Abstract
The circadian clock regulates cellular and molecular processes in mammals across all tissues including skeletal muscle, one of the largest organs in the human body. Dysregulated circadian rhythms are characteristic of aging and crewed spaceflight, associated with, for example, musculoskeletal atrophy. Molecular insights into spaceflight-related alterations of circadian regulation in skeletal muscle are still missing. Here, we investigated potential functional consequences of clock disruptions on skeletal muscle using published omics datasets obtained from spaceflights and other clock-altering, external (fasting and exercise), or internal (aging) conditions on Earth. Our analysis identified alterations of the clock network and skeletal muscle-associated pathways, as a result of spaceflight duration in mice, which resembles aging-related gene expression changes observed in humans on Earth (e.g., ATF4 downregulation, associated with muscle atrophy). Furthermore, according to our results, external factors such as exercise or fasting lead to molecular changes in the core-clock network, which may compensate for the circadian disruption observed during spaceflights. Thus, maintaining circadian functioning is crucial to ameliorate unphysiological alterations and musculoskeletal atrophy reported among astronauts.
Subject terms: Computational biology and bioinformatics, Systems biology
Introduction
Skeletal muscle is one of the most dynamic and plastic organ of the human body1. Skeletal muscle mass is regulated by the dynamic control of protein synthesis and degradation that are sensitive to factors such as nutritional status and physical activity2. Aging results in a gradual loss of muscle function, which varies based on sex and the level of muscle activity3. The accelerated loss of muscle mass and function, associated with increased adverse outcomes including falls and frailty, results in sarcopenia4 (also called muscle wasting).
In mammals, including humans, more than 2300 genes related to the striated muscle (heart and skeletal) are expressed with a circadian pattern5. Such circadian (about 24 h) rhythms are the result of the regulation via the endogenous biological clock, known as the circadian clock. The mammalian circadian clock regulates the timing of various physiological processes such as metabolism6, myogenesis7, and immune system8. Data from the circadian gene expression atlas for mammals unveiled different temporal organization between central and peripheral tissues9,10. Body temperature rhythms across the day for example are obvious signatures of plasticity and adaptation of mammalian circadian oscillators in peripheral tissues11.
The circadian system consists of a central pacemaker the suprachiasmatic nucleus (SCN), located in the anterior hypothalamus of the brain, and peripheral oscillators, present in peripheral tissues such as the liver12. The SCN clock synchronizes peripheral clocks by neuronal and hormonal signals to ensure coordinated physiological activities13. To remain aligned with the external environment, the clock must be daily re-adjusted, which can be achieved via external time cues known as Zeitgebers14. Light is the dominant environmental cue for the SCN and light therapy is reported to improve the sleep quality among patients with neurodegenerative disorders15,16, to decrease fatigue symptoms among cancer patients17,18, and to improve circadian misalignment in Space19,20. Besides light, the circadian system is also sensitive to other Zeitgebers related to meal timing (e.g., fasting and caloric restriction21) or to physical exercise22–24. At the molecular level, circadian rhythms in gene and protein expression are generated via transcriptional-translational feedback loops (TTFL) where Brain and muscle ARNTL-like 1 (BMAL1; also known as ARNTL) forms a heterodimer with Circadian locomotor output cycles kaput (CLOCK) and regulates the transcriptional activation of Period 1/2/3 (PER 1/2/3), and Cryptochrome 1/2 (CRY 1/2), which in turn inhibit BMAL1-CLOCK mediated transcription25. A further fine-tuning of BMAL1 is achieved via the opposing effects of RAR-related orphan receptor A/B/C (RORA/RORB/RORC) and Nuclear Receptor Subfamily 1 Group D Member 1/2 (NR1D1/NR1D2)26,27.
Recent evidence points towards an important role of the circadian clock in skeletal muscle homeostasis. Circadian rhythms play a prominent role in the maintenance of physiological muscle mass, and the loss of Bmal1 in a mouse model resulted in severe sarcopenia28 with profound consequences for life quality29. Aging directly influences circadian parameters leading to a decrease in amplitude and phase shift of the oscillations30,31. A mouse model of aging showed defects in synchronization to light-dark cycles32,33. Besides aging, studies on the effects of prolonged immobility (bedrest) among individuals due to injury or illness34, and in astronauts exposed to microgravity during spaceflight also reported severe muscle loss35. Moreover, astronauts exhibited a delay in circadian phases of core body temperature (+1 °C inflight) during their stay at the International Space Station (ISS)36, which was also seen in healthy participants during long-term bedrest37, as analogue to spaceflight.
Disrupted synchrony between environmental and endogenous circadian cycles during life may reduce workforce health38, lead to disease39 and decrease lifespan dramatically40. Thus, a proper functioning of the circadian clock is critical to maintain homeostasis and physiological functions, and the perturbation of this system may result in severe pathologies including cancer41,42. Abnormal changes in circadian rhythms have been reported in jet lag43, night-shift workers44, cancer45,46, metabolic disorders47,48, mental disorders49,50, and also as a consequence of spaceflight51–53. Space travellers report circadian rhythm disruption during spaceflight, which is visible in many physiological aspects, for example shorter sleep durations54. Astronauts consciousness and alert reactivity are compromised by alterations of their endogenous circadian rhythms leading to lower performance and associated risk during mission duties53. Moreover, circadian misalignment can affect not only sleep, but also medication intake during Space missions55,56.
In recent years, studies based on transcriptomics data reported altered circadian signalling pathways due to spaceflight in different peripheral tissues of murine models51,52,57. However, a detailed molecular characterization of circadian clock alterations in skeletal muscle due to spaceflight is still lacking. Whether exercise or fasting, based on the time of day, can be used as a preventative measure against spaceflight induced skeletal muscle loss also remains elusive. Physical exercise based on the time of day influences gene expression profiles in skeletal muscle58, and fasting was reported to promote a deep quiescent state in muscle stem cells59. Physical exercise is already implemented as a countermeasure against physiological alterations under microgravity as reported in spaceflight and bedrest conditions (reviewed in60,61). Likewise, also time-restricted feeding improved cardiac glucose usage and ameliorated cardiac dysfunction induced by simulated microgravity in rats62. Moreover, different nutritional interventions were tested to trigger muscle metabolism and homeostasis in astronauts63.
In this study, we carried out a systematic analysis to characterize the potential functional consequences of circadian clock disruptions in skeletal muscle due to intrinsic (e.g., alterations of the circadian clock due to genetic manipulation of clock genes or aging) and extrinsic factors (e.g., alteration of circadian rhythms in extreme environments like spaceflights and similar artificially generated conditions). For our analysis, we used datasets from 28 published genomics (Microarray, RNA-seq) and proteomics (LC-MS) based studies. To pinpoint the specific alterations in skeletal muscle due to spaceflight, we characterized the circadian phenotype within the skeletal muscle of healthy mammalian tissues, investigated the impact of core-clock specific alterations (Bmal1 knockout or Clock mutant or CLOCK knockdown vs. WT) on skeletal muscle phenotype.
In addition, we investigated the impact of spaceflight in alterations of the core-clock network and skeletal muscle-associated pathways, and whether such alterations could be mimicked under bedrest conditions, as an analogue to spaceflight, and inversely, whether hypergravity resulted in opposite changes in the core-clock network compared to microgravity. We compared molecular alterations observed under extreme environments with aging-related alterations in the expression profile of core-clock genes, to investigate whether spaceflights may confer an aging related phenotype to astronauts. Finally, we investigated whether external Zeitgebers like fasting and exercise have an impact on gene expression of core-clock network elements, and in the circadian profiles of skeletal muscle-related genes.
Our study shows that long-term spaceflight results in severe molecular alterations in the expression of circadian clock genes and skeletal muscle-associated pathways, and points to a common molecular dysregulation among these pathways between long-term spaceflight and aging condition datasets. Several core-clock genes like Rorc/RORC were downregulated in spaceflight and aging condition datasets, while its expression was upregulated in a fasting condition dataset. In addition, also skeletal muscle-associated genes like muscle atrophy associated gene activating transcription factor 4 (Atf4/ATF4) was downregulated in both spaceflight and aging datasets, while its expression in fasting and exercise conditions (depending on the type of exercise) was upregulated. Hence, insights from our study will help us to better understand how to ameliorate and/or reverse musculoskeletal atrophy common among astronauts due to spaceflight. There is an urgent need to establish preventive measures for astronauts using circadian biology to minimize the effect of Space missions on their health and performance64. The usage of extrinsic or intrinsic factors may allow to re-establish a robust circadian profile for improved adaptation to microgravity, health and performance on orbit. This can be applicable to, for example, in future extended missions like Deep Space Exploration programs (Moon, Mars), but also during recovery after return to Earth.
Results
A topology of circadian gene expression regulation in the mammalian skeletal muscle
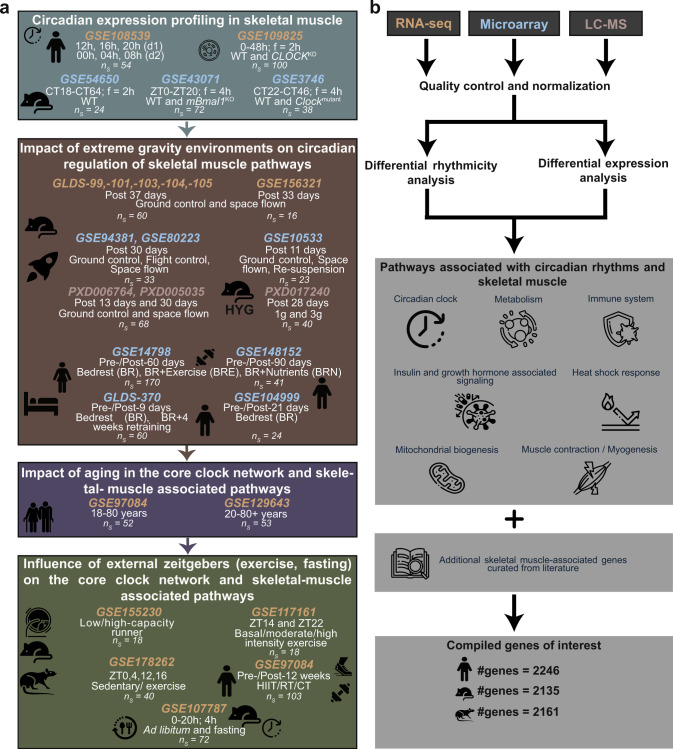
Like most mammalian organs, also skeletal muscle exhibits circadian rhythms in gene expression resulting in oscillations in metabolism, and myogenic capacity7. To pinpoint the specific molecular changes in mammalian skeletal muscle due to spaceflight, and whether these changes are similar to aging on Earth or can be altered via exercise/food regime, we gathered published omics datasets (microarray, RNA-seq, LC-MS) obtained from skeletal muscle tissue or cells (Fig. 1a), as indicated in the Methods.
Fig. 1. Schematic representation of the analysis workflow to elucidate the regulatory role of circadian rhythms under extreme gravity environmental conditions.
a Published sequencing (microarray, RNA-seq, LC-MS) datasets based on skeletal muscle were gathered from open source repositories (ns = number of samples; f: frequency). b Differential rhythmicity (for circadian datasets) and differential expression analysis were carried out after pre-processing of the raw sequencing datasets. Genes of interest were retrieved from KEGG, Reactome, and literature curation related to skeletal muscle-associated pathways and clock-controlled genes.
Skeletal muscle mass is controlled by multiple signalling pathways such as mTOR signalling, Calcineurin and NFATs65. Therefore, to examine the changes in skeletal muscle phenotype, we focused on the gene sets involved in these signalling pathways. The list of genes involved in skeletal muscle-associated pathways were retrieved from KEGG66, Reactome67, and literature curation68,69 (Fig. 1b; Supplementary Dataset 2–4). To prevent discrepancies in the downstream analysis, we retrieved the raw sequencing files and processed all files using the same pipeline and the same statistical cut-offs (Fig. 1b).
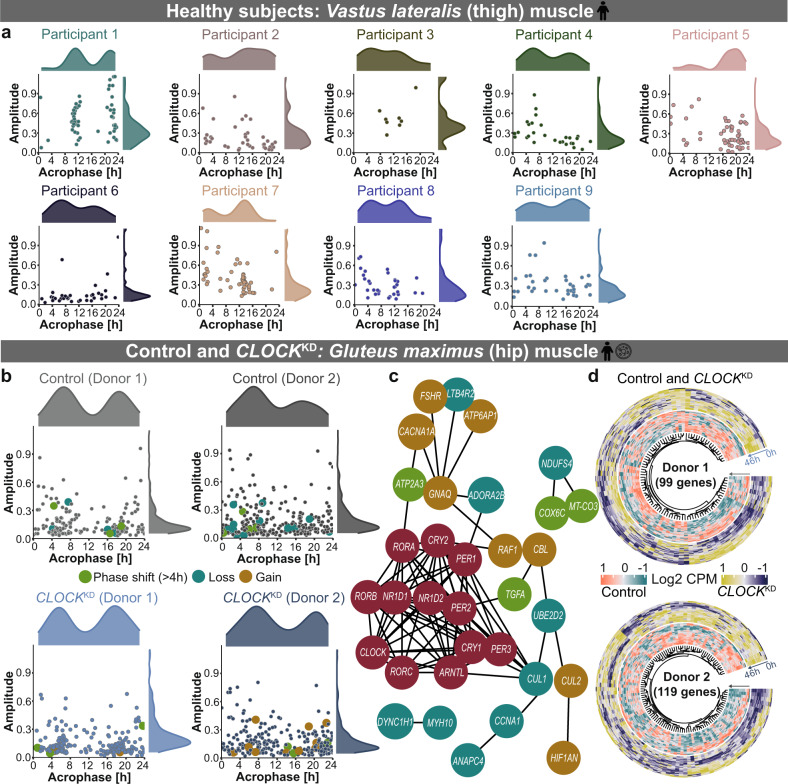
To investigate the relevance of circadian regulation on skeletal muscle specific pathways, we evaluated the circadian (~24 h) gene profile in human and mouse time course datasets (Figs. 2, 3). The assessment of circadian gene expression in human skeletal muscle was carried out using RNA-seq data derived from serial biopsies of nine healthy participants (8 males and 1 female; age = 22–54 years) taken every 4 h across two days (Fig. 2a). The circadian phenotype of genes of interest showed individual specific variations in all nine healthy participants (Fig. 2a). In total 335 genes were ~24 h in at least one of the nine participants. These included the myonuclei related gene, Sad1 and UNC84 Domain Containing 2 (SUN2), which is essential for the maintenance of muscle mass and the core-clock gene NR1D1, known to be relevant for the regulation of core-clock proteins and metabolism. The circadian gene profile also showed variation based on age- and sex- differences, e.g., for participant 5 (male; age = 54 years), the majority of ~24 h genes depicted a peak expression after 16 h (Fig. 2a), while for participant 1 (male, age = 22 years), the majority of ~24 h genes depicted a peak expression at 12 h. WW Domain Containing Transcription Regulator 1 (WWTR1) gene, which is important for myoblast transformation in skeletal muscle was ~24 h rhythmic in both participants 1 and 5, however, its peak expression was at 22 h in participant 1 and at 4 h in participant 5. In case of participant 2 (female, age = 37 years), the majority of ~24 h genes depicted a peak expression after 12 h, while in case of participant 4 (male, age = 33 years), the majority of ~24 h genes peaked before 12 h (Fig. 2a). Nuclear Factor of Activated T Cells 5 (NFAT5) gene, which plays an important role in myoblast migration during skeletal myogenesis was ~24 h rhythmic in both participants 2 and 4, and its peak expression was at 19 h in the female participant and at 23 h in male participant. To further identify whether our genes of interest are affected by perturbations in clock elements in human skeletal muscle, we analysed RNA-seq dataset of control and CLOCK knockdown (CLOCKKD) fusioned myotube cells obtained from two healthy male donors (age = 60 and 62 years) and their clock-altered (using siRNA transfection) counterparts (Fig. 2b–d). Cullin 3 (CUL3) gene is an important component of the ubiquitin proteasome complex essential for proteolysis and is circadian expressed in primary myotube cells. We also identified differences in circadian properties and gene expression among the two donors. Cytochrome C Oxidase Subunit 6 C (COX6C) involved in mitochondrial respiratory chain showed phase shift in Donor 1 (>4 h; q < 0.05) while Transforming Growth Factor Alpha (TGFA) associated with cell proliferation showed phase shift (>4 h; q < 0.05) with CLOCKKD in Donor 2 (Fig. 2b, c). A subsequent differential gene expression analysis showed upregulation in the core-clock gene CRY1, essential component of circadian machinery, and myogenesis related genes including Myogenin (MYOG), and Myosin Heavy Chain 3 (MYH3) that are essential for muscle differentiation, in at least one donor (Fig. 2d). While CLOCKKD resulted in the downregulation of core-clock genes (NR1D1, CLOCK, NR1D2), and genes like Myocyte Enhancer Factor 2 A (MEF2A), which is crucial for skeletal muscle regeneration.
Fig. 2. Genes of interest exhibit circadian properties in human healthy muscle tissue and cells which are altered upon CLOCKKD.
Scatter plot depicts the distribution of circadian (~24 h) genes of interest in (a) muscle biopsies collected from nine healthy participants and (b) myotubes cultured cells from two healthy control donors (upper panel) and siRNA transfected CLOCKKD cells (lower panel). c STRING network depicts the interaction between differential rhythmic genes due to CLOCKKD and the core-clock genes (red circles). d Circular heatmap visualizes the differentially expressed genes of interest due to CLOCKKD vs. WT in donor 1 (upper panel) and donor 2 (lower panel).
Fig. 3. Clock alterations resulted in changes among circadian properties and differential expression in mouse skeletal muscle.
a Scatter plot depicts the overall distribution of ~24 h genes of interest in WT and Clockmutant mice. b Acrophase bin plot depicts the distribution of phases of differentially rhythmic genes of interest between WT and Clockmutant. c Circular heatmap plot represents the expression profile of 772 differentially expressed genes of interest between WT and Clockmutant. d, g Scatter plot depicts the overall distribution of ~24 h genes of interest in Soleus and Tibialis anterior muscle of WT and mBmal1KO mice. e, h Acrophase bin plot depicts the distribution of phases of differentially rhythmic genes of interest between WT and mBmal1KO. f, i Circular heatmap plot represents the expression profile of 114 (in Soleus) and 198 (in Tibialis anterior) differentially expressed genes of interest between WT and mBmal1KO.
To assess circadian gene expression in WT mice and the impact of circadian clock alterations in mouse skeletal muscle, we analysed time-course microarray datasets derived from WT mice, muscle specific Bmal1 knockout mice (mBmal1KO) and from a Clock mutant mice (Clockmutant) (Fig. 3). We observed significant alterations in circadian properties and gene expression profile among genes of interest resulting from the alterations of core-clock components (Bmal1 or Clock) in mice skeletal muscle (Fig. 3).
In WT mice, we observed circadian expression of genes associated with skeletal muscle pathways such as Atf4, Fibroblast growth factor 2 (Fgf2), NDUFA4 mitochondrial complex associated like 2 (Ndufa4l2), and Fatty acid binding protein 3 (Fabp3). Atf4 acts as a regulator of metabolic and redox processes while Fgf2 is important for cytokine activity. Ndufa4l2 is an integral part of mitochondrial respiratory chain and Fabp3 participates in intracellular metabolism. The alteration in core-clock components (Bmal1 or Clock) in mice resulted in a phase shift among genes of interest when compared to their control conditions (Fig. 3b, e, h). A total of 87 genes showed a phase shift (>4 h; q < 0.05) in either mBmal1KO or in Clockmutant vs. their controls (Fig. 3b, e, h). The core-clock genes Nr1d2, Arntl and metabolism associated gene, Protein kinase AMP-activated non-catalytic subunit beta 2 (Prkab2) showed a phase shift (>4 h; q < 0.05) in Clockmutant vs. WT tissue (Fig. 3b). Moreover, we observed a phase shift in autophagy associated genes like GABA type A receptor associated protein like 1 (Gabarapl1) in Clockmutant and Autophagy related 12 (Atg12) in mBmal1KO vs. WT. We also observed upregulation of myonuclei associated gene Spectrin repeat containing nuclear envelope protein 1 (Syne1) in Clockmutant vs. WT (Fig. 3c). Myod1, which is an important component of myogenesis was phase shifted and also differentially upregulated in Soleus muscle of mBmal1KO vs. WT mice (Fig. 3e, f). Protein kinase C delta (Prkcd), associated with cell cycle progression showed phase shift (>4 h; q < 0.05) in both Tibialis anterior muscle of mBmal1KO (Fig. 3h) and Clockmutant mice datasets. Cry2 significantly lost rhythmicity (q < 0.05) due to mBmal1KO, while Myod1 and other clock-related genes (Nr1d1, Per2, D-box binding PAR BZIP transcription factor (Dbp)) showed significant rhythmicity loss in Clockmutant vs. WT (q < 0.05).
Our analysis identified several genes, out of the predefined genes of interest, which depicted circadian expression in the datasets derived from the muscle biopsies of human participants and WT mice. In at least one dataset of the healthy participants, we observed circadian expression of muscle signalling-associated genes like SUN2, Heme Oxygenase 1 (HMOX1), and WWTR1 and core-clock gene RORA. In WT mice datasets, we also observed circadian expression of Sun2, Hmox1, Wwtr1, and Rora. Altogether, our results showed that the genes of interest are clock regulated in both human and mouse skeletal muscle, and perturbations of core-clock elements affect their circadian properties.
Extreme gravity environmental conditions induce molecular alterations in core-clock elements and skeletal muscle-associated pathways
Microgravity exposure can result in decreased muscle strength and endurance with a risk of muscle atrophy, which raises a major concern for astronauts on prolonged space missions70. To identify alterations in clock- and skeletal muscle- associated pathways due to spaceflight, we analysed omics datasets derived from mice sent to Space for 11 days (GSE10533), 30 days (GSE94381, GSE80223), 33 days (GSE156321), or 37 days (GLDS-99/-101/-103/-104/-105) and their respective ground controls. Current available datasets from spaceflight-based omics studies are derived from a single time point sampling (e.g., post spaceflight vs. ground controls), which limits circadian investigation. To partially overcome such limitation, we carried out differential expression analysis and evaluated alterations in our genes of interest in terms of average expression.
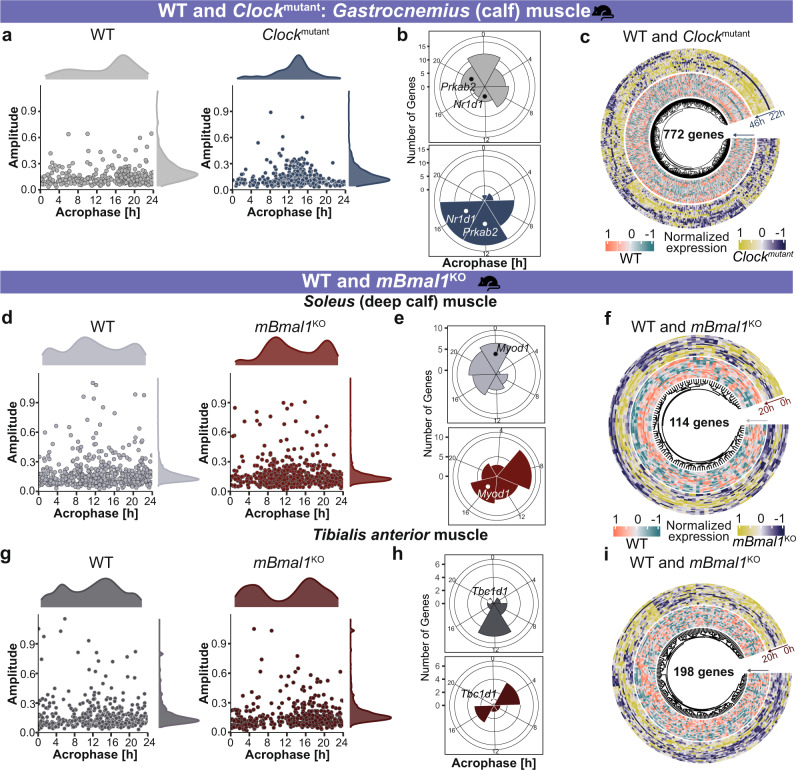
Bedrest, which is an analogue to spaceflight, also induces similar alterations leading to the impairment of muscle functional capacity71. We identified alterations in clock- and skeletal muscle-associated pathways in bedrest conditions, using microarray datasets derived from males subjected to bedrest for 9 days, 21 days, and 90 days and females subjected to bedrest for 60 days. We further categorized the spaceflight and bedrest datasets based on their duration (Fig. 4), and observed differential regulation among a pre-defined set of clock-related genes (NCRGs26) in at least one of the spaceflight datasets (Fig. 4a). A large number of skeletal muscle-associated genes were differentially expressed in the murine spaceflight datasets derived from 30 days (548 genes in at least one of the datasets), 33 days (430 genes), or 37 days (550 genes in at least one of the datasets) duration when compared to 11 days (61 genes) dataset. We selected for visualization genes that showed the same pattern (up-/down-regulation) in 30 days, 33 days, or 37 days spaceflight groups and then plotted the variation of those same genes in 11 days spaceflight dataset (Fig. 4b). The complete list of differentially expressed genes in each of the spaceflight datasets is provided in Supplementary Dataset 5.
Fig. 4. Strength of alterations in clock- and muscle- related genes correlates with the duration of spaceflight/bedrest in mammalian skeletal muscle.
To explore the differences in differential gene expression based on the duration of spaceflight or bedrest, we grouped the datasets accordingly. The groups for spaceflight datasets were 11 days (GSE10533), 30 days (GSE80223, GSE94381), 33 days (GSE156321), and 37 days (/GLDS-99/-101/-103/-104/-105). The groups for bedrest datasets were 9 days (GLDS-370), 21 days (GSE104999), 60 days (GSE14798), and 90 days (GSE148152). Lollipop plots represent the distribution of differentially expressed clock-regulated genes (NCRGs) and muscle related genes due to spaceflight (a–b) and bedrest (c–d), respectively.
For bedrest datasets, we analysed the differentially expressed NCRGs set and skeletal muscle specific genes in at least one of the datasets (Fig. 4c, d). Less number of genes were differentially expressed in females post 60 days bedrest (24 genes) compared to males subjected to 9 days (192 genes), 21 days (147 genes), or 90 days (250 genes) bedrest datasets. Core-clock genes like Per1 and Rora were significantly upregulated and CCGs like 5’-Aminolevulinate Synthase 1 (Alas1), Homeodomain Interacting Protein Kinase 2 (Hipk2), Calumenin (Calu), Basic Helix-Loop-Helix Family Member E41 (Bhlhe41) were significantly downregulated in at least one of the spaceflight datasets (Fig. 4a). For bedrest datasets, the same set of genes (PER1, RORA, ALAS1, HIPK2, CALU, BHLHE41) were also downregulated (Fig. 4c). Alas1 is associated with glucose intolerance in skeletal muscle and Hipk2 is associated with cell proliferation and inflammation in skeletal muscle. Calu encodes for calcium ion binding, essential for skeletal muscle contraction, and Bhlhe41 is known to inhibit inflammation and adipogenic differentiation in skeletal muscle. While, Per2 was significantly downregulated in at least one of the spaceflights and bedrest datasets, Per3 was significantly upregulated in the same datasets pointing to a compensation mechanism in the core-clock to maintain robustness (Fig. 4a, c). Actinin Alpha 2 (ACTN2), which is crucial for muscle contraction was significantly downregulated in bedrest datasets, while Actn2 showed both upregulation/downregulation in its expression depending on the spaceflight duration and skeletal muscle type (Fig. 4b, d). Long-term duration of spaceflight resulted in severe alterations in gene expression profile. Core-clock genes like Arntl, Clock, Cry1, and Neuronal PAS Domain Protein 2 (Npas2) were significantly upregulated while Cry2, Nr1d2, Per2, and Per3 were downregulated post 33 and 37 days in spaceflight mice vs. their ground controls. In addition, we observed upregulation of skeletal muscle-associated genes like Myod1, Nfat5, and Fos Proto-Oncogene, AP-1 Transcription Factor Subunit (Fos) and downregulation of Dbp post 30, 33, and 37 days in spaceflight (Fig. 4a, b). Fos gene is also known to be associated with aging phenotype in humans, as well as in mice72. Cyclin dependent kinase inhibitor 1 A (Cdkn1a) known to function as a regulator of cell cycle progression was significantly upregulated and Peroxisome proliferator activated receptor alpha (Ppara) associated with aging and metabolism was significantly downregulated in all spaceflight datasets, independent of duration (Fig. 4b).
We observed a higher number of differentially expressed genes in the datasets derived from long-term spaceflight duration (Fig. 4a, b). To investigate how many differentially expressed gene sets seen in long-term spaceflight datasets (37 days; GLDS-99/-101/-103/-104/-105) also exhibited circadian profile in WT mouse datasets, we carried out an intersection between the gene sets. Overall, 11207 genes showed ~24 h rhythmicity in at least one of the WT mouse circadian datasets (GSE54650, GSE3746, GSE43071) and 5017 genes were differentially expressed in at least one of the long-term spaceflight datasets. Out of 5017 genes, 3001 genes were circadian expressed in at least one of the WT mouse datasets. Within the predefined genes of interest, 1292 genes showed circadian expression in at least one of the WT mouse datasets. 760 genes of interest showed differential expression in at least one of the long-term spaceflight datasets and out of those, 550 genes were ~24 h rhythmic in at least one of the WT mouse circadian datasets. The core-clock elements Arntl, Clock, Cry1/2, Npas2, Nr1d1/2, Per1/2/3, Rora/Rorc and myogenesis associated genes like Myod1, Myh3/9/10, and Atf4/5/6 were differentially expressed in spaceflight datasets and were ~24 h rhythmic in WT mouse circadian datasets. Furthermore, a Pearson correlation analysis showed variation between gene pairs depending on the skeletal muscle type (Supplementary Fig. 1a). We observed a significant negative correlation between Cry1 and Cry2 in ground controls (GLDS-99: correlation coefficient (r) = −0.823, p = 0.04; GLDS-103: r = −0.951, p = 0.003) while in the spaceflight groups Cry1 and Cry2 were positively correlated though non-significant (GLDS-99: r = 0.452; GLDS-103: r = 0.543, p > 0.05). Furthermore, Clock showed a negative correlation with Cry2 gene in the ground controls (GLDS-104: r = −0.456; GLDS-105: r = −0.83, p = 0.04) while in the spaceflight group we observed a weaker negative correlation though non-significant between Clock and Cry2 (GLDS-104: r = −0.042; GLDS-105: r = −0.456, p > 0.05; Supplementary Fig. 1a).
In addition, to investigate whether artificial hypergravity conditions can alter the molecular profile compared to spaceflight, we analysed proteomics datasets derived from mice subjected to hypergravity (3 g) for 28 days vs. their controls under normal gravity (1 g). The proteomics datasets related to spaceflight also showed a smaller number of differentially expressed proteins post 14 days (2 proteins) and 30 days (307 proteins in at least one dataset). Ryanodine receptor 3 (Ryr3) gene which encodes for an ion channel crucial for muscle contraction was significantly downregulated post 37 days in spaceflight, however, its protein was significantly upregulated in hypergravity datasets, but did not show significant differential expression in the spaceflight proteomics datasets. Taken together, our results showed that spaceflight alters the clock and skeletal muscle-associated pathways and that these alterations directly correlate with spaceflight duration. Moreover, bedrest being the analogue of spaceflight also showed similar discrepancies at the transcriptomic level.
Age-induced circadian alterations in the expression profile of core-clock genes and skeletal muscle-associated pathways correlate with spaceflight induced gene expression alterations
Aging results in the gradual loss of muscle mass and its functional capacity, resulting in increased risk of sarcopenia73. In humans, comparisons between younger and older individuals reveal that fast-twitch fibres are smaller in the older, whereas slow-twitch fibres are less affected74. Aging brings a gradual decrease in size/volume of muscle fibres, and a replacement by fat and connective tissue74. Most importantly, aging is associated with impaired expression of core-clock genes75.
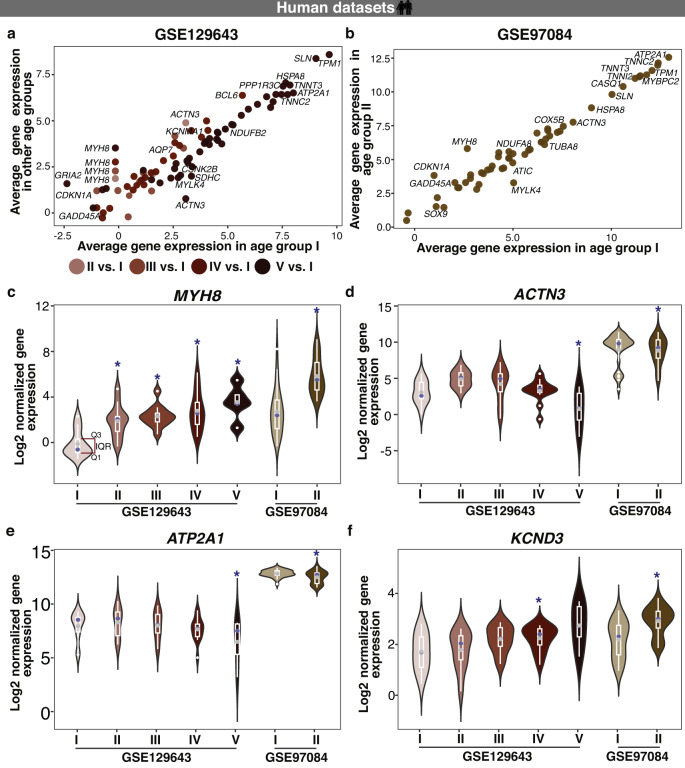
To investigate whether aging on Earth results in similar alterations among the genes of interest as seen during the spaceflight, we analysed RNA-seq datasets derived from muscle biopsies of one set of healthy subjects grouped according to age (GSE129643; Age group I = 20–34 years, Age group II = 35–49 years, Age group III = 50–64 years, Age group IV = 65–79 years, and Age group V = 80+ years), and an independent set of healthy subjects distributed in two age groups (GSE97084; Age group I = 20–30 years, Age group II = 65–75 years). Even though accumulating evidence points to alterations of circadian rhythms, and circadian regulated molecular and physiological processes with aging75, no publicly available time-course datasets from skeletal muscle samples in an aging scenario were found in the literature. We thus carried out differential expression analysis to investigate significant changes in average gene expression within clock and skeletal muscle-associated pathways. A total of 76 genes were differentially expressed in at least one of the age groups vs. age group I (Fig. 5a), and out of those, 58 genes were also differentially expressed in the other aging study dataset (Fig. 5b). We observed significant upregulation of Myosin Heavy Chain 8 (MYH8) in all aging groups in both datasets. MYH8 is an actin-based motor protein involved in skeletal muscle contraction, cell migration and cell adhesion (Fig. 5c). This MyH type of isoform is expressed mainly during foetal development, but also during muscle regeneration. Its expression rapidly diminishes in adult cells. Dominant mutations in that gene lead to Trismus and pseudocamtodactyly syndrome, a congenital contracture of hands, feet and jaw, as well as hand and foot deformities76,77. Whereas, genes like ACTN3 and ATP2A1 were significantly downregulated in age group V vs I (GSE129643) and in age group II vs I (GSE97084) datasets (Fig. 5d, e). ACTN3 encodes for alpha-actinin-3, which plays a major role in skeletal muscle. It is expressed predominantly in fast-twitch, glycolytic muscle fibres and acts as a binding protein with a structural role at the sarcomeric Z-line. Thus, it influences the force production and force transmission capabilities of muscle fibres. Moreover, ACTN3 regulates muscle metabolism. ATP2A1 encodes an enzyme sarcoplasmic/endoplasmic reticulum (SR) calcium ATPase 1 (SERCA1), which is responsible for the translocation of calcium ions from the cytosol into the SR of skeletal muscle. The SR serves as a store for calcium in muscle and can initiate muscle contraction by releasing calcium through the ryanodine receptor type-1 (RyR1), as well as muscle relaxation by active reuptake of calcium by SERCA. SERCA isoforms are distributed differently in skeletal muscle. SERCA1a can be found mainly in fast twitch muscle of adults whereas SERCA1b is predominantly expressed in foetal skeletal muscle. SERCA2 is predominantly expressed in slow twitch muscles (e.g. Soleus). Mutations in SERCA cause Brody’s disease that manifests in severe muscle cramps and exercise induced impairment of skeletal muscle function78. KCND3, which encodes the voltage-gated potassium ion channel was significantly upregulated in age group IV vs. I and also in age groups II vs. I (GSE97084 dataset) (Fig. 5f).
Fig. 5. Aging on Earth results in differential expression of clock- and skeletal muscle-related genes in humans.
Bubble plots represent (a) the average gene expression for differentially expressed genes in at least one age-group (Age group II = 35–49 years, III = 50–64 years, IV = 65–79 years, and V = 80 + years vs. Age group I = 20–34 years; GSE129643), that were also differentially expressed (b) in an independent age-related dataset (Age group II = 65–75 years vs. Age I = 20–30 years, GSE97084). Within the subset of differentially expressed genes of interest (c) MYH8 exhibited age associated changes in the expression profile in all age groups vs. age group I (20–34 years; GSE129643) and in age group II (65–75 years) vs. I (20–30 years) in GSE97084 dataset, (d) ACTN3 and (e) ATP2A1 showed significant downregulation in the Age group V (80 + years; GSE129643) and in age group II (65–75 years; GSE97084) compared to their reference groups, and (f) KCND3 showed significant upregulation in age group IV (65–79 years; GSE129643) and in age group II (65–75 years; GSE97084) vs. their reference groups (* represents the age groups that showed significant differential expression vs. reference group; Q1: 1st quartile; Q3: 3rd quartile; top and bottom whiskers: upper and lower adjacent values calculated as Q3 + 1.5IQR and Q1–1.5IQR, respectively; grey dots represent the mean value and blue dots represent the median value).
In addition, CDKN1A, SRY-Box Transcription Factor 9 (SOX9), Potassium Calcium-Activated Channel Subfamily M Alpha 1 (KCNMA1), were upregulated in age group IV vs. I (in GSE129643 dataset) and in age group II vs. I (in GSE97084 dataset). SOX9 is important for musculoskeletal development79 while KCNMA1 encodes for a voltage and calcium dependent potassium channel important for myoblast differentiation, and contributes to the cardiac transient outward potassium current during the repolarizing phase in the cardiac muscle cell contraction cycle80. Myosin Light Chain Kinase Family Member 4 (MYLK4), important for muscle strength and stiffness was significantly downregulated in age groups V vs. I (GSE129643 dataset) and also in age groups II vs. I (GSE97084 dataset).
Higher number of differentially expressed genes of interest were seen in comparisons between extreme age groups (GSE129643: Group V vs. Group I; GSE97084: Group II vs. Group I). Overall, 5263 genes showed ~24 h rhythmicity in at least one of the healthy human circadian datasets (GSE108539, GSE109825) and 3368 genes were differentially expressed in at least one of the extreme age group datasets. Out of 3368 genes, 1037 genes were circadian expressed in at least one of the human control datasets. Within our set of pre-defined genes of interest, 688 genes showed circadian expression in at least one of the healthy human datasets. 455 genes of interest showed differential expression in at least one of the aging datasets and out of those, 165 genes were ~24 h rhythmic in at least one of the healthy human circadian datasets. Clock elements such as ARNTL, BHLHE40 and genes associated to skeletal muscle pathways like FGF2/7, MYH3 were differentially expressed in extreme age groups datasets and were ~24 h rhythmic in human control datasets. Furthermore, we carried out a Pearson correlation analysis to evaluate the differences in the core-clock network in aging condition datasets (GSE129643: Group V vs. Group I; GSE97084: Group II vs. Group I; Supplementary Fig. 1b, c). In GSE129643 dataset, ARNTL showed negative correlation with PER1 in Group I (age = 20–34 years; r = −0.357, p = 0.006) whereas in Group V (age = 80+ years), ARNTL showed weaker though non-significant negative correlation with PER1 (r = -0.43, p > 0.05; Supplementary Fig. 1b). In GSE97084 dataset, we observed positive correlation between NR1D2 and RORA in Group I (age = 20–30 years; r = 0.867, p < 0.0001). While, NR1D2 and RORA showed negative (non-significant) correlation in Group II (age = 65–75 years; r = −0.155, p > 0.05) in GSE97084 dataset (Supplementary Fig. 1c).
To identify possible common molecular dysregulation between aging and spaceflight datasets, we compared the differentially expressed genes in both scenarios. A total of 129 genes were significantly upregulated in at least one of the aging condition datasets and in at least one of the spaceflight datasets. These included Calsequestrin 2 (CASQ2), and Fibroblast Growth Factor 1 (FGF1). CASQ2 acts as a calcium store for muscle function and FGF1 is involved in muscle development and regeneration. A total of 113 genes were significantly downregulated in at least one of the aging condition datasets and in at least one of the spaceflight datasets. Among the downregulated genes were Nitric Oxide Synthase 1 (NOS1), FABP3, and FGF13. NOS1 generates nitric oxide (NO) which is known to function as a gaseous and highly diffusible neurotransmitter in the brain but also as a co-mediator for skeletal muscle contractility or vascular smooth muscle wall dilation, FABP3 is associated with the maintenance of muscle strength, and FGF13 is important for skeletal muscle differentiation. Taken together, these results show molecular alterations in clock- and skeletal muscle-associated pathways, in human skeletal muscle, in the context of aging, which resemble gene expression alteration observed in spaceflight in murine datasets.
Extrinsic Zeitgebers like fasting and physical activity alter circadian regulation of skeletal muscle related elements
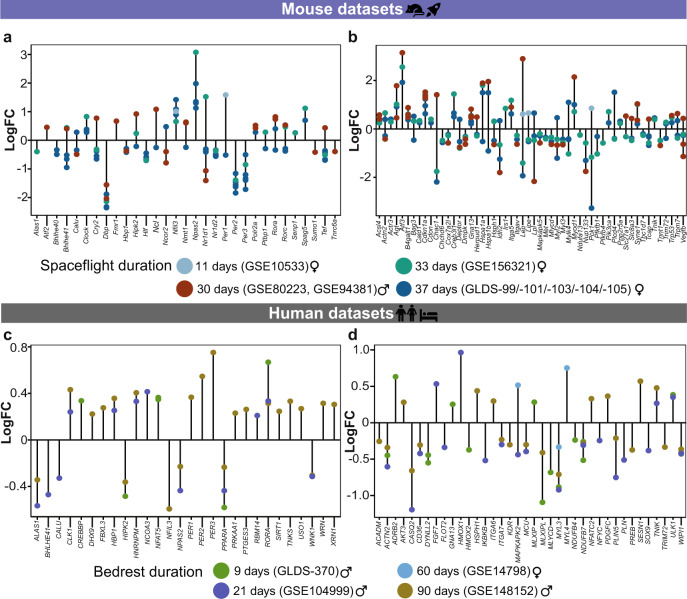
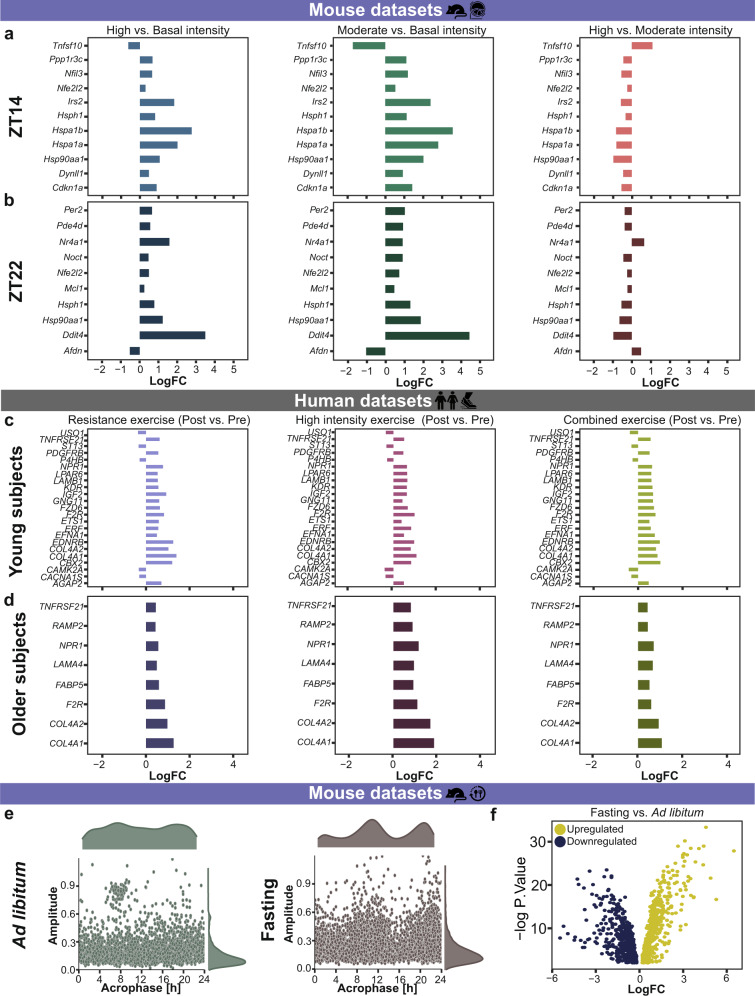
Physical activity or exercise are reported as effective countermeasures against general effects of aging (e.g., sarcopenia) and also play a major role in the prevention of musculoskeletal disorders81. Fasting improves metabolic health and is associated with the loss of lean body mass82. Yet, it is unclear whether exercise based on time or intensity, or fasting can help reverse the molecular alterations observed due to spaceflight, or aging on Earth. To investigate this hypothesis, we analyzed published RNA-seq datasets derived from mice subjected to basal (45% of aerobic capacity), moderate (55% of aerobic capacity), or high intensity (100% of aerobic capacity), running exercises at ZT (Zeitgeber Time) 14 (2 h within dark phase, termed as early) or ZT22 (10 h within dark phase, termed as late) (GSE117161), rats with low and high capacity running (GSE155230), mice subjected to running for predefined durations vs. sedentary groups (GSE178262), and human datasets derived from two age groups (Young: 20–30 years and Older: 65–75 years) subjected to 12 weeks of resistance (strength exercise using free weights) or high intensity (aerobic exercise using treadmill) or combined (resistance plus high intensity) exercise vs. pre-exercise (baseline; GSE97084). Based on our selection criteria, we retrieved one published time-course dataset based on fasting and mammalian skeletal muscle (GSE107787), where the skeletal muscle samples were obtained from mice subjected to 24 h fasting vs. ad libitum group.
The differentially expressed genes in mice skeletal muscle varied based on the type and time of exercise (Supplementary Fig. 2). To examine the molecular changes with type and time of exercise, we extracted the common differentially expressed genes between high vs. basal, moderate vs. basal, and high vs. moderate intensity exercise at ZT14 (Fig. 6a) and at ZT22 (Fig. 6b). A total of 11 common genes were differentially expressed for all exercise intensities at ZT14 (Fig. 6a), out of these, were NFE2 like BZIP transcription factor 2 (Nfe2l2), important for mitochondrial biogenesis induced by exercise in skeletal muscle, and Cdkn1a. A total of 10 common genes were differentially expressed for all exercise intensities at ZT22 (Fig. 6b), out of these were Nfe2l2 and Per2. Nfe2l2 was significantly upregulated in high vs. basal and moderate vs. basal intensity exercises and at both ZT14 and ZT22. Furthermore, we also investigated the individual impact of different exercise intensities at ZT14 and ZT22. Myonuclei associated genes Dctn1 and Dctn3 were significantly downregulated in moderate vs. basal intensity exercise at ZT14. While, Dctn1 was significantly upregulated in high vs. moderate intensity exercise at ZT22. In high vs. basal intensity groups, Dctn4 was upregulated at ZT14 while Cry1 and Per2 were upregulated at ZT22. In moderate vs. basal intensity groups, Myh11 was significantly upregulated. When we analysed a different time dependent exercise dataset (GSE178262), Dctn1 and Myh11 were also upregulated in a group subjected to exercise at ZT12 vs. ZT0. In addition, Myh11 was also significantly upregulated in the dataset derived from rats with high running capacity vs. rats with low running capacity, representing the impact of exercise type on skeletal muscle.
Fig. 6. Extrinsic Zeitgebers like exercise timing and intensity, and fasting affect differential expression of clock- and muscle-related genes in mammalian skeletal muscle tissue.
Histogram plot depicts the common differentially expressed genes independent of exercise intensity (a) at ZT14 and (b) at ZT22 in mouse skeletal muscle, (c) in young subjects and (d) in older subjects. e Scatter plot represents the circadian properties (amplitude, acrophase) of ~24 h genes after ad libitum and fasting. f Volcano plot represents significantly up- or down-regulated genes of interest between ad libitum and fasting groups.
The differentially expressed genes found in human skeletal muscle varied based on the type of exercise and age of the subjects (Supplementary Fig. 3). To examine the impact of exercise type on clock- and skeletal muscle-associated pathways, in an age-dependent manner, we analysed the data from young and older human subjects who underwent three types of exercise (resistance, high intensity, and combined) vs. their profile before exercise. A total of 23 common genes were differentially expressed in the young group subjected to different types of exercise (Fig. 6c) and out of these, were genes like ETS2 Repressor Factor (ERF) and Insulin like growth factor 2 (IGF2). ERF is important for cellular proliferation and IGF2 is critical for normal muscle growth, and is also associated with aging hallmarks83 (Fig. 6c). A total of 8 genes were differentially expressed in the older group subjected to different exercise type (Fig. 6d), including Laminin Subunit Alpha 4 (LAMA4) and FABP5. We also observed differences in differentially expressed genes based on the age of the subjects. For example, MYH9 and Transforming Growth Factor Beta 1 (TGFB1) were upregulated in young subjects post resistance exercise while were not differentially expressed among older subjects. The voltage ion channel gene VDAC1 was significantly downregulated among young subjects post high intensity exercise. The core-clock genes PER2, PER3, CRY2, and NR1D1 were significantly downregulated among older subjects in at least one of the exercise groups vs. pre-exercise. In addition, we also extracted the set of genes that were differentially expressed among young, as well as in older subjects depending on the exercise type. A total of 33 common genes were differentially expressed in both age groups during resistance exercise, out of which, there were skeletal muscle-associated genes like Emerin (EMD) and Leimodin 1 (LMOD1). EMD is important for cytoskeleton organization and its absence or defect is seen among Emery-Dreifuss muscular dystrophy84, while LMOD1 is associated with muscle contraction. A total of 80 genes were differentially expressed in both the young and older subjects during high intensity exercise, out of which were ATF1, linked with hypoxia response in muscle, and MYH10, crucial for myogenesis. 22 genes were common between young and older subjects from combined exercise, including myonuclei related gene DCTN1 and mitochondrial gene MT-CO2.
Furthermore, we investigated the alterations in the molecular profile of clock- and skeletal muscle- associated pathways in mice due to fasting (Fig. 6e, f). Interestingly, we observed higher number of ~24 h rhythmic gene sets in the fasting group (723 genes) vs. ad libitum group (337 genes). Moreover, we also observed an overall difference in the acrophase and amplitude between the two groups (Fig. 6e). Myh3, Myh11, Dctn2, and Dctn4 were ~24 h rhythmic in the fasting group when compared to the ad libitum group. A total of 1131 genes showed differential expression in fasting vs. ad libitum group, and out of them, 363 genes were downregulated, e.g., Myod1, Cry1, Per3, and Dbp and 768 genes were upregulated, e.g., Per1, Myh3, Dctn2, Npas2, Rorc, Mtor, Sun1, and Cry2 (Fig. 6f).
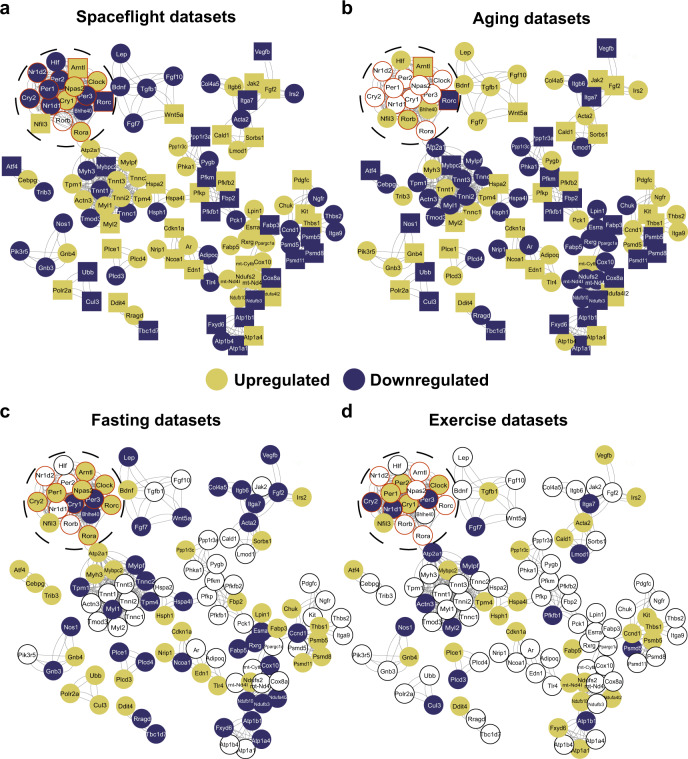
We further identified specific molecular alterations by retrieving the gene sets that were differentially expressed in at least one of the long-term spaceflight datasets (37 days) and in the older age group (Age group V vs. I (GSE129643) or in Age group II vs. I (GSE97084)). A total of 206 common genes were differentially expressed between long-term spaceflight and aging condition datasets. Using Cytoscape plugins (STRING and MCODE), we visualized the interaction between the obtained genes in spaceflight, aging, exercise, and fasting condition datasets, and included core-clock genes to the network even if they were not differentially expressed in the two conditions (Fig. 7a–d). Circadian clock related genes including Arntl, Bhlhe40, Cry2, Rorc and skeletal muscle-associated genes like Wnt family member 5A (Wnt5a), Atf4, Vascular endothelial growth factor beta (Vegfb), Cdkn1a, Myl2, Ndufa4l2, Fabp3, Ndufb3, Fgf2, Cul3, Acta2, Leptin (Lep), Actn3, and Heat shock protein family A member 8 (Hspa8) were differentially expressed in at least one of the long-term spaceflights, and aging condition datasets. Arntl was upregulated in the aging, spaceflight, and fasting condition datasets. In contrast, Rorc was downregulated in spaceflight (post 37 days) and aging condition datasets, while upregulated in the fasting condition dataset (Fig. 7). Myl2 was significantly upregulated in spaceflight and aging condition datasets, but upregulated in at least one of the exercise condition datasets. Wnt5a, which is known to promote myogenesis was upregulated in Space and aging condition datasets while, its expression was downregulated in fasting condition datasets. Atf4/ATF4 known to be associated with muscle atrophy and also with aging phenotype85 was significantly downregulated in Space and aging-related datasets, while its expression was upregulated in fasting condition dataset and significantly downregulated in young human participants subjected to 12-weeks of high-intensity exercise. Altogether, our analysis identified a set of genes with molecular profiles altered during spaceflight (especially long-term) or aging condition datasets, which can potentially be regulated by using external Zeitgebers to recover altered phenotypes associated with circadian dysregulation.
Fig. 7. Network representation of differential expressed genes altered in both spaceflight and aging datasets and their association with core-clock elements.
206 common genes were differentially expressed in at least one of (a) the long-term spaceflight datasets (37 days) and (b) in extreme age groups (older vs. young). In addition, core-clock elements (bold circles with red border) were also added to the network to explore the regulatory role of circadian clock machinery. Network analysis was carried out using STRING and MCODE, cytoscape based plugins. The same gene sets were plotted for (c) fasting and (d) exercise datasets. The gene sets were color coded based on their up- or down-regulation compared to their respective controls. Set of genes that depicted similar pattern (up or down-regulation) in spaceflight and aging datasets were shown as rectangles. Genes with no differential expression are represented as white circles.
Discussion
The European Space Agency (ESA) and the National Aeronautics and Space Administration (NASA) recently started to use Space omics technology in cells, animals and astronauts in spaceflight86–88. A number of clock genes with epigenetic modifications was reported through the fundamental Space omics research carried out by the NASA GeneLab project87. Such microgravity-triggered epigenetic modifications associated with clock genes was also seen in late pregnant rats89, thereby supporting the notion of epigenetic modifications triggered by microgravity in cells, small animals, and during development89. In a recent study using transcriptomics data, asynchrony among clock genes were reported in different peripheral tissues of space flown rodents52. In the retina from 37 days space flown mice onboard the ISS, for example, a number of genes were differently methylated with spaceflight vs. ground control (sex and age-matched) suggesting that microgravity decelerated the retinal clock at both epigenomic and transcriptomic levels with potential impact on eye-related disorders such as spaceflight-associated neuro-ocular syndrome including optic disc edema, seen among astronauts90. However, detailed molecular insights regarding circadian dysregulation specific to skeletal muscle due to different gravity environments is still lacking and is most relevant.
Circadian rhythms play a regulatory role in the skeletal muscle via processes like myogenesis, transcription of specific genes, and metabolism5. Our analysis strengthens such results and shows circadian expression of several genes that are important for skeletal muscle mass, as well as in elements of the circadian clock network in mammalian skeletal muscle datasets. Myonuclear positioning is important for normal muscle function and its dysregulation has been linked to pathologies like muscle dystrophies91. SUN2 gene is crucial for myonuclear positioning and its dysregulation affects cytoskeleton organization92. We observed clock-regulated expression of SUN2 gene in both human and WT mouse datasets. However, SUN2 circadian expression was not seen in clock manipulated mammalian datasets, highlighting a role for the clock in myonuclear organization. MYOG gene is essential for skeletal muscle homeostasis, and it also showed circadian expression in healthy human circadian datasets. Myog has been reported to regulate myocyte fusion, and its loss led to alterations in mTOR signalling in muscle cells93. Moreover, clock-regulated expression of MYOG was reported previously in rabbits, and night-restricted feeding also resulted in its increased expression94. Skeletal muscle differentiation is essential for development where MYH3 plays an important role95. Interestingly, our results show that MYH3 is circadian in skeletal muscle in both human and WT mice datasets. Such examples of clock-regulated genes strengthen the role of the circadian clock in skeletal muscle development.
In this study, we found that several genes undergo similar alterations due to spaceflight, as well as a result of aging on Earth. Extrinsic factors like exercise or fasting represent possible interventions that can help to minimize the molecular alterations resulting from spaceflight and/or aging on Earth. To overcome the lack of time-course datasets for spaceflight and aging conditions, we carried out differential expression analysis between space flown/aged groups and their respective controls, and used the circadian datasets derived from human and mouse skeletal muscle to visualize possible circadian variations in gene expression. Our analysis showed that the skeletal muscle-associated pathways are clock regulated in both human and mouse datasets, and core-clock alterations can result in similar molecular pattern as seen in spaceflight datasets. For example, skeletal muscle-associated genes like Nfat5, Fos, and Myod1 showed circadian expression in WT mouse and healthy human datasets while their rhythmicity was changed in clock altered tissues, in a mouse model. Nfat5 showed loss of rhythmicity in both the mouse core-clock altered datasets, and its expression was upregulated in at least one of the spaceflight datasets. Nfat5 is important for myoblast migration required for skeletal muscle regeneration and its deletion in a mouse model depicted a defect on muscle regeneration96. Myod1 showed phase shift with mBmal1KO vs. WT and its expression was also upregulated in both mBmal1KO and in at least one of the spaceflight datasets. Myod1 is the key regulator of skeletal muscle differentiation97 and its deletion in mouse skeletal muscle stem cells resulted in the inhibition of skeletal muscle regeneration98. We observed similar alterations in clock genes, such as Cry2, Nr1d2, Dbp, and Per2, which were downregulated due to both the mutation in Clock gene and also due to spaceflight. Dbp downregulation due to spaceflight was reported previously in different peripheral tissues from spaceflight experiments51,52. Interestingly, in datasets derived from patients with neurodegenerative diseases like Parkinson’s, an upregulation of DBP was reported among patients as compared to the healthy control groups99. This highlight potential implications of spaceflights in neurodegeneration and further research in this direction will be needed. Our observations point towards common molecular alterations resulting due to spaceflight and molecular perturbations of the circadian system and putative health impact for astronauts. Further studies are needed to pinpoint the specific impact of core-clock elements alterations on skeletal muscle signalling in mammalian tissue on Earth and in Space.
In addition, long-term spaceflights resulted in severe molecular alterations in clock- and skeletal muscle-associated pathways. In particular, the differential gene regulation observed during long-term spaceflight datasets resembled expression changes due to aging condition on Earth. In particular, skeletal muscle-associated genes like Atf4, Ndufa4l2, Fabp3, Cul3, Fgf2, and Wnt5a showed similar pattern (up-/down-regulation) in both spaceflight (post 37 days) and in aging condition datasets, as compared to the respective controls. Our analysis also shows a differential regulation of these genes found in fasting or exercise condition datasets, that can potentially serve as an external factor to minimize the circadian alterations in skeletal muscle. Moreover, several genes gained rhythmicity under fasting conditions, reflecting a tissue-specific and time-of-day dependent response to eating behaviour. Time-restricted feeding or caloric restriction may serve as a practicable alternative to minimize circadian alterations applicable to the daily routine of astronauts in Space. Indeed, the positive impact of time-restricted feeding on muscle function was reported both on Drosophila100 and rodents101–103 and may be a feasible intervention during spaceflights, also applicable to aging on Earth. Although fruit fly muscle pathology may not be comparable 1:1 to diseased vertebrate or mammalian skeletal muscle pathology, some of the obesity-induced changes reported in Drosophila muscle may serve as proof-of-concept for circadian rhythm-associated muscle dysfunction linked to extreme feeding conditions100. In fact, in 13 days space flown Drosophila (Shenzhou-9 spaceship) disrupted circadian rhythms resulted in altered lipid metabolism and life span104. In addition, caloric restriction, which involves time restricted feeding of less than 6 h has been shown to improve longevity in mammals, but so far not in Drosophila105,106. Applying such caloric restriction to astronauts may be less feasible due to their mission related energy balance, but it might still be an interesting approach to minimize age-related circadian dysregulation on Earth.
Previous studies, in healthy participants and athletes, reported the influence of exercise on skeletal muscle and performance based on the time of day107–110. Specific genes have been associated to performance of the skeletal muscle and thus are also interesting targets, which might be altered through exercise. Among those, Atf4 was downregulated in Space and aging condition datasets while its expression was upregulated in fasting and exercise (based on the type) condition datasets. Atf4 encodes a DNA-binding protein that functions as a leucine zipper transcription factor and plays an important role in mediating cellular stress responses. In immobilized mice, Atf4 is highly expressed in skeletal muscle and induces muscle fibre atrophy111. Whereas, Ndufa4l2 was upregulated in Space, aging and exercise condition datasets, its expression was downregulated under fasting conditions. Ndufa4l2 encodes a protein that is a subunit of NADH dehydrogenase (Complex I) and part of the respiratory chain in mitochondria. Its expression can be induced by hypoxic stimuli and results in decreased mitochondrial respiratory activity in order to keep levels of reactive oxygen species (ROS) as low as possible, but also leads to less important intramuscular metabolites (e.g. adenine nucleotides, NAD + )112. Fabp3 gene, associated with fatty acid metabolism, was downregulated in Space and aging condition while it was upregulated in fasting condition datasets. FABP3 modulates age-dependent lipid remodelling and its overexpression can cause ER stress and defective protein synthesis in skeletal muscle113. Fgf2, which encodes the growth factor and signalling protein was significantly upregulated in spaceflight and aging condition datasets, while it was downregulated in fasting condition dataset. Fgf2 plays an important role in the bone-muscle crosstalk and is mainly expressed by mesenchymal-derived stromal cells (e.g., fibroblasts/fibrocytes), osteoblasts but also skeletal myocytes. It can act as both promotor and inhibitor of osteoblastogenesis. In case of muscle injury, FGF-2, stored in the sarcoplasm of skeletal myofibers, is released and triggers an anabolic effect114. Wnt5a gene was downregulated in spaceflight and aging condition datasets while its expression was upregulated in fasting condition datasets. The Wnt signalling pathway is involved in cellular differentiation and proliferation in adult tissue. Wnt5a regulates the expression of MyoD and Myf5 that play an important role in myogenesis of skeletal muscle115. Through our preliminary analysis, we highlight the potential applications of either exercise or fasting as a countermeasure against molecular alterations due to aging on Earth or long-term spaceflight. For example, in the case of Ndufa4l2, fasting can serve as a countermeasure to minimize the alterations in gene expression profile (Fig. 8). Nevertheless, due to the limited availability of circadian datasets from the literature a comprehensive evaluation of the molecular circadian profile in datasets from space flown mice and aged human vs. their controls remain to be established by further studies.
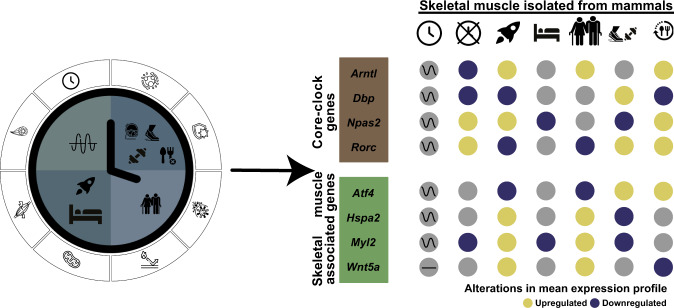
Fig. 8. Graphical representation of the study and main results.
This study mainly focused on investigating molecular changes in skeletal muscle-associated and circadian rhythm-associated pathways such as metabolism, myonuclei, myogenesis (left side; symbols) in healthy skeletal muscle, and altered conditions (i.e., clock manipulation, spaceflight, bed rest, aging, exercise, fasting) from left to right order. Core-clock genes and skeletal muscle-associated genes depicted similar patterns (upregulation: yellow; downregulation: blue) in gene expression profiles due to spaceflight and aging on Earth (e.g. Rorc, Atf4; right side). While exercise or fasting conditions showed opposite gene expression patterns in the same genes.
In future deep Space exploration, the duration and distance of Space travel impose great risks to the Crew´s health with the need to find smart countermeasures, thus mitigating such mission-related risks for both astronaut and work schedule. The outcome of our study supports the hypothesis of microgravity-triggered circadian clock changes in skeletal muscle-related pathways, found in studies with mice, bedrest or astronauts in spaceflight. Future experiments will be needed to further validate our findings and explore more insights to circadian regulation resulting from spaceflight using time-course experiments. Moreover, the current observations are retrieved from mouse and human studies and with different muscle types (slow vs. fast twitch), that are affected differently in microgravity conditions, and would be relevant to consider in following studies.
The obvious question will be how such knowledge may be translated to optimize countermeasures to mitigate or even prevent circadian dysregulation in future space missions. Monitoring the circadian rhythms will likely become an integral part of space missions, and new easy-to-use and non-invasive methods will be required for it107. Circadian rhythm-dependent muscle signalling and function nevertheless imposes a yet underestimated, but significant challenge not only for clinical cohorts suffering from various neuro-musculoskeletal disorders on Earth, but also for Space travellers health and performance in future missions with crewed spacecrafts and planetary habitats utilized for Deep Space and Planetary Exploration of Space Agencies to Moon and Mars.
Methods
Acquisition of publicly available RNA-seq datasets
Using a criterion of “skeletal muscle”, “mammalian tissue”, and “RNA-seq” on open source repositories (NCBI-GEO/ArrayExpress/NASA GeneLab), we obtained a total of 534 samples from 14 different datasets. Out of 14 RNA-seq datasets, 4 datasets were retrieved from healthy humans and 10 datasets were retrieved from mice.
Based on the human data, we collected RNA-seq datasets derived from:
Vastus lateralis (thigh) muscle biopsies collected from healthy subjects at 12:00 h–08:00 h, every 4 h (n = 9 (8 males and 1 female); Age = 29.9 ± 9.8 years; Accession number: GSE108539116);
Gluteus maximus (hip) muscle biopsies collected from healthy male subjects (n = 2; Age = 61.1 ± 1 years). Primary skeletal myoblasts were purified from the biopsies and differentiated into myotubes, which were transfected either with siControl or siCLOCK. siRNA transfection in cultured primary human skeletal myotubes resulted in the disruption of CLOCK rhythms, and also its downregulation compared to the untreated control cells116. Post-synchronization, samples were collected every 2 h from 0 h–48 h (Accession number: GSE109825116);
Vastus lateralis (thigh) muscle biopsies collected from healthy young and older subjects (sex and age matched) who underwent different exercise regimes. All subjects were randomly divided into: High-intensity interval exercise (HIIT; young (n = 14; Mean ± SD: 25.4 ± 4.3 years); older (n = 9; Mean ± SD: 70.7 ± 4.6 years)), Resistance exercise (RT; young (n = 11; Mean ± SD: 23.7 ± 3.5 years); older (n = 9; Mean ± SD: 70.3 ± 3.9 years)), and Combined exercise (CT: Resistance + high-intensity; young (n = 9; Mean ± SD: 26.3 ± 2.7 years); older (n = 8; Mean ± SD: 68.6 ± 3.4 years)). Biopsies were collected pre-exercise (baseline) and post-12-weeks exercise. Vastus lateralis (thigh) muscle biopsies were collected from young and older participants in the morning at 10 h (Accession number: GSE97084117);
Vastus lateralis (thigh) muscle biopsies collected from healthy male and female subjects (n = 58; Accession number: GSE129643118) from different age groups (20–34 years, n = 13; 35–49 years, n = 11; 50–64 years, n = 12; 65–79 years, n = 12; 80+ years, n = 10).
Based on the mouse model system, there were RNA-seq datasets derived from:
Gastrocnemius (calf) muscle collected from male C57BL/6 mice either subjected to ad libitum normal chow feeding (FED) or 24 h fasting (FAST) under 12 h light/12 h dark cycle. Samples were collected every 4 h from ZT0-ZT20 (n = 3 per time point per group; Accession number: GSE107787119). This is the only time course dataset available on feeding/fasting, based on our selection criteria;
Gastrocnemius (calf) muscle collected from low response exercise and high response exercise male rats before and after 8-weeks exercise program (Accession number: GSE155230120);
Gastrocnemius (calf) muscle from male C57BL/6 mice collected at ZT14 (early) and ZT22 (late) from basal, moderate, and high intensity running protocol (Accession number: GSE117161121);
Gastrocnemius (calf) and glycolytic quadriceps muscles collected from male C57BL/6Jrj mice with/without acute treadmill and chronic wheel running exercise at different times of the day (Accession number: GSE178262122);
Gastrocnemius (calf) muscle collected from female C57BL/6 N mice subjected to 33 days in spaceflight and their ground control (Accession number: GSE156321123). In addition, muscle samples were collected from un-injected mice post 33 days in spaceflight and their ground controls. The mice remained on-board of the ISS until the departure of SpaceX on January 7, 2020 and were delivered live to Explora Biolabs ∼32 h after splashdown in the Pacific Ocean (live animal return, LAR). The un-injected space flown and ground control datasets used in our analysis were retrieved from mice that were euthanized for analysis within the first 8 h after LAR123.
Different muscle tissues were collected from female C57BL/6 J mice subjected to 37 days in spaceflight (microgravity) and their ground controls, (namely 6) Extensor digitorum longus (foot lever) muscle (Accession number: GLDS-99),
Gastrocnemius (calf) muscle (Accession number: GLDS-101),
Quadriceps muscle (Accession number: GLDS-103),
Soleus (deep calf) muscle (Accession number: GLDS-104), and
Tibialis anterior muscle (Accession number: GLDS-105). For the mice used in the studies (6–10), carcasses were frozen in a pre-chilled Mini Cold Bag (MCB) before transfer to the MELFI freezer (−80 °C) and brought back to Earth where dissection was held. The mice in the ground control group also followed the same protocol. Total dissection time for each carcass was no longer than 30 min since collection of the first tissue.
The summary of omics datasets used in this study is provided in the Supplementary file 1.
Acquisition of publicly available Microarray datasets
Using a criterion of “skeletal muscle”, “mammalian tissue”, and “Microarray” in open source repositories (NCBI-GEO/ArrayExpress/NASA GeneLab), we obtained a total of 485 samples from 10 different datasets. Out of 10 microarray datasets, four datasets were retrieved from healthy humans and six datasets were retrieved from mice.
Based on the human samples, we collected microarray datasets derived from:
Soleus and Vastus lateralis muscle biopsies collected from healthy female pre- and post-60 days bedrest (BR; Accession number: GSE14798124). The subjects were randomly divided into: BRC (Age (Mean ± SD) = 34 ± 3 years; n = 8; bedrest alone), BRE (Age = 32 ± 3 years, n = 8; bedrest combined with exercise), and BRN (Age = 29 ± 3 years, n = 8; bedrest combined with protein supplements);
Vastus lateralis muscle biopsies collected from healthy male subjects pre- and post-21 days normoxic bedrest (Age (Mean ± SD) = 27 ± 6 years, n = 14; Accession number: GSE104999125);
Vastus lateralis muscle biopsies collected from healthy male pre- and post-90 days bedrest (Accession number: GSE148152126). The subjects were randomly divided into: BR (Age (Mean ± SD) = 33 ± 5 years; n = 9; bedrest alone) and BRE (Age (Mean ± SD) = 32 ± 4 years; n = 12; bedrest combined with exercise);
Vastus lateralis muscle biopsies collected from healthy male pre- and post-9 days bedrest (Age = 24–27 years, Accession number: GLDS-370). In addition, the subjects completed 4-weeks retraining program post-BR and biopsies were collected.
Based on the mouse samples, there were microarray datasets derived from:
Gastrocnemius (calf) muscle collected from male C57BL/6 mice every 2 h from CT18-CT64 (Accession number: GSE546509);
Tibialis anterior and Soleus muscles collected from WT and muscle specific Bmal1 KO mice every 4 h from ZT0-ZT20 (Accession number: GSE43071127). In mBmal1 KO mice, the region coding for the BMAL1 basic helix–loop–helix DNA binding domain was excised127;
Gastrocnemius (calf) muscle collected from male C57BL/6 J WT and Clock mutant mice every 4 h from CT22-CT46 (Accession number: GSE3746128). The Clock mutation in mice is a dominant negative (antimorphic) mutation that deletes exon 19 and causes an internal deletion of 51aa in the COOH-terminal activation domain of the clock protein128;
Longissimus dorsi (back) muscle collected from male C57BL/N6 mice subjected to 30 days in Bion-M1 spaceflight (microgravity; BF), Bion ground (BG) subjected to same habitat of space flown mice but exposed to gravity and flight controls in standard animal facility for the same time period. Both the space flown and the ground control mice were sacrificed on the same day within 12–14 h post-landing (Accession number: GSE94381129);
Soleus and Extensor digitorum longus muscles collected from male C57BL/N6 mice subjected to 30 days in Bion-M1 spaceflight, Bion ground subjected to same habitat of space flown mice but exposed to gravity, and flight controls in standard animal facility for the same time period. Both the space flown and the ground control mice were sacrificed on the same day within 12–14 h post-landing (Accession number: GSE80223130);
Gastrocnemius (calf) muscle collected from mice subjected to 11 days 19 h in STS-108 spaceflight and the controls in standard animal facility for same period. The space flown and ground control mice were sacrificed within 3.5–4 h after landing (Accession number: GSE10533131). In addition, different ground-based mice were subjected to 12 days hindlimb suspension or hindlimb suspension +3.5 h reloading and the controls. For more details about the microarray datasets used in this study, please refer to the Supplementary file 1.
Acquisition of publicly available LC-MS datasets
Using a criterion of “skeletal muscle”, “mammalian tissue”, and “Proteomics” in open source repositories (PRIDE), we obtained a total of 108 samples from 3 different datasets. All three LC-MS datasets were retrieved from the mouse model system.
The LC-MS datasets were derived from:
Soleus and Extensor digitorum longus (EDL) muscles collected from male C57BL/6 J mice followed by 28 days in hypergravity (3 g) and their corresponding ground controls (1 g; Accession number: PXD017240132);
Supraspinatus (shoulder) muscle collected from female C57BL/6 mice subjected to 13 days in STS-135 and male C57BL/6 N mice subjected to 30 days in Bion-M1 spaceflight and their corresponding ground controls (Accession number: PXD006764133);
Vastus lateralis, Soleus and Extensor digitorum longus (EDL) muscles collected from male C57BL/6 mice subjected to 30 days in Bion-M1 spaceflight and their corresponding ground controls. Additional, EDL muscle tissues were collected from mice subjected to 8 days recovery post-flight and their control group (Accession number: PXD005035134).
For more details about the datasets used in this study, please refer to the Supplementary file 1.
RNA-seq data analysis
For RNA-seq datasets, raw sequencing reads (fastq files) were retrieved from the NCBI-GEO and used for the pre-processing and downstream analysis. Quality assessment of raw RNA-seq reads were carried out using fastqcr R package (version 0.1.2), which helps in easy parsing and aggregation of FastQC135. Based on the FastQC reports, the respective adapter sequences and over-represented reads were trimmed from sequencing reads using Trimmomatic (version 0.39136) using default settings. After trimming, paired/single-end reads were aligned to their respective reference genome (human, mouse, and rat based on datasets). Paired/single-end reads from human datasets were aligned to human genome (Homo sapiens GRCh38, Ensembl release 105), from mouse datasets were aligned to mouse genome (Mus musculus GRCm39, Ensembl release 105), and from rat datasets were aligned to rat genome (Rattus norvegicus mRatBN7.2, Ensembl release 105) using STAR aligner (version 2.7.0137). Post-alignment, transcript-level abundances were quantified using Salmon (version 1.7.0138) in transcripts per million (TPM). Afterwards, tximport R package (version 1.22.0139) was used to import transcript-level abundance, estimate counts, and transcript lengths. After obtaining gene-level summarization from Tximport (txOut = FALSE), normalization was carried out using TMM method within edgeR package (version 3.36.0140). All gene features with at least 0.5 Counts per million (CPM) on average (specific to datasets) were retained and renormalized using selected features. The complete pipeline for the analysis is depicted in Fig. 1.
Microarray data analysis
For microarray datasets, raw intensity files (CEL for Affymetrix platform and TXT for Illumina platform) were retrieved from the NCBI-GEO for the downstream analysis. Probe intensities were retrieved from raw data using limma (version 3.50.3141) or oligo (version 1.58.0142) R package based on the type of microarray datasets. Pre-processing and normalization of expression levels was carried out using Robust Multi-Array Average (RMA) procedure as implemented in limma or oligo R package. ArrayQualityMetrics R package (version 3.50.0143) was used for quality control and statistical testing of the arrays. No outliers were identified. The datasets were annotated based on the associated platform annotation file available on NCBI-GEO. For the set of genes that mapped to multiple probes, the probe with the highest average expression was retained.
LC-MS data analysis
For protein datasets, raw intensity values were retrieved from the PRIDE database for the downstream analysis. MS spectra peaks detection and quantification was carried out using a standalone software MaxQuant (version 2.0.3.1144). It supports all main labeling techniques such as Tandem Mass Tag (TMT), as well as label-free quantification. MaxQuant performs mass calibration and database searches for protein identification, which later get quantified. Post quantification, the resulting evidence file (identified peptides and intensity values) from MaxQuant was used for downstream analysis. For the datasets (PXD017240, PXD006764, PXD005035), normalization was carried out using proteusLabelFree vignette within Proteus R package145.
Rhythmicity analysis
Out of the retrieved datasets, there were three circadian RNA-seq (GSE108539, GSE109825, GSE107787) and three circadian microarray (GSE54650, GSE43071, GSE3746) datasets. Unlogged CPM values (in case of RNA-seq) and normalized expression values (in case of microarray) were used to detect 24 h rhythmic signals using RAIN R package (version 1.28.0146). Following multiple test correction of RAIN p-values using Benjamini-Hochberg (BH) procedure circadian (24 h rhythmic) genes were obtained using a cut-off of q < 0.05. The acrophase and relative amplitude were estimated for circadian gene-sets using Cosinor within Discorhythm R package (version 1.6.0147).
Differential rhythmicity analysis
To detect the changes in circadian parameters (acrophase, amplitude) due to clock alterations or fasting, differentially rhythmicity analysis was carried out using Limorhyde R package148. After pairwise comparison (KO vs. WT) and q < 0.05, the list of genes that lost ~24 h rhythmicity, gained ~24 h rhythmicity, and phase-shifted (≥4 h) due to specific core-clock element deletion were obtained.
Differential expression analysis
For the circadian RNA-seq and microarray datasets, differential expression analysis was carried out using limma within Limorhyde R package148. For the protein datasets, differential expression analysis was carried out using limma within Proteus R package145. For all other datasets, differential expression analysis was carried out directly using limma R package (version 3.50.3141). A cut-off of nominal p < 0.01 and a log fold change (FC) ≥ | 0.2| was used to obtain significantly up- or down-regulated gene sets.
Network analysis
To gain further insight into the interactions between gene sets that were differentially expressed between spaceflight (post-37 days) and aging (80+ years vs. 20–34 years or 60–75 years vs. 20–30 years), network analysis using Cytoscape (version 3.9.1149) was carried out. Interactions between shortlisted genes were obtained using STRING150 plugin and clustered using Molecular Complex Detection plugin (MCODE151) within Cytoscape.
Curation of skeletal muscle and circadian clock associated pathways
Signalling pathways associated with skeletal muscle and circadian rhythms were retrieved from the Kyoto Encyclopedia of Genes and Genomes (KEGG66) using KEGGREST R package (version 1.36.0152) and manually downloaded from the Reactome67 database.
Using KEGG, the retrieved pathways associated with skeletal muscle were: (1) Adipocytokine signalling (hsa04920; 69 genes) where adipocytokines play a crucial role in stimulating glucose update within skeletal muscle153, (2) AMP-activated protein kinase signalling (hsa04152; 120 genes) regulates glucose and lipid metabolism154, (3) Calcium signalling (hsa04020; 240 genes), plays a crucial role in myoblast proliferation and differentiation155, (4) cAMP signalling (hsa04024; 221 genes), which contributes to changes in myofibers156 (5) FoxO signalling (hsa04068; 131 genes), essential for disuse muscle atrophy157, (6) Growth hormone synthesis (hsa04935; 119 genes), crucial for muscle strength158, (7) Insulin resistance (hsa04931; 108 genes), characterized by elevated fasting glucose level159, (8) Insulin signalling (hsa04910; 137 genes), increases glucose update and metabolism within skeletal muscle, (9) Mannose type O glycan biosynthesis (hsa00515; 23 genes), important for metabolism, (10) MAPK signalling (hsa04010; 97 genes), one of the main regulators of metabolism in response to stress160, (11) Mineral absorption (hsa04978; 60 genes), essential for skeletal muscle mass (12) mTOR signalling (hsa04150; 155 genes), helps in the maintenance of muscle mass161, (13) Oxidative phosphorylation (hsa00190; 134 genes), provides primary energy source for metabolism, (14) Pi3k-Akt signalling (hsa04151; 354 genes), crucial for skeletal mass development162, (15) PPAR signalling (hsa03320; 75 genes), plays an important role in development, inflammation, and metabolism163, and (16) Vascular smooth muscle contraction (hsa04270; 134 genes), crucial for muscle contraction.
Using Reactome, the retrieved pathways associated with skeletal muscle were: (1) Calcineurin activates NFAT (R-HSA-2025928; 9 genes), crucial for skeletal muscle maintenance, (2) Cellular response to heat stress (R-HAS-3371556; 101 genes), associated with cell survival, (3) Cellular response to stress (R-HSA-2262752; 749 genes), (4) Growth hormone receptor signalling (R-HSA-982772; 24 genes), (5) Mitochondrial biogenesis (R-HSA-1592230; 96 genes), a major adaptation of skeletal muscle to exercise training164, (6) mTOR signalling (R-HSA-165159; 41 genes), (7) Muscle contraction (R-HSA-397014; 196 genes), (8) Myogenesis (R-HSA-525793; 29 genes), (9) Oxidative stress induced senescence (R-HSA-2559580; 95 genes), (10) Pi3K-Akt activation (R-HSA-198203; 9 genes), (11) Smooth muscle contraction (R-HSA-445355; 39 genes), and (12) Striated muscle contraction (R-HSA-390522; 36 genes).
In addition, change in skeletal mass during exercise or unloading is associated with the nuclei of muscle fibres (myonuclei165). Therefore, we additionally retrieved myonuclei associated genes (43 genes) from the literature68,69.
Using KEGG, the retrieved pathways associated with circadian rhythms were: (1) Circadian entrainment (hsa04713; 97 genes), and (2) Circadian rhythm (hsa04710; 31 genes). Using Reactome, the retrieved pathways associated with circadian rhythm was Circadian clock (R-HSA-400253; 70 genes). In addition, we included a network of circadian regulated genes (NCRG; 161 genes) previously published by our group26. After combining the skeletal muscle and circadian rhythms associated genes, we obtained a unique set of 2251 genes (in human) and their orthologous sets in mouse (2135 genes) and rat (2161 genes) using Biomart166. For the complete gene lists, please refer to the Supplementary file 2–4.
Correlation analysis
Pearson correlation coefficient was calculated for the set of core-clock genes in spaceflight and aging datasets using the R function cor(). In addition, we used rcorr() function built in the R package Hmisc (CRAN - Package Hmisc (r-project.org)) to compute the significance levels for Pearson correlation.
Supplementary information
Acknowledgements
We are grateful to all members of Relógio group, as well as to the reviewers of the manuscript for their critical remarks and feedback. Vector icons used in this manuscript were obtained from Flaticon (https://www.flaticon.com/) and modified accordingly. The work in the group of A.R. was funded by the Dr. Rolf M. Schwiete Stiftung. M.Y. was additionally funded by the Berlin School of Integrative Oncology (BSIO) graduate program of the Charité Medical University Berlin and by the Einstein Foundation. D.B. and B.S. were supported by a grant from the Federal Department of Economy and Climate Protection (BMWK) through the German Space Agency, Deutsches Zentrum für Luft- und Raumfahrt (DLR e.V., Bonn-Oberkassel, Germany, #50WB2029 to D.B.).
Author contributions
A.R. conceptualized the study, attained the funding, carried out the investigation, provided supervision, prepared the initial draft, reviewed and revised the manuscript. D.M. conceptualized the study, carried out the investigation, carried out the omics data analysis, visualization, prepared the initial draft, reviewed and revised the manuscript. M.Y. carried out the investigation, carried out omics data analysis, visualization, reviewed and revised the manuscript. B.S. carried out the investigation, reviewed and revised the manuscript. D.B. attained the funding, provided supervision, carried out the investigation, reviewed and revised the manuscript. All authors have read and agreed to the final version of the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Data availability
The datasets used in this study were retrieved from open-access public repositories and are available as follows: (1) Circadian RNA-seq datasets derived from human skeletal muscle (NCBI-GEO, Accession number: GSE108539, GSE109825), (2) Circadian microarray datasets derived from mouse skeletal muscle (NCBI-GEO, Accession number: GSE54650, GSE43071, GSE3746), (3) Spaceflight omics datasets derived from mouse skeletal muscle (NASA GeneLab: GLDS-99/-101/-103/-104/-105; NCBI-GEO, Accession number: GSE156321, GSE94381, GSE80223, GSE10533; PRIDE, Accession number: PXD006764, PXD005035), (4) Hypergravity associated proteomics data derived from mouse skeletal muscle (PRIDE, Accession number: PXD017240), (5) Bedrest associated microarray datasets derived from human skeletal muscle biopsies (NASA GeneLab: GLDS-370, NCBI-GEO, Accession number: GSE14798, GSE148152, GSE104999), (6) Aging associated RNA-seq datasets derived from human skeletal muscle biopsies (NCBI-GEO, Accession number: GSE97084, GSE129643), (7) Exercise associated RNA-seq datasets derived from human, mouse or rat skeletal muscle (NCBI-GEO, Accession number: GSE155230, GSE117161, GSE178262, GSE97084), and (8) Fasting associated RNA-seq dataset derived from mouse skeletal muscle (NCBI-GEO, Accession number: GSE107787).
Code availability
All programs, packages, and functions used in this manuscript are freely available and are referred in the Methods section.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41526-023-00273-4.
References
- 1.Frontera WR, Ochala J. Skeletal muscle: a brief review of structure and function. Calcif. Tissue Int. 2015;96:183–195. doi: 10.1007/s00223-014-9915-y. [DOI] [PubMed] [Google Scholar]
- 2.Anthony TG. Mechanisms of protein balance in skeletal muscle. Domest. Anim. Endocrinol. 2016;56:S23–S32. doi: 10.1016/j.domaniend.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kirkendall DT, Garrett WE., Jr. The effects of aging and training on skeletal muscle. Am. J. Sports Med. 1998;26:598–602. doi: 10.1177/03635465980260042401. [DOI] [PubMed] [Google Scholar]
- 4.Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet (Lond., Engl.) 2019;393:2636–2646. doi: 10.1016/S0140-6736(19)31138-9. [DOI] [PubMed] [Google Scholar]
- 5.Harfmann BD, Schroder EA, Esser KA. Circadian rhythms, the molecular clock, and skeletal muscle. J. Biol. Rhythms. 2015;30:84–94. doi: 10.1177/0748730414561638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bass J, Takahashi JS. Circadian integration of metabolism and energetics. Sci. (N. Y., N. Y.) 2010;330:1349–1354. doi: 10.1126/science.1195027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andrews JL, et al. CLOCK and BMAL1 regulate MyoD and are necessary for maintenance of skeletal muscle phenotype and function. Proc. Natl. Acad. Sci. U. S. A. 2010;107:19090–19095. doi: 10.1073/pnas.1014523107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scheiermann C, Kunisaki Y, Frenette PS. Circadian control of the immune system. Nat. Rev. Immunol. 2013;13:190–198. doi: 10.1038/nri3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang R, Lahens NF, Ballance HI, Hughes ME, Hogenesch JB. A circadian gene expression atlas in mammals: implications for biology and medicine. Proc. Natl Acad. Sci. USA. 2014;111:16219–16224. doi: 10.1073/pnas.1408886111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mure, L. S. et al. Diurnal transcriptome atlas of a primate across major neural and peripheral tissues. Science (New York, N.Y.)359 (2018). 10.1126/science.aao0318. [DOI] [PMC free article] [PubMed]
- 11.Saini C, Morf J, Stratmann M, Gos P, Schibler U. Simulated body temperature rhythms reveal the phase-shifting behavior and plasticity of mammalian circadian oscillators. Genes Dev. 2012;26:567–580. doi: 10.1101/gad.183251.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bollinger T, Schibler U. Circadian rhythms - from genes to physiology and disease. Swiss Med. Wkly. 2014;144:w13984. doi: 10.4414/smw.2014.13984. [DOI] [PubMed] [Google Scholar]
- 13.Andrade-Silva J, Cipolla-Neto J, Peliciari-Garcia RA. The in vitro maintenance of clock genes expression within the rat pineal gland under standard and norepinephrine-synchronized stimulation. Neurosci. Res. 2014;81-82:1–10. doi: 10.1016/j.neures.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 14.Ashton, A., Foster, R. G. & Jagannath, A. Photic entrainment of the circadian system. Int. J. Mole. Sci.23 (2022). 10.3390/ijms23020729. [DOI] [PMC free article] [PubMed]
- 15.Endo T, et al. Bright light improves sleep in patients with Parkinson’s disease: possible role of circadian restoration. Sci. Rep. 2020;10:7982. doi: 10.1038/s41598-020-64645-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yalçin M, et al. It’s about time: the circadian network as time-keeper for cognitive functioning, locomotor activity and mental health. Front. Physiol. 2022;13:873237. doi: 10.3389/fphys.2022.873237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neikrug AB, et al. Bright light therapy protects women from circadian rhythm desynchronization during chemotherapy for breast cancer. Behav. Sleep. Med. 2012;10:202–216. doi: 10.1080/15402002.2011.634940. [DOI] [PubMed] [Google Scholar]
- 18.Wu LM, et al. The effect of systematic light exposure on sleep in a mixed group of fatigued cancer survivors. J. Clin. Sleep. Med. 2018;14:31–39. doi: 10.5664/jcsm.6874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brainard GC, Barger LK, Soler RR, Hanifin JP. The development of lighting countermeasures for sleep disruption and circadian misalignment during spaceflight. Curr. Opin. Pulm. Med. 2016;22:535–544. doi: 10.1097/MCP.0000000000000329. [DOI] [PubMed] [Google Scholar]
- 20.Fucci RL, et al. Toward optimizing lighting as a countermeasure to sleep and circadian disruption in space flight. Acta Astronautica. 2005;56:1017–1024. doi: 10.1016/j.actaastro.2005.01.029. [DOI] [PubMed] [Google Scholar]
- 21.Sen S, et al. Ultradian feeding in mice not only affects the peripheral clock in the liver, but also the master clock in the brain. Chronobiol. Int. 2017;34:17–36. doi: 10.1080/07420528.2016.1231689. [DOI] [PubMed] [Google Scholar]
- 22.Martin, R. A. & Esser, K. A. Time for exercise? Exercise and its influence on the skeletal muscle clock. J. Biol. Rhythms, 7487304221122662 (2022). 10.1177/07487304221122662. [DOI] [PMC free article] [PubMed]
- 23.Sato S, et al. Atlas of exercise metabolism reveals time-dependent signatures of metabolic homeostasis. Cell Metab. 2022;34:329–345. e328. doi: 10.1016/j.cmet.2021.12.016. [DOI] [PubMed] [Google Scholar]
- 24.Mistlberger RE, Skene DJ. Social influences on mammalian circadian rhythms: animal and human studies. Biol. Rev. Camb. Philos. Soc. 2004;79:533–556. doi: 10.1017/S1464793103006353. [DOI] [PubMed] [Google Scholar]
- 25.Andreani TS, Itoh TQ, Yildirim E, Hwangbo DS, Allada R. Genetics of circadian rhythms. Sleep. Med. Clin. 2015;10:413–421. doi: 10.1016/j.jsmc.2015.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lehmann R, et al. Assembly of a comprehensive regulatory network for the mammalian circadian clock: a bioinformatics approach. PloS One. 2015;10:e0126283. doi: 10.1371/journal.pone.0126283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hesse, J. et al. An optimal time for treatment-predicting circadian time by machine learning and mathematical modelling. Cancers (Basel)12 (2020). 10.3390/cancers12113103. [DOI] [PMC free article] [PubMed]
- 28.Kondratov RV, Kondratova AA, Gorbacheva VY, Vykhovanets OV, Antoch MP. Early aging and age-related pathologies in mice deficient in BMAL1, the core componentof the circadian clock. Genes Dev. 2006;20:1868–1873. doi: 10.1101/gad.1432206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DiGirolamo DJ, Kiel DP, Esser KA. Bone and skeletal muscle: neighbors with close ties. J. Bone Miner. Res.: Off. J. Am. Soc. Bone Miner. Res. 2013;28:1509–1518. doi: 10.1002/jbmr.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Froy O. Circadian aspects of energy metabolism and aging. Ageing Res. Rev. 2013;12:931–940. doi: 10.1016/j.arr.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 31.Yamazaki S, et al. Effects of aging on central and peripheral mammalian clocks. Proc. Natl. Acad. Sci. U. S. A. 2002;99:10801–10806. doi: 10.1073/pnas.152318499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chang HC, Guarente L. SIRT1 mediates central circadian control in the SCN by a mechanism that decays with aging. Cell. 2013;153:1448–1460. doi: 10.1016/j.cell.2013.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Valentinuzzi VS, Scarbrough K, Takahashi JS, Turek FW. Effects of aging on the circadian rhythm of wheel-running activity in C57BL/6 mice. Am. J. Physiol. 1997;273:R1957–R1964. doi: 10.1152/ajpregu.1997.273.6.R1957. [DOI] [PubMed] [Google Scholar]
- 34.Brower RG. Consequences of bed rest. Crit. Care Med. 2009;37:S422–S428. doi: 10.1097/CCM.0b013e3181b6e30a. [DOI] [PubMed] [Google Scholar]
- 35.Stein TP. Nutrition and muscle loss in humans during spaceflight. Adv. space Biol. Med. 1999;7:49–97. doi: 10.1016/S1569-2574(08)60007-6. [DOI] [PubMed] [Google Scholar]
- 36.Stahn AC, et al. Increased core body temperature in astronauts during long-duration space missions. Sci. Rep. 2017;7:16180. doi: 10.1038/s41598-017-15560-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mendt S, et al. Long-term bed rest delays the circadian phase of core body temperature. Front. Physiol. 2021;12:658707. doi: 10.3389/fphys.2021.658707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Amani R, Gill T. Shiftworking, nutrition and obesity: implications for workforce health- a systematic review. Asia Pac. J. Clin. Nutr. 2013;22:505–515. doi: 10.6133/apjcn.2013.22.4.11. [DOI] [PubMed] [Google Scholar]
- 39.Filipski E, et al. Effects of light and food schedules on liver and tumor molecular clocks in mice. J. Natl. Cancer Inst. 2005;97:507–517. doi: 10.1093/jnci/dji083. [DOI] [PubMed] [Google Scholar]
- 40.Davidson AJ, et al. Chronic jet-lag increases mortality in aged mice. Curr. Biol.: CB. 2006;16:R914–R916. doi: 10.1016/j.cub.2006.09.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sigurdardottir LG, et al. Circadian disruption, sleep loss, and prostate cancer risk: a systematic review of epidemiologic studies. Cancer Epidemiol., Biomark. Prev. Publ. Am. Assoc. Cancer Res., Cosponsored Am. Soc. Preventive Oncol. 2012;21:1002–1011. doi: 10.1158/1055-9965.EPI-12-0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Richards J, Gumz ML. Mechanism of the circadian clock in physiology. Am. J. Physiol. Regulatory, Integr. Comp. Physiol. 2013;304:R1053–R1064. doi: 10.1152/ajpregu.00066.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang F, et al. The effect of jet lag on the human brain: a neuroimaging study. Hum. Brain Mapp. 2020;41:2281–2291. doi: 10.1002/hbm.24945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boivin DB, Boudreau P, Kosmadopoulos A. Disturbance of the Circadian System in Shift Work and Its Health Impact. J. Biol. Rhythms. 2022;37:3–28. doi: 10.1177/07487304211064218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Malik S, Stokes Iii J, Manne U, Singh R, Mishra MK. Understanding the significance of biological clock and its impact on cancer incidence. Cancer Lett. 2022;527:80–94. doi: 10.1016/j.canlet.2021.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Molina-Montes E, et al. Circadian clock gene variants and their link with chronotype, chrononutrition, sleeping patterns and obesity in the European prospective investigation into cancer and nutrition (EPIC) study. Clin. Nutr. (Edinb., Scotl.) 2022;41:1977–1990. doi: 10.1016/j.clnu.2022.07.027. [DOI] [PubMed] [Google Scholar]
- 47.Zeb F, et al. Time-restricted feeding regulates molecular mechanisms with involvement of circadian rhythm to prevent metabolic diseases. Nutrition. 2021;89:111244. doi: 10.1016/j.nut.2021.111244. [DOI] [PubMed] [Google Scholar]
- 48.Cheng Q, Lu C, Qian R. The circadian clock regulates metabolic responses to physical exercise. Chronobiol. Int. 2022;39:907–917. doi: 10.1080/07420528.2022.2050384. [DOI] [PubMed] [Google Scholar]
- 49.Sahu M, et al. Cross talk mechanism of disturbed sleep patterns in neurological and psychological disorders. Neurosci. Biobehav. Rev. 2022;140:104767. doi: 10.1016/j.neubiorev.2022.104767. [DOI] [PubMed] [Google Scholar]
- 50.Singla R, Mishra A, Cao R. The trilateral interactions between mammalian target of rapamycin (mTOR) signaling, the circadian clock, and psychiatric disorders: an emerging model. Transl. Psychiatry. 2022;12:355. doi: 10.1038/s41398-022-02120-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.da Silveira WA, et al. Comprehensive multi-omics analysis reveals mitochondrial stress as a central biological hub for spaceflight impact. Cell. 2020;183:1185–1201.e1120. doi: 10.1016/j.cell.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fujita, S. I., Rutter, L., Ong, Q. & Muratani, M. Integrated RNA-seq analysis indicates asynchrony in clock genes between tissues under spaceflight. Life (Basel, Switzerland)10 (2020). 10.3390/life10090196. [DOI] [PMC free article] [PubMed]
- 53.Otsuka K, et al. Circadian challenge of astronauts’ unconscious mind adapting to microgravity in space, estimated by heart rate variability. Sci. Rep. 2018;8:10381. doi: 10.1038/s41598-018-28740-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pandi-Perumal SR, Gonfalone AA. Sleep in space as a new medical frontier: the challenge of preserving normal sleep in the abnormal environment of space missions. Sleep. Sci. (Sao Paulo, Braz.) 2016;9:1–4. doi: 10.1016/j.slsci.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Guo JH, et al. Keeping the right time in space: importance of circadian clock and sleep for physiology and performance of astronauts. Mil. Med. Res. 2014;1:23. doi: 10.1186/2054-9369-1-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Flynn-Evans EE, Barger LK, Kubey AA, Sullivan JP, Czeisler CA. Circadian misalignment affects sleep and medication use before and during spaceflight. NPJ Microgravity. 2016;2:15019. doi: 10.1038/npjmgrav.2015.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cahill, T. et al. Mammalian and invertebrate models as complementary tools for gaining mechanistic insight on muscle responses to spaceflight. Int. J. Mol. Sci.22 (2021). 10.3390/ijms22179470. [DOI] [PMC free article] [PubMed]
- 58.Casanova-Vallve N, et al. Daily running enhances molecular and physiological circadian rhythms in skeletal muscle. Mol. Metab. 2022;61:101504. doi: 10.1016/j.molmet.2022.101504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Benjamin DI, et al. Fasting induces a highly resilient deep quiescent state in muscle stem cells via ketone body signaling. Cell Metab. 2022;34:902–918. e906. doi: 10.1016/j.cmet.2022.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hedge ET, et al. Implementation of exercise countermeasures during spaceflight and microgravity analogue studies: developing countermeasure protocols for bedrest in older adults (BROA) Front. Physiol. 2022;13:928313. doi: 10.3389/fphys.2022.928313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Laurens C, et al. Revisiting the role of exercise countermeasure on the regulation of energy balance during space flight. Front. Physiol. 2019;10:321. doi: 10.3389/fphys.2019.00321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang XP, et al. Time-restricted feeding alleviates cardiac dysfunction induced by simulated microgravity via restoring cardiac FGF21 signaling. FASEB J. 2020;34:15180–15196. doi: 10.1096/fj.202001246RR. [DOI] [PubMed] [Google Scholar]
- 63.Stein TP. The relationship between dietary intake, exercise, energy balance and the space crafts. Arch.: Eur. J. Physiol. 2000;441:R21–R31. doi: 10.1007/s004240000352. [DOI] [PubMed] [Google Scholar]
- 64.Astaburuaga R, Basti A, Li Y, Herms D, Relógio A. Circadian regulation of physiology: relevance for space medicine. REACH. 2019;14-15:100029. doi: 10.1016/j.reach.2019.100029. [DOI] [Google Scholar]
- 65.Glass DJ. Signalling pathways that mediate skeletal muscle hypertrophy and atrophy. Nat. Cell Biol. 2003;5:87–90. doi: 10.1038/ncb0203-87. [DOI] [PubMed] [Google Scholar]
- 66.Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28:27–30. doi: 10.1093/nar/28.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jassal B, et al. The reactome pathway knowledgebase. Nucleic Acids Res. 2020;48:D498–d503. doi: 10.1093/nar/gkz1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Stroud MJ, Banerjee I, Veevers J, Chen J. Linker of nucleoskeleton and cytoskeleton complex proteins in cardiac structure, function, and disease. Circulation Res. 2014;114:538–548. doi: 10.1161/CIRCRESAHA.114.301236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Roman W, Gomes ER. Nuclear positioning in skeletal muscle. Semin. Cell Dev. Biol. 2018;82:51–56. doi: 10.1016/j.semcdb.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 70.Williams D, Kuipers A, Mukai C, Thirsk R. Acclimation during space flight: effects on human physiology. Cmaj. 2009;180:1317–1323. doi: 10.1503/cmaj.090628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.English KL, Paddon-Jones D. Protecting muscle mass and function in older adults during bed rest. Curr. Opin. Clin. Nutr. Metab. Care. 2010;13:34–39. doi: 10.1097/MCO.0b013e328333aa66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.de Magalhães JP, Toussaint O. GenAge: a genomic and proteomic network map of human ageing. FEBS Lett. 2004;571:243–247. doi: 10.1016/j.febslet.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 73.Miljkovic N, Lim JY, Miljkovic I, Frontera WR. Aging of skeletal muscle fibers. Ann. Rehabil. Med. 2015;39:155–162. doi: 10.5535/arm.2015.39.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lexell J. Human aging, muscle mass, and fiber type composition. The journals of gerontology. Ser. A, Biol. Sci. Med. Sci. 1995;50:11–16. doi: 10.1093/gerona/50a.special_issue.11. [DOI] [PubMed] [Google Scholar]
- 75.Duffy JF, Zitting KM, Chinoy ED. Aging and circadian rhythms. Sleep. Med. Clin. 2015;10:423–434. doi: 10.1016/j.jsmc.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tajsharghi H, Oldfors A. Myosinopathies: pathology and mechanisms. Acta Neuropathologica. 2013;125:3–18. doi: 10.1007/s00401-012-1024-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Park H, et al. Truncation of MYH8 tail in AML: a novel prognostic marker with increase cell migration and epithelial-mesenchymal transition utilizing RAF/MAPK pathway. Carcinogenesis. 2020;41:817–827. doi: 10.1093/carcin/bgz146. [DOI] [PubMed] [Google Scholar]
- 78.Periasamy M, Kalyanasundaram A. SERCA pump isoforms: their role in calcium transport and disease. Muscle Nerve. 2007;35:430–442. doi: 10.1002/mus.20745. [DOI] [PubMed] [Google Scholar]
- 79.Nagakura R, et al. Switching of Sox9 expression during musculoskeletal system development. Sci. Rep. 2020;10:8425. doi: 10.1038/s41598-020-65339-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tajhya RB, et al. Functional KCa1.1 channels are crucial for regulating the proliferation, migration and differentiation of human primary skeletal myoblasts. Cell Death Dis. 2016;7:e2426. doi: 10.1038/cddis.2016.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cartee GD, Hepple RT, Bamman MM, Zierath JR. Exercise promotes healthy aging of skeletal muscle. Cell Metab. 2016;23:1034–1047. doi: 10.1016/j.cmet.2016.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kvedaras M, Minderis P, Cesanelli L, Cekanauskaite A, Ratkevicius A. Effects of fasting on skeletal muscles and body fat of adult and old C57BL/6J mice. Exp. Gerontol. 2021;152:111474. doi: 10.1016/j.exger.2021.111474. [DOI] [PubMed] [Google Scholar]
- 83.Pun FW, et al. Hallmarks of aging-based dual-purpose disease and age-associated targets predicted using PandaOmics AI-powered discovery engine. Aging (Albany NY) 2022;14:2475–2506. doi: 10.18632/aging.203960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Niebroj-Dobosz I, Fidzianska A, Hausmanowa-Petrusewicz I. Expression of emerin and lamins in muscle of patients with different forms of Emery-Dreifuss muscular dystrophy. Acta Myol. 2003;22:52–57. [PubMed] [Google Scholar]
- 85.Aging Atlas C. Aging atlas: a multi-omics database for aging biology. Nucleic Acids Res. 2021;49:D825–D830. doi: 10.1093/nar/gkaa894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Deane CS, Space Omics Topical T, da Silveira WA, Herranz R. Space omics research in Europe: contributions, geographical distribution and ESA member state funding schemes. iScience. 2022;25:103920. doi: 10.1016/j.isci.2022.103920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Afshinnekoo E, et al. Fundamental biological features of spaceflight: advancing the field to enable deep-space exploration. Cell. 2020;183:1162–1184. doi: 10.1016/j.cell.2020.10.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Blottner D, et al. Space Omics and Tissue Response in Astronaut Skeletal Muscle after Short and Long Duration Missions. Int. J. Mol. Sci. 2023;24:4095. doi: 10.3390/ijms24044095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Najrana T, Sanchez-Esteban J. Mechanotransduction as an adaptation to gravity. Front. Pediatr. 2016;4:140. doi: 10.3389/fped.2016.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chen Z, et al. Spaceflight decelerates the epigenetic clock orchestrated with a global alteration in DNA methylome and transcriptome in the mouse retina. Precis. Clin. Med. 2021;4:93–108. doi: 10.1093/pcmedi/pbab012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liu J, et al. Regulation of myonuclear positioning and muscle function by the skeletal muscle-specific CIP protein. Proc. Natl. Acad. Sci. U. S. A. 2020;117:19254–19265. doi: 10.1073/pnas.1922911117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Meinke P, et al. Muscular dystrophy-associated SUN1 and SUN2 variants disrupt nuclear-cytoskeletal connections and myonuclear organization. PLoS Genet. 2014;10:e1004605. doi: 10.1371/journal.pgen.1004605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ganassi M, Badodi S, Wanders K, Zammit PS, Hughes SM. Myogenin is an essential regulator of adult myofibre growth and muscle stem cell homeostasis. eLife. 2020;9:e60445. doi: 10.7554/eLife.60445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Guo Y, et al. Night-restricted feeding improves locomotor activity rhythm and modulates nutrient utilization to accelerate growth in rabbits. FASEB J. 2021;35:e21166. doi: 10.1096/fj.202001265RR. [DOI] [PubMed] [Google Scholar]
- 95.Agarwal, M. et al. Myosin heavy chain-embryonic regulates skeletal muscle differentiation during mammalian development. Development (Cambridge, England)147 (2020). 10.1242/dev.184507. [DOI] [PMC free article] [PubMed]
- 96.O’Connor RS, Mills ST, Jones KA, Ho SN, Pavlath GK. A combinatorial role for NFAT5 in both myoblast migration and differentiation during skeletal muscle myogenesis. J. Cell Sci. 2007;120:149–159. doi: 10.1242/jcs.03307. [DOI] [PubMed] [Google Scholar]
- 97.Blum R, Dynlacht BD. The role of MyoD1 and histone modifications in the activation of muscle enhancers. Epigenetics. 2013;8:778–784. doi: 10.4161/epi.25441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yamamoto M, et al. Loss of MyoD and Myf5 in skeletal muscle stem cells results in altered myogenic programming and failed regeneration. Stem Cell Rep. 2018;10:956–969. doi: 10.1016/j.stemcr.2018.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Yalçin, M. et al. A Computational analysis in a cohort of Parkinson’s disease patients and clock-modified colorectal cancer cells reveals common expression alterations in clock-regulated genes. Cancers (Basel)13 (2021). 10.3390/cancers13235978. [DOI] [PMC free article] [PubMed]
- 100.Villanueva JE, et al. Time-restricted feeding restores muscle function in Drosophila models of obesity and circadian-rhythm disruption. Nat. Commun. 2019;10:2700. doi: 10.1038/s41467-019-10563-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hatori M, et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. 2012;15:848–860. doi: 10.1016/j.cmet.2012.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Manoogian ENC, Panda S. Circadian rhythms, time-restricted feeding, and healthy aging. Ageing Res. Rev. 2017;39:59–67. doi: 10.1016/j.arr.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chaix A, Manoogian ENC, Melkani GC, Panda S. Time-restricted eating to prevent and manage chronic metabolic diseases. Annu Rev. Nutr. 2019;39:291–315. doi: 10.1146/annurev-nutr-082018-124320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ma L, Ma J, Xu K. Effect of spaceflight on the circadian rhythm, lifespan and gene expression of Drosophila melanogaster. PloS one. 2015;10:e0121600. doi: 10.1371/journal.pone.0121600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Acosta-Rodríguez VA, de Groot MHM, Rijo-Ferreira F, Green CB, Takahashi JS. Mice under caloric restriction self-impose a temporal restriction of food intake as revealed by an automated feeder system. Cell Metab. 2017;26:267–277.e262. doi: 10.1016/j.cmet.2017.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mitchell SJ, et al. Daily fasting improves health and survival in male mice independent of diet composition and calories. Cell Metab. 2019;29:221–228.e223. doi: 10.1016/j.cmet.2018.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Basti A, et al. Diurnal variations in the expression of core-clock genes correlate with resting muscle properties and predict fluctuations in exercise performance across the day. BMJ Open Sport Exerc. Med. 2021;7:e000876. doi: 10.1136/bmjsem-2020-000876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Teo W, Newton MJ, McGuigan MR. Circadian rhythms in exercise performance: implications for hormonal and muscular adaptation. J. Sports Sci. Med. 2011;10:600–606. [PMC free article] [PubMed] [Google Scholar]
- 109.Facer-Childs E, Brandstaetter R. The impact of circadian phenotype and time since awakening on diurnal performance in athletes. Curr. Biol.: CB. 2015;25:518–522. doi: 10.1016/j.cub.2014.12.036. [DOI] [PubMed] [Google Scholar]
- 110.Gabriel BM, Zierath JR. Circadian rhythms and exercise - re-setting the clock in metabolic disease. Nat. Rev. Endocrinol. 2019;15:197–206. doi: 10.1038/s41574-018-0150-x. [DOI] [PubMed] [Google Scholar]
- 111.Fox DK, et al. p53 and ATF4 mediate distinct and additive pathways to skeletal muscle atrophy during limb immobilization. Am. J. Physiol. Endocrinol. Metab. 2014;307:E245–E261. doi: 10.1152/ajpendo.00010.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Liu Z, et al. Mitochondrial NDUFA4L2 is a novel regulator of skeletal muscle mass and force. FASEB J. 2021;35:e22010. doi: 10.1096/fj.202100066R. [DOI] [PubMed] [Google Scholar]
- 113.Lee SM, et al. FABP3-mediated membrane lipid saturation alters fluidity and induces ER stress in skeletal muscle with aging. Nat. Commun. 2020;11:5661. doi: 10.1038/s41467-020-19501-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Gomarasca M, Banfi G, Lombardi G. Myokines: The endocrine coupling of skeletal muscle and bone. Adv. Clin. Chem. 2020;94:155–218. doi: 10.1016/bs.acc.2019.07.010. [DOI] [PubMed] [Google Scholar]
- 115.Zhang ZK, et al. A newly identified lncRNA MAR1 acts as a miR-487b sponge to promote skeletal muscle differentiation and regeneration. J. Cachexia, Sarcopenia muscle. 2018;9:613–626. doi: 10.1002/jcsm.12281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Perrin, L. et al. Transcriptomic analyses reveal rhythmic and CLOCK-driven pathways in human skeletal muscle. eLife7 (2018). 10.7554/eLife.34114. [DOI] [PMC free article] [PubMed]
- 117.Koh JH, et al. Enhancement of anaerobic glycolysis - a role of PGC-1α4 in resistance exercise. Nat. Commun. 2022;13:2324. doi: 10.1038/s41467-022-30056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ubaida-Mohien, C. et al. Discovery proteomics in aging human skeletal muscle finds change in spliceosome, immunity, proteostasis and mitochondria. eLife8 (2019). 10.7554/eLife.49874. [DOI] [PMC free article] [PubMed]
- 119.Kinouchi K, et al. Fasting imparts a switch to alternative daily pathways in liver and muscle. Cell Rep. 2018;25:3299–3314.e3296. doi: 10.1016/j.celrep.2018.11.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kelahmetoglu Y, et al. Comparative analysis of skeletal muscle transcriptional signatures associated with aerobic exercise capacity or response to training in humans and rats. Front. Endocrinol. 2020;11:591476. doi: 10.3389/fendo.2020.591476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ezagouri S, et al. Physiological and molecular dissection of daily variance in exercise capacity. Cell Metab. 2019;30:78–91.e74. doi: 10.1016/j.cmet.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 122.Maier G, et al. Transcriptomic, proteomic and phosphoproteomic underpinnings of daily exercise performance and zeitgeber activity of training in mouse muscle. J. Physiol. 2022;600:769–796. doi: 10.1113/JP281535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lee SJ, et al. Targeting myostatin/activin A protects against skeletal muscle and bone loss during spaceflight. Proc. Natl. Acad. Sci. U. S. A. 2020;117:23942–23951. doi: 10.1073/pnas.2014716117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chopard A, et al. Large-scale mRNA analysis of female skeletal muscles during 60 days of bed rest with and without exercise or dietary protein supplementation as countermeasures. Physiol. Genomics. 2009;38:291–302. doi: 10.1152/physiolgenomics.00036.2009. [DOI] [PubMed] [Google Scholar]
- 125.Rullman E, Fernandez-Gonzalo R, Mekjavić IB, Gustafsson T, Eiken O. MEF2 as upstream regulator of the transcriptome signature in human skeletal muscle during unloading. Am. J. Physiol. Regulatory, Integr. Comp. Physiol. 2018;315:R799–r809. doi: 10.1152/ajpregu.00452.2017. [DOI] [PubMed] [Google Scholar]
- 126.Fernandez-Gonzalo R, et al. Three months of bed rest induce a residual transcriptomic signature resilient to resistance exercise countermeasures. Faseb J. 2020;34:7958–7969. doi: 10.1096/fj.201902976R. [DOI] [PubMed] [Google Scholar]
- 127.Dyar KA, et al. Muscle insulin sensitivity and glucose metabolism are controlled by the intrinsic muscle clock. Mol. Metab. 2014;3:29–41. doi: 10.1016/j.molmet.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.McCarthy JJ, et al. Identification of the circadian transcriptome in adult mouse skeletal muscle. Physiol. Genomics. 2007;31:86–95. doi: 10.1152/physiolgenomics.00066.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Gambara G, et al. Microgravity-induced transcriptome adaptation in mouse paraspinal longissimus dorsi muscle highlights insulin resistance-linked genes. Front. Physiol. 2017;8:279. doi: 10.3389/fphys.2017.00279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gambara G, et al. Gene expression profiling in slow-type calf soleus muscle of 30 days space-flown mice. PloS One. 2017;12:e0169314. doi: 10.1371/journal.pone.0169314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Allen DL, et al. Effects of spaceflight on murine skeletal muscle gene expression. J. Appl. Physiol. (Bethesda, Md.: 1985) 2009;106:582–595. doi: 10.1152/japplphysiol.90780.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Ohira T, et al. Proteomic analysis revealed different responses to hypergravity of soleus and extensor digitorum longus muscles in mice. J. Proteom. 2020;217:103686. doi: 10.1016/j.jprot.2020.103686. [DOI] [PubMed] [Google Scholar]
- 133.Shen H, et al. Effects of spaceflight on the muscles of the murine shoulder. Faseb J. 2017;31:5466–5477. doi: 10.1096/fj.201700320R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Tascher G, et al. Proteome-wide adaptations of mouse skeletal muscles during a full month in space. J. Proteome Res. 2017;16:2623–2638. doi: 10.1021/acs.jproteome.7b00201. [DOI] [PubMed] [Google Scholar]
- 135.Simon, A. FastQC: a quality control tool for high throughput sequence data. Available online: https://www.bioinformatics.babraham.ac.uk/projects/fastqc/. (2010).
- 136.Bolger AM, Lohse M, Usadel B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics. 2014;30:2114–2120. doi: 10.1093/bioinformatics/btu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Dobin A, et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics. 2013;29:15–21. doi: 10.1093/bioinformatics/bts635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Patro R, Duggal G, Love MI, Irizarry RA, Kingsford C. Salmon provides fast and bias-aware quantification of transcript expression. Nat. Methods. 2017;14:417–419. doi: 10.1038/nmeth.4197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Soneson, C., Love, M. I. & Robinson, M. D. Differential analyses for RNA-seq: transcript-level estimates improve gene-level inferences. F1000Research4 (2015). 10.12688/f1000research.7563.1. [DOI] [PMC free article] [PubMed]
- 140.Robinson MD, McCarthy DJ, Smyth GK. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics. 2010;26:139–140. doi: 10.1093/bioinformatics/btp616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ritchie ME, et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43:e47. doi: 10.1093/nar/gkv007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Carvalho BS, Irizarry RA. A framework for oligonucleotide microarray preprocessing. Bioinformatics. 2010;26:2363–2367. doi: 10.1093/bioinformatics/btq431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kauffmann A, Gentleman R, Huber W. arrayQualityMetric“ a bioconductor package for quality assessment of microarray data. Bioinformatics. 2009;25:415–416. doi: 10.1093/bioinformatics/btn647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Cox J, Mann M. MaxQuant enables high peptide identification rates, individualized p.p.b.-range mass accuracies and proteome-wide protein quantification. Nat. Biotechnol. 2008;26:1367–1372. doi: 10.1038/nbt.1511. [DOI] [PubMed] [Google Scholar]
- 145.Gierlinski, M., Gastaldello, F., Cole, C. & Barton, G. J. Proteus: an R package for downstream analysis of MaxQuant output. bioRxiv, 416511 (2018). 10.1101/416511.
- 146.Thaben PF, Westermark PO. Detecting rhythms in time series with RAIN. J. Biol. Rhythms. 2014;29:391–400. doi: 10.1177/0748730414553029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Carlucci M, et al. DiscoRhythm: an easy-to-use web application and R package for discovering rhythmicity. Bioinformatics. 2019;36:1952–1954. doi: 10.1093/bioinformatics/btz834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Singer JM, Hughey JJ. LimoRhyde: a flexible approach for differential analysis of rhythmic transcriptome data. J. Biol. Rhythms. 2019;34:5–18. doi: 10.1177/0748730418813785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Shannon P, et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13:2498–2504. doi: 10.1101/gr.1239303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Jensen LJ, et al. STRING 8–a global view on proteins and their functional interactions in 630 organisms. Nucleic Acids Res. 2009;37:D412–D416. doi: 10.1093/nar/gkn760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Bader GD, Hogue CW. An automated method for finding molecular complexes in large protein interaction networks. BMC Bioinforma. 2003;4:2. doi: 10.1186/1471-2105-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Tenenbaum D, M. B. KEGGREST: Client-side REST access to the kyoto encyclopedia of genes and genomes (KEGG). (2022).
- 153.Kudoh A, Satoh H, Hirai H, Watanabe T, Shimabukuro M. Preliminary evidence for adipocytokine signals in skeletal muscle glucose uptake. Front. Endocrinol. 2018;9:295. doi: 10.3389/fendo.2018.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Mihaylova MM, Shaw RJ. The AMPK signalling pathway coordinates cell growth, autophagy and metabolism. Nat. Cell Biol. 2011;13:1016–1023. doi: 10.1038/ncb2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Tu MK, Levin JB, Hamilton AM, Borodinsky LN. Calcium signaling in skeletal muscle development, maintenance and regeneration. Cell Calcium. 2016;59:91–97. doi: 10.1016/j.ceca.2016.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Berdeaux R, Stewart R. cAMP signaling in skeletal muscle adaptation: hypertrophy, metabolism, and regeneration. Am. J. Physiol. Endocrinol. Metab. 2012;303:E1–E17. doi: 10.1152/ajpendo.00555.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Senf SM, Dodd SL, Judge AR. FOXO signaling is required for disuse muscle atrophy and is directly regulated by Hsp70. Am. J. Physiol. Cell Physiol. 2010;298:C38–C45. doi: 10.1152/ajpcell.00315.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Urban RJ. Growth hormone and testosterone: anabolic effects on muscle. Horm. Res. Paediatr. 2011;76:81–83. doi: 10.1159/000329184. [DOI] [PubMed] [Google Scholar]
- 159.Merz KE, Thurmond DC. Role of skeletal muscle in insulin resistance and glucose uptake. Compr. Physiol. 2020;10:785–809. doi: 10.1002/cphy.c190029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kramer HF, Goodyear LJ. Exercise, MAPK, and NF-kappaB signaling in skeletal muscle. J. Appl. Physiol. (Bethesda, Md.: 1985) 2007;103:388–395. doi: 10.1152/japplphysiol.00085.2007. [DOI] [PubMed] [Google Scholar]
- 161.Yoon MS. mTOR as a key regulator in maintaining skeletal muscle mass. Front. Physiol. 2017;8:788. doi: 10.3389/fphys.2017.00788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Glass DJ. PI3 kinase regulation of skeletal muscle hypertrophy and atrophy. Curr. Top. Microbiol. Immunol. 2010;346:267–278. doi: 10.1007/82_2010_78. [DOI] [PubMed] [Google Scholar]
- 163.Manickam, R., Duszka, K. & Wahli, W. PPARs and microbiota in skeletal muscle health and wasting. Int. J. Mol. Sci.21 (2020). 10.3390/ijms21218056. [DOI] [PMC free article] [PubMed]
- 164.Irrcher I, Adhihetty PJ, Joseph AM, Ljubicic V, Hood DA. Regulation of mitochondrial biogenesis in muscle by endurance exercise. Sports Med. (Auckl., N. Z.) 2003;33:783–793. doi: 10.2165/00007256-200333110-00001. [DOI] [PubMed] [Google Scholar]
- 165.Shenkman BS, Turtikova OV, Nemirovskaya TL, Grigoriev AI. Skeletal muscle activity and the fate of myonuclei. Acta Nat. 2010;2:59–66. doi: 10.32607/20758251-2010-2-2-59-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Kinsella RJ, et al. Ensembl BioMarts: a hub for data retrieval across taxonomic space. Database.: J. Biol. Databases Curation. 2011;2011:bar030. doi: 10.1093/database/bar030. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used in this study were retrieved from open-access public repositories and are available as follows: (1) Circadian RNA-seq datasets derived from human skeletal muscle (NCBI-GEO, Accession number: GSE108539, GSE109825), (2) Circadian microarray datasets derived from mouse skeletal muscle (NCBI-GEO, Accession number: GSE54650, GSE43071, GSE3746), (3) Spaceflight omics datasets derived from mouse skeletal muscle (NASA GeneLab: GLDS-99/-101/-103/-104/-105; NCBI-GEO, Accession number: GSE156321, GSE94381, GSE80223, GSE10533; PRIDE, Accession number: PXD006764, PXD005035), (4) Hypergravity associated proteomics data derived from mouse skeletal muscle (PRIDE, Accession number: PXD017240), (5) Bedrest associated microarray datasets derived from human skeletal muscle biopsies (NASA GeneLab: GLDS-370, NCBI-GEO, Accession number: GSE14798, GSE148152, GSE104999), (6) Aging associated RNA-seq datasets derived from human skeletal muscle biopsies (NCBI-GEO, Accession number: GSE97084, GSE129643), (7) Exercise associated RNA-seq datasets derived from human, mouse or rat skeletal muscle (NCBI-GEO, Accession number: GSE155230, GSE117161, GSE178262, GSE97084), and (8) Fasting associated RNA-seq dataset derived from mouse skeletal muscle (NCBI-GEO, Accession number: GSE107787).
All programs, packages, and functions used in this manuscript are freely available and are referred in the Methods section.