–239 mg/dL or treated to goal | 2548 (28.7) |
| Poor | ≥ 240 mg/dL | 1565 (17.2) |
| Blood pressure, n (%) | ||
| Ideal | <120/<80 mm Hg | 4474 (49.1) |
| Intermediate | SBP 120–139 or DBP 80–89 mm Hg or treated to goal | 2933 (31.9) |
| Poor | SBP≥140 or DBP≥90 mm Hg | 1919 (20.0) |
| Glycated haemoglobin A1c, n (%) | ||
| Ideal | < 5.7% | 6509 (76.0) |
| Intermediate | 5.7%–6.4% or treated to goal | 1945 (16.8) |
| Poor | > 6.4% | 875 (7.2) |
*AHA’s healthy diet score includes five components: fruits and vegetables, whole grain, fish, sodium, and sugar-sweeten beverage, and a very small proportion (<0.5%) of US adults meet the ideal healthy diet. HEI-2010 is a continuous score consisting of 12 components representing major food groups including fruit and vegetables, whole grains, proteins, dairy, oils, sodium and empty calories. HEI-2010 score ranges from 0 to 100 with a higher score indicates more healthy diet. HEI-2010 has been validated to represent the diet quality in population. We used HEI-2010 as a proxy for AHA’s healthy diet score with ideal diet: HEI-2010≥81; intermediate diet: 51–80; and poor diet: ≤ 50.
CVH, cardiovascular health; CVD, cardiovascular disease; NHANES, National Health and Nutrition Examination Survey; AHA, The American Heart Association; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Although the AHA relies on fasting glucose to determine hyperglycaemic, we use HbA1c (HbA1c) concentrations for two reasons. First, recent recommendations from the American Diabetes Association allow the use of HbA1c to diagnose diabetes. Second, a significant percentage of NHANES participants who took the test did not fast. Therefore, we used HbA1c values<5.7%, 5.7%–6.4%, and>6.5% as a proxy for fasting plasma glucose levels<100 mg/dL, 100 to <126 mg/dL, and >126 mg/dL. Participants who reported having diabetes or being treated with insulin or an oral medication to lower blood glucose and had an HbA1c concentration between 5.7% and 6.4% were categorised as intermediate health. Similarly, participants who reported taking cholesterol lowering or antihypertensive medications and were treated to goal were categorised as ‘intermediate’, whereas participants with these conditions who were untreated or who were not treated to goal were categorised as ‘poor’ for that health factor. Use of antihypertensive, cholesterol-lowering, and glucose-lowering medications were self-reported. Total cholesterol and plasma glucose levels were measured with enzymatic methods (https://www.cdc.gov/nchs/nhanes/index.htm). BMI was calculated as the weight in kilograms divided by the height in metres squared. The mean blood pressure was estimated from up to three readings obtained under standard conditions during a single physical examination.
For each metric, participants received 0, 1, or 2 points, representing poor, intermediate or ideal categories, respectively. Participants with overall scores of 0–7, 8–11, or 12–14 points were categorised as having poor, intermediate, or ideal CVH, respectively. Owing to the relatively low number of people with an ideal CVH score in this sample, the intermediate and ideal CVH categories were combined.
Statistical analysis
We used the NHANES recommended weights to account for planned oversampling of specific groups. The continuous variables were expressed as the mean±SE, and the categorical variables were presented as counts (percentages). Baseline characteristics between the two CVH groups were compared using a t-test for continuous variables and a χ2 test for categorical variables.
Multiple logistic regression was used to examine the independent influence of CVH on sarcopenia comparing poor CVH versus intermediate or ideal CVH after adjustments for potential confounders, such as age, sex, and race/ethnicity, educational level, alcohol, congestive heart failure, coronary heart disease, angina and cancer. The OR and 95% CI were computed. We explored the relationship between CVH and sarcopenia in different subgroups (age, sex, race/ethnicity and education level). We also separately estimated the association between individual components of the CVH metrics and sarcopenia. When assessing the role of individual components, the age, sex and race/ethnicity, educational level, alcohol, congestive heart failure, coronary heart disease, angina and cancer were adjusted. Furthermore, we used multiple logistic regression analysis to assess the effect of a different number of ideal cardiovascular health metrics (ICVHMs) on the incidence of sarcopenia. A two-sided p value<0.05 indicated significance for all analyses. All data analyses were performed using SAS Release V.9.4 (SAS Institute) and Survey package in R software (V.4.0.4; R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline characteristics
This study shown that only 2.2% of the participants met the ideal diet criteria. The frequency in the present sample of participants meeting the ideal level for the remainder of CVH metrics were cigarette smoking (weighted, 75.2%), HbA1c (weighted, 76.0%), total cholesterol level (weighted, 54.1%), blood pressure (weighted, 49.1%), physical activity (weighted, 41.9%), and BMI (weighted, 31.1%) (table 1).
This cohort study involved 9326 adults>20 years of age, comprising 4733 females (weighted, 50.0%) and 4593 males (weighted, 50.0%), with a weighted mean (SE) age of 39.3±0.3 years. 3323 (weighted, 60.3%) were of non-Hispanic white ancestry, 967 (weighted, 7.3%) of Hispanic ancestry, and 1955 (weighted, 11.3%) of non-Hispanic Black ancestry. The study population characteristics are listed in table 2 by CVH metrics. The number of intermediate or ideal and CVH participants was 5654 and 3672, with mean CVH metrics of 9.70±0.03 and 5.66±0.04, respectively. The differences of CVH metrics were significant for age, race/ethnicity, and education (p<0.001). The frequency in the present sample of sarcopenia in participants with poor CVH metrics was 12.3%, nearly threefold as participants with intermediate or ideal CVH metrics (4.8%). Moreover, we analysed the characteristics of this study population by sarcopenic status. Sarcopenia was identified in 45.9% of 403 females based on the sarcopenia criteria and the non-Hispanic white ancestry more like to develop sarcopenia (47.5%) compared with other races/ethnicities. Furthermore, the patient with sarcopenia had poor education level, BMI risk, healthy diet score risk, blood pressure risk, HbA1c risk and overall CVH metrics. And more detailed analyses are presented in online supplemental table S1.
Table 2.
Baseline characteristics of the study population
| Characteristics | Total (n=9326) | Intermediate or ideal CVH (n=5654) | Poor CVH (n=3672) | P value |
| Age, mean (SE), years | 39.3 (0.3) | 36.4 (0.3) | 44.3 (0.3) | < 0.001 |
| Female, n (%) | 4733 (50.0) | 2933 (50.9) | 1800 (48.5) | 0.078 |
| Race/ethnicity, n (%) | ||||
| Mexican American | 1406 (11.1) | 846 (11.4) | 560 (10.5) | < 0.001 |
| Other Hispanic | 967 (7.3) | 598 (7.5) | 369 (7.0) | |
| Non-Hispanic White | 3323 (60.3) | 2067 (61.3) | 1256 (58.5) | |
| Non-Hispanic Black | 1955 (11.3) | 1001 (9.5) | 954 (14.7) | |
| Other | 1675 (9.9) | 1142 (10.3) | 533 (9.3) | |
| Heavy use of alcohol, n (%) * | ||||
| < 12 | 6636 (97.8) | 4111 (98.5) | 2525 (96.6) | 0.173 |
| ≥ 12 | 156 (2.2) | 75 (1.5) | 81 (3.4) | |
| Education levels, n (%) | ||||
| < 12 | 3675 (34.6) | 1989 (31.0) | 1686 (40.9) | < 0.001 |
| 12 | 3092 (34.0) | 1863 (33.6) | 1299 (34.6) | |
| > 12 | 2557 (31.4) | 1800 (35.4) | 757 (24.5) | |
| Scores of CVH metrics, mean (SE) | 8.24 (0.04) | 9.70 (0.03) | 5.66 (0.04) | < 0.001 |
| No | 8519 (92.5) | 5326 (95.2) | 3193 (87.7) | |
| Congestive heart failure | 97 (1.0) | 23 (0.2) | 74 (1.8) | < 0.001 |
| Coronary heart disease | 92 (1.0) | 17 (0.2) | 75 (2.2) | < 0.001 |
| Angina | 94 (1.0) | 30 (0.4) | 64 (2.2) | < 0.001 |
| Cancer | 349 (5.0) | 158 (3.9) | 191 (6.8) | < 0.001 |
| Sarcopenia, n (%) | ||||
| Yes | 807 (7.5) | 328 (4.8) | 479 (12.3) | < 0.001 |
| No | 8519 (92.5) | 5326 (95.2) | 3193 (87.7) | |
*Data missing>5%
CVH, cardiovascular health;
bmjopen-2022-061789supp002.pdf (135.9KB, pdf)
Association between CVH metrics and sarcopenia
The intermediate or ideal CVH was associated with an odds reduction of sarcopenia than poor CVH (OR 0.36, 0.29 to 0.44, p<0.001; table 3). After adjusting for age, sex, race/ethnicity, education level, alcohol use, congestive heart failure, coronary heart disease, angina and cancer, intermediate or ideal CVH was associated with an odds reduction of sarcopenia than poor CVH (adjusted OR (aOR): 0.36, 95% CI 0.26 to 0.50, p<0.001). In the fully adjusted model, the odds of sarcopenia were significantly lower for each incremental increase of 1 in CVH metrics (aOR: 0.75, 95% CI 0.71 to 0.79, p<0.001). Further stratified and interaction analyses were performed for age, sex, race/ethnicity, and education level. And the association between intermediate or ideal CVH and sarcopenia was significant in different subgroups. Notably, the age group also showed stronger association in the subgroup aged<45 years (aOR: 0.38, 95% CI 0.27 to 0.52, p<0.001). Further, among subgroups of non-Hispanic Black, the odds of sarcopenia decreased by 79% in participants with intermediate or ideal CVH than in participants with poor CVH (aOR: 0.21, 95% CI 0.08 to 0.50, p<0.001; table 3). For all of subgroups, there was no significant interaction (all p values for interaction>0.05), expect of education levels (p for interaction=0.014).
Table 3.
The association between CVH metrics and sarcopenia by selected subgroups
| Variable | No. (%) | Intermediate or Ideal CVH OR (95% CI) * | P value | Intermediate or Ideal CVH OR (95% CI) † | P value | P for interaction |
| Continuous | ||||||
| CVH (per 1 score) | 807/9326 | 0.77 (0.74 to 0.79) | <0.001 | 0.75 (0.71 to 0.79) | <0.001 | – |
| Categories * | ||||||
| Poor CVH | 479/3672 | 1 (Ref) | – | 1 (Ref) | – | – |
| Intermediate or Ideal CVH | 328/5654 | 0.36 (0.29 to 0.44) | <0.001 | 0.36 (0.26 to 0.50) | <0.001 | – |
| Subgroup | ||||||
| Age | ||||||
| <45 | 211/4200 | 0.41 (0.31 to 0.54) | <0.001 | 0.38 (0.27 to 0.52) | <0.001 | 0.189 |
| 45–59 | 117/1454 | 0.37 (0.27 to 0.52) | <0.001 | 0.32 (0.19 to 0.53) | <0.001 | |
| Sex | ||||||
| Male | 157/2721 | 0.33 (0.24 to 0.45) | <0.001 | 0.36 (0.24 to 0.53) | <0.001 | 0.827 |
| Female | 171/2933 | 0.40 (0.30 to 0.54) | <0.001 | 0.35 (0.21 to 0.58) | <0.001 | |
| Race | ||||||
| Mexican American | 127/864 | 0.41 (0.28 to 0.60) | <0.001 | 0.43 (0.28 to 0.67) | <0.001 | 0.704 |
| Other Hispanic | 44/598 | 0.32 (0.18 to 0.58) | <0.001 | 0.37 (0.20 to 0.70) | 0.003 | |
| Non-Hispanic White | 80/2067 | 0.30 (0.22 to 0.40) | 0.019 | 0.31 (0.17 to 0.56) | <0.001 | |
| Non-Hispanic Black | 8/1001 | 0.15 (0.07 to 0.32) | <0.001 | 0.21 (0.08 to 0.50) | <0.001 | |
| Other | 69/1142 | 0.40 (0.23 to 0.69) | 0.001 | 0.45 (0.22 to 0.95) | 0.036 | |
| Education levels | ||||||
| <12 | 179/1989 | 0.43 (0.33 to 0.57) | <0.001 | 0.49 (0.33 to 0.74) | <0.001 | 0.014 |
| 12 | 87/1863 | 0.39 (0.25 to 0.61) | <0.001 | 0.32 (0.19 to 0.54) | <0.001 | |
| >12 | 62/1800 | 0.30 (0.18 to 0.50) | <0.001 | 0.20 (0.10 to 0.40) | <0.001 | |
Poor CVH: CVH metrics scores 0–7; intermediate or ideal CVH: CVH metrics scores 8–14.
*Unadjusted model.
†Analyses were adjusted for age, sex, race/ethnicity, education level, alcohol use, congestive heart failure, coronary heart disease, angina and cancer.
CVH, cardiovascular health.;
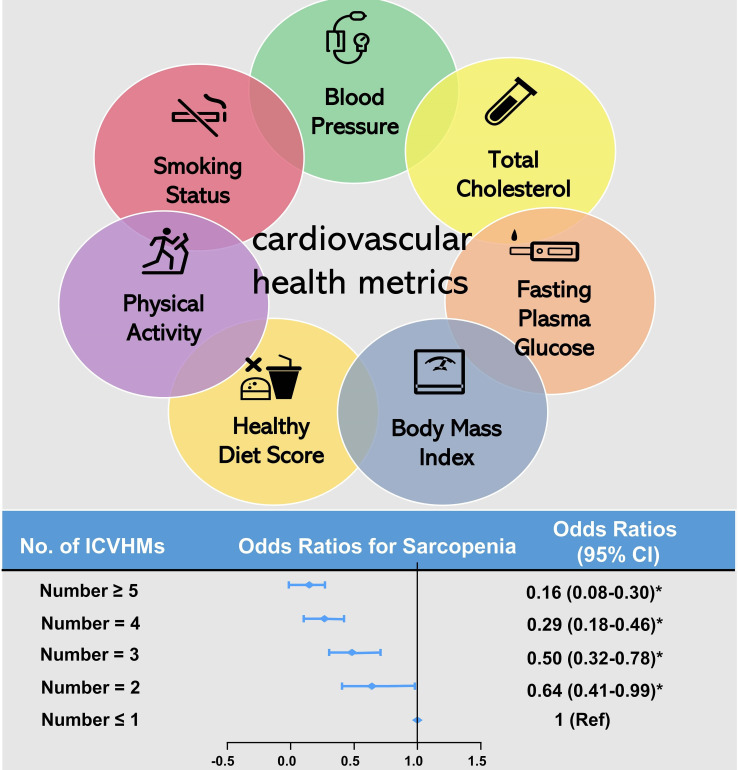
Association between number of ICVHMs and sarcopenia
Twenty-one percent of participants with sarcopenia had only 1 ICVHM and 5% had 5 ideal ICVHMs. In participants without sarcopenia, up to 70% had>3 ICVHMs (online supplemental figure S2). Logistic regression of the ICVHM number and the odds of sarcopenia revealed that the higher the number of ICVHMs, the lower the odds of sarcopenia. When participants had three ideal CVH metrics, the odds of sarcopenia decreased by 50% compared with participants with non-ideal CVH metrics (aOR: 0.50, 95% CI 0.32 to 0.78). If the number of ICVHMs was>5, the odds of sarcopenia decreased by up to 84% (aOR: 0.16, 95% CI 0.08 to 0.30; figure 1).
Figure 1.
Association between number of ICVHMs and sarcopenia. ICVHMs, Ideal cardiovascular health metrics. Model: adjusted by age, sex, and race/ethnicity, educational level, alcohol use, congestive heart failure, coronary heart disease, angina and cancer.*P<0.05.
Association between different individual CVH components and sarcopenia
In the subgroup analysis of the seven individual CVH components, participants defined as intermediate or poor CVH had a higher odds of sarcopenia odds than those with ideal CVH in all CVH metric subgroups except for the subgroup with cigarette smoking status, total cholesterol and physical activity. Especially in the BMI and healthy diet score subgroups, the odds of sarcopenia decreased>80% (BMI: (aOR: 0.08, 95% CI 0.05 to 0.13, p<0.001); healthy diet score: (aOR: 0.18, 95% CI 0.06 to 0.54, p=0.003)). A decreasing odd of sarcopenia trends were observed between increasing levels of CVH components for BMI, healthy diet score, HbA1c and blood pressure (all p for trend<0.05; table 4).
Table 4.
Adjusted ORs (95% CI) of sarcopenia by individual component of CVH metrics
| Variable | OR* | 95% CI | P value | P for trend |
| Smoking status | ||||
| Poor | 1 (Ref) | 1 (Ref) | NA | 0.201 |
| Intermediate | 0.84 | 0.33 to 2.12 | 0.706 | |
| Ideal | 1.25 | 0.87 to 1.80 | 0.223 | |
| Body mass index | ||||
| Poor | 1 (Ref) | 1 (Ref) | NA | <0.001 |
| Intermediate | 0.21 | 0.16 to 0.29 | <0.001 | |
| Ideal | 0.08 | 0.05 to 0.13 | <0.001 | |
| Healthy diet score | ||||
| Poor | 1 (Ref) | 1 (Ref) | NA | 0.005 |
| Intermediate | 0.66 | 0.46 to 0.93 | 0.019 | |
| Ideal | 0.18 | 0.06 to 0.54 | 0.003 | |
| Total cholesterol | ||||
| Poor | 1 (Ref) | 1 (Ref) | NA | 0.054 |
| Intermediate | 0.91 | 0.62 to 1.36 | 0.650 | |
| Ideal | 0.68 | 0.45 to 1.03 | 0.069 | |
| Glycated haemoglobin A1c | ||||
| Poor | 1 (Ref) | 1 (Ref) | NA | <0.001 |
| Intermediate | 0.37 | 0.21 to 0.63 | 0.001 | |
| Ideal | 0.28 | 0.14 to 0.36 | < 0.001 | |
| Physical activity | ||||
| Poor | 1 (Ref) | 1 (Ref) | NA | 0.401 |
| Intermediate | 0.93 | 0.56 to 1.54 | 0.774 | |
| Ideal | 0.89 | 0.67 to 1.18 | 0.402 | |
| Blood pressure | ||||
| Poor | 1 (Ref) | 1 (Ref) | NA | <0.001 |
| Intermediate | 0.62 | 0.43 to 0.89 | 0.010 | |
| Ideal | 0.37 | 0.26 to 0.52 | <0.001 | |
*Analyses were adjusted for age, sex, race/ethnicity, education level, alcohol use, congestive heart failure, coronary heart disease, angina and cancer.
CVH, cardiovascular health; NA, Not Applicable.
Discussion
This study used nationwide, population-based, cross-sectional data to demonstrate a significant association between CVH and sarcopenia and showed a significantly 64% decreased adjusted risk of sarcopenia in subjects with better CVH metrics. For each unit increase in the metrics of CVH, the risk of CVDs decreased by 25%. Furthermore, higher intermediate or ideal CVH metrics were associated with a lower prevalence of sarcopenia.
Our study yielded several interesting findings. First, the CVH metrics were not only associated with CVDs, but also non-CVDs, including sarcopenia. This result agreed with Han et al,16 who also reported that sarcopenia was independently associated with cardiovascular risk factors, including diabetes and hypertension. And these risk factors were shown to be associated with the prevalence of sarcopenia defined by the recommended algorithm of the Asian Working Group in the Chinese elderly.14 However, these results may only be applicable in patient with high-risk cardiovascular risk factors. In order to explore the association between sarcopenia and the common individual with average or only slightly unfavourable levels of risk factors, we chose CVH and elaborated on the detail and found that higher intermediate or ideal CVH metrics were associated with a lower prevalence of sarcopenia, as defined by the recommended algorithm of the FNIH in American adults. This finding suggests that the level of CVH influences the incidence of sarcopenia and emphasises the greater importance of CVH for healthcare and medical conditions. A previous study showed that the presence of more desirable CVH indicators was associated with a significant reduction in CVD morbidity and mortality.17 Our study broadens the application value of the CVH metrics; specifically, the higher the number of intermediate or ideal CVH metrics, the lower the incidence of sarcopenia. It showed that only a small percentage of American adults met the ideal criteria for six or seven ideal health metrics. This result is disappointing, but perhaps not surprising. Furthermore, this result challenges clinical and public health professionals to keep steering the health metrics in the desired direction. In the meantime, additional research is warranted in the future to explore CVH and non-cardiovascular fields to increase public awareness of CVH and promote achievement of AHA 2030 goals.
Second, we further observed the effects of CVH metrics on sarcopenia in different subgroups. We have reported that CVH influences the incidence of sarcopenia not only in the elderly population,14 but in the younger population. In addition, we demonstrated similar results in the sex and ethnicity subgroups. Surprisingly, it appeared that the ideal CVH metrics affect different levels of participant with different levels of education. Recent study shown that low education compared with high education was associated with lower odds of having ideal CVH.18 However, it appears that participants with higher levels of education are able to benefit more from the ideal CVH. At the same time, participants with low education levels also reduced the prevalence of sarcopenia by nearly 50% from the ideal CVH. Therefore, we not only need to focus on the ideal level of CVH for participants with low education levels, but also need to further increase the attainment rate of ideal CVH for participation with high education levels to achieve further benefits.
Third, we attempted to determine the effect of each indicator in CVH alone on sarcopenia in this study. Our study showed that reduced HbA1c levels were associated with a decreased risk of sarcopenia. This was consistent with the results of previous studies.19 This finding may be attributed to the fact that higher blood glucose levels accelerate the loss of muscle mass and strength.20 In addition, ideal blood pressure was the second significant feature associated with sarcopenia. Han et al14 also found that hypertension is an independent risk factor for sarcopenia. Although the mechanism underlying sarcopenia and hypertension is currently unknown, recent studies have concluded that inflammatory factors during ageing could impair blood flow by damaging the microvascular endothelium,21 which exerted a detrimental effect on the body of the elderly. Additional studies are needed to elucidate the causal relationship between hypertension and sarcopenia. Healthy eating is significantly associated with sarcopenia. The Papaioannou study22 highlighted the beneficial link between healthy eating and sarcopenia risk. There are several possible mechanisms to explain the beneficial effects of a healthy diet on skeletal muscle. First, a healthy diet rich in fruits and vegetables prevents metabolic acidosis and reduces protein hydrolysis and amino acid catabolism, thus reducing the risk of sarcopenia.23 In addition, unfavourable dietary patterns, including foods rich in saturated fats, may be detrimental to the maintenance of muscle health,24 while a fiber-rich diet reduces the risk of sarcopenia.25 Some studies, however, suggest that a lower BMI indicates the presence of sarcopenia and malnutrition and is associated with higher mortality in the older population.26 Conversely, obese patients may have a survival benefit.27 However, our study still found that being overweight or obese can significantly increase the risk of sarcopenia. The poor prediction of physical activity in the present study was unexpected, in contrast to previous studies28 that suggested only ideal physical activity does appear to be associated with the onset of sarcopenia. This finding might be due to the population in our study cohort included only young and middle-aged adults. Physical activity may be crucial for the occurrence of sarcopenia in the elderly population.
Our study has several limitations. First and foremost, cigarette smoking, physical activity, diseases, and diet were self-reported, and subjected to misclassification and recall bias, which can lead to an overestimated or underestimated association between CVH and sarcopenia. Second, as noted above, for practical reasons, we were not fully compliant with all of the AHA 2020 health indicators. Moreover, our study was cross sectional, so the association between CVH and sarcopenia cannot be interpreted as a direct cause-and-effect relationship. Finally, a half of initial cohort has been excluded in this study, which will increase the variance of the OR estimates. However, our results are still relatively reliable after weighting, since the main missing data are due to missing sampling.
Conclusion
In conclusion, our findings suggested a relationship between CVH indicators and the prevalence of sarcopenia among US adults. Our analysis confirms that CVH extends beyond protection against CVD. More research is needed to clarify the association between CVH and other non-CVDs. The results of our study can help facilitate the 2030 goal of achieving CVH for all because the AHA 2030 goal may be supported by efforts to reduce the prevalence of sarcopenia.
Supplementary Material
Acknowledgments
The authors thank all the participants and staff of the NHANES for their valuable contributions.
Footnotes
WC, SS and YJ contributed equally.
Contributors: WC: was responsible for designing the study, interpretation of the data, drafting the manuscript, revising the manuscript, and the approval of the final version. SS: participated in the design of analyses, data analysis, revising the manuscriptt, and approval of the final version. YJ: drafting the manuscript, revising the manuscript, and the approval of the final version. YL: interpretation of the data and the approval of the final version. KC: participated in formulating the research question, design of analyses, revising the manuscript, and the approval of the final version. RH and KH: participated in formulating the research question, design of analyses, data analysis, interpretation of the data, and the approval of the final version. All authors: read and approved the final version of the manuscript and are responsible for all aspects of the manuscript.
Funding: This study was supported by grants from the Summit Talent Plan, Beijing Hospital Management Center (plan no: DFL20190101) (Beijing, China), and the Natural Science Foundation of Fujian Provincial Science and Technology Department (2018J01405).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. The data link is https://www.cdc.gov/nchs/nhanes/index.htm
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by NHANES was approved by the NCHS Research Ethics Review Board (protocols Numbers: NHANES Protocol #2011-17 and NHANES Protocol #2018-01). Participants gave informed consent to participate in the study before taking part.
References
- 1.Mehta NK, Abrams LR, Myrskylä M. Us life expectancy stalls due to cardiovascular disease, not drug deaths. Proc Natl Acad Sci U S A 2020;117:6998–7000. 10.1073/pnas.1920391117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2., Mozaffarian D, Benjamin EJ, et al. , Writing Group Members . Heart disease and stroke Statistics-2016 update: a report from the American heart association. Circulation 2016;133:e38–60. 10.1161/CIR.0000000000000350 [DOI] [PubMed] [Google Scholar]
- 3.D'Agostino RB, Grundy S, Sullivan LM, et al. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA 2001;286:180–7. 10.1001/jama.286.2.180 [DOI] [PubMed] [Google Scholar]
- 4.Conroy RM, Pyörälä K, Fitzgerald AP, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the score project. Eur Heart J 2003;24:987–1003. 10.1016/S0195-668X(03)00114-3 [DOI] [PubMed] [Google Scholar]
- 5.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American heart association's strategic impact goal through 2020 and beyond. Circulation 2010;121:586–613. 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 6.Ommerborn MJ, Blackshear CT, Hickson DA, et al. Ideal cardiovascular health and incident cardiovascular events: the Jackson heart study. Am J Prev Med 2016;51:502–6. 10.1016/j.amepre.2016.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peng Y, Cao S, Yao Z, et al. Prevalence of the cardiovascular health status in adults: a systematic review and meta-analysis. Nutrition, Metabolism and Cardiovascular Diseases 2018;28:1197–207. 10.1016/j.numecd.2018.08.002 [DOI] [PubMed] [Google Scholar]
- 8.Enserro DM, Vasan RS, Xanthakis V. Twenty-Year trends in the American heart association cardiovascular health score and impact on subclinical and clinical cardiovascular disease: the Framingham offspring study. J Am Heart Assoc 2018;7. 10.1161/JAHA.118.008741. [Epub ahead of print: 17 05 2018]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Samieri C, Perier M-C, Gaye B, et al. Association of cardiovascular health level in older age with cognitive decline and incident dementia. JAMA 2018;320:657–64. 10.1001/jama.2018.11499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beaudart C, Zaaria M, Pasleau F, et al. Health outcomes of sarcopenia: a systematic review and meta-analysis. PLoS One 2017;12:e0169548. 10.1371/journal.pone.0169548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Curcio F, Testa G, Liguori I, et al. Sarcopenia and heart failure. Nutrients 2020;12:211. 10.3390/nu12010211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Han P, Chen X, Yu X, et al. The predictive value of sarcopenia and its individual criteria for cardiovascular and all-cause mortality in Suburb-Dwelling older Chinese. J Nutr Health Aging 2020;24:765–71. 10.1007/s12603-020-1390-8 [DOI] [PubMed] [Google Scholar]
- 13.Fülster S, Tacke M, Sandek A, et al. Muscle wasting in patients with chronic heart failure: results from the studies investigating co-morbidities aggravating heart failure (SICA-HF). Eur Heart J 2013;34:512–9. 10.1093/eurheartj/ehs381 [DOI] [PubMed] [Google Scholar]
- 14.Han P, Yu H, Ma Y, et al. The increased risk of sarcopenia in patients with cardiovascular risk factors in Suburb-Dwelling older Chinese using the AWGS definition. Sci Rep 2017;7:9592. 10.1038/s41598-017-08488-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for disease control and prevention, National center for health statistics . About the National health and nutrition examination survey. Available: https://www.cdc.gov/nchs/nhanes/about_nhanes.htm
- 16.Han E, Lee Y-H, Kim YD, et al. Nonalcoholic fatty liver disease and sarcopenia are independently associated with cardiovascular risk. Am J Gastroenterol 2020;115:584–95. 10.14309/ajg.0000000000000572 [DOI] [PubMed] [Google Scholar]
- 17.Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation 2012;125:987–95. 10.1161/CIRCULATIONAHA.111.049122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alam MT, Echeverria SE, DuPont-Reyes MJ, et al. Educational Attainment and Prevalence of Cardiovascular Health (Life’s Simple 7) in Asian Americans. Int J Environ Res Public Health 2021;18:1480. 10.3390/ijerph18041480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Han P, Kang L, Guo Q, et al. Prevalence and factors associated with sarcopenia in Suburb-dwelling older Chinese using the Asian Working group for sarcopenia definition. J Gerontol A Biol Sci Med Sci 2016;71:529–35. 10.1093/gerona/glv108 [DOI] [PubMed] [Google Scholar]
- 20.Morley JE, Malmstrom TK, Rodriguez-Mañas L, et al. Frailty, sarcopenia and diabetes. J Am Med Dir Assoc 2014;15:853–9. 10.1016/j.jamda.2014.10.001 [DOI] [PubMed] [Google Scholar]
- 21.Han K, Park Y-M, Kwon H-S, et al. Sarcopenia as a determinant of blood pressure in older Koreans: findings from the Korea National health and nutrition examination surveys (KNHANES) 2008-2010. PLoS One 2014;9:e86902. 10.1371/journal.pone.0086902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Papaioannou K-G, Nilsson A, Nilsson LM, et al. Healthy eating is associated with sarcopenia risk in physically active older adults. Nutrients 2021;13:2813. 10.3390/nu13082813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim J, Lee Y, Kye S, et al. Association of vegetables and fruits consumption with sarcopenia in older adults: the fourth Korea National health and nutrition examination survey. Age Ageing 2015;44:96–102. 10.1093/ageing/afu028 [DOI] [PubMed] [Google Scholar]
- 24.Montiel-Rojas D, Santoro A, Nilsson A, et al. Beneficial role of replacing dietary saturated fatty acids with polyunsaturated fatty acids in the prevention of sarcopenia: findings from the NU-AGE cohort. Nutrients 2020;12:3079. 10.3390/nu12103079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Montiel-Rojas D, Nilsson A, Santoro A, et al. Dietary fibre may mitigate sarcopenia risk: findings from the NU-AGE cohort of older European adults. Nutrients 2020;12:1075. 10.3390/nu12041075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Di Angelantonio E, Bhupathiraju S, et al. , Global BMI Mortality Collaboration . Body-Mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 2016;388:776–86. 10.1016/S0140-6736(16)30175-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amundson DE, Djurkovic S, Matwiyoff GN. The obesity paradox. Crit Care Clin 2010;26:583–96. 10.1016/j.ccc.2010.06.004 [DOI] [PubMed] [Google Scholar]
- 28.Bosaeus I, Rothenberg E. Nutrition and physical activity for the prevention and treatment of age-related sarcopenia. Proc Nutr Soc 2016;75:174–80. 10.1017/S002966511500422X [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-061789supp001.pdf (108.2KB, pdf)
bmjopen-2022-061789supp002.pdf (135.9KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. The data link is https://www.cdc.gov/nchs/nhanes/index.htm