Abstract
Background
It is not clear whether pre-existing macrovascular complications (ischemic heart disease, stroke or peripheral artery disease) are associated with health outcomes in people with diabetes mellitus hospitalized for COVID-19.
Methods
We conducted cohort studies of adults with pre-existing diabetes hospitalized for COVID-19 infection in the UK, France, and Spain during the early phase of the pandemic (between March 2020—October 2020). Logistic regression models adjusted for demographic factors and other comorbidities were used to determine associations between previous macrovascular disease and relevant clinical outcomes: mortality, intensive care unit (ICU) admission and use of invasive mechanical ventilation (IMV) during the hospitalization. Output from individual logistic regression models for each cohort was combined in a meta-analysis.
Results
Complete data were available for 4,106 (60.4%) individuals. Of these, 1,652 (40.2%) had any prior macrovascular disease of whom 28.5% of patients died. Mortality was higher for people with compared to those without previous macrovascular disease (37.7% vs 22.4%). The combined crude odds ratio (OR) for previous macrovascular disease and mortality for all four cohorts was 2.12 (95% CI 1.83–2.45 with an I2 of 60%, reduced after adjustments for age, sex, type of diabetes, hypertension, microvascular disease, ethnicity, and BMI to adjusted OR 1.53 [95% CI 1.29–1.81]) for the three cohorts. Further analysis revealed that ischemic heart disease and cerebrovascular disease were the main contributors of adverse outcomes. However, proportions of people admitted to ICU (adjOR 0.48 [95% CI 0.31–0.75], I2 60%) and the use of IMV during hospitalization (adjOR 0.52 [95% CI 0.40–0.68], I2 37%) were significantly lower for people with previous macrovascular disease.
Conclusions
This large multinational study of people with diabetes mellitus hospitalized for COVID-19 demonstrates that previous macrovascular disease is associated with higher mortality and lower proportions admitted to ICU and treated with IMV during hospitalization suggesting selective admission criteria. Our findings highlight the importance correctly assess the prognosis and intensive monitoring in this high-risk group of patients and emphasize the need to design specific public health programs aimed to prevent SARS-CoV-2 infection in this subgroup.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12933-022-01657-8.
Keywords: Diabetes, Macrovascular disease, Mortality, COVID-19
Background
Coronavirus disease 2019 (COVID-19) is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and is characterized by a variable clinical presentation that ranges from asymptomatic infection to fatal multi-organ damage and mortality [1, 2]. Since the emergence of SARS-CoV-2 in December 2019, cases of COVID-19 have rapidly increased worldwide. The updated WHO estimates on August 19th, 2022, reported 590,659,276 confirmed cases, including 6,440,163 deaths worldwide (https://covid19.who.int). The case fatality for COVID-19 has been estimated to be 0.5–1.0% [3, 4]. Nevertheless, certain characteristics, including increasing age, male sex, ethnicity, socio-economic deprivation, and comorbidities, have been associated with a higher risk of severe COVID-19 or death [5–7].
COVID-19 pandemic has had a large negative impact on both diabetes management [8] and diabetes-related mortality [9]. As well, pre-existing diabetes mellitus has been considered a risk factor for increased COVID-19 severity and worse outcomes, including higher mortality, irrespective of age and comorbidity status [7]. The estimates of diabetes prevalence in those who have died of COVID-19 range from 20 to 30% [10, 11]. A recent meta-analysis showed that people with diabetes were at higher risk of COVID-19-related mortality in comparison to people without diabetes [11]. In addition, diabetes is associated with more than double the risk for ICU admission and more than triple the risk of death compared to people without diabetes [12]. Therefore, identifying which clinical factors are associated with greater morbidity and mortality would be useful for the prevention and management of high-risk groups during future waves of the pandemic. In that sense, few studies have examined the possibility that micro- and macrovascular complications contribute to susceptibility to acute organ injury [13, 14] but with contradictory results [15].
Our study aimed to assess whether the presence of macrovascular complications (ischemic heart disease, stroke, or peripheral artery disease) prior to hospital admission is associated with intensive care unit admission, mechanical ventilation, and mortality in people with diabetes mellitus hospitalized for COVID-19 in four European cohorts.
Methods
Study design and participants
Retrospective data from hospitalized adults with pre-existing diabetes and concomitant COVID-19 infection were collected in the UK, France, and Spain. Adults with hyperglycaemia at admission but not pre-existing or subsequent diagnosis of diabetes (based on WHO criteria) were excluded from the analysis [16]. COVID-19 was defined as a SARS-CoV-2 infection confirmed by quantitative PCR (qPCR) performed on nasopharyngeal samples obtained by trained personnel and/or by fulfilling clinical and radiological diagnostic criteria at hospital admission. Further descriptions of each dataset have been published previously [17].
United Kingdom: association of British clinical diabetologists (ABCD) COVID-19 audit
The NHS supports audits with clear guidance for the contributing centers on using routine clinical practice data submitted anonymously via the secure NHS network [18]. Clinicians participating in the ABCD COVID-19 audit submitted data for adults with pre-existing type 1 and type 2 diabetes admitted with COVID-19 from hospitals across the UK. The audit is registered with Oxford University Hospitals NHS Foundation Trust (OUH), a Data Protection Impact Assessment was carried out and the audit was approved by the OUH Caldicott Guardian and the Public Benefit and Privacy Panel in Scotland (reference 2021-0111).
France: CORONADO (CORONAvirus-SARS-CoV-2 and diabetes outcomes)
The CORONADO study described the phenotypic characteristics and prognosis of people with diabetes admitted with COVID-19 between March 10 and April 10, 2020 [13, 19]. CORONADO is a cohort study from French hospitals volunteering to share data on hospitalized COVID-19 patients with diabetes. The study was sponsored by the Nantes University Hospital and designed in accordance with the Declaration of Helsinki. It obtained all regulatory approvals.
Spain—HM Hospitales cohort
The six hospitals in the HM Hospitales group collected anonymized observational data for people infected with COVID-19 during the first wave of the pandemics. This dataset is made available to researchers via “Covid Data Save Lives” [20]. The electronic hospital health records were collected for admitted persons, including pre-existing disease status, medication use, demographic, and outcome. A subset of people with pre-existing diabetes from this cross-sectional database was used in this study. Before access was granted, a formal petition, specific study protocol, and ethics committee approval were obtained. The study was approved by the Ethics Committee of the Primary Health Care University Research Institute (IDIAP) Jordi Gol, Barcelona (approval number: 20/089-PCV).
Spain—Barcelona cohort
An observational cohort study was conducted at the Hospital del Mar and Hospital de la Santa Creu i Sant Pau, two tertiary hospitals in Barcelona providing healthcare to 800,000 people. The two hospitals from Barcelona (Catalonia) collected anonymized observational data for people infected with COVID-19 during the first wave. Demographic, clinical, epidemiological, and whole-episode (laboratory workup, vital signs, treatment) data were extracted from electronic medical records using a standardized data collection method. All patients with type 2 diabetes mellitus admitted for COVID-19 between March and April 2020 were included. The Hospital del Mar Institutional Ethics Committee (CEIm-2020/9352) and the Hospital de la Santa Creu I Sant Pau Ethics Committee (HSCSP-20/117) approved the study and waived the informed consent need due to the study’s nature.
Data collection: definitions and outcomes
Demographic data included: age, sex, and type of diabetes. UK and France collected ethnicity data (White/Europid, Black/African, Asian/Asian, Other/Middle East and North African (MENA)). Medication use at the point of admission was collected with particular focus on those medications associated with diabetes or diabetes-related comorbidities. Microvascular disease (including retinopathy, neuropathy, and nephropathy) was collected for the UK, French and Spanish (Barcelona cohort) cohorts. The Spanish cohort (HM Hospitales) collected data on the presence of chronic kidney disease (CKD) alone based on clinical coding records. CKD was defined by eGFR < 60 ml/min or the presence of macroalbuminuria (urinary albumin-to-creatinine ratio ≥ 300 mg/g) [21].
Definition of macrovascular complications
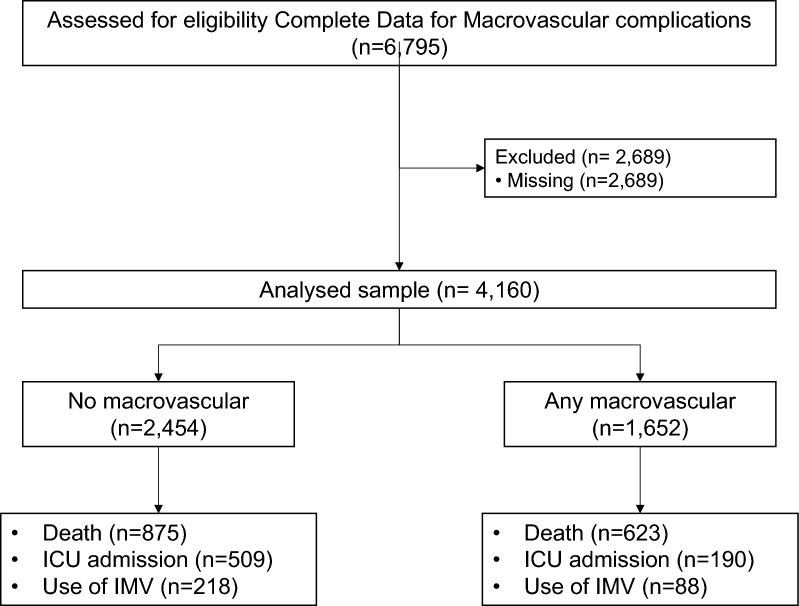
History of macrovascular disease was collected for all datasets. The presence of macrovascular complications was defined according to the presence of a previous history of ischemic heart disease (including a history of myocardial infarction and/or coronary artery revascularization or heart failure), cerebrovascular disease (including history of stroke or transient ischemic attack – TIA-) and/or peripheral artery disease (amputation owing to ischemic disease and/or lower limb artery revascularization). Data were obtained based on the information recorded in medical records or according international ICD10 classification. Of the 6,795 people included, 4,106 had complete data for macrovascular complications (all four cohorts) and/or the rest of the variables included (French, UK and Spanish HM Hospitales cohorts). The flowchart of the study is summarized in Fig. 1. The descriptive analysis compared the characteristics of people with and without complete data for macrovascular disease. The comparison of the clinical characteristics of people with complete data compared with those with missing data for macrovascular complications is shown in Table 1.
Fig. 1.
Inclusion and exclusion criteria
Table 1.
Comparison of the clinical characteristics of people with complete vs missing data for macrovascular complications
| UK | FRANCE | Spain—HM | Spain—Barcelona | |||||
|---|---|---|---|---|---|---|---|---|
| Complete data (n = 1846) | Missing data (n = 1333) | Complete data (n = 1510) | Missing data (n = 1333) | Complete data (n = 406) | Missing data (n = 0) | Complete data (n = 344) | Missing data (n = 23) | |
| Age (mean, SD) years | 72.5 (13.9) | 70.8 (14.4) | 70.1 (13.0) | 69.1 (13.3) | 74.7 (11.9) | – | 71.1 (13.9) | 74.0 (14.7) |
| Missing, n | 0 | 6 | 0 | 0 | 0 | – | 1 | 0 |
| Men, n (%) | 1140 (62) | 802 (60) | 933 (62) | 882 (66) | 250 (62) | – | 202 (59) | 11 (48) |
| Missing, n | 0 | 5 | 0 | 0 | 0 | – | 0 | 0 |
| BMI (mean, SD) kg/m2 | 29.3 (7.2) | 28.6 (6.9) | 29.9 (5.7) | 28.9 (6.1) | NA | – | 29.8 (6.6) | 33.2 (5.8) |
| Missing, n | 0 | 860 | 0 | 124 | NA | – | 295 | 21 |
| Ethnicity | – | |||||||
| White, n (%) | 1291 (70) | 624 (60) | 893 (59) | 517 (56) | NA | – | 77 (87) | 18 (86) |
| Asian, n (%) | 275 (15) | 167 (16) | 55 (4) | 33 (4) | NA | – | 1 (1) | 1 (5) |
| Black, n (%) | 116 (6) | 94 (9) | 242 (16.0) | 179 (20) | NA | – | 2 (2) | 0 (0) |
| Other, n (%) | 164 (9) | 157 (15) | 320 (21) | 187 (20) | NA | – | 9 (10) | 2 (10) |
| Missing, n | 0 | 291 | 0 | 417 | NA | – | 255 | 2 |
| Type of diabetes | ||||||||
| Type 1, n (%) | 93 (5) | 62 (5) | 48 (3) | 13 (1) | 4 (1) | – | 5 (5) | 0 (0.0) |
| Type 2, n (%) | 1753 (95) | 1163 (95) | 1462 (97) | 1079 (99) | 402 (99) | 88 (95) | 23 (100.0) | |
| Missing, n | 0 | 108 | 0 | 241 | 0 | – | 251 | 0 |
| Hypertension, n (%) | 1286 (70) | 774 (66) | 1204 (80) | 953 (73.0) | 286 (70) | – | 278 (81) | 18 (78) |
| Missing, n | 0 | 166 | 0 | 28 | 0 | – | 0 | 0 |
| Dyslipidaemia, n (%) | NA | NA | 767 (51) | 521 (42) | 198 (49) | – | NA | NA |
| Missing, n | - | - | 0 | 81 | 0 | – | – | – |
| Microvascular disease, n (%) | 807 (44) | 242 (39) | 701 (46) | 206 (42) | 38 (9) | – | 15 (17) | 0 |
| Missing, n | 0 | 710 | 0 | 848 | 0 | – | 257 | 23 |
| Macrovascular disease, n (%) | 804 (44) | 272 (40) | 640 (42) | 477 (39) | 98 (24) | – | 110 (32) | NA |
| Missing, n | 0 | 652 | 0 | 109 | 0 | – | 0 | 23 |
| Death (in-hospital mortality), n (%) | 715 (39) | 524 (39) | 290 (19) | 294 (22) | 79 (20) | – | 88 (28) | 8 (36) |
| Missing, n | 0 | 0 | 0 | 7 | 0 | – | 18 | 1 |
| ICU admission, n (%) | 193 (10) | 125 (13) | 412 (27) | 439 (33) | 35 (9) | – | 59 (17) | 1 (5) |
| Missing, n | 0 | 337 | 0 | 14 | 0 | – | 1 | 1 |
| Use of IMV, n (%) | NA | NA | 269 (18) | 297 (23) | 37 (9) | – | NA | NA |
| Missing, n | - | - | 0 | 14 | 0 | – | – | – |
BMI body mass index, ICU intensive care unit, IMV Mechanical ventilation, SD Standard deviation
Outcomes
The primary outcome was all-cause mortality (French data were collected to day 28 after admission, and Spanish and UK data included mortality during the whole hospital episode). The secondary outcomes were intensive care unit (ICU) admission for all four cohorts and use of invasive mechanical ventilation (IMV) during the hospitalization for the French and the Spanish HM Hospitales cohorts for which IMV data were available.
Statistical analysis
All quantitative data were tested for normality. Clinical characteristics were expressed as the number (percentage) of participants for categorical variables, mean ± standard deviation (SD) for normally distributed continuous variables, or median (25–75th percentile) for non-normally distributed continuous variables. Regulatory issues prevented us from sharing and combining individual level data from each contributing country, so, multivariable logistic regression models were used to analyse the association between the presence of macrovascular disease (main exposure) and primary (death) and secondary outcomes (ICU admission and IMV) in each country’s data separately. Logistic regression models were then used to adjust for potential confounders: age and sex (model 1), age, sex, type of diabetes, arterial hypertension, and the presence of microvascular disease (model 2) and age, sex, type of diabetes, arterial hypertension, microvascular disease, ethnicity, and BMI (model 3–data not available for HM cohort). Logistic regressions were performed using R in each contributing country; country-specific odds ratios were then pooled in both common effect and random effect meta-analysis (as needed according to I2 statistic) and using the inverse variance method. Heterogeneity across studies was evaluated using the I2 statistic. Results were expressed as odds ratio (OR) and 95% confidence interval (95% CI) and p-values < 0.05 were considered statistically significant. Statistical analyses were performed with R statistical software version 3.6.1 (https://www.r-project.org/).
Results
The UK ABCD COVID-19 audit collected data on 3,179 people with diabetes from over 40 hospitals between March and October 2020. Of these, 1,846 (58.1%) had complete data required for this study and were included in the analysis. CORONADO investigators collected data on 2,843 people with diabetes from 68 hospitals, with 1,510 (53.1%) having complete data. Spanish investigators from the HM Hospitales collected data on 2,310 individuals at six hospitals. There was complete data for 406 individuals (100.0%) with pre-existing diabetes. Finally, the Spanish investigators from Hospital del Mar and Hospital de la Santa Creu i Sant Pau collected data on 367 individuals, with 344 (93.7%) having complete data. A comparison of the complete dataset to that with missing data within all the countries (Table 1). Ethnicity data were not available for the Spain – HM Hospitales cohort.
The baseline characteristics of the cohort of patients in each country are summarized in Table 2. Data related to macrovascular disease status was available for 4,106 people. Of these, 1,652 (40.2%) had any prior macrovascular disease, 1,339 (32.6%) had a previous history of ischemic heart disease, 520 (12.7%) had previous cerebrovascular disease, and 457 (11.1%) had previous peripheral artery disease. In the four included cohorts, people with a history of macrovascular disease were older, had a higher percentage of men and had a higher prevalence of hypertension, dyslipidemia, and microvascular complications than the group with no history of macrovascular disease.
Table 2.
Clinical characteristics of subjects according to macrovascular status
| UK | FRANCE | Spain—HM | Spain—Barcelona | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All (n = 1846) | No MACRO (n = 1042) | Any MACRO (n = 804) | P | All (n = 1510) | No MACRO (n = 870) | Any MACRO (n = 640) | P | All (n = 406) | No MACRO (n = 308) | Any MACRO (n = 98) | P | All (n = 344) | No MACRO (n = 234) | Any MACRO (n = 110) | p | |
| Age (mean, SD) years | 72.5(13.9) | 69.1(14.8) | 76.8(11.2) | < 0.001 | 70.1(13.0) | 66.7(13.0) | 74.7(11.5) | < 0.001 | 74.7(11.9) | 72.8(11.9) | 80.6(9.7) | < 0.001 | 71.1(13.9) | 69.3(13.9) | 74.8(13.0) | < 0.001 |
| Men, n (%) | 1140(62) | 610 (59) | 530 (66) | 0.001 | 933 (62) | 495(57) | 438 (68.4) | < 0.001 | 250(62) | 185(60) | 65(66) | 0.322 | 202 (58.9) | 129 (55.1) | 73 (67.0) | 0.038 |
| Ethnicity, n (%) | < 0.001 | < 0.001 | NA | 0.688 | ||||||||||||
| White | 1291(70) | 655(63) | 626(78) | 893(59) | 467(54) | 426(66.6) | NA | NA | NA | 77(87) | 58(84) | 19(95) | ||||
| Asian | 275(15) | 200(19) | 75 (9) | 55(4) | 39(5) | 16(2.5) | NA | NA | NA | 1 (1) | 1 (2) | 0 (0) | ||||
| Black | 116(6) | 64(6) | 52 (6) | 242(16) | 173(20) | 69(10.8) | NA | NA | NA | 2 (2) | 2 (3) | 0 (0) | ||||
| Other | 164(9) | 123(12) | 41 (5) | 320(21) | 191(22) | 129(20.2) | NA | NA | NA | 9 (10) | 8 (12) | 1 (5) | ||||
| Type of diabetes | ||||||||||||||||
| Type 1, n (%) | 93(5) | 59(6) | 34(4) | 0.200 | 48(3) | 33(4) | 15(2.3) | 0.107 | 4 (1) | 3 (1) | 1 (1) | 1.000 | 5 (5) | 5 (7) | 0 (0.0) | 0.642 |
| Type 2, n (%) | 1753(95) | 983(94) | 770(96) | 1462(97) | 837(96) | 625(97.7) | 402(99) | 305(99) | 97(99) | 88 (95) | 68 (93) | 20(100.0) | ||||
| Oral agents, n (%) | 1123(61) | 673(65) | 450(56) | < 0.001 | 1092(72) | 684(79) | 408(64) | < 0.001 | 83 (20) | 68 (22) | 15(15) | 0.192 | 274 (80) | 189 (81) | 85 (78) | 0.452 |
| Insulin,n (%) | 696(38) | 402(39) | 294(37) | 0.40 | 678(44.9) | 320(36.8) | 358(56) | < 0.001 | 79 (20) | 61 (20) | 18 (18) | 0.868 | 97 (28) | 55 (24) | 42 (39) | 0.004 |
| Hypertension, n (%) | 1286(70) | 713(68) | 573(71) | 1204(80) | 635(73) | 569(88.9) | < 0.001 | 286(70) | 207(67) | 79(81) | 0.016 | 278(81) | 176(75) | 102(93) | < 0.001 | |
| RAASi, n (%) | 1319(71) | 715(69) | 604(75) | 0.003 | 858(56.9) | 446(51.3) | 412(64.5) | < 0.001 | 153 (38) | 115 (37) | 38 (39) | 0.892 | 199 (58) | 131 (56) | 68 (62) | 0.194 |
| Dyslipidaemia, n (%) | NA | NA | NA | NA | 767(51) | 363(42) | 404(63.1) | < 0.001 | 198(49) | 141(46) | 57(58) | 0.043 | NA | NA | NA | NA |
| Statins, n (%) | 1158(63) | 625(60) | 533(66) | 0.006 | 764(50.6) | 353(40.6) | 411(64.3) | < 0.001 | 107 (26) | 60 820) | 47 (48) | < 0.001 | 193 (56) | 112 (48) | 81 (74) | < 0.001 |
| BMI | 29.3 (7.2) | 29.9 (7.2) | 28.6 (7.1) | < 0.001 | 29.5 (5.9) | 29.9 (5.7) | 28.9 (6.1) | 0.02 | NA | NA | NA | NA | 29.8 (6.7) | 29.3 (6.4) | 33.3 (8.1) | 0.176 |
| Diabetes duration | NA | NA | NA | NA | 12 [6; 20] | 10 [5; 18] | 15 [10; 23] | < 0.001 | NA | NA | NA | NA | NA | NA | NA | NA |
| HbA1c (%), mean (SD) | 7.8 (4.2) | 7.9 (4.3) | 7.8 (4.1) | 0.270 | 8.1 (1.8) | 8.3 (2.0) | 7.9 (1.7) | < 0.001 | 8.1 (1.7) | 8.3 (1.8) | 7.7 (1.4) | 0.230 | 7.5 (1.5) | 7.3 (1.4) | 8.3 (1.8) | 0.022 |
| HbA1c mmol/mol, mean (SD) | 62 (22) | 63 (23) | 62 (21) | 0.270 | 65.2(20.2) | 67.1(21.5) | 62.7(18.2) | < 0.001 | 65.0(18.2) | 67.2(20.2) | 60.7(15.4) | 0.230 | 58.9(16.9) | 56.6(15.4) | 67.2(19.7) | 0.022 |
| Microvascular disease, n (%) | ||||||||||||||||
| Diabetic retinopathy, n (%) | 449(24) | 216(22) | 233(30) | < 0.001 | 252(17) | 104(12) | 148(23) | < 0.001 | 1(0.2) | 1(0.3) | 0(0.0) | 1.000 | 8/87 (9) | 7/71 (10) | 1/16 (6) | 0.652 |
| Diabetic kidney disease, n (%) | 420(23) | 156(15) | 264(33) | < 0.001 | 569 (38) | 220(25) | 349(54.5) | < 0.001 | 31(7.6) | 12(4) | 19(19) | < 0.001 | 6/87 (7) | 5/71 (7) | 1/16 (6) | 0.910 |
| Macrovascular disease, n (%) | ||||||||||||||||
| Ischemic heart disease/Heart failure, n (%) | 560(30) | 0 (0.0) | 560(70) | – | 410(27)/185(13) | 0(0) | 410(64)/185(39) | – | 54(13.3)/34(8.4) | 0 (0.0) | 54(55)/34(35) | – | 96 (28) | 0 (0.0) | 96 (88) | – |
| TIA/Stroke, n (%) | 295(16) | 0 (0.0) | 295(37) | – | 188(13) | 0(0) | 188(29.4) | – | 25 (6.2) | 0 (0.0) | 25(26) | – | 12 (3.5) | 0 (0.0) | 12 (11) | – |
| Peripheral artery disease, n (%) | 246(13) | 0 (0.0) | 246(31) | – | 198(13) | 0(0) | 198(31.0) | – | 10 (2.5) | 0 (0.0) | 10(10) | – | 3 (1) | 0 (0.0) | 3 (2.7) | – |
| CKD, n (%) | NA | NA | NA | NA | NA | NA | NA | NA | 51 (12.6) | 22(7) | 29(30) | < 0.001 | NA | NA | NA | NA |
| Death (in-hospital mortality), n (%) | 715(39) | 326(31) | 389(48) | < 0.001 | 290(19) | 118(14) | 172(26.9) | < 0.001 | 79(19.5) | 59(19) | 20(20) | 0.900 | 88(25.6) | 46(19.7) | 42(38.3) | < 0.001 |
| ICU admission, n (%) | 193(10) | 155(15) | 38(5) | < 0.001 | 412(27) | 282(32) | 130(20.3) | < 0.001 | 35(8.6) | 28(9) | 7 (7) | 0.695 | 59(17.2) | 44(18.8) | 15(13.6) | 0.249 |
| Use of IMV, n (%) | NA | NA | NA | NA | 269 (18) | 189(22) | 80 (12.5) | < 0.001 | 37 (9.1) | 29 (9) | 8 (8) | 0.862 | NA | NA | NA | NA |
BMI body mass index, CKD chronic kidney disease, ICU intensive care unit, IMV Mechanical ventilation, SD Standard deviation,
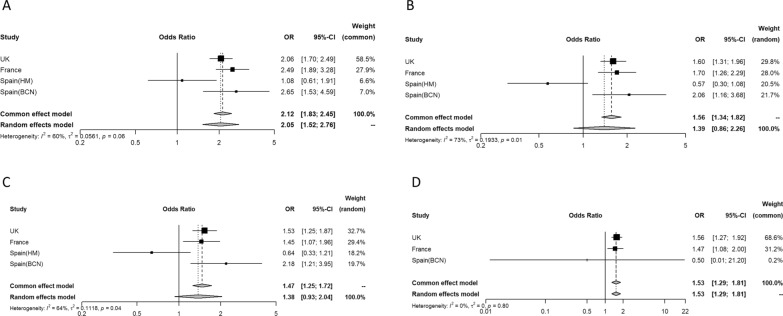
In total, 1,172 (28.5%, range 19.2–39.0%) people died. Mortality was higher for people with compared to without previous macrovascular disease (37.7% vs 22.4%). The combined crude odds ratio (OR) for previous macrovascular disease and mortality was 2.12 (95% CI 1.83–2.45) (Fig. 2A), with moderate heterogeneity (I2 60%). In the multivariable analyses, the results were attenuated after adjusting for age and sex (model 1: OR 1.39 [95% CI 0.86–2.26]) (Fig. 2B) and age, sex, type of diabetes, arterial hypertension, and the presence of microvascular disease (model 2: OR 1.38 [95% CI 0.93–2.04]) (Fig. 2C). The final model and additional adjustment for ethnicity and BMI (in a subset including 3 of the 4 cohorts) showed similar results (OR 1.53 [95% CI 1.29–1.81]) (Fig. 2D). Further, each component of macrovascular complications was analysed separately, to know which of the 3 diseases contributed the most. Both ischemic heart disease (unadjusted OR 1.78 [95% CI 1.20–2.63]), cerebrovascular disease (unadjusted OR 1.91 [95% CI 1.57–2.34]) and peripheral artery disease (unadjusted OR 1.70 [95% CI 2.38–2.10]) were associated with higher mortality (Additional file 1: Fig. S1, Additional file 2: Fig. S2, Additional file 3: Fig. S3). The results were maintained significant after further adjustments except for peripheral artery disease (Additional file 1: Fig. S1, Additional file 2: Fig. S2, Additional file 3: Fig. S3).
Fig. 2.
Odds ratio for the association between mortality and the presence of previous macrovascular disease in each of the four cohorts and overall (A). I2 indicates heterogeneity in the estimates. Odds ratio estimates adjusted for: model 1: age and sex (B); model 2: model 1 + type of diabetes, arterial hypertension, and the presence of microvascular disease (C); model 3: model 2 + ethnicity and BMI (D). HM cohort is excluded from model 3 due to lack of ethnicity data
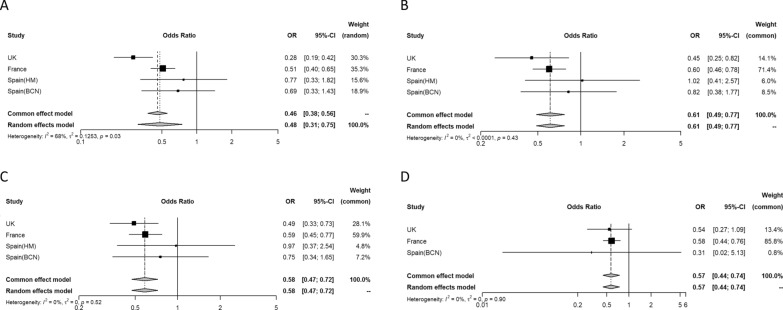
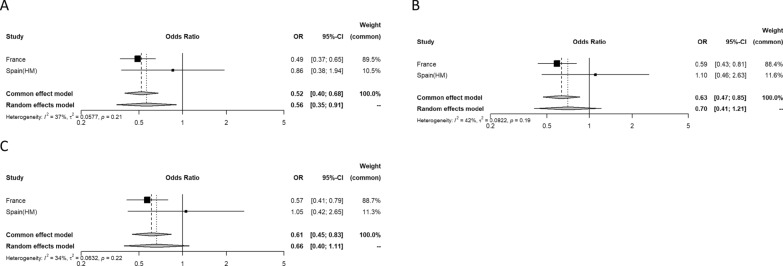
Regarding the secondary outcomes, 699 people (15.7%, range 8.6–22.3%) were admitted to ICU, and 306 (13.6%, range 9.1–17.8%) required IMV during hospitalization. The proportions admitted to ICU or treated with IMV during hospitalization were lower for those patients with previous macrovascular disease (11.5% vs 20.7% and 11.9% vs 18.5%, respectively). The overall odds ratio (OR) for previous macrovascular disease and ICU admission was 0.48 (95% CI 0.31–0.75) in the unadjusted analyses (Fig. 3A), with moderate heterogeneity (I2 68%). In the multivariable analyses, the estimates were similar after adjusting for age and sex (model 1: OR 0.61 [95% CI 0.49–0.77]) (Fig. 3B); age, sex, type of diabetes, arterial hypertension, and the presence of microvascular disease (model 2: OR 0.58 [95% CI 0.47–0.72]) (Fig. 3C); and age, sex, type of diabetes, arterial hypertension, microvascular disease, ethnicity, and BMI (model 3: OR 0.57 [95% CI 0.44–0.74]) (Fig. 3D). Both ischemic heart disease (unadjusted OR 0.53 [95% CI 0.44–0.64]), cerebrovascular disease (unadjusted OR 0.32 [95% CI 0.12–0.84]) and peripheral artery disease (unadjusted OR 0.48 [95% CI 0.34—0.66]) were associated with lower mortality (Additional file 1: Fig. S1, Additional file 2: Fig. S2, Additional file 3: Fig. S3). The results were maintained significant after further adjustments in all cases (Additional file 1: Fig. S1, Additional file 2: Fig. S2, Additional file 3: Fig. S3). Finally, the overall odds ratio (OR) for previous macrovascular disease and use of IMV during hospitalization was 0.52 (95% CI 0.40–0.68) in the unadjusted analyses (Fig. 4A), with little evidence of heterogeneity (I2 37%). In the multivariable analyses, the results were similar after adjusting for age and sex (model 1: OR 0.63 [95% CI 0.47–0.85]) (Fig. 4B) and age, sex, type of diabetes, arterial hypertension, and the presence of microvascular disease (model 2: OR 0.61 [95% CI 0.45–0.83]) (Fig. 4C). Ischemic heart disease (unadjusted OR 0.55 [95% CI 0.43–0.71]) was associated with lower mortality (Additional file 1: Fig. S1, Additional file 2: Fig. S2, Additional file 3: Fig. S3). The results were maintained significant after further adjustments in all cases (Additional file 1: Fig. S1, Additional file 2: Fig. S2, Additional file 3: Fig. S3). The association between cerebrovascular disease and peripheral artery disease and use of IMV during hospitalization was not tested for insufficient number of events.
Fig. 3.
Odds ratio for the association between intensive care unit admission and the presence of previous macrovascular disease in each of the four cohorts and overall (A). I2 indicates heterogeneity in the estimates. Odds ratio estimates adjusted for: model 1: age and sex (B); model 2: model 1 + type of diabetes, arterial hypertension, and the presence of microvascular disease (C); model 3: model 2 + ethnicity and BMI (D). HM cohort is excluded from model 3 due to lack of ethnicity data
Fig. 4.
Odds ratio for the association between use of invasive mechanical ventilation during the hospitalization and the presence previous of macrovascular disease in each of the two cohorts and overall (A). I2 indicates heterogeneity in the estimates. Odds ratio estimates adjusted for: model 1: age and sex (B); model 2: model 1 + type of diabetes, arterial hypertension, and the presence of microvascular disease (C)
Discussion
This is the first European retrospective study to specifically investigate the association between previous macrovascular disease and severe outcomes of people with diabetes mellitus hospitalized for COVID-19. The present study demonstrates that the presence of macrovascular complications (ischemic heart disease, stroke, peripheral artery disease) was associated with higher mortality. These findings remain significant after further adjustments for age, sex, type of diabetes, arterial hypertension, microvascular disease, ethnicity, and BMI. However, the proportions admitted to ICU and treated with IMV during hospitalization were lower for patients with previous macrovascular disease, reflecting clinical decisions around ICU admission.
COVID-19 is known to be associated with poorer outcomes for those with long-term conditions such as diabetes, and several potential mechanisms have been proposed [22]. Moreover, age, sex, ethnicity, deprivation, and other comorbidities such as obesity, hypertension and cardiovascular disease contribute to the increased risk [23]. The underlying mechanisms resulting in adverse outcomes in subjects with diabetes hospitalized for COVID-19 are therefore complex and unknown. In that sense, it has been suggested that both impaired glucose regulation and hyperglycemia [24] and the visceral adipose tissue expansion (and its associated ectopic fat depots) that characterize patients with diabetes and/or obesity activate the inflammatory cascade, increasing the production of interleukin-6, which has been proposed as a determinant factor of the “cytokine storm” associated with severe forms of COVID-19 [25].
A recent meta-analysis, including 158 observational studies with a total of 270,212 participants, of whom 57,801 had diabetes, reported that people with diabetes were at higher risk of COVID-19-related mortality with an OR 1.87 (95% CI 1.61–2.17) and higher risk of ICU admission (1.59 [95% CI 1.15–2.18]) and ventilation requirements (1.44 [95% CI 1.20–1.73]) in comparison to subjects without diabetes [11]. In addition, cardiovascular disease is common comorbidity observed in patients with COVID-19, associated with increased severity and mortality [22]. In that sense, it has been reported that patients with COVID-19 who have either hypertension or cardiovascular disease have an approximately 3–fourfold higher risk of developing severe disease [26]. By contrast, recent observational studies have demonstrated a significant association between statins (with anti-inflammatory and vasculo-protective effects) and reduced mortality in patients hospitalized with COVID-19, especially those with diabetes [27].
Moreover, an adverse effect on outcomes of diabetic complications in patients with diabetes during the COVID-19 pandemic has been recently identified. In a national population-based study in Scotland, associations with fatal or critical care unit treated COVID-19 among people with diabetes adjusted for age, sex, diabetes duration, and type of diabetes were reported for 35 factors, including heart disease (OR 2.43 [95% CI 2.14–2.75]), history of hospital admission with diabetic ketoacidosis (OR 2.87 [95% CI 1.85–4.46]), microalbuminuria (OR 1.35 [95% CI 1.16–1.58]), macroalbuminuria 1.92 [95% CI 1.52–2.43]) and severe retinopathy (OR 1.92 [95% CI 1.52–2.43]) [28]. The CORONADO study found that both microvascular (OR 2.14 [95% CI:1.16–3.94]) and macrovascular (OR 2.54 [95% CI: 1.44–4.50]) complications were independently associated with the risk of death on day seven of admission after adjusting for age, sex, comorbidities/complications, and glucose-lowering and anti-hypertensive treatment [13, 14, 19]. By contrast, no association was found between mortality (death by day seven of admission) and micro- or macrovascular complications in the ACCREDIT Study [15]. Nevertheless, both cohorts differ in several aspects such as mean age (69.8 in the CORONADO study vs. 74.1 for the ACCREDIT study cohort), median BMI (28.4 kg/m2 vs. 27.6 kg/m2), the mean HbA1c (8.1% vs. 7.7%), which may partially explain the different results regarding the outcomes [13–15, 19]. Our analysis suggests that participants living with diabetes hospitalized for COVID-19 with previous macrovascular complications (ischemic heart disease, stroke, peripheral artery disease) have an approximately 50% higher risk of mortality compared to people with no history of macrovascular disease after adjusting for all available confounding factors and that ischemic heart disease and stroke are the main contributors to this higher risk. However, proportions admitted to ICU or treated with IMV during hospitalization were lower for people with previous macrovascular disease. These results suggest unmeasured differences that may explain these opposing relationships, such as (1) the severity of the disease, (2) early mortality leading to potentially fewer patients admitted to ICU or meeting intubation criteria in the group of people with macrovascular disease or (3) the criteria used for ICU admission or IMV. In addition, it should be emphasized that our analysis revealed moderate heterogeneity in mortality and ICU admission for people with diabetes and previous cardiovascular disease with differences in the strength of the relationship between cohorts. While the higher mortality among people with history of macrovascular disease was consistently higher across the four cohorts, there were more marked differences regarding ICU admission and the use of IMV, being lower compared to the Spanish cohorts in the UK (ICU admission) and French cohorts (both ICU admission and use of IMV).
Our study is limited by the heterogeneity of data collection methods across the nations due to the use of databases that were designed separately and not specifically to answer the study question and, also by missing data. The meta-analysis combines the individual datasets to increase power but masks heterogeneity across nations. The relatively large proportion of people with missing data on one or more variables in the UK and French cohorts has occurred as a consequence of using routinely collected data from clinical practice and could introduce bias if data are not missing at random. As shown in Table 1, summary measures of the distribution of most variables used in model 3 (age, sex, type of diabetes, arterial hypertension, BMI, microvascular disease, macrovascular disease, death and ICU admission) were similar or had only modest differences between people with and without missing data in both UK and French cohorts. People of non-white ethnicity were over-represented in the missing data group in the UK cohort but not in the French cohort. Clinical data of the whole-episode, such as vital signs or arterial gasometry parameters, clinical severity scores (i.e. MEWS or CURB-65 score) or markers of inflammation (PCR, IL-6, serum ferritin) were not collected, as well as other potential confounding factors. In addition, the small sample size of patients with type 1 diabetes included made it impossible to analyze both groups separately to evaluate the potential differences between both. Lastly, we focused on people hospitalized for COVID-19; thus, our results cannot be generalized to all people with diabetes and COVID-19, especially those with less severe forms of the disease.
Conclusions
In conclusion, this large multinational study of people with diabetes mellitus hospitalized for COVID-19 demonstrates significant associations between previous macrovascular disease and higher mortality and with lower ICU admission and the use of IMV during hospitalization. This study is the first specifically designed to evaluate the association of macrovascular complications (ischemic heart disease, stroke, or peripheral artery disease) as main exposure with mortality, intensive care unit admission and mechanical ventilation in people with diabetes mellitus hospitalized for COVID-19 in Europe. Our findings highlight the importance correctly assess the prognosis and intensive monitoring in this high-risk group of patients and emphasize the need to design specific public health programs aimed to prevent SARS-CoV-2 infection in this subgroup (i.e. reinforcing vaccination campaigns). Nevertheless, further studies are required to confirm and extend these findings in these and other populations.
Supplementary Information
Additional file 1: Figure S1. Odds ratio for the association between mortality (1A–C), intensive care unit admission (2A–C) and use of invasive mechanical ventilation during the hospitalization (3A–C) and ischemic heart disease in each of the four cohorts and overall. I2 indicates heterogeneity in the estimates. Odds ratio estimates adjusted for: model 1: age and sex (B); model 2: model 1 + type of diabetes, arterial hypertension, and the presence of microvascular disease (C).
Additional file 2: Figure S2. Odds ratio for the association between mortality (1A–C), intensive care unit admission (2A–C) and and stroke in each of the four cohorts and overall. I2 indicates heterogeneity in the estimates. Odds ratio estimates adjusted for: model 1: age and sex (B); model 2: model 1 + type of diabetes, arterial hypertension, and the presence of microvascular disease (C).
Additional file 3: Figure S3. Odds ratio for the association between mortality (1A–C), intensive care unit admission (2A–C) and peripheral artery disease in each of the four cohorts and overall. I2 indicates heterogeneity in the estimates. Odds ratio estimates adjusted for: model 1: age and sex (B); model 2: model 1 + type of diabetes, arterial hypertension, and the presence of microvascular disease (C).
Acknowledgements
The contributors to national studies are listed below.
List of Contributors of the Spanish research group:
Juan Antonio Arroyo: Department of Internal Medicine, Hospital de la Santa Creu i Sant Pau, Barcelona, Spain; Juan-José Chillarón: Department of Endocrinology and Nutrition, Hospital del Mar; Institut Hospital del Mar d’Investigacions Mèdiques (IMIM), Barcelona, Spain; Rosa Corcoy: Department of Endocrinology and Nutrition, Hospital de la Santa Creu i Sant Pau; Department of Medicine, Universitat Autònoma de Barcelona, Barcelona, Spain; CIBER of Bioengineering, Biomaterials and Nanomedicine (CIBER-BBN), Instituto de Salud Carlos III (ISCIII), Spain; Roberto Güerri: Department of Infectious Diseases, Hospital del Mar; Institut Hospital del Mar d’Investigacions Mèdiques (IMIM), Barcelona, Spain; Manel Mata-Cases: Primary Health Care Center La Mina, Gerència d’Àmbit d’Atenció Primària Barcelona Ciutat, Institut Català de la Salut, Sant Adrià de Besòs, Spain. Emilio Ortega: CIBER of physiopathology of Obesity and Nutrition (CIBEROBN), Instituto de Salud Carlos III (ISCIII), Spain; Department of Endocrinology and Nutrition, Institut d’Investigacions Biomèdiques August Pi i Suñer, Hospital Clinic, Barcelona, Spain.
List of Contributors for the CORONADO study:
For CORONADO study, we thank the sponsor (DRCI, Nantes University Hospital), translational project manager (Matthieu Pichelin), Clinical Project Manager (Maëva Saignes) and assistant (Jeanne Saunier), Clinical Research Associates (Selma El Andaloussi, Joëlle Martin-Gauthier, Emily Rebouilleau) and data manager (Tanguy Roman). We also thank the Société Francophone du Diabète (SFD) and Société Française d’Endocrinologie (SFE) for disseminating CORONADO study design and organization, the Fédération Française des Diabétiques (FFD) for participating in the organization of the study. We are grateful to all the people who collected the data for this study.
List of Contributors for CORONADO study:
Bertrand CARIOU, CHU de Nantes, Nantes, bertrand.cariou@univ-nantes.fr.
Samy HADJADJ, CHU de Nantes, Nantes, samy.hadjadj@univ-nantes.fr.
Matthieu WARGNY, CHU de Nantes, Nantes, matthieu.wargny@chu-nantes.fr.
Pascale MAHOT, CHU de Nantes, Nantes, pascale.moreau@chu-nantes.fr.
Matthieu PICHELIN, CHU de Nantes, Nantes, matthieu.pichelin@univ-nantes.fr.
Anne-Laure FOURNIER-GUILLOUX, CHU de Nantes, Nantes, annelaure.fournierguilloux@chu-nantes.fr.
Nicolas MAUDUIT, CHU de Nantes, Nantes, nicolas.mauduit@chu-nantes.fr.
Edith BIGOT- CORBEL, CHU de Nantes, Nantes, edith.bigot@chu-nantes.fr.
Anne-Sophie BOUREAU, CHU de Nantes, Nantes, annesophie.boureau@chu-nantes.fr.
Laure DE DEKCER, CHU de Nantes, Nantes, laure.dedecker@chu-nantes.fr.
Audrey ERNOULD, CHU de Nantes, Nantes, audrey.ernould@chu-nantes.fr.
Claire PRIMOT, CHU de Nantes, Nantes, claire.primot@chu-nantes.fr.
Anne SEGUIN, CHU de Nantes, Nantes, anne.seguin@chu-nantes.fr.
Marielle JOLIVEAU, CHU de Nantes, Nantes, marielle.joliveau@chu-nantes.fr.
Sonia POUVREAU, CHU de Nantes, Nantes, sonia.pouvreau@chu-nantes.fr.
Chloé FOURNIER, CHU de Nantes, Nantes, chloe.fournier@chu-nantes.fr.
Jeremy THUREAU, CHU de Nantes, Nantes, jeremy.thureau@chu-nantes.fr.
Edith FONTENEAU, CHU de Nantes, Nantes, edith.fonteneau@chu-nantes.fr.
Pamela HUBLAIN, CHU de Nantes, Nantes, Pamela.HUBLAIN@chu-nantes.fr.
Carole AGASSE, CHU de Nantes, Nantes, Carole.AGASSE@chu-nantes.fr.
Mathilde DE KERGARADEC, CHU de Nantes, Nantes, laurence.dekergaradec@chu-nantes.fr.
Vincent MINVILLE, CHU Toulouse, Toulouse, minville.v@chu-toulouse.fr.
Fanny VARDON-BOUNES, CHU Toulouse, Toulouse, bounes.f@chu-toulouse.fr.
Guillaume MARTIN-BLONDEL, CHU Toulouse, Toulouse, martin-blondel.g@chu-toulouse.fr.
Pierre GOURDY, CHU Toulouse, Toulouse, pierre.gourdy@inserm.fr.
Blandine TRAMUNT, CHU Toulouse, Toulouse, blandine.tramunt@orange.fr.
Marie-Christine TURNIN, CHU Toulouse, Toulouse, turnin.mc@chu-toulouse.fr.
Hélène HANAIRE, CHU Toulouse, Toulouse, hanaire.h@chu-toulouse.fr.
Jean-Michel MANSUY, CHU Toulouse, Toulouse, mansuy.jm@chu-toulouse.fr.
Didier FABRE, CHU Toulouse, Toulouse, fabre.d@chu-toulouse.fr.
Marie-Blanche ARHAINX, CHU Toulouse, Toulouse, arhainx.mb@chu-toulouse.fr.
Laurent CAZALS, CHU Toulouse, Toulouse, cazals.l@chu-toulouse.fr.
Laure COMBES, CHU Toulouse, Toulouse, combes.l@chu-toulouse.fr.
Emmanuelle LAMI, CHU Toulouse, Toulouse, lami.e@chu-toulouse.fr.
Mallory CIANFERANI, CHU Toulouse, Toulouse, cianferani.m@chu-toulouse.fr.
Bruno MEGARBANE, Hôpital LARIBOISIERE, Paris, bruno.megarbane@aphp.fr.
Pierre LEROY, Hôpital LARIBOISIERE, Paris, pierre.leroy@aphp.fr.
Jean-François GAUTIER, Hôpital LARIBOISIERE, Paris, jean-francois.gautier@aphp.fr.
Tiphaine VIDAL-TRECAN, Hôpital LARIBOISIERE, Paris, tiphaine.vidal-trecan@aphp.fr.
Jean-Pierre RIVELINE, Hôpital LARIBOISIERE, Paris, jeanpierre.riveline@aphp.fr.
Jean-Louis LAPLANCHE, Hôpital LARIBOISIERE, Paris, jean-louis.laplanche@aphp.fr.
Stéphane MOULY, Hôpital LARIBOISIERE, Paris, stephane.mouly@aphp.fr.
Louis POTIER, Hôpital BICHAT, Paris, louis.potier@gmail.com.
Ronan ROUSSEL, Hôpital BICHAT, Paris, ronan.roussel@aphp.fr.
Malak TAHER, Hôpital BICHAT, Paris, malak.taher@aphp.fr.
Yawa ABOULEKA, Hôpital BICHAT, Paris, yawa.abouleka@aphp.fr.
Fetta YAKER, Hôpital BICHAT, Paris, fettaamel.yaker@aphp.fr.
Aurelie CARLIER, Hôpital BICHAT, Paris, aurelie.carlier@aphp.fr.
Anne BOUTTEN, Hôpital BICHAT, Paris, anne.boutten@aphp.fr.
Marilyne HALLOT-FERON, Hôpital BICHAT, Paris, marilyne.feron@aphp.fr.
Fadila MOURAH, Hôpital BICHAT, Paris, fadila.mourah@gmail.com.
Charles THIVOLET, Hôpital Lyon Sud, Pierre Bénite, charles.thivolet@chu-lyon.fr.
Emilie BLOND, Hôpital Lyon Sud, Pierre Bénite, emilie.blond@chu-lyon.fr.
Muriel ROLLAND, Hôpital Lyon Sud, Pierre Bénite, muriel.rolland@chu-lyon.fr.
Josep VERDECHO MENDEZ, Hôpital Lyon Sud, Pierre Bénite, josep.verdecho-mendez@chu-lyon.fr.
Marine ALEXANDRE, Hôpital Lyon Sud, Pierre Bénite, marine.alexandre@chu-lyon.fr.
Julien POTTECHER, Nouvel hôpital civil, Strasbourg, julien.pottecher@chru-strasbourg,fr.
Emilie RICHER, Nouvel hôpital civil, Strasbourg, emilie.richerdupont@chru-strasbourg.fr.
Laurent MEYER, Nouvel hôpital civil, Strasbourg, laurent.meyer@chru-strasbourg.fr.
Florina LUCA, Hôpital Hautepierre, Strasbourg, florina.luca@chru-strasbourg,fr.
Jean-Marc LESSINGER, Nouvel hôpital civil, Strasbourg, Jean-Marc.LESSINGER@chru-strasbourg.fr.
Thibault BAHOUGNE, Hospices civils, Strasbourg, thibault.bahougne@chru-strasbourg,fr.
Bruno GUERCI, CHU Brabois Université de Lorraine, Nancy, b.guerci@chru-nancy.fr.
Lisa LUDWIG, CHU Brabois Université de Lorraine, Nancy, L.LUDWIG@chru-nancy.fr.
Siham BENZIRAR, CHU Brabois Université de Lorraine, Nancy, s.benzirar@chru-nancy.fr.
Catherine MALAPLATE, CHU Brabois Université de Lorraine, Nancy, c.malaplate@chu-nancy.fr.
Thierry MATTON, CHU Brabois Université de Lorraine, Nancy, t.matton@chru-nancy.fr.
Julien POISSY, Hôpital salengro CHU, Lille, julien.poissy@chru-lille.fr.
Karine FAURE, Hôpital Huriez CHRU, Lille, karine.faure@chru-lille.fr.
Pierre FONTAINE, Hôpital Huriez CHRU, Lille, pierre.fontaine@chru-lille.fr.
Florence BAUDOUX, Hôpital Huriez CHRU, Lille, florence.baudoux@chru-lille.fr.
Anne VAMBERGUE, Hôpital Huriez CHRU, Lille, anne.vambergue@chru-lille.fr.
Jean David PEKAR, Hôpital Huriez CHRU, Lille, jeandavid.PEKAR@chru-lille.fr.
Marc LAMBERT, Hôpital Calmette CHU, Lille, marc.lambert@chru-lille.fr.
Cécile YELNIK, Hôpital Calmette CHU, Lille, cecile.yelnik@chru-lille.fr.
Amélie BRUANDET, Hôpital Huriez CHRU, Lille, amelie.bruandet@chru-lille.fr.
Laurent PETIT, CHU de Bordeaux, Bordeaux, laurent.petit@chu-bordeaux.fr.
Didier NEAU, CHU de Bordeaux, Bordeaux, didier.neau@chu-bordeaux.fr.
Vincent RIGALLEAU, CHU de Bordeaux, Pessac, vincent.rigalleau@chu-bordeaux.fr.
Annie BERARD, CHU de Bordeaux, Bordeaux, annie.berard@chu-Bordeaux.fr.
Amandine GALIOOT, CHU de Bordeaux, Pessac, amandine.galioot@chu-bordeaux.fr.
Remy COUDROY, CHU Poitiers, Poitiers, Remi.COUDROY@chu-poitiers.fr.
Arnaud THILLE, CHU Poitiers, Poitiers, arnaud.thille@chu-poitiers.fr.
René ROBERT, CHU Poitiers, Poitiers, rene.robert@chu-poitiers.fr.
France ROBLOT-CAZENAVE, CHU Poitiers, Poitiers, France.CAZENAVE-ROBLOT@chu-poitiers.fr.
Blandine RAMMAERT, CHU Poitiers, Poitiers, blandine.rammaert@chu-poitiers.fr.
Pierre Jean SAULNIER, CHU Poitiers, Poitiers, pierrejean.saulnier@gmail.com.
Xavier PIGUEL, CHU Poitiers, Poitiers, xavier.piguel@chu-poitiers.fr.
Nesrine BENHENDA, CHU Poitiers, Poitiers, Nesrine.BENHENDA@chu-poitiers.fr.
Camille HUSSON, CHU Poitiers, Poitiers, Camille.HUSSON@chu-poitiers.fr.
Celine OLIVIER, CHU Poitiers, Poitiers, celine.olivier@chu-poitiers.fr.
Florence TORREMOCHA, CHU Poitiers, Poitiers, florence.torremocha@chu-poitiers.fr.
Mathilde FRATY, CHU Poitiers, Poitiers, mathilde.fraty@chu-poitiers.fr.
Marie FLAMEN D'ASSIGNY, CHU Poitiers, Poitiers, marie.flamen-dassigny@chu-poitiers.fr.
Aurelie MIOT, CHU Poitiers, Poitiers, aurelie.miot@chu-poitiers.fr.
Valentin BOSSARD, CHU Poitiers, Poitiers, valentin.bossard988@gmail.com.
Kada KLOUCHE, Hôpital Lapeyronie, Chu Montpellier, k-klouche@chu-montpellier.fr.
Alain MAKINSON, Hôpital Lapeyronie, Chu Montpellier, a-makinson@chu-montpellier.fr.
Ariane SULTAN, Hôpital Lapeyronie, Chu Montpellier, a-sultan@chu-montpellier.fr.
Jean-Baptiste BONNET, Hôpital Lapeyronie, Chu Montpellier, jean-baptiste-bonnet@chu-montpellier.fr.
Vincent FOULONGNE, Hôpital St Eloi, Chu Montpellier, v-foulongne@chu-montpellier.fr.
Florence GALTIER, Hôpital St Eloi, Chu Montpellier, f-galtier@chu-montpellier.fr.
Cécile AUBRON, CHU de Brest, Brest, cecile.aubron@ch-brest.fr.
Séverine ANSART, CHU de Brest, Brest, severine.ansart@chu-brest.fr.
Véronique KERLAN, CHU de Brest, Brest, veronique.kerlan@chu-brest.fr.
Pascale QUINIOU, CHU de Brest, Brest, pascale.quiniou@chu-brest;fr.
Jean- Luc CARRE, CHU de Brest, Brest, jean-luc.carre@chu-brest.fr.
Stéphane QUESNOT, CHU de Brest, Brest, stephane.quesnot@chu-brest.fr.
Bruno LAVIOLLE, CHU de Rennes, Rennes, bruno.laviolle@chu-rennes.fr.
Carole SCHWEBEL, CHU Grenoble Alpes, Grenoble, Cschwebel@chu-grenoble.fr.
Olivier EPAULARD, CHU Grenoble Alpes, Grenoble, OEpaulard@chu-grenoble.fr.
Pierre-Yves BENHAMOU, CHU Grenoble Alpes, Grenoble, PYBenhamou@chu-grenoble.fr.
Cécile BETRY, CHU Grenoble Alpes, Grenoble, Cbetry@chu-grenoble.fr.
Anne-Laure BOREL, CHU Grenoble Alpes, Grenoble, ALBorel@chu-grenoble.fr.
Sandrine LABLANCHE, CHU Grenoble Alpes, Grenoble, Slablanche@chu-grenoble.fr.
Dorra GUERGOUR, CHU Grenoble Alpes, Grenoble, Dguergour@chu-grenoble.fr.
Catherine DUCLOS, Hôpital AVICENNE, Bobigny, catherine.duclos@aphp.fr.
Emmanuel COSSON, Hôpital AVICENNE, Bobigny, emmanuel.cosson@aphp.fr.
Erwan GUYOT, Hôpital AVICENNE, Bobigny, erwan.guyot@aphp.fr.
Aurore DENIAU, Hôpital AVICENNE, Bobigny, aurore.deniau@aphp.fr.
Phucthutrang NGUYEN, Hôpital AVICENNE, Bobigny, phucthutrang.nguyen@aphp.fr.
Yves REZNIK, CHU Caen Normandie, Caen, reznik-y@chu-caen.fr.
Michael JOUBERT, CHU Caen Normandie, Caen, joubert-m@chu-caen.fr.
Stéphane ALLOUCHE, CHU Caen Normandie, Caen, allouche-s@chu-caen.fr.
Lydia GUITTET, CHU Caen Normandie, Caen, guittet-l@chu-caen.fr.
Steven GRANGE, CHU Rouen, Rouen, steven.grange@chu-rouen.fr.
Manuel ETIENNE, CHU Rouen, Rouen, manuel.etienne@chu-rouen.fr.
Gaëtan PRÉVOST, CHU Rouen, Rouen, gaetan.prevost@chu-rouen.fr.
Valéry BRUNEL, CHU Rouen, Rouen, valery.brunel@chu-rouen.fr.
Jean-Christophe LAGIER, IHU Marseille, Marseille, JeanChristophe.LAGIER@ap-hm.fr.
Didier RAOULT, IHU Marseille, Marseille, didier.raoult@ap-hm.fr.
Anne DUTOUR, CHU Nord et Conception, Marseille, anne.dutour@ap-hm.fr.
Bénédicte GABORIT, CHU Nord et Conception, Marseille, benedicte.gaborit@ap-hm.fr.
Sandrine BOULLLU, CHU Nord, Marseille, sandrine.boullu@ap-hm.fr.
Patrice DARMON, CHU Nord et Conception, Marseille, patrice.darmon@ap-hm.fr.
Adèle LASBLEIZ, CHU Nord et Conception, Marseille, adele.lasbleiz@ap-hm.fr.
Mathieu CERINO, CHU Conception, Marseille, mathieu.cerino@ap-hm.fr.
Fanny ROMAIN, CHU Conception, Marseille, fanny.romain@ap-hm.fr.
Marie HOUSSAYS, CHU Conception, Marseille, marie.houssays@ap-hm.fr.
Jean Pierre QUENOT, CHU François Mitterand, Dijon, jean-pierre.quenot@chu-dijon.fr.
Lionel PIROTH, CHU François Mitterand, Dijon, lionel.piroth@chu-dijon.fr.
Bruno VERGÈS, CHU François Mitterand, Dijon, bruno.verges@chu-dijon.fr.
Laurence DUVILLARD, CHU François Mitterand, Dijon, laurence.duvillard@chu-dijon.fr.
Bernard BONNOTTE, CHU François Mitterand, Dijon, bernard.bonnotte@chu-dijon.fr.
Alain MERCAT, CHU ANGERS, Angers, almercat@chu-angers.fr.
Vincent DUBEE, CHU ANGERS, Angers, vincent.dubee@chu-angers.fr.
Ingrid ALLIX, CHU ANGERS, Angers, inallix@chu-angers.fr.
Patrice RODIEN, CHU ANGERS, Angers, parodien@chu-angers.fr.
Robin DHERSIN, CHU ANGERS, Angers, Robin.Dhersin@chu-angers.fr.
Maylis LEBEAULT, CHU ANGERS, Angers, maylis.lebeault@chu-angers.fr.
wojciech TRZEPIZUR, CHU ANGERS, Angers, WoTrzepizur@chu-angers.fr.
Jocelyne LOISON, CHU ANGERS, Angers, jocelyne.loison@chu-angers.fr.
Antoine BRANGIER, CHU ANGERS, Angers, antoine.brangier@chu-angers.fr.
Pierre ASFAR, CHU ANGERS, Angers, piasfar@chu-angers.fr.
Pascal REYNIER, CHU ANGERS, Angers, pareynier@chu-angers.fr.
Françoise LARCHER, CHU ANGERS, Angers, frlarcher@chu-angers.fr.
Françoise JOUBAUD, CHU ANGERS, Angers, frjoubaud@chu-angers.fr.
Marie-Rita ANDREU, CHU ANGERS, Angers, marierita.andreu@chu-angers.fr.
Geoffrey URBANSKI, CHU ANGERS, Angers, geoffrey.urbanski@chu-angers.fr.
Laurent HUBERT, CHU ANGERS, Angers, lahubert@chu-angers.fr.
Cedric ANNWEILER, CHU ANGERS, Angers, ceannweiler@chu-angers.fr.
Jean DELLAMONICA, CHU de Nice—Hôpital de l'Archet, Nice, dellamonica.j@chu-nice.fr.
Johan COURJON, CHU de Nice—Hôpital de l'Archet, Nice, courjon.j@chu-nice.fr.
Nicolas CHEVALIER, CHU de Nice—Hôpital de l'Archet, Nice, chevalier.n@chu-nice.fr.
Giulia CHINETTI, CHU de Nice—Hôpital Pasteur, Nice, chinetti.g@chu-nice.fr.
Magda CHAFAI, CHU de Nice—Hôpital de l'Archet, Nice, chafai.m@chu-nice.fr.
Bruno MOURVILLIER, CHU de Reims, Reims, bmourvillier@chu-reims.fr.
Firouze BANI-SADR, CHU de Reims, Reims, fbanisadr@chu-reims.fr.
Sarra BARRAUD, CHU de Reims, Reims, sbarraud@chu-reims.fr.
Brigitte DELEMER, CHU de Reims, Reims, bdelemer@chu-reims.fr.
Philippe GILLERY, CHU de Reims, Reims, pgillery@chu-reims.fr.
Pascale LABEDADE, Centre Hospitalier Sud-Francilien, Corbeil-Essonnes, pascale.labedade@chsf.fr.
Amélie CHABROL, Centre Hospitalier Sud-Francilien, Corbeil-Essonnes, amelie.chabrol@chsf.fr.
Alfred PENFORNIS, Centre Hospitalier Sud-Francilien, Corbeil-Essones, alfred.penfornis@chsf.fr.
Catherine PETIT, Centre Hospitalier Sud-Francilien, Corbeil-Essones, catherine.petit@chsf.fr.
Coralie AMADOU, Centre Hospitalier Sud-Francilien, Corbeil-Essonnes, coralie.amadou@chsf.fr.
Maxime ADLER, Centre Hospitalier Sud-Francilien, Corbeil-Essonnes, maxime.adler@chsf.fr.
Clément DUBOST, HIA Bégin, Saint Mandé, clement.dubost@intradef.gouv.fr.
Pierre-Louis CONAN, HIA Bégin, Saint Mandé, pierre-louis.conan@intradef.gouv.fr.
Lyse BORDIER, HIA Bégin, Saint Mandé, lyse.bordier@intradef.gouv.fr.
Franck CEPPA, HIA Bégin, Saint Mandé, franck.ceppa@intradef.gouv.fr.
Cyril GARCIA, HIA Bégin, Saint Mandé, cyril1.garcia@intradef.gouv.fr.
Mathilde SOLLIER, HIA Bégin, Saint Mandé, mathilde.sollier@intradef.gouv.fr.
Olivier DUPUY, GH Paris Saint Joseph, Paris, odupuy@hpsj.fr.
Sophie LAPLANCE, GH Paris Saint Joseph, Paris, slaplanche@hpsj.fr.
Olivier BILLUART, GH Paris Saint Joseph, Paris, obilluart@hpsj.fr.
Marie Joseph AROULANDA, GH Paris Saint Joseph, Paris, mjaroulanda@hpsj.fr.
Frédérique OLIVIER, CH CAHORS, Cahors, frederique.olivier@ch-cahors.fr.
Florence AYON, CH CAHORS, Cahors, florence.ayon@ch-cahors.fr.
Nathalie WILHELM, CH CAHORS, Cahors, nathalie.wilhelm@ch-cahors.fr.
Loic EPELBOIN, CHU Cayennes, Cayenne, loic.epelboin@ch-cayenne.fr.
Nadia SABBAH, CHU Cayennes, Cayenne, nadia.sabbah@ch-cayenne.fr.
Aurelie CHARPIN, CHU Cayennes, Cayenne, aurelie.charpin@ch-cayenne.fr.
Pierre SQUARA, Clinique Ambroise Paré, Paris, pierre.squara@orange.fr.
Olivier BELLIARD, Clinique Ambroise Paré, Paris, olivier_belliard@yahoo.fr.
Claude DUBOIS, Clinique Ambroise Paré, Paris, claude.dubois@clinique-a-pare.fr.
Michel MARRE, Clinique Ambroise Paré, Paris, marre.michel@gmail.com.
Johann AUCHABIE, CH Cholet, Cholet, johann.auchabie@ch-cholet.fr.
Roxane COURTOIS, CH Cholet, Cholet, roxane.courtois@ch-cholet.fr.
Thierry DURIEZ, CH Cholet, Cholet, thierry.duriez@ch-cholet.fr.
Tiphaine MERGEY, CH Cholet, Cholet, tiphaine.mergey@ch-cholet.fr.
Laura VALLEE, CH Cholet, Cholet, laura.vallee@ch-cholet.fr.
Laetitia SEGUIN, CH Cholet, Cholet, laetitia.seguin@ch-cholet.fr.
Abdallah AL-SALAMEH, CHU Amiens- Picardie, Amiens, al-salameh.abdallah@chu-amiens.fr.
Jean-Philippe LANOIX, CHU Amiens- Picardie, Amiens, lanoix.jean-philippe@chu-amiens.fr.
Sandrine SORIOT-THOMAS, CHU Amiens- Picardie, Amiens, soriot-thomas.sandrine@chu-amiens.fr.
Anne-Marie BOURGEOIS-DESCOULS, CHU Amiens- Picardie, Amiens, bourgeois.anne-marie@chu-amiens.fr.
Rachel DESAILLOUD, CHU Amiens- Picardie, Amiens, dessaillud.rachelàchu-amiens.fr.
Natacha GERMAIN, CHU de Saint Etienne, Saint Etienne, natacha.germain@chu-st-etienne.fr.
Bogdan GALUSCA, CHU de Saint Etienne, Saint Etienne, bogdan.galusca@chu-st-etienne.fr.
Gwenaelle BELLETON, CHU de Saint Etienne, Saint Etienne, gwenaelle.belleton@chu-st-etienne.fr.
Nesrine MAROUANI, CHU de Saint Etienne, Saint Etienne, nesrine.marouani@chu-st-etienne.fr.
Delia PALAGHIU, CHU de Saint Etienne, Saint Etienne, delia.palaghiu@chu-st-etienne.fr.
Amira HAMMOUR, CHU de Saint-Etienne, Saint-Etienne, amira.hammour@chu-st-etienne.fr.
Fernando BERDAGUER, Hôpital Nord Franche-Comté, Belfort, fberdaguer@hotmail.com.
Thimothée KLOPFENSTEIN, Hôpital Nord Franche-Comté, Belfort, Timothee.KLOPFENSTEIN@hnfc.fr.
Hajer ZAYET, Hôpital Nord Franche-Comté, Belfort, Hajer.ZAYET@hnfc.fr.
Patrice WINISZEWSKI, Hôpital Nord Franche-Comté, Belfort, Patrice.WINISZEWSKI@hnfc.fr.
Marie ZANUSSO, Hôpital Nord Franche-Comté, Belfort, marie.zanusso@hnfc.fr.
Pauline GARNIER, Hôpital Nord Franche-Comté, Belfort, pauline.garnier@hnfc.fr.
Ingrid JULIER, CH de Ales, Ales, dr.julier@ch-ales.fr.
Karim HAMZAOUI, CH de Ales, Ales, dr.hamzaoui@ch-ales.fr.
Sophie MARTY-GRES, CH de Ales, Ales, biologie@ch-ales.fr.
Tarik EL SADKI, CH de Ales, Ales, biologie@ch-ales.fr.
Lucile CADOT, CH de Ales, Ales, biologie@ch-ales.fr.
Jean-Louis DUBOST, CH de Pontoise, Pontoise, jean-louis.dubost@ght-novo.fr.
Céline GONFROY, CH de Pontoise, Pontoise, celine.gonfroy@ght-novo.fr.
Catherine CAMPINOS, CH de Pontoise, Pontoise, catherine.campinos@ght-novo.fr.
Pascale MARTRES, CH de Pontoise, Pontoise, pascale.martres@ght-novo.fr.
Marie Pierre COULHON, CH de Pontoise, Pontoise, marie-pierre.coulhon@ght-novo.fr.
Nicolas ALLOU, CHU Felix Guyon, Saint Denis, nicolas.allou@chu-reunion.fr.
Marwa BACHIR, CHU Felix Guyon, Saint Denis, marwa.bachir@chu-reunion.fr.
Stella HOANG, CHU Felix Guyon, Saint Denis, stella.hoang@chu-reunion.fr.
Candice KEMBELLEC, CHU Felix Guyon, Saint Denis, candice.kembellec@chu-reunion.fr.
Olivia SUPLY, CHU Felix Guyon, Saint Denis, olivia.suply@chu-reunion.fr.
Fatima KHARCHA, CHU Felix Guyon, Saint Denis, fatima.kharcha@chu-reunion.fr.
Anne-Claire DEVOUGE, CHU Felix Guyon, Saint Denis, anne-claire.devouge@chu-reunion.fr.
Anna FLAUS-FURMANUK, CHU Felix Guyon, Saint Denis, anna.flaus-furmaniuk@chu-reunion.fr.
Isabelle MADELINE, CHU Felix Guyon, Saint Denis, isabelle.madeline@chu-reunion.fr.
Vincent EHINGER, CHU Felix Guyon, Saint Denis, vincent.ehinger@chu-reunion.fr.
Sophie BASTARD, CHU Felix Guyon, Saint Denis, sophie.bastard@chu-reunion.fr.
Loic RAFFRAY, CHU Felix Guyon, Saint Denis, loic.raffray@chu-reunion.fr.
Frederic RENOU, CHU Felix Guyon, Saint Denis, frederic.renou@chu-reunion.fr.
Aude BOJARSKI, CHU Felix Guyon, Saint Denis, aude.bojarski@chu-reunion.fr.
Caroline PAUL, CHU Felix Guyon, Saint Denis, caroline.paul@chu-reunion.fr.
Karine BORSU, CHU Felix Guyon, Saint Denis, karine.borsu@chu-reunion.fr.
Angelique GORLIN, CHU Felix Guyon, Saint Denis, angelique.gorlin@chu-reunion.fr.
Servane DI BERNARDO, CHU Felix Guyon, Saint Denis, servane.dibernardo@chu-reunion.fr.
Carole TRUONG VAN UT, CHU Felix Guyon, Saint Denis, carole.truong-van-ut@chu-reunion.fr.
Stephane RENAUD, CHU Felix Guyon, Saint Denis, stephane.renaud@chu-reunion.fr.
Antoine VIGNOLES, CHU Felix Guyon, Saint Denis, antoine.vignoles@chu-reunion.fr.
Emilie FOCH, CHU Felix Guyon, Saint Denis, emilie.foch@chu-reunion.fr.
Laurie MASSE, CHU Felix Guyon, Saint Denis, laurie.masse@chu-reunion.fr.
Hubert GRAND, robert boulin, Libourne, hubert.grand@ch-libourne.fr.
Helene FERRAND, robert boulin, Libourne, helene.ferrand@ch-libourne.fr.
Christelle RAFFAITIN-CARDIN, robert boulin, Libourne, christelle.raffaitin@ch-libourne.fr.
Hadjer ZELLAGUI, robert boulin, Libourne, hadjer.zellagui@ch-libourne.fr.
Celine CASTANG-BRACHET, robert boulin, Libourne, celine.castang@ch-libourne.fr.
Frederique BOURY, robert boulin, Libourne, frederique.boury@ch-libourne.fr.
Ana ALVAREZ TENA, CH Albi, Albi, ana.alvareztena@ch-albi,fr.
Isabelle MOURA, CH Albi, Albi, isabelle.moura@ch-albi.fr.
Pierre KALFON, LOUIS PASTEUR, Le Coudray, pkalfon@ch-chartres.fr.
Juliana DARASTEANU, LOUIS PASTEUR, Le Coudray, jdarasteanu@ch-cahrtres.fr.
Arnaud MONIER, LOUIS PASTEUR, Le Coudray, amonier@ch-chartres.fr.
Pascal FOUCAULT, LOUIS PASTEUR, Le Coudray, pfoucault@ch-chartres.fr.
Alexandra DEPUILLE, LOUIS PASTEUR, Le Coudray, adepuille@ch-chartres.fr.
Stéphanie LAUGIER-ROBIOLLE, CH D'AUCH, 32,000, s.laugier-robiolle@ch-auch.fr.
Patrick CANEIRO, CH D'AUCH, 32,000, p.caneiro@ch-auch.fr.
Maud BASSO, CH D'AUCH, 32,000, maud.basso@ch-auch.fr.
Etienne LARGER, Hôpital COCHIN, Paris, etienne.larger@aphp.fr.
Samir BOUAM, Hôpital COCHIN, Paris, samir.bouam@aphp.fr.
Wahiba BENZENATI, Hôpital COCHIN, Paris, wahiba.benzenati-ext@aphp.fr.
Leila AIT BACHIR, Hopital francobritannique, Levallois, leila.aitbachir@ihfb.org.
Camille CUSSAC PILLEGAND, Hopital francobritannique, Levallois, camille.cussac-pillegand@ihfb.org.
Marc VASSE, Hopital francobritannique, Suresnes, marc.vasse@hopital-foch.fr.
Christophe MICHARD, CH du Forez, Montbrison, christophe.michard@ch-forez.fr.
Nathanaëlle MONTANIER, CH du Forez, Montbrison, nathanaelle.montanier@ch-forez.fr.
Luc MILLOT, CH du Forez, Montbrison, luc.millot@ch-forez.fr.
Françoise CREPET, CH du Forez, Montbrison, francoise.crepet@ch-forez.fr.
Danielle RATSIMBA, CH du Forez, Montbrison, danielle.ratsimba@ch-forez.fr.
Kevin BOUILLER, CHU JEAN MINJOZ, Besancon, kbouiller@chu-besancon.fr.
Sophie BOROT, CHU JEAN MINJOZ, Besancon, sophie.borot@univ-fcomte.fr.
Isabelle BRUCKERT, CHU JEAN MINJOZ, Besancon, ibruckert@chu-besancon.fr.
Annie CLERGEOT, CHU JEAN MINJOZ, Besancon, aclergeot@chu-besancon.fr.
Franck SCHILLO, CHU JEAN MINJOZ, Besancon, fschillo@chu-besancon.fr.
Dorothée VIGNES, CHU Antoine Béclère, Clamart, dorothée.vignes@aphp.fr.
Muriel BOURGEON-GHITTORI, CHU Antoine Béclère, Clamart, muriel.bourgeon@aphp.fr.
Hamoud LACHGAR, CHU Antoine Béclère, Clamart, hamoud.lachgar@aphp.fr.
Claire LAMBERT DE CURSAY, CHU Antoine Béclère, Clamart, claire.lambertdecursay@aphp.fr.
Stéphane LEVANTE, CHU Antoine Béclère, Clamart, stephane.levante@aphp.fr.
Jean Charles AUREGAN, CHU Antoine Béclère, Clamart, jean-charles.auregan@aphp.fr.
Antoine MERLET, CH Bretagne Atlantique, Vannes, antoine.merlet@ch-bretagne-atlantique.fr.
Cécile ZARAGOZA, CH Bretagne Atlantique, Vannes, cecile.zaragora@ch-bretagne-atlantique.fr.
Gwénaëlle ARNAULT, CH Bretagne Atlantique, Vannes, gwenaelle.arnault@ch-bretagne-atlantique.fr.
Anne-Gaëlle LE LOUPP, CH Bretagne Atlantique, Vannes, anne-gaelle-le8loupp@ch-bretagne-atlantique.fr.
Olivier LESIEUR, Saint Louis, La Rochelle, olivier.lesieur@ch-larochelle.fr.
Mariam RONCATO-SABERAN, Saint Louis, La Rochelle, mariam.roncato@ch-larochelle.fr.
Didier GOUET, Saint Louis, La Rochelle, didier.gouet@ch-larochelle.fr.
Romain LEMARIE, Saint Louis, La Rochelle, romain.lemarie@ch-larochelle.fr.
Hong_An ALLANO, Saint Louis, La Rochelle, hong-an.allano@ght-atlantique17.fr.
Emmanuel VIVIER, Saint-Joseph Saint-Luc, Lyon, evivier@ch-stjoseph-stluc-lyon.fr.
Caroline PARISET, Saint-Joseph Saint-Luc, Lyon, cpariset@ch-stjoseph-stluc-lyon.fr.
Cédric LUYTON, Saint-Joseph Saint-Luc, Lyon, cluyton@ch-stjoseph-stluc-lyon.fr.
Lucien MARCHAND, Saint-Joseph Saint-Luc, Lyon, lmarchand@ch-stjoseph-stluc-lyon.fr.
Fanny DOROSZEWSKI, Saint-Joseph Saint-Luc, LYON, fdoroszewski@ch-stjoseph-stluc-lyon.fr.
Matthieu PECQUET, Saint-Joseph Saint-Luc, Lyon, mpecquet@ch-stjoseph-stluc-lyon.fr.
Laurent PERARD, Saint-Joseph Saint-Luc, Lyon, lperard@ch-stjoseph-stluc-lyon.fr.
Sylvie VUILLERMOZ-BLAS, Saint-Joseph Saint-Luc, Lyon, svuillermoz@ch-stjoseph-stluc-lyon.fr.
Nicolas KACKI, CHD de Vendée, La Roche Sur Yon, nicolas.kacki@chd-vendée.fr.
Patricia CHARRIER, CHD de Vendée, La Roche Sur Yon, patricia.charrier@chd-vendée.fr.
Amélie DUCET-BOIFFARD, CHD de Vendée, La Roche Sur Yon, amelie.ducet-boiffard@chd-vendee.fr.
Françoise DESROYS DU ROURE, CHD de Vendée, La Roche Sur Yon, francois.desroysduroure@chd-vendee.fr.
Olivier BOURRON, Pitié-Salpêtrière, Paris, olivier.bourron@aphp.fr.
Dominique BONNEFONT-ROUSSELOT, Pitié-Salpêtrière, Paris, dominique.rousselot@aphp.fr.
Suzanne LAROCHE, Pitié-Salpêtrière, Paris, Suzanne.laroche@aphp.fr.
Franck PHAN, Pitié-Salpêtrière, Paris, franck.phan@aphp.fr.
Agnès HARTEMANN, Pitié-Salpêtrière, Paris, agnes.hartemann@aphp.fr.
Cyrielle CAUSSY, CHU LYON SUD, Pierre Benite, cyrielle.caussy@chu-lyon.fr.
Emmanuel DISSE, CHU LYON SUD, Pierre Benite, emmanuel.disse@chu-lyon.fr.
Emilie BLOND, CHU LYON SUD, Pierre Benite, emilie.blond@chu-lyon.fr.
Claude GUERIN, Hôpital Croix Rousse, Lyon, claude.guerin@chu-lyon.fr.
Thomas PERPOINT, Hôpital Croix Rousse, Lyon, thomas.perpoint@chu-lyon.fr.
Philippe MOULIN, Hôpital Louis pradel, Lyon, philippe.moulin@chu-lyon.fr.
Régine CARTIER, Hôpital Louis pradel, Lyon, regine.cartier@chu-lyon.fr.
Geoffroy HARIRI, Hôpital Saint-Antoine, Paris, geoffroy.hariri@aphp.fr.
Dorothée CHOPIN, Hôpital Saint-Antoine, Paris, dorothee.chopin@aphp.fr.
Camille VATIER, Hôpital Saint-Antoine, Paris, camille.vatier@aphp.fr.
Nathalie BOURCIGAUX, Hôpital Saint-Antoine, Paris, nathalie.bourcigaux@aphp.fr.
Emmanuelle CHAIGNEAU, Hôpital Saint-Antoine, Paris, emmanuelle.chaigneau@aphp.fr.
Sophie CHRISTIN-MAITRE, Hôpital Saint-Antoine, Paris, sophie.christin-maitre@aphp.fr.
Bruno DONADILLE, Hôpital Saint-Antoine, Paris, bruno.donadille@aphp.fr.
Bruno FEVE, Hôpital Saint-Antoine, Paris, bruno.feve@aphp.fr.
Sophie LAMOTHE, Hôpital Saint-Antoine, Paris, sophie.lamothe@aphp.fr.
Julie SARFATI, Hôpital Saint-Antoine, Paris, julie.sarfati@aphp.fr.
Pascal PERNET, Hôpital Saint-Antoine, Paris, pascal.pernet@aphp.fr.
Anne CHAMBON, CH Côtes Basques, Bayonne, achambon@ch-cotebasque.fr.
Delphine DEMARSY, CH Côtes Basques, Bayonne, ddemarsy@ch-cotebasque.fr.
Hugo CAMPAGNE, CH Côtes Basques, Bayonne, hcampagne@ch-cotebasque.fr.
Françoise LATIL-PLAT, CH Avignon, Avignon, fplat@ch-avignon.fr.
Monica BERNE, CH Avignon, Avignon, MBeyrne@ch-avignon.fr.
Marilyne GRINAND, CH Avignon, Avignon, GRINAND.Marilyne@ch-avignon.fr.
Marion TOUZET, CH Avignon, Avignon, TOUZET.Marion@ch-avignon.fr.
Aydrey ZABULON, CHU Martinique, Fort de France, audrey.zabulon@chu-martinique.fr.
Jocelyne CRASPAG, CHU Martinique, Fort de France, jocelyne.craspag@chu-martinique.fr.
Catherine LEDOUX, CHU Martinique, Fort de France, catherine.ledoux@chu-martinique.fr.
Cedric CONTARET, CHU Martinique, Fort de France, Cedric.CONTARET@chu-martinique.fr.
Blandine JANAND-DELENNE, CH du Pays d'Aix, Aix en Provence, bdelenne@ch-aix.fr.
Anaïs GIRAUD, CH du Pays d'Aix, Aix en Provence, agiraud@ch-aix.fr.
Marie Lou LACRIMINI, CH du Pays d'Aix, Aix en Provence, mlacrimini@ch-aix.fr.
Joëlle ARRIVIE, CH de Bigorre, Tarbes, jarrivie@ch-tarbes-vic.fr.
Deborah ANCELLE, CH Le Havre, Le Havre, deborah.ancelle@ch-havre.fr.
Carine GUILLOIS, CH Le Havre, Le Havre, carine.guillois@ch-havre.fr.
Bénédicte FREMY, CH Agen, Agen, fremyb@ch-agen-nerac.fr.
Amina CHAALAL, CH Agen, Agen, chaalalam@ch-agen-nerac.fr.
Gaëlle BARRANDE, CH Argenteuil, Argenteuil, gaelle.barrande@ch-argenteuil.fr.
Anne DORANGE, CH Le Mans, Le Mans, adorange@ch-lemans.fr.
Eglantine ROUANET, CH Le Mans, Le Mans, erouanet@ch-lemans.fr.
Dominique SERET-BEGUE, CH Gonesse, Gonesse, dominique.seret-begue@ch-gonesse.fr.
Audrey SAOUD, CH Gonesse, Gonesse, audrey.saoud@ch-gonesse.fr.
Anne-Marie GUEDJ, CH Nîmes, Nîmes, anne.marie.guedj@chu-nimes.fr.
Nathalie BEDOS, CH Nîmes, Nîmes, nathalie.bedos@chu-nimes.fr.
Fritz-Line VELAYOUDOM, CHU Guadeloupe, Les Abymes, fritz-line.velayoudom@univ-antilles.fr.
Marie DUMAS, Hôpital St Vincent de Paul, Lille, dumas.marie@ghicl.net.
Benoite GONDA, Hôpital St Vincent de Paul, Lille, Gonda.Benoite@ghicl.net.
Christine COFFIN, CH Perigueux, Perigueux, christine.coffin@ch-perigueux.fr.
Stéphanie GIBIAT, CH Perigueux, Perigueux, urc@ch-perigueux.fr.
Myriam LUNGO, CH de Bastia, Bastia, myriam.lungo@gmail.com.
Chantal BULLY, Les Portes du Sud, Venissieux, C.BULLY@LESPORTESDUSUD.NET.
Pierre SERUSCLAT, Les Portes du Sud, Venissieux, p.serusclat@lesportesdusud.net.
Stella BULLY, Les Portes du Sud, Venissieux, stellabully.ecsel@gmail.com.
Patricia CARRE, Les Portes du Sud, Venissieux, patcarre69@gmail.com.
Jean-Philippe LEBERRE, Medipôle Hôpital Mutualiste, Villeurbanne, j.leberre@resamut.fr.
Carlos ELKHOURY, Medipôle Hôpital Mutualiste, Villeurbanne, c.elkhoury@resamut.fr.
Marine THIEUX, Medipôle Hôpital Mutualiste, Villeurbanne, m.thieux@resamut.fr.
Laetitia PARADISI-PRIEUR, Medipôle Hôpital Mutualiste, Villeurbanne, l.paradisi-prieur@resamut.fr.
List of Contributors for the ABCD nationwide Covid 19 and Diabetes audit:
ABCD nationwide Covid 19 and Diabetes audit – initial setup, maintenance and nationwide analysis: Rustam Rea, Emma Wilmot, Kamlesh Khunti, Sarah Wild, Ben Field, Parth Narendran, Rajiv Gandhi, Sophie Harris, Dinesh Nagi, Robert Ryder, Jim Davies, Steve Harris, Oliver Freeman, Ben Maylor, Kinga A Várnai, Gail Roadknight, Melissa Cull. Statistician: Yue Ruan.
England
Barts Health NHS Trust, Newham University Hospital: Amy Edwards, Susan Gelding, Kirun Gunganah; Bolton NHS Foundation Trust,Royal Bolton Hospital: Pyei Aung, Moulinath Banerjee; Brighton and Sussex University Hospitals NHS Trust (Univeristy Hospitals Sussex NHS Foundation Trust), Royal Sussex County Hospital: Ali Chakera, Dominique Rouse; Countess of Chester Hospital NHS Foundation Trust, Countess of Chester Hospital: Syed Haris Ahmed, Ho Yee Cheung, Hywel Roberts, Susan Seal, Syed Saah Shah; Dartford and Gravesham NHS Trust, Darent Valley Hospital: Amir Hayat, Cynthia Mohandas.
East and North Hertfordshire NHS Trust, Lister Hospital: Htet Htet Aung, Su Khant Chel, Nyan Lin, Kavitia Narula, Furruq Quadri, Su Lei Yin, Yin Yin; East Kent Hospitals University NHS Foundation Trust, William Harvey Hospital (Ashford): Alamin Alkundi, Abdelmajid Musa; East Suffolk and North Essex NHS Foundation Trust, Colchester General Hospital: Emma Birbeck, Charles Bodmer; East Sussex Healthcare NHS Trust, Conquest Hospital & Eastbourne District General Hospital: Irene Bossman, Sathis Kumar, Umesh Dashora, Elizabeth Toubi, Mansoor Zafar; George Eliot Hospital NHS Trust, Diabetes Care Team, George Eliot Hospital: Vinod Patel, Amitha Gopinath; Hull University Teaching Hospitals NHS Foundation Trust, Hull Royal Infirmary: Belinda Allan, Remat Karim; King's College Hospital NHS Foundation Trust, King's College hospital: Dharshana Appuhamillage, Khubaib Ayoub, Sophie Harris, Charmaine Ilangaratne, Maliha Iqbal, Rory Maclean, Omar Mustafa; Lancashire Teaching Hospitals NHS Foundation Trust, Royal Preston Hospital: Susan Baxter; London North West University Healthcare NHS Trust, Ealing Hospital: Malgorzata Adamus, Kevin Baynes; Maidstone and Tunbridge Wells NHS trust, Maidstone Hospital: Siva Sivappriyan; Mid Yorkshire Hospitals NHS Trust, Pinderfields Hospital: Ryan D’Costa, Dinesh Nagi; North Bristol NHS Trust, Southmead Hospital: Vernon Parfitt; North West Anglia NHS Foundation Trust, Hinchingbrooke Hospital: Mazharul Islam, Sadia Nasir; Oxford University Hospitals NHS Foundation Trust, Oxford Centre for Diabetes, Endocrinology and Metabolism, Churchill Hospital: Rustam Rea, Gail Roadknight, Kinga Várnai, Senthil Vasan; Pennine Acute Hospitals NHS Trust, Diabetes Centre, North Manchester General Hospital: Vilashini Arul Devah; Royal Berkshire NHS Foundation Trust (Berkshire Healthcare NHS Foundation Trust), Centre for Diabetes & Endocrinology: Foteini Kavvoura; Royal Devon and Exeter NHS Foundation Trust, Royal Devon and Exeter Hospital (Wonford): Lina Ficken, James Gilham, Vincent Simpson, Neil Walker; Royal Free London NHS Foundation Trust, Royal Free Hospital: Umaira Aziz, Efthimia Karra, Dipesh Patel, Miranda Rosenthal; Salford Royal NHS Foundation Trust, Salford Royal Hospital: Tracy Curran, Angela Paisley; Sandwell & West Birmingham NHS Trust, Diabetes at SWBH: Melissa Cull, Parijat De P, May Thin Khine, Pari Qayyam, Robert Ryder, Priscilla Sarkar; Sheffield Teaching Hospitals NHS Foundation Trust, Northern General Hospital: Rajiv Gandhi; Surrey & Sussex Healthcare NHS Trust, East Surrey Hospital: Ben Field, James Clark, Vesna Hogan, Lauren Jackson, Jamie-Leigh Williamson, R Younes;Taunton and Somerset NHS Foundation Trust—Musgrove Park Hospital: Lucy Robin; The Newcastle Upon Tyne Hospitals NHS Foundation Trust, The Royal Victoria Infirmary: Lydia Grixti, Suann Tee; University Hospital of Derby and Burton NHS Foundation Trust, Royal Derby Hospital and Queen’s Hospital Burton: Abilash Sathya, Emma Wilmot; University Hospital Southampton NHS Foundation Trust, Diabetes at UHSNHSFT: Mayank Patel; University Hospitals Birmingham NHS Foundation Trust, Heartlands Hospital: Catherine Holmes; University Hospitals Birmingham NHS Foundation Trust, University Hospital of Birmingham: Wasim Hanif, Sandip Ghosh, Parth Narendran; University Hospitals of Leicester NHS Trust, Diabetes Research Centre, Leicester General Hospital: Ehtasham Ahmad, Ejaz Ahmed, Melanie Davies, Steven Hartshorn, Kamlesh Khunti, Lee Simons, David Webb; University of Leicester: Ben Maylor.
University of Oxford: Jim Davies, Oliver Freeman, Steve Harris, Yue Ruan; West Suffolk Hospital NHS Foundation Trust, West Suffolk Hospital: Anupam Brahma; Yeovil District Hospital NHS Foundation Trust, Yeovil District Hospital: Seshadri Pramodh.
Scotland
NHS Forth Valley, Forth Valley Royal Hospital: Katy Frew, Alison Mackenzie, Abigail Wild; NHS Greater Glasgow and Clyde, Queen Elizabeth University Hospital: Helen Casey, Deborah Morrison, Conor McKeag, Anne Sillars, Angus Stirling.
Wales
Aneurin Bevan University Health Board, Nevill Hall Hospital: Fiona Smeeton; Aneurin Bevan University Health Board, Royal Gwent Hospital: Syed Muhammad, Kofi Obuobie, Win Yin; Cardiff & Vale University Health Board, University Hospital Llandough: Neera Agarwal, Mike Atkinson; Cardiff & Vale University Health Board, University Hospital of Wales: Sai Ambati, Rahim Khan, Preethi Nalla, Arshiya Tabasum; Hywel Dda University Health Board, Glangwili General Hospital: Stamatios Zouras; Hywel Dda NHS Trust, Prince Philip Hospital: Akhila Mallipedhi; Swansea Bay University Health Board, Singleton Hospital: Richard Chudleigh, David Williams.
Abbreviations
- CKD
Chronic kidney disease
- COVID-19
Coronavirus disease 2019
- ICU
Intensive care unit
- IMV
Invasive mechanical ventilation
- OR
Odds ratio
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- SD
Standard deviation
- 95% CI
95% Confidence interval
Author contributions
GL, PD, DM collected the Hospital del Mar-Hospital de la Santa Creu I Sant Pau cohort and BV and JFN collected the cohort from HM Hospìtales. GL, BV and DM drafted the first version of the manuscript. BC, MW, PG and SaH designed and conducted the CORONADO study. PJS conducted the CORONADO study. RR, SHW, YR and KK (with additional colleagues) designed the ABCD COVID-19 national audit. YR conducted the statistical analysis of the ABCD data. All authors approved the final manuscript.
Funding
This research was supported by CIBER-Consorcio Centro de Investigación Biomédica en Red- (CB15/00071), Instituto de Salud Carlos III, Ministerio de Ciencia e Innovación. CORONADO study received the following funding: the Fondation Francophone de Recherche sur le Diabète (FFRD), supported by Novo Nordisk, MSD, Abbott, AstraZeneca, Lilly and FFD (Fédération Française des Diabétiques) – CORONADO initiative emergency grant; Société Francophone du Diabète (SFD) – CORONADO initiative emergency grant; Air Liquide Health Care international. CORONADO initiative emergency grant; Allergan. CORONADO initiative emergency grant; AstraZeneca. CORONADO initiative emergency grant; Elivie. CORONADO initiative emergency grant; Fortil. CORONADO initiative emergency grant; Lifescan. CORONADO initiative emergency grant; CORONADO initiative emergency grant; Nantes Métroplole. NHC. CORONADO initiative emergency grant; Novo Nordisk. CORONADO initiative emergency grant; Sanofi. CORONADO emergency grant; PHRC National COVID-19 Hospitalization and Care Organization Division (DGOS) as part of the Hospital Clinical Research Program (PHRC COVID-19–20-0138). All research facilities are acknowledged for providing research associates and research technicians for clinical investigations pro bono. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The ABCD nationwide COVID-19 and Diabetes audit is an independent audit which has received support from Public Health Wales and Novo Nordisk.
Availability of data and materials
Data are available on request from corresponding author and/or national study leads with appropriate data governance permission.
Declarations
Ethics approval and consent to participate
United Kingdom: association of British clinical diabetologists (ABCD) COVID-19 audit: The audit is registered with Oxford University Hospitals NHS Foundation Trust (OUH), a Data Protection Impact Assessment was carried out and the audit was approved by the OUH Caldicott Guardian and the Public Benefit and Privacy Panel in Scotland (reference 2021-0111). France: CORONADO: The study was sponsored by the Nantes University Hospital and designed in accordance with the Declaration of Helsinki. It obtained all regulatory approvals. Spain – HM Hospitales cohort: The study was approved by the Ethics Committee of the Primary Health Care University Research Institute (IDIAP) Jordi Gol, Barcelona (approval number: 20/089-PCV). Spain – Barcelona cohort: The Hospital del Mar Institutional Ethics Committee (CEIm-2020/9352) and the Hospital de la Santa Creu I Sant Pau Ethics Committee (HSCSP-20/117) approved the study and waived the informed consent need due to the study’s nature.
Consent for publication
All authors approved the final manuscript and give consent for the publication.
Competing interests
All other authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Gemma Llauradó, Bogdan Vlacho, Matthieu Wargny and Yue Ruan first co-authors equally contributed to the work
Kamlesh Khunti and Dídac Mauricio last co-authors equally contributed to this work
Contributor Information
Dídac Mauricio, Email: didacmauricio@gmail.com.
for the CORONADO, the ABCD COVID-19 diabetes national audit, HM Hospitales investigators and the Hospital del Mar - Hospital de la Santa Creu i Sant Pau Diabetes Research Group:
Juan Antonio Arroyo, Juan-José Chillarón, Rosa Corcoy, Roberto Güerri, Manel Mata-Cases, Emilio Ortega, Matthieu Pichelin, Maëva Saignes, Jeanne Saunier, Selma El Andaloussi, Joëlle Martin-Gauthier, Emily Rebouilleau, Tanguy Roman, Pascale Mahot, Matthieu Pichelin, Anne-Laure Fournier-Guilloux, Nicolas Mauduit, Edith Bigot- Corbel, Anne-Sophie Boureau, Laure De Dekcer, Audrey Ernould, Claire Primot, Anne Seguin, Marielle Joliveau, Sonia Pouvreau, Chloé Fournier, Jeremy Thureau, Edith Fonteneau, Pamela Hublain, Carole Agasse, Mathilde De Kergaradec, Vincent Minville, Fanny Vardon-Bounes, Guillaume Martin-Blondel, Blandine Tramunt, Marie-Christine Turnin, Hélène Hanaire, Jean-Michel Mansuy, Didier Fabre, Marie-Blanche Arhainx, Laurent Cazals, Laure Combes, Emmanuelle Lami, Bruno Megarbane, Pierre Leroy, Jean-François Gautier, Tiphaine Vidal-Trecan, Jean-Pierre Riveline, Jean-Louis Laplanche, Stéphane Mouly, Louis Potier, Ronan Roussel, Malak Taher, Yawa Abouleka, Fetta Yaker, Aurelie Carlier, Anne Boutten, Marilyne Hallot-Feron, Fadila Mourah, Charles Thivolet, Emilie Blond, Muriel Rolland, Josep Verdecho Mendez, Marine Alexandre, Julien Pottecher, Emilie Richer, Laurent Meyer, Florina Luca, Jean-Marc Lessinger, Thibault Bahougne, Bruno Guerci, Siham Benzirar, Catherine Malaplate, Thierry Matton, Julien Poissy, Karine Faure, Pierre Fontaine, Florence Baudoux, Anne Vambergue, Jean David Pekar, Marc Lambert, Cécile Yelnik, Amélie Bruandet, Laurent Petit, Didier Neau, Vincent Rigalleau, Annie Berard, Amandine Galioot, Remy Coudroy, Arnaud Thille, René Robert, France Roblot-Cazenave, Blandine Rammaert, Pierre Jean Saulnier, Xavier Piguel, Nesrine Benhenda, Camille Husson, Celine Olivier, Florence Torremocha, Mathilde Fraty, Marie Flamen D’assigny, Aurelie Miot, Valentin Bossard, Kada Klouche, Alain Makinson, Ariane Sultan, Jean-Baptiste Bonnet, Vincent Foulongne, Florence Galtier, Cécile Aubron, Séverine Ansart, Véronique Kerlan, Pascale Quiniou, Jean- Luc Carre, Stéphane Quesnot, Bruno Laviolle, Carole Schwebel, Olivier Epaulard, Pierre-Yves Benhamou, Cécile Betry, Anne-Laure Borel, Sandrine Lablanche, Dorra Guergour, Catherine Duclos, Emmanuel Cosson, Erwan Guyot, Aurore Deniau, Phucthutrang Nguyen, Yves Reznik, Michael Joubert, Stéphane Allouche, Lydia Guittet, Steven Grange, Manuel Etienne, Gaëtan Prévost, Valéry Brunel, Jean-Christophe Lagier, Didier Raoult, Anne Dutour, Bénédicte Gaborit, Sandrine Boulllu, Patrice Darmon, Adèle Lasbleiz, Mathieu Cerino, Fanny Romain, Marie Houssays, Jean Pierre Quenot, Lionel Piroth, Bruno Vergès, Laurence Duvillard, Bernard Bonnotte, Alain Mercat, Vincent Dubee, Ingrid Allix, Patrice Rodien, Robin Dhersin, Maylis Lebeault, Wojciech Trzepizur, Jocelyne Loison, Antoine Brangier, Pierre Asfar, Pascal Reynier, Françoise Larcher, Françoise Joubaud, Marie-Rita Andreu, Geoffrey Urbanski, Laurent Hubert, Cedric Annweiler, Jean Dellamonica, Johan Courjon, Nicolas Chevalier, Giulia Chinetti, Magda Chafai, Bruno Mourvillier, Firouze Bani-Sadr, Sarra Barraud, Brigitte Delemer, Philippe Gillery, Pascale Labedade, Amélie Chabrol, Alfred Penfornis, Catherine Petit, Coralie Amadou, Maxime Adler, Clément Dubost, Pierre-Louis Conan, Lyse Bordier, Franck Ceppa, Cyril Garcia, Mathilde Sollier, Olivier Dupuy, Sophie Laplance, Olivier Billuart, Marie Joseph Aroulanda, Frédérique Olivier, Florence Ayon, Nathalie Wilhelm, Loic Epelboin, Nadia Sabbah, Aurelie Charpin, Pierre Squara, Olivier Belliard, Claude Dubois, Michel Marre, Johann Auchabie, Roxane Courtois, Thierry Duriez, Tiphaine Mergey, Laura Vallee, Laetitia Seguin, Abdallah Al-Salameh, Jean-Philippe Lanoix, Sandrine Soriot-Thomas, Anne-Marie Bourgeois-Descouls, Rachel Desailloud, Natacha Germain, Bogdan Galusca, Gwenaelle Belleton, Nesrine Marouani, Delia Palaghiu, Amira Hammour, Fernando Berdaguer, Thimothée Klopfenstein, Hajer Zayet, Patrice Winiszewski, Marie Zanusso, Pauline Garnier, Ingrid Julier, Karim Hamzaoui, Sophie Marty-Gres, Tarik El Sadki, Lucile Cadot, Jean-Louis Dubost, Céline Gonfroy, Catherine Campinos, Pascale Martres, Marie Pierre Coulhon, Nicolas Allou, Marwa Bachir, Stella Hoang, Candice Kembellec, Olivia Suply, Fatima Kharcha, Anne-Claire Devouge, Anna Flaus-Furmanuk, Isabelle Madeline, Vincent Ehinger, Sophie Bastard, Loic Raffray, Frederic Renou, Aude Bojarsk, Karine Borsu, Angelique Gorlin, Servane Di Bernardo, Carole Truong Van Ut, Stephane Renaud, Antoine Vignoles, Emilie Foch, Laurie Masse, Hubert Grand, Helene Ferrand, Christelle Raffaitin-Cardin, Hadjer Zellagui, Celine Castang-Brachet, Frederique Boury, Ana Alvarez Tena, Isabelle Moura, Pierre Kalfon, Louis Pasteur, Juliana Darasteanu, Louis Pasteur, Arnaud Monier, Louis Pasteur, Pascal Foucault, Louis Pasteur, Alexandra Depuille, Louis Pasteur, Stéphanie Laugier-Robiolle, Patrick Caneiro, Maud Basso, Etienne Larger, Samir Bouam, Wahiba Benzenati, Leila Ait Bachir, Camille Cussac Pillegand, Marc Vasse, Christophe Michard, Nathanaëlle Montanier, Luc Millot, Françoise Crepet, Danielle Ratsimba, Kevin Bouiller, Sophie Borot, Isabelle Bruckert, Annie Clergeot, Franck Schillo, Dorothée Vignes, Muriel Bourgeon-GhittoriLachgar, Claire Lambert De Cursay, Stéphane Levante, Jean Charles Auregan, Antoine Merlet, Cécile Zaragoza, Gwénaëlle Arnault, Anne-Gaëlle Le Loupp, Olivier Lesieur, Mariam Roncato-Saberan, Didier Gouet, Romain Lemari, Hong-An Allano, Emmanuel Vivier, Caroline Pariset, Cédric Luyton, Lucien Marchand, Fanny Doroszewski, Matthieu Pecquet, Laurent Perard, Sylvie Vuillermoz-Blas, Nicolas Kacki, Patricia Charrier, Amélie Ducet-Boiffard, Françoise Desroys Du Roure, Olivier Bourron, Dominique Bonnefont-Rousselot, Suzanne Laroche, Franck Phan, Agnès Hartemann, Cyrielle Caussy, Emmanuel Disse, Emilie Blond, Claude Guerin, Thomas Perpoint, Philippe Moulin, Régine Cartier, Geoffroy Hariri, Dorothée Chopin, Camille Vatier, Nathalie Bourcigaux, Emmanuelle Chaigneau, Sophie Christin-Maitre, Bruno Donadille, Bruno Feve, Sophie Lamothe, Julie Sarfati, Pascal Pernet, Anne Chambon, Delphine Demarsy, Hugo Campagne, Françoise Latil-Plat, Monica Berne, Marilyne Grinand, Marion Touzet, Aydrey Zabulon, Jocelyne Craspag, Catherine Ledoux, Cedric Contaret, Blandine Janand-Delenne, Anaïs Giraud, Marie Lou Lacrimini, Joëlle Arrivie, Deborah Ancelle, Carine Guillois, Bénédicte Fremy, Amina Chaalal, Gaëlle Barrande, Anne Dorange, Eglantine Rouanet, Dominique Seret-Begue, Audrey Saoud, Anne-Marie Guedj, Nathalie Bedos, Fritz-Line Velayoudom, Marie Dumas, Benoite Gonda, Christine Coffin, Stéphanie Gibiat, Myriam Lungo, Chantal Bully, Pierre Serusclat, Stella Bully, Patricia Carre, Jean-Philippe Leberre, Carlos Elkhoury, Marine Thieux, Laetitia Paradisi-Prieur, Emma Wilmot, Sarah Wild, Ben Field, Parth Narendran, Rajiv Gandhi, Sophie Harris, Dinesh Nagi, Robert Ryder, Jim Davies, Steve Harris, Oliver Freeman, Ben Maylor, Kinga A. Várnai, Gail Roadknight, Melissa Cul, Amy Edwards, Susan Gelding, Kirun Gunganah, Pyei Aung, Moulinath Banerjee, Ali Chakera, Dominique Rouse, Syed Haris Ahmed, Ho Yee Cheung, Hywel Roberts, Susan Seal, Syed Saah Shah, Amir Hayat, Cynthia Mohandas, Htet Htet Aung, Su Khant Chel, Nyan Lin, Kavitia Narula, Furruq Quadri, Su Lei Yin, Yin Yin, Alamin Alkundi, Abdelmajid Musa, Emma Birbeck, Charles Bodmer, Irene Bossman, Sathis Kumar, Umesh Dashora, Elizabeth Toubi, Mansoor Zafar, Vinod Patel, Amitha Gopinath, Belinda Allan, Remat Karim, Dharshana Appuhamillage, Khubaib Ayoub, Sophie Harris, Charmaine Ilangaratne, Maliha Iqbal, Rory Maclean, Omar Mustafa, Susan Baxter, Malgorzata Adamus, Kevin Baynes, Siva Sivappriyan, Ryan D’Costa, Dinesh Nagi, Vernon Parfitt, Mazharul Islam, Sadia Nasir, Gail Roadknight, Kinga Várnai, Senthil Vasan, Vilashini Arul Devah, Foteini Kavvoura, Lina Ficken, James Gilham, Vincent Simpson, Neil Walker, Umaira Aziz, Efthimia Karra, Dipesh Patel, Miranda Rosenthal, Tracy Curran, Angela Paisley, Melissa Cull, Parijat De P, May Thin Khine, Pari Qayyam, Robert Ryder, Priscilla Sarkar, Rajiv Gandhi, Ben Field, James Clark, Vesna Hogan, Lauren Jackson, Jamie-Leigh Williamson, R. Younes, Lucy Robin, Lydia Grixti, Suann Tee, Abilash Sathya, Emma Wilmot, Mayank Patel, Catherine Holmes, Wasim Hanif, Sandip Ghosh, Parth Narendran, Ehtasham Ahmad, Ejaz Ahmed, Melanie Davies, Steven Hartshorn, Kamlesh Khunti, Lee Simons, David Webb, Ben Maylor, Jim Davies, Oliver Freeman, Steve Harris, Anupam Brahma, Seshadri Pramodh, Katy Frew, Alison Mackenzie, Abigail Wild, Helen Casey, Deborah Morrison, Conor McKeag, Anne Sillars, Angus Stirling, Fiona Smeeton, Syed Muhammad, Kofi Obuobie, Win Yin, Neera Agarwal, Mike Atkinson, Sai Ambati, Rahim Khan, Preethi Nalla, Arshiya Tabasum, Stamatios Zouras, Akhila Mallipedhi, Richard Chudleigh, David Williams, Mallory Cianferani, Lisa Ludwig, Caroline Paul, and Hamoud Lachgar
References
- 1.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020 doi: 10.1038/s41586-020-2951-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lippi G, Sanchis-Gomar F, Henry BM. COVID-19: unravelling the clinical progression of nature’s virtually perfect biological weapon. Ann Transl Med. 2020 doi: 10.21037/atm-20-3989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, Imai N, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020 doi: 10.1101/2020.03.09.20033357v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perez-Saez J, Lauer SA, Kaiser L, Regard S, Delaporte E, Guessous I, et al. Serology-informed estimates of SARS-CoV-2 infection fatality risk in Geneva, Switzerland. Lancet Infect Dis. 2021 doi: 10.1016/S1473-3099(20)30584-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 doi: 10.1038/s41598-021-89548-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020 doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cariou B, Wargny M, Boureau A-S, Smati S, Tramunt B, Desailloud R, et al. Impact of diabetes on COVID-19 prognosis beyond comorbidity burden: the CORONADO initiative. Diabetologia. 2022;65:1436–1449. doi: 10.1007/s00125-022-05734-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bellini B, Nreu B, Francesconi P, Mannucci E. Covid-19 pandemic, diabetes and glycemic control: results of a retrospective cohort study of 230.000 persons with diabetes in tuscany. Nutr Metab Cardiovasc Dis. 2022 doi: 10.1016/j.numecd.2022.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fedeli U, Casotto V, Schievano E, Bonora E, Zoppini G. Diabetes as a cause of death across different COVID-19 epidemic waves. Diabetes Res Clin Pract. 2022;190:109984. doi: 10.1016/j.diabres.2022.109984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barron E, Bakhai C, Kar P, Weaver A, Bradley D, Ismail H, et al. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. Lancet Diabetes Endocrinol. 2020 doi: 10.2139/ssrn.3605225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kastora S, Patel M, Carter B, Delibegovic M, Myint PK. Impact of diabetes on COVID-19 mortality and hospital outcomes from a global perspective: an umbrella systematic review and meta-analysis. Endocrinol diabetes Metab. 2022;5:e00338. doi: 10.1002/edm2.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roncon L, Zuin M, Rigatelli G, Zuliani G. Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. J Clin Virol Off Publ Pan Am Soc Clin Virol. 2020;127:104354. doi: 10.1016/j.jcv.2020.104354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cariou B, Hadjadj S, Wargny M, Pichelin M, Al-Salameh A, Allix I, et al. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study. Diabetologia. 2020 doi: 10.1007/s00125-020-05180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feldman EL, Savelieff MG, Hayek SS, Pennathur S, Kretzler M, Pop-Busui R. COVID-19 and diabetes: a collision and collusion of two diseases. Diabetes. 2020 doi: 10.2337/dbi20-0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Llanera DK, Wilmington R, Shoo H, Lisboa P, Jarman I, Wong S, et al. Clinical characteristics of COVID-19 patients in a regional population with diabetes mellitus: the ACCREDIT study. Front Endocrinol (Lausanne) 2021;12:777130. doi: 10.3389/fendo.2021.777130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Global report on diabetes. World Health Organization; 2016.
- 17.Harris S, Ruan Y, Wild SH, Wargny M, Hadjadj S, Delasalle B, et al. Association of statin and/or renin-angiotensin-aldosterone system modulating therapy with mortality in adults with diabetes admitted to hospital with COVID-19: a retrospective multicentre European study. Diabetes Metab Syndr. 2022;16:102484. doi: 10.1016/j.dsx.2022.102484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nagi D, Ryder RE, Ruan Y, Field BC, Narendran P, Gandhi R, Harris S, Várnai KA, Davies J, Wild SH, Wilmot EG. An audit of people admitted to hospitalwith diabetes and coronavirus (SARS-CoV-2):data collection methods. The Association of British Clinical Diabetologists (ABCD) Nationwide Audit. Br J Diabetes. 2021;21:96–99. doi: 10.15277/bjd.2021.299. [DOI] [Google Scholar]
- 19.Wargny M, Potier L, Gourdy P, Pichelin M, Amadou C, Benhamou P-Y, et al. Predictors of hospital discharge and mortality in patients with diabetes and COVID-19: updated results from the nationwide CORONADO study. Diabetologia. 2021;64:778–794. doi: 10.1007/s00125-020-05351-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ortega E, Corcoy R, Gratacòs M, Cos Claramunt FX, Mata-Cases M, Puig-Treserra R, et al. Risk factors for severe outcomes in people with diabetes hospitalised for COVID-19: a cross-sectional database study. BMJ Open. 2021;11:e051237. doi: 10.1136/bmjopen-2021-051237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Draznin B, Aroda VR, Bakris G, Benson G, Brown FM, Freeman R, et al. 11. Chronic kidney disease and risk management: standards of medical care in diabetes-2022. Diabetes Care. 2022;45:S175–S184. doi: 10.2337/dc22-S011. [DOI] [PubMed] [Google Scholar]
- 22.Singh AK, Gillies CL, Singh R, Singh A, Chudasama Y, Coles B, et al. Prevalence of co-morbidities and their association with mortality in patients with COVID-19: a systematic review and meta-analysis. Diabetes Obes Metab. 2020;22:1915–1924. doi: 10.1111/dom.14124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Apicella M, Campopiano MC, Mantuano M, Mazoni L, Coppelli A, Del PS. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol. 2020;8:782–792. doi: 10.1016/S2213-8587(20)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol. 2020;17:11–30. doi: 10.1038/s41574-020-00435-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Phan F, Boussouar S, Lucidarme O, Zarai M, Salem J-E, Kachenoura N, et al. Cardiac adipose tissue volume and IL-6 level at admission are complementary predictors of severity and short-term mortality in COVID-19 diabetic patients. Cardiovasc Diabetol. 2021;20:165. doi: 10.1186/s12933-021-01327-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang X, Fang X, Cai Z, Wu X, Gao X, Min J, et al. Comorbid chronic diseases and acute organ injuries are strongly correlated with disease severity and mortality among COVID-19 patients: a systemic review and meta-analysis. Research. 2020 doi: 10.34133/2020/2402961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lohia P, Kapur S, Benjaram S, Cantor Z, Mahabadi N, Mir T, et al. Statins and clinical outcomes in hospitalized COVID-19 patients with and without diabetes mellitus: a retrospective cohort study with propensity score matching. Cardiovasc Diabetol. 2021;20:140. doi: 10.1186/s12933-021-01336-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McGurnaghan SJ, Weir A, Bishop J, Kennedy S, Blackbourn LAK, McAllister DA, et al. Risks of and risk factors for COVID-19 disease in people with diabetes: a cohort study of the total population of Scotland. Lancet Diabetes Endocrinol. 2021;9:82–93. doi: 10.1016/S2213-8587(20)30405-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure S1. Odds ratio for the association between mortality (1A–C), intensive care unit admission (2A–C) and use of invasive mechanical ventilation during the hospitalization (3A–C) and ischemic heart disease in each of the four cohorts and overall. I2 indicates heterogeneity in the estimates. Odds ratio estimates adjusted for: model 1: age and sex (B); model 2: model 1 + type of diabetes, arterial hypertension, and the presence of microvascular disease (C).
Additional file 2: Figure S2. Odds ratio for the association between mortality (1A–C), intensive care unit admission (2A–C) and and stroke in each of the four cohorts and overall. I2 indicates heterogeneity in the estimates. Odds ratio estimates adjusted for: model 1: age and sex (B); model 2: model 1 + type of diabetes, arterial hypertension, and the presence of microvascular disease (C).
Additional file 3: Figure S3. Odds ratio for the association between mortality (1A–C), intensive care unit admission (2A–C) and peripheral artery disease in each of the four cohorts and overall. I2 indicates heterogeneity in the estimates. Odds ratio estimates adjusted for: model 1: age and sex (B); model 2: model 1 + type of diabetes, arterial hypertension, and the presence of microvascular disease (C).
Data Availability Statement
Data are available on request from corresponding author and/or national study leads with appropriate data governance permission.