Abstract
Cognitive impairment and dementia are burgeoning public health concerns, especially given the increasing longevity of the global population. These conditions not only affect the quality of life of individuals and their families, but also pose significant economic burdens on healthcare systems. In this context, our comprehensive narrative review critically examines the role of nutritional supplements in mitigating cognitive decline. Amidst growing interest in non-pharmacological interventions for cognitive enhancement, this review delves into the efficacy of vitamins, minerals, antioxidants, and other dietary supplements. Through a systematic evaluation of randomized controlled trials, observational studies, and meta-analysis, this review focuses on outcomes such as memory enhancement, attention improvement, executive function support, and neuroprotection. The findings suggest a complex interplay between nutritional supplementation and cognitive health, with some supplements showing promising results and others displaying limited or context-dependent effectiveness. The review highlights the importance of dosage, bioavailability, and individual differences in response to supplementation. Additionally, it addresses safety concerns and potential interactions with conventional treatments. By providing a clear overview of current scientific knowledge, this review aims to guide healthcare professionals and researchers in making informed decisions about the use of nutritional supplements for cognitive health.
Keywords: dementia, cognitive function, dietary supplement intervention, randomized controlled trial, vitamin, mineral, antioxidant, omega-3 polyunsaturated fatty acid
1. Introduction
Cognitive impairment and dementia are among the most significant health challenges of our time, especially as the global population ages [1,2,3,4]. The prevalence of dementia increases exponentially with advancing age [5,6,7], with a prevalence of 0.8% to 6.4% in the population over 65 years of age [8], and 28.5% at age 90 in the European Union [9]. The World Health Organization (WHO) estimates that approximately 50 million people worldwide live with dementia, a number expected to triple by 2050 [10]. Dementia, a syndrome encompassing over 200 conditions [11], is characterized by progressive cognitive impairment [12,13,14] and a decline in functional abilities, often accompanied by behavioral and psychological symptoms [15]. Two of the most prevalent forms of dementia are Vascular Cognitive Impairment (VCI) and Alzheimer’s Disease (AD), both contributing significantly to the global dementia burden [16,17,18,19]. These conditions not only impact the individuals suffering from them, but also place a considerable strain on families, caregivers, and healthcare systems. The societal and economic implications are profound, encompassing lost productivity, increased healthcare costs, and substantial emotional and physical burdens on caregivers [15].
The search for effective interventions to prevent, delay, or ameliorate cognitive decline is of paramount importance, especially given the complex mechanisms underlying age-related cognitive decline and dementia [20]. These mechanisms encompass a spectrum of pathologies, ranging from microvascular issues [21], including blood–brain barrier (BBB) disruption [22,23,24,25], impaired cerebral blood flow regulation [26,27,28,29], impaired glymphatic function [30], and small vessel disease [31,32] to macrovascular pathologies such as atherosclerosis [33] and stroke. Additionally, neuroinflammation [34,35], synapse loss, white matter damage [36,37] and changes in connectivity [38,39], neuronal metabolic dysfunction [40,41] and amyloid pathologies [42,43] play significant roles in the progression of cognitive impairment and dementia. These multifaceted and interrelated pathologies highlight the complexity of brain aging and the challenges in mitigating cognitive decline. While pharmacological treatments have shown some benefits, they may not fully address the multifaceted nature of cognitive decline [44,45,46]. This has led to growing interest in alternative approaches [47,48,49,50], particularly dietary interventions and nutritional supplementation [51,52,53,54], as a potential means to support cognitive health. Nutrition plays a crucial role in brain health, and deficiencies in specific nutrients have been linked to cognitive impairments [55,56,57]. This review aims to synthesize the current clinical research on the efficacy of various nutritional supplements—including vitamins, minerals, antioxidants, and other dietary components—in enhancing cognitive function and potentially mitigating the risk or progression of dementia.
Recent studies, including findings from the Chicago Health and Aging Project (CHAP), have highlighted the importance of a healthy lifestyle, comprising a balanced diet, regular physical activity, and cognitive engagement, in extending life expectancy and delaying the onset of dementia [51,58]. Moreover, as the efficiency of nutrient absorption decreases with age and is affected by certain medications, the role of dietary supplementation, such as vitamins B, C, D, antioxidants, and polyunsaturated fatty acids (PUFAs), becomes increasingly significant [59,60,61]. Moreover, elderly individuals typically engage in less physical activity and spend reduced time outdoors, leading to lower levels of sun exposure [62] and, consequently, diminished vitamin D synthesis in their skin. Given these factors, vitamin D supplementation emerges as a crucial intervention for health protection in the elderly [63]. The typical diet often lacks sufficient omega-3 PUFAs, leading to recommendations for consuming fatty fish like tuna or salmon twice a week, or taking fish oil capsules, particularly for those on a vegan diet [52,64,65,66,67,68,69,70,71,72].
This review critically examines the potential of nutritional supplements in addressing cognitive decline and dementia, taking into consideration the complexity of recommending dietary supplements based on individual dietary habits and health conditions. We aim to provide a comprehensive overview of the evidence supporting the use of nutritional supplements for cognitive health and to inform healthcare professionals and researchers about their potential role in a comprehensive approach to brain health.
2. Methods
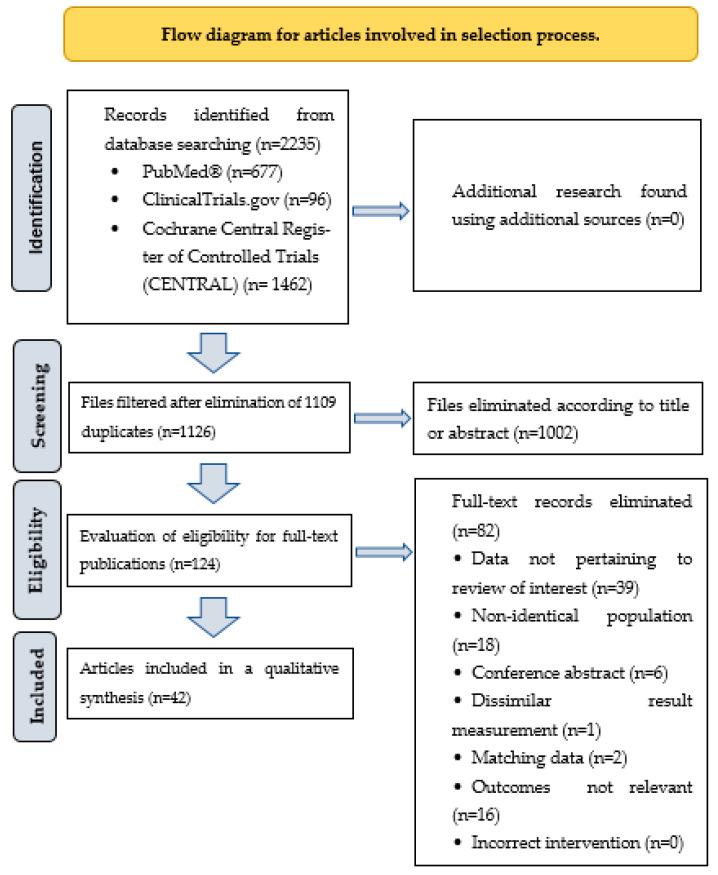
We conducted a literature search on dietary supplement interventions in the Cochrane Central Register of Controlled Trials (CENTRAL) databases, PubMed, and ClinicalTrials.gov from 31 October 2018 to 31 October 2023. We focused exclusively on randomized controlled trials (RCTs) and human clinical trials, seeking correlations with cognitive function. The search used specific and MESH keywords, including vitamins: “Vitamin A”, “Vitamin B 6”, “Vitamin B 9”, “Vitamin B 12”, “Vitamin C”, “Vitamin D”, “vitamin E”, “minerals”, “antioxidants”, “flavonoids”, “carotenoids”, “omega 3 fatty acids”, “cognition”, “memory”, “executive function”, “dementia”, “Alzheimer disease”, “cognition disorders”, “randomized controlled trial”, “controlled clinical trial”, without language restrictions. Between the words of the search words listed, we used the conjunctions “AND” or “OR”. Indexed duplicate articles were removed, then titles and abstracts were screened; those that did not meet inclusion criteria were excluded. The articles finally selected were carefully evaluated on the basis of their full text. This review does not cover the application of complex diets, such as the Dietary Approach to Stop Hypertension (DASH diet), high-protein diet, ketogenic diet, low-fat diet, the Mediterranean diet, low glycaemic index (GI) Diet, Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND), nor does it include animal experiments or in vitro research. The role of probiotics, prebiotics, and symbiotics in preserving and enhancing healthy cognitive functions has been demonstrated; however, this summary does not encompass that area due to the limitations of the article’s length. The aim of this review was to provide an up-to-date overview of recent findings on the relationship between the use of different dietary supplements (e.g., vitamins, minerals, antioxidants, essential fatty acids) and cognitive function, according to the PICO (Population, Intervention, Comparison, and Outcomes) criteria. The inclusion and exclusion criteria for the studies included in this review are given in Table 1. Figure 1 shows the flowchart of the articles involved in the selection process. In total, 42 articles and 11,913 patients were included in this review.
Table 1.
Inclusion and exclusion criteria for studies included in the current review.
| Inclusion Criteria | Description |
|---|---|
| Study design | Randomized controlled trial or human clinical trial. |
| Study population | Healthy people or patients admitted with a diagnosis of mild cognitive impairment or Alzheimer’s disease. |
| Intervention | Vitamins, antioxidants, minerals and micronutrients interventions. |
| Language of publication | No language restrictions applied. |
| Published articles | In the PubMed, ClinicalTrials.gov and Cochrane Central Register of Controlled Trials (CENTRAL) databases. |
| Output concepts | Different cognitive functions and their measurement tools, such as validated questionnaires: Full-Scale Intelligence Quotient (FSIQ), Wechsler Adult Intelligence Scale (WAIS), Mini Mental State Examination (MMSE), Stroop Color and Word Test (STROOP), Addenbrooke’s Cognitive Examination-Revised (ACE-R), Verbal Fluency Test. Cognitive index score and different cognitive function tests: attention, calculation, memory, verbal fluency, psychomotor speed, visual-constructional ability, neuropsychological function, reaction time, psychocognitive tests, etc. |
| Exclusion Criteria | |
| Animal experiments. | |
| In vitro studies. | |
| Macronutrients interventions, proteins, carbohydrates, fats, foods, medicines, pharmaceuticals, herbs, essential oils, melatonin and complex diets, such as Dietary Approach to Stop Hypertension (DASH diet), high-protein diet, ketogenic diet, low-fat diet, mediterranean diet, low glycaemic index (GI) diet, Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND). | |
| Interventions for various diseases, such as: tumour diseases, epilepsy, post-traumatic stress disorder, anxiety, depression, stroke, multiple sclerosis, chronic cerebral ischaemia, polycystic kidney disease, opioid patients, psychosis, delirium, schizophrenia, bipolar disorder, frontal lobe atrophy, COVID-19 patients, sepsis, autism, attention deficit hyperactivity disorder (ADHD), Wernicke-Korsakoff syndrome, Fragile X syndrome, and Down syndrome. | |
| Interventions for different ages and conditions, such as: infancy, adolescence, pregnancy and interventions for athletes. | |
| Dietary advice, food and nutrition interventions. | |
| Short-term interventions (<4 weeks). | |
| Intravenous or intramuscular interventions. | |
| Dietary supplement interventions for underweight patients (body mass index (BMI): <18.5 kg/m2). | |
Figure 1.
Flow diagram for articles involved in selection process.
3. Results
3.1. Vitamin A Supplementation
During the study period, no databases included randomized clinical controlled trials solely focusing on Vitamin A supplementation. However, its combined use with other supplements is discussed later in this article.
3.2. Vitamin B Supplementation and Cognitive Function
With regard to B vitamins, previous research has elucidated the beneficial role of folic acid, B12, and B6 vitamins in preserving cognitive functions. In the present study, we observed that when vitamin B supplementation was administered independently to patients [73,74] and when it was administered concomitantly with magnesium, vitamin D, vitamin C [75], and docosahexaenoic acid (DHA) [76], resulted in significant enhancements and substantial benefits in terms of memory and cognitive augmentation among healthy adults (p < 0.001), particularly when magnesium and antioxidant vitamins were included [75]. The combined supplementation with folic acid and vitamin B12 resulted in statistically significant improvements in cognitive scores, as reported by Ma F et al. [77]. In a study [76], folic acid + DHA supplementation significantly increased measured cognitive scores in comparison to the placebo group. The study by Ma F et al. [74] revealed that a 24-month regimen of folic acid supplementation (400 µg/day) significantly improved cognitive function and reduced blood biomarker levels of amyloid β protein (Aβ) in mild cognitive impairment (p < 0.05). In a study [78], the daily oral administration of folic acid (FA), DHA, and their concomitant administration for six months resulted in a significant enhancement in the Full Scale Intelligence Quotient (FSIQ) and specific subtests of the Wechsler Adult Intelligence Scale in comparison to the placebo group (p < 0.05). A summary of clinical investigations on the correlation between vitamin B supplementation and cognitive functions is presented in Table 2.
Table 2.
Association between vitamin B supplementation and cognitive function.
| Study | Design | Mean Follow-Up | Country | Sample Size | Average Age (Year) | Sex Male/Female (%) |
Intervention | Main Results |
|---|---|---|---|---|---|---|---|---|
| Zhang C et al. [75] | RCT | 30 days | China | 102 | 41.0 ± 9.1 | 47/53 | Magtein: 400 mg® Vitamin D3: 80 IU Vitamin C: 12 mg Vitamin B6: 4 mg; Phosphatidylserine 50 mg. Total: 2 g/person/day. |
Magtein®PS: Significant improvement in memory and cognition in healthy chinese adults (p < 0.001). |
| Ma F et al. [77] | RCT | 6 months | China | 240 | 70.5 ± 9.1 | 35/65 | Four treatment groups: 800 µg FA only, 25 µg vitamin B12 only, FA, and vitamin B12 supplementation or control group. | Supplementation with FA and Vitamin B12: Significant Improvements in FSIQ (d = 0.169, p = 0.024), verbal IQ (d = 0.146, p = 0.033), Information (d = 0.172, p = 0.019), and Digit Span Scores. |
| Gibson GE et al. [73] | RCT | 12 months | USA | 70 | 75.7 ± 7.0 | 41.4/58.6 | Benfotiamine treatment (300 mg/day twice a day) versus placebo group. | Benfotiamine Group vs. Placebo Group: 43% lower increase in ADAS-Cog Scores and 77% less worsening in CDR (p = 0.034) in Benfotiamine Group. |
| Kwok T et al. [79] | RCT | 24 months | Hong Kong | 279 | 78.0 ± 5.3 | 56.1/43.9 | MCI patients administered 500 μg methylcobalamin and 400 μg FA orally once daily. | Supplementation with Vitamin B12 and FA: No reduction in cognitive decline in older individuals with MCI and elevated serum homocysteine. |
| Bai D et al. [76] | RCT | 6 months | China | 138 | 68.3 ± 6.3 | 40/60 | FA (60.0 mg/day) + DHA (8 mg/day), FA (800.0 mg/day), DHA (8 mg/day) versus placebo. | FA, DHA, and FA + DHA vs. placebo: improvements in FSIQ, arithmetic, and picture complement scores with folic acid; FSIQ, information, arithmetic, and digit span scores with DHA; greater enhancements in arithmetic (1.67, 95% CI 1.02 to 2.31) and digit span (1.33, 95% CI 0.24 to 2.43) scores with FA + DHA. |
| Ma F et al. [74] | RCT | 24 months | China | 180 | 74.8 ± 2.8 | 42.7/57.3 | FA 400 µg/day. | FA supplementation linked to improved cognitive function and reduced blood levels of Aβ-related biomarkers in MCI (p < 0.05). |
| Li M et al. [78] | RCT | 6 months | China | 240 | 70.4 ± 6.7 | 42.5/57.5 | Intervention groups: FA + DHA (FA 800 μg/d + DHA 800 mg/d), FA (FA 800 μg/d), DHA (DHA 800 mg/d), and placebo. | Daily oral FA, DHA, and combined use for 6 months: significant improvements in FSIQ and select WAIS subtests compared to placebo (p < 0.05). |
ADAS-Cog: Alzheimer’s Disease Assessment Scale-Cognitive Subscale; CDR: clinical dementia rating; DHA: docosahexaenoic acid; FA: folic acid; FSIQ: full-scale intelligence quotient; IQ: intelligence quotient; IU: international unit; Magtein: Magnesium L-threonate; Magtein®PS: magnesium L-threonate (Magtein) and phosphatidylserine-based formula; MCI: mild cognitive impairment; RCT: randomized controlled trial; WAIS: Wechsler Adult Intelligence Scale.
3.3. Results on Antioxidants and Cognitive Function
Prominent antioxidants include specific vitamins, namely vitamins A, C, and E, minerals such as selenium, chromium, and zinc, as well as carotenoids, flavonoids, polyphenols, and lignans. These components protect against free radicals and help maintain healthy functioning of cognitive processes, such as memory, cognition, and concentration. In our current summary research, in a study by Thaung Zaw JJ et al. [80], a daily supplementation of 75 mg resveratrol resulted in a significant improvement in overall cognitive performance among middle-aged women. Foroumandi E et al. [81] demonstrated promising positive effects on memory, quality of life, and levels of selective oxidative indices in patients with mild to moderate Alzheimer’s disease (AD) who received 5 cc of fenugreek seed extract (equivalent to 500 mg of dry extract) (p < 0.001) for 4 months. The supplementation of 1000 mg/day of vitamin C [82], carotenoids: lutein and zeaxanthin (13 mg, or 27 mg/day) supplementation [83], as well as 1.6 g/day of alpha-lipoic acid [84] resulted in significant improvement compared to the control group in terms of attention, memory, and other observed cognitive tests (p < 0.05 for all). Additionally, administering 3 g of desert olive tree pearls/day for three months significantly improved (p < 0.05) psychomotor speed, reaction time, cognitive flexibility, processing speed, and executive function domains [85]. However, no significant improvement in cognitive tests was observed in healthy individuals supplemented with cocoa extract (containing 500 mg/day of flavanols) or Ginkgo biloba (240 mg/day in patients with Alzheimer’s disease) (Table 3).
Table 3.
Association between vitamin C and antioxidant supplementation and cognitive function.
| Study | Design | Mean Follow-Up | Country | Sample Size | Average Age (Year) | Sex Male/Female (%) |
Intervention | Main Results |
|---|---|---|---|---|---|---|---|---|
| Sim M et al. [82] | RCT | 4 weeks | Republic of Korea | 214 | 20–39 | 39.3/60.7 | 500 mg vitamin C twice a day. | Vitamin C supplementation notably increased attention and work absorption (p = 0.03), with a clear tendency towards fatigue improvement. |
| Morató X et al. [86] | RCT | 12 months | Spain | 50/50 | 73.1 ± 7.5 | 40/60 | Standardized extract of Ginkgo biloba EGb 761 240 mg tablets were given orally. | No significant differences between groups in MMSE, CDR, NBACE scores, or amnestic profile; higher scores in irritability/lability parameter (p = 0.006) and BDS (p = 0.048) in control group. |
| Thaung Zaw JJ et al. [80] | RCT | 24 months | Australia | 125 | 45–85 | 100% female | 75 mg trans-resveratrol or placebo per day. | Resveratrol supplementation led to 33% improvement in overall cognitive performance (Cohen’s d = 0.170, p = 0.005). |
| Lai S et al. [84] | RCT | 6 months | Italy | 59 | 45.1 ± 10.7 | 55.9/44.1 | ALA 1.6 g/day. | BDI-II, HAM-D, MMSE tests showed significant improvement (p = 0.007, p < 0.001, p < 0.001) in patients treated with ALA compared to control group. |
| Foroumandi E et al. [81] | RCT | 4 months | Iran | 82 | 72.0 ± 2.5 | 34.1/65.9 | Intervention group patients received 500 mg dry extract (5 cc) of fenugreek seed extract. | Positive effects on memory (p < 0.001), quality of life (p < 0.001) and selective oxidative index level. |
| Baker LD et al. [87] | RCT | 3 years | USA | 2262 | 73.0 | 40/60 | Daily administration of cocoa extract (containing 500 mg/day flavanols) versus placebo. | Cocoa extract had no effect on global cognition (mean z-score = 0.03, 95% CI: −0.02–0.08; p = 0.28). |
| Bell L et al. [88] | RCT | 12 weeks | UK | 60 | 18–30 | 10/90 | 400 mg of GSPE extract daily. | 400 mg of GSPE did not consistently improve cognitive function in healthy young adults. |
| Stringham NT et al. [83] | RCT | 6 months | Greece | 59 | 18–25 | 45.7/54.3 | Carotenoids lutein and zeaxanthin, along with the zeaxanthin isomer meso-zeaxanthin (13 mg/day or 27 mg/day total). | For cognitive measures, all scores for composite memory, verbal memory, sustained attention, psychomotor speed, and processing speed improved significantly in treatment groups (p < 0.05 for all) and remained unchanged in the placebo group. |
| Yoon J et al. [85] | RCT | 12 weeks | Japan | 36 + 36 | 69.5 ± 7.6 | 47/53 | Participants received 3 g of DOTP or placebo in olive oil twice daily for 12 weeks. | Among cognitive domains, complex attention had a significant time × group interaction effect (p = 0.049) between the DOTP and placebo groups. Time effects were significant (p < 0.05) for psychomotor speed, reaction time, cognitive flexibility, processing speed, and executive function domains. |
| Hashimoto M et al. [89] | RCT | 12 months | Japan | 44 | 70.2 ± 1.4 | 52.4/47.6 | Randomized participants in the PO group received soft gelatin capsules containing 1.47 mL of PO daily, and those in the PO + POPP group received soft gelatin capsules containing both 1.47 mL of PO and 1.12 g PP daily. | At the end of intervention, the POPP group showed significantly higher cognitive index scores than the PO group, POOP may improve age-related cognitive impairment in healthy elderly people. |
ALA: alpha lipoic acid; BDI-II: Beck Depression Inventory-II; BDS: Blessed Dementia Scale; CDR: clinical dementia rating; DOTP: desert olive tree pearl; GSPE: grape seed polyphenol; HAM-D: Hamilton Depression Rating Scale; MMSE: Mini-Mental State Examination; PO: Perilla frutescens seed oil; POPP: PO + ponkan powder.
3.4. Vitamin D Supplementation and Cognitive Function
Maintaining optimal levels of vitamin D can be effectively achieved through proper nutrition and time spent outdoors during the spring and summer months when sunlight exposure is higher. However, in autumn and spring, when the number of sunshine hours is reduced, it is advisable to supplement with vitamin D. Expert recommendations suggest that healthy adults should consume 1500–2000 IU of vitamin D daily, and even doubling this value to 4000 IU daily possible in some cases. In our review, we have observed that vitamin D is of utmost importance for mood and cognitive functions. Vitamin D supplementation may play a role in preventing dementia and enhancing cognitive function, although a study [90] involving 600 IU of vitamin D3 per day showed no significant effects on cognitive functions or mood. Similarly, Jorde R et al. [91] and Bischoff-Ferrari HA et al. [92] observed no substantial improvement in cognitive function with vitamin D supplementation.
Contrary to these studies, Jia J et al. [93], Yang T et al. [94], Castle M et al. [95], Ghaderi A et al. [96] and Hu J et al. [97] reported significant enhancements in cognitive performance as a result of vitamin D supplementation. A study [98] did not support a significant cognitive benefit from 2000 IU per day compared to 800 IU per day among healthy older adults. Meanwhile, Castle M et al. [95] described differential effects of vitamin D3 supplementation (600, 2000, or 4000 IU per day) on cognitive measurements across various functional domains (Table 4).
Table 4.
Association between vitamin D supplementation and cognitive function.
| Study | Design | Mean Follow-Up | Country | Sample Size | Average Age (Year) | Sex Male/Female (%) |
Intervention | Main Results |
|---|---|---|---|---|---|---|---|---|
| Jia J et al. [93] | RCT | 12 months | China | 210 | 68.0 ± 5.9 | 45/55 | Patients received 800 IU/day of vitamin D. | The FSIQ and cognitive test score were significantly higher in the intervention group than in the control group (p < 0.001). |
| Bischoff-Ferrari HA et al. [92] | RCT | 3 years | Switzerland | 2157 | 74.9 | 38.3/61.7 | 2000 IU/day of vitamin D3, 1 g/day of omega-3 strength-training exercise program. | Among adults aged 70 years or older, treatment with vitamin D3, omega-3, or a strength-training exercise program did not result in statistically significant differences in improving cognitive function. |
| Zajac IT et al. [90] | RCT | 6 months | Australia | 436 | 60–90 | 48.4/51.6 | 600 IU/day of vitamin D3 | No effect. |
| Yang T et al. [94] | RCT | 12 months | China | 183 | 67.2 ± 6.1 | 46/54 | 800 IU/day of vitamin D3 | The ANOVA showed improvements in the FSIQ, information, digit span, vocabulary, block design, and picture arrangement scores in the vitamin D group over the placebo group (p < 0.001). |
| Byrn MA et al. [99] | RCT | 12 weeks | USA | 206 | 55.71 | 17/83 | Administration of either weekly vitamin D3 supplementation (50,000 IU) or 5000 IU cholecalciferol once a week. | No significant differences in cognitive outcomes between participants who received high-dose therapy and those who received low dose. |
| Castle M et al. [95] | RCT | 1 year | USA | 138 | 58 ± 6 | 100% female | Vitamin D3 supplementation (600, 2000, or 4000 IU/day). | The CANTAB test results indicated that the 2000 IU/d group, when compared to other groups, performed better in PAL test parameters (p < 0.05). RTI was slower in the 4000 IU/d compared to 600 IU/d group for the 5-choice test (p < 0.01). |
| Jorde R et al. [91] | RCT | 4 months | Norway | 422 | 52 | 52.9/47.1 | Vitamin D 100,000 IU administered as a bolus dose followed by 20,000 IU per week versus placebo. | Vitamin D supplementation did not improve cognitive function during a four-month intervention. |
| Ghaderi A et al. [96] | RCT | 24 weeks | Iran | 64 | 59.2 ± 11.3 | 53/47 | Administration of either 50,000 IU vitamin D supplements (n = 32) or placebo (n = 32) every 2 weeks. | Subjects who were administered vitamin D had a significant reduction in IGT (β −6.25; 95% CI, −8.60 to −3.90; p < 0.001), and significant increases in VFT (β 2.82; 95% CI, 0.78–4.86; p = 0.007), immediate LM (β 1. 32; 95% CI, 0.27–2.37; p = 0.01), reverse DGS (β 2.06; 95% CI, 1.18–2.94; p < 0.001) and VWM (β 0.75; 95% CI, 0.33–1.16; p = 0.001). |
| Schietzel S et al. [98] | RCT | 2 years | Switzerland | 273 | 70.3 | 46.5/53.5 | 2000 or 800 IU vitamin D3/day | No effect. |
| Beauchet O et al. [100] | RCT | 3 months | Canada | 40 | ≥65 | 100% female | Fortified yogurt (400 IU vitamin D and 800 mg calcium). | Fortified yogurts with vitamin D and calcium maintained global cognitive performance (MMSE score (p = 0.022). Global cognitive performance decreased in the control group. |
| Owusu JE et al. [101] | RCT | 3 years | USA | 260 | 68.2 ± 4.9 | 100% female | Adminsitration of vitamin D (adjusted to achieve a serum level > 30 ng/mL) with calcium (diet and supplement total of 1.200 mg) | There is no evidence that vitamin D intakes above the recommended daily allowance are needed to prevent cognitive decline in this population. |
| Hu J et al. [97] | RCT | 12 months | China | 181 | 67.22 ± 6.1 | 44.5/55.5 | Administration of 800 IU/day of vitamin D. | The mean scores of information, DGS, vocabulary, block design and picture arrangement tests in the vitamin D3 group were significantly higher than that in the placebo group both before and after adjustment. In addition, the performance of FIQ (p < 0.001, d = 0.70), VIQ (p < 0.001, d = 0.77) and PIQ (p < 0.001, d = 0.70) was consistent with the five subtests mentioned above. |
| Macpherson H et al. [102] | RCT | 6 months | Australia | 147 | 70.2 ± 6.1 | 30/70 | Daily vitamin D (1000 IU) and omega-3 (900 mg EPA, 600 mg DHA) and protein (20 g) supplementation. | There were no significant between-group differences in cognition at 6 or 12 months. |
DHA: docosahexaenoic acid; EPA: Eicosapentaenoic acid; FSIQ: full scale intelligence quotient; PAL: Paired Associates Learning; RTI: reaction time; IGT: Iowa Gambling Task; VFT: Verbal Fluency Test; LM: Logic Memory; DGS: Digit Span; VWM: visual working memory; FIQ: full IQ; VIQ: verbal IQ; PIQ: performance IQ.
3.5. Omega-3 Dietary Supplements and Cognitive Function
Consistent use of omega-3 dietary supplements may be correlated with enhancements in cognitive ability and reduced susceptibility to cognitive deterioration. In addition to their pivotal role in immune function, omega-3 polyunsaturated fatty acids have the potential to improve memory and reduce the risk of chronic degenerative diseases such as Alzheimer’s disease and attention disorders. Empirical studies have revealed that omega-3 fatty acids may help improve memory and cognitive functions in various forms of dementia and reduce the risk of these conditions. It has also been documented that omega-3 fatty acids help maintain brain health and cognitive function in healthy adults. In our study, we found that patients who received 1 g of fish oil per day, either alone or in combination with vitamin E and carotenoids, experienced memory and mood improvement, a significant reduction in the number of errors in memory tasks, and enhancements in attention and executive functions [103,104,105,106]. Rasmussen J et al. [107] have given patients in the early stages of Alzheimer’s disease a safe and well-tolerated combination of docosahexaenoic acid, eicosapentaenoic acid, uridine monophosphate, choline, phospholipids, selenium, folic acid, and vitamins B12 and E, and have reported clinically significant benefits in various cognitive functions (e.g., attention, memory, executive function, p < 0.05). Nevertheless, we have encountered studies in which fish oil supplementation did not influence cognitive performance, memory, or mood, and the final analysis did not yield any evidence of its impact on cognitive function measurement [108,109,110,111,112] (Table 5).
Table 5.
Association between omega-3 PUFA supplementation and cognitive function.
| Study | Design | Mean Follow-Up | Country | Sample Size | Average Age (Year) | Sex Male/Female (%) |
Intervention | Main Results |
|---|---|---|---|---|---|---|---|---|
| Lin PY et al. [108] | RCT | 24 months | Taiwan | 163 | 77.8 ± 8.4 | 66.2/33.8 | 163 patients were randomly assigned to DHA (0.7 g/day), EPA (1.6 g/day), or EPA (0.8 g/day) + DHA (0.35 g/day) group for 24 months. | A statistically significant difference in cognitive, functional, and mood status scores, biochemical profiles, and inflammatory cytokines levels was not determined between the placebo and treatment groups. |
| Nolan JM et al. [103] | RCT | 12 months | Ireland | 50 + 27 | ≥65 | 53/47 | Patients consumed 1 g fish oil (of which 500 mg DHA, 150 mg EPA), 22 mg carotenoids (10 mg lutein, 10 mg meso-zeaxanthin, 2 mg zeaxanthin), and 15 mg vitamin E daily. | The active group performed better in objective measures of AD severity (i.e., memory and mood), with a statistically significant difference in the clinical collateral for memory (p < 0.001). |
| Giudici KV et al. [109] | RCT | 3 years | France | 1445 | 75.3 ± 4.4 | 35.8/64.2 | ω-3 (800 mg DHA and 225 mg EPA/day) | No effect. |
| Arellanes IC et al. [113] | RCT | 6 months | USA | 33 | 68 (58–90) | 18.2/81.8 | 33 individuals were provided with a vitamin B complex (1 mg of vitamin B12, 100 mg of vitamin B6 and 800 mcg of folic acid per day) and randomized to 2152 mg of DHA per day or placebo over 6 months. | No effect. |
| Rasmussen J. [107] | RCT | 24 months | Finland, Germany, Netherlands, Sweden | 311 | >65 | 45/55 | Patients were given a combination of DHA, EPA, uridine monophosphate, choline, phospholipids, selenium, folic acid, and vitamins B12 and E (>200% the recommended daily intake). | This intervention had the potential to improve the progression of Alzheimer’s disease (attention, memory, executive function p < 0.05). |
| Stavrinou PS et al. [104] | RCT | 6 months | Cyprus | 36 | 78.8 ± 7.3 | 38.8/61.2 | 20 mL dose of a formula containing a mixture of omega-3 (810 mg EPA and 4140 mg DHA) and omega-6 FA (1800 mg gamma-LA and 3150 mg LA) (1:1 w/w), with 0.6 mg of vitamin A, vitamin E (22 mg) plus pure γ-tocopherol (760 mg). | A significant interaction between supplementation and time was found on cognitive function (MMSE, ACE-R, STROOP) functional capacity (6 min walk test; p = 0.028) fatigue (p < 0.001), physical health (p = 0.007), and daily sleepiness (p = 0.007). |
| Mengelberg A et al. [110] | RCT | 12 months | New Zealand | 30 + 30 | 72.3 ± 6.1 | 69.8/30.2 | 1491 mg of DHA + 351 mg of EPA per day. | No effect. |
| Atmadja T et al. [105] | RCT | 90 days | Indonesia | 29 | 66.1 ± 5.3 | 20.6/79.4 | Subjects were divided into three groups: SO, CFO, and CO with omega-3 (catfish oil enriched with omega-3). The intervention involved 1000 mg of oil/day. | Significant effects on oxidative stress and cognitive function (p < 0.05), and significantly increased MMSE score (p < 0.05). |
| Leckie RL et al. [111] | RCT | 18 weeks | USA | 271 | 30–54 | 43.5/56.5 | Fish oil capsules (1400 mg/day of EPA and DHA). | No effect. |
| Kuszewski JC et al. [114] | RCT | 16 weeks | Australia | 64 | 65.8 ± 1.4 | 44/56 | Randomly assigned to either fish oil (2000 mg/d of DHA + 400 mg/d of EPA), curcumin (160 mg/d), or a combination. | Fish oil improved CVR to a processing speed test (4.4% ± 1.9% vs. −2.2% ± 2.1%; p = 0.023) and processing speed in males only (Z-score: 0.6 ± 0.2 vs. 0.1 ± 0.2; p = 0.043). |
| Patan MJ et al. [106] | RCT | 26 h | UK | 310 | 25–49 | 35/65 | Participants consumed either 900 mg of DHA/d and 270 mg of EPA/d (DHA-rich oil), 360 mg of DHA/d and 900 mg of EPA/d (EPA-rich oil), or 3000 mg/d of refined olive oil (placebo). | EPA supplementation improved global cognitive function, superior to oil enriched with DHA; improved memory accuracy compared with DHA (p = 0.034) |
| Sueyasu T et al. [112] | RCT | 24 weeks | Japan | 71 | 65.7 ± 1.0 | 45.1/54.9 | PUFA in Combination with LZ (containing 120 mg ARA, 300 mg DHA, and 100 mg EPA per day) combined with LZ (containing 10 mg lutein and 2 mg zeaxanthin per day). | LCPUFAs + LZ supplementation did not significantly affect memory function. |
ACE-R: Addenbrooke’s Cognitive Examination–Revised; CFO: commercial fish oil; CO: catfish oil; CVR: cerebrovascular responsiveness; DHA: docosahexaenoic acid; DHA: docosahexaenoic acid; EPA: Eicosapentaenoic acid; FA: fatty acid; LA: linolenic acid; LCPUFAs + LZ: Long-Chain Polyunsaturated Fatty Acids in Combination with Lutein and Zeaxanthin; MMSE: Mini-Mental State Examination; PUFA: Polyunsaturated Fatty Acid; SO: soybean oil; STROOP: Stroop Color and Word Test.
4. Discussion
In our current comprehensive research overview, we highlight the indisputable significance of various vitamins, minerals, antioxidants, and essential fatty acids in enhancing cognitive function. These essential nutrients play a pivotal role in sustaining the proper functioning of the central nervous system. As individuals age, nutrient deficiencies become more common, stemming from inadequate diet, reduced nutrient absorption, or medication-related side effects. Supplementation of these elements is, therefore, essential not only for the proper functioning of the immune system but also for the preservation of cognitive abilities, memory, and cognitive acumen. B vitamins are well documented to have profound effects on cognitive function, memory retention, and concentration. Deficiencies can lead to memory impairment and concentration deficits, and supplementation can improve cognitive abilities. Free radicals that impact neurons can cause damage or even complete loss, thereby contributing to the development of neurodegenerative diseases. Our comprehensive review underscores the critical importance of nutritional supplements, including various vitamins, minerals, antioxidants, and essential fatty acids in preserving/enhancing cognitive function in older adults. These supplements are pivotal in maintaining the central nervous system’s proper functioning, especially as nutrient deficiencies become more prevalent with age due to factors like inadequate diets, reduced nutrient absorption, or medication side effects. Supplementing these elements is crucial for preserving cognitive abilities, including memory and executive function.
4.1. Vitamin B
B vitamins play a crucial role in maintaining cognitive function during aging, acting as essential cofactors in various neurological processes [115]. As individuals age, the risk of B vitamin deficiencies increases, potentially leading to cognitive decline [116]. Vitamins B6, B9 (folate), and B12 are particularly important, as they contribute to the maintenance of normal brain function by influencing homocysteine metabolism, an amino acid linked to neurodegenerative diseases and cardiovascular and cerebrovascular impairment when present at elevated levels [117,118]. Studies [119,120,121] have demonstrated that a high intake of these B vitamins can significantly slow cognitive decline in older adults, particularly in those with elevated homocysteine levels or mild cognitive impairment [116,122]. For instance, supplementation with B vitamins has been shown to lower homocysteine levels, thereby reducing the rate of brain atrophy and improving cognitive outcomes [123]. Additionally, B vitamins are involved in the synthesis of neurotransmitters and the maintenance of myelin, the protective sheath around nerve fibers, which is crucial for efficient brain signaling [123]. This protective effect of B vitamins against cognitive decline is especially beneficial for older adults who are at an increased risk of dementia, suggesting that adequate intake of these nutrients could play a key role in preserving cognitive health in the aging population [115,116,119,120,122].
4.2. Vitamin C, Vitamin E and Other Antioxidants
Supplementation with vitamin C, vitamin E, and other antioxidants plays a potential important role in preserving cognitive function during aging, primarily through their ability to combat oxidative stress [124], a key factor in cellular aging [125] and the development of cardiovascular [126] and cerebrovascular impairment [127], neurodegeneration [128] and age-related cognitive decline [129].
Vitamin C is a potent antioxidant that can help protect the brain from oxidative stress, which can impair cognitive functions [130]. In addition, vitamin C plays a pivotal role in the synthesis and functioning of the neurotransmitters dopamine and noradrenaline found in the brain [130]. Several studies have explored the associations between vitamin C and physical and mental well-being; its deficiencies may increase the risk of severe conditions such as cancer, heart disease, and diabetes [131,132,133]. Research has also found links between vitamin C deficiency and attention, concentration, executive function, memory, linguistic and conceptual thinking [134,135,136]. Low levels of vitamin C can negatively affect mood, potentially leading to depression and cognitive impairment [137], in other words, higher levels of vitamin C are correlated with improved mood and reduced depression and confusion [134]. A meta-analysis has described how vitamin C supplementation can enhance the mood in individuals with depression [138]. Consequently, this can improve cognitive performance and reduce the “brain fog” associated with depression [138]. Further research and long-term follow-up studies involving more patients are needed to establish the preventive effect of vitamin C against the development and progression of Alzheimer’s disease [139]. In conclusion, there existing evidence suggests that maintaining healthy levels of vitamin C may be protective against age-related cognitive decline and neurodegenerative diseases, and that cognitive function improves with vitamin C supplementation [139,140].
Vitamin E is a potent fat-soluble antioxidant. It interacts and synergizes with several other antioxidants, such as glutathione, selenium, vitamin C, carotenes, and carotenoids [141]. Vitamin E protects brain cells from oxidative stress-induced damage [142] and is particularly effective in maintaining neuronal integrity and function. It is known for its protective effects against lipid peroxidation in cell membranes, which is vital for preserving cognitive health. Studies have shown that individuals with a higher intake or serum levels of these antioxidants have a lower risk of cognitive decline and dementia, including Alzheimer’s disease [141,142,143]. The existing evidence supports the inclusion of vitamin E supplementation in a dietary protocol aimed at preserving cognitive health in the elderly.
Polyphenols, including resveratrol and curcumin, represent a diverse group of compounds with potent antioxidant and anti-inflammatory properties, playing a significant role in the preservation of cognitive function in aging. Resveratrol, found in grapes and red wine, has gained attention for its potential neuroprotective effects. It is believed to activate pathways that help in protecting cells from damage and improve blood flow to the brain, thereby potentially enhancing cognitive functions and reducing the risk of neurodegenerative diseases [144]. Clinical evidence suggests that resveratrol supplementation can improve memory and cognitive performance in older adults [144,145].
Curcumin, the active component of turmeric, is another widely studied polyphenol known for its strong anti-inflammatory and antioxidant properties. It has been shown to cross the blood–brain barrier and exert neuroprotective effects, potentially helping in the prevention of age-related cognitive decline. Studies indicate that curcumin may improve memory and mood in people with mild, age-related memory loss [146,147].
Other polyphenols, like flavonoids, found in berries, tea, and cocoa, are also crucial for cognitive health [148,149]. Flavonoids have been associated with improved cognitive abilities, reduced risk of dementia, and enhanced memory and learning in older adults [150]. For example, epigallocatechin gallate (EGCG) from green tea has been studied for its role in protecting neurons, reducing the formation of amyloid plaques, and improving cognitive function [151].
Another class of polyphenols, anthocyanins, found in dark-colored fruits like blueberries, have been shown to improve neural signaling and enhance memory [152]. Regular consumption or supplementation with these polyphenols can provide antioxidative and anti-inflammatory benefits, which are particularly beneficial in countering age-related cognitive decline [145]. However, while the biological effects of these compounds are well-documented, more large-scale, long-term clinical trials are needed to conclusively establish their efficacy in preventing or slowing down cognitive impairment in older adults.
4.3. Vitamin D
Vitamin D, essential for overall health, plays a multifaceted role ranging from maintaining bone health to supporting immune system functions [153,154]. It aids in the absorption of calcium and phosphorus, crucial for optimal bone density, and is involved in normal muscle function and blood sugar metabolism [155,156]. Its significance extends to the development of the brain and nervous system in early childhood and is crucial for cognitive functions such as memory, thinking, and concentration in later life [157]. Vitamin D is also instrumental in producing neurotransmitters like dopamine and serotonin, which regulate mood and emotions [157].
Approximately 40% of the European population is affected by vitamin D deficiency, which can worsen during the late winter months [158]. Consequently, the recommended daily intake for adults has been increased to 2000 IU/day [158,159]. The elderly, along with individuals with chronic diseases, specific dietary preferences, or certain health conditions, are particularly vulnerable to this deficiency [160,161]. Notably, vitamin D deficiency is linked to an increased risk of diseases like type 2 diabetes, cancer, multiple sclerosis, depression, Parkinson’s, and Alzheimer’s disease [162,163]. A study [164] involving over 1600 elderly individuals revealed that those with mild vitamin D deficiency were over 50% more likely to develop dementia, and the risk was even higher in those with severely low levels. These findings underscore the importance of maintaining adequate vitamin D levels for cognitive health.
Clinical evidence supports the role of vitamin D supplementation in preserving cognitive function, especially in older adults [165,166,167]. Research has shown that adequate levels of vitamin D are associated with improved cognitive performance, and supplementation has been found to benefit those with deficiencies [165,166,167]. This is particularly crucial for cerebrovascular health, as vitamin D supports blood flow to the brain and reduces the risk of cerebrovascular diseases, which can impact cognitive abilities [162,163]. Its role in neuroprotection, neurotransmission, and brain plasticity highlights its potential as a key nutrient in maintaining brain health during aging [168,169]. Therefore, vitamin D supplementation could be a strategic approach in mitigating the risk of age-related cognitive impairment and supporting overall brain health in the elderly population. The exact mechanisms are thought to involve vitamin D’s role in neuroprotection, neurotransmission, and brain plasticity, highlighting its potential as a crucial nutrient in maintaining brain health with aging. However, while these associations are promising, further large-scale, long-term studies are needed to establish definitive causal links between vitamin D supplementation and cognitive function preservation in older adults [168,169].
4.4. Vitamin K
In the human body, vitamin K is an essential component for physiological processes and is also a fat-soluble vitamin [170]. It is naturally expressed in two forms, namely K1 (phylloquinone) and K2 (menaquinone), both of which play pivotal roles in a wide spectrum of physiological processes [170]. Its principal function is to modulate hemostasis through the synthesis of coagulation factors. In addition to these primary roles, vitamin K is also required for various functions in cell growth, proliferation, cell genesis, and apoptosis [170,171,172]. Maintenance of normal vitamin K levels may also contribute to the preservation of memory in the elderly [172]. There are studies suggesting a link between reduced serum concentrations of vitamin K and deterioration of cognitive function in the geriatric population (aged 65 years and above) [172,173,174]. Preclinical studies raise the possibility that vitamin K2 may protect nerve cells against the toxicity of amyloid β [175].
4.5. Omega-3 Polyunsaturated Fatty Acids
Omega-3 polyunsaturated fatty acids (PUFAs) [56,153] are increasingly recognized for their critical role in maintaining cognitive function during aging, with ongoing research continuously examining their positive effects on central nervous system functions, including memory, attention, concentration, learning capabilities, and overall well-being [52,65,176,177,178,179]. These fatty acids, particularly eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), are crucial components of cell membranes in the brain and are involved in various neurophysiological processes [52,64,176,178,180,181,182,183]. DHA, the most abundant omega-3 fatty acid in the brain, is vital for the maintenance and function of neural cells [65,177,178,179]. It is known for its role in enhancing synaptic plasticity and neuronal signaling, which are key factors in cognitive processes like learning and memory [181]. EPA, on the other hand, contributes to cognitive health primarily through its anti-inflammatory properties, which are beneficial in reducing neuroinflammation, a contributing factor to cognitive decline and the development of neurodegenerative diseases [52,64,176,178,180,181,182,183,184,185]. Higher doses of omega-3, typically ranging from 500 to 2000 mg per day, have been suggested to alleviate symptoms of depression and anxiety, further supporting cognitive health [186]. The Western diet, unfortunately, tends to contain more omega-6 fatty acids compared to omega-3, which can be detrimental to health [187]. The optimal ratio of omega-6 to omega-3 is closer to 2:1, and since the body cannot produce these fatty acids, they must be obtained through diet or supplements, with effective doses for various health conditions ranging from 250 to 4000 mg of omega-3 per day [187,188]. Sources of omega-3 include fatty fish like salmon, mackerel, tuna, and plant sources such as flaxseed, chia seeds, nuts, and canola oil [52,64].
Regular consumption of omega-3 supplements is beneficial for cognitive and emotional development, reading skills, and cognitive and concentration abilities [52,65,176,177,178,179]. Furthermore, omega-3 PUFAs have shown potential in reducing the risk of neurodegenerative diseases like Alzheimer’s disease [189], potentially slowing the progression of the disease, delaying its onset, and being associated with improved cognitive abilities. Clinical studies have also demonstrated that regular intake of omega-3 fatty acids can alleviate symptoms of mental health disorders such as depression [176,190,191]. DHA is also essential for the retina, with deficiency leading to vision problems and increased risk of eye diseases [192]. Additionally, omega-3 fatty acids positively affect bones, muscles, and joints, enhancing bone strength and reducing the risk of osteoporosis [193,194]. Therefore, consistent use of omega-3 supplements has been associated with multifaceted health benefits, including improved cognitive ability and reduced susceptibility to cognitive decline [52,64,176,178,180,181,182,183].
4.6. Mineral Supplementation
Mineral supplementation plays a critical role in supporting brain and cognitive health, particularly in the aging population [195,196]. Minerals, being inorganic substances essential for the body’s physiological functions, cannot be synthesized endogenously and must be obtained through diet or supplementation. Their impact on cognitive abilities is increasingly recognized [195,196].
Magnesium supplementation, for instance, is associated with enhanced cognitive functions and a reduced risk of dementia [197]. Studies [197,198] have demonstrated that individuals with higher magnesium levels have a notably lower risk of dementia. Increased magnesium intake is particularly beneficial for brain health and may help in preserving intellectual function and reducing the risk of dementia, as it protects nerve cells and positively influences blood pressure.
Iron is vital for numerous physiological processes, including cognitive function and cellular metabolism [199,200,201,202,203,204]. Even mild forms of iron deficiency can impair concentration and reduce immunity, and are linked with delayed neurological development and poorer academic performance. Iron supplementation has been shown to positively affect intelligence quotient (IQ) scores and iron-deficiency anemia in the elderly is associated with an increased prevalence of dementia and Alzheimer’s disease [199,200,201,202,203,204].
Selenium is a crucial component of antioxidant enzymes like glutathione peroxidase [205]. These enzymes protect the brain from oxidative stress, which is implicated in aging and neurodegenerative diseases like Alzheimer’s and Parkinson’s [205]. Oxidative stress damages brain cells and impairs cognitive function, so selenium’s role in combating this stress is vital for maintaining cognitive health [129,206,207,208,209,210]. Selenium, contributing to antioxidant defenses, can reduce the risk of diseases by boosting immune function. It has been found that higher levels of selenium in the blood are associated with a reduced risk of cognitive decline and certain types of cancer [211,212]. Selenium is also crucial for the proper functioning of the thyroid gland and plays a vital role in immune health.
Zinc, essential for growth, development, and immune system function [213], is beneficial for the nervous system and may help prevent depression due to its tranquilizing properties. However, zinc deficiency can lead to a decline in cognitive functions and memory [214,215]. Zinc is also vital for the functionality of the antioxidant enzyme superoxide dismutase, which helps eliminate free radicals [216,217,218].
Copper, involved in energy production, connective tissue formation, and the integrity of the cardiovascular and immune systems, requires a balanced intake with zinc [219]. Copper is found in diverse food sources and is also available as a dietary supplement. While copper performs many vital biological functions, the relationship between its intake and the development of diseases like Alzheimer’s disease remains complex, with research suggesting that both excess and deficiency may have adverse consequences [220,221].
In summary, minerals such as magnesium, iron, selenium, zinc, and copper are integral to maintaining cognitive health, particularly in the aging population. Their supplementation can support various brain functions, from cognitive performance to reducing the risk of neurodegenerative diseases. This highlights the importance of ensuring adequate mineral intake, either through diet or supplementation, as part of a strategy to preserve cognitive function and overall brain health in older adults.
5. Practical Considerations
When considering supplementation with vitamins, minerals, antioxidants, and other dietary supplements for cognitive health, it’s crucial to take into account several individual factors. These include age, sex, nutritional status, lifestyle, stress levels, physical activity, season, dietary habits, and specific diets [222,223,224]. Customizing supplementation for each individual is essential for maximizing cognitive health benefits. As we age, our body’s ability to absorb nutrients decreases, and our nutritional needs change [225,226]. Older adults may need higher doses of certain vitamins like B12, vitamin D, and calcium. However, excessive intake of certain supplements can be harmful, so it is important to adjust dosages appropriately [156]. Men and women have different nutritional requirements [64]. For instance, women may need more iron due to menstruation, while men may require more zinc. Post-menopausal women often need increased calcium and vitamin D to maintain bone health. Nutritional status should be assessed to determine any existing deficiencies. For example, a person with low vitamin D levels might need a higher supplementation dose compared to someone with adequate levels. Factors like smoking or alcohol consumption can affect the body’s nutrient levels. Smokers may need more vitamin C, while heavy drinkers might require additional B vitamins. High stress can deplete certain nutrients faster, such as B vitamins and vitamin C. Individuals under significant stress might benefit from higher doses of these. Active individuals have higher metabolic rates and might require more of certain nutrients and antioxidants to combat increased oxidative stress from physical exertion [227]. Vitamin D supplementation is particularly important in winter months or for individuals with limited sun exposure. In contrast, during summer, this might be less necessary. Vegetarians and vegans might lack certain nutrients like B12, iron, and omega-3 fatty acids, which are commonly found in animal products. People on specific diets might need to compensate for these gaps with supplements. It is important to consider personal health conditions and medications that can affect nutrient absorption. For instance, some medications can deplete certain vitamins, requiring supplementation.
Periodic blood tests can help monitor nutrient levels and adjust supplementation as needed. A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats is preferred. Supplementation should not replace a healthy diet, but rather complement it. Before starting any supplement regimen, patients should consult with a healthcare provider, especially for those with health conditions or taking medications. In general, high doses of supplements should be avoided to avoid adverse effects. It should be emphasized that high-quality supplements from reputable sources should be preferred to ensure safety and efficacy. In conclusion, while Table 6 provides a comprehensive list of supplements beneficial for cognitive health, the approach to supplementation should be personalized, considering the unique needs and circumstances of each individual. This tailored approach ensures optimal benefits for brain health and cognitive function.
Table 6.
Vitamins, minerals, antioxidants and other dietary supplements that can help support cognitive functions.
| Vitamins | Minerals | Antioxidants |
|---|---|---|
| Vitamin B Complex | Magnesium | Beta-carotene |
| Vitamin A | Selenium | Lutein |
| Vitamin C | Copper | Lycopene |
| Vitamin D | Iron | Coenzyme Q10 |
| Vitamin E | Zinc | Polyphenols |
| Vitamin K | Potassium | Curcumin (Turmeric) |
| Choline | Calcium | Acetyl-L-Carnitine |
| Omega 3 Polyunsaturated Fatty Acids (fish oils) | ||
| Probiotics, Prebiotics, Synbiotics | ||
Source: own ed. This review does not offer a detailed description of the effects of probiotics, prebiotics, synbiotics, carnitine, coenzyme Q10 supplementation.
6. Conclusions
The comprehensive analysis presented in this paper underscores the profound significance of nutritional supplementation in the preservation of cognitive health, particularly in the context of aging. Vitamins, minerals, antioxidants, dietary polyphenols, carotenoids and omega-3 PUFAs emerge as pivotal elements that play varied and crucial roles in maintaining and enhancing cognitive function. A combination of these offer neuroprotective benefits, enhancing memory, attention, and overall brain function. Their potent antioxidant properties are instrumental in combating oxidative stress, a key factor in age-related cognitive decline. Vitamins B, C, D, and E each contribute uniquely to brain health, from supporting neurotransmitter synthesis to protecting against neuronal damage and supporting mood regulation. Minerals such as magnesium, iron, selenium, zinc, and copper are equally essential, each playing a role in various brain functions and protecting against cognitive decline. Magnesium’s role in neurotransmission, iron’s importance in oxygen transport, selenium’s antioxidant capabilities, zinc’s neuroprotective properties, and copper’s involvement in energy production highlight the intricate interplay of these nutrients and minerals in maintaining cognitive health. It is, however, imperative to emphasize the necessity of individualized supplementation strategies. Factors such as age, sex [228], nutritional status, lifestyle, stress levels, physical activity, and specific dietary habits must be considered when tailoring supplementation regimes. A one-size-fits-all approach is insufficient; rather, personalized plans based on individual needs and conditions are crucial for optimal cognitive health benefits. In future studies on dietary supplements, it will be crucial to assess not only the cognitive benefits, but also the effects on the aging process itself, including impacts on biological age [229,230], to comprehensively understand how these interventions may influence overall health and longevity [231,232,233,234].
In conclusion, the role of dietary supplements in maintaining and enhancing cognitive function cannot be overstated. While our understanding of the exact mechanisms continues to evolve, the current evidence strongly supports the inclusion of these nutrients in a balanced diet or as part of a targeted supplementation strategy. Future research, particularly randomized controlled trials, will be pivotal in further elucidating these relationships and refining recommendations for dietary supplementation to preserve cognitive health, especially in the aging population. As we advance our understanding, it becomes increasingly clear that a holistic approach, combining dietary, lifestyle, and supplementation strategies, is essential for maintaining cognitive health and quality of life in older adults.
In the pursuit of healthy longevity, the integration of dietary supplementation within a holistic prevention plan is paramount [235,236,237,238,239,240,241,242,243]. The importance of healthy nutrition [183] and adopting a proper lifestyle cannot be understated in the context of preserving mental health [244] and cognitive function, especially as we age [245]. However, it is crucial to recognize that supplementation alone is not a panacea; instead, it should be viewed as one component of a comprehensive approach to healthy aging. A balanced and nutritious diet, rich in vitamins, minerals, and essential nutrients, forms the foundation of this holistic approach. Incorporating diets such as the MIND diet and the Mediterranean diet [246,247,248], known for their emphasis on whole grains, fruits, vegetables, healthy fats, and lean proteins, can significantly contribute to cognitive health and overall well-being. Regular physical activity is another cornerstone of this holistic plan [249,250,251,252]. Exercise not only enhances physical health but also has been shown to improve cognitive function, reduce stress, and boost mood [54,253,254,255,256]. Cognitive training [257] and engaging in mental activities, such as board games, reading, and puzzles [258], is equally important in old age. These activities stimulate the brain, helping to maintain its function and slow cognitive decline. Lifestyle modifications, including the cessation of smoking and the maintenance of healthy sleep patterns [259], are critical. Smoking cessation can significantly reduce the risk of diseases that impair cognitive function, while adequate, quality sleep is essential for brain health and memory consolidation. Regular monitoring of vital health indicators like blood pressure [260,261,262], blood sugar [263,264], and cholesterol levels further contributes to preventing conditions that could adversely impact cognitive health. In prescribing a combination of dietary supplements and lifestyle changes, healthcare providers should consider the individual’s overall health, lifestyle, and nutritional needs [265,266,267]. This tailored approach ensures not just the mitigation of disease risk but also the enhancement of life quality and longevity. Emphasizing patient education about the importance of each component in this holistic plan is key [268,269]. Patients should understand how lifestyle choices and dietary habits, combined with appropriate supplementation, work synergistically to promote optimal health. The future of Healthy Longevity Medicine lies in this multifaceted approach. By embracing a holistic strategy that combines nutrition, dietary supplements, physical activity, mental engagement, and lifestyle modifications, we can significantly enhance the prospects of not only living longer, but also enjoying a healthier, more fulfilling life in our later years.
Abbreviations
ACE-R: Addenbrooke’s Cognitive Examination–Revised; AD: Alzheimer’s disease; ADAS-Cog: Alzheimer’s Disease Assessment Scale-Cognitive Subscale; ALA: alpha lipoic acid; BDI-II,: Beck Depression Inventory-II; BMI: body mass index; CDR: clinical dementia rating; CDR: clinical dementia rating; CENTRAL: Central Register of Controlled Trials; CFO: commercial fish oil; CG: control group; CHAP: Chicago Health and Aging Project; CO: catfish oil; CVR: cerebrovascular responsiveness; DASH: Dietary Approaches to Stop Hypertension-Dietary Approach to Stop Hypertension; DHA: docosahexaenoic acid; DOTPs: desert olive tree pearls; EPA: eicosapentaenoic acid; FA: folic acid; FSIQ: full scale intelligence quotient; GI: glycaemic index; GSPE: grape seed polyphenol; HAM-D: Hamilton Depression Rating Scale; IG: intervention group; IQ: intelligence quotient; IU: international unit; LCPUFAs + LZ: Long-Chain Polyunsaturated Fatty Acids in Combination with Lutein and Zeaxanthin; Magtein®PS: magnesium L-threonate (Magtein) and phosphatidylserine-based formula; MCI: mild cognitive impairment; MIND: Mediterranean-DASH Intervention for Neurodegenerative Delay; MMSE: Mini-Mental State Examination; MUFA: monounsaturated fatty acid; NHANES: National Health and Nutrition Examination Survey; PO: Perilla frutescens seed oil; POPP: PO + ponkan powder; PUFA: polyunsaturated fatty acid; RCT: randomized controlled trial; SO: soybean oil; STROOP: Stroop Color and Word Test; WHO: World Health Organization.
Author Contributions
J.T.V., A.L. and M.F.: designed the study, wrote and published the manuscript. S.T., V.F.-P. and T.C.: supplemented and reviewed the manuscript. A.L. and Z.C.: prepared the manuscript for publication. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
Conflicts of Interest
The authors declare that they have no competing interest.
Funding Statement
Project: no. TKP2021-NKTA-47 was funded by the National Research, Development and Innovation Fund under the TKP2021-NKTA, with the support from the Ministry of Innovation and Technology of Hungary. The project was funded by the Ministry of Innovation and Technology under the National Cardiovascular Laboratory Program (RRF-2.3.1-21-2022-00003) from the National Research, Development and Innovation Fund. This work was also supported by the European University for Well-Being (EUniWell) program (grant agreement number: 101004093/EUniWell/EAC-A02-2019/EAC-A02-2019-1) and the National Institute on Aging (NIA R03AG070479, NIA K01AG073614), the American Heart Association AHA CDA941290, the NIA-supported Geroscience Training Program in Oklahoma (T32AG052363), the NIA-supported Oklahoma Nathan Shock Center, and the NIGMS-supported Center of Biomedical Research Excellence (CoBRE) (1P20GM125528-01A1). MF was supported by the ÚNKP-23-4-I-SE-2 New National Excellence Program of the Ministry for Innovation and Technology from the source of the National Research, Development and Innovation Fund. Funding sources played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Iadecola C., Duering M., Hachinski V., Joutel A., Pendlebury S.T., Schneider J.A., Dichgans M. Vascular Cognitive Impairment and Dementia: JACC Scientific Expert Panel. J. Am. Coll. Cardiol. 2019;73:3326–3344. doi: 10.1016/j.jacc.2019.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lane C.A., Hardy J., Schott J.M. Alzheimer’s disease. Eur. J. Neurol. 2018;25:59–70. doi: 10.1111/ene.13439. [DOI] [PubMed] [Google Scholar]
- 3.Li L., Hu L., Ji J., McKendrick K., Moreno J., Kelley A.S., Mazumdar M., Aldridge M. Determinants of Total End-of-Life Health Care Costs of Medicare Beneficiaries: A Quantile Regression Forests Analysis. J. Gerontol. A Biol. Sci. Med. Sci. 2022;77:1065–1071. doi: 10.1093/gerona/glab176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sebastiani P., Andersen S.L., Sweigart B., Du M., Cosentino S., Thyagarajan B., Christensen K., Schupf N., Perls T.T. Patterns of multi-domain cognitive aging in participants of the Long Life Family Study. Geroscience. 2020;42:1335–1350. doi: 10.1007/s11357-020-00202-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Corrada M.M., Brookmeyer R., Paganini-Hill A., Berlau D., Kawas C.H. Dementia incidence continues to increase with age in the oldest old: The 90+ study. Ann. Neurol. 2010;67:114–121. doi: 10.1002/ana.21915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stephan Y., Sutin A.R., Luchetti M., Terracciano A. Subjective age and risk of incident dementia: Evidence from the National Health and Aging Trends survey. J. Psychiatr. Res. 2018;100:1–4. doi: 10.1016/j.jpsychires.2018.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valsdottir V., Magnusdottir B.B., Chang M., Sigurdsson S., Gudnason V., Launer L.J., Jonsdottir M.K. Cognition and brain health among older adults in Iceland: The AGES-Reykjavik study. Geroscience. 2022;44:2785–2800. doi: 10.1007/s11357-022-00642-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rizzi L., Rosset I., Roriz-Cruz M. Global epidemiology of dementia: Alzheimer’s and vascular types. BioMed Res. Int. 2014;2014:908915. doi: 10.1155/2014/908915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lobo A., Launer L.J., Fratiglioni L., Andersen K., Di Carlo A., Breteler M.M., Copeland J.R., Dartigues J.F., Jagger C., Martinez-Lage J., et al. Prevalence of dementia and major subtypes in Europe: A collaborative study of population-based cohorts. Neurologic Diseases in the Elderly Research Group. Neurology. 2000;54((Suppl. 5)):S4–S9. [PubMed] [Google Scholar]
- 10.Shin J.H. Dementia Epidemiology Fact Sheet 2022. Ann. Rehabil. Med. 2022;46:53–59. doi: 10.5535/arm.22027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scott K.R., Barrett A.M. Dementia syndromes: Evaluation and treatment. Expert Rev. Neurother. 2007;7:407–422. doi: 10.1586/14737175.7.4.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gumus M., Multani N., Mack M.L., Tartaglia M.C., Alzheimer’s Disease Neuroimaging I. Progression of neuropsychiatric symptoms in young-onset versus late-onset Alzheimer’s disease. Geroscience. 2021;43:213–223. doi: 10.1007/s11357-020-00304-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van der Willik K.D., Licher S., Vinke E.J., Knol M.J., Darweesh S.K.L., van der Geest J.N., Schagen S.B., Ikram M.K., Luik A.I., Ikram M.A. Trajectories of Cognitive and Motor Function Between Ages 45 and 90 Years: A Population-Based Study. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:297–306. doi: 10.1093/gerona/glaa187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bendayan R., Zhu Y., Federman A.D., Dobson R.J.B. Multimorbidity Patterns and Memory Trajectories in Older Adults: Evidence From the English Longitudinal Study of Aging. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:867–875. doi: 10.1093/gerona/glab009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duong S., Patel T., Chang F. Dementia: What pharmacists need to know. Can. Pharm. J./Rev. Pharm. Du Can. 2017;150:118–129. doi: 10.1177/1715163517690745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Czakó C., Kovács T., Ungvari Z., Csiszar A., Yabluchanskiy A., Conley S., Csipo T., Lipecz A., Horváth H., Sándor G.L., et al. Retinal biomarkers for Alzheimer’s disease and vascular cognitive impairment and dementia (VCID): Implication for early diagnosis and prognosis. Geroscience. 2020;42:1499–1525. doi: 10.1007/s11357-020-00252-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.D’Arbeloff T. Cardiovascular fitness and structural brain integrity: An update on current evidence. Geroscience. 2020;42:1285–1306. doi: 10.1007/s11357-020-00244-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levit A., Hachinski V., Whitehead S.N. Neurovascular unit dysregulation, white matter disease, and executive dysfunction: The shared triad of vascular cognitive impairment and Alzheimer disease. Geroscience. 2020;42:445–465. doi: 10.1007/s11357-020-00164-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lopez M.E., Turrero A., Cuesta P., Rodriguez-Rojo I.C., Barabash A., Marcos A., Maestu F., Fernandez A. A multivariate model of time to conversion from mild cognitive impairment to Alzheimer’s disease. Geroscience. 2020;42:1715–1732. doi: 10.1007/s11357-020-00260-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fang X., Zhang J., Roman R.J., Fan F. From 1901 to 2022, how far are we from truly understanding the pathogenesis of age-related dementia? Geroscience. 2022;44:1879–1883. doi: 10.1007/s11357-022-00591-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Istvan L., Czako C., Elo A., Mihaly Z., Sotonyi P., Varga A., Ungvari Z., Csiszar A., Yabluchanskiy A., Conley S., et al. Imaging retinal microvascular manifestations of carotid artery disease in older adults: From diagnosis of ocular complications to understanding microvascular contributions to cognitive impairment. Geroscience. 2021;43:1703–1723. doi: 10.1007/s11357-021-00392-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Verheggen I.C.M., de Jong J.J.A., van Boxtel M.P.J., Gronenschild E., Palm W.M., Postma A.A., Jansen J.F.A., Verhey F.R.J., Backes W.H. Increase in blood-brain barrier leakage in healthy, older adults. Geroscience. 2020;42:1183–1193. doi: 10.1007/s11357-020-00211-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Verheggen I.C.M., de Jong J.J.A., van Boxtel M.P.J., Postma A.A., Jansen J.F.A., Verhey F.R.J., Backes W.H. Imaging the role of blood-brain barrier disruption in normal cognitive ageing. Geroscience. 2020;42:1751–1764. doi: 10.1007/s11357-020-00282-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kerkhofs D., Wong S.M., Zhang E., Uiterwijk R., Hoff E.I., Jansen J.F.A., Staals J., Backes W.H., van Oostenbrugge R.J. Blood-brain barrier leakage at baseline and cognitive decline in cerebral small vessel disease: A 2-year follow-up study. Geroscience. 2021;43:1643–1652. doi: 10.1007/s11357-021-00399-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Montagne A., Barnes S.R., Nation D.A., Kisler K., Toga A.W., Zlokovic B.V. Imaging subtle leaks in the blood-brain barrier in the aging human brain: Potential pitfalls, challenges, and possible solutions. Geroscience. 2022;44:1339–1351. doi: 10.1007/s11357-022-00571-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fan F., Roman R.J. Reversal of cerebral hypoperfusion: A novel therapeutic target for the treatment of AD/ADRD? Geroscience. 2021;43:1065–1067. doi: 10.1007/s11357-021-00357-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang S., Lv W., Zhang H., Liu Y., Li L., Jefferson J.R., Guo Y., Li M., Gao W., Fang X., et al. Aging exacerbates impairments of cerebral blood flow autoregulation and cognition in diabetic rats. Geroscience. 2020;42:1387–1410. doi: 10.1007/s11357-020-00233-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tarantini S., Balasubramanian P., Delfavero J., Csipo T., Yabluchanskiy A., Kiss T., Nyul-Toth A., Mukli P., Toth P., Ahire C., et al. Treatment with the BCL-2/BCL-xL inhibitor senolytic drug ABT263/Navitoclax improves functional hyperemia in aged mice. Geroscience. 2021;43:2427–2440. doi: 10.1007/s11357-021-00440-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vestergaard M.B., Lindberg U., Knudsen M.H., Urdanibia-Centelles O., Bakhtiari A., Mortensen E.L., Osler M., Fagerlund B., Benedek K., Lauritzen M., et al. Subclinical cognitive deficits are associated with reduced cerebrovascular response to visual stimulation in mid-sixties men. Geroscience. 2022;44:1905–1923. doi: 10.1007/s11357-022-00596-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sabayan B., Westendorp R.G.J. Neurovascular-glymphatic dysfunction and white matter lesions. Geroscience. 2021;43:1635–1642. doi: 10.1007/s11357-021-00361-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Szczesniak D., Rymaszewska J., Zimny A., Sasiadek M., Poltyn-Zaradna K., Smith E.E., Zatonska K., Zatonski T., Rangarajan S., Yusuf S., et al. Cerebral small vessel disease and other influential factors of cognitive impairment in the middle-aged: A long-term observational cohort PURE-MIND study in Poland. Geroscience. 2021;43:279–295. doi: 10.1007/s11357-020-00271-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cai M., Jacob M.A., Norris D.G., de Leeuw F.E., Tuladhar A.M. Longitudinal Relation Between Structural Network Efficiency, Cognition, and Gait in Cerebral Small Vessel Disease. J. Gerontol. A Biol. Sci. Med. Sci. 2022;77:554–560. doi: 10.1093/gerona/glab247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gardner A.W., Montgomery P.S., Wang M., Shen B., Casanegra A.I., Silva-Palacios F., Ungvari Z., Yabluchanskiy A., Csiszar A., Waldstein S.R. Cognitive decrement in older adults with symptomatic peripheral artery disease. Geroscience. 2021;43:2455–2465. doi: 10.1007/s11357-021-00437-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Luo J., le Cessie S., Blauw G.J., Franceschi C., Noordam R., van Heemst D. Systemic inflammatory markers in relation to cognitive function and measures of brain atrophy: A Mendelian randomization study. Geroscience. 2022;44:2259–2270. doi: 10.1007/s11357-022-00602-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lazar G., Jr., Varga J., Lazar G., Duda E., Takacs T., Balogh A., Lonovics J. The effects of glucocorticoids and a glucocorticoid antagonist (RU 38486) on experimental acute pancreatitis in rat. Acta Chir. Hung. 1997;36:190–191. [PubMed] [Google Scholar]
- 36.Boutzoukas E.M., O’Shea A., Kraft J.N., Hardcastle C., Evangelista N.D., Hausman H.K., Albizu A., Van Etten E.J., Bharadwaj P.K., Smith S.G., et al. Higher white matter hyperintensity load adversely affects pre-post proximal cognitive training performance in healthy older adults. Geroscience. 2022;44:1441–1455. doi: 10.1007/s11357-022-00538-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hausman H.K., Hardcastle C., Albizu A., Kraft J.N., Evangelista N.D., Boutzoukas E.M., Langer K., O’Shea A., Van Etten E.J., Bharadwaj P.K., et al. Cingulo-opercular and frontoparietal control network connectivity and executive functioning in older adults. Geroscience. 2022;44:847–866. doi: 10.1007/s11357-021-00503-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bray N.W., Pieruccini-Faria F., Witt S.T., Rockwood K., Bartha R., Doherty T.J., Nagamatsu L.S., Almeida Q.J., Liu-Ambrose T., Middleton L.E., et al. Frailty and functional brain connectivity (FBC) in older adults with mild cognitive impairment (MCI): Baseline results from the SYNERGIC Trial. Geroscience. 2023;45:1033–1048. doi: 10.1007/s11357-022-00702-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chino B., Cuesta P., Pacios J., de Frutos-Lucas J., Torres-Simon L., Doval S., Marcos A., Bruna R., Maestu F. Episodic memory dysfunction and hypersynchrony in brain functional networks in cognitively intact subjects and MCI: A study of 379 individuals. Geroscience. 2023;45:477–489. doi: 10.1007/s11357-022-00656-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sanchez-Roman I., Ferrando B., Holst C.M., Mengel-From J., Rasmussen S.H., Thinggaard M., Bohr V.A., Christensen K., Stevnsner T. Molecular markers of DNA repair and brain metabolism correlate with cognition in centenarians. Geroscience. 2022;44:103–125. doi: 10.1007/s11357-021-00502-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jiang J., Sheng C., Chen G., Liu C., Jin S., Li L., Jiang X., Han Y., Alzheimer’s Disease Neuroimaging I. Glucose metabolism patterns: A potential index to characterize brain ageing and predict high conversion risk into cognitive impairment. Geroscience. 2022;44:2319–2336. doi: 10.1007/s11357-022-00588-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lu W.H., Giudici K.V., Morley J.E., Guyonnet S., Parini A., Aggarwal G., Nguyen A.D., Li Y., Bateman R.J., Vellas B., et al. Investigating the combination of plasma amyloid-beta and geroscience biomarkers on the incidence of clinically meaningful cognitive decline in older adults. Geroscience. 2022;44:1489–1503. doi: 10.1007/s11357-022-00554-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Uleman J.F., Melis R.J.F., Quax R., van der Zee E.A., Thijssen D., Dresler M., van de Rest O., van der Velpen I.F., Adams H.H.H., Schmand B., et al. Mapping the multicausality of Alzheimer’s disease through group model building. Geroscience. 2021;43:829–843. doi: 10.1007/s11357-020-00228-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Casey D.A. Pharmacotherapy of neuropsychiatric symptoms of dementia. Pharm. Ther. 2015;40:284–287. [PMC free article] [PubMed] [Google Scholar]
- 45.Chaudhari K., Reynolds C.D., Yang S.H. Metformin and cognition from the perspectives of sex, age, and disease. Geroscience. 2020;42:97–116. doi: 10.1007/s11357-019-00146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Balazs N., Bereczki D., Ajtay A., Oberfrank F., Kovacs T. Cholinesterase inhibitors for the treatment of dementia: Real-life data in Hungary. Geroscience. 2022;44:253–263. doi: 10.1007/s11357-021-00470-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mandolesi L., Polverino A., Montuori S., Foti F., Ferraioli G., Sorrentino P., Sorrentino G. Effects of Physical Exercise on Cognitive Functioning and Wellbeing: Biological and Psychological Benefits. Front. Psychol. 2018;9:509. doi: 10.3389/fpsyg.2018.00509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang H. Nexus between cognitive reserve and modifiable risk factors of dementia. Int. Psychogeriatr. 2020;32:559–562. doi: 10.1017/S1041610220000320. [DOI] [Google Scholar]
- 49.Dhana K., Franco O.H., Ritz E.M., Ford C.N., Desai P., Krueger K.R., Holland T.M., Dhana A., Liu X., Aggarwal N.T. Healthy lifestyle and life expectancy with and without Alzheimer’s dementia: Population based cohort study. BMJ. 2022;377:e068390. doi: 10.1136/bmj-2021-068390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Berg-Weger M., Stewart D.B. Non-pharmacologic interventions for persons with dementia. Mo. Med. 2017;114:116. [PMC free article] [PubMed] [Google Scholar]
- 51.Choi H. Healthy lifestyles and more life years without dementia. BMJ. 2022;377:o885. doi: 10.1136/bmj.o885. [DOI] [PubMed] [Google Scholar]
- 52.Poddar J., Pradhan M., Ganguly G., Chakrabarti S. Biochemical deficits and cognitive decline in brain aging: Intervention by dietary supplements. J. Chem. Neuroanat. 2019;95:70–80. doi: 10.1016/j.jchemneu.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 53.Ungvari A., Gulej R., Csik B., Mukli P., Negri S., Tarantini S., Yabluchanskiy A., Benyo Z., Csiszar A., Ungvari Z. The Role of Methionine-Rich Diet in Unhealthy Cerebrovascular and Brain Aging: Mechanisms and Implications for Cognitive Impairment. Nutrients. 2023;15:4662. doi: 10.3390/nu15214662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ungvari Z., Fazekas-Pongor V., Csiszar A., Kunutsor S.K. The multifaceted benefits of walking for healthy aging: From Blue Zones to molecular mechanisms. Geroscience. 2023;45:3211–3239. doi: 10.1007/s11357-023-00873-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Azhar G., Wei J.Y., Schutzler S.E., Coker K., Gibson R.V., Kirby M.F., Ferrando A.A., Wolfe R.R. Daily Consumption of a Specially Formulated Essential Amino Acid-Based Dietary Supplement Improves Physical Performance in Older Adults With Low Physical Functioning. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:1184–1191. doi: 10.1093/gerona/glab019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dalle S., Van Roie E., Hiroux C., Vanmunster M., Coudyzer W., Suhr F., Bogaerts S., Van Thienen R., Koppo K. Omega-3 Supplementation Improves Isometric Strength But Not Muscle Anabolic and Catabolic Signaling in Response to Resistance Exercise in Healthy Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:406–414. doi: 10.1093/gerona/glaa309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kim C.S., Cha L., Sim M., Jung S., Chun W.Y., Baik H.W., Shin D.M. Probiotic Supplementation Improves Cognitive Function and Mood with Changes in Gut Microbiota in Community-Dwelling Older Adults: A Randomized, Double-Blind, Placebo-Controlled, Multicenter Trial. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:32–40. doi: 10.1093/gerona/glaa090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dhana K., Evans D.A., Rajan K.B., Bennett D.A., Morris M.C. Healthy lifestyle and the risk of Alzheimer dementia: Findings from 2 longitudinal studies. Neurology. 2020;95:e374–e383. doi: 10.1212/WNL.0000000000009816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cristina N.M., Lucia D. Nutrition and Healthy Aging: Prevention and Treatment of Gastrointestinal Diseases. Nutrients. 2021;13:4337. doi: 10.3390/nu13124337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Miller J.W. Proton pump inhibitors, H2-receptor antagonists, metformin, and vitamin B-12 deficiency: Clinical implications. Adv. Nutr. 2018;9:511S–518S. doi: 10.1093/advances/nmy023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Suliburska J., Chmurzynska A., Kocylowski R., Skrypnik K., Radziejewska A., Baralkiewicz D. Effect of iron and folic acid supplementation on the level of essential and toxic elements in young women. Int. J. Environ. Res. Public Health. 2021;18:1360. doi: 10.3390/ijerph18031360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mooldijk S.S., Licher S., Vernooij M.W., Ikram M.K., Ikram M.A. Seasonality of cognitive function in the general population: The Rotterdam Study. Geroscience. 2022;44:281–291. doi: 10.1007/s11357-021-00485-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fantini C., Corinaldesi C., Lenzi A., Migliaccio S., Crescioli C. Vitamin D as a Shield against Aging. Int. J. Mol. Sci. 2023;24:4546. doi: 10.3390/ijms24054546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fekete M., Csípő T., Fazekas-Pongor V., Fehér Á., Szarvas Z., Kaposvári C., Horváth K., Lehoczki A., Tarantini S., Varga J.T. The Effectiveness of Supplementation with Key Vitamins, Minerals, Antioxidants and Specific Nutritional Supplements in COPD-A Review. Nutrients. 2023;15:2741. doi: 10.3390/nu15122741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dighriri I.M., Alsubaie A.M., Hakami F.M., Hamithi D.M., Alshekh M.M., Khobrani F.A., Dalak F.E., Hakami A.A., Alsueaadi E.H., Alsaawi L.S. Effects of omega-3 polyunsaturated fatty acids on brain functions: A systematic review. Cureus. 2022;14:e30091. doi: 10.7759/cureus.30091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.De Magalhães J.P., Müller M., Rainger G.E., Steegenga W. Fish oil supplements, longevity and aging. Aging. 2016;8:1578. doi: 10.18632/aging.101021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fekete M., Szarvas Z., Fazekas-Pongor V., Lehoczki A., Tarantini S., Varga J.T. Effects of omega-3 supplementation on quality of life, nutritional status, inflammatory parameters, lipid profile, exercise tolerance and inhaled medications in chronic obstructive pulmonary disease. Ann. Palliat. Med. 2022;11:2819–2829. doi: 10.21037/apm-22-254. [DOI] [PubMed] [Google Scholar]
- 68.Innes J.K., Calder P.C. Omega-6 fatty acids and inflammation. Prostaglandins Leukot. Essent. Fat. Acids. 2018;132:41–48. doi: 10.1016/j.plefa.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 69.Kim J.S., Thomashow M.A., Yip N.H., Burkart K.M., Lo Cascio C.M., Shimbo D., Barr R.G. Randomization to Omega-3 Fatty Acid Supplementation and Endothelial Function in COPD: The COD-Fish Randomized Controlled Trial. Chronic Obs. Pulm. Dis. 2021;8:41–53. doi: 10.15326/jcopdf.8.1.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Leitão C., Mignano A., Estrela M., Fardilha M., Figueiras A., Roque F., Herdeiro M.T. The Effect of Nutrition on Aging-A Systematic Review Focusing on Aging-Related Biomarkers. Nutrients. 2022;14:554. doi: 10.3390/nu14030554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lane K., Derbyshire E., Li W., Brennan C. Bioavailability and potential uses of vegetarian sources of omega-3 fatty acids: A review of the literature. Crit. Rev. Food Sci. Nutr. 2014;54:572–579. doi: 10.1080/10408398.2011.596292. [DOI] [PubMed] [Google Scholar]
- 72.Smith D., Refsum H., Oulhaj A., de Jager C.A., Jerneren F. Beneficial Interactions Between B Vitamins and Omega-3 Fatty Acids in the Prevention of Brain Atrophy and of Cognitive Decline in Early Stage Alzheimer’s Disease. FASEB J. 2016;30:407.6. doi: 10.1096/fasebj.30.1_supplement.407.6. [DOI] [Google Scholar]
- 73.Gibson G.E., Luchsinger J.A., Cirio R., Chen H., Franchino-Elder J., Hirsch J.A., Bettendorff L., Chen Z., Flowers S.A., Gerber L.M., et al. Benfotiamine and Cognitive Decline in Alzheimer’s Disease: Results of a Randomized Placebo-Controlled Phase IIa Clinical Trial. J. Alzheimer’s Dis. 2020;78:989–1010. doi: 10.3233/JAD-200896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ma F., Li Q., Zhou X., Zhao J., Song A., Li W., Liu H., Xu W., Huang G. Effects of folic acid supplementation on cognitive function and Aβ-related biomarkers in mild cognitive impairment: A randomized controlled trial. Eur. J. Nutr. 2019;58:345–356. doi: 10.1007/s00394-017-1598-5. [DOI] [PubMed] [Google Scholar]
- 75.Zhang C., Hu Q., Li S., Dai F., Qian W., Hewlings S., Yan T., Wang Y. A Magtein(®), Magnesium L-Threonate, -Based Formula Improves Brain Cognitive Functions in Healthy Chinese Adults. Nutrients. 2022;14:5235. doi: 10.3390/nu14245235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bai D., Fan J., Li M., Dong C., Gao Y., Fu M., Huang G., Liu H. Effects of Folic Acid Combined with DHA Supplementation on Cognitive Function and Amyloid-β-Related Biomarkers in Older Adults with Mild Cognitive Impairment by a Randomized, Double Blind, Placebo-Controlled Trial. J. Alzheimer’s Dis. 2021;81:155–167. doi: 10.3233/JAD-200997. [DOI] [PubMed] [Google Scholar]
- 77.Ma F., Zhou X., Li Q., Zhao J., Song A., An P., Du Y., Xu W., Huang G. Effects of Folic Acid and Vitamin B12, Alone and in Combination on Cognitive Function and Inflammatory Factors in the Elderly with Mild Cognitive Impairment: A Single-blind Experimental Design. Curr. Alzheimer Res. 2019;16:622–632. doi: 10.2174/1567205016666190725144629. [DOI] [PubMed] [Google Scholar]
- 78.Li M., Li W., Gao Y., Chen Y., Bai D., Weng J., Du Y., Ma F., Wang X., Liu H., et al. Effect of folic acid combined with docosahexaenoic acid intervention on mild cognitive impairment in elderly: A randomized double-blind, placebo-controlled trial. Eur. J. Nutr. 2021;60:1795–1808. doi: 10.1007/s00394-020-02373-3. [DOI] [PubMed] [Google Scholar]
- 79.Kwok T., Wu Y., Lee J., Lee R., Yung C.Y., Choi G., Lee V., Harrison J., Lam L., Mok V. A randomized placebo-controlled trial of using B vitamins to prevent cognitive decline in older mild cognitive impairment patients. Clin. Nutr. 2020;39:2399–2405. doi: 10.1016/j.clnu.2019.11.005. [DOI] [PubMed] [Google Scholar]
- 80.Thaung Zaw J.J., Howe P.R., Wong R.H. Long-term effects of resveratrol on cognition, cerebrovascular function and cardio-metabolic markers in postmenopausal women: A 24-month randomised, double-blind, placebo-controlled, crossover study. Clin. Nutr. 2021;40:820–829. doi: 10.1016/j.clnu.2020.08.025. [DOI] [PubMed] [Google Scholar]
- 81.Foroumandi E., Javan R., Moayed L., Fahimi H., Kheirabadi F., Neamatshahi M., Shogofteh F., Zarghi A. The effects of fenugreek seed extract supplementation in patients with Alzheimer’s disease: A randomized, double-blind, placebo-controlled trial. Phytother. Res. 2023;37:285–294. doi: 10.1002/ptr.7612. [DOI] [PubMed] [Google Scholar]
- 82.Sim M., Hong S., Jung S., Kim J.S., Goo Y.T., Chun W.Y., Shin D.M. Vitamin C supplementation promotes mental vitality in healthy young adults: Results from a cross-sectional analysis and a randomized, double-blind, placebo-controlled trial. Eur. J. Nutr. 2022;61:447–459. doi: 10.1007/s00394-021-02656-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stringham N.T., Holmes P.V., Stringham J.M. Effects of macular xanthophyll supplementation on brain-derived neurotrophic factor, pro-inflammatory cytokines, and cognitive performance. Physiol. Behav. 2019;211:112650. doi: 10.1016/j.physbeh.2019.112650. [DOI] [PubMed] [Google Scholar]
- 84.Lai S., Petramala L., Muscaritoli M., Cianci R., Mazzaferro S., Mitterhofer A.P., Pasquali M., D’Ambrosio V., Carta M., Ansuini M., et al. α-lipoic acid in patients with autosomal dominant polycystic kidney disease. Nutrition. 2020;71:110594. doi: 10.1016/j.nut.2019.110594. [DOI] [PubMed] [Google Scholar]
- 85.Yoon J., Sasaki K., Nishimura I., Hashimoto H., Okura T., Isoda H. Effects of Desert Olive Tree Pearls Containing High Hydroxytyrosol Concentrations on the Cognitive Functions of Middle-Aged and Older Adults. Nutrients. 2023;15:3234. doi: 10.3390/nu15143234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Morató X., Marquié M., Tartari J.P., Lafuente A., Abdelnour C., Alegret M., Jofresa S., Buendía M., Pancho A., Aguilera N., et al. A randomized, open-label clinical trial in mild cognitive impairment with EGb 761 examining blood markers of inflammation and oxidative stress. Sci. Rep. 2023;13:5406. doi: 10.1038/s41598-023-32515-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Baker L.D., Manson J.E., Rapp S.R., Sesso H.D., Gaussoin S.A., Shumaker S.A., Espeland M.A. Effects of cocoa extract and a multivitamin on cognitive function: A randomized clinical trial. Alzheimer’s Dement. 2023;19:1308–1319. doi: 10.1002/alz.12767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bell L., Whyte A.R., Lamport D.J., Spencer J.P.E., Butler L.T., Williams C.M. Grape seed polyphenol extract and cognitive function in healthy young adults: A randomised, placebo-controlled, parallel-groups acute-on-chronic trial. Nutr. Neurosci. 2022;25:54–63. doi: 10.1080/1028415X.2019.1708033. [DOI] [PubMed] [Google Scholar]
- 89.Hashimoto M., Matsuzaki K., Maruyama K., Hossain S., Sumiyoshi E., Wakatsuki H., Kato S., Ohno M., Tanabe Y., Kuroda Y., et al. Perilla seed oil in combination with nobiletin-rich ponkan powder enhances cognitive function in healthy elderly Japanese individuals: A possible supplement for brain health in the elderly. Food Funct. 2022;13:2768–2781. doi: 10.1039/D1FO03508H. [DOI] [PubMed] [Google Scholar]
- 90.Zajac I.T., Barnes M., Cavuoto P., Wittert G., Noakes M. The Effects of Vitamin D-Enriched Mushrooms and Vitamin D3 on Cognitive Performance and Mood in Healthy Elderly Adults: A Randomised, Double-Blinded, Placebo-Controlled Trial. Nutrients. 2020;12:3847. doi: 10.3390/nu12123847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jorde R., Kubiak J., Svartberg J., Fuskevåg O.M., Figenschau Y., Martinaityte I., Grimnes G. Vitamin D supplementation has no effect on cognitive performance after four months in mid-aged and older subjects. J. Neurol. Sci. 2019;396:165–171. doi: 10.1016/j.jns.2018.11.020. [DOI] [PubMed] [Google Scholar]
- 92.Bischoff-Ferrari H.A., Vellas B., Rizzoli R., Kressig R.W., da Silva J.A.P., Blauth M., Felson D.T., McCloskey E.V., Watzl B., Hofbauer L.C., et al. Effect of Vitamin D Supplementation, Omega-3 Fatty Acid Supplementation, or a Strength-Training Exercise Program on Clinical Outcomes in Older Adults: The DO-HEALTH Randomized Clinical Trial. JAMA. 2020;324:1855–1868. doi: 10.1001/jama.2020.16909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Jia J., Hu J., Huo X., Miao R., Zhang Y., Ma F. Effects of vitamin D supplementation on cognitive function and blood Aβ-related biomarkers in older adults with Alzheimer’s disease: A randomised, double-blind, placebo-controlled trial. J. Neurol. Neurosurg. Psychiatry. 2019;90:1347–1352. doi: 10.1136/jnnp-2018-320199. [DOI] [PubMed] [Google Scholar]
- 94.Yang T., Wang H., Xiong Y., Chen C., Duan K., Jia J., Ma F. Vitamin D Supplementation Improves Cognitive Function Through Reducing Oxidative Stress Regulated by Telomere Length in Older Adults with Mild Cognitive Impairment: A 12-Month Randomized Controlled Trial. J. Alzheimer’s Dis. 2020;78:1509–1518. doi: 10.3233/JAD-200926. [DOI] [PubMed] [Google Scholar]
- 95.Castle M., Fiedler N., Pop L.C., Schneider S.J., Schlussel Y., Sukumar D., Hao L., Shapses S.A. Three Doses of Vitamin D and Cognitive Outcomes in Older Women: A Double-Blind Randomized Controlled Trial. J. Gerontol. A Biol. Sci. Med. Sci. 2020;75:835–842. doi: 10.1093/gerona/glz041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ghaderi A., Rasouli-Azad M., Farhadi M.H., Mirhosseini N., Motmaen M., Pishyareh E., Omidi A., Asemi Z. Exploring the Effects of Vitamin D Supplementation on Cognitive Functions and Mental Health Status in Subjects Under Methadone Maintenance Treatment. J. Addict. Med. 2020;14:18–25. doi: 10.1097/ADM.0000000000000550. [DOI] [PubMed] [Google Scholar]
- 97.Hu J., Jia J., Zhang Y., Miao R., Huo X., Ma F. Effects of vitamin D(3) supplementation on cognition and blood lipids: A 12-month randomised, double-blind, placebo-controlled trial. J. Neurol. Neurosurg. Psychiatry. 2018;89:1341–1347. doi: 10.1136/jnnp-2018-318594. [DOI] [PubMed] [Google Scholar]
- 98.Schietzel S., Fischer K., Brugger P., Orav E.J., Renerts K., Gagesch M., Freystaetter G., Stähelin H.B., Egli A., Bischoff-Ferrari H.A. Effect of 2000 IU compared with 800 IU vitamin D on cognitive performance among adults age 60 years and older: A randomized controlled trial. Am. J. Clin. Nutr. 2019;110:246–253. doi: 10.1093/ajcn/nqz081. [DOI] [PubMed] [Google Scholar]
- 99.Byrn M.A., Adams W., Penckofer S., Emanuele M.A. Vitamin D Supplementation and Cognition in People with Type 2 Diabetes: A Randomized Control Trial. J. Diabetes Res. 2019;2019:5696391. doi: 10.1155/2019/5696391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Beauchet O., Launay C.P., Galery K., Vilcocq C., Dontot-Payen F., Rousseau B., Benoit V., Allali G. Effects of Vitamin D and Calcium Fortified Yogurts on Gait, Cognitive Performances, and Serum 25-Hydroxyvitamin D Concentrations in Older Community-Dwelling Females: Results from the GAit, MEmory, Dietary and Vitamin D (GAME-D2) Randomized Controlled Trial. Nutrients. 2019;11:2880. doi: 10.3390/nu11122880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Owusu J.E., Islam S., Katumuluwa S.S., Stolberg A.R., Usera G.L., Anwarullah A.A., Shieh A., Dhaliwal R., Ragolia L., Mikhail M.B., et al. Cognition and Vitamin D in Older African-American Women- Physical performance and Osteoporosis prevention with vitamin D in older African Americans Trial and Dementia. J. Am. Geriatr. Soc. 2019;67:81–86. doi: 10.1111/jgs.15607. [DOI] [PubMed] [Google Scholar]
- 102.Macpherson H., Brownell S., Harris E., Duckham R.L., O’Connell S., Meyer B.J., Mirzaee S., Daly R.M. Effects of a 6-Month Multifaceted Diet and Exercise Intervention on Cognition in Older Adults at Risk of Cognitive Decline: The PONDER Double-Blind, Placebo-Controlled Randomized Trial. J. Alzheimer’s Dis. 2022;89:247–263. doi: 10.3233/JAD-220234. [DOI] [PubMed] [Google Scholar]
- 103.Nolan J.M., Power R., Howard A.N., Bergin P., Roche W., Prado-Cabrero A., Pope G., Cooke J., Power T., Mulcahy R. Supplementation With Carotenoids, Omega-3 Fatty Acids, and Vitamin E Has a Positive Effect on the Symptoms and Progression of Alzheimer’s Disease. J. Alzheimer’s Dis. 2022;90:233–249. doi: 10.3233/JAD-220556. [DOI] [PubMed] [Google Scholar]
- 104.Stavrinou P.S., Andreou E., Aphamis G., Pantzaris M., Ioannou M., Patrikios I.S., Giannaki C.D. The Effects of a 6-Month High Dose Omega-3 and Omega-6 Polyunsaturated Fatty Acids and Antioxidant Vitamins Supplementation on Cognitive Function and Functional Capacity in Older Adults with Mild Cognitive Impairment. Nutrients. 2020;12:325. doi: 10.3390/nu12020325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Atmadja T., Kusharto C., Sinaga T. Supplementation of Catfish (Clarias gariepinus) Oil Enriched with Omega-3 Soft Capsule Improves Oxidative Stress and Cognitive Function in Elderly. J. Nutr. Sci. Vitaminol. 2020;66:S47–S50. doi: 10.3177/jnsv.66.S47. [DOI] [PubMed] [Google Scholar]
- 106.Patan M.J., Kennedy D.O., Husberg C., Hustvedt S.O., Calder P.C., Khan J., Forster J., Jackson P.A. Supplementation with oil rich in eicosapentaenoic acid, but not in docosahexaenoic acid, improves global cognitive function in healthy, young adults: Results from randomized controlled trials. Am. J. Clin. Nutr. 2021;114:914–924. doi: 10.1093/ajcn/nqab174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Rasmussen J. The LipiDiDiet trial: What does it add to the current evidence for Fortasyn Connect in early Alzheimer’s disease? Clin. Interv. Aging. 2019;14:1481–1492. doi: 10.2147/CIA.S211739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lin P.Y., Cheng C., Satyanarayanan S.K., Chiu L.T., Chien Y.C., Chuu C.P., Lan T.H., Su K.P. Omega-3 fatty acids and blood-based biomarkers in Alzheimer’s disease and mild cognitive impairment: A randomized placebo-controlled trial. Brain Behav. Immun. 2022;99:289–298. doi: 10.1016/j.bbi.2021.10.014. [DOI] [PubMed] [Google Scholar]
- 109.Giudici K.V., de Souto Barreto P., Beard J., Cantet C., Araujo de Carvalho I., Rolland Y., Vellas B. Effect of long-term omega-3 supplementation and a lifestyle multidomain intervention on intrinsic capacity among community-dwelling older adults: Secondary analysis of a randomized, placebo-controlled trial (MAPT study) Maturitas. 2020;141:39–45. doi: 10.1016/j.maturitas.2020.06.012. [DOI] [PubMed] [Google Scholar]
- 110.Mengelberg A., Leathem J., Podd J., Hill S., Conlon C. The effects of docosahexaenoic acid supplementation on cognition and well-being in mild cognitive impairment: A 12-month randomised controlled trial. Int. J. Geriatr. Psychiatry. 2022;37:1–12. doi: 10.1002/gps.5707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Leckie R.L., Lehman D.E., Gianaros P.J., Erickson K.I., Sereika S.M., Kuan D.C.H., Manuck S.B., Ryan C.M., Yao J.K., Muldoon M.F. The effects of omega-3 fatty acids on neuropsychological functioning and brain morphology in mid-life adults: A randomized clinical trial. Psychol. Med. 2020;50:2425–2434. doi: 10.1017/S0033291719002617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sueyasu T., Yasumoto K., Tokuda H., Kaneda Y., Obata H., Rogi T., Izumo T., Kondo S., Saito J., Tsukiura T., et al. Effects of Long-Chain Polyunsaturated Fatty Acids in Combination with Lutein and Zeaxanthin on Episodic Memory in Healthy Older Adults. Nutrients. 2023;15:2825. doi: 10.3390/nu15132825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Arellanes I.C., Choe N., Solomon V., He X., Kavin B., Martinez A.E., Kono N., Buennagel D.P., Hazra N., Kim G., et al. Brain delivery of supplemental docosahexaenoic acid (DHA): A randomized placebo-controlled clinical trial. EBioMedicine. 2020;59:102883. doi: 10.1016/j.ebiom.2020.102883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kuszewski J.C., Howe P.R.C., Wong R.H.X. Evaluation of Cognitive Performance following Fish-Oil and Curcumin Supplementation in Middle-Aged and Older Adults with Overweight or Obesity. J. Nutr. 2020;150:3190–3199. doi: 10.1093/jn/nxaa299. [DOI] [PubMed] [Google Scholar]
- 115.Xu H., Wang S., Gao F., Li C. Vitamin B6, B9, and B12 Intakes and Cognitive Performance in Elders: National Health and Nutrition Examination Survey, 2011–2014. Neuropsychiatr. Dis. Treat. 2022;18:537. doi: 10.2147/NDT.S337617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Smith A.D., Refsum H., Bottiglieri T., Fenech M., Hooshmand B., McCaddon A., Miller J.W., Rosenberg I.H., Obeid R. Homocysteine and dementia: An international consensus statement. J. Alzheimer’s Dis. 2018;62:561–570. doi: 10.3233/JAD-171042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kataria N., Yadav P., Kumar R., Kumar N., Singh M., Kant R., Kalyani V. Effect of vitamin B6, B9, and B12 supplementation on homocysteine level and cardiovascular outcomes in stroke patients: A meta-analysis of randomized controlled trials. Cureus. 2021;13:e14958. doi: 10.7759/cureus.14958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Fekete M., Fazekas-Pongor V., Szőllősi G., Varga J.T. A krónikus obstruktív tüdőbetegség metabolikus következményei. Orvosi Hetil. 2021;162:185–191. doi: 10.1556/650.2021.31984. [DOI] [PubMed] [Google Scholar]
- 119.Wang Z., Zhu W., Xing Y., Jia J., Tang Y. B vitamins and prevention of cognitive decline and incident dementia: A systematic review and meta-analysis. Nutr. Rev. 2022;80:931–949. doi: 10.1093/nutrit/nuab057. [DOI] [PubMed] [Google Scholar]
- 120.Gong X., Shi L., Wu Y., Luo Y., Kwok T. B Vitamin Supplementation Slows Cognitive Decline in Mild Cognitive Impairment Patients with Frontal Lobe Atrophy. J. Alzheimer’s Dis. 2022;89:1453–1461. doi: 10.3233/JAD-220685. [DOI] [PubMed] [Google Scholar]
- 121.Smith A.D., Smith S.M., De Jager C.A., Whitbread P., Johnston C., Agacinski G., Oulhaj A., Bradley K.M., Jacoby R., Refsum H. Homocysteine-lowering by B vitamins slows the rate of accelerated brain atrophy in mild cognitive impairment: A randomized controlled trial. PLoS ONE. 2010;5:e12244. doi: 10.1371/journal.pone.0012244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Bottiglieri T. Folate, vitamin B12, and neuropsychiatric disorders. Nutr. Rev. 1996;54:382–390. doi: 10.1111/j.1753-4887.1996.tb03851.x. [DOI] [PubMed] [Google Scholar]
- 123.Calderón-Ospina C.A., Nava-Mesa M.O. B Vitamins in the nervous system: Current knowledge of the biochemical modes of action and synergies of thiamine, pyridoxine, and cobalamin. CNS Neurosci. Ther. 2020;26:5–13. doi: 10.1111/cns.13207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Jurcau A. The role of natural antioxidants in the prevention of dementia—Where do we stand and future perspectives. Nutrients. 2021;13:282. doi: 10.3390/nu13020282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Mock J.T., Chaudhari K., Sidhu A., Sumien N. The influence of vitamins E and C and exercise on brain aging. Exp. Gerontol. 2017;94:69–72. doi: 10.1016/j.exger.2016.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Moreau K.L., Hildreth K.L., Klawitter J., Blatchford P., Kohrt W.M. Decline in endothelial function across the menopause transition in healthy women is related to decreased estradiol and increased oxidative stress. Geroscience. 2020;42:1699–1714. doi: 10.1007/s11357-020-00236-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Feng J., Zheng Y., Guo M., Ares I., Martínez M., Lopez-Torres B., Martínez-Larrañaga M.-R., Wang X., Anadón A., Martínez M.-A. Oxidative stress, the blood–brain barrier and neurodegenerative diseases: The critical beneficial role of dietary antioxidants. Acta Pharm. Sin. B. 2023;13:3988–4024. doi: 10.1016/j.apsb.2023.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Sadowska-Bartosz I., Bartosz G. Effect of antioxidants supplementation on aging and longevity. BioMed Res. Int. 2014;2014:404680. doi: 10.1155/2014/404680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Shah H., Dehghani F., Ramezan M., Gannaban R.B., Haque Z.F., Rahimi F., Abbasi S., Shin A.C. Revisiting the Role of Vitamins and Minerals in Alzheimer’s Disease. Antioxidants. 2023;12:415. doi: 10.3390/antiox12020415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Figueroa-Méndez R., Rivas-Arancibia S. Vitamin C in health and disease: Its role in the metabolism of cells and redox state in the brain. Front. Physiol. 2015;6:397. doi: 10.3389/fphys.2015.00397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.McCall S.J., Clark A.B., Luben R.N., Wareham N.J., Khaw K.-T., Myint P.K. Plasma vitamin C levels: Risk factors for deficiency and association with self-reported functional health in the European Prospective Investigation into Cancer-Norfolk. Nutrients. 2019;11:1552. doi: 10.3390/nu11071552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Morelli M.B., Gambardella J., Castellanos V., Trimarco V., Santulli G. Vitamin C and cardiovascular disease: An update. Antioxidants. 2020;9:1227. doi: 10.3390/antiox9121227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Conner T.S., Fletcher B.D., Haszard J.J., Pullar J.M., Spencer E., Mainvil L.A., Vissers M.C. KiwiC for Vitality: Results of a Placebo-Controlled Trial Testing the Effects of Kiwifruit or Vitamin C Tablets on Vitality in Adults with Low Vitamin C Levels. Nutrients. 2020;12:2898. doi: 10.3390/nu12092898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sharma Y., Popescu A., Horwood C., Hakendorf P., Thompson C. Relationship between vitamin C deficiency and cognitive impairment in older hospitalised patients: A cross-sectional study. Antioxidants. 2022;11:463. doi: 10.3390/antiox11030463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Pearson J.F., Pullar J.M., Wilson R., Spittlehouse J.K., Vissers M.C., Skidmore P.M., Willis J., Cameron V.A., Carr A.C. Vitamin C status correlates with markers of metabolic and cognitive health in 50-year-olds: Findings of the CHALICE cohort study. Nutrients. 2017;9:831. doi: 10.3390/nu9080831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Travica N., Ried K., Sali A., Hudson I., Scholey A., Pipingas A. Plasma vitamin C concentrations and cognitive function: A cross-sectional study. Front. Aging Neurosci. 2019;11:72. doi: 10.3389/fnagi.2019.00072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Plevin D., Galletly C. The neuropsychiatric effects of vitamin C deficiency: A systematic review. BMC Psychiatry. 2020;20:315. doi: 10.1186/s12888-020-02730-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Yosaee S., Keshtkaran Z., Abdollahi S., Shidfar F., Sarris J., Soltani S. The effect of vitamin C supplementation on mood status in adults: A systematic review and meta-analysis of randomized controlled clinical trials. Gen. Hosp. Psychiatry. 2021;71:36–42. doi: 10.1016/j.genhosppsych.2021.04.006. [DOI] [PubMed] [Google Scholar]
- 139.Von Arnim C.A., Herbolsheimer F., Nikolaus T., Peter R., Biesalski H.K., Ludolph A.C., Riepe M., Nagel G. Dietary antioxidants and dementia in a population-based case-control study among older people in South Germany. J. Alzheimer’s Dis. 2012;31:717–724. doi: 10.3233/JAD-2012-120634. [DOI] [PubMed] [Google Scholar]
- 140.Harrison F.E. A critical review of vitamin C for the prevention of age-related cognitive decline and Alzheimer’s disease. J. Alzheimer’s Dis. 2012;29:711–726. doi: 10.3233/JAD-2012-111853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Pincemail J., Meziane S. On the Potential Role of the Antioxidant Couple Vitamin E/Selenium Taken by the Oral Route in Skin and Hair Health. Antioxidants. 2022;11:2270. doi: 10.3390/antiox11112270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Rizvi S., Raza S.T., Ahmed F., Ahmad A., Abbas S., Mahdi F. The role of vitamin E in human health and some diseases. Sultan Qaboos Univ. Med. J. 2014;14:e157. [PMC free article] [PubMed] [Google Scholar]
- 143.Mangialasche F., Solomon A., Kåreholt I., Hooshmand B., Cecchetti R., Fratiglioni L., Soininen H., Laatikainen T., Mecocci P., Kivipelto M. Serum levels of vitamin E forms and risk of cognitive impairment in a Finnish cohort of older adults. Exp. Gerontol. 2013;48:1428–1435. doi: 10.1016/j.exger.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 144.Rudrapal M., Khairnar S.J., Khan J., Dukhyil A.B., Ansari M.A., Alomary M.N., Alshabrmi F.M., Palai S., Deb P.K., Devi R. Dietary polyphenols and their role in oxidative stress-induced human diseases: Insights into protective effects, antioxidant potentials and mechanism (s) of action. Front. Pharmacol. 2022;13:283. doi: 10.3389/fphar.2022.806470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Meccariello R., D’Angelo S. Impact of polyphenolic-food on longevity: An elixir of life. An overview. Antioxidants. 2021;10:507. doi: 10.3390/antiox10040507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Sharifi-Rad J., Rayess Y.E., Rizk A.A., Sadaka C., Zgheib R., Zam W., Sestito S., Rapposelli S., Neffe-Skocińska K., Zielińska D. Turmeric and its major compound curcumin on health: Bioactive effects and safety profiles for food, pharmaceutical, biotechnological and medicinal applications. Front. Pharmacol. 2020;11:1021. doi: 10.3389/fphar.2020.01021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.El-Saadony M.T., Yang T., Korma S.A., Sitohy M., El-Mageed A., Taia A., Selim S., Al Jaouni S.K., Salem H.M., Mahmmod Y. Impacts of turmeric and its principal bioactive curcumin on human health: Pharmaceutical, medicinal, and food applications: A comprehensive review. Front. Nutr. 2023;9:1040259. doi: 10.3389/fnut.2022.1040259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Pervin M., Unno K., Ohishi T., Tanabe H., Miyoshi N., Nakamura Y. Beneficial effects of green tea catechins on neurodegenerative diseases. Molecules. 2018;23:1297. doi: 10.3390/molecules23061297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Tolun A., Altintas Z. Functional and Medicinal Beverages. Elsevier; Amsterdam, The Netherlands: 2019. Medicinal properties and functional components of beverages; pp. 235–284. [Google Scholar]
- 150.Minocha T., Birla H., Obaid A.A., Rai V., Sushma P., Shivamallu C., Moustafa M., Al-Shehri M., Al-Emam A., Tikhonova M.A. Flavonoids as promising neuroprotectants and their therapeutic potential against Alzheimer’s disease. Oxidative Med. Cell. Longev. 2022;2022:6038996. doi: 10.1155/2022/6038996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Fernandes L., Cardim-Pires T.R., Foguel D., Palhano F.L. Green tea polyphenol epigallocatechin-gallate in amyloid aggregation and neurodegenerative diseases. Front. Neurosci. 2021;15:718188. doi: 10.3389/fnins.2021.718188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zheng T., Bielinski D.F., Fisher D.R., Zhang J., Shukitt-Hale B. Protective effects of a polyphenol-rich blueberry extract on adult human neural progenitor cells. Molecules. 2022;27:6152. doi: 10.3390/molecules27196152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Lu W.H., de Souto Barreto P., Rolland Y., Bouyahia A., Fischer C., Mangin J.F., Giudici K.V., Vellas B., Group M.D. Biological and Neuroimaging Markers as Predictors of 5-Year Incident Frailty in Older Adults: A Secondary Analysis of the MAPT Study. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:e361–e369. doi: 10.1093/gerona/glaa296. [DOI] [PubMed] [Google Scholar]
- 154.Guralnik J.M., Sternberg A.L., Mitchell C.M., Blackford A.L., Schrack J., Wanigatunga A.A., Michos E., Juraschek S.P., Szanton S., Kalyani R., et al. Effects of Vitamin D on Physical Function: Results From the STURDY Trial. J. Gerontol. A Biol. Sci. Med. Sci. 2022;77:1585–1592. doi: 10.1093/gerona/glab379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Wacker M., Holick M.F. Vitamin D—Effects on skeletal and extraskeletal health and the need for supplementation. Nutrients. 2013;5:111–148. doi: 10.3390/nu5010111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Fekete M., Szarvas Z., Fazekas-Pongor V., Feher A., Csipo T., Forrai J., Dosa N., Peterfi A., Lehoczki A., Tarantini S. Nutrition strategies promoting healthy aging: From improvement of cardiovascular and brain health to prevention of age-associated diseases. Nutrients. 2022;15:47. doi: 10.3390/nu15010047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Anjum I., Jaffery S.S., Fayyaz M., Samoo Z., Anjum S. The role of vitamin D in brain health: A mini literature review. Cureus. 2018;10:e2960. doi: 10.7759/cureus.2960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Takács I., Dank M., Majnik J., Nagy G., Szabó A., Szabó B., Szekanecz Z., Sziller I., Toldy E., Tislér A. Magyarországi konszenzusajánlás a D-vitamin szerepéről a betegségek megelőzésében és kezelésében. Orvosi Hetil. 2022;163:575–584. doi: 10.1556/650.2022.32463. [DOI] [PubMed] [Google Scholar]
- 159.Dědečková E., Viták R., Jirásko M., Králová M., Topolčan O., Pecen L., Fürst T., Brož P., Kučera R. Vitamin D3 Supplementation: Comparison of 1000 IU and 2000 IU Dose in Healthy Individuals. Life. 2023;13:808. doi: 10.3390/life13030808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kennel K.A., Drake M.T., Hurley D.L. Vitamin D deficiency in adults: When to test and how to treat. Mayo Clin. Proc. 2010;85:752–758. doi: 10.4065/mcp.2010.0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Dominguez L.J., Farruggia M., Veronese N., Barbagallo M. Vitamin D sources, metabolism, and deficiency: Available compounds and guidelines for its treatment. Metabolites. 2021;11:255. doi: 10.3390/metabo11040255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Wang W., Li Y., Meng X. Vitamin D and neurodegenerative diseases. Heliyon. 2023;9:e12877. doi: 10.1016/j.heliyon.2023.e12877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Berridge M.J. Vitamin D cell signalling in health and disease. Biochem. Biophys. Res. Commun. 2015;460:53–71. doi: 10.1016/j.bbrc.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 164.Littlejohns T.J., Henley W.E., Lang I.A., Annweiler C., Beauchet O., Chaves P.H., Fried L., Kestenbaum B.R., Kuller L.H., Langa K.M. Vitamin D and the risk of dementia and Alzheimer disease. Neurology. 2014;83:920–928. doi: 10.1212/WNL.0000000000000755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Mayne P.E., Burne T.H. Vitamin D in synaptic plasticity, cognitive function, and neuropsychiatric illness. Trends Neurosci. 2019;42:293–306. doi: 10.1016/j.tins.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 166.Roy N.M., Al-Harthi L., Sampat N., Al-Mujaini R., Mahadevan S., Al Adawi S., Essa M.M., Al Subhi L., Al-Balushi B., Qoronfleh M.W. Impact of vitamin D on neurocognitive function in dementia, depression, schizophrenia and ADHD. Front. Biosci.-Landmark. 2020;26:566–611. doi: 10.2741/4908. [DOI] [PubMed] [Google Scholar]
- 167.Shea M.K., Barger K., Dawson-Hughes B., Leurgans S.E., Fu X., James B.D., Holland T.M., Agarwal P., Wang J., Matuszek G. Brain vitamin D forms, cognitive decline, and neuropathology in community-dwelling older adults. Alzheimer’s Dement. 2023;19:2389–2396. doi: 10.1002/alz.12836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Maharjan R., Diaz Bustamante L., Ghattas K.N., Ilyas S., Al-Refai R., Khan S. Role of Lifestyle in Neuroplasticity and Neurogenesis in an Aging Brain. Cureus. 2020;12:e10639. doi: 10.7759/cureus.10639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.DeLuca G., Kimball S., Kolasinski J., Ramagopalan S., Ebers G. The role of vitamin D in nervous system health and disease. Neuropathol. Appl. Neurobiol. 2013;39:458–484. doi: 10.1111/nan.12020. [DOI] [PubMed] [Google Scholar]
- 170.National Institutes of Heath Office of Dietary Supplements Vitamin K Fact Sheet for Health Professionals. [(accessed on 14 November 2023)];2018 Available online: https://ods.od.nih.gov/factsheets/VitaminK-HealthProfessional/
- 171.Mladěnka P., Macáková K., Kujovská Krčmová L., Javorská L., Mrštná K., Carazo A., Protti M., Remião F., Nováková L., Researchers O., et al. Vitamin K–sources, physiological role, kinetics, deficiency, detection, therapeutic use, and toxicity. Nutr. Rev. 2022;80:677–698. doi: 10.1093/nutrit/nuab061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Huang S.-H., Fang S.-T., Chen Y.-C. Molecular mechanism of vitamin K2 protection against amyloid-β-induced cytotoxicity. Biomolecules. 2021;11:423. doi: 10.3390/biom11030423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Presse N., Belleville S., Gaudreau P., Greenwood C.E., Kergoat M.J., Morais J.A., Payette H., Shatenstein B., Ferland G. Vitamin K status and cognitive function in healthy older adults. Neurobiol. Aging. 2013;34:2777–2783. doi: 10.1016/j.neurobiolaging.2013.05.031. [DOI] [PubMed] [Google Scholar]
- 174.Chouet J., Ferland G., Féart C., Rolland Y., Presse N., Boucher K., Barberger-Gateau P., Beauchet O., Annweiler C. Dietary Vitamin K Intake Is Associated with Cognition and Behaviour among Geriatric Patients: The CLIP Study. Nutrients. 2015;7:6739–6750. doi: 10.3390/nu7085306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Popescu A., German M. Vitamin K2 Holds Promise for Alzheimer’s Prevention and Treatment. Nutrients. 2021;13:2206. doi: 10.3390/nu13072206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.DiNicolantonio J.J., O’Keefe J.H. The Importance of Marine Omega-3s for Brain Development and the Prevention and Treatment of Behavior, Mood, and Other Brain Disorders. Nutrients. 2020;12:2333. doi: 10.3390/nu12082333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Glück T., Alter P. Marine omega-3 highly unsaturated fatty acids: From mechanisms to clinical implications in heart failure and arrhythmias. Vasc. Pharmacol. 2016;82:11–19. doi: 10.1016/j.vph.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 178.Djuricic I., Calder P.C. Beneficial Outcomes of Omega-6 and Omega-3 Polyunsaturated Fatty Acids on Human Health: An Update for 2021. Nutrients. 2021;13:2421. doi: 10.3390/nu13072421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Román G.C., Jackson R.E., Gadhia R., Román A.N., Reis J. Mediterranean diet: The role of long-chain ω-3 fatty acids in fish; polyphenols in fruits, vegetables, cereals, coffee, tea, cacao and wine; probiotics and vitamins in prevention of stroke, age-related cognitive decline, and Alzheimer disease. Rev. Neurol. 2019;175:724–741. doi: 10.1016/j.neurol.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 180.Derbyshire E. Brain Health across the Lifespan: A Systematic Review on the Role of Omega-3 Fatty Acid Supplements. Nutrients. 2018;10:1094. doi: 10.3390/nu10081094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Fekete M., Szőllősi G., Németh A.N., Varga J.T. Clinical value of omega-3 polyunsaturated fatty acid supplementation in chronic obstructive pulmonary disease. Orvosi Hetil. 2021;162:23–30. doi: 10.1556/650.2021.31973. [DOI] [PubMed] [Google Scholar]
- 182.Witte A.V., Kerti L., Hermannstädter H.M., Fiebach J.B., Schreiber S.J., Schuchardt J.P., Hahn A., Flöel A. Long-chain omega-3 fatty acids improve brain function and structure in older adults. Cereb. Cortex. 2014;24:3059–3068. doi: 10.1093/cercor/bht163. [DOI] [PubMed] [Google Scholar]
- 183.Fekete M., Csípő T., Fazekas-Pongor V., Bálint M., Csizmadia Z., Tarantini S., Varga J.T. The Possible Role of Food and Diet in the Quality of Life in Patients with COPD-A State-of-the-Art Review. Nutrients. 2023;15:3902. doi: 10.3390/nu15183902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Marton J., Farkas G., Takacs T., Nagy Z., Szasz Z., Varga J., Jarmay K., Balogh A., Lonovics J. Beneficial effects of pentoxifylline treatment of experimental acute pancreatitis in rats. Res. Exp. Med. 1997;197:293–299. doi: 10.1007/s004330050078. [DOI] [PubMed] [Google Scholar]
- 185.Márton J., Farkas G., Nagy Z., Takacs T., Varga J., Szasz Z., Balogh A., Lonovics J. Plasma levels of TNF and IL-6 following induction of acute pancreatitis and pentoxifylline treatment in rats. Acta Chir. Hung. 1997;36:223–225. [PubMed] [Google Scholar]
- 186.Su K.P., Tseng P.T., Lin P.Y., Okubo R., Chen T.Y., Chen Y.W., Matsuoka Y.J. Association of Use of Omega-3 Polyunsaturated Fatty Acids With Changes in Severity of Anxiety Symptoms: A Systematic Review and Meta-analysis. JAMA Netw. Open. 2018;1:e182327. doi: 10.1001/jamanetworkopen.2018.2327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Simopoulos A.P. Evolutionary aspects of diet, the omega-6/omega-3 ratio and genetic variation: Nutritional implications for chronic diseases. Biomed. Pharmacother. 2006;60:502–507. doi: 10.1016/j.biopha.2006.07.080. [DOI] [PubMed] [Google Scholar]
- 188.Simopoulos A.P. The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomed. Pharmacother. 2002;56:365–379. doi: 10.1016/S0753-3322(02)00253-6. [DOI] [PubMed] [Google Scholar]
- 189.Avallone R., Vitale G., Bertolotti M. Omega-3 Fatty Acids and Neurodegenerative Diseases: New Evidence in Clinical Trials. Int. J. Mol. Sci. 2019;20:4256. doi: 10.3390/ijms20174256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Grosso G., Galvano F., Marventano S., Malaguarnera M., Bucolo C., Drago F., Caraci F. Omega-3 fatty acids and depression: Scientific evidence and biological mechanisms. Oxidative Med. Cell. Longev. 2014;2014:313570. doi: 10.1155/2014/313570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Ross B.M., Seguin J., Sieswerda L.E. Omega-3 fatty acids as treatments for mental illness: Which disorder and which fatty acid? Lipids Health Dis. 2007;6:21. doi: 10.1186/1476-511X-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Hodge W., Barnes D., Schachter H.M., Pan Y., Lowcock E.C., Zhang L., Sampson M., Morrison A., Tran K., Miguelez M., et al. Effects of omega-3 fatty acids on eye health. Evid. Rep. Technol. Assess. (Summ.) 2005:1–6. [PMC free article] [PubMed] [Google Scholar]
- 193.Orchard T.S., Pan X., Cheek F., Ing S.W., Jackson R.D. A systematic review of omega-3 fatty acids and osteoporosis. Br. J. Nutr. 2012;107:S253–S260. doi: 10.1017/S0007114512001638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Sharma T., Mandal C.C. Omega-3 fatty acids in pathological calcification and bone health. J. Food Biochem. 2020;44:e13333. doi: 10.1111/jfbc.13333. [DOI] [PubMed] [Google Scholar]
- 195.Hathcock J. Vitamins and minerals: Efficacy and safety. Am. J. Clin. Nutr. 1997;66:427–437. doi: 10.1093/ajcn/66.2.427. [DOI] [PubMed] [Google Scholar]
- 196.Klimova B., Dziuba S., Cierniak-Emerych A. The effect of healthy diet on cognitive performance among healthy seniors—A mini review. Front. Hum. Neurosci. 2020;14:325. doi: 10.3389/fnhum.2020.00325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Alateeq K., Walsh E.I., Cherbuin N. Dietary magnesium intake is related to larger brain volumes and lower white matter lesions with notable sex differences. Eur. J. Nutr. 2023;62:2039–2051. doi: 10.1007/s00394-023-03123-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Ozawa M., Ninomiya T., Ohara T., Hirakawa Y., Doi Y., Hata J., Uchida K., Shirota T., Kitazono T., Kiyohara Y. Self-Reported Dietary Intake of Potassium, Calcium, and Magnesium and Risk of Dementia in the J apanese: The H isayama Study. J. Am. Geriatr. Soc. 2012;60:1515–1520. doi: 10.1111/j.1532-5415.2012.04061.x. [DOI] [PubMed] [Google Scholar]
- 199.Abbaspour N., Hurrell R., Kelishadi R. Review on iron and its importance for human health. J. Res. Med. Sci. Off. J. Isfahan Univ. Med. Sci. 2014;19:164. [PMC free article] [PubMed] [Google Scholar]
- 200.East P., Doom J.R., Blanco E., Burrows R., Lozoff B., Gahagan S. Iron deficiency in infancy and neurocognitive and educational outcomes in young adulthood. Dev. Psychol. 2021;57:962. doi: 10.1037/dev0001030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Chen Z., Yang H., Wang D., Sudfeld C.R., Zhao A., Xin Y., Chen J.C., Fawzi W.W., Xing Y., Li Z. Effect of Oral Iron Supplementation on Cognitive Function among Children and Adolescents in Low-and Middle-Income Countries: A Systematic Review and Meta-Analysis. Nutrients. 2022;14:5332. doi: 10.3390/nu14245332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Schieffer K.M., Chuang C.H., Connor J., Pawelczyk J.A., Sekhar D.L. Iron deficiency anemia is associated with hearing loss in the adult population. JAMA Otolaryngol. Head. Neck Surg. 2017;143:350. doi: 10.1001/jamaoto.2016.3631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Wolters F.J., Zonneveld H.I., Licher S., Cremers L.G., Ikram M.K., Koudstaal P.J., Vernooij M.W., Ikram M.A., Group H.B.C.C.R. Hemoglobin and anemia in relation to dementia risk and accompanying changes on brain MRI. Neurology. 2019;93:e917–e926. doi: 10.1212/WNL.0000000000008003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Hong C.H., Falvey C., Harris T.B., Simonsick E.M., Satterfield S., Ferrucci L., Metti A.L., Patel K.V., Yaffe K. Anemia and risk of dementia in older adults: Findings from the Health ABC study. Neurology. 2013;81:528–533. doi: 10.1212/WNL.0b013e31829e701d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Huang Z., Rose A.H., Hoffmann P.R. The role of selenium in inflammation and immunity: From molecular mechanisms to therapeutic opportunities. Antioxid. Redox Signal. 2012;16:705–743. doi: 10.1089/ars.2011.4145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Olufunmilayo E.O., Gerke-Duncan M.B., Holsinger R.D. Oxidative Stress and Antioxidants in Neurodegenerative disorders. Antioxidants. 2023;12:517. doi: 10.3390/antiox12020517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Cardoso B.R., Ong T.P., Jacob-Filho W., Jaluul O., Freitas M.I.d.Á., Cozzolino S.M.F. Nutritional status of selenium in Alzheimer’s disease patients. Br. J. Nutr. 2010;103:803–806. doi: 10.1017/S0007114509992832. [DOI] [PubMed] [Google Scholar]
- 208.Zhou J., Zhang W., Cao Z., Lian S., Li J., Nie J., Huang Y., Zhao K., He J., Liu C. Association of Selenium Levels with Neurodegenerative Disease: A Systemic Review and Meta-Analysis. Nutrients. 2023;15:3706. doi: 10.3390/nu15173706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Feng Y., Wang X. Antioxidant therapies for Alzheimer’s disease. Oxidative Med. Cell. Longev. 2012;2012:472932. doi: 10.1155/2012/472932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Zuo Y., Li Y., Gu X., Lei Z. The correlation between selenium levels and autoimmune thyroid disease: A systematic review and meta-analysis. Ann. Palliat. Med. 2021;10:4398–4408. doi: 10.21037/apm-21-449. [DOI] [PubMed] [Google Scholar]
- 211.Cai X., Wang C., Yu W., Fan W., Wang S., Shen N., Wu P., Li X., Wang F. Selenium exposure and cancer risk: An updated meta-analysis and meta-regression. Sci. Rep. 2016;6:19213. doi: 10.1038/srep19213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Peters U., Takata Y. Selenium and the prevention of prostate and colorectal cancer. Mol. Nutr. Food Res. 2008;52:1261–1272. doi: 10.1002/mnfr.200800103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Vega-Cabello V., Caballero F.F., Lana A., Arias-Fernandez L., Banegas J.R., Rodriguez-Artalejo F., Lopez-Garcia E., Struijk E.A. Association of Zinc Intake With Risk of Impaired Physical Function and Frailty Among Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2022;77:2015–2022. doi: 10.1093/gerona/glac014. [DOI] [PubMed] [Google Scholar]
- 214.Ranjbar E., Shams J., Sabetkasaei M., M-Shirazi M., Rashidkhani B., Mostafavi A., Bornak E., Nasrollahzadeh J. Effects of zinc supplementation on efficacy of antidepressant therapy, inflammatory cytokines, and brain-derived neurotrophic factor in patients with major depression. Nutr. Neurosci. 2014;17:65–71. doi: 10.1179/1476830513Y.0000000066. [DOI] [PubMed] [Google Scholar]
- 215.Szewczyk B. Zinc homeostasis and neurodegenerative disorders. Front. Aging Neurosci. 2013;5:33. doi: 10.3389/fnagi.2013.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Mondola P., Damiano S., Sasso A., Santillo M. The Cu, Zn superoxide dismutase: Not only a dismutase enzyme. Front. Physiol. 2016;7:594. doi: 10.3389/fphys.2016.00594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Pal A., Cerchiaro G., Rani I., Ventriglia M., Rongioletti M., Longobardi A., Squitti R. Iron in Alzheimer’s Disease: From Physiology to Disease Disabilities. Biomolecules. 2022;12:1248. doi: 10.3390/biom12091248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Wang L., Yin Y.-L., Liu X.-Z., Shen P., Zheng Y.-G., Lan X.-R., Lu C.-B., Wang J.-Z. Current understanding of metal ions in the pathogenesis of Alzheimer’s disease. Transl. Neurodegener. 2020;9:1–13. doi: 10.1186/s40035-020-00189-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Kitala K., Tanski D., Godlewski J., Krajewska-Włodarczyk M., Gromadziński L., Majewski M. Copper and Zinc Particles as Regulators of Cardiovascular System Function—A Review. Nutrients. 2023;15:3040. doi: 10.3390/nu15133040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Gunturu S., Dharmarajan T. Copper and zinc. Geriatr. Gastroenterol. 2020:1–17. doi: 10.1007/978-3-319-90761-1_25-1. [DOI] [Google Scholar]
- 221.Bagheri S., Squitti R., Haertlé T., Siotto M., Saboury A.A. Role of copper in the onset of Alzheimer’s disease compared to other metals. Front. Aging Neurosci. 2018;9:446. doi: 10.3389/fnagi.2017.00446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Varga J., Porszasz J., Boda K., Casaburi R., Somfay A. Felügyelt magas intenzitású folyamatos és intervallum, valamint otthoni tréning hatásának vizsgálata krónikus obstruktív tüdőbetegek rehabilitációjában. Med. Thor. 2008;61:135–143. [Google Scholar]
- 223.Pettersson H., Alexanderson H., Poole J.L., Varga J., Regardt M., Russell A.-M., Salam Y., Jensen K., Mansour J., Frech T. Exercise as a multi-modal disease-modifying medicine in systemic sclerosis: An introduction by The Global Fellowship on Rehabilitation and Exercise in Systemic Sclerosis (G-FoRSS) Best Pract. Res. Clin. Rheumatol. 2021;35:101695. doi: 10.1016/j.berh.2021.101695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Csizmadia Z., Ács P., Szőllősi G.J., Tóth B., Kerti M., Kovács A., Varga J.T. Freedive Training Gives Additional Physiological Effect Compared to Pulmonary Rehabilitation in COPD. Int. J. Environ. Res. Public Health. 2022;19:1549. doi: 10.3390/ijerph191811549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Gy B.N., Balikó Z., Kovács G. Egészségügyi szakmai irányelv a krónikus obstruktív tüdőbetegség (COPD) diagnosztikájáról és kezeléséről, az alap, a szak és a sürgősségi ellátás területén. Med. Thor. 2014;67:76112. [Google Scholar]
- 226.Shlisky J., Bloom D.E., Beaudreault A.R., Tucker K.L., Keller H.H., Freund-Levi Y., Fielding R.A., Cheng F.W., Jensen G.L., Wu D. Nutritional considerations for healthy aging and reduction in age-related chronic disease. Adv. Nutr. 2017;8:17–26. doi: 10.3945/an.116.013474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Varga J., Boda K., Somfay A. The effect of controlled and uncontrolled dynamic lower extremity training in the rehabilitation of patients with chronic obstructive pulmonary disease. Orvosi Hetil. 2005;146:2249–2255. [PubMed] [Google Scholar]
- 228.Eastman J., Bahorik A., Kornblith E., Xia F., Yaffe K. Sex Differences in the Risk of Dementia in Older Veterans. J. Gerontol. A Biol. Sci. Med. Sci. 2022;77:1250–1253. doi: 10.1093/gerona/glac029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Crimmins E.M., Thyagarajan B., Kim J.K., Weir D., Faul J. Quest for a summary measure of biological age: The health and retirement study. Geroscience. 2021;43:395–408. doi: 10.1007/s11357-021-00325-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Vaccarino V., Huang M., Wang Z., Hui Q., Shah A.J., Goldberg J., Smith N., Kaseer B., Murrah N., Levantsevych O.M., et al. Epigenetic Age Acceleration and Cognitive Decline: A Twin Study. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:1854–1863. doi: 10.1093/gerona/glab047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Vetter V.M., Sommerer Y., Kalies C.H., Spira D., Bertram L., Demuth I. Vitamin D supplementation is associated with slower epigenetic aging. Geroscience. 2022;44:1847–1859. doi: 10.1007/s11357-022-00581-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Syed M.A., Aiyegbusi O.L., Marston E., Lord J.M., Teare H., Calvert M. Optimising the selection of outcomes for healthy ageing trials: A mixed methods study. Geroscience. 2022;44:2585–2609. doi: 10.1007/s11357-022-00690-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Cummings S.R., Kritchevsky S.B. Endpoints for geroscience clinical trials: Health outcomes, biomarkers, and biologic age. Geroscience. 2022;44:2925–2931. doi: 10.1007/s11357-022-00671-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Amgalan A., Maher A.S., Ghosh S., Chui H.C., Bogdan P., Irimia A. Brain age estimation reveals older adults’ accelerated senescence after traumatic brain injury. Geroscience. 2022;44:2509–2525. doi: 10.1007/s11357-022-00597-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Dorhout B.G., Doets E.L., van Dongen E.J.I., de Groot L., Haveman-Nies A. In-Depth Analyses of the Effects of a Diet and Resistance Exercise Intervention in Older Adults: Who Benefits Most From ProMuscle in Practice? J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:2204–2212. doi: 10.1093/gerona/glab104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Lee-Bravatti M.A., O’Neill H.J., Wurth R.C., Sotos-Prieto M., Gao X., Falcon L.M., Tucker K.L., Mattei J. Lifestyle Behavioral Factors and Integrative Successful Aging Among Puerto Ricans Living in the Mainland United States. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:1108–1116. doi: 10.1093/gerona/glaa259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Zhou Y.F., Song X.Y., Pan X.F., Feng L., Luo N., Yuan J.M., Pan A., Koh W.P. Association Between Combined Lifestyle Factors and Healthy Ageing in Chinese Adults: The Singapore Chinese Health Study. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:1796–1805. doi: 10.1093/gerona/glab033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Boumenna T., Scott T.M., Lee J.S., Zhang X., Kriebel D., Tucker K.L., Palacios N. MIND Diet and Cognitive Function in Puerto Rican Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2022;77:605–613. doi: 10.1093/gerona/glab261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Maroto-Rodriguez J., Delgado-Velandia M., Ortola R., Garcia-Esquinas E., Martinez-Gomez D., Struijk E.A., Lopez-Garcia E., Rodriguez-Artalejo F., Sotos-Prieto M. A Mediterranean Lifestyle and Frailty Incidence in Older Adults: The Seniors-ENRICA-1 Cohort. J. Gerontol. A Biol. Sci. Med. Sci. 2022;77:1845–1852. doi: 10.1093/gerona/glab292. [DOI] [PubMed] [Google Scholar]
- 240.Merono T., Zamora-Ros R., Hidalgo-Liberona N., Rabassa M., Bandinelli S., Ferrucci L., Fedecostante M., Cherubini A., Andres-Lacueva C. Animal Protein Intake Is Inversely Associated With Mortality in Older Adults: The InCHIANTI Study. J. Gerontol. A Biol. Sci. Med. Sci. 2022;77:1866–1872. doi: 10.1093/gerona/glab334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Ortola R., Garcia-Esquinas E., Sotos-Prieto M., Struijk E.A., Caballero F.F., Lopez-Garcia E., Rodriguez-Artalejo F. Mediterranean Diet and Changes in Frequency, Severity, and Localization of Pain in Older Adults: The Seniors-ENRICA Cohorts. J. Gerontol. A Biol. Sci. Med. Sci. 2022;77:122–130. doi: 10.1093/gerona/glab109. [DOI] [PubMed] [Google Scholar]
- 242.Palta P., Griswold M., Ranadive R., Bandeen-Roche K., Folsom A.R., Petruski-Ivleva N., Burgard S., Kucharska-Newton A., Windham B.G. Midlife Cardiovascular Health and Robust Versus Frail Late-Life Status: The Atherosclerosis Risk in Communities Study. J. Gerontol. A Biol. Sci. Med. Sci. 2022;77:1222–1229. doi: 10.1093/gerona/glab310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Sheng L.T., Jiang Y.W., Feng L., Pan A., Koh W.P. Dietary Total Antioxidant Capacity and Late-Life Cognitive Impairment: The Singapore Chinese Health Study. J. Gerontol. A Biol. Sci. Med. Sci. 2022;77:561–569. doi: 10.1093/gerona/glab100. [DOI] [PubMed] [Google Scholar]
- 244.Jung S.J., Lee G.B., Nishimi K., Chibnik L., Koenen K.C., Kim H.C. Association between psychological resilience and cognitive function in older adults: Effect modification by inflammatory status. Geroscience. 2021;43:2749–2760. doi: 10.1007/s11357-021-00406-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Ungvari Z., Tabák A.G., Adany R., Purebl G., Kaposvári C., Fazekas-Pongor V., Csípő T., Szarvas Z., Horváth K., Mukli P. The Semmelweis Study: A longitudinal occupational cohort study within the framework of the Semmelweis Caring University Model Program for supporting healthy aging. Geroscience. 2023:1–28. doi: 10.1007/s11357-023-01018-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Dobreva I., Marston L., Mukadam N. Which components of the Mediterranean diet are associated with dementia? A UK Biobank cohort study. Geroscience. 2022;44:2541–2554. doi: 10.1007/s11357-022-00615-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Gensous N., Garagnani P., Santoro A., Giuliani C., Ostan R., Fabbri C., Milazzo M., Gentilini D., di Blasio A.M., Pietruszka B., et al. One-year Mediterranean diet promotes epigenetic rejuvenation with country- and sex-specific effects: A pilot study from the NU-AGE project. Geroscience. 2020;42:687–701. doi: 10.1007/s11357-019-00149-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Madarász B., Fazekas-Pongor V., Szarvas Z., Fekete M., Varga J.T., Tarantini S., Csiszar A., Lionetti V., Tabák A.G., Ungvari Z., et al. Survival and longevity of European rulers: Geographical influences and exploring potential factors, including the Mediterranean diet—A historical analysis from 1354 to the twentieth century. Geroscience. 2023 doi: 10.1007/s11357-023-00957-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Hegedűs B., Varga J., Somfay A. Az interdiszciplináris rehabilitáció hatása spondylitis ankylopoeticában szenvedő betegekben. Orvosi Hetil. 2016;157:1126–1132. doi: 10.1556/650.2016.30472. [DOI] [PubMed] [Google Scholar]
- 250.Varga J.T., Munkácsi A., Máthe C., Somfay A., Bálint B., Lovász O., Várdi K., Pesti A., Koncz M., Szilasi M. A belégző izmok fizikai tréningjének hatása a betegek fizikai állapotára COPD-ben. Med. Thorac. 2018;71:96–102. [Google Scholar]
- 251.Vágvölgyi A., Rozgonyi Z., Vadász P., Varga J.T. A mellkassebészeti műtéti teherbíró képesség megítélése, perioperatív légzésrehabilitáció. Orvosi Hetil. 2017;158:1989–1997. doi: 10.1556/650.2017.30862. [DOI] [PubMed] [Google Scholar]
- 252.Varga J. A légzésrehabiliáció elméleti és gyakorlati lapjai. Ellátási Színterei. Korányi Bull. 2016;1:44–47. [Google Scholar]
- 253.Kraal A.Z., Dotterer H.L., Sharifian N., Morris E.P., Sol K., Zaheed A.B., Smith J., Zahodne L.B. Physical Activity in Early- and Mid-Adulthood Are Independently Associated With Longitudinal Memory Trajectories in Later Life. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:1495–1503. doi: 10.1093/gerona/glaa252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Yoneda T., Lewis N.A., Knight J.E., Rush J., Vendittelli R., Kleineidam L., Hyun J., Piccinin A.M., Hofer S.M., Hoogendijk E.O., et al. The Importance of Engaging in Physical Activity in Older Adulthood for Transitions Between Cognitive Status Categories and Death: A Coordinated Analysis of 14 Longitudinal Studies. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:1661–1667. doi: 10.1093/gerona/glaa268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Zabetian-Targhi F., Srikanth V.K., Beare R., Breslin M., Moran C., Wang W., Wu F., Smith K.J., Callisaya M.L. The Association Between Physical Activity Intensity, Cognition, and Brain Structure in People With Type 2 Diabetes. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:2047–2053. doi: 10.1093/gerona/glab067. [DOI] [PubMed] [Google Scholar]
- 256.Varga J., Palinkas A., Lajko I., Horváth I., Boda K., Somfay A. Pulmonary arterial pressure response during exercise in COPD: A correlation with C-reactive protein (hsCRP) Open Respir. Med. J. 2016;10:1. doi: 10.2174/1874306401610010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Hardcastle C., Hausman H.K., Kraft J.N., Albizu A., O’Shea A., Boutzoukas E.M., Evangelista N.D., Langer K., Van Etten E.J., Bharadwaj P.K., et al. Proximal improvement and higher-order resting state network change after multidomain cognitive training intervention in healthy older adults. Geroscience. 2022;44:1011–1027. doi: 10.1007/s11357-022-00535-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Baciu M., Banjac S., Roger E., Haldin C., Perrone-Bertolotti M., Loevenbruck H., Demonet J.F. Strategies and cognitive reserve to preserve lexical production in aging. Geroscience. 2021;43:1725–1765. doi: 10.1007/s11357-021-00367-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Mahalakshmi A.M., Ray B., Tuladhar S., Bhat A., Bishir M., Bolla S.R., Yang J., Essa M.M., Chidambaram S.B., Guillemin G.J., et al. Sleep, brain vascular health and ageing. Geroscience. 2020;42:1257–1283. doi: 10.1007/s11357-020-00235-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Gosalia J., Montgomery P.S., Zhang S., Pomilla W.A., Wang M., Liang M., Csiszar A., Ungvari Z., Yabluchanskiy A., Proctor D.N., et al. Increased pulse wave velocity is related to impaired working memory and executive function in older adults with metabolic syndrome. Geroscience. 2022;44:2831–2844. doi: 10.1007/s11357-022-00640-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Aliberti M.J.R., Szlejf C., Lima-Costa M.F., de Andrade F.B., Alexandre T.S., Ferri C.P., Suemoto C.K. Frailty Modifies the Association of Hypertension With Cognition in Older Adults: Evidence From the ELSI-Brazil. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:1134–1143. doi: 10.1093/gerona/glaa303. [DOI] [PubMed] [Google Scholar]
- 262.Lennon M.J., Lam B.C.P., Crawford J., Brodaty H., Kochan N.A., Trollor J.N., Numbers K., Draper B., Thalamuthu A., Sachdev P.S. Does Antihypertensive Use Moderate the Effect of Blood Pressure on Cognitive Decline in Older People? J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:859–866. doi: 10.1093/gerona/glaa232. [DOI] [PubMed] [Google Scholar]
- 263.Li F.R., Yang H.L., Zhou R., Zheng J.Z., Chen G.C., Wu X.X., Zou M.C., Wang J.Y., Fu Q., Wu X.B. Influence of Diabetes Duration and Glycemic Control on Dementia: A Cohort Study. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:2062–2070. doi: 10.1093/gerona/glab221. [DOI] [PubMed] [Google Scholar]
- 264.Marseglia A., Darin-Mattsson A., Skoog J., Ryden L., Hadarsson-Bodin T., Kern S., Rydberg Sterner T., Shang Y., Zettergren A., Westman E., et al. Metabolic Syndrome Is Associated With Poor Cognition: A Population-Based Study of 70-Year-Old Adults Without Dementia. J. Gerontol. A Biol. Sci. Med. Sci. 2021;76:2275–2283. doi: 10.1093/gerona/glab195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Davidson K.T., Zhu Z., Balabanov D., Zhao L., Wakefield M.R., Bai Q., Fang Y. Beyond conventional medicine-a look at blueberry, a cancer-fighting superfruit. Pathol. Oncol. Res. 2018;24:733–738. doi: 10.1007/s12253-017-0376-2. [DOI] [PubMed] [Google Scholar]
- 266.Nicolson G.L. Lipid replacement/antioxidant therapy as an adjunct supplement to reduce the adverse effects of cancer therapy and restore mitochondrial function. Pathol. Oncol. Res. 2005;11:139–144. doi: 10.1007/BF02893390. [DOI] [PubMed] [Google Scholar]
- 267.Rusz O., Kahán Z. Bone homeostasis and breast cancer: Implications for complex therapy and the maintenance of bone integrity. Pathol. Oncol. Res. 2013;19:1–10. doi: 10.1007/s12253-012-9586-9. [DOI] [PubMed] [Google Scholar]
- 268.Farkas Á., Szipőcs A., Horváth A., Horváth I., Gálffy G., Varga J., Galambos K., Kugler S., Nagy A., Szalai Z. Establishment of relationships between native and inhalation device specific spirometric parameters as a step towards patient tailored inhalation device selection. Respir. Med. 2019;154:133–140. doi: 10.1016/j.rmed.2019.06.021. [DOI] [PubMed] [Google Scholar]
- 269.Zamanzadeh V., Jasemi M., Valizadeh L., Keogh B., Taleghani F. Effective factors in providing holistic care: A qualitative study. Indian. J. Palliat. Care. 2015;21:214. doi: 10.4103/0973-1075.156506. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.