Abstract
Background
falls and fall-related injuries are common in older adults, have negative effects on functional independence and quality of life and are associated with increased morbidity, mortality and health related costs. Current guidelines are inconsistent, with no up-to-date, globally applicable ones present.
Objectives
to create a set of evidence- and expert consensus-based falls prevention and management recommendations applicable to older adults for use by healthcare and other professionals that consider: (i) a person-centred approach that includes the perspectives of older adults with lived experience, caregivers and other stakeholders; (ii) gaps in previous guidelines; (iii) recent developments in e-health and (iv) implementation across locations with limited access to resources such as low- and middle-income countries.
Methods
a steering committee and a worldwide multidisciplinary group of experts and stakeholders, including older adults, were assembled. Geriatrics and gerontological societies were represented. Using a modified Delphi process, recommendations from 11 topic-specific working groups (WGs), 10 ad-hoc WGs and a WG dealing with the perspectives of older adults were reviewed and refined. The final recommendations were determined by voting.
Recommendations
all older adults should be advised on falls prevention and physical activity. Opportunistic case finding for falls risk is recommended for community-dwelling older adults. Those considered at high risk should be offered a comprehensive multifactorial falls risk assessment with a view to co-design and implement personalised multidomain interventions. Other recommendations cover details of assessment and intervention components and combinations, and recommendations for specific settings and populations.
Conclusions
the core set of recommendations provided will require flexible implementation strategies that consider both local context and resources.
Keywords: falls, injury, aged, guidelines, recommendations, clinical practice, world, global, consensus, older people
Key Points
The world’s population is ageing. Falls and related injuries are increasingly common, making their prevention and management a critical global challenge.
Opportunistic case-finding is necessary as older adults may not present following a fall and may be reluctant to report falls.
Multidomain interventions tailored to individual’s risks factors, when delivered, are effective.
Engaging older individual’s beliefs, attitudes and priorities about falls and their management is essential.
Application of some of these recommendations may need modification to meet low resource settings and country’s needs.
‘It takes a child one year to acquire independent movement and ten years
to acquire independent mobility. An old person can lose both in a day’
Professor Bernard Isaacs
(1924–1995)
Introduction
This quote from Bernard Isaacs portrays the unfortunate consequences that an older adult may experience after a single fall [1]. Falls occur at all ages and are an inevitable part of a bipedal gait and physical activity. They occur in 30% of adults aged over 65 years annually [2], for whom the consequences are more serious, despite concerted efforts of researchers and clinicians to understand, assess and manage their risks and causes. In addition to personal distress, falls and fall-related injuries are a serious health care problem because of their association with subsequent morbidity, disability, hospitalisation, institutionalisation and mortality [1, 3, 4]. In Europe, total deaths and disability-adjusted life years due to falls have increased steadily since 1990 [5]. The Global Burden of Disease study reported nearly 17 million years of life lost from falls in 2017 [3]. Related societal and economic consequences are substantial. In high-income countries, approximately 1% of health care costs are fall-related expenditures [6].
The number of falls and related injuries will likely further increase [7, 8], partly as there are more older adults, but also because of increasing prevalence of multimorbidity, polypharmacy and frailty among them. There appears to be differences in falls prevalence between and within regions of the world [3, 5]. For example, rates among ethnic Chinese populations across South East Asia have been reported as between 15 and 34% [4] and in the Latin America and Caribbean region rates ranged from 22% in Barbados to 34% in Chile [9]. These differences may be due in part to cultural and lifestyle differences [10]. There are also differences between settings with the incidence of falls being higher for older adults living in care homes or during a hospital stay [10]. This suggests that risk factors may differ across locations and settings, which could have relevance for preventative strategies.
The need for new guidelines
The World Falls Guidelines (WFG) Task Force was created following discussions in 2019 between 14 international experts to consider whether new guidelines on falls prevention were needed to reflect new evidence and clinical service challenges. A subsequent systematic review identified gaps in and inconsistencies between the existing guidelines developed nationally or by specialist international bodies and concluded that a new set of clinical practice guidelines should be created to address these issues and that the guidelines should incorporate an international perspective [7].
The National Institute for Health and Care Excellence in England (NICE) undertook a systematic assessment in 2019 of the need to update its 2013 guidelines [8] and concluded that new evidence reported up to February 2019 had likely impact on case-finding, falls risk assessments and preventative interventions. With further findings since then, there is now a substantial volume of research evidence that has not been systematically evaluated. Observational studies have clarified how to identify levels of risk among community dwelling and clinical populations [2, 11, 12]. Mechanistic and epidemiological studies have improved our understanding of falls in older adults with cognitive impairment [12–16]. The potential roles for e-health including wearables, virtual reality applications and environmental monitoring devices [17–19] have not been previously considered by prior guideline recommendations.
Falls are more common among older adults in clinical care settings, e.g. hospitals, subacute and rehabilitation units, assisted living settings and care homes. The risk factors in these settings and consensus on how to address them are not well captured in current clinical practice guidelines, but evidence specific to these settings is now available on which to base recommendations.
Perspectives of older adults with living experience, carers and other stakeholders have been inconsistently incorporated [7], but there is now emerging evidence that such views may inform the suitability and feasibility of guideline recommendations [20–22].
Purpose and scope of the guidelines
We believe that these guidelines will contribute to improving the health and well-being of older adults globally, which is the overarching aim of the United Nations Decade of Healthy Ageing (2021–2030). Healthy ageing relies on ‘the functional ability to be or to do what you have reason to value’ [23]. Reducing the incidence of falls and related injuries, notably fractures and head injuries, and enabling preserved functional mobility and reducing concerns about falling, which may limit activity, would all contribute to achieving this. Therefore, the objective of the WFG is to provide guidelines for healthcare and other professionals working with older adults on how to identify and assess the risk of falls and which interventions, alone or in combination, to offer as part of a person-centred approach. These guidelines are novel in systematically considering: (i) a person-centred approach, including the perspectives from older adults with lived experience, caregivers and other stakeholders: (ii) gaps detected in previous guidelines; (iii) recent developments in e-health and (iv) challenges of implementation across settings and locations with limited resources, including low- and middle-income countries (LMIC).
We adopted the World Health Organisation definition: a fall is an event which results in a person coming to rest inadvertently on the ground or floor or other lower level. Falls, trips and slips can occur on one level or from a height [24]. This definition of a fall includes syncopal events. In the health and social care systems of many countries, older adults are regarded as those aged 65 years or over, but in some circumstances, age 60 years may be more appropriate depending on the context and health expectancies. There is inconsistency in the ages of older participants in the research evidence underpinning these guidelines. There is no scientific rationale for the application of a strict chronological definition of older age when using these guidelines.
The guidelines are focused on individual person level actions. The intended beneficiaries include older adults living in the community and care homes, and hospital inpatients. We also considered the specific features of assessment and/or prevention applicable to older adults with common medical conditions associated with higher falls risk and where the evidence supported this (i.e. Parkinson’s disease [PD], post-stroke, post-hip fracture and significant cognitive impairment) we developed separate recommendations for these conditions.
The challenges of implementing falls prevention guidelines in LMIC, where barriers to accessing human and technical resources may be encountered, have not been previously considered [25]. As well, the most predictive risk factors for falls and the favoured interventions to prevent them may well differ in these countries compared with high-income ones. Accordingly, we have tried to include these considerations in the recommendations made and the advice provided for their implementation.
Management of fall-related injuries is beyond the scope of these guidelines, but as there is a close epidemiological and clinical relationship between falls and fragility fractures, explicit linkage is needed with clinicians and services that can assess bone health, identify osteoporosis and fracture risk and provide management for maintaining bone health. While details of these activities are not included in these guidelines, there are well developed multilingual ones available elsewhere [26, 27].
How should these guidelines be used?
Healthcare clinicians for whom these guidelines were developed include physicians, nurses, physiotherapists, occupational therapists, pharmacists and other allied health professionals. Application of these guidelines involves actions by non-specialist as well as specialist healthcare professionals, and service design of care pathways linking primary and community services to specialists where necessary. Therefore, optimal implementation will require actions at the operational level in healthcare and social care sectors. While adaptation to local context, healthcare arrangements and resources is inevitable, our recommendations encompass the global population of older adults. Population level approaches such as public health initiatives and community level actions such as environmental design and age-friendly communities that may directly or indirectly impact falls rates are beyond our scope.
We anticipate that the flexible application of our recommendations will support meeting the different needs of individuals with varying characteristics and priorities and residing in diverse settings and countries with variable resource availability and are consistent with the person-centred approach [28] described below.
Predictive: utilisation of available information to determine an individual’s risk of falls and fall-related injuries.
Preventative: focused on intention to prevent falls and related injuries whilst optimising functional ability.
Personalised: utilisation of identified fall risks factors and other relevant clinical information, such as cognition, to develop individualised fall prevention plans.
Participatory: intervention goals and plan developed in collaboration with the older adult, and others as they wish, to consider priorities, values and resources, such as carer support.
How were these guidelines produced?
A full description of the process is provided in Appendix 1, available in Age and Ageing online. The World Falls Guidelines Task Force assembled 96 experts from 39 countries and across 5 continents, with representation from 36 scientific and academic societies. Details how this task force was assembled have been previously described [25]. A Steering Committee developed the strategy and guided the project. Feedback from older adults was obtained through early and meaningful involvement in the consensus process, with the goal of making these guidelines better suited to the needs of older adults residing in the community and long-term care facilities. We conducted a systematic review in 2020 that examined existing falls prevention and management guidelines. The gaps identified informed the creation of specific working groups (WGs) addressing topics considered to be relevant or controversial [7]. Eleven topic specific WGs developed preliminary graded recommendations based on systematic reviews as described in detail in each of their WG Reports in Appendix 2, available in Age and Ageing online. Each WG was responsible for creating its own search strategy and their own PICO question. Details on selecting and appraising the articles are clarified in the full report for each WG in Appendix 2, available in Age and Ageing online. A further WG considered older adult’s perspectives as a cross-cutting theme. Ten ad hoc expert groups performed additional rapid reviews [29] of clinical areas not covered by the WGs. An international Experts Group provided external review and feedback on the preliminary and revised recommendations through a four-stage modified Delphi process, which culminated in a final vote on the recommendations that involved Steering Committee members and WG leaders and informed by structured feedback from an older adults’ panel.
In addition, an ad hoc WG of 8 clinician experts developed a falls assessment and management algorithm, linking risk stratification, assessment and interventions, based on the evidence provided by the WGs. The full membership lists of committees and WGs are shown in Appendix 4b, available in Age and Ageing online.
Grading of recommendations is presented according to the strength (1 strong to 2 weak-conditional) and quality of the contributing evidence (A–C, high to low) using a modified version of the widely used Grading of Recommendations, Assessment, and Evaluation (GRADE) criteria (Table 1) [30]. This modified GRADE is based on the original system, where numbers are used to indicate the strength of the recommendation. Where evidence was lacking, but a recommendation considered necessary, this modified system allowed for a recommendation to be graded as ‘E’ (expert consensus advice recommendation) (Tables 2 and 3).
Table 1.
Modified GRADE system description
| Strength of Recommendation | 1 | Strong: benefits clearly outweigh undesirable effects |
| 2 | Weak or conditional: either lower quality evidence or desirable and undesirable effects are more closely balanced | |
| Quality of evidence | A | High: ‘further research is unlikely to change confidence in the estimate of effect’ |
| B | Intermediate: ‘further research is likely to have an important impact on the confidence in the estimate of effect and may change the estimate’ | |
| C | Low: ‘further research is very likely to have an important impact on the confidence in the estimate of effect and is likely to change the estimate’ | |
| No evidence Available | E | Experts: ‘When the review of the evidence failed to identify any quality studies meeting standards set or evidence was not available, recommendations were formulated expert consensus’ |
Table 2.
Taxonomy used in the World Falls Guidelines
| Fall | An unexpected event in which an individual comes to rest on the ground, floor, or lower level |
| Recurrent falls | Two or more falls reported in the previous 12 months |
| Unexplained fall | When no apparent cause has been found for a fall on performing a multifactorial falls risk assessment and it cannot be explained by a failure to adapt to an environmental hazard or by any other gait or balance abnormality |
| Severe fall | Fall with injuries that are severe enough to require a consultation with a physician; result in the person lying on the ground without capacity to get up for at least one hour; prompt a visit to the emergency room (ER); associated with loss of consciousness |
| Fall related injury | An injury sustained following a fall. This includes an injury resulting in medical attention including hospitalisation for a fall such as fractures, joint dislocation, head injury, sprain or strain, bruising, swelling, laceration, or other serious injury following a fall |
| Fall risk stratification | A single or set of assessments performed to grade an individual’s risk of falling, to guide what further assessments or interventions might be necessary |
| Multifactorial falls risk assessment | A set of assessments performed across multiple domains to judge an individual’s overall level of risk of falling to identify the individual risk factors - potentially modifiable and non-modifiable -to inform the choice of an intervention |
| Caregiver | A caregiver provides assistance in meeting the daily needs of another person. Caregivers are referred to as either ‘formal’ or ‘informal.’ ‘Formal’ caregivers are paid for their services and have had training in providing care. This may include services from home health agencies and other trained professionals. ‘Informal’ caregivers, also called family caregivers, are persons who give care to family or friends usually without payment. A caregiver gives care, generally in the home environment, for an ageing parent, spouse, other relative or unrelated person, or for an ill, or disabled person. These tasks may include transportation, grocery shopping, housework, preparing meals. Also giving assistance with getting dressed, getting out of bed, help with eating and incontinence. |
| Exercise | Exercise is a subset of physical activity that is planned, structured, and repetitive and has as a final or an intermediate objective the improvement or maintenance of physical fitness. Physical fitness is a set of attributes that are either health- or skill-related |
| Fall risk increasing drugs (FRIDs) | Medications known to increase the risk of falls |
| Fall risk stratification algorithm | The systematic process of decision-making and intervention that should occur for falls risk case findings |
| Low- and Middle- income countries (LMIC) | As defined by World Bank Classification for Low- and Middle- Income Countries https://blogs.worldbank.org/opendata/new-world-bank-country-classifications-income-level-2021-2022 |
| Multicomponent exercise | This type of programme combines strength, aerobic, balance, gait and flexibility training |
| Multidomain interventions | A combination of two or more intervention components across two or more domains (e.g.: an exercise program and environmental modification) based on a multifactorial falls risk assessment and intended to prevent or minimise falls and related injuries |
| Multicomponent interventions | These are fixed combinations of two or more intervention components that are not individually tailored following a multifactorial falls risk assessment. Multicomponent interventions vary widely: for illustration, an example could be a medication review, home modifications and generic exercise advice |
| Physical activity | Any bodily movement produced by skeletal muscles that results in energy expenditure. The energy expenditure can be measured in kilocalories. Physical activity in daily life can be categorised into occupational, sports, conditioning, household, or other activities |
| Telehealth | Involves communicating with individuals at home via telephone or video calls |
| Smart home systems | System that aims to decrease environmental hazards and forecast potentially impending falls using sensors and Artificial Intelligence (AI) technology |
Table 3.
List of acronyms used in the text of the WFGs
| 3IQ | Three Incontinence Questionnaire |
| 3KQ | Three Key Questions |
| ADL | Activities of Daily Living |
| BMI | Body mass index |
| CFS | Clinical Frailty Scale |
| CGA | Comprehensive geriatric assessment |
| CST | Chair Stand Test |
| DT | Dual tasking |
| FES-I | Falls Efficacy Scale International |
| FOG | Freezing of gait |
| FP | Frailty phenotype |
| FRIDs | Fall risk increasing drugs |
| GDS | Geriatric Depression Scale |
| GRADE | Grading of Recommendations, Assessment, and Evaluation |
| IADL | Instrumental Activities of Daily Living |
| ICFSR | International Conference on Frailty and Sarcopenia |
| LMIC | Low- and middle-income countries |
| MCI | Mild Cognitive Impairment |
| MDS-UPDRS | Movement Disorders Society Unified Parkinson’s Disease Rating Scale |
| MNA | Mini Nutritional Assessment |
| MoCA | Montreal Cognitive Assessment |
| NEADL | Nottingham Extended Activities of Daily Living |
| NICE | National Institute for Health and Care Excellence |
| NSAIDs | Non-steroidal anti-inflammatory drugs |
| PD | Parkinson’s Disease |
| RCT | Randomised controlled trial |
| Short FES-I | Short Falls Efficacy Scale International |
| SNRIs | Serotonin norepinephrine reuptake inhibitors |
| SPPB | Short Physical Performance Battery |
| TMT | Trail Making Test |
| TMT-B | Trail Making Test Part B |
| TUG | Timed Up and Go |
| WFG | World Falls Guidelines |
| WGs | Working groups |
Framework of the guidelines
Fall Risk Stratification: a standard approach to assess an individual’s estimated level of risk for falls, in order to apply a proportionate detailed assessment and intervention according to level of risk.
Assessment: process of identifying and measuring the falls risk factors across multiple domains, using recommended tools if available, to indicate potentially modifiable areas for intervention. Combined with other components of a comprehensive geriatric assessment (CGA), this enables a person-centred approach.
Management and Interventions: description of various approaches to fall prevention including recommended treatments or actions which can reduce the risk of falls and may be suitable as single interventions or in combinations.
Assessment and Treatment Algorithm: this links the three stages of initial risk stratification, assessment and management, and encourages a ‘person-centred’ approach to design an individualised intervention.
Key messages
The world’s population is ageing. Falls and related injuries are increasingly common, making their prevention and management a critical global challenge.
Many falls can be prevented. Fall and injury prevention needs multidisciplinary management.
Engaging older adults is essential for prevention of falls and injuries: understanding their beliefs, attitudes and priorities about falls and their management is crucial to successfully intervening.
Managing many of the risk factors for falls (e.g. gait and balance problems) have wider benefits beyond falls prevention such as improved intrinsic capacities (physical and mental health), functioning and quality of life.
Estimates of risk of future falls can be done by trained clinicians with simple resources.
Multidomain interventions (i.e., a combination of interventions tailored to the individual), when delivered, are effective for reducing the rate of falls in high-risk community-dwelling older adults.
In care homes and hospital settings all older adults should be considered as high risk and a standard comprehensive assessment followed by multidomain interventions should be considered.
Vitamin D supplementation to prevent falls should be reserved for those at risk of vitamin D deficiency.
Modification to the approaches for assessment and interventions may be needed for older adults with certain medical conditions associated with an increased likelihood of falling.
Application of some of these recommendations may need modification to meet the needs of older adults in settings and locations with limited resources such as LMIC.
Falls risk stratification and algorithm
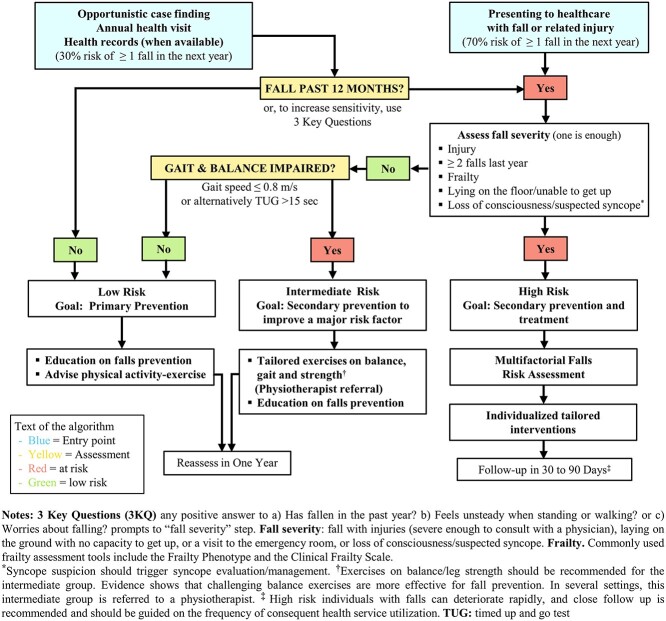
Following the seminal guidelines produced by the AGS /BGS/ AAOS panel on falls prevention and management published in 2001 and updated in 2011, we created a falls prevention and management approach and algorithm to be applied in community older adults. We stratified falls risk into the following three categories [31, 32], which was also used in our falls risk detection and management algorithm for community dwelling older adults (Figure 1):
Figure 1.
Algorithm for risk stratification, assessments and management/interventions for community-dwelling older adults.
older adults at low risk for falls who should be offered education about falls prevention and exercise for general health and/or fall prevention if interested;
older adults at intermediate risk for falls, who in addition to the above should be offered targeted exercise or a physiotherapist referral in order to improve balance and muscle strength, and reduce their fall risk; and
older adults at high risk for falls who should be offered a multifactorial falls risk assessment to inform individualised tailored interventions.
Categorisation into these three groups should occur during either opportunistic case-finding or when older adults present with a fall or related injury.
Opportunistic case-finding
Strong recommendation. Clinicians should routinely ask about falls in their interactions with older adults, as they often will not be spontaneously reported. GRADE: 1A.
Expert recommendation. Older adults in contact with healthcare for any reason should be asked, at least once yearly, if they have (i) experienced one or more falls in the last 12 months, and (ii) about the frequency, characteristics, context, severity and consequences of any fall/s. GRADE: E.
Expert recommendation. If resources and time are available, we conditionally recommend to additionally ask (iii) if they have experienced dizziness, loss of consciousness or any disturbance of gait or balance and (iv) if they experience any concerns about falling causing limitation of usual activities. GRADE: E.
Strong recommendation. Older adults who affirm any of the above inquiries should be offered an objective assessment of gait and balance for differentiating intermediate and high from low risk of falls as a component of initial falls risk stratification. GRADE: 1A.
Recommendation details and justification
Clinicians cannot rely solely on older adults reporting falls, as studies indicate that many do not for a variety of reasons [33]. This is particularly true for men with less than a third mentioning them to their clinician if not directly asked (Appendix 2, available in Age and Ageing online) [34].
Older adults presenting with falls or related injuries
Expert recommendation. Older adults presenting with a fall or related injury should be asked about the details of the event and its consequences, previous falls, transient loss of consciousness or dizziness and any pre-existing impairment of mobility or concerns about falling causing limitation of usual activities. GRADE: E.
Expert recommendation. An adult who sustains an injury requiring medical (including surgical) treatment, reports recurrent falls (≥2) in the previous 12 months, was laying on the floor unable to rise independently for at least one hour, is considered frail or is suspected to have experienced a transient loss of consciousness should be regarded as at high risk of future falls. GRADE: E.
Recommendation details and justification
These recommendations apply to the group of older individuals who present to Emergency departments or another facility [35, 36] such as to primary care physicians or a fracture service due to a fall-related injury or are seen at home by paramedics, and also to older adults whose fall was understood by the clinician to have been precipitated by an acute medical illness, such as infection [28, 37].
Assessment and algorithm flow
Our proposed algorithm has two entry points (Figure 1): first, opportunistic case finding, case finding during a health visit or using ‘e-health records’, and second, when older adults present to healthcare services as a result of a fall or related injury. Opportunistic case-finding is necessary as older adults may not present following a fall and may be reluctant to report falls [38–41]. Furthermore, recollection of the occurrence or date (e.g., how many months ago) of previous falls is unreliable [42]. Therefore, the 1-year timing is a pragmatic compromise between accuracy of recollection and the natural history of falls risk factor progression [43].
Opportunistic case finding starts with the single question ‘Have you fallen in last 12 months’. This single question is highly specific in predicting future falls [31, 32] but has a low sensitivity as it takes no account of common risk factors, and consequently, results in a high rate of false negatives.
Tools that assess more than one fall risk factor, such as the ‘three key questions’ (3KQ) [41], have a higher sensitivity. The questions are: (i) Have you fallen in the past year, (ii) Do you feel unsteady when standing or walking? (iii) Do you have worries about falling. If resources are available, we conditionally recommend its use. The Stay Independent self-risk assessment consisting of 12 self-administered questions, which is a component of the Centres for Disease Control and Prevention’s STEADI toolkit, can also be used as a sensitive approach to detecting future fall risk [44, 45]. Age distribution of the older adult population when selecting a fall risk screening tool is important, since sensitivity of the single question ‘Have you fallen in the past 12 months’ increases from 43% in those between 65 and 74 years old, to 67% in those over 85 years old. Gait or balance disturbances should be assessed following a positive answer to history of fall or any of the 3 key questions [31].
Strong recommendation. Regarding specific tests, we recommend including Gait Speed for predicting falls risk. GRADE: 1A. As an alternative, the Timed Up and Go Test can be considered, although the evidence for fall prediction is less consistent. GRADE: 1B.
Recommendation details and justification
There are several tests for assessing gait and balance impairment. For risk stratification, we recommend use of gait speed, with a cut-off value of <0.8 m/s on the basis of its predictive ability and simplicity [46]. Resources with simple instructions on how to measure gait speed can be found at www.worldfallsguidelines/resources.
Alternatively, the Timed Up and Go (TUG) test can be used, with a cut-off value of >15 seconds, although evidence for fall risk stratification is mixed. There is evidence that he TUG is predictive of falls in lower functioning adults [46].
An older adult who does not have a history of falling, or who had a single non-severe fall and no gait or balance problems, is deemed as being at low risk. Since low risk does not mean ‘no risk at all’, we recommend primary prevention for these older adults. This ‘low risk’ group should be reassessed annually. Older adults who had a single non-severe fall but also have gait and or balance problems, should be considered as being at ‘intermediate risk’ and would benefit from a strength and balance exercise intervention since evidence shows that this type of exercise is effective in reducing falls risk [2]. Finally, those at ‘high risk’ include older adults with a fall and one or more of the following characteristics: (i) accompanying injury, (ii) multiple falls (≥2 falls) in the previous 12 months, (iii) known frailty, (iv) inability to get up after the fall without help for at least an hour and (v) accompanied by (suspected) transient loss of consciousness. These high-risk older adults should be offered a multifactorial falls risk assessment. Suspicion of a syncopal fall should trigger syncope evaluation and management. With regard to frailty for risk stratification, this can be either previously identified frailty or a positive result on a validated instrument used for its detection. Commonly used frailty assessment instruments include the Frailty phenotype (FP) [47] and the Clinical Frailty Scale (CFS) [48]. The FP includes 5 criteria: slow gait speed, low physical activity, unintentional weight loss, exhaustion and muscle weakness; where ≥3 components categorises an individual as ‘frail’, 1 or 2 as prefrail, and 0 as not frail. The CFS is a semi-quantitative scale with pictograms that ranges from 1 (very fit) to 9 (terminally ill).A score ≥4 is considered as frail (https://www.dal.ca/sites/gmr/our-tools/clinical-frailty-scale.html). The algorithm for stratification and management in Figure 1 summarizes this approach.
Assessment
The purposes of the assessment are to address the mechanism of the fall, the consequences of the fall (e.g., injury, functional deficits, psychological effects such as concerns about falling), and the identification of potentially contributing fall risk factors.
Assessment with a view to reducing the risk of falling needs to consider the older adult’s history of falling and: their frequency; characteristics and context; presence of falls risks factors; their physical, cognitive, psychological and social resources; and, their goals, values, beliefs, and priorities. An assessment with a view to co-designing an intervention with the older adult requires a broad approach, as exemplified by a CGA. Our recommendations (based on the WG evidence-based reviews) describe the assessments needed to identify the key modifiable falls risk factors. In Table 4, we provide an overview of potential approaches for assessment of a number of individual modifiable fall risk factors.
Table 4.
Potential measurement instruments and approaches for multifactorial falls risk assessment
| Domains for assessment | Fall risk factor | Measurement/approach |
|---|---|---|
| Mobility | Balance | Screen for balance disorders for example by Tandem Stand, One Leg stand. If indicated, perform full assessment in structured manner, for example by Berg Balance Scale, Tinetti test, POMA (subscale balance), Mini-BEST test. Consider referral to physiotherapist. |
| Gait | Assess both qualitatively and quantitatively using 4-m walking length (<0.8 m/s), POMA (subscale gait), Dual Task test, Functional Gait Assessment. Screen for mobility problems using a structured approach for example by Short Physical Performance Battery (SPPB), Timed Up and Go (TUG), Get Up and Go including qualitative assessment). |
|
| Muscle strength | Screen quantitatively using for example CST or handgrip strength If indicated assess structurally specific muscle groups (MRC-scale) |
|
| Walking aid | If applicable, assess for appropriateness and proper of use of walking aid including potential mechanical deficits. | |
| Footwear and foot problems | Screen for potential inappropriate footwear (including bare footedness) Assess for potential foot problems. Consider referral to podiatrist. |
|
| Fear of falling | Assess Fear of (concerns about) Falling, preferably in structured manner, for example by Falls Efficacy Scale (FES-I) or short FES-I If indicated: assess for anxiety disorder, preferably by HADS. Consider referral to specialist. |
|
| Sensory function | Dizziness/vestibular | Screen with history taking and on indication perform Dix-Hallpike, Head Impulse Test. Consider referral to ENT/ORL specialist. |
| Vision | Assess subjective vision problems (history taking). Objective assessment of visual problems and acuity and appropriate use of glasses (including check multi−/bifocal glasses) If indicated, refer to ophthalmologist or optometrist |
|
| Hearing | Assess subjective hearing problems (history taking). Objective assessment of hearing problems. If indicated, refer to audiologist or ENT/ORL specialist. |
|
| Activities of daily living | Functional ability | Assess Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL) in structured manner, preferably by modified Katz (community dwellers) or NEADL or Barthel (personal care, also suitable for care home residents) |
| Cognitive function | Cognition | Screen for cognitive disorders including executive functioning for example by using clock drawing test or Montreal Cognitive Assessment (MoCA) or Trail Making Test Part B (TMT-B). If indicated, further assessment and additional testing, e.g. full neuropsychological test battery. |
| Delirium | Assess presence of delirium, preferably structured by, e.g. 4AT Delirium Assessment Tool (4AT), Delirium Observation Screening Scale (DOS) or Confusion assessment method (CAM), with clinical judgement. | |
| Behaviour | Assess behaviour, preferably structured. | |
| Autonomic function | Orthostatic Hypotension | Measure blood pressure first supine (after minimum of 5 minutes of bed rest) and repeatedly upon standing. Preferably continuously, or alternatively at 1 minute intervals up to minimal 3 minutes and optimally 5 minutes , check for symptom recognition. |
| Urinary incontinence | Assess with the 3IQ screening test. Additional testing and/or referral to urologist/gynaecologist. | |
| Disease history | Cardiovascular disorders | Assess by focused history taking about cardiovascular symptoms, history of cardiovascular disease, focused cardiovascular physical examination, measurement of orthostatic hypotension (see below for details), 12-lead surface electrocardiogram. If indicated, further assessment (may include tilt table testing including carotid sinus massage, ambulatory rhythm monitoring and/or blood pressure monitoring). Consider referral to cardiologist or syncope specialist. |
| Contributing diseases/atypical disease presentation | Perform a clinical geriatric assessment (history taking, physical examination, laboratory measurements, additional testing when indicated) with specific attention towards diabetes mellitus, osteoarthritis, neurological disorders including PD, polyneuropathy and stroke, cardiovascular diseases (see above), cognition (see above), depressive disorders (see below), delirium, anaemia, electrolyte disorders, thyroid disease, frailty, sarcopenia and fracture risk (osteoporosis). Assess for potential atypical disease presentation of acute conditions such as pneumonia, especially in acute care setting. |
|
| Parkinson Disease | Assess mobility problems (gait and balance control, strength, see above) including FOG, cognition including dual tasking (DT) (see above) and orthostatic hypotension (see above). | |
| Depressive disorders | Screen for depressive disorder (minimally 2 screening questions) for example by Geriatric Depression Scale (GDS). Consider referral to specialist. |
|
| Medication history | Medication | Perform a structured medication review that entails considering deprescribing of psychotropic, cardiovascular and other FRIDs, for example by applying STOPPFall or STEADI instrument. |
| Nutrition history | Nutritional status | Screen for malnutrition for example by MNA, Malnutrition Universal Screening Tool (MUST), Malnutrition Screening Tool (MST); for obesity; for sarcopenia (including sarcopenic obesity); for vitamin deficiencies (vitamin D see below; vitamin B1, B12, folic acid) and for substance abuse as well as light-moderate alcohol use. |
| Vitamin D | Assess vitamin D status in community dwellers based on local guidelines. If at high risk for deficiency (care home residents, home bound) measurement is not indicated as standard supplementation applies. | |
| Environmental risk | Environment | Recommended assessment tools for hazards are Westmead Home Safety Assessment and the Falls Behavioural Scale for the Older Person. In LMIC non-occupational therapists and self-administered home hazard assessment checklists are available |
Table 5.
List of recommendations from the WFGs by Working Groups*
| WG/domains | Area or Domain | Recommendation | Grade |
|---|---|---|---|
| WG 1 Gait and Balance Assessment Tools to Assess Risk for Falls |
Stratification | We recommend including gait speed for predicting falls risk. As an alternative the Timed Up and Go Test can be considered, although the evidence for fall prediction is less consistent. |
1A 1B |
| Assessment | We recommend that Gait and Balance should be assessed. | 1B | |
| WG 2 Polypharmacy, Fall Risk Increasing Drugs, and Falls |
Assessment | We recommend assessing for fall history and the risk of falls before prescribing potential fall risk increasing drugs (FRIDs) to older adults. |
1B |
| Assessment | We recommend the use of a validated, structured screening and assessment tool to identify FRIDs when performing a medication review or medication review targeted to falls prevention in older adults. | 1C | |
| Intervention | We recommend that medication review and appropriate deprescribing of FRIDs should be part of multidomain falls prevention interventions. | 1B | |
| Intervention | We recommend that in long-term care residents, the falls prevention strategy should always include rational deprescribing of fall-risk-increasing drugs. | 1C | |
| WG 3 Cardiovascular Risk Factors for Falls |
Assessment | We recommend, as part of a multifactorial falls risk assessment, that a cardiovascular assessment that initially include cardiac history, auscultation, lying and standing orthostatic blood pressure, and surface electrocardiogram should be performed. | 1B |
| Assessment | In the absence of abnormalities on initial cardiovascular assessment, no further cardiovascular assessment is required, unless syncope is suspected (i.e. recurrent unexplained falls). | 1C | |
| Assessment | We recommend that the further cardiovascular assessment for unexplained falls should be the same as that for syncope, in addition to the multifactorial falls risk assessment. | 1A | |
| Intervention | We recommend that management of orthostatic hypotension should be included as a component of multidomain intervention in fallers. | 1A | |
| Intervention | We recommend that interventions for cardiovascular disorders identified during assessment for risk of falls should be the same as that for similar conditions when associated with syncope, in the addition to other interventions based on the multifactorial falls risk assessment. | 1B | |
| WG 4 Exercise Interventions for Prevention of Falls and Related Injuries |
Exercise Intervention | We recommend exercise programmes for fall prevention for community-dwelling older adults which include balance challenging and functional exercises (e.g. sit-to-stand, stepping), with sessions three times or more weekly which are individualised, progressed in intensity for at least 12 weeks and continued longer for greater effect. | 1A |
| Exercise Intervention | We recommend inclusion, when feasible, of Tai Chi and/or additional individualised progressive resistance strength training. | 1B | |
| Exercise Intervention | We recommend individualised supervised exercise as a falls prevention strategy for adults living in long-term care settings. | 1B | |
| Exercise Intervention | We recommend that adults with PD at an early to mid-stage and with mild or no cognitive impairment are offered individualised exercise programmes including balance and resistant training exercise | 1A | |
| Exercise Intervention | We conditionally recommend that adults after a stroke participate in individualised exercise aimed at improving balance/strength/walking to prevent falls | 2C | |
| Exercise Intervention | We recommend that adults after sustaining a hip fracture participate in individualised and progressive exercise aimed at improving mobility (i.e. standing up, balance, walking, climbing stairs) as a fall prevention strategy. | 1B | |
| Exercise Intervention | We conditionally recommend that such programmes after a hip fracture be commenced as in-patients and be continued in the community. | 2C (In-patients) & 1A (Community) | |
| Intervention | We recommend that community-dwelling adults with cognitive impairment (mild cognitive impairment and mild to moderate dementia) participate in exercise to prevent falls, if willing and able to do so. | 1B | |
| WG 5 Falls in Hospitals and Care Homes |
Hospital Assessment | We recommend that hospitalised older adults >65 years of age have a multifactorial falls risk assessment. We recommend against using scored falls risk screening tools in hospitals for multifactorial falls risk assessment in older adults. | 2B |
| Hospitals management and interventions | We recommend that tailored education on falls prevention should be delivered to all hospitalised older adults (≥65 years of age) and other high-risk groups. | 1A | |
| Hospitals management and interventions | We recommend that personalised single or multidomain falls prevention strategies based on identified risk factors or behaviours (or situations) be implemented for all hospitalised older adults (≥65 years of age), or younger individuals identified by the health professionals as at risk of falls. | 1C (Acute care) & 1B (Sub-acute care) | |
| Care homes assessment | We recommend against falls risk screening to identify care home residents at risk for falls and we recommend that all residents should be considered at high risk of falls. | 1A | |
| Care homes assessment | We recommend performing a multifactorial falls risk assessment at admission to identify factors contributing to fall risk and implementing appropriate interventions to avoid falls and fall-related injuries in care home resident older adults. | 1C | |
| Care homes assessment | We recommend conducting a post-fall assessment in care home residents following a fall in order to reassess fall risk factors, adjust the intervention strategy for the resident and avoid unnecessary transfer to acute care. | E |
(Continued)
Table 5.
Continued.
| WG/domains | Area or Domain | Recommendation | Grade |
|---|---|---|---|
| Care Homes Management and Interventions | We recommend a multifaceted approach to falls reduction for care home residents including care home staff training, systematic use of a multidomain decision support tool and implementation of falls prevention actions | 1B | |
| Care homes management and interventions | We recommend against the use of physical restraints as a measure for falls prevention in care homes. | 1B | |
| Care homes management and interventions | We recommend nutritional optimisation including food rich in calcium and proteins, as well as vitamin D supplementation as part of a multidomain intervention for falls prevention in care home residents. | 1B | |
| Care homes management and interventions | We recommend including the promotion of physical activity (when feasible and safe) as part of a multidomain falls prevention intervention in care homes. | 1C | |
| WG 6 Cognition and Falls |
Cognition Assessment | We recommend that routine assessment of cognition should be included as part of multifactorial falls risk assessment in older adults. | 1B |
| Cognition Assessment | We recommend including both the older adult's and caregiver’s perspectives, when creating the individual falls prevention care plans for adults with cognitive impairment since this strategy has shown better adherence to interventions and outcomes. | 1C | |
| WG 7 Falls and PD and Related Disorders |
Assessment | We conditionally recommend a falls risk assessment for older adults with PD, including a self-report 3-risk factor assessment tool, which includes a history of falls in the previous year, FOG in the past month, and slow gait speed | 2B |
| Management and Intervention | We conditionally recommend that older adults with PD be offered multidomain interventions | 2B | |
| Management and Intervention | We recommend that adults with PD at an early to mid-stage and with mild or no cognitive impairment are offered individualised exercise programmes including balance and resistance training exercise. | 1A | |
| Management and Intervention | We conditionally recommend exercise training, targeting balance and strength, be offered to people with complex phase PD if supervision by a physiotherapist or other suitably qualified professional is available. | 1C | |
| WG 8 Falls and Technology |
Assessment and Interventions | We conditionally recommend using telehealth and/or smart home systems (when available) in combination with physical exercise as part of the falls prevention programmes in the community. | 2C |
| Interventions | Current evidence does not support the use of wearables for falls prevention. Emerging evidence show that when wearables are used in exercise programmes to prevent falls, they may increase participation. | 2C | |
| WG 9 Falls in Low- and Middle-Income Countries |
Implementation | Local context needs to be considered when implementing fall prevention programmes in LMIC. | 1B |
| Assessment | We conditionally recommend prioritising assessments of risk factors for cognitive impairment, obesity including sarcopenic obesity, diabetes, lack of appropriate footwear and environmental hazards as falls risk factors in LMIC | 2C | |
| Assessment | We conditionally recommend that in LMIC settings clinicians and caregivers use validated tools that are freely available in their country of residence to assess mobility, dependent on resource availability. | E | |
| WG 10 Multifactorial Assessment and Interventions for Falls (Environment recommendations informed by the ad hoc expert group on Environment and Falls) |
Multifactorial Assessment | We recommend multiprofessional, multifactorial assessment should be offered to community-dwelling older adults identified to be at high risk of falling, to guide tailored interventions. | 1B |
| Multidomain Interventions | We recommend multidomain interventions, informed by a multiprofessional, multifactorial falls risk assessment, should be offered to community-dwelling older adults identified to be at high risk of falling. | 1B | |
| Multifactorial (Environmental) Assessment | We recommend identification of an individual’s environmental hazards where they live and an assessment of their capacities and behaviours in relation to them, by a clinician trained to do so, should be part of a multifactorial falls risk assessment. | 1B | |
| Multifactorial (Environmental) Interventions | We recommend modifications of an older adult's physical home environment for fall hazards that consider their capacities and behaviours in this context, should be provided by a trained clinician, as part of a multidomain falls prevention intervention. | 1B | |
| WG 11 Older Adults' Perspectives on Falls |
Stratification | We recommend clinicians should routinely ask about falls in their interactions with older adults. | 1A |
| Assessment | As part of a comprehensive fall assessment, clinicians should enquire about the perceptions the older adult holds about falls, their causes, future risk, and how they can be prevented. | 1B | |
| Interventions | A care plan developed to prevent falls and related injuries should incorporate the goals, values and preferences of the older adult. | 1B | |
| WG 12 Concerns about Falling and Falls |
Assessment | We recommend including an evaluation of concern about falling in a multifactorial falls risk assessment of older adults | 1B |
| Assessment | We recommend using a standardized instrument to evaluate concerns about falling such as the Falls Efficacy Scale International (FES-I) or Short FES-I in community-dwelling older adults. | 1A | |
| Assessment | We recommend using the FES-I or especially the Short FES-I for assessing concerns about falling in acute care hospitals or long-term care facilities. | 1B | |
| Assessment | We recommend exercise, cognitive behavioural therapy and/or occupational therapy (as part of a multidisciplinary approach) to reduce fear of falling in community-dwelling older adults. | 1B |
*Note: these are the 12 original Working Groups that addressed the knowledge gaps identified from the review of previous clinical practice guidelines.
We will not cover all components of a CGA, for which there is guidance elsewhere [49], but we do note the important associations of falls with other geriatric syndromes [50] and conditions, the management of which may be important for some individuals. Falls in older adults, particularly those living with frailty, should be considered a warning sign of potentially unidentified underlying conditions. A fall may be the presenting feature of acute medical conditions such as pneumonia (particularly if accompanied by delirium [51]) or myocardial infarction without chest pain [52]. Choice of assessments in clinical practice should thus consider the clinical characteristics of the older adult (e.g. frail vs. non-frail), the setting (e.g. community, outpatient clinic, acute care, long-term care) and the resources available (e.g. cost, training, equipment).
Incorporating the perspective of the older adult
Strong recommendation. As part of a multifactorial falls risk assessment clinicians should enquire about the perceptions, the older adult holds about falls, their causes, future risk and how they can be prevented (Appendix 2, available in Age and Ageing online). GRADE: 1B.
Expert recommendation. As part of a multifactorial falls risk assessment clinicians should enquire about the goals and priorities; attitudes to activities, independence and risk; and willingness and capability of older adults to inform decision making on potential interventions. GRADE: E.
Recommendation details and justification
Studies indicate that older adults, particularly men, are reluctant to report falls with less than a third mentioning them to their clinician if not directly asked [34].
Many older adults have low levels of knowledge about causes and prevention of falls, with erroneous beliefs about the causes, their own risk of falling and how best to minimise the likelihood of future falls [53–57]. Knowing what their beliefs are would allow clinicians the opportunity to answer questions, address misconceptions and provide accurate information about falls and their prevention.
Multifactorial falls risk assessment
Strong recommendation. Offer multiprofessional, multifactorial assessment to community-dwelling older adults identified to be at high risk of falling, to guide tailored interventions (Appendix 2, available in Age and Ageing online). GRADE: 1B.
Recommendation details and justification
A multifactorial falls risk assessment for those at high risk of falling, which enables advice for falls prevention and management interventions, includes the following domains: gait and balance, muscle strength, medications, cardiovascular disorders including orthostatic hypotension, dizziness, functional ability and walking aids, vision and hearing, musculoskeletal disorders, foot problems and footwear, neurocognitive disorders (including delirium, depression, dementia, behavioural issues such as impulsiveness and agitation), neurological disorders (e.g. PD, neuropathy), underlying diseases (acute and chronic), concerns (fear) about falling, environmental hazards, nutritional status (including protein intake and vitamin D), alcohol consumption, urinary incontinence and pain.
The evidence for a multifactorial falls risk assessment follows from evidence that effective multidomain interventions should be based on modification where possible of the fall risks factors identified in the individual, and not on a generic intervention regardless of individual characteristics.
The strength of the evidence differs per component. Details can be found below in the section addressing individual components.
Assessment details for individual components
Gait and balance assessment
Strong recommendation. Gait and Balance should be assessed as part of the risk assessment of falls (see Table 4; Appendix 2, available in Age and Ageing online). GRADE: 1B.
Recommendation details and justification
Gait and balance impairment is one of the domains that most consistently predicts future falls [32].
Physical function tests of gait and balance can help choose fall prevention exercises, prescribe level of difficulty and dose and monitor progress.
Assessment tools that are useful and commonly used in the assessment of gait and balance include: gait speed, The Timed Up and Go (TUG) test, the untimed Get Up And Go test, Berg Balance Scale, the Chair Stand test (CST) and Short Physical Performance Battery (SPPB).
The SPPB includes timed tests of sit to stand, balance in standing and walking and has been found sensitive to change in intervention studies [58]. The TUG is another popular choice as it combines assessment of rising from sitting, walking and turning [59]. The untimed Get Up and Go test provides similar qualitative information [60].
For more impaired populations, tools that include more basic tasks will be more useful, such as the DEMMI [61], which also includes bed mobility. In more able populations, tools that include more challenging tasks can be used such as the Berg Balance Scale [62], which also includes single leg stance, turning and stepping onto a stool.
It may also be useful to assess rising from the floor and dual task activity performance. Other tests used in gait and balance assessment include the CST [42], One Leg Stand [63], Functional Reach [64], Dual Task tests [65], the Tinetti test/POMA (balance and gait subscales) [66], the MiniBEST Test [67] and the Physiological Profile Assessment Performance test [68].
The choice of test will also depend on equipment availability, resources, space and time available as well as familiarity and training. The Rehabilitation Measures Database provides a useful description of options and their clinimetric properties (www.sralab.org/rehabilitation-measures).
A structured assessment of gait by a trained clinician can be helpful in directing investigations for underlying conditions that may increase falls risk by impairing gait [69, 70].
The Floor Transfer Test is a reliable and valid measure for screening for physical disability, frailty and functional mobility [71, 72].
Medication assessment
Strong recommendation. Assess for fall history and the risk of falls before prescribing potential fall risk increasing drugs (FRIDs) to older adults (Appendix 2, available in Age and Ageing online). GRADE: 1B.
Strong recommendation. Use a validated, structured screening and assessment tool to identify FRIDs when performing a general medication review or medication review targeted to falls prevention. GRADE: 1C.
Recommendation details and justification
There is strong evidence that certain medications’ use increases fall risk in older adults, that a structured approach improves FRID identification and that medication review and deprescribing of FRIDs can significantly reduce fall risk [73–79].
Before prescribing potential FRIDs to older adults, enquire about falls and consider the relative benefits and risks of initiating therapy. For example, the following initiatives have listed FRIDs: Centre for Disease Control and Prevention’s STEADI initiative [80] and STOPPFall [76].
Medication-review tools such as the STOPP/START, STOPPFall, STOPPFrail, Beers Criteria, FORTA or Web-based Meds 75+ Guide [6, 76, 81–83] are suitable to systematically identify medication-related fall risks in older adults and to optimise deprescribing.
STOPPFall is a screening tool used to identify drugs that increase the risk of falls in older adults [84]. An online interactive version of the STOPPFall deprescribing tool is freely available: https://www.eugms.org/research-cooperation/task-finish-groups/frid-fall-risk-increasing-drugs.html.
Cognitive assessment
Strong recommendation. Assessment of cognition should be included as part of a multifactorial falls risk assessment in older adults (Appendix 2, available in Age and Ageing online). GRADE: 1B.
Recommendation details and justification
Dementia and mild cognitive impairment double the risk of falls and falls-related injuries including hip fractures, fractures of the arm and head injuries [41].
Low cognitive performance in older adults, particularly of executive function, even in the absence of a known cognitive impairment or formal diagnosis of dementia, is associated with an increased risk of falls, justifying cognitive testing as part of comprehensive falls risk assessment in all older adults [85].
Because executive dysfunction is strongly associated with falls, global cognitive screening tests that include executive function components such as the Montreal Cognitive Assessment (MoCA) or specific executive function tests, such as the Trail Making Test (TMT) part B, can be used [86].
Training on the administration of the cognitive tests used, to improve execution is recommended.
Concerns about falling and falls
Strong recommendation. Include an evaluation of concerns about falling in a multifactorial falls risk assessment of older adults (Appendix 2, available in Age and Ageing online). GRADE: 1B.
Strong recommendation. Use a standardized instrument to evaluate concerns about falling such as the Falls Efficacy Scale International (FES-I) or Short FES-I in community-dwelling older adults. GRADE: 1A.
Recommendation details and justification
We recommend clinicians adopt a holistic approach, combining concern about falling with balance and/or gait assessment as this will help to put the degree of concern in context, when assessing older adults in the community. Concerns about falling—or the closely related notion of fear of falling—shows heterogeneous results in predicting future falls in the community. The rationale for including concerns about falling as part of a comprehensive fall assessment is that this is a measure of an older adult's perceptions about the falls they have experienced, the impact falls have had on their quality of life, their openness to various interventions (e.g. an older adult inappropriately very fearful of falling may be reluctant to increase their physical activity and follow an exercise programme if this is not dealt with), and as a treatment outcome in a subset of older adults.
The Falls Efficacy Scale International (FES-I) and the Short Falls Efficacy Scale International (Short FES-I) have a strong to moderate level of evidence for their use in older adults living in the community. There is evidence from a recent systematic review and meta-analysis of 59 studies that the FES-I and Short FES-I are reliable and valid tools when used with both healthy older adults and those with conditions that put them at a greater risk of a fall (e.g. multiple sclerosis, stroke, vestibular disorders, PD) [87]. Both instruments demonstrate good internal consistency, test–retest reliability, inter-rater reliability and construct validity in these populations [87].
The complexity of the terms used for fall-related psychological effects arises from their different underlying constructs. These terms include ‘concerns about falling’, ‘fear of falling’, anxiety, ‘balance-related confidence’ and ‘self-efficacy’. More recent models are linking anxiety, fear of falling and self-efficacy [88, 89].
While fear of falling is the term used in much of the available peer-reviewed literature, making enquiries about concerns offers advantages to fear of falling. It is ‘less intense and emotional (and therefore may be more socially acceptable for older adults to disclose)’ [90], while fear has ‘psychiatric connotations implying analogy to phobias which may or may not be accurate’ [91].
The older adult panel we consulted about the recommendations preferred the term concern over fear. Based on this, we recommend that clinicians use the term concerns about falling when making enquiries. This is also congruent with the wording of the recommended FES-I questionnaires (Appendix 2, available in Age and Ageing online).
FES-I and Short FES-I are available free of charge in over 30 languages from www.fes-i.org and can be self-administered or done as part of a clinical interview. The 7-item Short FES-I can be useful for clinicians for a rapid assessment.
Cardiovascular assessment
Strong recommendation. Perform, as part of a multifactorial falls risk assessment, a cardiovascular assessment that initially includes cardiac history, auscultation, lying and standing orthostatic blood pressure, and surface 12-lead electrocardiogram (Appendix 2, available in Age and Ageing online). GRADE: 1B.
Strong recommendation. In the absence of abnormalities on initial cardiovascular assessment, no further cardiovascular assessment is required, unless syncope is suspected (i.e. described or witnessed syncope/pre-syncope or recurrent unexplained falls). GRADE: 1C.
Strong recommendation. We recommend that the further cardiovascular assessment for unexplained falls should be the same as that for syncope, in addition to the multifactorial falls risk assessment. GRADE: 1A.
Recommendation details and justification
Recurrent unexplained falls are most likely associated with a cardiovascular cause [92–95].
The commonest cardiovascular causes of falls in rank order are orthostatic hypotension, vasovagal syndrome, carotid sinus hypersensitivity, bradyarrhythmias and atrial and ventricular tachyarrhythmias [96].
The investigation (and subsequent management and specialist referral criteria) of syncope, and therefore, recurrent unexplained falls can be performed according to locally applicable guidelines such as the 2018 European Society of Cardiology Guidelines for the diagnosis and management of syncope [94].
If orthostatic hypotension is suspected but not detected using traditional methods—oscillometer or sphygmomanometer, referral for beat-to-beat orthostatic measurement is recommended as the association of falls with orthostatic hypotension measured using beat-to-beat methods is more consistent [97].
If vasovagal syncope or delayed orthostatic hypotension is suspected and diagnostic uncertainty remains, older adults should be referred for head up tilt tests [94, 98].
If arrhythmias are suspected after clinical assessment, based on locally applicable guidelines individuals should be referred for external or internal cardiac monitoring [19, 94, 99].
For assessment for orthostatic hypotension, individuals should be supine for at least 5 minutes before baseline blood pressure is recorded; on standing, blood pressure should be taken as soon as possible (40–60 seconds), followed by measurements at 1-minute intervals up to 3 minutes, or up to 5 minutes if symptoms suggested a delayed orthostatic hypotension response [94, 100].
Orthostatic hypotension most commonly occurs as a result of dehydration, concomitant medications, autonomic dysfunction and with alpha synucleopathy diseases (such as PD, dementia with Lewy Bodies or multisystem atrophy). It is also common in older adults with hypertension [96, 101].
Short-term 24–48 hours cardiac rhythm monitoring is not indicated unless events occur daily. Prolonged external or internal ambulatory cardiac monitoring is indicated if arrhythmias are suspected as a cause of falls or syncope, after clinical assessment [19, 94, 99].
Older adults with unexplained syncope, suspected syncope or unexplained falls who require carotid sinus massage or head up tilt tests should be referred to an appropriate specialist, according to locally applicable guidelines [94].
Dizziness and vestibular disorders assessment
Expert recommendation. Routinely ask about dizziness symptoms, and undertake follow-up assessment as necessary to identify cardiovascular, neurological and/or vestibular causes (Appendix 2, available in Age and Ageing online). GRADE: E.
Recommendation details and justification
Dizziness is a common complaint in older adults who fall, with different meanings between individuals, and often no single explanatory cause. Careful history taking is of particular importance. Presyncope and observable unsteadiness or ataxia may be present.
Additionally, the vestibular system has a key role in the control of posture and gait, and there is evidence of a high incidence of both benign paroxysmal positional vertigo and vestibular dysfunction in those presenting with falls [102–105]. In younger adults, such disorders can often be identified in the clinical history by a reported sensation of vertigo with clear positional or motion-provoked triggers. Identifying cases of vestibular dysfunction is more challenging in older adults due to more variable symptoms.
Where vertigo is reported, positional tests should be used to identify cases of benign paroxysmal positional vertigo from non-cases (e.g. Dix-Hallpike, Head Impulse Test); however, the sensitivity of case-finding algorithms based purely upon symptoms compared with screening with positional testing in older adults is unknown [102–105].
Vision and hearing assessment
Expert recommendation. Enquire about vision impairment as part of a multifactorial falls risk assessment, measure visual acuity and examine for other visual impairments such as hemianopia and neglect where appropriate. GRADE: E.
Expert recommendation. Enquire about hearing impairment as part of a multifactorial falls risk assessment, measure and examine for hearing impairments and refer to a specialist where appropriate. GRADE: E.
Recommendation details and justification
Impaired vision is an important and independent risk factor for falls in older adults who live in the community. Vision loss is the third most common chronic condition in older adults, and about 20% of people aged 70 years or older have a visual acuity of less than 6/12 [106]. Many older adults wear spectacles with outdated prescriptions or no spectacles at all and would benefit from wearing new spectacles with the correct prescription. This indicates the importance of regular eye examinations to prevent vision-related impairment and improve the quality of life.
Visual screening should not be limited to measurement of visual acuity and should incorporate contrast sensitivity and depth perception.
Impaired hearing is an independent risk factor for falls in older adults [107]. Possible explanations for the association between hearing loss and falls include coexistent vestibular pathology that increases fall risk, reduction in cognitive capacity for maintaining balance given the cognitive load of hearing loss and a loss of auditory perception leading to reduced spatial awareness [108]. Hearing loss itself is a highly prevalent condition among older adults that can be readily treated with amplification
Accessibility to hearing and visual assessments in LMIC should be enhanced and their additional benefit of falls prevention should be emphasised.
Delirium
Delirium, cognitive impairment and dementia are independent risk factors for falls in older adults in hospital settings, residential aged care, at home and in the community [78]. The key to preventing falls in older adults with these conditions is to deliver evidence-based, person-centred care. When delirium, dementia and cognitive impairment are managed well, falls are less prevalent [109]. Adapting the environment to promote safety and educating caregivers in strategies for safe mobility can also be of benefit in older adults with delirium. There is some evidence that staff education can help to reduce falls of hospitalised older adults experiencing delirium [110, 111]. Multidomain strategies which have been shown to reduce the risk of delirium include cognitive stimulation, daily orientation, early mobilisation, vision and hearing, fluid management, constipation management, feeding assistance, sleep and family involvement [112, 113]. At present, there is evidence that these strategies might reduce falls, therefore they should be considered as part of a comprehensive care package for older adults in hospital [114]. Promoting mobility to maintaining independence is important, yet there is a tension that needs to be managed between promoting mobility and preventing falls, especially in very frail older adults [115].
Urinary symptoms and incontinence assessment
Expert recommendation. Enquire about urinary symptoms as part of a multifactorial falls risk assessment GRADE: E.
Recommendation details and justification
A recent comprehensive systematic review and meta-analysis included 38 articles (total participants 230,129) and found that urinary incontinence was significantly associated with falls [116]. Subgroup analyses based on the age and sex of the participants revealed a significant association between urinary incontinence and falls in older (≥65 years) participants, and in both men and women.
A subgroup analysis showed that a significant association between urinary incontinence and falls was observed in older adults with both urgency urinary incontinence and stress urinary incontinence [116]. A recent systematic review and meta-analysis also showed that nocturia is associated with a 1.2-fold increased risk of falls and possibly a 1.3-fold increased risk of fractures [117].
The 3IQ screening questions for urinary incontinence can help to differentiate between stress, urge and mixed types of incontinence [118].
Pain assessment
Expert recommendation. Enquire about pain as part of a multifactorial falls risk assessment, followed as indicated by a comprehensive pain assessment. GRADE: E.
Recommendation details and justification
Pain is an established risk factor for falling [107, 119]. Symptoms of pain are common in older adults, with over 60% of community dwelling older adults reporting pain, mostly in multiple sites [120]. The most prevalent condition resulting in pain is arthritis, which is an independent risk factor for falling [107]. Other chronic conditions resulting in pain in older adults include diabetic complications, cancer-related pain and post-stroke pain [121].
A comprehensive pain assessment is needed to guide appropriate management. This includes defining its cause, type (nociceptive, neuropathic) and intensity by using a pain rating scale designed for older adults [122].
Environmental assessment
Strong recommendation. Identification of an individual’s environmental hazards where they live and an assessment of their capacities and behaviours in relation to them, by a clinician trained to do so, should be part of a multifactorial falls risk assessment. GRADE:1B.
Recommendation details and justification
Environmental factors are important in many falls. Environmental risk factors are influenced by the interaction between a person’s exposure to environmental fall hazards (such as slippery stairs, poor lighting at entrances, lack of a grab rail), risk taking behaviour (such as clutter in walkways, unsafe climbing on chairs or ladders) and their physical capacity [123].
Assessment by a clinician trained to do so (e.g. occupational therapists) needs to include the assessment of environmental hazards, capacities and behaviours of the individual and an understanding of the effect of the environment on function [77, 124].
Other elements considered crucial are using an assessment tool validated for the broad range of home fall-hazards and fall risk assessment along with consideration of the functional capacity of the person (including habitual behaviours, functional vision, cognition and mobility) within the context of their environment [77, 124]. Recommended assessment tools for hazards are the Westmead Home Safety Assessment and the Falls Behavioural Scale for the Older Person [125, 126].
If applicable, assess for appropriateness and proper use of walking aids including that the aid is not damaged or unsafe.
In LMIC, addressing environmental hazards by trained clinicians is also considered a priority. Due to lack of resources in some LMIC, training of personnel to conduct assessments, appropriate prescription of walking aids, along with the availability of affordable equipment and maintenance should be emphasised in LMIC settings.
The wording and grading of these recommendations are informed by a forthcoming update of the Cochrane systematic review [127].
Depression assessment
Expert recommendation. Enquire about depressive symptoms as part of a multifactorial falls risk assessment, followed by further mental state assessment if necessary and referral to a specialist where appropriate. GRADE: E.
Recommendation details and justification
Depression is a common and important cause of morbidity and mortality in older adults worldwide, affecting around 10–15% of community-dwelling older adults. If left untreated, symptoms may persist for years. Both untreated depression and antidepressant use contribute to fall risk [107, 128]. For details on fall risk and antidepressant use, we refer to the outcomes and recommendations of WG 2 (fall-risk increasing drugs, FRIDs).
Untreated depression is independently associated with increased fall risk: a meta-analysis showed a 37% of increased risk [107].
The pathophysiologic mechanisms underlying the association between depression and falling are complex. Major mechanisms are psychomotor retardation, deconditioning, gait and balance abnormalities, impaired sleep and impaired attention. Often, multiple pathways interact and co-occur. Also, excessive concern about falling contributes to increased fall risk in depressed older adults. It negatively influences gait and balance and thereby increases tendency to fall [128].
Antidepressants are FRIDs and contribute to (or cause) falling through causing sedation, impaired balance/reaction time, orthostatic hypotension, hyponatremia, cardiac conduction delay/arrhythmia and/or drug-induced Parkinsonism [128].
Screening for depression as a risk factor for falls should be considered in older individuals in LMIC. Strategies to raise awareness and reduce stigma of depression and mental illness are needed in these countries. However, longitudinal and interventions studies are required before firm recommendations can be made in this area.
Nutritional assessment including vitamin D
Expert recommendation. Assess nutritional status including vitamin D intake as part of a multifactorial falls risk assessment, followed by supplementation where appropriate. GRADE: E.
Recommendation details and justification
Nutritional assessment is an important part of the multifactorial falls risk assessment and should include assessment of adequate vitamin D intake and serum 25 OH vitamin D levels, when appropriate, and substance abuse and excessive alcohol intake, as well.
A recent systematic review showed that both nutritional status and body mass index (BMI) are associated with the risk of falls in community-dwelling older adults. In particular, being at risk of malnutrition or being malnourished may increase the risk of a fall. BMI showed a U-shaped association with the risk of falls, and BMI values between 24.5 and 30.0 were associated with the lowest risk of fall [129].
Poor nutritional status can be both a consequence of underlying morbid conditions and a causal factor of pathological ageing process and higher mortality. Underweight and undernourished individuals may both have increased risk of falls due to sarcopenia, impaired mobility and walking instability, as well as worse functional and clinical status. On the other hand, excess weight in obese people may also have a negative impact on postural stability, self-sufficiency and physical activity, all factors that may be associated with the falls [129].
Malnutrition assessment can be performed by using validated tools, such as the Mini Nutritional Assessment (MNA) [130].
Assessment of fracture risk
Osteoporotic fractures are associated with high morbidity, mortality and cost to society in terms of the use of health and social services. Both bone fragility and propensity to fall are important determinants of fracture risk. International consensus advises that fracture prevention should include identification of older adults at high falls risk, interventions to reduce that risk, identifying those with bone fragility (including osteoporosis) and instituting measures to reduce fracture risk (both pharmacological and non-pharmacological [131]).
Adults with low trauma fractures and those with osteoporosis should have a falls risk assessment. Fracture liaison services, which identify people with recent fractures, are now in place in many areas and their remit should include identification of those at high falls risk in addition to investigating for osteoporosis [132].
Conversely, those identified as having a moderate to high falls risk should have a bone health assessment using local protocols. In this regard, fracture risk assessment tools such FRAX, Garvan and QFracture can be employed to identify older adults at high fracture risk, and bone densitometry can be used to confirm osteoporosis [133, 134]. International consensus osteoporosis management guidelines are in place to guide treatment [135].
Individuals aged 60 years and over with pre-existing comorbidities and increased risk of fractures should be assessed regularly for modifiable falls risk factors in LMIC. Furthermore, in individuals with fractures or increased risk of fractures within LMIC, falls risk assessments should be incorporated into their management strategies.
Management and interventions
Management of older adults at low fall risk
Expert recommendation. Provide advice on how to maintain safe mobility and optimise physical functioning to older adults at low risk of falls from a clinician trained to do so. Such advice should consider the circumstances, priorities, preferences and resources of the older adult. This advice should reinforce health promotion/prevention messaging relevant to falls and fracture risks such as those on physical activity, lifestyle habits and nutrition including vitamin D intake (see algorithm, Figure 1). GRADE: E.
Recommendation details and justification
Older adults classified as low risk by our algorithm have an incidence of a single fall in the next year of approximately 20–30% [2, 136], but the individual risk varies according to easily recognisable attributes such as vision, hearing and foot problems, but also less measurable factors such as: context (what does the individual need to do and in what environment?); behaviours (is the person cautious, impulsive, erratic?); and, transient factors such as illness, or absence of usual support. Our recommendations promote a generic primary preventative approach which can be adapted to individual circumstances and characteristics.
There is a growing body of evidence showing a relationship between physical activity and fall risk at a population level, and evidence for effective interventions on habitual physical activity and exercise programmes for older adults at low to intermediate risk for falls [2, 137]. While the interventions may well merit a higher grade, this recommendation on provision of advice is at Grade E, as there is insufficient evidence on how this is best provided, taking into consideration the potential risks, including falls, to habitually inactive people who embark on activities such as brisk walking.
Recommendations on types and amounts of habitual physical activity and the avoidance of being sedentary are provided by national and international guidelines, such as the World Health Organisation [138] guidelines on physical activity and sedentary behaviour, the American College of Sports Medicine, and the UK Chief Medical Officers' Physical Activity Guidelines.
The WHO and the UK Physical Activity guidelines take a life course approach and include a specific focus on functional mobility and falls, as well as considering the merits of various activities and sports. The American College of Sports Medicine provides a wide range of exercise prescriptions for various situations.
The WHO and the UK Physical Activity guidelines recommend activities which challenge balance and include resistance training twice per week. General physical activity alone (e.g. walking) is unlikely to prevent falls.
We recommend that, where possible and safe, older adults should aim to participate in 150–300 minutes per week of intermediate-intensity physical activity or 75–150 minutes per week of vigorous-intensity physical activity. There is evidence from observational studies that meeting physical activity guidelines of moderate to vigorous intensity activity reduces future falls risk and reduces the chance of an individual falling, although these findings remain uncertain [139]. This promotion of healthy lifestyle can be expected to decrease fall risk indirectly through its positive impact on deconditioning, frailty, sarcopenia and cardiovascular health.
Uptake and adherence to exercise interventions and to increasing habitual physical activity may be helped by behaviour-change approaches such as coaching, supervision, group activity and educational material.
Generic health promotion guidelines include advice on lifestyle habits, periodic vision and hearing checks and footcare. WHO has provided guidelines on primary and community-based assessment and first level responses across five key domains which are collectively predictive of future disability [140].
Falls prevention advice in low risk older adults may include referral to local community health promotion or ‘ageing well’ programmes where available.
We recommend inclusion of fracture risk management (including need for osteoporosis treatment) to reduce fracture risk.
Interventions for community dwelling older adults at intermediate fall risk
Expert recommendation. Offer an exercise programme based on an individual assessment and according to the recommendations in the Exercise Interventions section (see algorithm, Figure 1). GRADE: E.
Recommendation details and justification
Supervised exercises that target balance and strength prevent falls [141]. Fall prevention exercise should focus on maintaining balance during functional tasks needed for daily life. The most relevant tasks for individuals vary according to lifestyle, domestic needs, physical function, environment and preferences.
Effective fall prevention programmes include individualised exercises that enable or support daily tasks or similar movements. Such exercises include sit-to-stand, squats, reaching which standing, standing with a narrower base of support, stepping and walking in different directions, speeds, environments and while dual tasking. Weights can be added to some exercises to increase difficulty. Exercises should be challenging (to enhance neural, muscular and skeletal function) but safe (to prevent injuries) and achievable (for sufficient dose and sense of mastery). Exercises should be reviewed and progressed regularly to ensure that optimal level of difficulty is maintained.
Multidomain interventions for community dwelling older adults at high fall risk
Developing a person-centred intervention
We recommend that a falls prevention plan be based on a holistic multifactorial falls risk assessment as previously described with shared decision being used to develop agreed goals and interventions (see Algorithm, Figure 1). This means paying attention to the entire clinical assessment and considering the priorities, beliefs, resources of the older person and other relevant individuals, such as caregivers in order to develop a feasible plan that addresses individually relevant risk factors in the context of other geriatric syndromes and conditions (Appendix 2, available in Age and Ageing online).
Strong recommendation. A care plan developed to prevent falls and related injuries should incorporate the values and preferences of the older adult. GRADE: 1B.
Strong recommendation. When creating falls prevention care plans for older adults with cognitive impairment, both the older adults’ and their caregivers’ perspectives should be included as it improves adherence to interventions and outcomes. GRADE: 1C.
Recommendation details and justification
Engaging older adults in a discussion about their preferences coupled with shared decision-making can improve adherence with recommendations and outcomes [142]. The aspects identified in a scoping review of 52 studies included: the meaning of falls, perceived causes, assessment of personal risk, reaction to this perceived risk and priority given to falls as a health concern.
For those with cognitive and functional limitations, the development and then implementation of a care plan to prevent falls and related injuries will also require the involvement and training of informal (unpaid) and/or formal (paid) caregivers.
Fall prevention interventions can be time-consuming, intensive and of long duration. An older adult should be informed of both benefits and burdens of falls prevention therapy, to enable them to make an informed choice about participation. An older adult’s knowledge and attitudes about falls and the priority they give to their prevention will determine whether, or what type, of therapeutic interventions they would be willing to engage in.
Multidomain falls risk intervention
Strong recommendation. Offer multidomain interventions, informed by a multiprofessional, multifactorial falls risk assessment to community-dwelling older adults identified to be at high risk of falling (Appendix 2, available in Age and Ageing online). GRADE: 1B.
Recommendation details and justification
Multidomain interventions encompass two or more components, individually targeted to the older adult based on findings from a multifactorial (or comprehensive) falls risk assessment. It is not a standardized set of interventions applied to everyone.
A multidomain intervention in older community-dwelling adults at a minimum should include: strength and balance exercise, medication review, management of orthostatic hypotension and cardiovascular diseases, management of underlying acute and chronic diseases, optimising vision (cataract surgery for those who need it, refraction) and hearing, addressing foot problems and appropriate footwear, vitamin D supplementation, optimising nutrition, continence management, interventions to address concerns about falling, individual education and environmental modification (including assisted devices and use of technology).
The recommended components are derived from the following literature: a 2021 comprehensive systematic review and network meta-analyses [79] on interventions for preventing falls in community dwelling older adults, two Cochrane systematic reviews [77, 143] assessing multidomain interventions for prevention of falls in older adults living in the community and two WHO summary reports on falls prevention in community dwelling older persons [24, 144].
The findings of two recent pragmatic RCTs [145, 146] suggest that both exercise and multifactorial strategies that have been shown to reduce falls in efficacy trials cannot easily be applied with sufficient fidelity through current existing services (RCTs based in UK and USA, respectively) to achieve equivalent benefits. These trial outcomes suggest the importance of the provision of sufficient resources to roll out and support high-quality sustainable delivery of fall prevention programmes that are in line with previous high quality successful efficacy trials [147, 148]. Though disappointing, the results of these two pragmatic trials did not substantively alter network meta-analysis results or our recommendations [79].
Component interventions
Exercise and physical activity interventions
Strong recommendation. Exercise programmes for fall prevention for community-dwelling older adults that include balance challenging and functional exercises (e.g. sit-to-stand, stepping) should be offered with sessions three times or more weekly which are individualised, progressed in intensity for at least 12 weeks and continued longer for greater effect (Appendix 2, available in Age and Ageing online). GRADE: 1A.
Strong recommendation. Include, when feasible, of Tai Chi and/or additional individualised progressive resistance strength training. GRADE: 1B.
Recommendation details and justification
The first recommendation applies to all older adults regardless of their assessed risk of falling or age. We recommend programmes that include balance and functional exercises (e.g. sit-to-stand, stepping): GRADE: 1A, programmes that include multicomponent exercise (i.e. multiple types of exercise), most commonly balance and functional exercises with strength exercise: GRADE: 1B, and Tai Chi: GRADE: 1B [137, 141].
Exercise programmes that need to be of sufficient intensity and duration should be delivered in a way that ensures safety and considers functional abilities.
Exercise programmes should be delivered by appropriately trained professionals who can adapt exercises appropriately to functional status and co-morbidities. These professionals could be physiotherapists, exercise physiologists or kinesiologists, trained exercise instructors or other allied health professionals. We acknowledge that this will be difficult in some settings but note that the vast majority of interventions found to be effective in trials used trained providers [137, 141].
Exercise needs to be progressive initially and maintained once a plateau is reached.
Benefits of exercise are lost on cessation so opportunities to continue with appropriate activity at the end of the programme are important. If individuals withdraw due to concurrent health issues or caring duties, they should be encouraged to return and programmes should be modified to ensure that the difficulty level and dose are appropriate [137, 141].
Exercise programmes can be delivered in a group or taught and supported as an individualised home exercise programme or a mix of both in order to achieve an effective dose [137, 141].
Group exercise, individualised home exercise or a combination of both may lead to better exercise programme adherence. In people with more severe cognitive impairment, smaller group or individual supervision may be necessary [149, 150].
Higher supervision levels or smaller group numbers are recommended for those at higher risk of a fall including those who are frail [137, 141].
An important aspect to consider is avoiding ‘long-lies’ and harm from being unable to get up from the floor. One in 8 older adults who fall report lying on the floor for more than 1 hour [151] and in those over the age of 90, up to 80% cannot rise from the floor after a fall [35]. Lying on the floor for more than an hour is associated with dehydration, electrolyte disturbance, renal failure, hypothermia, pneumonia and urinary tract infections, skin damage and pain [152, 153], and declines in mobility and restrictions in activity, probably due to fear of a repeat fall. ‘Lift and assist’ call outs should trigger falls prevention interventions [154]. Pendent or wrist alarms, telehealth falls detectors, cord alarms or mobile telephones are also important in enabling people to call for help if they cannot get up if they live alone (see section on technology) [35]. However, the oldest old often still lie on the floor for a long time before they use a call alarm so it is important to help them regain this skill if they have had a previous long-lie.
Regaining the skill to rise from the floor is most successfully re-learnt through practice of each of the specific movements required (often called backward-chaining) where the last step in the chain is taught first [155]. Some falls prevention exercise programmes also have a specific focus on this skill and have shown success in regaining this function [156].
Medication interventions
Strong recommendation. A medication review and appropriate deprescribing of FRIDs should be part of multidomain falls prevention interventions (Appendix 2, available in Age and Ageing online). GRADE: 1B.
Strong recommendation. We recommend that in long-term care residents, the falls prevention strategy should always include rational deprescribing of fall-risk-increasing drugs. GRADE: 1C.
Recommendation details and justification
Medication review with the aim of deprescribing FRIDs is a standard component of multidomain interventions to prevent falls, which have been proven effective in reducing the rate of falls (for details, we refer to WG 10) [24, 77]. It has also been shown to be one of the effective components of a multidomain intervention in a recent systematic review and network meta analyses [79].
Older adults characteristics, including frailty status, polypharmacy, co-morbidities, life expectancy, individual preferences and other geriatric syndromes, should be considered when performing a medication review as part of shared decision-making approach [157].
Successful implementation of deprescribing interventions to reduce risk of falls in older adults is supported by education of the older adult, family members and health care professionals, and ongoing monitoring and documentation [76, 158].
Shared decision-making results in better-informed older adults who tend to opt for deprescribing more often. Furthermore, shared decision-making improves compliance.
Cardiovascular interventions
Strong recommendation. Management of orthostatic hypotension should be included as a component of a multidomain intervention (Appendix 2, available in Age and Ageing online). GRADE: 1A.
Strong recommendation. Interventions for cardiovascular disorders identified during assessment for risk of falls should be the same as that for similar conditions when associated with syncope, in addition to other interventions based on the multifactorial falls risk assessment. GRADE 1B.
Recommendation details and justification
Whereas many multidomain fall prevention programmes have included strategies to treat orthostatic hypotension, including modification of possible culprit medications, rehydration, compression garments and medications (e.g. fludrocortisone and midodrine), there are no single intervention studies for orthostatic hypotension in falls prevention. In older adults with hypertension, symptoms may be ameliorated by the judicious use of antihypertensive medications titrated very slowly and with careful monitoring after changing the dose.
For the management of syncope, we advise following local syncope guidelines (e.g. European Cardiac Society Task force on Syncope [94]). Many multifactorial fall prevention programmes that have shown benefit for fall prevention have included strategies to modify orthostatic blood pressure.
The presence of more than one cardiovascular risk factor for falls is not uncommon. Clear causality for a single risk factor may be difficult to establish; therefore, all modifiable cardiovascular risk factors should be treated.
Interventions for bradycardic disorders (sinus node disease, atrioventricular conduction disorders, vasovagal syndrome and carotid sinus syndrome) and tachyarrhythmias (atrial fibrillation, supraventricular and ventricular tachycardia) include modification of culprit medications, specific anti-arrhythmic medication and, in some cases, implantable devices (such as pacemakers and implantable cardioverter-defibrillators) and are as per local syncope guidelines.
Telehealth and technology interventions
Expert recommendation. Use telehealth and/or smart home systems (when available) in combination with exercise training as part of falls prevention programmes in the community (Appendix 2, available in Age and Ageing online). GRADE: E.
Conditional recommendation. Current evidence does not support the use of wearables for falls prevention. However, emerging evidence show that when wearables are used in exercise programs to prevent falls, they may increase participation. GRADE: 2C.
Recommendation details and justification
There is emerging evidence in research settings that using wearable technology, i.e. devices worn on the body, to detect and prevent falls, could be efficacious for detection and prevention [159–171].
A recent systematic review and meta-analysis [172] that included 31 studies and a total of 2,500 older adults from 17 countries found that tele-health (telephone-based education) combined with exercise training were able to reduce fall risk by 16%. Notably, despite not being statistically significant, telehealth alone showed a point fall risk reduction of 20% in this meta-analysis [172].
A recent study showed [173] that for participants from the community who followed an exercise programme that included aerobic exercise or resistance training, those participants using a wearable device for physical activity monitoring had fewer falls compared with those not using the wearable device, suggesting better intervention adherence.
For optimal use of resources, it is advised to withhold this recommendation for LMIC until evidence on effectiveness and implementation of technology in LMIC settings become available.
Environmental interventions
Strong recommendation. Recommendations for modifications of an older adult’s physical home environment for fall hazards that consider their capacities and behaviours in this context should be provided by a trained clinician, as part of a multidomain falls prevention intervention. GRADE: 1B.
Recommendation details and justification
Interventions to reduce fall-hazards in and about the home can reduce the rate of falls and the number experiencing a fall [124, 127].
The greatest reductions are seen when the intervention is delivered to those at highest risk of falling [77, 124, 127, 174, 175].
Environmental assessment should be offered to older adults assessed as at high falls risk, such as older persons with a history of falling in the past year and an impairment in daily living activity or recently hospitalised from a fall, and those with severe vision impairment [77, 124, 127].
Evidence from randomised trials also provides evidence that the intervention is more effective when the aim of the visit, the assessment process and the intervention are highly tailored to falls, the outcome of interest. It is also more likely effective when delivered by an occupational therapist [124, 127].
Criteria for a quality home-fall hazard intervention include the use of a problem-solving approach involving the participant in identifying hazards and prioritising action, education relevant to falls, function and hazards; an action plan for removing or changing hazards and modifying risky behaviours; and adequate follow-up and support for adaptations and modifications [124, 125].
Vestibular interventions
Expert recommendation Managing vestibular issues should be considerd as part of multifactorial approach. GRADE: E
Recommedation details and justification
Particle repositioning (Epley) manoeuvres are an effective treatment for benign paroxysmal position and vertigo [176] and may reduce falls rates [177, 178], but evidence is limited. Vestibular rehabilitation therapy improves postural and gait stability in cases of vestibular dysfunction [179] although the optimal approach is still unclear as is the effect on falls rates.
As the risks of harm are low and improvements in health-related quality of life are potentially high, therapeutic interventions should always be sought where vestibular benign paroxysmal position and vertigo or vestibular dysfunction is identified. These treatments require trained staff but are low-cost and could be potentially applied in low resource settings.
Pain interventions
Expert recommendation. Adequate pain treatment should be considered as part of the multidomain approach. GRADE: E.
Recommendation details and justification
Adequate pain relief is likely to reduce the risk of falling while physically active. A personalised approach considering both non-pharmacological and pharmacological options is necessary to minimise risk of adverse events [180, 181]. Non-pharmacological approaches include physiotherapy and cognitive behavioural therapy.
Some analgesics, and in particular opioids, increase fall risk [182]. The mechanisms of fall risk associated with opioids in older adults include sedation, orthostatic hypotension and hyponatremia. Therefore, while the STOPP/START criteria suggest use of opioids for severe pain or when paracetamol and NSAIDs are ineffective [6], these potential adverse effects need to be anticipated, identified and managed. Weak opioids are preferably avoided, as the adverse events risk may outweigh the benefit. For neuropathic pain, first line treatment includes serotonin norepinephrine reuptake inhibitors, gabapentinoids and transdermal lidocaine or capsaicin [183]. For all analgesics, it is advisable to start slow, go slow and monitor efficacy and adverse effects. For general deprescribing recommendations, we refer to WG2 recommendations.
Concerns about falling and falls interventions
Strong recommendation. We recommend exercise, cognitive behavioural therapy and/or occupational therapy (as part of a multidisciplinary approach) to reduce concerns about falling in community-dwelling older adults (Appendix 2, available in Age and Ageing online). GRADE: 1B.
Recommendation details and justification
Different types of interventions can be effective in reducing concerns about falling, such as exercise interventions [184–186], cognitive behavioural therapy [187, 188] and occupational therapy [189], with small to moderate effect sizes. Two recent systematic reviews highlighted that supervised holistic exercise interventions in community settings, such as Pilates or yoga, had the largest effect sizes in reducing concerns about falling compared with other interventions [185, 186].
Existing fall prevention strategies, i.e. exercise interventions, can reduce concerns about falling in older adults.
Cognitive behavioural therapy and occupational therapy interventions can also reduce concerns about falling and should be considered as part of a multidomain fall prevention approach when available.
Vision interventions
Expert recommendation. Management of impaired vision should be considered as part of the multifactorial approach. GRADE: E.
Recommendation details and justification
Evidence from randomised controlled trials and prospective studies indicates cataract surgery for the first eye, [190] and both eyes [191] and achieving optimal safe functional vision by active older adults avoiding the wearing of multifocal glasses when outside [192] are effective fall prevention strategies.
Occupational therapy interventions involving home hazard reductions are also effective in preventing falls in older adults with severe visual impairments [193].
Although interventions involving vision assessment and provision of new spectacles undoubtedly improve performance in visual tests in community-dwelling older adults, such interventions have not yet been shown to reduce the risk of falls [194]. In fact, it is recommended that optometrists counsel their clients about likely short-term increased fall risk when dispensing new prescription glasses.
Vitamin D interventions
If older adults are considered at risk of deficiency, daily vitamin D supplementation should be recommended in accordance with national nutrition guidelines, but current evidence does not support universal vitamin D supplementation for preventing falls.
Vitamin D supplementation of ≥1,000 IU daily did not reduce falls in older community dwelling adults who achieved mean 25 (OH) vitamin D levels of ≥30 ng/ml versus those with levels <30 ng/ml. [195]. The key is to target its use in a manner that will confer benefit. Many studies on vitamin D supplementation and outcomes lack information on 25 (OH) vitamin D levels, thereby limiting definitive conclusions about the actual benefit of vitamin D supplementation.
Very frail individuals and those living in care homes are more likely to be frankly vitamin D deficient, and these are the individuals in whom supplementation is most likely to yield benefits. There is evidence that vitamin D can prevent falls in residential care, probably because levels are very low among residents [78].
Recent evidence from the VITAL trial shows that 2,000 or 4,000 IU daily is not harmful [196]. For older adults at increased risk for vitamin D deficiency, it is still reasonable to take 800–1,000 IU vitamin D per day, following established international recommendations [197–199].
Falls in hospitals
Risk stratification and assessment
Conditional recommendation. Perform a multifactorial falls risk assessment in all hospitalised older adults >65 years of age. We recommend against using scored falls risk screening tools in hospitals for multifactorial falls risk assessment in older adults (Appendix 2, available in Age and Ageing online). GRADE: 2B.
Strong recommendation. We recommend using the FES-I or especially the Short FES-I for assessing concerns about falling in acute care hospitals. GRADE: 1B.
Expert recommendation. We recommend conducting a post-fall assessment in hospitalised older adults following a fall in order to identify the mechanism of the fall, any resulting injuries, any precipitating factors (such as new intercurrent illness, complications or delirium), to reassess the individual's fall risk factors, and adjust the intervention strategy accordingly. GRADE: E.
Recommendation details and justification
Falls risk screening tools and multifactorial falls risk assessments are sometimes used interchangeably, but there are substantial differences. There is a case for dis-investing from fall risk screening tool scoring in the hospital setting as it does not reduce falls and takes valuable time. Falls risk assessment is a more detailed process used to identify underlying risk factors and inform the development of a care plan to reduce falls and injuries. Falls risk assessments should be reviewed if there is a change in a individual condition or if the older adult falls.
A stepped-wedge, cluster-RCT investigating the impact of removing a falls risk screening tool from an overall falls risk assessment programme found no impact on the falls rate [200].
Admission with a fall is defined as a severe fall incident in accordance with the risk stratification section and algorithm. Thus, older adults admitted with a fall are considered at high risk of a recurrent fall. Therefore, besides injury treatment, they should have the mechanism of the fall defined, and a multifactorial falls risk assessment. For details on the risk stratification and the multifactorial falls risk assessment, we refer to the respective sections.
Management and interventions
Strong recommendation. A tailored education on falls prevention should be delivered to all hospitalised older adults (≥65 years of age) and other high-risk groups (Appendix 2, available in Age and Ageing online). GRADE: 1A.
Strong recommendation. Personalised single or multidomain falls prevention strategies based on identified risk factors, behaviours or situations should be implemented for all hospitalised older adults (≥65 years of age), or younger individuals identified by health professionals as at risk of falls. GRADE: 1C (Acute care), GRADE: 1B (Sub-acute care).
Recommendation details and justification
A Cochrane review of 24 RCTs found that a multifactorial falls risk assessment, followed by implementation of multidomain interventions, may reduce the rate of falls in hospitals, but the very low-quality evidence precluded a definite conclusion. Reduction in falls rates was judged to be more likely in rehabilitation or geriatric ward settings [78].
The individual’s cognitive status (i.e. delirium or dementia) should be considered when implementing the education programmes. Use of several education modes (e.g. face-to-face discussions, handouts, videotapes) should be considered [201].
There is currently no robust research evidence to recommend the use of (i) bed/chair alarms, (ii) grip socks/non-slip socks for the purpose of falls prevention and (iii) the use of physical restraints when the sole purpose is falls prevention in hospitals.
We recommend that all hospitals should have protocols, policies and/or procedures for the prevention of falls consistent with best practice guidelines [202–205].
Falls in care homes
Risk stratification and assessment
Strong recommendation. Do not perform falls risk screening to identify care home residents at risk for falls as all residents should be considered at high risk of falls (Appendix 2, available in Age and Ageing online). GRADE: 1A.
Strong recommendation. Perform a comprehensive multifactorial assessment at admission to identify factors contributing to fall risk and implement appropriate interventions to avoid falls and fall-related injuries in care home older adults. GRADE: 1C.
Expert recommendation. We recommend conducting a post-fall assessment in care home residents following a fall in order to identify the mechanism of the fall, any resulting injuries, to reassess the resident's fall risk factors, adjust the intervention strategy for the resident and avoid unnecessary transfer to hospital. GRADE: E.
Strong recommendation. We recommend using the FES-I or especially the Short FES-I for assessing concerns about falling in long-term care facilities. GRADE: 1B.
Recommendation details and justification
All care home residents have a high risk of falling and may benefit from a multifactorial falls risk assessment and tailored intervention strategy.
A multifactorial falls risk assessment at admission should include identifying falls risk factors and be repeated at least once annually or when the resident's condition changes, based on resource availability in each setting.
Management and interventions
Strong recommendation. Take a multifaceted approach to falls reduction for care home residents including care home staff training, systematic use of a multidomain decision support tool and implementation of falls prevention actions (Appendix 2, available in Age and Ageing online). GRADE: 1B.
Strong recommendation. Do not use of physical restraints as a measure for falls prevention in care homes. GRADE: 1B.
Strong recommendation. Perform nutritional optimisation including food rich in calcium and proteins, as well as vitamin D supplementation as part of a multidomain intervention for falls prevention in care home residents. GRADE: 1B.
Strong recommendation. Include the promotion of exercise training (when feasible and safe) as part of a multidomain falls prevention intervention in care homes. GRADE: 1C.
Recommendation details and justification
The effectiveness of the multifaceted approach is based on one recent RCT [206]. The focus of implementation interventions should be on modifiable barriers and facilitators such as communication, knowledge and skills.
Examples of physical restraint devices that should be avoided for the purpose of falls prevention include lap belts, bed rails, Posey restraints or similar, chairs with tables attached, and chairs or mattresses that are difficult to get out of such as recliner chairs, water chairs, bean bags and curved edge mattresses [207, 208]. Use of some of these items may be justified for other well-defined purposes, subject to careful assessment and review and when agreed with the resident or their advocates.
Most residents in care homes are deficient in Vitamin D; therefore, we recommend vitamin D supplementation as part of a multidomain intervention for falls prevention in care home residents.
Individual supervised exercises in care homes as a prevention strategy are effective and should be offered in those who are willing and able to participate [138]. Programmes likely to be the most effective when individualised to residents’ functional abilities and preferences, incorporate a combination of exercises including balance and strength, as well as environmental modifications and staff training in falls prevention [209, 210].
Given the high level of disability in this group, where possible, an exercise specialist (physiotherapist, exercise physiologist) should be consulted to provide specialist, tailored advice on exercise and physical activity [209].
Specific clinical populations
Older adults with the clinical conditions included in this section may have specific falls risk factors and other attributes associated with their condition, in addition to the general risk factors found in the older population. Identifying these condition-associated factors may help n deciding on the most appropriate individually tailored intervention, by (i) suggesting a focus on a specific condition-related impairment or capacity, (ii) altering the likelihood of benefit from an effective intervention for the general older population, or (iii) changing the feasibility or acceptability of an intervention.
The recommendations in this section should be considered along with the general guidelines on multifactorial falls risk assessment and interventions.
Falls and PD and related disorders
Falls are very frequent in older adults with PD and related disorders. Current clinical practice guidelines do not address this population and their distinctive risks for falls and fall-related injuries and emerging strategies to reduce falls in this group are available but not yet represented in general guidelines (Appendix 2, available in Age and Ageing online).
Assessment
Conditional recommendation. Consider a falls risk assessment for older adults with PD, including a self-report 3-risk factor assessment tool, which includes a history of falls in the previous year, freezing of gait (FOG) in the past month, and slow gait speed. GRADE: 2B.
Recommendation details and justification
‘Freezing’ is an important falls risk factor in older adults with PD and can be targeted with specific interventions [211–216].
Both increases and decreases in falls rates have been observed in older adults with PD at a complex stage and/or cognitive impairment participating in exercise interventions [217, 218].
Frequent falls may occur at an early stage of Parkinson’s Plus syndromes and may merit specialist diagnostic assessment prior to considering a falls prevention intervention [219].
The self-report 3-risk factor assessment tool can be found at A Self-Reported Clinical Tool Predicts Falls in People with Parkinson's Disease.
Management and interventions
Conditional recommendation. Older adults with PD should be offered multidomain interventions, based on PD specific assessment and other identified falls risk factors. GRADE: 2B.
Strong recommendation. Older adults with PD at an early to mid-stage and with mild or no cognitive impairment should be offered individualised exercise programmes including balance and resistance training exercise. GRADE: 1A.
Strong recommendation. Consider offering exercise training, targeting balance and strength to people with complex phase PD if supervised by a physiotherapist or other suitably qualified professional. GRADE: 1C.
Recommendation details and justification
As a guide, a Movement Disorders Society Unified Parkinson’s Disease rating Scale (MDS-UPDRS) motor score ≥34 can be regarded as complex stage PD [220].
Supervision and modification of exercise interventions with PD individuals at a complex stage or with moderate or severe cognitive impairment requires specialist skills [221].
Falls prevention exercise interventions should be integrated in general mobility and ADL rehabilitation [221].
The effect of exercise on falls in older adults with PD that is more advanced (e.g. MDS-UPDRS motor score ≥ 34) and/or with substantial cognitive impairment is uncertain, but limited data indicate that minimally supervised exercise may increase the risk of falls [221].
A higher level of supervision is necessary in older adults with intermediate cognitive impairment, as such individuals may not be able to follow a self-directed programme, and for safety [221].
Specific subgroups of individuals (e.g. with FOG) may benefit from specifically targeted interventions (i.e. progressive balance and lower limb strengthening exercises) [212, 221].
Although preliminary evidence on the effectiveness of (pro-)cholinergic medications on falls is promising, the design, outcome assessment and size of clinical trials to date are inadequate to produce definitive evidence [221, 222].
Optimisation of medications to maximise motor function and minimise side effects (such as dyskinesia and hypotension) are critical first steps to falls prevention in PD treatment [221].
Stroke
Conditional recommendation. Older adults after a stroke should be offered participation in individualised exercise programmes aimed at improving balance/strength/walking to prevent falls. GRADE: 2C.
Recommendation details and justification
The recommendation is based on systematic review evidence of health benefits of exercise aimed at improving strength/balance/walking in this clinical group [138].
Falls prevention exercise should be integrated in more general mobility and ADL rehabilitation.
Higher supervision is warranted when there are more impairments following stroke.
Mild cognitive impairment and dementia
Strong recommendation. Community-dwelling older adults with cognitive impairment (mild cognitive impairment and mild to moderate dementia) should be offered an exercise programme to prevent falls. GRADE: 1B.
Recommendation details and justification
It has been shown that physical activity is feasible to perform by community-dwelling older adults with mild cognitive impairment or mild or moderate dementia [223–226].
Exercise interventions were found to be more effective to prevent falls in community dwelling older adults than in those living in residential care suggesting that these interventions may be more effective for individuals with relatively well-preserved abilities [223, 224].
Examples of effective stand-alone exercise interventions include balance training (e.g. Tai Chi) and multicomponent exercise (resistance + balance training) [227, 228].
Clinicians can promote better adherence to a care plan designed to reduce falls in older adults with cognitive impairment by involving caregivers of patients with cognitive impairment in (i) identifying and modifying environmental falls risk factors; (ii) modifying lifestyle in terms of diet/nutrition and exercise routines to reduce falls risks; (iii) detailed recording of falls incidents and (iv) determining what is prioritised and acceptable to the adult living with cognitive impairment, including attitudes to risks.
Hip fracture
Strong recommendation. Older adults after sustaining a hip fracture should be offered an individualised and progressive exercise programme aimed at improving mobility (i.e. standing up, balance, walking, climbing stairs) as a fall prevention strategy. GRADE: 1B.
Conditional recommendation. Such programmes for older adults after a hip fracture are best commenced in hospital (GRADE: 2C) and continued in the community (GRADE: 1A).
Recommendation details and justification
The strength of evidence for exercise in preventing falls in older adults after hip fracture is moderate [229]. This recommendation places a high value on preventing falls in this population with focus on mobility rehabilitation after hip fracture, including balance training and adequate pain control (see World Health Organisation guidelines). Furthermore, the minimal risk of harm contributes to the justification for a strong positive recommendation [230].
Falls in low- and middle- income countries
The majority of older adults alive today reside in a low- to middle- income country (LMIC). Correspondingly, as the population in LMIC ages at a rapid rate, the volume of research evidence emerging from these countries is now also increasing rapidly. Considering the heterogeneity of LMIC populations, as well as potential issues unique to these countries, this section specifically provides recommendations where LMIC may differ from higher income countries. The other recommendations in these guidelines apply to LMIC with the modifications and special considerations previously noted (Appendix 2, available in Age and Ageing online).
Strong recommendation. Local context needs to be considered when implementing fall prevention programmes in LMIC. GRADE: 1B
Recommendation details and justification
We advise that in LMIC, community dwelling adults aged 60 years and over should be screened opportunistically for fall risk during any clinical encounter, at least once a year, by enquiring about the presence of falls in the past 12 months.
Falls prevention should be included in LMIC policies using culturally sensitive strategies and tailored to local levels of expertise and resource availability.
Conditional recommendation. We conditionally recommend prioritising assessments of risk factors for cognitive impairment, obesity including sarcopenic obesity, diabetes, lack of appropriate footwear and environmental hazards as falls risk factors in LMIC. GRADE: 2C.
Recommendation details and justification
This recommendation highlights prominent risk factors for falls in LMIC which should be prioritised as part of the multifactorial falls risk assessment for falls.
The prevalence of obesity and diabetes is increasing rapidly in LMIC and these two conditions are more common in older adults. Available evidence from LMIC has linked obesity, particularly sarcopenic obesity, with falls, while diabetes emerges as a prominent risk factor in LMIC with high prevalence of diabetes [231–237].
Cognitive impairment is also rising in prevalence in LMIC with their rapidly ageing populations [238]. Multifactorial falls risk assessments in LMIC should include cognitive assessment using non-educationally and culturally biased tools that have been evaluated locally.
Footwear and environmental issues differ in LMIC, and hence, assessment and educational interventions should consider the cultural differences in footwear practices as well as in environmental safety [239].
Expert recommendation. Clinicians and caregivers in LMIC settings should preferably use validated tools that are freely available in their country of residence to assess mobility and fall risk. GRADE: E.
Recommendation details and justification
We recommend clinicians in LMIC begin with simple questions pertaining to fall history, followed by gait and balance assessments in individuals who screen positive to having had a fall in the past year.
Frailty, sarcopenia and falls
Falls are a common and important area of health care for older adults and relate closely, clinically and epidemiologically, to other common ‘geriatric syndromes.’ Here, we highlight sarcopenia and frailty for particular attention.
Frailty
Frailty is associated with an increased falls risk. Frailty is a state of increased vulnerability for developing dependency or mortality when exposed to a stressor. The prevalence for frailty is approximately 15% in the over 65 years of age group rises to more than 25% in those aged over 85 years, although the prevalence varies according to the definition and diagnostic methods used and the population studied [240]. A recent systematic review showed that frailty doubles the risk of recurrent falls while being pre-frail increases this risk by 30% [241]. Frailty has been associated with more injuries due to falls and hip fractures. As previously noted, our falls stratification algorithm includes frailty as marker of higher fall risk. A task force of the International Conference of Frailty and Sarcopenia has developed international clinical practice guidelines for the identification and management of physical frailty [240].
Further work is required to develop consensus on how to incorporate the frailty concept into management of older adults who fall and whether such an approach will reduce the risk of falls. Due to the association between frailty status and gait speed, the latter could potentially be considered a proxy of frailty [242].
Further studies are needed to assess the potential added value of using frailty as a proxy for intermediate to high fall risk and an entry point for personalised multifactorial falls risk assessment. From an implementation point of view, such an approach is promising as it would enable direct linkage to existing services and care pathways that opportunistically screen for frailty in the general older population.
Sarcopenia
Sarcopenia is a condition characterised by an age-associated loss of skeletal muscle mass and strength/function but also associated with low physical activity levels, other clinical conditions, and an increased risk of falls in older adults. The prevalence of sarcopenia and its association with falls varies according to the diagnostic definition used and the population studied. In the longitudinal iLSIRENTE study, the prevalence of sarcopenia was approximately 25% in people aged 80 years and above, and participants with sarcopenia were three times more likely to fall during a follow-up period of 2 years [243]. International clinical practice guidelines exist for the screening, diagnosis and management of sarcopenia [244, 245]. A growing number of clinicians and researchers advocate paying more attention to diagnosing and treating sarcopenia in older adults identified as being at a high risk of falls, although further research is required on how this should be conducted and whether applying non-exercise interventions for sarcopenia such as protein supplementation will reduce falls.
Delivery of these recommendation in the healthcare sector
Some of the recommendations provided in these guidelines explicitly apply only to certain countries (e.g. LMIC), care settings (e.g. hospitals or care homes) or populations (e.g. community-dwelling older adults).
In addition to considering the above, users of these guidelines should recognise that the ability to implement them successfully depends on the available resources and incentive structures, organisational culture and current processes of care delivery in a healthcare system, among other factors. Put simply, successful implementation requires a supportive organisational context, which should be assessed prior to implementing an organisational change addressing falls. Tools exist to help guideline implementers assess context (e.g. Consolidated Framework for Implementation Research) [246].
Context matters because many of the recommendations in these guidelines involve complex interventions.There are ‘multiple components or mechanisms of change’ and/or ‘how the intervention generates outcomes is dependent on exogenous factors, including the characteristics of recipients, and/or the context or system within which it is implemented’ [247]. For example, multifactorial programmes to prevent falls, by their nature, may involve multiple steps (screening, assessment and/or intervention) and multiple intervention components, which add complexity. In addition, many guideline recommendations will depend on the receptivity of various stakeholders to guideline implementation, because such recommendations might involve (i) reorganizing the delivery of healthcare services (e.g. setting up a robust process for referral of older adults from healthcare systems to community exercise programmes), which requires healthcare professional behaviour change; and (ii) asking for substantial behaviour change on the part of older adults (e.g. older adults’ willingness to exercise regularly and indefinitely).
Implementing some recommendations may require resources beyond what is currently available, requiring substantial buy-in at all levels of the healthcare system, which may or may not be present in a particular setting. Identifying the barriers and potential facilitators for changes required for implementing the recommendations at individual, clinical setting and health system levels should be part of developing a successful implementation strategy. For these reasons, guidelines should be implemented thoughtfully and deliberately, after verification of a favourable context to begin implementation. The implementation process should use quality improvement approaches and rigorous process evaluations to iteratively refine and improve intervention delivery, through measurement of care processes as well as regular interaction and engagement with key stakeholders involved in the changes being made [248, 249]. Finally, while there are studies of the barriers and facilitators of guideline uptake, there are very few outcome evaluations of the population impact of guidelines on fall occurrence. This research question poses complex methodological challenges that should be given priority as part of future guideline development.
Dissemination and implementation support
Our results and recommendations are accessible through our website (www.worldfallsguidelines.com) that provides many links to suggested resources and toolkits to facilitate implementation in different scenarios with accompanying decision trees and tools. We also have linked information on ongoing initiatives with regard to knowledge dissemination, implementation and evidence building. This includes links to advice and information produced by WHO and other international agencies, and eventually documents and tools to support implementation of these guidelines that will be developed in collaboration with older adults with lived fall experience. Our initiative does not conclude with these guidelines, which we plan to update regularly.
Limitations and concluding remarks
Our ambitious attempt at creating clinical practice guidelines for falls prevention and management based on an international consensus of experts and other stakeholders is not free of limitations. Although our team of experts from all relevant disciplines has a significant worldwide representation, one continent, Africa, is underrepresented. The input from older adults with lived experience on our process and recommendations was composed of English speaking older adults residing in high-income nations. We need to obtain more diverse feedback on our work.
Although we aimed for our recommendations and accompanying algorithm to be pragmatic and easy to apply and adaptable to older persons’ needs in different scenarios, no formal testing and validation of it was performed. Finally, we have tried to address areas where remaining knowledge gaps were detected, including e-technology, but evidence was still too scarce to provide strong recommendations. Several key areas for future research, where evidence is promising but inconclusive, were identified in each WG’s full report (Appendix 2, available in Age and Ageing online).
We believe that our guidelines will help clinicians around the world choose for their setting and resource availability effective approaches for the assessment and management of fall risk in older adults.
Supplementary Material
Acknowledgements
We would like to thank and acknowledge our central organisation support team composed by Dr Frederico Faria, Dr Yanina Sarquis-Adamson, Surim Son, Nattasha Clements and Jackie Liu. Also, we would like to thank and acknowledge Maureen Godfrey for offering her insights as an older adult with lived experience on our protocol paper, our panel of older adults (Clarke Heidrick, Elizabeth Retzer, Walter Retzer and Gerry Treble) for commenting and advising on the recommendations that were developed, and all other adults who supported the work of the individual working groups.
Contributor Information
Manuel Montero-Odasso, Gait and Brain Lab, Parkwood Institute, Lawson Health Research Institute, London, ON, Canada; Division of Geriatric Medicine, Department of Medicine, Schulich School of Medicine & Dentistry, University of Western Ontario, London, ON, Canada; Department of Epidemiology and Biostatistics, Schulich School of Medicine & Dentistry, University of Western Ontario, London, ON, Canada.
Nathalie van der Velde, Amsterdam UMC location University of Amsterdam, Internal Medicine, Section of Geriatric Medicine, Amsterdam, The Netherlands; Amsterdam Public Health, Aging and Later Life, Amsterdam, The Netherlands.
Finbarr C Martin, Population Health Sciences, Faculty of Life Sciences and Medicine, King's College London, London, UK.
Mirko Petrovic, Department of Internal Medicine and Paediatrics, Section of Geriatrics, Faculty of Medicine and Health Sciences, Ghent University, Ghent, Belgium.
Maw Pin Tan, Centre for Innovation in Medical Engineering (CIME), Faculty of Engineering, University of Malaya, Kuala Lumpur 50603, Malaysia; Department of Medicine, Faculty of Medicine, University of Malaya, Kuala Lumpur 50603, Malaysia.
Jesper Ryg, Department of Geriatric Medicine, Odense University Hospital, Odense, Denmark; Geriatric Research Unit, Department of Clinical Research, University of Southern Denmark, Odense, Denmark.
Sara Aguilar-Navarro, Department of Geriatric Medicine, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Mexico.
Neil B Alexander, Department of Internal Medicine, Division of Geriatric and Palliative Medicine, University of Michigan; Veterans Administration Ann Arbor Healthcare System Geriatrics Research Education Clinical Center, Ann Arbor, MI, USA.
Clemens Becker, Department of Clinical Gerontology and Geriatric Rehabilitation, Robert Bosch Hospital, Stuttgart, Germany.
Hubert Blain, Department of Geriatrics, Montpellier University hospital and MUSE, Montpellier, France.
Robbie Bourke, Department of Medical Gerontology Trinity College Dublin and Mercers Institute for Successful Ageing, St James’s Hospital, Dublin, Ireland.
Ian D Cameron, John Walsh Centre for Rehabilitation Research, Northern Sydney Local Health District and Faculty of Medicine and Health, University of Sydney. Department of Medicine (Neurology) and Neuroscience and Mental Health, Sydney, NSW, Australia.
Richard Camicioli, Department of Medicine (Neurology), Neuroscience and Mental Health Institute, University of Alberta, Edmonton, AB, Canada.
Lindy Clemson, Sydney School of Health Sciences, Faculty of Medicine & Health, The University of Sydney, Sydney, Australia.
Jacqueline Close, Falls, Balance and Injury Research Centre, Neuroscience Research Australia, University of New South Wales, Sydney, NSW, Australia; Prince of Wales Clinical School, Medicine, University of New South Wales, Sydney, NSW, Australia.
Kim Delbaere, Falls, Balance and Injury Research Centre, Neuroscience Research Australia, Sydney, NSW, Australia; School of Population Health, University of New South Wales, Kensington, NSW, Australia.
Leilei Duan, National Centre for Chronic and Noncommunicable Disease Control and Prevention, Chinese Centre for Disease Control and Prevention, Beijing, China.
Gustavo Duque, Research Institute of the McGill University HealthCentre, Montreal, Quebec, Canada.
Suzanne M Dyer, Flinders Health and Medical Research Institute, Flinders University, Adelaide, SA, Australia.
Ellen Freiberger, Friedrich-Alexander-University Erlangen-Nürnberg, Institute for Biomedicine of Aging, Nürnberg, Germany.
David A Ganz, Multicampus Program in Geriatric Medicine and Gerontology, David Geffen School of Medicine at UCLA and Veterans Affairs Greater Los Angeles Healthcare System, Los Angeles, CA, USA.
Fernando Gómez, Research Group on Geriatrics and Gerontology, International Association of Gerontology and Geriatrics Collaborative Center, University Caldas, Manizales, Colombia.
Jeffrey M Hausdorff, Center for the Study of Movement, Cognition and Mobility, Neurological Institute, Tel Aviv Sourasky Medical Center, Tel Aviv, Israel; Department of Physical Therapy, Sackler Faculty of Medicine, and Sagol School of Neuroscience, Tel Aviv University, Tel Aviv, Israel; Department of Orthopaedic Surgery, Rush Alzheimer's Disease Center, Rush University Medical Center, Chicago, IL, USA.
David B Hogan, Brenda Strafford Centre on Aging, O’BrienInstitute for Public Health, Cumming School of Medicine, University of Calgary, Calgary, AB, Canada.
Susan M W Hunter, School of Physical Therapy, Faculty of Health Sciences, Elborn College, University of Western Ontario, London, ON, Canada.
Jose R Jauregui, Ageing Biology Unit, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina.
Nellie Kamkar, Gait and Brain Lab, Parkwood Institute, Lawson Health Research Institute, London, ON, Canada.
Rose-Anne Kenny, Department of Medical Gerontology Trinity College Dublin and Mercers Institute for Successful Ageing, St James’s Hospital, Dublin, Ireland.
Sarah E Lamb, Faculty of Health and Life Sciences, Mireille Gillings Professor of Health Innovation, Medical School Building, Exeter, England, UK.
Nancy K Latham, Brigham and Women's Hospital, Boston, MA, USA.
Lewis A Lipsitz, Hinda and Arthur Marcus Institute for Aging Research, Hebrew SeniorLife, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA.
Teresa Liu-Ambrose, Djavad Mowafaghian Centre for Brain Health, Center for Hip Health and Mobility, Vancouver Coastal Health Research Institute, University of British Columbia, Vancouver, BC, Canada.
Pip Logan, School of Medicine, University of Nottingham, Nottingham, England, UK.
Stephen R Lord, Falls, Balance and Injury Research Centre, Neuroscience Research Australia, Sydney, NSW, Australia; School of Public Health and Community Medicine, University of New South Wales, Sydney, NSW, Australia.
Louise Mallet, Department of Pharmacy, Faculty of Pharmacy, McGill University Health Center, Université de Montréal, Montreal, QC, Canada.
David Marsh, University College London, London, England, UK.
Koen Milisen, Department of Public Health and Primary Care, Academic Centre for Nursing and Midwifery, KU Leuven, Leuven, Belgium; Department of Geriatric Medicine, University Hospitals Leuven, Leuven, Belgium.
Rogelio Moctezuma-Gallegos, Geriatric Medicine & Neurology Fellowship, Instituto Nacional de Ciencias Médicas y Nutrición “Salvador Zubirán”. Mexico City, Mexico; Geriatric Medicine Program, Tecnologico de Monterrey, School of Medicine and Health Sciences. Monterrey, Nuevo León, Mexico.
Meg E Morris, Healthscope and Academic and Research Collaborative in Health (ARCH), La Trobe University, Australia.
Alice Nieuwboer, Department of Rehabilitation Sciences, Neurorehabilitation Research Group (eNRGy), KU Leuven, Leuven, Belgium.
Monica R Perracini, Master’s and Doctoral programs in Physical Therapy, Universidade Cidade de Sao Paulo (UNICID), Sao Paulo, Brazil.
Frederico Pieruccini-Faria, Gait and Brain Lab, Parkwood Institute, Lawson Health Research Institute, London, ON, Canada; Division of Geriatric Medicine, Department of Medicine, Schulich School of Medicine & Dentistry, University of Western Ontario, London, ON, Canada.
Alison Pighills, Mackay Institute of Research and Innovation, Mackay Hospital and Health Service, Mackay, QLD, Australia.
Catherine Said, Western Health, University of Melbourne, Parkville, Melbourne, VIC, Australia; Australian Institute for Musculoskeletal Science (AIMSS), The University of Melbourne and Western Health, St Albans, VIC, Australia; Melbourne School of Health Sciences The University of Melbourne, Parkville, Australia.
Ervin Sejdic, Department of Electrical and Computer Engineering, Swanson School of Engineering, University of Pittsburgh, Pittsburgh, PA, USA.
Catherine Sherrington, Institute for Musculoskeletal Health, The University of Sydney and Sydney Local Health District, Sydney, Australia.
Dawn A Skelton, School of Health and Life Sciences, Research Centre for Health (ReaCH), Glasgow Caledonian University, Cowcaddens Road, Glasgow, Scotland, UK.
Sabestina Dsouza, Department of Occupational Therapy, Manipal College of Health Professions, Manipal Academy of Higher Education, Manipal, Karnataka, India.
Mark Speechley, Department of Epidemiology and Biostatistics, Schulich School of Medicine & Dentistry, University of Western Ontario, London, ON, Canada; Schulich Interfaculty Program in Public Health, Schulich School of Medicine & Dentistry, University of Western Ontario, London, ON, Canada.
Susan Stark, Program in Occupational Therapy, School of Medicine, Washington University in St. Louis, St. Louis, MO, USA.
Chris Todd, School of Health Sciences, Faculty of Biology, Medicine and Health, The University of Manchester, Manchester, England, UK; Manchester University NHS Foundation Trust, Manchester M13 9WL, UK.
Bruce R Troen, Division of Geriatrics and Palliative Medicine, Department of Medicine, Jacobs School of Medicine & Biomedical Sciences, University of Buffalo; Research Service, Veterans Affairs Western New York Healthcare System, Buffalo, New York, USA.
Tischa van der Cammen, Department of Human-Centred Design, Faculty of Industrial Design Engineering, Delft University of Technology, Delft, The Netherlands; Section of Geriatric Medicine, Department of Internal Medicine, Erasmus University Medical Center, Rotterdam, The Netherlands.
Joe Verghese, Division of Geriatrics, Department of Medicine, Albert Einstein College of Medicine, Bronx, New York, USA; Department of Neurology, Albert Einstein College of Medicine, Bronx, NY, USA.
Ellen Vlaeyen, Department of Public Health and Primary Care, Academic Centre for Nursing and Midwifery, KU Leuven, Leuven, Belgium; Faculty of Medicine and Life Sciences, Hasselt University, Hasselt, Belgium.
Jennifer A Watt, Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, ON, Canada; Department of Medicine, University of Toronto, Toronto, ON, Canada.
Tahir Masud, Department of Geriatric Medicine, The British Geriatrics Society, Nottingham University Hospitals NHS Trust, Nottingham, England, UK .
the Task Force on Global Guidelines for Falls in Older Adults:
Devinder Kaur Ajit Singh, Sara G Aguilar-Navarro, Edgar Aguilera Caona, Neil B Alexander, Natalie Allen, Cedric Anweiller, Alberto Avila-Funes, Renato Barbosa Santos, Frances Batchelor, Clemens Becker, Marla Beauchamp, Canan Birimoglu, Hubert Blain, Kayla Bohlke, Robert Bourke, Christina Alonzo Bouzòn, Stephanie Bridenbaugh, Patricio Gabriel Buendia, Ian Cameron, Richard Camicioli, Colleen Canning, Carlos Alberto Cano-Gutierrez, Juan Carlos Carbajal, Daniela Cristina Carvalho de Abreu, Alvaro Casas-Herrero, Alejandro Ceriani, Matteo Cesari, Lorenzo Chiari, Lindy Clemson, Jacqueline Close, Luis Manuel Cornejo Alemǻn, Rik Dawson, Kim Delbaere, Paul Doody, Sabestina Dsouza, Leilei Duan, Gustavo Duque, Suzanne Dyer, Toby Ellmers, Nicola Fairhall, Luigi Ferrucci, Ellen Freiberger, James Frith, Homero Gac Espinola, David A Ganz, Fabiana Giber, José Fernando Gómez, Luis Miguel Gutiérrez-Robledo, Sirpa Hartikainen, Jeffrey Hausdorff, David B Hogan, Chek Hooi Wong, Simon Howe, Susan Hunter, Javier Perez Jara, Ricardo Jauregui, Anton Jellema, Suen Jenni, Ditte Jepson, Sebastiana Kalula, Nellie Kamkar, Devinder Kaur Ajit Singh, Rose Anne Kenny, Ngaire Kerse, Olive Kobusingye, Reto Kressig, Wing Kwok, Sallie Lamb, Nancy Latham, Mei Ling Lim, Lewis Lipsitz, Teresa Liu-Ambrose, Pip Logan, Stephen Lord, Roberto Alves Lourenço, Kenneth Madden, Louise Mallet, Pedro Marín-Larraín, David R Marsh, Finbarr C Martin, Diego Martínez Padilla, Tahir Masud, Sumaiyah Mat, Lisa McGarrigle, Bill McIlroy, Felipe Melgar-Cuellar, Jasmine Menant, Koen Milisen, Alberto Mimenza, Rogelio Moctezuma-Gallegos, Manuel Montero-Odasso, Meg E Morris, Irfan Muneeb, Hossein Negahban, Alice Nieuwboer, Mireille Norris, Giulia Ogliari, Juliana Oliveira, José F Parodi, Sergio Perez, Monica Perracini, Mirko Petrovic, José Ernesto Picado Ovares, Frederico Pieruccini-Faria, Alison Pighills, Marina Pinheiro, Eveline Poelgeest, Xinia Ramirez Ulate, Katie Robinson, Jesper Ryg, Cathy Said, Ryota Sakurai, Marcelo Schapira, Ervin Sejdic, Lotta J Seppala, Aldo Sgaravatti, Cathie Sherrington, Dawn Skelton, Yu Song, Mark Speechley, Susan Stark, Munira Sultana, Anisha Suri, Maw Pin Tan, Morag Taylor, Katja Thomsen, Anne Tiedemann, Susana Lucia Tito, Chris Todd, Bruce Troen, Tischa Van der Cammen, Nathalie Van der Velde, Joe Verghese, Ellen Vlaeyen, Jennifer Watt, Ana-Karim Welmer, Chang Won Won, and G A Rixt Zijlstra
Declaration of Conflicts of Interest
The corresponding author declares on behalf of the group of authors that many of the co-authors receive funding and grants but that none pose a substantive conflict to this published work.
Declaration of Sources of Funding
The WFGs initiative is partially funded by a research grant from the St. Joseph Foundation, London, Ontario, Canada (grant no. 74531) and by a CIHR Planning and Dissemination Grant from the Institute of Ageing (RN476173-478689) obtained to fund the Delphi process and voting, website development, workshops, and production and publication of this guideline.
References
- 1. Bernard I. The Challenge of Geriatric Medicine. Oxford: Oxford University Press, 1992. [Google Scholar]
- 2. Ganz DA, Latham NK. Prevention of falls in community-dwelling older adults. N Engl J Med 2020; 382: 734–43. [DOI] [PubMed] [Google Scholar]
- 3. James SL, Lucchesi LR, Bisignano C et al. The global burden of falls: global, regional and national estimates of morbidity and mortality from the global burden of disease study 2017. Inj Prev 2020; 26: i3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kwan MM, Close JC, Wong AK, Lord SR. Falls incidence, risk factors, and consequences in Chinese older people: a systematic review. J Am Geriatr Soc 2011; 59: 536–43. [DOI] [PubMed] [Google Scholar]
- 5. Haagsma JA, Olij BF, Majdan M et al. Falls in older aged adults in 22 European countries: incidence, mortality and burden of disease from 1990 to 2017. Inj Prev 2020; 26: i67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. O'Mahony D, O'Sullivan D, Byrne S, O'Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 2015; 44: 213–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Montero-Odasso MM, Kamkar N, Pieruccini-Faria F et al. Evaluation of clinical practice guidelines on fall prevention and management for older adults: a systematic review. JAMA Netw Open 2021; 4: e2138911. 10.1001/jamanet-workopen.2021.38911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. National Instiute for Health and Care Excellence (NICE) . 2019 Surveillance of Falls in Older People: Assessing Risk and Prevention (NICE Guideline CG161). London: National Instiute for Health and Care Excellence, 2019. [PubMed] [Google Scholar]
- 9. Reyes-Ortiz CA, Al Snih S, Markides KS. Falls among elderly persons in Latin America and the Caribbean and among elderly Mexican-Americans. Rev Panam Salud Publica 2005; 17: 362–9. [DOI] [PubMed] [Google Scholar]
- 10. Lipsitz LA, Nakajima I, Gagnon M et al. Muscle strength and fall rates among residents of Japanese and American nursing homes: an International Cross-Cultural Study. J Am Geriatr Soc 1994; 42: 953–9. [DOI] [PubMed] [Google Scholar]
- 11. Lusardi MM, Fritz S, Middleton A et al. Determining risk of falls in community dwelling older adults: a systematic review and meta-analysis using posttest probability. J Geriatr Phys Ther 2017; 40: 1–36. 10.1519/JPT.0000000000000099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mirelman A, Herman T, Brozgol M et al. Executive function and falls in older adults: new findings from a five-year prospective study link fall risk to cognition. PLoS One 2012; 7: e40297. 10.1371/journal.pone.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Montero-Odasso M, Muir SW, Speechley M. Dual-task complexity affects gait in people with mild cognitive impairment: the interplay between gait variability, dual tasking, and risk of falls. Arch Phys Med Rehabil 2012; 93: 293–9. [DOI] [PubMed] [Google Scholar]
- 14. Fischer BL, Gleason CE, Gangnon RE, Janczewski J, Shea T, Mahoney JE. Declining cognition and falls: role of risky performance of everyday mobility activities. Phys Ther 2014; 94: 355–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Amboni M, Barone P, Hausdorff JM. Cognitive contributions to gait and falls: evidence and implications. Mov Disord 2013; 28: 1520–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Montero-Odasso M, Speechley M. Falls in cognitively impaired older adults: implications for risk assessment and prevention. J Am Geriatr Soc 2018; 66: 367–75. [DOI] [PubMed] [Google Scholar]
- 17. Robinovitch SN, Feldman F, Yang Y et al. Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study. Lancet 2013; 381: 47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pang I, Okubo Y, Sturnieks D, Lord SR, Brodie MA. Detection of near falls using wearable devices: a systematic review. J Geriatr Phys Ther 2019; 42: 48–56. [DOI] [PubMed] [Google Scholar]
- 19. Bhangu J, McMahon CG, Hall P et al. Long-term cardiac monitoring in older adults with unexplained falls and syncope. Heart 2016; 102: 681–6. [DOI] [PubMed] [Google Scholar]
- 20. Yardley L, Kirby S, Ben-Shlomo Y, Gilbert R, Whitehead S, Todd C. How likely are older people to take up different falls prevention activities? Prev Med 2008; 47: 554–8. [DOI] [PubMed] [Google Scholar]
- 21. Franco MR, Howard K, Sherrington C et al. Eliciting older people's preferences for exercise programs: a best-worst scaling choice experiment. J Physiother 2015; 61: 34–41. [DOI] [PubMed] [Google Scholar]
- 22. Dorresteijn TA, Rixt Zijlstra GA, Van Eijs YJ, Vlaeyen JW, Kempen GI. Older people's preferences regarding programme formats for managing concerns about falls. Age Ageing 2012; 41: 474–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. World Health Organization . World Report on Ageing and Health. Geneva: World Health Organization, 2015. [Google Scholar]
- 24. World Health Organization . Step Safely: Strategies for Preventing and Managing Falls across the Life-Course. Geneva: World Health Organization, 2021. [Google Scholar]
- 25. Montero-Odasso M, van der Velde N, Alexander NB et al. New horizons in falls prevention and management for older adults: a global initiative. Age Ageing 2021; 50: 1499–507. [DOI] [PubMed] [Google Scholar]
- 26. International Osteoporosis Foundation . What Is Osteoporosis? Switzerland: International Osteoporosis Foundation. Available at https://www.osteoporosis.foundation (June 2022, date last accessed). [Google Scholar]
- 27. Fragility Fracture Network . FFN Clinical Toolkit and Policy Toolkit Resources. Fragility Fracture Network. Available at https://fragilityfracturenetwork.org/about-2/resources-centre/ (June 2022, date last accessed). [Google Scholar]
- 28. Fougere BMJ, Arai H, Bauer JM et al. Precision medicine: the future management of geriatric conditions. J Nutr Health Aging 2018. 10.1007/s12603-018-1045-1. [DOI] [PubMed] [Google Scholar]
- 29. Tricco AC, Antony J, Zarin W et al. A scoping review of rapid review methods. BMC Med 2015; 13: 224. 10.1186/s12916-015-0465-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Guyatt GH, Oxman AD, Vist GE et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008; 336: 924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Burns ER, Lee R, Hodge SE, Pineau VJ, Welch B, Zhu M. Validation and comparison of fall screening tools for predicting future falls among older adults. Arch Gerontol Geriatr 2022; 101: 104713. 10.1016/j.archger.2022.104713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA 2007; 297: 77–86. [DOI] [PubMed] [Google Scholar]
- 33. Meekes WM, Korevaar JC, Leemrijse CJ, van de Goor IA. Practical and validated tool to assess falls risk in the primary care setting: a systematic review. BMJ Open 2021; 11: e045431. 10.1136/bmjopen-2020-045431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Stevens JA, Ballesteros MF, Mack KA, Rudd RA, DeCaro E, Adler G. Gender differences in seeking care for falls in the aged Medicare population. Am J Prev Med 2012; 43: 59–62. [DOI] [PubMed] [Google Scholar]
- 35. Fleming J, Brayne C, the Cambridge City over-75s Cohort (CC75C) study collaboration . Inability to get up after falling, subsequent time on floor, and summoning help: prospective cohort study in people over 90. BMJ 2008; 337: a2227. 10.1136/bmj.a2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bisson EJ, Peterson EW, Finlayson M. Delayed initial recovery and long lie after a fall among middle-aged and older people with multiple sclerosis. Arch Phys Med Rehabil 2015; 96: 1499–505. [DOI] [PubMed] [Google Scholar]
- 37. Vellas BJ, Wayne SJ, Garry PJ, Baumgartner RN. A two-year longitudinal study of falls in 482 community-dwelling elderly adults. J Gerontol A Biol Sci Med Sci 1998; 53: M264–74. [DOI] [PubMed] [Google Scholar]
- 38. World Bank . Life Expectancy at Birth, Total (Years) | Data (Worldbank.Org). World Bank website, 2022.
- 39. Tiedemann A, Mikolaizak AS, Sherrington C, Segin K, Lord SR, Close JC. Older fallers attended to by an ambulance but not transported to hospital: a vulnerable population at high risk of future falls. Aust N Z J Public Health 2013; 37: 179–85. [DOI] [PubMed] [Google Scholar]
- 40. Mikolaizak AS, Lord SR, Tiedemann A et al. A multidisciplinary intervention to prevent subsequent falls and health service use following fall-related paramedic care: a randomised controlled trial. Age Ageing 2017; 46: 200–7. [DOI] [PubMed] [Google Scholar]
- 41. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med 1988; 319: 1701–7. [DOI] [PubMed] [Google Scholar]
- 42. Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA 1989; 261: 2663–8. [PubMed] [Google Scholar]
- 43. Karlsson MK, Vonschewelov T, Karlsson C, Coster M, Rosengen BE. Prevention of falls in the elderly: a review. Scand J Public Health 2013; 41: 442–54. [DOI] [PubMed] [Google Scholar]
- 44. Stevens JA. The STEADI tool kit: a fall prevention resource for health care providers. IHS Prim Care Provid 2013; 39: 162–6. [PMC free article] [PubMed] [Google Scholar]
- 45. Centers for Disease Control and Prevention STEADI . Pocket Guide—Preventing Falls in Older Patients. Centers for Disease Control and Prevention, 2019. [Google Scholar]
- 46. Jepsen B, Robinson K, Ogliari G et al. Predicting falls in older adults: an umbrella review of instruments assessing fait, balance, and functional mobility. BMC Geriatr 2022; 22. 10.1186/s12877-022-03271-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Fried LP, Tangen CM, Walston J et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001; 56: M146–57. [DOI] [PubMed] [Google Scholar]
- 48. Rockwood K, Song X, MacKnight C et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005; 173: 489–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. British Geriatrics Society . Comprehensive Geriatric Assessment Toolkit for Primary Care Practioners. British Geriatrics Society, 2019. [Google Scholar]
- 50. Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc 2007; 55: 780–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sillner AY, Holle CL, Rudolph JL. The overlap between falls and delirium in hospitalized older adults: a systematic review. Clin Geriatr Med 2019; 35: 221–36. [DOI] [PubMed] [Google Scholar]
- 52. Nazarko L. Falls prevention in primary care. London J Prim Care (Abingdon) 2009; 2: 158–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ayton D, Morello R, Natora A, Yallop S, Barker A, Soh SE. Perceptions of falls and falls prevention interventions among personal alert Victoria clients. Health Soc Care Community 2018; 26: 970–8. [DOI] [PubMed] [Google Scholar]
- 54. Collins CE, Chandra A, Nguyen B et al. The rose-colored glasses of geriatric fall patients: inconsistencies between knowledge of risk factors for and actual causes of falls. Gerontol Geriatr Med 2020; 6: 233372142096788. 10.1177/2333721420967884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Delbaere K, Close JC, Brodaty H, Sachdev P, Lord SR. Determinants of disparities between perceived and physiological risk of falling among elderly people: cohort study. BMJ 2010; 341: c4165. 10.1136/bmj.c4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Jagnoor J, Keay L, Jaswal N, Kaur M, Ivers R. A qualitative study on the perceptions of preventing falls as a health priority among older people in northern India. Inj Prev 2014; 20: 29–34. [DOI] [PubMed] [Google Scholar]
- 57. Zecevic AA, Salmoni AW, Speechley M, Vandervoort AA. Defining a fall and reasons for falling: comparisons among the views of seniors, health care providers, and the research literature. Gerontologist 2006; 46: 367–76. [DOI] [PubMed] [Google Scholar]
- 58. Kwon S, Perera S, Pahor M et al. What is a meaningful change in physical performance? Findings from a clinical trial in older adults (the LIFE-P study). J Nutr Health Aging 2009; 13: 538–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Phys Ther 2000; 80: 896–903. [PubMed] [Google Scholar]
- 60. Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the ``get-up and go'' test. Arch Phys Med Rehabil 1986; 67: 387–9. [PubMed] [Google Scholar]
- 61. de Morton NA, Davidson M, Keating JL. The de Morton Mobility Index (DEMMI): an essential health index for an ageing world. Health Qual Life Outcomes 2008; 6: 63. 10.1186/1477-7525-6-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Berg KO, Wood-Dauphinee SL, Williams JI, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health 1992; 83: S7–11. [PubMed] [Google Scholar]
- 63. Bohannon R. Single limb stance times: a descriptive meta-analysis of data from individuals at least 60 years of age. Topics Geriatr Rehab 2006; 22: 70–7. [Google Scholar]
- 64. Weiner DK, Duncan PW, Chandler J, Studenski SA. Functional reach: a marker of physical frailty. J Am Geriatr Soc 1992; 40: 203–7. [DOI] [PubMed] [Google Scholar]
- 65. Bandinelli S, Pozzi M, Lauretani F et al. Adding challenge to performance-based tests of walking: the Walking InCHIANTI Toolkit (WIT). Am J Phys Med Rehabil 2006; 85: 986–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 1986; 34: 119–26. [DOI] [PubMed] [Google Scholar]
- 67. Horak FB, Wrisley DM, Frank J. The Balance Evaluation Systems Test (BESTest) to differentiate balance deficits. Phys Ther 2009; 89: 484–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Lord SR, Delbaere K, Gandevia SC. Use of a physiological profile to document motor impairment in ageing and in clinical groups. J Physiol 2016; 594: 4513–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Alexander NB. Gait disorders in older adults. J Am Geriatr Soc 1996; 44: 434–51. [DOI] [PubMed] [Google Scholar]
- 70. Lindemann U. Spatiotemporal gait analysis of older persons in clinical practice and research: which parameters are relevant? Z Gerontol Geriatr 2020; 53: 171–8. [DOI] [PubMed] [Google Scholar]
- 71. Ardali G, Brody LT, States RA, Godwin EM. Reliability and validity of the floor transfer test as a measure of readiness for independent living among older adults. J Geriatr Phys Ther 2019; 42: 136–47. [DOI] [PubMed] [Google Scholar]
- 72. Bergland A, Laake K. Concurrent and predictive validity of ``getting up from lying on the floor''. Aging Clin Exp Res 2005; 17: 181–5. [DOI] [PubMed] [Google Scholar]
- 73. de Vries M, Seppala LJ, Daams JG et al. Fall-risk-increasing drugs: a systematic review and meta-analysis: I. Cardiovascular drugs. J Am Med Dir Assoc 2018; 19: 371.e1–9. 10.1016/j.jamda.2017.12.013. [DOI] [PubMed] [Google Scholar]
- 74. Seppala LJ, van de Glind EMM, Daams JG et al. Fall-risk-increasing drugs: a systematic review and meta-analysis: III. Others. J Am Med Dir Assoc 2018; 19: 372.e1–8. 10.1016/j.jamda.2017.12.099. [DOI] [PubMed] [Google Scholar]
- 75. Seppala LJ, Wermelink A, de Vries M et al. Fall-risk-increasing drugs: a systematic review and meta-analysis: II. Psychotropics. J Am Med Dir Assoc 2018; 19: 371.e11–7. [DOI] [PubMed] [Google Scholar]
- 76. Seppala LJ, Petrovic M, Ryg J et al. STOPPFall (screening tool of older persons prescriptions in older adults with high fall risk): a Delphi study by the EuGMS task and finish group on fall-risk-increasing drugs. Age Ageing 2021; 50: 1189–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Gillespie LD, Robertson MC, Gillespie WJ et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012; 2021: CD007146. 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Cameron ID, Dyer SM, Panagoda CE et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev 2018; 9: CD005465. 10.1002/14651858.CD005465.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Dautzenberg L, Beglinger S, Tsokani S et al. Interventions for preventing falls and fall-related fractures in community-dwelling older adults: a systematic review and network meta-analysis. J Am Geriatr Soc 2021; 69: 2973–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Centeres for Disease Control and Prevention . STEADI—Older Adult Fall Prevention. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2020. Available at https://www.cdc.gov/steadi/steadi-rx.html (2022, date last accessed). [Google Scholar]
- 81. By the American Geriatrics Society Beers Criteria Update Expert P . American Geriatrics Society 2019 updated AGS beers criteria(R) for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2019; 67: 674–94. [DOI] [PubMed] [Google Scholar]
- 82. Pazan F, Wehling M. The FORTA (Fit fOR The Aged) app as a clinical tool to optimize complex medications in older people. J Am Med Dir Assoc 2017; 18: 893. 10.1016/j.jamda.2017.06.031. [DOI] [PubMed] [Google Scholar]
- 83. Johanna J. Meds75+. Fimea: Finnish Medicines Agency, 2020. Available at https://www.fimea.fi/web/en/databases_and_registeries/medicines_information/database_of_medication_for_older_persons. [Google Scholar]
- 84. Seppala LJ, Petrovic M, Ryg J et al. STOPPFall (screening tool of older persons prescriptions in older adults with high fall risk): a Delphi study by the EuGMS task and finish group on fall-risk-increasing drugs. Age Ageing 2020; 50: 189–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Muir SW, Gopaul K, Montero Odasso MM. The role of cognitive impairment in fall risk among older adults: a systematic review and meta-analysis. Age Ageing 2012; 41: 299–308. [DOI] [PubMed] [Google Scholar]
- 86. Montero-Odasso M, Almeida QJ, Bherer L et al. Consensus on shared measures of mobility and cognition: from the Canadian consortium on neurodegeneration in aging (CCNA). J Gerontol A Biol Sci Med Sci 2019; 74: 897–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. McGarrigle L, Yang Y, Lasrado R, Gittins M, Todd, C. A systematic review and meta-analysis of the psychometric properties of four variants of the falls efficacy scale-international (FES-I). Paper in preparation. 2022.
- 88. Adamczewska N, Nyman SR. A new approach to fear of falls from connections with the posttraumatic stress disorder literature. Gerontol Geriatr Med 2018; 4: 233372141879623. 10.1177/2333721418796238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Hughes CC, Kneebone II, Jones F, Brady B. A theoretical and empirical review of psychological factors associated with falls-related psychological concerns in community-dwelling old82er people. Int Psychogeriatr 2015; 27: 1071–87. [DOI] [PubMed] [Google Scholar]
- 90. Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005; 34: 614–9. [DOI] [PubMed] [Google Scholar]
- 91. Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol 1990; 45: P239–43. [DOI] [PubMed] [Google Scholar]
- 92. Davies AJ, Kenny RA. Falls presenting to the accident and emergency department: types of presentation and risk factor profile. Age Ageing 1996; 25: 362–6. [DOI] [PubMed] [Google Scholar]
- 93. Jansen S, Kenny RA, de Rooij SE, van der Velde N. Self-reported cardiovascular conditions are associated with falls and syncope in community-dwelling older adults. Age Ageing 2015; 44: 525–9. [DOI] [PubMed] [Google Scholar]
- 94. Brignole M, Moya A, de Lange FJ et al. 2018 ESC guidelines for the diagnosis and management of syncope. Eur Heart J 2018; 39: 1883–948. [DOI] [PubMed] [Google Scholar]
- 95. Parry SW, Kenny RA. Drop attacks in older adults: systematic assessment has a high diagnostic yield. J Am Geriatr Soc 2005; 53: 74–8. [DOI] [PubMed] [Google Scholar]
- 96. Cronin H, Kenny RA. Cardiac causes for falls and their treatment. Clin Geriatr Med 2010; 26: 539–67. [DOI] [PubMed] [Google Scholar]
- 97. Bourke R, Doody P, Perez S, Moloney D, Lipsitz LA, Kenny R. Cardiovascular abnormalities and falls among older adults: a systematic review for the task force on global guidelines for falls in older adults. Paper in preparation. 2022.
- 98. Heitterachi E, Lord SR, Meyerkort P, McCloskey I, Fitzpatrick R. Blood pressure changes on upright tilting predict falls in older people. Age Ageing 2002; 31: 181–6. [DOI] [PubMed] [Google Scholar]
- 99. Maggi R, Rafanelli M, Ceccofiglio A, Solari D, Brignole M, Ungar A. Additional diagnostic value of implantable loop recorder in patients with initial diagnosis of real or apparent transient loss of consciousness of uncertain origin [Europace 2014; 16: 1226-1230]. Europace 2015; 17: 1847. 10.1093/europace/euu308. [DOI] [PubMed] [Google Scholar]
- 100. Juraschek SP, Appel LJ, Mitchell CM et al. Comparison of supine and seated orthostatic hypotension assessments and their association with falls and orthostatic symptoms. J Am Geriatr Soc 2022; 70: 2310–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Mattace-Raso FU, van den Meiracker AH, Bos WJ et al. Arterial stiffness, cardiovagal baroreflex sensitivity and postural blood pressure changes in older adults: the Rotterdam study. J Hypertens 2007; 25: 1421–6. [DOI] [PubMed] [Google Scholar]
- 102. Oghalai JS, Manolidis S, Barth JL, Stewart MG, Jenkins HA. Unrecognized benign paroxysmal positional vertigo in elderly patients. Otolaryngol Head Neck Surg 2000; 122: 630–4. [DOI] [PubMed] [Google Scholar]
- 103. Gazzola JM, Gananca FF, Aratani MC, Perracini MR, Gananca MM. Circumstances and consequences of falls in elderly people with vestibular disorder. Braz J Otorhinolaryngol 2006; 72: 388–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Liston MB, Bamiou DE, Martin F et al. Peripheral vestibular dysfunction is prevalent in older adults experiencing multiple non-syncopal falls versus age-matched non-fallers: a pilot study. Age Ageing 2014; 43: 38–43. [DOI] [PubMed] [Google Scholar]
- 105. Hawke LJ, Barr CJ, McLoughlin JV. The frequency and impact of undiagnosed benign paroxysmal positional vertigo in outpatients with high falls risk. Age Ageing 2021; 50: 2025–30. [DOI] [PubMed] [Google Scholar]
- 106. Bourne RRA, Flaxman SR, Braithwaite T et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health 2017; 5: e888–97. [DOI] [PubMed] [Google Scholar]
- 107. Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology 2010; 21: 658–68. [DOI] [PubMed] [Google Scholar]
- 108. Jiam NT, Li C, Agrawal Y. Hearing loss and falls: a systematic review and meta-analysis. Laryngoscope 2016; 126: 2587–96. [DOI] [PubMed] [Google Scholar]
- 109. Damoiseaux-Volman BA, Medlock S, van der Eijk M, Romijn J, Abu-Hanna A, van der Velde N. Falls and delirium in older inpatients: work-as-imagined, work-as-done and preferences for clinical decision support systems. Safety Science 2021; 142: 105355. 10.1016/j.ssci.2021.105355. [DOI] [Google Scholar]
- 110. Morris ME, Webster K, Jones C et al. Interventions to reduce falls in hospitals: a systematic review and meta-analysis. Age Ageing 2022; 51. 10.1093/ageing/afac077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Toye C, Kitchen S, Hill A, Edwards D, Sin M, Maher S. Piloting staff education in Australia to reduce falls in older hospital patients experiencing delirium. Nurs Health Sci 2017; 19: 51–8. [DOI] [PubMed] [Google Scholar]
- 112. Ludolph P, Stoffers-Winterling J, Kunzler AM et al. Non-pharmacologic multicomponent interventions preventing delirium in hospitalized people. J Am Geriatr Soc 2020; 68: 1864–71. [DOI] [PubMed] [Google Scholar]
- 113. Siddiqi N, Harrison JK, Clegg A et al. Interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev 2016; 3: CD005563. 10.1002/14651858.CD005563.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Hshieh TT, Yang T, Gartaganis SL, Yue J, Inouye SK. Hospital Elder Life Program: Systematic Review and Meta-analysis of Effectiveness. Am J Geriatr Psychiatry 2018; 26: 1015–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Growdon ME, Shorr RI, Inouye SK. The tension between promoting mobility and preventing falls in the hospital. JAMA Intern Med 2017; 177: 759–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Moon S, Chung HS, Kim YJ et al. The impact of urinary incontinence on falls: a systematic review and meta-analysis. PLoS One 2021; 16: e0251711. 10.1371/jour-nal.pone.0251711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Pesonen JS, Vernooij RWM, Cartwright R et al. The impact of nocturia on falls and fractures: a systematic review and meta-analysis. J Urol 2020; 203: 674–83. [DOI] [PubMed] [Google Scholar]
- 118. Brown JS, Bradley CS, Subak LL et al. The sensitivity and specificity of a simple test to distinguish between urge and stress urinary incontinence. Ann Intern Med 2006; 144: 715–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Stubbs B, Schofield P, Binnekade T, Patchay S, Sepehry A, Eggermont L. Pain is associated with recurrent falls in community-dwelling older adults: evidence from a systematic review and meta-analysis. Pain Med 2014; 15: 1115–28. [DOI] [PubMed] [Google Scholar]
- 120. Lehti TE, Rinkinen MO, Aalto U et al. Prevalence of musculoskeletal pain and analgesic treatment among community-dwelling older adults: changes from 1999 to 2019. Drugs Aging 2021; 38: 931–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Schwan J, Sclafani J, Tawfik VL. Chronic pain management in the elderly. Anesthesiol Clin 2019; 37: 547–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Herr K. Pain assessment strategies in older patients. J Pain 2011; 12: S3–13. [DOI] [PubMed] [Google Scholar]
- 123. Pighills A, Clemson L. Environmental risk factors for falls. In: Lord S, Sherrington C, Naganathan V, eds. Falls in Older People: Risk Factors, Strategies for Prevention and Implications for Practice, 3rd edition. Cambridge: Cambridge University Press, 2021; 202–10. [Google Scholar]
- 124. Clemson L, Mackenzie L, Ballinger C, Close JC, Cumming RG. Environmental interventions to prevent falls in community-dwelling older people: a meta-analysis of randomized trials. J Aging Health 2008; 20: 954–71. [DOI] [PubMed] [Google Scholar]
- 125. Keglovits M, Clemson L, Hu YL et al. A scoping review of fall hazards in the homes of older adults and development of a framework for assessment and intervention. Aust Occup Ther J 2020; 67: 470–8. [DOI] [PubMed] [Google Scholar]
- 126. Clemson L, Pighills A. Environmental interventions to prevent falls at home and in the community. In: Lord S, Sherrington C, Naganathan V, eds. Falls in Older People: Risk Factors, Strategies for Prevention and Implications for Practice, 3rd edition. Cambridge, UK: Cambridge University Press, 2021; 360–77. [Google Scholar]
- 127. Clemson L, Stark S, Pighills A et al. Environmental interventions for preventing falls in older people living in the community (review). Cochrane Database Syst Rev 2022; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. van Poelgeest EP, Pronk AC, Rhebergen D, van der Velde N. Depression, antidepressants and fall risk: therapeutic dilemmas-a clinical review. Eur Geriatr Med 2021; 12: 585–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Trevisan C, Crippa A, Ek S et al. Nutritional status, body mass index, and the risk of falls in community-dwelling older adults: a systematic review and meta-analysis. J Am Med Dir Assoc 2019; 20: 569–582.e7. [DOI] [PubMed] [Google Scholar]
- 130. Guigoz Y. The Mini Nutritional Assessment (MNA) review of the literature—what does it tell us? J Nutr Health Aging 2006; 10: 466–85 discussion 85-7. [PubMed] [Google Scholar]
- 131. Blain H, Masud T, Dargent-Molina P et al. A comprehensive fracture prevention strategy in older adults: the European Union Geriatric Medicine Society (EUGMS) statement. J Nutr Health Aging 2016; 20: 647–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Li N, Hiligsmann M, Boonen A et al. The impact of fracture liaison services on subsequent fractures and mortality: a systematic literature review and meta-analysis. Osteoporos Int 2021; 32: 1517–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Masud T, Binkley N, Boonen S, Hannan MT, Members FPDC. Official positions for FRAX(R) clinical regarding falls and frailty: can falls and frailty be used in FRAX(R)? From Joint Official Positions Development Conference of the International Society for Clinical Densitometry and International Osteoporosis Foundation on FRAX(R). J Clin Densitom 2011; 14: 194–204. [DOI] [PubMed] [Google Scholar]
- 134. Beaudoin C, Moore L, Gagne M et al. Performance of predictive tools to identify individuals at risk of non-traumatic fracture: a systematic review, meta-analysis, and meta-regression. Osteoporos Int 2019; 30: 721–40. [DOI] [PubMed] [Google Scholar]
- 135. Kanis JA, Cooper C, Rizzoli R et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 2019; 30: 3–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Lamb SE, McCabe C, Becker C, Fried LP, Guralnik JM. The optimal sequence and selection of screening test items to predict fall risk in older disabled women: the Women's Health and Aging Study. J Gerontol A Biol Sci Med Sci 2008; 63: 1082–8. [DOI] [PubMed] [Google Scholar]
- 137. Sherrington C, Fairhall N, Kwok W et al. Evidence on physical activity and falls prevention for people aged 65+ years: systematic review to inform the WHO guidelines on physical activity and sedentary behaviour. Int J Behav Nutr Phys Act 2020; 17: 144. 10.1186/s12966-020-01041-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. World Health Organization . WHO Guidelines on Physical Activity and Sedentary Behaviour. Geneva: World Health Organization, 2020; Contract No.: Licence: CC BY-NC-SA 3.0 IGO. [PubMed] [Google Scholar]
- 139. Paganini-Hill A, Greenia DE, Perry S, Sajjadi SA, Kawas CH, Corrada MM. Lower likelihood of falling at age 90+ is associated with daily exercise a quarter of a century earlier: the 90+ study. Age Ageing 2017; 46: 951–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. World Health Organization . Integrated Care for Older People (ICOPE): Guidance for Person-Centred Assessment and Pathways in Primary Care. World Health Organization, 2019; Contract No.: License: CC BY-NC-SA 3.0 IGO). [Google Scholar]
- 141. Sherrington C, Fairhall NJ, Wallbank GK et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev 2019; 1: CD012424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Kim C, Armstrong MJ, Berta WB, Gagliardi AR. How to identify, incorporate and report patient preferences in clinical guidelines: a scoping review. Health Expect 2020; 23: 1028–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Hopewell S, Adedire O, Copsey BJ et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2018; 7: CD012221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. World Health Organization . Evidence Profile: Risk of Falls—Integrated Care for Older People. World Health Organization. [Google Scholar]
- 145. Bruce J, Hossain A, Lall R et al. Fall prevention interventions in primary care to reduce fractures and falls in people aged 70 years and over: the PreFIT three-arm cluster RCT. Health Technol Assess 2021; 25: 1–114. 10.3310/hta25340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Bhasin S, Gill TM, Reuben DB et al. A randomized trial of a multifactorial strategy to prevent serious fall injuries. N Engl J Med 2020; 383: 129–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. van der Velde N, Seppala L, Petrovic M et al. Sustainable fall prevention across Europe: challenges and opportunities. Aging Clin Exp Res 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Lamb S, Lee H. Multifactorial fall prevention strategies: where to next? In: Lord S, Sherrington C, Naganathan V, eds. Alls in Older People: Risk Factors, Strategies for Prevention and Implications for Practice, 3rd edition. Cambridge, UK: Cambridge University Press, 2019. [Google Scholar]
- 149. Izquierdo M, Merchant RA, Morley JE et al. International exercise recommendations in older adults (ICFSR): expert consensus guidelines. J Nutr Health Aging 2021; 25: 824–53. [DOI] [PubMed] [Google Scholar]
- 150. Di Lorito C, Bosco A, Booth V, Goldberg S, Harwood RH, Van der Wardt V. Adherence to exercise interventions in older people with mild cognitive impairment and dementia: a systematic review and meta-analysis. Prev Med Rep 2020; 19: 101139. 10.1016/j.pmedr.2020.101139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Simpson PM, Bendall JC, Tiedemann A, Lord SR, Close JC. Epidemiology of emergency medical service responses to older people who have fallen: a prospective cohort study. Prehosp Emerg Care 2014; 18: 185–94. [DOI] [PubMed] [Google Scholar]
- 152. Tinetti ME, Liu WL, Claus EB. Predictors and prognosis of inability to get up after falls among elderly persons. JAMA 1993; 269: 65–70. [PubMed] [Google Scholar]
- 153. Wild D, Nayak US, Isaacs B. How dangerous are falls in old people at home? Br Med J (Clin Res Ed) 1981; 282: 266–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Cone DC, Ahern J, Lee CH, Baker D, Murphy T, Bogucki S. A descriptive study of the "lift-assist" call. Prehosp Emerg Care 2013; 17: 51–6. [DOI] [PubMed] [Google Scholar]
- 155. Reece A, Simpson A. Preparing older people to cope after a fall. Physiotherapy 1996; 82: 227–35. [Google Scholar]
- 156. Skelton D, Dinan S, Campbell M, Rutherford O. Tailored group exercise (Falls Management Exercise—FaME) reduces falls in community-dwelling older frequent fallers (an RCT). Age Ageing 2005; 34: 636–9. [DOI] [PubMed] [Google Scholar]
- 157. Seppala LJ, van der Velde N. Fall-risk-increasing drugs: background, current evidence on deprescribing, and future perspectives. In: Integrated Care and Fall Prevention in Active and Healthy Aging. Hershey, PA, USA: IGI Global, 2021; 67–76. [Google Scholar]
- 158. Parekh N, Gahagan B, Ward L, Ali K. They must help if the doctor gives them to you': a qualitative study of the older person's lived experience of medication-related problems. Age Ageing 2019; 48: 147–51. [DOI] [PubMed] [Google Scholar]
- 159. Casilari E, Santoyo-Ramóna JA, Cano-Garcíaa JM. UMAFall: a multisensor dataset for the research on automatic fall detection. Procedia Computer Science 2017; 110: 32–9. [Google Scholar]
- 160. Alarifi A, Alwadain A. Killer heuristic optimized convolution neural network-based fall detection with wearable IoT sensor devices. Measurement 2021; 167: 108258. 10.1016/j.measurement.2020.108258. [DOI] [Google Scholar]
- 161. Bourke AK, Klenk J, Schwickert L et al. Temporal and kinematic variables for real-world falls harvested from lumbar sensors in the elderly population. Annu Int Conf IEEE Eng Med Biol Soc 2015; 2015: 5183–6. [DOI] [PubMed] [Google Scholar]
- 162. Scheurer S, Koch J, Kucera M et al. Optimization and technical validation of the AIDE-MOI fall detection algorithm in a real-life setting with older adults. Sensors (Basel) 2019; 19. 10.3390/s19061357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Saadeh W, Butt SA, Altaf MAB. A patient-specific single sensor IoT-based wearable fall prediction and detection system. IEEE Trans Neural Syst Rehabil Eng 2019; 27: 995–1003. [DOI] [PubMed] [Google Scholar]
- 164. Rescio G, Leone A, Siciliano P. Supervised machine learning scheme for electromyography-based pre-fall detection system. Expert Syst Appl 2018; 100: 95–105. [Google Scholar]
- 165. Reginatto B, Taylor K, Patterson MR et al. Context aware falls risk assessment: a case study comparison. Annu Int Conf IEEE Eng Med Biol Soc 2015; 2015: 5477–80. [DOI] [PubMed] [Google Scholar]
- 166. Chaudhuri S, Oudejans D, Thompson HJ, Demiris G. Real-world accuracy and use of a wearable fall detection device by older adults. J Am Geriatr Soc 2015; 63: 2415–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Marschollek M, Rehwald A, Wolf KH et al. Sensors vs. experts—a performance comparison of sensor-based fall risk assessment vs. conventional assessment in a sample of geriatric patients. BMC Med Inform Decis Mak 2011; 11: 48. 10.1186/1472-6947-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Levy SS, Thralls KJ, Kviatkovsky SA. Validity and reliability of a portable balance tracking system, BTrackS, in older adults. J Geriatr Phys Ther 2018; 41: 102–7. [DOI] [PubMed] [Google Scholar]
- 169. Liang S, Ning Y, Li H et al. Feature selection and predictors of falls with foot force sensors using KNN-based algorithms. Sensors (Basel) 2015; 15: 29393–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Di Rosa M, Hausdorff JM, Stara V et al. Concurrent validation of an index to estimate fall risk in community dwelling seniors through a wireless sensor insole system: a pilot study. Gait Posture 2017; 55: 6–11. [DOI] [PubMed] [Google Scholar]
- 171. Weiss A, Herman T, Plotnik M, Brozgol M, Giladi N, Hausdorff JM. An instrumented timed up and go: the added value of an accelerometer for identifying fall risk in idiopathic fallers. Physiol Meas 2011; 32: 2003–18. [DOI] [PubMed] [Google Scholar]
- 172. Chan JKY, Klainin-Yobas P, Chi Y, Gan JKE, Chow G, Wu XV. The effectiveness of e-interventions on fall, neuromuscular functions and quality of life in community-dwelling older adults: a systematic review and meta-analysis. Int J Nurs Stud 2021; 113: 103784. 10.1016/j.ijnurstu.2020.103784. [DOI] [PubMed] [Google Scholar]
- 173. Harris T, Kerry SM, Limb ES et al. Effect of a primary care walking intervention with and without nurse support on physical activity levels in 45- to 75-year-olds: the pedometer and consultation evaluation (PACE-UP) cluster randomised clinical trial. PLoS Med 2017; 14: e1002210. 10.1371/jour-nal.pmed.1002210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Chu MM, Fong KN, Lit AC et al. An occupational therapy fall reduction home visit program for community-dwelling older adults in Hong Kong after an emergency department visit for a fall. J Am Geriatr Soc 2017; 65: 364–72. [DOI] [PubMed] [Google Scholar]
- 175. Stark S, Keglovits M, Somerville E et al. Home hazard removal to reduce falls among community-dwelling older adults: a randomized clinical trial. JAMA Netw Open 2021; 4: e2122044. 10.1001/jamanetworkopen.2021.22044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev 2014; 8: CD003162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Gananca FF, Gazzola JM, Gananca CF, Caovilla HH, Gananca MM, Cruz OL. Elderly falls associated with benign paroxysmal positional vertigo. Braz J Otorhinolaryngol 2010; 76: 113–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Jumani K, Powell J. Benign paroxysmal positional vertigo: management and its impact on falls. Ann Otol Rhinol Laryngol 2017; 126: 602–5. [DOI] [PubMed] [Google Scholar]
- 179. McDonnell MN, Hillier SL. Vestibular rehabilitation for unilateral peripheral vestibular dysfunction. Cochrane Database Syst Rev 2015; 1: CD005397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons . Pharmacological management of persistent pain in older persons. Pain Med 2009; 10: 1062–83. [DOI] [PubMed] [Google Scholar]
- 181. Gloth FM 3rd. Pharmacological management of persistent pain in older persons: focus on opioids and nonopioids. J Pain 2011; 12: S14–20. [DOI] [PubMed] [Google Scholar]
- 182. Virnes RE, Tiihonen M, Karttunen N, van Poelgeest EP, van der Velde N, Hartikainen S. Opioids and falls risk in older adults: a narrative review. Drugs Aging 2022; 39: 199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Pickering G, Marcoux M, Chapiro S et al. An algorithm for neuropathic pain management in older people. Drugs Aging 2016; 33: 575–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Kendrick D, Kumar A, Carpenter H et al. Exercise for reducing fear of falling in older people living in the community. Cochrane Database Syst Rev 2014; 28: CD009848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Kruisbrink M, Crutzen R, Kempen G et al. Disentangling interventions to reduce fear of falling in community-dwelling older people: a systematic review and meta-analysis of intervention components. Disabil Rehabil 2021; 1–11. 10.1080/09638288.2021.1969452. [DOI] [PubMed] [Google Scholar]
- 186. Kruisbrink M, Delbaere K, Kempen G et al. Intervention characteristics associated with a reduction in fear of falling among community-dwelling older people: a systematic review and meta-analysis of randomized controlled trials. Gerontologist 2021; 61: e269–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. CHM C, Jiang Y, Lim S, Wu VX, Wang W. Effectiveness of cognitive behaviour therapy-based multicomponent interventions on fear of falling among community-dwelling older adults: a systematic review and meta-analysis. J Adv Nurs 2019; 75: 3299–315. [DOI] [PubMed] [Google Scholar]
- 188. Liu TW, Ng GYF, Chung RCK, Ng SSM. Cognitive behavioural therapy for fear of falling and balance among older people: a systematic review and meta-analysis. Age Ageing 2018; 47: 520–7. [DOI] [PubMed] [Google Scholar]
- 189. De Coninck L, Bekkering GE, Bouckaert L, Declercq A, Graff MJL, Aertgeerts B. Home- and community-based occupational therapy improves functioning in frail older people: a systematic review. J Am Geriatr Soc 2017; 65: 1863–9. [DOI] [PubMed] [Google Scholar]
- 190. Harwood RH, Foss AJE, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. Br J Ophthalmol 2005; 89: 53–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Keay L, Ho KC, Rogers K et al. The incidence of falls after first and second eye cataract surgery: a longitudinal cohort study. Med J Aust 2022; 217: 94–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Haran MJ, Cameron ID, Ivers RQ et al. Effect on falls of providing single lens distance vision glasses to multifocal glasses wearers: VISIBLE randomised controlled trial. Br Med J 2010; 340: c2265. 10.1136/bmj.c2265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Campbell AJ, Robertson MC, Grow SJL et al. Randomised controlled trial of prevention of falls in people aged ≥75 with severe visual impairment: the VIP trial. BMJ 2005; 331: 817. 10.1136/bmj.38601.447731.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Cumming RG, Ivers R, Clemson L et al. Improving vision to prevent falls in frail older people: a randomized trial. J Am Geriatr Soc 2007; 55: 175–81. [DOI] [PubMed] [Google Scholar]
- 195. Michos ED, Kalyani RR, Blackford AL et al. The relationship of falls with achieved 25-Hydroxyvitamin D levels from vitamin D supplementation: the STURDY trial. J Endocr Soc 2022; 6: bvac065. 10.1210/jendso/bvac065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. LeBoff MS, Murata EM, Cook NR et al. VITamin D and OmegA-3 TriaL (VITAL): effects of vitamin D supplements on risk of falls in the US population. J Clin Endocrinol Metab 2020; 105: 2929–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Dawson-Hughes B, Mithal A, Bonjour JP et al. IOF position statement: vitamin D recommendations for older adults. Osteoporos Int 2010; 21: 1151–4. [DOI] [PubMed] [Google Scholar]
- 198. Holick MF, Binkley NC, Bischoff-Ferrari HA et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2011; 96: 1911–30. [DOI] [PubMed] [Google Scholar]
- 199. Cosman F, de Beur SJ, LeBoff MS et al. Clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int 2014; 25: 2359–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Jellett J, Williams C, Clayton D, Plummer V, Haines T. Falls risk score removal does not impact inpatient falls: a stepped-wedge, cluster-randomised trial. J Clin Nurs 2020; 29: 4505–13. [DOI] [PubMed] [Google Scholar]
- 201. Heng H, Jazayeri D, Shaw L, Kiegaldie D, Hill AM, Morris ME. Hospital falls prevention with patient education: a scoping review. BMC Geriatr 2020; 20: 140. 10.1186/s12877-020-01515-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Dykes PC, Carroll DL, Hurley A et al. Fall prevention in acute care hospitals: a randomized trial. JAMA 2010; 304: 1912–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Hada A, Coyer F. Shift-to-shift nursing handover interventions associated with improved inpatient outcomes-falls, pressure injuries and medication administration errors: an integrative review. Nurs Health Sci 2021; 23: 337–51. [DOI] [PubMed] [Google Scholar]
- 204. Milisen K, Coussement J, Arnout H et al. Feasibility of implementing a practice guideline for fall prevention on geriatric wards: a multicentre study. Int J Nurs Stud 2013; 50: 495–507. [DOI] [PubMed] [Google Scholar]
- 205. Shaw L, Kiegaldie D, Morris ME. Educating health professionals to implement evidence-based falls screening in hospitals. Nurse Educ Today 2021; 101: 104874. 10.1016/j.nedt.2021.104874. [DOI] [PubMed] [Google Scholar]
- 206. Logan PA, Horne JC, Allen F et al. A multidomain decision support tool to prevent falls in older people: the FinCH cluster RCT. Health Technol Assess 2022; 26: 1–136. 10.3310/CWIB0236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Sze TW, Leng CY, Lin SK. The effectiveness of physical restraints in reducing falls among adults in acute care hospitals and nursing homes: a systematic review. JBI Libr Syst Rev 2012; 10: 307–51. [DOI] [PubMed] [Google Scholar]
- 208. Brugnolli A, Canzan F, Mortari L, Saiani L, Ambrosi E, Debiasi M. The effectiveness of educational training or multicomponent programs to prevent the use of physical restraints in nursing home settings: a systematic review and meta-analysis of experimental studies. Int J Environ Res Public Health 2020; 17. 10.3390/ijerph17186738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. Hewitt J, Goodall S, Clemson L, Henwood T, Refshauge K. Progressive resistance and balance training for falls prevention in long-term residential aged care: a cluster randomized trial of the sunbeam program. J Am Med Dir Assoc 2018; 19: 361–9. [DOI] [PubMed] [Google Scholar]
- 210. Logan PA, Horne JC, Gladman JRF et al. Multifactorial falls prevention programme compared with usual care in UK care homes for older people: multicentre cluster randomised controlled trial with economic evaluation. BMJ 2021; 375: e066991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. Pickering RM, Grimbergen YA, Rigney U et al. A meta-analysis of six prospective studies of falling in Parkinson's disease. Mov Disord 2007; 22: 1892–900. [DOI] [PubMed] [Google Scholar]
- 212. King LA, Mancini M, Smulders K et al. Cognitively challenging agility boot camp program for freezing of gait in Parkinson disease. Neurorehabil Neural Repair 2020; 34: 417–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Lindholm B, Nilsson MH, Hansson O, Hagell P. External validation of a 3-step falls prediction model in mild Parkinson's disease. J Neurol 2016; 263: 2462–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214. Paul SS, Canning CG, Sherrington C, Lord SR, Close JC, Fung VS. Three simple clinical tests to accurately predict falls in people with Parkinson's disease. Mov Disord 2013; 28: 655–62. [DOI] [PubMed] [Google Scholar]
- 215. Pelicioni PHS, Menant JC, Latt MD, Lord SR. Falls in Parkinson's disease subtypes: risk factors, locations and circumstances. Int J Environ Res Public Health 2019; 16. 10.3390/ijerph16122216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216. Latt MD, Lord SR, Morris JG, Fung VS. Clinical and physiological assessments for elucidating falls risk in Parkinson's disease. Mov Disord 2009; 24: 1280–9. [DOI] [PubMed] [Google Scholar]
- 217. Canning CG, Sherrington C, Lord SR et al. Exercise for falls prevention in Parkinson disease: a randomized controlled trial. Neurology 2015; 84: 304–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218. Chivers Seymour K, Pickering R, Rochester L et al. Multicentre, randomised controlled trial of PDSAFE, a physiotherapist-delivered fall prevention programme for people with Parkinson's. J Neurol Neurosurg Psychiatry 2019; 90: 774–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Parthimos TP, Schulpis KH. The progressive supranuclear palsy: past and present aspects. Clin Gerontol 2020; 43: 155–80. [DOI] [PubMed] [Google Scholar]
- 220. Skorvanek M, Martinez-Martin P, Kovacs N et al. Differences in MDS-UPDRS scores based on Hoehn and Yahr stage and disease duration. Mov Disord Clin Pract 2017; 4: 536–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Allen NE, Canning CG, Almeida LRS et al. Interventions for preventing falls in Parkinson's disease. Cochrane Database Syst Rev 2022; 6: CD011574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222. Henderson EJ, Lord SR, Brodie MA et al. Rivastigmine for gait stability in patients with Parkinson's disease (ReSPonD): a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Neurol 2016; 15: 249–58. [DOI] [PubMed] [Google Scholar]
- 223. Racey M, Markle-Reid M, Fitzpatrick-Lewis D et al. Fall prevention in community-dwelling adults with mild to moderate cognitive impairment: a systematic review and meta-analysis. BMC Geriatr 2021; 21: 689. 10.1186/s12877-021-02641-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Li F, Harmer P, Eckstrom E et al. Efficacy of exercise-based interventions in preventing falls among community-dwelling older persons with cognitive impairment: is there enough evidence? An updated systematic review and meta-analysis. Age Ageing 2021; 50: 1557–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225. Burton E, Cavalheri V, Adams R et al. Effectiveness of exercise programs to reduce falls in older people with dementia living in the community: a systematic review and meta-analysis. Clin Interv Aging 2015; 10: 421–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Suttanon P, Hill K, Said C, Dodd K. Can balance exercise programmes improve balance and related physical performance measures in people with dementia: a systematic review. Eur Rev Aging Phys Act 2010; 7: 13–25. [Google Scholar]
- 227. Nyman SR, Ingram W, Sanders J et al. Randomised controlled trial of the effect of tai Chi on postural balance of people with dementia. Clin Interv Aging 2019; 14: 2017–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Pitkala KH, Poysti MM, Laakkonen ML et al. Effects of the Finnish Alzheimer disease exercise trial (FINALEX): a randomized controlled trial. JAMA Intern Med 2013; 173: 894–901. [DOI] [PubMed] [Google Scholar]
- 229. Fairhall N, Dyer S, Kowk W, Mak J, Diong J, Sherrington C. Interventions for improving mobility after hip fracture surgery in adults. Cochrane Database Syst Rev Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230. Sherrington C, Michaleff ZA, Fairhall N et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med 2017; 51: 1750–8. [DOI] [PubMed] [Google Scholar]
- 231. Ozturk ZA, Turkbeyler IH, Abiyev A et al. Health-related quality of life and fall risk associated with age-related body composition changes; sarcopenia, obesity and sarcopenic obesity. Intern Med J 2018; 48: 973–81. [DOI] [PubMed] [Google Scholar]
- 232. Máximo R, Santos J, Perracini M, Oliveira C, Duarte Y, Alexandre T. Abdominal obesity, dynapenia and dynapenic-abdominal obesity as factors associated with falls. Braz J Phys Ther 2019; 23: 497–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233. Szlejf C, Parra-Rodriguez L, Rosas-Carrasco O. Osteosarcopenic obesity: prevalence and relation with frailty and physical performance in middle-aged and older women. J Am Med Dir Assoc 2017; 18: 733.e1–5. [DOI] [PubMed] [Google Scholar]
- 234. Waters DL, Qualls CR, Cesari M, Rolland Y, Vlietstra L, Vellas B. Relationship of incident falls with balance deficits and body composition in male and female community-dwelling elders. J Nutr Health Aging 2019; 23: 9–13. [DOI] [PubMed] [Google Scholar]
- 235. Allain TJ, Mwambelo M, Mdolo T, Mfune P. Falls and other geriatric syndromes in Blantyre, Malawi: a community survey of older adults. Malawi Med J 2014; 26: 105–8. [PMC free article] [PubMed] [Google Scholar]
- 236. Wettasinghe AH, Dissanayake DWN, Allet L, Katulanda P, Lord SR. Falls in older people with diabetes: identification of simple screening measures and explanatory risk factors. Prim Care Diabetes 2020; 14: 723–8. [DOI] [PubMed] [Google Scholar]
- 237. Wettasinghe A, Dissanayake D, Allet L, Katulanda P, Lord S. The impact of physical, neurological and cognitive deficits on risk of falls in people with type 2 diabetes mellitus: a review. SLJDEM 2020; 10: 18–25. [Google Scholar]
- 238. Prince M, Acosta D, Ferri CP et al. Dementia incidence and mortality in middle-income countries, and associations with indicators of cognitive reserve: a 10/66 Dementia Research Group population-based cohort study. Lancet 2012; 380: 50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239. Chaiwanichsiri D, Janchai S, Tantisiriwat N. Foot disorders and falls in older persons. Gerontology 2009; 55: 296–302. [DOI] [PubMed] [Google Scholar]
- 240. Dent E, Morley JE, Cruz-Jentoft AJ et al. Physical frailty: ICFSR international clinical practice guidelines for identification and management. J Nutr Health Aging 2019; 23: 771–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241. Chu W, Chang SF, Ho HY. Adverse health effects of frailty: systematic review and meta-analysis of middle-aged and older adults with implications for evidence-based practice. Worldviews Evid Based Nurs 2021; 18: 282–9. [DOI] [PubMed] [Google Scholar]
- 242. Islam A, Muir-Hunter SW, Speechley M, Montero-Odasso M. Facilitating frailty identification: comparison of two methods among community-dwelling order adults. J Frailty Aging 2014; 3: 216–21. [DOI] [PubMed] [Google Scholar]
- 243. Landi F, Liperoti R, Russo A et al. Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr 2012; 31: 652–8. [DOI] [PubMed] [Google Scholar]
- 244. Chen LK, Woo J, Assantachai P et al. Asian working group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc 2020; 21: 300–307.e2. [DOI] [PubMed] [Google Scholar]
- 245. Cruz-Jentoft AJ, Bahat G, Bauer J et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019; 48: 16–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009; 4: 50. 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247. Skivington K, Matthews L, Simpson SA et al. Framework for the development and evaluation of complex interventions: gap analysis, workshop and consultation-informed update. Health Technol Assess 2021; 25: 1–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Vlaeyen E, Stas J, Leysens G et al. Implementation of fall prevention in residential care facilities: a systematic review of barriers and facilitators. Int J Nurs Stud 2017; 70: 110–21. [DOI] [PubMed] [Google Scholar]
- 249. Braithwaite J, Marks D, Taylor N. Harnessing implementation science to improve care quality and patient safety: a systematic review of targeted literature. International J Qual Health Care 2014; 26: 321–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.