Abstract
Monkeypox is a zoonotic Orthopoxvirus infection usually present in regions of Africa. Recent outbreaks of Monkeypox infection have been reported in non endemic region and human-to-human contact is believed to be the main driver for propagation. While the disease is usually self-contained, severe complications, such as neurological and ocular involvements may arise. We report the case of a 34-year-old male who presented with myocarditis and concurrent genital Monkeypox infection. Other usual causes of myocardial injury were ruled out. We believe it to be the first documented case of myocarditis secondary to Monkeypox. We report a new complication of the disease and the possible underlying mechanisms. Our case report raises awareness about possible unknown complications of Monkeypox as outbreaks continue to happen around the world.
Keywords: Myocarditis, Monkeypox
Introduction
Monkeypox (MPX) is a zoonotic Orthopoxvirus infection that is endemic in central and western Africa. Recently, outbreaks of MPX infection in non endemic region have been reported in several western countries [1], [2]. Symptoms include an initial flu-like prodrome lasting up to five days and are usually followed by the appearance of characteristic, well defined, deep-seated lesions which often develop umbilication, more frequently on the palms of the hands and soles of the feet [3]. As new cases of the disease are reported, new symptomatology has recently been associated with the infection. The ongoing outbreak seems to be mediated by person-to-person contact, especially between men having sex with men, which suggests close contact with infectious material as the main risk factor for transmission [4], [5]. While MPX infections are usually self-limited, severe complications such as secondary infection, encephalitis and infection of the cornea with loss of vision can also occur [6].
Case report
On June 28th, 2022, a 34-year-old male presented to the emergency room (ER) of the Centre Hospitalier de l′Université de Montréal, Canada, with a 48-h history of fever and chills, and 24-h history of chest pain. He denied any prior medical conditions or allergies and was not taking any medication. He had a history of tobacco and methamphetamine use. Upon checking into the ER, he was administered a COVID-19 PCR test, which came back negative, and was put into a standard ER room.
The chest pain reported by the patient was constant, sharp, and pleuritic, without radiation, relieved when sitting upright and worse when lying down. The intensity of the pain increased over 24 h which prompted him to consult at the ER. He had tried taking methamphetamine “in an attempt to relieve his symptoms”, without success. He denied taking any drugs during the hours and days before the onset of the chest pain.
The physical examination revealed an oral temperature of 38.8 °C, blood pressure of 95/65 mmHg, pulse of 116 beats per minute, and oxygen saturation of 97 % on room air. Pulmonary and cardiac examination revealed no abnormalities.
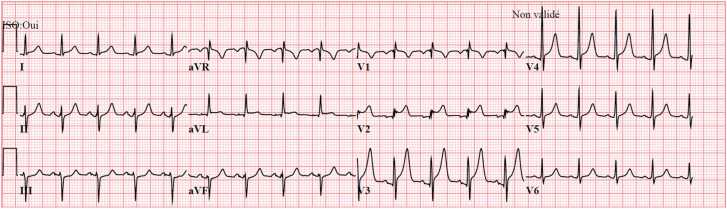
An ECG was performed, demonstrating sinus tachycardia with antero-lateral concave ST elevation compatible with pericarditis. Fig. 1. A chest x-ray was obtained which revealed non-specific retro-cardiac opacities. Initial blood analysis revealed a C-reactive protein at 154.5 mg/L, an elevated white blood cell count (WBC) of 13.9 * 109/L and initial high-sensitivity troponins at 211 ng/L. Other lab results are shown in Table 1. Given the patient’s fever and elevated WBC, blood cultures were collected, and an antibiotic (piperacillin-tazobactam) was empirically initiated.
Fig. 1.
ECG on arrival. Antero-lateral concave ST elevation compatible with pericarditis.
Table 1.
Laboratory results.
| Variable | Reference range | On admission | Hospital day 2 | Hospital day 3 | Hospital day 4 | Hospital day 5 | Hospital day 6 | Hospital day 7 |
|---|---|---|---|---|---|---|---|---|
| Hemoglobin (g/L) | 130–170 | 143 | 133 | 137 | 135 | 138 | ||
| White cells (× 109/L) | 4.0–10.0 | 13.9 | 6.1 | 5.5 | 7.6 | 11.5 | ||
| Neutrophils (× 109/L) | 2.0–7.0 | 10.2 | 3.1 | 2.5 | 3.8 | 6.4 | ||
| Lymphocytes (x109/L) | 1.0–4.0 | 1.5 | 1.7 | 1.8 | 2.6 | 3.2 | ||
| Monocytes (× 109/L) | 0.1–1.0 | 2.0 | 0.8 | 0.6 | 0.7 | 1.0 | ||
| Eosinophils (× 109/L) | 0.00–0.45 | 0.10 | 0.40 | 0.40 | 0.50 | 0.70 | ||
| Platelets | 130–400 | 205 | 271 | 290 | 355 | 377 | ||
| Sodium (mmol/L) | 135–145 | 130 | 138 | 141 | 143 | 141 | 141 | |
| Potassium (mmol/L) | 3.5–5.0 | 4.0 | 3.9 | 4.0 | 4.0 | 3.8 | 4.1 | |
| Creatinine (µmol/L) | 53–112 | 79 | 86 | 70 | 65 | 74 | 70 | |
| C-reactive protein (mg/L) | ≤ 10 | 154.5 | 116.8 | 82.9 | 47.3 | 32.9 | 22.8 | |
| Troponin (ng/L) | ≤ 20 | 211.5 ->181 | 8186.1 | 2500.9 | 1390.8 | 210.4 | 54.2 | 25.6 |
| NT pro-BNP (ng/L) | < 300: acute heart failure unlikely 300–450 acute heart failure possible > 450 acute heart failure probable |
283 |
After being assessed by cardiology, the presumptive diagnosis at that point was a myopericarditis of unknown etiology. Antibiotics were discontinued, followed by initiation of ibuprofen and colchicine on June 28th.
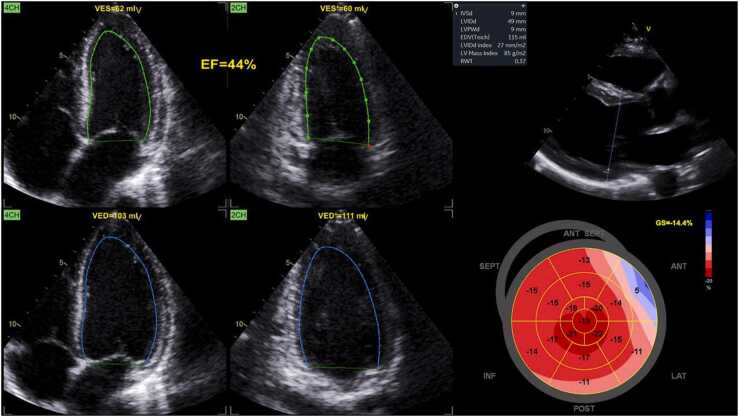
On June 29th, a trans-thoracic echocardiogram was performed, demonstrating a normal left ventricle (LV) size, a slightly reduced LV ejection fraction of 44 % with reduced global longitudinal strain (− 14.4 %), especially in the anterior and lateral walls. Fig. 2. The pulmonary artery pressure was normal as was the right ventricular function. There was no significant valvulopathy. Of note, no pericardial effusion was visualized. After the echocardiogram, high sensitivity troponins were repeated and had increased up to 8186 ng/L. The patient promptly underwent a coronary angiogram which showed no coronary artery disease and no signs of vasospasm. The patient was admitted to cardiology with continuous cardiac telemetry.
Fig. 2.
Trans-thoracic Echocardiogram performed the day after the presentation. Diffuse mild left ventricular systolic dysfunction, more important at the apex. Left ventricular ejection fraction is measured at 44 %.
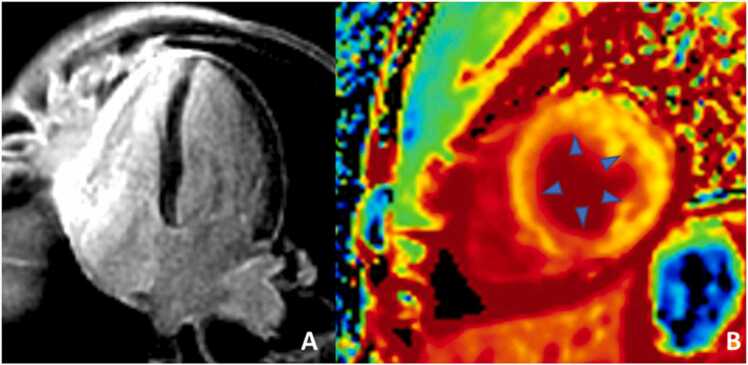
On June 30th, a cardiac MRI confirmed that the LV ejection fraction was mildly reduced with mild LV dilation. There was no late gadolinium enhancement. Fig. 3. Despite respiratory artifacts, T2 values suggested possible myocardial edema. Similarly, high extra cellular volumes values were also suggestive of myocardial edema and/or injury. Thus, the presumptive diagnosis remained a myocarditis of unknown etiology. An ACE inhibitor was initiated for LV dysfunction, but beta-blockade was avoided since the patient had polysubstance abuse disorder.
Fig. 3.
Cardiac MRI confirmed the mildly reduced ejection fraction. It demonstrated also a limited late gadolinium enhancement at the apex (left) as well as high T2 and extracellular volume values compatible with edema and injury of the myocardium (middle and right). No pericardial involvement was reported.
The same day, upon further interrogation for possible causes of myocarditis, the patient mentioned the presence of genital lesions that had appeared for the first time on June 25th. A careful examination revealed a well-circumscribed, umbilicated papule located on the pubis, as well as an ulcerated lesion on the glans penis. Additionally, inguinal lymph nodes were enlarged and painful to palpation bilaterally. The patient, who identifies himself as a heterosexual male, reported unprotected intercourse with a new female partner approximately 1–3 weeks prior to the onset of the genital lesions. Upon further questioning, he mentioned that he had stayed at a friend’s house two weeks earlier, who he presumed was homosexual, and was in contact with soiled linens.
Samples of the lesions were collected and sent for PCR analysis. The lesion on the glans was tested for HSV-1, HSV-2 and VZV, while the pubic lesion was tested for Simian Orthopoxvirus, the aspect being consistent with MPX. The patient was empirically started on acyclovir prior to obtaining the results and was moved to a negative pressure isolation room. Additionally, he was empirically treated with a standard dose of Ceftriaxone and Azithromycin pending the results of a routine screening panel for sexually transmitted infections, which later came back positive for Chlamydia and negative for Gonorrhea, HIV and syphilis.
On July 2nd, results confirmed the presence of Simian Orthopoxvirus in the pubic lesion. Considering the potential association of MPX and subsequent myocarditis, the patient was started on Tecovirimat for a duration of 14 days, as recommended by the CDC guidelines. Acyclovir was discontinued once HSV-1, HSV-2 and VZV PCR tests came back negative on July 5th. The patient clinical condition improved in the following days. No sign of neurological, corneal or other complications were identified. The crusted lesions as well as the inguinal adenopathy resolved on July 6th, at which point the patient was removed from his isolation and returned to a normal-pressure room. Inflammatory markers followed clinical improvement with decrease in CRP and troponins. The patient remained afebrile throughout the remainder of his hospital stay and did not develop any sign of heart failure.
Unfortunately, on July 7th, the patient left against medical advice prior to undergoing his control cardiac MRI. Before leaving, the patient was counseled regarding the need to remain isolated until complete disappearance of the lesions, as well as the use of proper barrier protection methods during intercourse.
Discussion
Our case presented with pericarditis-like chest pain, an important rise in troponins and ECG changes compatible with myopericarditis. While our suspicion for ischemic heart disease was low given the symptomatology and the age of the patient, it was still ruled out with a coronary angiogram. Other confounding factors such as methamphetamine use were present. Though this drug can cause coronary vasospasm and a rise in troponins, the consumption occurred after the onset of the symptoms which makes this hypothesis less likely [7]. Thus, given the presence of concurrent genital infection, the diagnosis of viral myocarditis seemed most probable. The patient’s clinical presentation, its ECG, the correlating mild left ventricular systolic dysfunction as well as edema on cardiac MRI (which took place 12 h after the troponin peak) were sufficient to confirm our diagnosis. A myocardial biopsy was not performed given the risks of the procedure as well as the unlikelihood of the results changing current management.
This case report outlines a possible association between MPX and myocarditis. As of writing this case report, a literature review found no previous publication outlining this potential association. Although many cases of myopericarditis are labeled as idiopathic, viral etiologies are presumably involved in most cases, although often not identified in a clinical setting [8], [9]. Herpes simplex infection has been associated with pericarditis [10]. Still, in this case, acute genital Herpes infection was ruled out by PCR testing, which makes an HSV myocarditis highly unlikely.
Myocarditis has been associated with smallpox vaccination. As Orthopoxviruses are closely related to the vaccinia virus used for vaccination, it is plausible that MPX could be associated with myocarditis as well. Some studies have reported a strong incidence rate of myocarditis after receiving a Smallpox vaccine, such as ACAM2000, a live replicating vaccine and JYNNEOS, a live non-replicating vaccine, though the exact mechanism remains unclear [11], [12]. The incidence of confirmed myocarditis secondary to smallpox vaccination is estimated to be 12 per 100,000 people in a review including 730,000 services members conducted by the United States Department of Defense [11]. Data in US service members cohorts also suggest the actual incidence rate of myocarditis secondary to smallpox vaccine could be as high as 10 %, reporting new onset chest pain, dyspnea, and/or palpitations in 10.6 % of smallpox vaccines up to 30 days after vaccination [13].
The JYNNEOS vaccine uses the Vaccinia virus as the inoculating agent, because of its similarity with the smallpox virus. This vaccine has also been demonstrated to be effective in protecting against MPX [14]. The CDC and the WHO reported an efficacy of up to 85% in protecting against Monkeypox, based on past data from Africa, clinical studies of the immunogenicity of the vaccine and efficacy data from animal studies. Hence, CDC recommends the administration of Smallpox vaccines as pre-exposure prophylaxis in individuals with high-risk exposure [15]. Some experts also suggest the administration of the vaccine after exposure could decrease the intensity and duration of symptoms, but not prevent the disease altogether. The similarity of those two agents suggests a possible association between Monkeypox and myocarditis.
While our case evolved favorably, it remains difficult to assess the effect of Tecovirimat on the myocardial inflammation without a follow-up cardiac MRI. This exam could also have helped in confirming and further documenting the extent of myocardial inflammation and edema, which can sometimes be delayed before appearing on cardiac MRI.
Conclusion
Our report outlines the first documented case of concomitant Simian Orthopoxvirus infection and myocarditis. While more data is needed to further evaluate the incidence of myocarditis as a complication of MPX, it raises important questions and hypothesizes on the possible association between these two clinical entities. More importantly, the effect of Tecovirimat as a potential treatment for MPX associated myocarditis remains unclear at this point. In the context of a current monkeypox outbreak, this report also outlines the importance of searching for signs of viral infections when patients present with a diagnosis of myocarditis, to better orient the treatment but also to prevent transmission within communities, by putting in place proper isolation measures.
Credit authorship contribution statement
All authors contributed equally.
Ethical approval
This case report was conducted in accordance with the fundamental principles of the Declaration of Helsinki.
Consent
The patient provided consent for this publication.
Conflict of interest
The authors report no declarations of interest.
Acknowledgements
Dre Tremblay is chairholder for the Pfizer Chair in Clinical and Translational Research on HIV at the Université de Montréal.
Dr Tournoux is a clinical researcher for the Fonds de Recherche du Québec – Santé.
No funding was used in the process of writing this paper.
References
- 1.Control European Centre for Disease Prevention and. Monkeypox cases reported in UK and Portugal; 2022. 〈https://www.ecdc.europa.eu/en/news-events/monkeypox-cases-reported-uk-and-portugal〉.
- 2.Minhaj F.S., Ogale Y.P., Whitehill F., et al. Monkeypox outbreak – nine states, May 2022. MMWR Morb Mortal Wkly Rep. 2022;71(23):764–769. doi: 10.15585/mmwr.mm7123e1. [(In eng)] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prevention Centers for Disease Control and. Monkeypox virus infection in the United States and other non-endemic countries; 2022. 〈https://emergency.cdc.gov/han/2022/han00466.asp〉.
- 4.Organization World Health. Multi-country monkeypox outbreak in non endemic-countries; 2022. 〈https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON385〉.
- 5.Prevention Centers for Disease Control and. Case identified after monkeypox clusters in several other countries; 2022. 〈https://www.cdc.gov/media/releases/2022/s0518-monkeypox-case.html〉.
- 6.Organization World Health. Monkeypox; 2022. 〈https://www.who.int/news-room/fact-sheets/detail/monkeypox〉.
- 7.Kevil Christopher G., Goeders Nicholas E., Woolard Matthew D., et al. Methamphetamine use and cardiovascular disease. Arterioscler Thromb Vasc Biol. 2019;39(9):1739–1746. doi: 10.1161/ATVBAHA.119.312461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bowles N.E., Ni J., Kearney D.L., et al. Detection of viruses in myocardial tissues by polymerase chain reaction. Evidence of adenovirus as a common cause of myocarditis in children and adults. J Am Coll Cardiol. 2003;42(3):466–472. doi: 10.1016/s0735-1097(03)00648-x. [(In eng)] [DOI] [PubMed] [Google Scholar]
- 9.Cooper L.T., Jr. Myocarditis. N Engl J Med. 2009;360(15):1526–1538. doi: 10.1056/NEJMra0800028. [(In eng)] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Breinholt J.P., Moulik M., Dreyer W.J., et al. Viral epidemiologic shift in inflammatory heart disease: the increasing involvement of parvovirus B19 in the myocardium of pediatric cardiac transplant patients. J Heart Lung Transpl. 2010;29(7):739–746. doi: 10.1016/j.healun.2010.03.003. [(In eng)] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keinath K., Church T., Kurth B., Hulten E. Myocarditis secondary to smallpox vaccination. BMJ Case Rep. 2018;2018 doi: 10.1136/bcr-2017-223523. [(In eng)] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Halsell Jeffrey S., Riddle James R., Atwood J.Edwin, et al. Myopericarditis following smallpox vaccination among vaccinia-naive US military personnel. JAMA. 2003;289(24):3283–3289. doi: 10.1001/jama.289.24.3283. [DOI] [PubMed] [Google Scholar]
- 13.Engler R.J., Nelson M.R., Collins L.C., Jr., et al. A prospective study of the incidence of myocarditis/pericarditis and new onset cardiac symptoms following smallpox and influenza vaccination. PLoS One. 2015;10(3) doi: 10.1371/journal.pone.0118283. [(In eng)] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rao A.K., Petersen B.W., Whitehill F., et al. Use of JYNNEOS (Smallpox and Monkeypox Vaccine, Live, Nonreplicating) for preexposure vaccination of persons at risk for occupational exposure to orthopoxviruses: recommendations of the advisory committee on immunization practices – United States, 2022. MMWR Morb Mortal Wkly Rep. 2022;71(22):734–742. doi: 10.15585/mmwr.mm7122e1. [(In eng)] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prevention Centers for Disease Control and. Monkeypox and smallpox vaccine guidance; 2022. 〈https://www.cdc.gov/poxvirus/monkeypox/clinicians/smallpox-vaccine.html〉.