Abstract
Background
Clinicians have difficulty predicting need for hospitalization in children with acute asthma exacerbations.
Objective
To develop and internally validate a multivariable Asthma Prediction Rule (APR) to inform hospitalization decision-making in children ages 5-17 years with acute asthma exacerbations.
Methods
Between April, 2008 and February, 2013 we enrolled a prospective cohort of patients ages 5-17 years with asthma who presented to our pediatric emergency department with acute exacerbations. Predictors for APR modeling included 15 demographic characteristics, asthma chronic control measures, and pulmonary examination findings in participants at the time of triage and before treatment. The primary outcome variable for APR modeling was need for hospitalization (length-of-stay > 24 hr for those admitted to hospital or relapse for those discharged). A secondary outcome was the hospitalization decision of the clinical team. We used penalized maximum likelihood multiple logistic regression modeling to examine the adjusted association of each predictor variable with the outcome. Backward step-down variable selection techniques were used to yield reduced-form models.
Results
Data from 928 of 933 participants was used for prediction rule modeling, with median [IQR] age 8.8 [6.9, 11.2] years, 61% male, and 59% African-American race. Both full (penalized) and reduced-form models for each outcome calibrated well, with bootstrap-corrected c-indices of 1.74 and 0.73 for need for hospitalization and 0.81 in each case for hospitalization decision.
Conclusion
The APR predicts the need for hospitalization of children with acute asthma exacerbations using predictor variables available at the time of presentation to an emergency department.
Keywords: pediatric acute asthma exacerbations, clinical prediction rule, hospitalization
INTRODUCTION
Asthma is the most prevalent chronic disease of childhood and the most frequent reason for childhood hospitalization in the United States.1, 2 A challenging clinical feature of this complex environmental and genetic disease is the heterogeneity of clinical expression.3 As such, the ability of clinicians to assess severity of acute asthma exacerbations is variable and limited in accuracy.4
Approximately thirty-six acute asthma severity scores have been proposed. The purpose of such a score is to assess severity at the bedside in order to assist clinicians in applying appropriate immediate treatment. Systematic reviews of sixteen of these acute severity scores concluded that their predictive validity was inadequate to justify their use for patient hospitalization decisions.5, 6
Further, investigators have noted the difficulty that clinicians have in predicting the need for hospitalization or in predicting relapse after evaluation and treatment of exacerbations in emergency departments (EDs).7 These features of exacerbations fulfill Steill’s five criteria that identify the need for a Clinical Prediction Rule (CPR).8
A CPR is a decision-making tool that incorporates two or more variables from the history, physical examination, or additional tests.9, 10 A CPR can be used in individual patients to predict the probability of an event or intervention such as hospital admission. As such, CPRs fulfill a role distinct from that of acute severity scores, assist clinicians in their clinical decision-making, and potentially improve resource utilization. To our knowledge, a CPR has not been developed to predict the need for hospitalization in pediatric patients with acute asthma exacerbations.
We sought to develop and internally validate a multivariable Asthma Prediction Rule (APR) to inform hospitalization decision-making in a population of children ages 5 to 17 years with acute asthma exacerbations, in accordance with contemporary clinical and biostatistical standards established for CPR development and internal validation.11-13
METHODS
Study Participants
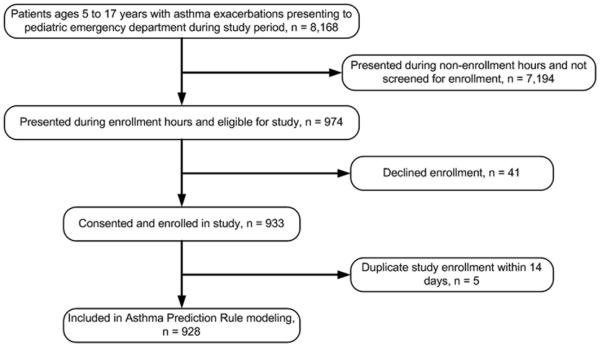
Detailed methods for our study have been presented in a previous report.13 We enrolled a prospective convenience sample aged 5 to 17 years with doctor-diagnosed asthma who presented with acute exacerbations to our academic, tertiary, urban children’s hospital emergency department (PED). We excluded patients with chronic lung disease other than asthma or with other causes for pertinent signs and symptoms. We included participants with more than one enrollment for APR modeling as long as the interval between enrollments was greater than 14 days (Figure 1). The rationale for this was that patient visits having this chronologic separation were likely to represent distinct exacerbation events.
Figure 1. Participant recruitment and study implementation.
Does not require a legend.
The clinical team maintained exclusive decision-making capacity regarding all management and hospitalization decisions. Study data were not made available to the clinical team, and the study protocol did not include informing clinical management. The study protocol was reviewed and approved by the Vanderbilt University IRB (protocol #080058); parents and participants provided informed written consent and assent.
Participant Measurements and Data Acquisition
Baseline data included medical history, family asthma history, demographic and social information, medications in use, coexisting illness, asthma symptom history, and asthma characteristics that encompassed chronic disease control, environmental exposures and prior adverse events.13 Additional clinical variables were measured and recorded before initiating treatment. These included oxygen saturation (SpO2) on room air, assessment for accessory muscle use (scalene, sternocleidomastoid-suprasternal, intercostal, subcostal), lung auscultation (inspiratory to expiratory ratio, wheezing, air entry) exhaled nitric oxide (eNO), and spirometry for %-predicted forced expiratory volume in 1-second (%FEV1).14, 15 Using bedside physical findings and SpO2 we calculated the Acute Asthma Intensity Research Score (AAIRS), a validated bedside acute severity score (though not a clinical prediction rule).16
Candidate Predictor Variables
Candidate predictor variables for a CPR should be clinically and biologically plausible, ideally with some established evidence of predictive value. For example, we have previously reported that accessory muscle group use is a physical sign readily assessed at the bedside and has a dose-response association with %FEV1.15, 16 Additionally, an APR will be more practical and widely used by clinicians if the predictor variables are available at the bedside.
We considered candidate predictor variables for APR development in accordance with these principles (Table 1). These included participant demographic and asthma characteristics, pulmonary exam findings, and measures of lung function and inflammation.
Table 1.
Pre-specified predictor variables for modeling the Asthma Prediction Rule
| Variable | Type | d.f. |
|---|---|---|
| Age | Continuous | 2 |
| BMI | 2 | |
| Race | Dichotomous | 1 |
| Gender | 1 | |
| Gina chronic control | ||
| Daytime sx > 2/wk | 1 | |
| Nocturnal sx > 1/wk | 1 | |
| Activity limitation | Dichotomous | 1 |
| Need for albuterol > 2/wk | 1 | |
| Asthma exacerbation tx with CCS (prior yr) |
1 | |
| SpO2 | Continuous | 1 |
| Accessory muscle use | ||
| SCM | 1 | |
| Intercostal | Dichotomous | 1 |
| Subcostal | 1 | |
| Inspiratory to expiratory ratio | Ordinal | 2 |
| Wheezing | 2 | |
|
|
||
| Total d.f. | 19 | |
d.f. = Degrees of freedom; BMI = Body mass index; sx = symptoms; tx = treatment; SpO2 = oxygen saturation on room air; SCM = sternocleidomastoid
A variable was excluded after data acquisition but before APR modeling if its value was subject to our hospital’s local practice and not generalizable (e.g., PCCU admission criteria), had high measurement variability or did not calibrate well to severity (e.g., respiratory rate), was rarely abnormal (e.g., scalene retractions), displayed multiple colinearity with another variable (e.g., air entry), had a high proportion of missing data (e.g., FEV1), or was difficult to measure or not available in clinical settings where acute asthma may be managed (e.g., exhaled nitric oxide, plethysmograph estimate of pulsus paradoxus). As a result, seven candidate variables were excluded (Table E1), and the final model included the fifteen predictor variables in Table 1.
Outcome Variables
A CPR must predict an outcome that is both clearly defined and clinically important.9, 17 The primary outcome variable was need for hospitalization, defined as length of stay >24 h (for admitted participants) or unscheduled return for asthma care to a physician or hospital within 48 h (for discharged participants).13 Prior to prediction rule modeling an expert studio panel recommended that a second pragmatic and relevant primary outcome variable would be the hospitalization decision of the clinical team. This outcome encompasses the multiplicity of factors that the clinical team considers in disposition decision-making, as well as individual variability within a culture of approximately 25 attending physicians for assessment of exacerbation severity, risk-tolerance, cost-efficiency and other characteristics that may influence this decision.18 This outcome has also been used for evaluation of acute asthma severity scores.19, 20
Statistical Analysis
Sample size calculation
Sample size for CPR modeling must be sufficiently large or the number of predictor variables must be sufficiently conservative for the model to be reliable and accurate on a future stream of similar patients.11 Specifically, there must be at least 10 participants having the primary outcome (i.e., hospitalization) per degrees of freedom (df) of all candidate predictor variables.21 Our model had 15 predictors and19 df (Table 1). There were 158 participants who met need for hospitalization criteria, thus allowing approximately 15 df for this model to avoid overfitting. In addition, there were 214 hospitalizations amongst 928 participants that would allow up to 21 df for the hospitalization decision model.
Statistical Modeling of the full-model APR
We used penalized maximum likelihood estimation logistic regression models to examine the independent association of each pre-specified predictor variable with the two outcomes need for hospitalization and hospitalization decision of the clinical team. We retained all pre-specified predictor variables in the full models and did not remove any of these variables based on statistical significance because doing so could introduce bias of the estimated regression coefficients for the remaining predictor variables as well as corresponding standard errors that are too low and confidence intervals that are falsely narrow.11, 22-24 Prediction models that retain all pre-specified predictor variables and that apply shrinkage of estimated regression coefficients might have greater predictive performance when used for future patients with similar characteristics.11, 25 Age and BMI were included as flexible smooth parameters using restricted cubic splines. We estimated the variance using the Huber-White robust sandwich estimator to account for correlated data due to repeated enrollment measurements from the same patient.26, 27 For odds ratios (OR), 95% confidence intervals (CI) were calculated.
Statistical modeling of the reduced-form APR
To decrease the complexity of the full model and to yield reduced-form models that would be more practical for bedside use, we performed step-down backward variable selection with an alpha criterion of 0.25 (type I error) within bootstrap validation.. We assessed model performance using the metrics described below and compared these with the respective full model performance metrics.
Assessment for Age-Gender Interaction
Males ages 5 – 17 years have been noted to have a higher rate of hospitalization for asthma, particularly amongst those males ages 5 – 10 years.2 With this in mind, interaction between age and sex was assessed to study whether effects of age were different for males and females.
Model Performance and Internal Validation
We assessed model performance using two metrics, calibration and discrimination.24, 28 Calibration is the accuracy of agreement of the predicted probability of the outcome provided by the model with the observed frequency of the outcome. A graphical assessment of calibration is possible with predictions on the x-axis and the actual outcomes on the y-axis. A 45° line represents perfect model calibration; deviation from this line represents bias in predicted values. For dichotomous outcomes, the plot contains only 0 and 1 values for the y-axis. Smoothing techniques (Loess algorithm) were used to estimate the observed probabilities of the outcome in relation to the predicted probabilities.
We assessed predictive discrimination for the ability of the model to distinguish between patients with different outcomes using the c-index and a histogram of predicted probabilities. The c-index is a rank order statistic that estimates the probability of concordance between predicted and observed outcomes and measures how well the model discriminates between different outcomes. For example a model with a high discriminative c-index (0.9) will be able to define high-risk groups better than one with low discriminative c-index (0.6).
Bootstrap internal Validation
Internal validation of the prediction model was assessed using 300 bootstrap replications with replacement.12, 24, 28-30 Bootstrap validation involves estimation of the likely future performance of the model on new patients of the same types, which involves estimation of the drop-off in performance when the model is applied to a new sample. Bootstrapping is also an efficient technique that involves random samples that are drawn with replacement from the original data set and that are the same size as the original cohort. Thus a patient in a bootstrap sample could be represented multiple times and another could appear 0 times.
The bootstrapping validation algorithm was applied as follows: 1) We first estimated the apparent predictive ability with the original sample dataset used to fit the model; 2) 300 bootstrap samples were drawn from the original sample, and for each bootstrap sample we fit the model and measured the apparent predictive ability; 3) We tested the accuracy measure by applying the bootstrap model to the original sample; 4) The optimism in predictive ability for this bootstrap model was calculated as the difference in performance between the bootstrap model and the original dataset; and 5) We used the average of the optimism over all 300 bootstrap samples as a correction factor to estimate a validated performance measure by subtracting the estimated optimism from the apparent predictive ability. The algorithm described above can be used to internally validate any measure of model calibration or discrimination.
Shrinkage using Penalized Maximum Likelihood Estimation
To correct for overfitting we applied penalized maximum likelihood estimation (PMLE).31 PMLE maximizes the penalized log likelihood rather than maximizing the log likelihood as in conventional logistic regression. Thus, the maximum log likelihood of the full model is adjusted (shrunk) by a penalty factor. The estimated regression coefficients are individually adjusted for overfitting in contrast to a uniform shrinkage method. PMLE provides smaller prediction errors and preserves the discriminative ability of the model while shrinking each predictor for overoptimism. The full penalized model and its internal validation are presented. Analyses were performed using R-software v. 3.1 (R statistical software, Institute for Statistics and Mathematics, Vienna, Austria).29, 30
RESULTS
Participant Characteristics
During the period of enrollment, April 8, 2008 to February 12, 2013 we invited 974 patients to participate in the study, 41 declined and 933 participated, 928 of whom were unique participants or previously enrolled participants with intervals between enrollments of at least 14 days (Figure 1). Thus 928 participants were included in APR modeling. Demographic and asthma characteristics of these participants are displayed in Table 2 along with the overall group of patients ages 5 – 17 years who presented to our PED with exacerbations during the study period.
Table II.
Characteristics of participants and of patients aged 5 - 17 years with acute asthma admitted to pediatric emergency department during study period
| Study Participants (n = 928) |
PED Asthma Patientsa (n = 8,168 ) |
|
|---|---|---|
| Age | 8.8 [6.9,11.2] | 7.1 [4.7, 10.3] |
| Male | 566 (61) | 5,135 (63) |
| BMI (Kg/M2) | 18.0 [15.6, 21.9] | NA |
| BMI percentile | 72.5 [ 41.5, 93.7] | |
| Race | ||
| African-American | 547 (59) | 4,623 (57) |
| White | 374 (40) | 2,792 (34) |
| Asian | 6 (1) | 86 (1) |
| Other | 2 (<1) | 667 (8) |
| Ethnicityb | ||
| Hispanic or Latino | 68 (7) | |
| Not Hispanic or Latin0 | 860 (93) | NAd |
| Not reported/unknown | 0 (0) | |
| Medicaid | 581 (63) | 5,198 (64) |
| Asthma characteristics | ||
| Asthma control and future riskc | ||
| Daytime sx > 2/wk | 457 (49) | |
| Nocturnal sx/awakening | 519 (56) | |
| Activity limitation | 471 (49) | |
| Need for rescue tx > 2/wk |
451 (49) | |
| Exacerbation in past year | 572 (62) | |
| Using inhaled corticosteroid | 430 (46) | NAd |
| Second-hand smoke exposure |
341 (37) | |
| Prior PCCU admission | 200 (22) | |
| Prior ETI | 42 (5) | |
| AAIRS | 5 [2, 8] | |
| Hospitalization decision of clinical team | ||
| Discharge to home | 712 (77) | |
| Admit to floor bed | 163 (18) | |
| Admit to PCCU | 51 (6) | |
n (%) except Age and AAIRS, which are median [IQR] AAIRS = acute asthma intensity research score;15 PCCU = pediatric critical care unit; ETI = endotracheal intubation for asthma
Baseline Population: all patients aged 5 to 17 years presenting to pediatric emergency department during study period with final primary diagnosis of asthma exacerbation by ICD code 493, including study sample
Hispanic ethnicity is not mutually exclusive of race.32
Global Initiative for Asthma (GINA) chronic control characteristics for preceding 3-month period.33
Not available in database used to identify PED asthma population
Participants were primarily in middle childhood, and the majority were male, African-American and publicly insured. Approximately 7% were of Hispanic or Latino ethnicity, and parents identified a primary race category independent of ethnicity designation (Table 2).32 Using the GINA chronic asthma control criteria for the preceding 3-month period, 16% of participants were controlled, 15% partly controlled, and 69% uncontrolled.33 In addition, a majority of participants had nocturnal awakenings due to asthma during this 3-month period, and 62% had an exacerbation in the preceding year that necessitated CCS treatment. Thirty-seven percent of our participants were exposed to second-hand smoke, and 22% had prior PCCU admissions for asthma. The majority of exacerbations necessitating the PED visit were of moderate severity measured using the AAIRS, and 24% were hospitalized. Of note, female participants greater than 6 years of age were more likely to be hospitalized than were males, in contrast to previous reports.2 The distributions of predicted probabilities of the outcomes for the full models are presented in Figure E1 with vertical bars representing probability by 5% increments.
Asthma Prediction Rule Modeling
Full models
We modeled the APR using penalized multiple logistic regression with the 15 predictor variables (Table 1). No statistically significant interaction between age and gender was detected (p > 0.3) thus we proceeded with the APR regression modeling without interaction terms. The final penalized full-model results are presented in Figure E2. These models compute the predicted probability of the outcomes for an individual patient, and the corresponding nomograms for these calculations are displayed in Figures E3 and E4. Of note, the Total Points and Predicted Probability scales do not align due to non-linearity of some associations.
Odds ratios and 95% confidence intervals (CIs) for the association of these predictor variables on the outcomes of interest are presented in Table 3. Two predictor variables were most strongly associated with need for hospitalization. These included SpO2 on room air (for 94% vs. 98%, OR 2.4, 95% confidence interval [CI] 1.9, 3.1) and inspiratory to expiratory ratio (≤ 1:3 vs. 1:1, OR 1.9, 95% CI 1.1, 3.1). Four predictor variables were most strongly associated with the hospitalization decision of the clinical team. These included SpO2 on room air (for a 4% decrease, OR 3.9, 95% CI 3.0, 5.0), intercostal retractions (OR 1.6, 95% CI 1.0, 2.4), inspiratory to expiratory ratio (≤ 1:3 vs. 1:1, OR 2.0, 95% CI 1.1, 3.7) and wheezing (inspiratory and expiratory vs. none, OR 2.1, 95% CI 1.2, 3.7). The penalized models yielded bootstrapping-corrected estimates of the c-indexes for discrimination of 0.74 (need for hospitalization) and 0.81 (hospitalization decision) with the calibration curves presented in Figure E5.11, 12 The models’ calibration estimates have minimal deviations from the apparent probabilities.
Table III.
Full Asthma Prediction Rule models, penalized odds ratios for associations of predictor variables with primary outcome of need for hospitalization and secondary outcome of decision of the clinical team for hospitalization in 928 participants aged 5 - 17 years with asthma exacerbations
| Need for hospitalization |
Hospitalization decision of the clinical team |
|
|---|---|---|
| Age (Years, change from 6.9 to 11 years) | 1.4 (1.1 – 1.9) | 1.3 (1.0 - 1.8) |
| BMI (Kg/M2) change from 15.6 to 22) | 1.0 (0.8 – 1.3) | 0.9 (0.7- 1.2) |
| SpO2 (%, change from 98 to 94%) | 2.4 (1.9 – 3.0) | 3.9 (3.0 - 5.0) |
| Gender (Female:Male) | 1.3 (0.9 – 1.8) | 1.1 (0.8 - 1.6) |
| Race (white:other) | 1.1 (0.8 – 1.6) | 0.9 (0.7 - 1.3) |
| Daytime asthma sx > 2/wk | 1.1 (0.7 -1.6) | 1.1 (0.7 - 1.7) |
| Nocturnal asthma sx or awakening | 1.0 (0.7 – 1.4) | 0.9 (0.6 - 1.4) |
| Limitation of activity due to asthma | 1.1 (0.8 – 1.6) | 1.1 (0.8 - 1.6) |
| Need for albuterol > 2/wk | 1.1 (0.8 – 1.7) | 1.0 (0.7 - 1.6) |
| Asthma exacerbation in past year | 1.1 (0.8 – 1.6) | 1.1 (0.8 - 1.6) |
| Sternomastoid-suprasternal retractions | 1.0 (0.7 – 1.5) | 1.1 (0.7 - 1.7) |
| Intercostal retractions | 1.4 (0.9 – 2.0) | 1.6 (1.0 - 2.4) |
| Subcostal retractions | 1.0 (0.7 – 1.4) | 1.0 (0.7 - 1.5) |
| Inspiratory:Expiratory ratio (1:2 vs. 1:1) | 1.0 (0.7 – 1.5) | 1.3 (0.8 – 2.0) |
| Inspiratory:Expiratory ratio (≤ 1:3 vs. 1:1) | 1.9 (1.1 – 3.1) | 2.0 (1.1 - 3.7) |
| Wheezing (expiratory:none) | 1.2 (0.8 – 1.90) | 1.4 (0.8 - 2.5) |
| Wheezing (inspiratory + expiratory vs. none) | 1.23 (0.8 – 2.0) | 2.1 (1.2 - 3.7) |
Age and BMI included as flexible smooth variables using restricted cubic splines.
BMI = body mass index; SpO2 = oxygen saturation on room air Values are odd ratios (95% CI) estimated using penalized maximum likelihood logistic regression.
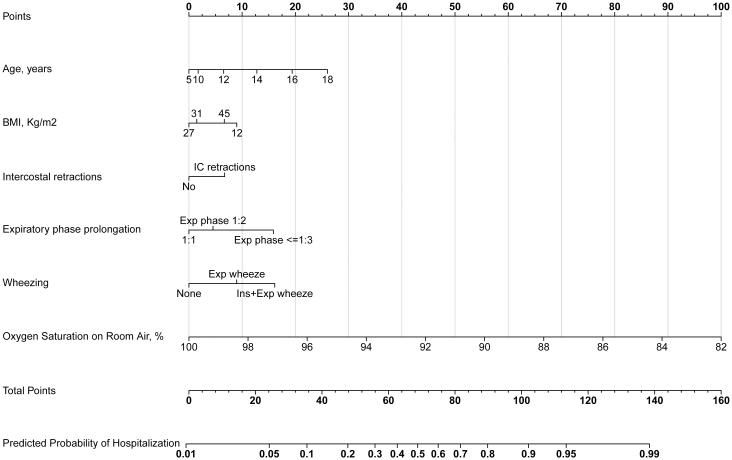
Reduced-form models
Backward step-down variable selection yielded the reduced-form models displayed in Table 4. The need for hospitalization model included age, gender, SpO2 on room air, need for albuterol > 2/wk, and expiratory phase prolongation, whereas the hospitalization decision model included age, BMI, SpO2 on room air, intercostal muscle retractions, expiratory phase prolongation, and wheezing. The reduced-form models yielded bootstrapping-corrected estimates of the c-indices for discrimination of 0.73 (need for hospitalization) and 0.81 (hospitalization decision) with the calibration curves presented in Figure E6.11, 12
Table IV.
Reduced-form Asthma Prediction Rule models, odds ratios for associations of predictor variables with primary outcome of need for hospitalization and secondary outcome of hospitalization decision of the clinical team in 928 participants aged 5 - 17 years with asthma exacerbations
| Need for hospitalization |
Hospitalization decision of the clinical team |
|
|---|---|---|
| Age (change from 6.9 to 11 years) | 1.5 (1.0 – 2.1) | 1.6 (1.2 – 2.2) |
| BMI (Kg/M2,change from 16 to 22) | NA | 0.7 (0.5 – 1.1) |
| Female gender | 1.44 (1.0 – 2.1) | NA |
| SpO2 (%, change from 98 to 94%) | 2.8 (2.1 – 3.6) | 4.4 (3.3 - 5.7) |
| Need for albuterol > 2/wk | 1.3 (0.9 – 1.9) | NA |
| Intercostal muscle retractions | NA | 1.6 (1.0 – 2.6) |
| Inspiratory:Expiratory ratio (≤ 1:3 vs. 1:1) | 4.4 (2.3 – 8.61) | 2.9 (1.3 – 6.5) |
| Wheezing (inspiratory + expiratory vs. none) | NA | 2.9 (1.4 – 5.6) |
Age and BMI included as flexible smooth variables using restricted cubic splines.
BMI = Body mass index; SpO2 = oxygen saturation on room air; NA = not included in this model (P > 0.25)
Values are odd ratios (95% CI) estimated using logistic regression.
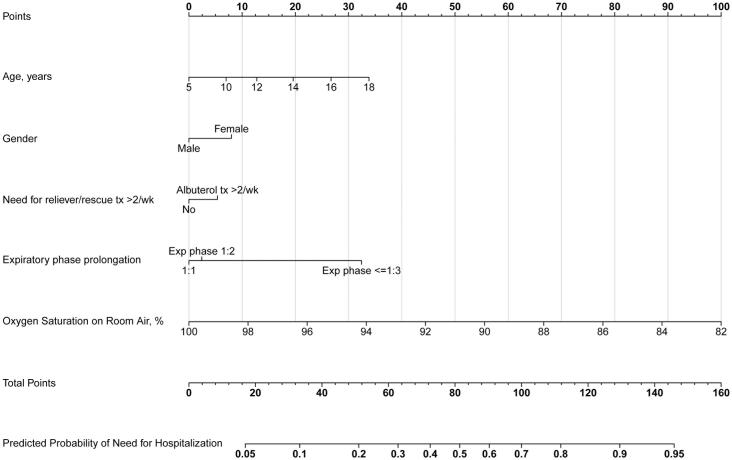
Nomograms
The APR nomograms (after shrinkage) for the full models are presented in Figures E3 and E4 and for the reduced-form models in Figures 2 and 3. To use the nomograms for an individual patient, the Points grid-line at the top of the nomogram is used to assign point values for each variable by aligning a vertical line from the grid-line to the line adjacent to the variable. The individual variable points are summed and a vertical line from the summed points on the Total Points grid-line to the Predicted Probability of Need of Hospitalization (Figure 2) provides an estimated probability of need for hospitalization. For example, for a female aged 14 years who does not use albuterol more than twice weekly and who has an inspiratory to expiratory ratio of 1:3 and a room-air oxygen saturation of 92%,the total point score is about 105 with a corresponding probability of need for hospitalization of approximately 74%. This calculation is further illustrated in Figure E7. As with all clinical prediction rules, this predicted probability might reduce uncertainty and assist the clinician in accurate decision-making for hospitalization but is not intended to prescribe a specific disposition or management plan.9, 10, 34
Figure 2.
Asthma Prediction Rule reduced-form nomogram for need for hospitalization: To use the nomogram for an individual patient, the points (top grid-line) for each predictor variable are first assigned and the total points calculated. A vertical line from this value on the Total Points grid-line provides a Probability of Need of Hospitalization grid-line. Exp = Expiratory; Ins = Inspiratory.
Figure 3.
Asthma Prediction Rule reduced-form nomogram for hospitalization decision of the clinical team: To use the nomogram for an individual patient, the points (top grid-line) for each predictor variable are first assigned and the total points calculated. A vertical line from this value on the Total Points grid-line provides a probability value on the Predicted Probability of Hospitalization grid-line. Exp = Expiratory; Ins = Inspiratory.
DISCUSSION
We have modeled and internally validated the Asthma Prediction Rule for children ages 5 – 17 years with acute asthma exacerbations in accordance with clinical and biostatistical standards established for CPR development.11-13, 22, 30, 35 To our knowledge, this is the first CPR for acute asthma exacerbations.
Although a number of CPRs have been derived for other conditions in pediatric patients, few have been validated, and other quality indicators have demonstrated various weaknesses of these models.9, 10 The APR includes predictor variables that are clinically intuitive and available at the bedside at the time of triage (before treatment). In addition, the rule internally validates well and might improve outcome prediction at the time of patient presentation, without the need to wait hours for assessment of response to therapy. As informatics-based clinical support becomes better integrated into patient care, the full-model APR can become electronically-automated and might enhance decision-support for clinicians. This might improve triage, patient management and resource utilization.
In addition, the reduced-form APR appears to be competitive with the full model for each outcome of interest. Clinicians might find the reduced-form and the accompanying nomogram to be more useful at the bedside because the limited number of predictor variables is less cumbersome.
Because the decision whether or not to hospitalize may be most clear for patients with mild or severe exacerbations, the APR may be of greatest use for those with moderate severity exacerbations. Indeed, study participants had a median AAIRS value of 5 [IQR 2, 8], indicating moderate severity episodes.16 It should also be noted that our cohort had a number of high-risk features, including the prevalence of uncontrolled chronic asthma measured using the GINA criteria, second-hand smoke exposure, and prior PCCU admission for asthma, yet a substantial proportion (46%) reported use of inhaled CCS. These participant characteristics are similar to other cohorts of pediatric patients with acute asthma exacerbations seeking care in PEDs.36
Although clinicians may determine that one of these outcomes, need for hospitalization or hospitalization decision, is most appropriate for their practice, oxygen saturation and expiratory phase prolongation contributed notably to each model. We believe that this is because these physical signs represent the most prominent physiologic derangements during acute asthma exacerbations, ventilation-perfusion mismatch and dynamic airway compression..
There are several limitations to our study. First, we enrolled a convenience sample of pediatric patients in an urban, tertiary, academic children’s hospital. Although the APR demonstrates strong internal validation, it may not be robust to change in measurement methods or clinical practice in other settings; as with all CPRs, external validation is needed.17, 34 We believe there is reason for optimism that this instrument will externally validate sufficiently to improve patient care and resource utilization. In this regard, a secondary outcome variable used for APR modeling was the decision of the clinical team for hospitalization. This included the decision-making of a large number of emergency medicine and pediatric emergency medicine attending physicians. This feature may reflect widely-applicable clinical practice and enhance external validity. Second, although the APR includes variables available at the bedside, calculating the probability of hospitalization using either the full-model nomograms or the underlying algebraic formulae may be cumbersome. We acknowledge that the full-model APR will be of greatest utility as a component of electronic decision-support. Finally, we have not demonstrated whether the APR will improve clinical outcomes or resource utilization, and the next step is an impact analysis to examine the effect of the APR on these important outcomes.34, 37
In summary, we developed an APR using predictor variables that are clinically intuitive and available at the bedside at the time of triage. The APR has the potential to facilitate expeditious triage, hospitalization and disposition decisions for pediatric patients with acute asthma exacerbations and may thus improve acute management and resource utilization. External validation and an impact analysis of the APR are the next steps before incorporation of this instrument into electronic decision-support.
Supplementary Material
HIGHLIGHTS BOX.
What is already known about this topic?
Clinicians have limited tools to inform asthma hospitalization decisions.
The predictive validity of available acute asthma severity scores is inadequate to justify use for hospitalization decisions.
An effective clinical prediction rule might facilitate hospitalization decision-making.
What does this article add to our knowledge?
We have developed and internally validated an Asthma Prediction Rule (APR) for need for hospitalization using predictor variables readily available before treatment.
SpO2 and expiratory prolongation were most strongly associated with need for hospitalization.
How does this study impact current management guidelines?
The APR might facilitate hospitalization decisions for children with acute asthma exacerbations and improve resource utilization.
External validation and an impact analysis are next steps before incorporation of the APR into routine decision-support.
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the nurses, respiratory therapists and other staff of the Vanderbilt Children’s Hospital Emergency Department.
Role of the Funding Source
The study was funded by the National Institutes of Health (K23 HL80005, Dr. Arnold), NIAID (K24 AI77930, Dr. Hartert) and NCRR [UL1 RR024975] (Vanderbilt CTSA). The design, analysis and writing of this report are entirely the work and responsibility of the authors, and Dr. Arnold had full access to all data and final responsibility for the decision to submit this work for publication.
Abbreviations
- AAIRS
acute asthma intensity research score
- APR
asthma prediction rule
- BMI
body mass index
- CCS
corticosteroid
- CPR
clinical prediction rule
- df:
degrees of freedom
- ED
emergency department
- eNO
exhaled nitric oxide
- %FEV1
%-predicted forced expiratory volume in 1 second
- GINA
global initiative for asthma
- IQR
inter-quartile range
- PCCU
pediatric critical care unit
- PED
pediatric emergency department
- PMLE
penalized maximum likelihood estimation
- SpO2
oxygen saturation by pulse oximetry
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, et al. Trends in asthma prevalence, health care use, and mortality in the United States, 2001-2010. NCHS Data Brief. 2012:1–8. [PubMed] [Google Scholar]
- 2.Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980-2007. Pediatrics. 2009;123(Suppl 3):S131–45. doi: 10.1542/peds.2008-2233C. [DOI] [PubMed] [Google Scholar]
- 3.Lemanske RF, Jr., Busse WW. Asthma: clinical expression and molecular mechanisms. J.Allergy Clin.Immunol. 2010;125:S95–102. doi: 10.1016/j.jaci.2009.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spiteri MA, Cook DG, Clarke SW. Reliability of eliciting physical signs in examination of the chest. Lancet. 1988;1:873–5. doi: 10.1016/s0140-6736(88)91613-3. [DOI] [PubMed] [Google Scholar]
- 5.van der Windt DA, Nagelkerke AF, Bouter LM, Dankert-Roelse JE, Veerman AJ. Clinical scores for acute asthma in pre-school children. A review of the literature. J.Clin.Epidemiol. 1994;47:635–46. doi: 10.1016/0895-4356(94)90211-9. [DOI] [PubMed] [Google Scholar]
- 6.Bekhof J, Reimink R, Brand PLP. Systematic review: Insufficient validation of clinical scores for the assessment of acute dyspnoea in wheezing children. Paediatric respiratory reviews. 2014;15:98–112. doi: 10.1016/j.prrv.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Ducharme FM, Kramer MS. Relapse following emergency treatment for acute asthma: can it be predicted or prevented? J.Clin.Epidemiol. 1993;46:1395–402. doi: 10.1016/0895-4356(93)90139-r. [DOI] [PubMed] [Google Scholar]
- 8.Stiell IG. In: Injury control: research and program evaluation. Cambridge University Press; Cambridge, UK: 2001. The Development of Clinical Decision Rules for Injury Care; pp. 217–35. [Google Scholar]
- 9.Laupacis A, Sekar N, Stiell IG. Clinical prediction rules. A review and suggested modifications of methodological standards. JAMA. 1997;277:488–94. [PubMed] [Google Scholar]
- 10.Maguire JL, Kulik DM, Laupacis A, Kuppermann N, Uleryk EM, Parkin PC. Clinical prediction rules for children: a systematic review. Pediatrics. 2011;128:e666–77. doi: 10.1542/peds.2011-0043. [DOI] [PubMed] [Google Scholar]
- 11.Harrell F. Regression modeling strategies : with applications to linear models, logistic regression, and survival analysis. Springer; New York: 2001. [Google Scholar]
- 12.Steyerberg EW. Clinical Prediction Models: A Practical Approach to Development, Validation, and Updating. Springer; New York: 2009. [Google Scholar]
- 13.Arnold DH, Gebretsadik T, Abramo TJ, Sheller JR, Resha DJ, Hartert TV. The Acute Asthma Severity Assessment Protocol (AASAP) study: objectives and methods of a study to develop an acute asthma clinical prediction rule. Emerg Med J. 2012;29:444–50. doi: 10.1136/emj.2010.110957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arnold DH, Gebretsadik T, Abramo TJ, Hartert TV. Noninvasive testing of lung function and inflammation in pediatric patients with acute asthma exacerbations. J Asthma. 2012;49:29–35. doi: 10.3109/02770903.2011.637599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arnold DH, Gebretsadik T, Sheller JR, Abramo TJ, Hartert TV. Accessory muscle use in pediatric patients with acute asthma exacerbations. Ann Allergy Asthma Immunol. 2011;106:344–6. doi: 10.1016/j.anai.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arnold DH, Saville BR, Wang W, Hartert TV. Performance of the Acute Asthma Intensity Research Score (AAIRS) for acute asthma research protocols. Ann Allergy Asthma Immunol. 2012;109:78–9. doi: 10.1016/j.anai.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stiell IG, Wells GA. Methodologic standards for the development of clinical decision rules in emergency medicine. Ann.Emerg.Med. 1999;33:437–47. doi: 10.1016/s0196-0644(99)70309-4. [DOI] [PubMed] [Google Scholar]
- 18.Montgomery K. Clinical judgment and the practice of medicine. Oxford University Press; Oxford: 2006. How Doctors Think. [Google Scholar]
- 19.Ducharme FM, Chalut D, Plotnick L, Savdie C, Kudirka D, Zhang X, et al. The Pediatric Respiratory Assessment Measure: A Valid Clinical Score for Assessing Acute Asthma Severity from Toddlers to Teenagers. The Journal of pediatrics. 2008;152:476–80. doi: 10.1016/j.jpeds.2007.08.034. e1. [DOI] [PubMed] [Google Scholar]
- 20.Gorelick MH, Stevens MW, Schultz TR, Scribano PV. Performance of a novel clinical score, the Pediatric Asthma Severity Score (PASS), in the evaluation of acute asthma. Acad.Emerg.Med. 2004;11:10–8. doi: 10.1197/j.aem.2003.07.015. [DOI] [PubMed] [Google Scholar]
- 21.Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–9. doi: 10.1016/s0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- 22.Steyerberg EW, Eijkemans MJ, Harrell FE, Jr., Habbema JD. Prognostic modeling with logistic regression analysis: in search of a sensible strategy in small data sets. Med Decis Making. 2001;21:45–56. doi: 10.1177/0272989X0102100106. [DOI] [PubMed] [Google Scholar]
- 23.Steyerberg EW, Eijkemans MJ, Habbema JD. Stepwise selection in small data sets: a simulation study of bias in logistic regression analysis. J Clin Epidemiol. 1999;52:935–42. doi: 10.1016/s0895-4356(99)00103-1. [DOI] [PubMed] [Google Scholar]
- 24.Harrell FE, Jr., Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–87. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 25.Steyerberg EW, Eijkemans MJC, Harrell FE, Habbema JDF. Prognostic modelling with logistic regression analysis: a comparison of selection and estimation methods in small data sets. Statistics in Medicine. 2000;19:1059–79. doi: 10.1002/(sici)1097-0258(20000430)19:8<1059::aid-sim412>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 26.Freedman DA. On The So-Called “Huber Sandwich Estimator” and “Robust Standard Errors”. The American Statistician. 2006;60:299–302. [Google Scholar]
- 27.Lin DY, Wei LJ. The Robust Inference for the Cox Proportional Hazards Model. Journal of the American Statistical Association. 1989;84:1074–8. [Google Scholar]
- 28.Justice AC, Covinsky KE, Berlin JA. Assessing the generalizability of prognostic information. Ann Intern Med. 1999;130:515–24. doi: 10.7326/0003-4819-130-6-199903160-00016. [DOI] [PubMed] [Google Scholar]
- 29.R Core Team . R: A language and Environment for Statistical Computing. Vienna, Austria: 2014. Available at http://www.r-project.org/. [Google Scholar]
- 30.Harrell FE., Jr. rms: S functions for biostatistical/epidemiological modeling, testing, estimation, validation, graphics, prediction, and typesetting by storing enhanced model design attributes in the fit. R Foundation for Statistical Computing; Vienna, Austria: 2009. [Google Scholar]
- 31.Moons KG, Donders AR, Steyerberg EW, Harrell FE. Penalized maximum likelihood estimation to directly adjust diagnostic and prognostic prediction models for overoptimism: a clinical example. J Clin Epidemiol. 2004;57:1262–70. doi: 10.1016/j.jclinepi.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 32.NIH NIH Policy on Reporting Race and Ethnicity Data. Subjects in Clinical Research. 2001 (NOT-OD-01-053) [Google Scholar]
- 33.Global Initiative for Asthma Global strategy for asthma management and prevention. 2014 Available from www.ginaasthma.org. [Google Scholar]
- 34.Wasson JH, Sox HC, Neff RK, Goldman L. Clinical prediction rules. Applications and methodological standards. N Engl J Med. 1985;313:793–9. doi: 10.1056/NEJM198509263131306. [DOI] [PubMed] [Google Scholar]
- 35.Steyerberg EW, Harrell FE, Jr., Borsboom GJ, Eijkemans MJ, Vergouwe Y, Habbema JD. Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol. 2001;54:774–81. doi: 10.1016/s0895-4356(01)00341-9. [DOI] [PubMed] [Google Scholar]
- 36.Scarfone RJ, Zorc JJ, Capraro GA. Patient self-management of acute asthma: adherence to national guidelines a decade later. Pediatrics. 2001;108:1332–8. doi: 10.1542/peds.108.6.1332. [DOI] [PubMed] [Google Scholar]
- 37.Reilly BM, Evans AT. Translating clinical research into clinical practice: impact of using prediction rules to make decisions. Ann Intern Med. 2006;144:201–9. doi: 10.7326/0003-4819-144-3-200602070-00009. [DOI] [PubMed] [Google Scholar]
- 38.Arnold DH, Jenkins CA, Hartert TV. Noninvasive assessment of asthma severity using pulse oximeter plethysmograph estimate of pulsus paradoxus physiology. BMC Pulm Med. 2010;10:17. doi: 10.1186/1471-2466-10-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arnold DH, Spiro DM, Desmond RA, Hagood JS. Estimation of airway obstruction using oximeter plethysmograph waveform data. Respir.Res. 2005;6:65. doi: 10.1186/1465-9921-6-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.