Abstract
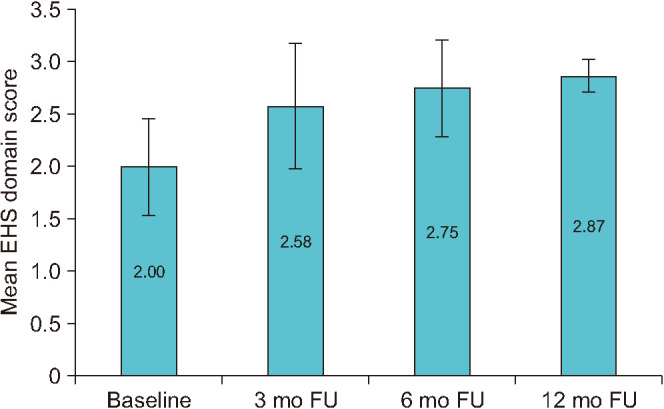
To review the evidence of clinical efficacy of low-intensity extracorporeal shock wave therapy (Li-ESWT) for the treatment of erectile dysfunction (ED). A search on PubMed using Medical Subject Headings terms [((low intensity extracorporeal shockwave therapy) OR (Li-ESWT)) AND (erectile dysfunction)] was conducted in August 2022, to obtain studies on the use of Li-ESWT for the treatment of ED. Its success rate in terms of International Index of Erectile Function-5 (IIEF-5) score and Erection Hardness Score (EHS) improvement was recorded and analysed. A total of 139 articles were reviewed. Overall, 52 studies were included in the final review. 17 studies were on vasculogenic ED, 5 on post pelvic surgery ED, 4 specifically on ED in diabetic patients, 24 on non-specified origin ED and 2 on mixed pathophysiological origin ED. The mean age of patients was 55.87±7.91 (standard deviation) years and the duration of ED was 4.36±2.08 years. The mean IIEF-5 score went from 12.04±2.67 at baseline to 16.12±5.72, 16.30±3.26 and 16.85±1.63 respectively at 3, 6 and 12 months. The mean EHS went from 2.00±0.46 at baseline to 2.58±0.60, 2.75±0.46 and 2.87±0.16 respectively at 3, 6 and 12 months. Li-ESWT may be a safe and efficacy option for the treatment and cure of ED. Further studies are needed to assess which patients are more suitable for this procedure and which Li-ESWT protocol can lead to the best outcomes.
Keywords: Erectile dysfunction, Extracorporeal shockwave therapy
INTRODUCTION
Erectile dysfunction (ED) is defined as the consistent or recurrent inability to attain and/or maintain penile erection sufficient for achieving satisfactory sexual performances [1,2]. It is a common disease worldwide, for which a tailored treatment strategy should be used according to invasiveness, tolerability and effectiveness of the different therapeutic options and patients’ expectations [1,3].
As a general premise, ED can be treated successfully with current treatments options, but it cannot be cured, with the potentially exceptions of psychogenic ED, post-traumatic arteriogenic ED in young patients and hormonal causes [1].
Although the oral therapy with phosphodiesterase type 5 inhibitors (PDE5Is) have long been considered the first line of treatment, some patients did not respond or poorly respond to this kind of medications; as a result, this led to additional non-surgical treatment options being sought, such as vacuum erection device (VED), intraurethral alprostadil and intracavernosal injections (ICIs) [4].
However, it was showed a consistent discontinuation rate for all these treatment options: 4.4% to 76% for PDE5I, 18.6% to 79.9% for ICI, 32% to 69.2% for urethral suppositories, and 50% to 64% for VED [1].
In recent years, low-intensity extracorporeal shock wave therapy (Li-ESWT) has been suggested as a promising treatment for vasculogenic ED, being the only currently available treatment that could provide a cure, which is the most desired outcome for most men suffering from ED [1,5,6,7,8,9,10,11,12].
The healing rationale is the documented effect of this acoustic waves in inducing cellular pathways that increase the expression of local growth factors, improving endothelial function, angiogenesis, and perhaps even regeneration of nerve fibers [12,13,14,15].
Moreover, following the first reporting of Li-ESWT in the treatment of ED by Vardi et al. [9] in 2010, several studies have evaluated the efficacy of Li-ESWT in different pathways of ED, either organic (vasculogenic or neurogenic) or mixed [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63]. The patients included in the studies show significant differences as regard cardiovascular risk factors, response to PDE5I, duration and severity of ED [1].
Furthermore, there is a wide heterogeneity among shockwave generators, type of shockwaves emitted, setting parameters, and treatment protocols used [1].
Against the background of this heterogeneous data, it is indeed difficult to establish across the board whether Li-ESWT is a viable option for the management of ED. To acquire evidence on the myths and the realities of the efficacy of Li-ESWT for the treatment of ED, we reviewed the available literature considering the achievable outcomes when applied to different patients, erectile disfunction aetiologies and protocols.
MATERIALS AND METHODS
1. Search strategy
We performed a search of PubMed database to investigate the current studies on Li-ESWT for patients with ED. The search terms were [((low intensity extracorporeal shockwave therapy) OR (Li-ESWT)) AND (erectile dysfunction)].
2. Inclusion and exclusion criteria
Titles and abstracts were examined, and manuscripts were classified. Randomized clinical trials, retrospective, prospective, and comparative studies on human man affecting by ED and treated with Li-ESWT were included in the review. Case reports, commentaries, letters to the editor, reviews, and non-English literature were excluded a priori. Full-text assessment was performed for the remaining articles with the same inclusion/exclusion criteria.
1) Characteristics of the patients
Participants were diagnosed as having ED according to European Guideline diagnostic criteria.
In light of the purpose of our review, there were no limitations on ethnicity, age, comorbidity and cardiovascular risk factors. Moreover, no restrictions were placed on PDE5I consumption during the Li-ESWT treatment period or after and on the duration and severity of ED.
According to this, we evaluated the following baseline characteristics of the patients: mean age, diagnosis of diabetes mellitus, smokers or ex ones, response to PDE5I, duration and stage of ED.
2) Li-ESWT protocol
We analysed the Li-ESWT protocols used in different studies, especially the duration and the total number of the treatments, the shocks per treatment, the shocks delivered for patient, the energy flux density (EFD) and the type of generators. We included studies in which patients could use PDE5I during the treatment; on the contrary we excluded the analyses on combination of Li-ESWT and other surgical and non-surgical therapies for ED. All types of shockwaves emitted, setting parameters, and treatment protocols were included, as well as all the different shockwave generators.
3) Outcomes
To evaluate the safety and efficacy of Li-ESWT in the management of ED we analysed the following main outcomes: International Index of Erectile Function-5 (IIEF-5) score, Erection Hardness Score (EHS), peak systolic velocity (PSV) on penile Doppler ultrasonography and the occurrence of adverse events. Moreover, any follow-up (FU) protocol was reported in this review.
3. Data handling and extraction
According to the predefined criteria, two independent authors (ACB and MP) evaluated and extracted data from papers. During the process of data extraction, disagreements were resolved through discussion with a third investigator (AC).
4. Statistical analysis
A pooled analysis was performed, and all collected data were evaluated using Statistical Package for Statistical Sciences, version 25.0 (IBM SPSS Corp.).
RESULTS
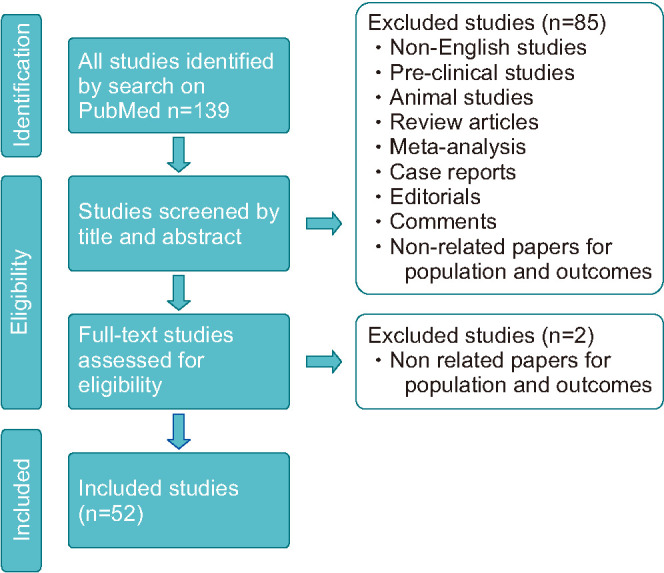
Of 139 records identified by database searching, a total of 52 studies have been finally included in this review. A flow diagram for study screening and selection is shown in Fig. 1. All the included studies were published between 2012 and 2022. Thirty-nine studies were randomized controlled trials (RCTs), of which 9 compared Li-ESWT versus sham treatment in the management of ED. We included 17 studies on vasculogenic ED, 5 studies on post pelvic surgery ED, 4 studies specifically on ED in diabetic patients, 24 studies on non-specified origin ED and 2 studies on mixed pathophysiological origin ED (1 on ED in kidney transplanted patients and 1 on ED due to priapism). In all the studies the FU was no longer than 12 months.
Fig. 1. Flowchart for study selection.
An overview of main data extracted are shown in the Supplementary Table.
Pooled mean age of patients was 55.87±7.91 years and pooled mean duration of ED was 4.36±2.08 years.
As concerning the characteristics of Li-ESWT, the pooled mean of number of shocks per treatment was 3,230±2,138, the pooled mean of total number of shocks was 26,310±18,324 and the pooled EFD was 0.01±0.03 mJ/mm2. Analyzing the baseline characteristics of the patients, the pooled mean IIEF-5 was 12.04±2.67 while the pooled mean EHS was 2.00±0.46.
Pooled characteristics of patients and of Li-ESWT protocols are shown in Table 1.
Table 1. Pooled characteristics of patients and of Li-ESWT protocols.
| Characteristic | Mean±standard deviation |
|---|---|
| Age (y) | 55.87±7.91 |
| Duration of erectile dysfunction (y) | 4.36±2.08 |
| Shocks per treatment | 3,230±2,138 |
| Total number of shocks | 26,310±18,324 |
| Energy flux density (mJ/mm2) | 0.01±0.03 |
Li-ESWT, low-intensity extracorporeal shock wave therapy.
After treatment, the pooled IIEF-5 at 3 months was 16.12±5.72, the pooled IIEF-5 at 6 months was 16.30±3.26 and the pooled IIEF-5 at 12 months was 16.85±1.63.
After treatment, the pooled EHS at 3 months was 2.58±0.60, the pooled EHS at 6 months was 2.75±0.46 and the pooled EHS at 12 months was 2.87±0.16.
The pooled IIEF-5 and EHS at baseline and at 3-6-12 months of FU are resumed by Table 2 and their improved scores from baseline are showed in Figs. 2, 3, respectively.
Table 2. Outcomes of the pooled IIEF-5 and EHS at baseline and at 3-6-12 months of FU.
| IIEF-5 | EHS | |
|---|---|---|
| Baseline | 12.04±2.67 | 2.00±0.46 |
| 3 mo FU | 16.12±5.72 | 2.58±0.60 |
| 6 mo FU | 16.30±3.26 | 2.75±0.46 |
| 12 mo FU | 16.85±1.63 | 2.87±0.16 |
Values are presented as mean±standard deviation.
FU, follow-up; IIEF-5, International Index of Erectile Function-5; EHS, Erection Hardness Score.
Fig. 2. Change from baseline in International Index of Erectile Function-5 (IIEF-5) domain score. FU, follow-up.
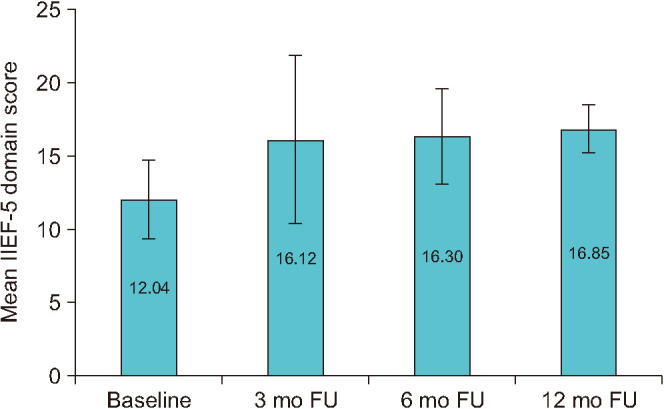
Fig. 3. Change from baseline in Erection Hardness Score (EHS) domain score. FU, follow-up.
DISCUSSION
Approximatively 30% of man >40 years old experience ED, and the prevalence further increases with age [1,2]. This condition can affect considerably the quality of life of men and their partners [3].
A variety of surgical and no-surgical therapies are available, including oral PDE5I, vacuum pumps, intraurethral medications, ICIs, and penile prosthesis [14,64]. However, none of these treatments can cure the underlying pathology and adverse effects, complications, or loss of sexual spontaneousness are common causes of elevated rates of discontinuation and dissatisfaction [14]. In recent years, Li-ESWT has emerged as a promising approach for ED’s treatment and cure and many publications on this topic have been released since 2010 [1,9].
Li-ESWT is a non-invasive technique that uses the targeted passing of acoustic waves through tissues to induce a stress effect [14]. On the whole, the shockwaves exert stress on tissues through two main mechanisms: the first is direct mechanical stress associated with the high-amplitude shockwave, and the second ones is correlated to the growth and violent collapse of cavitation bubbles in fluid [14]. The impact of cavitation is most likely to cause lesions within the blood vessels than surrounding tissue, as a bubble surrounded by tissue will be bound by it that will not allow it to pass through a cycle of violent growth and collapse [14]. Microbubbles, derived from bubbles implosion, cause disruption of the endothelium in vascularization and tissues can result in neoangiogenesis (by activation of resident stem cells with chemokine production attracting progenitor endothelial cells and release of VEGF) [2,65]. In addition, microbubble collapse induces shear stress and could simulate endothelial production of nitric oxide. Finally, shockwave therapy might also enhance Schwann-cell-mediated nitrergic-nerve repair after injury [14]. However, the exact mechanism of action of Li-ESWT for ED is not yet fully known, such as factors affecting the treatment success.
The effect of low-intensity shock waves has been studied in vitro models and in animal, in order to determine the mechanisms that can lead to a clinical improvement in patients with ED. For instance, in 2013 Qiu et al. [66] reported a positive effect of Li-ESWT on regeneration of nerves, endothelium and smooth muscle in diabetic rat models; later, Li et al. [67] demonstrated that angiogenesis, tissue and nerve generation can be promoted by this procedure in rats with pelvic neurovascular injuries. Also, in 2016 a review by Pan et al. [68] led to hypothesize that the shockwave-induced microtrauma and the subsequent angiogenic neovascularization resulted in an improvement in penile blood flow. Numerous systematic reviews and meta-analyses have been conducted to validate Li-ESWT for treatment of ED in human, although the heterogeneity of variables evaluated in literature is wide.
Above all, there is a broad heterogeneousness among shockwave generators (electrohydraulic, electromagnetic, piezoelectric, and electropneumatic), type of shockwaves emitted (focused, linear, semi-focused, and unfocused) setting parameters (EFD and number of pulses per session), and treatment protocols (duration of treatment, sessions number per week, total number of shockwave pulses delivered, and penile sites of application) [1]. All this results in a different influence on the shape and amplitude of the waves and their effects on tissues.
As regards the protocol, there is no standardized one and for instance, different authors reported a total number of treatments between 4 and 12 and a total number of shocks delivered between 6,000 and 80,000 with a variable EFD from 0.05 to 0.25 mJ/mm2.
Furthermore, several clinical studies have evaluated the changes that Li-ESWT can determine in patients with different comorbidities, risk factors and affected by distinct etiopathogenesis of ED. In 2012, Gruenwald et al. [12] demonstrated a significant improvement in IIEF-ED score in patients with severe ED that poorly responded to PDE5I. In a meta-analysis Lu et al. [69] patients with mild ED at baseline were shown to benefit most from Li-ESWT, whereas Yee et al. [16] highlighted the positive effect of Li-ESWT on both IIEF-ED score and EHS score when applied to patients with mild-moderate to severe ED, in a double-blinded placebo-controlled trial [5]. Later, a recent RCT conducted by Ortac et al. [52] a good impact on mild vasculogenic ED in young patients has been obtained with Li-ESWT compared to placebo in a RCT. Studies on Li-ESWT as a treatment for ED in diabetic patients have led to different outcomes. On one side, clinical amelioration have been reported in the RCT by Shendy et al. [45] and in the comparative study between Li-ESWT plus tadalafil vs tadalafil alone by Verze et al. [36]; on the other ones, no significant changes have been evidenced by Ergün and Akyüz [63] on diabetic patients with severe ED.
Regarding the penile rehabilitation after pelvic surgery, the efficacy of Li-ESWT is still controversial. If two studies on the use of Li-ESWT for ED following radical prostatectomy and cystectomy have led to significant improvement in the IIEF score [28,51], other ones on ED after nerve-sparing robot-assisted radical prostatectomy have reported just a slight improvement [19,43]. Regarding the various Li-ESWT protocols, Kalyvianakis et al. [33] have highlighted that better sexual performances can be achieved by increasing the number of treatments, and consequently the total amount of shocks delivered [6]. In addition, they suggested that patients may also benefit equally when the same number of treatments is applied with a different frequency (in terms of number of treatments per week), whereas a higher EFD can yield better results [33]. In this review, we summarized the main outcomes obtained with the use of Li-ESWT in distinct populations and with various Li-ESWT protocols. Despite the evaluation of the changes in PSV can provide objective data on the efficacy of Li-ESWT, just few studies reported this variable, so that was excluded from our results. Rather, we focused on two subjective outcomes that are widely explored in most of the studies: the change in the IIEF-5 score and EHS from baseline.
The pooled IIEF-5 score at three months (16.12±5.72) after the procedure compared with baseline (12.04±2.67), it suggests that Li-ESWT can induce a fast and effective result on the sexual function, which lasts up to twelve months (16.85±1.63). As regards EHS, compared to the baseline value (2.00±0.46) the improvement achieved at 3 months (2.58±0.60), tends to increase at six (2.75±0.46) and twelve months. (2.87±0.16). The increase of EHS in the short term appears more evident than the one of IIEF-5 score. The reason could be that the treatment rapidly allows to reach a greater penile hardness, but it improves less significantly the ability to maintain the erection in the first months.
Regarding the adverse events of Li-ESWT, only few studies have reported low grade complications, such as headache, dizziness, dyspepsia, local penile pain, fatigue and mild fever. This suggests the safety of the procedure.
The result of this review indicates that Li-ESWT can be a valid option in the wide range of treatments for ED, especially in patients who poorly respond to oral medications and who are unwilling to face more invasive procedures. Surely, further studies are needed to understand which patients may mostly benefit from treatment and which protocol it can give the best outcomes.
This review has some limits: most of the studies included small sample sizes and did not analyse objective outcomes, and the FU was relatively short. Moreover, comorbidities, different aetiology of ED, the variety of protocols and machines, and variable use of PDE5I during the treatment can add more confounding factors.
CONCLUSIONS
This review aims to assess the efficacy of Li-ESWT for the treatment of ED. The IIEF-5 score and EHS improved in patients who underwent the procedure with results maintained at 12 months of FU, highlighting the effectiveness of this treatment. Moreover, only few studies have reported low grade complications, suggesting the safety of the procedure. Additional studies are needed to explore the relationship between the aetiology and the severity of ED and the efficacy of Li-ESWT. Finally, a further effort must be directed to establish a standardized protocol for the shock waves delivery.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
FUNDING: None.
- Research conception and design: Alessia Celeste Bocchino.
- Data acquisition: Alessia Celeste Bocchino and Marta Pezzoli.
- Statistical analysis: Arturo Lo Giudice and Giorgio Ivan Russo.
- Data analysis and interpretation: Arturo Lo Giudice and Giorgio Ivan Russo.
- Drafting of the manuscript: Alessia Celeste Bocchino and Marta Pezzoli.
- Critical revision of the manuscript: Andrea Cocci and Juan Ignacio Martínez-Salamanca.
- Supervision: Andrea Cocci.
- Approval of the final manuscript: all authors.
SUPPLEMENTARY MATERIAL
Supplementary Table can be found via https://doi.org/10.4111/icu.20220327.
Summary of the included studies
References
- 1.European Association of Urology. EAU Guidelines; presented at the EAU Annual Congress Amsterdam; Arnhem: EAU Guidelines Office; 2022. pp. 46–71. [Google Scholar]
- 2.NIH Consensus Conference. Impotence. NIH Consensus Development Panel on Impotence. JAMA. 1993;270:83–90. [PubMed] [Google Scholar]
- 3.Irwin GM. Erectile dysfunction. Prim Care. 2019;46:249–255. doi: 10.1016/j.pop.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Burnett AL, Nehra A, Breau RH, Culkin DJ, Faraday MM, Hakim LS, et al. Erectile dysfunction: AUA guideline. J Urol. 2018;200:633–641. doi: 10.1016/j.juro.2018.05.004. Erratum in: J Urol 2022;207:743. [DOI] [PubMed] [Google Scholar]
- 5.Capogrosso P, Frey A, Jensen CFS, Rastrelli G, Russo GI, Torremade J, et al. Low-intensity shock wave therapy in sexual medicine-clinical recommendations from the European Society of Sexual Medicine (ESSM) J Sex Med. 2019;16:1490–1505. doi: 10.1016/j.jsxm.2019.07.016. [DOI] [PubMed] [Google Scholar]
- 6.Chung E, Cartmill R. Evaluation of clinical efficacy, safety and patient satisfaction rate after low-intensity extracorporeal shockwave therapy for the treatment of male erectile dysfunction: an Australian first open-label single-arm prospective clinical trial. BJU Int. 2015;115 Suppl 5:46–49. doi: 10.1111/bju.13035. [DOI] [PubMed] [Google Scholar]
- 7.Gruenwald I, Appel B, Kitrey ND, Vardi Y. Shockwave treatment of erectile dysfunction. Ther Adv Urol. 2013;5:95–99. doi: 10.1177/1756287212470696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olsen AB, Persiani M, Boie S, Hanna M, Lund L. Can low-intensity extracorporeal shockwave therapy improve erectile dysfunction? A prospective, randomized, double-blind, placebo-controlled study. Scand J Urol. 2015;49:329–333. doi: 10.3109/21681805.2014.984326. [DOI] [PubMed] [Google Scholar]
- 9.Vardi Y, Appel B, Jacob G, Massarwi O, Gruenwald I. Can low-intensity extracorporeal shockwave therapy improve erectile function? A 6-month follow-up pilot study in patients with organic erectile dysfunction. Eur Urol. 2010;58:243–248. doi: 10.1016/j.eururo.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Kitrey ND, Gruenwald I, Appel B, Shechter A, Massarwa O, Vardi Y. Penile low intensity shock wave treatment is able to shift PDE5i nonresponders to responders: a double-blind, sham controlled study. J Urol. 2016;195:1550–1555. doi: 10.1016/j.juro.2015.12.049. [DOI] [PubMed] [Google Scholar]
- 11.Hisasue S, China T, Horiuchi A, Kimura M, Saito K, Isotani S, et al. Impact of aging and comorbidity on the efficacy of low-intensity shock wave therapy for erectile dysfunction. Int J Urol. 2016;23:80–84. doi: 10.1111/iju.12955. [DOI] [PubMed] [Google Scholar]
- 12.Gruenwald I, Appel B, Vardi Y. Low-intensity extracorporeal shock wave therapy--a novel effective treatment for erectile dysfunction in severe ED patients who respond poorly to PDE5 inhibitor therapy. J Sex Med. 2012;9:259–264. doi: 10.1111/j.1743-6109.2011.02498.x. [DOI] [PubMed] [Google Scholar]
- 13.Katz JE, Clavijo RI, Rizk P, Ramasamy R. The basic physics of waves, soundwaves, and shockwaves for erectile dysfunction. Sex Med Rev. 2020;8:100–105. doi: 10.1016/j.sxmr.2019.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Young Academic Urologists Men's Health Group. Fode M, Hatzichristodoulou G, Serefoglu EC, Verze P, Albersen M. Low-intensity shockwave therapy for erectile dysfunction: is the evidence strong enough? Nat Rev Urol. 2017;14:593–606. doi: 10.1038/nrurol.2017.119. [DOI] [PubMed] [Google Scholar]
- 15.Assaly-Kaddoum R, Giuliano F, Laurin M, Gorny D, Kergoat M, Bernabé J, et al. Low intensity extracorporeal shock wave therapy improves erectile function in a model of type II diabetes independently of NO/cGMP pathway. J Urol. 2016;196:950–956. doi: 10.1016/j.juro.2016.03.147. [DOI] [PubMed] [Google Scholar]
- 16.Yee CH, Chan ES, Hou SS, Ng CF. Extracorporeal shockwave therapy in the treatment of erectile dysfunction: a prospective, randomized, double-blinded, placebo controlled study. Int J Urol. 2014;21:1041–1045. doi: 10.1111/iju.12506. [DOI] [PubMed] [Google Scholar]
- 17.Srini VS, Reddy RK, Shultz T, Denes B. Low intensity extracorporeal shockwave therapy for erectile dysfunction: a study in an Indian population. Can J Urol. 2015;22:7614–7622. [PubMed] [Google Scholar]
- 18.Ruffo A, Capece M, Prezioso D, Romeo G, Illiano E, Romis L, et al. Safety and efficacy of low intensity shockwave (LISW) treatment in patients with erectile dysfunction. Int Braz J Urol. 2015;41:967–974. doi: 10.1590/S1677-5538.IBJU.2014.0386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frey A, Sønksen J, Fode M. Low-intensity extracorporeal shockwave therapy in the treatment of postprostatectomy erectile dysfunction: a pilot study. Scand J Urol. 2016;50:123–127. doi: 10.3109/21681805.2015.1100675. [DOI] [PubMed] [Google Scholar]
- 20.Bechara A, Casabé A, De Bonis W, Ciciclia PG. Twelve-month efficacy and safety of low-intensity shockwave therapy for erectile dysfunction in patients who do not respond to phosphodiesterase type 5 inhibitors. Sex Med. 2016;4:e225–e232. doi: 10.1016/j.esxm.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsai CC, Wang CJ, Lee YC, Kuo YT, Lin HH, Li CC, et al. Low-intensity extracorporeal shockwave therapy can improve erectile function in patients who failed to respond to phosphodiesterase type 5 inhibitors. Am J Mens Health. 2017;11:1781–1790. doi: 10.1177/1557988317721643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kalyvianakis D, Hatzichristou D. Low-intensity shockwave therapy improves hemodynamic parameters in patients with vasculogenic erectile dysfunction: a triplex ultrasonography-based sham-controlled trial. J Sex Med. 2017;14:891–897. doi: 10.1016/j.jsxm.2017.05.012. Erratum in: J Sex Med 2018;15:270. [DOI] [PubMed] [Google Scholar]
- 23.Fojecki GL, Tiessen S, Osther PJ. Effect of low-energy linear shockwave therapy on erectile dysfunction-a double-blinded, sham-controlled, randomized clinical trial. J Sex Med. 2017;14:106–112. doi: 10.1016/j.jsxm.2016.11.307. [DOI] [PubMed] [Google Scholar]
- 24.Kalyvianakis D, Memmos E, Mykoniatis I, Kapoteli P, Memmos D, Hatzichristou D. Low-intensity shockwave therapy for erectile dysfunction: a randomized clinical trial comparing 2 treatment protocols and the impact of repeating treatment. J Sex Med. 2018;15:334–345. doi: 10.1016/j.jsxm.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 25.Fojecki GL, Tiessen S, Osther PJS. Effect of linear low-intensity extracorporeal shockwave therapy for erectile dysfunction-12-month follow-up of a randomized, double-blinded, sham-controlled study. Sex Med. 2018;6:1–7. doi: 10.1016/j.esxm.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Katz JE, Molina ML, Clavijo R, Prakash NS, Ramasamy R. A phase 2 randomized trial to evaluate different dose regimens of low-intensity extracorporeal shockwave therapy for erectile dysfunction: clinical trial update. Eur Urol Focus. 2018;4:336–337. doi: 10.1016/j.euf.2018.07.011. [DOI] [PubMed] [Google Scholar]
- 27.Kitrey ND, Vardi Y, Appel B, Shechter A, Massarwi O, Abu-Ghanem Y, et al. Low intensity shock wave treatment for erectile dysfunction-how long does the effect last? J Urol. 2018;200:167–170. doi: 10.1016/j.juro.2018.02.070. [DOI] [PubMed] [Google Scholar]
- 28.Zewin TS, El-Assmy A, Harraz AM, Bazeed M, Shokeir AA, Sheir K, et al. Efficacy and safety of low-intensity shock wave therapy in penile rehabilitation post nerve-sparing radical cystoprostatectomy: a randomized controlled trial. Int Urol Nephrol. 2018;50:2007–2014. doi: 10.1007/s11255-018-1987-6. [DOI] [PubMed] [Google Scholar]
- 29.de Oliveira PS, de Oliveira TR, Nunes Á, Martins F, Lopes T. Low-intensity shock wave therapy for erectile dysfunction and the influence of disease duration. Arch Ital Urol Androl. 2019;90:276–282. doi: 10.4081/aiua.2018.4.276. [DOI] [PubMed] [Google Scholar]
- 30.Yamaçake KGR, Carneiro F, Cury J, Lourenço R, Françolin PC, Piovesan AC, et al. Low-intensity shockwave therapy for erectile dysfunction in kidney transplant recipients. A prospective, randomized, double blinded, sham-controlled study with evaluation by penile Doppler ultrasonography. Int J Impot Res. 2019;31:195–203. doi: 10.1038/s41443-018-0062-2. [DOI] [PubMed] [Google Scholar]
- 31.Vita R, Benvenga S, Giammusso B, La Vignera S. Determinants of early response to low-intensity extracorporeal shockwaves for the treatment of vasculogenic erectile dysfunction: an open-label, prospective study. J Clin Med. 2019;8:1017. doi: 10.3390/jcm8071017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lurz K, Dreher P, Levy J, McGreen B, Piraino J, Brevik A, et al. Low-intensity shockwave therapy in the treatment of erectile dysfunction. Cureus. 2020;12:e11286. doi: 10.7759/cureus.11286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kalyvianakis D, Mykoniatis I, Memmos E, Kapoteli P, Memmos D, Hatzichristou D. Low-intensity shockwave therapy (LiST) for erectile dysfunction: a randomized clinical trial assessing the impact of energy flux density (EFD) and frequency of sessions. Int J Impot Res. 2020;32:329–337. doi: 10.1038/s41443-019-0185-0. [DOI] [PubMed] [Google Scholar]
- 34.Huang YP, Liu W, Liu YD, Zhang M, Xu SR, Lu MJ. Effect of low-intensity extracorporeal shockwave therapy on nocturnal penile tumescence and rigidity and penile haemodynamics. Andrologia. 2020;52:e13745. doi: 10.1111/and.13745. [DOI] [PubMed] [Google Scholar]
- 35.Kim KS, Jeong HC, Choi SW, Choi YS, Cho HJ, Ha US, et al. Electromagnetic low-intensity extracorporeal shock wave therapy in patients with erectile dysfunction: a sham-controlled, double-blind, randomized prospective study. World J Mens Health. 2020;38:236–242. doi: 10.5534/wjmh.190130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Verze P, Capece M, Creta M, La Rocca R, Persico F, Spirito L, et al. Efficacy and safety of low-intensity shockwave therapy plus tadalafil 5 mg once daily in men with type 2 diabetes mellitus and erectile dysfunction: a matched-pair comparison study. Asian J Androl. 2020;22:379–382. doi: 10.4103/aja.aja_121_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang J, Luo L, Zhao S, Liu Y, Zhu Z, Zhao Z. Low intensity extracorporeal shockwave Therapy shifts PDE5i nonresponders to responders. Int Braz J Urol. 2020;46:934–942. doi: 10.1590/S1677-5538.IBJU.2019.0374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sramkova T, Motil I, Jarkovsky J, Sramkova K. Erectile dysfunction treatment using focused linear low-intensity extracorporeal shockwaves: single-blind, sham-controlled, randomized clinical trial. Urol Int. 2020;104:417–424. doi: 10.1159/000504788. [DOI] [PubMed] [Google Scholar]
- 39.Eryilmaz R, Kaplan Ş, Aslan R, Demir M, Taken K. Comparison of focused and unfocused ESWT in treatment of erectile dysfunction. Aging Male. 2020;23:206–209. doi: 10.1080/13685538.2019.1610377. [DOI] [PubMed] [Google Scholar]
- 40.Baccaglini W, Pazeto CL, Corrêa Barros EA, Timóteo F, Monteiro L, Saad Rached RY, et al. The role of the low-intensity extracorporeal shockwave therapy on penile rehabilitation after radical prostatectomy: a randomized clinical trial. J Sex Med. 2020;17:688–694. doi: 10.1016/j.jsxm.2019.12.024. [DOI] [PubMed] [Google Scholar]
- 41.Vinay J, Moreno D, Rajmil O, Ruiz-Castañe E, Sanchez-Curbelo J. Penile low intensity shock wave treatment for PDE5I refractory erectile dysfunction: a randomized double-blind sham-controlled clinical trial. World J Urol. 2021;39:2217–2222. doi: 10.1007/s00345-020-03373-y. [DOI] [PubMed] [Google Scholar]
- 42.Akande TO, Akinwunmi OM, Adebayo SA, Akinyinka AO, Shittu OB. Efficacy and safety of low-intensity extracorporeal shockwave therapy for treatment of vascular erectile dysfunction in Nigerian men: report of a study in Ibadan, south-west Nigeria. Ann Ib Postgrad Med. 2021;19:8–14. [PMC free article] [PubMed] [Google Scholar]
- 43.Ladegaard PBJ, Mortensen J, Skov-Jeppesen SM, Lund L. Erectile dysfunction a prospective randomized placebo-controlled study evaluating the effect of low-intensity extracorporeal shockwave therapy (LI-ESWT) in men with erectile dysfunction following radical prostatectomy. Sex Med. 2021;9:100338. doi: 10.1016/j.esxm.2021.100338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lau W, Shum CF, Lua HCA, Teo CPC. Low-intensity shockwave therapy in the management of erectile dysfunction in Singapore. Ann Acad Med Singap. 2021;50:652–654. [PubMed] [Google Scholar]
- 45.Shendy WS, Elsoghier OM, El Semary MM, Ahmed AA, Ali AF, Saber-Khalaf M. Effect of low-intensity extracorporeal shock wave therapy on diabetic erectile dysfunction: randomised control trial. Andrologia. 2021;53:e13997. doi: 10.1111/and.13997. [DOI] [PubMed] [Google Scholar]
- 46.Tzou KY, Hu SW, Bamodu OA, Wang YH, Wu WL, Wu CC. Efficacy of penile low-intensity shockwave therapy and determinants of treatment response in Taiwanese patients with erectile dysfunction. Biomedicines. 2021;9:1670. doi: 10.3390/biomedicines9111670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lei Q, Wang D, Liu C, Ji Z, Yan S. Comparison of the efficacy and safety of low-intensity extracorporeal shock wave therapy versus on-demand sildenafil for erectile dysfunction. Transl Androl Urol. 2021;10:860–868. doi: 10.21037/tau-20-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Geyik S. Comparison of the efficacy of low-intensity shock wave therapy and its combination with platelet-rich plasma in patients with erectile dysfunction. Andrologia. 2021;53:e14197. doi: 10.1111/and.14197. [DOI] [PubMed] [Google Scholar]
- 49.Caretta N, De Rocco Ponce M, Minicuci N, De Santis I, Palego P, Garolla A, et al. Efficacy of penile low-intensity shockwave treatment for erectile dysfunction: correlation with the severity of cavernous artery disease. Asian J Androl. 2021;23:462–467. doi: 10.4103/aja.aja_15_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Palmieri A, Arcaniolo D, Palumbo F, Verze P, Liguori G, Mondaini N, et al. Low intensity shockwave therapy in combination with phosphodiesterase-5 inhibitors is an effective and safe treatment option in patients with vasculogenic ED who are PDE5i non-responders: a multicenter single-arm clinical trial. Int J Impot Res. 2021;33:634–640. doi: 10.1038/s41443-020-0332-7. [DOI] [PubMed] [Google Scholar]
- 51.Karakose A, Yitgin Y. Penile rehabilitation with low-intensity extracorporeal shock wave therapy in patients after prostate cancer surgery. Early physiological changes and postoperative follow-up outcomes. Int J Clin Pract. 2021;75:e14804. doi: 10.1111/ijcp.14804. [DOI] [PubMed] [Google Scholar]
- 52.Ortac M, Özmez A, Cilesiz NC, Demirelli E, Kadıoğlu A. The impact of extracorporeal shock wave therapy for the treatment of young patients with vasculogenic mild erectile dysfunction: a prospective randomized single-blind, sham controlled study. Andrology. 2021;9:1571–1578. doi: 10.1111/andr.13007. [DOI] [PubMed] [Google Scholar]
- 53.Daneshwar D, Nordin A. Low intensity extracorporeal shockwave therapy for chronic pelvic pain syndrome patients with erectile dysfunction. Medicine (Baltimore) 2022;101:e28546. doi: 10.1097/MD.0000000000028546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Geyik S. A single-centre result of two courses of low-intensity shockwave therapy (Li-SWT) in erectile dysfunction. Andrologia. 2022;54:e14324. doi: 10.1111/and.14324. [DOI] [PubMed] [Google Scholar]
- 55.Oginski N, Apel H, Richterstetter M, Lieb V, Fiebig C, Goebell PJ, et al. Analysis of the impact of clinical factors on low-intensity extracorporeal shockwave therapy for erectile dysfunction. Urol Int. 2022;106:1041–1049. doi: 10.1159/000520705. [DOI] [PubMed] [Google Scholar]
- 56.Gallo L, Pecoraro S, Sarnacchiaro P. Adjuvant daily therapy with L-arginine 2,500 mg and tadalafil 5 mg increases efficacy and duration of benefits of low-intensity extracorporeal shock wave therapy for erectile dysfunction: a prospective, randomized, single-blinded study with 1-year follow-up. Investig Clin Urol. 2022;63:83–91. doi: 10.4111/icu.20210317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ghahhari J, De Nunzio C, Lombardo R, Ferrari R, Gatti L, Ghidini N, et al. Shockwave therapy for erectile dysfunction: which gives the best results? A retrospective national, multi-institutional comparative study of different shockwave technologies. Surg Technol Int. 2022;40:213–218. doi: 10.52198/22.STI.40.UR1556. [DOI] [PubMed] [Google Scholar]
- 58.Kalyvianakis D, Mykoniatis I, Pyrgidis N, Kapoteli P, Zilotis F, Fournaraki A, et al. The effect of low-intensity shock wave therapy on moderate erectile dysfunction: a double-blind, randomized, sham-controlled clinical trial. J Urol. 2022;208:388–395. doi: 10.1097/JU.0000000000002684. [DOI] [PubMed] [Google Scholar]
- 59.Sandoval-Salinas C, Saffon JP, Martínez JM, Corredor HA, Gallego A. Are radial pressure waves effective for the treatment of moderate or mild to moderate erectile dysfunction? A randomized sham therapy controlled clinical trial. J Sex Med. 2022;19:738–744. doi: 10.1016/j.jsxm.2022.02.010. [DOI] [PubMed] [Google Scholar]
- 60.Chung E, Bailey W, Wang J. A prospective, randomized, double-blinded, clinical trial using a second-generation Duolith SD1 low-intensity shockwave machine in males with vascular erectile dysfunction. World J Mens Health. 2023;41:94–100. doi: 10.5534/wjmh.210123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tao R, Chen J, Wang D, Li Y, Xiang J, Xiong L, et al. The efficacy of Li-ESWT combined with VED in diabetic ED patients unresponsive to PDE5is: a single-center, randomized clinical trial. Front Endocrinol (Lausanne) 2022;13:937958. doi: 10.3389/fendo.2022.937958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cocci A, Fassio G, Migliorini F, Cito G, Antonelli A, Verrienti P, et al. Low-intensity extracorporeal shock wave therapy (Li-ESWT) for priapism-induced erectile dysfunction in young patients: the first case series. Int J Impot Res. 2022;34:277–279. doi: 10.1038/s41443-021-00429-4. [DOI] [PubMed] [Google Scholar]
- 63.Ergün M, Akyüz O. Is Li-ESWT effective in diabetic patients with severe erectile dysfunction? Asian J Androl. 2022;24:521–524. doi: 10.4103/aja2021105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F, et al. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. Eur Urol. 2010;57:804–814. doi: 10.1016/j.eururo.2010.02.020. [DOI] [PubMed] [Google Scholar]
- 65.di Mauro M, Russo GI, Della Camera PA, Di Maida F, Cito G, Mondaini N, et al. Extracorporeal shock wave therapy in Peyronie's disease: clinical efficacy and safety from a single-arm observational study. World J Mens Health. 2019;37:339–346. doi: 10.5534/wjmh.180100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Qiu X, Lin G, Xin Z, Ferretti L, Zhang H, Lue TF, et al. Effects of low-energy shockwave therapy on the erectile function and tissue of a diabetic rat model. J Sex Med. 2013;10:738–746. doi: 10.1111/jsm.12024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Li H, Matheu MP, Sun F, Wang L, Sanford MT, Ning H, et al. Low-energy shock wave therapy ameliorates erectile dysfunction in a pelvic neurovascular injuries rat model. J Sex Med. 2016;13:22–32. doi: 10.1016/j.jsxm.2015.11.008. Erratum in: J Sex Med 2016;13:732. [DOI] [PubMed] [Google Scholar]
- 68.Pan MM, Raees A, Kovac JR. Low-intensity extracorporeal shock wave as a novel treatment for erectile dysfunction. Am J Mens Health. 2016;10:146–148. doi: 10.1177/1557988315574511. [DOI] [PubMed] [Google Scholar]
- 69.Lu Z, Lin G, Reed-Maldonado A, Wang C, Lee YC, Lue TF. Low-intensity extracorporeal shock wave treatment improves erectile function: a systematic review and meta-analysis. Eur Urol. 2017;71:223–233. doi: 10.1016/j.eururo.2016.05.050. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Summary of the included studies


