Abstract
Background
Increasing lines of evidence indicate that traditional Chinese exercise (TCE) has potential benefits in improving chronic low back pain (CLBP) symptoms. To assess the clinical efficacy of TCE in the treatment of CLBP, we performed a systematic review of existing randomized controlled trials (RCTs) of CLBP and summarized the neural mechanisms underlying TCE in the treatment of CLBP.
Methods
A systematic search was conducted in four electronic databases: PubMed, Embase, the Cochrane Library, and EBSCO from January 1991 to March 2022. The quality of all included RCTs was evaluated by the Physiotherapy Evidence Database Scale (PEDro). The primary outcomes included pain severity and pain-related disability.
Results
A total of 11 RCTs with 1,256 middle-aged and elderly patients with CLBP were included. The quality of all 11 included RCTs ranged from moderate to high according to PEDro. Results suggested that TCE could considerably reduce pain intensity in patients with CLBP. Overall, most studies did not find any difference in secondary outcomes (quality of life, depression, and sleep quality).
Conclusion
The neurophysiological mechanism of TCE for treating CLBP could be linked to meditation and breathing, posture control, strength and flexibility training, and regulation of pain-related brain networks. Our systematic review showed that TCE appears to be effective in alleviating pain in patients with CLBP.
Keywords: chronic low back pain, traditional Chinese exercise, elderly people, Tai Chi, Qigong
Introduction
Incidence of low back pain (LBP) increases progressively with age (Neuhauser et al., 2005); it is estimated that 12% of adults over the age of 65 suffer from chronic LBP (CLBP) (Arnstein, 2010). When LBP in older population becomes chronic (lasting more than 12 weeks) (Deyo et al., 2014), it can lead to a variety of harmful consequences, including falls and fractures (Leveille et al., 2009), depression/anxiety (Meyer et al., 2007; Kroenke et al., 2013), social difficulties (Mackichan et al., 2013), and sleep disturbances (Weiner et al., 2006a). In addition, extraspinal conditions (i.e., osteoarthritis and fibromyalgia) are common in older adults with CLBP and may be linked to pain-related disability (Weiner et al., 2006b; Viniol et al., 2013; Rundell et al., 2017). Although clinicians have treated CLBP with conventional medication and surgery for a long time, many patients continue to experience pain without significant pain relief (Steffens et al., 2016; Maher et al., 2017). Therefore, over the past 30 years, many clinical guidelines have recommended that treatment of CLBP should focus on non-pharmacological treatments, such as exercise therapy and mind–body exercise (Bernstein et al., 2017; Qaseem et al., 2017; Wong et al., 2017; Stochkendahl et al., 2018; Zhang et al., 2019; Peng et al., 2022; Xiong et al., 2022). Exercise therapy, which includes a variety of interventions ranging from aerobic exercise to muscle strength training, has been shown to be useful in alleviating pain (Lawand et al., 2015; Wieland et al., 2017; Russo et al., 2018; Smith et al., 2022; Wu et al., 2022).
Under this condition, traditional Chinese exercise (TCE), as a therapeutic mind–body exercise, has been widely concerned by researchers (Koh, 1982; Chou et al., 2015; Guo et al., 2018). TCE [i.e., Tai Chi (Zou et al., 2017a) and Qigong (Zou et al., 2018a)] is becoming increasingly popular around the world and is being used to treat various diseases and prevent chronic disease progression (Zhu et al., 2016). TCE emphasizes mind–body integration; slow body movements should be synchronized with musculoskeletal relaxation, respiratory control, and mental focus in a meditative state (Luo et al., 2017; Zou et al., 2018c). In addition, TCE requires the stability of the trunk muscles to maintain the center of gravity, which embodies the principle of core stability training (Wang et al., 2013). In recent years, TCE has been successfully used worldwide for the treatment of CLBP and is recommended as a therapeutic activity according to the guidelines of the American College of Physicians (Qaseem et al., 2017). A meta-analysis also suggested that TCE might provide some pain relief in patients with LBP(Zhang et al., 2019). For instance, Blodt et al. (2015) suggested that Qigong training was no worse than exercise therapy for pain relief in patients with CLBP. Our previous work also supported that the patients with chronic non-specific LBP over the age of 50 engaging in Chen-style Tai Chi for 12 weeks had significantly reduced pain (Liu et al., 2019; Zou et al., 2019a). However, results from different randomized controlled trials (RCTs) are inconsistent, with some studies suggesting that yoga and Qigong had no effect on relieving CLBP possibly due to the small sample size or differences in pain sensitivity and processing in the elderly (Teut et al., 2016). The conclusions from current studies have remained controversial. In addition, there are no systematic reviews of TCE interventions for CLBP in the middle-aged and elderly. Therefore, further review and analysis of available data on TCE-related pain and disability in middle-aged and elderly patients with CLBP are necessary.
Materials and methods
Search strategy and inclusion criteria
This systematic review was registered with the Open Science Framework (10.17605/OSF.IO/NWGSF).1 PRISMA guidelines were followed (Moher et al., 2009). PubMed, Embase, the Cochrane Library, and EBSCO were searched from January 1991 to March 2022 for relevant clinical trials (Supplementary material 1). The following combination of terms was used as search keywords in the title and abstract: T1 = Tai Chi OR “Tai Chi *” OR Qigong OR Liuzijue OR Wuqinxi OR Yijinjing OR Baduanjin OR “traditional exercise” OR traditional Chinese medicine OR “Chinese traditional exercise” OR “traditional Chinese exercise” OR “Chinese exercise,” T2 = back pain OR low backache OR lower back pain OR lumbago OR lumbosacral pain OR sciatica. When screening clinical trials, the inclusion criteria are as follows:
-
(1)
Types of studies. We included only published articles from RCTs that examined the effect of TCE on LBP. The article language was limited to English.
-
(2)
Participants. All middle-aged and elderly patients (mean age > 35 years old) with a diagnosis of LBP were considered for this review.
-
(3)
Interventions. The interventions included different types of TCE (i.e., Tai Chi, Baduanjin, Yijinjing, Qigong, Liuzijue, and Wuqinxi). Clinical trials comparing TCE with no intervention, placebo (waiting-list, unaltered lifestyle), or other treatments (such as exercise therapy, massage, and physical activity) were included.
-
(4)
Types of outcome measures. Outcome measures should include at least one of two evaluations: pain and disability.
Study selection and data extraction
Two authors independently screened all titles, abstracts, and main text of the relevant papers according to the inclusion criteria. Papers that did not match the criteria for inclusion were omitted. Disagreements were settled by discussion or a third reviewer. The following information was extracted from the selected articles: (1) published data (author, year); (2) design of included studies (subject subgroup, sample size, randomization, follow-up, clinical outcome measures, and time points); (3) type of intervention (including dose regimen, duration); (4) characteristics of participants (including baseline demographic information and diagnostic/inclusion/exclusion criteria); and (5) adverse effects.
Quality assessment and data analysis
We used the Physiotherapy Evidence Database scale (PEDro) to assess the risk of bias for inclusion and the methodological quality of each study in this systematic review (Supplementary Table 1). Two authors independently evaluated the quality of the included RCTs, and all disagreements were settled by discussion or a third reviewer. The following information was evaluated: randomized allocation, concealed allocation, baseline comparability, blind subjects, blind therapists, blind assessors, adequate follow-up, intention-to-treat analysis, between-group comparisons, point estimates, and variability. Scores < 4 points were considered as poor quality; 4–5 points as modern quality; 6–8 points as high quality; 9–10 as excellent quality. The characteristics of the included RCTs were examined (Table 1). Then, The findings were then narratively presented in terms of the TCE’s mechanisms in the treatment of LBP, which were detailed and discussed in the following sections.
TABLE 1.
Summary of included studies.
| References | Country | Participant characteristic, sample size | Disease | Drugs | Intervention | Time point | Duration of trial period | Primary Outcomes | Result |
| Hall et al., 2011 | Australia | 160 subjects M = 41, F = 119 Mean age (± SD): 44.4 ± 13.2 |
Persistent low back pain | NA | G1 (n = 80): Tai Chi G2 (n = 80): Control group(usual health care) |
10 weeks | 18 sessions over 10 weeks (2 times per week for 8 weeks followed by once per week for 2 weeks) | 1. Pain intensity (NRS) 2. Disability (RMDQ) |
Tai Chi produced greater reductions in pain symptoms and pain-related disability than the control intervention. |
| Weifen et al., 2013 | China | 320 subjects M = 192, F = 128 Mean age (± SD): 37.6 ± 5.4 |
Chronic non-specific low back pain | NA | G1 (n = 141): Tai Chi group G2 (n = 47): Backward walking group G3 (n = 47): Jogging group G4 (n = 38): Swimming group G5 (n = 47): No exercise group |
6 months | G1: Five 45 min sessions per week for 6 months G2-5: Five 30 min sessions per week for 6 months |
1. Pain intensity (NRS) | After three and six months, no statistically significant difference in the intensity of LBP was demonstrated between the tai chi and swimming groups; significant differences were demonstrated among the tai chi and backward walking, jogging, and no exercise groups. |
| Blodt et al., 2015 | Germany | 127 subjects M = 25, F = 102 Mean age (± SD): 46.7 ± 10.4 |
Chronic non-specific low back pain | No medication taken during the period of study | G1 (n = 64): Qigong group G2 (n = 63): Exercise therapy group |
3 months | Weekly sessions of 90 min over a period of 3 months | 1. Pain intensity (VAS) | Qigong was not proven to be non-inferior to exercise therapy in the treatment of chronic LBP. |
| Teut et al., 2016 | Germany | 176 subjects M = 20, F = 156 Mean age (± SD): 73 ± 5.6 |
Chronic non-specific low back pain | No medication taken during the period of study | G1 (n = 61): Yoga group G2 (n = 58): Qigong group G3 (n = 57): Control group (no additional intervention) |
3 months | 1. Yoga (24 classes, 45 min each, during 3 months) 2. Qigong (12 classes, 90 min each, during 3 months) |
1. Pain intensity (VAS) 2. Pain (Functional Rating Index) |
Participation in a 3-month yoga or qigong program did not improve chronic LBP, back function and quality of life. |
| Hall et al., 2016 | England | 102 subjects M = 25, F = 77 Mean age: 66.5 |
Chronic non-specific low back pain | NA | G1 (n = 51): Tai Chi group G2 (n = 51): Wait-list Control group (usual care) |
10 weeks | Two 40 min sessions per week for the first 8 weeks, and one 40 min session class for the last 2 weeks | 1. Pain intensity (NRS) 2. Pain related disability (RMDQ) |
The total effects showed better outcome on measures for the tai chi group and were all significant at the 5% significance level. |
| Zou et al., 2019a | China | 43 subjects M = 11, F = 32 Mean age: 58 |
Chronic non-specific low back pain | NA | G1 (n = 15): Tai Chi group G2 (n = 15): Core stability training group G3 (n = 13): Control group (normal daily activities) |
12 weeks | Three sessions per week, with each session lasting 60 min for 12 weeks | 1. Pain intensity (VAS) 2. Neuromuscular function assessment |
Chen-style tai chi and Core stability training were found to have protective effects on neuromuscular function in aging individuals with non-specific LBP, while alleviating non-specific chronic pain. |
| Phattharasupharerk et al., 2019 | Thailand | 72 subjects M = 26, F = 46 Mean age: 35.25 |
Chronic non-specific low back pain | No medication taken during the period of study | G1 (n = 36): Qigong group G2 (n = 36): waiting list (general advice) |
6 weeks | 60 min session per week for 6 weeks | 1. Pain intensity (VAS) 2. Back functional disability (RMDQ) |
The qigong group showed significant improvement in pain and functional disability both within the group and between groups. |
| Liu et al., 2019 | China | 43 subjects M = 11, F = 32 Mean age: 59 |
Chronic non-specific low back pain | NA | G1 (n = 15): Tai Chi group G2 (n = 15): Core stabilization training group G3 (n = 13): No intervention |
12 weeks | Three 60-min sessions per week for 12 weeks | 1. Pain intensity (VAS) 2. Knee and ankle joint position sense |
Tai Chi and Core Stabilization training have significant effects on pain VAS but not on joint position sense. |
| Yao et al., 2020 | China | 72 subjects M = 14, F = 58 Mean age (± SD): 53.5 ± 15 |
Chronic non-specific low back pain | No medication taken during the period of study | G1 (n = 36): Wuqinxi group G2 (n = 36): General exercise group |
24 weeks | Four times a week with 1 h of each session for 24 weeks | 1. Pain intensity (VAS) 2. Trunk Muscle Strength |
Wuqinxi had better effects on chronic LBP for a long time compared with general exercise, including pain intensity and quality of life. |
| Ma et al., 2020 | China | 84 subjects M = 59, F = 25 Mean age: 36 |
Axial spondyloarthritis | NA | G1 (n = 42): Tai Chi group G2 (n = 42): Standard exercise therapy |
12 weeks | Three 30–40 min sessions per week for 12 weeks | 1. Pain intensity (VAS) 2. Spinal motor function |
Compared with standard exercise therapy, “tai chi spinal exercise” has an ideal effect in patients with axial spondyloarthritis, which can more effectively relieve patient’s LBP and improve spinal motor function, with shorter training time and better compliance. |
| Sherman et al., 2020 | USA | 57 subjects M = 22, F = 35 Mean age: 73 |
Chronic non-specific low back pain | NA | G1 (n = 28): Tai Chi group G2 (n = 12): Health education group G3 (n = 17): Usual care group |
12 weeks | Two 60 min sessions per week for 12 weeks | 1.0–10-point pain intensity measure 2. Pain related disability (RMDQ) |
Compared with health education, tai chi participants rated both the helpfulness of classes and their likelihood of recommending the classes to other significantly higher. |
LBP, low back pain; VAS, visual analog scale; NRS, numerical rating scale; RMDQ, Roland-Morris Disability Questionnaire.
Results
Search results
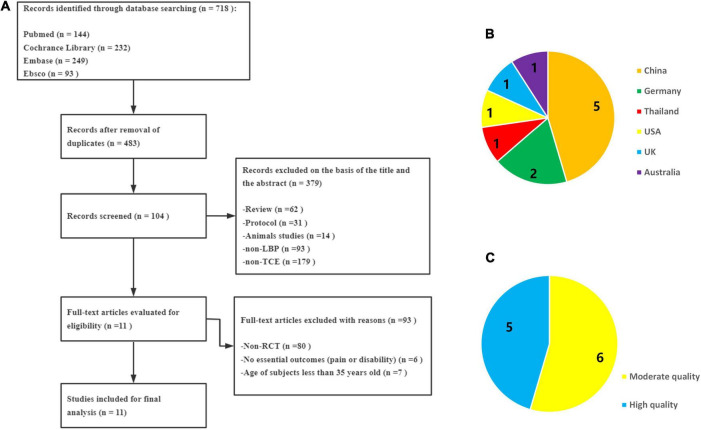
As shown in Figure 1A, 718 papers in related fields were retrieved from the four electronic databases. After removing 235 duplicates, 483 articles were screened for eligibility. Through reviewing the titles, abstracts, and full contents of the selected studies, we excluded another 472 articles (review = 62, protocol = 31, animal studies = 14, non-LBP = 93, non-TCE = 179, non-RCT = 80, no essential outcomes = 6, age of subjects less than 35 years old = 7). Finally, 11 RCTs were included in this review (Hall et al., 2011, 2016; Blodt et al., 2015; Teut et al., 2016; Qaseem et al., 2017; Liu et al., 2019; Phattharasupharerk et al., 2019; Zou et al., 2019a; Ma et al., 2020; Sherman et al., 2020; Yao et al., 2020).
FIGURE 1.
(A) A PRISMA flow diagram of the literature screening and selection processes. (B) Distribution of countries. (C) Quality assessment of PEDro.
Study characteristics
Table 1 shows the key characteristics of all included RCTs. Eleven RCTs involving 1,256 participants (810 females) ranging in age from 35 to 73 years were included. The sample size of each RCT ranged from 43 to 176. These RCTs were performed in China, Germany, Australia, England, Thailand, and the USA between 2013 and 2020 (Figure 1B). Three kinds of TCE programs were used to treat CLBP in all intervention groups (7 for Tai Chi, 3 for Qigong, and 1 for Wuqinxi). In the control group, active interventions (such as core training, exercise therapy, or yoga) or passive interventions (such as health education) were used. The treatment duration ranged from 6 weeks to 6 months, with each session lasting from 30 to 90 min, of which 12 weeks was the most common in six trials. The visual analogue scale (VAS) and the numerical rating scale (NRS) were used to evaluated the major outcomes for pain severity.
Quality assessment
Supplementary Table 1 summarizes the quality evaluation results for each RCT by using the PEDro scale. The quality of all 11 studies considered in this review ranged from moderate to high (Figure 1C). In most RCTs, participants, therapists, and assessors were not blinded.
Effect of traditional Chinese exercise on pain
All 11 included studies involving 1,256 patients with LBP examined the effect of different types of TCE on pain intensity. Ten studies suggested that TCE group outperformed the control group in terms of pain relief, but one of the studies found that the effectiveness of Qigong for pain relief decreased over time. Only one study found no significant difference in pain alleviation between the Qigong and the control groups (Teut et al., 2016).
Effect of traditional Chinese exercise on pain-related disability, quality of life, and sleep quality
Of the 11 included studies, five studies investigated the effects of TCE on back functional disability, three studies evaluated the effect on quality of life (QOL), and four studies determined the effect on sleep quality and satisfaction. Three studies suggested that Tai Chi had effectively improved back pain-related disability compared with the control group (Hall et al., 2011, 2016; Sherman et al., 2020). Phattharasupharerk et al. and Blödt et al. reported that Qigong did not improve back functional disability effectively because the Roland–Morris Disability Questionnaire (RMDQ) scores did not meet the minimal clinically important difference level (Blodt et al., 2015; Phattharasupharerk et al., 2019). Additionally, Qigong and Wuqinxi had effectively improved QOL and depression compared with the baseline, but no statistical difference was found compared with the control group (Blodt et al., 2015; Teut et al., 2016; Yao et al., 2020). Overall, most studies did not find any difference in the secondary outcomes tested (disability, QOL, and sleep quality).
Adverse events
Only two studies reported adverse events. Amanda et al. found that four subjects reported a slight increase in back pain at the beginning of Tai Chi training, which was relieved by the third or fourth week of the training (Hall et al., 2011). Blödt et al. found that both the Qigong group (n = 10) and exercise group (n = 10) reported suspected adverse events (e.g., muscle soreness and tenseness, dizziness, mood fluctuation, and increased back pain) (Blodt et al., 2015).
Discussion
Effectiveness of traditional Chinese exercise on middle-aged and elderly patients with chronic low back pain
Pain management in elderly patients with CLBP is particularly challenging, and long-term opioid use was associated with an increased risk of comorbidities (Makris et al., 2014), psychological distress [e.g., depression (Maher et al., 2017)] and other health problems (e.g., falls, osteoporosis, and muscular atrophy) (Chou et al., 2015). A previous review suggested that people who experienced LBP had a higher risk of recurrence (Taylor et al., 2014). Therefore, current guidelines recommend that treatment should focus on reducing pain and its associated dysfunction, and exercise is an effective treatment option (Koes et al., 2010; Zhang et al., 2020). This systematic review included 11 RCTs involving 1,256 patients with CLBP aged over 35 years to assess the overall effect of TCE in middle-aged and elderly patients with CLBP. Our results indicated that TCE could be an effective therapy for reducing pain and improving function in the patients. All treatments (Tai Chi, Qigong, and Wuqinxi) showed positive effects compared with baseline measurements.
Pain intensity relates to the degree to which a person is harmed by CLBP and can be quantified to estimate the severity of pain (Ostelo and de Vet, 2005). The results from this systematic review suggest that TCE significantly reduce the VAS or NRS scores of patients with CLBP. Compared with the control and exercise therapy groups, TCE showed better effects in alleviating pain, which is consistent with prior reviews on other exercise therapies (Hayden et al., 2005; Macedo et al., 2013). Only one study showed that 3 months of yoga or Qigong training had no effect on back pain, back function, or QOL in older patients with CLBP (Teut et al., 2016). However, the number of studies was insufficient to conclude every type of TCE. Additionally, several RCTs showed that Tai Chi/Qigong significantly contributed to proprioception and neuromuscular function in the lower limbs (Zou et al., 2019a). An RCT involving 84 patients showed that Tai Chi was more effective in improving spinal movement function, with shorter training time and better compliance compared with standard exercise therapy. Another RCT showed that office workers with CLBP achieved better health behavior after 6 weeks of Qigong exercise as well as significantly improved mental state, back function, range of motion, and core muscle strength (Phattharasupharerk et al., 2019). Despite the negative findings of some studies, the fact that CLBP is difficult to manage suggests that TCE could be a possible option for managing pain in middle-aged and elderly patients with CLBP.
Underlying mechanisms of traditional Chinese exercise for improving chronic low back pain
TCE focuses on the integration of mental regulation, breathing, and movement control in addition to internal energy regulation (Zou et al., 2019b).
First, as a foundation of mind–body interaction, meditation and rhythmic breathing can effectively boost vitality and induce energy to flow through the body, which in turn drives body movement to alleviate pain (Zou et al., 2017b). Self-awareness combined with self-correction of posture and movement of the body, flow of breath, and mental stilling activates natural self-regulatory (self-healing) abilities and stimulates a balanced release of endogenous neurohormones and a variety of natural health recovery mechanisms (Jahnke et al., 2010; Linek et al., 2020). Multiple elements of health, including mood, pain, immunity, and peripheral autonomic nervous system function, can be regulated by concentration and mindful meditation (Wayne and Kaptchuk, 2008). Some TCE programs use meditation and imagination to guide and distract attention away from pain, which can help reduce pain and enhance psychosocial health. Evidence indicates that poor pain-related outcomes (e.g., pain levels and disability) have been linked to a higher level of pain catastrophizing (Peng, 2012). Pain-related catastrophizing is a negative cognitive response to pain. For example, Hall et al. found that Tai Chi could help with pain-related symptoms by changing cognitive appraisal results, such as lowing catastrophic outcomes (Hall et al., 2016). Additionally, a recent meta-analysis suggested that adults with chronic diseases obtained reduced muscle pain through mindfulness-based training (Zou et al., 2018b).
Second, TCE relieves pain by combining muscle strength, static balance, and dynamic balance, and these concepts are quite similar to other pain-relieving therapies, such as core stabilization training (Hall et al., 2011; Gordon and Bloxham, 2016). TCE can help relieve back pain by strengthening lumbar muscles and improving pelvic–lumbar neuromuscular function and proprioception. Qigong, Tai Chi, and Wuqinxi involve a series of slow, flowing, dance-like body movements. In particular, combining slow coordinated postures can transfer upper and lower body momentum and achieve balance depending on continuous squatting and weight shifting on both legs throughout the exercise (Zou et al., 2018b). Improvements in lower limb function and lumbar flexibility improved CLBP-related physical activities (i.e., sitting and standing, stair climbing, and walking) (Masharawi and Nadaf, 2013). Compared with taking anti-osteoporosis drugs, Wuqinxi can significantly reduce pain symptoms and increase the bone density of lumbar vertebrae, suggesting the positive effect of Wuqinxi on CLBP (Wei et al., 2015). Our previous work also suggested that Chen-style Wai Chi had protective effects on neuromuscular function in elderly patients with CLBP while relieving non-specific chronic pain (Zou et al., 2019a).
In addition to correcting postural control and enhancing muscle strength to relieve back pain, the pain-relieving effects of TCE may be linked to changes in TCE-induced brain activity. Long-term Tai Chi practice resulted in an increase in cortical thickness of the inferior segment of the circular sulcus of the insula as well as a decrease in the functional homogeneity of the left anterior cingulate cortex (ACC) (Wei et al., 2013, 2014). ACC plays a crucial role in the emotional aspects of pain (Fuchs et al., 2014; Barthas et al., 2015). Inhibiting ACC may help alleviate chronic pain (Gu et al., 2015). The improvement of ACC functional specificity after Tai Chi training may contribute to pain relief, thereby explaining its analgesic effect. An increase cortical thickness of insula observed in long-term Tai Chi practitioners may also contribute to pain relief through better processing of pain-related cognitive information. To uncover the neurological mechanism underlying TCE-mediated pain relief, further studies should be conducted into the direct relationship between pain perception and TCE-mediated alterations in these brain regions.
This systematic review has some limitations. First, it has location and language bias, with five studies from China, two studies from Germany, and only one study from Thailand, the USA, the UK, and Australia, which were all published in English. Second, the TCE intervention differed greatly in terms of exercise type (Tai Chi, Qigong, Wuqinxi), duration (6–24 weeks), frequency (2–5 times/week), and control group. In the future, a detailed categorization of different types of TCE programs and controls will be required. Third, most of the included RCTs did not adopt blind methods (subject, therapist, and assessor blinding), which might lead to biased subjective expectations and exaggerate the research findings. Finally, most RCTs employed followed up for few months only, so the long-term efficacy of TCE in patients with CLBP remains unclear.
Conclusion
This systematic review shows that TCE is beneficial in relieving pain and improving pain-related dysfunction for middle-aged and elderly patients suffering from CLBP. As a convenient, cost-effective therapy with few adverse events, TCE could be recommended for elderly patients with CLBP. Nevertheless, the long-term efficacy of TCE in elderly patients with CLBP must be assessed, and theories on how TCE could treat and prevent CLBP require further investigation. In the future, more controlled studies with larger scale and stricter quality should be conducted to explore the long-term efficacy of TCE in elderly patients with CLBP.
Author contributions
X-QW and H-YX: software, formal analysis, data curation, writing – original draft preparation, visualization, and project administration. LH: conceptualization, methodology, validation, investigation, resources, supervision, and funding acquisition. S-HD and Q-HY: methodology, validation, and writing – review and editing. All authors contributed to the manuscript revision, read, and approved the submitted version.
Footnotes
Funding
This work was supported by the National Natural Science Foundation of China (Nos. 32071061 and 31822025), Shanghai Frontiers Science Research Base of Exercise and Metabolic Health, and Talent Development Fund of Shanghai Municipal (2021081).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnagi.2022.935925/full#supplementary-material
References
- Arnstein P. (2010). Balancing analgesic efficacy with safety concerns in the older patient. Pain Manag. Nurs. 11(Suppl. 2) S11–S22. 10.1016/j.pmn.2010.03.003 [DOI] [PubMed] [Google Scholar]
- Barthas F., Sellmeijer J., Hugel S., Waltisperger E., Barrot M., Yalcin I. (2015). The anterior cingulate cortex is a critical hub for pain-induced depression. Biol. Psychiatry 77 236–245. 10.1016/j.biopsych.2014.08.004 [DOI] [PubMed] [Google Scholar]
- Bernstein I. A., Malik Q., Carville S., Ward S. (2017). Low back pain and sciatica: Summary of NICE guidance. BMJ 356:i6748. 10.1136/bmj.i6748 [DOI] [PubMed] [Google Scholar]
- Blodt S., Pach D., Kaster T., Ludtke R., Icke K., Reisshauer A., et al. (2015). Qigong versus exercise therapy for chronic low back pain in adults–a randomized controlled non-inferiority trial. Eur. J. Pain 19 123–131. 10.1002/ejp.529 [DOI] [PubMed] [Google Scholar]
- Chou R., Turner J. A., Devine E. B., Hansen R. N., Sullivan S. D., Blazina I., et al. (2015). The effectiveness and risks of long-term opioid therapy for chronic pain: A systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann. Intern. Med. 162 276–286. 10.7326/M14-2559 [DOI] [PubMed] [Google Scholar]
- Deyo R. A., Dworkin S. F., Amtmann D., Andersson G., Borenstein D., Carragee E., et al. (2014). Report of the NIH task force on research standards for chronic low back pain. J. Pain 15 569–585. 10.1016/j.jpain.2014.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuchs P. N., Peng Y. B., Boyette-Davis J. A., Uhelski M. L. (2014). The anterior cingulate cortex and pain processing. Front. Integr. Neurosci. 8:35. 10.3389/fnint.2014.00035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon R., Bloxham S. (2016). A systematic review of the effects of exercise and physical activity on non-specific chronic low back pain. Healthcare (Basel) 4:22. 10.3390/healthcare4020022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu L., Uhelski M. L., Anand S., Romero-Ortega M., Kim Y. T., Fuchs P. N., et al. (2015). Pain inhibition by optogenetic activation of specific anterior cingulate cortical neurons. PLoS One 10:e0117746. 10.1371/journal.pone.0117746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y., Xu M., Wei Z., Hu Q., Chen Y., Yan J., et al. (2018). Beneficial effects of qigong wuqinxi in the improvement of health condition, prevention, and treatment of chronic diseases: Evidence from a systematic review. Evid. Based Complement. Alternat. Med. 2018:3235950. 10.1155/2018/3235950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall A. M., Kamper S. J., Emsley R., Maher C. G. (2016). Does pain-catastrophising mediate the effect of tai chi on treatment outcomes for people with low back pain? Complement. Ther. Med. 25 61–66. 10.1016/j.ctim.2015.12.013 [DOI] [PubMed] [Google Scholar]
- Hall A. M., Maher C. G., Lam P., Ferreira M., Latimer J. (2011). Tai chi exercise for treatment of pain and disability in people with persistent low back pain: A randomized controlled trial. Arthritis Care Res. (Hoboken) 63 1576–1583. 10.1002/acr.20594 [DOI] [PubMed] [Google Scholar]
- Hayden J. A., van Tulder M. W., Malmivaara A., Koes B. W. (2005). Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst. Rev. CD000335. 10.1002/14651858.CD000335.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahnke R., Larkey L., Rogers C., Etnier J., Lin F. (2010). A comprehensive review of health benefits of qigong and tai chi. Am. J. Health Promot. 24 e1–e25. 10.4278/ajhp.081013-LIT-248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koes B. W., van Tulder M., Lin C. W., Macedo L. G., McAuley J., Maher C. (2010). An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur. Spine J. 19 2075–2094. 10.1007/s00586-010-1502-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh T. C. (1982). Baduanjin – an ancient Chinese exercise. Am. J. Chin. Med. 10 14–21. 10.1142/S0192415X8200004X [DOI] [PubMed] [Google Scholar]
- Kroenke K., Outcalt S., Krebs E., Bair M. J., Wu J., Chumbler N., et al. (2013). Association between anxiety, health-related quality of life and functional impairment in primary care patients with chronic pain. Gen. Hosp. Psychiatry 35 359–365. 10.1016/j.genhosppsych.2013.03.020 [DOI] [PubMed] [Google Scholar]
- Larkey L., Jahnke R., Etnier J., Gonzalez J. (2009). Meditative movement as a category of exercise: Implications for research. J. Phys. Act. Health 6 230–238. 10.1123/jpah.6.2.230 [DOI] [PubMed] [Google Scholar]
- Lawand P., Lombardi Junior I., Jones A., Sardim C., Ribeiro L. H., Natour J. (2015). Effect of a muscle stretching program using the global postural reeducation method for patients with chronic low back pain: A randomized controlled trial. Joint Bone Spine 82 272–277. 10.1016/j.jbspin.2015.01.015 [DOI] [PubMed] [Google Scholar]
- Leveille S. G., Jones R. N., Kiely D. K., Hausdorff J. M., Shmerling R. H., Guralnik J. M., et al. (2009). Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA 302 2214–2221. 10.1001/jama.2009.1738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linek P., Noormohammadpour P., Mansournia M. A., Wolny T., Sikora D. (2020). Morphological changes of the lateral abdominal muscles in adolescent soccer players with low back pain: A prospective cohort study. J. Sport Health Sci. 9 614–619. 10.1016/j.jshs.2018.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Yeung A., Xiao T., Tian X., Kong Z., Zou L., et al. (2019). Chen-style tai chi for individuals (aged 50 years old or above) with chronic non-specific low back pain: A randomized controlled trial. Int. J. Environ. Res. Public Health 16:517. 10.3390/ijerph16030517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo L., Zou L., Fang Q., Wang H., Liu Y., Tian Z., et al. (2017). Effect of Taichi softball on function-related outcomes in older adults: A randomized control trial. Evid. Based Complement. Alternat. Med. 2017:4585424. 10.1155/2017/4585424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma C., Qu K., Wen B., Zhang Q., Gu W., Liu X., et al. (2020). Clinical effect of “Tai Chi spinal exercise” on spinal motor function in patients with axial spondyloarthritis. Int. J. Clin. Exp. Med. 82 673–681. 10.1016/j.cpr.2020.101928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macedo L. G., Bostick G. P., Maher C. G. (2013). Exercise for prevention of recurrences of nonspecific low back pain. Phys. Ther. 93 1587–1591. 10.2522/ptj.20120464 [DOI] [PubMed] [Google Scholar]
- Mackichan F., Adamson J., Gooberman-Hill R. (2013). ‘Living within your limits’: Activity restriction in older people experiencing chronic pain. Age Ageing 42 702–708. 10.1093/ageing/aft119 [DOI] [PubMed] [Google Scholar]
- Maher C., Underwood M., Buchbinder R. (2017). Non-specific low back pain. Lancet 389 736–747. 10.1016/S0140-6736(16)30970-9 [DOI] [PubMed] [Google Scholar]
- Makris U. E., Abrams R. C., Gurland B., Reid M. C. (2014). Management of persistent pain in the older patient: A clinical review. JAMA 312 825–836. 10.1001/jama.2014.9405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masharawi Y., Nadaf N. (2013). The effect of non-weight bearing group-exercising on females with non-specific chronic low back pain: A randomized single blind controlled pilot study. J. Back Musculoskelet. Rehabil. 26 353–359. 10.3233/BMR-130391 [DOI] [PubMed] [Google Scholar]
- Meyer T., Cooper J., Raspe H. (2007). Disabling low back pain and depressive symptoms in the community-dwelling elderly: A prospective study. Spine (Phila Pa 1976) 32 2380–2386. 10.1097/BRS.0b013e3181557955 [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G., Group P. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuhauser H., Ellert U., Ziese T. (2005). [Chronic back pain in the general population in Germany 2002/2003: Prevalence and highly affected population groups]. Gesundheitswesen 67 685–693. 10.1055/s-2005-858701 [DOI] [PubMed] [Google Scholar]
- Ostelo R. W., de Vet H. C. (2005). Clinically important outcomes in low back pain. Best Pract. Res. Clin. Rheumatol. 19 593–607. 10.1016/j.berh.2005.03.003 [DOI] [PubMed] [Google Scholar]
- Peng M. S., Wang R., Wang Y. Z., Chen C. C., Wang J., Liu X. C., et al. (2022). Efficacy of therapeutic aquatic exercise vs physical therapy modalities for patients with chronic low back pain: A randomized clinical trial. JAMA Netw. Open 5:e2142069. 10.1001/jamanetworkopen.2021.42069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng P. W. (2012). Tai chi and chronic pain. Reg. Anesth. Pain Med. 37 372–382. 10.1097/AAP.0b013e31824f6629 [DOI] [PubMed] [Google Scholar]
- Phattharasupharerk S., Purepong N., Eksakulkla S., Siriphorn A. (2019). Effects of Qigong practice in office workers with chronic non-specific low back pain: A randomized control trial. J. Bodyw. Mov. Ther. 23 375–381. 10.1016/j.jbmt.2018.02.004 [DOI] [PubMed] [Google Scholar]
- Qaseem A., Wilt T. J., McLean R. M., Forciea M. A. Clinical Guidelines Committee of the American College of Physicians Denberg T. D., et al. (2017). Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American college of physicians. Ann. Intern. Med. 166 514–530. 10.7326/M16-2367 [DOI] [PubMed] [Google Scholar]
- Rundell S. D., Sherman K. J., Heagerty P. J., Mock C. N., Dettori N. J., Comstock B. A., et al. (2017). Predictors of persistent disability and back pain in older adults with a new episode of care for back pain. Pain Med. 18 1049–1062. 10.1093/pm/pnw236 [DOI] [PubMed] [Google Scholar]
- Russo M., Deckers K., Eldabe S., Kiesel K., Gilligan C., Vieceli J., et al. (2018). Muscle control and non-specific chronic low back pain. Neuromodulation 21 1–9. 10.1111/ner.12738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman K. J., Wellman R. D., Hawkes R. J., Phelan E. A., Lee T., Turner J. A. (2020). T’ai Chi for chronic low back pain in older adults: A feasibility trial. J. Altern. Complement. Med. 26 176–189. 10.1089/acm.2019.0438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherwin D. C. (1992). Traditional Chinese medicine in rehabilitation nursing practice. Rehabil. Nurs. 17 253–255. 10.1002/j.2048-7940.1992.tb01560.x [DOI] [PubMed] [Google Scholar]
- Smith J. A., Stabbert H., Bagwell J. J., Teng H. L., Wade V., Lee S. P. (2022). Do people with low back pain walk differently? A systematic review and meta-analysis. J. Sport Health Sci. 11 450–465. 10.1016/j.jshs.2022.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffens D., Maher C. G., Pereira L. S., Stevens M. L., Oliveira V. C., Chapple M., et al. (2016). Prevention of low back pain: A systematic review and meta-analysis. JAMA Intern. Med. 176 199–208. 10.1001/jamainternmed.2015.7431 [DOI] [PubMed] [Google Scholar]
- Stochkendahl M. J., Kjaer P., Hartvigsen J., Kongsted A., Aaboe J., Andersen M., et al. (2018). National clinical guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. Eur. Spine J. 27 60–75. 10.1007/s00586-017-5099-2 [DOI] [PubMed] [Google Scholar]
- Taylor J. B., Goode A. P., George S. Z., Cook C. E. (2014). Incidence and risk factors for first-time incident low back pain: A systematic review and meta-analysis. Spine J. 14 2299–2319. 10.1016/j.spinee.2014.01.026 [DOI] [PubMed] [Google Scholar]
- Teut M., Knilli J., Daus D., Roll S., Witt C. M. (2016). Qigong or yoga versus no intervention in older adults with chronic low back pain-a randomized controlled trial. J. Pain 17 796–805. 10.1016/j.jpain.2016.03.003 [DOI] [PubMed] [Google Scholar]
- Viniol A., Jegan N., Leonhardt C., Brugger M., Strauch K., Barth J., et al. (2013). Differences between patients with chronic widespread pain and local chronic low back pain in primary care–a comparative cross-sectional analysis. BMC Musculoskelet. Disord. 14:351. 10.1186/1471-2474-14-351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X. Q., Huang L. Y., Liu Y., Li J. X., Wu X., Li H. P., et al. (2013). Effects of tai chi program on neuromuscular function for patients with knee osteoarthritis: Study protocol for a randomized controlled trial. Trials 14:375. 10.1186/1745-6215-14-375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wayne P. M., Kaptchuk T. J. (2008). Challenges inherent to t’ai chi research: Part I–t’ai chi as a complex multicomponent intervention. J. Altern. Complement. Med. 14 95–102. 10.1089/acm.2007.7170A [DOI] [PubMed] [Google Scholar]
- Wei G. X., Dong H. M., Yang Z., Luo J., Zuo X. N. (2014). Tai Chi Chuan optimizes the functional organization of the intrinsic human brain architecture in older adults. Front. Aging Neurosci. 6:74. 10.3389/fnagi.2014.00074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei G. X., Xu T., Fan F. M., Dong H. M., Jiang L. L., Li H. J., et al. (2013). Can Taichi reshape the brain? A brain morphometry study. PLoS One 8:e61038. 10.1371/journal.pone.0061038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei X., Xu A., Yin Y., Zhang R. (2015). The potential effect of Wuqinxi exercise for primary osteoporosis: A systematic review and meta-analysis. Maturitas 82 346–354. 10.1016/j.maturitas.2015.08.013 [DOI] [PubMed] [Google Scholar]
- Weiner D. K., Rudy T. E., Morrow L., Slaboda J., Lieber S. (2006a). The relationship between pain, neuropsychological performance, and physical function in community-dwelling older adults with chronic low back pain. Pain Med. 7 60–70. 10.1111/j.1526-4637.2006.00091.x [DOI] [PubMed] [Google Scholar]
- Weiner D. K., Sakamoto S., Perera S., Breuer P. (2006b). Chronic low back pain in older adults: Prevalence, reliability, and validity of physical examination findings. J. Am. Geriatr. Soc. 54 11–20. 10.1111/j.1532-5415.2005.00534.x [DOI] [PubMed] [Google Scholar]
- Weifen W., Muheremu A., Chaohui C., Md L. W., Lei S. (2013). Effectiveness of Tai Chi practice for non-specific chronic low back pain on retired athletes: A randomized controlled study. J. Musculoskelet. Pain 21 37–45. 10.3109/10582452.2013.763394 [DOI] [Google Scholar]
- Wieland L. S., Skoetz N., Pilkington K., Vempati R., D’Adamo C. R., Berman B. M. (2017). Yoga treatment for chronic non-specific low back pain. Cochrane Database Syst. Rev. 1:CD010671. 10.1002/14651858.CD010671.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong J. J., Cote P., Sutton D. A., Randhawa K., Yu H., Varatharajan S., et al. (2017). Clinical practice guidelines for the noninvasive management of low back pain: A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) collaboration. Eur. J. Pain 21 201–216. 10.1002/ejp.931 [DOI] [PubMed] [Google Scholar]
- Wu B., Zhou L., Chen C., Wang J., Hu L. I., Wang X. (2022). Effects of exercise-induced hypoalgesia and its neural mechanisms. Med. Sci. Sports Exerc. 54 220–231. 10.1249/MSS.0000000000002781 [DOI] [PubMed] [Google Scholar]
- Xiong H. Y., Zheng J. J., Wang X. Q. (2022). Non-invasive brain stimulation for chronic pain: State of the art and future directions. Front. Mol. Neurosci. 15:888716. 10.3389/fnmol.2022.888716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao C., Li Z., Zhang S., Wu Z., Zhu Q., Fang L. (2020). Effects of Wuqinxi in the Patients with chronic low back pain: A randomized controlled trial. Evid. Based Complement. Alternat. Med. 2020:1428246. 10.1155/2020/1428246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S., Kong L., Zhu Q., Wu Z., Li J., Fang M., et al. (2020). Efficacy of Tuina in patients with chronic low back pain: Study protocol for a randomized controlled trial. Trials 21:271. 10.1186/s13063-020-4198-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Loprinzi P. D., Yang L., Liu J., Liu S., Zou L. (2019). The Beneficial effects of traditional chinese exercises for adults with low back pain: A meta-analysis of randomized controlled trials. Medicina (Kaunas) 55:118. 10.3390/medicina55050118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Q., Huang L., Wu X., Wang L., Zhang Y., Fang M., et al. (2016). Effects of Tai Ji Quan training on gait kinematics in older Chinese women with knee osteoarthritis: A randomized controlled trial. J. Sport Health Sci. 5 297–303. 10.1016/j.jshs.2016.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou L., Wang C., Tian Z., Wang H., Shu Y. (2017a). Effect of yang-style Tai Chi on gait parameters and musculoskeletal flexibility in healthy Chinese older women. Sports (Basel) 5:52. 10.3390/sports5030052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou L., Wang H., Xiao Z., Fang Q., Zhang M., Li T., et al. (2017b). Tai chi for health benefits in patients with multiple sclerosis: A systematic review. PLoS One 12:e0170212. 10.1371/journal.pone.0170212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou L., Yeung A., Li C., Wei G. X., Chen K. W., Kinser P. A., et al. (2018a). Effects of meditative movements on major depressive disorder: A systematic review and meta-analysis of randomized controlled trials. J. Clin. Med. 7:195. 10.3390/jcm7080195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou L., Yeung A., Zeng N., Wang C., Sun L., Thomas G. A., et al. (2018c). Effects of mind-body exercises for mood and functional capabilities in patients with stroke: An Analytical review of randomized controlled trials. Int. J. Environ. Res. Public Health 15:721. 10.3390/ijerph15040721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou L., Yeung A., Quan X., Boyden S. D., Wang H. (2018b). A systematic review and meta-analysis of mindfulness-based (Baduanjin) exercise for alleviating musculoskeletal pain and improving sleep quality in people with chronic diseases. Int. J. Environ. Res. Public Health 15:206. 10.3390/ijerph15020206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou L., Zhang Y., Liu Y., Tian X., Xiao T., Liu X., et al. (2019a). The effects of Tai Chi Chuan versus core stability training on lower-limb neuromuscular function in aging individuals with non-specific chronic lower back pain. Medicina (Kaunas) 55:60. 10.3390/medicina55030060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou L., Zhang Y., Sasaki J. E., Yeung A. S., Yang L., Loprinzi P. D., et al. (2019b). Wuqinxi Qigong as an alternative exercise for improving risk factors associated with metabolic syndrome: A meta-analysis of randomized controlled trials. Int. J. Environ. Res. Public Health 16:1396. 10.3390/ijerph16081396 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.