Abstract
Introduction
The prevalence of type 2 diabetes (T2D) is increasing in the Latinx community. Despite telehealth and technology becoming more available, these resources are not reaching the Latinx population. Diabetes education is a cornerstone of treatment; however, access to culturally tailored content is a barrier to the Latinx population. Real-time continuous glucose monitoring (RT-CGM) is a patient-empowering tool that can improve glycaemic control, but it is not readily available for Latinx patients with T2D. We aim to evaluate a culturally tailored diabetes self-management education and support (DSMES) curriculum, using a team-based approach to improve glycaemic control, promote healthy behaviours and enhance patient access with the use of telehealth in Latinx individuals. The primary aim of the study is to evaluate the additive effectiveness of RT-CGM on glycaemia and behavioural changes among Latinx patients undergoing a culturally tailored DSMES. A sub aim of the study is to evaluate family members’ change in behaviours.
Methods
We propose a randomised controlled trial of blinded versus RT-CGM with 100 Latinx participants with T2D who will receive DSMES via telemedicine over 12 weeks (n=50 per group). The study will be conducted at a single large federally qualified health centre system. The control group will receive culturally tailored DSMES and blinded CGM. The intervention group will receive DSMES and RT-CGM. The DSMES is conducted by community health educators weekly over 12 weeks in Spanish or English, based on participant’s language preference. Patients in the RT-CGM group will have cyclical use with a goal of 50 days wear time. The primary outcomes are changes in haemoglobin A1c and CGM-derived metrics at 3 and 6 months. The secondary outcomes include participants’ self-management knowledge and behaviour and household members’ change in lifestyle.
Ethics and dissemination
The study proposal was approved by the University of Washington ethics/institutional review board (IRB) Committee as minimal risk (IRB ID: STUDY00014396) and the Sea Mar IRB committee.
Trial registration number
ClinicalTrials.gov identifier: NCT05394844
Keywords: DIABETES & ENDOCRINOLOGY, GENERAL MEDICINE (see Internal Medicine), Health Equity
Strengths and limitations of this study.
Training in digital literacy is an integral part of the study.
Culturally tailored diabetes self-management education and support (DSMES) is delivered through a telehealth platform to increase geographical outreach.
All curriculum and behaviour modification surveys are available in both English and Spanish.
This randomised controlled trial maybe underpowered if retention is less than expected.
Behaviour modification of participants’ household members after DSMES with and without real-time continuous glucose monitoring with no direct intervention targeting household members is also evaluated.
Introduction
The prevalence of diabetes in adults in the USA now exceeds 14%, with type 2 diabetes (T2D) accounting for 90–95% of all cases.1 Diabetes incurs healthcare costs of over US$200 billion annually in the USA alone2 and is the leading cause of blindness, chronic kidney disease, heart disease and amputations.3 The Latinx population is disproportionately affected by T2D, with a prevalence that is 80% higher than in non-Latinx whites.4 Latinx individuals with T2D experience higher rates of diabetes-related complications including retinopathy and chronic kidney disease.5 Latinx individuals with diabetes also face greater challenges accessing medical care and pharmacotherapies.6 Diabetes education is an integral part of diabetes self-care and empowerment. However, broader implementation of behavioural interventions has been limited to date by (1) lack of data-driven design, (2) inadequate patient access and (3) absence of culturally tailored curricula that are essential for reaching specific populations.7 8 Culturally tailored diabetes self-management education and support (DSMES) curricula are promising, but clinical data on optimal approaches for implementing these programmes are limited, with a particular scarcity of data in Latinx populations.9 10
The DSMES curriculum Compañeros en Salud (Partners in Health)11 is a multicultural and bilingual 12-module programme that was created specifically for Latinx populations to improve diabetes self-management. Compañeros en Salud was first tested in the Latinx population as five 2-hour sessions under the name ‘El Camino a la Salud’ and has been evaluated in two previous studies.12–14 In response to feedback on the initial curriculum, author KS (formerly named Two Feathers) updated the name to Compañeros en Salud in order to highlight the ‘communal’ strength in the Latinx population and changed the delivery to twelve 1-hour sessions in order to increase focus. The 12-session hourly curriculum was first studied in Native Hawaiians and Pacific Islanders15 and then piloted in an English-speaking Latinx population with in-person sessions in Seattle, Washington, USA.16 DSMES is the foundation of diabetes self-management, but additional tools are needed to reinforce behavioural change and to support participants’ self-empowerment. The use of real-time continuous glucose monitoring (RT-CGM) is a highly effective intervention for improving glycaemia in patients with type 1 diabetes,17–20 but its use in patients with T2D is limited, in part due to insurance barriers.21 22 The American Diabetes Association’s (ADA) guidelines highlight the utility of CGM for patients using non-insulin or basal insulin regimens.23 We previously showed that cyclical RT-CGM use over 3 months significantly improved haemoglobin A1c (A1c) in subjects with T2D not using prandial insulin24 and that this improvement was sustained beyond the period of RT-CGM use.25 Other studies using intermittent flash CGM technology and a multicentre CGM intervention in primary care clinics showed similar results.26 27 A key factor behind these benefits may be behaviour modification associated with RT-CGM, however, studies are lacking.28 Despite these benefits, CGM is not readily available to many people living with T2D.21 22 A small, single group pilot study with 15 Latinx adults evaluated the Compañeros en Salud DSMES curriculum and RT-CGM intervention in Seattle, Washington, USA.16 The average baseline A1c of 9.3% improved to a postintervention A1c of 8.5% (p<0.01). Participants lost an average of 5 pounds and there were significant improvements in systolic (p=0.03) and diastolic (p=0.002) blood pressure. Our exploratory data demonstrate both acceptance of and perceived benefit from RT-CGM in Latinx individuals with T2D. Telemedicine29 30 offers a novel strategy for addressing the lack of access to diabetes education, one of the largest barriers to improving diabetes control and a common challenge for the Latinx population.7 8 Telemedicine is often underused in populations such as those that identify as Latinx,31–33 as digital literacy and access to broadband internet are barriers that contribute to health inequalities in this population.
Beyond the impact of direct interventions on study participants, we are interested in the impact on other individuals in the participants’ lives. Spouses and partners of individuals with diabetes are at increased risk for developing T2D.34 35 Children are more likely to develop obesity if they have family members living with this disease36 and have a 20–40% absolute risk for developing diabetes if they have a parent with T2D.37 Diabetes in a family member has been shown to have a higher positive predictive value for developing T2D compared with obesity.38 This elevated risk, particularly in Latinx communities, is thought to result from a combination of genetic and environmental factors including shared nutritional and physical activity behaviours.39 40 Interventions that promote behavioural modification in an individual patient may have the potential to impact other members of the household. Family-based interventions are effective at reducing childhood obesity,41 42 a meta-analysis concluded that parent-only interventions are as effective as parent–child interventions for mitigating childhood obesity.43 Studies have also demonstrated an effect on spouses not participating in the intervention.44–47 This study has an exploratory objective to look at whether this intervention reaches household members in a so called ‘ripple’ effect.
Aims and objectives
The primary aim of this study is to determine the additive effectiveness of RT-CGM among Latinx patients with T2D undergoing culturally tailored DSMES curriculum at improving glycaemic indices (including A1c and CGM outcomes) at 12 and 24 weeks. The secondary objectives are to evaluate changes in blood pressure, lipid profile, waist circumference, medication adherence, lifestyle and diabetes distress changes and social determinants of health. A sub aim of this study is to explore whether a ‘ripple effect’ on nutritional or activity behaviours is observed in household members.
Study design
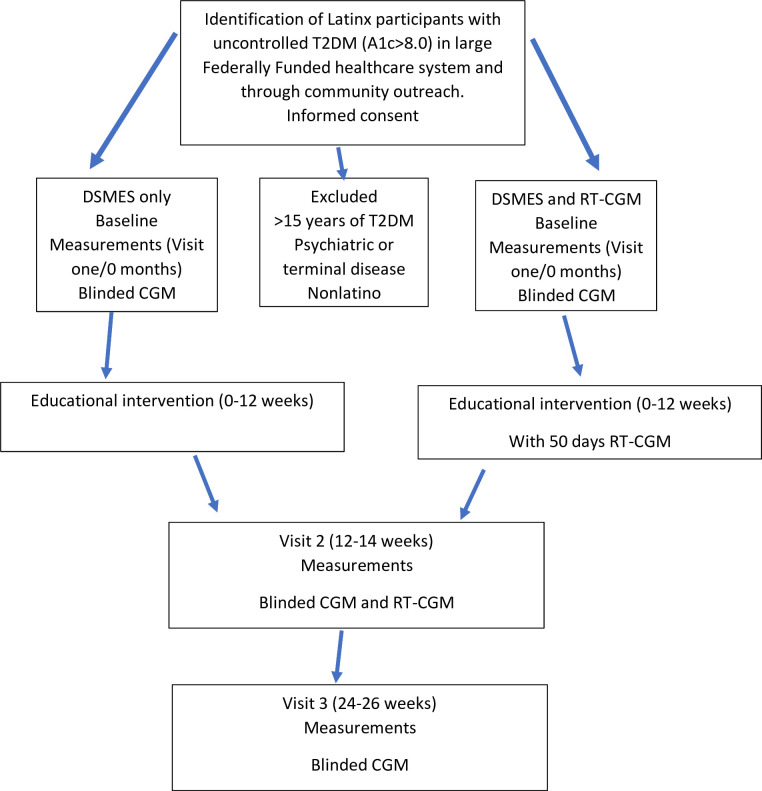
This study is a randomised controlled parallel group trial of DSMES with and without RT-CGM among Latinx patients with a diagnosis of T2D. Intervention assignments were generated (1:1 to either blinded CGM+Education or RT-CGM+Education) using permuted block randomisation with block sizes of 2, 4 or 6. Randomisation was stratified by baseline A1c (<9.0 or ≥9.0) on confirmed eligibility and consent using a REDCap database (Research Electronic Data Capture, Vanderbilt University). An independent study statistician generated the randomisation lists and is unblinded, though has no direct involvement with patients or outcomes assessors. The research coordinator (RC), health educators (HEs), community healthcare worker (CHW) and participants are unblinded to the intervention, but the primary investigator and co-investigators(CO-Is) are blinded to participants and their intervention. Outcome measurements are evaluated at baseline and after 12 and 24 weeks (figure 1).
Figure 1.
Flow chart. DSMES, diabetes self-management education and support; CGM, continuous glucose monitoring; RT-CGM, real-time CGM; T2DM, type 2 diabetes mellitus.
Population
Participants in this study are Latinx patients with T2D who receive care from one large, federally funded healthcare system in the greater Seattle area. Initial review of the six main clinics where potential recruitment occurs showed >450 Latinx patients with A1c>8.0%.
Inclusion and exclusion criteria
The goal is to recruit those that identify as Latinx with poorly controlled T2D (A1c>8.0%). See table 1 for a full list of inclusion and exclusion criteria.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria: | Exclusion criteria: |
| Participants must be 18–60 years old. | Duration of diabetes >15 years. |
| Self-identify as Latinx. | Type 1 diabetes or latent autoimmune diabetes. |
| A clinical diagnosis of T2D within the last 15 years with or without medication use. | Current use of prandial insulin. |
| A1c ≥8.0% at screening. | Any condition that prevents walking at least one city block. |
| Be physically and cognitively able to use the home CGM monitoring device. | History of serious mental illness other than adequately treated depression. |
| Be willing and able to follow all study procedures. | History of bariatric surgery or current participation in a weight management programme. |
| Current diagnosis of cancer or other serious or systemic medical condition or significant active cardiovascular or cerebrovascular disease after review by PI. | |
| Pregnancy. | |
| Known history of hypoglycaemia unawareness. |
A1c, haemoglobin A1c; CGM, continuous glucose monitoring; CO-I, co-investigator; PI, primary investigator; T2D, type 2 diabetes.
Recruitment
Patients are identified both by review of the most recent A1c documented in the electronic medical record and by screening clinicians’ and HEs office visit schedules in search of patients with a diagnosis of T2D. Additionally, flyers distributed in the community at places of worship, Young Men’s Christian Association facilities and other local community areas serve to further enhance community engagement. Participants are asked whether we may contact household members >8 years old to participate in two to three short surveys. Recruitment is quarterly and begins 1 month prior to each 12-week educational cycle. A total of four to six DSMES cycles are needed to reach 100 active participants, defined as those that complete at least one educational session.
Sample size estimation
We will enrol up to 130 participants to obtain a total of n=100 study participants who complete at least one educational session. The study is designed and sized first for assessing the change in A1c from baseline to 12 weeks among all study participants and secondarily to assess the impact of RT-CGM. To assess statistical power, we assume a SD in baseline A1c of 1.2 and a reduced SD of 1.0 at 12 weeks to reflect an anticipated reduction in A1c due to the Compañeros en Salud curriculum. We further assume a correlation in A1c measurements of r=0.5, which is likely to be higher, resulting in greater statistical power. Finally, assuming a 15% reduction in the effect sample size (n=85) due to attrition, the study is sized to detect reductions in A1c of 0.4% or larger with 90% statistical power. If the actual correlation between baseline and week 12 A1c measurements is r=0.7 or higher, the study has 90% power to detect differences in A1c as small as 0.3%. Under similar assumptions, the study is sized to detect a 0.6% difference in 12-week A1c between subjects randomised to RT-CGM versus blinded CGM (power=0.82 assuming r=0.5; power=0.93 assuming r=0.7). A two-sided type 1 error rate of 0.05 is assumed throughout.
Statistical analysis
The primary endpoint is the change in A1c from baseline to 12±2 weeks (end of the intervention period). Secondary outcomes include between-group differences in change in A1c at 24±2 weeks and changes in body weight, body mass index (BMI) and blood pressure at 12±2 and 24±2 weeks. We will use simple descriptive statistics to quantify between-group differences in changes in CGM indices, including time in range (TIR) mean glucose, mean amplitude of glycaemic excursions (MAGE), times above and below range (TAR and TBR) and coefficient of variation (COV). The primary outcome of A1c will be assessed using a random-intercept random-slope linear mixed effects regression model that adjusts for an indicator of RT-CGM and time (baseline, visit 2 and visit 3) as fixed effects. To assess the effectiveness of the Compañeros en Salud curriculum, inference for Aim 1 will focus on the change in A1c from baseline to 12 weeks for the entire cohort (regardless of RT-CGM status). Main secondary outcome measures will be TIR and mean glucose by CGM. Additional outcomes including BMI, waist circumference and systolic/diastolic blood pressure will be assessed similarly using a generalised linear mixed effects model appropriate for each type of outcome measurement. We will conduct a missing data analysis to describe and characterise enrolled participants who do not provide data due to attrition. Linear mixed effects models naturally handle intermittent missing data through maximum likelihood estimation. As described by Molenberghs and Kenward,48 we will use inverse probability weighting in secondary analysis within each longitudinal regression model to inflate the weights of cases that are under-represented in the analysis due to selective attrition and/or non-participation. We will also conduct sensitivity analyses using 10-fold multiple imputation to assess the robustness of the results when missing data are imputed. The characteristics of non-responders will be summarised in our final report, and we will present the sensitivity of the estimated treatment effect due to alternative missing data methods. The effect of wearing RT-CGM on CGM indices will be assessed using a similar analytical framework as with the analysis of A1c. The linear mixed model coefficient for RT-CGM will be coded to estimate the average difference in 12-week change in outcomes due to receiving real-time glucose data on the outcome of interest. The effectiveness of the Compañeros en Salud curriculum on glycaemic outcomes, sugared beverage intake, steps/day, reported walking and diabetes distress will be assessed both overall and by RT-CGM status, and models will additionally adjust for an indicator of survey language (English vs Spanish). Finally, exploratory outcomes include changes in nutritional behaviours for household members, specifically sugared beverage intake. Secondary outcomes for household members will include perception of benefit for the household member not actively engaged in the intervention or wearing the CGM. The outcomes of household members will be measured and assessed similarly but in separate generalised linear mixed effects models. For participants with involved household members, we will examine the associations of behavioural and dietary outcomes between participants and household members through direct adjustment of participant data in household member outcome models. We will explore temporal associations using time-lagged participant outcomes in the longitudinal model.
Data collection
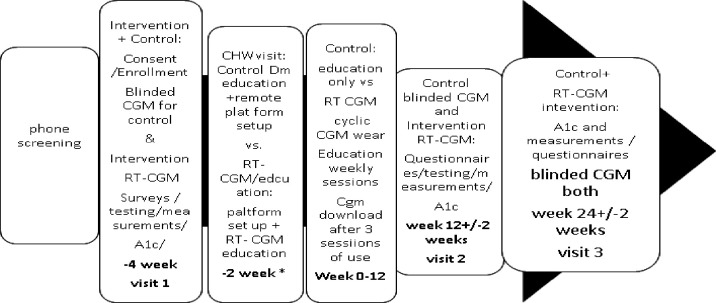
All data will be collected by HEs or CHWs and stored in REDCap (figure 2). CGM data will be reviewed and inputted by a study research coordinator. The following data will be collected from participants, when appropriate, using validated tools at baseline (Visit 1) and after the intervention period (3 months/Visit 2 and 6 months/Visit 3). Participants will be provided with compensation for each visit completed.
Figure 2.
Data collection schematic. DM, diabetes mellitus; CGM, continuous glucose monitoring; RT-CGM, real-time CGM.
Patient demographics
Age, gender, presence of diabetes complications, comorbidities, smoking status, alcohol use, medications, cohabitation, educational level, health insurance status, household income, access to internet and smartphone or personal electronic device will be collected directly from the patient.
Anthropometric, vital sign, laboratory and pedometry measurements
Height will be measured by a stadiometer. Weight will be measured using a digital scale, and BMI (kg/m2) will be calculated. Waist circumference will be measured using a flexible measuring tape. Participants will remain in a seated position for a minimum of 15 min prior to measurement of resting heart rate and blood pressure with an Omron Professional Digital blood pressure and heart rate monitor. Current A1c will be assessed by DCA Vantage Analyzer at all visits. Participants will be given a pedometer or if preferred will use one available on their smartphone. CGM data will be collected for 10 days after the first visit and for the 10 days prior to each of visits 2 and 3.
Glucose/CGM data /evaluation outcome measures
For participants in both the education-only and RT-CGM study arms, the % time the CGM device was worn over each period of use will be captured. Glycaemic outcome measures include TIR, mean glucose, COV, MAGE, % TBR (<70 mg/dL) and % TAR (>180 mg/dL). Between-group comparisons for CGM-derived glycaemic metrics will be assessed based on changes from baseline to study week 12 and baseline to study week 24.
Patient reported outcome measures
Participants will be asked questions about nutrition, physical activity, depression, diabetes distress, self-care, food insecurity and neighbourhood safety. See a full description in table 2.
Table 2.
Weekly education session topics for Compañeros en Salud
| Session | Topic |
| 1 | Glucose balance |
| 2 | Diabetes medication |
| 3 | Food |
| 4 | Diabetes diets |
| 5 | Exercise |
| 6 | Heart |
| 7 | Cholesterol |
| 8 | Feet |
| 9 | Stress |
| 10 | Preventing complications |
| 11 | Diabetes team |
| 12 | Living well with diabetes |
Patient /public involvement
The initial protocol was modelled after a telemedicine Diabetes Prevention Programme completed by our community partner federally qualified health centre during the COVID-19 pandemic. We have completed the first cycle of the education intervention and 15% of first pilot cycle participants (including those who completed at least 50% of the education curriculum plus those who dropped out of the programme) completed detailed interviewing with topics including: perceptions of the educational programme, comfort using telemedicine, barriers to taking care of health/diabetes and participation/engagement in the intervention and suggestions to increase enrolment and to improve cultural tailoring. These interviews will be repeated in cycle two to further adapt/improve the programme. The Washington State Department of Health, the Washington State Health Authority and local Latinx community advocacy programmes have been engaged early to support the programme and to begin discussions about sustainability and replication.
The intervention
The DSMES curriculum
Compañeros en Salud11 entails 12 hour-long weekly educational classes that will be led by certified diabetes educators and HEs. The intervention emphasises ADA clinical goals for blood glucose, A1c, blood pressure and lipids, and is designed to reduce risk factors associated with T2D complications by optimising T2D self-management activities (table 3). Target behaviours include healthy eating, physical activity, blood glucose monitoring, medication adherence, problem-solving, healthy coping, communicating with one’s healthcare team, asking for support from family and friends, taking an active role in individual healthcare and understanding what kind of T2D care is needed. The curriculum is written in a conversational tone in plain language that facilitates learning for participants with little formal education and ensures intervention fidelity. Group discussion, role-playing, problem-solving and hands-on activities are included to encourage engagement and enhance learning. Sociocultural strategies, which present T2D in the context of cultural values and community characteristics, are incorporated to increase the intervention’s salience to participants. For example, a facilitator might begin a class with a story about ordinary community members with T2D, using culturally relevant metaphors to link their situation with effective self-management behaviours.
Table 3.
Patient questionnaires about nutrition, physical activity, social determinants of health and perception of benefit of RT-CGM
| Nutrition | 1. Starting the Conversation is an eight-item, simplified food frequency instrument.52 2. The National Center for Health Statistics,53 six-item short form of the Food Security Survey. |
| Physical activity and neighbourhood safety | 1. The International Physical Activity Questionnaire (short) is a validated questionnaire that reviews the last 7 days of activity.54 2. The Neighbourhood Questionnaire/Neighbourhood Safety55 is a 16-item tool to assess sociability and an individual’s satisfaction with the family’s neighbourhood. It has three subscales, and we will ask the Neighbourhood Safety Subscale (items 1, 6, 10, 11 and 12) as a brief assessment of participants’ ability to safely engage in physical activity in their neighbourhoods 3. International Physical Activity Prevalence Study SELF-ADMINISTERED ENVIRONMENTAL MODULE (PANES):56(questions 2,4,6,9,13,14 and 16 of PANES with be assessed) |
| Behavioural health | 1. Depression symptoms will be assessed with the Patient Health Questionnaire 9.57 2. Diabetes distress will be assessed with The Problem Areas in Diabetes Scale 5.58 3. Self-care and Self-efficacy activities will be assessed with the Summary of Diabetes Self-Care Activities.59 4. Self-Efficacy for Diabetes scale.60 |
| RT-CGM | 1. Modified Harvard Joslin Diabetes Center CGM experiences, opinions, and expectations.61 2. Perception of behaviour change in nutrition and physical activity from RT-CGM use.51 |
| Family member | 1. Less than 13 years old habits questionnaire.62 2. Greater than 13 years old starting the conversation and physical activity questionnaire. 3. Greater than 13 years old perception of CGM use by the family member and behavioural changes made as a result of the family member using CGM. |
RT-CGM, real-time continuous glucose monitoring.
Medical device
CGM (DEXCOM (G6))49: A CGM is a tool that allows measurements of glucose levels in real-time throughout the day and night. A tiny electrode called a glucose sensor is inserted under the skin by a skin prick to measure glucose levels in tissue fluid for 10 days. The RT-CGM-education intervention group will wear the RT-CGM cyclically. The intervention participants will have RT-CGM data downloaded after three cyclic sessions of use and at five sessions of use and wear the CGM blinded at baseline and 24 weeks. The blinded-CGM education group participants will wear the blinded CGM at baseline, at 12 weeks and 24 weeks. CGM Ancillary Devices Dexcom CLARITY is an accessory for users of the Dexcom CGM system and it allows the transfer of glucose data from the CGM system to Dexcom remote servers for data management to allow the use of the CGM data by the user and by study personnel. Additionally, if participants desire, the Dexcom G6 CGM System comes with a built-in Dexcom Share feature allowing up to 10 people to follow a participant’s glucose levels, providing a circle of support. By downloading the Dexcom Follow application, followers can view participant’s glucose data directly from their smart device. For participants who do not have a smartphone, one will be provided to them.
Education and evaluation tools in Spanish
Compañeros en Salud50, CGM Education material and behaviour modification questionnaires for CGM are in Spanish. The culturally tailored English educational materials11 for the Latinx population have been piloted in a small English speaking Latinx population and have been translated to Spanish by the HE, native speaking research personnel and a Latinx physician on the research team who is also a native speaker.50 A questionnaire for perception on how CGM affects/changes lifestyles51 was previously developed and is now also available in Spanish (online supplemental material 1). Finally, an RT-CGM educational handout to explain glucose goals and how food and activity affects blood sugar was developed by an endocrinologist team-member and diabetes educational specialist and is available in both English and Spanish (online supplemental materials 2 and 3).
bmjopen-2023-082005supp001.pdf (19.6KB, pdf)
bmjopen-2023-082005supp002.pdf (28MB, pdf)
bmjopen-2023-082005supp003.pdf (14.7MB, pdf)
The DSMES curriculum with and without RT-CGM is an adjunct to participants’ current diabetes management in their primary care clinic which continues throughout the intervention and encourages engagement with their healthcare provider.
Digital literacy
HE or CWH will engage participants no more than 4 weeks prior to the start of the DSMES intervention to ensure participants have a working technology platform for the education sessions and to provide smartphones with data plans if needed. For all participants, CHWs/HEs will teach simple CGM insertion (blinded and RT). For those who are enrolled in the RT-CGM arm, the CHWs/HEs will set up a mobile application for the RT-CGM device. HEs/CHWs will conduct a single 30-min training session on CGM for participants in the study, with particular focus on the use of RT-CGM as a tool to understand the impact of food and activity choices. The DMSES curriculum Compañeros en Salud will be led by the HEs weekly and will take place on a digital platform and are encouraged but in person sessions are available. Sessions are recorded but live attendance is strongly encouraged.
Ethics and dissemination
The study proposal was approved by the University of Washington ethics/institutional review board (IRB) Committee (IRB ID: STUDY00014396 date 1/7/2022) and the Sea Mar IRB committee and funded by the American Diabetes Association Disparities of Healthcare grant 11-21-ICTSHD-51. The findings will be published in peer-reviewed journals and presented at scientific conferences. All recruited patients will be informed by the HE/CHW, verbally and in writing, about the objectives, methodology, tests and interventions they receive if they participate in the study. Patients will be included if they grant permission and sign the informed consent. Household members will give verbal assent. The consent document is available in both Spanish and English (online supplemental materials 4 and 5). All participant information will be stored on REDCap. Any modifications to the protocol will require a formal amendment to the protocol and acceptance by the ethics committee. We plan to publish the findings in peer-reviewed journals and share our findings at scientific conferences. The investigators will consider authorship following widely accepted criteria.
bmjopen-2023-082005supp004.pdf (175.3KB, pdf)
bmjopen-2023-082005supp005.pdf (199.3KB, pdf)
Limitations of the study
This study is limited due to involving only a single centre and smaller sample size. All participants receive an intervention with DSMES to enhance diabetes knowledge. We believe that those that receive RT-CGM with DSMES may have better initial diabetes indices after the DSMES intervention is completed given real-time feedback from CGM, and sustained improvement at 6 months without further intervention. However, the study may be underpowered if retention is less than expected. We will aim to recruit up to 130 participants given a likely 20–30% drop out prior to education given the population served. This estimate is based on experience by the community partner with other diabetes education programmes. We additionally do not have funding to evaluate longer-term effects (>1 year). While there may be initial improvement after intervention at 3 months and 6 months, long-term follow-up will need to be explored in future studies. Finally, although culturally tailored interventions are important, due to the heterogeneity within the Latinx population, adapting a single educational curriculum to reach all Latinx participants from many different backgrounds remains a challenge. We intentionally elected to use HEs and a bilingual bicultural physician working in the local community as the primary translators of the curriculum, with the purpose of capturing cultural nuances that may benefit communication with the participants. A formal translation service was not used, and we recognise that this could also be a potential limitation.
Supplementary Material
Acknowledgments
We acknowledge KS’ lifelong dedication to empowerment and support of vulnerable populations and her initial work on the culturally tailored diabetes education curriculum. We sadly report her passing during her current work on this project. We thank Tamara Swigert, RN, MSN, CDCES, at Children's Hospital Colorado for her initial work on the CGM education materials. We also thank Darinka Gil Menchaca, Sea Mar and Evelin Jones, University of Washington, for their significant work on the curriculum translation.
Footnotes
Twitter: @DrLorenaWright1
Contributors: NE wrote the manuscript. GF, PB, BCo, LM and LW contributed to the protocol and discussion and reviewed/edited the manuscript. BCe wrote the data analysis and sample size estimation and reviewed/edited the manuscript. KS contributed to the protocol. NE takes responsibility for the content of this article.
Funding: This work was funded by the American Diabetes Association Disparities of Health Care grant. Grant number: 11-21-ICTSHD-51.
Competing interests: NE has been on an advisory board for Dexcom, Bayer and Novo Nordisk and received investigator-initiated grants from Dexcom and educational grants from Merck and Novo Nordisk.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; peer reviewed for ethical and funding approval prior to submission.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Centers for Disease Control and Prevention . National diabetes statistics report website. Available: https://www.cdc.gov/diabetes/data/statistics-report/index.html [Accessed 28 Dec 2022].
- 2.American Diabetes Association . Economic costs of diabetes in the U.S. in 2017. Diabetes Care 2018;41:917–28. 10.2337/dci18-0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . Who fact sheet diabetes. Available: https://www.who.int/news-room/fact-sheets/detail/diabetes [Accessed 30 Dec 2022].
- 4.Aguayo-Mazzucato C, Diaque P, Hernandez S, et al. Understanding the growing epidemic of type 2 diabetes in the Hispanic population living in the United States. Diabetes Metab Res Rev 2019;35:e3097. 10.1002/dmrr.3097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CDC diabetes Hispanic. Available: https://www.cdc.gov/diabetes/library/features/hispanic-diabetes.html [Accessed 30 Dec 2022].
- 6.Hu J, Amirehsani K, Wallace DC, et al. Perceptions of barriers in managing diabetes: perspectives of Hispanic immigrant patients and family members. Diabetes Educ 2013;39:494–503. 10.1177/0145721713486200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hildebrand JA, Billimek J, Lee J-A, et al. Effect of diabetes self-management education on glycemic control in Latino adults with type 2 diabetes: a systematic review and meta-analysis. Patient Educ Couns 2020;103:266–75. 10.1016/j.pec.2019.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ricci-Cabello I, Ruiz-Pérez I, Rojas-García A, et al. Characteristics and effectiveness of diabetes self-management educational programs targeted to racial/ethnic minority groups: a systematic review, meta-analysis and meta-regression. BMC Endocr Disord 2014;14:60. 10.1186/1472-6823-14-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gonder-Frederick LA, Cox DJ, Ritterband LM. Diabetes and behavioral medicine: the second decade. J Consult Clin Psychol 2002;70:611–25. 10.1037//0022-006x.70.3.611 [DOI] [PubMed] [Google Scholar]
- 10.Norris SL, Lau J, Smith SJ, et al. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 2002;25:1159–71. 10.2337/diacare.25.7.1159 [DOI] [PubMed] [Google Scholar]
- 11.Partners in Care . PILI ‘OHANA - partnership for improving lifestyle intervention - people (Hawaii.Edu); 2023.
- 12.Two Feathers J, Kieffer EC, Palmisano G, et al. Racial and ethnic approaches to community health (REACH) detroit partnership: improving diabetes-related outcomes among African American and Latino adults. Am J Public Health 2005;95:1552–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spencer MS, Rosland A-M, Kieffer EC, et al. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am J Public Health 2011;101:2253–60. 10.2105/AJPH.2010.300106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feathers JT, Kieffer EC, Palmisano G, et al. The development, implementation, and process evaluation of the REACH detroit partnership’s diabetes lifestyle intervention. Diabetes Educ 2007;33:509–20. 10.1177/0145721707301371 [DOI] [PubMed] [Google Scholar]
- 15.Sinclair KA, Makahi EK, Shea-Solatorio C, et al. Outcomes from a diabetes self-management intervention for native Hawaiians and Pacific people: partners in care. Ann Behav Med 2013;45:24–32. 10.1007/s12160-012-9422-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wright L, Sinclair K. A pilot study with Latinx adults to evaluate the companeros en salud DSMES intervention with RT-CGM. Unpublished data 2020.
- 17.Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study group . Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med 2008;359:1464–76. 10.1056/NEJMoa0805017 [DOI] [PubMed] [Google Scholar]
- 18.Battelino T, Phillip M, Bratina N, et al. Effect of continuous glucose monitoring on hypoglycemia in type 1 diabetes. Diabetes Care 2011;34:795–800. 10.2337/dc10-1989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study group . Sustained benefit of continuous glucose monitoring on A1C, glucose profiles, and hypoglycemia in adults with type 1 diabetes. Diabetes Care 2009;32:2047–9. 10.2337/dc09-0846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lind M, Polonsky W, Hirsch IB, et al. Continuous glucose monitoring vs conventional therapy for glycemic control in adults with type 1 diabetes treated with multiple daily insulin injections: the GOLD randomized clinical trial. JAMA 2017;317:379. 10.1001/jama.2016.19976 [DOI] [PubMed] [Google Scholar]
- 21.Kompala T, Neinstein A. A new era: increasing continuous glucose monitoring use in type 2 diabetes. Am J Manag Care 2019;25(4 Spec No):SP123–6. [PubMed] [Google Scholar]
- 22.Danne T, Nimri R, Battelino T, et al. International consensus on use of continuous glucose monitoring. Diabetes Care 2017;40:1631–40. 10.2337/dc17-1600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American diabetes Association . Diabetes technology: standards of care in diabetes-2023. Diabetes Care 2023;46:S111–27. 10.2337/dc23-SDIS [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ehrhardt NM, Chellappa M, Walker MS, et al. The effect of real-time continuous glucose monitoring on glycemic control in patients with type 2 diabetes mellitus. J Diabetes Sci Technol 2011;5:668–75. 10.1177/193229681100500320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vigersky RA, Fonda SJ, Chellappa M, et al. Short- and long-term effects of real-time continuous glucose monitoring in patients with type 2 diabetes. Diabetes Care 2012;35:32–8. 10.2337/dc11-1438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wada E, Onoue T, Kobayashi T, et al. Flash glucose monitoring helps achieve better glycemic control than conventional self-monitoring of blood glucose in non-insulin-treated type 2 diabetes: a randomized controlled trial. BMJ Open Diab Res Care 2020;8:e001115. 10.1136/bmjdrc-2019-001115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martens T, Beck RW, Bailey R, et al. Effect of continuous glucose monitoring on glycemic control in patients with type 2 diabetes treated with basal insulin: a randomized clinical trial. JAMA 2021;325:2262–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ehrhardt N, Al Zaghal E. Behavior modification in prediabetes and diabetes: potential use of real-time continuous glucose monitoring. J Diabetes Sci Technol 2019;13:271–5. 10.1177/1932296818790994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Koonin LM, Hoots B, Tsang CA, et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic - United States, January-March 2020. MMWR Morb Mortal Wkly Rep 2020;69:1595–9. 10.15585/mmwr.mm6943a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tends in telehealth and its implications for health disparities: EXECUTIVE SUMMARY [Internet]. Kansas City, MO. 2022. Available: https://content.naic.org/sites/default/files/Telehealth%20and%20Health%20Disparities.pd [Accessed 30 Dec 2023]. [Google Scholar]
- 31.Silva MA, Perez OFR, Añez LM, et al. Telehealth treatment engagement with latinx populations during the COVID-19 pandemic. Lancet Psychiatry 2021;8:176–8. 10.1016/S2215-0366(20)30419-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Despoja OE, Chae M, Ojinnaka CO, et al. Utilization gaps during the COVID-19 pandemic: racial and ethnic disparities in telemedicine uptake in federally qualified health center clinics. J Gen Intern Med 2022;37:1191–7. 10.1007/s11606-021-07304-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Anderson A, O’Connell SS, Thomas C, et al. Telehealth interventions to improve diabetes management among black and Hispanic patients: a systematic review and meta-analysis. J Racial Ethn Health Disparities 2022;9:2375–86. 10.1007/s40615-021-01174-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med 2007;357:370–9. 10.1056/NEJMsa066082 [DOI] [PubMed] [Google Scholar]
- 35.Khan A, Lasker SS, Chowdhury TA. Are spouses of patients with type 2 diabetes at increased risk of developing diabetes Diabetes Care 2003;26:710–2. 10.2337/diacare.26.3.710 [DOI] [PubMed] [Google Scholar]
- 36.Pierce M, Keen H, Bradley C. Risk of diabetes in offspring of parents with non-insulin-dependent diabetes. Diabet Med 1995;12:6–13. 10.1111/j.1464-5491.1995.tb02054.x [DOI] [PubMed] [Google Scholar]
- 37.Whitaker RC, Wright JA, Pepe MS, et al. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med 1997;337:869–73. 10.1056/NEJM199709253371301 [DOI] [PubMed] [Google Scholar]
- 38.Adamson AJ, Foster E, Butler TJ, et al. Non-diabetic relatives of type 2 diabetic families: dietary intake contributes to the increased risk of diabetes. Diabet Med 2001;18:984–90. 10.1046/j.1464-5491.2001.00575.x [DOI] [PubMed] [Google Scholar]
- 39.Sargeant LA, Wareham NJ, Khaw KT. Family history of diabetes identifies a group at increased risk for the metabolic consequences of obesity and physical inactivity in EPIC-Norfolk: a population-based study. Int J Obes Relat Metab Disord 2000;24:1333–9. 10.1038/sj.ijo.0801383 [DOI] [PubMed] [Google Scholar]
- 40.Elder JP, Arredondo EM, Campbell N, et al. Individual, family, and community environmental correlates of obesity in Latino elementary school children. J Sch Health 2010;80:20–30. 10.1111/j.1746-1561.2009.00462.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hamid AMS, Sazlina SG. Interventions for obesity among schoolchildren: a systematic review and meta-analyses. PLoS One 2019;14:e0209746. 10.1371/journal.pone.0209746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shelton D, Le Gros K, Norton L, et al. Randomised controlled trial: a parent-based group education programme for overweight children. J Paediatr Child Health 2007;43:799–805. 10.1111/j.1440-1754.2007.01150.x [DOI] [PubMed] [Google Scholar]
- 43.Ewald H, Kirby J, Rees K, et al. Parent-only interventions in the treatment of childhood obesity: a systematic review of randomized controlled trials. J Public Health (Oxf) 2014;36:476–89. 10.1093/pubmed/fdt108 [DOI] [PubMed] [Google Scholar]
- 44.Aarts F, Radhakishun NNE, van Vliet M, et al. Gastric bypass may promote weight loss in overweight partners. J Am Board Fam Med 2015;28:90–6. 10.3122/jabfm.2015.01.140103 [DOI] [PubMed] [Google Scholar]
- 45.Woodard GA, Encarnacion B, Peraza J, et al. Halo effect for Bariatric surgery: collateral weight loss in patients' family members. Arch Surg 2011;146:1185–90. 10.1001/archsurg.2011.244 [DOI] [PubMed] [Google Scholar]
- 46.Gorin AA, Lenz EM, Cornelius T, et al. Randomized controlled trial examining the ripple effect of a nationally available weight management program on untreated spouses. Obesity (Silver Spring) 2018;26:499–504. 10.1002/oby.22098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gorin AA, Wing RR, et al. , Look AHEAD Home Environment Research Group . Weight loss treatment influences untreated spouses and the home environment: evidence of a ripple effect. Int J Obes (Lond) 2008;32:1678–84. 10.1038/ijo.2008.150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Molenberghs G, Kenward MG. Missing data in clinical studies. J Trop Pediatr 2007;53:294. 10.1093/tropej/fmm053 [DOI] [Google Scholar]
- 49.Dexcom G6 user manual. Available: https://www.dexcom.com/en-us/guides [Accessed 27 Feb 2023].
- 50.Link to Compañeros en Salud curriculum. Available: https://uwmdi.org/adult-care [Accessed 3 Mar 2023].
- 51.Ehrhardt N, Al Zaghal E. Continuous glucose monitoring as a behavior modification tool. Clin Diabetes 2020;38:126–31. 10.2337/cd19-0037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Paxton AE, Strycker LA, Toobert DJ, et al. Starting the conversation performance of a brief dietary assessment and intervention tool for health professionals. Am J Prev Med 2011;40:67–71. 10.1016/j.amepre.2010.10.009 [DOI] [PubMed] [Google Scholar]
- 53.Pruitt SL, Leonard T, Xuan L, et al. Who is food insecure? Implications for targeted recruitment and outreach, national health and nutrition examination survey, 2005-2010. Prev Chronic Dis 2016;13:E143. 10.5888/pcd13.160103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Booth M. Assessment of physical activity: an international perspective. Res Q Exerc Sport 2000;71(2 Suppl):S114–20. [PubMed] [Google Scholar]
- 55.Sanford School of Public Policy . Neighborhood questionnaire. Available: https://fasttrackproject.org/measure/neighborhood-questionnaire [Accessed 1 Jan 2023].
- 56.Beléndez M Sallis JF, Kerr J, Carlson JA, et al. Evaluating a brief self-report measure of neighborhood environments for physical activity research and surveillance: physical activity neighborhood environment scale (PANES). J Phys Act Health 2010;7:533–40. 10.1123/jpah.7.4.533 [DOI] [PubMed] [Google Scholar]
- 57.Wulsin L, Somoza E, Heck J. The feasibility of using the Spanish PHQ-9 to screen for depression in primary care in Honduras. Prim Care Companion J Clin Psychiatry 2002;4:191–5. 10.4088/pcc.v04n0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hernández-Mijares A, Marco J, Domínguez JR, et al. Validation of the Spanish version of the problem areas in diabetes (PAID-SP) scale. Diabetes Res Clin Pract 2014;106:e93–5. 10.1016/j.diabres.2014.09.012 [DOI] [PubMed] [Google Scholar]
- 59.Vincent D, McEwen MM, Pasvogel A. The validity and reliability of a Spanish version of the summary of diabetes self-care activities questionnaire. Nurs Res 2008;57:101–6. 10.1097/01.NNR.0000313484.18670.ab [DOI] [PubMed] [Google Scholar]
- 60.Ritter PL, Lorig K, Laurent DD. Characteristics of the Spanish- and English-language self-efficacy to manage diabetes scales. Diabetes Educ 2016;42:167–77. 10.1177/0145721716628648 [DOI] [PubMed] [Google Scholar]
- 61.Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group . Validation of measures of satisfaction with and impact of continuous and conventional glucose monitoring. Diabetes Technol Ther 2010;12:679–84. 10.1089/dia.2010.0015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Habits questionnaire. Available: https://5210.psu.edu/wp-content/uploads/2018/02/healthyhabitsqages10to18_hc_7-11-17s.pdf [Accessed 27 Feb 2023].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-082005supp001.pdf (19.6KB, pdf)
bmjopen-2023-082005supp002.pdf (28MB, pdf)
bmjopen-2023-082005supp003.pdf (14.7MB, pdf)
bmjopen-2023-082005supp004.pdf (175.3KB, pdf)
bmjopen-2023-082005supp005.pdf (199.3KB, pdf)