Abstract
The combination of glucagon-like peptide-1 (GLP-1) with other gut hormones including the glucose-dependent insulinotropic polypeptide (GIP) has been explored to complement and enhance further the GLP-1 effects on glycemia and weight loss. Tirzepatide is the first dual GLP-1/GIP receptor co-agonist which has been approved for treatment of type 2 diabetes mellitus (T2DM) based on the findings from the SURPASS program. The SURPASS trials assessed the safety and efficacy of tirzepatide in people with T2DM, from monotherapy through to insulin add-on in global populations, with another two trials dedicated to Japanese population. Over periods of treatment up to 104 weeks, once weekly tirzepatide 5 to 15 mg reduced glycosylated hemoglobin (1.87% to 3.02%), body weight (5.4 to 12.9 kg) and improved multiple cardiometabolic risk factors (including reduction in liver fat, new-onset macroalbuminuria, blood pressure, and lipids) across the T2DM spectrum. Tirzepatide provided better efficacy than placebo and other commonly used glucose-lowering medications such as semaglutide 1 mg, dulaglutide, insulin degludec, and glargine. All tirzepatide doses were well tolerated with similar side-effect profile to the GLP-1 receptor analogues. In people without diabetes, tirzepatide 5 to 15 mg once weekly for the treatment for obesity (SURMOUNT-1) resulted in substantial reductions in body weight (16.5% to 22.4%) over 72 weeks. Overall, the SURPASS program and SURMOUNT-1 study suggest that tirzepatide is marking a new era in T2DM and/or obesity management through dual agonism of gut hormones.
Keywords: Diabetes mellitus, type 2, Obesity, Tirzepatide, Glucagon-like peptide 1, Gastric inhibitory polypeptide
INTRODUCTION
The incidence of obesity has almost tripled since 1975, in parallel with an increase in the cases of type 2 diabetes mellitus (T2DM).1,2 Obesity is the strongest risk factor for T2DM as it causes insulin resistance, a key driver in development of T2DM.3 Overweight and obesity account for 44% of T2DM cases worldwide and prevalence of obesity-related diabetes is expected to increase further over the next years.3-5 Both obesity and T2DM are associated with multiple metabolic complications such as increased cardiovascular risk, hypertension, dyslipidemia, obstructive sleep apnoea, and nonalcoholic fatty liver disease (NAFLD).3 Considering the close relationship between obesity and T2DM, weight loss (WL) in people with T2DM can have beneficial effects on glycemic levels, insulin sensitivity, and cardiometabolic complications.3,6 Indeed, the latest American Diabetes Association/European Association for the Study of Diabetes (ADA/EASD) consensus guidelines for T2DM recommend 5% to 15% WL as a key component of care to improve quality of life and prevent complications.7
Although 5% WL is associated with metabolic benefits, it is the sustained WL of ≥10% which provides maximum benefit for prevention of T2DM and could reverse the underlying pathophysiology of T2DM.8,9 In people with obesity diagnosed with T2DM for ≤6 years, 64% of those who achieved and maintained ≥10 kg WL with a low calorie diet were able to achieve T2DM remission at 2 years (Diabetes Remission Clinical Trial [DiRECT] study) and remission rates were higher the more the WL achieved.9 Additionally, although an intensive lifestyle intervention for WL in the Look AHEAD: Action for Health in Diabetes (LookAHEAD) trial did not show reduction in major adverse cardiovascular events (MACE-4) in people with T2DM and obesity compared to a diabetes education and support program, a post hoc analysis demonstrated that those who lost ≥10% of their baseline body weight during the first year of the trial had a 21% lower risk for cardiovascular events over a 10 years follow-up period compared to those with stable weight or weight gain.10,11 Collating these results, it appears that ≥10% WL for people with obesity and T2DM is associated with improvements in glycemia, reduction in cardiometabolic risk factors as well as cardiovascular benefits, providing a WL threshold which facilitates achieving multiple key components of care in this population.
However, even with the most intensive lifestyle interventions only a minority of people with T2DM will be able to achieve and maintain ≥10% WL long-term.9,12 Weight regain is common after lifestyle interventions and approximately 80% of weight lost is expected to be regained over the next 5 years.13 Bariatric surgery was until recently the only intervention which could lead to sustained WL ≥15%, however it is not scalable to the population level.14
Over the last few years, glucagon-like peptide‐1 receptor analogues (GLP-1 RAs) have helped to transform the management of T2DM by combining effective reductions in glycemia with clinically important WL and weight maintenance.7 GLP-1 RAs also improve multiple cardiometabolic risk factors, reduce risk of cardiovascular events and cardiovascular mortality and have renoprotective effects in people with T2DM.15,16 Due to their efficacy in inducing WL and weight maintenance through reduction of appetite, some GLP-1 RAs (liraglutide and semaglutide) have been repurposed and approved at higher doses as treatments for obesity.17-19 Liraglutide 3 mg in combination with a moderate intensity lifestyle interventions can lead to 5.8% to 8.0% WL at 56 weeks (Satiety and Clinical Adiposity—Liraglutide Evidence in Nondiabetic and Diabetic Individuals Obesity and Prediabetes [SCALE] program) as well as weight maintenance after intensive lifestyle interventions.17,18,20,21 Additionally, semaglutide 2.4 mg once weekly resulted in 14.9% to 17.4% WL in people without diabetes (STEP program).19,22,23 However, the efficacy of GLP-1 RAs can be limited (mainly regarding WL in people with T2DM) and their adverse events (nausea and vomiting) are generally dose-dependent.21,24,25 As a result, a considerable number of people with T2DM are not able to achieve the metabolic, and WL targets with the currently existing therapies.26
THE CONCEPT OF CO-AGONISTS IN GLUCOSE-LOWERING AND WEIGHT LOSS TREATMENTS
In the search for the next step beyond GLP-1 RAs as treatment for T2DM and/or obesity, the combination of GLP‐1 with other gut hormones (including glucose-dependent insulinotropic polypeptide [GIP], amylin and glucagon) as dual or triple agonists has been trialled to complement and enhance further the metabolic benefits of GLP-1 by addressing multiple different mechanisms of action.27 The therapeutic potential of the combination of gut hormones (as dual or even triple agonists) is supported by the remarkable efficacy of bariatric surgery on WL and glycemia, an intervention leading to increased levels of multiple gut hormones with different actions, as well as from multiple preclinical studies and emerging clinical data.28,29 The combination of GLP-1 and GIP (the “twincretin” concept), appeared as one of the most attractive strategies for treating T2DM, considering that both these hormones have glucose-lowering actions.
GLP-1 AND GIP COMBINATION
The incretin effect describes the phenomenon whereby oral glucose elicits higher insulin secretion than does intravenous glucose, despite inducing similar levels of glycemia, in healthy individuals.30 This effect is mediated by the gut hormones GLP-1 and GIP which both promote insulin secretion and is uniformly defective in patients with T2DM.30,31
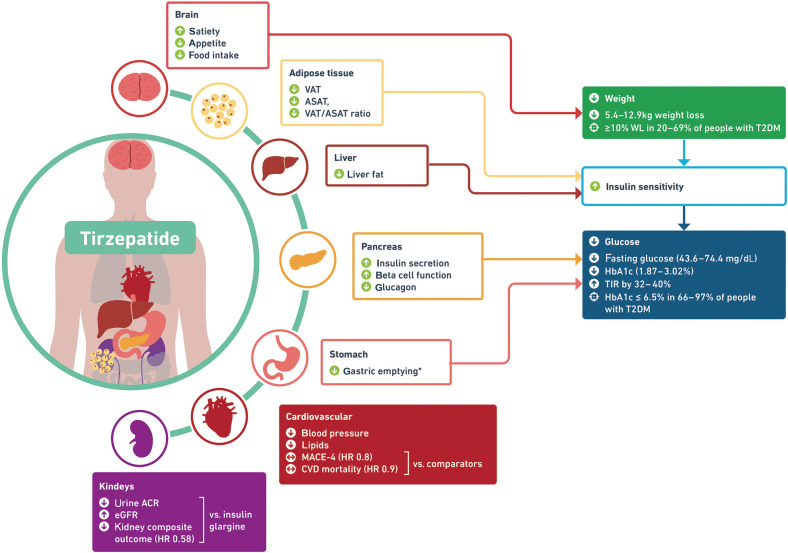
GLP-1 is secreted predominantly from L cells located in the ileum and colon in response to food intake.32 Exogenous GLP-1 infusion induces multiple glucose-lowering actions (Fig. 1) such as stimulation of glucose-induced insulin secretion, delay in gastric emptying and inhibition of glucagon secretion in healthy individuals as well as in people with T2DM.32-35 Additionally, exogenous GLP-1 infusion results in reduced food intake and appetite without direct changes in energy expenditure.35,36
Figure 1.
Pancreatic and exopancreatic actions of glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide‐1 (GLP-1). *Evidence from preclinical studies.
On the other hand, GIP is a peptide secreted by K cells in the duodenum and jejunum in response to nutrient ingestion. In people without diabetes, GIP stimulates insulin secretion but does not change glucagon release during hyperglycemia, whereas it increases glucagon release without affecting insulin secretion during hypoglycemia.37,38 In the context of T2DM, the ability of GIP to stimulate insulin secretion and to ameliorate glycemia is impaired; however, GIP sensitivity can be restored after improvement of glycemic control.39,40 GIP retains also the ability to stimulate glucagon secretion in people with T2DM and unlike what is reported in healthy people, subjects with T2DM demonstrate increased glucagon secretion in response to GIP during hyperglycemia.41 Other actions of GIP include increased lipogenesis and enhancement of the lipid-buffering capacity of the white adipose tissue, reduction of nausea and inhibition of bone resorption (Fig. 1).42-44 Preclinical studies have also shown that GIP receptor agonism lowers body weight through reduction of food intake.45
In preclinical models, the simultaneous administration of GLP-1 and GIP receptor agonists reduced food intake, body weight, and fat mass in mice with diet-induced obesity (DIO) to a greater extent than either agent alone, suggesting an additional effect.28,46 Further preclinical experiments showed that the combined activation of both GLP-1 and GIP receptor agonists had superior glucose-lowering efficacy compared to activation of either receptor alone.47,48 The greater metabolic effects observed with combined GLP-1 and GIP receptor activation in preclinical studies increased the interest for the development of unimolecular agonists of GLP-1 and GIP receptors, despite that this additive effect in glucose-lowering and food intake was not observed in some acute clinical studies.49,50
TIRZEPATIDE: PRECLINICAL STUDIES AND EARLY PHASE CLINICAL TRIALS
Tirzepatide, a once weekly unimolecular dual agonist of GLP-1 and GIP receptors, consists of 39 amino-acids and is the first dual gut hormone-based agonist which has been approved for the treatment of T2DM.51
Preclinical studies revealed that tirzepatide has a binding affinity to the GLP-1 receptor which is five times less than the native GLP-1, while it has comparable affinity to the native GIP for its receptors.52 Tirzepatide was also shown to induce glucose-dependent insulin secretion both in vitro and in vivo through actions on both incretin receptors. Chronic treatment with 10 nmol/kg of tirzepatide in DIO mice produced a dose-dependent decrease in body weight which was greater than with 30 nmol/kg semaglutide, primarily driven by a loss of fat mass due to reduction in food intake and a small increase in energy expenditure.53
Phase 1 clinical trials investigated the safety and tolerability of tirzepatide both in healthy people and people with T2DM. Pharmacokinetics and pharmacodynamics of tirzepatide as well as changes in glycemic parameters and WL compared to placebo and the GLP-1 RA dulaglutide were also assessed in these early phase trials.53 The pharmacokinetics of tirzepatide supported once weekly administration.53 Moreover, safety and good tolerability of tirzepatide in doses up to 15 mg once weekly was shown both in healthy people and those with T2DM, with gastrointestinal side effects being the most commonly reported.2,53,54 Dose and time-dependent reductions in body weight were observed across phase 1 studies and were greater than those observed with dulaglutide 1.5 mg at 29 days both for healthy individuals and for people with T2DM.2,53,54 Similarly, in people with T2DM, the reductions in glycosylated hemoglobin (HbA1c) were dose-dependent.53
Based on these findings, a randomised, double blind, placebo controlled phase 2 study was carried out in people with T2DM treated with lifestyle measures or metformin, aiming to assess the safety and efficacy of tirzepatide in comparison with placebo and dulaglutide 1.5 mg once weekly.55 Over 26 weeks, HbA1c improved by 1.6% to 2.4% with tirzepatide 5 to 15 mg compared to 1.1% reduction with dulaglutide and 0.1% HbA1c increase with placebo. WL was 4.8% to 11.3% over 26 weeks with tirzepatide 5 to 15 mg, with more than 20% of participants at tirzepatide 10 and 15 mg groups achieving WL ≥15% compared to 2% of those on dulaglutide.55 Adverse events were mainly mild or moderate in severity, with gastrointestinal symptoms being the most common. There were more gastrointestinal adverse events at the 15 mg tirzepatide group compared to dulaglutide 1.5 mg.55 A separate, phase 2, dose-escalation study found that by reducing the starting dose and increasing dose-escalation time to 8 weeks, gastrointestinal side effects could be reduced and study dropout rates were similar to that of placebo.56
POTENTIAL MECHANISMS OF ACTIONS OF TIRZEPATIDE
Mechanistic studies have shown that tirzepatide 15 mg leads to significant improvements in β-cell function and insulin sensitivity together with reduced glucagon secretion compared to placebo in people with T2DM.57 These actions, can explain at least partially the marked improvements in glycemia observed with tirzepatide in people with T2DM (Fig. 2).58 Moreover, tirzepatide 15 mg once weekly results in reduced energy intake (–348.4 kcal) at an ad libitum lunch in people with T2DM through reduction of the overall appetite, increased satiety and decreased prospective food consumption, which explains the reduction in weight.59 Further mechanistic studies assessing the changes in resting metabolic rate, energy intake and appetite with tirzepatide in people without T2DM (NCT04081337) as well as how it affects the appetite- and reward-related areas of the brain (NCT04311411) are ongoing.
Figure 2.
Mechanisms of action (white background boxes) and clinical outcomes (colored background boxes) with tirzepatide in SURPASS program. *Transient effect, MACE-4 (cardiovascular death, myocardial infarction, stroke, and hospitalisation for unstable angina), composite kidney outcome: time to first occurrence of estimated glomerular filtration rate (eGFR) decline of at least 40% from baseline, end-stage kidney disease, death due to kidney failure, or new-onset macroalbuminuria. VAT, visceral adipose tissue; ASAT, abdominal subcutaneous adipose tissue; WL, weight loss; T2DM, type 2 diabetes mellitus; HbA1c, glycosylated hemoglobin; TIR, time in range; MACE-4, major adverse cardiovascular event; HR, hazard ratio; CVD, cardiovascular disease; ACR, albumin-creatinine ratio.
SURPASS PROGRAM: METHODOLOGY
The results of the phase 2 trial led to the SURPASS program (composed of multiple phase 3 clinical trials) and seven randomised controlled trials have been published so far. Five of these were global multicenter trials, and two regional studies were carried out in Japan.60-66 Baseline demographics of participants and study designs of SURPASS program are presented in Table 1.
Table 1.
Summary of baseline characteristics and trial designs for SURPASS programme and SURMOUNT-1 study
| Study | Treatment arms | No. of participants | Inclusion criteria | Duration of trial; blinded/open label; randomisation ratio | Primary analysis point | Mean age (yr) | Female sex (%) | Mean duration of T2DM (yr) | Mean baseline weight (kg) | Mean baseline HbA1c (%) | Mean baseline BMI (kg/m2) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| SURPASS-1 | Tirzepatide 5, 10, 15 mg and placebo | 478 | HbA1c 7%–9.5%, BMI ≥ 23 kg/m2, treated with diet and exercise | 40 wk; blinded; 1:1:1:1 | 40 wk, mean change from baseline HbA1c | 54.1 | 48 | 4.7 | 85.9 | 7.94 | 31.9 |
| SURPASS-2 | Tirzepatide 5, 10, 15 mg and semaglutide 1 mg | 1,879 | HbA1c 7%–10.5%, BMI ≥ 25 kg/m2, treated with metformin | 40 wk; open label; 1:1:1:1 | 40 wk, mean change from baseline HbA1c | 56.6 | 53 | 8.6 | 93.7 | 8.28 | 34.2 |
| SURPASS-3 | Tirzepatide 5, 10, 15 mg and insulin degludec | 1,444 | HbA1c 7%–10.5%, BMI ≥ 25 kg/m2, treated with metformin ± SGLT2 inhibitor | 52 wk; open label; 1:1:1:1 | 52 wk, mean change from baseline HbA1c | 57.4 | 44 | 8.4 | 94.3 | 8.17 | 33.5 |
| SURPASS-4 | Tirzepatide 5, 10, 15 mg and insulin glargine | 2,002 | Increased cardiovascular risk, HbA1c 7.5%–10.5%, BMI ≥ 25 kg/m2, treated with metformin, SGLT2 inhibitor, sulfonylurea, or any combination of these | 104 wk; open label; 1:1:1:3 | 52 wk, mean change from baseline HbA1c | 63.6 | 38 | 11.8 | 90.3 | 8.52 | 32.6 |
| SURPASS-5 | Tirzepatide 5, 10, 15 mg and placebo | 475 | HbA1c 7%–10.5%, BMI ≥ 23 kg/m2, receiving once-daily insulin glargine ± metformin | 40 wk; open label; 1:1:1:1 | 40 wk, mean change from baseline HbA1c | 61.0 | 44 | 13.3 | 95.2 | 8.31 | 33.2– 33.6 |
| SURPASS J-mono | Tirzepatide 5, 10, 15 mg and dulaglutide 0.75 mg | 636 | HbA1c 7%–10%, BMI ≥ 23 kg/m2, treated with diet and exercise, or having discontinued anti-hyperglycemic monotherapy | 52 wk; blinded; 1:1:1:1 | 52 wk, mean change from baseline HbA1c | 56.6 | 24 | 4.8 | 78.2 | 8.2 | 28.1 |
| SURPASS J-combo | Tirzepatide 5, 10, 15 mg | 443 | HbA1c ≥ 7.0% to < 11.0%, BMI ≥ 23 kg/m2, treated with oral antihyperglycemic monotherapy | 52 wk; open label; 1:1:1 | 52 wk, incidence of treatment-emergent adverse events | 57.0 | 24 | 8.6 | 77.5 | 8.6 | 27.9 |
| SURMOUNT-1 | Tirzepatide 5, 10, 15 mg and placebo | 2,539 | At least one unsuccessful dietary effort to lose weight, and BMI ≥ 30 or ≥ 27 kg/m2 with hypertension/dyslipid- emia/obstructive sleep apnoea/cardiovascular disease | 72 wk; blinded; 1:1:1:1 | 72 wk, (1) % change in body weight from baseline and (2) weight loss ≥ 5% | 44.9 | 68 | NA | 104.8 | 5.6 | 38.0 |
T2DM, type 2 diabetes mellitus; HbA1c, glycosylated hemoglobin; BMI, body mass index; SGLT2, sodium-glucose co-transporter 2; NA, not applicable.
Individuals recruited to SURPASS covered a large part of the T2DM continuum, ranging from those with less than 5 years since diagnosis to those with advanced disease (>10 years). Participants were given subcutaneous tirzepatide 5, 10, or 15 mg once weekly either as monotherapy, or in combination with other glucose-lowering medications, including insulin, without additional support for lifestyle changes.67 Tirzepatide initiation dose was 2.5 mg once weekly and increased by 2.5 mg every 4 weeks until reaching the target dose (a lower starting dose and a slower escalation regime compared to the phase 2 trial).68
The effect of tirzepatide was assessed against placebo, basal insulins (glargine and degludec) and the GLP-1 RAs dulaglutide 0.75 mg and semaglutide 1 mg. The primary endpoint in all these studies was the change in HbA1c from baseline, except of SURPASS in Japanese population (SURPASS J-mono) which aimed to evaluate the safety of tirzepatide in the study population. The primary outcome was reported using two estimands for most studies, the efficacy estimand, and the treatment-regimen estimand. The efficacy estimand excludes data on the treatment after rescue therapy or discontinuation of study drugs. The treatment-regimen estimand represents efficacy of treatment regardless of study drug discontinuation or use of rescue therapy.62,68,69 This review will use the reported efficacy estimand for HbA1c and WL parameters (as this is reported in all the SURPASS studies) unless otherwise specified.
SURPASS PROGRAM: CLINICAL OUTCOMES
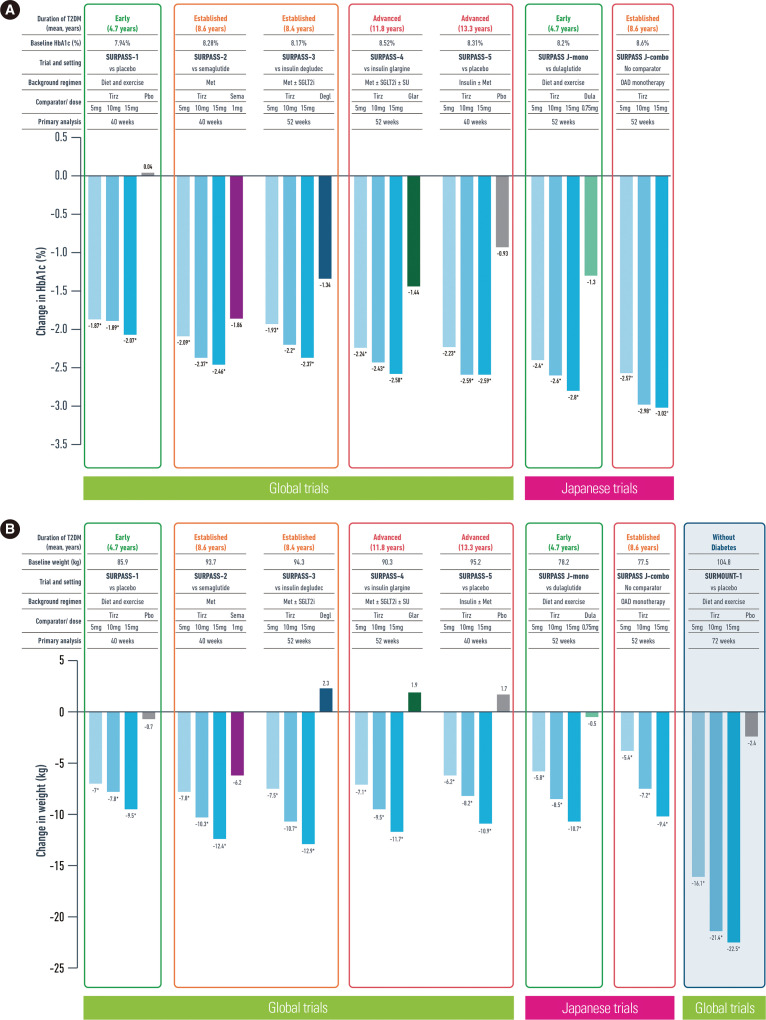
Glycemic outcomes
Tirzepatide reduced HbA1c in a dose-dependent manner across all the studies using both estimands (Table 2, Fig. 3).60-66 In people with early T2DM treated only with diet and exercise (SURPASS-1), tirzepatide 5 to 15 mg improved the HbA1c by 1.87% to 2.07% compared to 0.04% increase at the placebo group.60
Table 2.
Proportion of people achieving HbA1c and weight loss targets in SURPASS programme and SURMOUNT-1 study
| Trial | Treatment arm (no. randomised to each arm) | Efficacy estimand | Treatment-regimen estimand | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||||||||
| Change from baseline | Proportion (%) of people achieving the target | Change from baseline | Proportion (%) of people achieving the target | ||||||||||||||
|
|
|
||||||||||||||||
| HbA1c (%) | Weight | HbA1c <7% | HbA1c ≤ 6.5% | HbA1c < 5.7% | WL ≥5% | WL ≥10% | WL ≥15% | HbA1c (%) | Weight | HbA1c <7% | HbA1c ≤ 6.5% | HbA1c < 5.7% | WL ≥5% | WL ≥10% | WL ≥15% | ||
| SURPASS-1 | Tirzepatide 5 mg (n = 121) | –1.87 | –7.0 kg | 87 | 82 | 34 | 67 | 31 | 13 | –1.75 | –6.3 kg | 82 | 75 | 31 | 61 | 27 | 12 |
| Tirzepatide 10 mg (n = 121) | –1.89 | –7.8 kg | 92 | 81 | 31 | 78 | 40 | 17 | –1.71 | –7.0 kg | 85 | 74 | 27 | 71 | 34 | 16 | |
| Tirzepatide 15 mg (n = 121) | –2.07 | –9.5 kg | 88 | 86 | 52 | 77 | 47 | 27 | –1.69 | –7.8 kg | 78 | 73 | 38 | 62 | 38 | 23 | |
| Placebo (n = 115) | 0.04 | –0.7 kg | 19 | 10 | 1 | 14 | 1 | 0 | –0.09 | –1.0 kg | 23 | 11 | 1 | 11 | 0 | 0 | |
| SURPASS-2 | Tirzepatide 5 mg (n = 470) | –2.09 | –7.8 kg | 85 | 74 | 29 | 69 | 36 | 15 | –2.01 | –7.6 kg | 82 | 69 | 27 | 65 | 34 | 15 |
| Tirzepatide 10 mg (n = 469) | –2.37 | –10.3 kg | 89 | 82 | 45 | 82 | 53 | 28 | –2.24 | –9.3 kg | 86 | 77 | 40 | 76 | 47 | 24 | |
| Tirzepatide 15 mg (n = 470) | –2.46 | –12.4 kg | 92 | 87 | 51 | 86 | 65 | 40 | –2.30 | –11.2 kg | 86 | 80 | 46 | 80 | 57 | 36 | |
| Semaglutide 1 mg (n = 469) | –1.86 | –6.2 kg | 81 | 66 | 20 | 58 | 28 | 9 | –1.86 | –5.7 kg | 79 | 64 | 19 | 54 | 24 | 8 | |
| SURPASS-3 | Tirzepatide 5 mg (n = 358) | –1.93 | –7.5 kg | 82 | 71 | 26 | 66 | 37 | 13 | –1.85 | –7.0 kg | 79 | 67 | 24 | 61 | 35 | 12 |
| Tirzepatide 10 mg (n = 360) | –2.20 | –10.7 kg | 90 | 80 | 39 | 84 | 56 | 28 | –2.01 | –9.6 kg | 82 | 71 | 34 | 74 | 50 | 25 | |
| Tirzepatide 15 mg (n = 359) | –2.37 | –12.9 kg | 93 | 85 | 48 | 88 | 69 | 43 | –2.14 | –11.3 kg | 83 | 74 | 41 | 79 | 58 | 35 | |
| Insulin degludec (n = 360) | –1.34 | 2.3 kg | 61 | 44 | 5 | 6 | 3 | 0 | –1.25 | 1.9 kg | 58 | 42 | 5 | 8 | 3 | 0 | |
| SURPASS-4 | Tirzepatide 5 mg (n = 329) | –2.24 | –7.1 kg | 81 | 66 | 23 | 63 | 36 | 14 | –2.11 | –6.4 kg | 75 | 62 | 22 | 57 | 32 | 13 |
| Tirzepatide 10 mg (n = 328) | –2.43 | –9.5 kg | 88 | 76 | 33 | 78 | 53 | 24 | –2.30 | –8.9 kg | 83 | 70 | 31 | 74 | 50 | 23 | |
| Tirzepatide 15 mg (n = 338) | –2.58 | –11.7 kg | 91 | 81 | 43 | 85 | 66 | 37 | –2.41 | –10.6 kg | 85 | 74 | 38 | 77 | 59 | 33 | |
| Insulin lantus (n = 1000) | –1.44 | 1.9 kg | 51 | 32 | 3 | 8 | 2 | <1 | –1.39 | 1.7 kg | 49 | 31 | 4 | 9 | 2 | <1 | |
| SURPASS-5 | Tirzepatide 5 mg (n = 116) | –2.23 | –6.2 kg | 93 | 80 | 26 | 54 | 23 | 7 | –2.11 | –5.4 kg | 87 | 74 | 24 | 48 | 21 | 7 |
| Tirzepatide 10 mg (n = 119) | –2.59 | –8.2 kg | 97 | 95 | 48 | 65 | 47 | 27 | –2.40 | –7.5 kg | 90 | 86 | 42 | 58 | 42 | 24 | |
| Tirzepatide 15 mg (n = 120) | –2.59 | –10.9 kg | 94 | 92 | 62 | 85 | 51 | 32 | –2.34 | –8.8 kg | 85 | 80 | 50 | 72 | 41 | 23 | |
| Placebo (n = 120) | –0.93 | 1.7 kg | 34 | 17 | 3 | 6 | 1 | 0 | –0.86 | 1.6 kg | 35 | 17 | 3 | 6 | 1 | 0 | |
| SURPASS J-mono | Tirzepatide 5 mg (n = 159) | –2.4 | –5.8 kg | 94 | 92 | 51 | 61 | 34 | 16 | –2.24 | –5.4 kg | NR | NR | NR | NR | NR | NR |
| Tirzepatide 10 mg (n = 158) | –2.6 | –8.5 kg | 97 | 96 | 58 | 82 | 50 | 26 | –2.36 | –7.2 kg | NR | NR | NR | NR | NR | NR | |
| Tirzepatide 15 mg (n = 160) | –2.8 | –10.7 kg | 99 | 97 | 79 | 89 | 67 | 45 | –2.57 | –9.4 kg | NR | NR | NR | NR | NR | NR | |
| Dulaglutide 0.75 mg (n = 159) | –1.3 | –0.5 kg | 67 | 40 | 3 | 11 | 3 | 0 | –1.27 | –0.4 kg | NR | NR | NR | NR | NR | NR | |
| SURPASS J-combo | Tirzepatide 5 mg (n = 148) | –2.57 | –3.8 kg | 93 | 87 | 37 | 44 | 20 | 7 | NR | NR | NR | NR | NR | NR | NR | NR |
| Tirzepatide 10 mg (n = 147) | –2.98 | –7.5 kg | 98 | 93 | 67 | 71 | 48 | 29 | NR | NR | NR | NR | NR | NR | NR | NR | |
| Tirzepatide 15 mg (n = 148) | –3.02 | –10.2 kg | 97 | 92 | 71 | 84 | 64 | 41 | NR | NR | NR | NR | NR | NR | NR | NR | |
| SURMOUNT-1 | Tirzepatide 5 mg (n = 630) | NA | –16.0% | NA | NA | NA | 89 | 73 | 50 | NA | –15.0% | NA | NA | NA | 85 | 69 | 48 |
| Tirzepatide 10 mg (n = 636) | NA | –21.4% | NA | NA | NA | 96 | 86 | 74 | NA | –19.5% | NA | NA | NA | 89 | 78 | 67 | |
| Tirzepatide 15 mg (n = 630) | NA | –22.5% | NA | NA | NA | 96 | 90 | 78 | NA | –20.9% | NA | NA | NA | 91 | 84 | 71 | |
| Placebo (n = 643) | NA | –2.4% | NA | NA | NA | 28 | 14 | 6 | NA | –3.1% | NA | NA | NA | 35 | 19 | 9 | |
HbA1c, glycosylated hemoglobin; WL, weight loss; NR, not reported; NA, not applicable.
Figure 3.
(A) Change in glycosylated hemoglobin (HbA1c) with different doses of tirzepatide and comparators in SURPASS programme. (B) Change in weight with different doses of tirzepatide and comparators in SURPASS programme and SURMOUNT-1 study. All data is presented as efficacy estimand. *P< 0.05 for the estimated treatment difference with each dose of tirzepatide vs. placebo and/or active comparator. T2DM, type 2 diabetes mellitus; Met, metformin; SGLT2i, sodium-glucose co-transporter 2 inhibitor; SU, sulfonylurea; OAD, oral antidiabetic drug; Tirz, tirzepatide; Pbo, placebo; Sema, semaglutide; Degl, insulin degludec; Glar, insulin glargine; Dula, dulaglutide.
In SURPASS-2, people with established T2DM treated with tirzepatide 5 to 15 mg for 40 weeks and achieved HbA1c reduction 2.09% to 2.46% compared to 1.86% reduction with semaglutide 1 mg.61 Similarly, in SURPASS-3, tirzepatide 5 to 15 mg for 52 weeks resulted in 1.93% to 2.37% HbA1c reduction versus 1.34% decrease with insulin degludec.63
In people with advanced T2DM (>10 years) and increased cardiovascular risk (SURPASS-4), the use of tirzepatide 5 to 15 mg also decreased HbA1c by 2.24% to 2.58% compared to insulin glargine which improved HbA1c by 1.44% at 52 weeks.62 In SURPASS-5, when tirzepatide was added in people who were already on insulin glargine, it led to 2.23% to 2.59% reduction in HbA1c versus 0.93% with placebo—this improvement in glycemia was also associated with a reduction in insulin use.64
In Japanese populations, tirzepatide 5 to 15 mg decreased HbA1c by 2.4% to 3.02% after 52 weeks of treatment.65,66 Tirzepatide was also more effective for glycemic control compared to dulaglutide 0.75 mg once weekly in this population.
More patients in the tirzepatide groups achieved the HbA1c targets of <7%, ≤6.5%, and <5.7% both in the global and Japanese SURPASS studies compared to placebo or active comparators (Table 2).60-66
Fasting serum glucose (FSG) was lower with tirzepatide across all doses and studies (–43.6 to –74.4 mg/dL or –2.4 to –4.1 mmol/L) compared to baseline levels as well as compared to placebo, semaglutide 1 mg, and dulaglutide 0.75 mg (J-mono) (Table 3). In SURPASS-3, the FSG reduction with all tirzepatide doses was comparable to the FSG achieved with insulin degludec, when in SURPASS-4, only the 15 mg tirzepatide dose produced a significant FSG reduction compared to insulin glargine.60-66,68
Table 3.
Change from baseline fasting plasma glucose and cardiometabolic risk factors in SURPASS programme and SURMOUNT-1 study
| Trial | Treatment arm | Change from baseline | % Change from baseline | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| WC (cm) | FSG* (mg/dL) | SBP (mmHg) | DBP (mmHg) | Total cholesterol | LDL-C (mg/dL) | Triglycerides | HDL-C (mg/dL) | ALT | AST | ||
| SURPASS-1 | Tirzepatide 5 mg | –5.7 | –43.6 | –4.7† | –2.9† | –5.47 | –6.66† | –18.5 | 4.8 | –29.1 | –11.6 |
| Tirzepatide 10 mg | –6.9 | –45.9 | –5.2 | –3.1† | –6.34 | –7.58† | –18.2 | 3.2 | –25.7 | –9.5† | |
| Tirzepatide 15 mg | –7.2 | –49.3 | –4.7† | –3.4† | –8.43 | –12.43 | –21.0 | 7.5 | –32.9 | –13.9 | |
| Placebo | –2.0 | 12.9 | –2.0 | –1.4 | –0.76 | –1.64 | 4.7 | –3.8 | –10.2 | –2.6 | |
| SURPASS-2 | Tirzepatide 5 mg | –6.9 | –56.0 | –4.8 | –1.9 | –5.49† | –7.68† | –19.0 | 6.8 | –22.4† | –8.7† |
| Tirzepatide 10 mg | –9.6 | –61.6 | –5.3 | –2.5 | –5.96† | –5.59† | –24.1 | 7.9 | –29.2 | –13.7 | |
| Tirzepatide 15 mg | –9.9 | –63.4 | –6.5 | –2.9 | –6.26† | –5.15† | –24.8 | 7.1 | –30.0 | –14.1 | |
| Semaglutide 1 mg | –5.6 | –48.6 | –3.6 | –1.0 | –4.78 | –6.39 | –11.5 | 4.4 | –21.6 | –9.2 | |
| SURPASS-3 | Tirzepatide 5 mg | –7.1 | –48.2 | –4.9 | –2.0 | –4.25† | –6.01† | –15.4† | 5.5 | –22.3 | –11.4 |
| Tirzepatide 10 mg | –9.4 | –54.8† | –6.6 | –2.5 | –5.81† | –5.70† | –26.7 | 10.2 | –27.4 | –12.8 | |
| Tirzepatide 15 mg | –10.9 | –59.2† | –5.5 | –1.9 | –5.69† | –6.55† | –25.2 | 10.2 | –30.7 | –16.4 | |
| Insulin degludec | 0.7 | –55.7 | 0.5 | 0.4 | –2.92 | –2.71 | –12.2 | 1.0 | –17 | –5.8 | |
| SURPASS-4 | Tirzepatide 5 mg | –8.0 | –50.4† | –2.8 | –1.0 | –5.1 | –6.8 | –16.3 | 6.7 | NR | NR |
| Tirzepatide 10 mg | –10.1 | –54.9† | –3.7 | –0.8 | –5.5 | –8.3 | –20.1 | 9.7 | NR | NR | |
| Tirzepatide 15 mg | –8.9 | –59.3 | –4.8 | –1.0 | –5.6 | –7.9 | –22.5 | 10.8 | NR | NR | |
| Insulin lantus | 2.3 | –51.4 | 1.3 | 0.7 | 0 | 1.4 | –6.4 | 2.9 | NR | NR | |
| SURPASS-5 | Tirzepatide 5 mg | –3.8 | –61.4 | –6.1 | –2.0 | –8.8 | –8.9 | –15.2 | 2.1† | –19.4 | –4.1† |
| Tirzepatide 10 mg | –7.4 | –67.9 | –8.3 | –3.3 | –10.3 | –12.8 | –19.3 | 1.8† | –23.3 | –8.6 | |
| Tirzepatide 15 mg | –8.9 | –67.7 | –12.6 | –4.5 | –12.9 | –15.5 | –24.9 | 0.9† | –28.3 | –14.1 | |
| Placebo | 1.0 | –38.9 | –1.7 | –2.1 | –0.4 | 2.8 | –6.8 | 1.7 | –7.5 | 0.0 | |
| SURPASS J-mono | Tirzepatide 5 mg | –5.4 | –57.9 | –6.5 | –3.2 | –10.0 | –12.0 | –27.1 | 3.8 | –26.2 | –14.0 |
| Tirzepatide 10 mg | –6.8 | –64.4 | –8.8 | –4.0 | –11.6 | –12.8 | –32.8 | 5.4 | –30.7 | –14.9 | |
| Tirzepatide 15 mg | –9.8 | –67.6 | –11.0 | –5.6 | –15.4 | –19.3 | –37.7 | 5.9 | –32.4 | –17.9 | |
| Dulaglutide 0.75 mg | 0.4 | –31.9 | –1.4 | 0.1 | –3.8 | –4.8 | –8.2 | 0 | –0.9 | 2.2 | |
| SURPASS J-combo | Tirzepatide 5 mg | –3.3 | –58.6 | –5.1 | –2.7 | –11.1 | –13.6 | –21.9 | 0.9 | –14.7 | –4.7 |
| Tirzepatide 10 mg | –7.2 | –71.2 | –10.2 | –3.6 | –13.4 | –15.1 | –31.1 | 2.4 | –23.9 | –13.8 | |
| Tirzepatide 15 mg | –9.0 | –74.4 | –8.7 | –3.4 | –14.6 | –18.0 | –37.4 | 5.1 | –28.9 | –12.2 | |
| SURMOUNT-1 | Tirzepatide 5 mg | –14.6 | NA | –7.0 | –5.2 | –4.9 | –5.3 | –24.3 | 7.0 | –25.7 | –11.4 |
| Tirzepatide 10 mg | –19.4 | NA | –8.2 | –5.5 | –5.6 | –6.6 | –27.0 | 8.6 | –28.1 | –12.1 | |
| Tirzepatide 15 mg | –19.9 | NA | –7.6 | –4.6 | –7.4 | –8.6 | –31.4 | 8.2 | –30.3 | –14.2 | |
| Placebo | –3.4 | NA | –1.2 | –1.0 | –1.1 | –0.9 | –6.3 | 0.2 | –12.8 | –6.6 | |
*Efficacy estimand; †No significant difference from comparator.
WC, waist circumference; FSG, fasting serum glucose; SBP, systolic blood pressure; DBP, diastolic blood pressure; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol; ALT, alanine transaminase; AST, aspartate transaminase; NR, not reported; NA, not applicable.
Continuous glucose monitoring in a subgroup of participants in SURPASS-3, showed that all tirzepatide doses (5, 10, and 15 mg) improved the time in range (TIR, 70 to 180 mg/dL or 3.9 to 10 mmol/L) (TIR increased by 32% to 40% from baseline, achieving overall 85% to 91% TIR) compared to insulin degludec (TIR increased by 22% from baseline, achieving overall 75% TIR) at 52 weeks after randomisation.70 The tirzepatide groups had also less time below range (<70 mg/dL or <3.9 mmol/L) compared to insulin and reduced glycemic variability.70
Weight outcomes
Marked WL was seen in all tirzepatide groups across the SURPASS program (Fig. 2).60-66 In people with early onset T2DM, 40 weeks of tirzepatide 5 to 15 mg led to WL of 7 to 9.5 kg compared to 0.7 kg WL with placebo.60
In people with established T2DM, larger WL was achieved across all tirzepatide doses (–7.8, –10.3, and –12.4 kg with 5, 10, and 15 mg, respectively) compared to semaglutide 1 mg (–6.2 kg, SURPASS-2).61 Initiation of insulin degludec in SURPASS-3 caused weight gain of 2.3 kg after 52 weeks of treatment, whereas tirzepatide 5 to 15 mg reduced weight by 7.5 to 12.9 kg.63
In people with advanced T2DM, initiation of insulin glargine on a background of other glucose-lowering medications (SURPASS-4) led to weight gain of 1.9 kg after 52 weeks compared to 7.1 to 11.7 kg WL with tirzepatide.62 In SURPASS-5, all the participants were on basal insulin glargine and the tirzepatide group achieved 6.2 to 10.9 kg WL compared to 1.7 kg weight gain with placebo.64
In Japanese populations, tirzepatide 5 to 15 mg resulted in 3.8 to 10.7 kg WL at 52 weeks.65,66 Across the SURPASS program, 65% to 89% of people with T2DM who received tirzepatide 10 or 15 mg achieved ≥5% WL, 40% to 69% managed ≥10% WL, and 17% to 45% achieved ≥15% WL (Table 2).60-66
In SURPASS-3, a subgroup of participants underwent magnetic resonance imaging proton density fat fraction assessment prior to initiation of treatment with tirzepatide or insulin degludec and at 52 weeks after randomisation for assessment of the abdominal fat and liver fat content (LFC).71 Visceral abdominal tissue and abdominal subcutaneous adipose tissue were decreased compared to baseline with all tirzepatide doses. At week 52, LFC was reduced by 29.78% to 47.11% with tirzepatide compared to baseline, whereas it was reduced less (11.17%) with insulin. Notably, 67% to 81% of people treated with tirzepatide reached at least 30% relative reduction in LFC, a degree of response associated with improvements in liver histology—these results suggest that tirzepatide may be a treatment option for NAFLD.71
CARDIOMETABOLIC RISK FACTORS
Multiple cardiometabolic risk factors including waist circumference, blood pressure, and lipids improved with tirzepatide in the SURPASS trials (Table 3). Waist circumference reduced by 3.8 to 10.9 cm with tirzepatide 5 to 15 mg at SURPASS studies—this reduction was significant compared to placebo and active comparators.60-66,68 Systolic blood pressure was decreased with tirzepatide by 2.8 to 12.6 mmHg, and diastolic blood pressure was also reduced by 1 to 5.6 mmHg across the programme. Pulse rate was found to increase (0.7 to 8.3 beats/minute on average), a similar magnitude to that seen with use of GLP-1 RAs.60-66,68
INITIAL EVIDENCE ON CARDIOVASCULAR AND RENAL SAFETY
SURPASS-4 assessed the safety and efficacy of tirzepatide vs insulin glargine in a high cardiovascular risk population with advanced T2DM over a period of 2 years.62 Cardiovascular outcomes were assessed (as secondary outcome) using a composite of MACE-4 consisting of: cardiovascular death, myocardial infarction, stroke, and hospitalisation for unstable angina. Adjudicated MACE-4 events were not increased in tirzepatide groups compared to insulin glargine (hazard ratio [HR], 0.74; 95% confidence interval [CI], 0.51 to 1.08).62
A pre-specified cardiovascular meta-analysis included seven clinical trials with follow-up at least 26 weeks and compared the time to first occurrence of MACE-4 between pooled tirzepatide (n=4,887) and control groups (n=2,328).72 In a population with one-third having established cardiovascular disease, there were 142 participants who experienced at least one MACE-4 event after treatment for just over a year. The HRs comparing tirzepatide versus controls were 0.80 (95% CI, 0.57 to 1.11) for MACE-4; 0.90 (95% CI, 0.50 to 1.61) for cardiovascular death; and 0.80 (95% CI, 0.51 to 1.25) for all-cause death.72 These results suggest that there is no excess cardiovascular risk with tirzepatide use; however, the exact impact of tirzepatide on cardiovascular outcomes in people with T2DM and established cardiovascular disease will be addressed in the ongoing A Study of Tirzepatide Compared With Dulaglutide on Major Cardiovascular Events in Participants With Type 2 Diabetes (SURPASS-CVOT) study (NCT04255433).
An exploratory post hoc analysis of SURPASS-4 showed that tirzepatide delayed the rate of estimated glomerular filtration rate (eGFR) decline and reduced the urine albumin to creatinine ratio (UACR) compared with insulin glargine in people with T2DM and high cardiovascular risk.73 At baseline, participants had a mean eGFR of 81 mL/min/1.73 m2 and a median UACR of 15 mg/g (17% of participants had eGFR <60 mL/min/1.73 m2, 28% had microalbuminuria, and 8% had macroalbuminuria).73 The mean rate of eGFR decline was –1.4 mL/min/1.73 m2/year at the combined tirzepatide groups versus –3.6 mL/min/1.73 m2/year at the insulin group. UACR increased from baseline with insulin glargine (by 36.9%) but not with tirzepatide (–6.8%; between-group difference –31.9%).73 Participants on tirzepatide had lower occurrence of the composite kidney endpoint (time to first occurrence of eGFR decline of at least 40% from baseline, end-stage kidney disease, death due to kidney failure, or new-onset macroalbuminuria) compared with those who received insulin glargine (HR, 0.58; 95% CI, 0.43 to 0.8) and this finding was mainly driven by a reduction in new-onset macroalbuminuria.73
SAFETY AND TOLERABILITY
Tirzepatide 5 to 15 mg was largely well tolerated and serious adverse events during the SURPASS programme were reported by 1% to 8% of participants with early or established diabetes (SURPASS 1-3, SURPASS J-mono, and SURPASS J-combo) and by 6% to 17% of people with advanced diabetes (SURPASS 4-5)—these percentages were similar to the number of serious adverse events reported in placebo and active comparator groups (Table 4). The majority of adverse events were gastrointestinal in nature, and comparisons with semaglutide and dulaglutide show that these are similar to GLP-1 RAs. Most of the adverse events were mild-moderate in severity, dose-dependent and occurring during dose-escalation and reducing thereafter. There were very few cases of pancreatitis or cholelithiasis, and injection site reactions were also rare.60-66,68
Table 4.
Adverse events in the SURPASS and SURMOUNT-1 studies
| Trial | Treatment arm | Any AEs (%) | SAEs (%) | AEs leading to trial product discontinuation (%) | Acute pancreatitis (%) | Cholelithiasis (%) | Hypoglycemia (< 54 mg/dL) (%) | Diarrhea (%) | Nausea (%) | Vomiting (%) | Constipation (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| SURPASS-1 | Tirzepatide 5 mg (n = 121) | 69 | 4 | 3 | 0 | 1 | 0 | 12 | 12 | 3 | 6 |
| Tirzepatide 10 mg (n = 121) | 67 | 2 | 5 | 0 | 0 | 0 | 14 | 13 | 2 | 5 | |
| Tirzepatide 15 mg (n = 121) | 64 | 1 | 7 | 0 | 0 | 0 | 12 | 18 | 6 | 7 | |
| Placebo (n = 115) | 66 | 3 | 3 | 0 | 0 | 1 | 8 | 6 | 2 | 1 | |
| SURPASS-2 | Tirzepatide 5 mg (n = 470) | 64 | 7 | 5 | 0 | 0.2 | 0.6 | 13 | 17 | 6 | 7 |
| Tirzepatide 10 mg (n = 469) | 69 | 5 | 8 | 0.4 | 0.4 | 0.2 | 16 | 19 | 9 | 5 | |
| Tirzepatide 15 mg (n = 470) | 69 | 6 | 8 | 0.4 | 0.4 | 2 | 14 | 22 | 10 | 5 | |
| Semaglutide 1 mg (n = 469) | 64 | 3 | 4 | 0.6 | 0 | 0.4 | 12 | 18 | 8 | 6 | |
| SURPASS-3 | Tirzepatide 5 mg (n = 358) | 61 | 8 | 7 | 0 | 1 | 1 | 15 | 12 | 6 | NR |
| Tirzepatide 10 mg (n = 360) | 69 | 6 | 10 | 0 | <1 | 1 | 17 | 23 | 9 | NR | |
| Tirzepatide 15 mg (n = 359) | 73 | 7 | 11 | 0 | <1 | 2 | 16 | 24 | 10 | NR | |
| Insulin degludec (n = 360) | 54 | 6 | 1 | 0 | 0 | 7 | 4 | 2 | 1 | NR | |
| SURPASS-4 | Tirzepatide 5 mg (n = 329) | 71 | 15 | 11 | <1 | <1 | 9 | 13 | 12 | 5 | 5 |
| Tirzepatide 10 mg (n = 328) | 74 | 17 | 9 | <1 | <1 | 6 | 20 | 16 | 8 | 4 | |
| Tirzepatide 15 mg (n = 338) | 77 | 12 | 11 | <1 | <1 | 8 | 22 | 23 | 9 | 4 | |
| Insulin lantus (n = 1,000) | 68 | 19 | 5 | <1 | <1 | 19 | 4 | 2 | 2 | <1 | |
| SURPASS-5 | Tirzepatide 5 mg (n = 116) | 73 | 8 | 6 | 0 | 0.9 | 16 | 12 | 13 | 7 | 6 |
| Tirzepatide 10 mg (n = 119) | 68 | 11 | 8 | 0 | 0 | 19 | 13 | 18 | 8 | 7 | |
| Tirzepatide 15 mg (n = 120) | 78 | 8 | 11 | 0 | 0 | 14 | 21 | 18 | 13 | 7 | |
| Placebo (n = 120) | 68 | 8 | 3 | 0 | 0 | 13 | 10 | 3 | 3 | 2 | |
| SURPASS J-mono | Tirzepatide 5 mg (n = 159) | 82 | 5 | 8 | 0 | 1 | 0 | 17 | 12 | 8 | 15 |
| Tirzepatide 10 mg (n = 158) | 77 | 6 | 10 | 0 | 0 | 0 | 9 | 20 | 5 | 18 | |
| Tirzepatide 15 mg (n = 160) | 84 | 4 | 10 | 1 | 1 | 1 | 11 | 20 | 12 | 14 | |
| Dulaglutide 0.75 mg (n = 159) | 77 | 9 | 6 | 0 | 0 | 0 | 7 | 8 | 1 | 11 | |
| SURPASS J-combo | Tirzepatide 5 mg (n = 148) | 74 | 1 | 5 | 0 | 1 | 1 | 7 | 9 | 3 | 8 |
| Tirzepatide 10 mg (n = 147) | 74 | 7 | 5 | 0 | 1 | 1 | 14 | 14 | 7 | 14 | |
| Tirzepatide 15 mg (n = 148) | 84 | 7 | 11 | 0 | 1 | 2 | 14 | 27 | 10 | 15 | |
| SURMOUNT-1 | Tirzepatide 5 mg (n = 630) | 81 | 6 | 1 | 0.2 | 1 | 1 | 19 | 25 | 8 | 17 |
| Tirzepatide 10 mg (n = 636) | 82 | 7 | 3 | 0.2 | 1 | 2 | 21 | 33 | 11 | 17 | |
| Tirzepatide 15 mg (n = 630) | 79 | 5 | 3 | 0.2 | 0.6 | 2 | 23 | 31 | 12 | 12 | |
| Placebo (n = 643) | 72 | 7 | <1 | 0.2 | 0.9 | 0.2 | 7 | 10 | 2 | 6 |
AE, adverse event; SAE, serious adverse event; NR, not reported.
Incidence of clinically important/serious hypoglycemia (blood glucose <54 mg/dL) was low at tirzepatide groups in SURPASS 1-3, SURPASS J-mono, and combo (0% to 2%) (Table 4).60,61,63,65,66 In SURPASS-4, a high proportion of participants were on sulfonylureas (54%); however, the incidence of serious hypoglycemia in the tirzepatide groups (6% to 9%) was lower than that observed with insulin glargine (19%).62 On the other hand, in SURPASS-5 where all the participants were on background insulin glargine, the rates of serious hypoglycemia in the tirzepatide groups were higher (14% to 19%) compared to the placebo group (13%).64 In summary, treatment with tirzepatide does not appear to increase the risk of hypoglycemia unless it is combined with insulin or sulfonylurea.
TIRZEPATIDE AS TREATMENT FOR OBESITY IN PEOPLE WITHOUT DIABETES
At the recently published SURMOUNT-1 study, 2,539 participants with obesity or overweight were randomised to tirzepatide 5, 10, or 15 mg or placebo along with a moderate intensity lifestyle intervention.74 At 72 weeks, the mean WL was 16% to 22.5% in tirzepatide 5 to 15 mg groups versus 2.4% WL in the placebo group (Table 2). The 31.6% to 62.9% of participants treated with tirzepatide 5 to 15 mg achieved ≥20% WL and 16.5% to 39.7% achieved ≥25% WL compared to 1.3% and 0.3% with placebo, respectively.74 More than 95% of people with prediabetes converted to normoglycemia (HbA1c <5.7%) at 72 weeks, as compared to 62% of participants in the placebo group.74
Cardiometabolic risk factors (waist circumference, blood pressure, and lipids), inflammatory markers, and the physical function were all improved with tirzepatide compared to placebo in SURMOUNT-1 (Table 3).74
The most reported adverse events were similar to those at SURPASS program (nausea, diarrhea, vomiting, and constipation) (Table 4). Only 4.3% to 7.1% of participants taking tirzepatide discontinued the medication due to adverse events. In SURMOUNT-1, cholecystitis was reported more frequently with tirzepatide compared to placebo (overall incidence was still low <0.6%), possibly due to the considerable weight reduction with the medication.74
DISCUSSION
The WL (5.4 to 12.9 kg) and the improvement in glycemic control (1.87% to 3.02% HbA1c reduction) achieved with tirzepatide in SUPRASS programme suggests that we are entering a new era in T2DM pharmacotherapy where ≥10% WL and even ≥15% WL together with HbA1c ≤6.5% are feasible targets, independent of background glucose-lowering agents and even in people with >10 years of T2DM duration. In all the clinical trials with active comparators (basal insulins and once weekly GLP-1 RAs such as dulaglutide up to 1.5 mg and semaglutide 1 mg), tirzepatide was more efficacious not only in improving glycemia, but also in achieving clinically significant WL and improving multiple cardiometabolic risk factors. Based on these findings, the latest ADA/EASD 2022 consensus guidelines for T2DM recommend tirzepatide as a treatment with very high efficacy in helping people achieving both the glycemic and WL targets; however, data on cardiovascular outcomes with tirzepatide is currently limited compared to other glucose-lowering medications with known cardio-protective actions such as GLP-1 RAs and sodium-glucose co-transporter 2 (SGLT2) inhibitors.7 The ongoing SURPASS-CVOT trial will provide definite evidence on the effect of tirzepatide on cardiovascular outcomes in people with T2DM and established cardiovascular disease, but until then GLP-1 RAs and SGLT2 inhibitor with proven cardiovascular benefits remain the recommended glucose-lowering treatments for people with T2DM and pre-existing atherosclerotic cardiovascular disease or very high cardiovascular risk.7
In SURPASS-2, tirzepatide was compared to the GLP-1 RA semaglutide 1 mg which is also considered a treatment with very high efficacy for WL and glycemia improvement in people with T2DM. A composite outcome of (1) an HbA1c ≤6.5% together with (2) ≥10% WL and (3) without episodes of severe or clinically significant hypoglycemia was achieved by 22% of participants at the semaglutide 1 mg group, compared to 32% to 60% at the tirzepatide 5 to 15 mg groups after 40 weeks of treatment, demonstrating the potential of tirzepatide to improve further the current management of people with T2DM and obesity compared to the currently used GLP-1 RAs.61 Mechanistic studies have shown significant improvements in insulin sensitivity, β-cell function as well as reduction in glucagon secretion with tirzepatide 15 mg compared to semaglutide 1 mg in people with T2DM, which can explain the better efficacy of tirzepatide in improving glycemia.57 On the other hand, the reduction in energy intake during an ad libitum lunch (buffet style) with tirzepatide 15 mg (–348.4 kcal) was not significantly different compared to semaglutide 1 mg (–284.1 kcal, P=0.19) which may suggest that mechanisms other than reduced food intake and appetite are contributed to the more WL observed with tirzepatide 15 mg versus semaglutide 1 mg.59 An adjusted indirect treatment comparison between semaglutide 2 mg (the highest approved semaglutide dose for T2DM treatment) and tirzepatide 5 to 15 mg also showed that tirzepatide 10 and 15 mg reduced the weight (by 3.15 to 5.15 kg) and HbA1c (by 0.36% to 0.4%) significantly more compared to semaglutide 2 mg.75
The exact molecular mechanisms behind the more powerful therapeutic effects of tirzepatide in glycemic control and WL versus GLP-1 RA comparators are still under investigation.28 One hypothesis is that GLP-1 activity lowers glucose levels, facilitating the effects of GIP on re-sensitised β-cells76; however, other GLP-1/GIP dual agonists have not produced the same results as tirzepatide.77 Tirzepatide appears also to act as a biased agonist compared to GLP-1, with little β-arrestin recruitment and receptor internalization, which may explain the superior activity on target cells.76
In studies where T2DM treatment was escalated to tirzepatide vs initiation of basal insulin (SURPASS-3 and SURPASS-4), the estimated treatment difference regarding weight between the two groups was between 9.0 and 15.3 kg. The better glycemic control compared to basal insulin seems to be mainly due to the reduction of postprandial hyperglycemia.70 Moreover, in SURPASS-4, WL and improvement in HbA1c was maintained for 2 years with tirzepatide, providing some initial evidence for sustained improvements over time.62,68
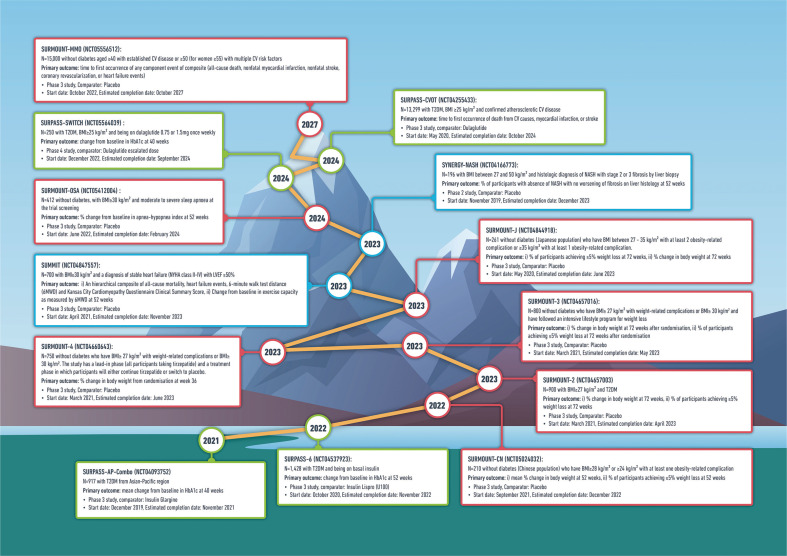
In SURPASS-5, tirzepatide was added to background basal insulin and there was an increase in episodes of hypoglycemia compared to placebo—clinicians may wish to consider reducing the dose of basal insulin by at least 20% on initiation of tirzepatide for people with HbA1c <8% and adjusting the dose of sulfonylureas.64 The ongoing SURPASS-6 study will also assess the safety and efficacy of adding tirzepatide versus prandial insulin lispro three times/day in people with T2DM who are already on basal insulin (Fig. 4).
Figure 4.
Selected ongoing clinical trials with tirzepatide (SURPASS program [green boxes], SURMOUNT program [red boxes], and other studies [blue boxes]). SURMOUNT-MMO, A Study of Tirzepatide on the Reduction on Morbidity and Mortality in Adults With Obesity; CV, cardiovascular; SURPASS-CVOT, A Study of Tirzepatide Compared With Dulaglutide on Major Cardiovascular Events in Participants With Type 2 Diabetes; T2DM, type 2 diabetes mellitus; BMI, body mass index; SURPASSSWITCH, A Study of Tirzepatide in Adult Participants With Type 2 Diabetes Switching From Dulaglutide; HbA1c, glycosylated hemoglobin; SYNERGY-NASH, A Study of Tirzepatide (LY3298176) in Participants With Nonalcoholic Steatohepatitis (NASH); NASH, nonalcoholic steatohepatitis; SURMOUNT-OSA, Obstructive Sleep Apnea Master Protocol GPIF: A Study of Tirzepatide in Participants With Obstructive Sleep Apnea; SUMMIT, A Study of Tirzepatide in Participants With Heart Failure With Preserved Ejection Fraction and Obesity; NYHA, New York Heart Association; LVEF, left ventricular ejection fraction; SURPASS-AP-Combo, A Study of Tirzepatide in Participants With Type 2 Diabetes on Metformin With or Without Sulfonylurea; SURMOUNT-CN, A Study of Tirzepatide in Chinese Participants Without Type 2 Diabetes Who Have Obesity or Overweight.
SURPASS J trials showed that the Japanese population tended to have greater HbA1c reductions with tirzepatide than the global population (from similar baselines), which may be due to differences in β-cell function and decreased insulin resistance in Asian populations compared to White populations.65,68
Based on the pharmacokinetics of tirzepatide in people with impaired kidney function, no dose adjustment is recommended for patients with renal impairment.78 However, there is very limited data with tirzepatide in people with severe renal impairment as SURPASS program (except from SURPASS-4 study) excluded participants with eGFR <30 mL/min/1.73 m2. An exploratory analysis of SURPASS-4, demonstrated that tirzepatide may have renoprotective actions compared to insulin glargine and these benefits were more pronounced in people with impaired kidney function, supporting the design of future clinical trials with tirzepatide in people with pre-existing kidney disease.73
People with non-proliferative diabetic retinopathy requiring acute therapy, proliferative diabetic retinopathy and macular edema have not been studied in the SURPASS program and for these patients tirzepatide should be used with caution and appropriate monitoring. Similarly, tirzepatide should be used with caution for those with a history of pancreatitis as this population has been excluded from the SURPASS studies.
Further research is also needed to establish the most appropriate time points in the T2DM continuum to initiate tirzepatide in different populations. For people with severe obesity (body mass index ≥35 kg/m2) and T2DM, evidence from bariatric surgery suggests that the earlier after the T2DM diagnosis that significant WL is achieved and maintained, the lower is the long-term risk for developing micro- and macrovascular complications.79 However, whether tirzepatide will lead to similar outcomes to bariatric surgery and whether this will be a cost-effective approach requires further assessment.
In people with obesity without T2DM, tirzepatide 10 and 15 mg for 72 weeks resulted in 35.0% to 39.7% achieving ≥25% WL. Though tirzepatide has not yet been approved for treatment of obesity, these results suggest that it may be more efficacious than semaglutide 2.4 mg once weekly (an approved treatment for obesity) in people without diabetes, and it approaches the effectiveness of sleeve gastrectomy.80 Lean muscle mass maintenance for people who achieve large amounts of WL with tirzepatide may become a challenge and the addition of exercise may help to improve body composition and physical function. The ongoing SURMOUNT program will assess the efficacy and safety of tirzepatide as treatment for chronic weight management in combination with different lifestyle interventions and in different populations.
FUTURE STUDIES WITH TIRZEPATIDE
The safety and efficacy of tirzepatide in populations with T2DM from the Asian-Pacific region will be evaluated at the A Study of Tirzepatide in Participants With Type 2 Diabetes on Metformin With or Without Sulfonylurea (SURPASS-AP-Combo). As discussed before, the SURPASS-CVOT will assess the non-inferiority and superiority of tirzepatide against dulaglutide 1.5 mg on cardiovascular safety in people with T2DM and confirmed atherosclerotic cardiovascular disease (Fig. 4).
Looking at the SURMOUNT program, the efficacy of tirzepatide for weight management in people with overweight/obesity and T2DM will be assessed in SURMOUNT-2. The ability of tirzepatide to maintain or add to WL achieved after an intensive lifestyle modification program will be investigated in SURMOUNT-3 when the SURMOUNT-4 will assess the effect of continuing tirzepatide vs switching to placebo on WL maintenance in adults with overweight or obesity. The A Study of Tirzepatide in Chinese Participants Without Type 2 Diabetes Who Have Obesity or Overweight (SURMOUNT-CN) and the SURMOUNT-J studies will evaluate tirzepatide as treatment for obesity in Chinese and Japanese populations without diabetes.
The effect of tirzepatide on morbidity and mortality in a high cardiovascular risk population living with obesity (without diabetes) will be assessed at the A Study of Tirzepatide on the Reduction on Morbidity and Mortality in Adults With Obesity (SURMOUNT-MMO) trial. Until today, no pharmacological intervention for chronic weight management has demonstrated reduction in major cardiovascular events in people living with obesity without diabetes; the Semaglutide Effects on Heart Disease and Stroke in Patients With Overweight or Obesity (SELECT) trial with semaglutide 2.4 mg once weekly is also expected to be completed in September 2023.
Apart from the SURPASS and SURMOUNT programs, the impact of tirzepatide in people with heart failure with preserved ejection fraction and obesity and in people with nonalcoholic steatohepatitis will be assessed at the SUMMIT and A Study of Tirzepatide (LY3298176) in Participants With Nonalcoholic Steatohepatitis (NASH) (SYNERGY-NASH) trial, respectively.
FURTHER POTENTIAL TREATMENTS FOR OBESITY AND T2DM
Beyond the GLP-1 and GIP co-agonism, multiple gut hormones are undergoing early phase clinical trials in combination with GLP-1 (as dual or triple agonists) as potential treatments for obesity and T2DM.81-84
Glucagon, a peptide secreted from pancreatic α-cells, which increases the blood glucose but also reduces energy intake and increase the energy expenditure could complement and enhance the WL actions of GLP-1.85 Currently, dual agonists acting on both GLP-1 and glucagon receptors (BI 456906 and SAR428599) are undergoing early phase clinical trials as treatments for T2DM and obesity.86
The clinical success of dual GLP-1/GIP agonism with tirzepatide on WL may also be surpassed by including glucagon receptor agonism. Triple agonists acting on GLP-1, GIP, and glucagon receptors (such as LY3437943 and SAR441255) have shown encouraging results in preclinical studies as well as in phase 1 clinical trials in terms of safety, tolerability, WL, and glucose-lowering effect.87,88
Another promising combination of gut hormones which has progressed to phase 3 trials (A Research Study to See How Well CagriSema Helps People With Type 2 Diabetes and Excess Body Weight Lose Weight [REDEFINE 2], NCT05394519) is the Cagri-Sema (2.4 mg/2.4 mg), a combination of semaglutide 2.4 mg with a new once weekly amylin analogue, cagrilintide 2.4 mg. Amylin agonism reduces the appetite and food intake and has also glucose-lowering actions by slowing the gastric emptying and suppressing glucagon secretion.89 In a phase 1b study, cagrilintide 2.4 mg in combination with semaglutide 2.4 mg led to 17.1% WL at 20 weeks compared with 9.8% loss with semaglutide 2.4 mg plus placebo with good tolerability.82
In the near future, there is a real prospect for gut hormone combinations to deliver improved outcomes over the currently available treatments for T2DM and obesity.
CONCLUSION
The efficacy and safety of once weekly subcutaneous tirzepatide in people with T2DM and/or obesity is supported by a growing body of evidence through the SURPASS and SURMOUNT clinical trial programmes. Tirzepatide marks a new era in the pharmacotherapy of T2DM and/or obesity where double digit WL and maintenance together with excellent glycemic control and optimisation of multiple cardiometabolic risk factors is feasible through combination of gut hormones. Additional research assessing long-term cardiovascular safety and effectiveness of tirzepatide as well as its potential impact on other cardiometabolic complications is awaited over the next years to help us understand better its position in the treatment algorithms for people with T2DM and/or obesity.
ACKNOWLEDGMENTS
This work was supported by the National Institute for Health and Care Research (NIHR) Leicester Biomedical Research Centre.
Footnotes
CONFLICTS OF INTEREST
Dimitris Papamargaritis has acted as speaker for Novo Nordisk and has received grants from Novo Nordisk, Novo Nordisk UK Research Foundation, Academy of Medical Sciences/Diabetes UK and Health Education East Midlands. Jack A. Sargeant has received funding in the form of an investigator-initiated study grant from AstraZeneca UK. Melanie J. Davies has acted as consultant, advisory board member and speaker for Boehringer Ingelheim, Lilly, Novo Nordisk, and Sanofi, an advisory board member and speaker for AstraZeneca, an advisory board member for Janssen, Lexicon, Pfizer and ShouTi Pharma Inc., a speaker for Napp Pharmaceuticals, Novartis and Takeda Pharmaceuticals International Inc. and has received grants in support of investigator and investigator-initiated trials from Novo Nordisk, Sanofi-Aventis, Lilly, Boehringer Ingelheim, Astrazeneca, and Janssen.
AUTHOR CONTRIBUTIONS
Study concept and design: RS, DP, JAS, and MJD; drafting of the manuscript: RS and DP; critical revision of the manuscript: JAS and MJD; and study supervision: DP, JAS, and MJD.
REFERENCES
- 1.NCD Risk Factor Collaboration (NCD-RisC), author Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387:1377–96. doi: 10.1016/S0140-6736(16)30054-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Min T, Bain SC. The role of tirzepatide, dual GIP and GLP-1 receptor agonist, in the management of type 2 diabetes: the SURPASS clinical trials. Diabetes Ther. 2021;12:143–57. doi: 10.1007/s13300-020-00981-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leitner DR, Fruhbeck G, Yumuk V, Schindler K, Micic D, Woodward E, et al. Obesity and type 2 diabetes: two diseases with a need for combined treatment strategies: EASO can lead the way. Obes Facts. 2017;10:483–92. doi: 10.1159/000480525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fried M, Yumuk V, Oppert JM, Scopinaro N, Torres A, Weiner R, et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg. 2014;24:42–55. doi: 10.1007/s11695-013-1079-8. [DOI] [PubMed] [Google Scholar]
- 5.Fruhbeck G, Toplak H, Woodward E, Yumuk V, Maislos M, Oppert JM. Obesity: the gateway to ill health: an EASO position statement on a rising public health, clinical and scientific challenge in Europe. Obes Facts. 2013;6:117–20. doi: 10.1159/000350627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lingvay I, Sumithran P, Cohen RV, le Roux CW. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Lancet. 2022;399:394–405. doi: 10.1016/S0140-6736(21)01919-X. [DOI] [PubMed] [Google Scholar]
- 7.Davies MJ, Aroda VR, Collins BS, Gabbay RA, Green J, Maruthur NM, et al. Management of hyperglycaemia in type 2 diabetes, 2022: a consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetologia. 2022;65:1925–66. doi: 10.1007/s00125-022-05787-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cefalu WT, Bray GA, Home PD, Garvey WT, Klein S, Pi-Sunyer FX, et al. Advances in the science, treatment, and prevention of the disease of obesity: reflections from a diabetes care editors' expert forum. Diabetes Care. 2015;38:1567–82. doi: 10.2337/dc15-1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lean MEJ, Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L, et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol. 2019;7:344–55. doi: 10.1016/S2213-8587(19)30068-3. [DOI] [PubMed] [Google Scholar]
- 10.Look AHEAD Research Group, author. Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: a post-hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2016;4:913–21. doi: 10.1016/S2213-8587(16)30162-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Look AHEAD Research Group, author. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369:145–54. doi: 10.1056/NEJMoa1212914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Look AHEAD Research Group, author. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity (Silver Spring) 2014;22:5–13. doi: 10.1002/oby.20662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hall KD, Kahan S. Maintenance of lost weight and long-term management of obesity. Med Clin North Am. 2018;102:183–97. doi: 10.1016/j.mcna.2017.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sjostrom L. Review of the key results from the Swedish Obese Subjects (SOS) trial: a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273:219–34. doi: 10.1111/joim.12012. [DOI] [PubMed] [Google Scholar]
- 15.Palmer SC, Tendal B, Mustafa RA, Vandvik PO, Li S, Hao Q, et al. Sodium-glucose cotransporter protein-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. BMJ. 2021;372:m4573. doi: 10.1136/bmj.m4573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sattar N, Lee MM, Kristensen SL, Branch KR, Del Prato S, Khurmi NS, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of randomised trials. Lancet Diabetes Endocrinol. 2021;9:653–62. doi: 10.1016/S2213-8587(21)00203-5. [DOI] [PubMed] [Google Scholar]
- 17.Pi-Sunyer X, Astrup A, Fujioka K, Greenway F, Halpern A, Krempf M, et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N Engl J Med. 2015;373:11–22. doi: 10.1056/NEJMoa1411892. [DOI] [PubMed] [Google Scholar]
- 18.Wadden TA, Hollander P, Klein S, Niswender K, Woo V, Hale PM, et al. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet-induced weight loss: the SCALE maintenance randomized study. Int J Obes (Lond) 2013;37:1443–51. doi: 10.1038/ijo.2013.120. [DOI] [PubMed] [Google Scholar]
- 19.Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384:989–1002. doi: 10.1056/NEJMoa2032183. [DOI] [PubMed] [Google Scholar]
- 20.Garvey WT, Birkenfeld AL, Dicker D, Mingrone G, Pedersen SD, Satylganova A, et al. Efficacy and safety of liraglutide 3.0 mg in individuals with overweight or obesity and type 2 diabetes treated with basal insulin: the SCALE insulin randomized controlled trial. Diabetes Care. 2020;43:1085–93. doi: 10.2337/dc19-1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davies MJ, Bergenstal R, Bode B, Kushner RF, Lewin A, Skjoth TV, et al. Efficacy of liraglutide for weight loss among patients with type 2 diabetes: the SCALE diabetes randomized clinical trial. JAMA. 2015;314:687–99. doi: 10.1001/jama.2015.9676. [DOI] [PubMed] [Google Scholar]
- 22.Wadden TA, Bailey TS, Billings LK, Davies M, Frias JP, Koroleva A, et al. Effect of subcutaneous semaglutide vs placebo as an adjunct to intensive behavioral therapy on body weight in adults with overweight or obesity: the STEP 3 randomized clinical trial. JAMA. 2021;325:1403–13. doi: 10.1001/jama.2021.1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rubino D, Abrahamsson N, Davies M, Hesse D, Greenway FL, Jensen C, et al. Effect of continued weekly subcutaneous semaglutide vs placebo on weight loss maintenance in adults with overweight or obesity: the STEP 4 randomized clinical trial. JAMA. 2021;325:1414–25. doi: 10.1001/jama.2021.3224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davies M, Færch L, Jeppesen OK, Pakseresht A, Pedersen SD, Perreault L, et al. Semaglutide 2.4 mg once a week in adults with overweight or obesity, and type 2 diabetes (STEP 2): a randomised, double-blind, double-dummy, placebo-controlled, phase 3 trial. Lancet. 2021;397:971–84. doi: 10.1016/S0140-6736(21)00213-0. [DOI] [PubMed] [Google Scholar]
- 25.Bettge K, Kahle M, Abd El Aziz MS, Meier JJ, Nauck MA. Occurrence of nausea, vomiting and diarrhoea reported as adverse events in clinical trials studying glucagon-like peptide-1 receptor agonists: a systematic analysis of published clinical trials. Diabetes Obes Metab. 2017;19:336–47. doi: 10.1111/dom.12824. [DOI] [PubMed] [Google Scholar]
- 26.Khunti K, Ceriello A, Cos X, De Block C. Achievement of guideline targets for blood pressure, lipid, and glycaemic control in type 2 diabetes: a meta-analysis. Diabetes Res Clin Pract. 2018;137:137–48. doi: 10.1016/j.diabres.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 27.Alexiadou K, Anyiam O, Tan T. Cracking the combination: gut hormones for the treatment of obesity and diabetes. J Neuroendocrinol. 2019;31:e12664. doi: 10.1111/jne.12664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baggio LL, Drucker DJ. Glucagon-like peptide-1 receptor co-agonists for treating metabolic disease. Mol Metab. 2021;46:101090. doi: 10.1016/j.molmet.2020.101090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miras AD, le Roux CW. Can medical therapy mimic the clinical efficacy or physiological effects of bariatric surgery? Int J Obes (Lond) 2014;38:325–33. doi: 10.1038/ijo.2013.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nauck MA, Meier JJ. The incretin effect in healthy individuals and those with type 2 diabetes: physiology, pathophysiology, and response to therapeutic interventions. Lancet Diabetes Endocrinol. 2016;4:525–36. doi: 10.1016/S2213-8587(15)00482-9. [DOI] [PubMed] [Google Scholar]
- 31.Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet. 2006;368:1696–705. doi: 10.1016/S0140-6736(06)69705-5. [DOI] [PubMed] [Google Scholar]
- 32.Muller TD, Finan B, Bloom SR, D'Alessio D, Drucker DJ, Flatt PR, et al. Glucagon-like peptide 1 (GLP-1) Mol Metab. 2019;30:72–130. doi: 10.1016/j.molmet.2019.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev. 2007;87:1409–39. doi: 10.1152/physrev.00034.2006. [DOI] [PubMed] [Google Scholar]
- 34.Nauck MA, Heimesaat MM, Orskov C, Holst JJ, Ebert R, Creutzfeldt W. Preserved incretin activity of glucagon-like peptide 1 [7-36 amide] but not of synthetic human gastric inhibitory polypeptide in patients with type-2 diabetes mellitus. J Clin Invest. 1993;91:301–7. doi: 10.1172/JCI116186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Flint A, Raben A, Astrup A, Holst JJ. Glucagon-like peptide 1 promotes satiety and suppresses energy intake in humans. J Clin Invest. 1998;101:515–20. doi: 10.1172/JCI990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Naslund E, Barkeling B, King N, Gutniak M, Blundell JE, Holst JJ, et al. Energy intake and appetite are suppressed by glucagon-like peptide-1 (GLP-1) in obese men. Int J Obes Relat Metab Disord. 1999;23:304–11. doi: 10.1038/sj.ijo.0800818. [DOI] [PubMed] [Google Scholar]
- 37.Meier JJ, Gallwitz B, Siepmann N, Holst JJ, Deacon CF, Schmidt WE, et al. Gastric inhibitory polypeptide (GIP) dose-dependently stimulates glucagon secretion in healthy human subjects at euglycaemia. Diabetologia. 2003;46:798–801. doi: 10.1007/s00125-003-1103-y. [DOI] [PubMed] [Google Scholar]
- 38.Khoo B, Tan TM. Combination gut hormones: prospects and questions for the future of obesity and diabetes therapy. J Endocrinol. 2020;246:R65–74. doi: 10.1530/JOE-20-0119. [DOI] [PubMed] [Google Scholar]
- 39.Christensen MB, Gasbjerg LS, Heimburger SM, Stensen S, Vilsboll T, Knop FK. GIP's involvement in the pathophysiology of type 2 diabetes. Peptides. 2020;125:170178. doi: 10.1016/j.peptides.2019.170178. [DOI] [PubMed] [Google Scholar]
- 40.Hojberg PV, Vilsboll T, Rabol R, Knop FK, Bache M, Krarup T, et al. Four weeks of near-normalisation of blood glucose improves the insulin response to glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide in patients with type 2 diabetes. Diabetologia. 2009;52:199–207. doi: 10.1007/s00125-008-1195-5. [DOI] [PubMed] [Google Scholar]
- 41.Lund A, Vilsboll T, Bagger JI, Holst JJ, Knop FK. The separate and combined impact of the intestinal hormones, GIP, GLP-1, and GLP-2, on glucagon secretion in type 2 diabetes. Am J Physiol Endocrinol Metab. 2011;300:E1038–46. doi: 10.1152/ajpendo.00665.2010. [DOI] [PubMed] [Google Scholar]
- 42.Samms RJ, Coghlan MP, Sloop KW. How may GIP enhance the therapeutic efficacy of GLP-1? Trends Endocrinol Metab. 2020;31:410–21. doi: 10.1016/j.tem.2020.02.006. [DOI] [PubMed] [Google Scholar]
- 43.Thondam SK, Daousi C, Wilding JP, Holst JJ, Ameen GI, Yang C, et al. Glucose-dependent insulinotropic polypeptide promotes lipid deposition in subcutaneous adipocytes in obese type 2 diabetes patients: a maladaptive response. Am J Physiol Endocrinol Metab. 2017;312:E224–33. doi: 10.1152/ajpendo.00347.2016. [DOI] [PubMed] [Google Scholar]
- 44.Christensen MB, Lund A, Calanna S, Jorgensen NR, Holst JJ, Vilsboll T, et al. Glucose-dependent insulinotropic polypeptide (GIP) inhibits bone resorption independently of insulin and glycemia. J Clin Endocrinol Metab. 2018;103:288–94. doi: 10.1210/jc.2017-01949. [DOI] [PubMed] [Google Scholar]
- 45.Zhang Q, Delessa CT, Augustin R, Bakhti M, Collden G, Drucker DJ, et al. The glucose-dependent insulinotropic polypeptide (GIP) regulates body weight and food intake via CNS-GIPR signaling. Cell Metab. 2021;33:833–44.e5. doi: 10.1016/j.cmet.2021.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Finan B, Ma T, Ottaway N, Muller TD, Habegger KM, Heppner KM, et al. Unimolecular dual incretins maximize metabolic benefits in rodents, monkeys, and humans. Sci Transl Med. 2013;5:209ra151. doi: 10.1126/scitranslmed.3007218. [DOI] [PubMed] [Google Scholar]
- 47.Gault VA, Kerr BD, Harriott P, Flatt PR. Administration of an acylated GLP-1 and GIP preparation provides added beneficial glucose-lowering and insulinotropic actions over single incretins in mice with type 2 diabetes and obesity. Clin Sci (Lond) 2011;121:107–17. doi: 10.1042/CS20110006. [DOI] [PubMed] [Google Scholar]
- 48.Norregaard PK, Deryabina MA, Tofteng Shelton P, Fog JU, Daugaard JR, Eriksson PO, et al. A novel GIP analogue, ZP4165, enhances glucagon-like peptide-1-induced body weight loss and improves glycaemic control in rodents. Diabetes Obes Metab. 2018;20:60–8. doi: 10.1111/dom.13034. [DOI] [PubMed] [Google Scholar]
- 49.Bergmann NC, Lund A, Gasbjerg LS, Meessen EC, Andersen MM, Bergmann S, et al. Effects of combined GIP and GLP-1 infusion on energy intake, appetite and energy expenditure in overweight/obese individuals: a randomised, crossover study. Diabetologia. 2019;62:665–75. doi: 10.1007/s00125-018-4810-0. [DOI] [PubMed] [Google Scholar]
- 50.Bergmann NC, Gasbjerg LS, Heimburger SM, Krogh LS, Dela F, Hartmann B, et al. No acute effects of exogenous glucose-dependent insulinotropic polypeptide on energy intake, appetite, or energy expenditure when added to treatment with a long-acting glucagon-like peptide 1 receptor agonist in men with type 2 diabetes. Diabetes Care. 2020;43:588–96. doi: 10.2337/dc19-0578. [DOI] [PubMed] [Google Scholar]
- 51.Syed YY. Tirzepatide: first approval. Drugs. 2022;82:1213–20. doi: 10.1007/s40265-022-01746-8. [DOI] [PubMed] [Google Scholar]
- 52.Willard FS, Douros JD, Gabe MB, Showalter AD, Wainscott DB, Suter TM, et al. Tirzepatide is an imbalanced and biased dual GIP and GLP-1 receptor agonist. JCI Insight. 2020;5:e140532. doi: 10.1172/jci.insight.140532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Coskun T, Sloop KW, Loghin C, Alsina-Fernandez J, Urva S, Bokvist KB, et al. LY3298176, a novel dual GIP and GLP-1 receptor agonist for the treatment of type 2 diabetes mellitus: from discovery to clinical proof of concept. Mol Metab. 2018;18:3–14. doi: 10.1016/j.molmet.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Furihata K, Mimura H, Urva S, Oura T, Ohwaki K, Imaoka T. A phase 1 multiple-ascending dose study of tirzepatide in Japanese participants with type 2 diabetes. Diabetes Obes Metab. 2022;24:239–46. doi: 10.1111/dom.14572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Frias JP, Nauck MA, Van J, Kutner ME, Cui X, Benson C, et al. Efficacy and safety of LY3298176, a novel dual GIP and GLP-1 receptor agonist, in patients with type 2 diabetes: a randomised, placebo-controlled and active comparator-controlled phase 2 trial. Lancet. 2018;392:2180–93. doi: 10.1016/S0140-6736(18)32260-8. [DOI] [PubMed] [Google Scholar]
- 56.Frias JP, Nauck MA, Van J, Benson C, Bray R, Cui X, et al. Efficacy and tolerability of tirzepatide, a dual glucose-dependent insulinotropic peptide and glucagon-like peptide-1 receptor agonist in patients with type 2 diabetes: a 12-week, randomized, double-blind, placebo-controlled study to evaluate different dose-escalation regimens. Diabetes Obes Metab. 2020;22:938–46. doi: 10.1111/dom.13979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Heise T, Mari A, DeVries JH, Urva S, Li J, Pratt EJ, et al. Effects of subcutaneous tirzepatide versus placebo or semaglutide on pancreatic islet function and insulin sensitivity in adults with type 2 diabetes: a multicentre, randomised, double-blind, parallel-arm, phase 1 clinical trial. Lancet Diabetes Endocrinol. 2022;10:418–29. doi: 10.1016/S2213-8587(22)00085-7. [DOI] [PubMed] [Google Scholar]
- 58.Urva S, Coskun T, Loghin C, Cui X, Beebe E, O'Farrell L, et al. The novel dual glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1 (GLP-1) receptor agonist tirzepatide transiently delays gastric emptying similarly to selective long-acting GLP-1 receptor agonists. Diabetes Obes Metab. 2020;22:1886–91. doi: 10.1111/dom.14110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Coskun T, Heise T, DeVries J, Urva S, Li J, Pratt EJ, et al. 338-OR: Tirzepatide reduces appetite, energy intake, and fat mass in people with T2D. Diabetes. 2022;71(Supplement_1):338–OR. doi: 10.2337/db22-338-OR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rosenstock J, Wysham C, Frias JP, Kaneko S, Lee CJ, Fernandez Lando L, et al. Efficacy and safety of a novel dual GIP and GLP-1 receptor agonist tirzepatide in patients with type 2 diabetes (SURPASS-1): a double-blind, randomised, phase 3 trial. Lancet. 2021;398:143–55. doi: 10.1016/S0140-6736(21)01324-6. [DOI] [PubMed] [Google Scholar]
- 61.Frias JP, Davies MJ, Rosenstock J, Perez Manghi FC, Fernandez Lando L, Bergman BK, et al. Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. N Engl J Med. 2021;385:503–15. doi: 10.1056/NEJMoa2107519. [DOI] [PubMed] [Google Scholar]
- 62.Del Prato S, Kahn SE, Pavo I, Weerakkody GJ, Yang Z, Doupis J, et al. Tirzepatide versus insulin glargine in type 2 diabetes and increased cardiovascular risk (SURPASS-4): a randomised, open-label, parallel-group, multicentre, phase 3 trial. Lancet. 2021;398:1811–24. doi: 10.1016/S0140-6736(21)02188-7. [DOI] [PubMed] [Google Scholar]
- 63.Ludvik B, Giorgino F, Jodar E, Frias JP, Fernandez Lando L, Brown K, et al. Once-weekly tirzepatide versus once-daily insulin degludec as add-on to metformin with or without SGLT2 inhibitors in patients with type 2 diabetes (SURPASS-3): a randomised, open-label, parallel-group, phase 3 trial. Lancet. 2021;398:583–98. doi: 10.1016/S0140-6736(21)01443-4. [DOI] [PubMed] [Google Scholar]
- 64.Dahl D, Onishi Y, Norwood P, Huh R, Bray R, Patel H, et al. Effect of subcutaneous tirzepatide vs placebo added to titrated insulin glargine on glycemic control in patients with type 2 diabetes: the SURPASS-5 randomized clinical trial. JAMA. 2022;327:534–45. doi: 10.1001/jama.2022.0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Inagaki N, Takeuchi M, Oura T, Imaoka T, Seino Y. Efficacy and safety of tirzepatide monotherapy compared with dulaglutide in Japanese patients with type 2 diabetes (SURPASS J-mono): a double-blind, multicentre, randomised, phase 3 trial. Lancet Diabetes Endocrinol. 2022;10:623–33. doi: 10.1016/S2213-8587(22)00188-7. [DOI] [PubMed] [Google Scholar]
- 66.Kadowaki T, Chin R, Ozeki A, Imaoka T, Ogawa Y. Safety and efficacy of tirzepatide as an add-on to single oral antihyperglycaemic medication in patients with type 2 diabetes in Japan (SURPASS J-combo): a multicentre, randomised, open-label, parallel-group, phase 3 trial. Lancet Diabetes Endocrinol. 2022;10:634–44. doi: 10.1016/S2213-8587(22)00187-5. [DOI] [PubMed] [Google Scholar]
- 67.Frias JP. Tirzepatide: a glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) dual agonist in development for the treatment of type 2 diabetes. Expert Rev Endocrinol Metab. 2020;15:379–94. doi: 10.1080/17446651.2020.1830759. [DOI] [PubMed] [Google Scholar]
- 68.De Block C, Bailey C, Wysham C, Hemmingway A, Allen SE, Peleshok J. Tirzepatide for the treatment of adults with type 2 diabetes: an endocrine perspective. Diabetes Obes Metab. 2023;25:3–17. doi: 10.1111/dom.14831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nauck MA, D'Alessio DA. Tirzepatide, a dual GIP/GLP-1 receptor co-agonist for the treatment of type 2 diabetes with unmatched effectiveness regrading glycaemic control and body weight reduction. Cardiovasc Diabetol. 2022;21:169. doi: 10.1186/s12933-022-01604-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Battelino T, Bergenstal RM, Rodriguez A, Fernandez Lando L, Bray R, Tong Z, et al. Efficacy of once-weekly tirzepatide versus once-daily insulin degludec on glycaemic control measured by continuous glucose monitoring in adults with type 2 diabetes (SURPASS-3 CGM): a substudy of the randomised, open-label, parallel-group, phase 3 SURPASS-3 trial. Lancet Diabetes Endocrinol. 2022;10:407–17. doi: 10.1016/S2213-8587(22)00077-8. [DOI] [PubMed] [Google Scholar]
- 71.Gastaldelli A, Cusi K, Fernandez Lando L, Bray R, Brouwers B, Rodriguez A. Effect of tirzepatide versus insulin degludec on liver fat content and abdominal adipose tissue in people with type 2 diabetes (SURPASS-3 MRI): a substudy of the randomised, open-label, parallel-group, phase 3 SURPASS-3 trial. Lancet Diabetes Endocrinol. 2022;10:393–406. doi: 10.1016/S2213-8587(22)00070-5. [DOI] [PubMed] [Google Scholar]
- 72.Sattar N, McGuire DK, Pavo I, Weerakkody GJ, Nishiyama H, Wiese RJ, et al. Tirzepatide cardiovascular event risk assessment: a pre-specified meta-analysis. Nat Med. 2022;28:591–8. doi: 10.1038/s41591-022-01707-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Heerspink HJ, Sattar N, Pavo I, Haupt A, Duffin KL, Yang Z, et al. Effects of tirzepatide versus insulin glargine on kidney outcomes in type 2 diabetes in the SURPASS-4 trial: post-hoc analysis of an open-label, randomised, phase 3 trial. Lancet Diabetes Endocrinol. 2022;10:774–85. doi: 10.1016/S2213-8587(22)00243-1. [DOI] [PubMed] [Google Scholar]
- 74.Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. Tirzepatide once weekly for the treatment of obesity. N Engl J Med. 2022;387:205–16. doi: 10.1056/NEJMoa2206038. [DOI] [PubMed] [Google Scholar]
- 75.Vadher K, Patel H, Mody R, Levine JA, Hoog M, Cheng AY, et al. Efficacy of tirzepatide 5, 10 and 15 mg versus semaglutide 2 mg in patients with type 2 diabetes: an adjusted indirect treatment comparison. Diabetes Obes Metab. 2022;24:1861–8. doi: 10.1111/dom.14775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tan TM, Khoo B. Tirzepatide and the new era of twincretins for diabetes. Lancet. 2021;398:95–7. doi: 10.1016/S0140-6736(21)01390-8. [DOI] [PubMed] [Google Scholar]
- 77.Holst JJ, Rosenkilde MM. GIP as a therapeutic target in diabetes and obesity: insight from incretin co-agonists. J Clin Endocrinol Metab. 2020;105:e2710–6. doi: 10.1210/clinem/dgaa327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Urva S, Quinlan T, Landry J, Martin J, Loghin C. Effects of renal impairment on the pharmacokinetics of the dual GIP and GLP-1 receptor agonist tirzepatide. Clin Pharmacokinet. 2021;60:1049–59. doi: 10.1007/s40262-021-01012-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sjostrom L, Peltonen M, Jacobson P, Ahlin S, Andersson-Assarsson J, Anveden A, et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA. 2014;311:2297–304. doi: 10.1001/jama.2014.5988. [DOI] [PubMed] [Google Scholar]
- 80.Arterburn D, Wellman R, Emiliano A, Smith SR, Odegaard AO, Murali S, et al. Comparative effectiveness and safety of bariatric procedures for weight loss: a PCORnet cohort study. Ann Intern Med. 2018;169:741–50. doi: 10.7326/M17-2786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Parker VE, Robertson D, Wang T, Hornigold DC, Petrone M, Cooper AT, et al. Efficacy, safety, and mechanistic insights of cotadutide, a dual receptor glucagon-like peptide-1 and glucagon agonist. J Clin Endocrinol Metab. 2020;105:dgz047. doi: 10.1210/clinem/dgz047. [DOI] [PubMed] [Google Scholar]
- 82.Enebo LB, Berthelsen KK, Kankam M, Lund MT, Rubino DM, Satylganova A, et al. Safety, tolerability, pharmacokinetics, and pharmacodynamics of concomitant administration of multiple doses of cagrilintide with semaglutide 2.4 mg for weight management: a randomised, controlled, phase 1b trial. Lancet. 2021;397:1736–48. doi: 10.1016/S0140-6736(21)00845-X. [DOI] [PubMed] [Google Scholar]
- 83.Papamargaritis D, le Roux CW, Holst JJ, Davies MJ. New therapies for obesity. Cardiovasc Res. 2022 Nov 30; doi: 10.1093/cvr/cvac176. [Epub].https://doi.org/10.1093/cvr/cvac176 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Muller TD, Bluher M, Tschop MH, DiMarchi RD. Anti-obesity drug discovery: advances and challenges. Nat Rev Drug Discov. 2022;21:201–23. doi: 10.1038/s41573-021-00337-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Habegger KM, Heppner KM, Geary N, Bartness TJ, DiMarchi R, Tschop MH. The metabolic actions of glucagon revisited. Nat Rev Endocrinol. 2010;6:689–97. doi: 10.1038/nrendo.2010.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zimmermann T, Thomas L, Baader-Pagler T, Haebel P, Simon E, Reindl W, et al. BI 456906: discovery and preclinical pharmacology of a novel GCGR/GLP-1R dual agonist with robust anti-obesity efficacy. Mol Metab. 2022;66:101633. doi: 10.1016/j.molmet.2022.101633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Urva S, Coskun T, Loh MT, Du Y, Thomas MK, Gurbuz S, et al. LY3437943, a novel triple GIP, GLP-1, and glucagon receptor agonist in people with type 2 diabetes: a phase 1b, multicentre, double-blind, placebo-controlled, randomised, multiple-ascending dose trial. Lancet. 2022;400:1869–81. doi: 10.1016/S0140-6736(22)02033-5. [DOI] [PubMed] [Google Scholar]
- 88.Bossart M, Wagner M, Elvert R, Evers A, Hubschle T, Kloeckener T, et al. Effects on weight loss and glycemic control with SAR441255, a potent unimolecular peptide GLP-1/GIP/GCG receptor triagonist. Cell Metab. 2022;34:59–74.e10. doi: 10.1016/j.cmet.2021.12.005. [DOI] [PubMed] [Google Scholar]
- 89.Dehestani B, Stratford NR, le Roux CW. Amylin as a future obesity treatment. J Obes Metab Syndr. 2021;30:320–5. doi: 10.7570/jomes21071. [DOI] [PMC free article] [PubMed] [Google Scholar]