A 17-year-old man with recurrent abdominal pain for 8 years was diagnosed with Crohn's disease (CD) with perforation. After surgery, the patient’s abdominal pain persisted despite treatment with azathioprine, adalimumab, and infliximab. Laboratory testing revealed a positive fecal occult blood test, markedly elevated fecal calprotectin (698 µg/g) and slightly elevated plasma C-reactive protein (CRP) level (8.5 mg/L). Colonoscopy showed an anastomotic ulcer and stricture. The patient was treated with an intravenous infusion of cyclophosphamide and oral thalidomide. After 6 months, his abdominal pain had disappeared and the inflammatory markers had returned to normal. Colonoscopy showed the anastomotic ulcer had disappeared but the stricture had worsened. Thalidomide therapy was maintained; however, after another 6 months, the patient again experienced abdominal pain and his inflammatory markers were significantly elevated (CRP 14 mg/L, fecal calprotectin 1376 µg/g). Computed tomographic enterography (CTE) showed the anastomotic stricture and thickened bowel wall without a fistula.
On colonoscopy, the scope could not be passed through the anastomosis and ulcers were visible again ( Fig. 1 ). After injecting contrast agent to delineate the proximal lumen ( Fig. 2 ), we performed endoscopic stricturotomy ( Video 1 ) as the stricture was short and straight and accompanied by ulceration ( Fig. 3 a,b ). We initially cut the mucosa on the opposite side from the ulcer, assumed to be the thicker part of the bowel wall, to avoid perforation. After the incision had been made, the colonoscope could be passed through the stricture into the small bowel, where an active ulcer was found ( Fig. 3 c ).
Fig. 1 .
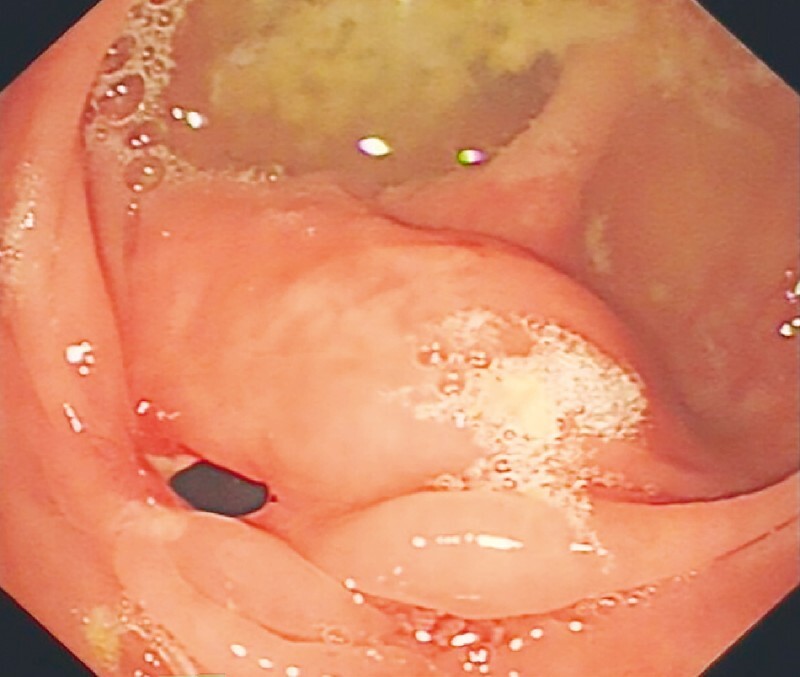
Endoscopic view of the anastomotic stricture with ulceration.
Fig. 2.
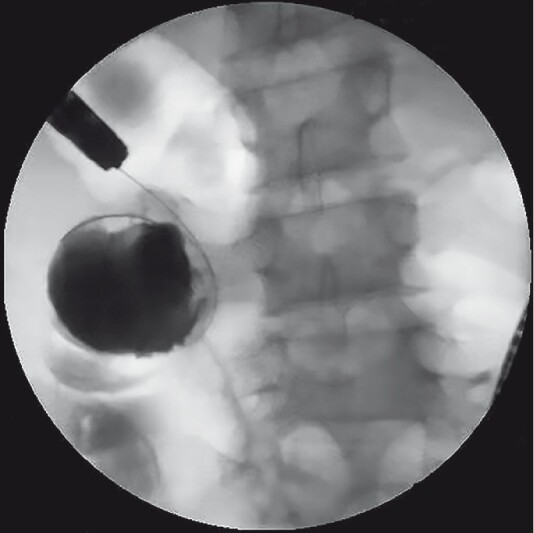
Radiographic image showing the contrast agent entering the intestinal lumen.
Fig. 3.
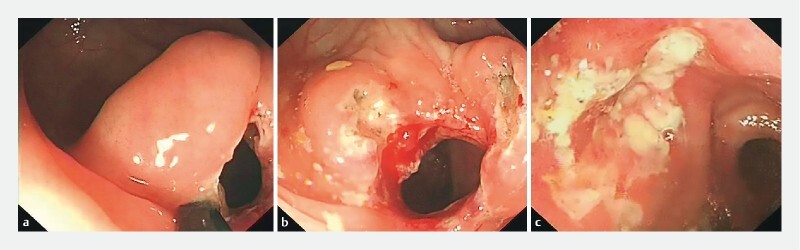
Endoscopic images showing: a incision of the anastomotic stricture; b the appearance of the anastomotic stoma after endoscopic stricturotomy; c ulceration on the oral side of anastomosis.
Video 1 Endoscopic stricturotomy was performed to treat an anastomotic stricture in a patient with Crohn’s disease.
The patient was subsequently treated with hormone therapy combined with methotrexate. Repeat colonoscopy after 6 months showed that the anastomotic stoma was significantly wider so the colonoscope could be passed through, and the ulcer on the oral side was well healed.
In conclusion, anastomotic strictures without fistulas could be effectively treated by endoscopic stricturotomy in CD patients. Where strictures are accompanied by ulcers, stricturotomy may be safer than endoscopic balloon dilation 1 2 3 4 .
Endoscopy_UCTN_Code_TTT_1AQ_2AF
Footnotes
Competing interests The authors declare that they have no conflict of interest.
Endoscopy E-Videos : https://eref.thieme.de/e-videos .
Endoscopy E-Videos is an open access online section, reporting on interesting cases and new techniques in gastroenterological endoscopy. All papers include a high quality video and all contributions are freely accessible online. Processing charges apply (currently EUR 375), discounts and wavers acc. to HINARI are available. This section has its own submission website at https://mc.manuscriptcentral.com/e-videos
References
- 1.Ueno F, Matsui T, Matsumoto T et al. Evidence-based clinical practice guidelines for Crohn's disease, integrated with formal consensus of experts in Japan. J Gastroenterol. 2013;48:31–72. doi: 10.1007/s00535-012-0673-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lan N, Shen B. Endoscopic stricturotomy versus balloon dilation in the treatment of anastomotic strictures in Crohnʼs disease. Inflamm Bowel Dis. 2018;24:897–907. doi: 10.1093/ibd/izx085. [DOI] [PubMed] [Google Scholar]
- 3.Mayberry J F, Lobo A, Ford A C et al. NICE clinical guideline (CG152): the management of Crohnʼs disease in adults, children and young people. Aliment Pharmacol Ther. 2013;37:195–203. doi: 10.1111/apt.12102. [DOI] [PubMed] [Google Scholar]
- 4.Bharadwaj S, Fleshner P, Shen B. Therapeutic armamentarium for stricturing Crohnʼs disease: medical versus endoscopic versus surgical approaches. Inflamm Bowel Dis. 2015;21:2194–2213. doi: 10.1097/MIB.0000000000000403. [DOI] [PubMed] [Google Scholar]


