Abstract
Introduction
In the past decade there has been an increasing interest in the field of patient-reported outcome measures (PROMs) which are now commonly used alongside traditional outcome measures, such as morbidity and mortality. Since the FACE-Q Aesthetic development in 2010, it has been widely used in clinical practice and research, measuring the quality of life and patient satisfaction. It quantifies the impact and change across different aspects of cosmetic facial surgery and minimally invasive treatments.
We review how researchers have utilized the FACE-Q Aesthetic module to date, and aim to understand better whether and how it has enhanced our understanding and practice of aesthetic facial procedures.
Methods
We performed a systematic search of the literature. Publications that used the FACE-Q Aesthetic module to evaluate patient outcomes were included. Publications about the development of PROMs or modifications of the FACE-Q Aesthetic, translation or validation studies of the FACE-Q Aesthetic scales, papers not published in English, reviews, comments/discussions, or letters to the editor were excluded.
Results
Our search produced 1189 different articles; 70 remained after applying in- and exclusion criteria. Significant findings and associations were further explored. The need for evidence-based patient-reported outcome caused a growing uptake of the FACE-Q Aesthetic in cosmetic surgery and dermatology an increasing amount of evidence concerning facelift surgery, botulinum toxin, rhinoplasty, soft tissue fillers, scar treatments, and experimental areas.
Discussion
The FACE-Q Aesthetic has been used to contribute substantial evidence about the outcome from the patient perspective in cosmetic facial surgery and minimally invasive treatments. The FACE-Q Aesthetic holds great potential to improve quality of care and may fundamentally change the way we measure success in plastic surgery and dermatology.
Level of Evidence III
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00266-022-02974-9.
Introduction
Facial Aesthetic procedures are the most performed procedures in plastic surgery [1]. The number of surgical and non-surgical procedures keeps rising steadily [1, 2].
To objectify improvement of (area-specific) appearance and overall health-related quality of life (HR-QOL) is often challenging. Patient-reported outcome measures (PROMs) have gained considerable traction in the past decades, adding value to patients, care providers, and the process of care [1]. The FACE-Q Aesthetic module was developed for facial esthetic procedures, and proved to be a reliable instrument to measure patient-reported outcomes following surgical and non-surgical facial rejuvenation [3].
The FACE-Q Aesthetic was developed using item response theory principles, which maximizes the applicability: The items within the scales are ranked clinically relevant and score a so-called underlying trait (e.g., ‘satisfaction with facial appearance’). Responses to the items are rated on a four-point Likert scale (strongly disagree strongly agree), summed, and transformed to a score from 0 to100 for interpretability. The scales are grouped in four categories: Health-related Quality of Life (10 scales), Appearance appraisal scales (24 scales), and Adverse Effect checklists (6 scales). Checklists functioning differently from scales. They cover a topic such as ‘complications’ but are not necessarily correlated (e.g., hematoma, infection) thus cannot be ranked on one scale since there is no underlying trait However, checklists can provide clinically important information, such as monitoring for post-treatment complications. Given the modular structure, researchers and clinicians can choose the scales suitable to their research question or clinical situation.
In this review, we set out to examine the use of the FACE-Q Aesthetic in the plastic surgery and dermatology research literature and how this has expanded the understanding of the facial esthetic practice.
Methods
A literature search of studies using the FACE-Q Aesthetic scales as outcome measures was conducted by a trained medical librarian (WMB). Five search engines were queried: Embase via embase.com, MEDLINE ALL via Ovid, Cochrane CENTRAL registry of Trials via Wiley, with the limits set to articles published 2010 up to January 2021. Searches were specifically created aiming for PROMs (specific search terms in supplemental materials) [4].
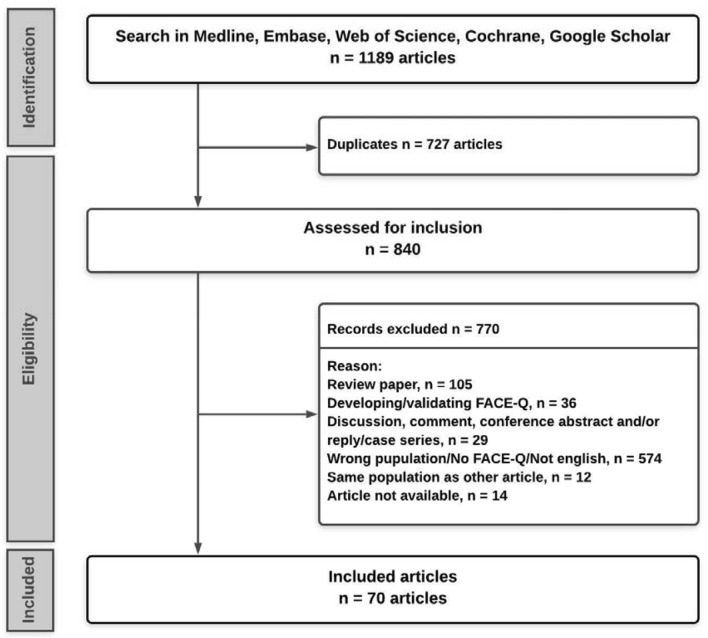
Articles were imported in Rayyan QCRI Review software and deduplicated using the method described by Bramer et al. [5]. Two authors (MO, IV) separately reviewed all the results by title and abstracts in a blinded fashion. All discrepancies were resolved through discussion or by a third author (Fig. 1).
Fig. 1.
Flowchart of article selection
Inclusion criteria consisted of using one or more FACE-Q Aesthetic scale to evaluate patient outcome, articles describing facial procedures, and primary research studies. Studies were excluded if they described the development of different PROMs, validated the FACE-Q Aesthetic in another language or culture, and if the format was either a conference abstract, (systematic) review, thesis, or a commentary (Table 1).
Table 1.
In- and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Using one or more domains of the FACE-Q esthetic to evaluate patient outcome | Developing and/or validating the FACE-Q or other PROM |
| Primary research study | Review |
| Facial procedures | Conference abstracts |
| Thesis | |
| Commentaries | |
| Letters to the editor | |
| A modified version of FACE-Q Aesthetic | |
| Other languages than English |
Full articles were reviewed. The following information was extracted: country of origin, sample size, FACE-Q Aesthetic scales, time of completion, and the level of evidence using Oxford Level of Evidence [6]. The time of completion of the FACE-Q Aesthetic was categorized in pre-treatment, short term (< 6 months post-treatment), and long term (> 6 months post-treatment). Scales Satisfaction with Decision, Satisfaction with Surgeon, Satisfaction with information, Satisfaction with office staff, Satisfaction with medical team, are not officially part of the Face-Q, we did include them in the review because a great number of articles did use them. It must be noted these scales are part of the Body-Q.
Results
Publications and Used Scales
Our search generated a total of 1189 results. After removing duplicates, a total of 840 unique publications remained. Following the abstract review, 166 articles remained for full-text analysis after applying exclusion criteria. A total of 70 articles from 13 different countries, published between 2012 and 2020, were included. Some metadata are displayed in Table 2.
Table 2.
Characteristics of the included articles
| Characteristics | Number |
|---|---|
| Total studies (n) | 70 |
| Number of patients | |
| Total | 5746 |
| Mean | 86 |
| Response rate (average with > FU point) | 83.2 |
| Before and after (no = 0, yes = 1) | 35 |
| Follow up (mean of max in months) | 16.7 |
| Follow up < 6months | 51 |
| Follow up > 6 months | 32 |
| Level of evidence | |
| Median | 3 |
| Mean | 2.96 |
From the 70 articles, a total of 5746 patients completed one or more FACE-Q Aesthetic scales, with an average number of included patients of 86 per publication. The average response rate was 83%. Thirty–five studies (50%) administered the FACE-Q Aesthetic before and after treatment. The average follow-up time was 16.7 months (ranging from 1 day to 70 months). For all studies, the mean level of evidence (possible scores 1–5) was 2.96 (median 3), corresponding to a case-control design. The Botox and fillers category scored highest with a mean level of evidence of 2.3 (median 2), encompassing all, except one, clinical trials.
Table 3 shows all scales from the FACE-Q Aesthetic and the number of times it was utilized. Supplementary information: papers using the FACE-Q Aesthetic, is an additional table, too large to be in the main body of text. It shows all the references and the scales that were utilized.
Table 3:
FACE-Q Aesthetic scales, number of times employed and papers in which they were used
| FACE-Q scale | Total | References |
|---|---|---|
| Appearance appraisal scales | ||
| Satisfaction with facial appearance overall | 32 | [7–40] |
| Satisfaction with skin | 6 | [22, 28, 36, 41–43] |
| Satisfaction with nose | 11 | [30, 32, 33, 38, 44–50] |
| Satisfaction with nostrils | 7 | [30, 37, 44–46, 48, 50] |
| Satisfaction with lips | 5 | [20, 36, 38, 51–55] |
| Satisfaction with forehead and eyebrows | 0 | – |
| Satisfaction with eyes | 3 | [56–58] |
| Satisfaction with eyelashes | 0 | – |
| Satisfaction with lower face and jawline | 15 | [10–15, 18, 20–22, 36, 37, 37, 55, 59, 60] |
| Satisfaction with chin | 8 | [13, 13, 15, 18, 31, 40, 59, 61] |
| Satisfaction with cheekbones | 1 | [15] |
| Satisfaction with cheeks | 13 | [9–15, 18, 28, 29, 36, 38, 60, 62] |
| Appraisal of lines–overall | 4 | [18, 22, 24, 63] |
| Appraisal of lines–between eyebrows | 1 | [64] |
| Appraisal of lines–forehead | 1 | [13] |
| Appraisal of lines–crow’s feet | 0 | – |
| Appraisal of lines–lips | 3 | [18, 53, 54] |
| Appraisal of lines–marionette | 1 | [18] |
| Appraisal of lines–nasolabial folds | 11 | [9, 10, 12–15, 18, 60, 65–68] |
| Appraisal of upper eyelids | 0 | – |
| Appraisal of lower eyelids | 0 | – |
| Appraisal of area under chin | 6 | [10, 11, 14, 40, 60, 69] |
| Appraisal of neck | 6 | [10–12, 14, 18, 60] |
| Total appearance appraisal scales | 116 | – |
| Quality of life scales | ||
| Psychological function | 30 | [9–14, 16, 17, 20, 23, 24, 26–31, 33, 37, 38, 40, 55, 58–63, 70, 71] |
| Social function | 26 | [9–14, 16, 17, 20, 22, 27, 28, 30, 33, 37, 38, 48, 50, 55, 58, 60–62, 70–72] |
| Age appraisal | 13 | [9–11, 14, 16–18, 26–29, 35, 73] |
| Age appraisal VAS | 12 | [10–12, 14, 17, 23, 26, 27, 29, 35, 62, 64] |
| Expectations | 2 | [30, 64] |
| Appearance-related distress | 5 | [30, 33, 58, 74, 75] |
| Recovery-early life impact | 15 | [8, 9, 11–14, 38, 51–54, 60, 61, 69, 73] |
| Satisfaction with outcome | 19 | [9, 11–14, 16, 28, 29, 33, 38, 52, 60–62, 64, 72, 76–78] |
| Satisfaction with decision | 15 | [9, 11–16, 29, 38, 56, 60, 61, 64, 70, 72] |
| Satisfaction with surgeon | 1 | [61] |
| Satisfaction with information | 0 | – |
| Satisfaction with medical team | 1 | [61] |
| Satisfaction with office staff | 0 | – |
| Total quality of life scales | 117 | – |
| Adverse effects checklists | ||
| Recovery–early symptoms | 8 | [13, 29, 52, 61, 62, 66, 69, 73] |
| Skin | 3 | [13, 29, 36] |
| Forehead, scalp, and eyebrows | 0 | – |
| Eyes | 0 | – |
| Nose | 0 | – |
| Cheeks, lower face and neck | 4 | [13, 37, 61, 79] |
| Lips | 0 | – |
| Total adverse effects checklists | 15 | – |
| Total (ALL) | 243 | – |
The top 3 FACE-Q Aesthetic scales used, consisted of ‘Satisfaction with Facial Appearance Overall’ (30 articles), ‘Psychological Function’ (25 articles), and ‘Social Function’ (21 articles), respectively.
Of the scales measuring appearance, the ‘Appearance appraisal’ scales were used more than satisfaction scales (120 times total, 19 out of 23 scales used). Specific area scales that were most used are: ‘Satisfaction with Lower Face and Jawline’(12 studies), ‘Satisfaction with Cheeks’(12 studies) and ‘Satisfaction with Nose’ (10 studies), and ‘Appraisal of Nasolabial Folds’(10 studies).
The second most used group was the HR-QoL group, and relatively frequently used (7 scales were used 91 times). The scale most utilized in this group was the ‘Psychological Function’ scale, used in 25 articles (43%). The studies that did not include a HRQoL scale (21/58) employed only 1 (median) appearance appraisal scale, reflecting an overall less elaborate use of FACE-Q scales in those studies.
The Adverse Effects group (checklists) was the least utilized, 13 studies (22%). The most used checklist in this group was the ‘Recovery–Early Symptoms’ checklist, used in 8 articles (13.8%). Only two scales of the ‘Patient Experience of Care’ category were used. Some scales were not used at all.
Facelift
A total of 10 articles comprising 563 patients used the FACE-Q Aesthetic for facelift procedures. 20 out of 40 independent FACE-Q Aesthetic scales were used. Three of these articles used the FACE-Q Aesthetic to evaluate patient-reported outcome before and after the facelift surgery. The average follow-up time was 27 months, with an average response rate of 72%. The median Oxford level of evidence score of these articles is 3. Most of these studies (70%) are retrospective and relatively small (average number of patients is 56 ranging from 13 to 124).
The most used scales targeting facial features were “Satisfaction with Facial Appearance Overall (8)”, “Satisfaction with Cheeks (8)”, “Satisfaction with Lower Face and Jawline (6)”, “Appraisal of Nasolabial Folds (6)”. The majority of the articles also measured “Psychological Function (7)”, “Social Function (7)”, “Satisfaction with Outcome (7),” and “Satisfaction with Decision (7)”.
The articles in this review used 20 out of 40 independent FACE-Q scales. Quantifying overall- and area-specific satisfaction to help understand the impact of facelift surgery.
Results show durability (1 year) [8, 62] and high satisfaction with facial appearance and psychological function for both surgical or minimally invasive facelift [8, 11, 14, 15, 62, 80]. Sinno et al. found that patients felt they appeared 2.5–7 years younger [14] .The use of area-specific FACE-Q scales showed significant improvement in multiple facial regions [9–11, 62, 80]. For example, using an alternative incision in bald facelift patients, Pascali et al. [12] found high satisfaction for the various critical areas examined, including scars. A facelift combined with blepharoplasty was significantly associated with a more remarkable improvement in satisfaction than a facelift without a blepharoplasty [10].
Rhinoplasty
A total of 10 articles comprising 937 patients (average of 94) used the FACE-Q Aesthetic to evaluate rhinoplasty procedures. The average follow-up item was 15 months, with an average response rate of 85%. Seventy percent collected data pre- and post-rhinoplasty. The average level of evidence for these articles is 2.7 (median 3). The “Satisfaction with Nose” scale was used in all ten articles. Followed by “Satisfaction with Nostrils” (5) and “Satisfaction with Facial Appearance Overall” (4), “Psychological Function” (4), and “Social Function” (5). Interestingly, the scales used to evaluate satisfaction with outcome or decision were used only once, compared to the facelift articles.
In rhinoplasty patients, factors such as age, race and income showed to be predicting success.
Studies showed an overall increase in quality of life, satisfaction with facial appearance, social function, and psychological function after rhinoplasty [30–32, 44, 48, 49]. Interestingly, not all groups benefited equally from a rhinoplasty. Two articles found being young, being of the Caucasian race, and having a high income associated with improved FACE-Q scores after rhinoplasty. Men reported improved satisfaction with facial appearance after rhinoplasty, but this did not result in a higher HRQoL than women [31, 44]. Also, Barone et al. found that older patients (> 65 years old) tend to be more focused on the tip of the nose [44].
Injectables
A total of 23 articles, including 2292 patients (average of 97), used the FACE-Q Aesthetic to evaluate injectable procedures. Of these articles, 12 had before and after measurements, the average follow-up time was 6.3 months. The response rate was 91% on average.
The most used appearance scale is “Satisfaction with Facial Appearance Overall” (9), after which “Satisfaction with Lips/Lower Face and Jawline (both 4) and “Appraisal of Nasolabial Folds” (also 4). The most used HR-QOL scale was “Psychological Function” (6), after which “Early Life Impact of Treatment,” “Age Appraisal,” and “Satisfaction with Outcome” were four times utilized. This category’s diverse character is reflected in the use of scales; not one scale is used by the majority of articles. For minimally invasive techniques, the FACE-Q was used mainly area-specific and proved to detect even small changes in satisfaction.
We found two studies measuring the effect of solely botulinum toxin treatment using the FACE-Q Aesthetic. These small-scale studies (n = 15 and 50 respectively) show significantly increased satisfaction on all FACE-Q domains after botulinum toxin treatment [18, 64]. Also, when using multimodal minimally invasive approaches to facial esthetic treatment, the outcome of perceived age after treatment seems to increase significantly [17, 18] and helped to guide daily practice [16, 17, 22, 24]—especially insights in selecting and combining treatment modalities. When performed by residents, nonsurgical facial rejuvenation procedures can improve patients’ quality of life and provide high satisfaction without compromising safety and enable constructive feedback. [16, 19] Fillers represent a valuable adjunct to surgical procedures for improving facial esthetics after injury and, consequently, patients’ quality of life affected by facial trauma. [24] Several studies used the FACE-Q to evaluate soft tissue fillers’ safety and effectiveness for peri–oral enhancement or midface contour deficiencies, a new type of filler for nasolabial folds [34], or jaw restoration [81]. These controlled trials [52, 53, 65, 66, 81] and prospective cohort studies [54, 78] demonstrated a significant improvement in satisfaction with facial appearance and showed the FACE-Q’s ability to detect small changes in satisfaction. Doyle et al. [57] found no significant difference between patients with silicone oil in situ and those with a phthisical eye (shrunken eye), providing valuable data for the shared decision-making process when considering this procedure, given its attached therapeutic, logistical, and financial implications. Bertossi et al. [75] Substantiated their algorithmic approach for facial fillers with FACE-Q scores.
Discussion
Since the introduction of the FACE-Q Aesthetic in 2010, it has been used to study facial surgery outcomes and helped to gain knowledge of the patient perspective and further deepen the understanding of what makes (non)-surgical esthetic procedures successful. The FACE-Q Aesthetic responses have shed light on evidence of patient satisfaction with (combinations) of different (non)-surgical techniques that would otherwise have stayed obscured. In facelifts durable results were shown, techniques were refined, patients felt they appeared 2.5–7 years younger and specific techniques such as scar placement in bald patients were investigated. In rhinoplasty patients, factors such as age, race and income showed to be predicting success. For minimally invasive techniques, the FACE-Q was used mainly area-specific and proved to detect even small changes in satisfaction.
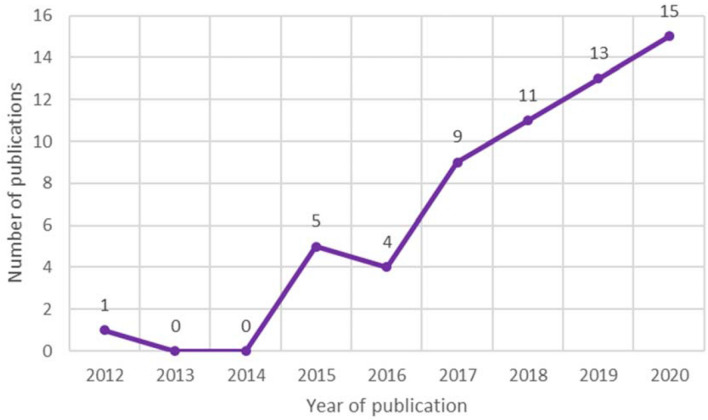
Since most cosmetic procedures are facial procedures, the impact of the FACE-Q could be substantial. The FACE-Q provides a standardized method to evaluate outcome, additionally providing the opportunity to monitor (rare) complications and adverse effects, as reported in Guarro et al.[82]. Since its inception, FACE-Q’s uptake has been increasing and more than tripled in the last three years (Fig. 2).
Fig. 2.
Number of articles using the FACE-Q Aesthetic by year
Some scales within the Appearance group were not used in published research. These scales measure appearance of eyelashes, crow’s feet, and lower/upper eyelid scales. The latter we found surprising because eyelid surgery is in the top 3 cosmetic surgical procedures.
Most studies used only a tiny subset of scales. It shows the versatility of the thirty–nine independently functioning scales and checklists but, in many cases, also leaves untapped potential since the FACE-Q comprises multiple scales, targeting different facial areas of interest, broadening its applicability. We expect that using the different FACE-Q Aesthetic scales will continue to increase since the importance of PROMS has been rapidly accepted by policymakers, clinicians, and researchers. Below we consider three main areas of practice and expand upon this review’s findings to shed light on where the FACE-Q Aesthetic has (and can) been used to understand the evidence-based, patient-centered surgical practice better.
Facelift, a Warm Welcome for PROMS
The potential of face lifting is unmatched in its ability to rejuvenate a sagging facial shape, affecting almost every area of the face. Numerous variations in the technique of facelift surgery have been described from skin excision only, to deep plane facelifts, to the current superficial musculoaponeurotic system operations. Instead of one technique being superior to another, a competent surgeon is likely to produce satisfactory results with different techniques when patients are appropriately selected. Although numerous studies have tried to compare outcomes produced by different techniques, high-quality data are scarce [83]. The FACE-Q adds a valuable perspective on the effectiveness of facelift procedures alongside traditional outcome measures such as morbidity and may provide the means to incorporate patient perspective and individualize our daily practice's algorithmic approach. For example, one study showed their artificial intelligence model to correctly estimate patients’ age reduction after different facelift techniques [60].
Rhinoplasty, Patient Characteristics and Prediction
Rhinoplasty is one of the most common operations performed–in 2020, well over 200.000 in the US alone [84].
It is among the most complex procedures in plastic surgery, and patients often have high expectations. Quantifying patient satisfaction pre- and post-rhinoplasty using FACE-Q scales (per area a specific scale could be added to obtain more specific insight alongside the more general scales) could help identify factors that hold a predictive value for success. And thus, it allows surgeons to determine in which areas and among which groups they are producing surgical success and where and among which groups they fail to do so. Moreover, it enables the surgeon to effectively identify specific anatomical areas of interest, patient expectations and, tailor treatment strategies.
We found age, income, and gender were found to be predictive of FACE-Q Aesthetic scores. Although it is beyond this review’s scope to speculate about the reasons behind the identified factors, other baseline characteristics such as disturbed body image, cause, history, and type of underlying deformity should be appreciated when interpreting outcomes [85].
Injectables (Botox and Fillers), FACE-Q Added to the Armamentarium
By far, botulinum toxin treatment is the most commonly performed facial enhancement method in the USA, followed by soft tissue fillers [1]. Together they generate close to $2 billion annually. We found that the use of Botox was associated with an increase in FACE-Q Aesthetic scores for all area specific scales, demonstrating effectiveness of Botox treatment and sensitivity of the FACE-Q Aesthetic as an instrument. Combining Botox and fillers in the aging face seems logical since skin quality and fat distribution change. The combined use lowered perceived age in patients. Also, after reconstructing traumatic wounds, fillers improved facial esthetics. These results seem to show great potential for the use of injectables in reconstructive surgery.
Difference in Score, When is it Important?
What are we to conclude if we find a difference in, e.g., four points FACE-Q score? Is the treatment effect large, warranting a widespread change in treatment strategies, or is it immaterial, suggesting no added value of the treatment? For example, the FACE-Q was used alongside 3D imagery in different studies to maximize the interpretability of their results: submental fat volume changes after deoxycholic acid injection [69, 77] nose morphometry after reconstruction [45], changes in facial appearance after treatment with sex hormones [25], and lower jaw contouring with titanium implants [37]. But how much change in score would mean a clinically relevant difference?
The minimally important difference (MID) provides a measure of the slightest change in the PRO of interest that patients perceive as important, leading the patient or clinician to consider a change in management [86]. Weinkle et al. [17] noticed a similar increase in FACE-Q score for their multimodal approach of non-surgical esthetic procedures to some studies evaluating surgical procedures. However, although a MID may help compare results across studies, care must be taken in applying the MID as it may differ for different situations as patient populations may vary.
There are two primary approaches for estimating a MID: distribution-based and anchor-based methods [87].
Heuristically—using the distribution-based method—one could take half the standard deviation of the mean score [86]. Using this method, in 2017, Klassen et al. found a MID for ‘Satisfaction with facial appearance’ of 7.0 for surgical and 7.1 for non-surgical procedures. Weitzman used the mean baseline standard deviation to calculate the MID for three scales: ‘Satisfaction With Nose’ scale (11.0); ‘Satisfaction With Nostrils’ (13.6); ‘Social Functioning’ (10.2). The anchor-based approach to calculating a MID compares changes in scores with an ‘anchor’ as a reference. Hall et al. looked at whether patients were still supportive of their decision to undergo treatment after peri–oral fillers [56].That binary question could potentially serve as an anchor for patients that seek peri–oral fillers. Although there are no accepted standards for appraising MID estimates’ credibility. [88], we suggest that future FACE-Q publications do calculate a MID, providing an intuitive measure for decision-makers.
Where to Go From Here?
As described in this review, the FACE-Q Aesthetic is increasingly used to determine the impact of different (combinations of) facial cosmetic procedures.
As plastic surgeons and dermatologists are eager to improve their practice using evidence-based medicine [89], with increase in volume and different types of facial esthetic procedures available, it is expedient to incorporate patient outcome measures routinely. FACE-Q implementation could be facilitated by using electronic data capture (EDC) software. Through the senior author, ready-to-use EDC formats can be obtained. Also, Computerized Adaptive Testing (CAT) could be applied- as it was developed using modern test theory (Rasch) -to reduce the burden for the patient to a minimum. Depending on the patients’ responses the computer selects the next item from the scale that provides the most information. It shortens the questionnaires during the assessment, while retaining accuracy [90, 91]. Data collected could be used in predictive models, helping doctors to identify patients who are highly likely to benefit from surgery and guide those unlikely to benefit from other treatment options [92].
The FACE-Q Aesthetic module and our review of the literature have several limitations. This review was not systematic and could have some omissions. However, we did not set out to conduct a systematic review. We did not have a specific question to answer; we wanted to provide healthcare providers with an overview of the published surgical research. Also, we did not include non-peer-reviewed studies, or those from conferences, although they might have contributed meaningful clinical data. Longitudinal research’s validity and reliability are highly dependent on the recruitment and retention of representative samples. The reported response rates of several references were marginal, impacting the studies’ reliability. Although the largest series in facelift started with 200 patients, it reported a response rate of only 38% [15]. Researchers may need practical and methodological support when asked to assist in collecting FACE-Q data to minimize bias. We should be cautious interpreting PROM results when comparing different techniques as outcomes do not only reflect procedures’ technical success. This makes it essential to combine PROM results with surgical or technical outcomes.
The discrepancy between the number of esthetic facial procedures performed and the FACE-Q’s use creates an opportunity to expand the understanding of treatment possibilities and patient satisfaction and improve our standard of care. Therefore, we encourage surgeons and dermatologists to introduce patient-reported outcome measurements into their esthetic practice in the future.
Conclusions
The FACE-Q is a PROM that allows both researchers and clinicians to answer essential questions on patient satisfaction, HR-QOL and adverse effects. Its modular structure with multiple scales enables researchers and clinicians to comprehensively answer clinical questions specific to surgical and nonsurgical facial interventions. The standardized scoring methodology is simple to use and permits comparisons between studies. FACE-Q’s uptake in research has markedly helped to amass knowledge of the patient perspective and increase the understanding of what makes esthetic procedures successful. While the use of FACE-Q has provided numerous valuable insights so far, the increased interest in PROs guarantees its continued use and ability to harbor innovations and standards of care.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
No funding was received for this article.
Declarations
Conflicts of interest
The FACE-Q is owned by Memorial Sloan-Kettering Cancer Center. The FACE-Q can be used free of charge for non-profit purposes (e.g., clinicians, researchers, and students). The other authors declared no potential conflicts of interest concerning the research, authorship, and publication of this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Plastic surgery statistics. In: American society of plastic surgeons. https://www.plasticsurgery.org/news/plastic-surgery-statistics. Accessed 10 Feb 2020
- 2.Cosmetic surgery stats: number of surgeries remains stable amid calls for greater regulation of quick fix solutions.| The British Association of Aesthetic Plastic Surgeons. https://baaps.org.uk/media/press_releases/1708/cosmetic_surgery_stats_number_of_surgeries_remains_stable_amid_calls_for_greater_regulation_of_quick_fix_solutions. Accessed 10 Feb 2020
- 3.Kosowski TR, McCarthy C, Reavey PL, et al. A systematic review of patient-reported outcome measures after facial cosmetic surgery and/or nonsurgical facial rejuvenation. Plast Reconstr Surg. 2009;123:1819–1827. doi: 10.1097/PRS.0b013e3181a3f361. [DOI] [PubMed] [Google Scholar]
- 4.Terwee CB, Jansma EP, Riphagen II, De Vet HCW. Development of a methodological pubmed search filter for finding studies on measurement properties of measurement instruments. Qual Life Res. 2009;18:1115–1123. doi: 10.1007/s11136-009-9528-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bramer WM, Giustini D, de Jonge GB, et al. De-duplication of database search results for systematic reviews in endnote. J Med Libr Assoc. 2016;104:240–243. doi: 10.3163/1536-5050.104.3.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guyatt GH, Oxman AD, Vist GE, et al. Grade: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clin res ed) 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tenna S, Cogliandro A, Barone M, et al. Comparative study using autologous fat grafts plus platelet-rich plasma with or without fractional CO2 laser resurfacing in treatment of acne scars: analysis of outcomes and satisfaction with FACE-Q. Aesthet Plast Surg. 2017;41:661–666. doi: 10.1007/s00266-017-0777-3. [DOI] [PubMed] [Google Scholar]
- 8.Kaye KO, Kästner S, Paprottka FJ, Gonser P. The liquid facelift: first hands-on experience with facial water jet-assisted liposuction as an additive technique for rhytidectomy–a case series of 25 patients. J Plast Reconstr Aesthet Surg. 2018;71:171–177. doi: 10.1016/j.bjps.2017.10.024. [DOI] [PubMed] [Google Scholar]
- 9.Gualdi A, Cambiaso-Daniel J, Gatti J, et al. Minimal undermining suspension technique (MUST): combined eyebrow and mid-face lift via temporal access. Aesth Plast Surg. 2017;41:40–46. doi: 10.1007/s00266-016-0745-3. [DOI] [PubMed] [Google Scholar]
- 10.Berger M, Weigert R, Pascal E, et al. Assessing improvement of patient satisfaction following facelift surgery using the FACE-Q scales: a prospective and multicenter study. Aesthet Plast Surg. 2019;43:370–375. doi: 10.1007/s00266-018-1277-9. [DOI] [PubMed] [Google Scholar]
- 11.Wang R, Yang J, Guo K, et al. Periauricular purse-string reinforced with SMAS plication and malaria fat pad elevation for mid-and lower facial rejuvenation: FACE-Q report. Ann Plast Surg. 2018;81:S59–S65. doi: 10.1097/SAP.0000000000001496. [DOI] [PubMed] [Google Scholar]
- 12.Pascali M, Botti C, Botti G. Face lifting in bald male patients: new trends and specific needs. Plast Reconstr Surg. 2020;145:60–69. doi: 10.1097/PRS.0000000000006397. [DOI] [PubMed] [Google Scholar]
- 13.Superficial S, Aponeurotic M, Gong M, et al. Lateral superficial muscular aponeurotic system systemectomy with orbicularis-malar fat repositioning: a procedure tailored for female asian patients. Dermatol Surg. 2020 doi: 10.1097/DSS.0000000000002202. [DOI] [PubMed] [Google Scholar]
- 14.Sinno S, Schwitzer J, Anzai L, Thorne CH. Face-lift satisfaction using the FACE-Q. Plast Reconstr Surg. 2015;136:239–242. doi: 10.1097/PRS.0000000000001412. [DOI] [PubMed] [Google Scholar]
- 15.Kappos EA, Temp M, Schaefer DJ, et al. Validating facial aesthetic surgery results with the FACE-Q. Plast Reconstr Surg. 2017;139:839–845. doi: 10.1097/PRS.0000000000003164. [DOI] [PubMed] [Google Scholar]
- 16.Qureshi AA, Parikh RP, Sharma K, et al. Nonsurgical facial rejuvenation: outcomes and safety of neuromodulator and soft-tissue filler procedures performed in a resident cosmetic clinic. Aesthet Plast Surg. 2017;41:1177–1183. doi: 10.1007/s00266-017-0892-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weinkle SH, Werschler WP, Teller CF, et al. Impact of comprehensive, minimally invasive, multimodal aesthetic treatment on satisfaction with facial appearance: the HARMONY Study. Aesthet Surg J. 2018;38:540–556. doi: 10.1093/asj/sjx179. [DOI] [PubMed] [Google Scholar]
- 18.Chang BL, Wilson AJ, Taglienti AJ, et al. Patient perceived benefit in facial aesthetic procedures: FACE-Q as a tool to study botulinum toxin injection outcomes. Aesthet Surg J. 2016;36:810–820. doi: 10.1093/asj/sjv244. [DOI] [PubMed] [Google Scholar]
- 19.Iorio ML, Stolle E, Brown BJ, et al. Plastic surgery training: evaluating patient satisfaction with facial fillers in a resident clinic. Aesthet Plast Surg. 2012;36:1361–1366. doi: 10.1007/s00266-012-9973-3. [DOI] [PubMed] [Google Scholar]
- 20.Chang CS, Chang BL, Lanni M, et al. Perioral rejuvenation: a prospective, quantitative dynamic three-dimensional analysis of a dual modality treatment. Aesthet Surg J. 2018;38:1225–1236. doi: 10.1093/asj/sjy060. [DOI] [PubMed] [Google Scholar]
- 21.Chin H, Observational A, Beer K, et al. Hyaluronic acid soft tissue filler for the treatment of the hypoplastic chin: an observational study. Dermatol Surg. 2020 doi: 10.1097/DSS.0000000000002326. [DOI] [PubMed] [Google Scholar]
- 22.Hible BP, Schwitzer J, Rossi AM. Assessing improvement of facial appearance and quality of life after minimally-invasive cosmetic dermatology procedures using the FACE-Q scales. J Drugs Dermatol. 2016;15:62–67. [PMC free article] [PubMed] [Google Scholar]
- 23.Ascher B, Rzany B, Kestemont P, et al. Significantly increased patient satisfaction following liquid formulation AbobotulinumtoxinA treatment in glabellar lines: FACE-Q outcomes from a phase 3 clinical trial. Aesthet Surg J. 2019;40:1–9. doi: 10.1093/asj/sjz248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bertossi D, Dell’Acqua I, Albanese M, et al. Face treatment using nonsurgical mini-invasive techniques as postsurgical procedure for traumatic injury. Aesthet Surg J. 2019;39:NP266–NP278. doi: 10.1093/asj/sjz017. [DOI] [PubMed] [Google Scholar]
- 25.Tebbens M, Nota NM, Liberton NPTJ, et al. Gender-affirming hormone treatment induces facial feminization in transwomen and masculinization in transmen: quantification by 3d scanning and patient-reported outcome measures. J Sex Med. 2019;16:746–754. doi: 10.1016/j.jsxm.2019.02.011. [DOI] [PubMed] [Google Scholar]
- 26.Denadai R, Chou P-Y, Su Y-Y, et al. The impacts of orthognathic surgery on the facial appearance and age perception of patients presenting skeletal class III deformity: an outcome study using the FACE-Q report and surgical professional-based panel assessment. Plast Reconstr Surg. 2020;145:1035–1046. doi: 10.1097/PRS.0000000000006650. [DOI] [PubMed] [Google Scholar]
- 27.Kaminer MS, Cohen JL, Shamban A, et al. Maximizing panfacial aesthetic outcomes: findings and recommendations from the HARMONY study. Dermatol Surg. 2020;46(6):810–817. doi: 10.1097/DSS.0000000000002271. [DOI] [PubMed] [Google Scholar]
- 28.Ozer K, Colak O. Micro-autologous fat transplantation combined with platelet-rich plasma for facial filling and regeneration. Clin Perspect Shad Evid-Based Med. 2019;30:672–677. doi: 10.1097/SCS.0000000000005122. [DOI] [PubMed] [Google Scholar]
- 29.Lee Z-H, Sinno S, Poudrier G, et al. Platelet rich plasma for photodamaged skin: a pilot study. J Cosmet Dermatol. 2018 doi: 10.1111/jocd.12676. [DOI] [PubMed] [Google Scholar]
- 30.East C, Badia L, Marsh D, et al. Measuring patient-reported outcomes in rhinoplasty using the FACE-Q: a single site study. Facial Plast Surg. 2017;33:461–469. doi: 10.1055/s-0037-1606637. [DOI] [PubMed] [Google Scholar]
- 31.Schwitzer JA, Albino FP, Mathis RK, et al. Assessing demographic differences in patient-perceived improvement in facial appearance and quality of life following rhinoplasty. Aesthet Surg J. 2015;35:784–793. doi: 10.1093/asj/sjv066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schwitzer JA, Sher SR, Fan KL, et al. Assessing patient-reported satisfaction with appearance and quality of life following rhinoplasty using the FACE-Q appraisal scales. Plast Reconstr Surg. 2015;135:830e–837e. doi: 10.1097/PRS.0000000000001159. [DOI] [PubMed] [Google Scholar]
- 33.Soni K, Patro SK, Aneja J, et al. Post-rhinoplasty outcomes in an Indian population assessed using the FACE-Q appraisal scales. Prospect Obs Study. 2020;134(3):247–251. doi: 10.1017/S0022215120000638. [DOI] [PubMed] [Google Scholar]
- 34.Kant SB, Mosterd K, Kelleners-smeets NWJ, et al. Measuring aesthetic results after facial skin cancer surgery by means of the FACE-Q. Eur J Plast Surg. 2020;43(5):541–548. doi: 10.1007/s00238-020-01625-z. [DOI] [Google Scholar]
- 35.Hersant B, SidAhmed-Mezi M, Chossat A, Meningaud JP. Multifractional microablative laser combined with spacially modulated ablative (SMA) technology for facial skin rejuvenation. Lasers Surg Med. 2017;49:78–83. doi: 10.1002/lsm.22561. [DOI] [PubMed] [Google Scholar]
- 36.Hassan H, Quinlan DJ, Ghanem A. Injectable platelet-rich fibrin for facial rejuvenation: a prospective, single-center study. J Cosmet Dermatol. 2020;19:3213–3221. doi: 10.1111/jocd.13692. [DOI] [PubMed] [Google Scholar]
- 37.Mommaerts MY. Patient- and clinician-reported outcomes of lower jaw contouring using patient-specific 3D-printed titanium implants. Int J Oral Maxillofac Surg. 2021;50:373–377. doi: 10.1016/j.ijom.2020.07.008. [DOI] [PubMed] [Google Scholar]
- 38.Hindin DI, Muetterties CE, Lee JC, et al. Internal distraction resulted in improved patient-reported outcomes for midface hypoplasia. J Craniofac Surg. 2018;29:139–143. doi: 10.1097/SCS.0000000000004109. [DOI] [PubMed] [Google Scholar]
- 39.Joseph AW, Ishii L, Joseph SS, et al. Prevalence of body dysmorphic disorder and surgeon diagnostic accuracy in facial plastic and oculoplastic surgery clinics. JAMA Facial Plast Surg. 2017;19:269–274. doi: 10.1001/jamafacial.2016.1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Beer K, Kaufman-Janette J, Bank D, et al. Safe and effective chin augmentation with the hyaluronic acid injectable filler, VYC-20L. Dermatol Surg. 2021;47:80–85. doi: 10.1097/DSS.0000000000002795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nacopoulos C, Gkouskou K, Karypidis D, et al. Telomere length and genetic variations affecting telomere length as biomarkers for facial regeneration with platelet-rich fibrin based on the low-speed centrifugation concept. J Cosmet Dermatol. 2018 doi: 10.1111/jocd.12666. [DOI] [PubMed] [Google Scholar]
- 42.Ogilvie P, Safa M, Chantrey J, et al. Improvements in satisfaction with skin after treatment of facial fine lines with VYC‐12 injectable gel: patient‐reported outcomes from a prospective study. J Cosmet Dermatol. 2020;19(5):1065–1070. doi: 10.1111/jocd.13129. [DOI] [PubMed] [Google Scholar]
- 43.Kalman DS, Hewlings S. The effect of oral hydrolyzed eggshell membrane on the appearance of hair, skin, and nails in healthy middle‐aged adults: a randomized double‐blind placebo‐controlled clinical trial. J Cosmet Dermatol. 2020;19(6):1463–1472. doi: 10.1111/jocd.13275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barone M, Cogliandro A, Cassotta G, et al. Rhinoplasty in elderly patients: analysis of outcomes and patient’s satisfaction following 20 years experiences. Eur J Plast Surg. 2018;41:395–400. doi: 10.1007/s00238-017-1387-7. [DOI] [Google Scholar]
- 45.Denadai R, Chou P-Y, Seo HJ, et al. Patient- and 3D morphometry-based nose outcomes after skeletofacial reconstruction. Sci Rep. 2020;10:4246. doi: 10.1038/s41598-020-61233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Barone M, Cogliandro A, Salzillo R, et al. The role of skin thickness in the choice of a rhinoplasty technique for thin-skinned patients: analysis of long-term results and patient satisfaction. Aesthet Plast Surg. 2020 doi: 10.1007/s00266-020-01763-6. [DOI] [PubMed] [Google Scholar]
- 47.Barone M, Cogliandro A, Salzillo R. Role of spreader flaps in rhinoplasty: analysis of patients undergoing correction for severe septal deviation with long-term follow-up. Aesthet Plast Surg. 2019;43:1006–1013. doi: 10.1007/s00266-019-01343-3. [DOI] [PubMed] [Google Scholar]
- 48.Fuller JC, Levesque PA, Lindsay RW. Analysis of patient-perceived nasal appearance evaluations following functional septorhinoplasty with spreader graft placement. JAMA Fac Plast Surg. 2019;21:305–311. doi: 10.1001/jamafacial.2018.2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Segreto F, Marangi GF, Cerbone V, et al. Nonsurgical rhinoplasty: a graft-BASED technique. Plast Reconstruct Surg Glob Open. 2019;7(6):e2241. doi: 10.1097/GOX.0000000000002241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Weitzman RE, Gadkaree SK, Justicz NS, et al. Patient‐perceived nasal appearance after septorhinoplasty with spreader versus extended spreader graft. Laryngoscope. 2020;131(4):765–772. doi: 10.1002/lary.28974. [DOI] [PubMed] [Google Scholar]
- 51.Taylor SC, Downie JB, Shamban A, Few J, Weichman BM, Schumacher A, Gallagher CJ. Lip and perioral enhancement with hyaluronic aciddermal fillers in individuals with skin of color. Dermatol Surg. 2019;45(7):959–967. doi: 10.1097/DSS.0000000000001842. [DOI] [PubMed] [Google Scholar]
- 52.Raspaldo H, Chantrey J, Belhaouari L, et al. Juvéderm volbella with lidocaine for lip and perioral enhancement: a prospective, randomized, controlled trial. Plastic Reconstr Surg Glob Open. 2015;3:1–8. doi: 10.1097/GOX.0000000000000266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Geronemus RG, Bank DE, Hardas B, et al. Safety and effectiveness of VYC-15L, a hyaluronic acid filler for lip and perioral enhancement: one-year results from a randomized, controlled study. Dermatol Surg. 2017;43:396–404. doi: 10.1097/DSS.0000000000001035. [DOI] [PubMed] [Google Scholar]
- 54.Rivkin A, Weinkle SH, Hardas B, et al. Safety and effectiveness of repeat treatment with VYC-15L for lip and perioral enhancement: results from a prospective multicenter study. Aesthet Surg J. 2019;39:413–422. doi: 10.1093/asj/sjy019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Denadai R, Chou P, Su Y, et al. Facial appearance and psychosocial features in orthognathic surgery: A FACE-Q- and 3D facial image-based comparative study of patient- clinician-, and lay-observer-reported outcomes. J clin med. 2019;8(6):909. doi: 10.3390/jcm8060909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hall MB, Roy S, Buckingham ED, et al. Novel use of a volumizing hyaluronic acid filler for treatment of infraorbital hollows author audio interview JAMA facial plastic surgery | original investigation. JAMA Facial Plast Surg. 2018;78746:1–6. doi: 10.1001/jamafacial.2018.0230. [DOI] [Google Scholar]
- 57.Doyle J, Yang Y, Norris JH, et al. A quality of life survey in patients with long-term silicone oil or phthisis bulbi. Graefes Arch Clin Exp Ophthalmol. 2018;256(5):879–884. doi: 10.1007/s00417-018-3934-8. [DOI] [PubMed] [Google Scholar]
- 58.Ar B, Ab K, Jl V, et al. Radiographic predictors of FACE-Q outcomes following non-operative orbital floor fracture management. J Craniofac Surg. 2020;31:388–391. doi: 10.1097/SCS.0000000000006356. [DOI] [PubMed] [Google Scholar]
- 59.Ogilvie P, Benouaiche L, Philipp-Dormston WG, et al. VYC-25L Hyaluronic acid injectable gel is safe and effective for long-term restoration and creation of volume of the lower face. Aesthet Surg J. 2020;40(9):NP499–NP510. doi: 10.1093/asj/sjaa013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gibstein AR, Chen K, Nakfoor B, et al. Facelift surgery turns back the clock: artificial intelligence and patient satisfaction quantitate value of procedure type and specific techniques. Aesthet Surg J. 2020;41(9):987–999. doi: 10.1093/asj/sjaa238. [DOI] [PubMed] [Google Scholar]
- 61.Tan SK, Leung WK, Tang ATH, Zwahlen RA. Patient’s satisfaction with facial appearance and psycho-social wellness after orthognathic surgery among Hong Kong Chinese using the FACE-Q. J Cranio-Maxillofac Surg. 2020;48:1106–1111. doi: 10.1016/j.jcms.2020.09.012. [DOI] [PubMed] [Google Scholar]
- 62.Nestor MS. Facial lift and patient satisfaction following treatment with absorbable suspension sutures: 12-month data from a prospective, masked, controlled clinical study. J Clin Aesthet Dermatol. 2019;12:18–26. [PMC free article] [PubMed] [Google Scholar]
- 63.Schlessinger J, Cohen JL, Shamban A, et al. A multicenter study to evaluate subject satisfaction with two treatments of AbobotulinumtoxinA a year in the glabellar lines. Dermatol Surg. 2020;47:504–509. doi: 10.1097/DSS.0000000000002846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Alouf E, Murphy T, Alouf G. Botulinum toxin type a: evaluation of onset and satisfaction. Plast Surg Nurs. 2018;38:105–113. doi: 10.1097/PSN.0000000000000236. [DOI] [PubMed] [Google Scholar]
- 65.Kaufman-Janette J, Taylor SC, Cox SE, et al. Efficacy and safety of a new resilient hyaluronic acid dermal filler, in the correction of moderate-to-severe nasolabial folds: a 64-week, prospective, multicenter, controlled, randomized, double-blind and within-subject study. J Cosmet Dermatol. 2019 doi: 10.1111/jocd.13100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Monheit G, Beer K, Hardas B, et al. Safety and effectiveness of the hyaluronic acid dermal filler VYC-17.5L for nasolabial folds: results of a randomized, controlled study. Dermatol Surg. 2018;44:670–678. doi: 10.1097/DSS.0000000000001529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Monheit G, Kaufman-Janette J, Joseph JH. Efficacy and safety of two resilient hyaluronic acid fillers in the treatment of moderate-to-severe nasolabial folds: a 64-week, prospective, multicenter, controlled, randomized, double-blinded, and within-subject study. Dermatol Surg. 2020;46:1521–1529. doi: 10.1097/DSS.0000000000002391. [DOI] [PubMed] [Google Scholar]
- 68.Dayan S, Maas CS, Grimes PE, et al. Safety and effectiveness of VYC-17.5 L for long-term correction of nasolabial folds. Aesthet Surg J. 2020;40:767–777. doi: 10.1093/asj/sjz200. [DOI] [PubMed] [Google Scholar]
- 69.Grow JN, Holding J, Korentager R. Assessing the efficacy of deoxycholic acid for the treatment of submental fat: a three-dimensional study. Aesthet Surg J. 2019;39:1400–1411. doi: 10.1093/asj/sjy194. [DOI] [PubMed] [Google Scholar]
- 70.Chou D, Chen P, Hsu C, et al. Comparison of orthognathic surgery outcomes between patients with and without underlying high-risk conditions: a multidisciplinary team-based approach and practical guidelines. J Clin Med. 2019;8:1760. doi: 10.3390/jcm8111760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schwitzer J, Albino F, Mathis R, et al. Assessing patient-reported outcomes following orthognathic surgery and osseous genioplasty. J Craniofac Surg. 2015;26:2293–2298. doi: 10.1097/SCS.0000000000001983. [DOI] [PubMed] [Google Scholar]
- 72.Kerckhove SBKCCEVD, Grzymala APD. Satisfaction with facial appearance and quality of life after treatment of face scars with a transparent facial pressure mask. Fac Plast Surg. 2017;34(04):394–399. doi: 10.1055/s-0038-1648249. [DOI] [PubMed] [Google Scholar]
- 73.Chang CS, Chang BL, Lanni M, et al. Perioral rejuvenation: a prospective, quantitative dynamic three-dimensional analysis of a dual modality treatment. Aesthet Surg J. 2018;38(11):1225–1236. doi: 10.1093/asj/sjy060. [DOI] [PubMed] [Google Scholar]
- 74.Occhiogrosso J, Derakhshan A, Hadlock TA, et al. Dermal filler treatment improves psychosocial well-being in facial paralysis patients. Fac Plast Surg Aesthet Med. 2020;22:1–8. doi: 10.1089/fpsam.2020.0148. [DOI] [PubMed] [Google Scholar]
- 75.Bertossi D, Nocini PF, Rahman E, et al. Non surgical facial reshaping using MD Codes. J Cosmet Dermatol. 2020;19:2219–2228. doi: 10.1111/jocd.13596. [DOI] [PubMed] [Google Scholar]
- 76.Samizadeh S, Belhaouari L. Effectiveness of growth factor‐induced therapy for skin rejuvenation: a case series. J Cosmet Dermatol. 2020;20(6):1867–1874. doi: 10.1111/jocd.13750. [DOI] [PubMed] [Google Scholar]
- 77.Jain M, Savage NE, Spiteri K, Snell BJ. A 3-dimensional quantitative analysis of volume loss following submental cryolipolysis. Aesthet Surg J. 2020;40:123–132. doi: 10.1093/asj/sjz145. [DOI] [PubMed] [Google Scholar]
- 78.Jones DH, Hessler J, Chapas A, et al. Microcannula injection of large gel particle hyaluronic acid for cheek augmentation and the correction of age-related midface contour deficiencies. Dermatol Surg. 2020;46:465–472. doi: 10.1097/DSS.0000000000002105. [DOI] [PubMed] [Google Scholar]
- 79.Chon BH, Hwang CJ, Perry JD. Long term patient experience with tetracycline injections for festoons. Plast Reconstr Surg. 2020;146(6):737e–743e. doi: 10.1097/PRS.0000000000007334. [DOI] [PubMed] [Google Scholar]
- 80.Wang R, Yang J, Guo K, et al. Asian facelift technique refinement with high patient satisfaction: FACE-Q report. Ann Plast Surg. 2018;81:1–7. doi: 10.1097/SAP.0000000000001496. [DOI] [PubMed] [Google Scholar]
- 81.Ogilvie P, Sattler G, Gaymans F, et al. Safe, effective chin and jaw restoration with VYC-25L hyaluronic acid injectable gel. Dermatol Surg. 2019;45:1294–1303. doi: 10.1097/DSS.0000000000001960. [DOI] [PubMed] [Google Scholar]
- 82.Guarro G, Brunelli F, Rasile B, Alfano C. Oculonasal synkinesis: video report and surgical solution of a rare phenomenon. Aesthet Surg J. 2017;37:879–883. doi: 10.1093/asj/sjx074. [DOI] [PubMed] [Google Scholar]
- 83.Chang S, Pusic A, Rohrich RJ. A systematic review of comparison of efficacy and complication rates among face-lift techniques. Plast Reconstr Surg. 2011;127:423–433. doi: 10.1097/PRS.0b013e3181f95c08. [DOI] [PubMed] [Google Scholar]
- 84.Plastic surgery statistics | Global plastic surgery statistics. In: ISAPS. https://www.isaps.org/medical-professionals/isaps-global-statistics/. Accessed 10 Sep 2021
- 85.van der Lei B, Bouman T. Validating facial aesthetic surgery results with the FACE-Q. Plast Reconstr Surg. 2018;141:184e–185e. doi: 10.1097/PRS.0000000000003987. [DOI] [PubMed] [Google Scholar]
- 86.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 87.Johnston BC, Ebrahim S, Carrasco-Labra A, et al. Minimally important difference estimates and methods: a protocol. BMJ Open. 2015 doi: 10.1136/bmjopen-2015-007953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Copay AG, Subach BR, Glassman SD, et al. Understanding the minimum clinically important difference: a review of concepts and methods. Spine J. 2007;7:541–546. doi: 10.1016/j.spinee.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 89.Ricci JA, Desai NS. Evidence-based medicine in plastic surgery: where did it come from and where is it going? Evidence-based medicine in plastic surgery. J Evid Based Med. 2014;7:68–71. doi: 10.1111/jebm.12096. [DOI] [PubMed] [Google Scholar]
- 90.Harrison CJ, Geerards D, Ottenhof MJ, et al. Computerised adaptive testing accurately predicts CLEFT-Q scores by selecting fewer, more patient-focused questions. J Plast Reconstr Aesthet Surg. 2019;72:1819–1824. doi: 10.1016/j.bjps.2019.05.039. [DOI] [PubMed] [Google Scholar]
- 91.Ottenhof MJ, Geerards D, Harrison C, et al. Applying computerized adaptive testing to the FACE-Q skin cancer module: individualizing patient-reported outcome measures in facial surgery. Plast Reconstr Surg. 2021 doi: 10.1097/PRS.0000000000008326. [DOI] [PubMed] [Google Scholar]
- 92.The arthroplasty candidacy help engine (The ACHE tool)—Health Economics Research Centre. https://www.herc.ox.ac.uk/research/estimating-costs-for-economic-evaluation/studies-12/the-arthroplasty-candidacy-help-engine-the-ache-tool-2. Accessed 18 Sep 2018
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.