Abstract
Background
Depression is one of the most studied mental health disorders, with varying prevalence rates reported across study populations in Uganda. A systematic review and meta-analysis was carried out to determine the pooled prevalence of depression and the prevalence of depression across different study populations in the country.
Methods
Papers for the review were retrieved from PubMed, Scopus, PsycINFO, African Journal OnLine, and Google Scholar databases. All included papers were observational studies regarding depression prevalence in Uganda, published before September 2021. The Joanna Briggs Institute Checklist for Prevalence Studies was used to evaluate the risk of bias and quality of the included papers, and depression pooled prevalence was determined using a random-effects meta-analysis.
Results
A total of 127 studies comprising 123,859 individuals were identified. Most studies were conducted among individuals living with HIV (n = 43; 33.9%), and the most frequently used instrument for assessing depression was the Depression sub-section of the Hopkins Symptom Checklist (n = 34). The pooled prevalence of depression was 30.2% (95% confidence interval [CI]: 26.7–34.1, I2 = 99.80, p<0.001). The prevalence of depression was higher during the COVID-19 pandemic than during the pre-pandemic period (48.1% vs. 29.3%, p = 0.021). Refugees had the highest prevalence of depression (67.6%; eight studies), followed by war victims (36.0%; 12 studies), individuals living with HIV (28.2%; 43 studies), postpartum or pregnant mothers (26.9%; seven studies), university students (26.9%; four studies), children and adolescents (23.6%; 10 studies), and caregivers of patients (18.5%; six studies).
Limitation
Significantly high levels of heterogeneity among the studies included.
Conclusion
Almost one in three individuals in Uganda has depression, with the refugee population being disproportionately affected. Targeted models for depression screening and management across various populations across the country are recommended.
Trial registration
Protocol registered with PROSPERO (CRD42022310122).
Introduction
The global prevalence rates of depression and other mental disorders have been increasing since 1990 [1], and approximately 3.8% of individuals worldwide have depression [2]. The prevalence of depression increased by an additional 27.6% globally during the coronavirus disease 2019 (COVID-19) pandemic (2020 to 2021) and by 23% in sub-Saharan Africa [3]. Despite the lower increase in the burden of depression in sub-Saharan Africa, most individuals with depression go undiagnosed and untreated in the region [4]. This has led to some individuals having extreme complications of depression, such as suicide [5–11]. The effect is even worse in low-income countries such as Uganda, with a high prevalence of depression (i.e., approximately one-fifth of the population between 2010 and 2017, and 27% of outpatients being depressed based on previous systematic review and meta-analyses [12, 13]).
In Uganda, due to the high burden of depression, various studies have been conducted among different populations (e.g., infected with human immunodeficiency virus [HIV], women, cancer patients, caregivers of patients, students, etc.) to understand its effects and design possible interventions [14–17]. Ugandan clinicians and researchers have employed various psychometrically validated tools to screen and diagnose depression among Ugandans, including the Patient Health Questionnaire (PHQ), Beck’s Depression Inventory (BDI), Hamilton Rating Scale for Depression, Symptom Checklist-20, Center for Epidemiologic Studies—Depression Scale, Akena Visual Depression Inventory, and the Mini-International Neuropsychiatric Interview (MINI) [18–24].
Uganda is a landlocked low-income country that has been affected by multiple adverse events, including civil wars, extreme poverty, high rates of HIV, various epidemics (e.g., Ebola), and poor mental health services, as well as being one of the largest refugee-hosting countries in the world [25–30]. These adverse events put many Ugandans at risk of developing depression due to the multiple physical, psychological, emotional, and social difficulties they are associated with. The effects of these difficulties are evidenced by the high levels of depression within various study groups in the country, such as women, children, students, individuals living with HIV, refugees, and members of the general public, with many groups reporting depression prevalence rates of over 70% [14, 31–37].
Due to the high burden of depression and a large amount of literature concerning mental health in Uganda, various systematic reviews have been conducted, especially among individuals living with HIV [12, 15, 38]. However, a comprehensive systematic synthesis of all published literature on depression in Uganda is lacking. Therefore, the present systematic review and meta-analysis aimed to determine the pooled prevalence of depression in Uganda and determine the prevalence of depression among various study populations in the country.
Methods
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [39] and the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines for systematic reviews and meta-analysis of observational studies [40]. The study protocol was prospectively registered with PROSPERO (CRD42022310122). The review question was formed according to the Joanna Briggs Institute (JBI) Checklist for Prevalence Studies and the CoCoPop (Condition, Context, and Population) [41]. The condition was depression, the context was Uganda, and the population was all studied groups. Therefore, the review’s research questions were: (i) “What is the prevalence of depression in Uganda?” and (ii) “What is the prevalence of depression among various study populations in Uganda?”
Search strategy
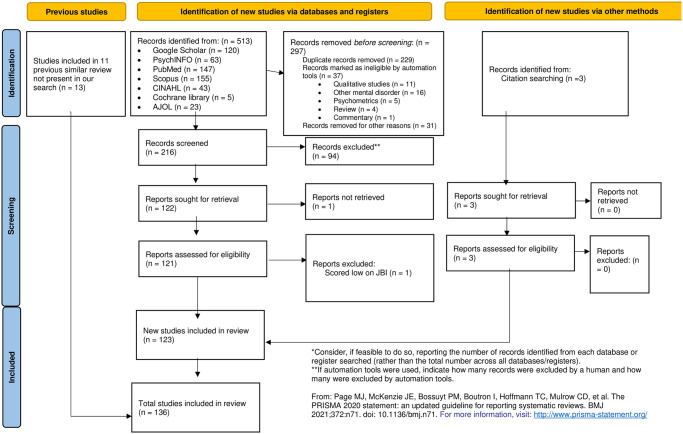
With the help of the university Librarian at Mbarara University of Science and Technology, relevant databases were used for the literature search, including PubMed, Scopus, PsychInfo, and Google Scholar (in the present review, eligible papers from the first 100 pages based on relevance were included), and African Journal OnLine (AJOL). The study included articles (both peer-reviewed and preprints) in all languages from 1972 (the first published paper about depression in Uganda [42]) to September 2021. The following key words were used in the literature search from different databases: (i) ‘depression,’ (ii) ‘Uganda,’ and (iv) ‘prevalence’ or ‘incidence.’ All systematic reviews concerning depression in Uganda, East Africa, and Africa were reviewed for eligible studies. The PRISMA 2020 flow chart shows the details of the search hits retrieved, included, or excluded papers [43] (Fig 1).
Fig 1. The PRISMA flow chart.
Inclusion criteria and exclusion criteria
The literature search included all observational studies (cross-sectional, case-control, and cohort studies) published in all languages regarding depression prevalence (based on different assessment tools or subjective reports) in Uganda, based on various assessment tools and cut-offs; and excluded case reports, case series, qualitative research, letters to the editor, commentaries, conference proceedings or abstracts, policy papers, protocols, reviews, and meta-analyses.
Study and data management
All identified papers were entered into EndNote 9 to ascertain duplicates. After removing duplicates and review articles, the titles and abstracts of the articles were screened for inclusion independently by two team members. MAM settled any discrepancies after a discussion with the two team members for the reason of exclusion. The final selected papers were read for the full review, and this was done in pairs after dividing the results into two. Two members of the research team reviewed the first half, and another two members of the research team reviewed the second half. For papers whose full texts were not fully accessible, the corresponding authors were contacted by email. The papers were assessed for a quality check using the JBI Checklist for Prevalence Studies [44], as used in other systematic reviews [45]. Finally, a research team member screened for eligible papers from the systematic reviews regarding depression in the region.
Data extraction
A pre-piloted and self-designed Google Forms document with the following information was used to collate the data. The data extracted included: the first author, year of data collection, study design, paper quality assessment questions based on the JBI Checklist, study group, sample size, age of participants, number of male and female participants, tools/questions used to assess for depression, and prevalence of depression.
Bias evaluation and quality assessment of the included papers
The nine-item JBI Checklist was used to evaluate the risk of bias and the quality of the included papers [44]. The JBI Checklist uses a four-point response system: “no,” “yes,” “unclear,” and “not applicable” for the following study characteristics: (i) appropriateness of the sample frame; (ii) recruitment procedure; (iii) adequacy of the sample size; (iv) description of participants and setting; (v) description of the identified sample; (vi) validity of the methods used to screen for depression; (vii) reliability of the methods used to screen for depression; (viii) adequacy of statistical analyses; and (ix) response rate. Articles were assigned one point for each ‘yes’ response, and the remaining responses were assigned zero points. Therefore, the total score ranged from 0 to 9. Studies with a score of 4 or above were considered good quality. One article was excluded due to scoring poorly on most parameters [42]. The scores of the papers are presented in Table 1.
Table 1. Participants’ characteristics of all studies included in the meta-analysis.
| First author, year of publication | Study design (JBI Checklist score) | Year of data collection | Districts | Study group | Sample size | Female (male) | Age (in years) | Tools used to access depression (cutoff) | Depression n (%) |
|---|---|---|---|---|---|---|---|---|---|
| Bolton 2004 [55] | CS (9) | 2000 | Masaka and Rakai | General population | 587 | 364 (223) | 39.3±2.9 | Depression section of the Hopkins Symptom Checklist (DHSCL) | 123 (21) |
| Ovuga 2006 [56] | CS (7) | 2000 and 2002 | Kampala | Non-medical undergraduate students in 2000 and undergraduate medical students in 2002 | 253 and 101 | 92 (161) and 31 (70) | 21.3± 2.4 and 23.5± 5.0 | Beck Depression Inventory (BDI)–(10) | 37 (16.2) and 4 (4) |
| Nakasujja 2007 [57] | CS (9) | 2001 | Kampala | Elderly patients in non-psychiatric wards | 127 | 64 (63) | Self-Reporting Questionnaire (SRQ 25)–(>5) | 23 (18) | |
| Nalugya-Sserunjogi 2016 [58] | CS (9) | 2003 | Mukono | school-going adolescents | 519 | 218 (301) | 16±2.18 | Children Depression Inventory (CDI)–(19) MINI-KID | 109 (21) and 8 (2.9) |
| Nakku 2006 [59] | CS (9) | 2002–2003 | Kampala | Women 6 weeks postpartum | 523 | 523 | 23.4±4.76 | MINI and SRQ-25 –(>5) | 32 (6.1) and 38 (7.3) |
| Kaharuza 2006 [60] | RCT (9) | 2003–2004 | Bugiri, Busia, Mbale, and Tororo | Individuals living with HIV | 1017 | 781 (236) | 31–40 = 452; 31–40 = 452; 41–50 = 291; and 50+ = 94 | Center for Epidemiological Studies Depression scale (CES-D) | 476 (47) |
| Kinyanda 2011b [61] | CS (9) | 2003–2004 | Adjumani, Apac, Arua, Bugiri, Bushenyi, Kaberamaido, Kapchorwa, Katakwi, Lira, Moyo, Mubende, Nebbi, Soroti, and Yumbe | General populations | 4,660 | DHSCL–(>1.75) | 1366 (29.3) | ||
| Ovuga 2005 [62] | CS (9) | Adjumani, Bugiri | General populations | 524 | BDI | 91 (17.4) | |||
| Lundberg 2011 [63] | CS (9) | 2004–2005 | Kampala, Mbarara | Residents from urban and semi-urban Kampala and Mbarara | 630 | 312 (334) | 18–24 = 337; 25–30 = 437 | DHSCL–(>1.75) | 96 (9.84) |
| Nakimuli-Mpungu 2013a [64] | CS (8) | 2004–2005 | Kiruhura | Individuals living with HIV | 244 | 156 (88) | 36.2±8.9; Range = 18–60 | DSMIV | 97 (40) |
| Agardh 2012 [65] | CS (8) | 2005 | Mbarara | Undergraduate university students at MUST | 976 | 362 (614) | Median age = 23. Younger ≤23: 628. Older>23: 329 (34.4), missing 23 | DHSCL-25—(31) | 146 (15) |
| Vinck 2007 [66] | CS (9) | 2005 | Gulu, Kitgum, Lira, and Soroti | War victims in displacement camps | 2585 | 1293 (1292) | 36.7±13.8 | DHSCL–(40) | 1151 (44.5) |
| Pfeiffer 2011 [67] | CS (7) | 2005 | Gulu | War victims | 72 | 31 (41) | Median = 23.7 | DHSCL–(>1.75) | 51 (71) |
| Martinez 2008 [68] | CS (9) | 2005 | Mbarara | Individuals living with HIV | 421 | 266 (155) | Median = 36, IQR = 11 | DHSCL–(>1.75) | 79 (18.8) |
| Muhwezi 2007 [69] | CS (9) | Kampala, Mpigi, and Mubende | Individuals attending primary health care facilities | 199 | 119 (80) | MINI | 74 (31.6) | ||
| Petrushkin 2005 [70] | CS (7) | Kampala | Individuals living with HIV | 46 | 24 (22) | 36.6 | MINI | 25 (54.35) | |
| Psaros 2015 [71] | Cohort (9) | 2005–2010 | Mbarara | Uganda AIDS Rural Treatment Outcomes (UARTO) cohort study | 453 | 314 (139) | 34.9±8.3 | DHSCL–(>1.75) | 172 (37.97) |
| Nakasujja 2010 [72] | CS (8) | 2005–2007 | Kampala | HIV-positive patients are at risk for cognitive impairment, and HIV-negative patients | 127 | 84 (43) | CES-D | 62 (48.82) | |
| Kaida 2014 [73] | Cohort (9) | 2005–2012 | Mbarara | Pregnant and postpartum HIV-positive women | 447 | 447 (0) | Median = 32; IQR = 10 | DHSCL–(>1.75) | 173 (38.9) |
| Roberts 2008 [74] | CS (9) | 2006 | Amuru, Gulu | War victims | 1210 | 727 (483) | 35.4 | DHSCL–(>1.75) | 811 (67) |
| Klasen 2013 [75] | CS (9) | 2006 | Gulu | Child soldiers (children and adolescents of war abducted victims who became soldiers) | 330 | 160 (170) | 14.44±1.57 | MINI-KID | 120 (36.4) |
| Klasen 2010a [76] | CS (9) | 2006 | Gulu | Child soldiers (children and adolescents of war abducted victims who became soldiers) | 330 | 160 (170) | 14.44±1.57 | MINI-KID | 120 (36.4) |
| Klasen 2010b [77] | CS (9) | 2006 | Gulu | Child soldiers (children and adolescents of war abducted victims who became soldiers) | 330 | 160 (170) | 14.44±1.57 | MINI-KID | 120 (36.4) |
| Abbo 2009 [78] | CS (9) | 2007 | Iganga and Jinja | Clients of traditional healers | 387 | 208 (178) | 34.8±13.55 | MINI | 21 (5.4) |
| Hatcher 2012 [79] | Secondary data analysis (9) | 2007 | Mbarara | HIV-infected women | 270 | 270 (0) | Median = 34. IQR = 10 | DHSCL–(>1.75) | 64 (6.7) |
| Pham 2009 [80] | CS (9) | 2007 | Amuria, Amuru, Gulu, Kitgum, Lira, Oyam, and Pader | War victims | 2875 | 1417 (1458) | 35.4±14.35 | DHSCL–(42) | 1150 (40) |
| Tsai 2012 [81] | Cohort (9) | 2007–2010 | Mbarara | Individuals living with HIV | 456 | 324 (132) | DHSCL–(>1.75) | 71 (15.57) | |
| Tsai 2016 [82] | Cohort (9) | 2007–2011 | Mbarara | Individuals living with HIV | 173 | 173 (0) | Median = 32; IQR = 11 | DHSCL–(>1.75) | 57 (33) |
| Nakimuli-Mpungu 2013b [83] | A prospective study (9) | 2007–2012 | Gulu, Kitgum, Soroti, Tororo | War victim with post-trauma disorder | 2868 | SRQ-20 | 1297 (45.22) | ||
| Winkler 2015 [84] | CS (9) | 2008 | Gulu, Kitgum, and Lira | child soldiers and war-affected victims | 843 | 355 (488) | 19.0±2.7. | DHSCL–(>2.65) | 64 (7.6) |
| Musisi 2009 [85] | CS (8) | Kampala | HIV positive adolescents | 82 | 46 (36) | 13.4±1.8 | SRQ-25 | 34 (40.8) | |
| Nsereko 2018 [51]–Thesis | CS (9) | 2018 | Kampala | School adolescents | 549 | 317 (228) | The Youth Self-Report (YSR) | 115 (21.1) | |
| Wagner 2012a [86] | Cohort (9) | 2008–2009 | Jinja, Kampala | Individuals living with HIV | 602 | 409 (193) | 35.7 | Patient Health Questionnaire– 9 (PHQ-9)–(10) | 78 (13) |
| Shumba 2013 [87] | CS (7) | 2008–2009 | Individuals living with HIV | 732 | 504 (228) | 19–39 = 294; 40–50 = 290; 50+ = 91 | Developed own tool | 432 (59) | |
| Okeke 2013 [88] | Cohort (9) | 2008–2010 | Kampala | Individuals living with HIV | 482 | 34.60±8.51 | PHQ-9 –(10) | 40 (8.3) | |
| Wagner 2014a [89] | Cohort (9) | 2008–2011 | Jinja, Kampala, Mityana, and Mukono | 3 study cohorts of Individuals living with HIV | 750 | 435 (315) | 34.5 | PHQ-9 –(10) | 45 (6) |
| Wagner 2017a [90] | Cohort (9) | 2008–2011 | Kampala, Mityana, Mukono, and Wakiso | Individuals living with HIV | 1021 | 653 (368) | 36 | PHQ-9 –(10) | 92 (9) |
| Wang 2018 [91] | CS (6) | 2009 | Wakiso | Individuals living with HIV | 981 | Self-report to a question, “During the last 12 months, have you had a period lasting several days when you felt sad, empty, or depressed?” | 221 (22.5) | ||
| Ager 2012 [92] | CS (9) | 2009 | Amuru, Gulu | National Humanitarian Aid Workers | 376 | 134 (238) | 30.88±6.60 | DHSCL–(>1.75) | 256 (68) |
| Wagner 2011 [93] | CS (9) | Jinja, Kampala | New HIV clients attending the clinics | 602 | 410 (192) | 36; Range = 20–62 | PHQ-9 –(10) | 78 (13) | |
| Ngo 2015 [34] | Cohort (9) | 2009–2011 | Mityana, Mukono, and Wakiso | Individuals living with HIV | 1903 | 1492 (411) | 36±9 | PHQ-9–10 and MINI | 1604 (84.3) |
| Kinyanda 2011a [94] | CS (9) | 2010 | Wakiso | Individuals living with HIV | 618 | 449 (169) | 18-24yrs = 58; 25–34 = 238; 35–44 = 217; and >44 = 103 | MINI | 50 (8.1) |
| Kinyanda 2012 [95] | CS (9) | 2010 | Wakiso | Individuals living with HIV | 618 | 449 (169) | 18-24yrs = 58; 25–34 = 238; 35–44 = 217; and >44 = 103 | MINI | 50 (8.1) |
| Morof 2014 [35] | CS (9) | 2010 | Kampala | female urban refugees | 117 | 117 (0) | 31.6±4.7 | DHSCL–(>1.75) and DHSCL–(>2.65) | 112 (92) and 70 (54) |
| Nakku 2013 [96] | CS (9) | 2010 | Wakiso | Individuals living with HIV | 618 | 449 (169) | 18-24yrs = 58; 25–34 = 238; 35–44 = 217; and >44 = 103 | MINI | 50 (8.1) |
| Kakyo 2012 [97] | CS (9) | Kabarole | Postpartum mothers | 202 | 202 (0) | 24±4.33 | Edinburgh postpartum depression scale (EPDS)–(10) | 87 (43) | |
| Wagner 2012b [98] | Cohort (9) | 2010–2011 | Kampala, Mityana, and Mukono | Individuals living with HIV | 798 | 530 (268) | 36.1±9.5 | MINI and PHQ-9 –(10) | 111 (13.9) and 187 (.23.43) |
| Wagner 2014b [99] | Cohort (9) | 2010–2011 | Jinja, Kampala | Individuals living with HIV | 1731 | 1131 (600) | 36 | PHQ-9 –(10) | 156 (9) |
| Kiene 2018 [100] | Cohort (9) | 2010–2011 | Butambala | HIV positive and HIV negative clients | 244 | 122 (122) | HIV positive = 34.60±9. 03; HIV negative = 33.28±10.12 | DHSCL–(>1.75) | 117 (48.0) |
| Okello 2015 [101] | Cohort (9) | 2010–2011 | Kampala | Individuals living with HIV | 798 | 530 (268) | 36.1± 9.53 | PHQ-9 –(10) | 100 (12.5) |
| Musisi 2014 [102] | Cohort (9) | 2010–2011 | Mukono, Wakiso, Kampala, and Mityana | Individuals living with HIV | 386 | 225 (161) | 35.7±8.7 | PHQ-9 –(10) | 116 (0.3) |
| Akena 2012 [103] | CS (9) | 2011 | Kampala | Individuals living with HIV | 368 | 265 (103) | 38.8±9.81; range = 18–71. | MINI | 64 (17.4) |
| Akena 2013 [104] | CS (9) | 2011 | Kampala | Individuals living with HIV | 735 | 525 (210) | 38±10.08, range = 18–71 | MINI | 72 (9.8) |
| Nakimuli-Mpungu 2011a [105] | CS (9) | 2011 | Mubende | Individuals living with HIV | 500 | 349 (151) | 40±10.7, range: = 18–80 | MINI | 230 (46) |
| Katende 2017 [106] | CS (7) | Kampala | Caregivers of cancer patients | 119 | 79 (40) | 33±10.69 | Hospital Anxiety and Depression Scale (HADS) standardized tool | ||
| Kinyanda 2013 [107] | CS (9) | Gulu, Kaberamaido, Lira, and Tororo | Children and adolescent | 1587 | 853 (734) | ≤5 = 286; 6–9 = 416; 10–13 = 550; 14–19 = 335 | MINI-KID | 136 (8.6) | |
| Spittal 2018 [108] | Cohort (9) | 2011–2012 | Amuru, Gulu, Nwoya | War victims—The Cango Lyec (Healing the Elephant) Project members 13 to 49 years who were sexually active | 2008 | 1189 (819) | Range 13–49 | DHSCL–(>1.75) | 337 (16.78) |
| Whyte 2015 [109] | CS (5) | 2011–2012 | Agago, Amuru, Gulu, and Nwoya | OPD patients in several districts in northern Uganda | 11325 | Clinician diagnosis | 40 (0.4) | ||
| Perkins 2018 [110] | CS (9) | 2011–2012 | Mbarara | General populations | 1499 | 822 (677) | below 30 = 640 | DHSCL–(>1.75) | 268 (17.88) |
| Malamba 2016 [111] | Cohort (9) | 2011–2012 | Gulu, Nwoya, and Amuru | War victims—The Cango Lyec (Healing the Elephant) Project members 13 to 49 years | 2388 | 1397 (991) | Range 13–49 | DHSCL–(>1.75) | 360 (14.9) |
| Hakim 2019 [112] | CS (9) | 2011–2013 | Kampala, Wakiso | All clients aged 13 or older attending Mildmay for client-initiated HIV testing and counseling | counseling | 6998 (5234) | 13–19 = 95; 20–24 = 2607; 25–34 = 5151; 35–49 = 3010; 50+ = 510 | PHQ-2 –(4) | 1884 (15.4) |
| Familiar 2019 [113] | Cohort (9) | 2011–2014 | Soroti | HIV-positive women attending a clinic | 288 | 288 (0) | 33.5; Range = 18–54 | DHSCL–(>1.75) | 139 (61) |
| Cavazos‑Rehg 2020 [114] | RCT (9) | 2012–2017 | Mbarara | HIV positive adolescents | 592 | 335 (257) | 12.13±0.65 | CDI | 298 (52.29) |
| Akena 2015 [115] | CS (9) | 2013 | Gulu, Kampala, and Mbarara | Patients with diabetes Mellitus | 437 | 283 (154) | 51±14.06, Range = 18–90 | MINI | 154 (34.8) |
| Familiar 2021 [116] | CS (9) | 2013 | Kampala | Self-settled Democratic Republic of Congo female refugees in Kampala | 580 | 580 (0) | Mean = 33.7. 18–24 = 121; 25–34 = 210; 35+ = 249 | PHQ-2 | 331 (57) |
| Akena 2016 [117] | Cohort (9) | 2013 | Luweero, Mityana, and Mpigi, Wakiso | Individuals living with HIV | 1252 | 961 (291) | 40±11. Range = 18–85 | PHQ-9 –(10) | 200 (67) |
| Rathod 2018 [118] | CS (9) | 2013 | Kamuli | General populations | 1893 | 1500 (393) | Median = 28; IQR = 15 | PHQ-9 –(10) | 80 (4.2) |
| Mugisha 2016 [28] | CS (9) | 2013 | Amuru, Gulu, and Nwoya | Individuals in post-conflict northern Uganda | 2361 | 1475 (886) | 49% of respondents were aged above 34 years | MINI | 599 (24.9) |
| Mugisha 2015 [29] | CS (9) | 2013 | Amuru, Gulu, and Nwoya | Community in the post-conflict northern Uganda | 2361 | 1475 (886) | 49% of respondents were aged above 34 years | MINI | 599 (24.7) |
| Mwesiga 2015 [119] | CS (9) | 2013 | Kampala | Individuals living with HIV | 345 | 245 (100) | Median = 35; (IQR = 12) | MINI | 17 (5) |
| Nakku 2019 [120] | CS (9) | 2013 | Kamuli | General populations | 1290 | 867 (423) | 16–30 = 494; 31–49 = 555; ≥ 50 = 240 | PHQ-9 –(10) | 325 (25.4) |
| Nalwadda 2018 [121] | CS (9) | 2013 | Kamuli | The male population in the region | 1129 | 0 (1129) | 33% of participants were below 30 years | PHQ-9 –(10) | 292 (25.9) |
| Jones 2017 [122] | Cohort (7) | 2013 | Kampala | Post-tuberculosis lung disease patients | 29 | 14 (15) | 45±13; Range = 17–69 | PHQ-9 –(5) | 7 (24) |
| Wagner 2017b [123] | Cohort (9) | 2013 | Luweero, Mityana, Mpigi, Wakiso | Individuals living with HIV | 1252 | 976 (276) | 39.8±11.2 | PHQ-9 –(10) | 375 (30) |
| Rukundo 2013 [124] | CS (9) | Mbarara | Physically ill patients | 258 | 120 (138) | 18–24 = 50, 25–40 = 130, 41–60 = 52 | MINI | 87 (33.7) | |
| Olema 2014 [125] | CS (9) | Gulu | Adolescents and their parents in GULU | 300 | DHSCL–(>1.75) | 120 (40) | |||
| Huang 2017 [126] | CS (9) | 2013–2014 | Parents of children in primary school | 303 | 248 (55) | 35.92±9.80; Range = 18–79 | PHQ-9 –(10) | 85 (28) | |
| Wagner 2016a [127] | Cohort (9) | 2013–2014 | Luweero, Mityana, Mpigi, and Wakiso | Individuals living with HIV | 1252 | 962 (290) | 40±11.2 | PHQ-9 –(10) | 375 (30) |
| Wagner 2016b [128] | Cohort (9) | 2013–2014 | Luweero, Mityana, Mpigi, and Wakiso | Individuals living with HIV | 1252 | 962 (290) | 40±11.2 | PHQ-9 –(10) | 375 (30) |
| Henry 2019 [129] | CS (7) | 2013–2015 | Kampala | Adolescents attending an adolescent health clinic | 514 | 372 (142) | 16; Range = 10–19 | Investigator designed tool (not standard) | 174 (33.9) |
| Meffert 2019 [15] | Cohort (9) | 2013–2017 | Individuals living with HIV | 475 | 282 (157) | 18–33 = 146; 34–48 = 227; 49–63 = 69; 65+ = 5 | CES-D | 104 (22) | |
| Swahn 2021 [130] | Cohort (9) | 2014 | Kampala | Individuals living with HIV—comparing HIV positive and non-HIV positive youth (12–18 years) | 1096 | 614 (481) | 12–14 = 219; 15–16 = 291; 17–18 = 586 | Self-report—“In the past year, did you ever feel so sad or hopeless almost every day for two weeks or more in a row that you stopped doing your usual activities?” | 673 (62) |
| Gyagenda 2015 [131] | CS (9) | 2014 | Kampala | Post-stroke patients | 73 | 43 (30) | 20–39 = 6; 40–59 = 25; 60–79 = 35; and 80–99 = 7 | PHQ-9 –(10) | 23 (31.5) |
| Fisher 2019 [31] | CS (6) | 2014 | Kisiro | Women attending OPD | 115 | 115 | SRQ-20 | 87 (75.65) | |
| Kinyanda 2020 [132] | CS (9) | 2014 | Kampala, Masaka | caregivers of patients with HIV | 1336 | Child and Adolescent Symptom Inventory-5 (CASI-5) | Baseline = 66 (5.0); 6month = 47 (4.2); 12months = 43 (4.4) | ||
| Muhammad 2018 [133] | CS (6) | 2014 | Kabarole | Individuals living with HIV | 150 | 84 (66) | 16.53±5.24 | - | 37 (47) |
| Nakku 2016 [21] | CS (9) | 2014 | Kamuli | Patients attending a health facility | 1415 | 1017 (398) | 33±13 | PHQ-9 –(8) | 140 (10) |
| Ashaba 2015 [134] | Case-control (9) | 2014 | Mbarara | Mother of malnourished children | 172 | 172 (0) | 25±4.43; Range = 18–40 | MINI | 46 (26.7) |
| Kinyanda 2016a [135] | CS (9) | Amuria, Katakwi | Post-conflict communities | 1110 | 631 (479) | 56% were aged between 18 to 44 years. | DHSCL–(>1.75) | 462 (41.6) | |
| Manne-Goehler 2019 [136] | Cohort (9) | Mbarara | Older individuals (above 40 years) living with HIV and HIV uninfected individuals of similar sex | 296 | 141 (155) | 52 | DHSCL–(>1.75) | 81 (27.36) | |
| Kinyanda 2016b [137] | CS (9) | Caregivers of patients with mental illness | 468 | 292 (176) | All above 50 | MINI | 43 (9.19) | ||
| Smith 2019 [138] | CS (9) | 2014–2015 | Mbarara | General populations | 1620 | 869 (751) | DHSCL–(>1.75) | 460 (28.39) | |
| Akimana 2019 [17] | CS (9) | 2015 | Kampala` | Children and adolescents with cancer | 352 | 112 (240) | 11.5±3.2; Range = 7–17 | MINI-KID | 91 (26) |
| Nampijja 2019 [139] | CS (9) | 2015 | Kampala | Postpartum women in Nsambya hospital | 300 | 300 (0) | 28±4.8; Range = 17–44 | MINI | 4 (1.3) |
| Cooper-Vince 2018 [140] | CS (9) | 2015 | Mbarara | Community-based study | 1603 | 898 (705) | DHSCL–(>1.75) | 461 (28.76) | |
| Kiene 2017 [141] | CS (8) | Individuals living with HIV | 325 | 165 (160) | Men = 34.93±10.59; Women = 32.21±8.93 | DHSCL–(>1.75) | 63 (19.4) | ||
| Kinyanda 2017b [142] | CS (9) | Masaka, Wakiso | Individuals living with HIV | 899 | 705 (194) | MINI | 126 (14.0) | ||
| Sohail 2019 [143] | CS (9) | 2015–2017 | Rakai | Rakai HIV community cohort | 333 | 160 (170) | 37± 9 | CES-D | 28 (8.4) |
| Raggio 2019 [144] | CS (8) | 2016 | Mbarara | Pregnant and non-pregnant women | 225 | 225 (0) | Median = 27; IQR = 9 | EPDS–(10) and DHSCL–(>1.75) | 26 (11.56) and 60 (26.67) |
| Kinyanda 2017a [145] | Cohort (9) | Masaka, Wakiso | Individuals living with HIV | 1099 | 847 (252) | 35.1± 9.3 | MINI | 155 (14.1) | |
| Akinbo 2016 [146] | CS (5) | Bushenyi | Alcoholic youth | 204 | 71 (133) | 30.6% were 15–19 years old | Researchers designed questionnaire | 4 (2) | |
| Cooper-Vince 2017 [147] | CS (9) | Mbarara | Female household head | 257 | 257 (0) | 33.5±7.9 | DHSCL–(>1.75) | 133 (44) | |
| Ashaba 2021 [148] | CS (9) | 2016–2017 | Mbarara | HIV positive adolescents | 224 | 131 (93) | 14.8±1.4. | MINI-KID | 37 (16) |
| Ashaba 2018 [149] | CS (9) | 2016–2017 | Mbarara | HIV positive adolescents | 224 | 131 (93) | 14.8±1.4. | MINI-KID | 37 (16) |
| Ortblad 2020 [150] | Prospective studies (9) | 2016–2019 | Kampala | Individuals living with HIV | 960 | Median = 28, IQR = 8 | PHQ-9 | 416 (43.2) | |
| Satinsky 2021 [151] | CS (9) | 2016–2018 | Mbarara | General populations | 1626 | 908 (718) | 17–26 = 409; 27–39 = 488; 40+ = 705 | DHSCL–(>1.75) and DSM V | 331 (20.36) and 159 (9.78) |
| Alinaitwe 2021 [152] | CS (9) | 2017 | Kampala | TB patients | 308 | 112 (188) | 36±10.8 | MINI | 73 (23.7) |
| Bapolisi 2020 [153] | CS (9) | 2017 | Isingiro | Refugees in Nakivale refugee camp | 387 | 219 (168) | 33.01±12.2 | MINI | 224 (58) |
| Forry 2019 [154] | CS (9) | 2017 | Mbarara | Prison inmates in Mbarara Municipality | 414 | 25 (389) | Aged 22–35 years (60%) | MINI | 182 (44) |
| Seffren 2018 [155] | Cohort (9) | Busia, Tororo | caregivers of HIV patients | 288 | 288 (0) | 33.5±5.8 | DHSCL–(>1.75) | 28 (9.7) | |
| Kuteesa 2020 [156] | CS (9) | 2017 | Mukono | 15–24 years individuals in a fishing community | 1281 | 606 (675) | Range = 15–24 | PHQ-9 –(10) | 29 (2) |
| Mubangizi 2020 [54]–Preprint | CS (9) | 2017–2018 | Kampala | Adults with sickle cell disease at Mulago Sickle cell clinic | 255 | 161 (94) | Median = 21, IQR = 6 | SRQ-25 –(>5) | 174 (68.2) |
| Nabunya 2020 [157] | Longitudinal cluster randomized study (9) | 2017–2022 (baseline) | Five districts in southwestern Uganda | Adolescent girls in southern Uganda | 1260 | 1260 (0) | 15.4±; Range = 14–15 | BDI–(21) | 580 (46.03) |
| Arach 2020 [158] | CS (9) | 2018 | Lira | Postpartum women | 1789 | 1789 (0) | 25±7; Range = 12–47 | EPDS–(14) | 377 (21.1) |
| Logie 2020 [159] | CS (9) | 2018 | Kampala | Refugee and displaced youth aged 16–24 living in five informal settlements in Kampala | 445 | 333 (112) | PHQ-9 –(10) | 297 (66.7) | |
| Ssewanyana 2021 [32] | CS (7) | 2018 | Kampala | Patients with stomas | 15 | 11 (3) | Range = 18–60 | PHQ-9 –(5) | 13 (88) |
| Musinguzi 2018 [160] | CS (9) | Masaka, Wakiso | Peri-urban Individuals living with HIV of Masaka and Entebbe | 201 | 160 (41) | 18–29 = 67; 30–34 = 39; 35–39 = 26; 40–49 = 48; 50+ = 21 | MINI | 62 (30.8) | |
| Muliira 2019 [161] | CS (9) | Kampala | Caregivers of cancer patients | 284 | 208 (76) | 36±13.8 | HADS–(8) | 137 (48.2) | |
| Lukenge 2019 [52]–Thesis | CS (9) | 2018–2019 | Kampala | Women attending infertility clinic | 377 | 377 (0) | PHQ-9 –(10) | 167 (44.3) | |
| Misghinna 2020 [162] | CS (9) | 2018–2019 | Kampala | Refugees | 374 | 218 (156) | 37.1±12.1 | MINI | 174 (46.52) |
| Bahati 2021 [36]–Preprint | CS (5) | 2019 | Mbarara | Urban refugees in Mbarara municipality | 343 | 145 (198) | 28.8±11.0 | PHQ-9 –(10) | 329 (96) |
| Boduszek 2021 [163] | CS (9) | 2019 | Primary and secondary school students aged 9–17 years | 11518 | 6035 (5483) | 14±1.95 | The 14-item Patient-Reported Outcomes Measurement Information System (PROMIS) Depression Short Form–(31) | 1224 (10.62) | |
| Kabunga 2020 [37] | CS (6) | 2019 | Isingiro | Refugees in Nakivale camp | 146 | 76 (70) | 18–30 = 26; 31–44 = 42; 44–59 = 45; and 60+ = 27 | PHQ-9 –(10) | 119 (81) |
| Kyohangirwe 2020 [164] | CS (9) | 2019 | Kampala | Adolescents | 281 | 176 (105) | 10–13 = 101; 14–17 = 180 | MINI-KID | 51 (18.2) |
| Olum 2020 [165] | CS (9) | 2019 | Kampala | Medical students at Makerere University | 331 | 133 (196) | 23.1±3.3 | PHQ-9 –(10) | 71 (21.5) |
| Mootz 2019 [166] | CS (9) | Amuria, Katakwi, and Kumi | Girls and women war victims | 605 | 605 (0) | DHSCL–(30) | 181 (30) | ||
| Ssebunnya 2019 [167] | CS (9) | Kamuli | General populations | 1290 | 848 (442) | <25 = 281; 25–34 = 367; 35–44 = 302; >44 = 337 | PHQ-9 –(10) | 82 (6.4) | |
| Kabunga 2021a [168] | CS (5) | 2020 | Isingiro | Refugees in Nakivale camp | 146 | 77 (69) | Majority of respondents 31.5% (n = 46) were aged between 44 and 59 | PHQ-9 –(10) | 66 (45.2) |
| Bongomin 2021 [33] | CS (9) | 2020 | Kampala | Patients with rheumatoid arthritis | 48 | 44 (4) | Median = 52; IQR = 17 | EQ-5D-5L anxiety/depression dimension | 34 (70.8) |
| Kabunga 2021b [169] | CS (9) | 2020 | Lira | Out-of-school adolescents | 164 | 87 (77) | 10–13 = 13; 14–16 = 48; 17–19 = 103 | PHQ-9 –(10) | 55 (34) |
| Kizito 2020 [53]–Thesis | Cohort (9) | 2020 | Masaka | Postpartum mothers | 167 | 167 (0) | The majority were between 25–29 | EPDS | 58 (34.7) |
| Ouma 2021 [170] | CS (9) | 2020 | Gulu | Female sex workers | 300 | 300 (0) | 26.4±6.0 | MINI | 143 (47.7) |
| Najjuka 2020 [14] | CS (9) | 2020 | University students | 321 | 123 (198) | 24.8±5.1 | Depression Anxiety and Stress Scale (DASS-21) | 259 (80.7) | |
| Mahmud 2021 [171] | Cohort (9) | 2020 | Kyenjojo | General population | 1075 | PHQ-9 –(10) | 150 (14) | ||
| Nyundo 2020 [6] | CS (9) | Iganga, Mayuge | Adolescents (10–19) | 598 | 286 (312) | 14.2±2.6 | the 6-Item Kutcher Adolescent Depression Scale (KADS-6) | 158 (26.5) | |
| Kaggwa 2021 [16] | CS (9) | 2021 | Isingiro | Married/cohabiting women | 153 | 153 (0) | 33.3±6.7. | PHQ-9 –(10) | 100 (65.4) |
Note: Table studies have been sorted according to the year of data collection. In those studies without the year of data collection, the year of submission to the journal was used to estimate the year of data collection. CS = Cross-sectional; DHSCL = Depression sub-section of the Hopkins Symptom Checklist; PHQ = Patient Health Questionnaire (PHQ); MINI = Mini-International Neuropsychiatric Interview; MINI-KID = Mini-International Neuropsychiatric Interview for Children and Adolescents; SRQ = Self-Reporting Questionnaire; CES-D = Center for Epidemiological Studies Depression Scale; EPDS = Edinburgh Postpartum Depression Scale; BDI = Beck Depression Inventory; CDI = Children Depression Inventory; HADS = Hospital Anxiety and Depression Scale; DSM = Diagnostic and Statistical Manual of Mental Disorders; CASI-5 = Child and Adolescent Symptom Inventory-5; DASS-21 = 21-item Depression Anxiety and Stress Scale; EQ-5D-5L = European Quality of Life Five Dimension-Five Level anxiety/depression dimension; KADS-6 = Kutcher Adolescent Depression Scale; PROMIS = Patient-Reported Outcomes Measurement Information System Depression Short Form
Ethical considerations
The present study was a secondary analysis of previously published literature. Therefore, formal clearance by a Research and Ethics Committee was not required.
Data synthesis and analysis
Data for this analysis are available at figshare [46]. Microsoft Office 2016 (Microsoft Inc., Washington, USA) and STATA 16.0 software (Stata Corp LLC, College Station, Texas, USA) were used for data cleaning and statistical analysis. Descriptive statistics and qualitative narrative analysis were used to present individual study and participant characteristics. A random-effects meta-analysis [47] was performed using the meta command to determine the pooled prevalence of depression and prevalence of depression in the different study groups. The results were presented on forest plots. The Higgins Inconsistency index (I2) and univariate random effect meta-regression [48] were used to evaluate the heterogeneity among the selected studies. Publication bias was assessed visually using funnel plots symmetry [49], and fill and trim estimated the number of missing studies [50]. Egger’s test was also used to assess for small study effects. Univariate meta-regression was used to determine the source of heterogeneity based on the following: mean age, number per gender (males or females), data collection period (pre-COVID-19 pandemic vs. during the pandemic), study design, JBI Checklist score, sample size, and depression assessment tool used. Subgroup analysis was also conducted based on study types, study tools used, the diagnostic status of the tool, and the data collection period.
Results
A total of 136 papers met the criteria for inclusion in the review (comprising three theses [51–53], two preprints [36, 54], and 131 peer-reviewed journal papers). Using Microsoft Excel 2016, duplicate papers were automatically identified [including republished datasets in different papers] (n = 9) based on year of data collection, type of study, district of study, sample size, study population, the prevalence of depression, and assessment tool used for depression. The remaining 127 papers, comprising a total of 123,859 individuals, comprised the total study sample (Table 1).
The identified papers were published between 2004 and 2021, and the data included were collected between 2000 and 2021 from 45 districts in Uganda.
Most of the studies were conducted in the capital city, Kampala (n = 43), followed by the districts of Mbarara (n = 23) and Gulu (n = 16). The pooled mean age of the participants was 27.19 years (95% CI: 24.31–30.09 years; I2 = 85.38, p<0.001). A total of eight studies were conducted during the COVID-19 pandemic [6, 14, 16, 33, 53, 168–171].
Tools used in assessing depression
Both diagnostic and screening tools were used to assess depression among different populations in Uganda (Table 1). The tools used included: (i) Depression sub-section of the Hopkins Symptom Checklist (DHSCL) (n = 34, 26.8%) [35, 55, 61, 63, 65–68, 71, 73, 74, 79–82, 84, 92, 100, 108, 110, 111, 113, 125, 135, 136, 138, 140, 141, 144, 147, 151, 155, 166], (ii) Patient Health Questionnaire (PHQ) (n = 33, 26.0%) [16, 21, 32, 34, 36, 37, 52, 86, 88–90, 93, 98, 99, 101, 102, 112, 116–118, 120–123, 126–128, 131, 150, 156, 159, 165, 167–169, 171], (iii) Mini-International Neuropsychiatric Interview (MINI) (n = 24, 18.9%) [28, 29, 34, 59, 69, 70, 78, 94–96, 98, 103–105, 115, 119, 124, 134, 137, 139, 142, 145, 152–154, 160, 162, 170], (iv) Mini-International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) (n = 6, 4.7%) [17, 58, 75–77, 107, 148, 149, 164], (v) Self-Reporting Questionnaire (SRQ) (n = 6, 4.7%) [31, 54, 57, 59, 83, 85] (vi) Center for Epidemiological Studies Depression Scale (CES-D) (n = 4, 3.1%) [15, 60, 72, 143], (vii) Edinburgh Postpartum Depression Scale (EPDS) (n = 4, 3.1%) [53, 97, 144, 158], (viii) Beck Depression Inventory (BDI) (n = 3, 2.4%) [56, 62, 157], (ix) Children Depression Inventory (CDI) (n = 2, 1.6%) [58, 114], (x) Hospital Anxiety and Depression Scale (HADS) standardized tool (n = 2, 1.6%) [106, 161], (xi) Diagnostic and Statistical Manual of Mental Disorders (DSM) (n = 2, 1.6%) [64, 151], (xii) Child and Adolescent Symptom Inventory-5 (CASI-5) (n = 1, 0.8%) [132], (xiii) European Quality of Life Five Dimension-Five Level (EQ-5D-5L) anxiety/depression dimension (n = 1, 0.8) [33], (xiv) the six-item Kutcher Adolescent Depression Scale (KADS-6) (n = 1, 0.8%) [6], (xv) the 14-item Patient-Reported Outcomes Measurement Information System (PROMIS) Depression Short Form (n = 1, 0.8%) [163], and (xvi) the Youth Self-Report (YSR) (n = 1) [51]. Two studies used a single self-report question to screen for depression [91, 130], and three studies developed their own tool to assess for depression [87, 129, 146]. One study used a clinician’s diagnosis of depression [109]. The DASS-21 was also used in one study [14]. Six studies used more than one tool to screen and/or diagnose depression [34, 58, 59, 98, 144, 151].
Prevalence of depression
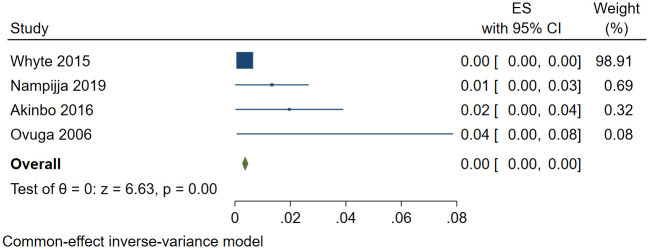
A total of 27,989 (out of 123,859) individuals screened positive for depression. The pooled prevalence of depression was 30.2% (95% confidence interval [CI]: 26.7%-34.1%; I2 = 99.80, p<0.001). The funnel plot was asymmetrical consistent with publication bias (S1 Fig). Despite the asymmetry, no studies were missing based on trim and fill analysis. The estimated slope from Egger’s test was 6.12 (standard error [SE] = 0.598, p<0.001), suggesting publication bias due to small study effects. A sensitivity analysis was performed using the four studies within the funnel [56, 109, 139, 146]. The pooled prevalence of depression was 0.9% (95% CI: 0.1%-1.7%; I2 = 37.82, p = 0.021) (Fig 2). In univariate meta-regression analysis (to explore potential sources of heterogeneity), depression increased with the use of DASS-21 or SRQ-20 assessment tools and studies conducted during the COVID-19 pandemic. However, depression decreased with increased sample size and the number of females in the study.
Fig 2. Forest plot showing the pooled prevalence of depression in Uganda following sensitivity analysis.
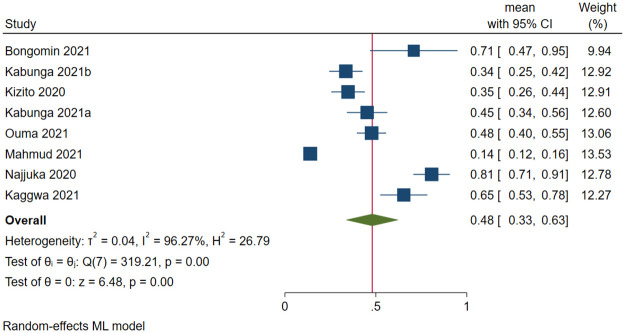
Due to the high heterogeneity, a subgroup analysis was performed. There were significant differences between the COVID-19 pandemic period (Q difference [QD] = 5.37, p<0.021), the assessment tool used for screening and/or diagnosing depression (QD = 2205.32, p<0.001), and the type of assessment tool used, i.e., diagnostic (DSM V, DSM VI, MINI, MINI-KID, and clinical diagnosis) or non-diagnostic (QD = 8.03, p = 0.005) (Table 2). The pooled prevalence of depression during the COVID-19 pandemic was higher than before the pandemic (48.1% vs. 29.3%). Fig 3 shows the forest plot of the prevalence of depression during the COVID-19 pandemic.
Table 2. Subgroup analysis of the prevalence of depression in Uganda.
| Categories | Subgroups | Number of studies | Pooled prevalence (95% CI) | Q | I2 | p-value | Group difference χ2 (p-value) |
|---|---|---|---|---|---|---|---|
| Pandemic | Pre-pandemic | 119 | 29.3 (25.5–33.0) | 23453.03 | 99.81 | <0.001 | 5.37 (0.021) |
| During the pandemic | 8 | 48.1 (32.6–63.6) | 319.21 | 96.74 | <0.001 | ||
| Type of Study | Cross-sectional | 92 | 31.3 (26.7–35.9) | 17035.98 | 99.84 | <0.001 | 1.06 (0.588) |
| Cohort | 32 | 29.0 (22.5–35.5) | 3616.12 | 99.43 | <0.001 | ||
| Case-control | 1 | 26.7 (19.0–34.5) | 0 | NA | NA | ||
| Tools used | BDI | 3 | 20.5 (2.9–38.1) | 256.48 | 98.75 | <0.001 | 2205.32 (<0.001) |
| CASI-5 | 1 | 4.9 (3.7–6.1) | 0 | NA | NA | ||
| CDI | 2 | 36.6 (5.9–67.3) | 83.04 | 98.80 | <0.001 | ||
| CES-D | 4 | 31.1 (11.8–50.4) | 225.02 | 98.60 | <0.001 | ||
| Clinician diagnosis | 1 | 0.4 (0.2–0.5) | 0 | NA | NA | ||
| DASS-21 | 1 | 80.7 (70.9–90.5) | 0 | NA | NA | ||
| DHSCL | 34 | 33.7 (27.3–45.4) | 2022.12 | 99.25 | <0.001 | ||
| DSM V | 1 | 9.8 (8.3–11.3) | 0 | NA | NA | ||
| DSM IV | 1 | 39.8 (31.8–47.7) | 0 | NA | NA | ||
| EPDS | 4 | 27.1 (13.4–40.8) | 49.28 | 96.62 | <0.001 | ||
| EQ-5D-5L | 1 | 70.8 (47.0–94.6) | 0 | NA | NA | ||
| HADS | 2 | 37.3 (15.5–59.0) | 12.66 | 92.10 | <0.001 | ||
| KADS-6 | 1 | 26.4 (22.3–30.5) | 0 | NA | NA | ||
| MINI | 24 | 24.9 (18.1–31.8) | 1296.48 | 99.16 | <0.001 | ||
| MINI-KID | 6 | 17.6 (7.7–27.4) | 253.96 | 98.93 | <0.001 | ||
| Study designed tool | 3 | 31.5 (-0.9–63.9) | 450.27 | 99.47 | <0.001 | ||
| PHQ-2 | 2 | 36.1 (-4.77.7) | 174.21 | 99.43 | <0.001 | ||
| PHQ-9 | 31 | 31.0 (21.9–40.1) | 3475.21 | 99.78 | <0.001 | ||
| PROMIS | 1 | 10.6 (10.0–11.2) | 0 | NA | NA | ||
| SRQ-20 | 2 | 59.4 (29.6–89.1) | 13.75 | 92.72 | <0.001 | ||
| SRQ-25 | 4 | 33.4 (6.7–60.1) | 154.00 | 98.20 | <0.001 | ||
| Self-report | 2 | 41.9 (3.8–80.0) | 191.34 | 99.48 | <0.001 | ||
| YSR | 1 | 20.9 (17.1–24.8) | 0 | NA | NA | ||
| Tool diagnostic | No | 94 | 33.2 (28.6–37.7) | 10489.46 | 99.68 | <0.001 | 8.03 (0.005) |
| Yes | 33 | 30.5 (26.7–34.2) | 3258.96 | 99.65 | <0.001 |
DHSCL = Depression sub-section of the Hopkins Symptom Checklist; PHQ = Patient Health Questionnaire (PHQ); MINI = Mini-International Neuropsychiatric Interview; MINI-KID = Mini-International Neuropsychiatric Interview for Children and Adolescents; SRQ = Self-Reporting Questionnaire; CES-D = Center for Epidemiological Studies Depression Scale; EPDS = Edinburgh Postpartum Depression Scale; BDI = Beck Depression Inventory; CDI = Children Depression Inventory; HADS = Hospital Anxiety and Depression Scale; DSM = Diagnostic and Statistical Manual of Mental Disorders; CASI-5 = Child and Adolescent Symptom Inventory-5; DASS-21 = 21-item Depression Anxiety and Stress Scale; EQ-5D-5L = European Quality of Life Five Dimension-Five Level anxiety/depression dimension; KADS-6 = Kutcher Adolescent Depression Scale; PROMIS = Patient-Reported Outcomes Measurement Information System Depression Short Form
Fig 3. Forest plot on the prevalence of depression during the COVID-19 pandemic.
Prevalence of depression in different study populations in Uganda
Depression was screened or diagnosed in the following study groups in Uganda: (i) individuals living with HIV (n = 43) [15, 34, 60, 64, 68, 70–73, 79, 81, 82, 85–91, 93–96, 98–105, 112–114, 117, 119, 123, 127, 128, 130, 132, 133, 136, 141–143, 145, 148–150, 160], (ii) females only (n = 25) [16, 31, 35, 52, 59, 73, 79, 97, 113, 116, 134, 139, 144, 158, 166, 170], including seven studies among pregnant or postpartum women [53, 59, 73, 97, 139, 144, 158], (iii) general population (n = 19) [55, 61–63, 78, 92, 110, 118, 120, 125, 140, 146, 151, 156, 167, 171], (iv) war victims (n = 12) [28, 29, 66, 67, 74–77, 80, 83, 84, 108, 111, 135, 166], (v) special patient groups (such as elderly, outpatients, diabetes mellitus, post-tuberculosis lung diseases, physically ill, post-stroke, cancer, tuberculosis patients, sickle cell disease, patients with stoma, rheumatoid arthritis) (n = 12) [17, 21, 31–33, 54, 57, 109, 115, 122, 124, 131, 152], (vi) children and adolescents (n = 10) [6, 17, 51, 58, 75–77, 84, 85, 107, 114, 129, 146, 157, 163, 164, 169], (vii) refugees (n = 8) [35–37, 116, 153, 159, 162, 168], (viii) caregivers of patients (n = 6) [106, 132, 134, 137, 155, 161], (ix) university students (n = 4) [14, 56, 65, 165], (x) prisoners (n = 1) [154], and males only (n = 1) [121] (S1 Table). The pooled prevalence of depression across the different study groups was highest among refugees (67.6%) and lowest among caregivers of patients (18.5%) (Fig 4).
Fig 4. Prevalence of depression in different study groups in Uganda.
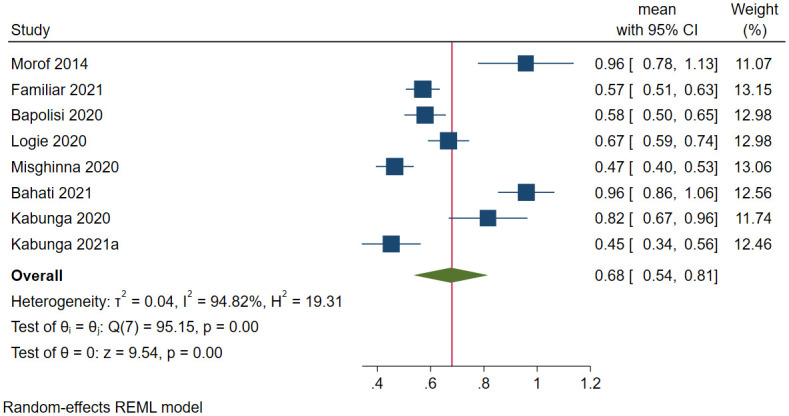
Depression among refugees in Uganda
A total of 2,538 refugees were assessed for depression in Uganda, and 1,652 screened positive for depression in eight studies. The prevalence of depression ranged between 45.2% [168] and 96% [36]. The pooled prevalence of depression was 67.6% (95 CI: 53.7%-81.5%; I2 = 94.82, p<0.001) (Fig 5). The estimated slope from Egger’s test was 6.67 (SE = 3.037, p<0.0281), suggesting publication bias due to small study effects. The funnel plot showed publication bias on visual inspection. A sensitivity analysis was performed using studies within the funnel [37, 159], and the pooled prevalence of depression was 72.7% (95 CI: 58.5%-87.0%; I2 = 67.51, p<0.001). Based on meta-regression, the prevalence decreased with the increase in mean age (β = -0.07, SE = 0.02, p<0.001). Other factors were not significant.
Fig 5. Forest plot on the prevalence of depression among refugees in Uganda.
Depression among studies involving only females in Uganda
A total of 4,222 out of 11476 females had depression in 25 female-only studies. The prevalence of depression ranged between 6.1% [59] and 92.0% [35]. The pooled prevalence of depression was 38.2% (95 CI: 29.0%-47.5%; I2 = 99.16, p<0.001) (Fig 6). The funnel plot showed asymmetrical distribution, therefore showing publication bias. The estimated slope from Egger’s test was 8.65 (SE = 0.1.428, p<0.001), suggesting publication bias due to small study effects. Following meta-regression, no factor significantly affected the prevalence of depression among females in Uganda.
Fig 6. Forest plot on the prevalence of depression among females in Uganda.
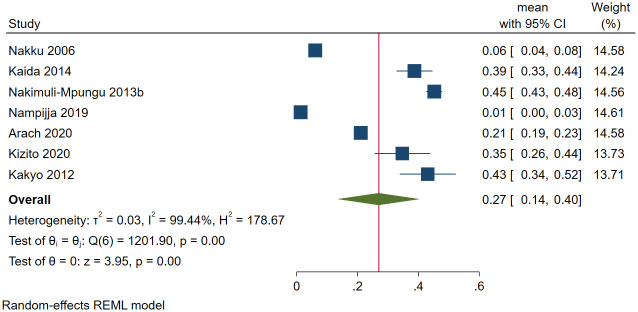
Depression among postpartum or pregnant women in Uganda
Out of the 6296 postpartum or pregnant women in Uganda, 2028 had depression in seven studies. The prevalence of depression ranged between 1.3% [139] and 45.2% [83]. The pooled prevalence of depression among postpartum or pregnant women was 26.9% (95 CI: 13.6%-40.3%; I2 = 99.44, p<0.001) (Fig 7). The estimated slope from Egger’s test was 6.76 (SE = 3.694, p<0.067), suggesting no publication bias due to small study effects. Based on meta-regression, the prevalence of depression among postpartum women statistically significantly decreased with use of MINI (β = -0.35, SE = 0.11, p = 0.002) and increased when the study design was cohort (β = 0.22, SE = 0.11, p = 0.045).
Fig 7. Forest plot on the prevalence of depression among postpartum or pregnant females in Uganda.
Depression among special patient groups in Uganda
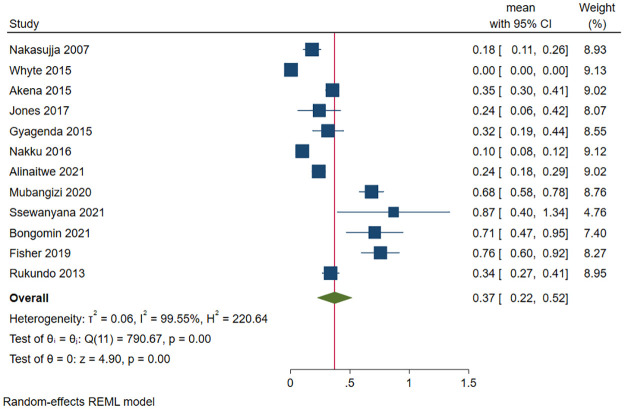
The prevalence of depression ranged from 0.4% among outpatients in northern Uganda [109] and 88% among patients with stomas [32]. The prevalence among those who (i) were elderly was 18% [57], (ii) had tuberculosis was 23.7% [152], (iii) had post-tuberculosis lung diseases was 24% [122], (iv) had cancer was 26% [17], (v) with post-stroke was 31.5% [131], (vi) were physically ill was 33.7% [124], (vii) had diabetes mellitus was 34.8% [115], (viii) had sickle cell disease was 68.2% [54], and (ix) had rheumatoid arthritis was 70.8% [33]. The pooled prevalence of depression from the 14,405 special patient groups (of whom 855 had depression) in 12 studies was 37.1% (95 CI: 22.3%-52.0%; I2 = 99.55, p<0.001) (Fig 8). The estimated slope from Egger’s test was 3.82 (SE = 1.124, p<0.001), suggesting publication bias due to small study effects. Due to the significant heterogeneity, a sensitivity analysis was performed with studies within the funnel, and [115, 122, 124, 131], the pooled prevalence of depression in these studies was 33.8% (95 CI: 29.8%-37.9%; I2 = 0.03, p<0.001). At meta-regression, the prevalence of depression among special patient groups statistically significantly increased with increase in the mean age (β = 0.01, SE = 0.004, p = 0.009) and use of SRQ-20 to assess depression (β = 0.75, SE = 0.30, p = 0.013).
Fig 8. Forest plot on the prevalence of depression among special patient groups in Uganda.
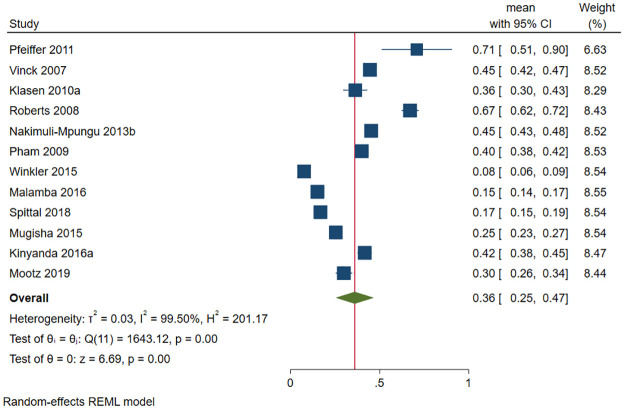
Depression among war victims in Uganda
A total of 6583 (out of 19255) war victims had depression in 12 studies. The prevalence of depression ranged between 7.6% [84] and 71% [67]. The pooled prevalence of depression was 36.0% (95 CI: 25.5%-46.6%; I2 = 99.50, p<0.001) (Fig 9). The estimated slope from Egger’s test was 5.24 (SE = 2.109, p = 0.013), suggesting publication bias due to small study effects. Only one study was within the funnel [75]. At meta-regression, no factor significantly affected the prevalence of depression among war victims in Uganda.
Fig 9. Forest plot on the prevalence of depression among war victims in Uganda.
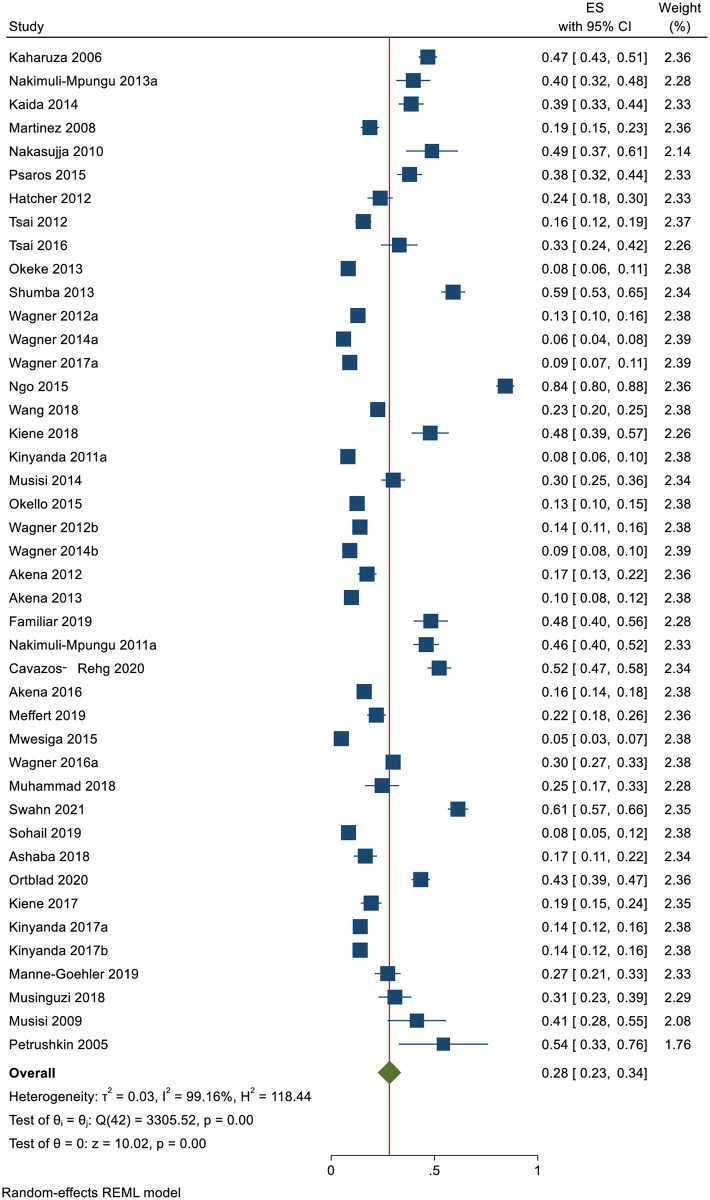
Depression among individuals living with HIV in Uganda
A total of 7704 (out of 26255) individuals living with HIV had depression in 43 studies. The prevalence of depression ranged between 5% [119] and 84% [34]. The pooled prevalence of depression was 28.2% (95 CI: 22.7%-33.7%; I2 = 99.16, p<0.001) (Fig 10).
Fig 10. Forest plot on the prevalence of depression among individuals living with HIV in Uganda.
The estimated slope from Egger’s test was 5.72 (SE = 0.1.406, p<0.001), suggesting publication bias due to small study effects. At meta-regression, no factor statistically significantly affected the prevalence of depression among HIV patients in Uganda.
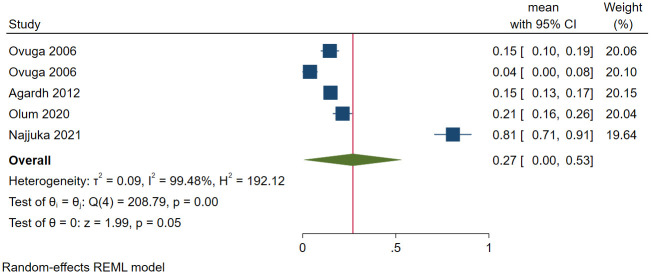
Depression among university students in Uganda
A total of 517 (out of 1982) university students had depression in five studies. The prevalence of depression ranged between 0.4% [56] and 80.7% [14]. The pooled prevalence of depression among university students was 26.9% (95 CI: 0.4%-53.4%; I2 = 99.48, p<0.001) (Fig 11). The estimated slope from Egger’s test was 19.85 (SE = 4.566, p<0.001), suggesting publication bias due to small study effects. The pooled prevalence from the studies within the funnel during sensitivity analysis was 14.9% (95 CI: 12.7%-17.0%; I2 = 0.04, p<0.001). The prevalence of depression among students was significantly higher when the DASS-21 was used to screen for depression (β = 0.71, SE = 0.10, p<0.001) and when the study was conducted during the COVID-19 pandemic (β = 0.67, SE = 0.09, p<0.001).
Fig 11. Forest plot on the prevalence of depression among university students in Uganda.
Depression among children and adolescents in Uganda
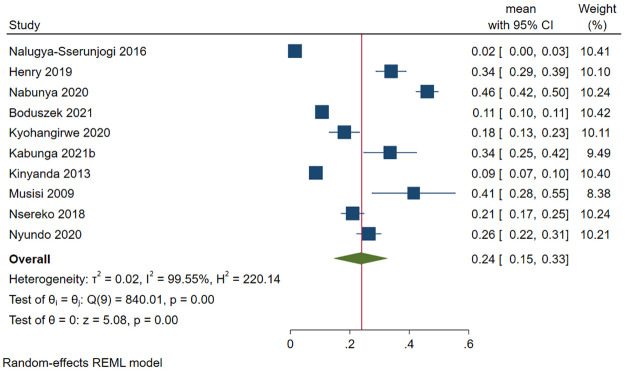
A total of 2535 (out of 17072) children and adolescents in Uganda screened positive for depression in 10 studies. The prevalence of depression among children and adolescents ranged from 2.9% [58] to 46.03% [157]. The pooled prevalence of depression among children and adolescents was 23.6% (95 CI: 14.5%-32.8%; I2 = 99.55, p<0.001) (Fig 12).
Fig 12. Forest plot on the prevalence of depression among children and adolescents in Uganda.
The estimated slope from Egger’s test was 5.27 (SE = 2.008, p = 0.009), suggesting publication bias due to small study effects. Only two studies were within the funnel [6, 51], and sensitivity analysis based on these studies had a pooled prevalence of 23.6% (95 CI: 18.3%-29.0%; I2 = 72.52, p<0.001). The prevalence of depression was significantly lower when the following assessment tools were used: (i) MINI-KID (β = -0.37, SE = 0.09, p<0.001), (ii) PROMIS (β = -0.35, SE = 0.11, p = 0.002), and (iii) YSR (β = -0.25, SE = 0.12, p = 0.032).
Depression among caregivers of patients in Uganda
Different types of caregivers were included in this review and they included caregivers for the following patients: individuals living with (i) HIV (n = 3) [112, 132, 155], cancer (n = 2) [106, 161], and (iii) mental health illness (n = 1) [137]. A total of 2189 (out of 14727) caregivers had depression. The pooled prevalence of depression was 18.5% (95 CI: 5.9%-31.2%; I2 = 99.62, p<0.001) (Fig 13). The estimated slope from Egger’s test was 6.88 (SE = 2.710, p<0.011), suggesting publication bias due to small study effects. Only one study was inside the funnel [106]. At meta-regression, no factor statistically significantly affected the prevalence of depression among caregivers of patients in Uganda.
Fig 13. Forest plot on the prevalence of depression among caregivers of selected patient groups in Uganda.
Depression among the general population
A total of 4,250 (out of 21,347) members of the general population screened positive for depression in 19 studies. The prevalence of depression ranged between 2.0% among individuals in a fishing community [156] and 68% among national humanitarian aid workers [92]. The pooled prevalence of depression was 20.8% (95 CI: 13.6%-27.9%; I2 = 99.61, p<0.001) (Fig 14). The estimated slope from Egger’s test was 10.91 (SE = 1.889, p<0.001), suggesting publication bias due to small study effects. At meta-regression, no factor statistically significantly affected the prevalence of depression among the general population in Uganda.
Fig 14. Forest plot on the prevalence of depression among the general population in Uganda.
Discussion
The present systematic review and meta-analysis pooling data of close to 124,000 Ugandans collected between 2000 and 2021 showed that approximately one in three individuals had depression. This finding is much higher than the global depression rate of 3.8% [2]. This large difference may be because the majority of the studies included in this review involved study populations that are at higher risk of developing depression, such as refugees, war victims, individuals living with HIV, and caregivers of patients, among others [172–175]. However, the prevalence of depression in Uganda was slightly higher than 27% from a previous systematic review and meta-analysis of the prevalence of depression among outpatients [13].
The prevalence of depression was also higher than previously obtained pooled prevalence rates of depression in Uganda (21.2% among adults and 20.2% among children for studies published between 2010 and 2018 [12]). Since all the previous review studies are included in this study, the difference between the pooled prevalence of depression between the present study and the previous reviews may be due to the effect of the COVID-19 pandemic that led to increased levels of depression [176]. This was clearly indicated by the subgroup analysis, which showed a higher difference between the pre-pandemic pooled prevalence of depression and that during the pandemic. The present systematic review had a different prevalence than the former studies because it included more studies which could have resulted in the pooled prevalence rate being closer to “the true value” of the prevalence of depression in Uganda.
The prevalence of depression in the different study groups was highest among refugees (67.6%) compared to other groups. This prevalence was over twice as high as a previously reported prevalence of depression among refugees and asylum seekers (31.5%) [172]. Uganda, the world’s fourth largest refugee hosting country, has been host to refugees from Congo, South Sudan, Rwanda, Burundi, Somalia, and Ethiopia, among other countries [25]. The high prevalence of depression may be due to refugees leaving their countries to come to a low-income country that is also affected by multiple health, social, and financial struggles, leaving many refugees with depression or worsening their psychological states [172]. The higher prevalence of depression among refugees compared to other studied groups may be because these refugees, on top of their struggles and settling into a new environment, are also affected by the challenges of the country to which other groups are used to.
Uganda has also been affected by civil wars, especially in the northern part of the country. The prevalence of depression among the war victims in Uganda (36.0%) was higher than the 27% global estimate from a systematic review and meta-analysis of war victims [173]. The psychological impact of civil war, refugees, and wars in the neighboring countries on the victims and the workers may be the high prevalence of depression among the national humanitarian workers compared to the rest of the general population.
Despite the declining prevalence of HIV among Ugandans [177], many individuals were affected by the mental and psychological impacts of HIV, such as depression [38, 178]. The prevalence of depression among individuals living with HIV in Uganda (28.2%) in the present study was lower than the global prevalence of 31% [179]. The lower prevalence may be attributed to the efforts made by many researchers to understand and reduce the burden of depression, as evidenced by the high number of studies regarding depression in the present review.
The prevalence was also lower than the previous prevalence of depression among Ugandans with HIV (30.88%) that involved studies published before 2018 [38]. This difference may be attributed to a few studies being included in the previous review (n = 10) [38]. In Uganda, depression among individuals living with HIV has been studied widely and has been assessed as various risk factors such as depression among caregivers of individuals living with HIV [112, 132, 155]. Based on the present review, caregivers of patients have less depression compared to the patients and other study groups. However, they play an integral role in patient care. The prevalence of depression among special groups of caregivers, such as cancer patient caregivers, was higher (42.3%) [180] compared to the pooled prevalence in the present review. This difference may be attributed to the Ugandan culture, where the caregiving role is shared among all family members and creates family support for the affected caregivers, helping prevent depression [161, 181, 182].
Being female was highly represented in the review, with a total of 25 studies being carried out among female-only studies compared to only one male-only study. This possibly shows neglect of male gender mental health by researchers. Future research should include more studies among males, so that true estimates of the burden of depression can be determined and evidence-based interventions can be designed. Depression among children and adolescents has also been studied more than studies of male adults. The prevalence of depression among children and adolescents (23.6%) was higher than 20.2% among children in Uganda for papers published between 2010 and 2018 [12].
Despite having no missing studies imputed into the overall prevalence, the heterogeneity was high. Following sensitivity analysis, the prevalence of depression in Uganda was 0.9%—a prevalence lower than the estimated global prevalence of 3.8% [2]. Based on the various analyses, the main sources of heterogeneity were (i) the COVID-19 pandemic, where the prevalence of depression was significantly higher than in the period before the pandemic as reported by various researchers and meta-analyses [176, 183]; and (ii) the tools used in screening/diagnosing depression with the DASS-21 detecting significantly higher prevalence rates of depression compared to other study tools. The significant difference may be due to the tool being used during the early stages of the COVID-19 pandemic [14] when many of the individuals were experiencing severe depression due to various stressors [176, 183]. The difference in the reported prevalence of depression could be due to various studies using different assessment tools with different psychometric properties regarding depression. Also, some tools were diagnostic, such as the DSM criteria, while others were screening tools, such as the DASS-21.
Limitations and recommendations
When interpreting these results, the following limitations need to be considered. First, despite only 16% of the 127 papers not having a total score of nine on the JBI Checklist and the use of random effect models, there were significantly high levels of heterogeneity due to the depression assessment tools and the period of study. Future researchers should conduct reviews of studies with fewer variations, especially in relation to the tools used to assess depression. However, for better quality and to increase reliability in future meta-analyses, future researchers should continue using the commonly used tools such as PHQ-9, DHSCL, and MINI. Also, the classification of the different study groups in the present study may have caused heterogeneity in the included studies, for example, among the general population. Second, some of the included studies were prone to recall biases since all their data were based on self-report. Third, despite data from various regions and districts in Uganda being presented, a large majority of the country was still not represented. This suggests more research regarding depression in other parts of this multicultural and multilingual country should be conducted and/or a nationally representative survey study [18]. Moreover, despite conducting a detailed literature search, some of the common databases (e.g., EMBASE, CINAHL) and journals that publish papers on mental health illness were not included. Therefore, some studies could have been missed. Also, the search strategy did not include some of the common terms associated with depression, such as mental health, psychological disorder/problem, and mood. It is recommended that future studies include sources for unpublished data to generalize the findings better.
While the meta-analysis was comprehensive and provided a broader picture of the prevalence of depression in various populations, it is still difficult to generalize the results because the prevalence of depression in Uganda in many regions was not represented, and different populations’ generalizations or groupings were subjective (e.g., humanitarian workers). Future studies within these populations and across wider regions in the country would be helpful in implementing treatments according to targeted needs (socioeconomic, cultural, refugee-status, etc.).
Conclusion
In the present meta-analysis, the synthesized data showed that approximately one in three individuals in Uganda has depression, which was highest among refugees and other special populations. Interventions for active screening, diagnosis, and management of depression among the general population and special populations and cohorts are recommended.
Supporting information
(TIF)
(TIF)
(DOCX)
Acknowledgments
We acknowledge the support and guidance provided by the Librarians at Mbarara University of Science and technology in developing the search strand strings and literature retrieval for the selected papers.
Data Availability
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, Dua T, et al. Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edition. The Lancet. 2016;387(10028):1672–85. doi: 10.1016/s0140-6736(15)00390-6 [DOI] [PubMed] [Google Scholar]
- 2.World Health Organisation. Depression 2021 [cited 2021 Novemeber 29, 2021]. https://www.who.int/health-topics/depression#tab=tab_1.
- 3.Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet. 2021;398(10312):1700–12. doi: 10.1016/S0140-6736(21)02143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sankoh O, Sevalie S, Weston M. Mental health in Africa. The Lancet Global Health. 2018;6(9):e954–e5. doi: 10.1016/S2214-109X(18)30303-6 [DOI] [PubMed] [Google Scholar]
- 5.Jörns-Presentati A, Napp A-K, Dessauvagie AS, Stein DJ, Jonker D, Breet E, et al. The prevalence of mental health problems in sub-Saharan adolescents: A systematic review. PloS One. 2021;16(5):e0251689. doi: 10.1371/journal.pone.0251689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nyundo A, Manu A, Regan M, Ismail A, Chukwu A, Dessie Y, et al. Factors associated with depressive symptoms and suicidal ideation and behaviours amongst sub-Saharan African adolescents aged 10–19 years: Cross-sectional study. Tropical Medicine & International Health. 2020;25(1):54–69. doi: 10.1111/tmi.13336 [DOI] [PubMed] [Google Scholar]
- 7.Kaggwa MM, Arinaitwe I, Nduhuura E, Muwanguzi M, Kajjimu J, Kule M, et al. Prevalence and factors associated with depression and suicidal ideation during the COVID-19 pandemic among university students in Uganda: A cross-sectional study. Frontiers in Psychiatry. 2022;13:842466. doi: 10.3389/fpsyt.2022.842466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaggwa MM, Muwanguzi M, Nduhuura E, Kajjimu J, Arinaitwe I, Kule M, et al. Suicide among Ugandan university students: Evidence from media reports for 2010–2020. BJPsych International. 2021;18(3):63–7. doi: 10.1192/bji.2021.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaggwa MM, Rukundo GZ, Wakida EK, Maling S, Sserumaga BM, Atim LM, et al. Suicide and suicide attempts among patients attending primary health care facilities in Uganda: A medical records review. Risk Management and Healthcare Policy. 2022;15:703–11. doi: 10.2147/RMHP.S358187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaggwa MM, Arinaitwe I, Muwanguzi M, Nduhuura E, Kajjimu J, Kule M, et al. Suicidal behaviours among Ugandan university students: A cross-sectional study. BMC Psychiatry. 2022;22(1):234. doi: 10.1186/s12888-022-03858-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mamun MA, Al Mamun F, Hosen I, Hasan M, Rahman A, Jubayar AM, et al. Suicidality in Bangladeshi young adults during the COVID-19 pandemic: The role of behavioral factors, COVID-19 risk and fear, and mental health problems. Risk Management and Healthcare Policy. 2021;14:4051–61. doi: 10.2147/RMHP.S330282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Opio JN, Munn Z, Aromataris E. Prevalence of Mental Disorders in Uganda: A Systematic Review and Meta-Analysis. The Psychiatric Quarterly. 2021. doi: 10.1007/s11126-021-09941-8 [DOI] [PubMed] [Google Scholar]
- 13.Wang J, Wu X, Lai W, Long E, Zhang X, Li W, et al. Prevalence of depression and depressive symptoms among outpatients: A systematic review and meta-analysis. BMJ Open. 2017;7(8):e017173. doi: 10.1136/bmjopen-2017-017173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Najjuka SM, Checkwech G, Olum R, Ashaba S, Kaggwa MM. Depression, anxiety, and stress among Ugandan university students during the COVID-19 lockdown: An online survey. African Health Sciences. 2021;21(4):1533–43. doi: 10.4314/ahs.v21i4.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meffert SM, Neylan TC, McCulloch CE, Maganga L, Adamu Y, Kiweewa F, et al. East African HIV care: Depression and HIV outcomes. Global Mental Health. 2019;6:e9. doi: 10.1017/gmh.2019.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaggwa MM, Namatanzi B, Kule M, Nkola R, Najjuka SM, Al Mamun F, et al. Depression in Ugandan rural women involved in a money saving group: The role of spouse’s unemployment, extramarital relationship, and substance use. International Journal of Womens Health. 2021;13:869–78. doi: 10.2147/IJWH.S323636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Akimana B, Abbo C, Balagadde-Kambugu J, Nakimuli-Mpungu E. Prevalence and factors associated with major depressive disorder in children and adolescents at the Uganda Cancer Institute. BMC Cancer. 2019;19(1):466. doi: 10.1186/s12885-019-5635-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaggwa MM, Najjuka SM, Ashaba S, Mamun MA. The psychometrics of Patient Health Questionnaire (PHQ-9) in Uganda: A systematic review. Frontiers in Psychiatry. 2022:13(781095). doi: 10.3389/fpsyt.2022.781095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller AP, Kintu M, Kiene SM. Challenges in measuring depression among Ugandan fisherfolk: a psychometric assessment of the Luganda version of the Center for Epidemiologic Studies Depression Scale (CES-D). BMC Psychiatry. 2020;20(1):45. doi: 10.1186/s12888-020-2463-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ashaba S, Cooper-Vince C, Vořechovská D, Maling S, Rukundo GZ, Akena D, et al. Development and validation of a 20-item screening scale to detect major depressive disorder among adolescents with HIV in rural Uganda: A mixed-methods study. SSM—Population Health. 2019;7:100332. doi: 10.1016/j.ssmph.2018.100332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nakku JEM, Rathod SD, Kizza D, Breuer E, Mutyaba K, Baron EC, et al. Validity and diagnostic accuracy of the Luganda version of the 9-item and 2-item Patient Health Questionnaire for detecting major depressive disorder in rural Uganda. Global Mental Health.2016;3:e20. doi: 10.1017/gmh.2016.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Natamba BK, Achan J, Arbach A, Oyok TO, Ghosh S, Mehta S, et al. Reliability and validity of the center for epidemiologic studies-depression scale in screening for depression among HIV-infected and -uninfected pregnant women attending antenatal services in northern Uganda: A cross-sectional study. BMC Psychiatry. 2014;14:303. doi: 10.1186/s12888-014-0303-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miller AP, Espinosa da Silva C, Ziegel L, Mugamba S, Kyasanku E, Bulamba RM, et al. Construct validity and internal consistency of the Patient Health Questionnaire-9 (PHQ-9) depression screening measure translated into two Ugandan languages. Psychiatry Research Communications. 2021;1(2):100002. doi: 10.1016/j.psycom.2021.100002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Akena D, Joska J, Stein DJ. Sensitivity and specificity of the Akena Visual Depression Inventory (AViDI-18) in Kampala (Uganda) and Cape Town (South Africa). The British Journal of Psychiatry. 2018;212(5):301–7. doi: 10.1192/bjp.2018.9 [DOI] [PubMed] [Google Scholar]
- 25.Reliefweb. Uganda resettlement and complementary pathways factsheet—31 October 2021 UN High Commissioner for Refugees 2021 [cited 2022 13 March]. https://reliefweb.int/report/uganda/uganda-resettlement-and-complementary-pathways-factsheet-31-october-2021#:~:text=UNHCR%20estimates%20that%20125%2C403%20refugees,Uganda%20since%201%20January%202021.
- 26.Musumari PM, Techasrivichien T, Srithanaviboonchai K, Wanyenze RK, Matovu JKB, Poudyal H, et al. HIV epidemic in fishing communities in Uganda: A scoping review. PloS One. 2021;16(4):e0249465. doi: 10.1371/journal.pone.0249465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaggwa MM, Nkola R, Najjuka SM, Bongomin F, Ashaba S, Mamun MA. Extrapyramidal side effects in a patient with alcohol withdrawal symptoms: A reflection of quality of the mental health care system. Risk Management and Healthcare Policy. 2021;14:2789–95. doi: 10.2147/RMHP.S314451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mugisha J, Muyinda H, Kagee A, Wandiembe P, Mpugu SK, Vancampfort D, et al. Prevalence of suicidal ideation and attempt: associations with psychiatric disorders and HIV/AIDS in post-conflict Northern Uganda. African Health Sciences. 2016;16(4):1027–35. doi: 10.4314/ahs.v16i4.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mugisha J, Muyinda H, Malamba S, Kinyanda E. Major depressive disorder seven years after the conflict in northern Uganda: Burden, risk factors and impact on outcomes (The Wayo-Nero Study). BMC Psychiatry. 2015;15:48. doi: 10.1186/s12888-015-0423-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Okware SI, Omaswa FG, Zaramba S, Opio A, Lutwama JJ, Kamugisha J, et al. An outbreak of Ebola in Uganda. Tropical Medicine & International Health. 2002;7(12):1068–75. doi: 10.1046/j.1365-3156.2002.00944.x [DOI] [PubMed] [Google Scholar]
- 31.Fischer M, Ramaswamy R, Fischer-Flores L, Mugisha G. Measuring and understanding depression in women in Kisoro, Uganda. Culture, Medicine, and Psychiatry. 2019;43(1):160–80. doi: 10.1007/s11013-018-9604-9 [DOI] [PubMed] [Google Scholar]
- 32.Ssewanyana Y, Ssekitooleko B, Suuna B, Bua E, Wadeya J, Makumbi TK, et al. Quality of life of adult individuals with intestinal stomas in Uganda: A cross sectional study. African Health Sciences. 2021;21(1):427–36. doi: 10.4314/ahs.v21i1.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bongomin F, Natukunda B, Sekimpi M, Olum R, Baluku JB, Makhoba A, et al. High prevalence of depressive symptoms among Ugandan patients with rheumatoid arthritis. Open access rheumatology: Research and Reviews. 2021;13:93–102. doi: 10.2147/OARRR.S306503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ngo VK, Wagner GJ, Nakasujja N, Dickens A, Aunon F, Musisi S. Effectiveness of antidepressants and predictors of treatment response for depressed HIV patients in Uganda. International Journal of STD & AIDS. 2015;26(14):998–1006. doi: 10.1177/0956462414564606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morof DF, Sami S, Mangeni M, Blanton C, Cardozo BL, Tomczyk B. A cross-sectional survey on gender-based violence and mental health among female urban refugees and asylum seekers in Kampala, Uganda. International Journal of Gynaecology and Obstetrics. 2014;127(2):138–43. doi: 10.1016/j.ijgo.2014.05.014 [DOI] [PubMed] [Google Scholar]
- 36.Bahati R, Ainamani HE, Sigmund CD, Rukundo GZ. Association between stigma and depression among urban refugees in Mbarara Municipality, Southwestern Uganda. Research Square (Preprint). 2021. doi: 10.21203/rs.3.rs-17932/v1 [DOI] [Google Scholar]
- 37.Kabunga A. Depressive disorders in refugees in Uganda: A case of Nakivale Refugee Camp. Journal of Psychology and Neuroscience. 2020;2(3). doi: 10.47363/JNRRR/2021(3)132 [DOI] [Google Scholar]
- 38.Ayano G, Solomon M, Abraha M. A systematic review and meta-analysis of epidemiology of depression in people living with HIV in East Africa. BMC Psychiatry. 2018;18(1):254. doi: 10.1186/s12888-018-1835-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PloS Medicine. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of Observational Studies in EpidemiologyA Proposal for Reporting. JAMA. 2000;283(15):2008–12. doi: 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 41.Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. International Journal of Eidence-based Halthcare. 2015;13(3):147–53. doi: 10.1097/XEB.0000000000000054 [DOI] [PubMed] [Google Scholar]
- 42.Assael MI, Namboze JM, German GA, Bennett FJ. Psychiatric disturbances during pregnancy in a rural group of African women. Social Science & Medicine (1967). 1972;6(3):387–95. doi: 10.1016/0037-7856(72)90109-6 [DOI] [PubMed] [Google Scholar]
- 43.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Joanna Briggs Institute. The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews. Checklist for Prevalence Studies. 2017 [cited 2022 13 March]. https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Prevalence_Studies2017_0.pd.
- 45.Kaggwa MM, Kajjimu J, Sserunkuma J, Najjuka SM, Atim LM, Olum R, et al. Prevalence of burnout among university students in low- and middle-income countries: A systematic review and meta-analysis. PloS One. 2021;16(8):e0256402. doi: 10.1371/journal.pone.0256402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kaggwa MM. Prevalence of depression in Uganda. A systematic review and meta-analysis; 2022[cited 2022 29 July]. Database: Figshare [internet]. doi: 10.6084/m9.figshare.19579096.v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.StataCorp. STATA Meta-analysis reference manual release 17 2021 [cited 2022 18/July/2021]. https://www.stata.com/manuals/meta.pdf.
- 48.Thompson SG, Higgins JPT. How should meta-regression analyses be undertaken and interpreted? Statistics in Medicine. 2002;21(11):1559–73. doi: 10.1002/sim.1187 [DOI] [PubMed] [Google Scholar]
- 49.Sterne JAC, Sutton AJ, Ioannidis JPA, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. doi: 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- 50.Shi L, Lin L. The trim-and-fill method for publication bias: practical guidelines and recommendations based on a large database of meta-analyses. Medicine. 2019;98(23):e15987. doi: 10.1097/MD.0000000000015987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nsereko JR. The prevalence and risk factors of symptoms of depression, anxiety and somatic syndromes among secondary school students in Kampala, Uganda [thesis]. South Africa: Stellenbosch: Stellenbosch University; 2018.
- 52.Lukenge E. Prevalence of depression, associated factors and coping styles among women attending infertility clinic at Mulago Hospital Kampala, Uganda [Dissertation]. School of Medicine Collections: Makerere University.; 2019.
- 53.Kizito S. Maternal mental illness, infant growth and infant psychomotor functioning in rural Masaka district, Uganda: A longitudinal cohort study [Thesis]. South Africa: Stellenbosch University; 2020.
- 54.Mubangizi I, Nakimuli-Mpungu E, Kawooya I, Sekaggya-wiltshire C. Prevalence and factors associated with depression among adults with sickle cell disease at Mulago Hospital, Uganda: A cross sectional study. Research Square (Preprint). 2020. doi: 10.21203/rs.3.rs-104883/v1 [DOI] [Google Scholar]
- 55.Bolton P, Wilk CM, Ndogoni L. Assessment of depression prevalence in rural Uganda using symptom and function criteria. Social Psychiatry and Psychiatric Epidemiology. 2004;39(6):442–7. doi: 10.1007/s00127-004-0763-3 [DOI] [PubMed] [Google Scholar]
- 56.Ovuga E, Boardman J, Wasserman D. Undergraduate student mental health at Makerere university, Uganda. World Psychiatry. 2006;5(1):51–2. https://pubmed.ncbi.nlm.nih.gov/16757997. [PMC free article] [PubMed] [Google Scholar]
- 57.Nakasujja N, Musisi S, Walugembe J, Wallace D. Psychiatric disorders among the elderly on non-psychiatric wards in an African setting. International Psychogeriatrics. 2007;19(4):691–704. doi: 10.1017/S1041610207005418 [DOI] [PubMed] [Google Scholar]
- 58.Nalugya-Sserunjogi J, Rukundo GZ, Ovuga E, Kiwuwa SM, Musisi S, Nakimuli-Mpungu E. Prevalence and factors associated with depression symptoms among school-going adolescents in Central Uganda. Child and Adolescent Psychiatry and Mental Health. 2016;10:39. doi: 10.1186/s13034-016-0133-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nakku JE, Nakasi G, Mirembe F. Postpartum major depression at six weeks in primary health care: Prevalence and associated factors. African Health Sciences. 2006;6(4):207–14. doi: 10.5555/afhs.2006.6.4.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kaharuza FM, Bunnell R, Moss S, Purcell DW, Bikaako-Kajura W, Wamai N, et al. Depression and CD4 cell count among persons with HIV infection in Uganda. AIDS and Behavior. 2006;10(4 Suppl):S105–11. doi: 10.1007/s10461-006-9142-2 [DOI] [PubMed] [Google Scholar]
- 61.Kinyanda E, Woodburn P, Tugumisirize J, Kagugube J, Ndyanabangi S, Patel V. Poverty, life events and the risk for depression in Uganda. Social Psychiatry and Psychiatric Epidemiology. 2011;46(1):35–44. doi: 10.1007/s00127-009-0164-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ovuga E, Boardman J, Wasserman D. The prevalence of depression in two districts of Uganda. Social Psychiatry and Psychiatric Epidemiology. 2005;40(6):439–45. doi: 10.1007/s00127-005-0915-0 [DOI] [PubMed] [Google Scholar]
- 63.Lundberg P, Rukundo G, Ashaba S, Thorson A, Allebeck P, Östergren P-O, et al. Poor mental health and sexual risk behaviours in Uganda: A cross-sectional population-based study. BMC Public Health. 2011;11(1):125. doi: 10.1186/1471-2458-11-125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nakimuli-Mpungu E, Munyaneza GM. Depression, alcohol abuse, and disclosure of HIV serostatus among rural HIV-positive individuals in western Uganda. Neurobehavioral HIV Medicine. 2013;3:3–19. doi: 10.2147/NBHIV.S13277 [DOI] [Google Scholar]
- 65.Agardh A, Cantor-Graae E, Ostergren PO. Youth, sexual risk-taking behavior, and mental health: a study of university students in Uganda. International Journal of Behavioral Medicine. 2012;19(2):208–16. doi: 10.1007/s12529-011-9159-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Vinck P, Pham PN, Stover E, Weinstein HM. Exposure to war crimes and implications for peace building in northern Uganda. JAMA. 2007;298(5):543–54. doi: 10.1001/jama.298.5.543 [DOI] [PubMed] [Google Scholar]
- 67.Pfeiffer A, Elbert T. PTSD, depression and anxiety among former abductees in Northern Uganda. Conflict and Health. 2011;5(1):14. doi: 10.1186/1752-1505-5-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Martinez P, Andia I, Emenyonu N, Hahn JA, Hauff E, Pepper L, et al. Alcohol use, depressive symptoms and the receipt of antiretroviral therapy in southwest Uganda. AIDS and Behavior. 2008;12(4):605–12. doi: 10.1007/s10461-007-9312-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Muhwezi WW, Ågren H, Musisi S. Detection of major depression in Ugandan primary health care settings using simple questions from a subjective well-being (SWB) subscale. Social Psychiatry and Psychiatric Epidemiology. 2007;42(1):61–9. doi: 10.1007/s00127-006-0132-5 [DOI] [PubMed] [Google Scholar]
- 70.Petrushkin H, Boardman J, Ovuga E. Psychiatric disorders in HIV-positive individuals in urban Uganda. Psychiatric Bulletin. 2005;29(12):455–8. doi: 10.1192/pb.29.12.455 [DOI] [Google Scholar]
- 71.Psaros C, Haberer JE, Boum Y 2nd, Tsai AC, Martin JN, Hunt PW, et al. The factor structure and presentation of depression among HIV-positive adults in Uganda. AIDS and Behavior. 2015;19(1):27–33. doi: 10.1007/s10461-014-0796-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nakasujja N, Skolasky RL, Musisi S, Allebeck P, Robertson K, Ronald A, et al. Depression symptoms and cognitive function among individuals with advanced HIV infection initiating HAART in Uganda. BMC Psychiatry. 2010;10:44. doi: 10.1186/1471-244X-10-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kaida A, Matthews LT, Ashaba S, Tsai AC, Kanters S, Robak M, et al. Depression during pregnancy and the postpartum among HIV-infected women on antiretroviral therapy in Uganda. Journal of Acquired Immune Deficiency Syndromes (1999). 2014;67 Suppl 4(Suppl 4):S179–87. doi: 10.1097/QAI.0000000000000370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Roberts B, Ocaka KF, Browne J, Oyok T, Sondorp E. Factors associated with post-traumatic stress disorder and depression amongst internally displaced persons in northern Uganda. BMC Psychiatry. 2008;8(1):38. doi: 10.1186/1471-244X-8-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Klasen F, Gehrke J, Metzner F, Blotevogel M, Okello J. Complex trauma symptoms in former Ugandan child soldiers. Journal of Aggression, Maltreatment & Trauma. 2013;22(7):698–713. doi: 10.1080/10926771.2013.814741 [DOI] [Google Scholar]
- 76.Klasen F, Oettingen G, Daniels J, Adam H. Multiple trauma and mental health in former Ugandan child soldiers. Journal of Traumatic Stress. 2010;23(5):573–81. doi: 10.1002/jts.20557 [DOI] [PubMed] [Google Scholar]
- 77.Klasen F, Oettingen G, Daniels J, Post M, Hoyer C, Adam H. Posttraumatic resilience in former Ugandan child soldiers. Child Development. 2010;81(4):1096–113. doi: 10.1111/j.1467-8624.2010.01456.x [DOI] [PubMed] [Google Scholar]
- 78.Abbo C, Ekblad S, Waako P, Okello E, Musisi S. The prevalence and severity of mental illnesses handled by traditional healers in two districts in Uganda. African Health Sciences. 2009;9 Suppl 1(Suppl 1):S16–22. [PMC free article] [PubMed] [Google Scholar]
- 79.Hatcher AM, Tsai AC, Kumbakumba E, Dworkin SL, Hunt PW, Martin JN, et al. Sexual relationship power and depression among HIV-infected women in Rural Uganda. PloS One. 2012;7(12):e49821. doi: 10.1371/journal.pone.0049821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pham PN, Vinck P, Stover E. Returning home: forced conscription, reintegration, and mental health status of former abductees of the Lord’s Resistance Army in northern Uganda. BMC Psychiatry. 2009;9(1):23. doi: 10.1186/1471-244X-9-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tsai AC, Bangsberg DR, Frongillo EA, Hunt PW, Muzoora C, Martin JN, et al. Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Social Science & Medicine (1982). 2012;74(12):2012–9. doi: 10.1016/j.socscimed.2012.02.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tsai AC, Wolfe WR, Kumbakumba E, Kawuma A, Hunt PW, Martin JN, et al. Prospective study of the mental health consequences of sexual violence among women living with HIV in rural Uganda. Journal of Interpersonal Violence. 2016;31(8):1531–53. doi: 10.1177/0886260514567966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nakimuli-Mpungu E, Alderman S, Kinyanda E, Allden K, Betancourt TS, Alderman JS, et al. Implementation and scale-up of psycho-trauma centers in a post-conflict area: A case study of a private-public partnership in northern Uganda. PloS Medicine. 2013;10(4):e1001427. doi: 10.1371/journal.pmed.1001427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Winkler N, Ruf-Leuschner M, Ertl V, Pfeiffer A, Schalinski I, Ovuga E, et al. From war to classroom: PTSD and depression in formerly abducted youth in Uganda. Frontier in Psychiatry. 2015;6:2. doi: 10.3389/fpsyt.2015.00002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Musisi S, Kinyanda E. Emotional and behavioural disorders in HIV seropositive adolescents in urban Uganda. East African Medical Journal. 2009;86(1):16–24. doi: 10.4314/eamj.v86i1.46923 [DOI] [PubMed] [Google Scholar]
- 86.Wagner GJ, Ghosh-Dastidar B, Garnett J, Kityo C, Mugyenyi P. Impact of HIV antiretroviral therapy on depression and mental health among clients with HIV in Uganda. Psychosomatic Medicine. 2012;74(9):883–90. doi: 10.1097/PSY.0b013e31826629db [DOI] [PubMed] [Google Scholar]
- 87.Shumba C, Atukunda R, Imakit R, Memiah P. Prevalence of depressive symptoms amongst highly active antiretroviral therapy (HAART) patients in AIDSRelief Uganda. Journal of Public Health in Africa. 2013;4(2):e19. doi: 10.4081/jphia.2013.e19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Okeke EN, Wagner GJ. AIDS treatment and mental health: evidence from Uganda. Social Science & Medicine (1982). 2013;92:27–34. doi: 10.1016/j.socscimed.2013.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wagner GJ, Ghosh-Dastidar B, Slaughter ME, Akena D, Nakasujja N, Musisi S. Changes in condom use during the first year of HIV treatment in Uganda and the relationship to depression. Annals of Behavioral Medicine. 2014;48(2):175–83. doi: 10.1007/s12160-013-9586-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wagner GJ, Slaughter M, Ghosh-Dastidar B. Depression at treatment initiation predicts HIV antiretroviral adherence in Uganda. Journal of the International Association of Providers of AIDS Care. 2017;16(1):91–7. doi: 10.1177/2325957416677121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wang C, Pu R, Ghose B, Tang S. Chronic musculoskeletal pain, self-reported health and quality of life among older populations in South Africa and Uganda. International Journal of Environmental Research and Public Health. 2018;15(12). doi: 10.3390/ijerph15122806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ager A, Pasha E, Yu G, Duke T, Eriksson C, Cardozo BL. Stress, mental health, and burnout in national humanitarian aid workers in Gulu, northern Uganda. Journal of Traumatic Stress. 2012;25(6):713–20. doi: 10.1002/jts.21764 [DOI] [PubMed] [Google Scholar]
- 93.Wagner GJ, Holloway I, Ghosh-Dastidar B, Kityo C, Mugyenyi P. Understanding the influence of depression on self-efficacy, work status and condom use among HIV clients in Uganda. Journal of Psychosomatic Research. 2011;70(5):440–8. doi: 10.1016/j.jpsychores.2010.10.003 [DOI] [PubMed] [Google Scholar]
- 94.Kinyanda E, Hoskins S, Nakku J, Nawaz S, Patel V. Prevalence and risk factors of major depressive disorder in HIV/AIDS as seen in semi-urban Entebbe district, Uganda. BMC Psychiatry. 2011;11:205. doi: 10.1186/1471-244X-11-205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kinyanda E, Hoskins S, Nakku J, Nawaz S, Patel V. The prevalence and characteristics of suicidality in HIV/AIDS as seen in an African population in Entebbe district, Uganda. BMC Psychiatry. 2012;12(1):63. doi: 10.1186/1471-244X-12-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nakku J, Kinyanda E, Hoskins S. Prevalence and factors associated with probable HIV dementia in an African population: A cross-sectional study of an HIV/AIDS clinic population. BMC Psychiatry. 2013;13(1):126. doi: 10.1186/1471-244X-13-126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kakyo TA, Muliira JK, Mbalinda SN, Kizza IB, Muliira RS. Factors associated with depressive symptoms among postpartum mothers in a rural district in Uganda. Midwifery. 2012;28(3):374–9. doi: 10.1016/j.midw.2011.05.001 [DOI] [PubMed] [Google Scholar]
- 98.Wagner GJ, Ghosh-Dastidar B, Dickens A, Nakasujja N, Okello E, Luyirika E, et al. Depression and its Relationship to Work Status and Income Among HIV Clients in Uganda. World journal of AIDS. 2012;2(3):126–34. doi: 10.4236/wja.2012.23018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wagner GJ, Ghosh-Dastidar B, Slaughter M, Akena D, Nakasujja N, Okello E, et al. The role of depression in work-related outcomes of HIV treatment in Uganda. International Journal of Behavioral Medicine. 2014;21(6):946–55. doi: 10.1007/s12529-013-9379-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kiene SM, Dove M, Wanyenze RK. Depressive symptoms, disclosure, HIV-related stigma, and coping following HIV testing among outpatients in Uganda: A daily process analysis. AIDS and Behavior. 2018;22(5):1639–51. doi: 10.1007/s10461-017-1953-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Okello ES, Wagner GJ, Ghosh-Dastidar B, Garnett J, Akena D, Nakasujja N, et al. Depression, internalized HIV stigma and HIV disclosure. World Journal of AIDS. 2015;5(01):30. doi: 10.4236/wja.2015.51004 [DOI] [Google Scholar]
- 102.Musisi S, Wagner GJ, Ghosh-Dastidar B, Nakasujja N, Dickens A, Okello E. Depression and sexual risk behaviour among clients about to start HIV antiretroviral therapy in Uganda. International Journal of STD & AIDS. 2014;25(2):130–7. doi: 10.1177/0956462413495186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Akena D, Musisi S, Joska J, Stein DJ. The association between aids related stigma and major depressive disorder among HIV-positive individuals in Uganda. PloS One. 2012;7(11):e48671. doi: 10.1371/journal.pone.0048671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Akena D, Stein DJ, Joska J. Does screening HIV-positive individuals in Uganda for major depressive disorder improve case detection rates and antidepressant prescription? AIDS and Behavior. 2013;17(8):2802–7. doi: 10.1007/s10461-012-0383-y [DOI] [PubMed] [Google Scholar]
- 105.Nakimuli-Mpungu E, Musisi S, Katabira E, Nachega J, Bass J. Prevalence and factors associated with depressive disorders in an HIV+ rural patient population in southern Uganda. Journal of Affective Disorders. 2011;135(1–3):160–7. doi: 10.1016/j.jad.2011.07.009 [DOI] [PubMed] [Google Scholar]
- 106.Katende G, Nakimera L. Prevalence and correlates of anxiety and depression among family carers of cancer patients in a cancer care and treatment facility in Uganda: A cross-sectional study. African Health Sciences. 2017;17(3):868–76. doi: 10.4314/ahs.v17i3.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kinyanda E, Kizza R, Abbo C, Ndyanabangi S, Levin J. Prevalence and risk factors of depression in childhood and adolescence as seen in 4 districts of north-eastern Uganda. BMC International Health and Human Rights. 2013;13(1):19. doi: 10.1186/1472-698X-13-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Spittal PM, Malamba SS, Ogwang MD, Musisi S, Ekwaru JP, Sewankambo NK, et al. Cango Lyec (healing the elephant): Gender differences in HIV infection in post-conflict Northern Uganda. Journal of Acquired Immune Deficiency Syndromes (1999). 2018;78(3):257–68. doi: 10.1097/QAI.0000000000001671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Whyte SR, Park SJ, Odong G, Ojara M, Lamwaka A. The visibility of non-communicable diseases in Northern Uganda. African Health Sciences. 2015;15(1):82–9. doi: 10.4314/ahs.v15i1.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Perkins JM, Nyakato VN, Kakuhikire B, Tsai AC, Subramanian SV, Bangsberg DR, et al. Food insecurity, social networks and symptoms of depression among men and women in rural Uganda: A cross-sectional, population-based study. Public Health Nutrition. 2018;21(5):838–48. doi: 10.1017/S1368980017002154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Malamba SS, Muyinda H, Spittal PM, Ekwaru JP, Kiwanuka N, Ogwang MD, et al. “The Cango Lyec Project—Healing the Elephant”: HIV related vulnerabilities of post-conflict affected populations aged 13–49 years living in three Mid-Northern Uganda districts. BMC infectious diseases. 2016;16(1):690. doi: 10.1186/s12879-016-2030-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hakim AJ, Mukasa B, Hundley L, Odiit M, Ogwal M, Sendagala S, et al. Correlates of undiagnosed HIV infection and retesting among voluntary HIV testing clients at Mildmay Clinic, Uganda. AIDS and Behavior. 2019;23(4):820–34. doi: 10.1007/s10461-018-2274-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Familiar I, Sikorskii A, Murray S, Ruisenor-Escudero H, Nakasujja N, Korneffel C, et al. Depression symptom trajectories among mothers living with HIV in rural Uganda. AIDS and Behavior. 2019;23(12):3411–8. doi: 10.1007/s10461-019-02465-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Cavazos-Rehg P, Xu C, Kasson E, Byansi W, Bahar OS, Ssewamala FM. Social and economic equity and family cohesion as potential protective factors from depression among adolescents living with HIV in Uganda. AIDS and Behavior. 2020;24(9):2546–54. doi: 10.1007/s10461-020-02812-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Akena D, Kadama P, Ashaba S, Akello C, Kwesiga B, Rejani L, et al. The association between depression, quality of life, and the health care expenditure of patients with diabetes mellitus in Uganda. Journal of Affective Disorders. 2015;174:7–12. doi: 10.1016/j.jad.2014.11.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Familiar I, Muniina PN, Dolan C, Ogwal M, Serwadda D, Kiyingi H, et al. Conflict-related violence and mental health among self-settled Democratic Republic of Congo female refugees in Kampala, Uganda–a respondent driven sampling survey. Conflict and Health. 2021;15(1):42. doi: 10.1186/s13031-021-00377-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Akena D, Ngo V, Guotman P, Glick P, Musisi S, Wagner GJJR, et al. Accuracy of depression evaluations by trained lay and medical health workers in HIV clinics in Uganda. Research and Advances in Psychiatry 2016;3:44–52. [Google Scholar]
- 118.Rathod SD, Roberts T, Medhin G, Murhar V, Samudre S, Luitel NP, et al. Detection and treatment initiation for depression and alcohol use disorders: Facility-based cross-sectional studies in five low-income and middle-income country districts. BMJ Open. 2018;8(10):e023421. doi: 10.1136/bmjopen-2018-023421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Mwesiga EK, Mugenyi L, Nakasujja N, Moore S, Kaddumukasa M, Sajatovic M. Depression with pain co morbidity effect on quality of life among HIV positive patients in Uganda: A cross sectional study. Health and Quality of Life Outcomes. 2015;13(1):206. doi: 10.1186/s12955-015-0403-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Nakku JEM, Rathod SD, Garman EC, Ssebunnya J, Kangere S, De Silva M, et al. Evaluation of the impacts of a district-level mental health care plan on contact coverage, detection and individual outcomes in rural Uganda: A mixed methods approach. International Journal of Mental Health Systems. 2019;13:63. doi: 10.1186/s13033-019-0319-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Nalwadda O, Rathod SD, Nakku J, Lund C, Prince M, Kigozi F. Alcohol use in a rural district in Uganda: findings from community-based and facility-based cross-sectional studies. International Journal of Mental Health Systems. 2018;12:12. doi: 10.1186/s13033-018-0191-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Jones R, Kirenga BJ, Katagira W, Singh SJ, Pooler J, Okwera A, et al. A pre–post intervention study of pulmonary rehabilitation for adults with post-tuberculosis lung disease in Uganda. International Journal of Chronic Obstructive Pulmonary Diseases 2017;12:3533–3539. doi: 10.2147/COPD.S146659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wagner GJ, Ghosh-Dastidar B, Robinson E, Ngo VK, Glick P, Musisi S, et al. Effects of depression alleviation on work productivity and income among HIV patients in Uganda. International Journal of Behavioral Medicine. 2017;24(4):628–33. doi: 10.1007/s12529-017-9642-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Rukundo ZG, Musisi S, Nakasujja N. Psychiatric morbidity among physically ill patients in a Ugandan Regional Referral Hospital. African Health Sciences. 2013;13(1):87–93. doi: 10.4314/ahs.v13i1.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Olema DK, Catani C, Ertl V, Saile R, Neuner F. The hidden effects of child maltreatment in a war region: Correlates of psychopathology in two generations living in Northern Uganda. Journal of Traumatic Stress. 2014;27(1):35–41. doi: 10.1002/jts.21892 [DOI] [PubMed] [Google Scholar]
- 126.Huang KY, Abura G, Theise R, Nakigudde J. Parental depression and associations with parenting and children’s physical and mental health in a Sub-Saharan African setting. Child Psychiatry and Human Development. 2017;48(4):517–27. doi: 10.1007/s10578-016-0679-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Wagner G, Ghosh-Dastidar B, Ngo V, Robinson E, Musisi S, Glick P, et al. A cluster randomized controlled trial of two task-shifting depression care models on depression alleviation and antidepressant response among HIV clients in Uganda. Research and Advances in Psychiatry. 2016;3(1):12–21. [PMC free article] [PubMed] [Google Scholar]
- 128.Wagner GJ, Ngo V, Goutam P, Glick P, Musisi S, Akena D. A structured protocol model of depression care versus clinical acumen: A cluster randomized trial of the effects on depression screening, diagnostic evaluation, and treatment uptake in Ugandan HIV clinics. PloS One. 2016;11(5):e0153132. doi: 10.1371/journal.pone.0153132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Henry MB, Bakeera-Kitaka S, Lubega K, Snyder SA, LaRussa P, Pfeffer B. Depressive symptoms, sexual activity, and substance use among adolescents in Kampala, Uganda. African Health Sciences. 2019;19(2):1888–96. doi: 10.4314/ahs.v19i2.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Swahn MH, Culbreth R, Masyn KE, Salazar LF, Wagman J, Kasirye R. The intersection of alcohol use, gender based violence and HIV: Empirical findings among disadvantaged service-seeking youth in Kampala, Uganda. AIDS and Behavior. 2021;25(10):3106–14. doi: 10.1007/s10461-021-03301-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Gyagenda JO, Ddumba E, Odokonyero R, Kaddumukasa M, Sajatovic M, Smyth K, et al. Post-stroke depression among stroke survivors attending two hospitals in Kampala Uganda. African Health Sciences. 2015;15(4):1220–31. doi: 10.4314/ahs.v15i4.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kinyanda E, Salisbury TT, Muyingo SK, Ssembajjwe W, Levin J, Nakasujja N, et al. Major depressive disorder among HIV infected youth in Uganda: Incidence, persistence and their predictors. AIDS and Behavior. 2020;24(9):2588–96. doi: 10.1007/s10461-020-02815-3 [DOI] [PubMed] [Google Scholar]
- 133.Muhammad Usman K, Okorie P, Umahi E, Paul S. Factors influencing the occurrence of mental illness in persons living with HIV/AIDS in Kabarole District, Uganda. International Journal of HIV/AIDS Prevention, Education and Behavioural Science. 2018;4(2):35–43. doi: 10.4314/njpar.v39i2 [DOI] [Google Scholar]
- 134.Ashaba S, Rukundo GZ, Beinempaka F, Ntaro M, LeBlanc JC. Maternal depression and malnutrition in children in southwest Uganda: A case control study. BMC Public Health. 2015;15:1303. doi: 10.1186/s12889-015-2644-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kinyanda E, Weiss HA, Mungherera M, Onyango-Mangen P, Ngabirano E, Kajungu R, et al. Intimate partner violence as seen in post-conflict eastern Uganda: Prevalence, risk factors and mental health consequences. BMC International Health and Human Rights. 2016;16(1):5. doi: 10.1186/s12914-016-0079-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Manne-Goehler J, Kakuhikire B, Abaasabyoona S, Bärnighausen TW, Okello S, Tsai AC, et al. Depressive symptoms before and after antiretroviral therapy initiation among older-aged individuals in rural Uganda. AIDS and Behavior. 2019;23(3):564–71. doi: 10.1007/s10461-018-2273-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kinyanda E, Kuteesa M, Scholten F, Mugisha J, Baisley K, Seeley J. Risk of major depressive disorder among older persons living in HIV-endemic central and southwestern Uganda. AIDS Care. 2016;28(12):1516–21. doi: 10.1080/09540121.2016.1191601 [DOI] [PubMed] [Google Scholar]
- 138.Smith ML, Kakuhikire B, Baguma C, Rasmussen JD, Perkins JM, Cooper-Vince C, et al. Relative wealth, subjective social status, and their associations with depression: Cross-sectional, population-based study in rural Uganda. SSM—Population Health. 2019;8:100448. doi: 10.1016/j.ssmph.2019.100448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Nampijja M, Natamba B, Mpango R, Kinyanda E. The burden and risk factors for postnatal depression and depressive symptomatology among women in Kampala. Tropical Doctor. 2019;49(3):170–7. doi: 10.1177/0049475519837107 [DOI] [PubMed] [Google Scholar]
- 140.Cooper-Vince CE, Arachy H, Kakuhikire B, Vořechovská D, Mushavi RC, Baguma C, et al. Water insecurity and gendered risk for depression in rural Uganda: A hotspot analysis. BMC Public Health. 2018;18(1):1143. doi: 10.1186/s12889-018-6043-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Kiene SM, Lule H, Sileo KM, Silmi KP, Wanyenze RK. Depression, alcohol use, and intimate partner violence among outpatients in rural Uganda: Vulnerabilities for HIV, STIs and high risk sexual behavior. BMC Infectious Diseases. 2017;17(1):88. doi: 10.1186/s12879-016-2162-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kinyanda E, Nakasujja N, Levin J, Birabwa H, Mpango R, Grosskurth H, et al. Major depressive disorder and suicidality in early HIV infection and its association with risk factors and negative outcomes as seen in semi-urban and rural Uganda. Journal of Affective Disorders. 2017;212:117–27. doi: 10.1016/j.jad.2017.01.033 [DOI] [PubMed] [Google Scholar]
- 143.Sohail S, Nakigozi G, Anok A, Batte J, Kisakye A, Mayanja R, et al. Headache prevalence and its functional impact among HIV-infected adults in rural Rakai District, Uganda. Journal of Neurovirology. 2019;25(2):248–53. doi: 10.1007/s13365-018-0710-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Raggio GA, Psaros C, Fatch R, Goodman G, Matthews LT, Magidson JF, et al. High rates of biomarker-confirmed alcohol use among pregnant women living with HIV in South Africa and Uganda. Journal of Acquired Immune Deficiency Syndromes (1999). 2019;82(5):443–51. doi: 10.1097/QAI.0000000000002156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kinyanda E, Weiss HA, Levin J, Nakasujja N, Birabwa H, Nakku J, et al. Incidence and persistence of major depressive disorder among people living with HIV in Uganda. AIDS and Behavior. 2017;21(6):1641–54. doi: 10.1007/s10461-016-1575-7 [DOI] [PubMed] [Google Scholar]
- 146.Akinbo E, Agwu E, Okoruwa G, Adedeji A. Prevalence and Magnitude of alcohol-related health problems among youths in disease endemic Bushenyi district, Uganda. Special Pathogens Review Journal. 2016; 1(2):53–9. [Google Scholar]
- 147.Cooper-Vince CE, Kakuhikire B, Vorechovska D, McDonough AQ, Perkins J, Venkataramani AS, et al. Household water insecurity, missed schooling, and the mediating role of caregiver depression in rural Uganda. Global Mental Health. 2017;4:e15. doi: 10.1017/gmh.2017.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Ashaba S, Cooper-Vince CE, Maling S, Satinsky EN, Baguma C, Akena D, et al. Childhood trauma, major depressive disorder, suicidality, and the modifying role of social support among adolescents living with HIV in rural Uganda. Journal of Affective Disorders Reports. 2021;4:100094. doi: 10.1016/j.jadr.2021.100094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ashaba S, Cooper-Vince C, Maling S, Rukundo GZ, Akena D, Tsai AC. Internalized HIV stigma, bullying, major depressive disorder, and high-risk suicidality among HIV-positive adolescents in rural Uganda. Global Mental Health. 2018;5:e22. doi: 10.1017/gmh.2018.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ortblad KF, Musoke DK, Chanda MM, Ngabirano T, Velloza J, Haberer JE, et al. Knowledge of HIV status is associated with a decrease in the severity of depressive symptoms among female sex workers in Uganda and Zambia. Journal of Acquired Immune Deficiency Syndromes (1999). 2020;83(1):37–46. doi: 10.1097/QAI.0000000000002224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Satinsky EN, Kakuhikire B, Baguma C, Rasmussen JD, Ashaba S, Cooper-Vince CE, et al. Adverse childhood experiences, adult depression, and suicidal ideation in rural Uganda: A cross-sectional, population-based study. PloS Medicine. 2021;18(5):e1003642–e. doi: 10.1371/journal.pmed.1003642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Alinaitwe R, Birungi C, Bangirana P, Nakasujja N. Prevalence and factors associated with depressive illness in patients with tuberculosis in Mulago hospital, Kampala- Uganda: A cross sectional study. Journal of Psychosomatic Research. 2021;149:110591. doi: 10.1016/j.jpsychores.2021.110591 [DOI] [PubMed] [Google Scholar]
- 153.Bapolisi AM, Song SJ, Kesande C, Rukundo GZ, Ashaba S. Post-traumatic stress disorder, psychiatric comorbidities and associated factors among refugees in Nakivale camp in southwestern Uganda. BMC Psychiatry. 2020;20(1):53. doi: 10.1186/s12888-020-2480-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Forry JB, Ashaba S, Rukundo GZ. Prevalence and associated factors of mental disorders among prisoners in Mbarara municipality, southwestern Uganda: A cross-sectional study. BMC Psychiatry. 2019;19(1):178. doi: 10.1186/s12888-019-2167-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Seffren V, Familiar I, Murray SM, Augustinavicius J, Boivin MJ, Nakasujja N, et al. Association between coping strategies, social support, and depression and anxiety symptoms among rural Ugandan women living with HIV/AIDS. AIDS Care. 2018;30(7):888–95. doi: 10.1080/09540121.2018.1441969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kuteesa MO, Weiss HA, Cook S, Seeley J, Ssentongo JN, Kizindo R, et al. Epidemiology of alcohol misuse and illicit drug use among young people aged 15–24 years in fishing communities in Uganda. International Journal of Enviromental Research and Public Health 2020;17(7):2401. doi: 10.3390/ijerph17072401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Nabunya P, Damulira C, Byansi W, Muwanga J, Bahar OS, Namuwonge F, et al. Prevalence and correlates of depressive symptoms among high school adolescent girls in southern Uganda. BMC Public Health. 2020;20(1):1792. doi: 10.1186/s12889-020-09937-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Arach AAO, Nakasujja N, Nankabirwa V, Ndeezi G, Kiguli J, Mukunya D, et al. Perinatal death triples the prevalence of postpartum depression among women in Northern Uganda: A community-based cross-sectional study. PloS One. 2020;15(10):e0240409. doi: 10.1371/journal.pone.0240409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Logie CH, Okumu M, Mwima S, Hakiza R, Chemutai D, Kyambadde P. Contextual factors associated with depression among urban refugee and displaced youth in Kampala, Uganda: findings from a cross-sectional study. Conflict and Health. 2020;14(1):45. doi: 10.1186/s13031-020-00289-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Musinguzi K, Obuku A, Nakasujja N, Birabwa H, Nakku J, Levin J, et al. Association between major depressive disorder and pro-inflammatory cytokines and acute phase proteins among HIV-1 positive patients in Uganda. BMC Immunology. 2018;19(1):1. doi: 10.1186/s12865-017-0239-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Muliira JK, Kizza IB. The other untold burden of cancer in sub-Saharan Africa: Anxiety and depressive symptoms among family caregivers of adult cancer patients. International Journal of Africa Nursing Sciences. 2019;11:100166. doi: 10.1016/j.ijans.2019.100166 [DOI] [Google Scholar]
- 162.Misghinna TK, Nakimuli-Mpungu E, Abbo C, Kinyanda E,. Major depressive disorder and associated factors among adult refugees attending a refugee center in Kampala, Uganda. African Journal of Traumatic Stress. 2020;5(1):1–21. [Google Scholar]
- 163.Boduszek D, Debowska A, Ochen EA, Fray C, Nanfuka EK, Powell-Booth K, et al. Prevalence and correlates of non-suicidal self-injury, suicidal ideation, and suicide attempt among children and adolescents: Findings from Uganda and Jamaica. Journal of Affective Disorders. 2021;283:172–8. doi: 10.1016/j.jad.2021.01.063 [DOI] [PubMed] [Google Scholar]
- 164.Kyohangirwe L, Okello E, Namuli JD, Ndeezi G, Kinyanda E. Prevalence and factors associated with major depressive disorder among adolescents attending a primary care facility in Kampala, Uganda. Tropical Doctor. 2020;50(1):30–6. doi: 10.1177/0049475519879586 [DOI] [PubMed] [Google Scholar]
- 165.Olum R, Nakwagala FN, Odokonyero R. Prevalence and factors associated with depression among medical students at Makerere university, Uganda. Advance in Medical Education and Practice. 2020;11:853–60. doi: 10.2147/AMEP.S278841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Mootz JJ, Muhanguzi F, Greenfield B, Gill M, Gonzalez MB, Panko P, et al. Armed conflict, intimate partner violence, and mental distress of women in Northeastern Uganda: A mixed methods study. Psychology of Women Quarterly. 2019;43(4):457–71. doi: 10.1177/0361684319864366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Ssebunnya J, Medhin G, Kangere S, Kigozi F, Nakku J, Lund C. Prevalence, correlates and help-seeking behaviour for depressive symptoms in rural Uganda: a population-based survey. Global Mental Health. 2019;6:e27. Epub 2019/12/07. doi: 10.1017/gmh.2019.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Kabunga A, Anyayo L. Depression and associated factors among refugees amidst covid-19 in Nakivale refugee camp in Uganda. Journal of Neurology Research Reviews & Reports. 2021;3:1–5. doi: 10.47363/JNRRR/2021(3)132 [DOI] [Google Scholar]
- 169.Kabunga A, Nambozo S. Prevalence and factors associated with depression among out-of-school adolescents in Ayere village, Northern Uganda. International Journal of Academic Research in Progressive Education and Development. 2021;10. doi: 10.6007/IJARPED/v10-i1/9080 [DOI] [Google Scholar]
- 170.Ouma S, Tumwesigye NM, Ndejjo R, Abbo C. Prevalence and factors associated with major depression among female sex workers in post-conflict Gulu district: A cross-sectional study. BMC Public Health. 2021;21(1):1134. doi: 10.1186/s12889-021-11207-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Mahmud M, Riley E. Household response to an extreme shock: Evidence on the immediate impact of the Covid-19 lockdown on economic outcomes and well-being in rural Uganda. World Development. 2021;140:105318. doi: 10.1016/j.worlddev.2020.105318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Blackmore R, Boyle JA, Fazel M, Ranasinha S, Gray KM, Fitzgerald G, et al. The prevalence of mental illness in refugees and asylum seekers: A systematic review and meta-analysis. PloS Medicine. 2020;17(9):e1003337. doi: 10.1371/journal.pmed.1003337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Morina N, Stam K, Pollet TV, Priebe S. Prevalence of depression and posttraumatic stress disorder in adult civilian survivors of war who stay in war-afflicted regions. A systematic review and meta-analysis of epidemiological studies. Journal of Affective Disorders. 2018;239:328–38. doi: 10.1016/j.jad.2018.07.027 [DOI] [PubMed] [Google Scholar]
- 174.Nanni MG, Caruso R, Mitchell AJ, Meggiolaro E, Grassi L. Depression in HIV infected patients: A review. Current Psychiatry Report. 2015;17(1):530. doi: 10.1007/s11920-014-0530-4 [DOI] [PubMed] [Google Scholar]
- 175.Del-Pino-Casado R, Rodríguez Cardosa M, López-Martínez C, Orgeta V. The association between subjective caregiver burden and depressive symptoms in carers of older relatives: A systematic review and meta-analysis. Plos One. 2019;14(5):e0217648. doi: 10.1371/journal.pone.0217648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Al Mamun F, Hosen I, Misti JM, Kaggwa MM, Mamun MA. Mental disorders of Bangladeshi students during the COVID-19 pandemic: A systematic review. Psychological Research and Behavior Management. 2021;14:645–54. doi: 10.2147/PRBM.S315961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Vithalani J, Herreros-Villanueva M. HIV epidemiology in Uganda: Survey based on age, gender, number of sexual partners and frequency of testing. African Health Sciences. 2018;18(3):523–30. doi: 10.4314/ahs.v18i3.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Lundberg P, Nakasujja N, Musisi S, Thorson AE, Cantor-Graae E, Allebeck P. HIV prevalence in persons with severe mental illness in Uganda: a cross-sectional hospital-based study. International Journal of Mental Health Systems. 2013;7(1):20. doi: 10.1186/1752-4458-7-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Rezaei S, Ahmadi S, Rahmati J, Hosseinifard H, Dehnad A, Aryankhesal A, et al. Global prevalence of depression in HIV/AIDS: A systematic review and meta-analysis. BMJ Supportive & Palliative Care. 2019;9(4):404–12. doi: 10.1136/bmjspcare-2019-001952 [DOI] [PubMed] [Google Scholar]
- 180.Geng HM, Chuang DM, Yang F, Yang Y, Liu WM, Liu LH, et al. Prevalence and determinants of depression in caregivers of cancer patients: A systematic review and meta-analysis. Medicine. 2018;97(39):e11863. doi: 10.1097/MD.0000000000011863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Muliira JK, Kizza IB, Nakitende G. Roles of family caregivers and perceived burden when caring for hospitalized adult cancer patients: Perspective from a low-income country. Cancer Nursing. 2019;42(3):208–17. doi: 10.1097/NCC.0000000000000591 [DOI] [PubMed] [Google Scholar]
- 182.Adejoh SO, Boele F, Akeju D, Dandadzi A, Nabirye E, Namisango E, et al. The role, impact, and support of informal caregivers in the delivery of palliative care for patients with advanced cancer: A multi-country qualitative study. Palliative Medicine. 2020;35(3):552–62. doi: 10.1177/0269216320974925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Johns G, Samuel V, Freemantle L, Lewis J, Waddington L. The global prevalence of depression and anxiety among doctors during the covid-19 pandemic: Systematic review and meta-analysis. Journal of Affective Disorders. 2022;298(Pt A):431–41. doi: 10.1016/j.jad.2021.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]