Abstract
HIV stigma is associated with negative physical and mental health outcomes. Intersectional stigma among persons living with HIV (PLHIV) results from interrelated, synergistic impacts of experiencing multiple stigma forms. Its relation with mental health outcomes is still an emerging area of study in this key population. This study aimed to evaluate associations of intersectional stigma, defined as endorsing high levels of HIV and substance use stigmas, with depressive and anxiety symptoms in a cohort of 111 PLHIV who inject drugs in St. Petersburg, Russia. Over a third of participants (37%) reported experiencing intersectional stigma, i.e., both stigma scores above the median. In adjusted analysis, lower Patient Health Questionnaire depression scale (PHQ-9) scores (beta (β=−4.31, 95% CI: −7.11 – −1.51, p=0.003) and Generalized Anxiety Disorders Scale (GAD-7) scores (β=−3.64, 95% CI: −5.57 – −1.71, p<0.001) were associated with having low scores for both HIV and substance use stigmas. Lower PHQ-9 scores (β=−3.46, 95% CI: −5.72 – −1.19, p=0.003) and GAD-7 scores (β=−3.06, 95% CI: −4.62 – −1.50, p<0.001) were also associated with high stigma on either HIV or substance use stigma scales. Controlling for demographics, depressive symptoms approximately linearly increased from both forms of stigma low to experiencing either form of stigma high to experiencing intersectional stigma, while levels of anxiety symptoms were comparable among participants with both types of stigma low and one stigma high. Participants who experienced intersectional stigma reported the greatest severity of both depressive and anxiety symptoms, as compared to individuals who endorsed low stigma scores (i.e., low stigma on both HIV and substance use stigma scales) or high scores of only one form of stigma. This suggests that intersectional stigma in this population of PLHIV who inject drugs in Russia is linked with worsened mental health outcomes, exceeding the effects of experiencing one form of stigma alone. Interventions to help people cope with intersectional stigma need to consider affective symptoms and tailor coping strategies to address impacts of multiple forms of mental health distress.
Keywords: stigmatization, HIV/AIDS, substance use, mental health, Russian Federation
INTRODUCTION
Comprised of cognitive, emotional, and behavioral aspects, stigma is a social determinant of health associated with worsened health outcomes, worsened quality of life, and limited treatment seeking behaviors [1–4]. Individuals may experience various stigma manifestations, such as internalized (i.e., a person’s endorsement of feelings about their stigmatized condition), experienced (i.e., experiences of being stigmatized and discriminated against by others), or anticipated (i.e., expectations of stigma experiences) stigma [4–6].
HIV is a commonly stigmatized condition, and HIV stigma is recognized as a barrier to prevention and care engagement [7]. HIV stigma is associated with diminished social support [8], poor antiretroviral treatment (ART) adherence [3,8], and worsened mental health outcomes, including depression and anxiety [3,7,9]. HIV stigma independently contributes to psychological distress over and above impacts from poor health status and HIV somatic symptoms [10,11]. Past research demonstrates that experiencing HIV stigma is prospectively associated with symptoms of depression, panic, and generalized anxiety [12].
Multiple stigmatized conditions and behaviors frequently co-occur among persons living with HIV (PLHIV). Of note, rates of substance use are high among PLHIV [13]. Substance use disorders are heavily stigmatized, even more than other marginalized health conditions [14–16]. Experiencing substance use stigma results in poor physical and mental health [15] and has been implicated as a cause of missed HIV appointments [17]. Among PLHIV who use substances, HIV- and substance-use stigma commonly occur [18].
The term “intersectionality” was introduced by Dr. Kimberlé Crenshaw in 1989 [19]. Established in Black feminism and Critical Race Theory, intersectionality was introduced to address the marginalization of Black women in feminist and antiracist theory, politics, and law [19]. This construct is used today to provide a lens through which to view interacting aspects of identity and experience. Regarding stigma, intersectional stigma results from the interrelated, and often synergistic, effects of experiencing different types of stigmas [6,20]. Effects of intersectional stigma vary depending on context [21] and can result in heightened vulnerability for negative health outcomes [6]. Globally, stigma is a crucial element to address when promoting health in any context, in particular HIV-related outcomes, and it is vital to consider how intersectionality plays a large role in affecting health outcomes [22–26].
As culture and context impact stigma outcomes [21, 27], stigma effects may differ in varying settings. In the Russian Federation (Russia), an estimated one million people are living with HIV [28]. In contrast to other countries in the European region, cases of HIV in Russia are continuing to rise [28]. Injection drug use is implicated as a major driver of the ongoing epidemic in Russia [29], and over 25% of people who inject drugs are HIV-positive [28,30]. Numerous reports detail the high rates of HIV- and substance use-stigma that are especially prevalent in Russia [31–34]. In Russia, studies have highlighted extensive HIV and substance use stigma directed towards people with HIV and those who inject drugs [35]. Russia currently criminalizes substance use and limits addiction treatment service options [36–38]. In order to access drug treatment in Russia, individuals must formally register as a person who uses drugs, which then necessitates additional monitoring over the following five years with corresponding restrictions on employment, vehicle licensure, and military service. Many individuals are marked as social outcasts and if confidentiality is breached, are vulnerable to police harassment [39]. Examples of harassment includes unjust arrests, planting false evidence, and extrajudicial syringe confiscations [37]. Experiencing these stigma forms in Russia predicts poorer physical and mental health outcomes [35]. Past work has evaluated intersectional stigma in Russia using separate measures for each form of stigma and found that those who experience high levels of both HIV and substance use stigma have poorer health outcomes and lower access to care, as compared with lower stigma levels or single stigma experiences [35,41].
While negative mental health outcomes stemming from HIV stigma, particularly depression, are relatively well-established, there is less work evaluating the links of intersectional stigma (particularly HIV- and substance use stigma) and mental health outcomes. This is especially true among populations of PLHIV who inject drugs. Little is known about associations between intersectional stigma and anxiety symptoms in these populations. Studies on the relationship between intersectional HIV and substance use stigma with mental health outcomes have not yet been published either in Russia or among the HIV key population of PLHIV who inject drugs.
This study’s aim was to evaluate the relations of HIV, substance use, and a derived intersectional stigma variable with depressive and anxiety symptoms in a sample of PLHIV who inject drugs in St. Petersburg, Russia. We hypothesized that high levels of intersectional stigma (i.e., reporting both high HIV and substance use stigma) will be associated with greater severity of depressive and anxiety symptoms than those experiencing low levels of stigma.
METHODS
Study Design and Setting
This study used baseline, pre-randomization data from the SCRIPT randomized controlled trial evaluating a behavioral stigma coping intervention among PLHIV who inject drugs [40]. The SCRIPT trial tested the feasibility and effectiveness of a behavioral stigma coping intervention, which consisted of three weekly group sessions among 100 participants (plus 11 pilot participants). Assessments occurred at baseline, 1-month post-randomization, and 6-months post-randomization. Results from this trial will be reported elsewhere. The present cross-sectional analysis used baseline data, prior to randomization for all participants from the SCRIPT study. Participants in the parent study were recruited from Humanitarian Action in St. Petersburg, Russia, a civil society organization that provides harm reduction and HIV prevention services in mobile units (i.e., outreach buses) for no user fee and offers medical, social, and psychological resources for individuals who use substances.
Participants
Eligibility criteria for study participants included the following: age 18 or older; HIV-positive; current injection drug use (past 30 days); not currently on ART; address within 100 kilometers of St. Petersburg; and possession of a home or mobile phone. Exclusion criteria included lack of fluency in Russian; cognitive impairment resulting in inability to provide informed consent (assessor-determined); or acute severe psychiatric illness (Appendix 1). Participants could be newly diagnosed with HIV, or they could have had a longstanding diagnosis of HIV.
Procedures
Baseline data were collected between October 2019 and September 2020. 81% of participants who were eligible from phone screening reported for in-person screening. A research assessor screened patients, obtained written informed consent, and administered the baseline survey at the recruitment site. Data collected included demographic, behavioral (e.g., substance use, alcohol use) and clinical (e.g., ART adherence, mental health variables) characteristics of participants. Local team members fluent in English and Russian translated the instruments. Participants received an equivalent to approximately 30 USD in Russian rubles as compensation for their time and transportation expenses.
Outcomes
Outcomes included depressive and anxiety symptoms at baseline. Depressive symptoms were measured using the Patient Health Questionnaire depression scale (nine item version; PHQ-9) [42,43]. The PHQ-9 is among the most frequently used screeners for depression globally [44] and shows excellent psychometric properties [45,46]. Items are scored on a “0” (not at all) to “3” (nearly every day) scale; scores of 5, 10, 15, and 20 represented mild, moderate, moderately severe, and severe depression, respectively [46]. Anxiety symptoms were measured using the 7-item Generalized Anxiety Disorders Scale (GAD-7) [47], which has demonstrated strong reliability and validity in varied settings [48]. The items assessed symptoms such as feeling nervous, excessive worry, difficult relaxing, and feeling restless. Response options ranged from “not at all” to “nearly every day” on a 0–3 scale, with cut points of 5, 10, and 15 commonly interpreted as representing mild, moderate, and severe levels of anxiety [47].
Exposure
Please see Appendix 2 for a description of the instruments used. HIV stigma was evaluated using the 10-item abbreviated Berger HIV Stigma Scale [49,50], which was rated on a four-point Likert-type response ranging from 1 (strongly disagree) to 4 (strongly agree). The measure consists of the following subscales: (1) personalized HIV stigma (e.g. enacted stigma): 3 items (e.g., “I have been hurt by how people reacted to learning I have HIV”); (2) disclosure concerns (e.g. anticipated stigma): 2 items (“I am very careful who I tell that I have HIV”); (3) negative self-image (e.g. internalized stigma): 3 items (“I feel that I am not as good a person as others because I have HIV”); and 4) concerns with public attitudes toward HIV-positive people (e.g. perceived stigma): 2 items (“Most people think that a person with HIV is disgusting”). We calculated continuous total HIV stigma scores as the sum of each participant’s responses to all questions.
Substance use stigma was assessed via the abbreviated 16-item Substance Abuse Self-Stigma Scale (SASSS) [51], which was scored using a 5-point Likert scale [44]. The SASSS included the following subscales: (1) internalized stigma, self-devaluation (e.g., “I have the thought that a major reason for my problems with substances is my own poor character”); (2) fear of enacted stigma (e.g., “People think I’m worthless if they know about my substance use history”); (3) stigma avoidance (e.g., “I would choose to avoid someone who seemed interested in my friendship if I knew they had never used substances”); and (4) values disengagement (e.g., “I do things that are good for me, even if I feel like I don’t deserve it”). Higher scores indicated higher stigma and stigma-related manifestations.
We defined intersectional stigma, analogous to prior studies [52,53], as a 3-category variable: 1) low stigma (both HIV and substance use stigma scores below the median), 2) one form of stigma high (either HIV or substance use stigma scores equal to or above the median), and 3) high intersectional stigma (both HIV and substance use stigma scores equal to or above the median).
Covariates
The set of covariates included the following demographic variables: age in years; self-reported sex; relationship status (married/partnered vs. living alone); employment status (full or part-time employment vs. unemployed, home-makers, students); education (secondary education/college vs. nine grades or less); and monthly individual income (measured as a categorical variable with eight intervals) dichotomized at 15,000 RUB (aimed to have balanced groups; approximately 200 USD).
Data Analysis
We described participant characteristics with frequencies and proportions for categorical variables and 5-number summaries for numeric variables (mean, standard deviation (SD), median, interquartile range, range). Distributions of outcomes were visualized with histograms and qq-plots and were approximately normal. We did not use statistical tests to assess normality of distributions considering that all tests are conservative. We used linear regressions to assess associations between intersectional stigma and mental health outcomes. Both unadjusted and adjusted estimates were calculated. The set of covariates was pre-defined based on the literature [41,52]. We tested model assumptions (i.e., whether the residuals met the criteria), and there were no clear violations. To visualize the association of interest, we plotted predicted values of outcomes by the intersectional stigma using boxplots. There was no missing data. We conducted all analyses in R, version 4.0.5 (Copyright (C) 2021 The R Foundation for Statistical Computing).
Ethics Approval
The study protocol and instruments received ethical approval from the Institutional Review Boards at Boston University Medical Campus and Pavlov University. All study participants provided written informed consent.
RESULTS
Characteristics of the Study Participants
We included all 111 PLHIV who participated in the SCRIPT trial in this analysis (Table 1). All data reported in this work are from the baseline timepoint, prior to randomization. The sample was 53% male with a mean age of 38 years (SD: 5 years). The majority of the sample reported being married or partnered (71%), having a secondary or college education (69%), and did not have full or part-time employment (58%). The mean age of first injection was 18.6 years (SD 3.8). The mean number of years since first positive HIV test was 10 years (SD: 6 years) (n=100).
Table 1.
Characteristic of persons living with HIV and who inject drugs from a cross-sectional study in St. Petersburg, Russia.
| Characteristic | N = 111 |
|---|---|
| Sex | |
| Male | 59 (53%) |
| Female | 52 (47%) |
| Age | |
| Mean (SD) | 38.2 (5.2) |
| Median (IQR) | 38.0 (36.0, 41.0) |
| Range | 19.0, 55.0 |
| Relationship status | |
| Married/Partnered | 79 (71%) |
| Living alone | 32 (29%) |
| Level of education | |
| Nine grades or less | 31 (28%) |
| Secondary Education/College | 77 (69%) |
| Higher Education | 3 (2.7%) |
| Employment pattern | |
| Employed (full time or part time) | 47 (42%) |
| Unemployed / Full-time home maker / Full-time student | 64 (58%) |
| Monthly income | |
| ≤15.000 RUB (approx. $200 USD) | 50 (45%) |
| >15.000 RUB | 61 (55%) |
| Berger HIV stigma | |
| Mean (SD) | 22.2 (3.7) |
| Median (IQR) | 22.0 (20.0, 25.0) |
| Range | 13.0, 31.0 |
| Substance use (SU) stigma | |
| Mean (SD) | 31.5 (7.2) |
| Median (IQR) | 32.0 (26.5, 36.0) |
| Range | 12.0, 46.0 |
| Intersectional HIV and substance use stigma | |
| Low (HIV & SU stigma less than median levels) | 24 (22%) |
| One form of stigma high (one form of stigma is low, another form of stigma is high) | 46 (41%) |
| Intersectional (HIV & SU stigma equal to or greater than median levels) | 41 (37%) |
| PHQ-9 scores | |
| Mean (SD) | 8.4 (5.6) |
| Median (IQR) | 8.0 (4.0, 13.0) |
| Range | 0.0, 21.0 |
| GAD-7 scores | |
| Mean (SD) | 5.3 (4.0) |
| Median (IQR) | 4.0 (2.0, 8.0) |
| Range | 0.0, 17.0 |
Depressive and Anxiety Symptoms
Mean score on the PHQ-9 was 8.4 (SD: 5.6), which corresponds to mild or moderate depressive symptoms based upon clinical cutoffs. Mean score on the GAD-7 was 5.3 (SD: 4.0), which corresponds to mild anxiety symptoms based upon clinical cutoffs [42,43,47].
In adjusted linear regressions, lower PHQ-9 scores (beta (β)=−2.44, 95% confidence interval (CI): −4.63 – −0.25, p=0.029) and GAD-7 scores (β=−2.19, 95% CI: −3.70 – −0.68, p=0.005) were associated with having a full or part-time employment. Higher GAD-7 scores were associated with having received secondary or college education (β=1.99, 95% CI: 0.39 – 3.59, p=0.015) (Table 2).
Table 2.
Unadjusted and adjusted linear associations from linear regression models between intersectional stigma and mental health among persons living with HIV and who inject drugs in St. Petersburg, Russia (n=111).
| PHQ-9 Score | GAD-7 Score | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| Unadjusted | Adjusted | Unadjusted | Adjusted | |||||||||
| Predictors | Beta | 95% CI | p | Beta | 95% CI | p | Beta | 95% CI | p | Beta | 95% CI | p |
| (Intercept) | 10.9 | 9.27 – 12.54 | <0.001 | 7.33 | −1.57 – 16.24 | 0.106 | 7.29 | 6.13 – 8.46 | <0.001 | 8.59 | 2.45 – 14.73 | 0.007 |
| Intersectional stigma: low (ref.: high) | −5.03 | −7.72 – −2.34 | <0.001 | −4.31 | −7.11 – −1.51 | 0.003 | −3.79 | −5.71 – −1.87 | <0.001 | −3.64 | −5.57 – −1.71 | <0.001 |
| Intersectional stigma: one form of stigma high (ref.: high) | −3.4 | −5.65 – −1.15 | 0.003 | −3.46 | −5.72 – −1.19 | 0.003 | −2.77 | −4.38 – −1.17 | 0.001 | −3.06 | −4.62 – −1.50 | <0.001 |
| Sex: female (ref.: male) | 1.78 | −0.55 – 4.10 | 0.133 | 0.35 | −1.26 – 1.95 | 0.669 | ||||||
| Age, years | 0.07 | −0.13 – 0.27 | 0.485 | −0.05 | −0.19 – 0.09 | 0.462 | ||||||
| Relationship: married/partnered (ref.: living alone) | −0.41 | −2.72 – 1.90 | 0.724 | −0.01 | −1.60 – 1.58 | 0.991 | ||||||
| Employment: employed (ref.: unemployed / home maker / student) | −2.44 | −4.63 – −0.25 | 0.029 | −2.19 | −3.70 – −0.68 | 0.005 | ||||||
| Monthly income: >15.000 RUB or ~200 USD (ref.: ≤15.000 RUB) | 0.21 | −2.00 – 2.42 | 0.851 | 0.16 | −1.37 – 1.68 | 0.837 | ||||||
| Education: secondary education/college (ref.: nine grades or less) | 1.53 | −0.79 – 3.85 | 0.194 | 1.99 | 0.39 – 3.59 | 0.015 | ||||||
| Observations | 111 | 111 | 111 | 111 | ||||||||
| R2 / R2 adjusted | 0.129 / 0.113 | 0.197 / 0.134 | 0.149 / 0.133 | 0.268 / 0.210 | ||||||||
HIV, Substance Use, and Intersectional Stigma
Mean score on the abbreviated HIV Berger scale was 22.2 (SD: 3.7). Mean score on the abbreviated SASSS scale was 31.5 (SD: 7.2). Regarding intersectional stigma, 22% (n=24) of participants had low levels of both HIV and substance use stigma, 41% (n=46) had high levels of stigma related to either HIV or substance use, and 37% (n=41) had intersectional stigma (i.e., high levels of both HIV- and substance use-related stigma). All stigma scales were dichotomized for analysis.
Mental Health and Intersectional Stigma
In adjusted analysis, lower PHQ-9 scores (β=−4.31, 95% CI: −7.11 – −1.51, p=0.003) and GAD-7 scores (β=−3.64, 95% CI: −5.57 – −1.71, p<0.001) were associated with low stigma. Lower PHQ-9 scores (β=−3.46, 95% CI: −5.72 – −1.19, p=0.003) and GAD-7 scores (β=−3.06, 95% CI: −4.62 – −1.50, p<0.001) were also associated with one form of stigma high (Table 2). In other words, participants with low levels of both stigmas had lower average scores for depressive and anxiety symptoms compared with those who endorsed high levels of both stigmas. Similarly, people with only one form of stigma high had lower mean scores on the PHQ-9 and the GAD-7 relative to people with both stigmas high. Controlling for demographics, PHQ-9 scores approximately linearly increased across the categories of intersectional stigma: depressive symptoms were lower among those with low levels of both HIV and substance use stigma, moderate among those with high levels of stigma related to either HIV or substance use, and highest among those experiencing intersectional stigma (i.e., high levels of both HIV- and substance use-related stigma). Levels of anxiety did not differ between those with both forms of stigma low and either form of stigma high, with GAD-7 scores comparable among participants with both types of stigma low and one stigma high (Figure 1).
Figure 1.
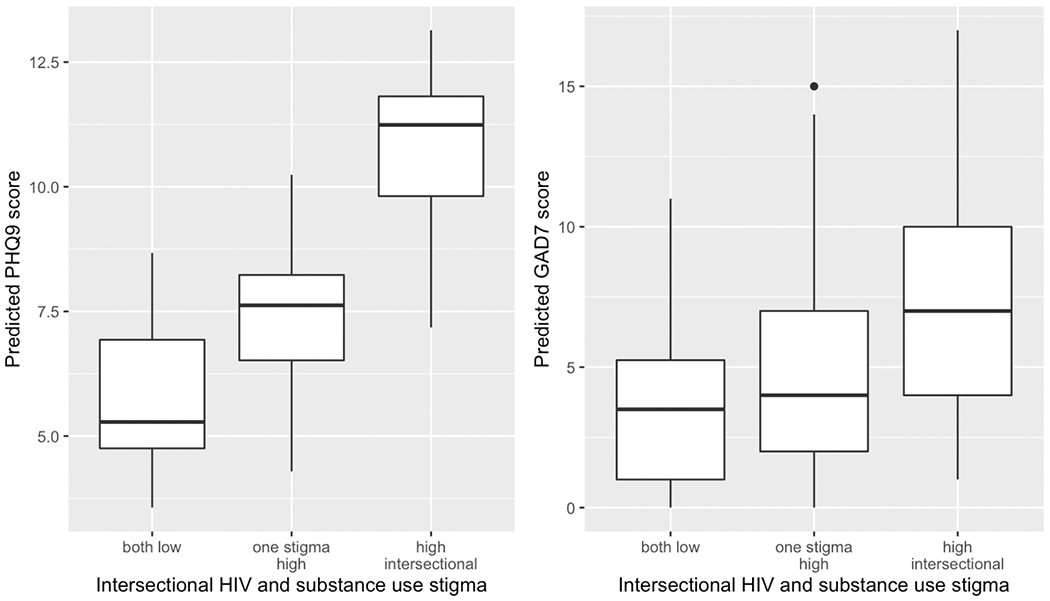
PHQ-9 and GAD-7 scores by intersectional HIV and substance use stigma adjusted by demographics (age, sex, relationship status, employment, education, income) among persons living with HIV and who inject drugs in St. Petersburg, Russia (n=111).
DISCUSSION
In this study, we found that over a third of participants (37%) reported experiencing intersectional stigma, defined as high HIV and substance use stigmas. An additional 41% of this sample reported experiencing a high form of either HIV or substance use stigma. When constructing the derived intersectional stigma variable, we evaluated differences between high HIV/low substance use stigma and low HIV/high substance use stigma. We found similar outcomes between these permutations. As past work suggested that both HIV and substance-use stigma have damaging effects to mental health among PLHIV [54], we posit that intersectional stigma manifested in excess of single forms of stigma on people’s mental health in this population.
Participants who experienced intersectional stigma reported the greatest severity of both depressive and anxiety symptoms, as compared to individuals who endorsed low stigma experiences or only one form of high stigma experiences. This suggests that intersectional stigma is associated with negative mental health outcomes, over and above the effects of experiencing one form of stigma high but not the other, which is consistent with conceptualizations of the synergistic effects of intersectional stigma [6]. Effects of intersectional stigma on depressive outcomes in this study are aligned with past work, which has suggested that symptoms are more profound among individuals who internalized both HIV and substance use stigma [55] and among individuals who internalized both HIV and chronic pain stigma [53].
While depressive disorders are common among the key population of PLHIV who inject drugs [56], anxiety, and effects of anxiety on HIV outcomes, are not well-articulated in the current literature and represent an important next step in improving knowledge of possible pathways to improve treatment engagement and quality of life among PLHIV [7,8,57]. Compared to depressive outcomes, effects of intersectional stigma on anxiety symptoms are less explored in the current literature. While overall mean scores of depressive symptoms were higher than anxiety symptoms, participants on average endorsed mild anxiety symptoms, which increased to moderate symptoms among those endorsing intersectional stigma. Stigma effects may operate differently on depressive and anxiety symptoms: depressive symptoms increased in nearly a stepwise fashion as stigma experiences increased, suggesting escalating effects. Anxiety symptoms were linked to more drastic increases in intersectional stigma. While the GAD-7 was originally developed to screen specifically for generalized anxiety disorder, it has also been found to perform well for other anxiety disorders (e.g., social anxiety disorder) [58]. One possibility is that the GAD-7 is sensitive to social devaluing experiences of stigma that may be most pronounced among those experiencing intersectional stigma. Social devaluation is particularly detrimental among people with HIV who inject drugs in Russia, as the country’s cultural and structural institutions have identified HIV and injection drug use as undesirable characteristics [35].
As depressive and anxiety disorders are highly comorbid [59], evaluating both mental health outcomes among PLHIV is critical in order to improve HIV health outcomes (and overall health outcomes). A body of literature strongly links mental health distress experienced by PLHIV, particularly depressive symptoms, to worsened quality of life, impaired medication adherence, and disease progression [60–62]. Physical health, mental health, and stigma likely interact in multidirectional pathways; for example, poor physical health is linked with worsened mental health [63]; results from this work and others support the interaction between stigma and mental health. In addition, poor mental health is associated with difficulty with HIV care engagement [64,65] and HIV prevention behaviors [66]. Building upon the current understanding of how intersectional stigma impacts a variety of mental health outcomes, including depressive and anxiety symptoms, will be critical to tailor interventions that fully address mental health needs, which in turn may impact HIV care engagement and retention [67–70]. This study evaluated aggregate effects of HIV and substance use stigma experiences (including enacted, anticipated, internalized, and perceived HIV stigma, as well as internalized and enacted substance use stigma). Exploring sub-scales of stigma (e.g., internalized, experienced anticipated) and associated depressive and anxiety outcomes is an important next step to better parse understanding of the role that various combinations of stigma (thus intersectional stigma) play in affecting mental health. Existing work highlights linkages between depressive symptoms with experienced and internalized HIV stigma [7,71]. Anxiety symptoms may possibly be most affected by anticipated, perceived, and internalized stigma [7]. However, further work to identify which stigma experiences most directly impact specific forms of mental health symptoms, in which contexts, and in which combinations, is needed.
Finally, this study explored the specific effects of intersectional HIV and substance use stigma on mental health symptom severity among PLHIV in Russia, which is a key geographical region as it is one of the few globally with still increasing HIV incidence rates [28]. Punitive drug policing practices in Russia have been shown to be associated with increased HIV risk behaviors among people who use drugs [37]. In addition, Russian PLHIV who use drugs experience high levels of stigma, in part due to the country’s social devaluation of people who have HIV and use substances [35]. Russia’s unique cultural, social, and political determinants of stigma and their effects on mental health cannot be ignored. Ongoing work to evaluate both stigma and mental health effects in varied cultural settings is particularly important, as both stigma and mental health are directly impacted, modified, and specified by context [21,27,72]. Similarly, as in other regions, our findings suggest that intersectional stigma is significantly and negatively linked with the mental health of PLHIV in Russia [66]. Unfortunately, a large treatment gap for mental health interventions for PLHIV, particularly in low- and middle-income countries (which includes Russia [73]), exists [74–76]. Notably, a recent systematic review of clinical trials of interventions aiming to improve the mental health of PLHIV did not find a single study in Russia, Eastern Europe, or Central Asia [75], which highlights the need for strengthened investment in HIV and mental health interventions in the region.
Limitations
There are several limitations that bear consideration. This study was cross-sectional, which limits our ability to determine if internalized stigma predicts subsequent depressive and anxiety symptoms, and longitudinal studies would be useful in evaluating these distinctions. Furthermore, our sample size was small and limited to PLHIV with a history of substance use utilizing civil society organization services in St. Petersburg. Experiences of stigma may be different in formal healthcare settings, which include government-funded hospitals. As indicated earlier, utilizing services from these government-funded hospitals requires government registration of one’s substance use status and HIV status. Future efforts should aim at higher sample sizes, as we were not able to adjust for all potential confounders in our models, and should examine whether these outcomes hold in larger samples in different settings.
Additionally, the measures used in this study were developed in the United States (including the PHQ-9, GAD-7, the Berger HIV Stigma Scale, and the Substance Abuse Self-Stigma Scale), and there may be cultural distinctions in stigma or mental health that are not fully captured on the scales. We recognize the need for continued validation of these measures and believe that ongoing measure validation is an important next step in understanding and evaluating intersectional stigma.
Furthermore, this analysis does not take into account stigma from race, gender, or sexual orientation. We do not ask participants to disclose their sexual orientation for their personal safety, and the majority of participants identified as white in this sample. Future research would benefit from considering other forms of stigma. In our analyses, we also did not include length of HIV diagnosis or substance us history in our model. While stigma is a stable construct over time, negative mental health effects may be exacerbated by factors such as a newly onset HIV diagnosis or present substance use. Similarly, age, and stigmatizing experiences that occur over the life course may also affect acknowledgement of stigma. Future work that evaluates stigma effects in congruence with these constructs would expand on this present work.
Finally, consensus around defining and measuring intersectional stigma is still evolving. While our method of deriving the intersectional stigma variable from two separate stigma scales is aligned with past efforts, it is possible that some participants in this sample may have been mischaracterized. Future efforts to evaluate intersectional stigma using geometrical approaches is indicated [71].
Future Directions
PLHIV who use substances are prone to experience social loneliness, hopelessness, guilt, and shame, which arises from stigma and social isolation; this in turn is associated with mental health indicators including symptoms of depression and anxiety [77,78]. Accordingly, in a study conducted in Russia among PLHIV, social loneliness was associated with depressive and anxiety symptoms [79]. Social loneliness was also associated with lack of acceptance of HIV diagnosis and, therefore, negatively impacted care-seeking behavior [79]. However, studies that targeted reduction in shame, guilt, and negative thoughts and emotions, particularly through interventions such as Acceptance and Commitment Therapy [80,81] and other strengths-based interventions [82], have shown promising results. Utilizing group therapy sessions, through which individuals may feel socially connected with people with similar health conditions, might help to decrease the feeling of social alienation and hopelessness, in turn assisting social adaptation and enhancing care-seeking behavior.
Conclusions
In Russia, PLHIV who inject drugs report common experiences of HIV and substance use stigma. Those who experience intersectional stigma (i.e., high levels of both forms of stigma) endorsed worsened depressive and anxiety symptoms. Interventions to help people cope with intersectional stigma need to consider different types of mental health outcomes, particularly depressive and anxiety symptoms, that may be impacted by stigma. Treatments that address stigma and mental health effects of stigma may also be important in improving treatment engagement and adherence.
Funding:
This study was supported by NIDA R00DA041245 and 5P30AI042853-22. KH is supported by NIMH T32MH116140. The sponsors had no role in study design; in the collection, analysis and interpretation of data; in the writing of the article; and in the decision to submit it for publication.
Appendix 1.
Psychiatric Illness Exclusion Criteria
1. Have you experienced any of the following in the past 3 months:
| a. Have you heard things that other people couldn’t hear, like noises or voices of people talking when there was no one around? | 0□ NO | 1□ Yes | □ Refused |
| b. Have you seen things that other people couldn’t see? | 0□ NO | 1□ Yes | □ Refused |
| c. Have you experienced mental health symptoms prompting a visit to the ED or hospital? | 0□ NO | 1□ Yes | □ Refused |
| d. Have you had mental health medication changes due to worsening symptoms? | 0□ NO | 1□ Yes | □ Refused |
| e. Have you been diagnosed with a severe personality disorder? | 0□ NO | 1□ Yes | □ Refused |
| f. Have you made plans about taking your life? | 0□ NO | 1□ Yes | □ Refused |
Presence of any one of these items warranted exclusion from the parent study.
Appendix 2. Study instruments.
ADAPTED BERGER HIV STIGMA SCALE
These next questions ask about some experiences and feelings you may have had because of HIV.
| Strongly Disagree | Disagree | Agree | Strongly Agree | Refused | |
|---|---|---|---|---|---|
| 1. I have been hurt by how people reacted to learning I have HIV. | 1 | 2 | 3 | 4 | 8 |
| 2. I have stopped socializing with some people because of their reaction of my having HIV. | 1 | 2 | 3 | 4 | 8 |
| 3. I have lost friends by telling them I have HIV. | 1 | 2 | 3 | 4 | 8 |
| 4. I am very careful who I tell that I have HIV. | 1 | 2 | 3 | 4 | 8 |
| 5. I worry that people who know I have HIV will tell others. | 1 | 2 | 3 | 4 | 8 |
| 6. I feel that I am not as good a person as others because I have HIV. | 1 | 2 | 3 | 4 | 8 |
| 7. Having HIV makes me feel unclean. | 1 | 2 | 3 | 4 | 8 |
| 8. Having HIV makes me feel that I’m a bad person. | 1 | 2 | 3 | 4 | 8 |
| 9. Most people think that a person with HIV is disgusting. | 1 | 2 | 3 | 4 | 8 |
| 10. Most people with HIV are rejected when others find out. | 1 | 2 | 3 | 4 | 8 |
ADAPTED SUBSTANCE ABUSE SELF-STIGMA SCALE
For this questionnaire, we use the term “substance problem” or “problem with substances” to refer to any problems that you have experienced as a result of your use of drugs or alcohol.
Here is a list of statements describing thoughts or feelings that you may have from time to time or may be familiar to you. Most of these statements describe thoughts and feelings that are generally painful or negative in some way. Try to be as honest as you can in responding.
As you see it now, please rate how often you have the thoughts or experiences listed here.
| Never or almost never | Rarely | Sometimes | Often | Very often | Refused | ||
|---|---|---|---|---|---|---|---|
| 1 | I have the thought that a major reason for my problems with substances is my own poor character. | 1 | 2 | 3 | 4 | 5 | 8 |
| 2 | I have the thought that I should be ashamed of myself. | 1 | 2 | 3 | 4 | 5 | 8 |
| 3 | I feel inferior to people who have never had a problem with substances. | 1 | 2 | 3 | 4 | 5 | 8 |
| 4 | I feel out of place in the world because of my problems with substances. | 1 | 2 | 3 | 4 | 5 | 8 |
Please choose the number that indicates how many people you think would react to you as described for each statement. Please do not omit any item.
| Few People (0-20 percent) | Some people (20-40 percent) | Many people (40-60 percent) | Most People (60-80 percent) | Almost Everyone (80-100 percent) | Refused | ||
|---|---|---|---|---|---|---|---|
| 5 | People think I’m worthless if they know about my substance use history. | 1 | 2 | 3 | 4 | 5 | 8 |
| 6 | People would be scared of me if they knew about my substance abuse history. | 1 | 2 | 3 | 4 | 5 | 8 |
| 7 | If someone were to find out about my history of substance use, they would doubt my character. | 1 | 2 | 3 | 4 | 5 | 8 |
| 8 | People think the bad things that have happened to me are my fault. | 1 | 2 | 3 | 4 | 5 | 8 |
| Never or almost never true | Rarely True | Sometimes true | Often true | Always or almost always true | Refused | ||
| 9 | I would choose to avoid someone who seemed interested in my friendship if I knew they had never used substances. | 1 | 2 | 3 | 4 | 5 | 8 |
| 10 | I avoid doing things where I would be blamed if it didn’t work out. | 1 | 2 | 3 | 4 | 5 | 8 |
| 11 | Shame gets in the way of how I want to live my life. | 1 | 2 | 3 | 4 | 5 | 8 |
| 12 | I avoid situations that make me feel different. | 1 | 2 | 3 | 4 | 5 | 8 |
| 13 | I do things that are good for me, even if I feel like I don’t deserve it. | 1 | 2 | 3 | 4 | 5 | 8 |
| 14 | I pursue important goals in life, even when I fear I might not follow through. | 1 | 2 | 3 | 4 | 5 | 8 |
| 15 | Even if I knew the employer didn’t like to hire people in recovery, I would still apply for a job if it interested me. | 1 | 2 | 3 | 4 | 5 | 8 |
| 16 | I can set a direction for my life even if I feel hopeless. | 1 | 2 | 3 | 4 | 5 | 8 |
Here you will find a list of statements. As you see it now, please rate how true each statement is for you.
Footnotes
Competing interests: The authors declare that they have no competing interests.
Ethics approval: The study protocol and instruments received ethical approval from the Institutional Review Boards at Boston University Medical Campus, Boston, MA, USA and Pavlov University in St. Petersburg, Russia.
Consent to participate: Informed consent to participate was obtained from participants.
Consent for publication: Not applicable.
Availability of data and material: Available upon reasonable request.
Code availability: Not applicable.
REFERENCES
- 1.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103:813–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weiss MG. Stigma and the social burden of neglected tropical diseases. PLoS Negl Trop Dis. 2008;2:e237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kane J, Elafros M, Murray S, Mitchell E, Augustinavicius J, Causevic S et al. A scoping review of health-related stigma outcomes for high-burden diseases in low- and middle-income countries. BMC Medicine. 2019;17(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patten S, Williams J, Lavorato D, Bulloch A, Charbonneau M, Gautam M et al. Perceived stigma among recipients of mental health care in the general Canadian population. Can J Psychiatry. 2016;61(8):480–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mickelson K, Williams S. Perceived stigma of poverty and depression: Examination of interpersonal and intrapersonal mediators. J Soc Clin Psychol. 2008;27(9):903–930. [Google Scholar]
- 6.Turan J, Elafros M, Logie C, Banik S, Turan B, Crockett K et al. Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Medicine. 2019;17(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turan B, Hatcher A, Weiser S, Johnson M, Rice W, Turan J. Framing Mechanisms Linking HIV-Related Stigma, Adherence to Treatment, and Health Outcomes. Am. J. Public Health. 2017;107(6):863–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rueda S, Mitra S, Chen S, Gogolishvili D, Globerman J, Chambers L, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: A series of meta-analyses. BMJ Open. 2016;6: e011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lowther K, Selman L, Harding R, Higginson I. Experience of persistent psychological symptoms and perceived stigma among people with HIV on antiretroviral therapy (ART): A systematic review. Int J Nurs Stud. 2014;51(8):1171–1189. [DOI] [PubMed] [Google Scholar]
- 10.Cramer R, Colbourn S, Gemberling T, Graham J, Stroud C. Substance-related coping, HIV-related factors, and mental health among an HIV-positive sexual minority community sample. AIDS Care. 2015;27(9):1063–1068. [DOI] [PubMed] [Google Scholar]
- 11.Stutterheim S, Pryor J, Bos A, Hoogendijk R, Muris P, Schaalma H. HIV-related stigma and psychological distress: the harmful effects of specific stigma manifestations in various social settings. AIDS. 2009;23(17):2353–2357. [DOI] [PubMed] [Google Scholar]
- 12.Hatzenbuehler M, O’Cleirigh C, Mayer K, Mimiaga M, Safren S. Prospective associations between HIV-related stigma, transmission risk behaviors, and adverse mental health outcomes in men who have sex with men. Ann Behav Med. 2011;42(2):227–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Substance Abuse and Mental Health Services Administration. The National Survey on Drug Use and Health Report: HIV/AIDS and Substance Use. Rockville, MD; 2010. Available at: https://www.samhsa.gov/sites/default/files/hiv-aids-and-substance-use.pdf [Google Scholar]
- 14.Stringer KL, Marotta P, Baker E, Turan B, Kempf MC, Drentea P, Stepanikova I, Turan JM. Substance use stigma and antiretroviral therapy adherence among a drug-using population living with HIV. AIDS Patient Care STDS. 2019. Jun;33(6):282–293. doi: 10.1089/apc.2018.0311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahern J, Stuber J, Galea S. Stigma, discrimination and the health of illicit drug users. Drug Alcohol Depend. 2007. May 11;88(2–3):188–96. doi: 10.1016/j.drugalcdep.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 16.Livingston JD, Milne T, Fang ML, Amari E. The effectiveness of interventions for reducing stigma related to substance use disorders: a systematic review. Addiction. 2012. Jan;107(1):39–50. doi: 10.1111/j.1360-0443.2011.03601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Batchelder AW, Foley JD, Wirtz MR, Mayer K, O’Cleirigh C. Substance use stigma, avoidance coping, and missed HIV appointments among MSM who use substances. AIDS Behav. 2021. May;25(5):1454–1463. doi: 10.1007/s10461-020-02982-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Do M, Ho H, Dinh H, Le H, Truong T, Dang T et al. Intersecting stigmas among HIV-positive people who inject drugs in Vietnam. Health Serv. Insights. 2021;14:117863292110135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carbado DW, Crenshaw KW, Mays VM, Tomlinson B. Intersectionality: Mapping the movements of a theory. Du Bois Rev. 2013;10(2):303–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalichman SC, Shkembi B, Eaton LA. Finding the right angle: A geometric approach to measuring intersectional HIV stigma. AIDS Behav. 2021,26(Suppl 1),27–38. [DOI] [PubMed] [Google Scholar]
- 21.Crenshaw K Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Rev. 1991;43:1241–99. [Google Scholar]
- 22.Medina-Perucha L, Scott J, Chapman S, Barnett J, Dack C, Family H. A qualitative study on intersectional stigma and sexual health among women on opioid substitution treatment in England: Implications for research, policy and practice. Soc Sci Med. 2019;222:315–322. [DOI] [PubMed] [Google Scholar]
- 23.Lyons CE, Olawore O, Turpin G, Coly K, Ketende S, Liestman B, et al. Intersectional stigmas and HIV-related outcomes among a cohort of key populations enrolled in stigma mitigation interventions in Senegal. AIDS. 2020;34 Suppl 1:S63–S71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ghasemi E, Rajabi F, Negarandeh R, Vedadhir A, Majdzadeh R. HIV, migration, gender, and drug addiction: A qualitative study of intersectional stigma towards Afghan immigrants in Iran. Health Soc Care Community. 2021;10.1111/hsc.13622. doi: 10.1111/hsc.13622 [DOI] [PubMed] [Google Scholar]
- 25.Nelson LE, Nyblade L, Torpey K, et al. Multi-level intersectional stigma reduction intervention to increase HIV testing among men who have sex with men in Ghana: Protocol for a cluster randomized controlled trial. PLoS One. 2021;16(11):e0259324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rodriguez-Hart C, Mackson G, Belanger D, et al. HIV and intersectional stigma reduction among organizations providing HIV services in New York City: A mixed-methods implementation science project. AIDS Behav. 2022;26(5):1431–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kleinman A, Hall-Clifford R. Stigma: a social, cultural and moral process. J Epidemiol Community Health. 2009. Jun;63(6):418–9. doi: 10.1136/jech.2008.084277. [DOI] [PubMed] [Google Scholar]
- 28.Stuikyte R, Barbosa I, Kazatchkine M. Getting to grips with the HIV epidemic in Russia. Curr Opin HIV AIDS. 2019. Sep;14(5):381–386. doi: 10.1097/COH.0000000000000573. [DOI] [PubMed] [Google Scholar]
- 29.Kozlov AP, Skochilov RV, Toussova OV, Verevochkin SV, Krasnoselskikh TV, Malov SV, Shaboltas AV. HIV incidence and behavioral correlates of HIV acquisition in a cohort of injection drug users in St Petersburg, Russia. Medicine. 2016; 95(44):e5238. doi: 10.1097/MD.0000000000005238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.UNAIDS. Country Factsheets: Russian Federation. 2020. https://www.unaids.org/en/regionscountries/countries/russianfederation
- 31.Balabanova Y, Coker R, Atun RA, Drobniewski F. Stigma and HIV infection in Russia. AIDS Care. 2006;18(7):846–52. [DOI] [PubMed] [Google Scholar]
- 32.Burki T Stigmatisation undermining Russia’s HIV control efforts. Lancet Infect Dis. 2015;15(8):881–2. [DOI] [PubMed] [Google Scholar]
- 33.Kelly J, Amirkhanian Y, Yakovlev A, Musatov V, Meylakhs A, Kuznetsova A, et al. Stigma reduces and social support increases engagement in medical care among persons with HIV infection in St. Petersburg, Russia. J Int AIDS Soc. 2014;17(4 Suppl 3):19618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burke SE, Calabrese SK, Dovidio JF, Levina OS, Uusküla A, Niccolai LM, Abel-Ollo K, Heimer R. A tale of two cities: stigma and health outcomes among people with HIV who inject drugs in St. Petersburg, Russia and Kohtla-Järve, Estonia. Soc Sci Med. 2015. Apr;130:154–61. doi: 10.1016/j.socscimed.2015.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Calabrese SK, Burke SE, Dovidio JF, Levina OS, Uusküla A, Niccolai LM, Heimer R. Internalized HIV and drug stigmas: Interacting forces threatening health status and health service utilization among people with HIV who inject drugs in St. Petersburg, Russia. AIDS Behav. 2016;20(1):85–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Code of Administrative Offences of The Russian Federation. No 195-Fz Of December 30. 2001. [Google Scholar]
- 37.Lunze K, Lunze FI, Raj A, Samet JH. Stigma and human rights abuses against people who inject drugs in Russia: A qualitative investigation to inform policy and public health strategies. PLoS One. 2015;10(8):e0136030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kelly J, Amirkhanian Y, Yakovlev A, Musatov V, Meylakhs A, Kuznetsova A, Chaika N. Stigma reduces and social support increases engagement in medical care among persons with HIV infection in St. Petersburg, Russia. J Int AIDS Soc. 2014;17(4 Suppl 3):19618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bobrova N, Rhodes T, Power R, Alcorn R, Neifeld E, Krasiukov N, Latyshevskaia N, Maksimova S. Barriers to accessing drug treatment in Russia: A qualitative study among injecting drug users in two cities. Drug Alcohol Depend. 2006;82 Suppl 1:S57–63. [DOI] [PubMed] [Google Scholar]
- 40.Rossi SL, Sereda Y, Luoma JB, et al. Addressing intersectional stigma as a care barrier for HIV-positive people who inject drugs: Design of an RCT in St. Petersburg, Russia. Contemp Clin Trials Commun. 2021;24:100861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vetrova M, Cheng D, Bendiks S, Gnatienko N, Lloyd-Travaglini C, Jiang W et al. HIV and substance use stigma, intersectional stigma and healthcare among HIV-positive PWID in Russia. AIDS Behav. 2021;25(9):2815–2826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Löwe B, Kroenke K, Herzog W, Gräfe K. Measuring depression outcome with a brief self report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord. 2004; 81, 61–66. [DOI] [PubMed] [Google Scholar]
- 43.Löwe B, Spitzer RL, Gräfe K, Kroenke K, Quenter A, Zipfel S, et al. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. J Affect Disord. 2004; 78, 131–140. doi: 10.1016/s0165-0327(02)00237-9 [DOI] [PubMed] [Google Scholar]
- 44.Kroenke K PHQ-9: global uptake of a depression scale. World Psychiatry. 2021;20(1):135–136. doi: 10.1002/wps.20821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kroenke K, Spitzer RL, Williams JB, Löwe B. The Patient Health Questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345–359. [DOI] [PubMed] [Google Scholar]
- 46.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 48.Rutter LA, Brown TA. Psychometric properties of the Generalized Anxiety Disorder Scale-7 (GAD-7) in outpatients with anxiety and mood disorders. J Psychopathol Behav Assess. 2017;39(1):140–146. doi: 10.1007/s10862-016-9571-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24:518–29. [DOI] [PubMed] [Google Scholar]
- 50.Wright K, Naar-King S, Lam P, Templin T, Frey M. Stigma scale revised: reliability and validity of a brief measure of stigma for HIV+ youth. J Adolesc Health. 2007;40:96–8. 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Luoma JB, Nobles RH, Drake CE, Hayes SC, O’Hair A, Fletcher L, Kohlenberg BS. Self-stigma in substance abuse: Development of a new measure. J Psychopathol Behav Assess. 2013;35(2):223–234. doi: 10.1007/s10862-012-9323-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sereda Y, Kiriazova T, Makarenko O, Carroll JJ, Rybak N, Chybisov A, et al. Stigma and quality of co-located care for HIV-positive people in addiction treatment in Ukraine: a cross-sectional study. J Int AIDS Soc. 2020;23(5):e25492. doi: 10.1002/jia2.25492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Goodin BR, Owens MA, White DM, Strath LJ, Gonzalez C, Rainey RL, Okunbor JI, Heath SL, Turan JM, Merlin JS. Intersectional health-related stigma in persons living with HIV and chronic pain: implications for depressive symptoms. AIDS Care. 2018;30(sup2):66–73. doi: 10.1080/09540121.2018.1468012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li L, Lin C, Feng N, Nguyen DB, Cao W, Le AT, Nguyen AT. Stigma related to HIV and drug use: Layers, types, and relations to mental health. AIDS Behav. 2020;24(8):2347–2354. doi: 10.1007/s10461-020-02794-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Earnshaw V, Smith L, Cunningham C, Copenhaver M. Intersectionality of internalized HIV stigma and internalized substance use stigma: Implications for depressive symptoms. J Health Psychol. 2013;20(8):1083–1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hook K, Sereda Y, Makarenko O, Bendiks S, Rybak NR, Dutta A, et al. Tuberculosis stigma and its correlates among HIV-positive people who inject drugs in Ukraine. 2021. Int J Tuberc Lung Dis. 2021;25(9),747–753. doi: 10.5588/ijtld.21.0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brandt C, Zvolensky MJ, Woods SP, Gonzalez A, Safren SA, O’Cleirigh CM. Anxiety symptoms and disorders among adults living with HIV and AIDS: A critical review and integrative synthesis of the empirical literature. Clin Psychol Rev. 2017. Feb;51:164–184. doi: 10.1016/j.cpr.2016.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Johnson SU, Ulvenes PG, Øktedalen T, Hoffart A. Psychometric properties of the General Anxiety Disorder 7-Item (GAD-7) scale in a heterogeneous psychiatric sample. Front Psychol. 2019;10:1713. doi: 10.3389/fpsyg.2019.01713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Aina Y, Susman JL. Understanding comorbidity with depression and anxiety disorders. J Am Osteopath Assoc. 2006;106(5 Suppl 2):S9–14. [PubMed] [Google Scholar]
- 60.Leserman J Role of depression, stress, and trauma in HIV disease progression. Psychosom. Med 2008;70(5):539–545. [DOI] [PubMed] [Google Scholar]
- 61.Rivera Rivera Y, Vazquez Santiago F. Impact of depression and inflammation on the progression of HIV disease. Journal of Clinical & Cellular Immunology. 2016;7(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nanni M, Caruso R, Mitchell A, Meggiolaro E, Grassi L. Depression in HIV infected patients: a review. Curr Psychiatry Rep. 2014;17(1). [DOI] [PubMed] [Google Scholar]
- 63.Doherty AM, Gaughran F. The interface of physical and mental health. Soc Psychiatry Psychiatr Epidemiol. 2014. May;49(5):673–82. doi: 10.1007/s00127-014-0847-7. [DOI] [PubMed] [Google Scholar]
- 64.Bengtson AM, Pence BW, Mimiaga MJ, Gaynes BN, Moore R, Christopoulos K, O’Cleirigh C, Grelotti D, Napravnik S, Crane H, Mugavero M. Depressive symptoms and engagement in Human Immunodeficiency Virus care following antiretroviral therapy initiation. Clin Infect Dis. 2019. Jan 18;68(3):475–481. doi: 10.1093/cid/ciy496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Relf MV, Pan W, Edmonds A, Ramirez C, Amarasekara S, Adimora AA. Discrimination, medical distrust, stigma, depressive symptoms, antiretroviral medication adherence, engagement in care, and quality of life among women living with HIV in North Carolina: A mediated structural equation model. J Acquir Immune Defic Syndr. 2019. Jul 1;81(3):328–335. doi: 10.1097/QAI.0000000000002033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Collins PY, Velloza J, Concepcion T, Oseso L, Chwastiak L, Kemp CG, Simoni J, Wagenaar BH. Intervening for HIV prevention and mental health: a review of global literature. J Int AIDS Soc. 2021. Jun;24 Suppl 2(Suppl 2):e25710. doi: 10.1002/jia2.25710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Safren SA, O’Cleirigh C, Tan JY, Raminani SR, Reilly LC, Otto MW, Mayer KH. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychol. 2009;28(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Safren SA, O’Cleirigh C, Andersen LS, Magidson JF, Lee JS, Bainter SA, Musinguzi N, Simoni J, Kagee A, Joska JA. Treating depression and improving adherence in HIV care with task-shared cognitive behavioural therapy in Khayelitsha, South Africa: A randomized controlled trial. J Int AIDS Soc. 2021;24(10):e25823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Abas M, Nyamayaro P, Bere T et al. Feasibility and acceptability of a task-shifted intervention to enhance adherence to HIV medication and improve depression in people living with HIV in Zimbabwe, a low income country in sub-Saharan Africa. AIDS Behav. 2018;22:86–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Batchelder AW, Moskowitz JT, Jain J, Cohn M, Earle MA, Carrico AW. A novel technology-enhanced internalized stigma and shame intervention for HIV-positive persons with substance use disorders. Cogn Behav Pract. 2020;27(1):55–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Earnshaw VA, Eaton LA, Collier ZK, Watson RJ, Maksut JL, Rucinski KB, Kelly JF, Kalichman SC. HIV stigma, depressive symptoms, and substance use. AIDS Patient Care STDS. 2020;34(6):275–280. doi: 10.1089/apc.2020.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gopalkrishnan N Cultural diversity and mental health: Considerations for policy and practice. Front Public Health. 2018;6:179. doi: 10.3389/fpubh.2018.00179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.World Bank Country and Lending Groups. (n.d.). https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- 74.Chibanda D Depression and HIV: integrated care towards 90-90-90. Int Health. 2017. Mar 1;9(2):77–79. doi: 10.1093/inthealth/ihw058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nakimuli-Mpungu E, Musisi S, Smith CM, Von Isenburg M, Akimana B, Shakarishvili A, Nachega JB, Mills EJ, Chibanda D, Ribeiro M, V Williams A, Joska JA. Mental health interventions for persons living with HIV in low- and middle-income countries: a systematic review. J Int AIDS Soc. 2021. Jun;24 Suppl 2(Suppl 2):e25722. doi: 10.1002/jia2.25722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hook K, Bogdanov S. Mental health care in Eastern Europe and Central Asia: An analysis of needs and a call for greater investment. 2021; The Lancet Regional Health–Europe. 10.1016/j.lanepe.2021.100182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Toussova O, Vetrova M, Blokhina E, Bushara N, Bendiks S, Gnatienko N, et al. Dual stigma affecting HIV-positive PWID in Russia: a qualitative study [Internet]. San Diego, USA; 2018. Available from: https://www.drugabuse.gov/international/abstracts/double-stigma-among-hiv-positive-people-who-inject-drugs-in-russia-hiv-care-qualitative-study [Google Scholar]
- 78.Ingram I, Kelly PJ, Deane FP, Baker AL, Goh MC, Raftery DK, Dingle GA. (2020). Loneliness among people with substance use problems: A narrative systematic review. Drug and Alcohol Review. 39(5):447–483. [DOI] [PubMed] [Google Scholar]
- 79.Kryukova TL, Shargorodskaya OV. Loneliness as a barrier in coping with HIV-infection. Yaroslavl Pedagogical Bulletin. 2015;3:205–9. [Google Scholar]
- 80.Luoma JB, Kohlenberg BS, Hayes SC, Fletcher L. Slow and steady wins the race: A randomized clinical trial of acceptance and commitment therapy targeting shame in substance use disorders. J Consult Clin Psychol. 2012;80(1):43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Osaji J, Ojimba C, Ahmed S. The use of acceptance and commitment therapy in substance use disorders: A review of literature. Journal of Clinical Medicine Research. 2020;12(10), 629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: Moving toward resilience. Stigma and Health. 2015;1(S):60–74. [DOI] [PMC free article] [PubMed] [Google Scholar]


