Abstract
Androgens are an important and diverse group of steroid hormone molecular species. They play varied functional roles, such as the control of metabolic energy fate and partition, the maintenance of skeletal and body protein and integrity and the development of brain capabilities and behavioral setup (including those factors defining maleness). In addition, androgens are the precursors of estrogens, with which they share an extensive control of the reproductive mechanisms (in both sexes). In this review, the types of androgens, their functions and signaling are tabulated and described, including some less-known functions. The close interrelationship between corticosteroids and androgens is also analyzed, centered in the adrenal cortex, together with the main feedback control systems of the hypothalamic–hypophysis–gonads axis, and its modulation by the metabolic environment, sex, age and health. Testosterone (T) is singled out because of its high synthesis rate and turnover, but also because age-related hypogonadism is a key signal for the biologically planned early obsolescence of men, and the delayed onset of a faster rate of functional losses in women after menopause. The close collaboration of T with estradiol (E2) active in the maintenance of body metabolic systems is also presented Their parallel insufficiency has been directly related to the ravages of senescence and the metabolic syndrome constellation of disorders. The clinical use of T to correct hypoandrogenism helps maintain the functionality of core metabolism, limiting excess fat deposition, sarcopenia and cognoscitive frailty (part of these effects are due to the E2 generated from T). The effectiveness of using lipophilic T esters for T replacement treatments is analyzed in depth, and the main problems derived from their application are discussed.
Keywords: androgens, testosterone, dehydroepiandrosterone, estradiol, dihydrotestosterone, anabolic steroids, metabolic regulation, senescence, metabolic syndrome, testosterone replacement therapy
1. Introduction
In recent decades, as a consequence of the methodological advances in analysis and clinical characterization of steroid hormones, we have exponentially advanced in the understanding of their diverse functions in the control of human metabolism and behavior. Our knowledge of steroid hormone physiological functions, however, lags behind. This is due, in part to the need to combine the (predominant) pharmacologically oriented objectives, with a slower pace of advances in adequate analytical technologies. The growing complexity of the newly acquired (albeit partial and often piecemeal) knowledge is further compounded by the extension of the studies to a widening number of branching and specialized fields, such as cell/tissue compartmentation [1] and molecular biophysics [2]; this may complicate the interpretation of the metabolic-regulative picture as a whole, from fragmented (and often isolated) information.
The additional presence of bias against the “sex hormones”, for different reasons (basically unsupported by scientific knowledge) [3], and the excessive focalization of most studies on only a limited number of natural hormones [4], has left enormous gaps of knowledge about the actual functions of the steroid hormones. In contrast, the common incorporation of many drugs derived from them or mimicking some of their actions [5] continues to rise.
In humans (and most mammals), steroid hormones are conventionally classified using the classical names of their most representative molecular forms: 21C corticosteroids (i.e., glucocorticoids (GC) and mineralocorticoids), 21C progestogens (with a pregnane structure), 18C estrogens (sharing the estrane skeleton) and 19C androgens (based on the androstane structure). At present, we also include in this extensive grouping, the 24C bile acids [6] (with a cholane structure), and the 27C hydroxyl-calciferols and vitamin D vitamers [7,8] (derived from cholesterol’s 27C-cholestane skeleton, albeit not retaining its four-ring structure). There are many more steroidal hormone types, assumedly restricted to other kingdoms and phyla, but most of them remain yet to be identified and/or characterized.
The use of names for these large groups of molecules is difficult to justify when taking into account the compounds’ physiological (and more often than not, their pharmacological) effects. The molecular species within any given group are often included within broad general descriptions that try to include all of them (e.g., estrogenic activity, androgen deficit, iatrogenic effects of GC) in a short overall definition of function and belonging. The systematic use of this convention is deeply embedded in both clinical and basic science studies, commonly assuming that the different molecules may show, perhaps, a different binding ability and variable overall effects, but nonetheless, their effects remain cohesive and directly interrelated within the context of each of these groups. This interpretation is further muddled by the often scant differences on specific pharmacological actions of a number of both natural and synthetic derivatives, which, assumedly, maintain or “improve” some of the hormone functional effects (in fact, simply noting their pharmacological actions). The classical groups of steroid hormones and derived “families” need to be actualized to incorporate the ample present-day knowledge as a whole. There is a need for more precise ways to organize and differentiate (at least) the natural steroidal hormones according to their structure and function, but (mainly) taking into account the critical importance of their mechanisms of action, functions and regulation, extended to their synthetic (or location-related) pathways [9].
Androgens are a clear example of this often forsaken (or unexpected) diversity. It is generally assumed that androgens are hormones primarily related to sex/reproduction, identified with the male-oriented physiology and psychology traits and patterns. Androgens, together with estrogens (often also including progesterone), are usually also known with the old and restrictive term of “sex hormones” [4]. Androgens, consequently, are assumed to modulate body growth and differentiation following the male blueprint; they modify brain development and the functional structure along patterns (and behavior) linked to maleness [10], thus, establishing an, also presumed, wide gap with estrogens (i.e., the main female sex hormones) which characterize (and distinguish) the complex biological standing of females in the reproductive continuity [11,12]. In a social and very general sense, these simplifications may be acceptable, but they could not be used within a precise scientific or medical context. The reasons for not using them abound; for instance, the circulating levels of some estrogens are often as high in men as they are in women; in addition, children of both genders (and women) may have similar total androgen levels than (sexually functional) adult men [13]. The question is whether the term “androgens” includes a wide number of molecular species that exert many different specific functions, some of them hardly related to reproduction, at least in a direct way. The same can be said of estrogens [9]. Thus, the indiscriminate use of compounds from each of the steroid hormone groups for the treatment of a wide (and widening) range of disorders (endocrine, metabolic or even aesthetic), could not be justified without a thorough analysis of the whole, contrasting the known effects of specific molecular species with the results expected and including the probable consequences of their eventual medical application [14,15].
2. Age Dependence of the Biological and Social Functions of Androgens in Males
Evidently, at the core, estrogens and androgens are clearly related to reproduction—in addition to maintaining body functions and energy homeostasis [16,17]—since all these functions are inextricable from the biological drive of species’ survival. The decrease in circulating estradiol (E2) after menopause is linked to the programmed disconnection of the ovulatory cycles. Women’s age, fitness and the onset of menopause make their ability to endure (in time) the ordeal of bearing and nurturing children biologically improbable, and thus, their reproductive functions are discontinued earlier. This planned obsolescence results in “collateral” disorders affecting many systems, since estradiol helps maintain the function of a many key metabolic processes which could no longer be fully supported [18] when its availability fails.
Nevertheless, in men, the production of viable sperm (and thus, the possibility of siring descendants) is often maintained up to an advanced age [19]. This gender difference has logical nutrient-economy reasons, since the reproductive cost in time and biological resources is obviously much easier for men than the severe metabolic strain women endure in the extended time- and nutrient-expense burden of childbearing/raising. Notwithstanding, in men, reproductive activity decreases progressively with age from their apex of physical/sexual performance in youth, which is earlier than full maturity. This is due, in part, to men’s lower biological resilience, coupled with an age-related decrease in muscular power, and especially, the larger cumulative male death toll, of which is a consequence of higher risk-taking, competence for mating and the altruistic risk of defending the group against predators. This has been compounded, along evolution/history, by the risks and energy cost of family/tribe protection tasks and social role programming. Most men do not attain an advanced age, largely because of a higher cumulative exposure to mortality than women [20]. In the context of group survival, most men are expendable (and/or needed by the community for shorter lifetime periods than females). Consequently, progressive attrition lowers their ranks, socially favoring the channeling of available food resources (and protection) to fertile women and viable children. This is a common blueprint across many species, which we humans share.
Thus, in parallel to women, men are also subjected to important hormonal changes with aging [21]. Usually, the process of andropause [22] is less abrupt in its presentation than menopause is in women, but its results are nonetheless crippling [23]. The aging-generated changes limit even more the men’s “usefulness” for the group, which directly affects their individual survival. At present, however, the relative abundance of food (and better overall health) tends to partly ease this early culling. However, the few differences in the basic hormonal makeup of men and women result in a higher predisposition of men to develop the metabolic syndrome (MS) earlier and more severely [24,25]. The progressive decrease in testosterone (T) levels with advancing age contrasts with the maintained hormone cycle-sustained ovulation in women, that ceases in a short timespan at menopause [26]. MS is much more frequent in adult (and, especially, in aging) men than in women [27], but not in the very old. Menopause is associated with hyperandrogenism [28], caused largely by adrenal androgens [29], whilst lower T availability is a known critical factor for MS development in men [30,31]. This difference is indirect well-known proof that not all androgens’ functions are equal.
Hypogonadism is one of the most constant (and defining) characteristics of MS [31], which, in men, compounds the (programmed) hormonal fall caused by aging [32]. The progressive lowering of T levels elicits a cluster of negative consequences: altered body protein maintenance, decreased fitness for exercise/fight [33], diminished cognitive functioning [34], lower incentive and eligibility for mating, and a growing number of metabolic disorders. The latter are, in a significant part, a consequence of the parallel decrease in estrogen synthesis (and availability) [35] caused by the dwindling precursor T production [30]. Estrogens control energy partition [3], and their insufficient levels foment obesity [36]. This programmed obsolescence of males’ functionality in the wake of the progressive loss of T may be described either as a key consequence or as a main cause of MS.
3. Types of Androgens—Synthesis, Structure and Functions
Androgens are synthesized from cholesterol in the testes (and annex structures), largely in the Leydig cells [37] of men, as well as in the ovaries of women. The brain can also synthesize a number of androgens, including DHEA [38]. Other organs (i.e., skin, adipose tissue) produce several molecular species of androgens [39] from DHEA or other precursors [40].
In addition, androgens are massively synthesized in the adrenal cortex, in the outer glomerulosa layer—along with mineralocorticoids [41]—in the intermediate fasciculata with glucocorticoids [42] and in the inner reticularis layer with dehydroepiandrosterone (DHEA) [43]. The 11-keto-androgens (KTs), largely 11-keto-testosterone (KT), are major androgens [44] synthesized largely in the fasciculata and reticularis zones [13,45]. The testes are also an important site for KT synthesis [44].
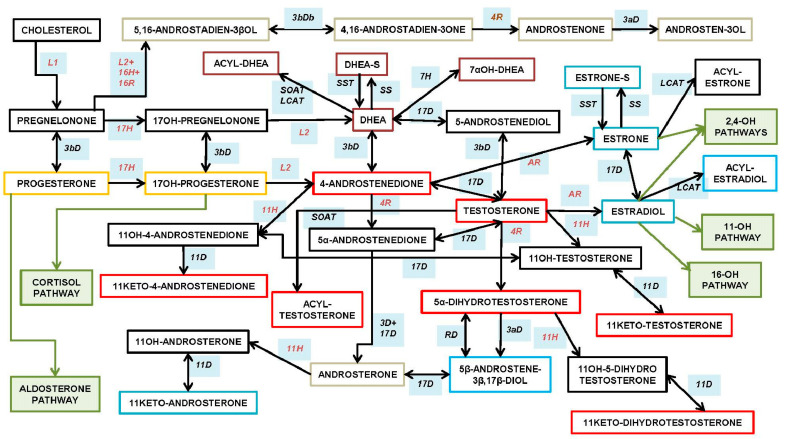
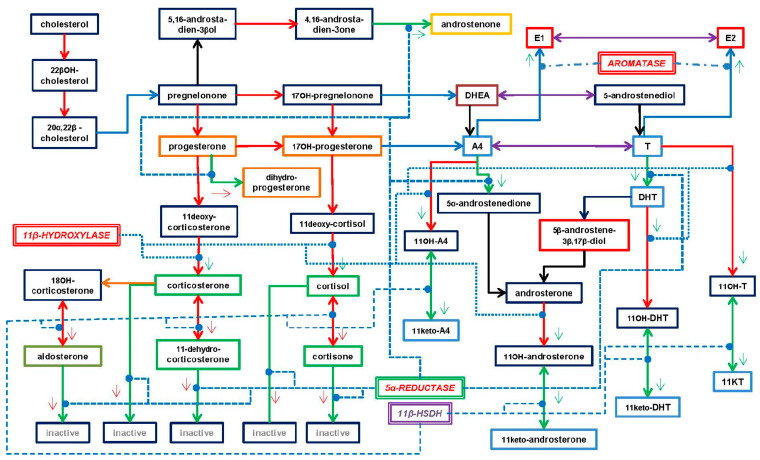
Figure 1 shows the synthetic pathways of the steroid hormones in the adrenal cortex (i.e., in men and women, from a child to an elderly person), testes and other tissues (e.g., skin). Quantitatively, the main androgenic products of adrenal glands are DHEA—found mainly as its sulfate (DHEAS)—and KT, while the testes produce, essentially, T, and to a lower extent, dihydrotestosterone (DHT), but also secrete pheromones (also synthesized in the skin). Interconversions between some androgens—and essentially, the aromatization to estrogens [46]—have been described also in adipose tissue [47,48], the brain [49] and other sites [50].
Figure 1.
Main androgen sytntheis pathways. This figure represents the physiological molecular species secreted in/by adrenal glands (intermediate and cortical layers), testicles, ovaries and the brain, as well by a number of other organs or tissues with a critical participation in these processes (e.g., skin, liver, adipose tissue). Since the synthesis of androgens (especially in the adrenal glands) is closely related to the two parallel corticosteroid synthesis pathways (they share location and a few enzyme activities), the start of these paths has been indicated in green squares. This includes the estrogens, which metabolism is much more closely intertwined with that of the main androgens. The 16-[estriol] and 11-hydroxylative pathways, as well as the catechol-estrogen specific pathway, have been included only as annotations in green labels. Black arrows show the enzyme-driven changes between molecular species; two-headed arrows show reactions that are potentially bidirectional. The main androgen molecule borders are red, violet in those sharing androgen and estrogen capabilities and blue in the fully estrogenic molecules; the progestogen borders are marked in yellow, and the androgenic pheromone species are in grey. The remaining molecules (black borders) may show a limited (if any) androgen receptor binding ability. The enzymes intervening in the reactions depicted are listed below the figure. They are presented in borderless pale blue rectangles in contact with the corresponding black arrows; the letters are in brown for mitochondrial and black for microsomal (and other location) enzymes.
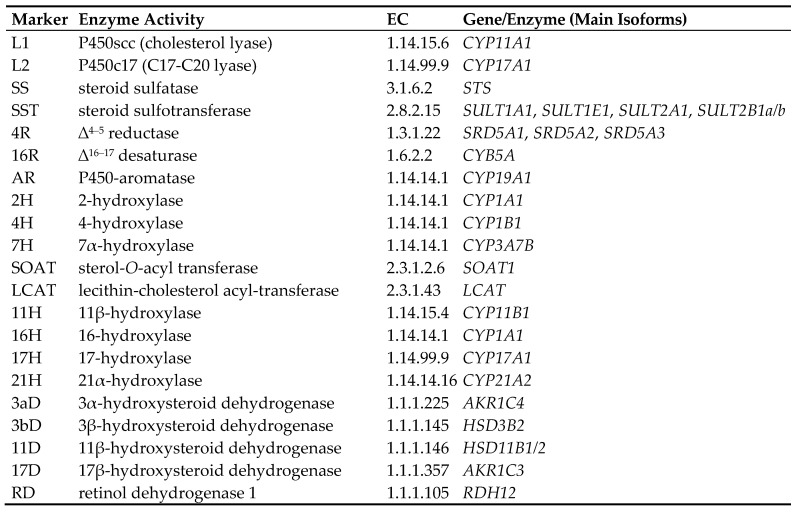
Figure 2 shows the main structure/function types of natural androgens, which main synthetic pathways are shown in Figure 1. These different types of androgens are briefly described below.
Figure 2.
Types of human androgens. The androgen molecular species (or groups of them) show similar chemical structures, are synthesized in a number of different tissues (but mainly in adrenal glands and the gonads) and elicit physiological effects that are largely complementary. DHEA: dehydroepiandrosterone; T: testosterone; AcT: 17β-acyl-T, a group of esters; KTs: 11-keto-androgens (essentially derived from T, DHT and A4; the 11-keto forms are more active than the 11-hydroxyl ones); DHT: dihydrotestosterone; A4: 4-androstenedione; AP: androgenic pheromones; EA: estrogenic androgens (i.e., they bind to the ER and AR); Ane: androsterone—a catabolite of T—which is an agonist of the farnesoid receptor, acting in the regulation of bile acid signaling. There are many other androgen catabolism products and intermediate molecular species of the androgen metabolism, which specialized functions have not been described in depth, but have been studied as pharmacological subjects, metabolic markers or substrates for synthetic hormone production. The androgens susceptible of aromatization are marked with green benzene icons. Small red arrows point to the distinguishing structural features of the different groups of androgens in comparison with T taken as the standard and best-known androgen.
-
○
DHEA dehydroepiandrosterone (DHEA): 7OH-DHEA and its esters: DHEAS and acyl-DHEA.
-
○
DHEA is formed from cholesterol via pregnelonone and 17OH-pregnelonone. Its hydrophilic sulfate ester, DHEAS, is the main steroid hormone in the human bloodstream [51]. DHEA binds both (albeit not strongly) the androgen (AR) and estrogen (ER) receptors [52]. Acyl-DHEA can be formed by plasma lipoproteins [53], via lecithin-cholesterol acyltransferase [54], and has been related to DHEA transport into tissues [55]. DHEA affects the regulation of corticosteroids [56,57], but all its functions have not been fully unraveled.
-
○
T testosterone (T).
T is the main and best-known androgen. It was isolated [58] and first synthesized in 1935 [59]. T is formed from DHEA via 3β- and 17β-hydroxylases; the intermediate precursors being either 5-androstenediol or 4-androstenedione (A4).
-
○
AcT 17 β-acyl-testosterone esters (AcT).
In natural AcT, the acyl group is usually a C16-C18 fatty acid. AcT are found in small amounts in tissues [60] and, especially, in lipoproteins [61]. AcT are formed via acyl-CoA transferase esterification on C17 [62], and are assumedly hydrolyzed to fatty acids and T by a number of acyl-esterases [63]. Under physiological conditions, AcT are not aromatized to acyl-E2 [64].
-
○
KTs 11-oxo-androgens, such as 11β-hydroxy-testosterone and 11-keto-testosterone (KT).
This group also includes the 11-oxo derivatives of 4-androstenedione and 5-dihydrotestosterone. KT is the main adrenal “true” androgen [65,66], but it is also produced by the testes [67]. The key enzyme in their synthesis is a 11β-hydroxylase, which also intervenes in the formation of GC, but (at least in the zebrafish) it favors the oxidation mode, which allows the conversion of 11-OH-T to produce KT. This mode is not adequate for the synthesis of active hydroxyl-corticoids from their 11-keto pairs, since a reducing (i.e., not oxidizing) reaction is needed. The function and regulation of this enzyme may possibly constitute an important node in the interrelationship between androgens and glucocorticoids in the adrenal glands [68]. KT is predominant, and has more androgenic effects than 11β-hydroxy-testosterone [42,69]. The formation of both 11-oxo-DHT derivatives seems to be of lesser entity than those of T [69,70].
-
○
DHT 4,5-dihydro-testosterone (DHT).
DHT is the natural androgen [71] with the highest affinity for the androgen receptor [72,73] (AR, often referred to as “DHT receptor”). DHT is formed by a reduction in the ∆4–5 double bond, in the A ring of T, and by the 5α-reductase; there is an additional “backdoor” path of unclear quantitative importance that eludes the direct use of T in the formation of DHT [74]. DHT shows androgenic activity in the absence of T [75]; it is not aromatizable, and consequently, can maintain its function even under conditions of aromatase inhibition [76].
-
○
A4 androstenedione (4-androstenedione, A4).
A4 androstenedione is a mild but important androgen [77]; it binds the AR with low affinity [73]. A4 is formed from DHEA or 17OH-progesterone through 3β hydroxylation [78]. It is the main precursor for the synthesis of T in adrenal cells, testicles and ovaries [77]; in the latter, T is produced this way for many years after menopause [79]. A4 is also oxidized to 17-keto-androstenedione [80], and plays an important role in the KTs metabolism [81].
-
○
AP ∆16–17 androgenic pheromones: androstenone, androstenols.
AP ∆16–17-androgenic pheromones are a peculiar and little-studied group of androgens which do not seem to bind the AR [82]. Their main synthesis pathway is derived from pregnelonone via steroid-17-hydroxylase, 1-20-lyase and a peculiar ∆16–17-desaturase, followed by 3β-dehydrogenation and the action of 5α-reductase [83] to yield a unique group of molecules with a ∆16–17 double bond in the D-ring. This pathway is quite different from the canonic androgen synthesis [84]. Some sort of pheromone-like communication exists, in humans, based on these (and other) compounds, and basically acting in the direction from men to women [85,86,87].
-
○
EA estrogenic androgens (e.g., 5-androstene-3α,17β-diol).
This is a polyphyletic group, characterized by their binding to the ER. However, DHEA and some of its derivatives can also bind the ER [88,89], playing an important role in the function of this ambivalent hormone. In addition, there is a small group of androgens that is structurally related to androsterone (Ane), such as the 5-androstene-diols, that bind the ER, inducing estrogenic effects [90]. It has been postulated, however, that the 5-androstene-diols (3α,17β and 3β,17β) are quite important for the androgen effects on anxiety and cognitive enhancement, which are carried out through the activation of ERβ [91,92]. The 11-Keto androstenedione—the product of the 11β–hydroxylation of Ane—also has estrogenic effects.
-
○
Ane androsterone (5α-androsterone, Ane).
Ane is a catabolite of T and DHT, which does not bind the ER and is a weak androgen itself; however, it is a natural agonist of the FXR (farnesol X receptor), playing a role in the control of bile acid recycling and function [93], and thus, it indirectly acts on the bile acid path of energy metabolism regulation [6]. Ane has been postulated as a neurosteroid, and a mammal pheromone, but the evidence for the latter function is so far inconclusive, at least for humans [94].
-
○
Other androgen metabolism intermediates and excretion molecular species.
This is not a specific function-directed class of androgens, but a mixed bag of intermediate or end-metabolism molecular species. A number of androgen catabolism-derived molecules have been studied as starting bases for the synthesis of (or their possible use as) anabolic drugs [95], but also as markers of androgen metabolism [96]. Most of the intermediate molecular species involved in the synthesis of androgens show mild androgenic effects, but often their possible physiological relevance as androgenic agonists has not been clarified, or even tested. On the other side, the catabolites of T and DHT have received considerable attention because of their varied metabolic effects [97,98], abundance and commercial (probably unjustified) distribution since their physiological significance has not (or perhaps not yet) been sufficiently established.
Only T, A4 and KT (albeit not DHT, but including the T eventually derived from AcT hydrolysis) are substrates for aromatase [99], i.e., they can be directly converted to estrogens: A4 → E1 (estrone); T → E2, KT → 11-keto-E2, with quite different estrogenic effects.
4. Mechanisms of Action of Androgens
4.1. Canonic Androgen Receptor Signaling
The androgen receptor (AR) is a classical nuclear receptor, primarily acting through the selective induction of the translation of DNA strands to eventually synthetize specific proteins. The AR elicits the expression of a number of genes depending on the target cells and the modulation of its signal. In any case, as it corresponds to steroid hormones, the effects of this stimulation are not immediate, but are relatively delayed in time [9]. The AR belongs to a subfamily of steroid hormone receptors closely related to the progesterone receptor, GC and aldosterone receptors (3-ketosteroid receptors) [100], and to a lesser structural but more dynamic relationship with the ER [101]. The AR gene, NR3C4, is in the X chromosome, and contains eight exons, which translate to proteins; the AR acts as a homodimer structure [102,103]. Two main isoforms, A (187 kDa) and B (110 kDa), have been described [104].
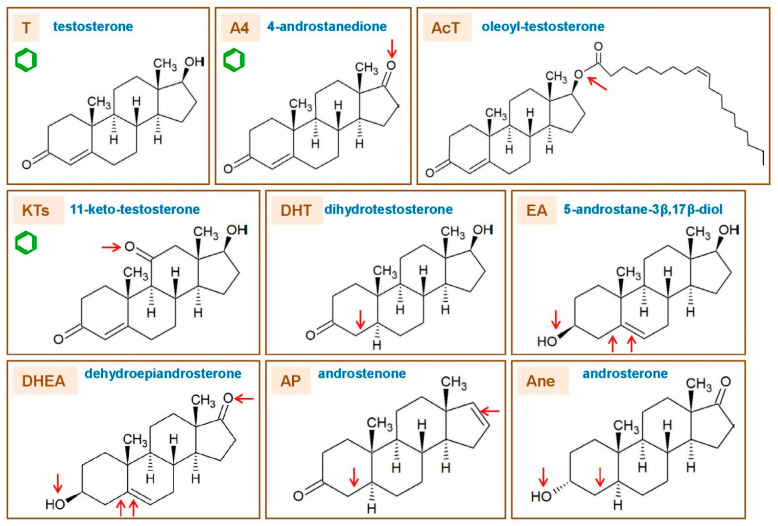
The AR monomer has a lineal structure which contains a small zone of high flexibility, or a hinge (Figure 3), and joins two larger arms; the longer one contains the N-terminal and the DNA-binding domains, and the shorter incorporates the C-terminal domain on the other side of the hinge [105]. The N-terminal section contains poly-Gln and poly-Gly sequences which allow for an additional, highly variable structural modification [106]. Functionally, this section contains the AF1 (activation function 1) active site [107], which binds a number of agonists, affecting the AR function depending on its nature and binding patterns, thus, extending the possibilities of regulative modulation [108,109]. The cysteine-rich DNA-binding domain is where the AR binds to the ARE (selective Androgen Response Elements) sequence of the promoter [110]. In the nucleus, the dimeric AR binds consecutive (duplicate) ARE binding sites, forming a stable AR–ARE (promoter) complex, which then bind to specific DNA sequences [111]. Other enhancer or regulatory proteins (or miRNAs) may bind to this complex of the DNA fiber, further increasing the possibilities of AR regulation [112,113]. Then, the active AR system elicits the translation of tissue-specific genes [114,115].
Figure 3.
Functional structure of the androgen receptor (AR). The diagram shows the two distinct parts of the protein chain, joined at a flexible joint (hinge). The longest arm contains the N-terminal domain, incorporating the AF1 (activation function 1) binding sites, as well as the DNA-binding domain and a short sequence (nuclear localization signal) needed for the nuclear transport of the AR. The shorter arm (C-terminal domain) contains the AF2 (activation function 2) binding site. This domain contains a key binding niche, the LBP (ligand-binding pocket), in the core of AF2.
The DNA-binding domain also contains a short amino acid sequence (nuclear localization signal) which is essential for the recognition by the nuclear membrane, allowing the transfer to the nucleus of the activated AR [116,117]. The hinge domain is also susceptible of modulation by methylation, acetylation or other regulatory processes [118].
In the cytoplasm, the inactive AR molecules are linked to heat-shock protein chaperones [119]. When a suitable ligand binds the AR, these proteins separate from the complex. Then, the ligand-modified AR enters the nucleus crossing the nuclear membrane. In the nucleus, the AR dimer binds the promoter (ARE) and, together with other modulators, finally binds the DNA to express AR-related genes [120]. The C-terminal ligand domain contains the AF2 (activation function 2) active site in a more lipophilic environment than the AF1; this is the binding site of hormone agonists and other ligands [107]. The AF2 contains a particular depression (ligand-binding pocket) which binds the receptor agonists through its fitting anchorage to several specific points [121].
It has been postulated that the main agonist of the AR is DHT [122], and the AR has often been assumed to be essentially a DHT receptor, at least in prostate [123]. The higher (several-fold) binding affinity of DHT for the AR than that of T, A4 and KT [73,100] reinforces this assumption. The high prostatic activity of 5α-reductase suggests a rapid conversion of cytoplasmic T into DHA, which may increase the overall effectiveness of AR signaling, thus, resulting in a stronger response of the translation process [123,124]. However, the multiplicity of agonists, the marked difference—in terms of DHT function—between males and females, and the notable differences between tissues regarding the presence of 5α-reductase [125] and functional ARs [126,127], suggest that this process, described for prostate, could not be fully applicable to the response to T of all androgen-sensitive cells. This is just another example of the extensive ability to modulate the responses to androgens by different organs and tissues.
The AR can be further modulated by the modification of its structure, largely on the AF1 branch, by different agents, which bind or break out portions of domains (such as the SARD, or specific AR degraders) [128]. However, most of the specific binding and modulation of the AR actions are related to the N-terminal arm, which contains diverse binding sites [129,130].
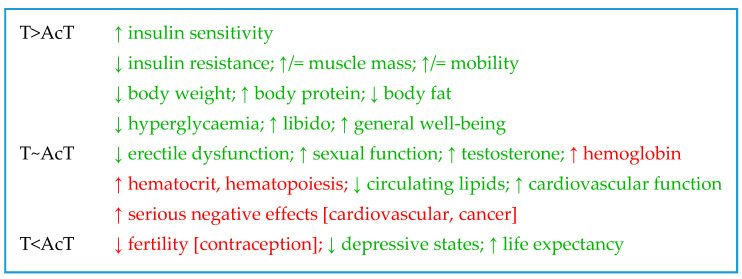
Table 1 presents some of the best-known different functions of androgen classes by showing their effects on concrete specific paths or functions. Thus, physiological T and DHT effects are more marked in men than in women, probably because of their higher production in males, despite also having faster metabolic clearance rates [131]. Obviously, most androgens bind to the AR, but it is unclear whether the AcT can bind the AR on the main specific agonist site; DHEA also binds the ER [52], and the AP binds neither of these receptors [82]. However, the strength of androgens binding to SHBG is maximal for DHT: DHT >> T >> A4 > DHEA [132] (but not DHEAS) [133]. The Sertoli cells synthesize an intra-testicular T binding protein (ABP: androgen-binding protein) [134], a remnant of other less-evolved mammalian T carriers).
Table 1.
Comparison of the physiologic and metabolic effects elicited by the main groups of androgens.
| DHEA | T | AcT | KT | DHT | A4 | AP | |
|---|---|---|---|---|---|---|---|
| Gender influences effects | M~F | M > F | ~ | M~F | M > F | M~F | M > (F) |
| Binds to AR | (+) | ++ | ~ | ++ | +++ | + | (−) |
| Binds to ER | + | − | − | − | − | − | − |
| Binds to SHBG | (+) 1 | + | − | (−) | ++ | − | ~ |
| Male secondary sex effects | − | (+) | ~ | − | +++ | − | − |
| Aromatase substrate in vivo | − | + | − | + | − | + | − |
| Activates sexual development | + | + | (+) | + | + | + | − |
| Increases libido | + F>M | +.M&F | ~ | − | + M | ~ | ~ |
| Enhances muscle mass | − | + | (+) | + | + | − | − |
| Low levels are obesogenic | + M&F | + M | (+) M | ~ | ~ | + M&F | ~ |
| Lowers insulin resistance | + | + | (+) | − | + | − 2 | − |
| Anti-GC effects | ++ | − 3 | ~ | (+) 4 | ~ | ~ | ~ |
| Pheromone effects | − | − | − | − | − | − | + |
Headings: DHEA (dehydroepiandrosterone); T (testosterone); AcT (17-acyl-testosterone esters); KT (11-keto-testosterone); DHT (dihydrotestosterone); A4 (4-androstenedione); AP (androgenic pheromones). The EA (estrogenic androgens), Ane (5-androsterone) and other androgen metabolites—not described in Section 3—have not been included in the table because of their unclear functions and few (and/or) chemically variable molecule representatives. The distinguishing feature for EA, in any case, is their ability to bind to ER and not to AR. Symbols: F = female, M = male (superscript symbols carry the same meaning); ~ = unknown, i.e., no data found/available; + = induces the effect described; − = does not induce the effect described. A symbol between parentheses represents a supposed/hypothetical effect, or an unproven deduction not supported by sufficient (or specific) hard data. Other acronyms; AR (androgen receptor); ER (estrogen receptor); SHBG (sex-hormone binding globulin); GC (glucocorticoid). Cells shadowed in pale green indicate a coincidence in the effects of the marked androgen groups on the same line (i.e., a probably shared effect). The cells with pale brown background show that the given effect is only induced by the marked androgen type (column). Superscript numbers correspond to the notes listed below: 1 This effect corresponds to free DHEA, since DHEAS does not bind SHBG [135]. 2 Insulin resistance is increased in women with PCOS [136,137]. 3 The reverse is true—glucocorticoids tend to antagonize the synthesis and effects of T. 4 The synthesis of 11-keto-androgens from 11OH precursors requires oxidation, whereas the formation of active 11OH-corticosteroids requires reduction (Section 5.2); thus, the synthesis of active functional GC is probably not compatible with that of (also active) 11-keto-androgens.
4.2. Main Non-Canonic Receptor Signaling (AcT, SARM)
The high occurrence of prostate cancer and the implication of the AR signaling in its growth [124,138] resulted in the need to find drugs able to sustain most of the anabolic and protein-protective functions of T because of the limited (or counterproductive) benefits of T deprivation [139,140,141,142]. These efforts resulted in the development of a large number of selective AR modulators (SARM) [143,144]. Most of them bind (albeit in a non-canonical way [145]) the AR (mainly at the AF2), on or close to the ligand-binding pocket [146]. Ideally, they stimulate the AR to increase muscle mass and body protein (consequently, facilitating leanness) [145,147], with limited effects on many of the other functions of T (largely sex-related) [145]. The objective of SARM design was to maintain some of the AR functions, but not completely blocking the prostate androgen-related functions (or to limit excessive prostatic activity) [148]. This mild effect was directly sought for the use of the drugs in the repression of the AR-promoted/sustained prostatic cancer [149]. The SARM can, thus, be considered anabolic drugs, but they are not necessarily steroidal, and are not aromatizable to yield estrogens [150]. The ease with which they may bind the AR over (i.e., not directly on) the core binding site, and exert a number of androgen functions, have been studied [151]; however, so far, it is unclear how the natural androgens may induce the selective modulation of the multiple actions on the AR mediated by T and DHT.
The case of AcT is more complex since they are carried in the blood in small, albeit significant, amounts [61,152], and are stored in adipose tissue [153]. The idea of converting T into a highly lipophilic waxy compound for the storage of a readily usable hormone [60,154] has been found to be partly true by the continued use of synthetic T esters as drugs for long-term androgenic treatments, since they share the structure and binding properties of the AcT described above. In any case, it is generally assumed that to induce androgenic effects, the AcT needs to be first hydrolyzed by esterases to release T. The tight spatial constrictions of the AR AF2 ligand-binding pocket depression on the AR surface limit the possibility of direct binding to this site of the large hydrophobic AcT ester molecules (at least in the way the smaller DHT and T bind) [121].
Alternatively, and following the parallelism with estrogens, acyl-estrogens show marked and distinct effects on metabolism [9,155]. Acyl-E2 are powerful estrogens as such, but acyl-E1 are not [9]. Acyl-E1, however, bind the ER [156], but not on the main ligand site, acting probably as SERM [9], and eliciting a powerful mobilization of stored or dietary lipids [157,158]. These natural estrogen acyl-esters are also found in small but significant amounts in plasma and tissues [159]. The levels of AcT in blood seem to be even lower than those of the estrogenic esters, and are found specifically in the brain [160], testes and adipose tissue [153]. Castration slowly reduces their levels in testicles and adipose tissue to the (already low) levels found in adult females [153]. At least in the brain, the AcT are synthetized by a specific 3β-5-androsterone-hydroxysteroid acyl-transferase [161,162], the main fatty acid used being stearic acid, with lauric acid following in a lower proportion [163]; both natural AcT are seldom—if ever—used in medicine. The sex differences, the specificity of the acyl moiety and that of the acyl-transferase point towards a function related with brain sex-related organization, but unfortunately, we do not have systematic studies on the metabolic effects of natural AcT. A number of short and medium-chain esters of T, as well as modified larger and cyclic acids, are used for prolonged androgenic substitution treatments. The enormously higher doses of AcT used in comparison to the natural AcT do not allow for viable comparisons, but suggest that they may act, at least, along some of the characteristic functions of androgens (i.e., those observed at pharmacological levels) [153]. These actions do not include binding the AR, since their previous hydrolysis to T is required both for oral [164] or injected T esters [165]. However, the different effects on body composition and metabolic environment caused by prolonged treatment of humans with different AcT at pharmacological levels (see Section 7.3) suggest that this is, yet, a dark zone of our knowledge, affecting, precisely, the androgens most widely used in clinical practice.
The possibility that natural, larger androgen-derived molecules could exert the effects elicited by SARMs cannot be ruled out. The parallelism of the action of SERMs and E2 with respect to the ER [9] and that of SARMs on the AR hints to the few and insufficiently studied natural AcT as possible drug candidates, given the relative differences observed between the treatment of low T availability using synthetic AcT as compared to T alone.
4.3. Cell Membrane-Related Androgen Signaling
In line with what can be observed in a number of steroid hormones [166,167], some effects of androgens are too fast to be justified solely by the canonic nuclear hormone mechanism of action described above for the AR [168]. In any case, at present, the most accepted proof of androgenicity is the direct binding of a given molecular species to the AR [169]. This specific aspect of most androgens is by no means an established prerequisite for androgenic signaling, despite their induction of quite a number of physiological responses. As shown below, the non-AR androgenic signaling (usually “rapid” metabolic responses) is widely extended and may be responsible for a wider and deeper spectrum of androgenic action (albeit often complementary) than the canonical path of gene expression control initiated by cytosolic AR activation. There are no data enough to quantify this non-canonic contribution, but the extensive number of studies and results hint to a well-settled series of effects that complement the other “fast” peculiarity of T and its unusually rapid turnover.
There are reports of a close association of AR to plasma membranes [170] as well as to subcellular structures, such as mitochondria [171], a situation somewhat comparable to that observed in estrogens [172]. The nature of membrane androgen signaling is essentially different from that of nuclear receptors [173]. A considerable number of studies have addressed this issue, with a higher focus on four postulated mechanisms:
SHBG-mediated signaling. In this case, SHBG is purportedly used as an anchor for membrane AR androgen binding [174]. SHBG is produced in a number of cell types, containing its receptors in the cell surface [175,176]; they can bind the AR agonists, primarily T [175], but can also bind E2 [177]. After the agonist is bound, the SHBG-receptor-agonist complex is internalized, and then activates a membrane-related adenylate kinase, inducing the production of cAMP [176,178]. A number of effects of androgens have been attributed to these mechanisms [179,180].
Attachment to membrane G-proteins This mechanism is based on the attachment of the AR to membrane G-proteins [170], in a way similar to that of estrogens. The binding of DHT or other agonists to AR in the membrane immediacy may then induce the activation of cytoplasmic protein kinase C, resulting in rapid effects of androgens [181]; in this case the action is also mediated by the AR, albeit not in the nucleus (i.e., not through gene expression).
Implication of ion channels. This possibility relies on the formation of a complex of membrane G-proteins plus the AR and an agonist (as described in the previous alternative); however, this time, this affects the membrane zinc transporters [182] and the calcium channels, increasing the Ca2+ input [183,184]. The rise in calcium can activate the A- or MAP-kinases, inducing fast (and short-term) effects [185,186]. However, MAP-kinase and Ca2+ are also known modulators of gene expression, thus, AR activation may (in addition) indirectly induce genomic actions through this pathway [175].
Activation of cytoplasmic AR near the cell membrane. A possible action on the control of membrane receptor-induced signals may result in binding AR close to the cell membrane (perhaps bound to a G-protein), previously activated by androgenic agonists and binding a tyrosine kinase [186] in healthy and tumor cells. Tyrosine kinase is also a critical modulator of the AR function [187].
This list is neither complete nor exhaustive. The simple direct binding of T/DHA to membrane-related AR has been often described [188,189]. This experimental finding, however, requires that either the signal of the AR bound to an agonist would derive to another (complementary) signal path (e.g., cAMP, Ca2+, phosphorylation of signaling proteins, etc.), or else it would carry the signal all the way to the nucleus. The above list shows plausible published mechanisms, but other alternatives may be found.
A clearly distinct case is that of the androgens which do not bind the AR, since none of the alternatives implying the nuclear receptor may explain their actual mechanism of action. This leaves out the DHEA (in part), AcT, AP and EA types (Figure 2). The case of EA is obvious, since their target is the ER, not the AR, and they are listed here only because of their androgenic origin (but not function) and for the absence of an aromatic A ring, the most differentiating estrogenic structural characteristic.
DHEA (and/or DHEAS) is quite peculiar, since it is basically a promoter hormone [190,191], acting through interactions with multiple hormonal receptors [52,89], with mild androgenic and estrogenic effects [89]. DHEA has a marked anti-glucocorticoid activity [56,57] that, at least in part, may be explained by its structure [192]. Its physiological effects are wide and varied; DHEA is a principal neurosteroid [193,194] which participates in the regulation of neuronal apoptosis [195] and is an antagonist of the GABA A receptor [196]. In addition to its key role in the synthesis of androgens and estrogens, it helps maintain hormonal (and substrate) homeostasis [197], and participates in a number of different functions, such as anti-inflammatory [198], stress control [199] or erythropoiesis [200]. Its high implication in human health and disease [51,201] helps set this hormone away from other mainstay androgens because of its limited classic androgenicity.
In parallel to T, however, DHEA can be made more hydrophobic by esterification with fatty acids in plasma lipoproteins [53], in this case via lecithin: cholesterol acyl-transferase [54]. The possible function of these low concentration steroid derivatives [54] has not been yet clarified.
Probably the most curious mechanism of androgen signaling is that of the AP. Their effects (through chemical signaling) are not exerted on the same organism producing them, but act on other (remote) individuals. The AP have been proposed as human pheromones [202,203] because of their synthesis in the skin [204], volatility and odorous signaling [87,205]. Despite being commercially sold as “sex attractants”, their known effects on other (non-ape) species’ vomeronasal organs [206] have not been fully proven in humans because the presence of this organ is—at most—vestigial [207,208]. Nevertheless, AP receptors in the nasal epithelium have been directly found to signal the close-by hypothalamus [209].
Androgenic pheromones are unrelated to the canonic AR [82]. In many mammals, including primates, the AP may bind protein receptors in the nasal epithelial cell surface, which genes are conserved in humans [210], such as G-proteins [211]. Binding activates ion channel systems, such as the TRP (transient receptor proteins) [212], which activate neural circuits [213]. The receptor-putative pheromone ligands are generally assumed to possibly play a role in this area [214] full of uncertain homologies with other animals, difficult investigation procedures and a limited availability of hard data. The fact that the AP modulate GABA channels [215], the ubiquitous distribution of TRP and a variety of cell AP-binding “receptors”, suggest that AP may play other regulative functions through interpersonal signaling of social or collective situations, such as the transmission of information on food (or sexual) availability [216].
5. The Varied Physiological Functions of Androgens
The described (direct or indirect) interactions of androgens with the normal functions of metabolism and its regulation, both in health and under altered situations, cover practically every possibility for intervention or interaction. The variety of mechanisms described in Section 4.3, and the control of gene expression through the activation of AR, often results in widely different effects. The high number of gene targets may be further modulated by AR responses to the varied different molecular species of androgens, resulting in an exponential continuum of modulatory possibilities. Despite our yet limited knowledge of these variations, there are a few general targets/mechanisms, in which it is generally accepted that androgens intervene, eliciting significant effects by action or restriction.
5.1. Estrogen Synthesis
The androgens are a necessary previous step for the synthesis of active estrogens in sufficient amounts, especially its main representative, E2. Consequently, the actions of estrogens derived from androgen precursors may help explain a growing number of apparently paradoxical or opposed “androgen” effects. It is important to note that T is the main substrate for estrogen synthesis, which is not a reversible process. The metabolic actions of T are in part a consequence of its conversion to E2 [217,218], and low T levels are correlated with increased insulin resistance [219,220]. However, E2 decreases insulin resistance [221] and T, whereby low levels are associated with diminished insulin sensitivity [220], and may elicit an increase in insulin resistance in the WAT of female rats [222]. T also acts on glucose metabolism via aromatization to E2 [223], as explained in depth in a previous review [9]. Furthermore, E2 also exerts critical cell-protecting anti-oxidative effects [35]. On the other side, glucocorticoids increase insulin resistance [224], favoring the deposition of body fat.
5.2. The Complex “Love-Hate” Interactions of Androgens and GC
The androgens and GC families of steroid hormones tend to favor the maintenance of homeostasis; however, they exert their actions using different, complementary (albeit often opposite) processes. In any case, both groups of steroids help maintain energy, substrate and global homeostasis, despite their functional constrictions, by normalizing the consequences of the variability of the nature and availability of substrates. The interaction of androgens with GC needs a further direct and deep study because of often disparate interpretations caused by the unperceived complexity of their continuous interactions.
DHEA is a known (and important) inhibitor of corticosteroid action [57], in part by interfering with the glucocorticoid receptor (GR) function [225], and counteracting the effects of GC [56]. However, the GC decreases the synthesis of T via downregulation of gonadotropins [226], thus, decreasing T-related sex responses [227] and spermatogenesis [228].
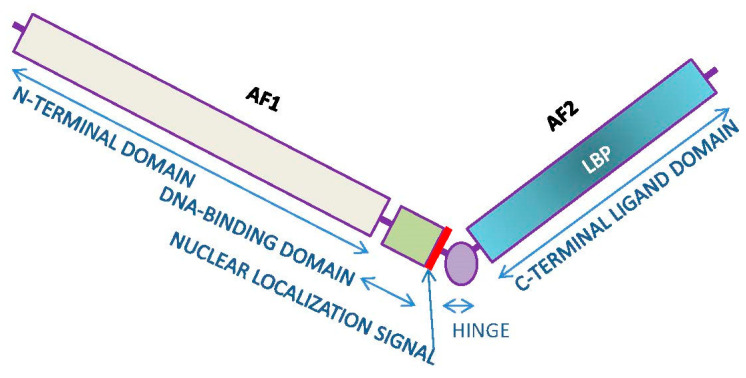
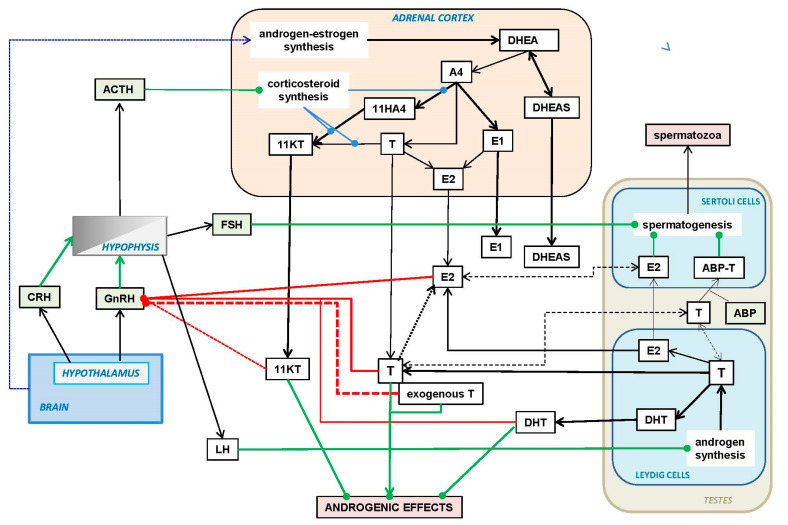
Figure 4 shows the close interrelationship between GC and androgens (and estrogens) in the adrenal glands. The key point is the sharing of a few regulatory enzymes in GC and androgen synthesis/activation pathways, thus, able to inversely enhance (or diminish) the hormonal output of androgens (and estrogens) or GC. Adrenal androgens (i.e., KT) are quantitatively important and are synthesized by adrenal glands and gonads [13,65,66]. At least in women, their main site of production are the adrenal glands [66,229,230], via 11β-hydroxylase [45,231], which also promote the specific synthesis of GC (by oxidizing C11) that characterizes this group of hormones. The interconversion of 11-hydroxy- and 11-keto-androgens is catalyzed by 11β-hydroxysteroid dehydrogenase [232]—again, the same enzyme which interconverts the hydroxyl and keto forms of GC [233], playing a critical role in the regulation of GC activity [234]. Active androgens (such as KTs vs. its less active 11β-OH-T paired molecule [232]) and inactive GC (such as. cortisone vs. its active form. cortisol) are interchanged (and their predominant function—regulated) by the same enzyme, 11β-hydroxysteroid dehydrogenase (11βHSDH), which may determine the predominance of their counteractive regulatory functions on energy partition and protein N maintenance [227], despite collaborative synergy [235] on specific situations such as tissue repair and energy homeostasis [236]. This is due, in part, to GH secretion (activated by GC [237]) and the accrual and preservation of body N by T [238].
Figure 4.
Main shared enzyme activities in the control of glucocorticoid and androgen metabolism in the adrenal gland. Critical role of four key enzymes: aromatase, 5α-reductase, 11β-hydroxylase and 11β-hydroxysteroid dehydrogenase, in the activity and regulation of the main synthesis interrelationships between glucocorticoids, androgens and estrogens. Main glucocorticoids: green-rimmed rectangles (aldosterone: olive green); androgens: dark blue (DHEA: brown) and estrogens: red. The reductive reactions are green arrows, oxidative reactions; red arrows; coenzyme-dependent reversible oxidation-reduction reactions; violet double-pointed arrows (i.e., oxidative or reductive, depending on the tissue redox status). The enzymes are oxidative in red capital letters, reductive in green and equilibrium-oxidation-reductive in violet. Only the four selected key enzymes are listed; those intervening in androgen metabolism have been already described in detail in Figure 1. The actions of enzymes are separately described. The reactions catalyzed have been marked with the color corresponding to the effect elicited: red—oxidation, green—reduction; additional small arrows mark the effects on the product of the overall reaction. Enzyme actions are marked by blue discontinuous lines: aromatase is the point-dash line; 5α-reductase is the dashed line; 11β-hydroxylase is the points line; and 11β-HSDH is the thinner dashed line. Mixed reactions (such as that of aromatase) or actions carried out by non-oxidative-reductive enzymes have been left in black. As explained in the text, the formation of KT and similar compounds are oxidative-activating processes for androgens, but oxidative-inhibiting processes for glucocorticoids. In a reverse way, the action of 5α-reductase enhances the synthesis of DHT and androstenone, but inactivates the oxidized forms of glucocorticoids. Finally, aromatase irreversibly converts A4 or T into estrogens, thus, leaving a narrow (and critically controlled) path for the production of estrogens. In fact, a few key enzymes and a varying metabolic oxidative or reductive ambiance may deeply affect the outcome of the main classes of steroid hormones in a coordinate and partly auto-regulating mechanism.
A critical point is the cross-reverted inhibition due to the predominance of synthesis/degradation of androgens and corticosteroids in their active forms because of the common sharing of 11βHSDH. Overall tissue oxidative drive (i.e., decreased production of NADPH) favors the conversion of the 11-hydroxyl groups to 11-keto (the oxidized form, producing NADPH) of both androgens and corticosteroids. Thus, in oxidative mode, the enzyme–coenzyme system drives, in parallel, an increase in the androgen response (by enhancing KT production) and a decrease in GC activity by lowering the response through the conversion of cortisol or corticosterone to their much less active pairs (cortisone and 11-dihydro-corticosterone), and consuming NADPH to yield NADP+.
A parallel situation of a single enzyme regulating in opposite directions (also shown in Figure 4) is the enhancement of androgen action; the consequent decrease in GC activity is the case of 5α-reductase [239]. This enzyme reduces T (consuming NADPH) to the more powerful DHT (thus, enhancing overall androgenicity), but also acts on cortisol (or corticosterone), reducing them to their inactive catabolites 5α-dihydro-cortisol and 5α-dihydro-corticosterone. The 5α-reductase acts on a larger number of steroid hormones (and drugs), inducing deep shifts in the regulation of the corresponding hormone action. Again, a reductive action of the enzyme, consuming NADPH (i.e., reductive mode), results in the loss of GC activity and a global increase in the ability to stimulate the AR, since DHT has much more affinity for the AR than T.
There are some similarities between the functions of androgens and GC. They are derived, in part, from their common precursor pregnelonone, and they share a fair proportion of the enzymes implied in their synthetic pathways. This likeness of sorts can be seen too in the largely shared structure of their receptors, since they belong to the 3-ketosteroid receptors (3-C) group (which includes the AR, GR, mineralocorticoid receptor and progesterone receptor) [100]. This common structure of receptors is not shared by the ER, or estrogen-related receptors (3-B) group comprising only the ERα, β and γ types [100]. Despite all being nuclear receptors, the structural genetic and regulative differences are not the same, and are largely marked by their physiological agonists. In this case, the main differencing factor may be found in the irreversible phenolic nature of the estrogen A-ring, necessarily affecting the shape of the receptor’s binding site.
The CG are related to the appearance and development of depression [240,241], and androgens are known to lower the severity of this disorder [217]. GC are secreted as a response to stress [240], in which body fat and glucose availability are relatively protected [242,243] at the expense of growth and body protein [244], with the maintenance sustained by androgens [238,245]. Nevertheless, the metabolic effects of KT (and T) share (at least in part) the homeostatic growth-promoting effects of GC, insulin and GH [236]. The protein synthesis-linked anabolic nature of T, KT and DHT [245] contrasts with the drive of GC to favor protein scraping to fuel glucose availability [246,247].
5.3. Modulation of the Immune Response
There is an important implication of androgens in the shaping of the—sex-dependent—immune response [248], which also affects T [249]. Most of these interactions of T inhibit the immune response [250]. However, both androgens and GC protect and enhance specific facets of the immune function [251,252], acting through different paths to enhance protection, despite their mode of action not being coincident but complementary [253,254]. The DHEA inhibition of overall GC action is a part of these finely balanced mechanisms that prevent excess defensive actions in situations where they may be counterproductive.
5.4. Androgens and Reproduction
The implication of androgens in the reproductive process remains, probably, their best-known global function. However, their actions can be further dissected (despite considerable overlapping) in:
The production of spermatozoa. Androgens elicit the production and maturation of spermatozoa through the activation of the testicle Sertoli cells [255,256,257] and their incorporation to the seminal fluid. The use of large doses (and extended treatments) of T, AcT or DHT (but also E2) partially block the action of FSH [255]. Both FSH and testosterone are needed to produce viable spermatozoa [255,258]; the alteration of this delicate process often destabilizes spermatogenesis, resulting in sterility [259].
The development of male sexual secondary characteristics. The male secondary sex characteristics are typically induced by T [230], but are generally attributed to DHT [260,261] (rather than T, which obviously also induces them [262]), because of the higher response elicited by DHT, which seem final for this purpose in comparison with the T intervention in a wide panoply of functions and paths. T seems to stimulate the defining characteristics of “maleness”, at least in part, via its conversion by 5α-reductase to DHT [263], where isozymes are considered to be responsible for most of the male-defining physical and behavioral characteristics [264]. The genetic absence of 5α-reductase isoforms may even result in individuals arriving to adolescence with a full female phenotype. However, in many cases, they become fully fertile men with male behavioral orientation, albeit they are initially devoid of secondary male sex characteristics; they often recover/develop the necessary functional and anatomical structures to allow successful mating [265] and impregnation. Nevertheless, sexual development is probably induced by a full collaborative effort of most types of androgens (except AP, AE, and probably natural AcT), and requires the presence of E2 in addition to T and/or DHT [266]; this conjoint action includes successful spermatogenesis [267].
Interpersonal communication and signaling. This is a process in which intervene the AP, sex-specific pheromone [85,87]. Some of these compounds display neurosteroid functions [215], but they mostly have been related to inter-individual communication as pheromones [87,202,268] and/or odorous markers [205]. They are produced by and secreted from skin apocrine glands and other organs such as the brain, adrenals, ovaries and testes [83,215], and have been detected in circulating boar plasma [269].
The focussing of brain structure/function (and behavior) towards reproduction. This includes extensive behavioral and social energy (and time) investments [270,271]. T is necessary for mating and the maintenance of a sexual/affective relationship for both sexes [272]. T activates mating relationships [273] through complex mechanisms in which cortisol [274] and reward systems, such as endorphins [275] and oxytocin [276], play important roles. The settling of durable relationships result in a decrease in T [277] and increase in oxytocin [278,279] levels in males. This change may be, in part, justified by the need to temper the aggressiveness and dominance drive elicited by high testosterone [280] or DHT. The varied effects of DHEA [281], T and DHT on sexual drive are well known, but DHEA effects are more extensive in females than in males [282], and those of DHT are practically circumscribed to men due to the direct relationship of DHT with male secondary sex characteristics. In women, DHT levels are normally low [283], rising only in some pathologies [284] and provoking serious metabolic complications in animal models when administered (i.e., PCOS [285]). Consequently, the activation and maintenance of libido is largely centered on T, for both men [286] and women [287]. The implication of KTs in these sex-related processes has not yet been clarified, but we can hypothesize that they may not be critical on this issue, since the highest circulating levels of KTs are found in childhood (in both sexes), i.e., before sexual maturity. In any case, the effects of T on the libido of women correlate with T administration/levels [288] (as in males), irrespective of their already higher and maintained KT levels [289].
The potentiation of growth and development. This is achieved through gender-related differentiation; this is especially marked on the effects induced on brain organization [290,291], behavior [270,292] and fulfillment of the biological male phenotype [293]. The effects may be quite different with DHEA, which neurosteroid nature [194] and diverse brain effects range from behavior (i.e., aggression [294] or mood [281]) to cognition [281,295]. There is scant information on the possible effects of DHT on the nervous system, but in the brain, T reduction to DHT has been described [296]. Similarly, the known role of KTs on fish neural development has not yet been observed (albeit it is hinted to [297]) in humans.
The accrual, maintenance and regulation of body (i.e., muscle) protein. Androgens play a critical participation in the regulation of body protein content (including, especially, muscle mass and distribution) [245]. The marked decay of testosterone availability with senescence [298] lowers muscle mass and function [299] down to sarcopenia [300]. The consequences are compounded by the limitation of estrogen production because of insufficient T. The use of T as senolytic helps limit the consequences of this deficiency [301,302]. Androgens are commonly used as drugs for the development, growth and maintenance of body protein, especially muscle mass [245,303]. This is a complex process in which other hormones intervene, such as insulin [304], growth hormones [305] and estrogens [306], and is dependent on the adequate supply of dietary energy and protein. The main androgen agents favoring body protein accrual and maintenance are KTs, T and DHT; the intervention of AcT is also probable because of their unique natural long half-life, but no specific information is available on their effects under physiological conditions. However, there is considerable evidence of the protein sparing/mass-enhancing effects of long-term TRT (T replacement therapy) [307,308], including their use for the treatment of sarcopenia [309,310]. Furthermore, the abuse of AcT as anabolic agents for sport doping, or body muscular build-up (i.e., often for non-health-related purposes) has shown that their overuse indeed results in an exacerbated growth of muscle mass [311,312] partly at the expense of body fat [313]. Their use may also result in the development of dependence [314]; often inducing severe cardiovascular, behavioral and reproductive disorders too [315].
Energy partition and handling. Androgens are directly implicated in the mechanisms of energy partition and utilization for metabolic function. They participate in the intertwined regulation of energy metabolism with estrogens and other regulatory hormones, such as GH [305,316], insulin [317,318], calciferols [319] and cytokines such as leptin [317], but also favoring an anti-inflammatory vs. inflammatory cytokine distribution [320]. These actions have been essentially described for T and KT, but can also be elicited by AcT-based TRT [321]. Hypoandrogenism is correlated with obesity [322] and it is one of the key MS disorders (and markers) [323]. Consequently, the “recovery” of androgen levels (lost to age and/or MS) may be expected to favor the shedding of excess body fat. In fact, treatments using T decrease adiposity [324,325,326]. However, longer treatments with exogenous AcT may reduce body fat, but not massively [327,328,329,330]. Some estrogens (such as E2 and acyl-E1) are known to lower body fat [9], and hypoandrogenism results in the insufficient availability/circulation of E2 [331] because the lack of T deprives the process of aromatization to E2 of its main substrate. It can be assumed that the “adipolytic” effect of T is probably (or, potentially, mainly) a consequence of the restitution to normalcy of E2 levels [9] elicited by the T administration. Thus, only aromatizable androgens may be expected to significantly influence body fat when used for substitutive androgenization treatments. A low T is correlated with lower insulin sensitivity in men [332,333]; insulin resistance does not affect T but the reverse is true [219], since T lowers insulin resistance [220], and helps maintain glycaemia [334,335]. DHEA also decrease insulin resistance [336,337]. However, DHT (in men) has been found to increase insulin sensitivity [317,338]. The effects on insulin sensitivity/resistance induced by long-term pharmacological treatment with T and AcT are presented and discussed in Section 7.2. Effects on insulin resistance/sensitivity were observed both using T- [325,335,339] and AcT-based [329,330,340] TRTs.
This list, evidently, shows the existence of a large number of redundant, or even contradictory actions, but when compared with the chemical-functional groups described in Figure 2, a clear trend can be established between molecular structures and the general functions of the different androgen classes.
6. Regulation of Testosterone Synthesis and Availability
6.1. Hypothalamus–Hypophysis Axis Regulation of Androgens
In humans and other primates, the main androgens (i.e., DHT, T and KT) and estrogen (E2) are partially transported in blood by SHBG [133,341] instead of ABP (regulation not shown in Figure 5), but also by albumin and other proteins [342]. SHBG is a complex protein, with multiple functional forms, whereby the affinity for hormones is regulated in part via proteolysis [343], or the binding of non-steroidal ligands [344]. The transporting role is complemented by its function in signal transduction, or as a marker-transductor of other metabolic-regulation functions such as those described in Section 4.3 in relation to androgen signaling.
Figure 5.
Regulation of the androgen (and estrogen) synthesis by the adrenal cortex and testes. Abbreviations: GnRH: gonadotropin-releasing hormone; CRH: corticotropin-releasing hormone; ACTH: corticotropin; (gonadotropins) FSH: follicle-stimulating hormone; LH: luteotropic hormone; E1: estrone; E2: 3,17β-estradiol; ABP: androgen-binding protein. The other abbreviations have been described in Figure 2. The solid black arrows show paths or relationships. The dotted black line depicts the brain modulation of steroid hormone synthesis by the brain through other additional means (i.e., nervous signals and non-steroidal hormones). The dashed black lines indicate the possibility of direct interchange of pools between tissue and blood. The green lines show stimulatory/activating effects, and the red lines inhibitory/deactivating effects. The effects of exogenous T (i.e., administered as a drug) on GnRH functions overall have been presented as a red dashed line to somehow differentiate it from the tissue-released T.
The circulating levels of T, E2, KT and DHT modulate the pulse secretion of GnRH (gonadotropin-releasing hormone) from the hypothalamus [345,346,347] directly into the hypophysis portal vein system [348], despite GnRH regulatory effects extending to other organs of the HHG (hypothalamus–hypophysis–gonads) axis [349]. The hypothalamus also releases the antithetic hormone GnIH (gonadotropin-inhibitory hormone), which inhibits the secretion of hypothalamic gonadotropins [350]. Prolactin also inhibits GnRH action by lowering gonadotropin secretion [351].
An even more complex and physiologically important mechanism to control the release in gonadotropins (in addition to direct neural/neurochemical signaling) is the effect of glucocorticoids, such as cortisol as blockers of the hypophysis response to GnRH [352] in part through the regulation of its gene expression [353]. This effect, complemented by the direct action of glucocorticoids inhibiting testicular functions [354], completes the link between stress and metabolic strife with the modulation of androgen–estrogen availability and the reproductive function.
This strong controlling relationship between glucocorticoids and androgens/estrogens is critically centered in the adrenal cortex (as explained in Section 5.2), thus, the shared (but opposite) adrenal control of corticosteroids and androgens also has a brain connection, or an additional control node, in the hypothalamus. CRH (corticotropin-releasing hormone) is secreted from the hypothalamus following the direct portal vein path to the hypophysis, but along an even more complex circuit than that of GnRH [355]. CRH elicits the release of ACTH (corticotropin or adrenocorticotropic hormone) by the hypophysis. The process is controlled by a feedback loop based on blood glucocorticoid levels [356], parallel to that described for T and LH. ACTH is the main hormone controlling the synthesis of corticosteroids in the adrenal glands, but we lack information on whether ACTH also regulates the adrenal production of androgens (and consequently, of estrogens).
Figure 5 presents a general view of the main system controlling the circulating levels of T (and in general, of the principal androgens). T is mainly synthesized by the Leydig cells of the testes [357], but also by the prostate, epididymis, ovary and adrenal glands [358,359,360]. DHT is produced largely (albeit not exclusively) in the testes and annex structures, and the KT in the testes and adrenal glands [44]. Part of the T is transported, within the testes, by a specific T-carrier protein, ABP (androgen-binding protein) [361]. This protein, excreted by the Sertoli cells [362], is found in humans almost exclusively in the testes (it is also expressed in cardiomyocytes [363]), but is a common (main, because of the absence—or almost—of SHBG [364]) steroid hormone-transporting protein in many other animal species [364,365]; the family of ABP-transporters is subjected to a considerable evolutionary pressure [365]. ABP binds T with high affinity [366], and helps maintain the availability of T to allow spermatogenesis in the Sertoli cells [367,368] even under conditions of low T availability.
The posterior lobe of hypophysis responds to the GnRH stimuli by increasing the production (and release to systemic blood) of gonadotropins: LH (luteotropic hormone) and FSH (follicle-stimulating hormone). These hormones play a key role in the regulation of the ovarian cycle in females, but also control, respectively, the testicular synthesis of androgens in Leydig cells [357] and spermatogenesis by the Sertoli cells [258], the latter with the necessary intervention of T [367] and E2 [267]. LH secretion is the direct mechanism for the activation of gonadal steroidogenesis, modulated by progesterone [369] and cortisol [352], but mainly through essential direct feedback regulation by T, E2 and DHT [370]. Spermatogenesis is a more complex issue, and the factors which regulate the process are multiple and intertwined [371,372], including local additional regulative processes in the testes [373].
6.2. Hormone Availability, Interactions and Turnover
The control of T levels (and those of DHT, and largely, E2) is dependent on the balance between the synthesis of T and its (hepatic-intestinal) inactivation [374,375]. However, it also depends on its irreversible conversion to other androgens (DHT, KT) or aromatization to E2, since none of these processes could compensate the loss of T. Thus, in an adult male, the turnover of (mainly) testes-derived T needs to be fairly high [376], with a T production in the range of mg/day. This large amount of T is needed to accomplish most of the functions described above; consequently, the incapacity to meet these needs results in hypoandrogenism/hypogonadism [377]. The insufficient supply of T (and E2) affects Sertoli cell spermatogenesis [378], eliciting a lower mass and functionality of testes [379,380]. However, this also results in negative feedback on the Leydig cells, producing even less androgen, and consequently, aggravating the hypoandrogenic situation. The initial cause of low T availability may be either a failure of the testicle to produce T—because of a hormonal, developmental or toxic disorder. But it may be due to an insufficient response/production of gonadotropins, mainly LH [381], or a lower effectiveness of LH, enough to stimulate the synthesis and release of T [382]). It is possible, too, that the progressive decrease in T along maturity and old age in men [383,384], aggravated in MS [385,386,387], may contribute significantly to this snowballing of metabolic disorders caused by the loss of available T.
Substitutive treatment of hypotestosteronemia may help improve the situation by adding an exogenous source of T (if what is given is indeed T) to limit or reverse the fall in circulating T. However, in biology, things seldom are so simple and direct. Theoretically, giving T as a drug helps sustain its circulating levels, but its maintenance along time may make redundant the natural HHG regulation of its synthesis, affecting, this way, the critical function of producing spermatozoa for reproduction [388]. The pharmacologically increased T will probably inhibit the secretion of GnRH and gonadotropins, at least on a system in which the low T levels should (and could) activate the eventual higher production of GnRH—and then LH—to enhance the natural synthesis of T. A relatively short androgenic drug treatment may allow for the ulterior recovery of testicular function [389], but excessively long-term treatments may induce more severe and enduring damage to the HHG axis regulation, affecting fertility and even inducing sterility [390,391]. Thus, it is critical to keep in mind the need to reach equilibrium between preserving regulatory and testicular functions and the need to provide exogenous T to fuel them, including the “recovery” of the full operability of the testes themselves. The administration of T for relatively short periods should result in the maintenance of circulating T (also for short periods), but the partially preserved feedback loop could hopefully induce a decrease in gonadotropin secretion, thus, further limiting the falsely “unnecessary” (because of the feedback inhibitory signals of the exogenous T) internal production of T. Nevertheless, the inclusion of regular HHG-activating “interludes with no-exogenous-T” along the treatment may force the HHG axis to step in to cover for the withdrawal of exogenous T. This way, the system should be forced (if operative) to reactivate gonadotropin stimulation. This reset induced by the “rest” periods of treatment has two theoretical advantages: a) reinstate the natural regulation of T levels to a body being adapted to higher T availability and b) to prevent further (possibly long-lasting) damage to the whole regulatory system. Despite the endogenous T production being probably insufficient, at least the regulatory mechanisms may be maintained, and a new period of exogenous T may help to increasingly restore the so far poorly active endogenous T synthesis and regulation system. The possibilities of the feed-back procedure to restore the functional HHG axis regulation are, in any case, better than those of an uninterrupted full-extended long pharmacological TRT. This approach has the advantage of maintaining spermatogenesis due to the high affinity of ABP for T, which seems to help spermatogenesis to function even under fairly low circulating levels of T [392].
There is probably a parallelism between the male hypoandrogenism of maturity and the female “hyperandrogenism” conditions of POCS (polycystic ovarian syndrome) and post-menopause. In women, the critical hormone classically insufficiently affects E2 mainly, a main factor responsible of the efficient control of energy metabolism and reproduction. There are at least four important converging processes justifying the E2 deficit: (a) the lower relative availability of T, especially in the ovary after menopause [393,394]; (b) insufficient channeling of A4 to T (and then to E2) in the adrenal glands of POCS patients [395], showing higher A4 and E1 levels in the glands and plasma [396]; (c) decreased aromatase function induced (in POCS) by FSH in adrenal gland granulosa cells [397]; (d) acute interference of glucocorticoids over FSH in granulosa cells affecting aromatase [398]. The combined result is a global decrease in aromatase activity, and the predominance of A4 over T as key androgen in adrenal glands (and in part in the blood). In some way, compounding: (a) the limitation of DHEA availability, (b) the probable setting of adrenal glands in a “glucocorticoid” mode (high CG/low androgen) and (c) the limited capability of the ovary to produce enough T. In these two quite different metabolic situations, the result is a lower aromatase activity on T → E2, but is displaced to produce a relative excess of E1 from A4. The conversion of E1 to E2 is problematic, and E1 could not substitute E2 in most of its functions. One of the consequences of this adrenal disarray is the accumulation of unused A4, despite lower synthesis. The loss of endocrine ovary functions could not be substituted by the adrenal glands with respect to estrogen synthesis (more E2 is needed, not E1) in a way comparable to the lower testicular endocrine activity that could not either be fully compensated in many critical functions by the adrenal cortex.
7. Current Pharmacological Utilization of Androgens
7.1. The First Studies: T as Senolytic/Energizer
Even before the full hormonal nature and discovery of T were established, preparations (“extracts”) from animals’ testicles were used [399] as a possible treatment for the loss of sexual vigor, muscle power, clarity of mind and many other functions already attributed to youth via fully functional testes [400]. The earlier studies—including experimental self-administration of testicular preparations, with tens of thousands of elders expecting “rejuvenation” [401]—used ill-defined and aleatory “extracts” from pigs, bulls, monkeys, rats and a long list of unfortunate suppliers [402] (including human cadavers). Evidently, there were no adequate controls (and the identity of the wonder agent was unknown), but the rapid (and short-lived) “miraculous” effects were highly publicized and avidly followed [403]. Intents to rationalize the studies, and the surge of medium-term serious sequelae (immunity reactions, rapid loss of effectivity, severe complications, erratic availability of sources, social squealing, etc.), terminated this first bout of exploration. In any case, the seed of this line of work continued to grow, arriving at the purification of T [404] shortly afterwards. The next step—necessary to supply the growing demand of T—was its complete synthesis [405]. Additionally, from then on, its generalized use (despite not being universally available) started with two main applications: senolytic (anti-aging/gerontology, but also sexual enhancer) and anabolic (bodybuilding/sport-doping), which continue to be developed at present.
7.2. The Practical Difficulties of Oral Administration of T
The main problem that poses the direct oral use of T is its rapid first-pass inactivation by the liver [374]. Most steroid hormones (including T) are well absorbed from the intestine aqueous medium [406]. Intestinal cells and microbiota may modify the steroid molecules, as is the case of bile salts, by breaking them up, freeing the bile acids and/or modifying their molecular structure. This process may be important for the use of AcT by releasing free T (which may be further modified and/or absorbed [407]). The intestinal T is carried in part via lymph [408], but most of it is essentially transported by the blood to the liver via a portal vein. There, T is massively inactivated in the first pass [406,409], yielding oxidized derivatives [410] and/or esterified to T-glucuronate [411] since these compounds are mostly inactive and excreted [406]. Therefore, only a small part of oral T can reach (intact) the systemic circulation from the hepatic venous efflux and lymph (and thus, able to reach the brain, muscle, testes and other organs and tissues), because most of the ingested T had been previously inactivated. The interactions of T with the gut and its microbiota follow a crossed regulatory system akin to that found between the microbiota and other regulatory axes [412].
The T produced in one day by adult humans amounts to 7–8 mg in men, and about 0.5 mg in women [131,376,413,414,415]; this is a fairly high figure for a hormone that has a fast turnover, in the range of minutes [416]. However, its direct (mainly gonadal) secretion into the systemic bloodstream helps circumvent the hepatic portal system trap.
The adrenal cortex production of KTs again eludes the direct first-pass through the liver, but we lack sufficient information on the disposal of this important source of mainstream androgens. To limit the problems of hepatic inactivation, pharmacological procedures for the application of T were initially explored and developed [321,417]: (A) The direct deep intramuscular injection of T was dissolved in an oily excipient to create a tissue-embedded depot of T, which was expected to slowly release the hormone [418]; (B) The oral administration of T, in which the C17 hydroxyl group was esterified with organic acids (i.e., AcT) [419], and thus, was in part transported via lymph (because of the added hydrophobicity [408]), therefore, limiting the liver inactivation because the only T hydroxyl group was already “occupied” by a lipophilic acid, and thus, could not be glucuronized. Consequently, a fair number of T 17-hydroxy esters were synthesized [417]. However, some T was released by the action of intestinal esterases on these AcT, and the free T was then subjected to the same problem: hepatic first pass losses, as free oral T did [420]; (C) These same T esters were also injected into tissues dissolved in lipophilic carriers, mainly for medium- or long-term depot treatments. The length and nature of the esterifying acid affected its lipophilia and the estimated resistance to esterase action, being used to adjust the supply of T in clinical applications [59,321,417]; (D) Maintaining T as a main molecule and supplying it using repeated trans-dermal procedures, such as the use of hydro-alcoholic gels [421], skin sprays [421] or patches of varying releasing potency, efficiency and distribution [422], slow-releasing T pellets [423], silicone implants [424] or subcutaneous injections [425]. This last approach also circumvents the initial passage through the liver, since the T (or AcT) was absorbed slowly over large surfaces and not through the gut–liver system. Initial studies specifically used testicular patches [426], but the incommodity of their use made this galenic preparation fairly unpopular; (E) Buccal adhesives, oral tablets [427] and other trans-mucosal approaches [321].
Overall, many of these procedures were not well tolerated by the patients because of the long treatment periods and the uncomfortable and frequent application procedures.
7.3. The Widely Extended Use of T Acyl-Esters in the Treatment of Hypoandrogenism in Men
A considerable number of pharmacological preparations for the administration of T have been developed [321,417]. In addition to the use of free T, a large part of the TRTs rely in the modification of T by esterification (i.e., producing androgen drugs structurally akin to AcT) using [428] short, branched, odd-carbon, unsaturated or cyclic fatty acids. The products were designed to limit the hydrolysis of the ester bond (in fact acquiring a better control of the release timing) and were assumed to liberate T lineally over time. In addition, the esterification provides more stability to the drug, because it prevents glucuronization and limits oxidation, thus, extending the effectiveness of the “T pharmacological preparation” over time.
The main T esters used in TRT (or as anabolic drugs) are, nowadays, largely centered on T undecanoate [429,430,431], but also include propionate [432,433,434,435], isobutyrate [436], oleate—a natural AcT—[437], enanthate [438,439,440], undecenoate [441], cypionate [442], butyryl-cyclocarbonate [443], phenyl-propionate and decanoate [444]. Gradual-release T ester blends are also used to obtain extended time-uniform T release patterns, as is the case of Sustanon 250 [445,446] (a mixture of T propionate, isocaproate, phenyl-propionate and decanoate).
The direct deep i.m. injection of T or T esters (usually dissolved in edible oil—triacyl-glycerols (TAG)—or a similar, neutral, slowly dissolved hydrophobic metabolizable vehicle, is at present, probably the method most often used for the administration of androgens [447]. The intramuscular lipid blob is slowly disintegrated via phagocyte or tissue extracellular lipases/esterases, which hydrolyze the excipient acyl-glycerols and the T esters, yielding T, fatty acids and glycerol. However, its pathogenic persistence may occur [448]. The presence of acyl-steroid esterases in many tissues [63], including liver, intestine (and the microbiota), may liberate T from its orally ingested esters. A large part of oral testosterone undecanoate is hydrolyzed to T just in the intestinal wall [420], and then it is freely absorbed and distributed at least in a small significant part via lymph [408]. The enzymatic dissolution of the oily TAG deposit excipient exposes the AcT, which are then in part carried by the blood and may act as a natural AcT—this is a question that so far has not been sufficiently studied. It is generally assumed that the released AcT are rapidly hydrolyzed by tissue or cell esterases (probably including unspecific sterol-esterases). The result is a more or less steady flow of T from the injection site to the systemic circulation [449]. The injection methods have the advantage of easy administration, needing only a few applications per year to maintain a theoretically regular and fairly stable flow of androgen to the blood [449]. On the negative side, the volume of the injected preparation may induce a local focus of disturbance affecting the surrounding tissue and blood vessels. Nevertheless, the main direct problem caused by this method of administration is probably its relative irreversibility. After injection, the drug will keep being released from its depot for a long time at an expected estimated (albeit diminishing) rate, dependent on the mass of AcT remaining in the injection site, a process that could not be stopped.
The (usually) daily transdermal administration of T using patches [450,451] or the extension of hydro-alcoholic gels over bare skin [452,453] have the advantage of relative immediacy, and the possibility to control the time of exposure to the hormone [454]. Its main problems are the cumbersome procedure of extension (gel) or the limited area of application (patches). There is an added difficulty using this approach: the estimation of the dose actually received by the patient, since only a fraction of the T is in contact with the skin, is eventually absorbed and carried by the systemic circulation [455]. Furthermore, the dose may be further diminished because the skin can metabolize T to produce DHT and other androgens (such as AP); thus, repeated application (direct exposure) may result in local unwanted effects on the skin and the integumentary system [456]. In the case of gels, care must be taken for (unexpected) delayed T transfer to other individuals’ skin or mucosae through direct contact with T-loaded skin [457]. In any case, a clear advantage of the use of gels is the easy way to stop the treatment: simply washing out the hormone not yet absorbed.
A number of other approaches to an efficient, safe (and comfortable) method of administration of T have been postulated and commercialized [451]: subcutaneous pellets [423], nasal gel or other applications [458,459], buccal tablets [460], subcutaneous injections [425], new oral preparations [427], combined transdermal and injected T [461], etc. In all cases, we encounter the same inactivation barrier problems (liver, digestive tract), and/or the difficulties of assessing concrete and precise doses of T for defined periods of time. An important factor is the easiness and comfortability of the administration, and the compliance of the patients during the often very long periods of treatment (including the danger of overdosing because of the time needed to achieve the expected results).
Last, but not least, most “testosterone” drug preparations are indeed AcT. However, T and AcT are different androgen types, and in most cases, we do not know yet whether their physiological and pharmacological effects are equivalent. In fact, we have reasons to believe they are not, based on the data and analysis of their different effects presented in Section 7.4 and Section 7.5.
The use of synthetic androgens, SARMs and the massive utilization of some of the T ester-based drugs derived from the initial use of senolytics and muscle-building to an extensive indiscriminate use, more often than not unjustified for addictive, body-building objectives, including an inaccurate understanding of what maleness is, means and is manifested; this is precisely based on their more socially undesirable aggressive facets. Androgenic treatments may cause functional problems, but there is not a clear similitude or continuity between the effects of even long-term TRT without medically advised anabolic use [462,463]. These drugs have been intensely studied, developed and often used without safe knowledge. Unfortunately, this situation continues and keeps expanding.
There are few doubts about the danger the use of anabolizers may carry for the cardiovascular system [464,465] and the brain [466], including behavioral and psychiatric disorders [467], but also extreme musculation, metabolically distorting bodybuilding [313], and obviously, alterations of the sexual (and reproductive) functions [468,469]. The extended lack of differentiation between androgen classes may be, in part, a justification for the confuse hoarding of all androgens in a single group of anabolic hormones (or anabolic drugs). However, anabolizers could not be easily equaled to the natural hormones, at least in their function-effects at the doses and paths of administration used, but especially with respect to hormonal regulation and a number of essential biochemical pathways that are alien to the most used drugs. Nevertheless, not all is negative, since some androgen-derived or related anabolic drugs (including SARMS), represent a fully productive pharmacological line, to treat common senile- or malnutrition-derived disorders, such as sarcopenia and cachexia [470], which continues to be developed at present.
7.4. Justification, Expectations and Variability of Long-Term “Testosterone” Treatments
The main focus of the initial TRT was largely to restore hormonal functionality of adolescents (and adults) with endocrine or reproductive disorders [471], but it was extended (often out of the clinical milieu) to “return” the libido and youth memories of sexual functionality to old men [472]. The prevention or correction of sarcopenia is an important application that is also being actively developed [301]. The use of T in the maintenance of physical health and psychological well-being came in later (despite being just the core of the pioneer experiments), and remains the most common reason exposed for their extended (and often uncontrolled) use [473,474,475]. However, the question over the effects of TRT on depression [476,477] is not closed, despite being an issue that is probably deeply influenced by the methodology and characteristics of the treatment and its high social impact, aggravated by our not yet sufficient understanding of the biochemical basis of depression.
Most of the substitutive hormonal treatments using androgens have been carried out without a sufficient knowledge of what androgens are and what they can do. This is especially applicable to the properties of the molecular species used, the duration of treatment and effects on natural T and other hormone functions, and their conjoint regulation. An example of this attitude is the extended confusion between T and AcT formulations, in a large part of the clinical literature, which assume unabashedly that all T-containing (free or esterified) pharmaceutical preparations used for TRT are simply galenic-equivalent vectors of T. This opinion is widely shared, and many of the meta-analyses, reviews and position papers on TRT compare results and conclusions but do not discriminate (or, even describe [478,479]) which specific molecular species, and/or via for their administration, induce the differential results observed [463,474,480,481,482]. In a few studies, however, the dose was modulated according to partial results, thus, helping prevent further complications [483].
Nevertheless, most studies and reviews on TRT show similar effects (largely those presented in Table 2), and are also favorable to the use of TRT in men, hypoandrogenic because of their age or other metabolic disorders. The idea behind the use of AcT instead of T (described in Section 7.3) is to facilitate and increase the regularity of treatments. However, this use of AcT does not take into account that T is not the “only” important androgen in the (male) body. The sizeable production of KT’s, the higher AR-binding capacity of DHT and the short half-life of T in plasma are factors essentially ignored in most of the clinically-oriented literature. Similarly, the androgenic environment modulation of patients under TRT is essentially unknown because of the generalized absence of markers, molecular comparisons of gene activation, binding, transport and disposal of the androgens given. Any comparison with the effects on endogenous androgens T, KT and DHT (but also including E2) is again absent. Unfortunately, most of the comparative studies on androgenization as a medical treatment seldom consider these questions, and neither check the comparative potency, toxicity, disposal and spectrum of metabolic effects of the “testosterone” drugs used.
Table 2.
Main effects on men of prolonged “testosterone” replacement treatments using either T or AcT.
|
Main Effects
Observed |
↑
Testosterone |
↑
Glycaemia |
↓
Insulin Resistance |
↑
Insulin Sensitivity |
↓
Body Weight |
↓
Body Fat |
↑
Ipid Oxidation |
↓
Circulating Lipids |
↑
Body Protein |
↑=
Muscle-Mass |
↑=
Mobility |
↑
Cardiovascular Function |
↓
Liver Steatosis |
|
| H | V | T | GLUCOSE | LIPIDS | PROTEIN | SYSTEMS | ||||||||
| T | Tr | [335,339,474,497,498,499,500] | [325,335,339,501] | [325,335,339,501] | [325,335,339] | [325,497] | [324,325,326,497,498,499,502,503] | [110] | [325,335,501,504,505] | [339,497,498] | [479,499,500] | [497,502] | [506,507,508,509,510] | |
| Inj | [388,511,512] | [318] | [318] | [318,512] | [512] | |||||||||
| Or | [513] | |||||||||||||
| TU | Tr | [514] | ||||||||||||
| Inj | [327,494,514,515,516,517,518,519,520,521,522,523] | [328,340,475,514,515,516,524] | [340,515,522] | [329,330,340] | [328,516,517,519,521,522,524,525] | [327,328,329,330,475,516,517,523] | [31,327,328,475,514,515,516,519,524] | [524,526] | [517,523] | |||||
| Or | [523] | [527,528] | ||||||||||||
| TE | Inj | [529,530,531,532] | [533] | [533] | [520,533] | [529,531] | [534,535] | [307,532,536] | [537] | [509,538] | ||||
| TC | Inj | [509,538,539] | ||||||||||||
| UN | ND | [540] | [540,541] | [540,541] | [540,541] | [540,542] | [482] | [463,478,479,541] | ||||||
| Tr | [317,543] | [514] | [317] | [544] | ||||||||||
| Inj | [525,533,545,546] | [339,525,547] | [339,525] | [492,522,525] | [525,526,548] | [328,525] | [549] | [329,515,539,550,551,552,553] | ||||||
| Or | [554] | [528] | ||||||||||||
|
Main Effects
Observed |
↑=
Bone Function |
↑
Kidney Function |
↓
Erectile Ysfunction |
↑
Sexual Function |
↑
Libido |
↓
Fertility Contraception |
↑
Life Expectancy |
↓
Depressive States |
↑
General Well-Being |
↑
Sleep Time |
↑
Hemoglobin |
↑
Hematocrit Hematopoiesis |
↑
Serious Negative Effects |
|
| H | V | SYSTEMS | REPRODUCTIVE | LIFE AND BEHAVIOR | BLOOD | NEGATIVE | ||||||||
| T | Tr | [326,497,513,555] | [325,326,473,474] | [325] | [507] | [474] | [473,474,512] | [497] | [500,556] | [311,462] | ||||
| Inj | [388] | [511] | ||||||||||||
| Or | [513 | [462] | ||||||||||||
| TU | Tr | [557] | ||||||||||||
| Inj | [523,558] | [518] | [475,559] | [476,521] | [559] | [507,523] | [476] | [475] | [327,494,519,526] | [494,518,556] | [556] | |||
| Or | [430,528] | [560] | [430] | [500] | ||||||||||
| TE | Inj | [561] | [533,535] | [535] | [438,520] | [538] | [507] | [329] | [529,556] | [556] | ||||
| TC | Inj | [562] | [538,563] | [507] | [549] | [564] | [556] | [556,565] | ||||||
| UN | ND | [482,541] | [482] | [482,566] | [478,541] | [482,567] | [542] | [482,541,542] | [480,508] | |||||
| Tr | [317] | [568] | ||||||||||||
| Inj | [543] | [545] | [545,551,569,570] | [388] | [546,551,563] | [549,571] | [492] | [564] | [565,572,573,574] | [550,565,568,572,575,576,577] | ||||
| Or | [568] | |||||||||||||
The numbers shown in the table are references to studies of the effects of T treatment in men. These studies show, as principal or significant, most of the effects listed in the first row (in addition to further information and other effects not so generally acknowledged). Thus, the top row (vertical descriptors) shows the main effects observed in most of the studies (↑ meaning an increase or improvement, ↑= maintenance within normalcy, and ↓ decrease or reduction in the parameter, which may represent an improvement or not). The effects generally considered positive are shown using a pale green cell background, and pink has been used for those considered negative or potentially dangerous. The effects have been loosely grouped according to the type or subject of the function described. The last column/section, NEGATIVE, corresponds to other varied, general or undetailed negative effects of the treatment (mainly cancer or cardiovascular disorders). Hormone (column H): T = testosterone; TU = T undecanoate; TE = T enanthate; TC = T cypionate; UN = undefined/unknown T derivatives, formulations or combinations of androgens used in TRTs. Mode of administration/via (column V): ND = not described, or combinations of ways (i.e., in the context of meta-analyses or reviews); Tr = transdermal: gels, patches or other similar procedures; Inj = injection, largely deep i.m.; Or = oral administration.
The assumption of pharmacological equivalence is essentially based on the control observations of increased T levels after months or years of substitutive treatment using T or exogenous AcT. The T newly found in the blood of TRT patients is directly assumed to be formed via ester hydrolysis; this is responsible for the androgenic effects observed in the patients. However, this critical point has not been proven so far, and we do not even know how the synthetic esters of T affect the dynamics of DHT, KT or E2 synthesis in addition to that of T itself. Evidently, using long-lasting injections (i.e., providing a maintained flow of T for months) necessarily alters the natural mechanisms of control of T via the HHG axis, a factor that in most cases is simply ignored, practically relying only on checking the circulating T (only T) levels. This is probably the main disruption caused by the non-discriminate use of standard (albeit undefined) TRTs. The continued exposition to T release may produce serious alterations in the regulation of FSH and LH secretion, which may result in a chaotic regulation of the closer T-derived hormones (E2, DHT), which roles should necessarily participate in the normalizing physiological response to any TRT.
The rise in T elicited by TRT seldom takes into account the circulating levels of the same AcT injected, which are supposed to quantitatively yield T via esterase hydrolysis. The analysis of AcT, including the T esters used as drugs, is technically feasible [152,484], and injected AcT have been detected unaltered even in dry blood stains [485]. However, the information on their dynamics after or during treatment in blood, tissues and excreta is generally unpublished (or unavailable to the scientific community). The practical absence of molecule-to-molecule effectiveness comparisons, together with the absence of quantitative analyses, and the additional “corner-cutting” or unjustified generalizations when comparing different times, schedules, patterns, doses and the use of pre-established mechanisms for comparison, severely compounds the problem of endocrine/clinical evaluation of the effectiveness of deep intramuscular AcT injections for TRT.
The time-honored precaution of using a washout period after a short-time treatment with drugs or hormones, such as T or AcT, is seldom (and inadequately) followed [486], and for logistical reasons, cannot be applied to large oleome-depot doses of AcT. The practical question of commodity of treatment: such as a few injections for a long time, has taken hold, despite the need to use safety systems [482,487]. The application of known pharmacokinetics of T and AcT used to apply different modes of administration [488] often are not included in detail (and neither checked) when planning or applying a TRT. This also goes for the safe use of washout or recovery periods interspersed along time in long-term drug treatments [489], but also used for long-term hormone treatments [490,491], and even for short-term TRTs [492]. The use of trans-dermic T for alternate months (i.e., no treatment in the washout period) was found to produce the same expected physiological responses with a halved T dose over the total time [493].
7.5. Effectiveness and Insufficient Overall Analysis, of Long-Term Use of AcT for TRT
Table 2 compares the effects of long-term administration of T and the main AcT drugs in use. It is difficult to try to assess whether there are real differences between treatments using T or its “preparations”, largely those using esterified T, since the populations of subjects (mostly adolescents or adult men) studied. These variables include age, disorders, presence of controls, use of a placebo group, purpose of the study and methodology used, size of the sample, molecular species used, dose(s), way of administration, duration, pattern and evaluation/safety parameters analyzed. These variables are compounded with the assumption that T is the only molecular species responsible for the effects induced by any of the hormonal precursors or agonists using an unproven premise that has been maintained for more than four decades. Despite its obviousness, this aspect has not been challenged, instead centering most of the interest in obtaining more effective and safe preparations [494,495,496].
The wide dispersion of data and results available for TRT is not only a consequence of the polyphyletic origin/purpose of the large number of studies conducted so far, but especially of the unproven assumptions ruling the “practical clinical” use of androgens. There are a considerable number of comparative studies and meta-analyses on the effects of TRTs, but comparisons are difficult because of the reasons explained above that can be summarized in three main problems affecting homogeneity: (a) what is actually known as “testosterone” by the authors? (b) the variability in extension, objectives and methodology (duration, dose, mode of administration) and (c) the absence of periodic patterns of administration as a way to protect the integrity of function of the HHG axis.
Thus, I decided to just list the articles directly available, and pair the papers with the effects most commonly described of androgens in the series studied. This is in line with other previous analyses [474,482]. The most common types of androgens used were differentiated in the analysis: T and the AcT. Most of the T studies consulted were carried out using gels and patches (largely short-term), whereas most of the AcT treatments were long-term, and largely referred to injections of—mostly—T undecanoate. The studies using T were essentially transdermal, short-term and oral, inducing mostly positive responses, whilst the effects of AcT—largely injections and long-term—were also effective, but, with respect to those of T, there were different lists of results, now including some negative effects. These included circulating lipids, cardiovascular disorders and contraception, but also included positive influences on the widely discussed issues of T incidence on life expectancy and depression.
Since the data were not statistically comparable, a crude analysis was carried out, relying on the interpretations of the conclusions presented in the papers cited (many of them already being meta-analyses and reviews). The number of citations sustaining the different effects described were counted irrespective of the mode of administration and a rough ratio of T vs. AcT was estimated for each entry after correcting for the total number of references counted. The following short list presents the parameters analyzed (only those with a minimum of data, or those including several other effects), listed according to the number obtained from this ratio compared with T. In green, the “positive” results are shown, and in red the “negative”; the up arrows represent an increase (or improvement), and the down arrows show a decrease (or worsening condition).
A large part of the AcT differential pre-eminence on some effects may be a consequence of the extremely long periods of treatment, the use of high overall doses and the obvious alterations of the physiological regulation of androgen levels and functions. These problems also affect the transdermal procedures used for T, but the TRTs duration is often counted in weeks or months (far away from the months or years of most AcT-based TRTs). In any case, there is a graded difference in the type of effects observed between T and AcT, despite their coincidence on questions related with sexual functions and the effect on circulating T. This superficial analysis shows, however, that the references in the studies analyzed to issues more related to energy metabolism, such as insulin control (and glycaemia) and body protein, were more frequent when describing the effects of non-esterified T. Thus, the results obtained for AcT were—probably—a consequence of the released T rather than direct effects of the larger ester molecules. The apparently marked beneficial effects of transdermal T on insulin resistance and the increase in insulin sensitivity, which were necessarily observed under relative short-term treatment (gel), can be directly related to the implication of E2 in the control of glucose metabolism (and lipid oxidation). This difference hints to the facility of aromatization of abundant free T to E2 as a critical control node of glucose (3C) and 2C energy metabolism, as previously reported [3].
Injected AcT depots release T, but probably not in the ideal (i.e., circa-T endocrine homeostasis) conditions to sustain a sufficient and controlled flow of E2 to maintain energy partition and increase lipid oxidation, as deduced from the different profiles on E2-dependent effects of free T and AcT administration. However, this flow did not hinder the conversion of T to DHT, which may take place even when T remains esterified [578]. The main differences in clinical effects between both types of treatment, however, were those derived from cardiovascular protection/damage. Almost not cited for transdermal T, they were represented both in favor of protection and as possible causes of serious ill effects in the AcT group [511,542,556,573,579]. The differences were, again, more marked between T and AcT for the TRT effects on contraception—an effect sought for long-term treatment [388,438,520] with often uncertain results [580]. Notwithstanding, infertility may also be an unwanted consequence of TRT [482,529]. The application of T as a male contraceptive has been used for a long time [447,581,582], but nevertheless, remains a hormonal option despite some shortcomings and relative unreliability [581,583,584].
There are, also, differences on hematopoiesis between the two TRT groups described. Long TRTs seem to clearly interfere with erythropoiesis, essentially by increasing erythropoietin activation and inhibiting hepcidin [585,586], which results in higher blood cell counts, hematocrit and hemoglobin. These effects are patent in long-term TRT using AcT in comparison with T gels [587]. Nowadays, warnings about these negative blood alterations are already present in direct access information on TRT products [578], and are taken into account when planning androgen substitutive treatments. The T effects on polycythemia do not require aromatization [588], which can be assumed to be not mediated by E2.
The analysis presented above is not quantitative and has no statistically endorsed reliability, but is the narrative sum of a fair number of widely different sources. A main reason for using this low-certainty procedure is the generalized absence of unifying criteria, which, however, have the advantage of preventing the (common and selective) exclusion of many studies, thus, adopting a wider encompassing (albeit less defined) vision. The studies analyzed were carried out using quite different criteria, methodology, focus, subjects, duration and even types of molecules or combinations. In addition, they were developed under different contexts of knowledge (along several decades) on the function, use and analysis of steroid hormones and the pathologies they were used to limit/prevent.
Nevertheless, the number of studies included their size, criteria of selection, and, especially, the availability of the reviews and analyses are important aspects to be taken into account, in part as “negative” factors that may affect the relevance of the present analysis. The obvious caveat of precisely using the specific papers cited is the logical assumption that any other selection may result in different (albeit also provisional) conclusions. However, the number of studies analyzed their varied “age”, context, origin, purpose and widely varied focus (plus the exclusion of animal-based studies as a rule), which may help to set the context for the practical usefulness of the limited results obtained: hints, at the most. The fact that there is a notable coincidence in the summary of effects with previous studies [482] also helps to show that only the most apparent common ground has been highlighted. The observations are necessarily limited, but nevertheless clearly indicative of the existence of differences in the effects elicited by using T or its esters.
Continuous treatment with AcT alters the hematopoietic system in a way apparently not (or, possibly, not yet) detected during short-term (and largely transdermal) TRTs using T [587]. Since a fair number of androgen derivatives elicit porphyrin (and hemoglobin) synthesis and erythropoiesis [589,590], the differences between T and AcT may hint at natural AcT implication on this aspect of metabolism, but there are no specific data to sustain this appreciation.
The effects observed on body composition and circulating lipids may be a consequence of the normalization of circulating T levels, which also help explain the improvements in sexual arousal and function. Nevertheless, the present analysis does not support a clearly different functional role for the physiologic AcT and T, other from those related to E2 production and AR binding. It has been postulated that AcT could act as a temporal storage (limited in mass) for T in tissues [60,153,591]. Thus, the function of AcT at physiological levels may be not quite as different from that of T, as are the widely different functions of estrogens and their fatty esters [9]. This is in agreement with the variability of physiological fatty acid moieties in the small pool of natural circulating AcT [437].
It is fundamental to obtain a critical and systematic analysis of the effects of the different molecular species used for TRT. At present, we already have available (and rapidly developing) the powerful methodology to effectively analyze the kinetics of utilization of these drugs and to establish their interaction with other androgens (and other classes of steroid hormones). The overlapping, limited, selective TRT studies available often repeat incomplete analyses, or select very specific targets in highly constricted conditions, leaving large (and repeated) gaps in our knowledge. Consequently, they do not help enough to consolidate what is known. This discontinuity in the research focus is fully in line with a recent general comment on the clinical studies’ repetitiveness and focus inconsistence with respect to previous analyses [592].
The higher lipophilia of AcT used in pharmacological preparations is a bonus for the smooth absorption and extended effects of T [408] whilst preventing its immediate inactivation via glucuronic acid conjugation. Notwithstanding, the sustained use of AcT drugs for long-term anabolic, restitutive or simply senolytic actions, must come with two important caveats to control and/or take into account: (a) the need to watch the red blood cell and hemoglobin levels [573,593]; and (b) the deep and long-lasting interference of a continuous and persistent supply of T, from deep intramuscular injections on the control of the HHG axis, deregulating the levels, function and adjustment of both T and E2 (and indirectly, those of DHT, other androgens and gonadotropins) [594,595].
7.6. Additional Questions Posed by TRT in Women
So far, a large majority of TRT studies have been centered on men, but there are a growing number of studies dealing with the therapeutic use of T in women [596,597,598]. The ease with which T is aromatized to E2 is a fundamental aspect to consider when using TRT in women, despite their quantitative needs of T being apparently lower than in men. Nevertheless, this question has to be taken into account because of the danger posed by the possible potentiation by E2 of estrogen-sensitive cancers [599].
A key question, however, is the indiscriminate use of the polysemic term “androgenization” applied to women, both to POCS patients [600] and postmenopausal women [601]. There are marked differences in the discrimination, definition and, consequently, pathognomic explanation of the POCS dual disorder: ovarian or adrenocortical [602]; however, androgenic dysfunctions [603] and insulin resistance [604,605] are common occurrences in both, including the superimposed appearance of menopause on POCS patients [606] The similarities of POCS with MS have been also associated, too, with common pathogenic manifestations
The question of androgens in women is even more complex than in men, especially because of the relatively new finding of KTs, hence, increasing the adrenal cortex importance in supplying a steady flow of androgens to women [13]. Androgens in women are essential, for functions not necessarily coincident with those of T’s full spectrum of actions). The blood levels of androgens (as a whole) are fairly higher in women than those of estrogens (even when he KTs are not taken into account [607]:
| DHEAS > DHEA > A4 > T > DHT |
At least 25% of T is produced in the ovary, 25% more in the adrenals and the rest is the consequence of peripheral interconversions (cited by [608]). The ovary does not cease its production of T in women for at least one decade after menopause [79], but the overall production of A4 by the adrenals decreases markedly, which converts T in the main androgen produced overall (as compared to A4) [609]. The global body production of T in post-menopause compared with the reproductive period decreases by one third, whereas those of A4 and DHEA are halved [608]. In POCS, there is a higher thecal secretion of A4 [609], increasing the androgen levels in adrenal glands [610], but the conversion of A4 to E1 is enhanced, thus, further decreasing A4 availability [611].
In ovarian vs. peripheral blood, oophorectomy decreases the levels of T and E1, but not those of A4, E2 and DHEA [79]. The faster turnover of T, however, could not be sufficiently compensated by a fairly maintained T production at menopause and further on. A comparison of androgen and estrogen levels in ovary blood vs. systemic blood [612] showed a 15-fold decrease in T levels compared with “only” 4-fold for A4 and 2-fold for E1 and E2. This may explain the quantitative importance of A4, but also, probably—and mistakenly—includes the dubious “androgenic” contribution of the fairly maintained levels of DHEA to the “androgenization” often described for old women. It has been found, however, that 11-keto-androgens are the main adrenal androgens in PCOS [613]. Thus, despite the marked adrenal decrease in women in A4 production with advanced age [614], the decrease in T at menopause may have a more effective result when lowering the androgen availability of postmenopausal women. There are other possible explanations to the post-menopausal androgenization, such as aging [614] and the manifold increase in the possibility of developing MS [615] when the HHG-elicited production of E2 falls at menopause, helping spur obesity and finally equalizing older women with mature men’s long navigation through MS. Increases in T can be also attributed to cancer and other metabolic disorders in the postmenopausal period [616,617]. We lack information about the roles played by T, its aromatase conversion to E2 and the unexplained possible function of excess availability of E1 in this critical period. In fact, its association with obesity [618], and the adipogenic effect observed in rats [619], may help explain in part the shift in lipid metabolism at menopause, and its leaning towards a MS situation.
The changes in the hormonal makeup of women after menopause may also give more transcendence to the modulation of KTs and their closely associated corticosteroids in the adrenal cortex (Section 5.3). The fall in tissue E2 and T availability is probably directly related to a shift in the adrenals, with a lower production of classical androgens and more marked corticosteroid effects [620] including higher circulating cortisol [621]. However, the treatment with DHEA helps limit the corticosteroid effects [622]. These data agree with a shift of the adrenal cortex towards the synthesis of corticosteroids in the detriment of androgens.
Menopause also induces a change (to worse) in the maintenance of bone health [623,624], largely due to the fall in E2 and the decrease in its support of bone homeostasis. However, this could also be due to increased glucocorticoid activity [625], since glucocorticoids promote the development of osteoporosis in animal models [626]. Osteoporosis is common in post-menopause [627,628], and is often found to be associated with obesity [629,630], even with sarcopenic obesity [631]. The implication of a wide number of regulatory mechanisms, such as the relationship of post-menopausal bone health with bone marrow adipocytes, have been studied [632]. The use of E2 replacement protocols helps correct the danger of osteopenia/osteoporosis [633,634]. The metabolic and hormonal turmoil of menopause also affects brain function [635], protein pool maintenance [636] and the combined consequences of a lower availability of T and E2 on senescence, sexual functions, behavior and well-being. These effects can be partly counteracted with T and E2 replacement therapies. There are, yet, few studies on substitutive androgenic treatment in women for the improvement of the already patent T deficits in post-menopause [596,598,637] or heart conditions [638]; the dual therapy of T and E2 have been already tested [639]. However, the weight of misconceptions and lack of acknowledgement of the crucial metabolic regulation role of T in all humans, irrespective of gender, somehow restrain the full clinical use of T for the treatment of disorders related to menopause (and often compounded by MS) in women [598].
The duality of T and KT (and 4A, probably to a minor extent) as key female pre-menopausal androgens, and their coincidence (or not) in functions, needs to be more specifically studied, as it is a critical point for the eventual effective androgenic treatment of women with hypoandrogenism. This includes the clarification of the (differentiated) path for DHEA treatment, which beneficial effects are well known. However, we still need to understand why so much T is produced, and also, why it simply seems to vanish (unused?). Any sustainable explanation needs to seriously take into account the third party in this steroid hormone age-related disorder: corticosteroids. Unfortunately, we do not have enough concrete information on the interconnection between corticosteroids and the basic genetically coded processes of senescence and age-driven systemic-obsolescence (with T and E2E2, as explained above). These processes have evolved to determine the inherited functional protocols on which stand the survival of our species, and are hardly subjected to rapid modifications along a few generations.
In summary, hypoandrogenism in men is usually related to aging and/or the development of MS [576,640] and related disorders. The key factors being an insufficient production/availability of T, and consequently, an even deeper insufficiency of E2. In women, however, menopause may induce a different kind of hyperandrogenism, characterized by a limited E2 availability largely due to insufficient T, not compensated by the lower A4, but with higher proportions (but not levels) of DHEA; all of this context is paralleled by higher E1 over E2. The assumption of androgenicity in old women may be caused mainly by the interpretation of relative data: total androgen (largely indexes, not levels and no discrimination of molecular species) rises (over pre-menopausal conditions) with respect to E2, since E1 predominates, and the drop in circulating T (and to a minor extent A4) is “compensated” by lower changes in DHEA (misinterpreted as a full androgen, in the testosterone sense). Thus, actual female menopausal hypoandrogenism is largely hidden behind a screen of indexed data, and occasionally true hyperandrogenism caused by other pathologies. Senescence in women, thus, reverts to the same problem that hypoandrogenic old men endure: insufficiency of both T and E2 (playing havoc on glucose and lipid metabolism: Section 5.1 and Section 5.4); a situation mimicked in the Turner syndrome [641], induced essentially because of low T availability.
8. The Use of Androgens for the Treatment of Functional Disorders
The substitutive administration of androgens to hypoandrogenic men is conceptually similar to that of estrogens to women, in which the ovaries are no longer functional (for ovulation, but not always for endocrine secretion). However, the sex differences are critical: the deficit (of T and E2) affects not only old men, but also much larger (commonly younger) groups of men [385,387,642] and women [386] with MS. The planned obsolescence of the HHG axis starts sooner in men than in women, but both genders tend to show similar situations in advanced age, despite a slower long progression in men vs. an abrupt acceleration in post-menopausal women. The feeling of unexpected loss of functions already experienced by mature (i.e., not yet old) men produce deep changes in their attitudes, intending to maintain (or recover) their intrinsic maleness. This ancestral fear has been always tried to correct, to no avail, mainly because of a lack of knowledge and adequate means. It affects other animals, especially those societies with alpha-males hoarding a number of females (harems) [643]; these situations invariably result in the challenge and substitution/demise of the old patriarch [644]. Testosterone levels and dynamics play a critical role in the maintenance of this reproductive selection system [645].
Despite the caveats and preparation of Medical Societies-endorsed position papers, the normalized use of efficient TRTs is far from being established. There is a constant evolution, reflected in the short-time between actualizations of these statements [481,646,647,648,649]; but the use of TRT for aging (and/or MS-derived hypogonadism) keeps growing [650]. The focus is now shifting to the discussed and controversial use of TRT in women [651,652,653], which may be related to the deeply ingrained (and scientifically unjustifiable) notion that sex hormones fully imply an “absolute” link to gender: androgen for males and estrogen for females, with no space in between. This unproved belief has been a pillar of “sex hormone medical knowledge”, and remains true up to the present for generations of physicians, scientists and social leaders and activists.
To my knowledge, the KTs have not yet been used for androgenization treatments in the general clinical practice to help maintain steady and effective growth/tissue maintenance and the basic androgen functions of metabolism. However, they may be called to—at least in part—substitute T (and synthetic AcT) in these tasks with a higher degree of safety. Their antipodal relationship with GC has yet a dearth of potential applications to be understood, tested and developed.
The contemporary massive use of androgens as senolytic agents has been re-initiated by gerontologists, but now it has extended to other areas of medicine, being finally (but reluctantly) accepted by the endocrinologists probably because of the consequences of their generalized (and often uncontrolled) use [654,655], and especially, because part of the ravages of old age and MS are clinically improved by TRTs [656,657]. In addition, TRTs also help regularize glycaemia [658], maintain muscle mass [659,660], improve well-being [661] and reduce the development/severity of cardiovascular disorders [662]. However, the uncontrolled use of androgenic drugs has been observed to induce serious health problems, as described in Section 7.3, including psychological and personality alterations [663] and even reproduction-related loss of function [664,665], including infertility [390].
A large number of old people show a marked loss of body protein in special muscle mass [666,667,668], often compounded with osteopenia [669]. These changes fit in the widely extended sarcopenia spectrum [670,671], inducing or compounding frailty [672]. These changes are commonly associated with disorders grouped under the metabolic syndrome umbrella, and/or aggravate previous disorders and pathologic chronic conditions [673,674], globally enhancing the severity of frailty and increasing the dysfunctionality, morbidity, dependence and mortality of the subjects [675,676]. The changes in body composition (affecting mainly protein), decreasing turnover of structural proteins [677], and thus, reducing their reposition and functionality, do not necessarily affect body lipid stores. Thus, sarcopenia can often develop while maintaining obesity (e.g., sarcopenic obesity) [678,679]. The obese can become sarcopenic and frail while maintaining their main energy (TAG) stores full, with a largely unused mass of fat which constitutes an additional burden [680]. A key metabolic difference between sarcopenia and cachexia is the indiscriminate use, in cachexia, of all body substrates susceptible to be used for energy (fat or protein), [681,682]. TRTs have been also used to complement the diet, using an adequate (supplementary) supply of energy, protein and micronutrients, as a way to limit the ravages of malnutrition [683,684,685], sarcopenia [300,301,686] or even advancing cachexia [687,688].
In men, old age by itself tends to correlate with lower levels of T [332,689], but often maintains normal or high levels of gonadotropins [690,691], helping suppress the gonadal production of T [691,692]. This situation suggests that hypoandrogenism in older males is a probable consequence of the HHG axis dysregulation. The deficit in estrogens in women can be treated via the substitutive administration of estrogens (often combined with progestogen) [693]. This may help to correct the problem of the E2 deficit, but not that of T, which could not be improved this way, since the aromatization path is not reversible. In people enduring gender reaffirmation processes, the exogenous hormonal treatments tend to overwhelm the (often diminished) physiological synthesis of either T (for men [694]) or E2 (for women [695,696]); therefore, at least during the transition phase, the HHG regulative system is expected to be largely inoperative because of signal saturation blockage. Hormonal treatments may be effective without the need for additional modulation using gonadotropins or GnRH [697].
There is considerable (recent) literature on gender-normalization endocrine handling, but in male reaffirmation procedures, the basic treatment is similar to the long-term hypoandrogenism situation described in Section 7.5, i.e.; that the administration of T or AcT helps the masculinization of brain [698], restores musculation and functional re-adjustments [699], as well as inducing the manifestation of secondary sex characteristics [700,701]. In affirmative male-gender men, T treatment does not exacerbate a pre-existing POCS disorder [702], but increases endothelial inflammation [703,704]. In reaffirming women, the specific suppression of T synthesis may be even eliminated from the treatment because a high part of the naturally produced T is largely aromatized to E2. However, the use of T enanthate for the hormonal reaffirmation of men [449,705] may help explain the absence of the expected rise in E2 [706]. The use of T in gels [707] or subcutaneous injections has been found to work better in practice for this purpose [425], probably because T can yield E2 more easily than AcT.
When discussing the benefits of TRT to patients with hypoandrogenism, it is critical to think of T not only as an androgenic vector, able to regulate metabolic functions, maintain muscle, cognitive functions and the diverse functions sought to recover, but that T is also the main precursor for E2 synthesis. Consequently, E2 has a pivotal role in energy partition, anti-oxidative functions and for the cooperation with T itself, and even GC, to regulate substrate utilization. The beneficial effects of T on MS rely not only on T itself but on the cooperative muscle–bone–liver–brain interactions between T and E2, including the control of fat deposition and its disposal. This dance-duet equilibrium is fundamental to recover full metabolic homeostasis. Steroid hormone treatment of a metabolic disorder (or a constellation of them, such as MS) should consider this special relationship.
In short: the estrogen collaboration to TRT may help considerably in the adjustment of metabolic energy partition [3,9,18], which directly affects body fat stores [708,709,710], protects the heart [711,712], maintains muscle function [713,714], exerts neuro-protective effects [715,716,717,718,719] and regulates mitochondrial integrity and function [35,720,721], in part because of E2 anti-oxidative effects [35,722,723]. E2 is also necessary for spermatogenesis in the testes [724,725]. The main metabolic function of E2 is probably its role in the control of energy balance and substrate energy partition, in part by controlling insulin action in the regulation of glucose metabolism [3,9,726].
There is enough basic and clinical knowledge to develop MS treatments based on the careful correction of its main hormonal deficit, T. However, care must be taken to control the oscillations of T (and E2) levels along the whole treatment, interspersing—necessarily—periods of rest or washout (i.e., no hormonal treatment) sufficient to maintain (and prevent blocking) the periodicity of gonadotropin secretion and protection of endogenous testicular endocrine (and reproductive) function. The widely used avenue of the substitution of T by AcT has shown—so far—only limited effects on glucose levels (Section 7.5), compared with the consistent inverse relationship between T levels and insulin resistance [219,727,728], with a direct incidence on MS and body lipid handling [727,729,730]. The differences between T and AcT hint at the T effect being probably mediated (at least in part) by E2, especially if we compare the known effects on lipid handling and body mass elicited by estrogens and acyl-estrogen SERMs [3,9,155].
Testosterone may be an excellent senolytic when, and if, administered reasonably: i.e., only when needed, and in a carefully balanced way, to just cover the deficit (with as few disturbances as possible) of patients of hypoandrogenism correctly diagnosed. This implies that repeated checks and controls should be maintained (at least) throughout the whole treatment to prevent unwanted effects. Nevertheless, utmost care must be taken on the clinical use of androgens, with the focus set on the individual conditions of the patients. The preservation of muscle mass and cognitive functions should be the main objectives of TRT due to their critical role in the maintenance of the quality of life.
Box 1 shows a list of the main factors to consider when planning or developing a pharmacological intervention to treat hypoandrogenism, such as is presented in senescence and MS. The points described are simply a summary of most of the questions treated along this review.
Box 1. Aspects to consider in the design of a substitutive androgenization treatment.
Any plan to carry out an androgen substitutive/compensating treatment should consider, at least, these aspects:
-
Patient conditions.
First, the real existence of a need for androgenization treatment must be clearly established after an intensive and exhaustive metabolic and hormonal analysis of the subject. Then, the plausibility of carrying out an androgenization treatment must be decided upon, taking into account the individual conditions: sex, age, nutrition or hormonal disorders (especially including metabolic syndrome and its related pathologies, andropause, menopause, old age and hypogonadism). These aspects should be weighed according to the severity of the conditions, time available and health objectives sought. Psychological factors must be considered because of the probable duration of the process and the behavioral/social changes expected.
-
Molecular species used
Currently, practically all androgenization treatments are based in either T or a number of eka-T products, as described in the text, but their mode of action is not the same. This analysis should be open to specific (even combined) treatments including T, AcT, KTs and the fully synthetic drugs available at present (not discussed in this review), tailoring the molecules to the needs of the treatment (and the extent of the risks taken with their use). Evidently, age, sex and metabolic disorders are critical factors to ponder in addition to a solid reason for applying an androgenic supplementation treatment. The eventual addition of other hormones, such as E2, should be also considered.
-
Way of administration and dose
This aspect directly depends on the molecule(s) selected, the disorder to be treated, and the real rates of release/inactivation. The problems posed by the different methods of administration are known and should be better specifically known through more extensive and complete checks of the molecular species involved. In general, it is better to use repeated short term procedures (i.e., transdermal applications) to maximize the possibilities of adjustment, evaluation, control or interruption of the treatment as needed.
-
Duration of the treatment
Time of treatment is closely related to the two previous points, since most of the procedures used so far rely, essentially, on massive, uninterrupted and prolonged treatment with (usually) a single hormonal agent. However, hormones are extremely sensitive to physiological modulation and are carefully regulated in vivo. Only good feedback of the effects sought by the treatment may provide the sufficient level of safety and effectivity to carry on. This is another reason favoring shorter treatments (preferably repeated after safety interludes), and the continued control of physiological functions, hormone levels and related markers, as well as behavior/patient satisfaction (and compliance) feedback.
-
Maintenance of hormonal homeostasis
The administration of a drug with hormonal effects constitutes per se a destabilizing intrusion in the body humoral homeostasis, obviously, irrespective of the nature and quality of that homeostasis. In the case of “testosterone” long-term treatments, often the only guide available (differential effects) can begin to be observable after long saturation (resulting in inactivation) of the physiological control systems, after using high doses and a prolonged time. Only a few studies include periods of “rest”, interspersed after several months of treatment. This is a critical point that needs further (and deeper) development, extending the treatment periods based on limiting the overwhelming damage to the natural biological cycles (i.e., monthly, bi-weekly or even shorter alternate periods), and leaving time and space for the homeostatic systems (essentially the HHG and HHA axes) to re-start and help solve the disorder instead of enduring or fighting the powerful and continuous drug intrusion.
9. Conclusions and Perspectives
As in the case of estrogens [9], androgens are a group of hormones with quite different (often complementary) functions and modes of action, which are synthesized along a pathway (closely related to those of corticosteroids, and especially, estrogens) distributed in a few organs, strategically located to serve their multiple functions. They are all hormones acting not immediately, but essentially in the mid-term. This is accomplished largely (albeit not exclusively) via the modulation of gene expression, thus, their actions are of relatively prolonged effects, and are exquisitely regulated by a complex web of mechanisms to adjust their responses to the changing needs of the organism. They complement (and often also regulate) the shorter-acting hormones (e.g., insulin, catecholamines). Androgens (largely T) add a component of continuity and stability to hormonal regulation. This is the general trend, but in the specific case of testosterone, its half-life is much shorter than in most steroid hormones, a factor that allows for faster (bulk) responses (often non-genomic, and thus, also faster), but which extremely complicates its administration, and consequently, the maintenance of pharmacologically stable levels.
This is an open door for the treatment of MS and associated (or derived) disorders (obesity, type 2 diabetes, cognitive impairment, senility, sarcopenia, cachexia), but also includes frailty and the reproductive problems—about sex/fertility—often directly related to T deficiency. Most of the initial work in this field has already been carried out and is available (albeit disperse, and often forsaken) in the literature, thus, we need to widen our scope, learn/remember what is already known, organize and cross-check this huge amount of information with present day metabolic knowledge. When carrying out this actualization, we will be able to design and apply safe and adjusted procedures to help stop the increasingly extending epidemics of metabolic disorders which blueprint origin is within us, coded in our genes.This complex protracted decay situationcannot be solved using untested procedures of dubious effectivity, such as dietary manipulation or applying (untested) narrow-function drugs, instead of relying on new research and the sidetracked or forgotten scientific knowledge obtained by our predecessors in Science, an stored legacy which is (theoretically, at least) available to us.
An adequate focus of T substitutive treatments allows for the maintenance of T and E2 levels and functionality, but exerting a persistent blockage of the HHG axis and the brain attempts to keep the circulating T homeostatiss. Circadian variations in T have been described for men, in parallel to gonadotropins, E2 and other hormones [731,732,733], rhythms that tend to be less marked with advancing age and lower T levels [734]. However, ultradian cycles have been much less studied; there are sparse data showing a seasonal variation of plasma T in men, but the dispersion does not allow to clearly establish periodicity and duration [735]. Nevertheless, a study on 20 subjects showed the existence of several-day cycles (8–30 days, with most subjects in the 20–22-day range) in T levels in normal men [736]. Unfortunately, there is not enough information on this critical issue, since most TRT are prolonged from months to years without pause, necessarily interfering/destroying the physiological rhythmicity of the circulating T.
A number of genetically, epigenetically or man-made (e.g., diet, disease) disorders, such as MS or senescence-related hypoandrogenism, bring us again to the same questions (and provisional answers). All of them share a common distinctive alteration, such as the deficit of T (and, more or less directly related, deficit of E2); generated with the participation of the brain (hypothalamus) and our adjustment to life patterns established along evolution. These sets of life cycles seem hardly applicable to many present-day individuals (despite sharing the same physiological make-up as our ancestors of a few millennia ago). Public health, food availability, literacy knowledge, the structure of our society and many other advances, mark the difference in the survival of humans as species (however, not always in a positive way), drifting the massive reproduction/early death strategy by that of controlled reproduction/longer active life, obviously not without severe problems from the present environment (in a broad sense) and from our genes (i.e., planned obsolescence of men via MS, executed in part through a HHG-mastered dwindling of T (and E2) levels). These disorders affect hundreds of millions of individuals, and we do not yet have available and effective ways to cope with them. This may be a direct consequence of the genetic resilience that helps maintain our species to thrive.
There are sufficient pointers signaling the deficit of T as one of the most extended, repeated and mistreated medical problems. Thus, caution is needed, along with knowledge, to guide the use of exogenous T to correct metabolic-functional disorders caused by age, pre-established biological obsolescence mechanisms, a maladjustment to diet, stress, disease or a cumulative sum of the life-history of any human. This should always be taken as a palliative remedy, seldom as a cure for a settled or unstoppable disorder. It may help improve life conditions, extend the period of (worthy) life and compensate for the disorders observed because of the decreased availability of T. In fact, T is an extraordinary hormone, a true “elixir of life” [737], as was often defined by the pioneers in their study, only comparable to its life-peer E2; however, it is not a panacea, and does not work alone, but within a coordinated group of steroid hormones and controlling factors that induce the smooth changes expected from steroid hormones in both women and men along their entire life.
Abbreviations
| A4 | 4-androstenedione |
| ABP | androgen-binding protein |
| AcT | * acyl-testosterone |
| ACTH | corticotropin-[adrenocorticotropic] hormone |
| Ane | * androsterone [5α-androsterone] |
| AP | * ∆16–17-androgenic pheromones |
| AR | androgen receptor |
| ARE | androgen response element |
| CRH | corticotropin-releasing hormone |
| DHEA | dehydroepiandrosterone |
| DHEAS | dehydroepiandrosterone-sulfate |
| DHT | dihydrotestosterone |
| E1 | estrone |
| E2 | estradiol [17β-estradiol] |
| EA | * estrogenic androgens |
| ER | estrogen receptor |
| FSH | follicle-stimulating hormone |
| GC | glucocorticoid(s) |
| GH | growth hormone |
| GnIH | gonadotropin-inhibitory hormone |
| GnRH | gonadotropin-releasing hormone |
| GR | glucocorticoid receptor |
| HHA | hypothalamus–hypophysis–adrenals (axis) |
| HHG | hypothalamus–hypophysis–gonads (axis) |
| KT | * 11-keto-testosterone |
| KTs | * 11-oxo-androgens in general |
| LH | luteotropic hormone |
| MS | * metabolic syndrome |
| POCS | polycystic ovary syndrome |
| SARM | selective AR modulator |
| SERM | selective ER modulator |
| SHBG | sex-hormone binding globulin |
| T | testosterone |
| TAG | triacyl-glycerol(s) |
| TRP | transient receptor protein |
| TRT | testosterone-replacement therapy |
| 11βHSDH | 11β-hydroxysteroid dehydrogenase |
| * non-standard abbreviations/acronyms. | |
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The author declares no conflict of interest.
Funding Statement
This research received no funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Comitato R., Saba A., Turrini A., Arganini C., Virgili F. Sex hormones and macronutrient metabolism. Crit. Rev. Food Sci. Nutr. 2015;55:227–241. doi: 10.1080/10408398.2011.651177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giudicelli Y., Dieudonne M.N., Lacasa D., Pasquier Y.N., Pecquery R. Modulation by sex hormones of the membranous transducing system regulating fatty acid mobilization in adipose tissue. Prostaglandins Leukot. Essent. Fat. Acids. 1993;48:91–100. doi: 10.1016/0952-3278(93)90015-O. [DOI] [PubMed] [Google Scholar]
- 3.Remesar X., Alemany M. Dietary energy partition: The central role of glucose. Int. J. Mol. Sci. 2020;21:7729. doi: 10.3390/ijms21207729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stumpf W.E. Steroid hormones and the cardiovascular system: Direct actions of estradiol, progesterone, testosterone, gluco- and mineralcorticoids, and soltriol (vitamin D) on central nervous regulatory and peripheral tissues. Experientia. 1990;46:13–25. doi: 10.1007/BF01955408. [DOI] [PubMed] [Google Scholar]
- 5.Fietta P., Fietta P., Delsante G. Central nervous system effects of natural and synthetic glucocorticoids. Psychiatry Clin. Neurosci. 2009;63:613–622. doi: 10.1111/j.1440-1819.2009.02005.x. [DOI] [PubMed] [Google Scholar]
- 6.Zhou H., Hylemon P.B. Bile acids are nutrient signaling hormones. Steroids. 2014;86:62–68. doi: 10.1016/j.steroids.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Norman A.W., Henry H.L. Vitamin D to 1,25-dihydroxycholecalciferol: Evolution of a steroid hormone. Trends Biochem. Sci. 1979;4:14–18. doi: 10.1016/0968-0004(79)90239-1. [DOI] [Google Scholar]
- 8.Tintut Y., Demer L.L. Potential impact of the steroid hormone, vitamin D, on the vasculature. Am. Heart J. 2021;239:147–153. doi: 10.1016/j.ahj.2021.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alemany M. Estrogens and the regulation of glucose metabolism. World J. Diabetes. 2021;12:1622–1654. doi: 10.4239/wjd.v12.i10.1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barsoum I., Hung-Chang Yao H. The road to maleness: From testis to Wolffian duct. Trends Endocrinol. Metab. 2006;17:223–228. doi: 10.1016/j.tem.2006.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moos W.H., Dykens J.A., Nohynek D., Rubinchik E., Howell N. Review of the effects of 17 α-estradiol in humans: A less feminizing estrogen with neuroprotective potential. Drug Dev. Res. 2009;70:23. doi: 10.1002/ddr.20284. [DOI] [Google Scholar]
- 12.Van Pelt R.E., Gavin K.M., Kohrt W.M. Regulation of body composition and bioenergetics by estrogens. Endocrinol. Metab. Clin. N. Am. 2015;44:663–676. doi: 10.1016/j.ecl.2015.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Turcu A.F., Nanba A.T., Auchus R.J. The rise, fall, and resurrection of 11-oxygenated androgens in human physiology and disease. Horm. Res. Paediatr. 2018;89:284–291. doi: 10.1159/000486036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu J.D., Wu Y.Q. Anabolic-androgenic steroids and cardiovascular risk. Chin. Med. J. 2019;132:2229–2236. doi: 10.1097/CM9.0000000000000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Song S.H., Sung S., Her Y.S., Oh M., Shin D.H., Lee J., Baek J., Lee W.S., Kim D.S. Misuse of testosterone replacement therapy in men in infertile couples and its influence on infertility treatment. Clin. Exp. Reprod. Med. 2019;46:173–177. doi: 10.5653/cerm.2019.00290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keller J.L., Casson P.R., Toth M.J. Relationship of androgens to body composition, energy and substrate metabolism and aerobic capacity in healthy, young women. Steroids. 2011;76:1247–1251. doi: 10.1016/j.steroids.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu Y., Lopez M. Central regulation of energy metabolism by estrogens. Mol. Metab. 2018;15:104–115. doi: 10.1016/j.molmet.2018.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mauvais-Jarvis F., Clegg D.J., Hevener A.L. The role of estrogens in control of energy balance and glucose homeostasis. Endocr. Rev. 2013;34:309–338. doi: 10.1210/er.2012-1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harris I.D., Fronczak C., Roth L., Meacham R.B. Fertility and the aging male. Rev. Urol. 2011;13:e184–e190. [PMC free article] [PubMed] [Google Scholar]
- 20.Majer I.M., Nusselder W.J., Mackenbach J.P., Kunst A.E. Life expectancy and life expectancy with disability of normal weight, overweight, and obese smokers and nonsmokers in Europe. Obesity. 2011;19:1451–1459. doi: 10.1038/oby.2011.46. [DOI] [PubMed] [Google Scholar]
- 21.Konstantinov V.V., Deev A.D., Kapustina A.V., Shestov D.B., Timofeeva T.N., Lelchuk I.N., Balanova Y.A., Oganov R.G. Prevalence of excessive body mass and its relation to mortality from cardiovascular and main chronic noninfectious diseases among urban male population of geographical different regions in Russia. Kardiologiya. 2002;42:45–49. [PubMed] [Google Scholar]
- 22.Tan R.S., Pu S.J. Impact of obesity on hypogonadism in the andropause. Int. J. Androl. 2002;25:195–201. doi: 10.1046/j.1365-2605.2002.00356.x. [DOI] [PubMed] [Google Scholar]
- 23.Carr M.C. The emergence of the metabolic syndrome with menopause. J. Clin. Endocrinol. Metab. 2003;88:2404–2411. doi: 10.1210/jc.2003-030242. [DOI] [PubMed] [Google Scholar]
- 24.Kuk J.L., Ardern C.I. Age and sex differences in the clustering of metabolic syndrome factors. Association with mortality risk. Diabetes Care. 2010;33:2457–2461. doi: 10.2337/dc10-0942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Forti P., Pirazzoli G.L., Maltoni B., Bianchi G., Magalotti D., Muscari A., Mariani E., Ravaglia G., Zoli M. Metabolic syndrome and all-cause mortality in older men and women. Eur. J. Clin. Invest. 2012;42:1000–1009. doi: 10.1111/j.1365-2362.2012.02688.x. [DOI] [PubMed] [Google Scholar]
- 26.Guarner-Lans V., Rubio-Ruiz M.E., Pérez-Torres I., Baños de MacCarthy G. Relation of aging and sex hormones to metabolic syndrome and cardiovascular disease. Exp. Gerontol. 2011;46:517–523. doi: 10.1016/j.exger.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 27.Regitz-Zagrosek V., Lehmkuhl E., Weickert M.O. Gender differences in the metabolic syndrome and their role for cardiovascular disease. Clin. Res. Cardiol. 2006;95:136–147. doi: 10.1007/s00392-006-0351-5. [DOI] [PubMed] [Google Scholar]
- 28.Korhonen S., Hippeläinen M., Vanhala M., Heinonen S., Niskanen L. The androgenic sex hormone profile is an essential feature of metabolic syndrome in premenopausal women: A controlled community-based study. Fertil. Steril. 2003;79:1327–1334. doi: 10.1016/S0015-0282(03)00347-9. [DOI] [PubMed] [Google Scholar]
- 29.Markopoulos M.C., Kassi E., Alexandraki K.I., Mastorakos G., Kaltsas G. Management of endocrine disease: Hyperandrogenism after menopause. Eur. J. Endocrinol. 2015;172:R79–R91. doi: 10.1530/EJE-14-0468. [DOI] [PubMed] [Google Scholar]
- 30.Tsujimura A., Miyagawa Y., Takezawa K., Okuda H., Fukuhara S., Kiuchi H., Takao T., Yamamoto R., Nishida M., Yamauchi-Takihara K., et al. Is low testosterone concentration a risk factor for metabolic syndrome in healthy middle-aged men? Urology. 2013;82:814–819. doi: 10.1016/j.urology.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 31.Dimopoulou C., Goulis D.G., Corona G., Maggi M. The complex association between metabolic syndrome and male hypogonadism. Metab.-Clin. Exp. 2018;86:61–68. doi: 10.1016/j.metabol.2018.03.024. [DOI] [PubMed] [Google Scholar]
- 32.Blouin K., Despres J.P., Couillard C., Tremblay A., Prud’homme D., Bouchard C., Tchernof A. Contribution of age and declining androgen levels to features of the metabolic syndrome in men. Metab. Clin. Exp. 2005;54:1034–1040. doi: 10.1016/j.metabol.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 33.Chasland L.C., Yeap B.B., Maiorana A.J., Chan Y.X., Maslen B.A., Cooke B.R., Dembo L., Naylor L.H., Green D.J. Testosterone and exercise: Effects on fitness, body composition, and strength in middle-to-older aged men with low-normal serum testosterone levels. Am. J. Physiol. 2021;320:H1985–H1998. doi: 10.1152/ajpheart.00010.2021. [DOI] [PubMed] [Google Scholar]
- 34.Hua J.T., Hildreth K.L., Pelak V.S. Effects of testosterone therapy on cognitive function in aging: A systematic review. Cogn. Behav. Neurol. 2016;29:122–138. doi: 10.1097/WNN.0000000000000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Borràs C., Gambini J., López-Grueso R., Pallardó F.V., Viña J. Direct antioxidant and protective effect of estradiol on isolated mitochondria. Biochim. Biophys. Acta. 2010;1802:205–211. doi: 10.1016/j.bbadis.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 36.Grande G., Barrachina F., Soler-Ventura A., Jodar M., Mancini F., Marana R., Chiloiro S., Pontecorvi A., Oliva R., Milardi D. The role of testosterone in spermatogenesis: Lessons from proteome profiling of human spermatozoa in testosterone deficiency. Front. Endocrinol. 2022;13:852661. doi: 10.3389/fendo.2022.852661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang Y., Chen F., Ye L., Zirkin B., Chen H. Steroidogenesis in Leydig cells: Effects of aging and environmental factors. Reproduction. 2017;154:R111–R122. doi: 10.1530/REP-17-0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zwain I.H., Yen S.S.C. Dehydroepiandrosterone: Biosynthesis and metabolism in the brain. Endocrinology. 1999;140:880–887. doi: 10.1210/endo.140.2.6528. [DOI] [PubMed] [Google Scholar]
- 39.Blouin K., Veilleux A., Luu-The V., Tchernof A. Androgen metabolism in adipose tissue: Recent advances. Mol. Cell. Endocrinol. 2009;301:97–103. doi: 10.1016/j.mce.2008.10.035. [DOI] [PubMed] [Google Scholar]
- 40.Karbowska J., Kochan Z. Effect of DHEA on endocrine functions of adipose tissue, the involvement of PPARγ. Biochem. Pharmacol. 2005;70:249–257. doi: 10.1016/j.bcp.2005.04.022. [DOI] [PubMed] [Google Scholar]
- 41.Hu C., Rusin C.G., Tan Z., Guagliardo N.A., Barrett P.Q. Zona glomerulosa cells of the mouse adrenal cortex are intrinsic electrical oscillators. J. Clin. Invest. 2012;122:2046–2053. doi: 10.1172/JCI61996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Koldzic-Zivanovic N., Tu H., Juelich T.L., Rady P.L., Tyring S.K., Hudnall S.D., Smith E.M., Hughes T.K. Regulation of adrenal glucocorticoid synthesis by interleukin-10: A preponderance of IL-10 receptor in the adrenal zona fasciculata. Brain Behav. Immun. 2006;20:460–468. doi: 10.1016/j.bbi.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 43.Endoh A., Kristiansen S.B., Casson P.R., Buster J.E., Hornsby P.J. The zona reticularis is the site of biosynthesis of dehydroepiandrosterone and dehydroepiandrosterone sulfate in the adult human adrenal cortex resulting from its low expression of 3β-hydroxysteroid dehydrogenase. J. Clin. Endocrinol. Metab. 1996;81:3558–3565. doi: 10.1210/jcem.81.10.8855801. [DOI] [PubMed] [Google Scholar]
- 44.Yazawa T., Sato T., Nemoto T., Nagata S., Imamichi Y., Kitano T., Sekiguchi T., Uwada J., Sayful Islam M., Mikami D., et al. 11-Ketotestosterone is a major androgen produced in porcine adrenal glands and testes. J. Steroid Biochem. Mol. Biol. 2021;210:105847. doi: 10.1016/j.jsbmb.2021.105847. [DOI] [PubMed] [Google Scholar]
- 45.Turcu A.F., Auchus R.J. Clinical significance of 11-oxygenated androgens. Curr. Opin. Endocrinol. Diabetes Obes. 2017;24:252–259. doi: 10.1097/MED.0000000000000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Meinhardt U., Mullis P.E. The essential role of the aromatase/P450arom. Semin. Reprod. Med. 2002;20:277–284. doi: 10.1055/s-2002-35374. [DOI] [PubMed] [Google Scholar]
- 47.Charlier T.D., Cornil C.A., Ball G.F., Balthazart J. Diversity of mechanisms involved in aromatase regulation and estrogen action in the brain. Biochim. Biophys. Acta. 2010;1800:1094–1105. doi: 10.1016/j.bbagen.2009.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cornil C.A., Charlier T.D. Rapid behavioural effects of oestrogens and fast regulation of their local synthesis by brain aromatase. J. Neuroendocrinol. 2010;22:664–673. doi: 10.1111/j.1365-2826.2010.02023.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hojo Y., Murakami G., Mukai H., Higo S., Hatanaka Y., Ogiue-Ikeda M., Ishii H., Kimoto T., Kawato S. Estrogen synthesis in the brain-Role in synaptic plasticity and memory. Mol. Cell. Endocrinol. 2008;290:31–43. doi: 10.1016/j.mce.2008.04.017. [DOI] [PubMed] [Google Scholar]
- 50.Stocco C. Tissue physiology and pathology of aromatase. Steroids. 2012;77:27–35. doi: 10.1016/j.steroids.2011.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kroboth P.D., Salek F.S., Pittenger A.L., Fabian T.J., Frye R.F. DHEA and DHEA-S: A review. J. Clin. Pharmacol. 1999;39:327–348. doi: 10.1177/00912709922007903. [DOI] [PubMed] [Google Scholar]
- 52.Webb S.J., Geoghegan T.E., Prough R.A., Michael Miller K.K. The biological actions of dehydroepiandrosterone involves multiple receptors. Drug Metab. Rev. 2006;38:89–116. doi: 10.1080/03602530600569877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Leszczynski D.E., Schafer R.M., Perkins E.G., Jerrell J.P., Kummerow F.A. Esterificaction of dehydroepiandrosterone by human plasma HDL3. Biochim. Biophys. Acta. 1989;1014:90–97. doi: 10.1016/0167-4889(89)90245-0. [DOI] [PubMed] [Google Scholar]
- 54.Lavallée B., Provost P.R., Bélanger A. Formation of pregnelonone- and dehydroepiandrosterone-fatty acid esters by lecithin-cholesterol acyltransferase in human plasma high density lipoproteins. Biochim. Biophys. Acta. 1996;1299:306–312. doi: 10.1016/0005-2760(95)00222-7. [DOI] [PubMed] [Google Scholar]
- 55.Lavallée B., Provost P.R., Roy R., Gauthier M.-C., Bélanger A. Dehydroepiandrosterone-fatty acid esters in human plasma: Formation, transport and delivery to steroid target tissues. J. Endocrinol. 1996;150:S119–S124. doi: 10.1677/joe.0.150S119. [DOI] [PubMed] [Google Scholar]
- 56.Kalimi M., Shafagoj Y., Loria R., Padgett D., Regelson W. Anti-glucocorticoid effects of dehydroepiandrosterone (DHEA) Mol. Cell. Biochem. 1994;131:99–104. doi: 10.1007/BF00925945. [DOI] [PubMed] [Google Scholar]
- 57.McNelis J.C., Manolopoulos K.N., Gathercole L.L., Bujalska I.J., Stewart P.M., Tomlinson J.W., Arlt W. Dehydroepiandrosterone exerts antiglucocorticoid action on human preadipocyte proliferation, differentiation, and glucose uptake. Am. J. Physiol. 2013;305:E1134–E1144. doi: 10.1152/ajpendo.00314.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Morales A. The long and tortuous history of the discovery of testosterone and its clinical application. J. Sex. Med. 2013;10:1178–1183. doi: 10.1111/jsm.12081. [DOI] [PubMed] [Google Scholar]
- 59.Nieschlag E., Nieschlag S. The history of discovery, synthesis and development of testosterone for clinical use. Eur. J. Endocrinol. 2019;180:R201–R212. doi: 10.1530/EJE-19-0071. [DOI] [PubMed] [Google Scholar]
- 60.Vihma V., Tikkanen M.J. Fatty acid esters of steroids: Synthesis and metabolism in lipoproteins and adipose tissue. J. Steroid Biochem. Mol. Biol. 2011;124:65–76. doi: 10.1016/j.jsbmb.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 61.De la Torre X., Segura J., Polettini A., Montagna M. Detection of testosterone esters in human plasma. J. Mass Spectrom. 1995;30:1393–1404. doi: 10.1002/jms.1190301004. [DOI] [Google Scholar]
- 62.Kanji S.S., Kuohung W., Labaree D.C., Hochberg R.B. Regiospecific esterification of estrogens by lecithin: Cholesterol acyltransferase. J. Clin. Endocrinol. Metab. 1999;84:2481–2488. doi: 10.1210/jcem.84.7.5755. [DOI] [PubMed] [Google Scholar]
- 63.Lund-Pero M., Jeppson B., Arneklo-Nobin B., Sjögren H.O., Holmgren K., Pero R.W. Non-specific steroidal esterase activity and distribution in human and other mammalian tissues. Clin. Chim. Acta. 1994;224:9–20. doi: 10.1016/0009-8981(94)90116-3. [DOI] [PubMed] [Google Scholar]
- 64.Larner J.M., Pahuja S.L., Brown V.M., Hochberg R.B. Aromatase and testosterone fatty acid esters: The search for a cryptic biosynthetic pathway to estradiol esters. Steroids. 1992;57:475–479. doi: 10.1016/0039-128x(92)90040-g. [DOI] [PubMed] [Google Scholar]
- 65.Pretorius E., Arlt W., Storbeck K.-H. A new dawn for androgens: Novel lessons from 11-oxygenated C19 steroids. Mol. Cell. Endocrinol. 2017;441:76–85. doi: 10.1016/j.mce.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 66.Rege J., Turcu A., Kasa-Vubu J.Z., Lerario A.M., Auchus G.C., Auchus R.J., Smith J.M., White P.C., Rainey W.E. 11-ketotestosterone is the dominant circulating bioactive androgen during normal and premature adrenarche. J. Clin. Endocrinol. Metab. 2018;103:4589–4598. doi: 10.1210/jc.2018-00736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Imamichi Y., Yuhki K.-I., Orisaka M., Kitano T., Mukai K., Ushikubi F., Taniguchi T., Umezawa A., Miyamoto K., Yazawa T. 11-Ketotestosterone is a major androgen produced in human gonads. J. Clin. Endocrinol. Metab. 2016;101:3582–3591. doi: 10.1210/jc.2016-2311. [DOI] [PubMed] [Google Scholar]
- 68.Tsachaki M., Meyer A., Weger B., Kratschmar D.V., Tokarz J., Adamski J., Belting H.-G., Affolter M., Dickmeis T., Odermatt A. Absence of 11-keto reduction of cortisone and 11-ketotestosterone in the model organism zebrafish. J. Endocrinol. 2017;232:323–335. doi: 10.1530/JOE-16-0495. [DOI] [PubMed] [Google Scholar]
- 69.Turcu A.F., Rege J., Auchus R.J., Rainey W.E. 11-Oxygenated androgens in health and disease. Nat. Rev. Endocrinol. 2020;16:284–296. doi: 10.1038/s41574-020-0336-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pretorius E., Africander D.J., Vlok M., Perkins M.S., Quanson J., Storbeck K.-H. 11-Ketotestosterone and 11-ketodihydrotestosterone in castration resistant prostate cancer: Potent androgens which can no longer be ignored. PLoS ONE. 2016;11:e0159867. doi: 10.1371/journal.pone.0159867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Swerdloff R.S., Dudley R.E., Page S.T., Wang C., Salameh W.A. Dihydrotestosterone: Biochemistry, physiology, and clinical implications of elevated blood levels. Endocr. Rev. 2017;38:220–254. doi: 10.1210/er.2016-1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Roy A.K., Lavrovsky Y., Song C.S., Chen S., Jung M.H., Velu N.K., Bi B.Y., Chatterjee B. Regulation of androgen action. Vitam. Horm. 1998;55:309–352. doi: 10.1016/s0083-6729(08)60938-3. [DOI] [PubMed] [Google Scholar]
- 73.Fang H., Tong W., Branham W.S., Moland C.L., Dial S.L., Hong H., Xie Q., Perkins R., Owens W., Sheehan D.M. Study of 202 natural, synthetic, and environmental chemicals for binding to the androgen receptor. Chem. Res. Toxicol. 2003;16:1338–1358. doi: 10.1021/tx030011g. [DOI] [PubMed] [Google Scholar]
- 74.Auchus R.J. The backdoor pathway to dihydrotestosterone. Trends Endocrinol. Metab. 2004;15:432–438. doi: 10.1016/j.tem.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 75.Swerdloff R.S., Wang C. Dihydrotestosterone: A rationale for its use as a non-aromatizable androgen replacement therapeutic agent. Baillière’s Clin. Endocrinol. Metab. 1998;12:501–506. doi: 10.1016/S0950-351X(98)80267-X. [DOI] [PubMed] [Google Scholar]
- 76.Sartorius G.A., Ly L.P., Handelsman D.J. Male sexual function can be maintained without aromatization: Randomized placebo-controlled trial of dihydrotestosterone (DHT) in healthy, older men for 24 months. J. Sex. Med. 2014;11:2562–2570. doi: 10.1111/jsm.12550. [DOI] [PubMed] [Google Scholar]
- 77.Badawy M.T., Sobeh M., Xiao J., Farag M.A. Androstenedione (a natural steroid and a drug supplement): A comprehensive review of its consumption, metabolism, health effects, and toxicity with sex differences. Molecules. 2021;26:6210. doi: 10.3390/molecules26206210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Flickinger G.L., Wu C.-H., Touchstone J.C. Neutral steroid metabolites of dehydroepiandrosterone-7α-3H in human ovarian tissues. Steroids. 1968;11:389–399. doi: 10.1016/S0039-128X(68)80149-7. [DOI] [PubMed] [Google Scholar]
- 79.Fogle R.H., Stanczyk F.Z., Zhang X., Paulson R.J. Ovarian androgen production in postmenopausal women. J. Clin. Endocrinol. Metab. 2007;92:3040–3043. doi: 10.1210/jc.2007-0581. [DOI] [PubMed] [Google Scholar]
- 80.Bloem L.M., Storbeck K.-H., Schloms L., Swart A.C. 11β-Hydroxyandrostenedione returns to the steroid arena: Biosynthesis, metabolism and function. Molecules. 2013;18:13228–13244. doi: 10.3390/molecules181113228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Barnard L., du Toit T., Swart A.C. Back where it belongs: 11β-hydroxyandrostenedione compels the re-assessment of C11-oxy androgens in steroidogenesis. Mol. Cell. Endocrinol. 2021;525:111189. doi: 10.1016/j.mce.2021.111189. [DOI] [PubMed] [Google Scholar]
- 82.Gower D.B. 16-Unsaturated C19 steroids a review of their chemistry, biochemistry and possible physiological role. J. Steroid Biochem. 1972;3:45–103. doi: 10.1016/0022-4731(72)90011-8. [DOI] [PubMed] [Google Scholar]
- 83.Weusten J.J.A.M., Legemaat G., van der Wouw M.P.M.E., Smals A.G.H., Kloppenborg P.W.C., Benraad T.J. The mechanism of the synthesis of 16-androstenes in human testicular homogenates. J. Steroid Biochem. 1989;32:689–694. doi: 10.1016/0022-4731(89)90513-X. [DOI] [PubMed] [Google Scholar]
- 84.Dufort I., Soucy P., Lacoste L., Luu-The V. Comparative biosynthetic pathway of androstenol and androgens. J. Steroid Biochem. Mol. Biol. 2001;77:223–227. doi: 10.1016/S0960-0760(01)00057-7. [DOI] [PubMed] [Google Scholar]
- 85.Semwal A., Kumar R., Teotia U.V.S., Singh R. Pheromones and their role as aphrodisiacs: A review. J. Acute Dis. 2013;2:253–261. doi: 10.1016/S2221-6189(13)60140-7. [DOI] [Google Scholar]
- 86.Sobel N., Brown W.M. The scented brain: Pheromonal responses in humans. Neuron. 2001;31:512–514. doi: 10.1016/S0896-6273(01)00406-8. [DOI] [PubMed] [Google Scholar]
- 87.Wyart C., Webster W.W., Chen J.H., Wilson S.R., McClary A., Khan R.M., Sobel N. Smelling a single component of male sweat alters levels of cortisol in women. J. Neurosci. 2007;27:1261–1265. doi: 10.1523/JNEUROSCI.4430-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sun H.Z., Zang W.J., Zhou B., Xu L., Wu S.F. DHEA suppresses longitudinal bone growth by acting directly at growth plate through estrogen receptors. Endocrinology. 2011;152:1423–1433. doi: 10.1210/en.2010-0920. [DOI] [PubMed] [Google Scholar]
- 89.Engdahl C., Lagerquist M.K., Stubelius A., Andersson A., Studer E., Ohlsson C., Westberg L., Carlsten H., Forsblad-d’Elia H. Role of androgen and estrogen receptors for the action of dehydroepiandrosterone (DHEA) Endocrinology. 2014;155:889–896. doi: 10.1210/en.2013-1561. [DOI] [PubMed] [Google Scholar]
- 90.Langley E., Velazquez-Cruz R., Parra-Torres A., Enriquez J. The non-aromatic Δ5-androstenediol derivative of dehydroepiandrosterone acts as an estrogen agonist in neonatal rat osteoblasts through an estrogen receptor α-related mechanism. Endocr. Res. 2019;44:87–102. doi: 10.1080/07435800.2018.1559185. [DOI] [PubMed] [Google Scholar]
- 91.Osborne D.M., Edinger K., Frye C.A. Chronic administration of androgens with actions at estrogen receptor beta have anti-anxiety and cognitive-enhancing effects in male rats. Age. 2009;31:191–198. doi: 10.1007/s11357-009-9114-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Frye C.A., Koonce C.J., Edinger K.L., Osborne D.M., Walf A.A. Androgens with activity at estrogen receptor beta have anxiolytic and cognitive-enhancing effects in male rats and mice. Horm. Behav. 2008;54:726–734. doi: 10.1016/j.yhbeh.2008.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang S., Lai K., Moy F.J., Bhat A., Hartman H.B., Evans M.J. The nuclear hormone receptor farnesoid X receptor (FXR) is activated by androsterone. Endocrinology. 2006;147:4025–4033. doi: 10.1210/en.2005-1485. [DOI] [PubMed] [Google Scholar]
- 94.Maiworm R.E., Langthaler W.U. Influence of androstenol and androsterone on the evalulation of men of varying attractiveness levels. In: Doty R.L., Müller-Schwarze D., editors. Chemical Signals in Vertebrates. Volume 6. Springer; Boston, MA, USA: 1992. pp. 575–579. [Google Scholar]
- 95.Büttner A., Thieme D. Side effects of anabolic androgenic steroids: Pathological findings and structure–activity relationships. Handb. Exp. Pharmacol. 2010;195:459–484. doi: 10.1007/978-3-540-79088-4_19. [DOI] [PubMed] [Google Scholar]
- 96.Sessa F., Salerno M., di Mizio G., Bertozzi G., Messina G., Tomaiuolo B., Pisanelli D., Maglietta F., Ricci P., Pomara C. Anabolic androgenic steroids: Searching new molecular biomarkers. Front. Pharmacol. 2018;9:1321. doi: 10.3389/fphar.2018.01321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sebo Z.L., Rodeheffer M.S. Testosterone metabolites differentially regulate obesogenesis and fat distribution. Mol. Metab. 2021;44:101141. doi: 10.1016/j.molmet.2020.101141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pingili A.K., Jennings B.L., Mukherjee K., Akroush W., Gonzalez F.J., Malik K.U. 6β-Hydroxytestosterone, a metabolite of testosterone generated by CYP1B1, contributes to vascular changes in angiotensin II-induced hypertension in male mice. Biol. Sex Differ. 2020;11:4. doi: 10.1186/s13293-019-0280-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Simpson E.R., Clyne C., Rubin G., Boon W.C., Robertson K., Britt K., Speed C., Jones M. Aromatase. A brief overview. Annu. Rev. Physiol. 2002;64:93–127. doi: 10.1146/annurev.physiol.64.081601.142703. [DOI] [PubMed] [Google Scholar]
- 100.Alexander S.P.H., Cidlowski J.A., Kelly E., Mathie A., Peters J.A., Veale E.L., Armstrong J.F., Faccenda E., Harding S.D., Pawson A.J., et al. The concise guide to pharmacology. 2019/20: Nuclear hormone receptors. Br. J. Pharmacol. 2019;176:S229–S246. doi: 10.1111/bph.14750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bleach R., McIlroy M. The divergent function of androgen receptor in breast cancer; analysis of steroid mediators and tumor intracrinology. Front. Endocrinol. 2018;9:594. doi: 10.3389/fendo.2018.00594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Gao W., Bohl C.E., Dalton J.T. Chemistry and structural biology of androgen receptor. Chem. Rev. 2005;105:3352–3370. doi: 10.1021/cr020456u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lu N.Z., Wardell S.E., Burnstein K.L., Defranco D., Fuller P.J., Giguere V., Hochberg R.B., McKay L., Renoir J.-M., Weigel N.L., et al. International Union of Pharmacology. LXV. The pharmacology and classification of the nuclear receptor superfamily: Glucocorticoid, mineralocorticoid, progesterone, and androgen receptors. Pharmacol. Rev. 2006;58:782–797. doi: 10.1124/pr.58.4.9. [DOI] [PubMed] [Google Scholar]
- 104.Gao T., McPhaul M.J. Functional activities of the A and B forms of the human androgen receptor in response to androgen receptor agonists and antagonists. Mol. Endocrinol. 1998;12:654–663. doi: 10.1210/mend.12.5.0112. [DOI] [PubMed] [Google Scholar]
- 105.Davey R.A., Grossmann M. Androgen receptor structure, function and biology: From bench to bedside. Clin. Biochem. Rev. 2016;37:3–15. [PMC free article] [PubMed] [Google Scholar]
- 106.Brinkmann A.O., Faber P.W., van Rooij H.C.J., Kuiper G.G.J.M., Ris C., Klaassen P., van der Korput J.A.G.M., Voorhorst M.M., van Laar J.H., Mulder E., et al. The human androgen receptor: Domain structure, genomic organization and regulation of expression. J. Steroid Biochem. 1989;34:307–310. doi: 10.1016/0022-4731(89)90098-8. [DOI] [PubMed] [Google Scholar]
- 107.McEwan I.J. Molecular mechanisms of androgen receptor-mediated gene regulation: Structure-function analysis of the AF-1 domain. Endocr.-Relat. Cancer. 2004;11:281–293. doi: 10.1677/erc.0.0110281. [DOI] [PubMed] [Google Scholar]
- 108.Verrijdt G. Selective DNA recognition by the androgen receptor as a mechanism for hormone-specific regulation of gene expression. Mol. Genet. Metab. 2003;78:175–185. doi: 10.1016/S1096-7192(03)00003-9. [DOI] [PubMed] [Google Scholar]
- 109.Gelmann E.P. Molecular biology of the androgen receptor. J. Clin. Oncol. 2002;20:3001–3015. doi: 10.1200/JCO.2002.10.018. [DOI] [PubMed] [Google Scholar]
- 110.Shaffer P.L., Jivan A., Dollins D.E., Claessens F., Gewirth D.T. Structural basis of androgen receptor binding to selective androgen response elements. Proc. Natl. Acad. Sci. USA. 2004;101:4758–4763. doi: 10.1073/pnas.0401123101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Takane K.K., McPhaul M.J. Functional analysis of the human androgen receptor promoter. Mol. Cell. Endocrinol. 1996;119:83–93. doi: 10.1016/0303-7207(96)03800-2. [DOI] [PubMed] [Google Scholar]
- 112.Xiao J., Gong A.-Y., Eischeid A.N., Chen D., Deng C., Young C.Y.F., Chen X.-M. miR-141 modulates androgen receptor transcriptional activity in human prostate cancer cells through targeting the small heterodimer partner protein. Prostate. 2012;72:1514–1522. doi: 10.1002/pros.22501. [DOI] [PubMed] [Google Scholar]
- 113.Fujii S., Kagechika H. Androgen receptor modulators: A review of recent patents and reports (2012–2018) Expert Opin. Ther. Pat. 2019;29:439–453. doi: 10.1080/13543776.2019.1618831. [DOI] [PubMed] [Google Scholar]
- 114.Verrijdt G., Schoenmakers E., Haelens A., Peeters B., Verhoeven G., Rombauts W., Claessens F. Change of specificity mutations in androgen-selective enhancers. J. Biol. Chem. 2000;275:12298–12305. doi: 10.1074/jbc.275.16.12298. [DOI] [PubMed] [Google Scholar]
- 115.Hunter I., Hay C.W., Esswein B., Watt K., McEwan I.J. Tissue control of androgen action: The ups and downs of androgen receptor expression. Mol. Cell. Endocrinol. 2018;465:27–35. doi: 10.1016/j.mce.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 116.Jenster G., Trapman J., Brinkmann A.O. Nuclear import of the human androgen receptor. Biochem. J. 1993;293:761–768. doi: 10.1042/bj2930761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cutress M.L., Whitaker H.C., Mills I.G., Stewart M., Neal D.E. Structural basis for the nuclear import of the human androgen receptor. J. Cell Sci. 2008;121:957–968. doi: 10.1242/jcs.022103. [DOI] [PubMed] [Google Scholar]
- 118.Clinckemalie L., Vanderschueren D., Boonen S., Claessens F. The hinge region in androgen receptor control. Mol. Cell. Endocrinol. 2012;358:1–8. doi: 10.1016/j.mce.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 119.Veldscholte J., Berrevoets C.A., Zegers N.D., van der Kwast T.H., Grootegoed J.A., Mulder E. Hormone-induced dissociation of the androgen receptor-heat-shock protein complex: Use of a new monoclonal antibody to distinguish transformed from nontransformed receptors. Biochemistry. 1992;31:7422–7430. doi: 10.1021/bi00147a029. [DOI] [PubMed] [Google Scholar]
- 120.Claessens F., Verrijdt G., Schoenmakers E., Haelens A., Peeters B., Verhoeven G., Rombauts W. Selective DNA binding by the androgen receptor as a mechanism for hormone-specific gene regulation. J. Steroid Biochem. Mol. Biol. 2001;76:23–30. doi: 10.1016/S0960-0760(00)00154-0. [DOI] [PubMed] [Google Scholar]
- 121.Pereira de Jésus-Tran K., Côté P.L., Cantin L., Blanchet J., Labrie F., Breton R. Comparison of crystal structures of human androgen receptor ligand-binding domain complexed with various agonists reveals molecular determinants responsible for binding affinity. Protein Sci. 2006;15:987–999. doi: 10.1110/ps.051905906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Askew E.B., Gampe R.T., Stanley T.B., Faggart J.L., Wilson E.M. Modulation of androgen receptor activation function 2 by testosterone and dihydrotestosterone. J. Biol. Chem. 2007;282:25801–25816. doi: 10.1074/jbc.M703268200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Tan M.E., Li J., Xu H.E., Melcher K., Yong E.-L. Androgen receptor: Structure, role in prostate cancer and drug discovery. Acta Pharmacol. Sin. 2015;36:3–23. doi: 10.1038/aps.2014.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Dehm S.M., Tindall D.J. Androgen receptor structural and functional elements: Role and regulation in prostate cancer. Mol. Endocrinol. 2007;21:2855–2863. doi: 10.1210/me.2007-0223. [DOI] [PubMed] [Google Scholar]
- 125.Azzouni F., Godoy A., Li Y., Mohler J. The 5α-reductase isozyme family: A review of basic biology and their role in human diseases. Adv. Urol. 2012;2012:530121. doi: 10.1155/2012/530121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Dart D.A., Waxman J., Aboagye E.O., Bevan C.L. Visualising androgen receptor activity in male and female mice. PLoS ONE. 2013;8:e71694. doi: 10.1371/journal.pone.0071694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Takeda H., Chodak G., Mutchnik S., Nakamoto T., Chang C. Immunohistochemical localization of androgen receptors with mono- and polyclonal antibodies to androgen receptor. J. Endocrinol. 1990;126:17–25. doi: 10.1677/joe.0.1260017. [DOI] [PubMed] [Google Scholar]
- 128.Shibata N., Nagai K., Morita Y., Ujikawa O., Ohoka N., Hattori T., Koyama R., Sano O., Imaeda Y., Nara H., et al. Development of protein degradation inducers of androgen receptor by conjugation of androgen receptor ligands and inhibitor of apoptosis protein ligands. J. Med. Chem. 2018;61:543–575. doi: 10.1021/acs.jmedchem.7b00168. [DOI] [PubMed] [Google Scholar]
- 129.Li J., White J.T., Saavedra H., Wrabl J.O., Motlagh H.N., Liu K., Sowers J., Schroer T.A., Thompson E.B., Hilser V.J. Genetically tunable frustration controls allostery in an intrinsically disordered transcription factor. eLife. 2017;6:e30688. doi: 10.7554/eLife.30688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.McEwan I.J. Intrinsic disorder in the androgen receptor: Identification, characterisation and drugability. Mol. Biosyst. 2012;8:82–90. doi: 10.1039/C1MB05249G. [DOI] [PubMed] [Google Scholar]
- 131.Southren A.L., Gordon G.G., Tochimoto S., Pinzon G., Lane D.R., Stypulkowski W. Mean plasma concentration, metabolic clearance and basal plasma production rates of testosterone in normal young men and women using a constant infusion procedure: Effect of time of day and plasma concentration on the metabolic clearance rate of testosterone. J. Clin. Endocrinol. 1967;27:686–694. doi: 10.1210/jcem-27-5-686. [DOI] [PubMed] [Google Scholar]
- 132.Vermeulen A., Verdonck L. Studies on the binding of testosterone to human plasma. Steroids. 1968;11:609–635. doi: 10.1016/S0039-128X(68)80009-1. [DOI] [PubMed] [Google Scholar]
- 133.Philip A. Ph.D. Thesis. McGill University; Montreal, QC, Canada: 1988. [(accessed on 27 August 2022)]. Steroid Binding to Sex Hormone-Binding Globulin: Studies on Relative Binding of Estradiol and Testosterone, and Characterization of certain previously unrecognized ligands in pregnancy. Available online: https://escholarship.mcgill.ca/concern/theses/z890rw87g. [Google Scholar]
- 134.Bardin C.W., Musto N., Gunsalus G., Kotite N., Cheng S.L., Larrea F., Becker R. Extracellular androgen binding proteins. Annu. Rev. Physiol. 1981;43:189–198. doi: 10.1146/annurev.ph.43.030181.001201. [DOI] [PubMed] [Google Scholar]
- 135.Baulieu E.-E. Dehydroepiandrosterone (DHEA): A fountain of youth? J. Clin. Endocrinol. Metab. 1996;81:3147–3151. doi: 10.1210/jcem.81.9.8784058. [DOI] [PubMed] [Google Scholar]
- 136.Goodarzi M.O., Korenman S.G. The importance of insulin resistance in polycystic ovary syndrome. Fertil. Steril. 2003;80:255–258. doi: 10.1016/S0015-0282(03)00734-9. [DOI] [PubMed] [Google Scholar]
- 137.Ducluzeau P.H., Cousin P., Malvoisin E., Bornet H., Vidal H., Laville M., Pugeat M. Glucose-to-insulin ratio rather than sex hormone-binding globulin and adiponectin levels is the best predictor of insulin resistance in Nonobese women with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 2003;88:3626–3631. doi: 10.1210/jc.2003-030219. [DOI] [PubMed] [Google Scholar]
- 138.Özturan D., Morova T., Lack N.A. Androgen receptor-mediated transcription in prostate cancer. Cells. 2022;11:898. doi: 10.3390/cells11050898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Choi S.Y., Lim B., Chi B.H., Lee W., Kim J.H., Kyung Y.S., You D., Kim C.-S. The curative effect of androgen deprivation therapy alone is insufficient in high-risk prostate cancer. Medicine. 2021;100:e26833. doi: 10.1097/MD.0000000000026833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Cinar O., Turunc T., Kazaz I.O., Yildirim O., Deliktas H., Cihan A., Gudeloglu A., Ure I., Deveci S., Sahin B., et al. Effects of androgen deprivation therapy on cognitive functions in patients with metastatic prostate cancer: A multicentric, prospective study of the Society of Urological Surgery Andrology group. Int. J. Clin. Pract. 2021;75:e14095. doi: 10.1111/ijcp.14095. [DOI] [PubMed] [Google Scholar]
- 141.Corona G., Filippi S., Bianchi N., Dicuio M., Rastrelli G., Concetti S., Sforza A., Maggi M. Cardiovascular risks of androgen deprivation therapy for prostate cancer. World J. Men’s Health. 2021;39:429–443. doi: 10.5534/wjmh.200109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Lee H.H., Park S., Joung J.Y., Kim S.H., Lee H. How does androgen deprivation therapy affect mental health including cognitive dysfunction in patients with prostate cancer? World J. Men’s Health. 2021;39:598–605. doi: 10.5534/wjmh.200092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Negro-Vilar A. Selective androgen receptor modulators (SARMs): A novel approach to androgen therapy for the new millennium. J. Clin. Endocrinol. Metab. 1999;84:3459–3462. doi: 10.1210/jcem.84.10.6122. [DOI] [PubMed] [Google Scholar]
- 144.Zhi L., Martinborough E. Selective androgen receptor modulators (SARMs) Annu. Rep. Med. Chem. 2001;36:169–180. doi: 10.1016/S0065-7743(01)36057-8. [DOI] [Google Scholar]
- 145.Mohler M.L., Bohl C.E., Jones A., Coss C.C., Narayanan R., He Y., Hwang D.J., Dalton J.T., Miller D.D. Nonsteroidal selective androgen receptor modulators (SARMS): Dissociating the anabolic and androgenic activities of the androgen receptor for therapeutic benefit. J. Med. Chem. 2009;52:3597–3617. doi: 10.1021/jm900280m. [DOI] [PubMed] [Google Scholar]
- 146.Bhasin S., Jasuja R. Selective androgen receptor modulators as function promoting therapies. Curr. Opin. Clin. Nutr. Metab. Care. 2009;12:232–240. doi: 10.1097/MCO.0b013e32832a3d79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Wesley Peixoto da Fonseca G., Dworatzek E., Ebner N., von Haehling S. Selective androgen receptor modulators (SARMs) as pharmacological treatment for muscle wasting in ongoing clinical trials. Expert Opin. Invest. Drugs. 2020;29:881–891. doi: 10.1080/13543784.2020.1777275. [DOI] [PubMed] [Google Scholar]
- 148.Estébanez-Perpiñá E., Bevan C.L., McEwan I.J. Eighty years of targeting androgen receptor activity in prostate cancer: The fight goes on. Cancers. 2021;13:509. doi: 10.3390/cancers13030509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Nyquist M.D., Ang L.S., Corella A., Coleman I.M., Meers M.P., Christiani A.J., Pierce C., Janssens D.H., Meade H.E., Bose A., et al. Selective androgen receptor modulators activate the canonical prostate cancer androgen receptor program and repress cancer growth. J. Clin. Invest. 2021;131:e146777. doi: 10.1172/JCI146777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Schmidt A., Harada S.-I., Kimmel D.B., Bai C., Chen F., Rutledge S.J., Vogel R.L., Scafonas A., Gentile M.A., Nantermet P.V., et al. Identification of anabolic selective androgen receptor modulators with reduced activities in reproductive tissues and sebaceous glands. J. Biol. Chem. 2009;284:36367–36376. doi: 10.1074/jbc.M109.049734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Zhou W., Duan M., Fu W., Pang J., Tang Q., Sun H., Xu L., Chang S., Li D., Hou T. Discovery of novel androgen receptor ligands by structure-based virtual screening and bioassays. Genom. Proteom. Bioinform. 2018;16:416–427. doi: 10.1016/j.gpb.2018.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Forsdahl G., Vatne H.K., Geisendorfer T., Gmeiner G. Screening of testosterone esters in human plasma. Drug Test. Anal. 2013;5:826–833. doi: 10.1002/dta.1560. [DOI] [PubMed] [Google Scholar]
- 153.Borg W., Shackleton C.H.L., Pahuja S.L., Hochberg R.B. Long-lived testosterone esters in the rat. Proc. Natl. Acad. Sci. USA. 1995;92:1545–1549. doi: 10.1073/pnas.92.5.1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Xu S.Y., Zhu B.T., Conney A.H. Effect of clofibrate administration on the esterification and deesterification of steroid hormones by liver and extrahepatic tissues in rats. Biochem. Pharmacol. 2002;63:985–992. doi: 10.1016/S0006-2952(01)00921-2. [DOI] [PubMed] [Google Scholar]
- 155.Remesar X., Fernández-López J.A., Alemany M. Oleoyl-estrone. Med. Res. Rev. 2012;32:1263–1291. doi: 10.1002/med.20240. [DOI] [PubMed] [Google Scholar]
- 156.Bailly J., Raab S., Clerc R., Sebokova E., Krust A., Chambon P. The effect of oleoyl-estrone on body weight is mediated via the alpha estrogen receptor and not the beta estrogen receptor. Obes. Rev. 2005;6:48. [Google Scholar]
- 157.Grasa M.M., Cabot C., Esteve M., Yubero P., Masanés R.M., Blay M.T., Vilà R., López-Martí J., Fernández-López J.A., Remesar X., et al. Daily oral oleoyl-estrone gavage induces a dose-dependent loss of fat in Wistar rats. Obes. Res. 2001;9:202–209. doi: 10.1038/oby.2001.22. [DOI] [PubMed] [Google Scholar]
- 158.Sanchis D., Balada F., Grasa M.M., Virgili J., Peinado J., Monserrat C., Fernández-López J.A., Remesar X., Alemany M. Oleoyl-estrone induces the loss of body fat in rats. Int. J. Obes. 1996;20:588–594. [PubMed] [Google Scholar]
- 159.Badeau M., Vihma V., Mikkola T.S., Tiitinen A., Tikkanen M.J. Estradiol fatty acid esters in adipose tissue and serum of pregnant and pre- and postmenopausal women. J. Clin. Endocrinol. Metab. 2007;92:4327–4331. doi: 10.1210/jc.2007-1372. [DOI] [PubMed] [Google Scholar]
- 160.Mauvais-Jarvis F. Sex differences in metabolic homeostasis, diabetes, and obesity. Biol. Sex Differ. 2015;6:14. doi: 10.1186/s13293-015-0033-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Vourc’h C., Eychenne B., Jo D.-H., Raulin J., Lapous D., Baulieu E.-E., Robel P. Δ5-3β-Hydroxysteroid acyl transferase activity in the rat brain. Steroids. 1992;57:210–215. doi: 10.1016/0039-128X(92)90104-H. [DOI] [PubMed] [Google Scholar]
- 162.Robel P., Bourreau E., Corpéchot C., Dang D.C., Halberg F., Clarke C., Haug M., Schlegel M.L., Synguelakis M., Vourch C., et al. Neuro-steroids: 3β-hydroxy-Δ5-derivatives in rat and monkey brain. J. Steroid Biochem. 1987;27:649–655. doi: 10.1016/0022-4731(87)90133-6. [DOI] [PubMed] [Google Scholar]
- 163.Smith A.J., Watson T.G. The Δ5-3β-hydroxy steroid acyl transferase activities in tissues of the male rat and sheep. Steroids. 1997;62:422–426. doi: 10.1016/S0039-128X(97)00009-3. [DOI] [PubMed] [Google Scholar]
- 164.Nieschlag E., Mauss J., Coert A., Kićović P. Plasma androgen levels in men after oral administration of testosterone or testosterone undecanoate. Acta Endocrinol. 1975;79:366–374. doi: 10.1530/acta.0.0790366. [DOI] [PubMed] [Google Scholar]
- 165.Hammond J., Le Q., Goodyer C., Gelfand M., Trifiro M., LeBlanc A. Testosterone-mediated neuroprotection through the androgen receptor in human primary neurons. J. Neurochem. 2001;77:1319–1326. doi: 10.1046/j.1471-4159.2001.00345.x. [DOI] [PubMed] [Google Scholar]
- 166.Moenter S.M., Chu Z. Rapid nongenomic effects of oestradiol on gonadotrophin-releasing hormone neurones. J. Neuroendocrinol. 2012;24:117–121. doi: 10.1111/j.1365-2826.2011.02135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Schwartz N., Verma A., Bivens C.B., Schwartz Z., Boyan B.D. Rapid steroid hormone actions via membrane receptors. Biochim. Biophys. Acta. 2016;1863:2289–2298. doi: 10.1016/j.bbamcr.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 168.Michels G., Hoppe U.C. Rapid actions of androgens. Front. Neuroendocrinol. 2008;29:182–198. doi: 10.1016/j.yfrne.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 169.Bauer E.R.S., Meyer H.H.D., Stahlschmidt-Allner P., Sauerwein H. Application of an androgen receptor assay for the characterisation of the androgenic or antiandrogenic activity of various phenylurea herbicides and their derivatives. Analyst. 1998;123:2485–2487. doi: 10.1039/a804606i. [DOI] [PubMed] [Google Scholar]
- 170.Shihan M., Bulldan A., Scheiner-Bobis G. Non-classical testosterone signaling is mediated by a G-protein-coupled receptor interacting with Gnα11. Biochim. Biophys. Acta. 2014;1843:1172–1181. doi: 10.1016/j.bbamcr.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 171.Bajpai P., Koc E., Sonpavde G., Singh R., Singh K.K. Mitochondrial localization, import, and mitochondrial function of the androgen receptor. J. Biol. Chem. 2019;294:6621–6634. doi: 10.1074/jbc.RA118.006727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Yager J.D., Chen J.Q. Mitochondrial estrogen receptors-new insights into specific functions. Trends Endocrinol. Metab. 2007;18:89–91. doi: 10.1016/j.tem.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 173.Thomas P. Membrane androgen receptors unrelated to nuclear steroid receptors. Endocrinology. 2019;160:772–781. doi: 10.1210/en.2018-00987. [DOI] [PubMed] [Google Scholar]
- 174.Ding V.D.H., Moller D.E., Feeney W.P., Didolkar V., Nakhla A.M., Rhodes L., Rosner W., Smith R.G. Sex hormone-binding globulin mediates prostate androgen receptor action via a novel signaling pathway. Endocrinology. 1998;139:213–218. doi: 10.1210/endo.139.1.5681. [DOI] [PubMed] [Google Scholar]
- 175.Heinlein C.A., Chang C. The roles of androgen receptors and androgen-binding proteins in nongenomic androgen actions. Mol. Endocrinol. 2002;16:2181–2187. doi: 10.1210/me.2002-0070. [DOI] [PubMed] [Google Scholar]
- 176.Kahn S.M., Hryb D.J., Nakhla A.M., Romas N.A., Rosner W. Beyond carrier proteins: Sex hormone-binding globulin is synthesized in target cells. J. Endocrinol. 2002;175:113–120. doi: 10.1677/joe.0.1750113. [DOI] [PubMed] [Google Scholar]
- 177.Fortunati N., Fissore F., Comba A., Becchis M., Catalano M.G., Fazzari A., Berta L., Frairia R. Sex steroid-binding protein and its membrane receptor in estrogen-dependent breast cancer: Biological and pathophysiological impact. Horm. Res. 1996;45:202–206. doi: 10.1159/000184788. [DOI] [PubMed] [Google Scholar]
- 178.Rosner W., Hryb D.J., Khan M.S., Nakhla A.M., Romas N.A. Sex hormone-binding globulin mediates steroid hormone signal transduction at the plasma membrane. J. Steroid Biochem. Mol. Biol. 1999;69:481–485. doi: 10.1016/S0960-0760(99)00070-9. [DOI] [PubMed] [Google Scholar]
- 179.Navarro G., Xu W., Jacobson D.A., Wicksteed B., Allard C., Zhang G., de Gendt K., Kim H.S., Wu H., Zhang H., et al. Extranuclear actions of the androgen receptor enhance glucose-stimulated insulin secretion in the male. Cell Metab. 2016;23:837–851. doi: 10.1016/j.cmet.2016.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Troncoso M.F., Pavez M., Wilson C., Lagos D., Duran J., Ramos S., Barrientos G., Silva P., Llanos P., Basualto-Alarcón C., et al. Testosterone activates glucose metabolism through AMPK and androgen signaling in cardiomyocyte hypertrophy. Biol. Res. 2021;54:3. doi: 10.1186/s40659-021-00328-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Gatson J.W., Kaur P., Singh M. Dihydrotestosterone differentially modulates the mitogen-activated protein kinase and the phosphoinositide 3-kinase/akt pathways through the nuclear and novel membrane androgen receptor in C6 cells. Endocrinology. 2006;147:2028–2034. doi: 10.1210/en.2005-1395. [DOI] [PubMed] [Google Scholar]
- 182.Thomas P., Pang Y., Dong J. Membrane androgen receptor characteristics of human ZIP9 (SLC39A) zinc transporter in prostate cancer cells: Androgen-specific activation and involvement of an inhibitory G protein in zinc and MAP kinase signaling. Mol. Cell. Endocrinol. 2017;447:23–34. doi: 10.1016/j.mce.2017.02.025. [DOI] [PubMed] [Google Scholar]
- 183.Sun Y.-H., Gao X., Tang Y.-J., Xu C.-L., Wang L.-H. Androgens induce increases in intracellular calcium via a G protein-coupled receptor in LNCaP prostate cancer cells. J. Androl. 2006;27:671–678. doi: 10.2164/jandrol.106.000554. [DOI] [PubMed] [Google Scholar]
- 184.Gorczynska E., Handelsman D.J. Androgens rapidly increase the cytosolic calcium concentration in Sertoli cells. Endocrinology. 1995;136:2052–2059. doi: 10.1210/endo.136.5.7720654. [DOI] [PubMed] [Google Scholar]
- 185.Conde K., Fabelo C., Krause W.C., Propst R., Goethel J., Fischer D., Hur J., Meza C., Ingraham H.A., Wagner E.J. Testosterone rapidly augments retrograde endocannabinoid signaling in proopiomelanocortin neurons to suppress glutamatergic input from steroidogenic factor 1 neurons via upregulation of diacylglycerol lipase-α. Neuroendocrinology. 2017;105:341–356. doi: 10.1159/000453370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Castoria G., Auricchio F., Migliaccio A. Extranuclear partners of androgen receptor: At the crossroads of proliferation, migration, and neuritogenesis. FASEB J. 2017;31:1289–1300. doi: 10.1096/fj.201601047R. [DOI] [PubMed] [Google Scholar]
- 187.Guo Z., Dai B., Jiang T., Xu K., Xie Y., Kim O., Nesheiwat I., Kong X., Melamed J., Handratta V.D., et al. Regulation of androgen receptor activity by tyrosine phosphorylation. Cancer Cell. 2006;10:309–319. doi: 10.1016/j.ccr.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 188.Xu X., de Pergola G., Björntorp P. The effects of androgens on the regulation of lipolysis in adipose precursor cells. Endocrinology. 1990;126:1229–1234. doi: 10.1210/endo-126-2-1229. [DOI] [PubMed] [Google Scholar]
- 189.Benten W.P.M., Lieberherr M., Giese G., Wrehlke C., Stamm O., Sekeris C.E., Mossmann H., Wunderlich F. Functional testosterone receptors in plasma membranes of T cells. FASEB J. 1999;13:123–133. doi: 10.1096/fasebj.13.1.123. [DOI] [PubMed] [Google Scholar]
- 190.Tang J., Chen L.-R., Chen K.-H. The utilization of dehydroepiandrosterone as a sexual hormone precursor in premenopausal and postmenopausal women: An overview. Pharmaceuticals. 2022;15:46. doi: 10.3390/ph15010046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Traish A.M., Kang H.P., Saad F., Guay A.T. Dehydroepiandrosterone (DHEA)—A precursor steroid or an active hormone in human physiology (CME) J. Sex. Med. 2011;8:2960–2982. doi: 10.1111/j.1743-6109.2011.02523.x. [DOI] [PubMed] [Google Scholar]
- 192.Muller C., Hennebert O., Morfin R. The native anti-glucocorticoid paradigm. J. Steroid Biochem. Mol. Biol. 2006;100:95–105. doi: 10.1016/j.jsbmb.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 193.Friess E., Schiffelholz T., Steckler T., Steiger A. Dehydroepiandrosterone—A neurosteroid. Eur. J. Clin. Invest. 2000;30:46–50. doi: 10.1046/j.1365-2362.2000.0300s3046.x. [DOI] [PubMed] [Google Scholar]
- 194.Baulieu E.-E., Robel P. Dehydroepiandrosterone (DHEA) and dehydroepiandrosterone sulfate (DHEAS) as neuroactive neurosteroids. Proc. Natl. Acad. Sci. USA. 1998;95:4089–4091. doi: 10.1073/pnas.95.8.4089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Lazaridis I., Charalampopoulos I., Alexaki V.-I., Avlonitis N., Pediaditakis I., Efstathopoulos P., Calogeropoulou T., Castanas E., Gravanis A. Neurosteroid dehydroepiandrosterone interacts with nerve growth factor (NGF) receptors, preventing neuronal apoptosis. PLoS Biol. 2011;9:e1001051. doi: 10.1371/journal.pbio.1001051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Majewska M.D., Demirgören S., Spivak C.E., London E.D. The neurosteroid dehydroepiandrosterone sulfate is an allosteric antagonist of the GABAA receptor. Brain Res. 1990;526:143–146. doi: 10.1016/0006-8993(90)90261-9. [DOI] [PubMed] [Google Scholar]
- 197.Prough R.A., Clark B.J., Klinge C.M. Novel mechanisms for DHEA action. J. Mol. Endocrinol. 2016;56:R139–R155. doi: 10.1530/JME-16-0013. [DOI] [PubMed] [Google Scholar]
- 198.Cao J., Lu M., Yan W., Li L., Ma H. Dehydroepiandrosterone alleviates intestinal inflammatory damage via GPR30-mediated Nrf2 activation and NLRP3 inflammasome inhibition in colitis mice. Free. Radic. Biol. Med. 2021;172:386–402. doi: 10.1016/j.freeradbiomed.2021.06.025. [DOI] [PubMed] [Google Scholar]
- 199.Dutheil F., de Saint Vincent S., Pereira B., Schmidt J., Moustafa F., Charkhabi M., Bouillon-Minois J.-B., Clinchamps M. DHEA as a biomarker of stress: A systematic review and meta-analysis. Front. Psychiatry. 2021;12:688367. doi: 10.3389/fpsyt.2021.688367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Harada K., Hanayama Y., Obika M., Itoshima K., Okada K., Otsuka F. Involvement of serum dehydroepiandrosterone sulfate in erythropoietic activity. Aging Male. 2020;23:756–763. doi: 10.1080/13685538.2019.1592151. [DOI] [PubMed] [Google Scholar]
- 201.Johnson M.D., Bebb R.A., Sirrs S.M. Uses of DHEA in aging and other disease states. Ageing Res. Rev. 2002;1:29–41. doi: 10.1016/S0047-6374(01)00369-4. [DOI] [PubMed] [Google Scholar]
- 202.Pause B.M. Are androgen steroids acting as pheromones in humans? Physiol. Behav. 2004;83:21–29. doi: 10.1016/S0031-9384(04)00345-2. [DOI] [PubMed] [Google Scholar]
- 203.Kohl J.V., Atzmueller M., Fink B., Grammer K. Human pheromones: Integrating neuroendocrinology and ethology. Neuroendocrinol. Lett. 2011;22:309–321. [PubMed] [Google Scholar]
- 204.Beier K., Ginez I., Schaller H. Localization of steroid hormone receptors in the apocrine sweat glands of the human axilla. Histochem. Cell Biol. 2005;123:61–65. doi: 10.1007/s00418-004-0736-3. [DOI] [PubMed] [Google Scholar]
- 205.Kanlayavattanakul M., Lourith N. Body malodours and their topical treatment agents. Int. J. Cosmet. Sci. 2011;33:298–311. doi: 10.1111/j.1468-2494.2011.00649.x. [DOI] [PubMed] [Google Scholar]
- 206.Voznessenskaya V.V., Klyuchnikova M.A., Wysocki C.J. Roles of the main olfactory and vomeronasal systems in the detection of androstenone in inbred strains of mice. Curr. Zool. 2010;56:813–818. doi: 10.1093/czoolo/56.6.813. [DOI] [Google Scholar]
- 207.Monti-Bloch L., Jennings-White C., Dolberg D.S., Berliner D.L. The human vomeronasal system. Psychoneuroendocrinology. 1994;19:673–686. doi: 10.1016/0306-4530(94)90049-3. [DOI] [PubMed] [Google Scholar]
- 208.Moran D.T., Jafek B.W., Rowley J.C. The vomeronasal (Jacobson’s) organ in man: Ultrastructure and frequency of occurence. J. Steroid Biochem. Mol. Biol. 1991;39:545–552. doi: 10.1016/0960-0760(91)90251-Y. [DOI] [PubMed] [Google Scholar]
- 209.Bhutta M.F. Sex and the nose: Human pheromonal responses. J. R. Soc. Med. 2007;100:268–274. doi: 10.1177/014107680710000612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Rodriguez I., Greer C.A., Mok M.Y., Mombaerts P. A putative pheromone receptor gene expressed in human olfactory mucosa. Nat. Genet. 2000;26:18–19. doi: 10.1038/79124. [DOI] [PubMed] [Google Scholar]
- 211.Takeda S., Kadowaki S., Haga T., Takaesu H., Mitaku S. Identification of G protein-coupled receptor genes from the human genome sequence. FEBS Lett. 2002;520:97–101. doi: 10.1016/S0014-5793(02)02775-8. [DOI] [PubMed] [Google Scholar]
- 212.Yildirim E., Birnbaumer L. TRPC2: Molecular biology and functional importance. Handb. Exp. Pharmacol. 2007;179:53–75. doi: 10.1007/978-3-540-34891-7_3. [DOI] [PubMed] [Google Scholar]
- 213.Restrepo D., Delay R., Lin W., López F., Bacigalupo J. TRP channels in transduction for responses to odorants and pheromones. In: Madrid R., Bacigalupo J., editors. TRP Channels in Sensory Transduction. Springer International Publishing; Cham, Switzerland: 2015. pp. 111–125. [DOI] [Google Scholar]
- 214.Precone V., Paolacci S., Beccari T., Dalla Ragione L., Stuppia L., Baglivo M., Guerri G., Manara E., Tonini G., Herbst K. Pheromone receptors and their putative ligands: Possible role in humans. Eur. Rev. Med. Pharmacol. Sci. 2020;24:2140–2150. doi: 10.26355/eurrev_202002_20394. [DOI] [PubMed] [Google Scholar]
- 215.Kaminski R.M., Marini H., Ortinski P.I., Vicini S., Rogawski M.A. The pheromone androstenol (5α-androst-16-en-3α-ol) is a neurosteroid positive modulator of GABAA receptors. J. Pharmacol. Exp. Ther. 2006;317:694–703. doi: 10.1124/jpet.105.098319. [DOI] [PubMed] [Google Scholar]
- 216.Zhu J., Huang X. Endocrine function of pheromones couples fat rationing and nutrient scarcity. Sci. China-Life Sci. 2022;65:1267–1269. doi: 10.1007/s11427-022-2082-6. [DOI] [PubMed] [Google Scholar]
- 217.Carrier N., Saland S.K., Duclot F., He H., Mercer R., Kabbaj M. The anxiolytic and antidepressant-like effects of testosterone and estrogen in gonadectomized male rats. Biol. Psychiatry. 2015;78:259–269. doi: 10.1016/j.biopsych.2014.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Sierra-Ramírez A., Morato T., Campos R., Rubio I., Calzada C., Méndez E., Ceballos G. Acute effects of testosterone on intracellular Ca2+ kinetics in rat coronary endothelial cells are exerted via aromatization to estrogens. Am. J. Physiol. 2004;287:H63–H71. doi: 10.1152/ajpheart.00784.2003. [DOI] [PubMed] [Google Scholar]
- 219.Ottarsdottir K., Niisson A.G., Heilgren M., Lindblad U., Daka B. The association between serum testosterone and insulin resistance: A longitudinal study. Endocr. Connect. 2018;7:1491–1500. doi: 10.1530/EC-18-0480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Zitzmann M. Testosterone deficiency, insulin resistance and the metabolic syndrome. Nat. Rev. Endocrinol. 2009;5:673–681. doi: 10.1038/nrendo.2009.212. [DOI] [PubMed] [Google Scholar]
- 221.Song D.Z., Arikawa E., Galipeau D.M., Yeh J.N., Battell M.L., Yuen V.G., McNeill J.H. Chronic estrogen treatment modifies insulin-induced insulin resistance and hypertension in ovariectomized rats. Am. J. Hypertens. 2005;18:1189–1194. doi: 10.1016/j.amjhyper.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 222.Corbould A. Chronic testosterone treatment induces selective insulin resistance in subcutaneous adipocytes of women. J. Endocrinol. 2007;192:585–594. doi: 10.1677/joe.1.07070. [DOI] [PubMed] [Google Scholar]
- 223.Gray J.M., Núñez A.A., Siegel L.I., Wade G.N. Effects of testosterone on body weight and adipose tissue: Role of aromatization. Physiol. Behav. 1979;23:465–469. doi: 10.1016/0031-9384(79)90045-3. [DOI] [PubMed] [Google Scholar]
- 224.Geer E.B., Islam J., Buettner C. Mechanisms of glucocorticoid-induced insulin resistance focus on adipose tissue function and lipid metabolism. Endocrinol. Metab. Clin. N. Am. 2014;43:75–102. doi: 10.1016/j.ecl.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Pinto A., Malacrida B., Oieni J., Serafini M.M., Davin A., Galbiati V., Corsini E., Racchi M. DHEA modulates the effect of cortisol on RACK1 expression via interference with the splicing of the glucocorticoid receptor. Br. J. Pharmacol. 2015;172:2918–2927. doi: 10.1111/bph.13097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Welsh T.H., Bambino T.H., Hsueh A.J.W. Mechanism of glucocorticoid-induced suppression of testicular androgen biosynthesis in vitro. Biol. Reprod. 1982;27:1138–1146. doi: 10.1095/biolreprod27.5.1138. [DOI] [PubMed] [Google Scholar]
- 227.Alemany M. Do the interactions between glucocorticoids and sex hormones regulate the development of the metabolic syndrome? Front. Endocrinol. 2012;3:27. doi: 10.3389/fendo.2012.00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Ren L., Zhang Y., Xin Y., Chen G., Sun X., Chen Y., He B. Dysfunction in Sertoli cells participates in glucocorticoid-induced impairment of spermatogenesis. Mol. Reprod. Dev. 2021;88:405–415. doi: 10.1002/mrd.23515. [DOI] [PubMed] [Google Scholar]
- 229.Turcu A.F., Nanba A.T., Chomic R., Upadhyay S.K., Giordano T.J., Shields J.J., Merke D.P., Rainey W.E., Auchus R.J. Adrenal-derived 11-oxygenated 19-carbon steroids are the dominant androgens in classic 21-hydroxylase deficiency. Eur. J. Endocrinol. 2016;174:601–609. doi: 10.1530/EJE-15-1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Stárka L., Dušková M., Vítků J. 11-Keto-testosterone and other androgens of adrenal origin. Physiol. Res. 2020;69:S187–S192. doi: 10.33549/physiolres.934516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Gomez-Sanchez E.P., Gomez-Sanchez C.E. 11β-hydroxysteroid dehydrogenases: A growing multi-tasking family. Mol. Cell. Endocrinol. 2021;526:111210. doi: 10.1016/j.mce.2021.111210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Handelsman D.J., Cooper E.R., Heather A.K. Bioactivity of 11 keto and hydroxy androgens in yeast and mammalian host cells. J. Steroid Biochem. Mol. Biol. 2022;218:106049. doi: 10.1016/j.jsbmb.2021.106049. [DOI] [PubMed] [Google Scholar]
- 233.Mindnich R., Möller G., Adamski J. The role of 17 beta-hydroxysteroid dehydrogenases. Mol. Cell. Endocrinol. 2004;218:7–20. doi: 10.1016/j.mce.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 234.Draper N., Stewart P.M. 11β-Hydroxysteroid dehydrogenase and the pre-receptor regulation of corticosteroid hormone action. J. Endocrinol. 2005;186:251–271. doi: 10.1677/joe.1.06019. [DOI] [PubMed] [Google Scholar]
- 235.Gibney J., Wolthers T., Johannsson G., Umpleby A.M., Ho K.K.Y. Growth hormone and testosterone interact positively to enhance protein and energy metabolism in hypopituitary men. Am. J. Physiol. 2005;289:E266–E271. doi: 10.1152/ajpendo.00483.2004. [DOI] [PubMed] [Google Scholar]
- 236.Kraemer W.J., Ratamess N.A., Hymer W.C., Nindl B.C., Fragala M.S. Growth hormone(s), testosterone, insulin-like growth factors, and cortisol: Roles and integration for cellular development and growth with exercise. Front. Endocrinol. 2020;11:33. doi: 10.3389/fendo.2020.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Mazziotti G., Giustina A. Glucocorticoids and the regulation of growth hormone secretion. Nat. Rev. Endocrinol. 2013;9:265–276. doi: 10.1038/nrendo.2013.5. [DOI] [PubMed] [Google Scholar]
- 238.Lam T., Poljak A., McLean M., Bahl N., Ho K.K.Y., Birzniece V. Testosterone prevents protein loss via the hepatic urea cycle in human. Eur. J. Endocrinol. 2017;176:489–496. doi: 10.1530/EJE-16-0868. [DOI] [PubMed] [Google Scholar]
- 239.Nasiri M., Nikolaou N., Parajes S., Krone N.P., Valsamakis G., Mastorakos G., Hughes B., Taylor A., Bujalska I.J., Gathercole L.L., et al. 5α-Reductase type 2 regulates glucocorticoid action and metabolic phenotype in human hepatocytes. Endocrinology. 2015;156:2863–2871. doi: 10.1210/en.2015-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Qin D.D., Rizak J., Feng X.L., Yang S.C., Lu L.B., Pan L., Yin Y., Hu X.T. Prolonged secretion of cortisol as a possible mechanism underlying stress and depressive behaviour. Sci. Rep. 2016;6:30187. doi: 10.1038/srep30187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Zunszain P.A., Anacker C., Cattaneo A., Carvalho L.A., Pariante C.M. Glucocorticoids, cytokines and brain abnormalities in depression. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2011;35:722–729. doi: 10.1016/j.pnpbp.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Kong X.C., Yu J., Bi J.H., Qi H.M., Di W.J., Wu L., Wang L., Zha J.M., Lv S., Zhang F., et al. Glucocorticoids transcriptionally regulate miR-27b expression promoting body fat accumulation via suppressing the browning of white adipose tissue. Diabetes. 2015;64:393–404. doi: 10.2337/db14-0395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Holt H.B., Wild S.H., Postle A.D., Zhang J., Koster G., Umpleby M., Shojaee-Moradie F., Dewbury K., Wood P.J., Phillips D.I., et al. Cortisol clearance and associations with insulin sensitivity, body fat and fatty liver in middle-aged men. Diabetologia. 2007;50:1024–1032. doi: 10.1007/s00125-007-0629-9. [DOI] [PubMed] [Google Scholar]
- 244.Burt M.G., Gibney J., Ho K.K.Y. Protein metabolism in glucocorticoid excess: Study in Cushing’s syndrome and the effect of treatment. Am. J. Physiol. 2007;292:E1426–E1432. doi: 10.1152/ajpendo.00524.2006. [DOI] [PubMed] [Google Scholar]
- 245.Griggs R.C., Kingston W., Jozefowicz R.F., Herr B.E., Forbes G., Halliday D. Effect of testosterone on muscle mass and muscle protein synthesis. J. Appl. Physiol. 1989;66:498–503. doi: 10.1152/jappl.1989.66.1.498. [DOI] [PubMed] [Google Scholar]
- 246.Wang R.X., Jiao H.C., Zhao J.P., Wang X.J., Lin H. Glucocorticoids enhance muscle proteolysis through a myostatin-dependent pathway at the early stage. PLoS ONE. 2016;11:e0156225. doi: 10.1371/journal.pone.0156225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Tiao G., Fagan J., Roegner V., Lieberman M., Wang J.J., Fischer J.E., Hasselgren P.-O. Energy-ubiquitin-dependent muscle proteolysis during sepsis in rats is regulated by glucocorticoids. J. Clin. Invest. 1996;97:339–348. doi: 10.1172/JCI118421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Bouman A., Schipper M., Heineman M.J., Faas M.M. Gender difference in the non-specific and specific immune response in humans. Am. J. Reprod. Immunol. 2004;52:19–26. doi: 10.1111/j.1600-0897.2004.00177.x. [DOI] [PubMed] [Google Scholar]
- 249.Boonekamp J.J., Ros A.H.F., Verhulst S. Immune activation suppresses plasma testosterone level: A meta-analysis. Biol. Lett. 2008;4:741–744. doi: 10.1098/rsbl.2008.0347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Trigunaite A., Dimo J., Jørgensen T.N. Suppressive effects of androgens on the immune system. Cell. Immunol. 2015;294:87–94. doi: 10.1016/j.cellimm.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 251.Cain D.W., Cidlowski J.A. Immune regulation by glucocorticoids. Nat. Rev. Immunol. 2017;17:233–247. doi: 10.1038/nri.2017.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Franchimont D. Overview of the actions of glucocorticoids on the immune response. A good model to characterize new pathways of immunosuppression for new treatment strategies. Ann. N. Y. Acad. Sci. 2004;1024:124–137. doi: 10.1196/annals.1321.009. [DOI] [PubMed] [Google Scholar]
- 253.Machado Xavier A., Olimpio Anunciato A.K., Rosado Rosenstock T., Glezer I. Gene expression control by glucocorticoid receptors during innate immune responses. Front. Endocrinol. 2016;7:31. doi: 10.3389/fendo.2016.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Oppong E., Cato A.C.B. Effects of glucocorticoids in the immune system. Adv. Exp. Med. Biol. 2015;872:217–233. doi: 10.1007/978-1-4939-2895-8_9. [DOI] [PubMed] [Google Scholar]
- 255.Walker W.H., Cheng J. FSH and testosterone signaling in Sertoli cells. Reproduction. 2005;130:15–28. doi: 10.1530/rep.1.00358. [DOI] [PubMed] [Google Scholar]
- 256.Walker W.H. Non-classical actions of testosterone and spermatogenesis. Phil. Trans. R. Soc. B. 2010;365:1557–1569. doi: 10.1098/rstb.2009.0258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Dimitriadis F., Tsiampali C., Chaliasos N., Tsounapi P., Takenaka A., Sofikitis N. The Sertoli cell as the orchestra conductor of spermatogenesis: Spermatogenic cells dance to the tune of testosterone. Hormones. 2015;14:479–503. doi: 10.14310/horm.2002.1633. [DOI] [PubMed] [Google Scholar]
- 258.Ramaswamy S., Weinbauer G.F. Endocrine control of spermatogenesis: Role of FSH and LH/ testosterone. Spermatogenesis. 2014;4:e996025. doi: 10.1080/21565562.2014.996025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Dierich A., Sairam M.R., Monaco L., Fimia G.M., Gansmuller A., LeMeur M., Sassone-Corsi P. Impairing follicle-stimulating hormone (FSH) signaling in vivo: Targeted disruption of the FSH receptor leads to aberrant gametogenesis and hormonal imbalance. Proc. Natl. Acad. Sci. USA. 1998;95:13612–13617. doi: 10.1073/pnas.95.23.13612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Wilson J.D., Griffin J.E., Leshin M., George F.W. Role of gonadal hormones in development of the sexual phenotypes. Hum. Genet. 1981;58:78–84. doi: 10.1007/BF00284153. [DOI] [PubMed] [Google Scholar]
- 261.Marchetti P.M., Barth J.H. Clinical biochemistry of dihydrotestosterone. Ann. Clin. Biochem. 2013;50:95–107. doi: 10.1258/acb.2012.012159. [DOI] [PubMed] [Google Scholar]
- 262.McGinnis M.Y., Dreifuss R.M. Evidence for a role of testosterone-androgen receptor interactions in mediating masculine sexual behavior in male rats. Endocrinology. 1989;124:618–626. doi: 10.1210/endo-124-2-618. [DOI] [PubMed] [Google Scholar]
- 263.Sinisi A.A., Pasquali D., Notaro A., Bellastella A. Sexual differentiation. J. Endocrinol. Invest. 2003;26:23–28. [PubMed] [Google Scholar]
- 264.Okeigwe I., Kuohung W. 5-Alpha reductase deficiency: A 40-year retrospective review. Curr. Opin. Endocrinol. Diabetes Obes. 2014;21:483–487. doi: 10.1097/MED.0000000000000116. [DOI] [PubMed] [Google Scholar]
- 265.Kang H.-J., Imperato-Mcginley J., Zhu Y.-S., Rosenwaks Z. The effect of 5α-reductase-2 deficiency on human fertility. Fertil. Steril. 2014;101:310–316. doi: 10.1016/j.fertnstert.2013.11.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Schulster M., Bernie A.M., Ramasamy R. The role of estradiol in male reproductive function. Asian J. Androl. 2016;18:435–440. doi: 10.4103/1008-682X.173932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.O’Donnell L., Robertson K.M., Jones M.E., Simpson E.R. Estrogen and Spermatogenesis. Endocr. Rev. 2001;22:289–318. doi: 10.1210/edrv.22.3.0431. [DOI] [PubMed] [Google Scholar]
- 268.Banner A., Frumin I., Shamay-Tsoory S.G. Androstadienone, a chemosignal found in human sweat, increases individualistic behavior and decreases cooperative responses in men. Chem. Senses. 2018;43:189–196. doi: 10.1093/chemse/bjy002. [DOI] [PubMed] [Google Scholar]
- 269.Bone C., Anderson C., Lou Y., Squires E.J. The characterization of androstenone transport in boar plasma. J. Steroid Biochem. Mol. Biol. 2019;185:218–224. doi: 10.1016/j.jsbmb.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 270.Brain P.F. Androgens and human behaviour: A complex relationship. Behav. Brain Sci. 1998;21:363–364. doi: 10.1017/S0140525X98231220. [DOI] [Google Scholar]
- 271.Simmons Z.L., Roney J.R. Variation in CAG repeat length of the androgen receptor gene predicts variables associated with intrasexual competitiveness in human males. Horm. Behav. 2011;60:306–312. doi: 10.1016/j.yhbeh.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 272.Sherwin B.B. A comparative analysis of the role of androgen in human male and female sexual behavior: Behavioral specificity, critical thresholds, and sensitivity. Psychobiology. 1988;16:416–425. doi: 10.3758/BF03327339. [DOI] [Google Scholar]
- 273.Roney J.R., Gettler L.T. The role of testosterone in human romantic relationships. Curr. Opin. Psychol. 2015;1:81–86. doi: 10.1016/j.copsyc.2014.11.003. [DOI] [Google Scholar]
- 274.Ketay S., Welker K.M., Slatcher R.B. The roles of testosterone and cortisol in friendship formation. Psychoneuroendocrinology. 2017;76:88–96. doi: 10.1016/j.psyneuen.2016.11.022. [DOI] [PubMed] [Google Scholar]
- 275.Ponzi D., Dandy M. The influence of endogenous opioids on the relationship between testosterone and romantic bonding. Hum. Nat. 2019;30:98–116. doi: 10.1007/s12110-018-9332-4. [DOI] [PubMed] [Google Scholar]
- 276.Jiang Y., Sheng F., Belkaya N., Platt M.L. Oxytocin and testosterone administration amplify viewing preferences for sexual images in male rhesus macaques. Philos. Trans. R. Soc. B. 2022;377:20210133. doi: 10.1098/rstb.2021.0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Grebe N.M., Sarafin R.E., Strenth C.R., Zilioli S. Pair-bonding, fatherhood, and the role of testosterone: A meta-analytic review. Neurosci. Biobehav. Rev. 2019;98:221–233. doi: 10.1016/j.neubiorev.2019.01.010. [DOI] [PubMed] [Google Scholar]
- 278.Bakermans-Kranenburg M.J., Verhees M.W.F.T., Lotz A.M., Alyousefi-van Dijk K., van IJzendoorn M.H. Is paternal oxytocin an oxymoron? Oxytocin, vasopressin, testosterone, oestradiol and cortisol in emerging fatherhood. Phil. Trans. R. Soc. B. 2022;377 doi: 10.1098/rstb.2021.0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Gettler L.T., Kuo P.X., Sarma M.S., Trumble B.C., Burke Lefever J.E., Braungart-Rieker J.M. Fathers’ oxytocin responses to first holding their newborns: Interactions with testosterone reactivity to predict later parenting behavior and father-infant bonds. Dev. Psychobiol. 2021;63:1384–1398. doi: 10.1002/dev.22121. [DOI] [PubMed] [Google Scholar]
- 280.Mazur A., Booth A. Testosterone and dominance in men. Behav. Brain Sci. 1998;21:353–397. doi: 10.1017/S0140525X98001228. [DOI] [PubMed] [Google Scholar]
- 281.Pluchino N., Drakopoulos P., Bianchi-Demicheli F., Wenger J.M., Petignat P., Genazzani A.R. Neurobiology of DHEA and effects on sexuality, mood and cognition. J. Steroid Biochem. Mol. Biol. 2015;145:273–280. doi: 10.1016/j.jsbmb.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 282.Spark R.F. Dehydroepiandrosterone: A springboard hormone for female sexuality. Fertil. Steril. 2002;77:19–25. doi: 10.1016/S0015-0282(02)02987-4. [DOI] [PubMed] [Google Scholar]
- 283.Rothman M.S., Carlson N.E., Xu M., Wang C., Swerdloff R., Lee P., Goh V.H.H., Ridgway E.C., Wierman M.E. Reexamination of testosterone, dihydrotestosterone, estradiol and estrone levels across the menstrual cycle and in postmenopausal women measured by liquid chromatography–tandem mass spectrometry. Steroids. 2011;76:177–182. doi: 10.1016/j.steroids.2010.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Chrousos G.P., Peck G.L., Gross E.G., Cutler G.B., Loriaux D.L. Adrenal function in women with idiopathic acne. J. Invest. Dermatol. 1982;78:468–471. doi: 10.1111/1523-1747.ep12510160. [DOI] [PubMed] [Google Scholar]
- 285.Mannerås L., Cajander S., Holmäng A., Seleskovic Z., Lystig T., Lönn M., Stener-Victorin E. A new rat model exhibiting both ovarian and metabolic characteristics of polycystic ovary syndrome. Endocrinology. 2007;148:3781–3791. doi: 10.1210/en.2007-0168. [DOI] [PubMed] [Google Scholar]
- 286.Rastrelli G., Corona G., Maggi M. Testosterone and sexual function in men. Maturitas. 2018;112:46–52. doi: 10.1016/j.maturitas.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 287.Davis S.R., Tran J. Testosterone influences libido and well being in women. Trends Endocrinol. Metab. 2001;12:33–37. doi: 10.1016/S1043-2760(00)00333-7. [DOI] [PubMed] [Google Scholar]
- 288.Wåhlin-Jacobsen S., Tønnes Pedersen A., Kristensen E., Læssøe N.C., Lundqvist M., Cohen A.S., Hougaard D.M., Giraldi A. Is there a correlation between androgens and sexual desire in women? J. Sex. Med. 2015;12:358–373. doi: 10.1111/jsm.12774. [DOI] [PubMed] [Google Scholar]
- 289.Caron P., Turcotte V., Guillemette C. A quantitative analysis of total and free 11-oxygenated androgens and its application to human serum and plasma specimens using liquid-chromatography tandem mass spectrometry. J. Chromatogr. A. 2021;1650:462228. doi: 10.1016/j.chroma.2021.462228. [DOI] [PubMed] [Google Scholar]
- 290.Hulshoff Pol H.E., Cohen-Kettenis P.T., van Haren N.E.M., Peper J.S., Brans R.G.H., Cahn W., Schnack H.G., Gooren L.J.G., Kahn R.S. Changing your sex changes your brain: Influences of testosterone and estrogen on adult human brain structure. Eur. J. Endocrinol. 2006;155:S107–S114. doi: 10.1530/eje.1.02248. [DOI] [Google Scholar]
- 291.Lombardo M.V., Ashwin E., Auyeung B., Chakrabarti B., Taylor K., Hackett G., Bullmore E.T., Baron-Cohen S. Fetal testosterone influences sexually dimorphic gray matter in the human brain. J. Neurosci. 2012;32:674–680. doi: 10.1523/JNEUROSCI.4389-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Celec P., Ostatníková D., Hodosy J. On the effects of testosterone on brain behavioral functions. Front. Neurosci. 2015;9:12. doi: 10.3389/fnins.2015.00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Savic I., Frisen L., Manzouri A., Nordenstrom A., Lindén Hirschberg A. Role of testosterone and Y chromosome genes for the masculinization of the human brain. Hum. Brain Mapp. 2017;38:1801–1814. doi: 10.1002/hbm.23483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Soma K.K., Rendon N.M., Boonstra R., Albers H.E., Demas G.E. DHEA effects on brain and behavior: Insights from comparative studies of aggression. J. Steroid Biochem. Mol. Biol. 2015;145:261–272. doi: 10.1016/j.jsbmb.2014.05.011. [DOI] [PubMed] [Google Scholar]
- 295.Maggio M., de Vita F., Fisichella A., Colizzi E., Provenzano S., Lauretani F., Luci M., Ceresini G., dall’Aglio E., Caffarra P., et al. DHEA and cognitive function in the elderly. J. Steroid Biochem. Mol. Biol. 2015;145:281–292. doi: 10.1016/j.jsbmb.2014.03.014. [DOI] [PubMed] [Google Scholar]
- 296.Stoffel-Wagner B. Neurosteroid metabolism in the human brain. Eur. J. Endocrinol. 2001;145:669–680. doi: 10.1530/eje.0.1450669. [DOI] [PubMed] [Google Scholar]
- 297.Cumberland A.L., Hirst J.J., Badoer E., Wudy S.A., Greaves R.F., Zacharin M., Walker D.W. The enigma of the adrenarche: Identifying the early life mechanisms and possible role in postnatal brain development. Int. J. Mol. Sci. 2021;22:4296. doi: 10.3390/ijms22094296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Zirkin B.R., Tenover J.L. Aging and declining testosterone: Past, present, and hopes for the future. J. Androl. 2012;33:1111–1118. doi: 10.2164/jandrol.112.017160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Yuki A., Otsuka R., Kozakai R., Kitamura I., Okura T., Ando F., Shimokata H. Relationship between low free testosterone levels and loss of muscle mass. Sci. Rep. 2013;3:1818. doi: 10.1038/srep01818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Moctezuma-Velazquez C., Low G., Mourtzakis M., Ma M., Burak K.W., Tandon P., Montano-Loza A.J. Association between low testosterone levels and sarcopenia in cirrhosis: A cross-sectional study. Ann. Hepatol. 2018;17:615–623. doi: 10.5604/01.3001.0012.0930. [DOI] [PubMed] [Google Scholar]
- 301.Rodrigues dos Santos M., Storer T.W. Testosterone treatment as a function-promoting therapy in sarcopenia associated with aging and chronic disease. Endocrinol. Metab. Clin. N. Am. 2022;51:187–204. doi: 10.1016/j.ecl.2021.11.012. [DOI] [PubMed] [Google Scholar]
- 302.Sinclair M., Grossmann M., Hoermann R., Angus P.W., Gow P.J. Testosterone therapy increases muscle mass in men with cirrhosis and low testosterone: A randomised controlled trial. J. Hepatol. 2016;65:906–913. doi: 10.1016/j.jhep.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 303.Urban R.J., Bodenburg Y.H., Gilkison C., Foxworth J., Coggan A.R., Wolfe R.R., Ferrando A. Testosterone administration to elderly men increases skeletal muscle strength and protein synthesis. Am. J. Physiol. 1995;269:E820–E826. doi: 10.1152/ajpendo.1995.269.5.E820. [DOI] [PubMed] [Google Scholar]
- 304.Pal M., Khan J., Kumar R., Surolia A., Gupta S. Testosterone supplementation improves insulin responsiveness in HFD fed male T2DM mice and potentiates insulin signaling in the skeletal muscle and C2C12 myocyte cell line. PLoS ONE. 2019;14:e0224162. doi: 10.1371/journal.pone.0224162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Giannoulis M.G., Jackson N., Shojaee-Moradie F., Nair K.S., Sonksen P.H., Martin F.C., Umpleby A.M. The effects of growth hormone and/or testosterone on whole body protein kinetics and skeletal muscle gene expression in healthy elderly men: A randomized controlled trial. J. Clin. Endocrinol. Metab. 2008;93:3066–3074. doi: 10.1210/jc.2007-2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Gharahdaghi N., Phillips B.E., Szewczyk N.J., Smith K., Wilkinson D.J., Atherton P.J. Links between testosterone, oestrogen, and the growth hormone/insulin-like growth factor axis and resistance exercise muscle adaptations. Front. Physiol. 2021;11:621226. doi: 10.3389/fphys.2020.621226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Ferrando A.A., Sheffield-Moore M., Yeckel C.W., Gilkison C., Jiang J., Achacosa A., Lieberman S.A., Tipton K., Wolfe R.R., Urban R.J. Testosterone administration to older men improves muscle function: Molecular and physiological mechanisms. Am. J. Physiol. 2002;282:E601–E607. doi: 10.1152/ajpendo.00362.2001. [DOI] [PubMed] [Google Scholar]
- 308.Kruse R., Petersson S.J., Christensen L.L., Kristensen J.M., Sabaratnam R., Ørtenblad N., Andersen M., Højlund K. Effect of long-term testosterone therapy on molecular regulators of skeletal muscle mass and fibre-type distribution in aging men with subnormal testosterone. Metab.-Clin. Exp. 2020;112:154347. doi: 10.1016/j.metabol.2020.154347. [DOI] [PubMed] [Google Scholar]
- 309.Kovacheva E.L., Hikim A.P.S., Shen R.Q., Sinha I., Sinha-Hikim I. Testosterone supplementation reverses sarcopenia in aging through regulation of myostatin, c-Jun NH2-terminal kinase, Notch, and Akt signaling pathways. Endocrinology. 2010;151:628–638. doi: 10.1210/en.2009-1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Wendowski O., Redshaw Z., Mutungi G. Dihydrotestosterone treatment rescues the decline in protein synthesis as a result of sarcopenia in isolated mouse skeletal muscle fibres. J. Cachexia Sarcopenia Muscle. 2017;8:48–56. doi: 10.1002/jcsm.12122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Basaria S., Coviello A.D., Travison T.G., Storer T.W., Farwell W.R., Jette A.M., Eder R., Tennstedt S., Ulloor J., Zhang A., et al. Adverse events associated with testosterone administration. N. Engl. J. Med. 2010;363:109–122. doi: 10.1056/NEJMoa1000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Evans N.A. Current concepts in anabolic-androgenic steroids. Am. J. Sport. Med. 2004;32:534–542. doi: 10.1177/0363546503262202. [DOI] [PubMed] [Google Scholar]
- 313.Nordström A., Hogström G., Eriksson A., Bonnerud P., Tegner Y., Malm C. Higher muscle mass but lower gynoid fat mass in athletes using anabolic androgenic steroids. J. Strength Cond. Res. 2012;26:246–250. doi: 10.1519/JSC.0b013e318218daf0. [DOI] [PubMed] [Google Scholar]
- 314.Kanayama G., Brower K.J., Wood R.I., Hudson J.I., Pope Jr H.G. Anabolic-androgenic steroid dependence: An emerging disorder. Addiction. 2009;104:1966–1978. doi: 10.1111/j.1360-0443.2009.02734.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Nottin S., Nguyen L.D., Terbah M., Obert P. Cardiovascular effects of androgenic anabolic steroids in male bodybuilders determined by tissue Doppler imaging. Am. J. Cardiol. 2006;97:912–915. doi: 10.1016/j.amjcard.2005.10.026. [DOI] [PubMed] [Google Scholar]
- 316.Mauras N., Rini A., Welch S., Sager B., Murphy S.P. Synergistic effects of testosterone and growth hormone on protein metabolism and body composition in prepubertal boys. Metabolism. 2003;52:964–969. doi: 10.1016/S0026-0495(03)00163-X. [DOI] [PubMed] [Google Scholar]
- 317.Simon D., Charles M.-A., Lahlou N., Nahoul K., Oppert J.-M., Gouault-Heilmann M., Lemort N., Thibult N., Joubert E., Balkau B., et al. Androgen therapy improves insulin sensitivity and decreases leptin level in healthy adult men with low plasma total testosterone. Diabetes Care. 2001;24:2149. doi: 10.2337/diacare.24.12.2149. [DOI] [PubMed] [Google Scholar]
- 318.Dhindsa S., Ghanim H., Batra M., Kuhadiya N.D., Abuaysheh S., Sandhu S., Green K., Makdissi A., Hejna J., Chaudhuri A., et al. Insulin resistance and inflammation in hypogonadotropic hypogonadism and their reduction after testosterone replacement in men with type 2 diabetes. Diabetes Care. 2016;39:82–91. doi: 10.2337/dc15-1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.D’Andrea S., Martorella A., Coccia F., Castellini C., Minaldi E., Totaro M., Parisi A., Francavilla F., Francavilla S., Barbonetti A. Relationship of vitamin D status with testosterone levels: A systematic review and meta-analysis. Endocrine. 2021;72:49–61. doi: 10.1007/s12020-020-02482-3. [DOI] [PubMed] [Google Scholar]
- 320.Bianchi V.E. The anti inflammatory effects of testosterone. J. Endocr. Soc. 2019;3:91–107. doi: 10.1210/js.2018-00186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Srinivas-Shankar U., Wu F.C.W. Drug insight: Testosterone preparations. Nat. Clin. Pract. Urol. 2006;3:653–665. doi: 10.1038/ncpuro0650. [DOI] [PubMed] [Google Scholar]
- 322.Fui M.N.T., Hoermann R., Cheung A.S., Gianatti E.J., Zajac J.D., Grossmann M. Obesity and age as dominant correlates of low testosterone in men irrespective of diabetes status. Andrology. 2013;1:906–912. doi: 10.1111/j.2047-2927.2013.00124.x. [DOI] [PubMed] [Google Scholar]
- 323.Haring R., Völzke H., Felix S.B., Schipf S., Dörr M., Rosskopf D., Nauck M., Schöfl C., Wallaschofski H. Prediction of metabolic syndrome by low serum testosterone levels in men results from the study of health in Pomerania. Diabetes. 2009;58:2027–2031. doi: 10.2337/db09-0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Frederiksen L., Højlund K., Hougaard D.M., Mosbech T.H., Larsen R., Flyvbjerg A., Frystyk J., Brixen K., Andersen M. Testosterone therapy decreases subcutaneous fat and adiponectin in aging men. Eur. J. Endocrinol. 2012;166:469–476. doi: 10.1530/EJE-11-0565. [DOI] [PubMed] [Google Scholar]
- 325.Jones T.H., Arver S., Behre H.M., Buvat J., Meuleman E., Moncada I., Morales A.M., Volterrani M., Yellowlees A., Howell J.D., et al. Testosterone replacement in hypogonadal men with type 2 diabetes and/or metabolic syndrome (the TIMES2 Study) Diabetes Care. 2011;34:828–837. doi: 10.2337/dc10-1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Steidle C., Schwartz S., Jacoby K., Sebree T., Smith T., Bachand R. AA2500 Testosterone gel normalizes androgen levels in aging males with improvements in body composition and sexual function. J. Clin. Endocrinol. Metab. 2003;88:2673–2681. doi: 10.1210/jc.2002-021058. [DOI] [PubMed] [Google Scholar]
- 327.Canguven O., Talib R.A., El Ansari W., Yassin D.J., Salman M., Al-Ansari A. Testosterone therapy has positive effects on anthropometric measures, metabolic syndrome components (obesity, lipid profile, Diabetes Mellitus control), blood indices, liver enzymes, and prostate health indicators in elderly hypogonadal men. Andrologia. 2017;49:e12768. doi: 10.1111/and.12768. [DOI] [PubMed] [Google Scholar]
- 328.Haider A., Saad F., Doros G., Gooren L. Hypogonadal obese men with and without diabetes mellitus type 2 lose weight and show improvement in cardiovascular risk factors when treated with testosterone: An observational study. Obes. Res. Clin. Pract. 2014;8:e339–e349. doi: 10.1016/j.orcp.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 329.Mårin P., Holmang S., Jonsson L., Sjostrom L., Kvist H., Holm G., Lindstedt G., Björntorp P. The effects of testosterone treatment on body-composition and metabolism in middle-aged obese men. Int. J. Obes. 1992;16:991–997. [PubMed] [Google Scholar]
- 330.Reddy K.C.O., Yadav S.B. Effect of testosterone replacement therapy on insulin sensitivity and body composition in congenital hypogonadism: A prospective longitudinal follow-up study. J. Postgrad. Med. 2021;67:67–74. doi: 10.4103/jpgm.JPGM_887_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Rochira V., Balestrieri A., Madeo B., Zirilli L., Granata A.R.M., Carani C. Osteoporosis and male age-related hypogonadism: Role of sex steroids on bone (patho)physiology. Eur. J. Endocrinol. 2006;154:175–185. doi: 10.1530/eje.1.02088. [DOI] [PubMed] [Google Scholar]
- 332.Grossmann M., Thomas M.C., Panagiotopoulos S., Sharpe K., MacIsaac R.J., Clarke S., Zajac J.D., Jerums G. Low testosterone levels are common and associated with insulin resistance in men with diabetes. J. Clin. Endocrinol. Metab. 2008;93:1834–1840. doi: 10.1210/jc.2007-2177. [DOI] [PubMed] [Google Scholar]
- 333.Traish A.M., Saad F., Guay A. The dark side of testosterone deficiency: II. Type 2 diabetes and insulin resistance. J. Androl. 2009;30:23–32. doi: 10.2164/jandrol.108.005751. [DOI] [PubMed] [Google Scholar]
- 334.Pal M., Gupta S. Testosterone supplementation improves glucose homeostasis despite increasing hepatic insulin resistance in male mouse model of type 2 diabetes mellitus. Nutr. Diabetes. 2016;6:e236. doi: 10.1038/nutd.2016.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Heufelder A.E., Saad F., Bunck M.C., Gooren L. Fifty-two-week treatment with diet and exercise plus transdermal testosterone reverses the metabolic syndrome and improves glycemic control in men with newly diagnosed type 2 diabetes and subnormal plasma testosterone. J. Androl. 2009;30:726–733. doi: 10.2164/jandrol.108.007005. [DOI] [PubMed] [Google Scholar]
- 336.Weiss E.P., Villareal D.T., Fontana L., Han D.H., Holloszy J.O. Dehydroepiandrosterone (DHEA) replacement decreases insulin resistance and lowers inflammatory cytokines in aging humans. Aging-US. 2011;3:533–542. doi: 10.18632/aging.100327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Li L.L., Yao Y., Zhao J.L., Cao J., Ma H.T. Dehydroepiandrosterone protects against hepatic glycolipid metabolic disorder and insulin resistance induced by high fat via activation of AMPK-PGC-1 alpha-NRF-1 and IRS1-AKT-GLUT2 signaling pathways. Int. J. Obes. 2020;44:1075–1086. doi: 10.1038/s41366-019-0508-8. [DOI] [PubMed] [Google Scholar]
- 338.Mårin P., Holmäng S., Gustafsson C., Jönsson L., Kvist H., Elander A., Eldh J., Sjöström L., Holm G., Björntorp P. Androgen treatment of abdominally obese men. Obes. Res. 1993;1:245–251. doi: 10.1002/j.1550-8528.1993.tb00618.x. [DOI] [PubMed] [Google Scholar]
- 339.Groti K., Žuran I., Antonič B., Foršnarič L., Pfeifer M. The impact of testosterone replacement therapy on glycemic control, vascular function, and components of the metabolic syndrome in obese hypogonadal men with type 2 diabetes. Aging Male. 2018;21:158–169. doi: 10.1080/13685538.2018.1468429. [DOI] [PubMed] [Google Scholar]
- 340.Caliber M., Saad F. Testosterone therapy for prevention and reversal of type 2 diabetes in men with low testosterone. Curr. Opin. Pharmacol. 2021;58:83–89. doi: 10.1016/j.coph.2021.04.002. [DOI] [PubMed] [Google Scholar]
- 341.Grishkovskaya I., Avvakumov G.V., Hammond G.L., Catalano M.G., Muller Y.A. Steroid ligands bind human sex hormone-binding globulin in specific orientations and produce distinct changes in protein conformation. J. Biol. Chem. 2002;277:32086–32093. doi: 10.1074/jbc.M203999200. [DOI] [PubMed] [Google Scholar]
- 342.Jayaraj A., Schwanz H.A., Spencer D.J., Bhasin S., Hamilton J.A., Jayaram B., Goldman A.L., Krishna M., Krishnan M., Shah A., et al. Allosterically coupled multisite binding of testosterone to human serum albumin. Endocrinology. 2021;162:bgaa199. doi: 10.1210/endocr/bqaa199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Sanchez W.Y., de Veer S.J., Swedberg J.E., Hong E.J., Reid J.C., Walsh T.P., Hooper J.D., Hammond G.L., Clements J.A., Harris J.M. Selective cleavage of human sex hormone-binding globulin by kallikrein-related peptidases and effects on androgen action in LNCaP Prostate cancer cells. Endocrinology. 2012;153:3179–3189. doi: 10.1210/en.2012-1011. [DOI] [PubMed] [Google Scholar]
- 344.Round P., Das S., Wu T.S., Wahala K., Van Petegem F., Hammond G.L. Molecular interactions between sex hormone-binding globulin and nonsteroidal ligands that enhance androgen activity. J. Biol. Chem. 2020;295:1202–1211. doi: 10.1016/S0021-9258(17)49880-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Veldhuis J.D., Urban R.J., Dufau M.L. Evidence that androgen negative feedback regulates hypothalamic gonadotropin-releasing hormone impulse strength and the burst-like secretion of biologically active luteinizing hormone in men. J. Clin. Endocrinol. Metab. 1992;74:1227–1235. doi: 10.1210/jcem.74.6.1592863. [DOI] [PubMed] [Google Scholar]
- 346.Ryan G.E., Bohaczuk S.C., Cassin J., Witham E.A., Shojaei S., Ho E.V., Thackray V.G., Mellon P.L. Androgen receptor positively regulates gonadotropin-releasing hormone receptor in pituitary gonadotropes. Mol. Cell. Endocrinol. 2021;530:111286. doi: 10.1016/j.mce.2021.111286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Krsmanovic L.Z., Hu L., Leung P.-K., Feng H., Catt K.J. The hypothalamic GnRH pulse generator: Multiple regulatory mechanisms. Trends Endocrinol. Metab. 2009;20:402–408. doi: 10.1016/j.tem.2009.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Popa G. A portal circulation from the pituitary to the hypothalamic region. J. Anat. 1930;65:88–91. [PMC free article] [PubMed] [Google Scholar]
- 349.Ramakrishnappa N., Rajamahendran R., Lin Y.-M., Leung P.C.K. GnRH in non-hypothalamic reproductive tissues. Anim. Reprod. Sci. 2005;88:95–113. doi: 10.1016/j.anireprosci.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 350.George J.T., Hendrikse M., Veldhuis J.D., Clarke I.J., Anderson R.A., Millar R.P. Effect of gonadotropin-inhibitory hormone on luteinizing hormone secretion in humans. Clin. Endocrinol. 2017;86:731–738. doi: 10.1111/cen.13308. [DOI] [PubMed] [Google Scholar]
- 351.Koike K., Miyake A., Aono T., Sakamoto T., Ohmichi M., Yamaguchi M., Tanizaw O. Effect of prolactin on the secretion of hypothalamic GnRH and pituitary gonadotropins. Horm. Res. 1991;35:5–12. doi: 10.1159/000181921. [DOI] [PubMed] [Google Scholar]
- 352.Breen K.M., Davis T.L., Doro L.C., Nett T.M., Oakley A.E., Padmanabhan V., Rispoli L.A., Wagenmaker E.R., Karsch F.J. Insight into the neuroendocrine site and cellular mechanism by which cortisol suppresses pituitary responsiveness to gonadotropin-releasing hormone. Endocrinology. 2008;149:767–773. doi: 10.1210/en.2007-0773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Gore A.C., Attardi B., DeFranco D.B. Glucocorticoid repression of the reproductive axis: Effects on GnRH and gonadotropin subunit mRNA levels. Mol. Cell. Endocrinol. 2006;256:40–48. doi: 10.1016/j.mce.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 354.Whirledge S., Cidlowski J.A. Glucocorticoids, stress, and fertility. Minerva Endocrinol. 2010;35:109–125. [PMC free article] [PubMed] [Google Scholar]
- 355.Calogero A.E., Gallucci W.T., Gold P.W., Chrousos G.P. Multiple feedback regulatory loops upon rat hypothalamic corticotropin-releasing hormone secretion. Potential clinical implications. J. Clin. Invest. 1988;82:767–774. doi: 10.1172/JCI113677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Dallman M.F., Akana S.F., Jacobson L., Levin N., Cascio C.S., Shinsako J. Characterization of corticosterone feedback regulation of ACTH secretion. Ann. N. Y. Acad. Sci. 1987;512:402–414. doi: 10.1111/j.1749-6632.1987.tb24976.x. [DOI] [PubMed] [Google Scholar]
- 357.Mori H., Christensen A.K. Morphometric analysis of Leydig cells in the normal rat testis. J. Cell Biol. 1980;84:340–354. doi: 10.1083/jcb.84.2.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Luu-The V., Bélanger A., Labrie F. Androgen biosynthetic pathways in the human prostate. Best Pract. Res. Clin. Endocrinol. Metab. 2008;22:207–221. doi: 10.1016/j.beem.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 359.Turcu A., Smith J.M., Auchus R., Rainey W.E. Adrenal androgens and androgen precursors-definition, synthesis, regulation and physiologic actions. Compr. Physiol. 2014;4:1369–1381. doi: 10.1002/cphy.c140006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Wen X., Li D., Tozer A.J., Docherty S.M., Iles R.K. Estradiol, progesterone, testosterone profiles in human follicular fluid and cultured granulosa cells from luteinized pre-ovulatory follicles. Reprod. Biol. Endocrinol. 2010;8:117. doi: 10.1186/1477-7827-8-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Hagen F.S., Arguelles C., Sui L.M., Zhang W., Seidel P.R., Conroy S.C., Petra P.H. Mammalian expression of the human sex steroid-binding protein of plasma (SBP or SHBG) and testis (ABP)-characterization of the recombinant protein. FEBS Lett. 1992;299:23–27. doi: 10.1016/0014-5793(92)80091-T. [DOI] [PubMed] [Google Scholar]
- 362.Hansson V., Weddington S.C., Naess O., Attramadal A., French F.S., Kotite N., Nayfeh S.N. Testicular androgen binding protein (ABP): A parameter of Sertoli cell secretory function. Curr. Top. Mol. Endocrinol. 1975;2:323–336. doi: 10.1007/978-1-4613-4440-7_23. [DOI] [PubMed] [Google Scholar]
- 363.Schock H.W., Herbert Z., Sigusch H., Figulla H.R., Jirikowski G.F., Lotze U. Expression of androgen-binding protein (ABP) in human cardiac myocytes. Horm. Metab. Res. 2006;38:225–229. doi: 10.1055/s-2006-925331. [DOI] [PubMed] [Google Scholar]
- 364.Hansson V., Ritzen M.E., French F.S., Weddington S.C., Nayfeh S.N. Testicular androgen-binding protein (ABP): Comparison of ABP in rabbit testis and epididymis with a similar androgen-binding protein (TeBG) in rabbit serum. Mol. Cell. Endocrinol. 1975;3:1–20. doi: 10.1016/0303-7207(75)90028-3. [DOI] [PubMed] [Google Scholar]
- 365.Karn R.C., Yazdanifar G., Pezer Z., Boursot P., Laukaitis C.M. Androgen-binding protein (ABP) evolutionary history: Has positive selection caused fixation of different paralogs in different taxa of the genus Mus? Genome Biol. Evol. 2021;13:evab220. doi: 10.1093/gbe/evab220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Kirchhoff J., Soffie M., Rousseau G.G. Differences in the steroid-binding site specificities of rat prostate androgen receptor and epididymal androgen-binding protein (ABP) J. Steroid Biochem. 1979;10:487–497. doi: 10.1016/0022-4731(79)90209-7. [DOI] [PubMed] [Google Scholar]
- 367.Walker W.H. Testosterone signaling and the regulation of spermatogenesis. Spermatogenesis. 2011;1:116–120. doi: 10.4161/spmg.1.2.16956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Walker W.H. Androgen actions in the testis and the regulation of spermatogenesis. Adv. Exp. Med. Biol. 2021;1288:175–203. doi: 10.1007/978-3-030-77779-1_9. [DOI] [PubMed] [Google Scholar]
- 369.Soules M.R., Steiner R.A., Clifton D.K., Cohen N.L., Aksel S., Bremner W.J. Progesterone modulation of pulsatile luteinizing hormone secretion in normal women. J. Clin. Endocrinol. Metab. 1984;58:378–383. doi: 10.1210/jcem-58-2-378. [DOI] [PubMed] [Google Scholar]
- 370.Veldhuis J.D., Dufau M.L. Steroidal regulation of biologically active luteinizing hormone secretion in men and women. Hum. Reprod. 1993;8:84–96. doi: 10.1093/humrep/8.suppl_2.84. [DOI] [PubMed] [Google Scholar]
- 371.Wang H.-Q., Zhang W.-D., Yuan B., Zhang J.-B. Advances in the regulation of mammalian follicle-stimulating hormone secretion. Animals. 2021;11:1134. doi: 10.3390/ani11041134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Navarro V.M., Castellano J.M., Fernández-Fernández R., Tovar S., Roa J., Mayen A., Barreiro M.L., Casanueva F.F., Aguilar E., Diéguez C., et al. Effects of KiSS-1 peptide, the natural ligand of GPR54, on follicle-stimulating hormone secretion in the rat. Endocrinology. 2005;146:1689–1697. doi: 10.1210/en.2004-1353. [DOI] [PubMed] [Google Scholar]
- 373.Ying S.-Y. Inhibins, activins, and follistatins: Gonadal proteins modulating the secretion of follicle-stimulating hormone. Endocr. Rev. 1988;9:267–293. doi: 10.1210/edrv-9-2-267. [DOI] [PubMed] [Google Scholar]
- 374.Zhang H., Basit A., Busch D., Yabut K., Bhatt D.K., Drozdzik M., Ostrowski M., Li A., Collins C., Oswald S., et al. Quantitative characterization of UDP-glucuronosyltransferase 2B17 in human liver and intestine and its role in testosterone first -pass metabolism. Biochem. Pharmacol. 2018;156:32–42. doi: 10.1016/j.bcp.2018.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Galetin A., Houston J.B. Intestinal and hepatic metabolic activity of five cytochrome P450 enzymes: Impact on prediction of first-pass metabolism. J. Pharmacol. Exp. Ther. 2006;318:1220–1229. doi: 10.1124/jpet.106.106013. [DOI] [PubMed] [Google Scholar]
- 376.Vierhapper H., Nowotny P., Waldhäusl W. Determination of testosterone production rates in men and women using stable isotope/dilution and mass spectrometry. J. Clin. Endocrinol. Metab. 1997;82:1492–1496. doi: 10.1210/jcem.82.5.3958. [DOI] [PubMed] [Google Scholar]
- 377.Grinspon R.P., Bergadá I., Rey R.A. Male hypogonadism and disorders of sex development. Front. Endocrinol. 2020;11:211. doi: 10.3389/fendo.2020.00211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Jarow J.P., Zirkin B.R. The androgen microenvironment of the human testis and hormonal control of spermatogenesis. Ann. N. Y. Acad. Sci. USA. 2005;1061:208–220. doi: 10.1196/annals.1336.023. [DOI] [PubMed] [Google Scholar]
- 379.Sharpe R.M., McKinnell C., Kivlin C., Fisher J.S. Proliferation and functional maturation of Sertoli cells, and their relevance to disorders of testis function in adulthood. Reproduction. 2003;125:769–784. doi: 10.1530/rep.0.1250769. [DOI] [PubMed] [Google Scholar]
- 380.Takihara H., Cosentino M.J., Sakatoku J., Cockett A.T.K. Significance of testicular size measurement in andrology: II. Correlation of testicular size with testicular function. J. Urol. 1987;137:416–419. doi: 10.1016/S0022-5347(17)44053-5. [DOI] [PubMed] [Google Scholar]
- 381.Dhindsa S., Prabhakar S., Sethi M., Bandyopadhyay A., Chaudhuri A., Dandona P. Frequent occurrence of hypogonadotropic hypogonadism in type 2 diabetes. J. Clin. Endocrinol. Metab. 2004;89:5462–5468. doi: 10.1210/jc.2004-0804. [DOI] [PubMed] [Google Scholar]
- 382.Bakhtyukov A.A., Derkach K.V., Dar’in D.V., Sharova T.S., Shpakov A.O. Decrease in the basal and luteinizing hormone receptor agonist-stimulated testosterone production in aging male rats. Adv. Gerontol. 2019;9:179–185. doi: 10.1134/S2079057019020036. [DOI] [PubMed] [Google Scholar]
- 383.Kaplan S.A., Meehan A.G., Shah A. The age related decrease in testosterone is significantly exacerbated in obese men with the metabolic syndrome. What are the implications for the relatively high incidence of erectile dysfunction observed in these men? J. Urol. 2006;176:1524–1527. doi: 10.1016/j.juro.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 384.Midzak A.S., Chen H.L., Papadopoulos V., Zirkin B.R. Leydig cell aging and the mechanisms of reduced testosterone synthesis. Mol. Cell. Endocrinol. 2009;299:23–31. doi: 10.1016/j.mce.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 385.Corona G., Monami M., Rastrelli G., Aversa A., Tishova Y., Saad F., Lenzi A., Forti G., Mannucci E., Maggi M. Testosterone and metabolic syndrome: A meta-analysis study. J. Sex. Med. 2011;8:272–283. doi: 10.1111/j.1743-6109.2010.01991.x. [DOI] [PubMed] [Google Scholar]
- 386.Liang J., Peng Q., Yang X., Yang C. The association between serum testosterone levels and metabolic syndrome among women. Diabetol. Metab. Syndr. 2021;13:26. doi: 10.1186/s13098-021-00643-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Saad F., Gooren L. The role of testosterone in the metabolic syndrome: A review. J. Steroid Biochem. Mol. Biol. 2009;114:40–43. doi: 10.1016/j.jsbmb.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 388.Handelsman D.J., Conway A.J., Boylan L.M. Suppression of human spermatogenesis by testosterone implants. J. Clin. Endocrinol. Metab. 1992;75:1326–1332. doi: 10.1210/jcem.75.5.1430094. [DOI] [PubMed] [Google Scholar]
- 389.McBride J.A., Coward R.M. Recovery of spermatogenesis following testosterone replacement therapy or anabolic-androgenic steroid use. Asian J. Androl. 2016;18:373–380. doi: 10.4103/1008-682X.173938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.Crosnoe L.E., Grober E., Ohl D., Kim E.D. Exogenous testosterone: A preventable cause of male infertility. Transl. Androl. Urol. 2013;2:106–113. doi: 10.3978/j.issn.2223-4683.2013.06.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Patel A.S., Leong J.Y., Ramos L., Ramasamy R. Testosterone is a contraceptive and should not be used in men who desire fertility. World J. Men’s Health. 2019;37:45–54. doi: 10.5534/wjmh.180036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Gill-Sharma M.K. Testosterone retention mechanism in Sertoli cells: A biochemical perspective. Open Biochem. J. 2018;12:103–112. doi: 10.2174/1874091X01812010103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Labrie F. All sex steroids are made intracellularly in peripheral tissues by the mechanisms of intracrinology after menopause. J. Steroid Biochem. Mol. Biol. 2015;145:133–138. doi: 10.1016/j.jsbmb.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 394.Zhao D., Guallar E., Ouyang P., Subramanya V., Vaidya D., Ndumele C.E., Lima J.A., Allison M.A., Shah S.J., Bertoni A.G., et al. Endogenous sex hormones and incident cardiovascular disease in post-menopausal women. J. Am. Coll. Cardiol. 2018;71:2555–2566. doi: 10.1016/j.jacc.2018.01.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Barnes R.B. The pathogenesis of polycystic ovary syndrome: Lessons from ovarian stimulation studies. J. Endocrinol. Invest. 1998;21:567–579. doi: 10.1007/BF03350782. [DOI] [PubMed] [Google Scholar]
- 396.Panidis D., Farmakiotis D., Rousso D., Katsikis I., Kourtis A., Diamanti-Kandarakis E. Serum luteinizing hormone levels are markedly increased and significantly correlated with Δ4-androstenedione levels in lean women with polycystic ovary syndrome. Fertil. Steril. 2005;84:538–540. doi: 10.1016/j.fertnstert.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 397.Bhatia B., Price C.A. Insulin alters the effects of follicle stimulating hormone on aromatase in bovine granulosa cells in vitro. Steroids. 2001;66:511–519. doi: 10.1016/S0039-128X(00)00218-X. [DOI] [PubMed] [Google Scholar]
- 398.Hsueh A.J.W., Erickson G.F. Glucocorticoid inhibition of FSH-induced estrogen production in cultured rat granulosa cells. Steroids. 1978;32:639–648. doi: 10.1016/0039-128X(78)90074-0. [DOI] [PubMed] [Google Scholar]
- 399.Brown Séquard C.E. Note on the effects produced on man by subcutaneous injections of a liquid obtained from the testicles of animals. Lancet. 1889;134:105–107. doi: 10.1016/S0140-6736(00)64118-1. [DOI] [Google Scholar]
- 400.Freeman E.R., Bloom D.A., McGuire E.J. A brief history of testosterone. J. Urol. 2001;165:371–373. doi: 10.1097/00005392-200102000-00004. [DOI] [PubMed] [Google Scholar]
- 401.Joubert S.W. Rejuvenation: Steinach vs. Voronoff. S. Afr. Med. J. 1928;2:8–10. [Google Scholar]
- 402.Stanley L.L. An analysis of one thousand testicular substance implantations. Endocrinology. 1922;6:787–794. doi: 10.1210/endo-6-6-787. [DOI] [Google Scholar]
- 403.Borrell M. Brown-Séquard’s organotherapy and its appearance in America at the end of the nineteenth century. Bull. Hist. Med. 1976;50:309–320. [PubMed] [Google Scholar]
- 404.David K., Dingemanse E., Freud J., Laqueur E. Über krystallinisches männliches Hormon aus Hoden (Testosteron), wirksamer als aus Harn oder aus Cholesterin bereitetes Androsteron [About a crystalline male hormone from testicles (testosterone), more effective than androsterone prepared from urine or cholesterol] Hoppe-Seyler Z. Physiol. Chem. 1935;233:281–283. doi: 10.1515/bchm2.1935.233.5-6.281. [DOI] [Google Scholar]
- 405.Butenandt A., Hanisch G. Über Testosteron. Umwandlung des Dehydro-androsterons in Androstendiol und Testosteron; ein Weg zur Darstellung des Testosterons aus Cholesterin [About testosterone. conversion of dehydro-androsterone into androstenediol and testosterone; a way of preparing testosterone from cholesterol] Hoppe-Seyler Z. Physiol. Chem. 1935;237:89–97. doi: 10.1515/bchm2.1935.237.1-3.89. [DOI] [Google Scholar]
- 406.Shinohara Y., Baba S., Kasuya Y. Absorption, metabolism, and excretion of oral testosterone in humans by mass fragmentography. J. Clin. Endocrinol. Metab. 1980;51:1459–1462. doi: 10.1210/jcem-51-6-1459. [DOI] [PubMed] [Google Scholar]
- 407.Farthing M.J., Vinson G.P., Edwards C.R., Dawson A.M. Testosterone metabolism by the rat gastrointestinal tract, in vitro and in vivo. Gut. 1982;23:226–234. doi: 10.1136/gut.23.3.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Noguchi T., Charman W.N.A., Stella V.J. The effect of drug lipophilicity and lipid vehicles on the lymphatic absorption of various testosterone esters. Int. J. Pharm. 1985;24:173–184. doi: 10.1016/0378-5173(85)90018-3. [DOI] [Google Scholar]
- 409.Birzniece V. Hepatic actions of androgens in the regulation of metabolism. Curr. Opin. Endocrinol. Diabetes Obes. 2018;25:201–208. doi: 10.1097/MED.0000000000000405. [DOI] [PubMed] [Google Scholar]
- 410.Sohlenius-Sternbeck A.-K., Orzechowski A. Characterization of the rates of testosterone metabolism to various products and of glutathione transferase and sulfotransferase activities in rat intestine and comparison to the corresponding hepatic and renal drug-metabolizing enzymes. Chem.-Biol. Interact. 2004;148:49–56. doi: 10.1016/j.cbi.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 411.Trane I., Sager G., Sveberg Dietrichs E., Westrheim Ravna A. Molecular modeling study of the testosterone metabolizing enzyme UDP-glucuronosyltransferase 2B17. Bioorganic Med. Chem. 2021;36:116060. doi: 10.1016/j.bmc.2021.116060. [DOI] [PubMed] [Google Scholar]
- 412.Li X., Cheng W., Shang H., Wei H., Deng C. The interplay between androgen and gut microbiota: Is there a microbiota-gut-testis axis. Reprod. Sci. 2022;29:1674–1684. doi: 10.1007/s43032-021-00624-0. [DOI] [PubMed] [Google Scholar]
- 413.Korenman S.G., Wilson H., Lipsett M.B. Testosterone production rates in normal adults. J. Clin. Invest. 1963;42:1753–1760. doi: 10.1172/JCI104860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Horton R., Shinsako J., Forsham P.H. Testosterone production and metabolic clearance rates with volumes of distributon in normal adult men and women. Acta Endocrinol. 1965;48:446–458. doi: 10.1530/acta.0.0480446. [DOI] [PubMed] [Google Scholar]
- 415.Southren A.L., Tochimoto S., Carmody N.C., Isurugi K. Plasma production rates of testosterone in normal adult men and women and in patients with the syndrome of feminizing testes. J. Clin. Endocrinol. Metab. 1965;25:1441–1450. doi: 10.1210/jcem-25-11-1441. [DOI] [PubMed] [Google Scholar]
- 416.Knapstein P., Wortmann W., Krämer C. Metabolism and plasma half life of [14C]testosterone plus [3H]testosterone [35S]sulfate perfused through human liver or injected intravenously. Hoppe-Seyler Z. Physiol. Chem. 1972;353:1447–1453. doi: 10.1515/bchm2.1972.353.2.1447. [DOI] [PubMed] [Google Scholar]
- 417.Shoskes J.J., Wilson M.K., Spinner M.L. Pharmacology of testosterone replacement therapy preparations. Transl. Androl. Urol. 2016;5:834–843. doi: 10.21037/tau.2016.07.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Porst H. Intramuscular testosterone treatment in elderly men: Evidence of memory decline and altered brain function. J. Sex. Med. 2008;5:534. doi: 10.1210/jc.2006-1805. [DOI] [PubMed] [Google Scholar]
- 419.Täuber U., Schröder K., Düsterberg B., Matthes H. Absolute bioavailability of testosterone after oral administration of testosterone-undecanoate and testosterone. Eur. J. Drug Metab. Pharmacokinet. 1986;11:145–149. doi: 10.1007/BF03189840. [DOI] [PubMed] [Google Scholar]
- 420.Zgair A., Dawood Y., Ibrahem S.M., Back H.-m., Kagan L., Gershkovich P., Lee J.B. Predicting intestinal and hepatic first-pass metabolism of orally administered testosterone undecanoate. Appl. Sci. 2020;10:7283. doi: 10.3390/app10207283. [DOI] [Google Scholar]
- 421.Wang C., Ilani N., Arver S., McLachlan R.I., Soulis T., Watkinson A. Efficacy and safety of the 2% formulation of testosterone topical solution applied to the axillae in androgen-deficient men. Clin. Endocrinol. 2011;75:836–843. doi: 10.1111/j.1365-2265.2011.04152.x. [DOI] [PubMed] [Google Scholar]
- 422.Tajbakhsh M., Saeedi M., Morteza-Semnani K., Akbari J., Nokhodchi A. Innovation of testosome as a green formulation for the transdermal delivery of testosterone enanthate. J. Drug Deliv. Sci. Technol. 2020;57:101685. doi: 10.1016/j.jddst.2020.101685. [DOI] [Google Scholar]
- 423.Handelsman D.J., Conway A.J., Boylan L.M. Pharmacokinetics and pharmacodynamics of testosterone pellets in man. J. Clin. Endocrinol. Metab. 1990;71:216–222. doi: 10.1210/jcem-71-1-216. [DOI] [PubMed] [Google Scholar]
- 424.Kesler D.J., Christensen D.C., Wallace M.E. The effect of esterification on the release of testosterone and estradiol from silicone implants. Drug Dev. Ind. Pharm. 1996;22:275–279. doi: 10.3109/03639049609058572. [DOI] [Google Scholar]
- 425.Spratt D.I., Stewart I.I., Savage C., Craig W., Spack N.P., Chandler D.W., Spratt L.V., Eimicke T., Olshan J.S. Subcutaneous injection of testosterone is an effective and preferred alternative to intramuscular injection: Demonstration in female-to-male transgender patients. J. Clin. Endocrinol. Metab. 2017;102:2349–2355. doi: 10.1210/jc.2017-00359. [DOI] [PubMed] [Google Scholar]
- 426.Arver S., Dobs A.S., Meikle A.W., Caramelli K.E., Rajaram L., Sanders S.W., Mazer N.A. Long-term efficacy and safety of a permeation-enhanced testosterone transdermal system in hypogonadal men. Clin. Endocrinol. 1997;47:727–737. doi: 10.1046/j.1365-2265.1997.3071113.x. [DOI] [PubMed] [Google Scholar]
- 427.Korbonits M., Slawik M., Cullen D., Ross R.J., Stalla G., Schneider H., Reincke M., Bouloux P.M., Grossman A.B. A comparison of a novel testosterone bioadhesive buccal system, Striant, with a testosterone adhesive patch in hypogonadal males. J. Clin. Endocrinol. Metab. 2004;89:2039–2043. doi: 10.1210/jc.2003-030319. [DOI] [PubMed] [Google Scholar]
- 428.Hattori K., Igarashi M., Itoh M., Tomisawa H., Tateishi M. Specific induction by glucocorticoids of steroid esterase in rat hepatic microsomes and its release into serum. Biochem. Pharmacol. 1992;43:1921–1927. doi: 10.1016/0006-2952(92)90634-U. [DOI] [PubMed] [Google Scholar]
- 429.Coert A., Geelen J., de Visser J., van der Vies J. The pharmacology and metabolism of testosterone undecanoate (TU), a new orally active androgen. Acta Endocrinol. 1975;79:789–800. doi: 10.1530/acta.0.0790789. [DOI] [PubMed] [Google Scholar]
- 430.Skakkebaek N.E., Bancroft J., Davidson D.W., Warner P. Androgen replacement with oral testosterone undecanoate in hypogonadal men: A double blind controlled study. Clin. Endocrinol. 1981;14:49–61. doi: 10.1111/j.1365-2265.1981.tb00364.x. [DOI] [PubMed] [Google Scholar]
- 431.Edelstein D., Basaria S. Testosterone undecanoate in the treatment of male hypogonadism. Expert Opin. Pharmacother. 2010;11:2095–2106. doi: 10.1517/14656566.2010.505920. [DOI] [PubMed] [Google Scholar]
- 432.Nieschlag E., Cüppers H.J., Wiegelmann W., Wickings E.J. Bioavailability and LH-suppressing effect of different testosterone preparations in normal and hypogonadal men. Horm. Res. 1976;7:138–145. doi: 10.1159/000178721. [DOI] [PubMed] [Google Scholar]
- 433.Frisch F., Sumida K.D. Temporal effects of testosterone propionate injections on serum lipoprotein concentrations in rats. Med. Sci. Sport. Exerc. 1999;31:664–669. doi: 10.1097/00005768-199905000-00007. [DOI] [PubMed] [Google Scholar]
- 434.Sadowska-Krepa E., Klapcinska B., Jagsz S., Sobczak A., Chrapusta S.J., Chalimoniuk M., Grieb P., Poprzecki S., Langfort J. High-dose testosterone propionate treatment reverses the effects of endurance training on myocardial antioxidant defenses in adolescent male rats. Cardiovasc. Toxicol. 2011;11:118–127. doi: 10.1007/s12012-011-9105-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435.Lourenço Í., Krause Neto W., dos Santos Portella Amorim L., Moraes Munhoz Ortiz V., Lopes Geraldo V., da Silva Ferreira G.H., Torres de Lima J., Alves Ribeiro Massoni A., Massensini Oliveira B., Anaruma C.A., et al. Previous short-term use of testosterone propionate enhances muscle hypertrophy in Wistar rats submitted to ladder-based resistance training. Tissue Cell. 2022;75:101741. doi: 10.1016/j.tice.2022.101741. [DOI] [PubMed] [Google Scholar]
- 436.Whitsel E.A., Boyko E.J., Matsumoto A.M., Anawalt B.D., Siscovick D.S. Intramuscular testosterone esters and plasma lipids in hypogonadal men: A meta-analysis. Am. J. Med. 2001;111:261–269. doi: 10.1016/S0002-9343(01)00833-6. [DOI] [PubMed] [Google Scholar]
- 437.Kishimoto Y. Fatty acid esters of testosterone in rat brain: Identification, distribution, and some properties of enzymes which synthesize and hydrolyze the esters. Arch. Biochem. Biophys. 1973;159:528–542. doi: 10.1016/0003-9861(73)90485-2. [DOI] [PubMed] [Google Scholar]
- 438.Steinberger E., Smith K.D. Effect of chronic administration of testosterone enanthate on sperm production and plasma testosterone, follicle-stimulating hormone, and luteinizing hormone levels: A preliminary evaluation of a possible male contraceptive. Fertil. Steril. 1977;28:1320–1328. doi: 10.1016/S0015-0282(16)42977-8. [DOI] [PubMed] [Google Scholar]
- 439.Snyder P.J., Lawrence D.A. Treatment of male hypogonadism with testosterone enanthate. J. Clin. Endocrinol. Metab. 1980;51:1335–1339. doi: 10.1210/jcem-51-6-1335. [DOI] [PubMed] [Google Scholar]
- 440.Bjelic M.M., Stojkov N.J., Radovic S.M., Baburski A.Z., Janjic M.M., Kostic T.S., Andric S.A. Prolonged in vivo administration of testosterone-enanthate, the widely used and abused anabolic androgenic steroid, disturbs prolactin and cAMP signaling in Leydig cells of adult rats. J. Steroid Biochem. Mol. Biol. 2015;149:58–69. doi: 10.1016/j.jsbmb.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 441.Al-Futaisi A.M., Al-Zakwani I.S., Almahrezi A.M., Morris D.J. Subcutaneous administration of testosterone. A pilot study report. Saudi Med. J. 2006;27:1843–1846. [PubMed] [Google Scholar]
- 442.Nankin H.R. Hormone kinetics after intramuscular testosterone cypionate. Fertil. Steril. 1987;47:1004–1009. doi: 10.1016/S0015-0282(16)59237-1. [DOI] [PubMed] [Google Scholar]
- 443.Schürmeyer T., Nieschlag E. Comparative pharmacokinetics of testosterone enanthate and testosterone cyclohexanecarboxylate as assessed by serum and salivary testosterone levels in normal men. Int. J. Androl. 1984;7:181–187. doi: 10.1111/j.1365-2605.1984.tb00775.x. [DOI] [PubMed] [Google Scholar]
- 444.Brady B.M., Amory J.K., Perheentupa A., Zitzmann M., Hay C.J., Apter D., Anderson R.A., Bremner W.J., Pollanen P., Nieschlag E., et al. A multicentre study investigating subcutaneous etonogestrel implants with injectable testosterone decanoate as a potential long-acting male contraceptive. Hum. Reprod. 2006;21:285–294. doi: 10.1093/humrep/dei300. [DOI] [PubMed] [Google Scholar]
- 445.Al-Aubody N.M., Al-Diwan M.A. Histopathological changes of liver, kidneys and heart of male rats caused by abusing of Sustanon® 250. Basrah J. Vet. Res. 2018;17:457–471. [Google Scholar]
- 446.Jones T.H. Testosterone replacement therapy. Br. J. Hosp. Med. 2007;68:547–553. doi: 10.12968/hmed.2007.68.10.27326. [DOI] [PubMed] [Google Scholar]
- 447.Gu Y.Q., Liang X.W., Wu W.X., Liu M.L., Song S.X., Cheng L.F., Bo L.W., Xiong C.L., Wang X.H., Liu X.Z., et al. Multicenter contraceptive efficacy trial of injectable testosterone undecanoate in Chinese men. J. Clin. Endocrinol. Metab. 2009;94:1910–1915. doi: 10.1210/jc.2008-1846. [DOI] [PubMed] [Google Scholar]
- 448.Hamm C., Azad S. Delayed oleoma formation with injection of oil-suspended testosterone: A case report and review of pathogenesis. SAGE Open Med. Case Rep. 2022;10:2050313x221086318. doi: 10.1177/2050313X221086318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 449.Narayana N.S., Ly L.P., Jayadev V., Fennell C., Savkovic S., Conway A.J., Handelsman D.J. Optimal injection interval for testosterone undecanoate treatment of hypogonadal and transgender men. Endocr. Connect. 2021;10:758–766. doi: 10.1530/EC-21-0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450.Gooren L.J.G., Bunck M.C.M. Transdermal testosterone delivery: Testosterone patch and gel. World J. Urol. 2003;21:316–319. doi: 10.1007/s00345-003-0368-6. [DOI] [PubMed] [Google Scholar]
- 451.Nieschlag E. Testosterone treatment comes of age: New options for hypogonadal men. Clin. Endocrinol. 2006;65:275–281. doi: 10.1111/j.1365-2265.2006.02618.x. [DOI] [PubMed] [Google Scholar]
- 452.Belkoff L., Brock G., Carrara D., Neijber A., Ando M., Mitchel J. Efficacy and safety of testosterone replacement gel for treating hypogonadism in men: Phase III open-label studies. Andrologia. 2018;50:e12801. doi: 10.1111/and.12801. [DOI] [PubMed] [Google Scholar]
- 453.Kamal N.S., Alayoubi A., Elfakhri K.H., Ibrahim S., Seggel M., Ashraf M., Zidan A. Effects of formulation variables on the in vitro performance of testosterone transdermal gel. Int. J. Pharm. 2020;590:119951. doi: 10.1016/j.ijpharm.2020.119951. [DOI] [PubMed] [Google Scholar]
- 454.Retzler J., Smith A.B., Goncalves A.S.O., Whitty J.A. Preferences for the administration of testosterone gel: Evidence from a discrete choice experiment. Patient Prefer. Adherence. 2019;13:657–664. doi: 10.2147/PPA.S197469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 455.Puiu A.A., Radke S., Votinov M., Habel U., Herpertz-Dahlmann B., Turetsky B., Konrad K. Serum testosterone and cortisol concentrations after single-dose administration of 100-mg transdermal testosterone in healthy men. Front. Pharmacol. 2019;10:1397. doi: 10.3389/fphar.2019.01397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456.Rolf C., Nieschlag E. Potential adverse effects of long-term testosterone therapy. Baillière’s Clin. Endocrinol. Metab. 1998;12:521–534. doi: 10.1016/S0950-351X(98)80305-4. [DOI] [PubMed] [Google Scholar]
- 457.Miller M.G., Rogol A.D., ZumBrunnen T.L. Secondary exposure to testosterone from patients receiving replacement therapy with transdermal testosterone gels. Curr. Med. Res. Opin. 2012;28:267–269. doi: 10.1185/03007995.2011.652255. [DOI] [PubMed] [Google Scholar]
- 458.Gronski M.A., Grober E.D., Gottesman I.S., Ormsby R.W., Bryson N. Efficacy of nasal testosterone gel (natesto) stratified by baseline endogenous testosterone levels. J. Endocr. Soc. 2019;3:1652–1662. doi: 10.1210/js.2019-00183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 459.Banks W.A., Morley J.E., Niehoff M.L., Mattern C. Delivery of testosterone to the brain by intranasal administration: Comparison to intravenous testosterone. J. Drug Target. 2009;17:91–97. doi: 10.1080/10611860802382777. [DOI] [PubMed] [Google Scholar]
- 460.Dobs A.S., Hoover D.R., Chen M.-C., Allen R. Pharmacokinetic characteristics, efficacy, and safety of buccal testosterone in hypogonadal males: A pilot study1. J. Clin. Endocrinol. Metab. 1998;83:33–39. doi: 10.1210/jcem.83.1.4505. [DOI] [PubMed] [Google Scholar]
- 461.Narukawa T., Soh J., Kanemitsu N., Harikai S., Ukimura O. Efficacy of combined treatment of intramuscular testosterone injection and testosterone ointment application for late-onset hypogonadism: An open-labeled, randomized, crossover study. Aging Male. 2021;23:1059–1065. doi: 10.1080/13685538.2019.1666814. [DOI] [PubMed] [Google Scholar]
- 462.Albert S.G., Morley J.E. Testosterone therapy, association with age, initiation and mode of therapy with cardiovascular events: A systematic review. Clin. Endocrinol. 2016;85:436–443. doi: 10.1111/cen.13084. [DOI] [PubMed] [Google Scholar]
- 463.Maggi M., Wu F.C.W., Jones T.H., Jackson G., Behre H.M., Hackett G., Martin-Morales A., Balercia G., Dobs A.S., Arver S.T.E., et al. Testosterone treatment is not associated with increased risk of adverse cardiovascular events: Results from the Registry of Hypogonadism in Men (RHYME) Int. J. Clin. Pract. 2016;70:843–852. doi: 10.1111/ijcp.12876. [DOI] [PubMed] [Google Scholar]
- 464.McCullough D., Webb R., Enright K.J., Lane K.E., McVeigh J., Stewart C.E., Davies I.G. How the love of muscle can break a heart: Impact of anabolic androgenic steroids on skeletal muscle hypertrophy, metabolic and cardiovascular health. Rev. Endocr. Metab. Disord. 2021;22:389–405. doi: 10.1007/s11154-020-09616-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 465.Onasanya O., Iyer G., Lucas E., Lin D., Singh S., Alexander G.C. Association between exogenous testosterone and cardiovascular events: An overview of systematic reviews. Lancet Diabetes Endocrinol. 2016;4:943–956. doi: 10.1016/S2213-8587(16)30215-7. [DOI] [PubMed] [Google Scholar]
- 466.Zelleroth S., Nylander E., Ortenblad A., Stam F., Nyberg F., Gronbladh A., Hallberg M. Structurally different anabolic androgenic steroids reduce neurite outgrowth and neuronal viability in primary rat cortical cell cultures. J. Steroid Biochem. Mol. Biol. 2021;210:105863. doi: 10.1016/j.jsbmb.2021.105863. [DOI] [PubMed] [Google Scholar]
- 467.Hauger L.E., Havnes I.A., Jørstad M.L., Bjørnebekk A. Anabolic androgenic steroids, antisocial personality traits, aggression and violence. Drug Alcohol Depend. 2021;221:108604. doi: 10.1016/j.drugalcdep.2021.108604. [DOI] [PubMed] [Google Scholar]
- 468.Corona G., Rastrelli G., Marchiani S., Filippi S., Morelli A., Sarchielli E., Sforza A., Vignozzi L., Maggi M. Consequences of anabolic-androgenic steroid abuse in males; sexual and reproductive perspective. World J. Men’s Health. 2022;40:165–179. doi: 10.5534/wjmh.210021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 469.De Oliveira Vilar Neto J., da Silva C.A., Bruno da Silva C.A., Pinto D.V., de Sá Roriz Caminha J., de Matos R.S., Nunes J.C.C., Alves F.R., Magalhães S.C., de Francesco Daher E. Anabolic androgenic steroid-induced hypogonadism, a reversible condition in male individuals? A systematic review. Andrologia. 2021;53:e14062. doi: 10.1111/and.14062. [DOI] [PubMed] [Google Scholar]
- 470.Falqueto H., Rodrigues dos Santos M., Manfredi L.H. Anabolic-androgenic steroids and exercise training: Breaking the myths and dealing with better outcome in sarcopenia. Front. Physiol. 2022;13:838526. doi: 10.3389/fphys.2022.838526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 471.Stancampiano M.R., Lucas-Herald A.K., Bryce J., Russo G., Barera G., Balsamo A., Baronio F., Bertelloni S., Valiani M., Cools M., et al. Testosterone therapy and its monitoring in adolescent boys with hypogonadism: Results of an international survey from the I-DSD registry. Sex. Dev. 2021;15:236–243. doi: 10.1159/000516784. [DOI] [PubMed] [Google Scholar]
- 472.Travison T.G., Morley J.E., Araujo A.B., O’Donnell A.B., McKinlay J.B. The relationship between libido and testosterone levels in aging men. J. Clin. Endocrinol. Metab. 2006;91:2509–2513. doi: 10.1210/jc.2005-2508. [DOI] [PubMed] [Google Scholar]
- 473.Amano T., Imao T., Takemae K., Iwamoto T., Yamakawa K., Baba K., Nakanome M., Sugimori H., Tanaka T., Yoshida K., et al. Profile of serum testosterone levels after application of testosterone ointment (Glowmin) and its clinical efficacy in late-onset hypogonadism patients. J. Sex. Med. 2008;5:1727–1736. doi: 10.1111/j.1743-6109.2007.00689.x. [DOI] [PubMed] [Google Scholar]
- 474.Snyder P.J., Bhasin S., Cunningham G.R., Matsumoto A.M., Stephens-Shields A.J., Cauley J.A., Gill T.M., Barrett-Connor E., Swerdloff R.S., Wang C., et al. Effects of testosterone treatment in older men. N. Engl. J. Med. 2016;374:611–624. doi: 10.1056/NEJMoa1506119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 475.Yassin D.J., Doros G., Hammerer P.G., Yassin A.A. Long-term testosterone treatment in elderly men with hypogonadism and erectile dysfunction reduces obesity parameters and improves metabolic syndrome and health-related quality of life. J. Sex. Med. 2014;11:1567–1576. doi: 10.1111/jsm.12523. [DOI] [PubMed] [Google Scholar]
- 476.Giltay E.J., Tishova Y.A., Mskhalaya G.J., Gooren L.J.G., Saad F., Kalinchenko S.Y. Effects of testosterone supplementation on depressive symptoms and sexual dysfunction in hypogonadal men with the metabolic syndrome. J. Sex. Med. 2010;7:2572–2582. doi: 10.1111/j.1743-6109.2010.01859.x. [DOI] [PubMed] [Google Scholar]
- 477.Bhasin S., Seidman S. Testosterone treatment of depressive disorders in men. JAMA Psychiatry. 2019;76:9–10. doi: 10.1001/jamapsychiatry.2018.2661. [DOI] [PubMed] [Google Scholar]
- 478.Wallis C.J.D., Lo K., Lee Y., Krakowsky Y., Garbens A., Satkunasivam R., Herschorn S., Kodama R.T., Cheung P., Narod S.A., et al. Survival and cardiovascular events in men treated with testosterone replacement therapy: An intention-to-treat observational cohort study. Lancet Diabetes Endocrinol. 2016;4:498–506. doi: 10.1016/S2213-8587(16)00112-1. [DOI] [PubMed] [Google Scholar]
- 479.Loo S.Y., Chen B.Y., Yu O.H.Y., Azoulay L., Renoux C. Testosterone replacement therapy and the risk of stroke in men: A systematic review. Maturitas. 2017;106:31–37. doi: 10.1016/j.maturitas.2017.08.013. [DOI] [PubMed] [Google Scholar]
- 480.Finkle W.D., Greenland S., Ridgeway G.K., Adams J.L., Frasco M.A., Cook M.B., Fraument J.F., Hoover R.N. Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PLoS ONE. 2014;9:e85805. doi: 10.1371/journal.pone.0085805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 481.Bhasin S., Brito J.P., Cunningham G.R., Hayes F.J., Hodis H.N., Matsumoto A.M., Snyder P.J., Swerdloff R.S., Wu F.C., Yialamas M.A. Testosterone therapy in men with hypogonadism: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2018;103:1715–1744. doi: 10.1210/jc.2018-00229. [DOI] [PubMed] [Google Scholar]
- 482.Bhasin S. Testosterone replacement in aging men: An evidence-based patient-centric perspective. J. Clin. Invest. 2021;131:e146607. doi: 10.1172/JCI146607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 483.Abildgaard J., Petersen J.H., Bang A.K., Aksglaede L., Christiansen P., Juul A., Jørgensen N. Long-term testosterone undecanoate treatment in the elderly testosterone deficient male: An observational cohort study. Andrology. 2022;10:322–332. doi: 10.1111/andr.13124. [DOI] [PubMed] [Google Scholar]
- 484.Forsdahl G., Erceg D., Geisendorfer T., Turkalj M., Plavec D., Thevis M., Tretzel L., Gmeiner G. Detection of testosterone esters in blood. Drug Test. Anal. 2015;7:983–989. doi: 10.1002/dta.1914. [DOI] [PubMed] [Google Scholar]
- 485.Solheim S.A., Levernæs M.C.S., Mørkeberg J., Juul A., Upners E.N., Nordsborg N.B., Dehnes Y. Stability and detectability of testosterone esters in dried blood spots after intramuscular injections. Drug Test. Anal. 2021 doi: 10.1002/dta.3030. [DOI] [PubMed] [Google Scholar]
- 486.Wahjoepramono E.J., Asih P.R., Aniwiyanti V., Taddei K., Dhaliwal S.S., Fuller S.J., Foster J., Carruthers M., Verdile G., Sohrabi H.R., et al. The effects of testosterone supplementation on cognitive functioning in older men. CNS Neurol. Disord.-Drug Targets. 2016;15:337–343. doi: 10.2174/1871527315666151110125704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 487.Kaweski S. Anti-aging medicine: Hormone replacement therapy in men. Plast. Reconstr. Surg. 2004;113:1506–1510. doi: 10.1097/01.PRS.0000125283.18798.DA. [DOI] [PubMed] [Google Scholar]
- 488.Cherrier M.M., Matsumoto A.M., Amory J.K., Ahmed S., Bremner W., Peskind E.R., Raskind M.A., Johnson M., Craft S. The role of aromatization in testosterone supplementation. Effects on cognition in older men. Neurology. 2005;64:290–296. doi: 10.1212/01.WNL.0000149639.25136.CA. [DOI] [PubMed] [Google Scholar]
- 489.Nelson J.A., Strauss L., Skowronski M., Ciufo R., Novak R., McFadden E.R. Effect of long-term salmeterol treatment on exercise-induced asthma. N. Engl. J. Med. 1998;339:141–146. doi: 10.1056/NEJM199807163390301. [DOI] [PubMed] [Google Scholar]
- 490.Kamp G.A. High dose growth hormone treatment induces acceleration of skeletal maturation and an earlier onset of puberty in children with idiopathic short stature. Arch. Dis. Child. 2002;87:215–220. doi: 10.1136/adc.87.3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 491.Alemany M., Fernández-López J.A., Petrobelli A., Granada M., Foz M., Remesar X. Pérdida de peso en un paciente con obesidad mórbida en tratamiento con oleoil-estrona (Weight loss in a patient with morbid obesity under treatment with oleoyl-estrone) Med. Clínica. 2003;121:496–499. doi: 10.1016/S0025-7753(03)74000-7. [DOI] [PubMed] [Google Scholar]
- 492.Liu P.Y., Yee B., Wishart S.M., Jimenez M., Jung D.G., Grunstein R.R., Handelsman D.J. The short-term effects of high-dose testosterone on sleep, breathing, and function in older men. J. Clin. Endocrinol. Metab. 2003;88:3605–3613. doi: 10.1210/jc.2003-030236. [DOI] [PubMed] [Google Scholar]
- 493.Mayo A., Macintyre H., Wallace A.M., Ahmed S.F. Transdermal testosterone application: Pharmacokinetics and effects on pubertal status, short-term growth, and bone turnover. J. Clin. Endocrinol. Metab. 2004;89:681–687. doi: 10.1210/jc.2003-031086. [DOI] [PubMed] [Google Scholar]
- 494.Tan W.S., Low W.Y., Ng C.J., Tan W.K., Tong S.F., Ho C., Khoo E.M., Lee G., Lee B.C., Lee V., et al. Efficacy and safety of long-acting intramuscular testosterone undecanoate in aging men: A randomised controlled study. Br. J. Urol. Int. 2013;111:1130–1140. doi: 10.1111/bju.12037. [DOI] [PubMed] [Google Scholar]
- 495.Partsch C.-J., Weinbauer G.F., Fang R., Nieschlag E. Injectable testosterone undecanoate has more favourable pharmacokinetics and pharmacodynamics than testosterone enanthate. Eur. J. Endocrinol. 1995;132:514–519. doi: 10.1530/eje.0.1320514. [DOI] [PubMed] [Google Scholar]
- 496.Gooren L.J.G. A ten-year safety study of the oral androgen testosterone undecanoate. J. Androl. 1994;15:212–215. doi: 10.1002/j.1939-4640.1994.tb00433.x. [DOI] [PubMed] [Google Scholar]
- 497.Snyder P.J., Peachey H., Berlin J.A., Hannoush P., Haddad G., Dlewati A., Santanna J., Loh L., Lenrow D.A., Holmes J.H., et al. Effects of testosterone replacement in hypogonadal men. J. Clin. Endocrinol. Metab. 2000;85:2670–2677. doi: 10.1210/jc.85.8.2670. [DOI] [PubMed] [Google Scholar]
- 498.Magnussen L.V., Glintborg D., Hermann P., Hougaard D.M., Højlund K., Andersen M. Effect of testosterone on insulin sensitivity, oxidative metabolism and body composition in aging men with type 2 diabetes on metformin monotherapy. Diabetes Obes. Metab. 2016;18:980–989. doi: 10.1111/dom.12701. [DOI] [PubMed] [Google Scholar]
- 499.Allan C.A., Strauss B.J.G., Burger H.G., Forbes E.A., McLachlan R.I. Testosterone therapy prevents gain in visceral adipose tissue and loss of skeletal muscle in nonobese aging men. J. Clin. Endocrinol. Metab. 2008;93:139–146. doi: 10.1210/jc.2007-1291. [DOI] [PubMed] [Google Scholar]
- 500.Barnouin Y., Armamento-Villareal R., Celli A., Jiang B., Paudyal A., Nambi V., Bryant M.S., Marcelli M., Garcia J.M., Qualls C., et al. Testosterone replacement therapy added to intensive lifestyle intervention in older men with obesity and hypogonadism. J. Clin. Endocrinol. Metab. 2021;106:E1096–E1110. doi: 10.1210/clinem/dgaa917. [DOI] [PubMed] [Google Scholar]
- 501.Frederiksen L., Højlund K., Hougaard D.M., Brixen K., Andersen M. Testosterone therapy increased muscle mass and lipid oxidation in aging men. Age. 2012;34:145–156. doi: 10.1007/s11357-011-9213-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 502.Magnussen L.V., Hvid L.G., Hermann A.P., Hougaard D.M., Gram B., Caserotti P., Andersen M.S. Testosterone therapy preserves muscle strength and power in aging men with type 2 diabetes-a randomized controlled trial. Andrology. 2017;5:946–953. doi: 10.1111/andr.12396. [DOI] [PubMed] [Google Scholar]
- 503.Howell S.J., Radford J.A., Adams J.E., Smets E.M.A., Warburton R., Shalet S.M. Randomized placebo-controlled trial of testosterone replacement in men with mild Leydig cell insufficiency following cytotoxic chemotherapy. Clin. Endocrinol. 2001;55:315–324. doi: 10.1046/j.1365-2265.2001.01297.x. [DOI] [PubMed] [Google Scholar]
- 504.Snyder P.J., Peachey H., Berlin J.A., Rader D., Usher D., Loh L., Hannoush P., Dlewati A., Holmes J.H., Santanna J., et al. Effect of transdermal testosterone treatment on serum lipid and apolipoprotein levels in men more than 65 years of age. Am. J. Med. 2001;111:255–260. doi: 10.1016/S0002-9343(01)00813-0. [DOI] [PubMed] [Google Scholar]
- 505.Kenny A.M., Prestwood K.M., Gruman C.A., Fabregas G., Biskup B., Mansoor G. Effects of transdermal testosterone on lipids and vascular reactivity in older men with low bioavailable testosterone levels. J. Gerontol. A. 2002;57:M460–M465. doi: 10.1093/gerona/57.7.M460. [DOI] [PubMed] [Google Scholar]
- 506.English K.M., Steeds R.P., Jones T.H., Diver M.J., Channer K.S. Low-dose transdermal testosterone therapy improves angina threshold in men with chronic stable angina. Circulation. 2000;102:1906–1911. doi: 10.1161/01.CIR.102.16.1906. [DOI] [PubMed] [Google Scholar]
- 507.Quang L.M., Kalhan A. Cardiovascular benefits and risks of testosterone replacement therapy in hypogonadal men with type 2 diabetes mellitus and/or the metabolic syndrome: A systematic review. Br. J. Diabetes. 2018;18:141–146. doi: 10.15277/bjd.2018.192. [DOI] [Google Scholar]
- 508.Chasland L.C., Green D.J., Schlaich M.P., Maiorana A.J., Cooke B.R., Cox K.L., Naylor L.H., Yeap B.B. Effects of testosterone treatment, with and without exercise training, on ambulatory blood pressure in middle-aged and older men. Clin. Endocrinol. 2021;95:176–186. doi: 10.1111/cen.14442. [DOI] [PubMed] [Google Scholar]
- 509.Shores M.M., Walsh T.J., Korpak A., Krakauer C., Forsberg C.W., Fox A.E., Moore K.P., Heckbert S.R., Thompson M.L., Smith N.L., et al. Association between testosterone treatment and risk of incident cardiovascular events among US male veterans with low testosterone levels and multiple medical comorbidities. J. Am. Heart Assoc. 2021;10:e020562. doi: 10.1161/JAHA.120.020562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 510.Budoff M.J., Ellenberg S.S., Lewis C.E., Mohler E.R., III, Wenger N.K., Bhasin S., Barrett-Connor E., Swerdloff R.S., Stephens-Shields A., Cauley J.A., et al. Testosterone treatment and coronary artery plaque volume in older men with low testosterone. J. Am. Med. Assoc. 2017;317:708–716. doi: 10.1001/jama.2016.21043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 511.Drinka P.J., Jochen A.L., Cuisinier M., Bloom R., Rudman I., Rudman D. Polycythemia as a complication of testosterone replacement therapy in nursing home men with low testosterone levels. J. Am. Geriatr. Soc. 1995;43:899–901. doi: 10.1111/j.1532-5415.1995.tb05534.x. [DOI] [PubMed] [Google Scholar]
- 512.Malkin C.J., Pugh P.J., Morris P.D., Kerry K.E., Jones R.D., Jones T.H., Channer K.S. Testosterone replacement in hypogonadal men with angina improves ischaemic threshold and quality of life. Heart. 2004;90:871–876. doi: 10.1136/hrt.2003.021121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 513.Aversa A., Isidori A.M., de Martino M.U., Caprio M., Fabbrini E., Rocchietti-March M., Frajese G., Fabbri A. Androgens and penile erection: Evidence for a direct relationship between free testosterone and cavernous vasodilation in men with erectile dysfunction. Clin. Endocrinol. 2000;53:517–522. doi: 10.1046/j.1365-2265.2000.01118.x. [DOI] [PubMed] [Google Scholar]
- 514.Aversa A., Bruzziches R., Francomano D., Rosano G., Isidori A.M., Lenzi A., Spera G. Effects of testosterone undecanoate on cardiovascular risk factors and atherosclerosis in middle-aged men with late-onset hypogonadism and metabolic syndrome: Results form a 24-month, randomized, double-blind, placebo-controlled study. J. Sex. Med. 2010;7:3495–3503. doi: 10.1111/j.1743-6109.2010.01931.x. [DOI] [PubMed] [Google Scholar]
- 515.Antonic K.G., Antonic B., Zuran I., Pfeifer M. Testosterone treatment longer than 1 year shows more effects on functional hypogonadism and related metabolic, vascular, diabetic and obesity parameters (results of the 2-year clinical trial) Aging Male. 2021;23:1442–1454. doi: 10.1080/13685538.2020.1793132. [DOI] [PubMed] [Google Scholar]
- 516.Kato Y., Shigehara K., Nakashima K., Iijima M., Kawagushi S., Nohara T., Izumi K., Kadono Y., Konaka H., Namiki M., et al. The five-year effects of testosterone replacement therapy on lipid profile and glucose tolerance among hypogonadal men in Japan: A case control study. Aging Male. 2020;23:23–28. doi: 10.1080/13685538.2018.1550060. [DOI] [PubMed] [Google Scholar]
- 517.Yassin A.A., Alwani M., Talib R., Almehmadi Y., Nettleship J.E., Alrumaihi K., Albaba B., Kelly D.M., Saad F. Long-term testosterone therapy improves liver parameters and steatosis in hypogonadal men: A prospective controlled registry study. Aging Male. 2021;23:1553–1563. doi: 10.1080/13685538.2020.1867094. [DOI] [PubMed] [Google Scholar]
- 518.Alwani M., Al-Zoubi R.M., Al-Qudimat A., Yassin A., Aboumarzouk O., Al-Rumaihi K., Talib R., Al-Ansari A. The impact of long-term testosterone therapy (TTh) in renal function (RF) among hypogonadal men: An observational cohort study. Ann. Med. Surg. 2021;69:102748. doi: 10.1016/j.amsu.2021.102748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 519.Saad F., Gooren L., Haider A., Yassin A. An exploratory study of the effects of 12 month administration of the novel long-acting testosterone undecanoate on measures of sexual function and the metabolic syndrome. Arch. Androl. 2007;53:353–357. doi: 10.1080/01485010701730880. [DOI] [PubMed] [Google Scholar]
- 520.Young N.R., Baker H.W.G., Liu G.D., Seeman E. Body-composition and muscle strength in healthy-men receiving testosterone enanthate for contraception. J. Clin. Endocrinol. Metab. 1993;77:1028–1032. doi: 10.1210/jcem.77.4.8408450. [DOI] [PubMed] [Google Scholar]
- 521.Hackett G., Cole N., Bhartia M., Kennedy D., Raju J., Wilkinson P., Saghir A. The response to testosterone undecanoate in men with type 2 diabetes is dependent on achieving threshold serum levels (the BLAST study) Int. J. Clin. Pract. 2014;68:203–215. doi: 10.1111/ijcp.12235. [DOI] [PubMed] [Google Scholar]
- 522.Kalinchenko S.Y., Tishova Y.A., Mskhalaya G.J., Gooren L.J.G., Giltay E.J., Saad F. Effects of testosterone supplementation on markers of the metabolic syndrome and inflammation in hypogonadal men with the metabolic syndrome: The double-blinded placebo-controlled Moscow study. Clin. Endocrinol. 2010;73:602–612. doi: 10.1111/j.1365-2265.2010.03845.x. [DOI] [PubMed] [Google Scholar]
- 523.Deng Q., Rasool R.U., Russell R.M., Natesan R., Asangani I.A. Targeting androgen regulation of TMPRSS2 and ACE2 as a therapeutic strategy to combat COVID-19. iScience. 2021;24:102254. doi: 10.1016/j.isci.2021.102254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 524.Haider A., Yassin A., Haider K.S., Doros G., Saad F., Rosano G.M.C. Men with testosterone deficiency and a history of cardiovascular diseases benefit from long-term testosterone therapy: Observational, real-life data from a registry study. Vasc. Health Risk Manag. 2016;12:251–261. doi: 10.2147/VHRM.S108947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 525.Francomano D., Lenzi A., Aversa A. Effects of five-year treatment with testosterone undecanoate on metabolic and hormonal parameters in ageing men with metabolic syndrome. Int. J. Endocrinol. 2014;2014:527470. doi: 10.1155/2014/527470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 526.Mathur A., Malkin C., Saeed B., Muthusamy R., Jones T.H., Channer K. Long-term benefits of testosterone replacement therapy on angina threshold and atheroma in men. Eur. J. Endocrinol. 2009;161:443–449. doi: 10.1530/EJE-09-0092. [DOI] [PubMed] [Google Scholar]
- 527.Wittert G.A., Chapman I.M., Haren M.T., Mackintosh S., Coates P., Morley J.E. Oral testosterone supplementation increases muscle and decreases fat mass in healthy elderly males with low–normal gonadal status. J. Gerontol. A. 2003;58:M618–M625. doi: 10.1093/gerona/58.7.M618. [DOI] [PubMed] [Google Scholar]
- 528.Boyanov M.A., Boneva Z., Christov V.G. Testosterone supplementation in men with type 2 diabetes, visceral obesity and partial androgen deficiency. Aging Male. 2003;6:1–7. doi: 10.1080/tam.6.1.1.7. [DOI] [PubMed] [Google Scholar]
- 529.Morley J.E., Perry H.M., III, Kaiser F.E., Kraenzle D., Jensen J., Houston K., Mattammal M., Perry H.M., Jr. Effects of testosterone replacement therapy in old hypogonadal males: A preliminary study. J. Am. Geriatr. Soc. 1993;41:149–152. doi: 10.1111/j.1532-5415.1993.tb02049.x. [DOI] [PubMed] [Google Scholar]
- 530.Hall G.M., Larbre J.P., Spector T.D., Perry L.A., da Silva J.A.P. A randomized trial of testosterone therapy in males with rheumatoid arthritis. Br. J. Rheumatol. 1996;35:568–573. doi: 10.1093/rheumatology/35.6.568. [DOI] [PubMed] [Google Scholar]
- 531.Page S.T., Amory J.K., Bowman F.D., Anawalt B.D., Matsumoto A.M., Bremner W.J., Tenover J.L. Exogenous testosterone (T) alone or with finasteride increases physical performance, grip strength, and lean body mass in older men with low serum T. J. Clin. Endocrinol. Metab. 2005;90:1502–1510. doi: 10.1210/jc.2004-1933. [DOI] [PubMed] [Google Scholar]
- 532.Casaburi R., Bhasin S., Cosentino L., Porszasz J., Somfay A., Lewis M.I., Fournier M., Storer T.W. Effects of testosterone and resistance training in men with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2004;170:870–878. doi: 10.1164/rccm.200305-617OC. [DOI] [PubMed] [Google Scholar]
- 533.Giagulli V.A., Carbone M.D., Ramunni M.I., Licchelli B., de Pergola G., Sabbà C., Guastamacchia E., Triggiani V. Adding liraglutide to lifestyle changes, metformin and testosterone therapy boosts erectile function in diabetic obese men with overt hypogonadism. Andrology. 2015;3:1094–1103. doi: 10.1111/andr.12099. [DOI] [PubMed] [Google Scholar]
- 534.Ferrando A.A., Sheffield-Moore M., Paddon-Jones D., Wolfe R.R., Urban R.J. Differential anabolic effects of testosterone and amino acid feeding in older men. J. Clin. Endocrinol. Metab. 2003;88:358–362. doi: 10.1210/jc.2002-021041. [DOI] [PubMed] [Google Scholar]
- 535.Svartberg J., Aasebø U., Hjalmarsen A., Sundsfjord J., Jorde R. Testosterone treatment improves body composition and sexual function in men with COPD, in a 6-month randomized controlled trial. Respir. Med. 2004;98:906–913. doi: 10.1016/j.rmed.2004.02.015. [DOI] [PubMed] [Google Scholar]
- 536.Sheffield-Moore M., Dillon E.L., Casperson S.L., Gilkison C.R., Paddon-Jones D., Durham W.J., Grady J.J., Urban R.J. A randomized pilot study of monthly cycled testosterone replacement or continuous testosterone replacement versus placebo in older men. J. Clin. Endocrinol. Metab. 2011;96:E1831–E1837. doi: 10.1210/jc.2011-1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 537.Amory J.K., Chansky H.A., Chansky K.L., Camuso M.R., Hoey C.T., Anawalt B.D., Matsumoto A.M., Bremner W.J. Preoperative supraphysiological testosterone in older men undergoing knee replacement surgery. J. Am. Geriatr. Soc. 2002;50:1698–1701. doi: 10.1046/j.1532-5415.2002.50462.x. [DOI] [PubMed] [Google Scholar]
- 538.Cheetham T.C., An J.J., Jacobsen S.J., Niu F., Sidney S., Quesenberry C.P., VanDenEeden S.K. Association of testosterone replacement with cardiovascular outcomes among men with androgen deficiency. JAMA Intern. Med. 2017;177:491–499. doi: 10.1001/jamainternmed.2016.9546. [DOI] [PubMed] [Google Scholar]
- 539.Jaffe M.D. Effect of testosterone cypionate on postexercise ST segment depression. Br. Heart J. 1977;39:1217–1222. doi: 10.1136/hrt.39.11.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 540.Li S.Y., Zhao Y.L., Yang Y.F., Wang X., Nie M., Wu X.Y., Mao J.F. Metabolic effects of testosterone replacement therapy in patients with type 2 diabetes mellitus or metabolic syndrome: A meta-analysis. Int. J. Endocrinol. 2020;2020:4732021. doi: 10.1155/2020/4732021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 541.Hackett G.I. Testosterone replacement therapy and mortality in older men. Drug Saf. 2016;39:117–130. doi: 10.1007/s40264-015-0348-y. [DOI] [PubMed] [Google Scholar]
- 542.Fernandez-Balsells M.M., Murad M.H., Lane M., Lampropulos J.F., Albuquerque F., Mullan R.J., Agrwal N., Elamin M.B., Gallegos-Orozco J.F., Wang A.T., et al. Adverse effects of testosterone therapy in adult men: A systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 2010;95:2560–2575. doi: 10.1210/jc.2009-2575. [DOI] [PubMed] [Google Scholar]
- 543.Snyder P.J., Peachey H., Hannoush P., Berlin J.A., Loh L., Holmes J.H., Dlewati A., Staley J., Santanna J., Kapoor S.C., et al. Effect of testosterone treatment on bone mineral density in men over 65 years of age1. J. Clin. Endocrinol. Metab. 1999;84:1966–1972. doi: 10.1210/jcem.84.6.5741. [DOI] [PubMed] [Google Scholar]
- 544.Li H., Benoit K., Wang W., Motsko S. Association between use of exogenous testosterone therapy and risk of venous thrombotic events among exogenous testosterone treated and untreated men with hypogonadism. J. Urol. 2016;195:1065–1072. doi: 10.1016/j.juro.2015.10.134. [DOI] [PubMed] [Google Scholar]
- 545.Hackett G., Cole N., Saghir A., Jones P., Strange R.C., Ramachandran S. Testosterone replacement therapy: Improved sexual desire and erectile function in men with type 2 diabetes following a 30-week randomized placebo-controlled study. Andrology. 2017;5:905–913. doi: 10.1111/andr.12399. [DOI] [PubMed] [Google Scholar]
- 546.Hackett G., Heald A.H., Sinclair A., Jones P.W., Strange R.C., Ramachandran S. Serum testosterone, testosterone replacement therapy and all-cause mortality in men with type 2 diabetes: Retrospective consideration of the impact of PDE5 inhibitors and statins. Int. J. Clin. Pract. 2016;70:244–253. doi: 10.1111/ijcp.12779. [DOI] [PubMed] [Google Scholar]
- 547.Wittert G., Bracken K., Robledo K.P., Grossmann M., Yeap B.B., Handelsman D.J., Stuckey B., Conway A., Inder W., McLachlan R., et al. Testosterone treatment to prevent or revert type 2 diabetes in men enrolled in a lifestyle programme (T4DM): A randomised, double-blind, placebo-controlled, 2-year, phase 3b trial. Lancet Diabetes Endocrinol. 2021;9:32–45. doi: 10.1016/S2213-8587(20)30367-3. [DOI] [PubMed] [Google Scholar]
- 548.Malkin C.J., Pugh P.J., Jones R.D., Kapoor D., Channer K.S., Jones T.H. The effect of testosterone replacement on endogenous inflammatory cytokines and lipid profiles in hypogonadal men. J. Clin. Endocrinol. Metab. 2004;89:3313–3318. doi: 10.1210/jc.2003-031069. [DOI] [PubMed] [Google Scholar]
- 549.Crawford B.A.L., Liu P.Y., Kean M.T., Bleasel J.F., Handelsman D.J. Randomized placebo-controlled trial of androgen effects on muscle and bone in men requiring long-term systemic glucocorticoid treatment. J. Clin. Endocrinol. Metab. 2003;88:3167–3176. doi: 10.1210/jc.2002-021827. [DOI] [PubMed] [Google Scholar]
- 550.Baillargeon J., Urban R.J., Kuo Y.-F., Ottenbacher K.J., Raji M.A., Du F., Lin Y.-l., Goodwin J.S. Risk of myocardial infarction in older men receiving testosterone therapy. Ann. Pharmacother. 2014;48:1138–1144. doi: 10.1177/1060028014539918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 551.Lunenfeld B., Nieschlag E. Testosterone therapy in the aging male. Aging Male. 2007;10:139–153. doi: 10.1080/13685530701485998. [DOI] [PubMed] [Google Scholar]
- 552.Hackett G. Metabolic effects of testosterone therapy in men with type 2 diabetes and metabolic syndrome. Sex. Med. Rev. 2019;7:476–490. doi: 10.1016/j.sxmr.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 553.Anderson J.L., May H.T., Lappé D.L., Bair T., Le V., Carlquist J.F., Muhlestein J.B. Impact of testosterone replacement therapy on myocardial infarction, stroke, and death in men with low testosterone concentrations in an integrated health care system. Am. J. Cardiol. 2016;117:794–799. doi: 10.1016/j.amjcard.2015.11.063. [DOI] [PubMed] [Google Scholar]
- 554.Wu S., Weng X. Therapeutic effect of andriol on serum lipids and apolipoproteins in elderly male coronary heart disease patients. Chin. Med. Sci. J. 1992;7:137–141. [PubMed] [Google Scholar]
- 555.Aversa A., Isidori A.M., Spera G., Lenzi A., Fabbri A. Androgens improve cavernous vasodilation and response to sildenafil in patients with erectile dysfunction. Clin. Endocrinol. 2003;58:632–638. doi: 10.1046/j.1365-2265.2003.01764.x. [DOI] [PubMed] [Google Scholar]
- 556.Calof O.M., Singh A.B., Lee M.L., Kenny A.M., Urban R.J., Tenover J.L., Bhasin S. Adverse events associated with testosterone replacement in middle-aged and older men: A meta-analysis of randomized, placebo-controlled trials. J. Gerontol. 2005;60:1451–1457. doi: 10.1093/gerona/60.11.1451. [DOI] [PubMed] [Google Scholar]
- 557.Muraleedharan V., Marsh H., Kapoor D., Channer K.S., Jones T.H. Testosterone deficiency is associated with increased risk of mortality and testosterone replacement improves survival in men with type 2 diabetes. Eur. J. Endocrinol. 2013;169:725–733. doi: 10.1530/EJE-13-0321. [DOI] [PubMed] [Google Scholar]
- 558.Ng Tang Fui M., Hoermann R., Bracken K., Handelsman D.J., Inder W.J., Stuckey B.G.A., Yeap B.B., Ghasem-Zadeh A., Robledo K.P., Jesudason D., et al. Effect of testosterone treatment on bone microarchitecture and bone mineral density in men: A 2-year RCT. J. Clin. Endocrinol. Metab. 2021;106:E3143–E3158. doi: 10.1210/clinem/dgab149. [DOI] [PubMed] [Google Scholar]
- 559.Garcia J.A., Sanchez P.E., Fraile C., Escovar P. Testosterone undecanoate improves erectile dysfunction in hypogonadal men with the metabolic syndrome refractory to treatment with phosphodiesterase type 5 inhibitors alone. Andrologia. 2011;43:293–296. doi: 10.1111/j.1439-0272.2009.00991.x. [DOI] [PubMed] [Google Scholar]
- 560.Emmelot-Vonk M.H., Verhaar H.J.J., Nakhai-Pour H.R., Grobbee D.E., van der Schouw Y.T. Effect of testosterone supplementation on sexual functioning in aging men: A 6-month randomized controlled trial. Int. J. Impot. Res. 2009;21:129–138. doi: 10.1038/ijir.2009.5. [DOI] [PubMed] [Google Scholar]
- 561.Amory J.K., Watts N.B., Easley K.A., Sutton P.R., Anawalt B.D., Matsumoto A.M., Bremner W.J., Tenover J.L. Exogenous testosterone or testosterone with finasteride increases bone mineral density in older men with low serum testosterone. J. Clin. Endocrinol. Metab. 2004;89:503–510. doi: 10.1210/jc.2003-031110. [DOI] [PubMed] [Google Scholar]
- 562.Colleluori G., Aguirre L., Napoli N., Qualls C., Villareal D.T., Armamento-Villareal R. Testosterone therapy effects on bone mass and turnover in hypogonadal men with type 2 diabetes. J. Clin. Endocrinol. Metab. 2021;106:E3058–E3068. doi: 10.1210/clinem/dgab181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 563.Shores M.M., Smith N.L., Forsberg C.W., Anawalt B.D., Matsumoto A.M. Testosterone treatment and mortality in men with low testosterone levels. J. Clin. Endocrinol. Metab. 2012;97:2050–2058. doi: 10.1210/jc.2011-2591. [DOI] [PubMed] [Google Scholar]
- 564.Sih R., Morley J.E., Kaiser F.E., Perry H.M., Patrick P., Ross C. Testosterone replacement in older hypogonadal men: A 12-month randomized controlled trial. J. Clin. Endocrinol. Metab. 1997;82:1661–1667. doi: 10.1210/jcem.82.6.3988. [DOI] [PubMed] [Google Scholar]
- 565.Poirier-Blanchette L., Koolian M., Blair Schwartz C. Testosterone replacement therapy causing extensive portal and mesenteric vein thrombosis. Am. J. Med. 2021;134:E426–E427. doi: 10.1016/j.amjmed.2020.12.018. [DOI] [PubMed] [Google Scholar]
- 566.Steinkampf M.P., Malizia B.A. Male infertility—A common side effect of testosterone therapy. Ala. BME Newsl. Rep. 2011;26:1–3. [Google Scholar]
- 567.Amore M., Innamorati M., Costi S., Sher L., Girardi P., Pompili M. Partial androgen deficiency, depression, and testosterone supplementation in aging men. Int. J. Endocrinol. 2012;2012:280724. doi: 10.1155/2012/280724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 568.Vigen R., O’Donnell C.I., Baron A.E., Grunwald G.K., Maddox T.M., Bradley S.M., Barqawi A., Woning G., Wierman M.E., Plomondon M.E., et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. J. Am. Med. Assoc. 2013;310:1829–1836. doi: 10.1001/jama.2013.280386. [DOI] [PubMed] [Google Scholar]
- 569.Matthiesson K.L., Amory J.K., Berger R., Ugoni A., McLachlan R.I., Bremner W.J. Novel male hormonal contraceptive combinations: The hormonal and spermatogenic effects of testosterone and levonorgestrel combined with a 5α-reductase inhibitor or gonadotropin-releasing hormone antagonist. J. Clin. Endocrinol. Metab. 2005;90:91–97. doi: 10.1210/jc.2004-1228. [DOI] [PubMed] [Google Scholar]
- 570.Windfeld-Mathiasen J., Dalhoff K.P., Andersen J.T., Klemp M., Horwitz A., Horwitz H. Male fertility before and after androgen abuse. J. Clin. Endocrinol. Metab. 2021;106:442–449. doi: 10.1210/clinem/dgaa837. [DOI] [PubMed] [Google Scholar]
- 571.Tan R.S., Pu S.J. A pilot study on the effects of testosterone in hypogonadal aging male patients with Alzheimer’s disease. Aging Male. 2003;6:13–17. doi: 10.1080/tam.6.1.13.17. [DOI] [PubMed] [Google Scholar]
- 572.Loo S.Y., Azoulay L., Nie R., dell’Aniello S., Yu O.H.Y., Renoux C. Cardiovascular and cerebrovascular safety of testosterone replacement therapy among aging men with low testosterone levels: A cohort study. Am. J. Med. 2019;132:1069–1077. doi: 10.1016/j.amjmed.2019.03.022. [DOI] [PubMed] [Google Scholar]
- 573.Jones S.D., Dukovac T., Sangkum P., Yafi F.A., Hellstrom W.J.G. Erythrocytosis and polycythemia secondary to testosterone replacement therapy in the aging male. Sex. Med. Rev. 2015;3:101–112. doi: 10.1002/smrj.43. [DOI] [PubMed] [Google Scholar]
- 574.Tenover J.S. Effects of testosterone supplementation in the aging male. J. Clin. Endocrinol. Metab. 1992;75:1092–1098. doi: 10.1210/jcem.75.4.1400877. [DOI] [PubMed] [Google Scholar]
- 575.Grossmann M., Hoermann R., Wittert G., Yeap B.B. Effects of testosterone treatment on glucose metabolism and symptoms in men with type 2 diabetes and the metabolic syndrome: A systematic review and meta-analysis of randomized controlled clinical trials. Clin. Endocrinol. 2015;83:344–351. doi: 10.1111/cen.12664. [DOI] [PubMed] [Google Scholar]
- 576.Laouali N., Brailly-Tabard S., Helmer C., Ancelin M.L., Tzourio C., Singh-Manoux A., Dugravot A., Elbaz A., Guiochon-Mantel A., Canonico M. Testosterone and all-cause mortality in older men: The role of metabolic syndrome. J. Endocr. Soc. 2018;2:322–335. doi: 10.1210/js.2018-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 577.Martínez C., Suissa S., Rietbrock S., Katholing A., Freedman B., Cohen A.T., Handelsman D.J. Testosterone treatment and risk of venous thromboembolism: Population based case-control study. Br. Med. J. 2016;355:i5968. doi: 10.1136/bmj.i5968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 578.FDA Approved Drug Products: TLANDO (Testosterone Undecanoate) Capsules, for Oral Use. Full Prescribing Information. FDA; Bethesda, MD, USA: 2022. [(accessed on 27 August 2022)]. Report Number. 4959091. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/208088s000lbl.pdf. [Google Scholar]
- 579.Zhu B., Chen Y., Xu F., Shen X., Chen X., Lv J., Zhang S. Androgens impair β-cell function in a mouse model of polycystic ovary syndrome by activating endoplasmic reticulum stress. Endocr. Connect. 2021;10:265–272. doi: 10.1530/EC-20-0608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 580.Yoshida A., Kaji T., Imaizumi J., Shirakawa A., Suga K., Nakagawa R., Maeda K., Irahara M., Iwasa T. Transgender man receiving testosterone treatment became pregnant and delivered a girl: A case report. J. Obstet. Gynaecol. Res. 2022;48:866–868. doi: 10.1111/jog.15145. [DOI] [PubMed] [Google Scholar]
- 581.Nieschlag E. Use of testosterone alone as hormonal male contraceptive. Basic Clin. Androl. 2012;22:136–140. doi: 10.1007/s12610-012-0187-y. [DOI] [Google Scholar]
- 582.Thirumalai A., Page S.T. Recent developments in male contraception. Drugs. 2019;79:11–20. doi: 10.1007/s40265-018-1038-8. [DOI] [PubMed] [Google Scholar]
- 583.World Health Organization Task Force on Methods for the Regulation of Male Fertility. Contraceptive efficacy of testosterone-induced azoospermia and oligozoospermia in normal men. Fertil. Steril. 1996;65:821–829. doi: 10.1016/S0015-0282(16)58221-1. [DOI] [PubMed] [Google Scholar]
- 584.Gava G., Meriggiola M.C. Update on male hormonal contraception. Ther. Adv. Endocrinol. Metab. 2019;10:2042018819834846. doi: 10.1177/2042018819834846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 585.Guo W., Bachman E., Li M., Roy C.N., Blusztajn J., Wong S., Chan S.Y., Serra C., Jasuja R., Travison T.G., et al. Testosterone administration inhibits hepcidin transcription and is associated with increased iron incorporation into red blood cells. Aging Cell. 2013;12:280–291. doi: 10.1111/acel.12052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 586.Bachman E., Travison T.G., Basaria S., Davda M.N., Guo W., Li M., Westfall J.C., Bae H., Gordeuk V., Bhasin S. Testosterone induces erythrocytosis via increased erythropoietin and suppressed hepcidin: Evidence for a new erythropoietin/hemoglobin set point. J. Gerontol. A. 2014;69:725–735. doi: 10.1093/gerona/glt154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 587.Zitzmann M., Cremers J.F., Krallmann C., Kliesch S. The HEAT-Registry (HEmatopoietic Affection by Testosterone): Comparison of a transdermal gel vs long-acting intramuscular testosterone undecanoate in hypogonadal men. Aging Male. 2022;25:134–144. doi: 10.1080/13685538.2022.2063830. [DOI] [PubMed] [Google Scholar]
- 588.Rochira V., Zirilli L., Madeo B., Maffei L., Carani C. Testosterone action on erythropoiesis does not require its aromatization to estrogen: Insights from the testosterone and estrogen treatment of two aromatase-deficient men. J. Steroid Biochem. Mol. Biol. 2009;113:189–194. doi: 10.1016/j.jsbmb.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 589.Molinari P.F., Rosenkrantz H. Erythropoietic activity and androgenic implications of 29 testosterone derivatives in orchiectomized rats. J. Lab. Clin. Med. 1971;78:399–410. doi: 10.5555/uri:pii:0022214371901132. [DOI] [PubMed] [Google Scholar]
- 590.Kochakian C.D., Welder A.A. Anabolic-androgenic steroids: In cell culture. In Vitro Cellular and Developmental Biology. Animal. 1993;29:433–438. doi: 10.1007/BF02639373. [DOI] [PubMed] [Google Scholar]
- 591.Bélanger C., Hould F.S., Lebel S., Biron S., Brochu G., Tchernof A. Omental and subcutaneous adipose tissue steroid levels in obese men. Steroids. 2006;71:674–682. doi: 10.1016/j.steroids.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 592.Sheng J., Kimmelman J., Zarin D. Citation-Impaired Clinical Trialing. The Scientist Digest. Jul 1, 2022. pp. 9–10.
- 593.Osterberg E.C., Bernie A.M., Ramasamy R. Risks of testosterone replacement therapy in men. Indian J. Urol. 2014;30:2–7. doi: 10.4103/0970-1591.124197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 594.Khodamoradi K., Khosravizadeh Z., Parmar M., Kuchakulla M., Ramasamy R., Arora H. Exogenous testosterone replacement therapy versus raising endogenous testosterone levels: Current and future prospects. Fertil. Steril. Rev. 2021;2:32–42. doi: 10.1016/j.xfnr.2020.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 595.Westfield G., Kaiser U.B., Lamb D.J., Ramasamy R. Short-acting testosterone: More physiologic? Front. Endocrinol. 2020;11:572465. doi: 10.3389/fendo.2020.572465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 596.Bolour S., Braunstein G. Testosterone therapy in women: A review. Int. J. Impot. Res. 2005;17:399–408. doi: 10.1038/sj.ijir.3901334. [DOI] [PubMed] [Google Scholar]
- 597.Dunsmoor-Su R., Fuller A., Voedisch A. Testosterone therapy in women: A clinical challenge. Obstet. Gynecol. 2021;138:809–812. doi: 10.1097/AOG.0000000000004566. [DOI] [PubMed] [Google Scholar]
- 598.Glaser R., Dimitrakakis C. Testosterone therapy in women: Myths and misconceptions. Maturitas. 2013;74:230–234. doi: 10.1016/j.maturitas.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 599.Somboonporn W., Davis S.R. Testosterone effects on the breast: Implications for testosterone therapy for women. Endocr. Rev. 2004;25:374–388. doi: 10.1210/er.2003-0016. [DOI] [PubMed] [Google Scholar]
- 600.Pasquali R., Zanotti L., Fanelli F., Mezzullo M., Fazzini A., Labate A.M.M., Repaci A., Ribichini D., Gambineri A. Defining hyperandrogenism in women with polycystic ovary syndrome: A challenging perspective. J. Clin. Endocrinol. Metab. 2016;101:2013–2022. doi: 10.1210/jc.2015-4009. [DOI] [PubMed] [Google Scholar]
- 601.Zaman A., Rothman M.S. Postmenopausal hyperandrogenism: Evaluation and treatment strategies. Endocrinol. Metab. Clin. N. Am. 2021;50:97–111. doi: 10.1016/j.ecl.2020.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 602.Cussons A.J., Stuckey B.G.A., Walsh J.P., Burke V., Norman R.J. Polycystic ovarian syndrome: Marked differences between endocrinologists and gynaecologists in diagnosis and management. Clin. Endocrinol. 2005;62:289–295. doi: 10.1111/j.1365-2265.2004.02208.x. [DOI] [PubMed] [Google Scholar]
- 603.Abbott D.H., Dumesic D.A., Levine J.E. Hyperandrogenic origins of polycystic ovary syndrome-implications for pathophysiology and therapy. Expert Rev. Endocrinol. Metab. 2019;14:131–143. doi: 10.1080/17446651.2019.1576522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 604.Diamanti-Kandarakis E., Dunaif A. Insulin resistance and the polycystic ovary syndrome revisited: An update on mechanisms and implications. Endocr. Rev. 2012;33:981–1030. doi: 10.1210/er.2011-1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 605.Jeanes Y.M., Reeves S. Metabolic consequences of obesity and insulin resistance in polycystic ovary syndrome: Diagnostic and methodological challenges. Nutr. Res. Rev. 2017;30:97–105. doi: 10.1017/S0954422416000287. [DOI] [PubMed] [Google Scholar]
- 606.Markopoulos M.C., Rizos D., Valsamakis G., Deligeoroglou E., Grigoriou O., Chrousos G.P., Creatsas G., Mastorakos G. Hyperandrogenism in women with polycystic ovary syndrome persists after menopause. J. Clin. Endocrinol. Metab. 2011;96:623–631. doi: 10.1210/jc.2010-0130. [DOI] [PubMed] [Google Scholar]
- 607.Burger H.G. Androgen production in women. Fertil. Steril. 2002;77:3–5. doi: 10.1016/S0015-0282(02)02985-0. [DOI] [PubMed] [Google Scholar]
- 608.Foth D., Römer T. Postmenopausal hyperandrogenemia (android obesity, insulin resistance, diabetes mellitus) and therapeutic consequences. In: Fischl F.H., editor. Menopause Andropause. Hormone Replacement Therapy through the Ages. New Cognition and Therapy Concepts. 1st ed. Krause & Pachernegg; Gablitz, Austria: 2001. pp. 159–163. [Google Scholar]
- 609.Gilling-Smith C., Willis D.S., Beard R.W., Franks S. Hypersecretion of androstenedione by isolated thecal cells from polycystic ovaries. J. Clin. Endocrinol. Metab. 1994;79:1158–1165. doi: 10.1210/jcem.79.4.7962289. [DOI] [PubMed] [Google Scholar]
- 610.Kumar A., Woods K.S., Bartolucci A.A., Azziz R. Prevalence of adrenal androgen excess in patients with the polycystic ovary syndrome (PCOS) Clin. Endocrinol. 2005;62:644–649. doi: 10.1111/j.1365-2265.2005.02256.x. [DOI] [PubMed] [Google Scholar]
- 611.MacDonald P.C., Edman C.D., Hemsell D.L., Porter J.C., Siiteri P.K. Effect of obesity on conversion of plasma androstenedione to estrone in postmenopausal women with and without endometrial cancer. Am. J. Obstet. Gynecol. 1978;130:448–455. doi: 10.1016/0002-9378(78)90287-9. [DOI] [PubMed] [Google Scholar]
- 612.Judd H.L., Judd G.E., Lucas W.E., Yen S.S.C. Endocrine function of the postmenopausal ovary: Concentration of androgens and estrogens in ovarian and peripheral vein blood. J. Clin. Endocrinol. Metab. 1974;39:1020–1024. doi: 10.1210/jcem-39-6-1020. [DOI] [PubMed] [Google Scholar]
- 613.O’Reilly M.W., Kempegowda P., Jenkinson C., Taylor A.E., Quanson J.L., Storbeck K.-H., Arlt W. 11-Oxygenated C19 steroids are the predominant androgens in polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 2017;102:840–848. doi: 10.1210/jc.2016-3285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 614.Gonzales G.F., Góñez C., Villena A. Adrenopause or decline of serum adrenal androgens with age in women living at sea level or at high altitude. J. Endocrinol. 2002;173:95–102. doi: 10.1677/joe.0.1730095. [DOI] [PubMed] [Google Scholar]
- 615.Pandey S., Srinivas M., Agashe S., Joshi J., Galvankar P., Prakasam C.P., Vaidya R. Menopause and metabolic syndrome: A study of 498 urban women from western India. J. Midlife Health. 2010;1:63–69. doi: 10.4103/0976-7800.76214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 616.Golden S.H., Ding J., Szklo M., Schmidt M.I., Duncan B.B., Dobs A. Glucose and insulin components of the metabolic syndrome are associated with hyperandrogenism in postmenopausal women: The Atherosclerosis Risk in Communities Study. Am. J. Epidemiol. 2004;160:540–548. doi: 10.1093/aje/kwh250. [DOI] [PubMed] [Google Scholar]
- 617.Alpañés M., González-Casbas J.M., Sánchez J., Pián H., Escobar-Morreale H.F. Management of postmenopausal virilization. J. Clin. Endocrinol. Metab. 2012;97:2584–2588. doi: 10.1210/jc.2012-1683. [DOI] [PubMed] [Google Scholar]
- 618.Brind J., Strain G., Miller L., Zumoff B., Vogelman J., Orentreich N. Obese men have elevated plasma levels of estrone sulfate. Int. J. Obes. 1990;14:483–486. [PubMed] [Google Scholar]
- 619.Remesar X., Tang V., Ferrer E., Torregrosa C., Virgili J., Masanés R.M., Fernández-López J.A., Alemany M. Estrone in food: A factor influencing the development of obesity? Eur. J. Nutr. 1999;38:247–253. doi: 10.1007/s003940050068. [DOI] [PubMed] [Google Scholar]
- 620.Glintborg D., Hermann A.P., Brusgaard K., Hangaard J., Hagen C., Andersen M. Significantly higher adrenocorticotropin-stimulated cortisol and 17-hydroxyprogesterone levels in 337 consecutive, premenopausal, caucasian, hirsute patients compared with healthy controls. J. Clin. Endocrinol. Metab. 2005;90:1347–1353. doi: 10.1210/jc.2004-1214. [DOI] [PubMed] [Google Scholar]
- 621.Cagnacci A., Cannoletta M., Caretto S., Zanin R., Xholli A., Volpe A. Increased cortisol level: A possible link between climacteric symptoms and cardiovascular risk factors. Menopause. 2011;18:273–278. doi: 10.1097/gme.0b013e3181f31947. [DOI] [PubMed] [Google Scholar]
- 622.Genazzani A.R., Pluchino N., Begliuomini S., Stomati M., Bernardi F., Pierv M., Casarosa E., Palumbo M., Genazzani A.D., Luisi M. Long-term low-dose oral administration of dehydroepiandrosterone modulates adrenal response to adrenocorticotropic hormone in early and late postmenopausal women. Gynecol. Endocrinol. 2006;22:627–635. doi: 10.1080/09513590601024681. [DOI] [PubMed] [Google Scholar]
- 623.Anagnostis P., Bosdou J.K., Vaitsi K., Goulis D.G., Lambrinoudaki I. Estrogen and bones after menopause: A reappraisal of data and future perspectives. Hormones. 2021;20:13–21. doi: 10.1007/s42000-020-00218-6. [DOI] [PubMed] [Google Scholar]
- 624.Heiss C.J., Sanborn C.F., Nichols D.L., Bonnick S.L., Alford B.B. Associations of body fat distribution, circulating sex hormones, and bone density in postmenopausal women. J. Clin. Endocrinol. Metab. 1995;80:1591–1596. doi: 10.1210/jcem.80.5.7745005. [DOI] [PubMed] [Google Scholar]
- 625.Altindag O., Altindag A., Asoglu M., Gunes M., Soran N., Deveci Z. Relation of cortisol levels and bone mineral density among premenopausal women with major depression. Int. J. Clin. Pract. 2007;61:416–420. doi: 10.1111/j.1742-1241.2006.01276.x. [DOI] [PubMed] [Google Scholar]
- 626.Zhang Z., Ren H., Shen G., Qiu T., Liang D., Yang Z., Yao Z., Tang J., Jiang X., Wei Q. Animal models for glucocorticoid-induced postmenopausal osteoporosis: An updated review. Biomed. Pharmacother. 2016;84:438–446. doi: 10.1016/j.biopha.2016.09.045. [DOI] [PubMed] [Google Scholar]
- 627.Lindsay R. The menopause and osteoporosis. Obstet. Gynecol. 1996;87:16S–19S. doi: 10.1016/0029-7844(95)00430-0. [DOI] [PubMed] [Google Scholar]
- 628.Tella S.H., Gallagher J.C. Prevention and treatment of postmenopausal osteoporosis. J. Steroid Biochem. Mol. Biol. 2014;142:155–170. doi: 10.1016/j.jsbmb.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 629.Blain H., Carrière I., Favier F., Jeandel C., Papoz L. Body weight change since menopause and percentage body fat mass are predictors of subsequent bone mineral density change of the proximal femur in women aged 75 years and older: Results of a 5 year prospective study. Calcif. Tissue Int. 2004;75:32–39. doi: 10.1007/s00223-003-0192-4. [DOI] [PubMed] [Google Scholar]
- 630.Marzullo P., Mele C., Mai S., Nardone A., Scacchi M., Aimaretti G. Obesity and bone loss at menopause: The role of sclerostin. Diagnostics. 2021;11:1914. doi: 10.3390/diagnostics11101914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 631.Lin Y.-H., Teng M., Huo M. Association of possible sarcopenic obesity with osteoporosis and fragility fractures in postmenopausal women. Arch. Osteoporos. 2022;17:65. doi: 10.1007/s11657-022-01107-8. [DOI] [PubMed] [Google Scholar]
- 632.Li J., Chen X., Lu L.Y., Yu X.J. The relationship between bone marrow adipose tissue and bone metabolism in postmenopausal osteoporosis. Cytokine Growth Factor Rev. 2020;52:88–98. doi: 10.1016/j.cytogfr.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 633.Abdi F., Mobedi H., Bayat F., Mosaffa N., Dolatian M., Tehranif F.R. The effects of transdermal estrogen delivery on bone mineral density in postmenopausal women: A meta-analysis. Iran. J. Pharm. Res. 2017;16:380–389. [PMC free article] [PubMed] [Google Scholar]
- 634.Khastgir G., Studd J., Holland N., Alaghband-Zadeh J., Fox S., Chow J. Anabolic effect of estrogen replacement on bone in postmenopausal women with osteoporosis: Histomorphometric evidence in a longitudinal study. J. Clin. Endocrinol. Metab. 2001;86:289–295. doi: 10.1210/jc.86.1.289. [DOI] [PubMed] [Google Scholar]
- 635.Bonomo S.M., Rigamonti A.E., Giunta M., Galimberti D., Guaita A., Gagliano M.G., Müller E.E., Cella S.G. Menopausal transition: A possible risk factor for brain pathologic events. Neurobiol. Aging. 2009;30:71–80. doi: 10.1016/j.neurobiolaging.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 636.Van Geel T.A.C.M., Geusens P.P., Winkens B., Sels J.P.J.E., Dinant G.J. Measures of bioavailable serum testosterone and estradiol and their relationships with muscle mass, muscle strength and bone mineral density in postmenopausal women: A cross-sectional study. Eur. J. Endocrinol. 2009;160:681–687. doi: 10.1530/EJE-08-0702. [DOI] [PubMed] [Google Scholar]
- 637.Panzer C., Guay A. Testosterone replacement therapy in naturally and surgically menopausal women (CME) J. Sex. Med. 2009;6:8–18. doi: 10.1111/j.1743-6109.2008.01128.x. [DOI] [PubMed] [Google Scholar]
- 638.Iellamo F., Volterrani M., Caminiti G., Karam R., Massaro R., Fini M., Collins P., Rosano Giuseppe M.C. Testosterone therapy in women with chronic heart failure. J. Am. Coll. Cardiol. 2010;56:1310–1316. doi: 10.1016/j.jacc.2010.03.090. [DOI] [PubMed] [Google Scholar]
- 639.Flöter A., Nathorst-Böös J., Carlström K., von Schoultz B. Addition of testosterone to estrogen replacement therapy in oophorectomized women: Effects on sexuality and well-being. Climacteric. 2002;5:357–365. doi: 10.1080/cmt.5.4.357.365. [DOI] [PubMed] [Google Scholar]
- 640.Lunenfeld B. Testosterone deficiency and the metabolic syndrome. Aging Male. 2007;10:53–56. doi: 10.1080/13685530701390800. [DOI] [PubMed] [Google Scholar]
- 641.Hansen Viuff M., Just J., Brun S., Vrist Dam T., Hansen M., Melgaard L., Hougaard D.M., Lappe M., Højbjerg Gravholt C. Women with Turner syndrome are both estrogen and androgen deficient: The impact of hormone replacement therapy. J. Clin. Endocrinol. Metab. 2022;107:1983–1993. doi: 10.1210/clinem/dgac167. [DOI] [PubMed] [Google Scholar]
- 642.Tanabe M., Akehil Y., Nomiyama T., Murakami J., Yanase T. Total testosterone is the most valuable indicator of metabolic syndrome among various testosterone values in middle-aged Japanese men. Endocr. J. 2015;62:123–132. doi: 10.1507/endocrj.EJ14-0313. [DOI] [PubMed] [Google Scholar]
- 643.Maestripieri D., Mayhew J., Carlson C.L., Hoffman C.L., Radtke J.M. One-male harems and female social dynamics in Guinea baboons. Folia Primatol. 2007;78:56–68. doi: 10.1159/000095686. [DOI] [PubMed] [Google Scholar]
- 644.Teichroeb J.A., Jack K.M. Alpha male replacements in nonhuman primates: Variability in processes, outcomes, and terminology. Am. J. Primatol. 2017;79:e22674. doi: 10.1002/ajp.22674. [DOI] [PubMed] [Google Scholar]
- 645.Beehner J.C., Bergman T.J., Cheney D.L., Seyfarth R.M., Whitten P.L. Testosterone predicts future dominance rank and mating activity among male Chacma baboons. Behav. Ecol. Sociobiol. 2006;59:469–479. doi: 10.1007/s00265-005-0071-2. [DOI] [Google Scholar]
- 646.Bhasin S., Cunningham G.R., Hayes F.J., Matsumoto A.M., Snyder P.J., Swerdloff R.S., Montori V.M. Testosterone therapy in adult men with androgen deficiency syndromes: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2006;91:1995–2010. doi: 10.1210/jc.2005-2847. [DOI] [PubMed] [Google Scholar]
- 647.Bhasin S., Cunningham G.R., Hayes F.J., Matsumoto A.M., Snyder P.J., Swerdloff R.S., Montori V.M. Testosterone therapy in men with androgen deficiency Syndromes: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2010;95:2536–2559. doi: 10.1210/jc.2009-2354. [DOI] [PubMed] [Google Scholar]
- 648.Dimopoulou C., Ceausu I., Depypere H., Lambrinoudaki I., Mueck A., Pérez-López F.R., Rees M., van der Schouw Y.T., Senturk L.M., Simonsini T., et al. EMAS position statement: Testosterone replacement therapy in the aging male. Maturitas. 2016;84:94–99. doi: 10.1016/j.maturitas.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 649.Pelzman D.L., Hwang K. Testosterone therapy: Where do the latest guidelines agree and differ? Curr. Opin. Endocrinol. Diabetes Obes. 2020;27:397–403. doi: 10.1097/MED.0000000000000581. [DOI] [PubMed] [Google Scholar]
- 650.Handelsman D.J. Global trends in testosterone prescribing, 2000–2011: Expanding the spectrum of prescription drug misuse. Med. J. Aust. 2013;199:548–551. doi: 10.5694/mja13.10111. [DOI] [PubMed] [Google Scholar]
- 651.Wierman M.E., Basson R., Davis S.R., Khosla S., Miller K.K., Rosner W., Santoro N. Androgen therapy in women: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2006;91:3697–3710. doi: 10.1210/jc.2006-1121. [DOI] [PubMed] [Google Scholar]
- 652.Parish S.J., Simon J.A., Davis S.R., Giraldi A., Goldstein I., Goldstein S.W., Kim N.N., Kingsberg S.A., Morgentaler A., Nappi R.E., et al. International Society for the Study of Women’s Sexual Health clinical practice guideline for the use of systemic testosterone for hypoactive sexual desire disorder in women. J. Women’s Health. 2021;30:474–491. doi: 10.1089/jwh.2021.29037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 653.Davis S.R., Baber R., Panay N., Bitzer J., Perez S.C., Islam R.M., Kaunitz A.M., Kingsbergg S.A., Lambrinoudaki I., Liu J., et al. Global consensus position statement on the use of testosterone therapy for women. Maturitas. 2019;128:89–93. doi: 10.1016/j.maturitas.2019.07.001. [DOI] [PubMed] [Google Scholar]
- 654.Handelsman D.J. Androgen misuse and abuse. Endocr. Rev. 2021;42:457–501. doi: 10.1210/endrev/bnab001. [DOI] [PubMed] [Google Scholar]
- 655.Kanayama G., Pope H.G. Illicit use of androgens and other hormones. Curr. Opin. Endocrinol. Diabetes Obes. 2012;19:211–219. doi: 10.1097/MED.0b013e3283524008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 656.Myers J.B., Meacham R.B. Androgen replacement therapy in the aging male. Rev. Urol. 2003;5:216–226. [PMC free article] [PubMed] [Google Scholar]
- 657.Morgentaler A., Zitzmann M., Traish A.M., Fox A.W., Jones T.H., Maggi M., Arver S., Aversa A., Chan J.C.N., Dobs A.S., et al. Fundamental concepts regarding testosterone deficiency and treatment. Mayo Clin. Proc. 2016;91:881–896. doi: 10.1016/j.mayocp.2016.04.007. [DOI] [PubMed] [Google Scholar]
- 658.Grossmann M. Testosterone and glucose metabolism in men: Current concepts and controversies. J. Endocrinol. 2014;220:R37–R55. doi: 10.1530/JOE-13-0393. [DOI] [PubMed] [Google Scholar]
- 659.Brodsky I.G., Balagopal P., Nair K.S. Effects of testosterone replacement on muscle mass and muscle protein synthesis in hypogonadal men. A clinical research center study. J. Clin. Endocrinol. Metab. 1996;81:3469–3475. doi: 10.1210/jcem.81.10.8855787. [DOI] [PubMed] [Google Scholar]
- 660.Wang C., Cunningham G., Dobs A., Iranmanesh A., Matsumoto A.M., Snyder P.J., Weber T., Berman N., Hull L., Swerdloff R.S. Long-term testosterone gel (AndroGel) treatment maintains beneficial effects on sexual function and mood, lean and fat mass, and bone mineral density in hypogonadal men. J. Clin. Endocrinol. Metab. 2004;89:2085–2098. doi: 10.1210/jc.2003-032006. [DOI] [PubMed] [Google Scholar]
- 661.Straftis A.A., Gray P.B. Sex, energy, well-being and low testosterone: An exploratory survey of U. S. men’s experiences on prescription testosterone. Int. J. Environ. Res. Public Health. 2019;16:3261. doi: 10.3390/ijerph16183261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 662.Kaur H., Werstuck G.H. The effect of testosterone on cardiovascular disease and cardiovascular risk factors in men: A review of clinical and preclinical data. CJC Open. 2021;3:1238–1248. doi: 10.1016/j.cjco.2021.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 663.Bahrke M.S., Yesalis C.E., Wright J.E. Psychological and behavioural effects of endogenous testosterone and anabolic-androgenic steroids. Sport. Med. 1996;22:367–390. doi: 10.2165/00007256-199622060-00005. [DOI] [PubMed] [Google Scholar]
- 664.Parkinson A.B., Evans N.A. Anabolic androgenic steroids: A survey of 500 users. Med. Sci. Sport. Exerc. 2006;38:644–651. doi: 10.1249/01.mss.0000210194.56834.5d. [DOI] [PubMed] [Google Scholar]
- 665.Nieschlag E., Vorona E. Mechanisms in endocrinology: Medical consequences of doping with anabolic androgenic steroids: Effects on reproductive functions. Eur. J. Endocrinol. 2015;173:R47–R58. doi: 10.1530/EJE-15-0080. [DOI] [PubMed] [Google Scholar]
- 666.Graf C.E., Pichard C., Herrmann F.R., Sieber C.C., Zekry D., Genton L. Prevalence of low muscle mass according to body mass index in older adults. Nutrition. 2017;34:124–129. doi: 10.1016/j.nut.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 667.Lu Y.X., Karagounis L.G., Ng T.P., Carre C., Narang V., Wong G., Ying Tan C.T., Zin Nyunt M.S., Gao Q., Abel B., et al. Systemic and metabolic signature of sarcopenia in community-dwelling older adults. J. Gerontol. A. 2020;75:309–317. doi: 10.1093/gerona/glz001. [DOI] [PubMed] [Google Scholar]
- 668.Papadopoulou S.K. Sarcopenia: A contemporary health problem among older adult populations. Nutrients. 2020;12:1293. doi: 10.3390/nu12051293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 669.Lee D.-Y., Shin S. Association of sarcopenia with osteopenia and osteoporosis in community-dwelling older Korean adults: A cross-sectional study. J. Clin. Med. 2022;11:129. doi: 10.3390/jcm11010129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 670.Batsis J.A., Mackenzie T.A., Barre L.K., Lopez-Jimenez F., Bartels S.J. Sarcopenia, sarcopenic obesity and mortality in older adults: Results from the National Health and Nutrition Examination Survey III. Eur. J. Clin. Nutr. 2014;68:1001–1007. doi: 10.1038/ejcn.2014.117. [DOI] [PubMed] [Google Scholar]
- 671.Sanchez-Rodriguez D., Marco E., Cruz-Jentoft A.J. Defining sarcopenia: Some caveats and challenges. Curr. Opin. Clin. Nutr. Metab. Care. 2020;23:127–132. doi: 10.1097/MCO.0000000000000621. [DOI] [PubMed] [Google Scholar]
- 672.Basile G., Sardella A. From cognitive to motor impairment and from sarcopenia to cognitive impairment: A bidirectional pathway towards frailty and disability. Aging Clin. Exp. Res. 2021;33:469–478. doi: 10.1007/s40520-020-01550-y. [DOI] [PubMed] [Google Scholar]
- 673.Park S.W., Gooodpaster B.H., Lee J.S., Kuller L.H., Boudreau R., de Rekeneire N., Harris T.B., Kritchevsky S., Tylavsky F.A., Nevitt M., et al. Excessive loss of skeletal muscle mass in older adults with type 2 diabetes. Diabetes Care. 2009;32:1993–1997. doi: 10.2337/dc09-0264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 674.Tong Q., Wang X., Sheng Y., Chen S., Lai B., Lv R., Yu J. Metabolic syndrome and its association with components of sarcopenia in older community-dwelling Chinese. J. Biomed. Res. 2022;36:120–126. doi: 10.7555/JBR.36.20210143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 675.Petermann-Rocha F., Gray S.R., Pell J.P., Ho F.K., Celis-Morales C. The joint association of sarcopenia and frailty with incidence and mortality health outcomes: A prospective study. Clin. Nutr. 2021;40:2427–2434. doi: 10.1016/j.clnu.2020.10.044. [DOI] [PubMed] [Google Scholar]
- 676.Thompson M.Q., Yu S., Tucker G.R., Adams R.J., Cesari M., Theou O., Visvanathan R. Frailty and sarcopenia in combination are more predictive of mortality than either condition alone. Maturitas. 2021;144:102–107. doi: 10.1016/j.maturitas.2020.11.009. [DOI] [PubMed] [Google Scholar]
- 677.Murton A.J. Muscle protein turnover in the elderly and its potential contribution to the development of sarcopenia. Proc. Nutr. Soc. 2015;74:387–396. doi: 10.1017/S0029665115000130. [DOI] [PubMed] [Google Scholar]
- 678.Batsis J.A., Petersen C.L., Crow R.S., Cook S.B., Stevens C.J., Seo L.M., Brooks E., Mackenzie T.A. Weight change and risk of the foundation of National Institute of Health Sarcopenia-defined low lean mass: Data from the National Health and Nutrition examination surveys 1999-2004. Clin. Nutr. 2020;39:2463–2470. doi: 10.1016/j.clnu.2019.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 679.Khadra D., Itani L., Chebaro Y., Obeid M., Jaber M., Ghanem R., Ayton A., Kreidieh D., Masri D.E., Kimura A., et al. Association between sarcopenic obesity and metabolic syndrome in adults: A systematic review and meta-analysis. Curr. Cardiol. Rev. 2020;16:153–162. doi: 10.2174/1573403X16666200214104122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 680.Gallagher D., Delegge M. Body composition (sarcopenia) in obese patients. J. Parenter. Enter. Nutr. 2011;35:21S–28S. doi: 10.1177/0148607111413773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 681.Kim E.Y., Lee H.Y., Kim Y.S., Park I., Ahn H.K., Cho E.K., Jeong Y.M., Kim J.H. Prognostic significance of cachexia score assessed by CT in male patients with small cell lung cancer. Eur. J. Cancer Care. 2018;27:e12695. doi: 10.1111/ecc.12695. [DOI] [PubMed] [Google Scholar]
- 682.Argilés J.M., Busquets S., Felipe A., López-Soriano F.J. Molecular mechanisms involved in muscle wasting in cancer and ageing: Cachexia versus sarcopenia. Int. J. Biochem. Cell Biol. 2005;37:1084–1104. doi: 10.1016/j.biocel.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 683.Chapman I.M., Visvanathan R., Hammond A.J., Morley J.E., Field J.B., Tai K., Belobrajdic D.P., Chen R.Y., Horowitz M. Effect of testosterone and a nutritional supplement, alone and in combination, on hospital admissions in undernourished older men and women. Am. J. Clin. Nutr. 2009;89:880–889. doi: 10.3945/ajcn.2008.26538. [DOI] [PubMed] [Google Scholar]
- 684.Ikizler T.A., Cano N.J., Franch H., Fouque D., Himmelfarb J., Kalantar-Zadeh K., Kuhlmann M.K., Stenvinkel P., Terwee P., Teta D., et al. Prevention and treatment of protein energy wasting in chronic kidney disease patients: A consensus statement by the International Society of Renal Nutrition and Metabolism. Kidney Int. 2013;84:1096–1107. doi: 10.1038/ki.2013.147. [DOI] [PubMed] [Google Scholar]
- 685.Visvanathan R., Piantadosi C., Lange K., Naganathan V., Hunter P., Cameron I.D., Chapman I. The randomized control trial of the effects of testosterone and a nutritional supplement on hospital admissions in undernourished, community dwelling, older people. J. Nutr. Health Aging. 2016;20:769–779. doi: 10.1007/s12603-016-0689-y. [DOI] [PubMed] [Google Scholar]
- 686.Rhee H., Navaratnam A., Oleinikova I., Gilroy D., Scuderi Y., Heathcote P., Nguyen T., Wood S., Ho K.K.Y. A novel liver-targeted testosterone therapy for sarcopenia in androgen deprived men with prostate cancer. J. Endocr. Soc. 2021;5:bvab116. doi: 10.1210/jendso/bvab116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 687.Burney B.O., Hayes T.G., Smiechowska J., Cardwell G., Papusha V., Bhargava P., Konda B., Auchus R.J., Garcia J.M. Low testosterone levels and increased inflammatory markers in patients with cancer and relationship with cachexia. J. Clin. Endocrinol. Metab. 2012;97:E700–E709. doi: 10.1210/jc.2011-2387. [DOI] [PubMed] [Google Scholar]
- 688.Gullett N.P., Hebbar G., Ziegler T.R. Update on clinical trials of growth factors and anabolic steroids in cachexia and wasting. American J. Clin. Nutr. 2010;91:1143S–1147S. doi: 10.3945/ajcn.2010.28608E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 689.Laughlin G.A., Barrett-Connor E., Bergstrom J. Low serum testosterone and mortality in older men. J. Clin. Endocrinol. Metab. 2008;93:68–75. doi: 10.1210/jc.2007-1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 690.Gray A., Feldman H.A., Mckinlay J.B., Longcope C. Age, disease, and changing sex hormone levels in middle-aged men: Results of the Massachusetts Male Aging Study. J. Clin. Endocrinol. Metab. 1991;73:1016–1025. doi: 10.1210/jcem-73-5-1016. [DOI] [PubMed] [Google Scholar]
- 691.Morley J.E., Kaiser F.E., Perry H.M., Patrick P., Morley P.M.K., Stauber P.M., Vellas B., Baumgartner R.N., Garry P.J. Longitudinal changes in testosterone, luteinizing hormone, and follicle-stimulating hormone in healthy older men. Metabolism. 1997;46:410–413. doi: 10.1016/S0026-0495(97)90057-3. [DOI] [PubMed] [Google Scholar]
- 692.Vaninetti S., Baccarelli A., Romoli R., Fanelli M., Faglia G., Spada A. Effect of aging on serum gonadotropin levels in healthy subjects and patients with nonfunctioning pituitary adenomas. Eur. J. Endocrinol. 2000;142:144–149. doi: 10.1530/eje.0.1420144. [DOI] [PubMed] [Google Scholar]
- 693.Archer D.F. Lower doses of oral estrogen and progestogens as treatment for postmenopausal women. Semin. Reprod. Med. 2005;23:188–195. doi: 10.1055/s-2005-869487. [DOI] [PubMed] [Google Scholar]
- 694.Irwig M.S. Testosterone therapy for transgender men. Lancet Diabetes Endocrinol. 2017;5:301–311. doi: 10.1016/S2213-8587(16)00036-X. [DOI] [PubMed] [Google Scholar]
- 695.Siqueira Cunha F., Domenice S., Palma Sircili M.H., Bilharinho de Mendonca B., Frade Costa E.M. Low estrogen doses normalize testosterone and estradiol levels to the female range in transgender women. Clinics. 2018;73:e86. doi: 10.6061/clinics/2018/e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 696.Tangpricha V., den Heijer M. Oestrogen and anti-androgen therapy for transgender women. Lancet Diabetes Endocrinol. 2017;5:291–300. doi: 10.1016/S2213-8587(16)30319-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 697.Pappas I.I., Craig W.Y., Spratt L.V., Spratt D.I. Efficacy of sex steroid therapy without progestin or GnRH agonist for gonadal suppression in adult transgender patients. J. Clin. Endocrinol. Metab. 2021;106:E1290–E1300. doi: 10.1210/clinem/dgaa884. [DOI] [PubMed] [Google Scholar]
- 698.Burke S.M., Manzouri A.H., Dhejne C., Bergstrom K., Arver S., Feusner J.D., Savic-Berglund I. Testosterone effects on the brain in transgender men. Cereb. Cortex. 2018;28:1582–1596. doi: 10.1093/cercor/bhx054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 699.Christensen L.L., Glintborg D., Tauberg Kristensen T., Diederichsen A., T’Sjoen G., Frystyk J., Skovsager Andersen M. Masculinising testosterone treatment and effects on preclinical cardiovascular disease, muscle strength and power, aggression, physical fitness and respiratory function in transgender men: Protocol for a 10-year, prospective, observational cohort study in Denmark at the Body Identity Clinic (BIC) BMJ Open. 2020;10:e045714. doi: 10.1136/bmjopen-2020-045714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 700.Hodges-Simeon C.R., Grail G.P.O., Albert G., Groll M.D., Stepp C.E., Carré J.M., Arnocky S.A. Testosterone therapy masculinizes speech and gender presentation in transgender men. Sci. Rep. 2021;11:3494. doi: 10.1038/s41598-021-82134-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 701.Irwig M.S., Childs K., Hancock A.B. Effects of testosterone on the transgender male voice. Andrology. 2017;5:107–112. doi: 10.1111/andr.12278. [DOI] [PubMed] [Google Scholar]
- 702.Chan K.J., Liang J.J., Jolly D., Weinand J.D., Safer J.D. Exogenous testosterone does not induce or exacerbate the metabolic features associated with PCOS among transgender men. Endocr. Pract. 2018;24:565–572. doi: 10.4158/EP-2017-0247. [DOI] [PubMed] [Google Scholar]
- 703.Iannantuoni F., Salazar J.D., de Marañón A., Martínez Bañuls C., López-Doménech S., Rocha M., Hurtado-Murillo F., Morillas C., Gómez-Balaguer M., Víctor V.M. Testosterone administration increases leukocyte-endothelium interactions and inflammation in transgender men. Fertil. Steril. 2021;115:483–489. doi: 10.1016/j.fertnstert.2020.08.002. [DOI] [PubMed] [Google Scholar]
- 704.Gulanski B.I., Flannery C.A., Peter P.R., Leone C.A., Stachenfeld N.S. Compromised endothelial function in transgender men taking testosterone. Clin. Endocrinol. 2020;92:138–144. doi: 10.1111/cen.14132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 705.Kirisawa T., Ichihara K., Sakai Y., Morooka D., Iyoki T., Masumori N. Physical and psychological effects of gender-affirming hormonal treatment using intramuscular testosterone enanthate in Japanese transgender men. Sex. Med. 2021;9:100306. doi: 10.1016/j.esxm.2020.100306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 706.Chan K.J., Jolly D., Liang J.J., Weinand J.D., Safer J.D. Estrogen levels do not rise with testosterone treatment for transgender men. Endocr. Pract. 2018;24:329–333. doi: 10.4158/EP-2017-0203. [DOI] [PubMed] [Google Scholar]
- 707.Nolan B.J., Zwickl S., Wong A.F.Q., Locke P., Simpson S., Li L., Zajac J.D., Cheung A.S. Testosterone concentrations and prescription patterns of 1% testosterone gel in transgender and gender diverse individuals. Ther. Adv. Endocrinol. Metab. 2022;13:20420188221083512. doi: 10.1177/20420188221083512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 708.Hevener A.L., Clegg D.J., Mauvais-Jarvis F. Impaired estrogen receptor action in the pathogenesis of the metabolic syndrome. Mol. Cell. Endocrinol. 2015;418:306–321. doi: 10.1016/j.mce.2015.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 709.Rubinow K.B. Estrogens and body weight regulation in men. Adv. Exp. Med. Biol. 2017;1043:285–313. doi: 10.1007/978-3-319-70178-3_14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 710.Ting W.J., Huang C.Y., Jiang C.H., Lin Y.M., Chung L.C., Shen C.Y., Pai P., Lin K.H., Viswanadha V.P., Liao S.C. Treatment with 17β-estradiol reduced body weight and the risk of cardiovascular disease in a high-fat diet-induced animal model of obesity. Int. J. Mol. Sci. 2017;18:629. doi: 10.3390/ijms18030629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 711.Bendale D.S., Karpe P.A., Chhabra R., Shete S.P., Shah H., Tikoo K. 17-β Oestradiol prevents cardiovascular dysfunction in post-menopausal metabolic syndrome by affecting SIRT1/AMPK/H3 acetylation. Br. J. Pharmacol. 2013;170:779–795. doi: 10.1111/bph.12290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 712.Mikkola T.S., Tuomikoski P., Lyytinen H., Korhonen P., Hoti F., Vattulainen P., Gissler M., Ylikorkala O. Estradiol-based postmenopausal hormone therapy and risk of cardiovascular and all-cause mortality. Menopause. 2015;22:976–983. doi: 10.1097/GME.0000000000000450. [DOI] [PubMed] [Google Scholar]
- 713.Maher A.C., Akhtar M., Tarnopolsky M.A. Men supplemented with 17β-estradiol have increased beta-oxidation capacity in skeletal muscle. Physiol. Genom. 2010;42:342–347. doi: 10.1152/physiolgenomics.00016.2010. [DOI] [PubMed] [Google Scholar]
- 714.Torres M.J., Kew K.A., Ryan T.E., Pennington E.R., Lin C.T., Buddo K.A., Fix A.M., Smith C.A., Gilliam L.A., Karvinen S., et al. 17β-Estradiol directly lowers mitochondrial membrane microviscosity and improves bioenergetic function in skeletal muscle. Cell Metab. 2018;27:167–179. doi: 10.1016/j.cmet.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 715.De Vanna M., Carlino D., Aguglia E. Neuroprotection by estradiol: Molecular mechanism of action and implications for neuropsychopharmacology. Int. J. Psychiatry Clin. Pract. 2003;7:81–92. doi: 10.1080/13651500310001905. [DOI] [Google Scholar]
- 716.Elzer J.G., Muhammad S., Wintermantel T.M., Regnier-Vigouroux A., Ludwig J., Schütz G., Schwaninger M. Neuronal estrogen receptor-α mediates neuroprotection by 17β-estradiol. J. Cereb. Blood Flow Metab. 2010;30:935–942. doi: 10.1038/jcbfm.2009.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 717.Groeger M., Plesnila N. The neuroprotective effect of 17β-estradiol is independent of its antioxidative properties. Brain Res. 2014;1589:61–67. doi: 10.1016/j.brainres.2014.08.029. [DOI] [PubMed] [Google Scholar]
- 718.Imtiaz B., Tolppanen A.M., Solomon A., Soininen H., Kivipelto M. Estradiol and cognition in the cardiovascular risk factors, Aging and Dementia (CAIDE) Cohort Study. J. Alzheimer’s Dis. 2017;56:453–458. doi: 10.3233/JAD-160643. [DOI] [PubMed] [Google Scholar]
- 719.Lebesgue D., Chevaleyre V., Zukin R.S., Etgen A.M. Estradiol rescues neurons from global ischemia-induced cell death: Multiple cellular pathways of neuroprotection. Steroids. 2009;74:555–561. doi: 10.1016/j.steroids.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 720.Galmés-Pascual B.M., Nadal-Casellas A., Bauzá-Thorbrugge M., Sbert-Roig M., García-Palmer F.J., Proenza A.M., Gianotti M., Lladó I. 17β-estradiol improves hepatic mitochondrial biogenesis and function through PGC1B. J. Endocrinol. 2017;232:297–308. doi: 10.1530/JOE-16-0350. [DOI] [PubMed] [Google Scholar]
- 721.Klinge C.M. Estrogenic control of mitochondrial function. Redox Biol. 2020;31:101435. doi: 10.1016/j.redox.2020.101435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 722.Lee M.Y., Jung S.C., Lee J.H., Han H.J. Estradiol-17β protects against hypoxia-induced hepatocyte injury through ER-mediated upregulation of Bcl-2 as well as ER-independent antioxidant effects. Cell Res. 2008;18:491–499. doi: 10.1038/cr.2008.42. [DOI] [PubMed] [Google Scholar]
- 723.Shwaery G.T., Vita J.A., Keaney J.F. Antioxidant protection of LDL by physiologic concentrations of estrogens is specific for 17-beta-estradiol. Atherosclerosis. 1998;138:255–262. doi: 10.1016/S0021-9150(98)00020-3. [DOI] [PubMed] [Google Scholar]
- 724.Kim K.G., Park Y.S. Oestradiol-17β is a local factor inducing the early stage of spermatogenesis in mouse testes. Andrologia. 2018;50:e12905. doi: 10.1111/and.12905. [DOI] [PubMed] [Google Scholar]
- 725.Tao K., Sun Y., Chao Y., Xing L., Leng L., Zhou D., Zhu W., Fan L. β-Estradiol promotes the growth of primary human fetal spermatogonial stem cells via the induction of stem cell factor in Sertoli cells. J. Assist. Reprod. Genet. 2021;38:2481–2490. doi: 10.1007/s10815-021-02240-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 726.Kumar R., Balhuizen A., Amisten S., Lundquist I., Salehi A. Insulinotropic and antidiabetic effects of 17β-estradiol and the GPR30 agonist G-1 on human pancreatic islets. Endocrinology. 2011;152:2568–2579. doi: 10.1210/en.2010-1361. [DOI] [PubMed] [Google Scholar]
- 727.Kapoor D., Goodwin E., Channer K.S., Jones T.H. Testosterone replacement therapy improves insulin resistance, glycaemic control, visceral adiposity and hypercholesterolaemia in hypogonadal men with type 2 diabetes. Eur. J. Endocrinol. 2006;154:899–906. doi: 10.1530/eje.1.02166. [DOI] [PubMed] [Google Scholar]
- 728.Yeap B.B., Chubb S.A.P., Hyde Z., Jamrozik K., Hankey G.J., Flicker L., Norman P.E. Lower serum testosterone is independently associated with insulin resistance in non-diabetic older men: The health in men study. Eur. J. Endocrinol. 2009;161:591–598. doi: 10.1530/EJE-09-0348. [DOI] [PubMed] [Google Scholar]
- 729.Rao P.M., Kelly D.M., Jones T.H. Testosterone and insulin resistance in the metabolic syndrome and T2DM in men. Nat. Rev. Endocrinol. 2013;9:479–493. doi: 10.1038/nrendo.2013.122. [DOI] [PubMed] [Google Scholar]
- 730.Cheung A.S., Hoermann R., Dupuis P., Joon D.L., Zajac J.D., Grossmann M. Relationships between insulin resistance and frailty with body composition and testosterone in men undergoing androgen deprivation therapy for prostate cancer. Eur. J. Endocrinol. 2016;175:229–237. doi: 10.1530/EJE-16-0200. [DOI] [PubMed] [Google Scholar]
- 731.Faiman C., Winter J.S.D. Diurnal cycles in plasma FSH, testosterone and cortisol in men. J. Clin. Endocrinol. Metab. 1971;33:186–192. doi: 10.1210/jcem-33-2-186. [DOI] [PubMed] [Google Scholar]
- 732.Bodenheemer S., Winter J.S.D., Faiman C. Diurnal rhythms of serum gonadotropins, testosterone, estradiol and cortisol in blind men. J. Clin. Endocrinol. Metab. 1973;37:472–475. doi: 10.1210/jcem-37-3-472. [DOI] [PubMed] [Google Scholar]
- 733.Barbería J.M., Giner J., Cortés-Gallegos V. Diurnal variations of plasma testosterone in men. Steroids. 1973;22:615–626. doi: 10.1016/0039-128X(73)90110-4. [DOI] [PubMed] [Google Scholar]
- 734.Kanabar R., Mazur A., Plum A., Schmied J. Correlates of testosterone change as men age. Aging Male. 2022;25:29–40. doi: 10.1080/13685538.2021.2023493. [DOI] [PubMed] [Google Scholar]
- 735.Smith R.P., Coward R.M., Kovac J.R., Lipshultz L.I. The evidence for seasonal variations of testosterone in men. Maturitas. 2013;74:208–212. doi: 10.1016/j.maturitas.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 736.Doering C.H., Kraemer H.C., Brodie H.K.H., Hamburg D.A. A cycle of plasma testosterone in the human male. J. Clin. Endocrinol. Metab. 1975;40:492–500. doi: 10.1210/jcem-40-3-492. [DOI] [PubMed] [Google Scholar]
- 737.Graupner H. Elixiere des Lebens-von Hormonen und Vitaminen. Wegweiser-Verlag; Berlin, Germany: 1939. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.