Abstract
While non-alcoholic fatty liver disease (NAFLD) is a prevalent and frequent cause of liver-related morbidity and mortality, it is also strongly associated with cardiovascular disease-related morbidity and mortality, likely driven by its associations with insulin resistance and other manifestations of metabolic dysregulation. However, few satisfactory pharmacological treatments are available for NAFLD due in part to its complex pathophysiology, and challenges remain in stratifying individual patient’s risk for liver and cardiovascular disease related outcomes. In this review, we describe the development and progression of NAFLD, including its pathophysiology and outcomes. We also describe different tools for identifying patients with NAFLD who are most at risk of liver-related and cardiovascular-related complications, as well as current and emerging treatment options, and future directions for research.
Keywords: NAFLD, MAFLD, NASH, non-invasive tests, metabolic syndrome, cirrhosis, cardiovascular disease
1. Introduction
History, Prevalence, Nomenclature Controversies
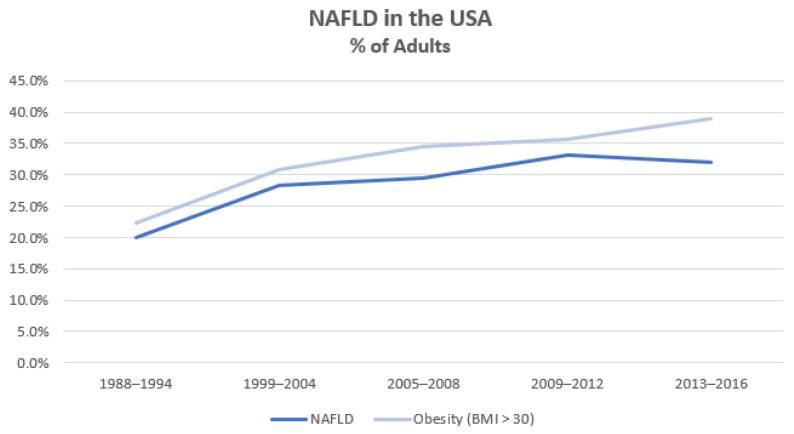
Liver disease is the 11th most common cause of mortality and the 15th most common cause of morbidity globally [1]. While liver disease has many aetiologies including viral hepatitis, alcohol, autoimmune and genetic disorders, the proportion attributable to non-alcoholic fatty liver disease (NAFLD) has been growing rapidly—paralleling the global obesity epidemic (Figure 1). Patients with NAFLD have increased mortality compared with matched control populations due to cardiovascular, liver and/or malignant causes [2].
Figure 1.
Proportion of U.S.A. adults with NAFLD and/or obesity (adapted from Younossi et al. [3]).
NAFLD encapsulates a spectrum of disease, from simple hepatic steatosis (defined as >5% of hepatocytes containing fat) through to non-alcoholic steatohepatitis (NASH), fibrosis, and cirrhosis [4]. The diagnostic criteria for NAFLD rely on ‘ruling-out’ hepatic steatosis due to other factors such as alcohol and drugs. Indeed, as the name suggests, alcohol is explicitly listed as an exclusion criterion. Since NAFLD was first coined in 1987 [5], its incidence has risen dramatically, with an estimated 25% of the world’s adult population now affected [6,7]. Furthermore, NAFLD is on track to become the leading cause of liver-related morbidity, mortality, and transplant [8,9,10].
Defining a disease entity via predominantly negative criteria has attracted criticism. As early as 2002, questions were raised regarding NAFLD’s nomenclature and aetiology following research associating the condition with metabolic abnormalities [11] and the demonstration of a link between the pathophysiology of NAFLD with insulin resistance and the metabolic syndrome [12,13]. Additionally, new evidence emerged that NAFLD may worsen outcomes in patients with chronic hepatitis C [14]—however, patients, by definition, were not classified as having concomitant NAFLD. Multiple position statements and editorials over the next 18 years espoused the merits of renaming NAFLD to better encapsulate the pathogenesis of the disease [15,16,17].
In this context, the term metabolic dysfunction associated fatty liver disease (MAFLD) was recently coined in 2020 by a large international consensus group [18,19] that utilises ‘inclusion-based diagnostic criteria’ of having hepatic steatosis (determined either by imaging, blood biomarkers or scores, or histology) with one or more of: overweight, type 2 diabetes mellitus (T2DM), or two or more features of metabolic dysfunction [18]. Although there are several favourable outcomes associated with renaming NAFLD to MAFLD including a stronger link between the underlying pathophysiology and disease state that relates diagnostic criteria to phenotype and pathological outcomes, as well as allowing multi-aetiologic liver disease diagnoses that may include NAFLD, the proposed nomenclature change is not without controversy [20]. Several concerns have been raised, including: (i) while NAFLD is an imperfect name, changing nomenclature would be better undertaken once identifiable pathophysiological subtypes are identified; (ii) the concept and definition of metabolic health or abnormalities are contentious; (iii) various regulatory agencies use the histological presence of NASH as a key criteria for drug trials, and MAFLD implies removing NASH as a concept; (iv) the implications for patient and non-specialist disease recognition are unknown; and (v) there was a perceived lack of engagement with non-physician interest groups to coalesce around a new nomenclature that better serves all relevant parties. Given this debate is on-going and the revised nomenclature is relatively recent, our review will focus on NAFLD, highlighting developments in the field and opportunities for improving outcomes.
2. Body
2.1. The Pathogenesis of NAFLD and NASH
The pathogenesis of NAFLD remains incompletely understood, and likely varies between individuals. However, the “multiple-hit hypothesis” is a useful framework to aid in our understanding of this condition [21,22]. The development of hepatic steatosis is the “first hit”, and sequential or simultaneous combinations of genetic susceptibilities, dietary habits, lifestyle factors, metabolic dysfunction (primarily insulin resistance), and/or alterations in the gut microbiome are all potential contributors to the development of more advanced liver disease [23,24]. Through this pathway, the subsequent or concurrent activation of the adaptive and innate immune system leads to the activation of hepatic stellate cells and Kupffer cells, promoting fibrosis and cirrhosis [25].
2.2. Hepatic Fatty Acid Metabolism
The liver is the major site of fatty acid metabolism in humans [26]. Fatty acids—taken into hepatocytes via plasma or formed by de novo lipogenesis (DNL)—are primarily used for energy production through oxidation or are excreted back into plasma in the form of very low density lipoproteins (VLDL) [26,27]. When metabolically healthy, the esterification of free fatty acids (FFAs) to glycerol (forming triglycerides) and subsequent storage in hepatocytes is rare; any significant hepatic accumulation of fat is, thus, considered abnormal. In obese NAFLD, there are three primary sources of hepatic fatty acid accumulation: DNL (15–40%) [28], dietary intake (~15%) [29], and (predominantly adipose tissue-derived) serum esterified fatty acids (~59%) [29]. While the rate of DNL is significantly different between NAFLD and non-NAFLD subjects [30,31], NAFLD is also characterised by increased adipose tissue fatty acid flux and peripheral insulin resistance [31]. Indeed, both adipose tissue insulin resistance [32] and the anatomic location of fat [33] (visceral vs. subcutaneous) may influence the development of NAFLD. As discussed in recent reviews of adipose tissue and insulin resistance [34,35] as well as via recent lipidomic studies [36], it is likely that our understanding of the role of extra-hepatic adipose tissue and fatty acid flux on NAFLD development will continue to expand.
However, irrespective of their source, excess hepatic fatty acids and their metabolic products may be toxic. Fatty acids—either via incomplete oxidation or pathologic metabolic pathways—may lead to the development of sphingolipids (such as ceramides) and/or diacylglycerols which can worsen insulin resistance [37,38,39]. Further, in the presence of an excess of fatty acids, a subgroup of patients are vulnerable to direct cellular insults. FFAs may induce the enzymatic production of reactive oxygen species (ROS) which cause cellular damage and hepatotoxicity [40]. Dysfunctional mitochondria, when exposed to FFAs, may also precipitate the generation of ROS—though whether mitochondria are pathogenic or bystanders in the NAFLD/NASH process is an area of active research [41]. ROS generation is a likely contributor to NASH and to the development of progressive fibrosis and cirrhosis. An improved understanding of these processes may also lead to new treatment options as dysfunctional metabolic pathways may directly contribute to hepatic steatogenesis. For example, acetyl-CoA carboxylase is required for DNL. As mentioned above, DNL is a significant contributor to hepatic steatosis; given this, pharmacotherapy inhibiting acetyl-CoA carboxylase has been studied in rodents [42,43] and humans [44] and may reduce both hepatic steatosis and fibrosis. Future work will likely elucidate additional pathophysiological pathways and potentially add to our treatment armamentarium.
2.3. Genetics and Heritability
Multiple studies have found that NAFLD is partly heritable. Several gene variants have been implicated in the presence, pathogenesis, and severity of NAFLD [45,46], though only 10–20% of NAFLD cases are associated with currently recognised gene variants [47]. The most studied and well recognised of these is PNPLA3, which was first linked to NAFLD by a 2008 genome-wide association study [48]. PNPLA3 encodes a protein on hepatocyte lipid droplets. When dysfunctional, it may accumulate, impairing the access of other lipase enzymes to the lipid droplets, leading to impaired triglyceride hydrolysis and consequently lipid accumulation in hepatocytes [27]. Other genetic abnormalities affecting lipid transport and metabolism are implicated in the pathogenesis of NAFLD, including TM6SF2, GCKR, and HSD17B13 [46]. When pathological, these single nucleotide polymorphisms (SNPs) may influence VLDL transport, FFA production and hepatocellular uptake, and glycolysis. In essence, SNPs affecting almost all stages of hepatic fatty acid metabolism are implicated in the development of NAFLD, emphasising that many metabolic pathways are involved in hepatic steatogenesis. Additionally, well characterised metabolic disorders such as familial hypobetalipoproteinaemia may cause a heritable form of hepatic steatosis [49]. While familial hypobetalipoproteinaemia may not be related to insulin resistance and is commonly associated with low serum lipids [49] and possible cardioprotection [50], its impact on histological liver disease severity and progression remains uncertain [51].
2.4. Dietary Intake
Multiple dietary habits contribute to the development of NAFLD and can be considered in terms of their overall energy load and/or energy-containing macronutrient constituents which may have differing biological effects. Both observational and interventional studies have shown that excess caloric intake is associated with NAFLD irrespective of diet composition [52,53]. Additionally, a study of NAFLD pre- and post-dietary advice showed an association between weight gain and the development of NAFLD as well as weight loss with NAFLD resolution [52]. Mechanistically, increased dietary intake of carbohydrate (increasing hepatic substrates for DNL) or FFAs may overwhelm the capacity to manage FFA hepatocyte flux, promoting NAFLD development. Macronutrient constituents also matter. For example, glucose and fructose—which are energetically equivalent—influence metabolic pathways and affect steatogenesis differently [54,55]. Similarly, saturated fatty acids (SFAs) have different biological effects than mono- or poly-unsaturated fatty acids (MUFAs or PUFAs) [56]. In one over-feeding trial comparing SFA intake to unsaturated fatty acid and simple carbohydrate intake, SFA-based overfeeding was associated with significantly higher hepatic fat content than other overfeeding—though all participants experienced worsened hepatic steatosis [57]. Additional experimental studies have shown that even amongst unsaturated fatty acids there are differences, for example, omega-3 PUFAs have been shown to reduce liver fat content when compared with olive oil [58], possibly via the suppression of hepatic DNL and concurrently increased fatty acid oxidation. Cross-sectional observational studies also show that macronutrient composition is important independent of total caloric intake. Inverse associations between PUFA intake and NAFLD have been shown [59], as have direct links between sugar-sweetened beverages and the presence of NAFLD [60,61]. Specific foodstuffs may also play a role in the presence of NAFLD. One study has shown an association between red and/or processed meat and NAFLD [62], and there are possible inverse associations between NAFLD and green leafy vegetable intake [63]. There are additional micronutrient dietary factors that may influence the development of NAFLD and NASH—these are listed in Table 1. For more comprehensive reviews, see Pickett-Blakely et al. [64] and Licata et al. [65].
Table 1.
Micronutrients and NAFLD/NASH.
| Dietary Factor | Epidemiological Association | Proposed Mechanism | Micronutrient Effect on NAFLD Progression |
|---|---|---|---|
| Vitamins | |||
| Vitamin E | Poorly defined [66] | Regulates oxidative stress, inflammation, cellular apoptosis [67] | ↓ (Sometimes used for treatment) |
| Vitamin A | Low serum levels in NAFLD/NASH [68] | Regulates de novo lipogenesis and hepatic lipid metabolism [67] | ?↓ (Complex interplay [69]) |
| Vitamin C | Low intake in NAFLD/NASH [70] | Regulates oxidative stress, adiponectin | ?↓ (Possibly contributes [70]) |
| Vitamin D | (Probably) low in NAFLD/NASH [71,72] | Oxidative stress [72], insulin resistance [67], autophagy [67] | ↓ |
| Minerals | |||
| Zinc | Mixed data [73,74] | Deficiency may worsen oxidative stress [64] and insulin resistance [75] | ?↓ (Animal model [64] and preliminary human [76] data) |
| Selenium | Mixed data [77] | Antioxidant, apoptosis regulation [77] | ?↓ (Reduced fibrosis [78]) |
| Copper | Low hepatic and serum copper in NAFLD/NASH [79] | Oxidative stress, upregulate triglyceride synthesis [64] | ↓ |
| Iron | Elevated ferritin associated with NAFLD/NASH severity [80,81] | Hepatic lipid peroxidation [82], impairment of hepatic lipid homeostasis [64] | ↑ |
?: means possible; ↓: means decrease; ↑: means increase.
Other non-energetic dietary constituents have benefits in NAFLD and liver disease. For example, coffee intake has been previously inversely linked to cardiovascular disease, cancer incidence, and all-cause mortality [83,84]. Its use is inversely associated with abnormal liver function tests (LFTs) and liver fibrosis in various diseases including hepatitis B, hepatitis C, and NAFLD [85,86]. It is associated with a reduced risk of developing hepatocellular carcinoma (HCC) [87], a leading cause of mortality in liver disease. Multiple mechanisms have been proposed [88], including reducing the deposition of liver fat and collagen and increasing glutathione synthesis (ameliorating damage from ROS). These mechanisms are not just due to caffeine—coffee contains multiple bioactive compounds, including chlorogenic acid and other polyphenols, and decaffeinated coffee has some benefit in human HCC [87] and murine NAFLD [89]. Supporting this, a U.K. study has shown similar benefits of caffeinated compared with decaffeinated coffee consumption on outcomes in chronic liver disease (CLD) [90]. Further, considering caffeine in isolation, total intake is not associated with NAFLD prevalence nor degree of fibrosis [91].
2.5. Physical Activity
In addition to diet, other lifestyle factors are implicated in the development of NAFLD. Multiple observational studies have shown an association between a sedentary lifestyle and the incidence and prevalence of NAFLD [92,93,94]. However, the amount of physical activity required to reduce the incidence of NAFLD is relatively high. In one study, when adjusting for covariates (including visceral adiposity and insulin resistance) only those in the highest quartile of metabolic equivalents had a reduced hazard of developing NAFLD [95]. Indeed, even short-term periods of inactivity can worsen metabolic health—one study showed 14 days of marked inactivity caused significant deterioration in insulin sensitivity and increased liver fat [96]. Recent meta-analyses of interventional studies have also shown that both aerobic and resistance training can improve hepatic steatosis [97,98]—often independent of weight change. However, in addition to structured exercise, non-exercise physical activity is an important marker of health. It has been shown to be independently inversely associated with cardiovascular disease risk and all-cause mortality [99,100]. While this area is under-studied in NAFLD, one study has shown that patients with NAFLD spend more time being sedentary and walk fewer daily steps than controls [92]. In addition to the associations between an active lifestyle and weight control, exercise may independently improve insulin sensitivity [101] (improving hepatic energy kinetics) and increase hepatic VLDL clearance [102].
2.6. Metabolic Dysfunction and Insulin Resistance
Metabolic dysfunction and insulin resistance are strongly associated with NAFLD; indeed, insulin resistance is often described as a key pathogenic feature of NAFLD. However, it is important to note that insulin resistance in NAFLD is not only present within the liver itself (leading to increased hepatic DNL), but also in skeletal muscle (impairing glucose disposal) and adipose tissue (causing lipolysis and increased fatty acid delivery to the liver) [28,103]. Furthermore, the relationship between NAFLD and insulin resistance is not unidirectional. Various data link hepatokines in NAFLD with the development of peripheral insulin resistance and impaired pancreatic insulin secretion [103]. As such, while the prevalence of NAFLD in patients with T2DM ranges from 30 to 87% [104,105], NAFLD may also pre-date the development of T2DM in some patients [106].
Additional features of metabolic dysfunction, including dyslipidaemia, hypertension, raised high sensitivity C-reactive protein, and advanced atherosclerosis, are over-represented in patients with NAFLD [107,108]. While some of these findings may be due to shared pathophysiologic pathways, some are likely pathogenic. For example, one study has linked NAFLD with increased vascular resistance, higher serum aldosterone, and sympathetic nervous system activation—all potential contributors to hypertension [109]. Others are likely the result of a shared metabolic pathway—some data suggest that there is reduced HDL cholesterol efflux capacity in NAFLD, independently associated with atherosclerosis [110]. This combination of over-expressed pathologic metabolic abnormalities in NAFLD, particularly T2DM and/or obesity, are also associated with an increased risk of liver fibrosis and incident severe liver disease [111].
2.7. Gut-Liver Axis
The gut microbiome and the gut–liver axis are also implicated in the development and progression of NAFLD [112,113]. While there are a variety of microbiome signatures implicated in NAFLD/NASH, the data are relatively immature, and firm conclusions are necessarily difficult due to potential heterogeneity in studied population ages, geographies, and diets, as well as the actual tools used to sequence the microbiome [114]. Different microbiotal signatures may predispose to NAFLD and liver fibrosis through multiple different pathways which are beyond the scope of this review, though are well-described in Aron-Wisnewsky et al. [114] and Gupta et al. [115]. However, one microbiotal constituent consistently implicated is lipopolysaccharide (LPS), a Gram-negative bacteria cell wall component, which has been recently linked to multiple metabolic diseases including atherosclerosis and T2DM as well as NAFLD [113,116]. By far the most significant source of LPS in humans is from our commensal gut microbiota. In health, the intestinal barrier provides a structural and functional impediment to the translocation of gut bacteria and bacteria-derived antigens (such as LPS) into the portal circulation. While a detailed description of LPS-associated proinflammatory pathways is beyond the scope of this paper, disruption of gut barrier function and LPS translocation causes the release of proinflammatory mediators which can co-activate both hepatic stellate cells and Kupffer cells, causing progressive fibrosis [113]. This disruption and translocation can be caused by multiple pathological pathways: (i) small intestinal bacterial overgrowth [117] (causing excess LPS and translocation); (ii) increased intestinal permeability [118], caused by various factors including exogenous [119] and endogenously-produced [120] ethanol exposure, and/or lifestyle [121]; and (iii) high fat diets [122,123]; all can alter the composition of the intestinal microbiome and/or intestinal permeability.
2.7.1. Case Identification for NAFLD and NASH
While biopsy remains the gold standard for identifying NAFLD, it is imperfect; there are inherent safety risks [124] (pain, infection, bleeding), liver tissue heterogeneity (leading to sampling error(s) with mis-classification) [125,126], histopathological reporting accuracy [127], and the impracticality of acquiring liver biopsies in all patients suspected of NAFLD. As such, various other surrogate tests are often used in clinical and public health research settings (summarised in Table 2).
Hepatic steatosis can be identified with reasonable accuracy using ultrasonography [128,129], computed tomography [129,130], and magnetic resonance spectroscopy (MRS) or magnetic resonance imaging protein density fat fraction (MRI-PDFF) [130]. While all these techniques have limitations in terms of sensitivity, their use as a surrogate for liver biopsy is commonplace and appropriate. A recent development in non-invasive assessment is liver stiffness measurement by vibration controlled transient elastography (LSM-VCTE) with an associated controlled attenuation parameter (CAP), allowing for both the identification of hepatic steatosis [131,132] via CAP as well as concurrent assessment of potential fibrosis/cirrhosis [133].
Due to time and cost constraints, it is impractical to use liver biopsy, MRI-PDFF, or other radiological assessments on a public health level to determine hepatic steatosis. Therefore, other tools have been developed with greater applicability that combine clinical and biochemical parameters to calculate scores to rule in or out hepatic steatosis (e.g., fatty liver index [134], hepatic steatosis index [135], Framingham steatosis index [136], and Dallas steatosis index [137]). These are accurate and convenient enough for epidemiological modelling and finding associations between conditions in large datasets, though are not yet part of routine clinical practice for identifying individual NAFLD patients. Additionally, while these tests have been externally validated, results may vary by the ethnicity and/or comorbidities of individuals. It is also important to note that the non-invasive identification of NASH is much more difficult than NAFLD. A recent meta-analysis has shown that we lack adequate evidence to differentiate between NAFLD and NASH in clinical practice [138]. Many early composite scores relied on inflammatory biomarkers not collected in routine practice and often lacked the requisite accuracy to alter management [139]. There are emerging novel tests such as the NIS4 [140] which may find a role in risk stratification in the future, though further validation and cost-efficacy assessment will be required.
Table 2.
Methods to identify NAFLD.
| Surrogate Test for NAFLD Case-ID | Test Components | Sensitivity | Specificity |
|---|---|---|---|
| Radiology | |||
| Liver Ultrasound [128,129] | 84.8% | 93.6% | |
| Nb. More sensitive with increasing degrees of steatosis | – | ||
| Liver Computed Tomography [130,141] | 72.7–82% | 91.3–100% | |
| Nb. More sensitive with increasing degrees of steatosis | – | ||
| MRI-PDFF [142] | – | 93% | 94% |
| FibroScan CAP [131,132] | |||
| M Probe | 79% | 74% | |
| Nb. Cut-off of 294 dB/m can be used to differentiate no steatosis from any degree of steatosis [132] | – | ||
| XL Probe | |||
| Nb. Cut-off of 297 dB/m can be used to differentiate no steatosis from any degree of steatosis [132] | 79.8% | 73.5% | |
| Composite Scores | |||
| Fatty Liver Index [134,143] | BMI, waist circumference, triglycerides, γ-glutamyltransferase | ||
| FLI < 30 (used to rule out NAFLD) | 81–87% | 64–65% | |
| FLI ≥ 60 (used to rule in NAFLD) | 44–61% | 86–90% | |
| Framingham Steatosis Index [136,144] | Age, sex, BMI, triglycerides, hypertension, diabetes mellitus, alanine aminotransferase (ALT), aspartate aminotransferase (AST) | ||
| FSI ≥ 23 (used to rule in/out NAFLD) | 52–79% | 71–80% | |
| Dallas Steatosis Index [137] | Age, sex, BMI, triglycerides, hypertension, diabetes mellitus, ALT, ethnicity, glucose | ||
| <−1.4 risk (low risk of NAFLD) | 86% | 59% | |
| ≥0% risk (high risk of NAFLD) | 51% | 90% | |
| Hepatic Steatosis Index [135,144] | Sex, BMI, diabetes mellitus, ALT, AST | ||
| HSI < 30 (used to rule out NAFLD) | 87.8–93.1% | 25–40% | |
| HSI ≥ 36 (used to rule in NAFLD) | 25–46% | 79–93.1% | |
| NAFLD Liver Fat Score [144,145] | Diabetes mellitus, metabolic syndrome, ALT, AST, fasting insulin | ||
| NAFLD-LFS < −0.640 (used to rule in/out NAFLD) | 48.1–86% | 71–83.4% |
2.7.2. Differential Diagnoses for Hepatic Steatosis
As outlined above, NAFLD requires the exclusion of alternative or secondary causes of steatosis, the most common of which is ethanol [18]. Ethanol’s most direct steatogenic effects are via inhibition of fatty acid oxidation in combination with increased fatty acid synthesis [146]. Additionally, ethanol increases hepatic uptake of fatty acids [147] and impairs a concurrent homeostatic increase in hepatic VLDL synthesis [147]. Ethanol can also alter intestinal barrier function, increasing LPS translocation into the portal system [119] and driving steatosis/fibrosis in a manner similar to that seen in NAFLD. Interestingly, advanced alcohol-related liver disease is associated with PNPLA3 variants [148] that are classically associated with NAFLD. Mechanistically this is plausible—steatosis, irrespective of cause, is likely worsened by the inability to adequately process hepatocyte lipid droplets.
Other CLDs may also be steatogenic. Hepatitis C (particularly genotype 3) is associated with hepatic steatosis [149]—and steatosis in that setting may worsen outcomes [14]. Preliminary data suggest that hepatitis C can cause dyslipidaemia and insulin resistance [150]. These may pre-date the development of hepatic steatosis, and the combination of these features has been previously called hepatitis C-associated dysmetabolic syndrome. Wilson’s disease is also associated with hepatic steatosis, though the pathophysiology is complex and incompletely understood [151].
Other systemic conditions or disturbances of stable enteral nutrition may also cause hepatic steatosis including total parenteral nutrition (TPN) via small intestinal bacterial overgrowth (due to bowel rest), choline deficiency, protein malnutrition (preventing triglyceride excretion in VLDL particles), excess total calories, and potentially the direct inflammatory and oxidative effects of parenterally-delivered fatty acids [152]. Additionally, refeeding in patients with anorexia nervosa can also lead to hepatic steatosis [153]. polycystic ovarian syndrome (PCOS) is also associated with hepatic steatosis [154,155]; this is due to a combination of insulin resistance, overweight/obesity, and hyperandrogenism.
Some medications are also considered steatogenic or to promote steatohepatitis. Tamoxifen [156], glucocorticoids [157], amiodarone [158], and multiple others [159] are implicated, and by definition, patients with drug-related steatosis cannot be diagnosed as having NAFLD. As such, careful history taking and biochemical assessment are important in making a firm diagnosis of NAFLD.
2.7.3. Cirrhosis and Cardiovascular Risk Assessment
Patients with NAFLD are at risk of progressive fibrosis, cirrhosis, and cardiovascular disease. Liver fibrosis, as a precursor to cirrhosis and subsequent liver-related morbidity and mortality, can be identified through biopsy results (showing features of NASH or progressive fibrosis/cirrhosis) [160], non-invasive devices (e.g., LSM-VCTE) [161], proprietary [140,162,163] or experimental serological tests [164,165] (e.g., enhanced liver fibrosis test [ELF]), or validated non-invasive scores [162] such as FIB-4 [166] and NAFLD fibrosis score [167] (Table 3). Importantly, work has validated the use of many of these scores, particularly LSM-VCTE and FIB-4, to assist with risk stratifying and predicting liver-related outcomes [168].
However, when considering these fibrosis assessment tools, many in use were not developed for cardiovascular risk assessment (e.g., FIB-4, LSM-VCTE). Interestingly though, subsequent work has shown an association between worsening liver fibrosis and cardiovascular outcomes [161,169]—as such, these tools may contribute to cardiovascular risk assessment for individuals with NAFLD. Further, other tests (e.g., QRISK3 [170], Framingham risk estimator [171]), while not created specifically for individuals with NAFLD, may still be used to estimate cardiovascular risk in patients with NAFLD. It remains unknown whether those risk scores are accurate for individuals with NAFLD and advanced fibrosis.
Due to the differential accuracy and cost when utilising these tests, two tier systems have been developed to assist with screening and risk stratifying patients with hepatic steatosis by fibrosis stage in primary care. Generally, these involve the use of an accessible low-cost test (e.g., FIB-4) followed by a second assessment in the case of an indeterminate result. Multiple groups have studied different iterations, including using FIB-4 and ELF [172] or FIB-4 and LSM-VCTE [133,173]. Modelling has shown these two-tier assessments are cost-effective and improve resource utilisation [174,175], though further prospective work in different populations, different countries, and with different funding models will be important.
Table 3.
Methods to identify liver fibrosis.
| Risk Assessment in NAFLD | Test Components | Sensitivity | Specificity |
|---|---|---|---|
| Radiology—Advanced Fibrosis | |||
| Magnetic Resonance Elastography [176] | – | 83% | 89% |
| LSM-VCTE [133] | |||
| Nb. Different literature uses different cut-offs | |||
| Cut-offs: | |||
| LSM < 7.4 kPa (used to rule out advanced fibrosis) | – | 90% | 60% |
| LSM ≥ 12.1 kPa (used to rule in advanced fibrosis) | 55% | 90% | |
| Composite Scores—Advanced Fibrosis | |||
| FIB-4 [133,166] | ALT, AST, platelets, age | ||
| Nb. Different literature uses different cut-offs | |||
| Cut-offs: | |||
| FIB-4 < 0.88 (used to rule out advanced fibrosis) | 90% | 39% | |
| FIB-4 < 1.3 (used to rule out advanced fibrosis) | 74% | 64% | |
| FIB-4 > 2.31 (used to rule in advanced fibrosis) | 38% | 90% | |
| FIB-4 > 2.67 (used to rule in advanced fibrosis) | 30% | 94% | |
| FIB-4 (for those ≥ 65 years of age) [177] | ALT, AST, platelets, age | ||
| Nb. Different literature uses different cut-offs | |||
| Cut-offs: | |||
| FIB-4 < 1.3 (used to rule out advanced fibrosis) | 93% | 35% | |
| FIB-4 > 2.0 (used to rule in advanced fibrosis) | 77% | 70% | |
| NAFLD Fibrosis Score (NFS) [133] | Age, BMI, impaired fasting glucose, T2DM, ALT, AST, platelets, albumin | ||
| Nb. Different literature uses different cut-offs | |||
| Cut-offs: | |||
| NFS < −2.55 (used to rule out advanced fibrosis) | 90% | 36% | |
| NFS > 0.28 (used to rule in advanced fibrosis) | 29% | 90% | |
| Enhanced Liver Fibrosis Test [163,172] | Type III procollagen peptide, hyaluronic acid, tissue inhibitor of metalloproteinase-1 | ||
| Cut-offs: | |||
| ELF < 9.8 (used to rule out advanced fibrosis) | 57.5–65% | 86–88.9% | |
| ELF > 11.3 (used to rule in advanced fibrosis) | 19.5–36% | 96–99.1% | |
| FibroTest [178] | α2 -macroglobulin, apolipoprotein A1, haptoglobin, total bilirubin, γ-glutamyltranspeptidase (GGT) |
||
| Cut-offs: | |||
| FibroTest < 0.30 (used to rule out advanced fibrosis) | 92% | 71% | |
| FibroTest > 0.70 (used to rule in advanced fibrosis) | 25% | 97% | |
| BARD Score [162,179] | BMI, ALT, AST, T2DM | ||
| Cut-off: | |||
| Score ≥ 2 (used to rule in/out advanced fibrosis) | 75.2% | 61.6% | |
| FORNS Index [180,181] | Age, platelets, cholesterol, GGT | ||
| Nb. Data are limited for NAFLD | |||
| Cut-offs: | |||
| Score ≤ 4.2 (used to rule out advanced fibrosis) | 100% | 54.8% | |
| Score > 6.9 (can be used to rule in fibrosis) | 42.9% | 95.7% | |
| FibroScan-AST (FAST) Score [182] | VCTE-LSM, CAP, AST | ||
| Nb. Composite of LSM-VCTE and biochemistry | |||
| Cut-offs: | |||
| FAST ≤ 0.35 (used to rule out advanced fibrosis) | 89% | 64% | |
| FAST ≥ 0.65 (used to rule in advanced fibrosis) | 49% | 92% |
3. Outcomes of NAFLD and NASH
3.1. NAFLD—Liver Outcomes
The rate of progression from NAFLD through to NASH, fibrosis, and cirrhosis is both unpredictable and heterogenous [183]. Many patients are likely to not progress at all, however, due to the large population-at-risk, NAFLD is still a significant and growing cause of cirrhosis, liver-related morbidity/mortality, and HCC [7,184]. There are multiple risk factors readily assessed in routine practice that contribute to this risk of progression, including age > 50 years, degree of steatosis, T2DM, and/or obesity. Interestingly, and unlike what is seen in many other liver conditions, the development of HCC in NAFLD can occur prior to the development of advanced fibrosis/cirrhosis. Further, NAFLD/NASH-related liver disease is growing rapidly and is now the second most common indication for liver transplant in the U.S.A. [10]; this trend is likely to extend globally in the near future. Importantly, the progression from simple steatosis through to significant fibrosis and cirrhosis not only increases the risk of liver-related outcomes; worsening biopsy-proven or non-invasive fibrosis stages also correlate with all-cause [160,185] and non-liver [186,187,188] morbidity and mortality.
3.2. NAFLD—Cardiovascular Outcomes
While NAFLD is associated with various aspects of metabolic dysregulation (including dysglycaemia and atherogenic dyslipidaemia), several studies have also shown that NAFLD is independently associated with subclinical [189] and clinical [186] cardiovascular disease. As previously described, NAFLD is associated with increased insulin resistance [13,28] which is itself associated with cardiovascular disease [190]. However, while an in-depth review is outside the scope of this article, there are additional potential mechanisms associated with NAFLD, including systemic inflammation and gut dysbiosis or endotoxemia. Systemic inflammation in NAFLD is associated with cardiovascular disease due to consequent endothelial dysfunction and enhanced atheromatous plaque formation [191,192]. The altered lipid metabolism inherent to NAFLD (characterised by increased VLDL and small dense LDL with reduced HDL) is additionally pro-atherogenic [191,192]. Finally, intestinal dysbiosis is a potential pathogenic feature of NAFLD [112,113] as well as cardiovascular disease [191,192], possibly due to a combination of LPS-associated inflammatory effects alongside pathogenic microbiotal metabolites such as trimethylamine-N-oxide [193,194].
3.3. NAFLD—Diabetes Mellitus and Chronic Kidney Disease
There is a bi-directional relationship between NAFLD and T2DM [195]. The prevalence of NAFLD in T2DM is as high as 87.1% in some series [104]—however, in patients with NAFLD and without T2DM, rates of insulin resistance and the subsequent development of T2DM are elevated compared with healthy controls. Similarly, patients with NAFLD are at markedly increased risk of developing incident chronic kidney disease (CKD) when compared with healthy controls [187,196]. It is likely that similar pathophysiologic processes associated with CVD in NAFLD drive the association with CKD, including features of the metabolic syndrome and intestinal dysbiosis [196].
3.4. NAFLD—Obstructive Sleep Apnoea
There is a possible bi-directional relationship between NAFLD and OSA. While OSA is associated with obesity [197] (which is, in turn, associated with NAFLD), the prevalence of hepatic steatosis in patients with OSA may be as high as 75% [198]. Further, OSA may also be associated with high rates of non-invasively assessed liver fibrosis [198]. While many of these findings are primarily driven by BMI, OSA remains independently associated with NAFLD, and it is reasonable to recommend that patients with NAFLD at risk of OSA be appropriately screened and referred.
3.5. Impact of Steatosis on Other Liver Diseases
NAFLD, by definition, cannot co-occur with other liver diseases. In spite of this, however, the interplay between simple steatosis or histopathological features of NASH and other liver diseases is an area of active research. Some of this work is being performed using the new MAFLD nomenclature. Recent work has shown that patients with MAFLD and chronic hepatitis C may have more significant fibrosis and increased histological inflammation than those with chronic hepatitis C without MAFLD [199]. In CHB, one study has shown an association between CHB-MAFLD having reduced transplant-free or HCC-free survival than CHB alone [200], and another has shown that hepatic steatosis improves rates of hepatitis B seroclearance in treatment naïve patients—but still leads to worsening fibrosis stage [201]. While the interplay between steatosis and other liver diseases is a topic of further research, these preliminary data support the role of assessing for hepatic steatosis in patients with chronic viral hepatitis and, by extension, with other liver diseases, and to ensure adequate follow-up of MAFLD subjects irrespective of other liver disease diagnoses.
4. Treatment Options
4.1. Lifestyle Modification—Diet
There are a variety of lifestyle options with which to treat NAFLD—diet and exercise [2,4], coffee consumption [85], and the removal of hepatotoxic drugs (including tobacco [202] and alcohol [203]) are all likely to improve hepatic steatosis/fibrosis. Both weight loss [204,205] and improved dietary composition [204,206] (independent of change in energy intake) can improve steatosis. Weight loss of 7–10% bodyweight is recommended in both European [4] and American [2] guidelines for the management of NAFLD, as it is associated with reductions in histological NASH as well as the potential resolution of steatosis. These guidelines are well supported. A landmark paired biopsy study of hypocaloric diet and exercise showed marked improvements in histological NASH and NAFL activity correlating to the degree of bodyweight lost [205].
Determining whether specific dietary patterns should be recommended has also been a focus of research. When considering weight loss as a specific treatment goal, small studies have shown very low calorie diets (VLCDs) are effective for individuals with NAFLD. One has shown improvement in LSM, LFTs, and cardiovascular risk profile without adverse events [207]. Another small study in patients with T2DM showed improvement in diabetic parameters and hepatic fat content [208]. Dietary macronutrient composition and meal timing has also been examined. One recent randomised trial of a calorie-reduced low-carbohydrate high fat (LCHF) diet vs. intermittent fasting vs. standard of care showed that both dietary interventions improved steatosis and led to reductions in bodyweight [209], though patient satisfaction was better with the intermittent fasting. While hypocaloric LCHF diets may lead to more rapid reductions in intrahepatic lipid content than low fat diets, this is not sustained over the longer term [210,211]. Isocaloric LCHF diets may also reduce intrahepatic lipid content [212], though longer-term follow-up is required. The Mediterranean diet (high in antioxidants, fibre, and UFAs) has also been examined in several trials with conflicting results. Two early studies [206,213] provided support for improvements in ALT, hepatic steatosis, and insulin sensitivity. However, a recent randomised controlled trial showed no clinically significant differences between the Mediterranean diet and a low-fat diet [214]. Despite this, given the Mediterranean diet is shown to improve cardiovascular outcomes [215,216], recommendations to follow a Mediterranean-like diet in NAFLD remain reasonable.
Coffee intake is recognised as protective in NAFLD, with a recent systematic review showing reduced rates of hepatic fibrosis in individuals with NAFLD who drink coffee [217]. Its role in protecting against simple steatosis is less clear, though a recent dose–response meta-analysis provides some support for high coffee intake (>3 cups per day) being protective against NAFLD development [218]. However, with significant heterogeneity in trials amongst coffee dosing, form (instant, espresso, filter) and caffeine content, definitive conclusions are limited. While recommendations to increase coffee intake are often made [4] (to reduce the risk of developing fibrosis or HCC), further prospective studies in NAFLD are needed to optimise dose and type, and to ensure efficacy.
4.2. Lifestyle Modification—Exercise
Exercise is beneficial for the treatment of NAFLD. In addition to known benefits of exercise in terms of improving insulin resistance [219], dyslipidaemia [220], and hypertension [221], a 2017 review by Hashida et al. [97] highlighted the benefits of both aerobic and anaerobic exercise in improving hepatic steatosis. Both observational and randomised controlled trials almost universally showed improvement in hepatic steatosis, BMI, and ALT levels. Some also showed a modest improvement in hepatic steatosis of 2.65% even without a significant weight change [97]. In practical terms, the median effective exercise duration seen in the Hashida et al. [97] systematic review was 40 min three times per week at 4.8 metabolic equivalents (METs) for aerobic exercise, and a similar duration but lower intensity 45 min three times per week at 3.5 METs for resistance exercise, both for a minimum of 12 weeks. However, the median BMI in these studies was approximately 30 kg/m2 and the median age of participants was approximately 49 years. Another recent analysis provides some support to the notion that continuous higher intensity training is more effective than other forms of exercise [222], though it remains unknown how practical intense or long duration exercise would be for those with class III obesity and/or in the elderly.
4.3. Lifestyle Modification—Tobacco and Alcohol
Tobacco smoking—passive and active—contributes to the development of NAFLD [202]. Similarly, active smoking or a smoking history of ≥10 pack years is associated with an increased risk of fibrosis in NAFLD [223]. However, no prospective trials on smoking cessation or on the use of nicotine replacement therapy have been instituted; while smoking cessation is strongly recommended to reduce all-cause and cardiovascular mortality [224], its role in improving liver-specific outcomes is less certain.
Understanding the role of alcohol harm minimisation or cessation in NAFLD is challenging due to the diagnosis of NAFLD mandating no or low-level alcohol intake at baseline. However, some preliminary work has been performed. A recent systematic review notes that even moderate or low-level drinking in NAFLD may worsen liver related outcomes [225]. However, other data suggest that moderate alcohol intake may reduce the risk of CVD-related hospitalisation in NAFLD (with no impact on mortality) [226]. Future trials evaluating the role of alcohol cessation in NAFLD will help to answer these questions.
4.4. Supplementation and Pharmacotherapy
Various therapeutic options have been trialled in NAFLD and NASH to ameliorate disease and reduce histologic severity or cause fibrosis regression. Results to date, however, have been largely disappointing, though multiple trials in late-stage clinical development are on-going (Table 3). Vitamin E (as alpha-tocopherol) was one of the first therapeutic agents to show any potential benefit in NAFLD/NASH—both AASLD and EASL guidelines tentatively recommend its use in biopsy-proven NASH in non-diabetic patients [2,4]. Vitamin E has multiple effects, including as an antioxidant, anti-inflammatory, and apoptosis mediator. Multiple studies have been performed showing some improvements in surrogates of liver damage, steatosis, hepatocellular ballooning, and fibrosis. However, in diabetic patients, the benefits have not been as clearly demonstrated. While one small study showed histological improvement with vitamin E combined with pioglitazone for NAFLD patients with comorbid T2DM, vitamin E alone did not improve any histological markers of NAFLD/NASH apart from steatosis itself [227]. Additionally, vitamin E is not necessarily risk free. A Cochrane review has suggested that there is a trend towards vitamin E supplementation increasing all-cause mortality [228]. While a subsequent analysis of blood tocopherol levels (as a marker of overall intake) has shown no link or slightly reduced risk of mortality [229], given these conflicting results and potential confounding co-occurring phytochemicals when evaluating dietary vitamin E intake, in our experience, many physicians prescribe vitamin E cautiously.
Given that glucose, lipid metabolism, and inflammation have all been implicated in the pathogenesis of NAFLD/NASH, various therapies modulating these pathways have been evaluated. Obeticholic acid (OCA) is one such example. OCA, a Farnesoid X receptor (FXR) agonist and semi-synthetic bile acid analogue, has previously been shown to have anti-inflammatory and anti-fibrotic effects [230]. Following encouraging phase 2 trial data [231], two large randomised controlled trials evaluating the efficacy and safety of OCA in non-cirrhotic NAFLD/NASH have been performed [232,233]. Both showed greater improvements in fibrosis stage with OCA compared with placebo, though side-effects were common, including pruritus and worsening dyslipidaemia. In light of this finding and the need to refer OCA patients to primary care for lipid-lowering therapy in the 2015 RCT [232], a study comparing OCA plus low-dose statin showed that the OCA-induced dyslipidaemia could be successfully ameliorated. Longer term studies evaluating the risk/benefit of combination therapy on clinical liver and cardiovascular outcomes would be useful, however, and multiple OCA trials are on-going (Table 3).
Due to the metabolic dysregulation and shared pathways linking T2DM and NAFLD/NASH, T2DM pharmaceuticals have also been tried, including pioglitazone and metformin. Pioglitazone, a thiazolidinedione, has been trialled both alone and in combination, for NAFLD/NASH [234,235,236,237]. Thiazolidinediones stimulate PPAR-γ, increasing GLUT1 and GLUT4 levels while concurrently lowering FFAs [238], improving insulin sensitivity, and decreasing hepatic gluconeogenesis, potentially improving histopathological features of NASH [235,237]. Pioglitazone’s benefits have been seen in both a non-diabetic cohort [235] and a T2DM cohort [234,237]. However, in the landmark PIVENS trial which compared pioglitazone, vitamin E, and placebo, pioglitazone showed a numerical improvement in histological response which did not reach the a priori significance level of p < 0.025 [236]. Further, concerns around the long-term effects of pioglitazone (weight gain, fracture risk, exacerbating congestive cardiac failure) have likely limited its uptake and use [239]. Given this, newer pan-PPAR agonists such as Lanifibranor are currently being studied (Table 3) but are not yet recommended or approved for routine use. Metformin, a biguanide, has a multitude of incompletely understood actions which sum to reduced hepatic gluconeogenesis and improved peripheral tissue insulin sensitivity [240]. While small trials of metformin have shown some promising results in improving LFTs and BMI, histological findings have been consistently negative [241]. Given these data, pioglitazone has only limited endorsement in the AASLD and EASL NAFLD guidelines, specifically for biopsy proven NASH, and metformin is not currently recommended.
Newer studies have evaluated more modern T2DM therapies such as sodium–glucose co-transporter 2 (SGLT-2) inhibitors and glucagon-like peptide-1 receptor agonists (GLP-1RAs). SGLT-2 inhibitors function to increase glucosuria by impairing the nephron’s ability to resorb glucose lost through glomerular filtration [242]. Further, they may promote ketogenesis, cause natriuresis, and modulate the renin–aldosterone–angiotensin system; through these, they have anti-obesity, anti-atherosclerotic, and hepato-protective effects in vitro [242]. These findings have been confirmed in patients with T2DM and NAFLD/NASH—small studies have shown the administration of SGLT-2 inhibitors improves ALT, hepatic steatosis, and possibly, fibrosis [243]. GLP-1RAs have also been primarily studied in individuals with T2DM. Early clinical work has shown improvement in steatosis, hepatocyte ballooning, and other histological features of NASH, without significant changes in fibrosis [244]. Further, GLP-1RAs are often used off-label to promote weight loss, even in individuals without T2DM [245,246]. However, similar to SGLT-2 inhibitors, minimal work on NAFLD patients without T2DM has been performed, and recommending these medications for the primary purpose of treating NAFLD/NASH is premature—though trials are on-going (Table 4).
Table 4.
Current late phase pharmaceutical trials in NAFLD (retrieved from ClinicalTrials.gov, accessed on 11 January 2023).
| Trial Name | Trial Therapies | Recruiting | ClinicalTrials.gov ID |
|---|---|---|---|
| An Investigator Initiated Prospective, Four Arms Randomized Comparative Study of Efficacy and Safety of Saroglitazar, Vitamin E and Life Style Modification in Patients With Nonalcoholic Fatty Liver Disease (NAFLD)/Non-alcoholic Steatohepatitis (NASH) |
|
Yes | NCT04193982 |
| Lanifibranor in Patients With Type 2 Diabetes & Nonalcoholic Fatty Liver Disease |
|
Yes | NCT03459079 |
| A Phase 3 Study to Evaluate the Safety and Biomarkers of Resmetirom (MGL-3196) in Non Alcoholic Fatty Liver Disease (NAFLD) Patients (MAESTRO-NAFLD1) |
|
No | NCT04197479 |
| A Phase 3 Study to Evaluate Safety and Biomarkers of Resmetirom (MGL-3196) in Patients With Non-alcoholic Fatty Liver Disease (NAFLD), MAESTRO-NAFLD-Open-Label-Extension (MAESTRO-NAFLD-OLE) |
|
Yes | NCT04951219 |
| Randomized Global Phase 3 Study to Evaluate the Impact on NASH With Fibrosis of Obeticholic Acid Treatment (REGENERATE) |
|
No | NCT02548351 |
| Study Evaluating the Efficacy and Safety of Obeticholic Acid in Subjects With Compensated Cirrhosis Due to Nonalcoholic Steatohepatitis (REVERSE) |
|
No | NCT03439254 |
| Comparative Study Between Obeticholic Acid Versus Vitamin E in Patients With Non-alcoholic Steatohepatitis |
|
No | NCT05573204 |
| Research Study on Whether Semaglutide Works in People With Non-alcoholic Steatohepatitis (NASH) (ESSENCE) |
|
Yes | NCT04822181 |
| Study of Semaglutide for Non-Alcoholic Fatty Liver Disease (NAFLD), a Metabolic Syndrome With Insulin Resistance, Increased Hepatic Lipids, and Increased Cardiovascular Disease Risk (The SLIM LIVER Study) |
|
Yes | NCT04216589 |
| Researching an Effect of GLP-1 Agonist on Liver STeatosis (REALIST) (REALIST) |
|
No | NCT03648554 |
| A Study of Tirzepatide (LY3298176) in Participants With Nonalcoholic Steatohepatitis (NASH) (SYNERGY-NASH) |
|
Yes | NCT04166773 |
| Dapagliflozin Efficacy and Action in NASH (DEAN) |
|
Yes | NCT03723252 |
| Dapagliflozin in Type 2 Diabetes Mellitus Patients (T2DM) With Nonalcoholic Fatty Liver Disease (NAFLD) |
|
Yes | NCT05459701 |
| A Single Center, Randomized, Open Label, Parallel Group, Phase 3 Study to Evaluate the Efficacy of Dapagliflozin in Subjects With Nonalcoholic Fatty Liver Disease |
|
Yes | NCT05308160 |
| Effect of Empagliflozin on Liver Fat in Non-diabetic Patients |
|
No | NCT04642261 |
| Efficacy and Safety of Dapagliflozin in Patients With Non-alcoholic Steatohepatitis |
|
Yes | NCT05254626 |
| Canagliflozin on Liver Inflammation Damage in Type 2 Diabetes Patients With Nonalcoholic Fatty Liver Disease |
|
No | NCT05422092 |
| Effect of Oral Anti-diabetic Medication on Liver Fat in Subjects With Type II Diabetes and Non-alcoholic Fatty Liver |
|
Yes | NCT04976283 |
| Low-Dose Pioglitazone in Patients With NASH (AIM 2) |
|
Yes | NCT04501406 |
Tirzepatide is a dual-action GLP-1RA and glucose-dependent insulinotropic polypeptide recently trialled in both T2DM [247] and non-T2DM obese patients [248]. In the first trial, improvements in T2DM control were significantly improved compared with semaglutide (a GLP-1RA) with concurrent improvements in transaminases, fasting glucose, insulin sensitivity, lipid profile, and bodyweight [247]. Similar improvements were seen in the obese non-diabetic group [248], and a substudy of a T2DM tirzepatide trial (SURPASS-3 MRI) [249] showed improvements in liver fat content with tirzepatide compared with insulin. However, no histological assessments for improvement/resolution of NASH or fibrosis have been performed to date. However, given these improvements in metabolic profile and steatosis, a trial of tirzepatide in NAFLD/NASH is on-going (Table 3).
Statins (HMG-CoA reductase inhibitors), while routinely used in the management of cardiovascular disease [250], have been less popular in their use in NAFLD—even in patients with a guideline-supported indication for statin therapy [251] due to potential concerns of hepatotoxicity. However, multiple studies have shown that initiating statin therapy is safe in patients with elevated transaminases, NAFLD/NASH, and/or other underlying liver diseases [252,253]. As such, various studies evaluating the role of statin therapies in improving outcomes in NAFLD/NASH have been performed with mixed results. While early post-hoc and case-controlled analyses have shown improvements in LFTs and radiographic markers of steatosis in statin users compared with non-users, very few reported histopathological results [252]. More recently, a large, nested case-controlled study based on the FLI and BARD scores suggested that statins may reduce the rate of NAFLD development, as well as potentially protect against fibrosis [254]. Further work regarding the protective role of statins on NAFLD, NASH and/or fibrosis is, therefore, needed. There are other potential benefits of statins in NAFLD also. Preliminary work suggests a possible reduction in the risk of developing HCC [255], as well as potentially ameliorating some of the complications of cirrhosis [256]. These findings require confirmation via additional efficacy and safety studies of statin therapy/chemoprophylaxis.
Aspirin has also been evaluated in the management of NAFLD, both regarding the presence of NASH and in terms of preventing cirrhosis and HCC. A prospective cohort study has shown that aspirin users had a time-dependent reduced risk of biopsy-proven NASH and reduced rates of fibrosis progression [257]. Other cross-sectional work supports this—one study showed an inverse relationship between aspirin use and NAFLD prevalence, with results most marked in the elderly and males [258]. Aspirin has also been evaluated for prevention of HCC in CLD—a recent meta-analysis of observational studies confirmed aspirin use conferred a relative risk reduction of 39% [259]. This only included one study of aspirin in confirmed NAFLD, however. As such the role of aspirin as a therapeutic strategy in NAFLD/NASH has not been evaluated in the setting of a randomised-controlled trial and consequently is not a component of NAFLD management guidelines.
4.5. Future Directions in NAFLD
As the link between hepatic steatosis and metabolic dysregulation is further crystallised, the need to prospectively evaluate options for improving liver and cardiovascular outcomes in NAFLD (e.g., aspirin and/or statin therapy as primary prevention) should be considered. Further nuanced risk stratification tools and biomarkers will be important to develop a priori, so that scarce healthcare resources can be directed appropriately to those most at risk from this condition that affects upwards of 30% of the Western adult population. Targeting the most appropriate therapies to those most likely to benefit will be critical, especially as many off-label therapies being studied (e.g., GLP-1 agonists) are expensive. Understanding the implications of co-occurring metabolic disease, hepatic steatosis, and other liver diseases (particularly alcohol-related liver disease) will be important to prognosticate and risk-stratify. Finally, country- and health-service-specific prospective evaluations of different models of care will be important so that each region can cost-effectively and proactively manage this public health threat.
5. Conclusions
NAFLD is a large and growing cause of liver-related and cardiovascular mortality and morbidity globally. The global burden of disease continues to grow—new risk assessment tools and pathways to manage NAFLD as a component of dysregulated metabolic processes will be vital in combatting this escalating major public health challenge. While there is a large pipeline of repurposed medications to improve the health of patients with NAFLD, identifying those most likely to benefit—and improving lifestyle factors to reduce the incidence of NAFLD—will be critical in reducing the burden of cardiovascular and chronic liver disease in the future.
Author Contributions
Conceptualization, D.C.-C., S.K.R.; writing—original draft preparation, D.C.-C.; writing—review and editing, D.C.-C., S.K.R., W.K., A.M., J.S.L., A.H. All authors have read and agreed to the published version of the manuscript.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors have no conflict of interest to declare.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Cheemerla S., Balakrishnan M. Global Epidemiology of Chronic Liver Disease. Clin. Liver Dis. 2021;17:365–370. doi: 10.1002/cld.1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chalasani N., Younossi Z., Lavine J.E., Charlton M., Cusi K., Rinella M., Harrison S.A., Brunt E.M., Sanyal A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–357. doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 3.Younossi Z.M., Stepanova M., Younossi Y., Golabi P., Mishra A., Rafiq N., Henry L. Epidemiology of chronic liver diseases in the USA in the past three decades. Gut. 2020;69:564–568. doi: 10.1136/gutjnl-2019-318813. [DOI] [PubMed] [Google Scholar]
- 4.European Association for the Study of the Liver (EASL) European Association for the Study of Diabetes (EASD) European Association for the Study of Obesity (EASO) EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 2016;64:1388–1402. doi: 10.1016/j.jhep.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 5.Schaffner F., Thaler H. Nonalcoholic fatty liver disease. Prog. Liver Dis. 1986;8:283–298. [PubMed] [Google Scholar]
- 6.Le M.H., Yeo Y.H., Li X., Li J., Zou B., Wu Y., Ye Q., Huang D.Q., Zhao C., Zhang J., et al. 2019 Global NAFLD Prevalence: A Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2021;20:2809–2817.e28. doi: 10.1016/j.cgh.2021.12.002. [DOI] [PubMed] [Google Scholar]
- 7.Younossi Z.M., Koenig A.B., Abdelatif D., Fazel Y., Henry L., Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 8.Estes C., Anstee Q.M., Arias-Loste M.T., Bantel H., Bellentani S., Caballeria J., Colombo M., Craxi A., Crespo J., Day C.P., et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J. Hepatol. 2018;69:896–904. doi: 10.1016/j.jhep.2018.05.036. [DOI] [PubMed] [Google Scholar]
- 9.Estes C., Razavi H., Loomba R., Younossi Z., Sanyal A.J. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67:123–133. doi: 10.1002/hep.29466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Younossi Z.M., Stepanova M., Ong J., Trimble G., AlQahtani S., Younossi I., Ahmed A., Racila A., Henry L. Nonalcoholic Steatohepatitis Is the Most Rapidly Increasing Indication for Liver Transplantation in the United States. Clin. Gastroenterol. Hepatol. 2021;19:580–589.e585. doi: 10.1016/j.cgh.2020.05.064. [DOI] [PubMed] [Google Scholar]
- 11.Neuschwander-Tetri B.A., Caldwell S.H. Nonalcoholic steatohepatitis: Summary of an AASLD Single Topic Conference. Hepatology. 2003;37:1202–1219. doi: 10.1053/jhep.2003.50193. [DOI] [PubMed] [Google Scholar]
- 12.Cortez-Pinto H., Camilo M.E., Baptista A., De Oliveira A.G., De Moura M.C. Non-alcoholic fatty liver: Another feature of the metabolic syndrome? Clin. Nutr. 1999;18:353–358. doi: 10.1016/S0261-5614(99)80015-6. [DOI] [PubMed] [Google Scholar]
- 13.Marchesini G., Brizi M., Morselli-Labate A.M., Bianchi G., Bugianesi E., McCullough A.J., Forlani G., Melchionda N. Association of nonalcoholic fatty liver disease with insulin resistance. Am. J. Med. 1999;107:450–455. doi: 10.1016/S0002-9343(99)00271-5. [DOI] [PubMed] [Google Scholar]
- 14.Leandro G., Mangia A., Hui J., Fabris P., Rubbia-Brandt L., Colloredo G., Adinolfi L.E., Asselah T., Jonsson J.R., Smedile A., et al. Relationship between steatosis, inflammation, and fibrosis in chronic hepatitis C: A meta-analysis of individual patient data. Gastroenterology. 2006;130:1636–1642. doi: 10.1053/j.gastro.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 15.Loria P., Lonardo A., Carulli N. Should nonalcoholic fatty liver disease be renamed? Dig. Dis. 2005;23:72–82. doi: 10.1159/000084728. [DOI] [PubMed] [Google Scholar]
- 16.Ratziu V., Bellentani S., Cortez-Pinto H., Day C., Marchesini G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J. Hepatol. 2010;53:372–384. doi: 10.1016/j.jhep.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 17.Bellentani S., Tiribelli C. Is it time to change NAFLD and NASH nomenclature? Lancet Gastroenterol. Hepatol. 2017;2:547–548. doi: 10.1016/S2468-1253(17)30146-2. [DOI] [PubMed] [Google Scholar]
- 18.Eslam M., Newsome P.N., Sarin S.K., Anstee Q.M., Targher G., Romero-Gomez M., Zelber-Sagi S., Wai-Sun Wong V., Dufour J.F., Schattenberg J.M., et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 2020;73:202–209. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 19.Eslam M., Sanyal A.J., George J., International Consensus P. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology. 2020;158:1999–2014.e1. doi: 10.1053/j.gastro.2019.11.312. [DOI] [PubMed] [Google Scholar]
- 20.Younossi Z.M., Rinella M.E., Sanyal A.J., Harrison S.A., Brunt E.M., Goodman Z., Cohen D.E., Loomba R. From NAFLD to MAFLD: Implications of a Premature Change in Terminology. Hepatology. 2021;73:1194–1198. doi: 10.1002/hep.31420. [DOI] [PubMed] [Google Scholar]
- 21.Tilg H., Moschen A.R. Evolution of inflammation in nonalcoholic fatty liver disease: The multiple parallel hits hypothesis. Hepatology. 2010;52:1836–1846. doi: 10.1002/hep.24001. [DOI] [PubMed] [Google Scholar]
- 22.Takaki A., Kawai D., Yamamoto K. Multiple hits, including oxidative stress, as pathogenesis and treatment target in non-alcoholic steatohepatitis (NASH) Int. J. Mol. Sci. 2013;14:20704–20728. doi: 10.3390/ijms141020704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pafili K., Roden M. Nonalcoholic fatty liver disease (NAFLD) from pathogenesis to treatment concepts in humans. Mol. Metab. 2021;50:101122. doi: 10.1016/j.molmet.2020.101122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Powell E.E., Wong V.W.-S., Rinella M. Non-alcoholic fatty liver disease. Lancet. 2021;397:2212–2224. doi: 10.1016/S0140-6736(20)32511-3. [DOI] [PubMed] [Google Scholar]
- 25.Chung K.W., Cho Y.E., Kim S.J., Hwang S. Immune-related pathogenesis and therapeutic strategies of nonalcoholic steatohepatitis. Arch. Pharm. Res. 2022;45:229–244. doi: 10.1007/s12272-022-01379-1. [DOI] [PubMed] [Google Scholar]
- 26.Alves-Bezerra M., Cohen D.E. Triglyceride Metabolism in the Liver. Compr. Physiol. 2017;8:1–8. doi: 10.1002/cphy.c170012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mashek D.G. Hepatic lipid droplets: A balancing act between energy storage and metabolic dysfunction in NAFLD. Mol. Metab. 2021;50:101115. doi: 10.1016/j.molmet.2020.101115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith G.I., Shankaran M., Yoshino M., Schweitzer G.G., Chondronikola M., Beals J.W., Okunade A.L., Patterson B.W., Nyangau E., Field T., et al. Insulin resistance drives hepatic de novo lipogenesis in nonalcoholic fatty liver disease. J. Clin. Investig. 2020;130:1453–1460. doi: 10.1172/JCI134165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Donnelly K.L., Smith C.I., Schwarzenberg S.J., Jessurun J., Boldt M.D., Parks E.J. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J. Clin. Investig. 2005;115:1343–1351. doi: 10.1172/JCI23621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lambert J.E., Ramos-Roman M.A., Browning J.D., Parks E.J. Increased de novo lipogenesis is a distinct characteristic of individuals with nonalcoholic fatty liver disease. Gastroenterology. 2014;146:726–735. doi: 10.1053/j.gastro.2013.11.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Luukkonen P.K., Qadri S., Ahlholm N., Porthan K., Mannisto V., Sammalkorpi H., Penttila A.K., Hakkarainen A., Lehtimaki T.E., Gaggini M., et al. Distinct contributions of metabolic dysfunction and genetic risk factors in the pathogenesis of non-alcoholic fatty liver disease. J. Hepatol. 2022;76:526–535. doi: 10.1016/j.jhep.2021.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lomonaco R., Ortiz-Lopez C., Orsak B., Webb A., Hardies J., Darland C., Finch J., Gastaldelli A., Harrison S., Tio F., et al. Effect of adipose tissue insulin resistance on metabolic parameters and liver histology in obese patients with nonalcoholic fatty liver disease. Hepatology. 2012;55:1389–1397. doi: 10.1002/hep.25539. [DOI] [PubMed] [Google Scholar]
- 33.Saponaro C., Sabatini S., Gaggini M., Carli F., Rosso C., Positano V., Armandi A., Caviglia G.P., Faletti R., Bugianesi E., et al. Adipose tissue dysfunction and visceral fat are associated with hepatic insulin resistance and severity of NASH even in lean individuals. Liver Int. 2022;42:2418–2427. doi: 10.1111/liv.15377. [DOI] [PubMed] [Google Scholar]
- 34.Mocciaro G., Gastaldelli A. Obesity-Related Insulin Resistance: The Central Role of Adipose Tissue Dysfunction. In: Eckel J., Clément K., editors. From Obesity to Diabetes. Springer International Publishing; Cham, Switzerland: 2022. pp. 145–164. [DOI] [PubMed] [Google Scholar]
- 35.Parker R. The role of adipose tissue in fatty liver diseases. Liver Res. 2018;2:35–42. doi: 10.1016/j.livres.2018.02.002. [DOI] [Google Scholar]
- 36.Ooi G.J., Meikle P.J., Huynh K., Earnest A., Roberts S.K., Kemp W., Parker B.L., Brown W., Burton P., Watt M.J. Hepatic lipidomic remodeling in severe obesity manifests with steatosis and does not evolve with non-alcoholic steatohepatitis. J. Hepatol. 2021;75:524–535. doi: 10.1016/j.jhep.2021.04.013. [DOI] [PubMed] [Google Scholar]
- 37.Cusi K. Role of obesity and lipotoxicity in the development of nonalcoholic steatohepatitis: Pathophysiology and clinical implications. Gastroenterology. 2012;142:711–725.e716. doi: 10.1053/j.gastro.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 38.Guerra S., Mocciaro G., Gastaldelli A. Adipose tissue insulin resistance and lipidome alterations as the characterizing factors of non-alcoholic steatohepatitis. Eur. J. Clin. Investig. 2022;52:e13695. doi: 10.1111/eci.13695. [DOI] [PubMed] [Google Scholar]
- 39.Yki-Jarvinen H. Ceramides: A Cause of Insulin Resistance in Nonalcoholic Fatty Liver Disease in Both Murine Models and Humans. Hepatology. 2020;71:1499–1501. doi: 10.1002/hep.31095. [DOI] [PubMed] [Google Scholar]
- 40.Chen Z., Tian R., She Z., Cai J., Li H. Role of oxidative stress in the pathogenesis of nonalcoholic fatty liver disease. Free Radic. Biol. Med. 2020;152:116–141. doi: 10.1016/j.freeradbiomed.2020.02.025. [DOI] [PubMed] [Google Scholar]
- 41.Karkucinska-Wieckowska A., Simoes I.C.M., Kalinowski P., Lebiedzinska-Arciszewska M., Zieniewicz K., Milkiewicz P., Gorska-Ponikowska M., Pinton P., Malik A.N., Krawczyk M., et al. Mitochondria, oxidative stress and nonalcoholic fatty liver disease: A complex relationship. Eur. J. Clin. Investig. 2022;52:e13622. doi: 10.1111/eci.13622. [DOI] [PubMed] [Google Scholar]
- 42.Goedeke L., Bates J., Vatner D.F., Perry R.J., Wang T., Ramirez R., Li L., Ellis M.W., Zhang D., Wong K.E., et al. Acetyl-CoA Carboxylase Inhibition Reverses NAFLD and Hepatic Insulin Resistance but Promotes Hypertriglyceridemia in Rodents. Hepatology. 2018;68:2197–2211. doi: 10.1002/hep.30097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ross T.T., Crowley C., Kelly K.L., Rinaldi A., Beebe D.A., Lech M.P., Martinez R.V., Carvajal-Gonzalez S., Boucher M., Hirenallur-Shanthappa D., et al. Acetyl-CoA Carboxylase Inhibition Improves Multiple Dimensions of NASH Pathogenesis in Model Systems. Cell Mol. Gastroenterol. Hepatol. 2020;10:829–851. doi: 10.1016/j.jcmgh.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Loomba R., Kayali Z., Noureddin M., Ruane P., Lawitz E.J., Bennett M., Wang L., Harting E., Tarrant J.M., McColgan B.J., et al. GS-0976 Reduces Hepatic Steatosis and Fibrosis Markers in Patients with Nonalcoholic Fatty Liver Disease. Gastroenterology. 2018;155:1463–1473.e6. doi: 10.1053/j.gastro.2018.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Trepo E., Valenti L. Update on NAFLD genetics: From new variants to the clinic. J. Hepatol. 2020;72:1196–1209. doi: 10.1016/j.jhep.2020.02.020. [DOI] [PubMed] [Google Scholar]
- 46.Eslam M., George J. Genetic contributions to NAFLD: Leveraging shared genetics to uncover systems biology. Nat. Rev. Gastroenterol. Hepatol. 2020;17:40–52. doi: 10.1038/s41575-019-0212-0. [DOI] [PubMed] [Google Scholar]
- 47.Sookoian S., Pirola C.J. Genetic predisposition in nonalcoholic fatty liver disease. Clin. Mol. Hepatol. 2017;23:1–12. doi: 10.3350/cmh.2016.0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Romeo S., Kozlitina J., Xing C., Pertsemlidis A., Cox D., Pennacchio L.A., Boerwinkle E., Cohen J.C., Hobbs H.H. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat. Genet. 2008;40:1461–1465. doi: 10.1038/ng.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lonardo A., Lombardini S., Scaglioni F., Carulli L., Ricchi M., Ganazzi D., Adinolfi L.E., Ruggiero G., Carulli N., Loria P. Hepatic steatosis and insulin resistance: Does etiology make a difference? J. Hepatol. 2006;44:190–196. doi: 10.1016/j.jhep.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 50.Welty F.K. Hypobetalipoproteinemia and abetalipoproteinemia: Liver disease and cardiovascular disease. Curr. Opin. Lipidol. 2020;31:49–55. doi: 10.1097/MOL.0000000000000663. [DOI] [PubMed] [Google Scholar]
- 51.Lonardo A., Bellentani S., Argo C.K., Ballestri S., Byrne C.D., Caldwell S.H., Cortez-Pinto H., Grieco A., Machado M.V., Miele L., et al. Epidemiological modifiers of non-alcoholic fatty liver disease: Focus on high-risk groups. Dig. Liver Dis. 2015;47:997–1006. doi: 10.1016/j.dld.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 52.Wehmeyer M.H., Zyriax B.C., Jagemann B., Roth E., Windler E., Schulze Zur Wiesch J., Lohse A.W., Kluwe J. Nonalcoholic fatty liver disease is associated with excessive calorie intake rather than a distinctive dietary pattern. Medicine. 2016;95:e3887. doi: 10.1097/MD.0000000000003887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yki-Jarvinen H., Luukkonen P.K., Hodson L., Moore J.B. Dietary carbohydrates and fats in nonalcoholic fatty liver disease. Nat. Rev. Gastroenterol. Hepatol. 2021;18:770–786. doi: 10.1038/s41575-021-00472-y. [DOI] [PubMed] [Google Scholar]
- 54.Lim J.S., Mietus-Snyder M., Valente A., Schwarz J.M., Lustig R.H. The role of fructose in the pathogenesis of NAFLD and the metabolic syndrome. Nat. Rev. Gastroenterol. Hepatol. 2010;7:251–264. doi: 10.1038/nrgastro.2010.41. [DOI] [PubMed] [Google Scholar]
- 55.Jegatheesan P., De Bandt J.P. Fructose and NAFLD: The Multifaceted Aspects of Fructose Metabolism. Nutrients. 2017;9:230. doi: 10.3390/nu9030230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gentile C.L., Pagliassotti M.J. The role of fatty acids in the development and progression of nonalcoholic fatty liver disease. J. Nutr. Biochem. 2008;19:567–576. doi: 10.1016/j.jnutbio.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Luukkonen P.K., Sadevirta S., Zhou Y., Kayser B., Ali A., Ahonen L., Lallukka S., Pelloux V., Gaggini M., Jian C., et al. Saturated Fat Is More Metabolically Harmful for the Human Liver Than Unsaturated Fat or Simple Sugars. Diabetes Care. 2018;41:1732–1739. doi: 10.2337/dc18-0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Green C.J., Pramfalk C., Charlton C.A., Gunn P.J., Cornfield T., Pavlides M., Karpe F., Hodson L. Hepatic de novo lipogenesis is suppressed and fat oxidation is increased by omega-3 fatty acids at the expense of glucose metabolism. BMJ Open Diabetes Res. Care. 2020;8:e000871. doi: 10.1136/bmjdrc-2019-000871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Makela T.N.K., Tuomainen T.P., Hantunen S., Virtanen J.K. Associations of serum n-3 and n-6 polyunsaturated fatty acids with prevalence and incidence of non-alcoholic fatty liver disease. Am. J. Clin. Nutr. 2022;116:759–770. doi: 10.1093/ajcn/nqac150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zelber-Sagi S., Nitzan-Kaluski D., Goldsmith R., Webb M., Blendis L., Halpern Z., Oren R. Long term nutritional intake and the risk for non-alcoholic fatty liver disease (NAFLD): A population based study. J. Hepatol. 2007;47:711–717. doi: 10.1016/j.jhep.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 61.Chen H., Wang J., Li Z., Lam C.W.K., Xiao Y., Wu Q., Zhang W. Consumption of Sugar-Sweetened Beverages Has a Dose-Dependent Effect on the Risk of Non-Alcoholic Fatty Liver Disease: An Updated Systematic Review and Dose-Response Meta-Analysis. Int. J. Environ. Res. Public Health. 2019;16:2192. doi: 10.3390/ijerph16122192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zelber-Sagi S., Ivancovsky-Wajcman D., Fliss Isakov N., Webb M., Orenstein D., Shibolet O., Kariv R. High red and processed meat consumption is associated with non-alcoholic fatty liver disease and insulin resistance. J. Hepatol. 2018;68:1239–1246. doi: 10.1016/j.jhep.2018.01.015. [DOI] [PubMed] [Google Scholar]
- 63.Li H., Wang X., Ye M., Zhang S., Zhang Q., Meng G., Liu L., Wu H., Gu Y., Wang Y., et al. Does a high intake of green leafy vegetables protect from NAFLD? Evidence from a large population study. Nutr. Metab. Cardiovasc. Dis. 2021;31:1691–1701. doi: 10.1016/j.numecd.2021.01.009. [DOI] [PubMed] [Google Scholar]
- 64.Pickett-Blakely O., Young K., Carr R.M. Micronutrients in Nonalcoholic Fatty Liver Disease Pathogenesis. Cell Mol. Gastroenterol. Hepatol. 2018;6:451–462. doi: 10.1016/j.jcmgh.2018.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Licata A., Zerbo M., Como S., Cammilleri M., Soresi M., Montalto G., Giannitrapani L. The Role of Vitamin Deficiency in Liver Disease: To Supplement or Not Supplement? Nutrients. 2021;13:4014. doi: 10.3390/nu13114014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Podszun M.C., Alawad A.S., Lingala S., Morris N., Huang W.-C.A., Yang S., Schoenfeld M., Rolt A., Ouwerkerk R., Valdez K., et al. Vitamin E treatment in NAFLD patients demonstrates that oxidative stress drives steatosis through upregulation of de-novo lipogenesis. Redox. Biol. 2020;37:101710. doi: 10.1016/j.redox.2020.101710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Raza S., Tewari A., Rajak S., Sinha R.A. Vitamins and non-alcoholic fatty liver disease: A Molecular Insight. Liver Res. 2021;5:62–71. doi: 10.1016/j.livres.2021.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liu Y., Chen H., Wang J., Zhou W., Sun R., Xia M. Association of serum retinoic acid with hepatic steatosis and liver injury in nonalcoholic fatty liver disease. Am. J. Clin. Nutr. 2015;102:130–137. doi: 10.3945/ajcn.114.105155. [DOI] [PubMed] [Google Scholar]
- 69.Saeed A., Dullaart R.P.F., Schreuder T., Blokzijl H., Faber K.N. Disturbed Vitamin A Metabolism in Non-Alcoholic Fatty Liver Disease (NAFLD) Nutrients. 2017;10:29. doi: 10.3390/nu10010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ipsen D.H., Tveden-Nyborg P., Lykkesfeldt J. Does vitamin C deficiency promote fatty liver disease development? Nutrients. 2014;6:5473–5499. doi: 10.3390/nu6125473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhu S., Wang Y., Luo F., Liu J., Xiu L., Qin J., Wang T., Yu N., Wu H., Zou T. The Level of Vitamin D in Children and Adolescents with Nonalcoholic Fatty Liver Disease: A Meta-Analysis. Biomed. Res. Int. 2019;2019:7643542. doi: 10.1155/2019/7643542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nelson J.E., Roth C.L., Wilson L.A., Yates K.P., Aouizerat B., Morgan-Stevenson V., Whalen E., Hoofnagle A., Mason M., Gersuk V., et al. Vitamin D Deficiency Is Associated with Increased Risk of Non-alcoholic Steatohepatitis in Adults with Non-alcoholic Fatty Liver Disease: Possible Role for MAPK and NF-kappaB? Am. J. Gastroenterol. 2016;111:852–863. doi: 10.1038/ajg.2016.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Akdas S., Yazihan N. Serum zinc level and dietary zinc intake status in non-alcoholic fatty liver disease: A meta-analysis and systematic review. Hepatol. Forum. 2020;1:59–67. doi: 10.14744/hf.2020.2020.0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Toshimitsu K., Matsuura B., Ohkubo I., Niiya T., Furukawa S., Hiasa Y., Kawamura M., Ebihara K., Onji M. Dietary habits and nutrient intake in non-alcoholic steatohepatitis. Nutrition. 2007;23:46–52. doi: 10.1016/j.nut.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 75.Cruz K.J.C., de Oliveira A.R.S., Morais J.B.S., Severo J.S., Mendes P.M.V., de Sousa Melo S.R., de Sousa G.S., Marreiro D.D.N. Zinc and Insulin Resistance: Biochemical and Molecular Aspects. Biol. Trace Elem. Res. 2018;186:407–412. doi: 10.1007/s12011-018-1308-z. [DOI] [PubMed] [Google Scholar]
- 76.Fathi M., Alavinejad P., Haidari Z., Amani R. The Effect of Zinc Supplementation on Steatosis Severity and Liver Function Enzymes in Overweight/Obese Patients with Mild to Moderate Non-alcoholic Fatty Liver Following Calorie-Restricted Diet: A Double-Blind, Randomized Placebo-Controlled Trial. Biol. Trace Elem. Res. 2020;197:394–404. doi: 10.1007/s12011-019-02015-8. [DOI] [PubMed] [Google Scholar]
- 77.Polyzos S.A., Kountouras J., Goulas A., Duntas L. Selenium and selenoprotein P in nonalcoholic fatty liver disease. Hormones. 2020;19:61–72. doi: 10.1007/s42000-019-00127-3. [DOI] [PubMed] [Google Scholar]
- 78.Reja M., Makar M., Visaria A., Marino D., Rustgi V. Increased serum selenium levels are associated with reduced risk of advanced liver fibrosis and all-cause mortality in NAFLD patients: National Health and Nutrition Examination Survey (NHANES) III. Ann. Hepatol. 2020;19:635–640. doi: 10.1016/j.aohep.2020.07.006. [DOI] [PubMed] [Google Scholar]
- 79.Aigner E., Strasser M., Haufe H., Sonnweber T., Hohla F., Stadlmayr A., Solioz M., Tilg H., Patsch W., Weiss G., et al. A role for low hepatic copper concentrations in nonalcoholic Fatty liver disease. Am. J. Gastroenterol. 2010;105:1978–1985. doi: 10.1038/ajg.2010.170. [DOI] [PubMed] [Google Scholar]
- 80.Kowdley K.V., Belt P., Wilson L.A., Yeh M.M., Neuschwander-Tetri B.A., Chalasani N., Sanyal A.J., Nelson J.E., Network N.C.R. Serum ferritin is an independent predictor of histologic severity and advanced fibrosis in patients with nonalcoholic fatty liver disease. Hepatology. 2012;55:77–85. doi: 10.1002/hep.24706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ryan J.D., Armitage A.E., Cobbold J.F., Banerjee R., Borsani O., Dongiovanni P., Neubauer S., Morovat R., Wang L.M., Pasricha S.R., et al. Hepatic iron is the major determinant of serum ferritin in NAFLD patients. Liver Int. 2018;38:164–173. doi: 10.1111/liv.13513. [DOI] [PubMed] [Google Scholar]
- 82.MacDonald G.A., Bridle K.R., Ward P.J., Walker N.I., Houglum K., George D.K., Smith J.L., Powell L.W., Crawford D.H., Ramm G.A. Lipid peroxidation in hepatic steatosis in humans is associated with hepatic fibrosis and occurs predominately in acinar zone 3. J. Gastroenterol. Hepatol. 2001;16:599–606. doi: 10.1046/j.1440-1746.2001.02445.x. [DOI] [PubMed] [Google Scholar]
- 83.Grosso G., Micek A., Godos J., Sciacca S., Pajak A., Martinez-Gonzalez M.A., Giovannucci E.L., Galvano F. Coffee consumption and risk of all-cause, cardiovascular, and cancer mortality in smokers and non-smokers: A dose-response meta-analysis. Eur. J. Epidemiol. 2016;31:1191–1205. doi: 10.1007/s10654-016-0202-2. [DOI] [PubMed] [Google Scholar]
- 84.Kim Y., Je Y., Giovannucci E. Coffee consumption and all-cause and cause-specific mortality: A meta-analysis by potential modifiers. Eur. J. Epidemiol. 2019;34:731–752. doi: 10.1007/s10654-019-00524-3. [DOI] [PubMed] [Google Scholar]
- 85.Hodge A., Lim S., Goh E., Wong O., Marsh P., Knight V., Sievert W., de Courten B. Coffee Intake Is Associated with a Lower Liver Stiffness in Patients with Non-Alcoholic Fatty Liver Disease, Hepatitis C, and Hepatitis B. Nutrients. 2017;9:56. doi: 10.3390/nu9010056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Saab S., Mallam D., Cox G.A., 2nd, Tong M.J. Impact of coffee on liver diseases: A systematic review. Liver Int. 2014;34:495–504. doi: 10.1111/liv.12304. [DOI] [PubMed] [Google Scholar]
- 87.Kennedy O.J., Roderick P., Buchanan R., Fallowfield J.A., Hayes P.C., Parkes J. Coffee, including caffeinated and decaffeinated coffee, and the risk of hepatocellular carcinoma: A systematic review and dose-response meta-analysis. BMJ Open. 2017;7:e013739. doi: 10.1136/bmjopen-2016-013739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Morisco F., Lembo V., Mazzone G., Camera S., Caporaso N. Coffee and liver health. J. Clin. Gastroenterol. 2014;48((Suppl. 1)):S87–S90. doi: 10.1097/MCG.0000000000000240. [DOI] [PubMed] [Google Scholar]
- 89.Brandt A., Nier A., Jin C.J., Baumann A., Jung F., Ribas V., Garcia-Ruiz C., Fernandez-Checa J.C., Bergheim I. Consumption of decaffeinated coffee protects against the development of early non-alcoholic steatohepatitis: Role of intestinal barrier function. Redox. Biol. 2019;21:101092. doi: 10.1016/j.redox.2018.101092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kennedy O.J., Fallowfield J.A., Poole R., Hayes P.C., Parkes J., Roderick P.J. All coffee types decrease the risk of adverse clinical outcomes in chronic liver disease: A UK Biobank study. BMC Public Health. 2021;21:970. doi: 10.1186/s12889-021-10991-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Shen H., Rodriguez A.C., Shiani A., Lipka S., Shahzad G., Kumar A., Mustacchia P. Association between caffeine consumption and nonalcoholic fatty liver disease: A systemic review and meta-analysis. Ther. Adv. Gastroenterol. 2016;9:113–120. doi: 10.1177/1756283X15593700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hallsworth K., Thoma C., Moore S., Ploetz T., Anstee Q.M., Taylor R., Day C.P., Trenell M.I. Non-alcoholic fatty liver disease is associated with higher levels of objectively measured sedentary behaviour and lower levels of physical activity than matched healthy controls. Frontline Gastroenterol. 2015;6:44–51. doi: 10.1136/flgastro-2014-100432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zelber-Sagi S., Nitzan-Kaluski D., Goldsmith R., Webb M., Zvibel I., Goldiner I., Blendis L., Halpern Z., Oren R. Role of leisure-time physical activity in nonalcoholic fatty liver disease: A population-based study. Hepatology. 2008;48:1791–1798. doi: 10.1002/hep.22525. [DOI] [PubMed] [Google Scholar]
- 94.Bowden Davies K.A., Sprung V.S., Norman J.A., Thompson A., Mitchell K.L., Harrold J.O.A., Finlayson G., Gibbons C., Wilding J.P.H., Kemp G.J., et al. Physical Activity and Sedentary Time: Association with Metabolic Health and Liver Fat. Med. Sci. Sport. Exerc. 2019;51:1169–1177. doi: 10.1249/MSS.0000000000001901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kwak M.S., Kim D., Chung G.E., Kim W., Kim J.S. The preventive effect of sustained physical activity on incident nonalcoholic fatty liver disease. Liver Int. 2017;37:919–926. doi: 10.1111/liv.13332. [DOI] [PubMed] [Google Scholar]
- 96.Bowden Davies K.A., Sprung V.S., Norman J.A., Thompson A., Mitchell K.L., Halford J.C.G., Harrold J.A., Wilding J.P.H., Kemp G.J., Cuthbertson D.J. Short-term decreased physical activity with increased sedentary behaviour causes metabolic derangements and altered body composition: Effects in individuals with and without a first-degree relative with type 2 diabetes. Diabetologia. 2018;61:1282–1294. doi: 10.1007/s00125-018-4603-5. [DOI] [PubMed] [Google Scholar]
- 97.Hashida R., Kawaguchi T., Bekki M., Omoto M., Matsuse H., Nago T., Takano Y., Ueno T., Koga H., George J., et al. Aerobic vs. resistance exercise in non-alcoholic fatty liver disease: A systematic review. J. Hepatol. 2017;66:142–152. doi: 10.1016/j.jhep.2016.08.023. [DOI] [PubMed] [Google Scholar]
- 98.Babu A.F., Csader S., Lok J., Gomez-Gallego C., Hanhineva K., El-Nezami H., Schwab U. Positive Effects of Exercise Intervention without Weight Loss and Dietary Changes in NAFLD-Related Clinical Parameters: A Systematic Review and Meta-Analysis. Nutrients. 2021;13:3135. doi: 10.3390/nu13093135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ekblom-Bak E., Ekblom B., Vikstrom M., de Faire U., Hellenius M.L. The importance of non-exercise physical activity for cardiovascular health and longevity. Br. J. Sport. Med. 2014;48:233–238. doi: 10.1136/bjsports-2012-092038. [DOI] [PubMed] [Google Scholar]
- 100.Hamer M., de Oliveira C., Demakakos P. Non-exercise physical activity and survival: English longitudinal study of ageing. Am. J. Prev. Med. 2014;47:452–460. doi: 10.1016/j.amepre.2014.05.044. [DOI] [PubMed] [Google Scholar]
- 101.Cuthbertson D.J., Shojaee-Moradie F., Sprung V.S., Jones H., Pugh C.J., Richardson P., Kemp G.J., Barrett M., Jackson N.C., Thomas E.L., et al. Dissociation between exercise-induced reduction in liver fat and changes in hepatic and peripheral glucose homoeostasis in obese patients with non-alcoholic fatty liver disease. Clin. Sci. 2016;130:93–104. doi: 10.1042/CS20150447. [DOI] [PubMed] [Google Scholar]
- 102.Shojaee-Moradie F., Cuthbertson D.J., Barrett M., Jackson N.C., Herring R., Thomas E.L., Bell J., Kemp G.J., Wright J., Umpleby A.M. Exercise Training Reduces Liver Fat and Increases Rates of VLDL Clearance But Not VLDL Production in NAFLD. J. Clin. Endocrinol. Metab. 2016;101:4219–4228. doi: 10.1210/jc.2016-2353. [DOI] [PubMed] [Google Scholar]
- 103.Watt M.J., Miotto P.M., De Nardo W., Montgomery M.K. The Liver as an Endocrine Organ-Linking NAFLD and Insulin Resistance. Endocr. Rev. 2019;40:1367–1393. doi: 10.1210/er.2019-00034. [DOI] [PubMed] [Google Scholar]
- 104.Dai W., Ye L., Liu A., Wen S.W., Deng J., Wu X., Lai Z. Prevalence of nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus: A meta-analysis. Medicine. 2017;96:e8179. doi: 10.1097/MD.0000000000008179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Younossi Z.M., Golabi P., de Avila L., Paik J.M., Srishord M., Fukui N., Qiu Y., Burns L., Afendy A., Nader F. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J. Hepatol. 2019;71:793–801. doi: 10.1016/j.jhep.2019.06.021. [DOI] [PubMed] [Google Scholar]
- 106.Hazlehurst J.M., Woods C., Marjot T., Cobbold J.F., Tomlinson J.W. Non-alcoholic fatty liver disease and diabetes. Metabolism. 2016;65:1096–1108. doi: 10.1016/j.metabol.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Marchesini G., Bugianesi E., Forlani G., Cerrelli F., Lenzi M., Manini R., Natale S., Vanni E., Villanova N., Melchionda N., et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37:917–923. doi: 10.1053/jhep.2003.50161. [DOI] [PubMed] [Google Scholar]
- 108.Yeniova A.O., Küçükazman M., Ata N., Dal K., Kefeli A., Başyiğit S., Aktaş B., Ağladioğlu K., Akin K.O., Ertugrul D.T., et al. High-sensitivity C-reactive protein is a strong predictor of non-alcoholic fatty liver disease. Hepatogastroenterology. 2014;61:422–425. [PubMed] [Google Scholar]
- 109.Zhao Y.C., Zhao G.J., Chen Z., She Z.G., Cai J., Li H. Nonalcoholic Fatty Liver Disease: An Emerging Driver of Hypertension. Hypertension. 2020;75:275–284. doi: 10.1161/HYPERTENSIONAHA.119.13419. [DOI] [PubMed] [Google Scholar]
- 110.Fadaei R., Poustchi H., Meshkani R., Moradi N., Golmohammadi T., Merat S. Impaired HDL cholesterol efflux capacity in patients with non-alcoholic fatty liver disease is associated with subclinical atherosclerosis. Sci. Rep. 2018;8:11691. doi: 10.1038/s41598-018-29639-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jarvis H., Craig D., Barker R., Spiers G., Stow D., Anstee Q.M., Hanratty B. Metabolic risk factors and incident advanced liver disease in non-alcoholic fatty liver disease (NAFLD): A systematic review and meta-analysis of population-based observational studies. PLoS Med. 2020;17:e1003100. doi: 10.1371/journal.pmed.1003100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kirpich I.A., Marsano L.S., McClain C.J. Gut-liver axis, nutrition, and non-alcoholic fatty liver disease. Clin. Biochem. 2015;48:923–930. doi: 10.1016/j.clinbiochem.2015.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.An L., Wirth U., Koch D., Schirren M., Drefs M., Koliogiannis D., Niess H., Andrassy J., Guba M., Bazhin A.V., et al. The Role of Gut-Derived Lipopolysaccharides and the Intestinal Barrier in Fatty Liver Diseases. J. Gastrointest. Surg. 2022;26:671–683. doi: 10.1007/s11605-021-05188-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Aron-Wisnewsky J., Vigliotti C., Witjes J., Le P., Holleboom A.G., Verheij J., Nieuwdorp M., Clement K. Gut microbiota and human NAFLD: Disentangling microbial signatures from metabolic disorders. Nat. Rev. Gastroenterol. Hepatol. 2020;17:279–297. doi: 10.1038/s41575-020-0269-9. [DOI] [PubMed] [Google Scholar]
- 115.Gupta H., Min B.H., Ganesan R., Gebru Y.A., Sharma S.P., Park E., Won S.M., Jeong J.J., Lee S.B., Cha M.G., et al. Gut Microbiome in Non-Alcoholic Fatty Liver Disease: From Mechanisms to Therapeutic Role. Biomedicines. 2022;10:550. doi: 10.3390/biomedicines10030550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Caussy C., Aubin A., Loomba R. The Relationship Between Type 2 Diabetes, NAFLD, and Cardiovascular Risk. Curr. Diab. Rep. 2021;21:15. doi: 10.1007/s11892-021-01383-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wigg A.J., Roberts-Thomson I.C., Dymock R.B., McCarthy P.J., Grose R.H., Cummins A.G. The role of small intestinal bacterial overgrowth, intestinal permeability, endotoxaemia, and tumour necrosis factor alpha in the pathogenesis of non-alcoholic steatohepatitis. Gut. 2001;48:206–211. doi: 10.1136/gut.48.2.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.De Munck T.J.I., Xu P., Verwijs H.J.A., Masclee A.A.M., Jonkers D., Verbeek J., Koek G.H. Intestinal permeability in human nonalcoholic fatty liver disease: A systematic review and meta-analysis. Liver Int. 2020;40:2906–2916. doi: 10.1111/liv.14696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Parlesak A., Schäfer C., Schütz T., Bode J.C., Bode C. Increased intestinal permeability to macromolecules and endotoxemia in patients with chronic alcohol abuse in different stages of alcohol-induced liver disease. J. Hepatol. 2000;32:742–747. doi: 10.1016/S0168-8278(00)80242-1. [DOI] [PubMed] [Google Scholar]
- 120.Volynets V., Kuper M.A., Strahl S., Maier I.B., Spruss A., Wagnerberger S., Konigsrainer A., Bischoff S.C., Bergheim I. Nutrition, intestinal permeability, and blood ethanol levels are altered in patients with nonalcoholic fatty liver disease (NAFLD) Dig. Dis. Sci. 2012;57:1932–1941. doi: 10.1007/s10620-012-2112-9. [DOI] [PubMed] [Google Scholar]
- 121.Vancamelbeke M., Vermeire S. The intestinal barrier: A fundamental role in health and disease. Expert Rev. Gastroenterol. Hepatol. 2017;11:821–834. doi: 10.1080/17474124.2017.1343143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Moreira A.P., Texeira T.F., Ferreira A.B., Peluzio Mdo C., Alfenas Rde C. Influence of a high-fat diet on gut microbiota, intestinal permeability and metabolic endotoxaemia. Br. J. Nutr. 2012;108:801–809. doi: 10.1017/S0007114512001213. [DOI] [PubMed] [Google Scholar]
- 123.Rohr M.W., Narasimhulu C.A., Rudeski-Rohr T.A., Parthasarathy S. Negative Effects of a High-Fat Diet on Intestinal Permeability: A Review. Adv. Nutr. 2020;11:77–91. doi: 10.1093/advances/nmz061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Myers R.P., Fong A., Shaheen A.A. Utilization rates, complications and costs of percutaneous liver biopsy: A population-based study including 4275 biopsies. Liver Int. 2008;28:705–712. doi: 10.1111/j.1478-3231.2008.01691.x. [DOI] [PubMed] [Google Scholar]
- 125.Ratziu V., Charlotte F., Heurtier A., Gombert S., Giral P., Bruckert E., Grimaldi A., Capron F., Poynard T., Group L.S. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128:1898–1906. doi: 10.1053/j.gastro.2005.03.084. [DOI] [PubMed] [Google Scholar]
- 126.Ooi G.J., Clouston A., Johari Y., Kemp W.W., Roberts S.K., Brown W.A., Burton P.R. Evaluation of the histological variability of core and wedge biopsies in nonalcoholic fatty liver disease in bariatric surgical patients. Surg. Endosc. 2021;35:1210–1218. doi: 10.1007/s00464-020-07490-y. [DOI] [PubMed] [Google Scholar]
- 127.Kim H.P., Idowu M.O., Mospan A.R., Allmon A.G., Roden M., Newsome P., Lok A.S., Thuluvath P.J., Taunk J., Fried M.W., et al. Liver biopsy in the real world-reporting, expert concordance and correlation with a pragmatic clinical diagnosis. Aliment. Pharm. Ther. 2021;54:1472–1480. doi: 10.1111/apt.16674. [DOI] [PubMed] [Google Scholar]
- 128.Hernaez R., Lazo M., Bonekamp S., Kamel I., Brancati F.L., Guallar E., Clark J.M. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: A meta-analysis. Hepatology. 2011;54:1082–1090. doi: 10.1002/hep.24452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Schwenzer N.F., Springer F., Schraml C., Stefan N., Machann J., Schick F. Non-invasive assessment and quantification of liver steatosis by ultrasound, computed tomography and magnetic resonance. J. Hepatol. 2009;51:433–445. doi: 10.1016/j.jhep.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 130.Lee S.S., Park S.H. Radiologic evaluation of nonalcoholic fatty liver disease. World J. Gastroenterol. 2014;20:7392–7402. doi: 10.3748/wjg.v20.i23.7392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Karlas T., Petroff D., Sasso M., Fan J.G., Mi Y.Q., de Ledinghen V., Kumar M., Lupsor-Platon M., Han K.H., Cardoso A.C., et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J. Hepatol. 2017;66:1022–1030. doi: 10.1016/j.jhep.2016.12.022. [DOI] [PubMed] [Google Scholar]
- 132.Petroff D., Blank V., Newsome P.N., Shalimar, Voican C.S., Thiele M., de Lédinghen V., Baumeler S., Chan W.K., Perlemuter G., et al. Assessment of hepatic steatosis by controlled attenuation parameter using the M and XL probes: An individual patient data meta-analysis. Lancet Gastroenterol. Hepatol. 2021;6:185–198. doi: 10.1016/S2468-1253(20)30357-5. [DOI] [PubMed] [Google Scholar]
- 133.Mozes F.E., Lee J.A., Selvaraj E.A., Jayaswal A.N.A., Trauner M., Boursier J., Fournier C., Staufer K., Stauber R.E., Bugianesi E., et al. Diagnostic accuracy of non-invasive tests for advanced fibrosis in patients with NAFLD: An individual patient data meta-analysis. Gut. 2021;71:1006–1019. doi: 10.1136/gutjnl-2021-324243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bedogni G., Bellentani S., Miglioli L., Masutti F., Passalacqua M., Castiglione A., Tiribelli C. The Fatty Liver Index: A simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006;6:33. doi: 10.1186/1471-230X-6-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Lee J.H., Kim D., Kim H.J., Lee C.H., Yang J.I., Kim W., Kim Y.J., Yoon J.H., Cho S.H., Sung M.W., et al. Hepatic steatosis index: A simple screening tool reflecting nonalcoholic fatty liver disease. Dig. Liver Dis. 2010;42:503–508. doi: 10.1016/j.dld.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 136.Long M.T., Pedley A., Colantonio L.D., Massaro J.M., Hoffmann U., Muntner P., Fox C.S. Development and Validation of the Framingham Steatosis Index to Identify Persons with Hepatic Steatosis. Clin. Gastroenterol. Hepatol. 2016;14:1172–1180.e2. doi: 10.1016/j.cgh.2016.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.McHenry S., Park Y., Browning J.D., Sayuk G., Davidson N.O. Dallas Steatosis Index Identifies Patients with Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 2020;18:2073–2080.e7. doi: 10.1016/j.cgh.2020.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Verhaegh P., Bavalia R., Winkens B., Masclee A., Jonkers D., Koek G. Noninvasive Tests Do Not Accurately Differentiate Nonalcoholic Steatohepatitis From Simple Steatosis: A Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2018;16:837–861. doi: 10.1016/j.cgh.2017.08.024. [DOI] [PubMed] [Google Scholar]
- 139.Adams L.A., Chan W.K. Noninvasive Tests in the Assessment of NASH and NAFLD Fibrosis: Now and Into the Future. Semin. Liver Dis. 2020;40:331–338. doi: 10.1055/s-0040-1713006. [DOI] [PubMed] [Google Scholar]
- 140.Harrison S.A., Ratziu V., Boursier J., Francque S., Bedossa P., Majd Z., Cordonnier G., Sudrik F.B., Darteil R., Liebe R., et al. A blood-based biomarker panel (NIS4) for non-invasive diagnosis of non-alcoholic steatohepatitis and liver fibrosis: A prospective derivation and global validation study. Lancet Gastroenterol. Hepatol. 2020;5:970–985. doi: 10.1016/S2468-1253(20)30252-1. [DOI] [PubMed] [Google Scholar]
- 141.Zheng D., Tian W., Zheng Z., Gu J., Guo Z., He X. Accuracy of computed tomography for detecting hepatic steatosis in donors for liver transplantation: A meta-analysis. Clin. Transpl. 2017;31:e13013. doi: 10.1111/ctr.13013. [DOI] [PubMed] [Google Scholar]
- 142.Gu J., Liu S., Du S., Zhang Q., Xiao J., Dong Q., Xin Y. Diagnostic value of MRI-PDFF for hepatic steatosis in patients with non-alcoholic fatty liver disease: A meta-analysis. Eur. Radiol. 2019;29:3564–3573. doi: 10.1007/s00330-019-06072-4. [DOI] [PubMed] [Google Scholar]
- 143.Castellana M., Donghia R., Guerra V., Procino F., Lampignano L., Castellana F., Zupo R., Sardone R., De Pergola G., Romanelli F., et al. Performance of Fatty Liver Index in Identifying Non-Alcoholic Fatty Liver Disease in Population Studies. A Meta-Analysis. J. Clin. Med. 2021;10:1877. doi: 10.3390/jcm10091877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Jung T.Y., Kim M.S., Hong H.P., Kang K.A., Jun D.W. Comparative Assessment and External Validation of Hepatic Steatosis Formulae in a Community-Based Setting. J. Clin. Med. 2020;9:2851. doi: 10.3390/jcm9092851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kotronen A., Peltonen M., Hakkarainen A., Sevastianova K., Bergholm R., Johansson L.M., Lundbom N., Rissanen A., Ridderstrale M., Groop L., et al. Prediction of non-alcoholic fatty liver disease and liver fat using metabolic and genetic factors. Gastroenterology. 2009;137:865–872. doi: 10.1053/j.gastro.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 146.Louvet A., Mathurin P. Alcoholic liver disease: Mechanisms of injury and targeted treatment. Nat. Rev. Gastroenterol. Hepatol. 2015;12:231–242. doi: 10.1038/nrgastro.2015.35. [DOI] [PubMed] [Google Scholar]
- 147.Jeon S., Carr R. Alcohol effects on hepatic lipid metabolism. J. Lipid Res. 2020;61:470–479. doi: 10.1194/jlr.R119000547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Salameh H., Raff E., Erwin A., Seth D., Nischalke H.D., Falleti E., Burza M.A., Leathert J., Romeo S., Molinaro A., et al. PNPLA3 Gene Polymorphism Is Associated with Predisposition to and Severity of Alcoholic Liver Disease. Am. J. Gastroenterol. 2015;110:846–856. doi: 10.1038/ajg.2015.137. [DOI] [PubMed] [Google Scholar]
- 149.Rubbia-Brandt L., Quadri R., Abid K., Giostra E., Malé P.J., Mentha G., Spahr L., Zarski J.P., Borisch B., Hadengue A., et al. Hepatocyte steatosis is a cytopathic effect of hepatitis C virus genotype 3. J. Hepatol. 2000;33:106–115. doi: 10.1016/S0168-8278(00)80166-X. [DOI] [PubMed] [Google Scholar]
- 150.Lonardo A., Adinolfi L.E., Restivo L., Ballestri S., Romagnoli D., Baldelli E., Nascimbeni F., Loria P. Pathogenesis and significance of hepatitis C virus steatosis: An update on survival strategy of a successful pathogen. World J. Gastroenterol. 2014;20:7089–7103. doi: 10.3748/wjg.v20.i23.7089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Stattermayer A.F., Traussnigg S., Dienes H.P., Aigner E., Stauber R., Lackner K., Hofer H., Stift J., Wrba F., Stadlmayr A., et al. Hepatic steatosis in Wilson disease--Role of copper and PNPLA3 mutations. J. Hepatol. 2015;63:156–163. doi: 10.1016/j.jhep.2015.01.034. [DOI] [PubMed] [Google Scholar]
- 152.Mitra A., Ahn J. Liver Disease in Patients on Total Parenteral Nutrition. Clin. Liver Dis. 2017;21:687–695. doi: 10.1016/j.cld.2017.06.008. [DOI] [PubMed] [Google Scholar]
- 153.Rosen E., Bakshi N., Watters A., Rosen H.R., Mehler P.S. Hepatic Complications of Anorexia Nervosa. Dig. Dis. Sci. 2017;62:2977–2981. doi: 10.1007/s10620-017-4766-9. [DOI] [PubMed] [Google Scholar]
- 154.Rocha A.L.L., Faria L.C., Guimaraes T.C.M., Moreira G.V., Candido A.L., Couto C.A., Reis F.M. Non-alcoholic fatty liver disease in women with polycystic ovary syndrome: Systematic review and meta-analysis. J. Endocrinol. Investig. 2017;40:1279–1288. doi: 10.1007/s40618-017-0708-9. [DOI] [PubMed] [Google Scholar]
- 155.Spremovic Radenovic S., Pupovac M., Andjic M., Bila J., Sreckovic S., Gudovic A., Dragas B., Radunovic N. Prevalence, Risk Factors, and Pathophysiology of Nonalcoholic Fatty Liver Disease (NAFLD) in Women with Polycystic Ovary Syndrome (PCOS) Biomedicines. 2022;10:131. doi: 10.3390/biomedicines10010131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Nishino M., Hayakawa K., Nakamura Y., Morimoto T., Mukaihara S. Effects of tamoxifen on hepatic fat content and the development of hepatic steatosis in patients with breast cancer: High frequency of involvement and rapid reversal after completion of tamoxifen therapy. AJR Am. J. Roentgenol. 2003;180:129–134. doi: 10.2214/ajr.180.1.1800129. [DOI] [PubMed] [Google Scholar]
- 157.Woods C.P., Hazlehurst J.M., Tomlinson J.W. Glucocorticoids and non-alcoholic fatty liver disease. J. Steroid Biochem. Mol. Biol. 2015;154:94–103. doi: 10.1016/j.jsbmb.2015.07.020. [DOI] [PubMed] [Google Scholar]
- 158.Lewis J.H., Mullick F., Ishak K.G., Ranard R.C., Ragsdale B., Perse R.M., Rusnock E.J., Wolke A., Benjamin S.B., Seeff L.B., et al. Histopathologic analysis of suspected amiodarone hepatotoxicity. Hum. Pathol. 1990;21:59–67. doi: 10.1016/0046-8177(90)90076-H. [DOI] [PubMed] [Google Scholar]
- 159.Amacher D.E., Chalasani N. Drug-induced hepatic steatosis. Semin. Liver Dis. 2014;34:205–214. doi: 10.1055/s-0034-1375960. [DOI] [PubMed] [Google Scholar]
- 160.Dulai P.S., Singh S., Patel J., Soni M., Prokop L.J., Younossi Z., Sebastiani G., Ekstedt M., Hagstrom H., Nasr P., et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: Systematic review and meta-analysis. Hepatology. 2017;65:1557–1565. doi: 10.1002/hep.29085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Shili-Masmoudi S., Wong G.L., Hiriart J.B., Liu K., Chermak F., Shu S.S., Foucher J., Tse Y.K., Bernard P.H., Yip T.C., et al. Liver stiffness measurement predicts long-term survival and complications in non-alcoholic fatty liver disease. Liver Int. 2020;40:581–589. doi: 10.1111/liv.14301. [DOI] [PubMed] [Google Scholar]
- 162.Xiao G., Zhu S., Xiao X., Yan L., Yang J., Wu G. Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: A meta-analysis. Hepatology. 2017;66:1486–1501. doi: 10.1002/hep.29302. [DOI] [PubMed] [Google Scholar]
- 163.Vali Y., Lee J., Boursier J., Spijker R., Loffler J., Verheij J., Brosnan M.J., Bocskei Z., Anstee Q.M., Bossuyt P.M., et al. Enhanced liver fibrosis test for the non-invasive diagnosis of fibrosis in patients with NAFLD: A systematic review and meta-analysis. J. Hepatol. 2020;73:252–262. doi: 10.1016/j.jhep.2020.03.036. [DOI] [PubMed] [Google Scholar]
- 164.Rosenberg W.M., Voelker M., Thiel R., Becka M., Burt A., Schuppan D., Hubscher S., Roskams T., Pinzani M., Arthur M.J., et al. Serum markers detect the presence of liver fibrosis: A cohort study. Gastroenterology. 2004;127:1704–1713. doi: 10.1053/j.gastro.2004.08.052. [DOI] [PubMed] [Google Scholar]
- 165.Heyens L.J.M., Busschots D., Koek G.H., Robaeys G., Francque S. Liver Fibrosis in Non-alcoholic Fatty Liver Disease: From Liver Biopsy to Non-invasive Biomarkers in Diagnosis and Treatment. Front. Med. 2021;8:615978. doi: 10.3389/fmed.2021.615978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Shah A.G., Lydecker A., Murray K., Tetri B.N., Contos M.J., Sanyal A.J., Nash Clinical Research N. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin. Gastroenterol. Hepatol. 2009;7:1104–1112. doi: 10.1016/j.cgh.2009.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Angulo P., Hui J.M., Marchesini G., Bugianesi E., George J., Farrell G.C., Enders F., Saksena S., Burt A.D., Bida J.P., et al. The NAFLD fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45:846–854. doi: 10.1002/hep.21496. [DOI] [PubMed] [Google Scholar]
- 168.Boursier J., Hagstrom H., Ekstedt M., Moreau C., Bonacci M., Cure S., Ampuero J., Nasr P., Tallab L., Canivet C.M., et al. Non-invasive tests accurately stratify patients with NAFLD based on their risk of liver-related events. J. Hepatol. 2022;76:1013–1020. doi: 10.1016/j.jhep.2021.12.031. [DOI] [PubMed] [Google Scholar]
- 169.Vieira Barbosa J., Milligan S., Frick A., Broestl J., Younossi Z., Afdhal N., Lai M. Fibrosis-4 Index Can Independently Predict Major Adverse Cardiovascular Events in Nonalcoholic Fatty Liver Disease. Am. J. Gastroenterol. 2022;117:453–461. doi: 10.14309/ajg.0000000000001606. [DOI] [PubMed] [Google Scholar]
- 170.Hippisley-Cox J., Coupland C., Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: Prospective cohort study. BMJ. 2017;357:j2099. doi: 10.1136/bmj.j2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.D’Agostino R.B., Sr., Vasan R.S., Pencina M.J., Wolf P.A., Cobain M., Massaro J.M., Kannel W.B. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 172.Younossi Z.M., Felix S., Jeffers T., Younossi E., Nader F., Pham H., Afendy A., Cable R., Racila A., Younoszai Z., et al. Performance of the Enhanced Liver Fibrosis Test to Estimate Advanced Fibrosis among Patients with Nonalcoholic Fatty Liver Disease. JAMA Netw. Open. 2021;4:e2123923. doi: 10.1001/jamanetworkopen.2021.23923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Srivastava A., Gailer R., Tanwar S., Trembling P., Parkes J., Rodger A., Suri D., Thorburn D., Sennett K., Morgan S., et al. Prospective evaluation of a primary care referral pathway for patients with non-alcoholic fatty liver disease. J. Hepatol. 2019;71:371–378. doi: 10.1016/j.jhep.2019.03.033. [DOI] [PubMed] [Google Scholar]
- 174.Crossan C., Majumdar A., Srivastava A., Thorburn D., Rosenberg W., Pinzani M., Longworth L., Tsochatzis E.A. Referral pathways for patients with NAFLD based on non-invasive fibrosis tests: Diagnostic accuracy and cost analysis. Liver Int. 2019;39:2052–2060. doi: 10.1111/liv.14198. [DOI] [PubMed] [Google Scholar]
- 175.Srivastava A., Jong S., Gola A., Gailer R., Morgan S., Sennett K., Tanwar S., Pizzo E., O’Beirne J., Tsochatzis E., et al. Cost-comparison analysis of FIB-4, ELF and fibroscan in community pathways for non-alcoholic fatty liver disease. BMC Gastroenterol. 2019;19:122. doi: 10.1186/s12876-019-1039-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Selvaraj E.A., Mozes F.E., Jayaswal A.N.A., Zafarmand M.H., Vali Y., Lee J.A., Levick C.K., Young L.A.J., Palaniyappan N., Liu C.H., et al. Diagnostic accuracy of elastography and magnetic resonance imaging in patients with NAFLD: A systematic review and meta-analysis. J. Hepatol. 2021;75:770–785. doi: 10.1016/j.jhep.2021.04.044. [DOI] [PubMed] [Google Scholar]
- 177.McPherson S., Hardy T., Dufour J.F., Petta S., Romero-Gomez M., Allison M., Oliveira C.P., Francque S., Van Gaal L., Schattenberg J.M., et al. Age as a Confounding Factor for the Accurate Non-Invasive Diagnosis of Advanced NAFLD Fibrosis. Am. J. Gastroenterol. 2017;112:740–751. doi: 10.1038/ajg.2016.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Ratziu V., Massard J., Charlotte F., Messous D., Imbert-Bismut F., Bonyhay L., Tahiri M., Munteanu M., Thabut D., Cadranel J.F., et al. Diagnostic value of biochemical markers (FibroTest-FibroSURE) for the prediction of liver fibrosis in patients with non-alcoholic fatty liver disease. BMC Gastroenterol. 2006;6:6. doi: 10.1186/1471-230X-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Harrison S.A., Oliver D., Arnold H.L., Gogia S., Neuschwander-Tetri B.A. Development and validation of a simple NAFLD clinical scoring system for identifying patients without advanced disease. Gut. 2008;57:1441–1447. doi: 10.1136/gut.2007.146019. [DOI] [PubMed] [Google Scholar]
- 180.Forns X., Ampurdanes S., Llovet J.M., Aponte J., Quinto L., Martinez-Bauer E., Bruguera M., Sanchez-Tapias J.M., Rodes J. Identification of chronic hepatitis C patients without hepatic fibrosis by a simple predictive model. Hepatology. 2002;36:986–992. doi: 10.1053/jhep.2002.36128. [DOI] [PubMed] [Google Scholar]
- 181.Ballestri S., Mantovani A., Baldelli E., Lugari S., Maurantonio M., Nascimbeni F., Marrazzo A., Romagnoli D., Targher G., Lonardo A. Liver Fibrosis Biomarkers Accurately Exclude Advanced Fibrosis and Are Associated with Higher Cardiovascular Risk Scores in Patients with NAFLD or Viral Chronic Liver Disease. Diagnostics. 2021;11:98. doi: 10.3390/diagnostics11010098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Newsome P.N., Sasso M., Deeks J.J., Paredes A., Boursier J., Chan W.-K., Yilmaz Y., Czernichow S., Zheng M.-H., Wong V.W.-S., et al. FibroScan-AST (FAST) score for the non-invasive identification of patients with non-alcoholic steatohepatitis with significant activity and fibrosis: A prospective derivation and global validation study. Lancet Gastroenterol. Hepatol. 2020;5:362–373. doi: 10.1016/S2468-1253(19)30383-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Rinella M.E., Tacke F., Sanyal A.J., Anstee Q.M., the Participants of the AASLD/EASL Workshop Report on the AASLD/EASL joint workshop on clinical trial endpoints in NAFLD. J. Hepatol. 2019;71:823–833. doi: 10.1016/j.jhep.2019.04.019. [DOI] [PubMed] [Google Scholar]
- 184.Alexander M., Loomis A.K., van der Lei J., Duarte-Salles T., Prieto-Alhambra D., Ansell D., Pasqua A., Lapi F., Rijnbeek P., Mosseveld M., et al. Risks and clinical predictors of cirrhosis and hepatocellular carcinoma diagnoses in adults with diagnosed NAFLD: Real-world study of 18 million patients in four European cohorts. BMC Med. 2019;17:95. doi: 10.1186/s12916-019-1321-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Kim D., Kim W.R., Kim H.J., Therneau T.M. Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology. 2013;57:1357–1365. doi: 10.1002/hep.26156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Mantovani A., Csermely A., Petracca G., Beatrice G., Corey K.E., Simon T.G., Byrne C.D., Targher G. Non-alcoholic fatty liver disease and risk of fatal and non-fatal cardiovascular events: An updated systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2021;6:903–913. doi: 10.1016/S2468-1253(21)00308-3. [DOI] [PubMed] [Google Scholar]
- 187.Mantovani A., Petracca G., Beatrice G., Csermely A., Lonardo A., Schattenberg J.M., Tilg H., Byrne C.D., Targher G. Non-alcoholic fatty liver disease and risk of incident chronic kidney disease: An updated meta-analysis. Gut. 2022;71:156–162. doi: 10.1136/gutjnl-2020-323082. [DOI] [PubMed] [Google Scholar]
- 188.Kim G.A., Lee H.C., Choe J., Kim M.J., Lee M.J., Chang H.S., Bae I.Y., Kim H.K., An J., Shim J.H., et al. Association between non-alcoholic fatty liver disease and cancer incidence rate. J. Hepatol. 2017;68:140–146. doi: 10.1016/j.jhep.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 189.Zhou Y.Y., Zhou X.D., Wu S.J., Fan D.H., Van Poucke S., Chen Y.P., Fu S.W., Zheng M.H. Nonalcoholic fatty liver disease contributes to subclinical atherosclerosis: A systematic review and meta-analysis. Hepatol. Commun. 2018;2:376–392. doi: 10.1002/hep4.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Ormazabal V., Nair S., Elfeky O., Aguayo C., Salomon C., Zuniga F.A. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc. Diabetol. 2018;17:122. doi: 10.1186/s12933-018-0762-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Francque S.M., van der Graaff D., Kwanten W.J. Non-alcoholic fatty liver disease and cardiovascular risk: Pathophysiological mechanisms and implications. J. Hepatol. 2016;65:425–443. doi: 10.1016/j.jhep.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 192.Stahl E.P., Dhindsa D.S., Lee S.K., Sandesara P.B., Chalasani N.P., Sperling L.S. Nonalcoholic Fatty Liver Disease and the Heart: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019;73:948–963. doi: 10.1016/j.jacc.2018.11.050. [DOI] [PubMed] [Google Scholar]
- 193.Moludi J., Maleki V., Jafari-Vayghyan H., Vaghef-Mehrabany E., Alizadeh M. Metabolic endotoxemia and cardiovascular disease: A systematic review about potential roles of prebiotics and probiotics. Clin. Exp. Pharm. Physiol. 2020;47:927–939. doi: 10.1111/1440-1681.13250. [DOI] [PubMed] [Google Scholar]
- 194.Schiattarella G.G., Sannino A., Toscano E., Giugliano G., Gargiulo G., Franzone A., Trimarco B., Esposito G., Perrino C. Gut microbe-generated metabolite trimethylamine-N-oxide as cardiovascular risk biomarker: A systematic review and dose-response meta-analysis. Eur. Heart J. 2017;38:2948–2956. doi: 10.1093/eurheartj/ehx342. [DOI] [PubMed] [Google Scholar]
- 195.Valenti L., Bugianesi E., Pajvani U., Targher G. Nonalcoholic fatty liver disease: Cause or consequence of type 2 diabetes? Liver Int. 2016;36:1563–1579. doi: 10.1111/liv.13185. [DOI] [PubMed] [Google Scholar]
- 196.Byrne C.D., Targher G. NAFLD as a driver of chronic kidney disease. J. Hepatol. 2020;72:785–801. doi: 10.1016/j.jhep.2020.01.013. [DOI] [PubMed] [Google Scholar]
- 197.Jehan S., Zizi F., Pandi-Perumal S.R., Wall S., Auguste E., Myers A.K., Jean-Louis G., McFarlane S.I. Obstructive Sleep Apnea and Obesity: Implications for Public Health. Sleep Med. Disord. 2017;1:00019. [PMC free article] [PubMed] [Google Scholar]
- 198.Jullian-Desayes I., Trzepizur W., Boursier J., Joyeux-Faure M., Bailly S., Benmerad M., Le Vaillant M., Jaffre S., Pigeanne T., Bizieux-Thaminy A., et al. Obstructive sleep apnea, chronic obstructive pulmonary disease and NAFLD: An individual participant data meta-analysis. Sleep Med. 2021;77:357–364. doi: 10.1016/j.sleep.2020.04.004. [DOI] [PubMed] [Google Scholar]
- 199.Al-Omary A., Byth K., Weltman M., George J., Eslam M. The importance and impact of recognizing metabolic dysfunction-associated fatty liver disease in patients with chronic hepatitis C. J. Dig. Dis. 2022;23:33–43. doi: 10.1111/1751-2980.13071. [DOI] [PubMed] [Google Scholar]
- 200.van Kleef L.A., Choi H.S.J., Brouwer W.P., Hansen B.E., Patel K., de Man R.A., Janssen H.L.A., de Knegt R.J., Sonneveld M.J. Metabolic dysfunction-associated fatty liver disease increases risk of adverse outcomes in patients with chronic hepatitis B. JHEP Rep. 2021;3:100350. doi: 10.1016/j.jhepr.2021.100350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Mak L.Y., Hui R.W., Fung J., Liu F., Wong D.K., Cheung K.S., Yuen M.F., Seto W.K. Diverse effects of hepatic steatosis on fibrosis progression and functional cure in virologically quiescent chronic hepatitis B. J. Hepatol. 2020;73:800–806. doi: 10.1016/j.jhep.2020.05.040. [DOI] [PubMed] [Google Scholar]
- 202.Jung H.S., Chang Y., Kwon M.J., Sung E., Yun K.E., Cho Y.K., Shin H., Ryu S. Smoking and the Risk of Non-Alcoholic Fatty Liver Disease: A Cohort Study. Am. J. Gastroenterol. 2019;114:453–463. doi: 10.1038/s41395-018-0283-5. [DOI] [PubMed] [Google Scholar]
- 203.Younossi Z.M., Stepanova M., Ong J., Yilmaz Y., Duseja A., Eguchi Y., El Kassas M., Castellanos-Fernandez M., George J., Jacobson I.M., et al. Effects of Alcohol Consumption and Metabolic Syndrome on Mortality in Patients with Nonalcoholic and Alcohol-Related Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 2019;17:1625–1633.e1. doi: 10.1016/j.cgh.2018.11.033. [DOI] [PubMed] [Google Scholar]
- 204.Thoma C., Day C.P., Trenell M.I. Lifestyle interventions for the treatment of non-alcoholic fatty liver disease in adults: A systematic review. J. Hepatol. 2012;56:255–266. doi: 10.1016/j.jhep.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 205.Vilar-Gomez E., Martinez-Perez Y., Calzadilla-Bertot L., Torres-Gonzalez A., Gra-Oramas B., Gonzalez-Fabian L., Friedman S.L., Diago M., Romero-Gomez M. Weight Loss Through Lifestyle Modification Significantly Reduces Features of Nonalcoholic Steatohepatitis. Gastroenterology. 2015;149:367–378.e365; quiz e314–e365. doi: 10.1053/j.gastro.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 206.Ryan M.C., Itsiopoulos C., Thodis T., Ward G., Trost N., Hofferberth S., O’Dea K., Desmond P.V., Johnson N.A., Wilson A.M. The Mediterranean diet improves hepatic steatosis and insulin sensitivity in individuals with non-alcoholic fatty liver disease. J. Hepatol. 2013;59:138–143. doi: 10.1016/j.jhep.2013.02.012. [DOI] [PubMed] [Google Scholar]
- 207.Scragg J., Avery L., Cassidy S., Taylor G., Haigh L., Boyle M., Trenell M.I., Anstee Q.M., McPherson S., Hallsworth K. Feasibility of a Very Low Calorie Diet to Achieve a Sustainable 10% Weight Loss in Patients with Nonalcoholic Fatty Liver Disease. Clin. Transl. Gastroenterol. 2020;11:e00231. doi: 10.14309/ctg.0000000000000231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Lim E.L., Hollingsworth K.G., Aribisala B.S., Chen M.J., Mathers J.C., Taylor R. Reversal of type 2 diabetes: Normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia. 2011;54:2506–2514. doi: 10.1007/s00125-011-2204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Holmer M., Lindqvist C., Petersson S., Moshtaghi-Svensson J., Tillander V., Brismar T.B., Hagstrom H., Stal P. Treatment of NAFLD with intermittent calorie restriction or low-carb high-fat diet—A randomised controlled trial. JHEP Rep. 2021;3:100256. doi: 10.1016/j.jhepr.2021.100256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Ahn J., Jun D.W., Lee H.Y., Moon J.H. Critical appraisal for low-carbohydrate diet in nonalcoholic fatty liver disease: Review and meta-analyses. Clin. Nutr. 2019;38:2023–2030. doi: 10.1016/j.clnu.2018.09.022. [DOI] [PubMed] [Google Scholar]
- 211.El-Agroudy N.N., Kurzbach A., Rodionov R.N., O’Sullivan J., Roden M., Birkenfeld A.L., Pesta D.H. Are Lifestyle Therapies Effective for NAFLD Treatment? Trends Endocrinol. Metab. TEM. 2019;30:701–709. doi: 10.1016/j.tem.2019.07.013. [DOI] [PubMed] [Google Scholar]
- 212.Mardinoglu A., Wu H., Bjornson E., Zhang C., Hakkarainen A., Rasanen S.M., Lee S., Mancina R.M., Bergentall M., Pietilainen K.H., et al. An Integrated Understanding of the Rapid Metabolic Benefits of a Carbohydrate-Restricted Diet on Hepatic Steatosis in Humans. Cell Metab. 2018;27:559–571.e555. doi: 10.1016/j.cmet.2018.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Fraser A., Abel R., Lawlor D.A., Fraser D., Elhayany A. A modified Mediterranean diet is associated with the greatest reduction in alanine aminotransferase levels in obese type 2 diabetes patients: Results of a quasi-randomised controlled trial. Diabetologia. 2008;51:1616–1622. doi: 10.1007/s00125-008-1049-1. [DOI] [PubMed] [Google Scholar]
- 214.George E.S., Reddy A., Nicoll A.J., Ryan M.C., Itsiopoulos C., Abbott G., Johnson N.A., Sood S., Roberts S.K., Tierney A.C. Impact of a Mediterranean diet on hepatic and metabolic outcomes in non-alcoholic fatty liver disease: The MEDINA randomised controlled trial. Liver Int. 2022;42:1308–1322. doi: 10.1111/liv.15264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Martinez-Gonzalez M.A., Salas-Salvado J., Estruch R., Corella D., Fito M., Ros E., Predimed I. Benefits of the Mediterranean Diet: Insights From the PREDIMED Study. Prog. Cardiovasc. Dis. 2015;58:50–60. doi: 10.1016/j.pcad.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 216.George E.S., Georgousopoulou E.N., Mellor D.D., Chrysohoou C., Pitsavos C., Panagiotakos D.B. Exploring the Path of Mediterranean Diet, Non-Alcoholic Fatty Liver Disease (NAFLD) and Inflammation towards 10-Year Cardiovascular Disease (CVD) Risk: The ATTICA Study 10-Year Follow-Up (2002–2012) Nutrients. 2022;14:2367. doi: 10.3390/nu14122367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Sewter R., Heaney S., Patterson A. Coffee Consumption and the Progression of NAFLD: A Systematic Review. Nutrients. 2021;13:2381. doi: 10.3390/nu13072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Chen Y.P., Lu F.B., Hu Y.B., Xu L.M., Zheng M.H., Hu E.D. A systematic review and a dose-response meta-analysis of coffee dose and nonalcoholic fatty liver disease. Clin. Nutr. 2019;38:2552–2557. doi: 10.1016/j.clnu.2018.11.030. [DOI] [PubMed] [Google Scholar]
- 219.Mann S., Beedie C., Balducci S., Zanuso S., Allgrove J., Bertiato F., Jimenez A. Changes in insulin sensitivity in response to different modalities of exercise: A review of the evidence. Diabetes Metab. Res. Rev. 2014;30:257–268. doi: 10.1002/dmrr.2488. [DOI] [PubMed] [Google Scholar]
- 220.Pattyn N., Cornelissen V.A., Eshghi S.R., Vanhees L. The effect of exercise on the cardiovascular risk factors constituting the metabolic syndrome: A meta-analysis of controlled trials. Sport. Med. 2013;43:121–133. doi: 10.1007/s40279-012-0003-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Sharman J.E., La Gerche A., Coombes J.S. Exercise and cardiovascular risk in patients with hypertension. Am. J. Hypertens. 2015;28:147–158. doi: 10.1093/ajh/hpu191. [DOI] [PubMed] [Google Scholar]
- 222.Katsagoni C.N., Georgoulis M., Papatheodoridis G.V., Panagiotakos D.B., Kontogianni M.D. Effects of lifestyle interventions on clinical characteristics of patients with non-alcoholic fatty liver disease: A meta-analysis. Metabolism. 2017;68:119–132. doi: 10.1016/j.metabol.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 223.Zein C.O., Unalp A., Colvin R., Liu Y.C., McCullough A.J., Nonalcoholic Steatohepatitis Clinical Research Network Smoking and severity of hepatic fibrosis in nonalcoholic fatty liver disease. J. Hepatol. 2011;54:753–759. doi: 10.1016/j.jhep.2010.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Anthonisen N.R., Skeans M.A., Wise R.A., Manfreda J., Kanner R.E., Connett J.E. The effects of a smoking cessation intervention on 14.5-year mortality: A randomized clinical trial. Ann. Intern. Med. 2005;142:233–239. doi: 10.7326/0003-4819-142-4-200502150-00005. [DOI] [PubMed] [Google Scholar]
- 225.Jarvis H., O’Keefe H., Craig D., Stow D., Hanratty B., Anstee Q.M. Does moderate alcohol consumption accelerate the progression of liver disease in NAFLD? A systematic review and narrative synthesis. BMJ Open. 2022;12:e049767. doi: 10.1136/bmjopen-2021-049767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Janjua M., Knuiman M., Divitini M., McQuillan B., Olynyk J.K., Jeffrey G.P., Adams L.A. Alcohol Consumption and Cardiovascular Outcomes in Patients with Nonalcoholic Fatty Liver Disease: A Population-Based Cohort Study. Hepatol. Commun. 2022;6:526–534. doi: 10.1002/hep4.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Bril F., Biernacki D.M., Kalavalapalli S., Lomonaco R., Subbarayan S.K., Lai J., Tio F., Suman A., Orsak B.K., Hecht J., et al. Role of Vitamin E for Nonalcoholic Steatohepatitis in Patients with Type 2 Diabetes: A Randomized Controlled Trial. Diabetes Care. 2019;42:1481–1488. doi: 10.2337/dc19-0167. [DOI] [PubMed] [Google Scholar]
- 228.Bjelakovic G., Nikolova D., Gluud L.L., Simonetti R.G., Gluud C. Antioxidant supplements for prevention of mortality in healthy participants and patients with various diseases. Cochrane Database Syst. Rev. 2012:CD007176. doi: 10.1002/14651858.CD007176.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Aune D., Keum N., Giovannucci E., Fadnes L.T., Boffetta P., Greenwood D.C., Tonstad S., Vatten L.J., Riboli E., Norat T. Dietary intake and blood concentrations of antioxidants and the risk of cardiovascular disease, total cancer, and all-cause mortality: A systematic review and dose-response meta-analysis of prospective studies. Am. J. Clin. Nutr. 2018;108:1069–1091. doi: 10.1093/ajcn/nqy097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Abenavoli L., Falalyeyeva T., Boccuto L., Tsyryuk O., Kobyliak N. Obeticholic Acid: A New Era in the Treatment of Nonalcoholic Fatty Liver Disease. Pharmaceuticals. 2018;11:104. doi: 10.3390/ph11040104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Mudaliar S., Henry R.R., Sanyal A.J., Morrow L., Marschall H.U., Kipnes M., Adorini L., Sciacca C.I., Clopton P., Castelloe E., et al. Efficacy and safety of the farnesoid X receptor agonist obeticholic acid in patients with type 2 diabetes and nonalcoholic fatty liver disease. Gastroenterology. 2013;145:574–582.e571. doi: 10.1053/j.gastro.2013.05.042. [DOI] [PubMed] [Google Scholar]
- 232.Neuschwander-Tetri B.A., Loomba R., Sanyal A.J., Lavine J.E., Van Natta M.L., Abdelmalek M.F., Chalasani N., Dasarathy S., Diehl A.M., Hameed B., et al. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): A multicentre, randomised, placebo-controlled trial. Lancet. 2015;385:956–965. doi: 10.1016/S0140-6736(14)61933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Younossi Z.M., Ratziu V., Loomba R., Rinella M., Anstee Q.M., Goodman Z., Bedossa P., Geier A., Beckebaum S., Newsome P.N., et al. Obeticholic acid for the treatment of non-alcoholic steatohepatitis: Interim analysis from a multicentre, randomised, placebo-controlled phase 3 trial. Lancet. 2019;394:2184–2196. doi: 10.1016/S0140-6736(19)33041-7. [DOI] [PubMed] [Google Scholar]
- 234.Belfort R., Harrison S.A., Brown K., Darland C., Finch J., Hardies J., Balas B., Gastaldelli A., Tio F., Pulcini J., et al. A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis. N. Engl. J. Med. 2006;355:2297–2307. doi: 10.1056/NEJMoa060326. [DOI] [PubMed] [Google Scholar]
- 235.Aithal G.P., Thomas J.A., Kaye P.V., Lawson A., Ryder S.D., Spendlove I., Austin A.S., Freeman J.G., Morgan L., Webber J. Randomized, placebo-controlled trial of pioglitazone in nondiabetic subjects with nonalcoholic steatohepatitis. Gastroenterology. 2008;135:1176–1184. doi: 10.1053/j.gastro.2008.06.047. [DOI] [PubMed] [Google Scholar]
- 236.Sanyal A.J., Chalasani N., Kowdley K.V., McCullough A., Diehl A.M., Bass N.M., Neuschwander-Tetri B.A., Lavine J.E., Tonascia J., Unalp A., et al. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N. Engl. J. Med. 2010;362:1675–1685. doi: 10.1056/NEJMoa0907929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Cusi K., Orsak B., Bril F., Lomonaco R., Hecht J., Ortiz-Lopez C., Tio F., Hardies J., Darland C., Musi N., et al. Long-Term Pioglitazone Treatment for Patients with Nonalcoholic Steatohepatitis and Prediabetes or Type 2 Diabetes Mellitus: A Randomized Trial. Ann. Intern. Med. 2016;165:305–315. doi: 10.7326/M15-1774. [DOI] [PubMed] [Google Scholar]
- 238.Gillies P.S., Dunn C.J. Pioglitazone. Drugs. 2000;60:333–343. doi: 10.2165/00003495-200060020-00009. [DOI] [PubMed] [Google Scholar]
- 239.Shah P., Mudaliar S. Pioglitazone: Side effect and safety profile. Expert Opin. Drug. Saf. 2010;9:347–354. doi: 10.1517/14740331003623218. [DOI] [PubMed] [Google Scholar]
- 240.LaMoia T.E., Shulman G.I. Cellular and Molecular Mechanisms of Metformin Action. Endocr. Rev. 2021;42:77–96. doi: 10.1210/endrev/bnaa023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Li Y., Liu L., Wang B., Wang J., Chen D. Metformin in non-alcoholic fatty liver disease: A systematic review and meta-analysis. Biomed. Rep. 2013;1:57–64. doi: 10.3892/br.2012.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Ala M. SGLT2 Inhibition for Cardiovascular Diseases, Chronic Kidney Disease, and NAFLD. Endocrinology. 2021;162:bqab157. doi: 10.1210/endocr/bqab157. [DOI] [PubMed] [Google Scholar]
- 243.Mantovani A., Petracca G., Csermely A., Beatrice G., Targher G. Sodium-Glucose Cotransporter-2 Inhibitors for Treatment of Nonalcoholic Fatty Liver Disease: A Meta-Analysis of Randomized Controlled Trials. Metabolites. 2020;11:22. doi: 10.3390/metabo11010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Mantovani A., Petracca G., Beatrice G., Csermely A., Lonardo A., Targher G. Glucagon-Like Peptide-1 Receptor Agonists for Treatment of Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis: An Updated Meta-Analysis of Randomized Controlled Trials. Metabolites. 2021;11:73. doi: 10.3390/metabo11020073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Astrup A., Carraro R., Finer N., Harper A., Kunesova M., Lean M.E., Niskanen L., Rasmussen M.F., Rissanen A., Rossner S., et al. Safety, tolerability and sustained weight loss over 2 years with the once-daily human GLP-1 analog, liraglutide. Int. J. Obes. 2012;36:843–854. doi: 10.1038/ijo.2011.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Wilding J.P.H., Batterham R.L., Calanna S., Davies M., Van Gaal L.F., Lingvay I., McGowan B.M., Rosenstock J., Tran M.T.D., Wadden T.A., et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N. Engl. J. Med. 2021;384:989–1002. doi: 10.1056/NEJMoa2032183. [DOI] [PubMed] [Google Scholar]
- 247.Frias J.P., Davies M.J., Rosenstock J., Perez Manghi F.C., Fernandez Lando L., Bergman B.K., Liu B., Cui X., Brown K., SURPASS-2 Investigators Tirzepatide versus Semaglutide Once Weekly in Patients with Type 2 Diabetes. N. Engl. J. Med. 2021;385:503–515. doi: 10.1056/NEJMoa2107519. [DOI] [PubMed] [Google Scholar]
- 248.Jastreboff A.M., Aronne L.J., Ahmad N.N., Wharton S., Connery L., Alves B., Kiyosue A., Zhang S., Liu B., Bunck M.C., et al. Tirzepatide Once Weekly for the Treatment of Obesity. N. Engl. J. Med. 2022;387:205–216. doi: 10.1056/NEJMoa2206038. [DOI] [PubMed] [Google Scholar]
- 249.Gastaldelli A., Cusi K., Fernández Landó L., Bray R., Brouwers B., Rodríguez Á. Effect of tirzepatide versus insulin degludec on liver fat content and abdominal adipose tissue in people with type 2 diabetes (SURPASS-3 MRI): A substudy of the randomised, open-label, parallel-group, phase 3 SURPASS-3 trial. Lancet Diabetes Endocrinol. 2022;10:393–406. doi: 10.1016/S2213-8587(22)00070-5. [DOI] [PubMed] [Google Scholar]
- 250.Naci H., Brugts J.J., Fleurence R., Tsoi B., Toor H., Ades A.E. Comparative benefits of statins in the primary and secondary prevention of major coronary events and all-cause mortality: A network meta-analysis of placebo-controlled and active-comparator trials. Eur. J. Prev. Cardiol. 2013;20:641–657. doi: 10.1177/2047487313480435. [DOI] [PubMed] [Google Scholar]
- 251.Del Ben M., Baratta F., Polimeni L., Pastori D., Loffredo L., Averna M., Violi F., Angelico F. Under-prescription of statins in patients with non-alcoholic fatty liver disease. Nutr. Metab. Cardiovasc. Dis. 2017;27:161–167. doi: 10.1016/j.numecd.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 252.Tziomalos K., Athyros V.G., Paschos P., Karagiannis A. Nonalcoholic fatty liver disease and statins. Metabolism. 2015;64:1215–1223. doi: 10.1016/j.metabol.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 253.Pastori D., Pani A., Di Rocco A., Menichelli D., Gazzaniga G., Farcomeni A., D’Erasmo L., Angelico F., Del Ben M., Baratta F. Statin liver safety in non-alcoholic fatty liver disease: A systematic review and metanalysis. Br. J. Clin. Pharm. 2022;88:441–451. doi: 10.1111/bcp.14943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Lee J.I., Lee H.W., Lee K.S., Lee H.S., Park J.Y. Effects of Statin Use on the Development and Progression of Nonalcoholic Fatty Liver Disease: A Nationwide Nested Case-Control Study. Am. J. Gastroenterol. 2021;116:116–124. doi: 10.14309/ajg.0000000000000845. [DOI] [PubMed] [Google Scholar]
- 255.Huang D.Q., El-Serag H.B., Loomba R. Global epidemiology of NAFLD-related HCC: Trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 2021;18:223–238. doi: 10.1038/s41575-020-00381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Bosch J., Gracia-Sancho J., Abraldes J.G. Cirrhosis as new indication for statins. Gut. 2020;69:953–962. doi: 10.1136/gutjnl-2019-318237. [DOI] [PubMed] [Google Scholar]
- 257.Simon T.G., Henson J., Osganian S., Masia R., Chan A.T., Chung R.T., Corey K.E. Daily Aspirin Use Associated with Reduced Risk for Fibrosis Progression in Patients with Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 2019;17:2776–2784.e4. doi: 10.1016/j.cgh.2019.04.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Shen H., Shahzad G., Jawairia M., Bostick R.M., Mustacchia P. Association between aspirin use and the prevalence of nonalcoholic fatty liver disease: A cross-sectional study from the Third National Health and Nutrition Examination Survey. Aliment. Pharm. Ther. 2014;40:1066–1073. doi: 10.1111/apt.12944. [DOI] [PubMed] [Google Scholar]
- 259.Memel Z.N., Arvind A., Moninuola O., Philpotts L., Chung R.T., Corey K.E., Simon T.G. Aspirin Use Is Associated with a Reduced Incidence of Hepatocellular Carcinoma: A Systematic Review and Meta-analysis. Hepatol. Commun. 2021;5:133–143. doi: 10.1002/hep4.1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.