Abstract
Background
The clinical outcomes of single-level anterior cervical discectomy and fusion (ACDF) with the Zero-profile (Zero-p) were evaluated in comparison with the anterior cervical cage–plate construct (CPC).
Methods
We performed a systematic search covering PubMed, Embase, Cochrane Central Register of Controlled Trials, Web of Science, Medline, China National Knowledge Infrastructure (NCKI), Wan Fang Database, and Wei Pu Database. Articles focused on single-level ACDF or data of the single - level that can be extracted were included, and articles that did not directly compare Zero-p and CPC were excluded. Twenty-seven studies were included with a total of 1866 patients, 931 in the Zero-p group and 935 in the CPC group. All outcomes were analyzed using Review Manager 5.4.
Results
The meta-analysis outcomes indicated that operative time (WMD = − 12.47, 95% CI (− 16.89, − 8.05), P < 0.00001), intraoperative blood loss (WMD = − 13.30, 95% CI (− 18.83, − 7.78), P < 0.00001), risk of adjacent segment degeneration (ASD) (OR 0.31, 95% CI (0.20, 0.48), P < 0.0001), risk of dysphagia of short-term (OR 0.40, 95% CI (0.30, 0.54), P < 0.0001), medium-term (OR 0.31, 95% CI (0.20, 0.49), P < 0.0001), and long-term (OR 0.29, 95% CI (0.17, 0.51), P < 0.0001) of Zero-p group were significantly lower. The JOA score of Zero-p group at the final follow-up was significantly higher (WMD = − 0.17, 95% CI (− 0.32, − 0.03), P = 0.02). There were no significant differences in length of stay (LOS), Neck Disability Index (NDI), Visual Analogue Score (VAS), fusion rate, segmental Cobb angle, cervical Cobb angle, prevertebral soft tissue thickness (PSTT), SF-36, subsidence, implant failure, and hoarseness between the two groups. This study was registered with PROSPERO, CRD42022347146.
Conclusion
Zero-p group reduced operative time, intraoperative blood loss, JOA score at follow-up and reduced the incidence of dysphagia and postoperative ASD, but the two devices had the same efficacy in restoring the cervical curvature, preventing the cage subsidence, and in postoperative VAS, NDI, LOS, PSTT, SF-36, fusion rate, implant failure, and hoarseness in single-level ACDF. The use of Zero-p in single-level ACDF was recommended.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13018-022-03387-9.
Keywords: Single level, Zero-profile, Anterior cervical discectomy and fusion, ACDF, Clinical outcome
Background
The number of patients who need surgical treatment with degenerative cervical spondylosis (DCS) has increased in recent years [1]. Since it was introduced by Cloward in 1958 [2], anterior cervical discectomy and fusion (ACDF) has been the gold-standard surgical technique for both single- and multi-level DCS [3]. The anterior cage and plate construct (CPC), which can be utilized for single- and multi-level cervical spondylosis, is a commonly adopted surgical device. Its superior stability, decompression rate, and fusion rate have been endorsed in great amount of studies; therefore, it is widely used in clinical practice [4]. However, complications such as a higher incidence rate of postoperative dysphagia and adjacent segment degeneration (ASD) have been documented [5, 6].
A Zero-profile interbody spacer (Zero-p) is presently being utilized in clinical trials to reduce the risk of the aforementioned complications. The Zero-p, unlike the CPC, can be inserted into the intervertebral space without the necessity for an extra titanium plate in front of the vertebral body. It has been proven in several studies to greatly reduce the incidence of postoperative dysphagia and ASD [7–10]. This may be due to its integrated design, which does not protrude the front rim of the cervical vertebrate [11]. However, the literature shows that the Zero-p cannot effectively maintain intervertebral height and cervical curvature after the surgery when compared to the CPC [12]. According to the biomechanical study of Li et al. [13], the range of motion (ROM) and maximum stress of the Zero-p were lower than those of CPC.
Recently, several studies have compared the clinical and radiological outcomes of Zero-p and CPC in ACDF for treating multi-level DCS. However, there was no meta-analysis comparing the Zero-p and CPC in single-level ACDF with complete outcomes was found. The goal of this study is to compare the clinical and radiological results of the Zero-p and CPC in ACDF for single-level DSC to provide complete evidence to support the use of Zero-p in the single-level ACDF.
Methods
Literature search
Our research follows the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) standards [14, 15]. Two independent investigators (Kahaer and Chen) investigated electronic databases or platforms (PubMed, Embase, Cochrane Central Register of Controlled Trials, Web of Science, Medline, NCKI, Wan Fang Database, and Wei Pu Database). The search was conducted with the following searching strategy as follows: “zero profile,” “Zero-profile,” “Zero-p,” “zero p,” “no-profile,” “anchored,” “ROI-C,” “self-locking,” “ACDF,” “anterior cervical discectomy and fusion” with various combinations of the “AND,” “NOT,” and “OR.” We restricted the language to English and Chinese. By preserving the literature that offered the most comprehensive information for overlapping patients, information duplication was avoided.
Selection criteria
The inclusion criteria were as follows: (1) the literature compared patients with DSC who underwent the single-level ACDF using Zero-p and CPC and (2) the literature reported one of the followings: operative time, Intraoperative blood loss, length of stay (LOS), Neck Disability Index (NDI), Japanese Orthopaedic Association (JOA) score, Visual Analogue Score (VAS), prevertebral soft tissue thickness (PSTT), 36-Item Short Form Survey (SF-36), segmental and cervical Cobb angle, fusion rate, adjacent segment degeneration (ASD), cage subsidence, dysphagia, implant failure, hoarseness.
The exclusion criteria were as follows: (1) There was no evidence of the Zero-p or CPC or ACDF, (2) literature reviews, meeting abstracts, pathology reports, conference reports, editorials, expert opinions, animal trials, autopsies, meta-analyses, case reports, biomechanical studies, and other associated investigations, (3) the literature in which data cannot be extracted, (4) presence of infection, tumor, history of previous cervical spine surgery, severe ossification of the posterior longitudinal ligament, and (5) the literature of two or multi-level ACDF.
Quality assessment and data extraction
Using a predesigned data extraction sheet, pairs of authors (Kahaer and Chen) independently extracted data from the included literature. Non-randomized controlled studies used Newcastle–Ottawa Scale (NOS) to evaluate the quality. A maximum of 9 points and greater than 6 were considered the high-quality literature. Randomized controlled trials (RCTs) used the Delphi list to evaluate the quality. Two authors independently assessed the quality of each study and then cross-checked, with a third evaluator (Maitusong) handling any disagreements. Authors, publication date, title, study design, indications, fusion levels, follow-up time, number of patients, mean age of patients, design of the Zero-p device, and clinical outcomes were extracted from the qualified literature. This study was registered with PROSPERO, CRD42022347146.
Statistical analysis
Data analysis was performed using Review Manager Software (RevMan 5.4, The Cochrane Collaboration). Continuous data including operative time, intraoperative blood loss, LOS, NDI, JOA, VAS, PSTT, SF-36, segmental Cobb angle, and cervical Cobb angle were analyzed using weighted mean differences (WMD) and 95% confidence intervals (CI). Dichotomous outcomes including fusion, adjacent segment degeneration (ASD), cage subsidence, dysphagia, implant failure, and hoarseness were analyzed using the odds ratio (OR). Heterogeneity between studies was tested using the I2 statistic. When the I2 > 50% (high heterogeneity), a random effect model was used. If it was ≤ 50% (low heterogeneity), a fixed-effect model was used. A funnel plot was also used to assess publication bias. P < 0.05 was considered statistically significant.
Results
Literature search
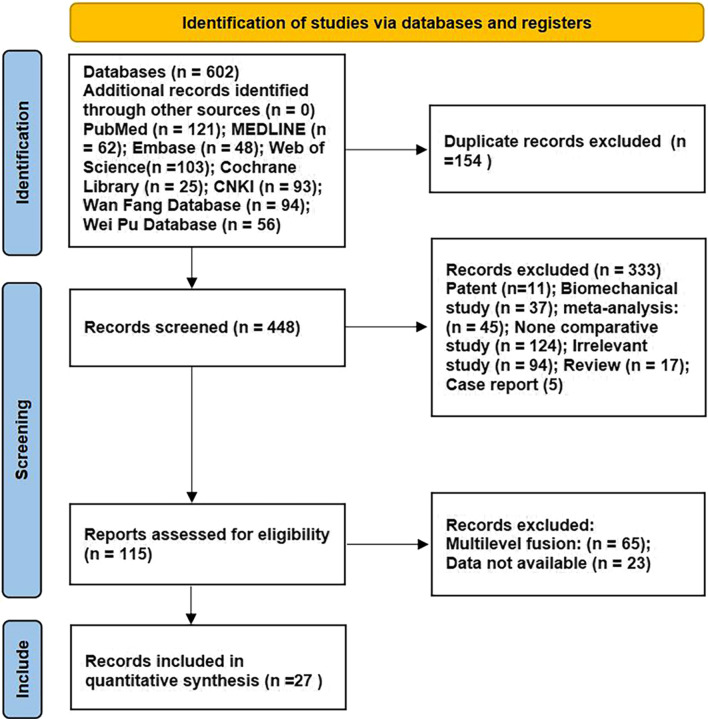
There were 602 studies which were searched from 8 electronic databases (PubMed, n = 121; Embase, n = 48; Cochrane Central Register of Controlled Trials, n = 25; Web of Science, n = 103; Medline, n = 62; NCKI, n = 93; Wan Fang Database, n = 94; Wei Pu Database, n = 56). Of these, 154 were duplicates and 448 were excluded after the title and abstract screening. After careful full-text evaluation, as a result, 27 studies including English and Chinese were included [7–11, 16–37] and data were extracted. A flow diagram of the literature searching strategy is shown in Fig. 1.
Fig. 1.
Flow diagram of study selection
Literature characteristic and quality assessment
Four prospective RCTs [20, 22, 26, 30] and 23 retrospective observational literature [7, 8, 10, 11, 16–19, 21, 23–25, 27–29, 31–38] were included. A total of 931 patients with Zero-p and 935 patients with CPC were compared. The design of the Zero-p devices was as follows: Zero-p (DePuy, Synthes, USA), Zero-p (Synthes GmbH, Oberdorf, Switzerland), and Zero-p (Synthes, Zuchwil, Switzerland), ROI-C, and PREVAIL (Medtronic Sofamor Danek, Memphis, TN, USA). The differences in the patient’s age, BMD, BMI, and follow-up time were not significant (Additional file 1). The basic characteristics and demographics are presented in Table 1. The description of clinical features is presented in Table 2. In terms of quality assessment, NOS was used for the non-randomized controlled trials. The scores of all included literature covered 6–9 points, defined as high quality, as shown in Table 3. Quality assessment of RCTs based on the Delphi list is given in Table 4.
Table 1.
Study characteristics and demographics
| References | Year | Study design | Sample size | Mean age | Operation Time (min) | Blood Loss (mL) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Zero-p | CPC | Zero-p | CPC | Zero-p | CPC | Zero-p | CPC | |||
| Lan et al. [7] | 2017 | R OS | 35 | 33 | 54.05 ± 10.11 | 52.09 ± 10.46 | 101.57 ± 14.36 | 107.88 ± 14.35 | 93.4 ± 9.04 | 97.94 ± 10.76 |
| Vaishnav et al. [8] | 2018 | R OS | 41 | 23 | 48.58 ± 10.72 | 46.37 ± 8.4 | 44.88 ± 6.54 | 54.43 ± 14.71 | 27.32 ± 9.23 | 30.68 ± 13.21 |
| Wei et al. [11] | 2022 | R OS | 68 | 28 | 48.7 ± 7.3 | 47.2 ± 6.7 | 55.24 ± 5.17 | 53.16 ± 5.29 | 34.52 ± 6.42 | 32.46 ± 8.31 |
| He et al. [16] | 2021 | R OS | 42 | 45 | 62.59 ± 8.21 | 61.15 ± 7.52 | 84 ± 23 | 98 ± 27 | 139 ± 22 | 154 ± 33 |
| Noh et al. [17] | 2021 | R OS | 38 | 42 | 51.9 ± 10.21 | 52.6 ± 8.61 | 108.31 ± 17.15 | 123.25 ± 28.23 | 72.39 ± 13.11 | 92.12 ± 38.65 |
| Lee et al. [18] | 2015 | R OS | 23 | 18 | 57.26 ± 13.28 | 52.89 ± 7.71 | NS | NS | NS | NS |
| Son et al. [19] | 2014 | R OS | 21 | 27 | 55.4 ± 9.7 | 50.2 ± 10.9 | 159.5 ± 52.1 | 147.4 ± 48.4 | 90 ± 148 | 146.5 ± 138.0 |
| Nemoto et al. [20] | 2015 | P RCT | 24 | 22 | 40.9 ± 7.2 | 41.6 ± 7.0 | 116.4 ± 17.1 | 128.5 ± 17.4 | NS | NS |
| Wang et al. [21] | 2014 | R OS | 22 | 25 | 50.86 ± 8.79 | 53.68 ± 8.96 | 98.18 ± 15.55 | 105.4 ± 14.43 | 87.95 ± 12.02 | 92.4 ± 11.28 |
| Li et al. [22] | 2015 | P RCT | 23 | 23 | NS | NS | NS | NS | NS | NS |
| Wang et al. [23] | 2015 | R OS | 27 | 30 | 51.6 ± 11.3 | 54 ± 8.5 | 98.2 ± 15.2 | 109.8 ± 16.9 | 88.2 ± 12.9 | 95.2 ± 11.6 |
| Yan et al. [24] | 2014 | R OS | 37 | 35 | 63.55 ± 7.12 | 64.28 ± 8.76 | 76.59 ± 14.53 | 53.78 ± 17.91 | 52.74 ± 26.84 | 85.46 ± 23.97 |
| Li et al. [25] | 2020 | R OS | 24 | 27 | 65.7 ± 7.5 | 62.3 ± 3.4 | NS | NS | NS | NS |
| Liu et al. [26] | 2016 | P RCT | 31 | 31 | 48.5 ± 9.1 | 45.2 ± 10.6 | 63.45 ± 10.87 | 85.97 ± 12.04 | 44.35 ± 11.53 | 66.26 ± 19.62 |
| Shao et al. [27] | 2016 | R OS | 63 | 76 | 47.6 ± 6.4 | 50.3 ± 8.2 | 63.7 ± 12.5 | 71.8 ± 13.2 | 83.6 ± 14.5 | 86.1 ± 14.3 |
| Yi et al. [28] | 2017 | R OS | 80 | 84 | 52.12 ± 5.893 | 51.95 ± 6.267 | 148.46 ± 27.239 | 165.37 ± 28.538 | 76.87 ± 21.38 | 80.46 ± 31.409 |
| Wang et al. [29] | 2016 | R OS | 12 | 16 | 50.5 ± 13.5 | 52.0 ± 12.0 | 113 ± 8.6 | 160.44 ± 17.2 | 51.67 ± 24.2 | 52.13 ± 24.54 |
| Guo et al. [30] | 2015 | P RCT | 49 | 49 | 43.1 ± 16.9 | 43.3 ± 17.7 | 70.8 ± 17.3 | 87.6 ± 23.4 | 49.5 ± 17.2 | 65.2 ± 25.3 |
| Sun et al. [31] | 2017 | R OS | 25 | 28 | 53 ± 10.26 | 53.57 ± 10.66 | 88.88 ± 25.8 | 109.2 ± 20.4 | 83.22 ± 33.24 | 117.33 ± 23.57 |
| Hu et al. [32] | 2017 | R OS | 23 | 31 | 49.78 ± 10.4 | 45.54 ± 40.22 | 78.22 ± 14.01 | 82.19 ± 6.51 | 19.52 ± 6.95 | 37.16 ± 5.25 |
| Sha et al. [33] | 2021 | R OS | 30 | 31 | 52.9 ± 9.27 | 50.33 ± 8.57 | 81.33 ± 10.74 | 93.67 ± 11.59 | 77.33 ± 22.43 | 108.33 ± 24.08 |
| Chang et al. [9] | 2017 | R OS | 21 | 24 | 54.6 ± 3.5 | 53.2 ± 4.2 | 62.7 ± 17.3 | 87.6 ± 23.2 | 78.4 ± 29.6 | 80.2 ± 36.8 |
| Ruan et al. [34] | 2018 | R OS | 21 | 18 | 56.3 ± 9.8 | 59.6 ± 12.5 | 68.6 ± 8.2 | 79.7 ± 9.3 | 41.2 ± 7.4 | 78.9 ± 9.2 |
| Zhu et al. [35] | 2019 | R OS | 19 | 26 | 55.42 ± 8.03 | 59.15 ± 8.04 | 129 ± 25 | 172 ± 29 | 88 ± 29 | 151 ± 33 |
| Zhang et al. [36] | 2020 | R OS | 56 | 67 | 45.2 ± 13.9 | 48.7 ± 13.2 | 76.96 ± 8.98 | 82.31 ± 7.57 | 51.64 ± 20.35 | 57.97 ± 17.9 |
| Gou et al. [10] | 2022 | R OS | 16 | 16 | 48.5 ± 6.7 | 52.4 ± 7.2 | 75.1 ± 6.0 | 90.6 ± 8.1 | 61.9 ± 9.9 | 60.3 ± 12.6 |
| Luo et al. [37] | 2021 | R OS | 60 | 60 | 59.1 ± 16.4 | 59.8 ± 14.4 | 75.22 ± 7.57 | 90.39 ± 8.1 | 77.53 ± 37.27 | 72.24 ± 34.74 |
R, retrospective; P, prospective; OS, observational; RCT, randomized controlled trial; and NS, not specified
Table 2.
Description of clinical features of studies
| Study | Indication (s) | Design of Zero-profile device | Fusion level (Zero-p/CPC) | Mean follow-up time (month) | |||||
|---|---|---|---|---|---|---|---|---|---|
| C3/4 | C4/5 | C5/6 | C6/7 | C7/T1 | Zero-p | CPC | |||
| Lan et al. [7] | CR, CSM | Zero-p | 8/7 | 10/12 | 13/11 | 4/3 | 23.68 ± 1.93 | 24.39 ± 2.00 | |
| Vaishnav et al. [8] | NS | Zero-p | 2/1 | 2/3 | 8/5 | 12/13 | NS | NS | |
| Wei et al. [11] | CR, CSM | Zero-p | 5/6 | 8/21 | 15/32 | 9/9 | 15.3 ± 5.2 | 15.1 ± 5.2 | |
| He et al. [16] | CR, CSM | ROI-C | 22.6 ± 3.3 | 27.1 ± 3.5 | |||||
| Noh et al. [17] | CR | Zero-p | 8/8 | 19/24 | 11/14 | 37.6 ± 5.91 | 37.1 ± 15.7 | ||
| Lee et al. [18] | CR | Zero-p | 4/1 | 2/4 | 13/9 | 4/4 | 12.57 ± 2.09 | 28.89 ± 20.24 | |
| Son et al. [19] | CR | Zero-p | 3/2 | 4/6 | 10/14 | 4/5 | ≥ 6 | ≥ 6 | |
| Nemoto et al. [20] | CR | PREVAIL | 2/2 | 4/6 | 10/10 | 6/6 | 24 | 24 | |
| Wang et al. [21] | CSM | Zero-p | 33.59 ± 5.52 | 33.16 ± 5.97 | |||||
| Li et al. [22] | CR, CSM | Zero-p | 11/9 | 9/11 | 3/3 | 24 | 24 | ||
| Wang et al. [23] | CSM | Zero-p | 2/3 | 8/7 | 9/12 | 8/8 | 35.2 | 35.5 | |
| Yan et al. [24] | CR, CSM | Zero-p | 12/13 | 25/22 | 15.32 ± 2.13 | 14.26 ± 2.35 | |||
| Li et al. [25] | CR, CSM | Zero-p | 5/7 | 10/10 | 9/10 | 81.0 ± 4.4 | 79.0 ± 3.4 | ||
| Liu et al. [26] | CSM | Zero-p | 3/2 | 9/13 | 13/11 | 6/5 | 15.52 ± 1.93 | 16.10 ± 2.33 | |
| Shao et al. [27] | NS | Zero-p | 2/4 | 24/27 | 31/36 | 6/9 | 23.6 ± 4.5 | 25.2 ± 4.8 | |
| Yi et al. [28] | CR, CSM | Zero-p | > 12 | > 12 | |||||
| Wang et al. [29] | CR, CSM | Zero-p | 2/5 | 6/8 | 4/6 | NS | NS | ||
| Guo et al. [30] | CR, CSM | Zero-p | 13/10 | 9/13 | 9/9 | 10/12 | 9/5 | 18.5 ± 17.5 | 18.5 ± 17.5 |
| Sun et al. [31] | CR, CSM | ROI-C | 3–24 | 3–24 | |||||
| Hu et al. [32] | CR, CSM | ROI-C | 15.7 ± 2.4 | 15.7 ± 2.4 | |||||
| Sha et al. [33] | CR, CSM | ROI-C | 8/7 | 10/11 | 12/13 | 13.5 ± 1.5 | 13.5 ± 1.5 | ||
| Chang et al. [9] | CSM | Zero-p | 3/4 | 10/12 | 5/5 | 3/3 | 12–16 | 12–16 | |
| Ruan et al. [34] | CSM | ROI-C | 0/1 | 2/4 | 12/8 | 7/5 | 13.3 ± 1.9 | 14.9 ± 1.7 | |
| Zhu et al. [35] | CR, CSM | ROI-C | > 12 | > 12 | |||||
| Zhang et al. [36] | CR, CSM | ROI-C | 7/11 | 17/23 | 23/25 | 9/8 | 21.46 ± 4.51 | 21.46 ± 4.51 | |
| Gou et al. [10] | CSM | Zero-p | 2/1 | 5/4 | 7/6 | 2/5 | 6–18 | 6–18 | |
| Luo et al. [37] | CR | Zero-p | 5/3 | 9/10 | 23/22 | 13/15 | ≥ 24 | ≥ 24 | |
CR = cervical radiculopathy, CSM = cervical spondylotic myelopathy, NS = not specified
Table 3.
Quality assessment using the Newcastle–Ottawa quality assessment scale for each non-randomized controlled trial
| Variable | Lan et al. [7] | Vaishnav et al. [8] | Wei et al. [11] | He et al. [16] | Noh et al. [17] | Lee et al. [18] | Son et al. [19] | Wang et al. [21] | Wang et al. [23] | Yan et al. [24] | Li et al. [25] | Shao et al. [27] | Yi et al. [28] | Wang et al. [29] | Sun et al. [31] | Hu et al. [32] | Sha et al. [33] | Chang et al. [9] | Ruan et al. [34] | Zhu et al. [35] | Zhang et al. [36] | Gou et al. [10] | Luo et al. [37] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Selection | |||||||||||||||||||||||
| Representativeness of exposed cohort | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Selection of non-exposed cohort | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Ascertainment of exposure | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Demonstration that outcome of interest was not present at start of study | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||||||||
| Comparability | |||||||||||||||||||||||
| Study controlled for age or gender | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Study controlled for any additional factor | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| Outcome | |||||||||||||||||||||||
| Assessment of outcome | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Follow-up long enough for outcomes to occur | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Adequacy of follow-up of cohort | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||
| Total | 8 | 8 | 9 | 8 | 7 | 7 | 8 | 8 | 8 | 8 | 8 | 9 | 9 | 6 | 8 | 8 | 7 | 8 | 8 | 9 | 8 | 8 | 8 |
Table 4.
Methodological quality assessment of included randomized controlled trials using Delphi list
| Variable | Study | |||
|---|---|---|---|---|
| Nemoto et al. [20] | Li et al. [22] | Liu et al. [26] | Guo et al. [30] | |
| Randomization method used | Yes | Yes | Yes | Yes |
| Groups were similar at baseline regarding most important prognostic indicators | Yes | Yes | Yes | Yes |
| Eligibility criteria were specified | Yes | Yes | Yes | No |
| Outcome assessor was blinded | No | No | Yes | No |
| Care provider was blinded | No | No | No | No |
| Patient was blinded | No | Yes | No | No |
| Point estimates and measures of variability were presented for primary outcome measures | Yes | Yes | Yes | Yes |
| Analysis includes an intention-to-treat analysis | No | No | No | No |
Clinical outcomes
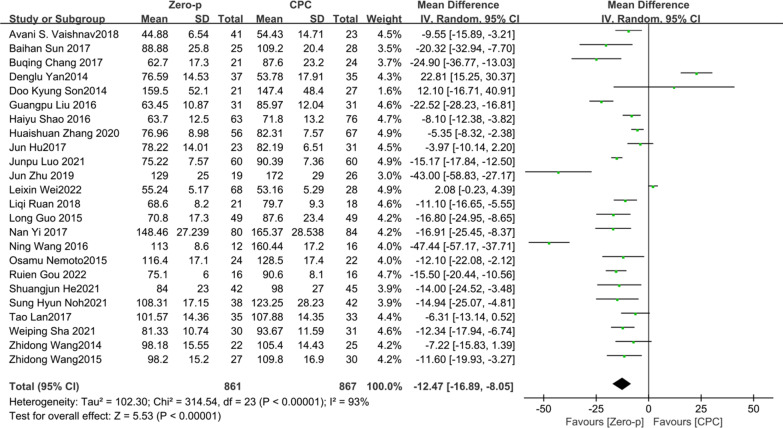
Operative time
24 studies [7–11, 16, 17, 19–21, 23, 24, 26–37] consisting of 1728 patients (Zero-p group, 861; CPC group, 867) compared the mean operative time. There was significant heterogeneity in the literature (P < 0.00001, I2 = 93%). Meta-analysis was performed using random-effect model, and the result showed that operative time in the CPC group was significantly greater than that of in Zero-p group (WMD = − 12.47, 95% CI (− 16.89, − 8.05), P < 0.00001). The corresponding forest plot was shown in Fig. 2.
Fig. 2.
Meta-analysis of Zero-p group versus CPC group in operative time
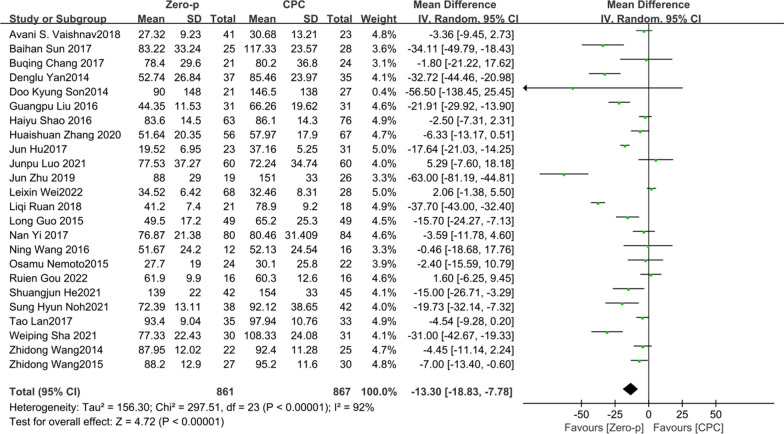
Intraoperative blood loss
Studies [7–11, 16, 17, 19–21, 23, 24, 26–37] consisting of 1728 patients (Zero-p group, 861; CPC group, 867) compared the mean intraoperative blood loss. There was a significant heterogeneity in the literature (P < 0.00001, I2 = 92%). Meta-analysis was performed using random-effect model, and the result showed that intraoperative blood loss in the CPC group was significantly greater than that of in Zero-p group (WMD = − 13.30, 95% CI (− 18.83, − 7.78), P < 0.00001). The corresponding forest plot was shown in Fig. 3.
Fig. 3.
Meta-analysis of Zero-p group versus CPC group in intraoperative blood loss
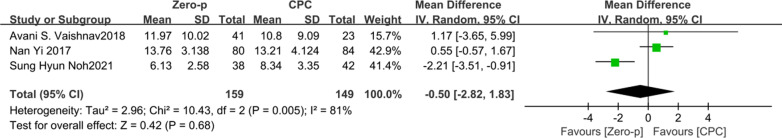
Length of stay (LOS)
Three studies [8, 17, 28] consisting of 308 patients (Zero-p group, 159; CPC group, 149) compared the LOS. There was a significant heterogeneity in the literature (P = 0.005, I2 = 81%). Meta-analysis was performed using random-effect model, and the result showed that there was no significant difference in LOS between the Zero-p and CPC group (WMD = − 0.50, 95% CI (− 2.82, 1.83), P = 0.68). The corresponding forest plot was shown in Fig. 4.
Fig. 4.
Meta-analysis of Zero-p group versus CPC group in length of stay
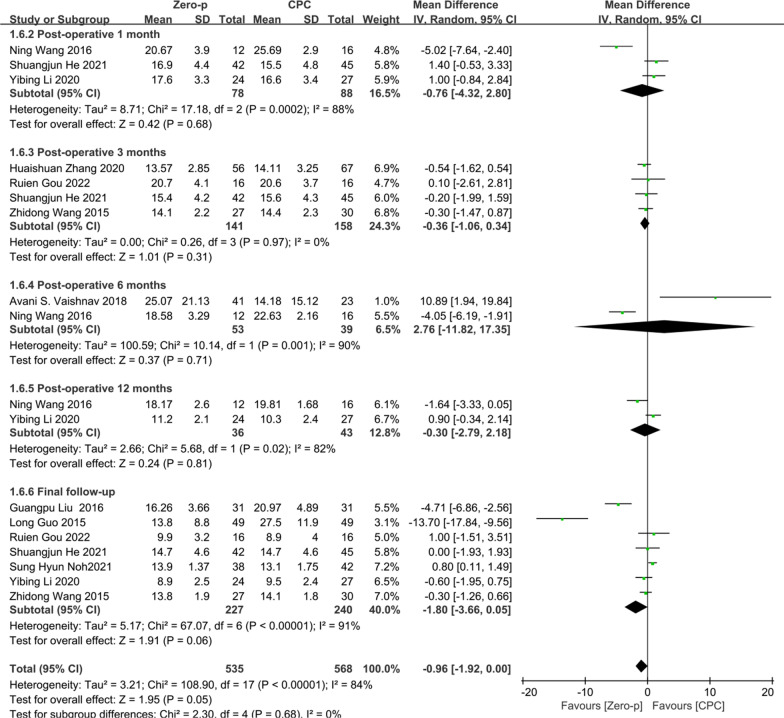
NDI score
10 studies [8, 10, 16, 17, 23, 25, 26, 29, 30, 36] consisting of 682 patients (Zero-p group, 336; CPC group, 346) compared the NDI score. Three studies [16, 25, 29] reported the NDI score at postoperative 1 month. Four studies [10, 16, 23, 36] reported at postoperative 3 months. Two studies [8, 29] reported at postoperative 6 months. Two studies [25, 29] reported at postoperative 12 months. Seven studies [10, 16, 17, 23, 25, 26, 30] reported at final follow-up. No statistical difference was found preoperative period between the two groups (P = 0.65), (Additional file 2). There was a significant heterogeneity in the literature (P < 0.00001, I2 = 84%). Meta-analysis was performed using random-effect model and the results of subgroup analysis showed that there was no significant difference in NDI score between the Zero-p and CPC group after postoperative 1 month (WMD = − 0.76, 95% CI (− 4.32, 2.80), P = 0.68), postoperative 3 months (WMD = − 0.36, 95% CI (− 1.06, 0.34), P = 0.31), postoperative 6 months (WMD = 2.76, 95% CI (− 11.82, 17.35), P = 0.71), postoperative 12 months (WMD = − 0.30, 95% CI (− 2.79, 2.18), P = 0.81), and final follow-up (WMD = − 1.80, 95% CI (− 3.66, 0.05), P = 0.06). The corresponding forest plot was shown in Fig. 5.
Fig. 5.
Meta-analysis of Zero-p group versus CPC group in NDI score
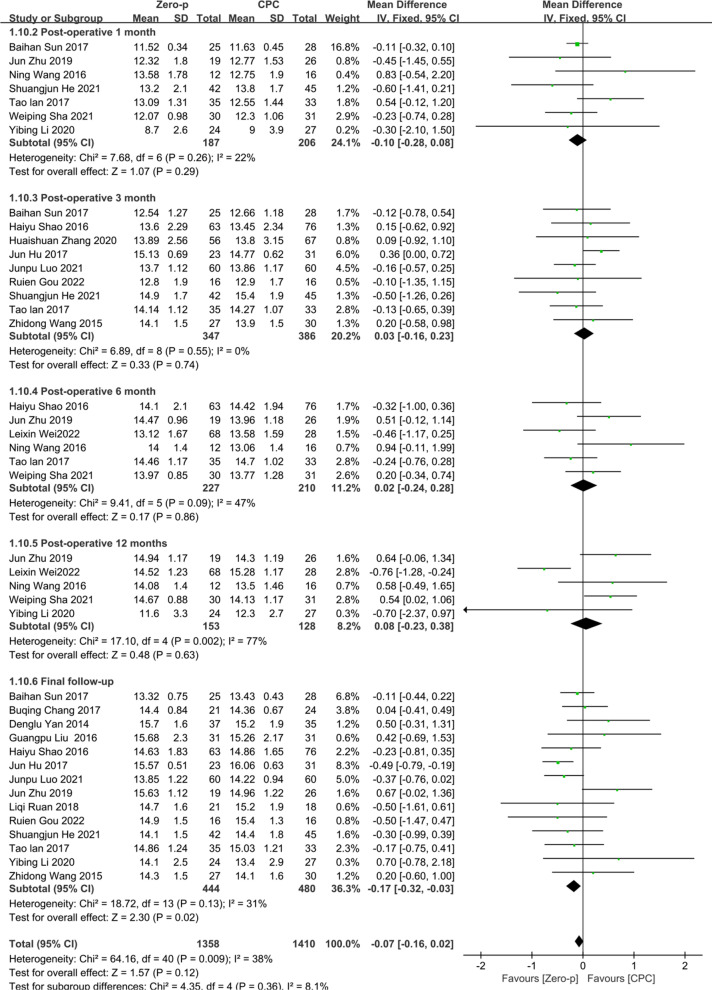
JOA score
18 studies [7, 9–11, 16, 23–27, 29, 31–37] consisting of 1232 patients (Zero-p group, 610; CPC group, 622) compared the JOA score. Seven studies [7, 16, 25, 29, 31, 33, 35] reported the JOA score at postoperative 1 month. Nine studies [7, 10, 16, 23, 27, 31, 32, 36, 37] reported at postoperative 3 months. Five studies [7, 11, 27, 29, 33, 35] reported at postoperative 6 months. Five studies [11, 25, 29, 33, 35] reported at postoperative 12 months. 15 studies [7, 9, 10, 16, 23–27, 31, 32, 34, 35, 37] reported at final follow-up. No significant statistical difference was found in preoperative JOA score between the two groups (P = 0.08), (Additional file 3). There was no significant heterogeneity in the literature (P = 0.0009, I2 = 38%). Meta-analysis was performed using fixed-effect model, and the results of subgroup analysis showed that there was no significant difference in JOA score between the Zero-p and CPC group after postoperative 1 month (WMD = − 0.10, 95% CI (− 0.28, 0.08), P = 0.29), postoperative 3 months (WMD = 0.03, 95% CI (− 0.16, 0.23), P = 0.74), postoperative 6 months (WMD = 0.02, 95% CI (− 0.24, 0.28), P = 0.86), postoperative 12 months (WMD = 0.08, 95% CI (− 0.23, 0.38), P = 0.63), and final follow-up (WMD = − 0.17, 95% CI (− 0.32, − 0.03), P = 0.02). The corresponding forest plot was shown in Fig. 6.
Fig. 6.
Meta-analysis of Zero-p group versus CPC group in JOA score
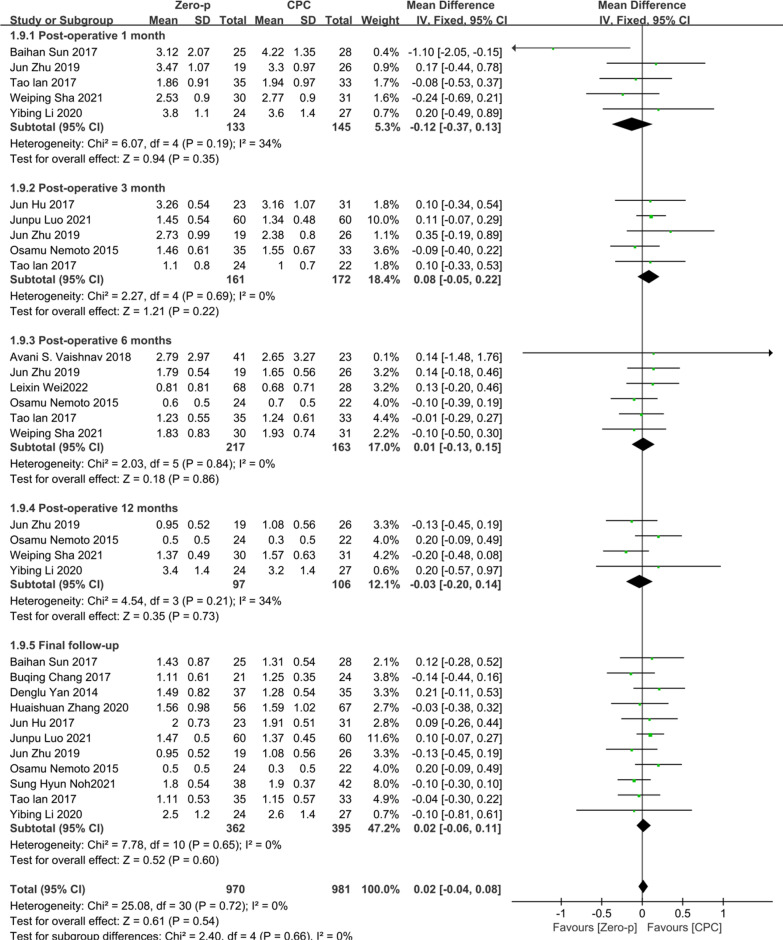
VAS
14 studies [7–9, 11, 17, 20, 24, 25, 31–33, 35–37] consisting of 978 patients (Zero-p group, 501; CPC group, 477) compared the VAS. Five studies [7, 25, 31, 33, 35] reported the VAS at postoperative 1 month. Five studies [7, 20, 32, 35, 37] reported at postoperative 3 months. Six studies [7, 8, 11, 20, 33, 35] reported at postoperative 6 months. Four studies [20, 25, 33, 35] reported at postoperative 12 months. 11 studies [7, 9, 17, 20, 24, 25, 31, 32, 35–37] reported at final follow-up. No statistical difference was found in preoperative VAS between the two groups (P = 0.67), (Additional file 4). There was no significant heterogeneity in the literature (P = 0.72, I2 = 0%). Meta-analysis was performed using fixed-effect model, and the results of subgroup analysis showed that there was no significant difference in VAS between the Zero-p and CPC group after postoperative 1 month (WMD = − 0.12, 95% CI (− 0.37, 0.13), P = 0.35), postoperative 3 months (WMD = 0.08, 95% CI (− 0.05, 0.22), P = 0.22), postoperative 6 months (WMD = 0.01, 95% CI (− 0.13, 0.15), P = 0.86), postoperative 12 months (WMD = − 0.03, 95% CI (− 0.20, 0.14), P = 0.73), final follow-up (WMD = 0.02, 95% CI (− 0.06, 0.11), P = 0.60). The corresponding forest plot was shown in Fig. 7.
Fig. 7.
Meta-analysis of Zero-p group versus CPC group in VAS
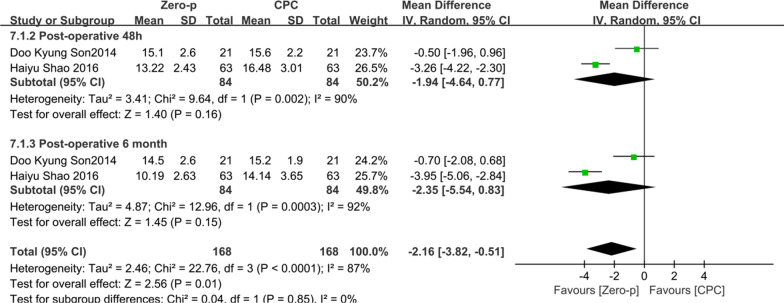
Prevertebral soft tissue thickness (PSTT)
Two studies [19, 27] consisting of 168 patients (Zero-p group, 84; CPC group, 84) compared the PSTT. Two studies [19, 27] reported the PSTT at postoperative 48 h. Two studies [19, 27] reported at postoperative 6 months. No statistical difference was found preoperative period between the two groups (P = 0.90), (Additional file 5). There was significant heterogeneity in the literature (P < 0.0001, I2 = 87%). Meta-analysis was performed using random-effect model, and the results of subgroup analysis showed that there was no significant difference in PSTT between the Zero-p and CPC group after postoperative 24 h (WMD = − 1.94, 95% CI (− 4.64, 0.77), P = 0.16), and postoperative 6 months (WMD = − 2.35, 95% CI (− 5.54, 0.83), P = 0.15). The corresponding forest plot shown in Fig. 8.
Fig. 8.
Meta-analysis of Zero-p group versus CPC group in PSTT
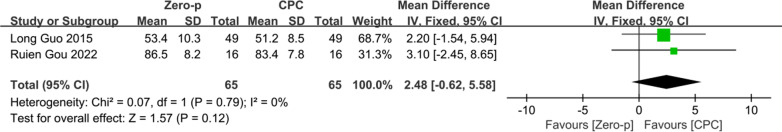
36-Item Short Form Survey (SF-36)
Two studies [10, 30] consisting of 130 patients (Zero-p group, 65; CPC group, 65) compared the SF-36. Two studies [10, 30] reported the SF-36 at the final follow-up. There was no significant heterogeneity in the literature (P = 0.79, I2 = 0%). Meta-analysis was performed using fixed-effect model, and the result showed that there was no significant difference in SF-36 between the Zero-p and CPC group at final follow-up (WMD = 2.48, 95% CI (− 0.62, 5.58), P = 0.12). The corresponding forest plot was shown in Fig. 9.
Fig. 9.
Meta-analysis of Zero-p group versus CPC group in SF-36
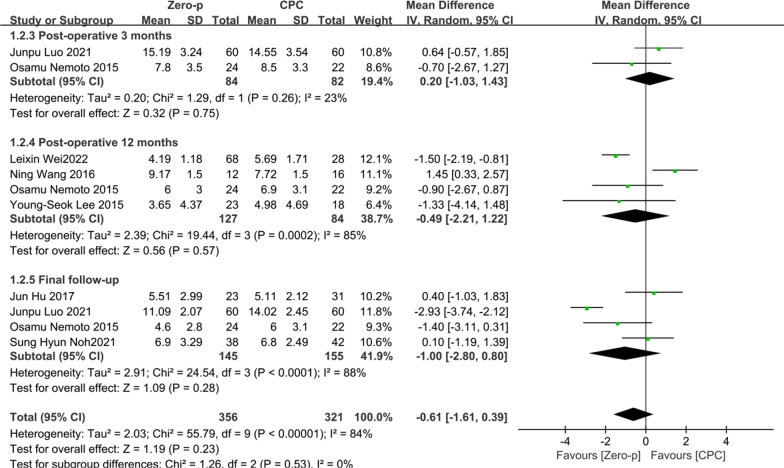
Segmental Cobb angle
Seven studies [11, 17, 18, 20, 29, 32, 37] consisting of 465 patients (Zero-p group, 248; CPC group, 217) compared the postoperative segmental Cobb angle. Two literature [20, 37] reported at postoperative 3 months. Four literature [11, 18, 20, 29] reported at postoperative 12 months. Four literature [17, 20, 32, 37] reported at final follow-up. There was significant heterogeneity in the literature (P < 0.00001, I2 = 84%). Meta-analysis was performed using random-effect model and the results of subgroup analysis showed that there was no significant difference in segmental Cobb angle between the Zero-p and CPC group after postoperative 3 month (WMD = 0.20, 95% CI (− 1.03, 1.43), P = 0.75), postoperative 6 months (WMD = − 0.49, 95% CI (− 2.21, 1.22), P = 0.57), and final follow-up (WMD = − 1.00, 95% CI (− 2.80, 0.80), P = 0.28). The corresponding forest plot was shown in Fig. 10.
Fig. 10.
Meta-analysis of Zero-p group versus CPC group in postoperative segmental Cobb angle
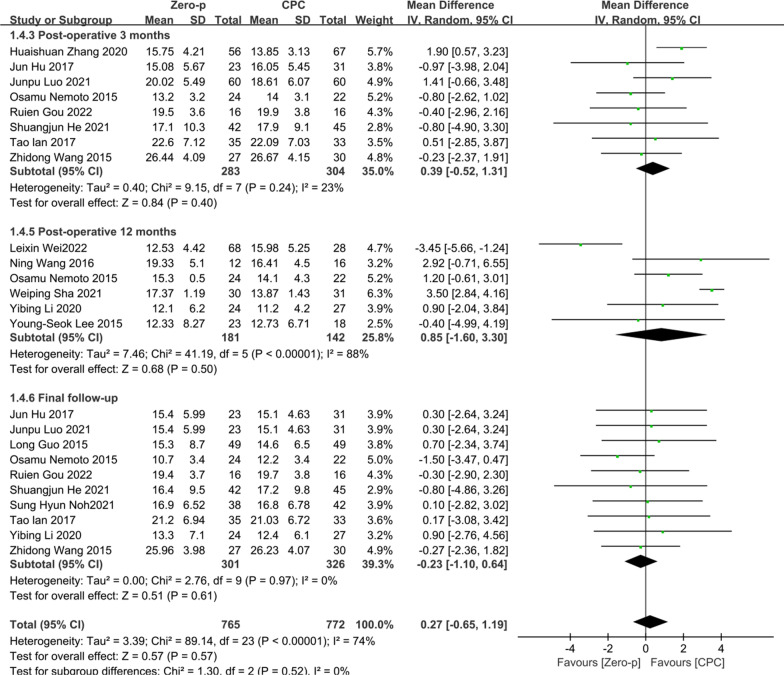
Cervical Cobb angle
15 studies [7, 10, 11, 16–18, 20, 23, 25, 29, 30, 32, 33, 36, 37] consisting of 1042 patients (Zero-p group, 527; CPC group, 515) compared the postoperative cervical Cobb angle. Eight literature [7, 16, 20, 23, 30, 32, 36, 37] reported at postoperative 3 months. Six literature [11, 18, 20, 25, 29, 33] reported at postoperative 12 months. 10 literature [7, 10, 16, 17, 20, 23, 25, 30, 31, 37] reported at final follow-up. There was significant heterogeneity in the literature (P < 0.00001, I2 = 74%). Meta-analysis was performed using random-effect model, and the results of subgroup analysis showed that there was no significant difference in cervical Cobb angle between the Zero-p and CPC group after postoperative 3 month (WMD = 0.39, 95% CI (− 0.52, 1.31), P = 0.40), postoperative 12 months (WMD = 0.85, 95% CI (− 1.60, 3.30), P = 0.50), and final follow-up (WMD = − 0.23, 95% CI (− 1.10, 0.64), P = 0.61). The corresponding forest plot was shown in Fig. 11.
Fig. 11.
Meta-analysis of Zero-p group versus CPC group in postoperative cervical Cobb angle
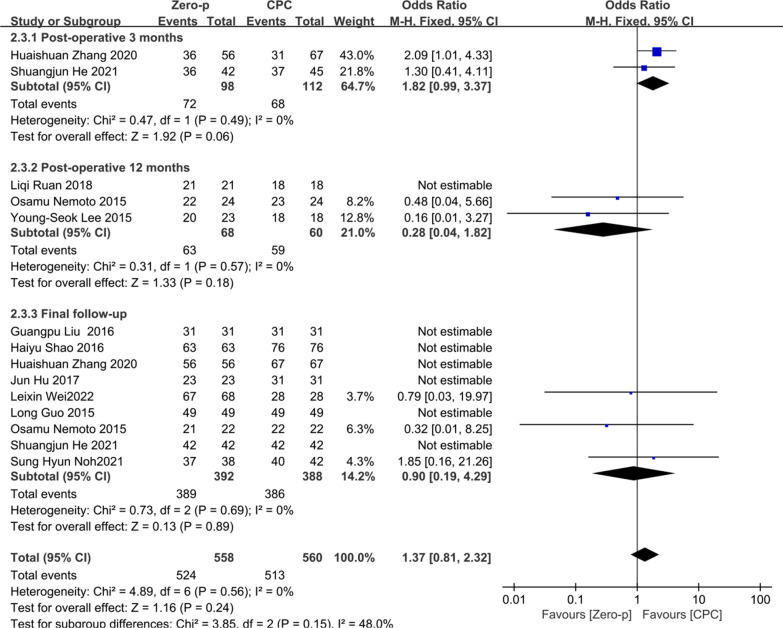
Fusion rate
10 studies [12, 16–18, 20, 26, 27, 30, 32, 34, 36] consisting of 819 patients (Zero-p group, 413; CPC group, 406) compared the fusion rate. Two studies [16, 36] reported the fusion rate at postoperative 3 months. Three studies [18, 20, 34] reported at postoperative 12 months. Nine studies [12, 16, 17, 20, 26, 27, 30, 32, 36] reported at final follow-up. There was no significant heterogeneity in the literature (P = 0.56, I2 = 0%). Meta-analysis was performed using fixed-effect model, and the results of subgroup analysis showed that there was no significant difference in fusion rate between the Zero-p and CPC group after postoperative 3 months (OR= 1.82, 95% CI (0.99, 3.37), P = 0.06), postoperative 12 months (OR= 0.28, 95% CI (0.04, 1.82), P = 0.18), and final follow-up (OR= 0.90, 95% CI (0.19, 4.29), P = 0.89). The corresponding forest plot was shown in Fig. 12.
Fig. 12.
Meta-analysis of Zero-p group versus CPC group in fusion rate
Complications
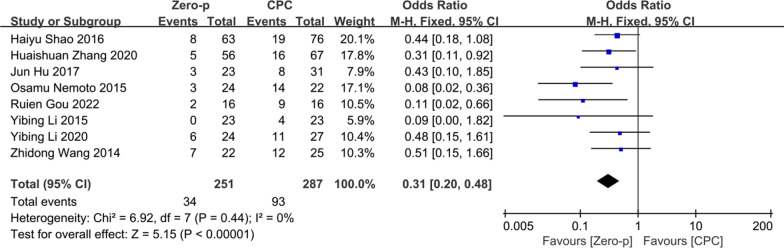
Adjacent segment degeneration (ASD)
Eight studies [10, 20–22, 25, 27, 32, 36] consisting of 538 patients (Zero-p group, 251; CPC group, 287) compared the ASD. There was no significant heterogeneity in the literature (P = 0.44, I2 = 0%). Meta-analysis was performed using fixed-effect model, and the result showed that there was a higher risk of ASD in the CPC group (OR= 0.31, 95% CI (0.20, 0.48), P < 0.0001). The corresponding forest plot was shown in Fig. 13.
Fig. 13.
Meta-analysis of Zero-p group versus CPC group in ASD
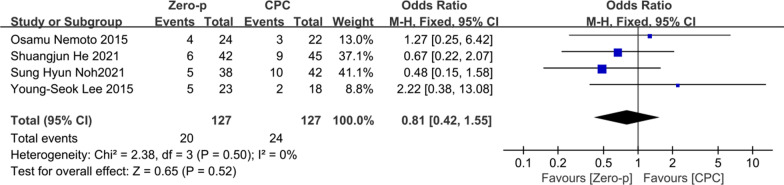
Subsidence
Four studies [16–18, 20] consisting of 254 patients (Zero-p group, 127; CPC group, 127) compared the cage subsidence. There was no significant heterogeneity in the literature (P = 0.50, I2 = 0%). Meta-analysis was performed using fixed-effect model, and the result showed there was no significant difference in subsidence between the Zero-p and CPC group (OR= 0.81, 95% CI (0.42, 1.55), P = 0.52). The corresponding forest plot was shown in Fig. 14.
Fig. 14.
Meta-analysis of Zero-p group versus CPC group in cage subsidence
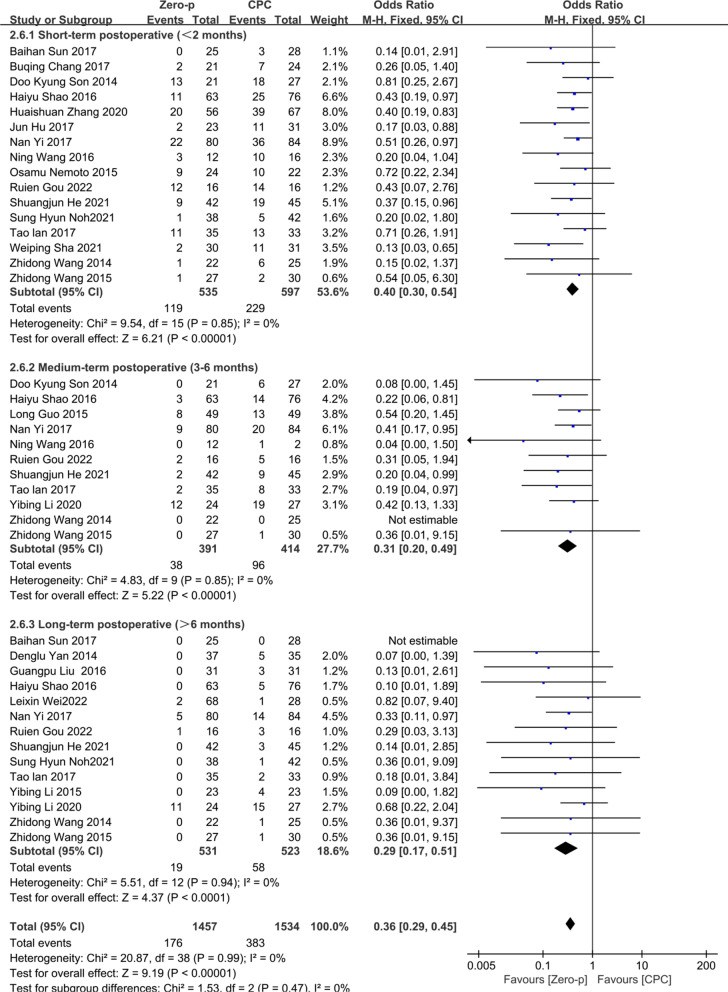
Dysphagia
22 studies [7, 9–11, 16, 17, 19–33, 36] consisting of 1557 patients (Zero-p group, 767; CPC group, 790) compared the incidence of postoperative dysphagia. 16 studies [7, 9, 10, 16, 17, 19–21, 23, 27–29, 31–33, 36] reported the short-term (< 2 months), 11 studies [7, 10, 16, 19, 21, 23, 25, 27–30] reported medium-term (3–6 months), and 14 studies [7, 10, 11, 16, 17, 21–28, 31] reported long-term (> 6 months) dysphagia. There was no significant heterogeneity in the literature (P = 0.99, I2 = 0%). Meta-analysis was performed using fixed-effect model, and the results of subgroup analysis showed that the CPC group had a higher risk of dysphagia in short term (OR= 0.40, 95% CI (0.30, 0.54), P < 0.00001), medium term (OR= 0.31, 95% CI (0.20, 0.49), P < 0.00001), and long term (OR= 0.29, 95% CI (0.17, 0.51), P < 0.0001). The corresponding forest plot analysis is shown in Fig. 15.
Fig. 15.
Meta-analysis of Zero-p group versus CPC group in postoperative dysphagia
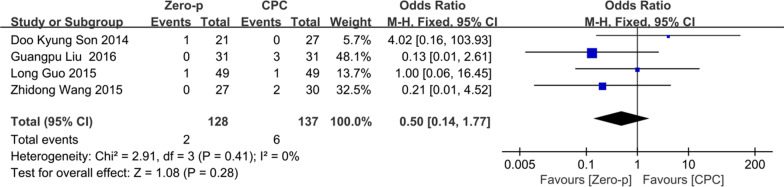
Implant failure
Four studies [19, 21, 26, 30] consisting of 265 patients (Zero-p group, 128; CPC group, 137) compared the incidence of implant failure. There was no significant heterogeneity in the literature (P = 0.41, I2 = 0%). Meta-analysis was performed using fixed-effect model, and the result showed there was no significant difference in the incidence of implant failure between the Zero-p and CPC group (OR= 0.50, 95% CI (0.14, 1.77), P = 0.28). The corresponding forest plot was shown in Fig. 16.
Fig. 16.
Meta-analysis of Zero-p group versus CPC group in postoperative implant failure
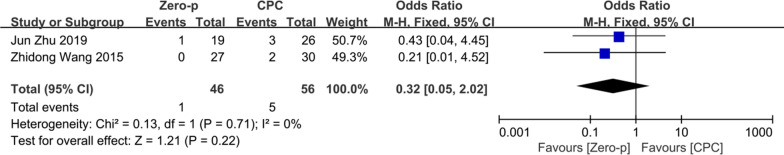
Hoarseness
Two studies [23, 35] consisting of 102 patients (Zero-p group, 46; CPC group, 56) compared the incidence of postoperative hoarseness. There was no significant heterogeneity in the literature (P = 0.71, I2 = 0%). Meta-analysis was performed using fixed-effect model, and the result showed there was no significant difference in the incidence of hoarseness between the Zero-p and CPC group (OR= 0.32, 95% CI (0.05, 2.02), P = 0.22). The corresponding forest plot was shown in Fig. 17.
Fig. 17.
Meta-analysis of Zero-p group versus CPC group in postoperative hoarseness
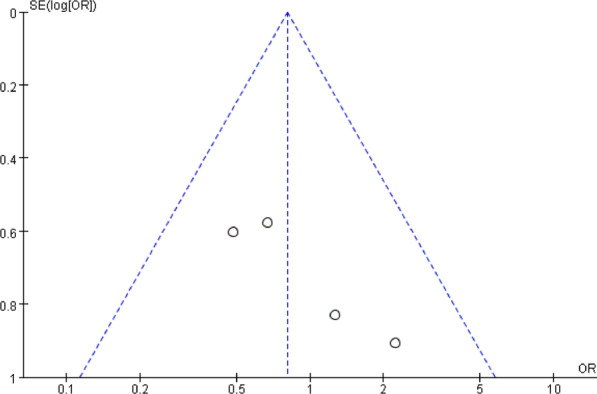
Publication bias and sensitivity analysis
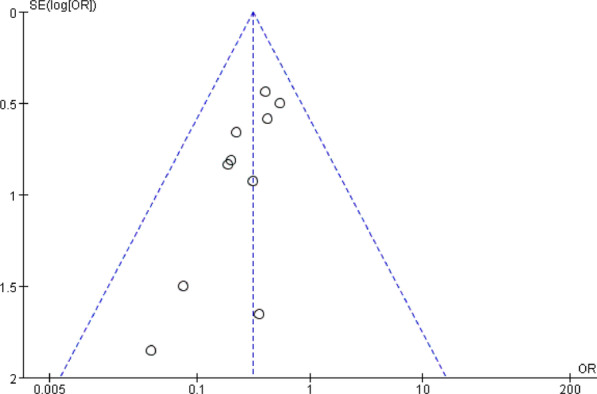
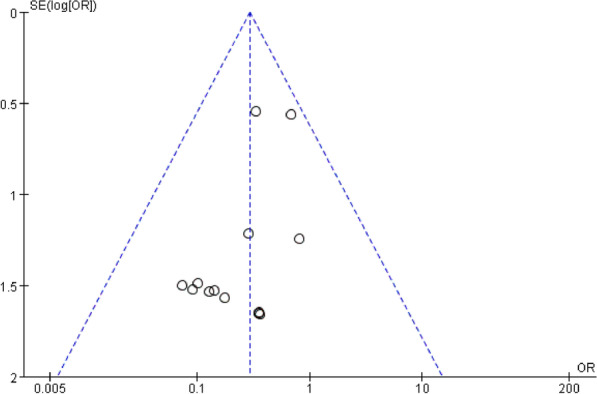
Funnel plots of the fusion rate, ASD, subsidence, dysphagia, and implant failure were shown in Fig. 18, 19, respectively. Funnel plots of the incidence of dysphagia at postoperative short term, medium term, and long term are shown in Fig. 20, 21, 22, respectively. All studies were within the 95% CI, indicating less publication bias. Sensitivity analysis by reanalyzing the data after sequential omission of individual studies revealed no significant changes.
Fig. 18.
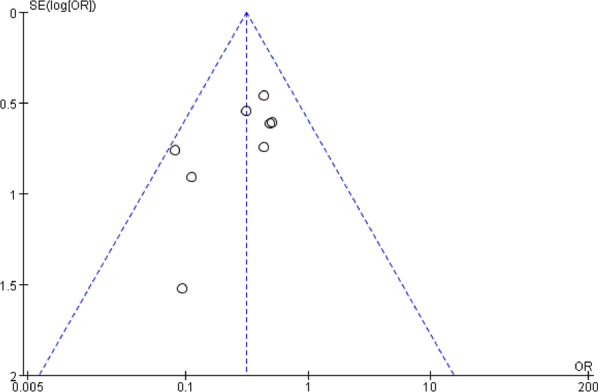
Funnel plot for publication bias of ASD at final follow-up
Fig. 19.
Funnel plot for publication bias of cage subsidence at final follow-up
Fig. 20.
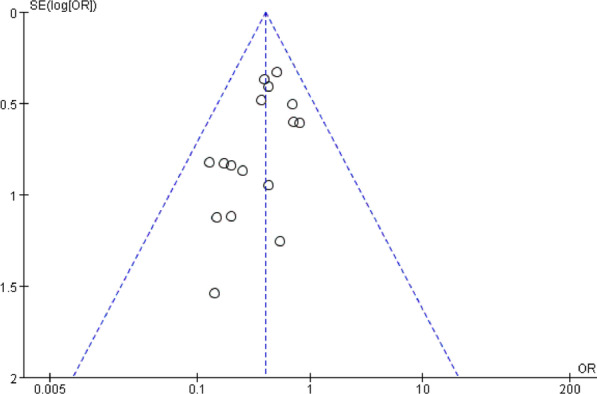
Funnel plot for publication bias of dysphagia at postoperative short-term
Fig. 21.
Funnel plot for publication bias of dysphagia at postoperative medium-term
Fig. 22.
Funnel plot for publication bias of dysphagia at postoperative long-term
Discussion
DCS is a common cervical disease in adults, resulting in neck pain and decreased muscle strength of the extremities, seriously affecting the quality of life. After ineffective non-surgical treatment, patients with symptomatic DCS were often need surgical treatment. ACDF is a mainstay for the treatment of DCS [3, 38]. With the development of spinal internal fixation, CPC has been widely used in ACDF, which can address the needs of complete decompression, restoration of cervical physiological curvature, and improvement of stability and fusion rate. However, CPC has the risk of several defects such as dysphagia and tracheal injury. In addition, anterior irregularity of the vertebral body including osteophyte and mild spondylolisthesis in front of the vertebral body caused by degeneration of the cervical spine is often causing the postoperative loosening of the anterior cervical titanium plate and increasing the risk of ASD [5, 6, 39]. Zero-p, in addition to the advantages of CPC, can effectively avoid the disadvantages of CPC [7–10]. Several studies have been conducted about the therapeutic effects of Zero-p and CPC in recent years, but the sample sizes were small and there were no multi-center studies with large samples, leading to inconsistent conclusions. For this reason, this study is based on the differences in clinical efficacy between the two devices from an evidence-based medicine perspective to determine which device is more beneficial to the postoperative recovery of patients with DCS who underwent single-level ACDF.
In the aspect of operative time (I2 = 93%, P < 0.00001) and intraoperative blood loss (I2 = 92%, P < 0.00001), high heterogeneity among different studies may be related to the study type, sample size, and data statistics of the literature. Moreover, both of them were affected by the experience and surgical habits of the surgeon. Previously, Duan et al. [40] demonstrated that operative time between the Zero-p group and CPC group in one-level ACDF was not significant, but there was a significant reduction in intraoperative blood loss. In contrast, Nambiar et al. [41] demonstrated that Zero-p significantly reduced the operative time, but was inferior in significantly reducing the intraoperative blood loss. The shortening of operative time and intraoperative blood loss will help to reduce the occurrence of perioperative risks and complications. It is superior in the postoperative rehabilitation of patients to the CPC group. There is no significant difference in LOS between the two groups, while Nambiar et al. [41] did not discuss the LOS in the previous meta-analysis. There is no significant difference in SF-36 between the two groups. It indicates that the influence of two devices on physical and mental health was insignificant.
In this study, we found that there was no statistically significant difference in postoperative VAS and NDI scores in the Zero-p CPC group. The JOA score in Zero-p group was significantly higher at follow-up (WMD = − 0.17, 95% CI (− 0.32, − 0.03), P = 0.02). The results suggest that Zero-p can achieve the same clinical efficacy as CPC in single-level ACDF. Nambiar et al. [41] and Lu et al. [12] had similar results in a meta-analysis of Zero-p versus CPC in single-level and two-level ACDF, respectively.
In terms of radiological outcomes, the differences of the postoperative segmental and cervical Cobb angle between the two groups were not significant. This was consistent with the results of Nambiar et al. [41]. It indicates that Zero-p and CPC groups were equally effective in restoring cervical curvature in single-level ACDF. Perrini et al. [42] reported that CPC was more conducive to the recovery of cervical curvature during two-level ACDF. Dong et al. [43] revealed that CPC was significantly superior in maintaining the segmental Cobb angle. No articles with single-level ACDF were included in Yang et al. [44], and only two articles with single-level ACDF were included in Sun et al. [45], and the results revealed a significant increase in cervical lordosis in the CPC group, but the current meta-analysis revealed no significant difference in both segmental and cervical Cobb between Zero-p and CPC group, indicating that Zero-p has similar efficacy in maintaining the segmental curvature with CPC in single-level ACDF. Thus, we recommend using Zero-p in single-level ACDF, but not in multi-level ACDF.
In addition, the PSTT in the Zero-p group was thinner, attributing to the smaller surgical exposure, milder stimulus to the prevertebral soft tissue and esophagus, and preserving anatomical tissues. Both two sub-groups analyses were not significant, possibly due to the limited sample size resulting in low statistical power comparison. There was no significant difference in fusion rate between the two groups at 3 months, 12 months, and final follow-up (73.5% VS 60.7%; 92.6% VS 98.3%; 99.2% VS 99.5%). Zero-p was demonstrated to provide good postoperative stability in single-level ACDF, consistent with Duan et al. [40], Nambiar et al. [41], and Dong et al. [43]. Scholz et al. [46] demonstrated that both two devices provide the same biomechanical environment, leading to the similar fusion rates.
In terms of the postoperative complications in the two groups, the Zero-p group significantly reduced the incidence of ASD (13.5% VS 32.4%), which was not mentioned by Nambiar et al. [41]. Chuang et al. [5] demonstrated that the distance between the edge of plate and adjacent segment less than 5 mm was a risk factor for ASD. Zero-p, however, is far from the adjacent segment and reduces the incidence of ASD. Liu et al. [47] demonstrated that CPC had a significantly higher subsidence rate, but Nambiar et al. [41] demonstrated that it was similar. Previously reported subsidence rates of Zero-P were not accordant. The result of this study was consistent with Nambiar et al. [41]. It indicates that Zero-p does not increase the risk of subsidence in single-level ACDF. Kim et al. [48] demonstrated that the presence of subsidence was significantly associated with adverse clinical outcomes. The results of this study showed that the incidence of dysphagia in the Zero-p group was significantly lower than that in the CPC group in postoperative short term (< 2 months), medium term (3–6 months), and long term (> 6 months), (22.2% VS 38.4%, 9.71% VS 23.2%, 3.6% VS 11.1%). Therefore, the use of zero-p can significantly reduce the incidence of postoperative dysphagia. Fountas et al. [6] demonstrated that postoperative dysphagia may be related to prevertebral soft tissue edema and adhesion, postoperative hematoma, and esophageal injury. Accordingly, postoperative PSTT in the Zero-p group was thinner in this study (Fig. 8). The reason why intraoperative blood loss was significantly reduced in the Zero-p group was less damage to the soft tissues and blood vessels around the esophagus. In addition, this result may explain why the incidence of postoperative dysphagia is low in the Zero-p group. Lu et al. [12] reported that there was no significant difference between the stand-alone cage group and CPC group in contiguous two-level ACDF. Nambiar et al. [41] demonstrated an insignificant difference in postoperative dysphagia, but significant at the final follow-up. The reason why this was different from the results of our study may be due to the fewer included literature. There were significant differences between two groups in the early postoperative period, 3 months postoperative period, and the final follow-up in Lu et al. [49] and the postoperative period in Zhang et al. [50], but both studies included single-level and multi-level ACDF. Incidence of implant failure and hoarseness were not reported in the previous meta-analysis [12, 40, 41, 49, 50]. In this study, there was no significant difference in both incidence of implant failure and hoarseness between the two groups.
This study also has some limitations, such as not only including RCTs but also including retrospective studies. Different regions, populations, and ethnicities may also have some impact on the results. In addition, the lack of both surgical and hospitalization costs in the included literature resulted in the inability to comprehensively compare the advantages and disadvantages of the two devices. Further high-quality meta-analyses are still needed to validate the results of this study.
Conclusions
In conclusion, Zero-p in single-level ACDF has significant advantages because it reduces the operative time, intraoperative blood loss, JOA score at follow-up, and the incidence of postoperative ASD and dysphagia. However, Zero-p and CPC have similar efficacy in terms of postoperative VAS, NDI, LOS, fusion rate, segmental Cobb angle, cervical Cobb angle, PSTT, SF-36, subsidence, implant failure, and hoarseness. The use of Zero-p in single-level ACDF was recommended.
Supplementary Information
Additional file 1. (A) Meta-analysis of Zero-p group versus CCP group in age; (B) Meta-analysis of Zero-p group versus CCP group in BMD; (C) Meta-analysis of Zero-p group versus CCP group in BMI; (D) Meta-analysis of Zero-p group versus CCP group in follow-up time.
Additional file 2. Meta-analysis of Zero-p group versus CCP group in preoperative NDI score.
Additional file 3. Meta-analysis of Zero-p group versus CCP group in preoperative JOA score.
Additional file 4. Meta-analysis of Zero-p group versus CCP group in preoperative VAS score.
Additional file 5. Meta-analysis of Zero-p group versus CCP group in preoperative PSTT.
Abbreviations
- ACDF
Anterior cervical discectomy and fusion
- CPC
Cervical cage–plate construct
- JOA
Japanese Orthopaedic Association
- NDI
Neck Disability Index
- VAS
Visual analog scale
- PSTT
Prevertebral soft tissue thickness
- SF-36
36-Item Short Form Survey
- ASD
Adjacent segment degeneration
Author contributions
KA and RLC contributed to concept, literature search, and data collection. KA, MM, and MP were involved in statistics, data analysis, and interpretation. KA, RLC, and MM drafted the article. KA and PR contributed to critical revision of article. All authors read and approved the final manuscript.
Funding
This study was supported by grants from the Natural Science Foundation of Xinjiang Uygur Autonomous Region, Science Foundation for Distinguished Young Scholars (Grant No. 2021D01E29).
Availability of data and materials
The data used to support the findings of this study are included within the article.
Declarations
Ethical approval and consent to participate
Not applicable.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Ruilin Chen is the co-first author
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Peierdun Mijiti, Email: perdonjan@126.com.
Paerhati Rexiti, Email: parhart@vip.sina.com.
References
- 1.Nouri A, Tetreault L, Singh A, et al. Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine (Phila Pa 1976) 2015;40:E675–E693. doi: 10.1097/BRS.0000000000000913. [DOI] [PubMed] [Google Scholar]
- 2.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg Spine. 1958;6:496–511. doi: 10.3171/spi.2007.6.5.496. [DOI] [PubMed] [Google Scholar]
- 3.Mummaneni PV, Kaiser MG, Matz PG, et al. Cervical surgical techniques for the treatment of cervical spondylotic myelopathy. J Neurosurg Spine. 2009;11:130–141. doi: 10.3171/2009.3.SPINE08728. [DOI] [PubMed] [Google Scholar]
- 4.Song KJ, Yoon SJ, Lee KB. Three-and four-level anterior cervical discectomy and fusion with a PEEK cage and plate construct. Eur Spine J. 2012;1:2492–2497. doi: 10.1007/s00586-012-2447-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chung JY, Kim SK, Jung ST, et al. Clinical adjacent-segment pathology after anterior cervical discectomy and fusion: results after a minimum of 10-year follow-up. Spine J. 2014;14:2290–2298. doi: 10.1016/j.spinee.2014.01.027. [DOI] [PubMed] [Google Scholar]
- 6.Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 2007;32:2310–2317. doi: 10.1097/BRS.0b013e318154c57e. [DOI] [PubMed] [Google Scholar]
- 7.Lan T, Lin JZ, Hu SY, et al. Comparison between Zero-profile spacer and plate with cage in the treatment of single level cervical spondylosis. J Back Musculoskelet Rehabil. 2018;31:299–304. doi: 10.3233/BMR-169708. [DOI] [PubMed] [Google Scholar]
- 8.Vaishnav AS, Saville P, McAnany S, et al. Predictive factors of postoperative dysphagia in single-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2019;44:E400–E407. doi: 10.1097/BRS.0000000000002865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang BQ, Feng H, Yu CG, et al. Comparison of clinical effects between anterior cervical Zero-incision fusion system and traditional nail plate system in the treatment of cervical spondylotic myelopathy. China J Orthopaed Traumatol. 2017;30:411–416. doi: 10.3969/j.issn.1003-0034.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 10.Gou RE, Hao SF, Cao J, et al. Application of Zero-notch anterior cervical interbody fusion system in cervical spondylotic myelopathy. Chin J Anat Clin. 2022;27:201–205. doi: 10.3760/cma.j.cn101202-20210226-00052. [DOI] [Google Scholar]
- 11.Wei L, Xu C, Dong M, et al. Application of a new integrated low-profile anterior plate and cage system in single-level cervical spondylosis: a preliminary retrospective study. J Orthop Surg Res. 2022;17:26. doi: 10.1186/s13018-022-02917-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lu VM, Mobbs RJ, Fang B, et al. Clinical outcomes of locking stand-alone cage versus anterior plate construct in two-level anterior cervical discectomy and fusion: a systematic review and meta-analysis. Eur Spine J. 2019;28:199–208. doi: 10.1007/s00586-018-5811-x. [DOI] [PubMed] [Google Scholar]
- 13.Li XF, Jin LY, Liang CG, et al. Adjacent-level biomechanics after single-level anterior cervical interbody fusion with anchored Zero-profile spacer versus cage-plate construct: a finite element study. BMC Surg. 2020;20:66. doi: 10.1186/s12893-020-00729-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 15.Phan K, Mobbs RJ. Systematic reviews and meta-analyses in spine surgery, neurosurgery and orthopedics: guidelines for the surgeon scientist. J Spine Surg. 2015;1:19–27. doi: 10.3978/j.issn.2414-469X.2015.06.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.He S, Zhou Z, Lv N, et al. Comparison of clinical outcomes following anterior cervical discectomy and fusion with zero-profile anchored spacer-ROI-C-fixation and combined intervertebral cage and anterior cervical discectomy and fusion: a retrospective study from a single center. Med Sci Monit. 2021;27:e931050. doi: 10.12659/MSM.931050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Noh SH, Park JY, Kuh SU, et al. Comparison of zero-profile anchored spacer versus plate-and-cage after 1-Level ACDF with complete uncinate process resection. Clin Spine Surg. 2021;34:176–182. doi: 10.1097/BSD.0000000000001129. [DOI] [PubMed] [Google Scholar]
- 18.Lee YS, Kim YB, et al. Does a zero-profile anchored cage offer additional stabilization as anterior cervical plate? Spine (Phila Pa 1976) 2015;40:E563–570. doi: 10.1097/BRS.0000000000000864. [DOI] [PubMed] [Google Scholar]
- 19.Son DK, Son DW, Kim HS, et al. Comparative study of clinical and radiological outcomes of a zero-profile device concerning reduced postoperative Dysphagia after single level anterior cervical discectomy and fusion. J Korean Neurosurg Soc. 2014;56:103–107. doi: 10.3340/jkns.2014.56.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nemoto O, Kitada A, Naitou S, et al. Stand-alone anchored cage versus cage with plating for single-level anterior cervical discectomy and fusion: a prospective, randomized, controlled study with a 2-year follow-up. Eur J Orthop Surg Traumatol. 2015;25(Suppl 1):S127–S134. doi: 10.1007/s00590-014-1547-4. [DOI] [PubMed] [Google Scholar]
- 21.Wang ZD, Zhu RF, Yang HL, et al. The application of a zero-profile implant in anterior cervical discectomy and fusion. J Clin Neurosci. 2014;21:462–466. doi: 10.1016/j.jocn.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 22.Li Y, Hao D, He B, et al. The efficiency of zero-profile implant in anterior cervical discectomy fusion: a prospective controlled long-term follow-up study. J Spinal Disord Tech. 2015;28:398–403. doi: 10.1097/BSD.0000000000000032. [DOI] [PubMed] [Google Scholar]
- 23.Wang Z, Zhu R, Yang H, et al. Zero-profile implant (Zero-p) versus plate cage benezech implant (PCB) in the treatment of single-level cervical spondylotic myelopathy. BMC Musculoskelet Disord. 2015;16:290. doi: 10.1186/s12891-015-0746-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yan D, Li J, Zhang Z. Anterior cervical discectomy and fusion with the zero-profile implant system for cervical spondylotic myelopathy. Tech Orthop. 2014;29:49–53. doi: 10.1097/BTO.0b013e3182908ff0. [DOI] [Google Scholar]
- 25.Li YB, Gao WJ, Yang XW. Comparison of efficacy of anterior cervical decompression and fusion with Zero-P plate and traditional plate internal fixation for single-segment cervical spondylosis. Chin J Bone Joint Injury. 2020;35:225–228. doi: 10.7531/j.issn.1672-9935.2020.03.001. [DOI] [Google Scholar]
- 26.Liu GP, Han M, Tang H. Zero-profile interbody fusion device versus plate cage benezech in the treatment of single-level cervical spondylotic myelopathy. Chin J Anat Clin. 2016;21:541–546. doi: 10.3760/cma.j.issn.2095-7041.2016.06.017. [DOI] [Google Scholar]
- 27.Shao HY, Zhang J, Yang D, et al. Case-control study on Zero-profile implant for anterior cervical discectomy and fusion and conventional cage plate internal fixation for the treatment of single segmental cervical intervertebral disc herniation. China J Orthop Trauma. 2016;29:530–537. doi: 10.3969/j.issn.1003-0034.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 28.Yi N, Yang Y, Ma LT, et al. Comparison of the incidence and severity of dysphagia after single level anterior cervical decompression and fusion using the Zero-P implant system and the traditional anterior plate. J Cervicodynia Lumbodynia. 2017;38:568–572. doi: 10.3969/j.issn.1005-7234.2017.06.005. [DOI] [Google Scholar]
- 29.Wang N, He BX, Bao G, Lian MX, Li CK, Lian HP. Clinical effects of Zero-P vs. traditional titanium plate for single level cervical spondylosis. J Xi'an Jiaotong Univ (Med Sci) 2016;2(174–177):186. doi: 10.7652/jdyxb201602005. [DOI] [Google Scholar]
- 30.Guo L, Fan SW. Effectiveness comparision between anterior cervical zero-profile interbody fusion device and anterior cervical plate cage benezech. Chin J Reparat Reconstr Surg. 2015;9:840–844. doi: 10.7507/1002-1892.20150182. [DOI] [PubMed] [Google Scholar]
- 31.Sun BH, Zheng B, Huang D, et al. Effect comparison of zero profile anterior cervical interbody fusion ROI-C and traditional plate fixation for treatment of cervical spondylotic myelopathy. China Med Herald. 2017;14:100–103. [Google Scholar]
- 32.Hu J, Tang PY, Ma QH, et al. Efficacy analysis of anterior cervical ROI-C and traditional titanium cage-plate in the treatment of cervical disc herniation. J Nanjing Med Univ (Nat Sci Ed) 2017;37:1594–1596. doi: 10.7655/NYDXBNS20171212. [DOI] [Google Scholar]
- 33.Sha WP, Chen GZ, Wang LM. Short-term clinical effect of double bladed zero-profile anchored spacer and locking plate in the treatment of single segmental ceivical spondylosis. Orthopaedics. 2021;12:414–420. doi: 10.3969/j.issn.1674-8573.2021.05.005. [DOI] [Google Scholar]
- 34.Ruan LQ, Shi JD. A comparative study of effects between ROI-C interbody fusion cage and plate fixation combined cage in ACDF for single segment cervical spondylotic myelopathy. Chin J Bone Joint Injury. 2018;33:901–904. doi: 10.7531/j.issn.1672-9935.2018.09.002. [DOI] [Google Scholar]
- 35.Zhu J, Yuan F, Peng KX, et al. Comparison of Zero-profile Double Bladed Zero⁃Profile Anchoredspacer and Locking Titanium Plate with Cage in ACDF. Shandong Med J. 2019;59:77–80. doi: 10.3969/j.issn.1002-266X.2019.04.021. [DOI] [Google Scholar]
- 36.Zhang HS, Zhang M, Pan YL, et al. Anterior cervical discetomy and fusion by using ROI-C cage for single-segment cervical spondylosis. J Chin Pract Diagn. 2020;34:1036–1039. doi: 10.13507/j.issn.1674-3474.2020.10.018. [DOI] [Google Scholar]
- 37.Luo JP, He YZ, Lin B, et al. Effectiveness comparison between anterior cervical decompression separately combined with cage and zero-p interbody fusion internal fixation in the treatment of single-segment cervical spondylosis. Chin J Bone Joint Injury. 2021;36:897–900. doi: 10.7531/j.issn.1672-9935.2021.09.001. [DOI] [Google Scholar]
- 38.Korinth M. Treatment of cervical degenerative disc disease-current status and trends. Zentralbl Neurochir. 2008;69:113–124. doi: 10.1055/s-2008-1081201. [DOI] [PubMed] [Google Scholar]
- 39.Barbagallo GM, Romano D, Certo F, et al. Zero-p: a new Zero-profile cage-plate device for single and multilevel ACDF A single institution series with four years maximum follow-up and review of the literature on Zero-profile devices. Eur Spine J. 2013;22(Suppl 6):S868–S878. doi: 10.1007/s00586-013-3005-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Duan Y, Yang Y, Wang Y, et al. Comparison of anterior cervical discectomy and fusion with the zero-profile device versus plate and cage in treating cervical degenerative disc disease: a meta-analysis. J Clin Neurosci. 2016;33:11–18. doi: 10.1016/j.jocn.2016.01.046. [DOI] [PubMed] [Google Scholar]
- 41.Nambiar M, Phan K, Cunningham JE, et al. Locking stand-alone cages versus anterior plate constructs in single-level fusion for degenerative cervical disease: a systematic review and meta-analysis. Eur Spine J. 2017;26:2258–2266. doi: 10.1007/s00586-017-5015-9. [DOI] [PubMed] [Google Scholar]
- 42.Perrini P, Cagnazzo F, Benedetto N, et al. Cage with anterior plating is advantageous over the stand-alone cage for segmental lordosis in the treatment of two-level cervical degenerative spondylopathy: a retrospective study. Clin Neurol Neurosurg. 2017;163:27–32. doi: 10.1016/j.clineuro.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 43.Dong J, Lu M, Lu T, et al. Meta-analysis comparing zero-profile spacer and anterior plate in anterior cervical fusion. PLoS ONE. 2015;10:e0130223. doi: 10.1371/journal.pone.0130223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yang Z, Zhao Y, Luo J. Incidence of dysphagia of zero-profile spacer versus cage-plate after anterior cervical discectomy and fusion: a meta-analysis. Medicine (Baltimore) 2019;98:e15767. doi: 10.1097/MD.0000000000015767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sun Z, Liu Z, Hu W, et al. Zero-profile versus cage and plate in anterior cervical discectomy and fusion with a minimum 2 years of follow-up: a meta-analysis. World Neurosurg. 2018;120:e551–e561. doi: 10.1016/j.wneu.2018.08.128. [DOI] [PubMed] [Google Scholar]
- 46.Scholz M, Reyes PM, Schleicher P, et al. A new stand-alone cervical anterior interbody fusion device: biomechanical comparison with established anterior cervical fixation devices. Spine (Phila Pa 1976) 2009;34:156–160. doi: 10.1097/BRS.0b013e31818ff9c4. [DOI] [PubMed] [Google Scholar]
- 47.Liu W, Hu L, Wang J, et al. Comparison of zero-profile anchored spacer versus plate-cage construct in treatment of cervical spondylosis with regard to clinical outcomes and incidence of major complications: a meta-analysis. Ther Clin Risk Manag. 2015;11:1437–1447. doi: 10.2147/TCRM.S92511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim SJ, Kim SD. Anterior cervical discectomy and fusion using a double cylindrical cage versus an anterior cervical plating system with iliac crest autografts for the treatment of cervical degenerative disc disease. J Korean Neurosurg Soc. 2014;55:12–17. doi: 10.3340/jkns.2014.55.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lu Y, Fang Y, Shen X, et al. Does zero-profile anchored cage accompanied by a higher postoperative subsidence compared with cage-plate construct? A meta-analysis. J Orthop Surg Res. 2020;15:189. doi: 10.1186/s13018-020-01711-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang T, Guo N, Gao G, et al. Comparison of outcomes between Zero-p implant and anterior cervical plate interbody fusion systems for anterior cervical decompression and fusion: a systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2022;17:47. doi: 10.1186/s13018-022-02940-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. (A) Meta-analysis of Zero-p group versus CCP group in age; (B) Meta-analysis of Zero-p group versus CCP group in BMD; (C) Meta-analysis of Zero-p group versus CCP group in BMI; (D) Meta-analysis of Zero-p group versus CCP group in follow-up time.
Additional file 2. Meta-analysis of Zero-p group versus CCP group in preoperative NDI score.
Additional file 3. Meta-analysis of Zero-p group versus CCP group in preoperative JOA score.
Additional file 4. Meta-analysis of Zero-p group versus CCP group in preoperative VAS score.
Additional file 5. Meta-analysis of Zero-p group versus CCP group in preoperative PSTT.
Data Availability Statement
The data used to support the findings of this study are included within the article.