ABSTRACT
There is no well-established procedure for the management of small penis syndrome (SPS), especially when psychological interventions fail. This study aimed at systematically evaluating the physical and psychological benefits of penile augmentation (PA) using injectable hyaluronic acid (HA) gel. Thirty-eight patients receiving PA with HA gel from January 2017 to March 2020 were included and followed up for 1 year. Penile size, erectile function, and psychological burden measured by the Index of Male Genital Image (IMGI), Index of International Erectile Function (IIEF), and Beliefs about Penis Size (BPAS), respectively, were assessed at the beginning and at 1, 3, 6, and 12 months postinjection. The volume of HA gel injected was 21.5 ± 3.7 ml. Compared to baseline data, flaccid penile girth and length significantly increased by 3.41 ± 0.95 cm (P < 0.01) and 2.55 ± 0.55 cm (P < 0.01) at the 1st month postinjection, respectively. At the endpoint, despite attenuations, statistically significant improvements in flaccid penis size were still obtained, namely 2.44 ± 1.14 cm in girth (P < 0.01) and 1.65 ± 0.59 cm in length (P < 0.01). Similarly, erectile penile girth statistically increased by 1.32 ± 1.02 cm (P < 0.01) at the 1st month but were only 0.80 ± 0.54 cm bigger than baseline (P < 0.01) at the endpoint. At the 1st month, the average score of IMGI and the mean score of IIEF statistically increased by 46.2 ± 10.5 (P < 0.01) and 7.6 ± 6.2 (P < 0.01), respectively; the score of BAPS significantly decreased by 18.3 ± 4.5 (P < 0.01). These alterations remained steady during follow-up. Considering the significant penile size improvement, lasting psychological benefit, and low complication rate, PA with HA might serve as an appropriate alternative for patients with SPS.
Keywords: hyaluronic acid, penile augmentation, small penis syndrome
INTRODUCTION
Throughout history, penis size has been a continuous concern associated with masculinity for men.1 Recently, with emphasis on sexual liberation and openness, a greater frequency of occurrence of sex-related occasions in daily lives has led to a growing interest in penile size and consequent potential feelings of sexual inferiority.2 Besides, as pornography and commercial advertisements claim “bigger is better” and promote a misleading penile size,3 even a man with a normal penis may have distorted penile cognition and experience great anxiety, and this is called the “small penis syndrome (SPS)”. This anxiety lowers men’s sexual self-esteem and engenders avoidance of occasions where genitals have to be exposed in front of others.4 Body dysmorphic disorder (BDD) might occur in some extreme cases, resulting in more psychological burdens and personal ability impairments.5 Subsequently, a demand for penile enlargement appears.
Deficiency of high-quality evidence makes it difficult to evaluate which procedure is the most suited for the management of SPS.6,7 Education and psychological consultation are recommended for patients, in order to correct their wrong perceptions about penile size and restore sexual self-esteem.4,5 Although many studies have reported that the majority of patients seeking penile augmentation might give up after consultation, there is no consensus on ways to conduct this procedure.3 Presence of many alternative methods, after the failure of psychological intervention, confuses the patient due to the dearth of evidences to supporting their choice of treatment. Noninvasive methods, including vacuum devices, penile extenders, and botulinum toxin, have been reported to have limited temporary effects.8 Surgical strategies, such as dissection of the suspensory ligament, autologous fat, or venous graft transplantation, have been proven valid, but have high complication rates.9 An effective and less invasive measure is urgently needed.
Injectable hyaluronic acid (HA) gel is one of the most commonly used soft tissue filler for plastic surgeries.10 The application of HA for penile augmentation (PA) has recently gained increasing popularity owing to its biocompatibility and mild transient adverse effects.11,12 Besides, HA is more cost-effective than other materials with reasonable efficacy.13 Newly invented cross-linked HA has more durable effect over time.14 These suggest that penile augmentation with HA might be an appropriate alternative for patients after unsuccessful psychological consultation. In this study, we aimed to provide a comprehensive profile for this method.
PATIENTS AND METHODS
Patients
Thirty-eight patients receiving PA using HA gel from January 2017 to March 2020 at Peking University People’s Hospital (Beijing, China) and Eden Hospital (Beijing, China) were included. Detailed criteria of inclusion were as follows: (1) age >18 years and <70 years; (2) extremely unsatisfactory penile size; (3) strong desire for penile size alterations after initial psychological consultation; and (4) absence of congenital or acquired phallus defects, such as micropenis and Peyronie’s disease. A thorough review of medical history was performed to exclude mental illness, diabetes mellitus, coagulopathy, or previous penile surgery. Written informed consent was obtained from all the participants before surgery. Ethic approval was obtained at Eden Hospital (No. S2017011).
Injection procedure
Patients were placed in the supine position. Local anesthesia was achieved by injecting 1 ml of 0.2% lidocaine into the phallus root. Injection of HA gel (Perfectfill; Kailepu Co., Ltd., Jinan, China) into the potential space between the Dartos’ fascia and Buck’s fascia along the penile axis was conducted after reconfirmation of the penile block. The Fanning technique, as previously published, was applied.15 Details are shown in Figure 1. First, penile dorsal skin was incised at 1 o’clock or 11 o’clock positions to avoid dorsal pedicle injury. Thereafter, the subcutaneous space was fully dilated with an 18-gauge cannula needle to facilitate the injection of HA. To evenly distribute the filler along the penile axis, the direction of the cannula was constantly adjusted while the HA gel was continuously injected. A low dose of HA gel (approximately 0.3 ml) per injection was recommended. Hand molding was also helpful for shaping. If necessary, the injection cannula was inserted between the 1 o’clock and 5 o’clock positions or between the 7 o’clock and 11 o’clock positions (multiple-puncture technique). A supplementary injection with a 30-gauge cannula was used to restore a natural penile shape. Care was taken that the injected material did not cover the ventral part of the penis in cases of urethral compression or injury. After the procedure, the injected surface was thoroughly massaged to redistribute the HA as uniformly as possible. Abstinence from sexual intercourse for 4 weeks was recommended.
Figure 1.
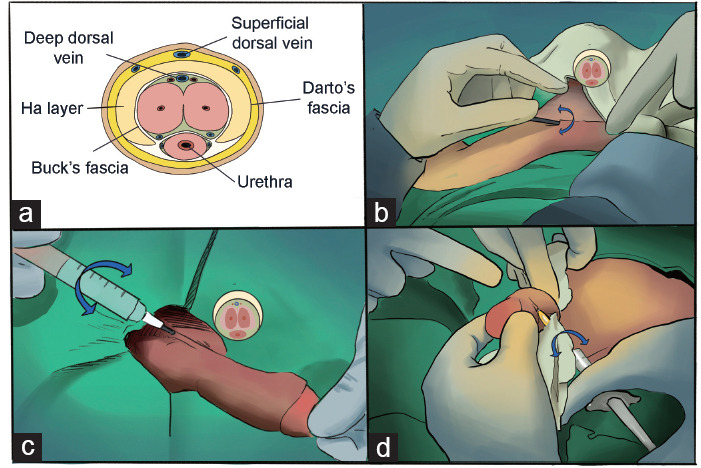
Illustration of penile augmentation with hyaluronic acid injection. (a) Cross sectional view of penile augmentation with hyaluronic acid. (b) Full dilation of penile shaft subcutaneous space via an 18-gauge cannula needle through incisions at penile root. (c) Representative of hyaluronic acid injection using Fanning technique. (d) Supplementary injection of hyaluronic acid.
Penile girth and length
Penile size was measured in both the flaccid state, without stretching, and the erectile state. The circumference of the penis was repeatedly measured at the root, sub-coronal sulcus, and middle. The mean girth of the penis was defined as the average value of the circumferences at these three sites. With the urethral meatus set as the base point, length was defined as the linear distance from the pubic-penile junction to the tip of the glans. Penile girth and length were measured at 1 week before surgery and 1, 3, 6 and 12 months postoperatively.
Index of Male Genital Image (IMGI)
IMGI was firstly reported by Davis et al.16 This brief scale is composed of 14 items that focus on actual genital image, and its score is a reflection of men’s overall satisfaction with their genitals. High IMGI scores imply overall satisfaction with the genital image. We chose IMGI as the main objective outcome measurement to evaluate alterations in penile images caused by PA using HA gel. Patients were required to complete this scale every time the measurements were conducted.
International Index of Erectile Function (IIEF)
IIEF was first invented as an evaluation tool for erectile function and clinical outcome during the development of sildenafil.17 Considering the specific function of the penis, it was vital to evaluate the effects of PA using HA gel on erectile function. Therefore, we chose IIEF as the main method of measurement to evaluate these effects. The questionnaire was also completed at the time points mentioned above.
Beliefs about Penis Size (BAPS)
The BAPS is a brief scale consisting of 10 items designed for measuring shame resulting from distorted cognition of penis size.18 This short scale was proven effective in measuring patients’ concerns about the phallus and the consequent psychological burden. We adopted this self-reporting scale to evaluate patients’ psychological status. High BAPS scores indicated severe shame.
Safety assessment
Medical records were thoroughly reviewed for perioperative adverse effects. General physical examination and andrological examination were performed each time the patients returned to our hospital for follow-up. Adverse complications reported by the patients were reconfirmed and recorded by physicians.
Statistical analyses
Descriptive analysis was applied to the demographic data. Continuous variables are described as mean ± standard deviation (s.d.). Baseline data were compared to those obtained before surgery. A paired t-test was used for comparisons between baseline data and each group of data obtained after injection. Data analysis was conducted using SPSS (version 25.0; SPSS, Chicago, IL, USA) for Windows. P < 0.05 was considered statistically significant.
RESULTS
Demographic data
Thirty-eight patients were successfully followed-up. The age of the men was 31.2 ± 6.7 years. Most of them were single and heterosexual. The detailed information is shown in Table 1. The initial penile length was 5.39 ± 0.47 cm in the flaccid unstretched state and 10.09 ± 1.25 cm in the erect state. The baseline circumference of the penis was 7.46 ± 0.62 cm before erection and 9.96 ± 1.24 cm after erection.
Table 1.
Descriptive demographic information of patients
| Category | Patient, n (%) |
|---|---|
| Age (year) | |
| >30 | 21 (55.3) |
| ≤30 | 17 (44.7) |
| Marital status | |
| Single | 24 (63.2) |
| Coupled | 14 (36.8) |
| Body mass index (kg cm−2) | |
| ≥18.5 and ≤24.9 | 6 (15.8) |
| ≥25.0 and ≤29.9 | 20 (52.6) |
| ≥30.0 | 12 (31.6) |
| Sexual orientation | |
| Heterosexual | 36 (94.8) |
| Homosexual | 2 (5.2) |
| Bisexual | 0 (0) |
Penile size alterations
The mean time required for the whole process was 35.4 min and the volume of HA injected was 21.5 ± 3.7 ml. The size-augmenting effects of HA injection on the penis are shown in Supplementary Figure 1 (784.1KB, tif) . Compared to baseline, the enhancing effect on penile circumference peaked at 1 month after injection. Flaccid penile circumference at this time statistically increased to 10.87 ± 0.71 cm (P < 0.01). This enhancement gradually decreased with time. At the end of follow-up, the flaccid penile circumference decreased to 9.89 ± 0.68 cm but remained statistically larger than baseline (P < 0.01). Alterations in penile length were also observed after injection. At the 1st month postoperation, flaccid length statistically increased to 7.44 ± 0.33 cm (P < 0.01). Then the penis also shortened gradually. The length of the flaccid penis finally decreased to 7.04 ± 0.43 cm, which was still statistically longer than baseline (P < 0.01). With regard to erectile size, we observed similar trends. The erect penile girth and length statistically increased to 11.28 ± 0.89 cm (P < 0.01) and 10.81 ± 1.11 cm (P < 0.01) at the 1st month postinjection, respectively. By the end of follow-up, despite attenuations in augmenting effects, the erect penile girth and length were still statistically improved than baseline, that is, 10.76 ± 0.85 cm (P < 0.01) in girth and 10.49 ± 0.89 cm (P < 0.01) in length. The increment in erect penile size was smaller than that of flaccid penile size. Detailed penile data are presented in Figure 2 and Supplementary Table 1.
Figure 2.
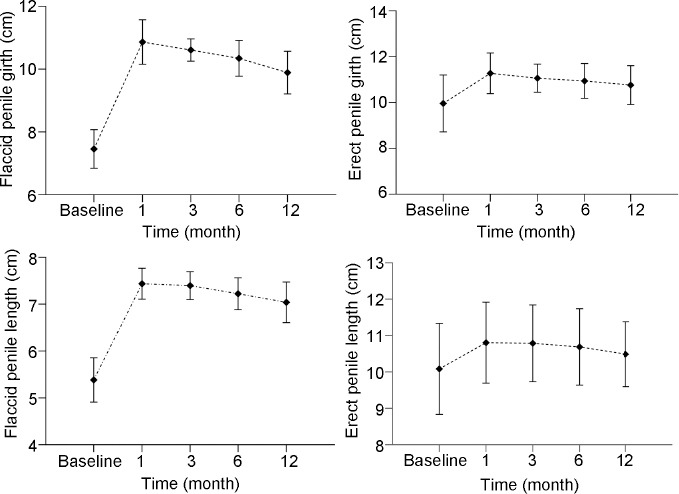
Alteration trends in penile size after penile augmentation with hyaluronic acid.
Supplementary Table 1.
Baseline penile size and gains after injection
| Baseline | Increments | ||||
|---|---|---|---|---|---|
|
| |||||
| 1 month* | 3 months* | 6 months* | 12 months* | ||
| Flaccid penile girth/cm | 7.46±0.62 | 3.41±0.95 | 2.85±0.85 | 2.58±0.97 | 2.44±1.14 |
| Erect penile girth/cm | 9.96±1.24 | 1.32±1.02 | 1.19±0.81 | 0.91±0.75 | 0.80±0.54 |
| Flaccid penile length/cm | 5.39±0.45 | 2.55±0.55 | 2.15±0.85 | 1.78±0.97 | 1.65±0.59 |
| Erect penile length/cm | 10.09±1.25 | 1.34±0.76 | 0.98±0.73 | 0.90±0.46 | 0.64±0.41 |
*Statistically significant difference (P<0.01) for paired t-test when compared with baseline data
Psychological outcomes
Before injection, the mean IMGI score was 33.0 ± 9.9. Improvement was observed postoperatively. The mean IMGI score significantly increased to 79.8 ± 6.3 at the 1st month (vs baseline, P < 0.01). Then, the IMGI scores remained steady and did not coincide with the objective trend of alterations of penis size (Figure 3 and Supplementary Table 2), indicating that psychological outcomes were more constant than clinical outcomes. Although this procedure only altered penis size, satisfaction also improved in other aspects of genital image, such as the pubic hair, shape of glans, and genital veins. This finding might partly result from the possibility that this intervention could help build up sexual self-esteem.
Figure 3.
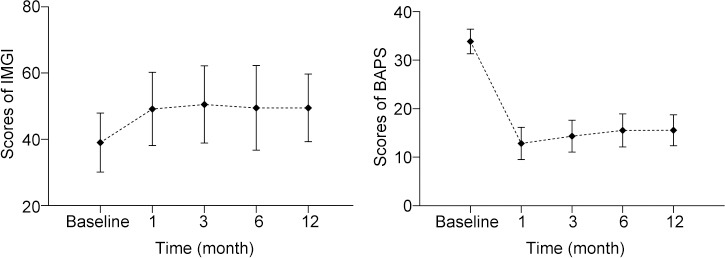
Changes of scores of IMGI and BAPS. IMGI: index of male genital image; BAPS: Beliefs about Penis Size.
Supplementary Table 2.
Changes of Scale scores during the study
| Baseline | 1 month* | 3 months* | 6 months* | 12 months* | |
|---|---|---|---|---|---|
| IIEF | 48.1±4.0 | 55.6±5.6 | 56.2±5.7 | 56.3±5.8 | 55.7±6.4 |
| BAPS | 33.9±2.5 | 12.8±3.3 | 14.3±3.3 | 15.5±3.4 | 15.6±3.2 |
| IMGI | 33.0±9.9 | 79.8±6.3 | 78.7±6.2 | 78.3±6.1 | 79.2±6.0 |
*Statistically significant difference (P<0.01) for paired t-test when compared with baseline data. IMGI: Index of Male Genital Image; IIEF: Index of International Erectile Function; BAPS: beliefs about penis size
Before the intervention, the average IIEF score was 48.1 ± 4.0. Postoperatively, the mean IIEF score statistically increased to 55.6 ± 5.6 in the 1st month (P < 0.01). Apart from function evaluation, other elements of the IIEF also measured sexual desire, intercourse satisfaction, and overall satisfaction. It is not surprising that the total IIEF score also improved. IIEF scores did not vary much in the following observations (Figure 3 and Supplementary Table 2).
The mean BAPS score was 33.9 ± 2.5 before surgery and statistically decreased to 12.8 ± 3.3 at the 1st month (P < 0.01), indicating revised beliefs about penis size and greater satisfaction achieved by means of PA with HA gel. Routine follow-up showed that the BAPS score was fixed at a steady level, which indicated that psychological outcomes were more constant than clinical outcomes (Figure 3 and Supplementary Table 2).
Safety assessment
In total, we observed two cases of penile edema and one case of subcutaneous bleeding, which resolved spontaneously without extra medication in 4 weeks, indicating that PA using HA gel is a safe procedure.
DISCUSSION
In total, 38 patients receiving PA with HA completed the follow-up and were enrolled in the analysis. Compared to the data derived from a previous large population-based study measuring penis size of Chinese healthy men, the mean penile size of our sample was smaller but still within the normal range.19
Our results indicated that PA with HA gel was effective in enlarging the phallus. Improvements in the girth and length of the flaccid penis were observed in all cases. The maximal increase of girth (3.41 ± 0.95 cm) and length (2.55 ± 0.55 cm) in the flaccid state are similar to those reported in previous studies.11,15 First, the even distribution of HA gel directly enlarged the diameter of the flaccid penis. Second, the injection disrupted the integrity of the Dartos’ fascia and further liberated the corpus penis due to reduced contraction force. In addition, the HA gel we used had high density and strong hydrophilicity. Although the injection volume of HA was 21.5 ± 3.7 ml, the weight and volume gain (measured by water absorbed by HA gel) were relatively high when compared to the original penis itself. The increase in gravity countered further contraction of the corpus penile, especially in the flaccid state. The size gains in the erect state were smaller. Maximal increments of girth and length were 1.40 ± 0.34 cm and 1.34 ± 0.76 cm, respectively. In the erect state, compression of the penile skin and penile position switch limited the impact of injected HA gel on penile size. As a result, it is not surprising that the increments of erectile girth and length were smaller.20
Apart from alterations in penile size, psychological benefits were also observed, as demonstrated by statistically significant changes in IMGI and BAPS scores. This is vital for PA because it is conducted mainly for the sake of anxiety elimination. We also found that BAPS and IMGI scores remained quite steady despite the fact that the augmenting effects of HA gel injection diminished gradually with time. This indicates that psychological outcomes were more constant than clinical outcomes. Previous literature illustrated a lasting penile size modification after PA using HA gel for 18 months.11 Therefore, we infer that the psychological benefits brought about by HA injection also persisted, since penile size would never change rapidly. Future studies will help to prove this hypothesis.
Safety is essential in surgical augmentation for patients with SPS. Severe complications could be disastrous and engender great dissatisfaction, as patients who underwent surgery were physically normal. The adverse effects observed were mild and transient and all disappeared in 4 weeks when treated with caution, which is similar to previous research, demonstrating that HA injection is a safe technique.21,22 Penile edema occurred in two (5.3%) patients with a redundant prepuce. Transient oedema was associated with lymphatic compression caused by accumulated HA gel in the distal penis.22 Circumcision and HA injection at the same time for patients with a redundant prepuce might prevent postoperative oedema. Application of an elastic bandage could accelerate the disappearance of oedema. Subcutaneous bleeding occurred in one (2.6%) patient due to direct vascular damage. This complication resolved spontaneously without any intervention. Overall, it is inferred that PA using HA is safe.
Currently, various penile augmentation strategies have been applied to men seeking penile enlargement. A summary of previous studies on penile augmentation using a single technique for patients with SPS are shown in Table 2.
Table 2.
Studies related to penile shaft augmentation with single technique
| Study | n | Technique | Follow-up (month) | Flaccid penile shaft circumference (cm) | Flaccid penile length (cm) | Complication | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||
| Baseline | Endpoint | Gain | Baseline | Endpoint | Gain | Case (n) | Rate (%) | ||||
| Nikoobakht et al.232011 | 23 | Extender | 3 | 8.8±1.2a | 10.5±1.2a | NR | NR | NR | NR | NR | NR |
| Nowroozi et al.242015 | 54 | Extender | 6 | 8.6±1.0a | 10.3±1.4a | 1.7±0.8a | NR | NR | NR | NR | NR |
| Gontero et al.252009 | 16 | Extender | 6 | NR | NR | 2.05±1.32a | NR | NR | 0.03d | NR | NR |
| Aghamir et al.262006 | 30 | Vacuum pump | 8 | 6.9–9.4b | 7–9.7b | NR | NR | NR | NR | NR | NR |
| Kang et al.272012 | 52 | Autologous fat injection | 6 | NR | NR | NR | 7.01±0.39a | 9.29±0.82a | NR | 1 | 1.92 |
| Xu et al.202016 | 23 | Dermal fat graft | 6 | 6.27±0.53a | 8.54±0.99a | 2.27±0.54a | 8.25±0.60a | 9.92±0.89a | 1.67±0.46a | 23 | 100 |
| Shaeer282014 | 40 | Flap | 18 | 5.8±1.3a | 8.5±1.4a | 31.8%a | 9.3±1.1a | 14.5±1.1a | 55.6%a | 40 | 100 |
| Xu et al.292019 | 78 | Acellular dermal matrix | 3 | NR | NR | NR | NR | NR | 1.1 (0.5–2.1)c | 56 | 71.79 |
| Alei et al.302012 | 69 | Acellular dermal matrix | 12 | 8.1 (5.4–10.7)c | 11.3 (8.2–13.2)c | NR | NR | NR | NR | 69 | 100 |
| Jin et al.312011 | 69 | Collagen scaffold | 6 | NR | NR | NR | 8.18±0.83a | 12.19±1.27a | NR | 6 | 8.70 |
| Protogerou et al.322010 | 40 | Ligament dissection | 12 | 9.5±2.2a | NR | 3.5±1.3a | NR | NR | NR | 1 | 2.5 |
| Zhang et al.332016 | 17 | Dermal graft | 4 | 4.1±2.4a | 6.8±1.2a | 2.7±1.4a | 5.8±1.0a | 7.3±0.9a | 1.5±0.6a | 8 | 26.7 |
aMean±s.d.; brange; cmean (range); dmean. NR: not reported; s.d.: standard deviation
For noninvasive penile augmentation, vacuum pumps and penile extenders are popular, especially in commercial fields. However, few studies have assessed the efficacy and safety of noninvasive penile extenders or vacuum pumps for SPS, and the results were disappointing. Both the penile extender and vacuum pump require daily or weekly hours of application. Only limited augmenting effects have been reported. Once the treatment is discontinued, the penis returns to its initial size within months.23,24,25,26 For example, a vacuum pump was recommended for 20–30 min per session, three times a week for 6 months in the study by Aghamir et al.26 Only 11.1% of patients reported a length gain of >1 cm. The satisfaction rate was approximately 30%. In the study by Nowroozi et al.,24 wearing a penile extender daily for 4–6 h was recommended for 6 months. A length gain of 1.7 ± 0.8 cm was reported. When treatment was discontinued, no improvement was observed. Similar findings have been reported in other studies. Based on time-consuming applications and limited temporary augmenting effects, it is difficult to say that these methods are satisfactory.
Surgical penile augmentation has definite and lasting effects. Kang et al.27 reported significant penile girth improvement and high satisfaction in patients receiving autologous fat injections. However, this result is contentious. It is well known that impaired blood supply can easily cause fat reabsorption and result in penile morphosis.20 Dermal fat grafts were superior to pure fat grafts in terms of volume maintenance. However, this procedure is more invasive and requires a much longer recovery time (i.e., 2–3 months). In the study by Xu et al.20, all patients had postoperative penile edema that resolved within 2–8 weeks. Moreover, unaesthetic scars at the graft harvest site were inevitable. In the study by Shaeer,28 penile augmentation with a superficial circumflex iliac flap achieved 38% gains in length and 55.6% gains in girth compared to baseline flaccid penis size. The augmenting effects were surprisingly good. However, this technique is complicated and traumatic. The mean operation time was 2.5 h. Severe complications, including penile skin ulceration, donor site dehiscence, and infection occurred in 17% patients. Further plastic surgery may have been required for scar revision. Penile augmentation with biological patches is another simple strategy for achieving definite augmenting effects.29,30,31 However, the severe complication rates of this procedure were unacceptably high. Xu et al.29 reported that 34.62% of patients underwent postoperative wound hematoma, delayed healing, infection, and penile skin necrosis. SPS patients all have a normal penis. Severe postoperative complications might increase patients’ psychological burden and cause potential conflicts. Currently, invasive PA is not recommended by mainstream doctors because of its high complication rates. Penile ligament dissection can only increase penile length and is often conducted with other techniques for better results.32
When compared to the surgical methods mentioned above, the augmenting effects of PA with HA were comparable. However, several advantages make PA with HA a more appropriate choice. First, this method is minimally invasive and easy to perform. An unobvious 4-mm long incision was required. Subcutaneous injection was performed under local anesthesia with an operation time of 35.4 ± 16.2 min. Second, the patients’ psychological burden could be effectively relieved after injection. Furthermore, the postinjection complication rate is low, and most cases are mild and easy to handle. Finally, durable effects can be achieved by consistent supplementary injection in theory.
In this study, we provided a thorough and comprehensive profile of PA using HA for the management of SPS compared to previous studies. The study population was restricted to those who underwent unsuccessful psychological consultations. Therefore, unnecessary interventions were avoided. Moreover, the application of structured psychometry also enabled us to research the patients’ psychological traits more precisely. However, several limitations still exist. The small size of the population limited the generalizability of our study. The combined questionnaire in this study contained 53 items, which brought about a huge responsive burden for participants. However, we believe that this helped to comprehensively evaluate the benefits of PA with HA. In addition, we did not compare PA using HA gel with other penile augmentation strategies in a randomized manner. Further studies, including traditional surgical penile augmentation methods, might be needed to standardize the management of SPS patients after failure of psychological interventions.
CONCLUSIONS
PA with HA gel is an effective and minimally invasive method for the management of SPS and could be an appropriate alternative for patients who experience psychological intervention failures.
AUTHOR CONTRIBUTIONS
CLZ participated in the surgery, study design, and follow-up and wrote this manuscript. YQ performed data acquisition and data analysis and helped draft this manuscript. HL participated in follow-up. QL, WJB, and TX participated in the study design. XWZ performed all the surgeries, designed, and guaranteed this study. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declare no competing interests.
Supplementary Information is linked to the online version of the paper on the Asian Journal of Andrology website.
Postinjection effects of penile augmentation with hyaluronic acid injection.
ACKNOWLEDGMENTS
This work was supported by grant from the Beijing Municipal Natural Science Foundation (No. 7194327).
REFERENCES
- 1.Soubra A, Natale C, Brimley S, Hellstrom WJ. Revelations on men who seek penile augmentation aurgery:a review. Sex Med Rev. 2021 doi: 10.1016/j.sxmr.2021.10.003. Doi:10.1016/j.sxmr.2021.10.003. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
- 2.Lindau ST, Schumm LP, Laumann EO, Levinson W, O’Muircheartaigh CA, et al. A study of sexuality and health among older adults in the United States. N Engl J Med. 2007;357:762–74. doi: 10.1056/NEJMoa067423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marra G, Drury A, Tran L, Veale D, Muir GH, et al. Systematic review of surgical and nonsurgical interventions in normal men complaining of small penis size. Sex Med Rev. 2020;8:158–80. doi: 10.1016/j.sxmr.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 4.Wylie KR, Eardley I. Penile size and the ‘small penis syndrome’. BJU Int. 2007;99:1449–55. doi: 10.1111/j.1464-410X.2007.06806.x. [DOI] [PubMed] [Google Scholar]
- 5.Veale D, Miles S, Read J, Troglia A, Wylie K, et al. Sexual functioning and behavior of men with body dysmorphic disorder concerning penis size compared with men anxious about penis size and with controls:a cohort study. Sex Med. 2015;3:147–55. doi: 10.1002/sm2.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghanem H, Glina S, Assalian P, Buvat J. Position paper:management of men complaining of a small penis despite an actually normal size. J Sex Med. 2013;10:294–303. doi: 10.1111/j.1743-6109.2012.02725.x. [DOI] [PubMed] [Google Scholar]
- 7.Yoram V, Ilan G. The status of penile enhancement procedures. Curr Opin Urol. 2009;19:601–5. doi: 10.1097/MOU.0b013e3283318f31. [DOI] [PubMed] [Google Scholar]
- 8.Oderda M, Gontero P. Non-invasive methods of penile lengthening:fact or fiction? BJU Int. 2011;107:1278–82. doi: 10.1111/j.1464-410X.2010.09647.x. [DOI] [PubMed] [Google Scholar]
- 9.Vardi Y, Harshai Y, Gil T, Gruenwald I. A critical analysis of penile enhancement procedures for patients with normal penile size:surgical techniques, success, and complications. Eur Urol. 2009;54:1042–50. doi: 10.1016/j.eururo.2008.07.080. [DOI] [PubMed] [Google Scholar]
- 10.Born T. Hyaluronic acids. Clin Plast Surg. 2006;33:525–38. doi: 10.1016/j.cps.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 11.Kwak TI, Oh M, Kim JJ, Moon DG. The effects of penile girth enhancement using injectable hyaluronic acid gel, a filler. J Sex Med. 2011;8:3407–13. doi: 10.1111/j.1743-6109.2010.01748.x. [DOI] [PubMed] [Google Scholar]
- 12.Moon DG, Kwak TI, Kim JJ. Glans penis augmentation using hyaluronic acid gel as an injectable filler. World J Mens Health. 2015;33:50–61. doi: 10.5534/wjmh.2015.33.2.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang DY, Jeong HC, Ko K, Lee SH, Lee YG, et al. Comparison of clinical outcomes between hyaluronic and polylactic acid filler injections for penile augmentation in men reporting a small penis:a multicenter, patient-blinded/evaluator-llinded, non-inferiority, randomized comparative trial with 18 months of follow-up. J Clin Med. 2020;9:1024. doi: 10.3390/jcm9041024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goldberg DJ. Breakthroughs in US dermal fillers for facial soft-tissue augmentation. J Cosmet Laser Ther. 2009;11:240–7. doi: 10.3109/14764170903341731. [DOI] [PubMed] [Google Scholar]
- 15.Sito G, Marlino S, Santorelli A. Use of Macrolane VRF 30 in emicircumferential penis enlargement. Aesthet Surg J. 2013;33:258–64. doi: 10.1177/1090820X12472337. [DOI] [PubMed] [Google Scholar]
- 16.Davis SN, Binik YM, Amsel R, Carrier S. The index of male genital image:a new scale to assess male genital satisfaction. J Urol. 2013;190:1335–9. doi: 10.1016/j.juro.2013.03.121. [DOI] [PubMed] [Google Scholar]
- 17.Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, et al. The International Index of Erectile Function (IIEF):a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–30. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 18.Veale D, Eshkevari E, Read J, Miles S, Troglia A, et al. Beliefs about penis size:validation of a scale for men ashamed about their penis size. J Sex Med. 2014;11:84–92. doi: 10.1111/jsm.12294. [DOI] [PubMed] [Google Scholar]
- 19.Chen XB, Li RX, Yang HN, Dai JC. A comprehensive, prospective study of penile dimensions in Chinese men of multiple ethnicities. Int J Impot Res. 2014;26:172–6. doi: 10.1038/ijir.2014.9. [DOI] [PubMed] [Google Scholar]
- 20.Xu L, Zhao M, Chen W, Li Y, Yang Z, et al. Augmentation phalloplasty with autologous dermal fat graft in the treatment of “small penis”. Ann Plast Surg. 2016;77(Suppl 1):S60–5. doi: 10.1097/SAP.0000000000000782. [DOI] [PubMed] [Google Scholar]
- 21.Yang DY, Jeong HC, Ahn ST, Bae WJ, Moon DG, et al. A comparison between hyaluronic acid and polylactic acid filler injections for temporary penile augmentation in patients with small penis syndrome:a multicenter, patient/evaluator-blind, comparative, randomized trial. J Sex Med. 2020;17:133–41. doi: 10.1016/j.jsxm.2019.10.006. [DOI] [PubMed] [Google Scholar]
- 22.Quan Y, Gao ZR, Dai X, Kuang L, Zhang M, et al. Complications and management of penile augmentation with hyaluronic acid injection. Asian J Androl. 2021;23:392–5. doi: 10.4103/aja.aja_78_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nikoobakht M, Shahnazari A, Rezaeidanesh M, Mehrsai A, Pourmand G. Effect of penile-extender device in increasing penile size in men with shortened penis:preliminary results. J Sex Med. 2011;8:3188–92. doi: 10.1111/j.1743-6109.2009.01662.x. [DOI] [PubMed] [Google Scholar]
- 24.Nowroozi MR, Amini E, Ayati M, Jamshidian H, Radkhah K, et al. Applying extender devices in patients with penile dysmorphophobia:assessment of tolerability, efficacy, and impact on erectile function. J Sex Med. 2015;12:1242–7. doi: 10.1111/jsm.12870. [DOI] [PubMed] [Google Scholar]
- 25.Gontero P, Di Marco M, Giubilei G, Bartoletti R, Pappagallo G, et al. A pilot phase-II prospective study to test the ‘efficacy’ and tolerability of a penile-extender device in the treatment of ‘short penis’. BJU Int. 2009;103:793–7. doi: 10.1111/j.1464-410X.2008.08083.x. [DOI] [PubMed] [Google Scholar]
- 26.Aghamir MK, Hosseini R, Alizadeh F. A vacuum device for penile elongation:fact or fiction? BJU Int. 2006;97:777–8. doi: 10.1111/j.1464-410X.2006.05992.x. [DOI] [PubMed] [Google Scholar]
- 27.Kang DH, Chung JH, Kim YJ, Lee HN, Cho SH, et al. Efficacy and safety of penile girth enhancement by autologous fat injection for patients with thin penises. Aesthetic Plast Surg. 2012;36:813–8. doi: 10.1007/s00266-012-9891-4. [DOI] [PubMed] [Google Scholar]
- 28.Shaeer O. Girth augmentation of the penis using flaps “Shaeer’s augmentation phalloplasty” :the superficial circumflex iliac flap. J Sex Med. 2014;11:1856–62. doi: 10.1111/jsm.12537. [DOI] [PubMed] [Google Scholar]
- 29.Xu T, Zhang G, Bai W, Li Q, Yang A, et al. Complications and management of penile girth enhancement with acellular dermal matrix. J Sex Med. 2019;16:2011–7. doi: 10.1016/j.jsxm.2019.09.010. [DOI] [PubMed] [Google Scholar]
- 30.Alei G, Letizia P, Ricottilli F, Simone P, Alei L, et al. Original technique for penile girth augmentation through porcine dermal acellular grafts:results in a 69-patient series. J Sex Med. 2012;9:1945–53. doi: 10.1111/j.1743-6109.2012.02744.x. [DOI] [PubMed] [Google Scholar]
- 31.Jin Z, Wu YG, Yuan YM, Peng J, Gong YQ, et al. Tissue engineering penoplasty with biodegradable scaffold Maxpol-T cografted autologous fibroblasts for small penis syndrome. J Androl. 2011;32:491–5. doi: 10.2164/jandrol.110.011247. [DOI] [PubMed] [Google Scholar]
- 32.Protogerou V, Anagnostopolou S, Venierates D, Troupis T, Plagou M, et al. Penis ligaments:their use in “increasing” the size of the penis in penile augmentation procedures. Anatomical description in human cadavers and clinical results of a phalloplasty series. Ann Ital Chir. 2010;81:199–204. [PubMed] [Google Scholar]
- 33.Zhang GX, Weng M, Wang MD, Bai WJ. Autologous dermal graft combined with a modified degloving procedure for penile augmentation in young adults:a preliminary study. Andrology. 2016;4:927–31. doi: 10.1111/andr.12192. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Postinjection effects of penile augmentation with hyaluronic acid injection.


