Abstract
Objectives:
For the first time ever, as emphasized by inclusion in the Healthy People 2020 goals, sleep health is an emphasis of national health aims. The National Healthy Sleep Awareness Project (NHSAP) was tasked to propose questions for inclusion in the next Behavioral Risk Factor Surveillance System (BRFSS), a survey that includes a number of questions that target behaviors thought to impact health, as a means to measure community sleep health. The total number of questions could not exceed five, and had to include an assessment of the risk for obstructive sleep apnea (OSA).
Methods:
An appointed workgroup met via teleconference and face-to-face venues to develop an inventory of published survey questions being used to identify sleep health, to develop a framework on which to analyze the strengths and weaknesses of current survey questions concerning sleep, and to develop recommendations for sleep health and disease surveillance questions going forward.
Results:
The recommendation was to focus on certain existing BRFSS questions pertaining to sleep duration, quality, satisfaction, daytime alertness, and to add to these other BRFSS existing questions to make a modified STOP-BANG questionnaire (minus the N for neck circumference) to assess for risk of OSA.
Conclusions:
Sleep health is an important dimension of health that has previously received less attention in national health surveys. We believe that 5 questions recommended for the upcoming BRFSS question banks will assist as important measures of sleep health, and may help to evaluate the effectiveness of interventions to improve sleep health in our nation.
Citation:
Morgenthaler TI, Croft JB, Dort LC, Loeding LD, Mullington JM, Thomas SM. Development of the National Healthy Sleep Awareness Project sleep health surveillance questions. J Clin Sleep Med 2015;11(9):1057–1062.
Keywords: healthy sleep awareness, Healthy People 2020
To promote optimal health and prevent illness, the US Department of Health and Human Services recommends that Americans “…Eat smart, exercise regularly, and get routine health screenings. Be an active participant in managing your health. Start leading a healthy lifestyle.”1 While this advice includes quitting smoking, limiting alcohol, and cutting back on risky behaviors, it says nothing about sleep—most likely because national and state-level sleep surveillance data have not been as available as the other risk behaviors. However, there is growing appreciation for the importance of sleep in health maintenance and disease prevention. Healthy People 2020 added topics on sleep, including the intent to increase public knowledge of how adequate sleep and treatment of sleep disorders improve health, productivity, wellness, quality of life; it also includes topics on safety in the workplace and on the roads.2 With the intention of facilitating the attainment of these goals, in 2013 the Centers for Disease Control and Prevention (CDC) partnered with two professional societies for sleep, the American Academy of Sleep Medicine and the Sleep Research Society, to create the National Healthy Sleep Awareness Project (NHSAP). Details of the project's activities can be found at http://www.sleepeducation.com/healthysleep/about-the-national-healthy-sleep-awareness-project/.
One of the central missions of the NHSAP is to improve surveillance of sleep health in America, and as such, the NHSAP Surveillance and Epidemiology Workgroup, comprised of the authors, was formed and tasked to propose questions for inclusion in the next Behavioral Risk Factor Surveillance System (BRFSS), a survey that includes a number of questions that target behaviors thought to impact health.3 The NHSAP chose to work to propose questions for inclusion in the BRFSS rather than another survey because it is conducted by telephone interview in all 50 states, District of Columbia, and the territories, and therefore achieves a demographically representative sampling of Americans. It is a very well-established, government-supported, annual surveillance tool, with a high standard of quality control of test questions, having been used in surveillance since 1984. The BRFSS has grown from approximately 100,000 telephone interviews in 1993, to over 500,000 per year at this time.
The BRFSS has included a sleep question since 1995, “During the past 30 days, for about how many days have you felt you did not get enough rest or sleep?,” and sleep questions are in the list of “core” questions asked on alternating years. Since 2009, an optional sleep module has been included that asks, “On average, how many hours of sleep do you get in a 24-hour period?”, “Do you snore?”, “During the past 30 days, for about how many days did you find yourself unintentionally falling asleep during the day?”; “During the past 30 days, have you ever nodded off or fallen asleep, even just for a brief moment, while driving?”
The BRFSS is conducted at state level to monitor prevalence of behaviors known or suspected to be associated with premature morbidity and mortality, and to characterize regional specific needs for targeted health awareness programs development and/or introduction. Further, once health risks are identified and interventions are developed and applied, the BRFSS can be used to evaluate the outcomes and the comparative effectiveness of interventional programs. For a new question to be included, a committee of professionals with expertise in the area of test development must screen the BRFSS question. Very few questions can be included each year because the BRFSS encompasses a large inventory of behaviors, space for questions is competitive, and they must be evidence-based. In addition, once sufficient evidence exists to warrant inclusion of a behavior for surveillance, it needs to be tested further and shown to be valid in order to maintain its inclusion.
The NHSAP Surveillance and Epidemiology Workgroup was specifically tasked to develop no more than five standardized survey questions that would assist in evaluating sleep health and risk for obstructive sleep apnea syndrome (OSA) for potential inclusion in the BRFSS. The rationale for and process by which questions were selected to propose to the BRFSS selection committee by the NHSAP is described below, followed by a description of next steps and future perspectives.
DEVELOPMENT PROCESS
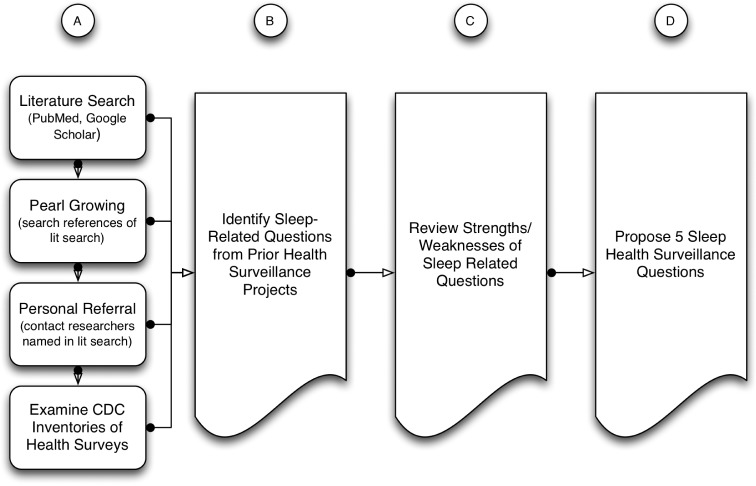
The Workgroup met via teleconference monthly and via face-to-face meetings on three occasions. The work progressed in four stages: (A) perform a search for prior population health surveys that included sleep-related questions, (B) develop an inventory of current instruments being used to identify sleep health and disease, (C) extract a list of prior sleep related questions from existing sleep health-related surveillance data, (D) determine a framework on which to analyze the strengths and weaknesses of current survey questions concerning sleep, and develop recommendations for sleep health and disease surveillance going forward (see Figure 1). Due to the required economies involved in national surveillance programs, the Workgroup was asked to identify no more than five questions to be used in the surveillance project. We jointly determined it would be desirable, where possible, to use established sleep health questions for two reasons: (a) data could be trended over longer periods of time by making use of prior survey data, and (b) time and money would be saved by avoiding the need to re-validate and address the question approval process for national surveys.
Figure 1. Overview of the sleep health surveillance question development process.
Inventory of Current Instruments
We began by identifying and evaluating current surveys and datasets with a sleep related component, including but not limited to those that have been previously administered by the CDC. We searched the medical literature using PubMed and Google Scholar, and conducted an updated review of the surveys reported in the National Heart, Lung, and Blood Institute (NHLBI) National Center on Sleep Disorders Research Guide to Selected Publicly Available Sleep-Related Data Resources.4 A literature search for articles including sleep related surveillance data was conducted using the title of the survey (e.g., Behavioral Risk Factor Surveillance System) and the following keywords in the title or abstract of the publication: sleep, duration, satisfaction, quality, or apnea. The search was limited to studies that were done in humans and published in the English language. The databases were searched on September 5, 2014, with no starting publication date restrictions. In addition to the search, we augmented our inventory by pearl growing (examining the articles referenced in those studies located by the formal literature search for relevance), by examining inventories of health surveys maintained by the CDC, and by interviewing personal sleep experts and public health contacts. Using the search results (Figure 1A), we compiled an inventory of surveys—and in particular, of the sleep related questions used in currently administered health surveillance surveys (Figure 1B). This yielded a large number of questions related in various ways to sleep duration, sleep quality, sleep satisfaction, symptoms of OSA, daytime sleepiness, daytime fatigue, etc. (Figures 1C and 2).
Figure 2. Review scheme and results of review.
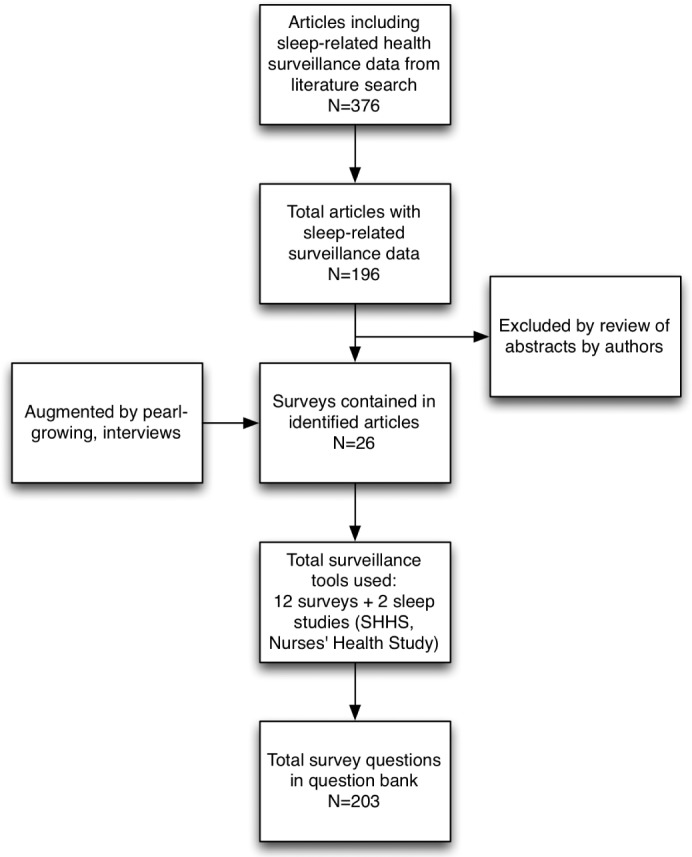
Our search yielded 376 publications that used health surveillance data containing sleep related questions. The following search results were found for each survey name coupled with the term sleep in the title/abstract: Behavioral Risk Factor Surveillance System (41 articles), Youth Risk Behavior Survey (12 articles), National Health Interview Survey (33 articles), National Health and Nutrition Examination Survey (67 articles), National Survey of Children's Health (10 articles), National Comorbidity Survey (16 articles), American Time Use Survey (5 articles), PatientsLikeMe Survey (1 article), Sleep In America Poll/National Sleep Foundation (21 articles), Pregnancy Risk Assessment Monitoring System (15 articles), National Survey of Early Childhood Health (2 articles), Nurses' Health Study (21 articles), General Social Survey (2 articles), Sleep Heart Health Study (130 articles). A further refined search coupled the survey name with the terms sleep duration, satisfaction, quality, or apnea which overlapped the original results. A complete list of returned references is provided in the supplemental material.
Framework for Analyzing Sleep Health
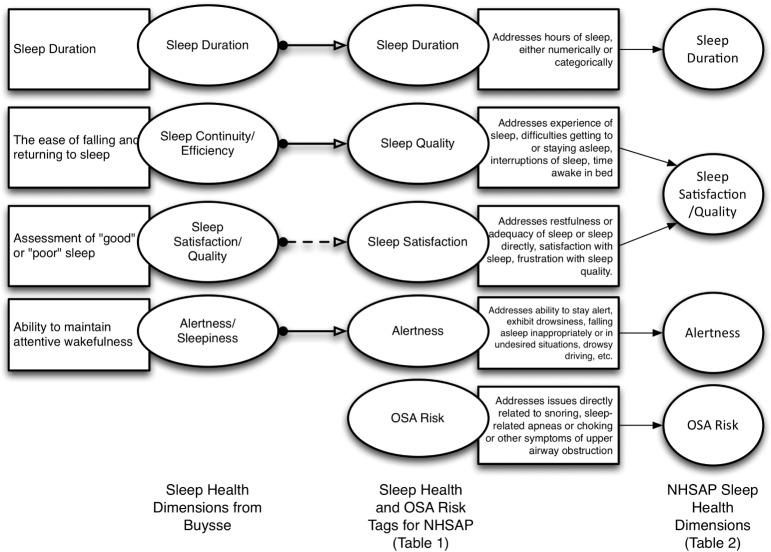
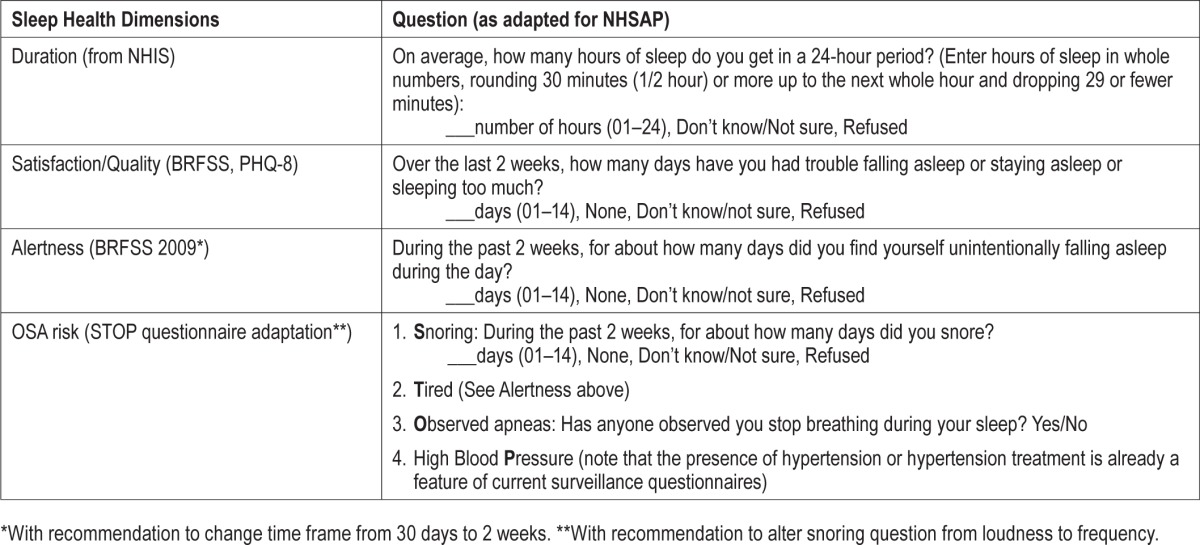
Although there have recently been at least two expert conferences convened to determine normative data for healthy sleep duration, sleep duration is only one aspect of sleep health,5–7 and there are currently no widely accepted constructs defining a more comprehensive way of assessing sleep health. In order to evaluate the usefulness of the sleep related questions found from our search as indicators for sleep health, we needed to come to consensus regarding the desirable elements of sleep health. We found the dimensions of sleep health described and justified by Buysse compelling: sleep duration, sleep continuity or efficiency, sleep timing, alertness/sleepiness, and sleep satisfaction/quality.8 Our question inventory from the search above was first qualitatively examined to look for similarities and differences between the existing question and these dimensions of sleep health. We found significant but incomplete overlap. For example, many existing survey questions attempt to ascertain a measure of sleep duration, although the actual questions vary. Alertness/sleepiness were assessed by some questions in surveys, but not using identical questions. In contrast, the concept of sleep satisfaction/quality described by Buysse as “the subjective assessment of ‘good’ or ‘poor’ sleep” was not directly asked in the existing question bank at all, though some questions alluded to the refreshing or the disrupted nature of sleep. Using this, we determined that we would use five general categories with which to tag the existing survey questions as we reviewed them: sleep duration, sleep quality, sleep satisfaction, alertness, and OSA risk (Table 1, Figure 3).
Table 1.
National Healthy Sleep Awareness Project sleep health categories for tagging survey questions.
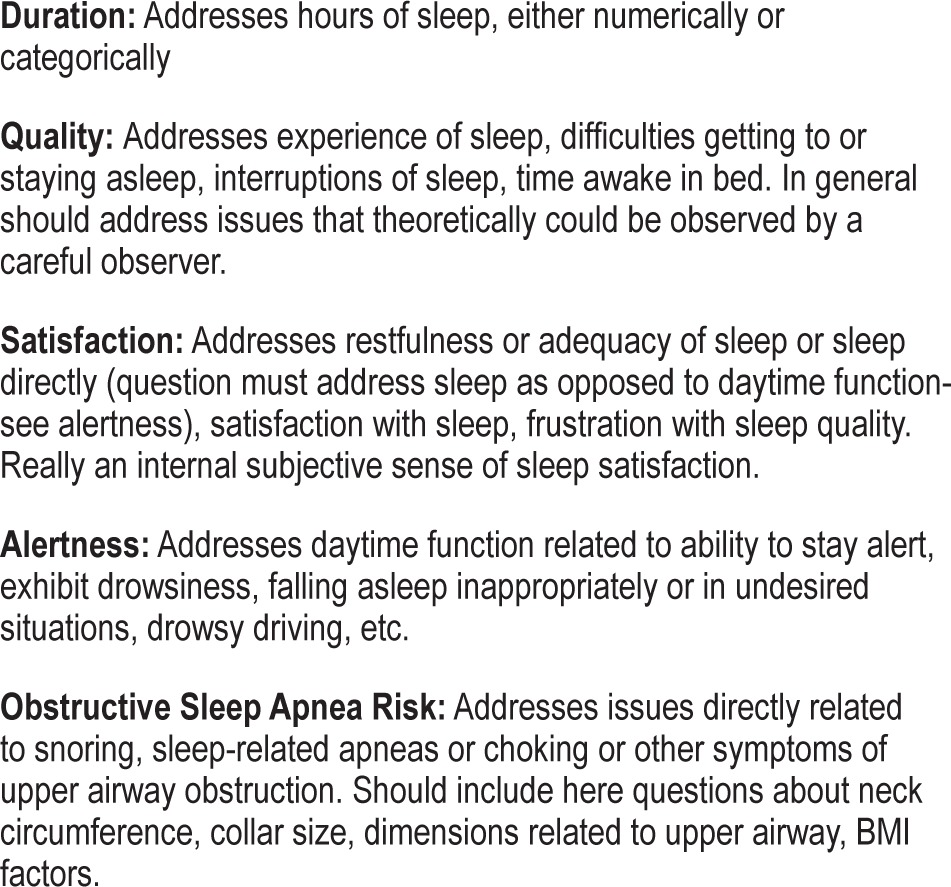
Figure 3. Moving from sleep dimensions of Buysse to NHSAP sleep health dimensions.
We specifically considered whether or not to include questions about segmented sleep or sleep timing, one of Buysse's sleep health dimensions, in our development of survey questions. Existing questions pertaining to the sleep timing dimension would certainly be altered by whether or not the surveyed participant was involved in shift work or not, making comparison over time important but challenging. In addition, we needed to economize in order to remain within our allotment for five questions. Therefore, although circadian timing of sleep and its segmentation are very important, we decided to forego questions focusing on sleep timing for this iteration of question development.
Analysis of the Question Bank
The Workgroup members next constructed a data table, tagging questions in the question bank according to the NHSAP Sleep Health Categories (Table 1). For each question, we also noted the number of publications using that question, which population(s) was being addressed, and health outcomes that had been linked or evaluated in the context of those questions. Using these data, the Workgroup discussed the limitations and disadvantages of the current questions in view of our goal and the sleep health construct.
From this analysis, we decided to adapt questions from the National Health Interview Survey (NHIS) related to duration, from the BRFSS/Personal Health Questionnaire (PHQ-8) to form a combined dimension of sleep satisfaction/quality, and from the BRFSS to determine aspects of alertness (Table 2, Figure 3).
Table 2.
National Healthy Sleep Awareness Project question recommendations.
The Special Problem of Assessing for the Risk of Obstructive Sleep Apnea
The clinical risk factors for and symptoms of obstructive sleep apnea syndrome are well described. However, none alone are sufficiently sensitive or specific to rightly assign a risk for OSA. Because of this, many clinical prediction rules have been developed to guide clinicians in their ability to stratify risk for OSA. For population surveys, we needed to depend upon self-answered questions and to minimize the number of such questions used. Surveying for sleep duration, satisfaction/quality, and alertness consumed three of our five questions, leaving us room for two more questions in our survey question proposal. We agreed that using elements of the STOP questionnaire would be most advantageous (Table 2). Other questions in the BRFSS question bank already assess for hypertension (the “P” in STOP is for high blood pressure). Therefore, we reasoned that if our survey questions addressed Snoring, Tiredness, and Observed apneas, we could construct some inferences regarding the relative risk for OSA in survey respondents.
THE NHSAP SLEEP HEALTH QUESTIONS
Utilizing an informal consensus process and including the considerations above, we have selected the questions shown in Table 2. We arrived at these questions by following these principles:
When possible, use existing questions from prior surveys. This reduces question development time and costs and allows comparison of answers across longer periods of time.
Select questions that, as much as possible, correspond to a construct descriptive of sleep health across several dimensions, inclusive of sleep duration, timing, restorative quality, and satisfaction.
Select questions that will help stratify risk for OSA.
Select no more than 5 questions (a design parameter provided by the CDC).
The selected questions do satisfy these design features.
LIMITATIONS
This is a very ambitious project, and there are many potential limitations to our approach. First, without significant and validated prior measurement of sleep health across many dimensions, this must be considered an initial effort. Prior validated instruments which assess sleep quality (e.g., the Pittsburgh Sleep Quality Index, Calgary Sleep Apnea Quality of Life) require many more questions and are often disease-specific. There is no doubt that choosing and using only a limited number of questions will leave many questions about sleep health unanswered. There are also few data to determine if the particular dimensions of sleep quality chosen are most correlated with the biosocial consequences of “poor” sleep. Hopefully, however, these questions, which address several dimensions of sleep, will serve to begin a more general understanding of sleep health in the United States.
The decision to reduce the amount of time from 30 days to two weeks in the sleep alertness question might be considered a limitation of the chosen approach, as it deviates from the historically used time frame included in the BRFSS for these questions. However, it was considered that it would be preferable to keep the time frame consistent across all questions. As the satisfaction question is based on two weeks, and recall is generally more accurate for this timeframe, the Workgroup chose to recommend using it consistently. Another item that was adopted but in a different form than previously used is the snoring item. Due to evidence presented by Caffo et al.9 that showed that snoring frequency had more importance than snoring loudness in the prediction of respiratory disturbance index (RDI), the Work-group decided to recommend the frequency item for inclusion.
Limitations of current surveillance surveys to assess sleep health include that the information obtained is retrospective and has potential for recall bias. Furthermore, the questions often assess sleep related complaints, which may be open to interpretation and could reflect a variety of underlying sleep disorders. Because large annual population surveys such as the NHIS and BRFSS are very expensive, time-limited, and do not allow a clinical examination, surveillance information on sleep health and sleep disorders is a subjective self-report and has no objective measurement for clinical validation. In population surveys such as the National Health and Nutrition Examination Survey (NHANES), which do include a physical examination, the use of either polysomnography or actigraphy is prohibitive in terms of cost, time limitations, and respondents' willingness to participate over more than one assessment day.
A major strength of current CDC surveillance surveys is that respondents represent the general population in contrast to participants selected according to specific inclusion-exclusion criteria in clinical studies. Therefore, the survey population is much more representative of the actual patient population that enters a physician's office with sleep complaints. An additional strength is the large sample sizes obtained for CDC surveillance surveys such as the NHIS, NHANES, BRFSS, and Youth Risk Behavior Survey (YRBS); this allows statistical power to assess disparities between groups defined by age, race/ethnicity, gender, educational attainment, income, and in some cases geography, that clinical studies cannot assess. Furthermore, each question represents a simple one-time measure of sleep disturbance that will permit analysis of secular trends.
NEXT STEPS AND RECOMMENDATIONS FOR FURTHER DEVELOPMENT
These questions have been proposed and accepted for implementation in the BRFSS surveillance system. This is a formal process that involves presentation of the new questions for review by the BRFSS state coordinators. If selected for inclusion into a survey cycle, the questions then also undergo cognitive testing by an external group, and the process may also involve slight revisions of each question.
Selecting “good” questions that can be included in an existing survey without further evaluation increases the likelihood of their inclusion in the near future. “A good question is one that produces answers that are reliable and valid measures of something we want to describe.”10 Questions must be asked and understood in a consistent manner, whether read by the respondents or read aloud by an interviewer. They should elicit the kind of answers that researchers want and expect. Questions should be ones that all respondents will have an answer to and are willing to answer. Evaluation studies are conducted to determine if the question captures the intended concept and is interpreted consistently over the range of demographic groups included in the survey.
A variety of quantitative and qualitative methods are used to ensure the questions produce valid answers with minimum measurement error.11 Cognitive interviewing is the primary method used by the Questionnaire Design Research Laboratory (QDRL) of the CDC and other government agencies.12 Cognitive interviewing involves conducting interviews of several selected sample groups of up to approximately 50 respondents, summarizing and comparing across respondents, across groups, and then formulating conclusions about question performance. Inclusion in surveys such as the BRFSS requires that questions have been developed and evaluated according to current accepted methodology.
If selected as an optional module by the BRFSS state coordinators, then an individual state health department determines whether that state's BRFSS will add the sleep health module to their annual survey. Interest in the addition of this module could often be determined by whether the information obtained in the module will provide additional guidance for state chronic disease programs or will enhance or add value to ongoing prevention and intervention programs being implemented by organizations such as the state sleep society. Continued implementation of the sleep health module in further survey years will also be determined by the analysis, interpretation, and use of the information.
Researchers in the sleep field are encouraged to make use of the BRFSS and other CDC surveillance data and to query and publish results of analyses of sleep health and risk for morbidity and mortality in many health domains. The use of the data will ensure that this information continues to be collected and that findings get attention and consideration by decision makers and stakeholders working to improve the health and wellness of the nation.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Morgenthaler and Dr. Croft have indicated no financial conflicts of interest. Dr. Dort is Editor In Chief of the Journal of Dental Sleep Medicine, has received royalties from a patent she holds with MPowRx, and has stock in Zephyr. Dr. Mullington received a travel reimbursement from Merck. Dr. Thomas and Ms. Loeding are employees of the American Academy of Sleep Medicine. Funding for this project was provided by the American Academy of Sleep Medicine and Sleep Research Society, and by the cooperative agreement number 1U50DP004930-01 from the Centers for Disease Control and Prevention (CDC). The findings and conclusions in this report are those of the authors and do not necessarily represent the official views of the CDC.
SUPPLEMENTAL MATERIAL
Complete List of Returned References from Literature Search
Behavioral Risk Factor Surveillance System
- 1.Liu Y, Njai RS, Greenlund KJ, Chapman DP, Croft JB. Relationships between housing and food insecurity, frequent mental distress, and insufficient sleep among adults in 12 US States, 2009. Preventing chronic disease. 2014;11:E37. doi: 10.5888/pcd11.130334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scott D, Paterson JL, Happell B. Poor sleep quality in Australian adults with comorbid psychological distress and physical illness. Behavioral sleep medicine. 2014;12(4):331–341. doi: 10.1080/15402002.2013.819469. [DOI] [PubMed] [Google Scholar]
- 3.Liu Y, Wheaton AG, Chapman DP, Croft JB. Sleep duration and chronic diseases among U.S. adults age 45 years and older: evidence from the 2010 Behavioral Risk Factor Surveillance System. Sleep. 2013;36(10):1421–1427. doi: 10.5665/sleep.3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maia Q, Grandner MA, Findley J, Gurubhagavatula I. Short and long sleep duration and risk of drowsy driving and the role of subjective sleep insufficiency. Accident; analysis and prevention. 2013;59:618–622. doi: 10.1016/j.aap.2013.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Faestel PM, Littell CT, Vitiello MV, Forsberg CW, Littman AJ. Perceived insufficient rest or sleep among veterans: Behavioral Risk Factor Surveillance System 2009. J Clin Sleep Med. 2013;9(6):577–584. doi: 10.5664/jcsm.2754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lemasters T, Madhavan S, Sambamoorthi U, Kurian S. A population-based study comparing HRQoL among breast, prostate, and colorectal cancer survivors to propensity score matched controls, by cancer type, and gender. Psychooncology. 2013;22(10):2270–2282. doi: 10.1002/pon.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu Y, Croft JB, Wheaton AG, et al. Association between perceived insufficient sleep, frequent mental distress, obesity and chronic diseases among US adults, 2009 behavioral risk factor surveillance system. BMC public health. 2013;13:84. doi: 10.1186/1471-2458-13-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chapman DP, Liu Y, Presley-Cantrell LR, et al. Adverse childhood experiences and frequent insufficient sleep in 5 U.S. States, 2009: a retrospective cohort study. BMC public health. 2013;13:3. doi: 10.1186/1471-2458-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease C, Prevention. Drowsy driving - 19 states and the District of Columbia, 2009-2010. MMWR. Morbidity and mortality weekly report. 2013;61(51-52):1033–1037. [PubMed] [Google Scholar]
- 10.Mochari-Greenberger H, Mosca L. Caregiver burden and nonachievement of healthy lifestyle behaviors among family caregivers of cardiovascular disease patients. American journal of health promotion : AJHP. 2012;27(2):84–89. doi: 10.4278/ajhp.110606-QUAN-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grandner MA, Hale L, Jackson N, Patel NP, Gooneratne NS, Troxel WM. Perceived racial discrimination as an independent predictor of sleep disturbance and daytime fatigue. Behavioral sleep medicine. 2012;10(4):235–249. doi: 10.1080/15402002.2012.654548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grandner MA, Patel NP, Perlis ML, et al. Obesity, diabetes, and exercise associated with sleep-related complaints in the American population. Zeitschrift fur Gesundheitswissenschaften = Journal of public health. 2011;19(5):463–474. doi: 10.1007/s10389-011-0398-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grandner MA, Martin JL, Patel NP, et al. Age and sleep disturbances among American men and women: data from the U.S. Behavioral Risk Factor Surveillance System. Sleep. 2012;35(3):395–406. doi: 10.5665/sleep.1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grandner MA, Jackson NJ, Pigeon WR, Gooneratne NS, Patel NP. State and regional prevalence of sleep disturbance and daytime fatigue. J Clin Sleep Med. 2012;8(1):77–86. doi: 10.5664/jcsm.1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grandner MA, Jackson NJ, Pak VM, Gehrman PR. Sleep disturbance is associated with cardiovascular and metabolic disorders. J Sleep Res. 2012;21(4):427–433. doi: 10.1111/j.1365-2869.2011.00990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choudhary E, Smith M, Bossarte RM. Depression, anxiety, and symptom profiles among female and male victims of sexual violence. American journal of men's health. 2012;6(1):28–36. doi: 10.1177/1557988311414045. [DOI] [PubMed] [Google Scholar]
- 17.Grundstrom AC, Guse CE, Layde PM. Risk factors for falls and fall-related injuries in adults 85 years of age and older. Archives of gerontology and geriatrics. 2012;54(3):421–428. doi: 10.1016/j.archger.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li C, Balluz LS, Okoro CA, et al. Surveillance of certain health behaviors and conditions among states and selected local areas --- Behavioral Risk Factor Surveillance System, United States, 2009. Morbidity and mortality weekly report. Surveillance summaries. 2011;60(9):1–250. [PubMed] [Google Scholar]
- 19.Chapman DP, Wheaton AG, Perry GS, Sturgis SL, Strine TW, Croft JB. Household demographics and perceived insufficient sleep among US adults. Journal of community health. 2012;37(2):344–349. doi: 10.1007/s10900-011-9451-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wheaton AG, Perry GS, Chapman DP, McKnight-Eily LR, Presley-Cantrell LR, Croft JB. Relationship between body mass index and perceived insufficient sleep among U.S. adults: an analysis of 2008 BRFSS data. BMC public health. 2011;11:295. doi: 10.1186/1471-2458-11-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease C, Prevention. Unhealthy sleep-related behaviors--12 States, 2009. MMWR. Morbidity and mortality weekly report. 2011;60(8):233–238. [PubMed] [Google Scholar]
- 22.Shankar A, Syamala S, Kalidindi S. Insufficient rest or sleep and its relation to cardiovascular disease, diabetes and obesity in a national, multiethnic sample. PLoS ONE. 2010;5(11):e14189. doi: 10.1371/journal.pone.0014189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sabanayagam C, Shankar A. The association between active smoking, smokeless tobacco, second-hand smoke exposure and insufficient sleep. Sleep Med. 2011;12(1):7–11. doi: 10.1016/j.sleep.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grandner MA, Patel NP, Gehrman PR, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010;11(5):470–478. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease C, Prevention. Perceived insufficient rest or sleep among adults - United States, 2008. MMWR. Morbidity and mortality weekly report. 2009;58(42):1175–1179. [PubMed] [Google Scholar]
- 26.Gorman BK, Chu M. Racial and ethnic differences in adult asthma prevalence, problems, and medical care. Ethnicity & health. 2009;14(5):527–552. doi: 10.1080/13557850902954195. [DOI] [PubMed] [Google Scholar]
- 27.Chowdhury PP, Balluz L, Strine TW. Health-related quality of life among minority populations in the United States, BRFSS 2001–2002. Ethnicity & disease. 2008;18(4):483–487. [PubMed] [Google Scholar]
- 28.Centers for Disease C, Prevention. Perceived insufficient rest or sleep--four states, 2006. MMWR. Morbidity and mortality weekly report. 2008;57(8):200–203. [PubMed] [Google Scholar]
- 29.Richardson LC, Wingo PA, Zack MM, Zahran HS, King JB. Health-related quality of life in cancer survivors between ages 20 and 64 years: population-based estimates from the Behavioral Risk Factor Surveillance System. Cancer. 2008;112(6):1380–1389. doi: 10.1002/cncr.23291. [DOI] [PubMed] [Google Scholar]
- 30.Strine TW, Chapman DP, Balluz LS, Moriarty DG, Mokdad AH. The associations between life satisfaction and health-related quality of life, chronic illness, and health behaviors among U.S. community-dwelling adults. Journal of community health. 2008;33(1):40–50. doi: 10.1007/s10900-007-9066-4. [DOI] [PubMed] [Google Scholar]
- 31.Strine TW, Chapman DP, Balluz L, Mokdad AH. Health-related quality of life and health behaviors by social and emotional support. Their relevance to psychiatry and medicine. Social psychiatry and psychiatric epidemiology. 2008;43(2):151–159. doi: 10.1007/s00127-007-0277-x. [DOI] [PubMed] [Google Scholar]
- 32.Ford JD, Adams ML, Dailey WF. Factors associated with receiving help and risk factors for disaster-related distress among Connecticut adults 5–15 months after the September 11th terrorist incidents. Social psychiatry and psychiatric epidemiology. 2006;41(4):261–270. doi: 10.1007/s00127-006-0031-9. [DOI] [PubMed] [Google Scholar]
- 33.Smith DW, McFall SL. The relationship of diet and exercise for weight control and the quality of life gap associated with diabetes. J Psychosom Res. 2005;59(6):385–392. doi: 10.1016/j.jpsychores.2005.06.062. [DOI] [PubMed] [Google Scholar]
- 34.Strine TW, Hootman JM, Chapman DP, Okoro CA, Balluz L. Health-related quality of life, health risk behaviors, and disability among adults with pain-related activity difficulty. American journal of public health. 2005;95(11):2042–2048. doi: 10.2105/AJPH.2005.066225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Strine TW, Chapman DP, Kobau R, Balluz L. Associations of self-reported anxiety symptoms with health-related quality of life and health behaviors. Social psychiatry and psychiatric epidemiology. 2005;40(6):432–438. doi: 10.1007/s00127-005-0914-1. [DOI] [PubMed] [Google Scholar]
- 36.Strine TW, Okoro CA, Chapman DP, et al. Health-related quality of life and health risk behaviors among smokers. American journal of preventive medicine. 2005;28(2):182–187. doi: 10.1016/j.amepre.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 37.Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Med. 2005;6(1):23–27. doi: 10.1016/j.sleep.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 38.Smith DW. The population perspective on quality of life among Americans with diabetes. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2004;13(8):1391–1400. doi: 10.1023/B:QURE.0000040785.59444.7c. [DOI] [PubMed] [Google Scholar]
- 39.Krause JS. Factors associated with risk for subsequent injuries after traumatic spinal cord injury. Archives of physical medicine and rehabilitation. 2004;85(9):1503–1508. doi: 10.1016/j.apmr.2004.01.017. [DOI] [PubMed] [Google Scholar]
- 40.Adams ML, Ford JD, Dailey WF. Predictors of help seeking among Connecticut adults after September 11, 2001. American journal of public health. 2004;94(9):1596–1602. doi: 10.2105/ajph.94.9.1596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hathaway JE, Mucci LA, Silverman JG, Brooks DR, Mathews R, Pavlos CA. Health status and health care use of Massachusetts women reporting partner abuse. American journal of preventive medicine. 2000;19(4):302–307. doi: 10.1016/s0749-3797(00)00236-1. [DOI] [PubMed] [Google Scholar]
Youth Risk Behavior Survey
- 1.Meldrum RC, Restivo E. The behavioral and health consequences of sleep deprivation among U.S. high school students: relative deprivation matters. Preventive medicine. 2014;63:24–28. doi: 10.1016/j.ypmed.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 2.Wheaton AG, Perry GS, Chapman DP, Croft JB. Self-reported sleep duration and weight-control strategies among U.S. high school students. Sleep. 2013;36(8):1139–1145. doi: 10.5665/sleep.2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hildenbrand AK, Daly BP, Nicholls E, Brooks-Holliday S, Kloss JD. Increased risk for school violence-related behaviors among adolescents with insufficient sleep. The Journal of school health. 2013;83(6):408–414. doi: 10.1111/josh.12044. [DOI] [PubMed] [Google Scholar]
- 4.Zalsman G. Genetics of Suicidal Behavior in Children and Adolescents. In: Dwivedi Y, editor. The Neurobiological Basis of Suicide. Boca Raton, FL: CRC Press; 2012. [PubMed] [Google Scholar]
- 5.Park S, Sherry B, Foti K, Blanck HM. Self-reported academic grades and other correlates of sugar-sweetened soda intake among US adolescents. Journal of the Academy of Nutrition and Dietetics. 2012;112(1):125–131. doi: 10.1016/j.jada.2011.08.045. [DOI] [PubMed] [Google Scholar]
- 6.Lowry R, Eaton DK, Foti K, McKnight-Eily L, Perry G, Galuska DA. Association of Sleep Duration with Obesity among US High School Students. Journal of obesity. 2012;2012:476914. doi: 10.1155/2012/476914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Foti KE, Eaton DK, Lowry R, McKnight-Ely LR. Sufficient sleep, physical activity, and sedentary behaviors. American journal of preventive medicine. 2011;41(6):596–602. doi: 10.1016/j.amepre.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 8.McKnight-Eily LR, Eaton DK, Lowry R, Croft JB, Presley-Cantrell L, Perry GS. Relationships between hours of sleep and health-risk behaviors in US adolescent students. Preventive medicine. 2011;53(4-5):271–273. doi: 10.1016/j.ypmed.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 9.Kim DS, Kim HS. Early initiation of alcohol drinking, cigarette smoking, and sexual intercourse linked to suicidal ideation and attempts: findings from the 2006 Korean Youth Risk Behavior Survey. Yonsei medical journal. 2010;51(1):18–26. doi: 10.3349/ymj.2010.51.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Brien EM, Mindell JA. Sleep and risk-taking behavior in adolescents. Behavioral sleep medicine. 2005;3(3):113–133. doi: 10.1207/s15402010bsm0303_1. [DOI] [PubMed] [Google Scholar]
- 11.Roberts RE, Lee ES, Hemandez M, Solari AC. Symptoms of insomnia among adolescents in the lower Rio Grande Valley of Texas. Sleep. 2004;27(4):751–760. doi: 10.1093/sleep/27.4.751. [DOI] [PubMed] [Google Scholar]
- 12.Eisenmann JC. Secular trends in variables associated with the metabolic syndrome of North American children and adolescents: a review and synthesis. American journal of human biology : the official journal of the Human Biology Council. 2003;15(6):786–794. doi: 10.1002/ajhb.10214. [DOI] [PubMed] [Google Scholar]
National Health Interview Survey
- 1.Donat M, Brown C, Williams N, et al. Linking sleep duration and obesity among black and white US adults. Clinical practice. 2013;10(5) doi: 10.2217/cpr.13.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jackson CL, Redline S, Kawachi I, Hu FB. Association between sleep duration and diabetes in black and white adults. Diabetes care. 2013;36(11):3557–3565. doi: 10.2337/dc13-0777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jackson CL, Redline S, Kawachi I, Williams MA, Hu FB. Racial disparities in short sleep duration by occupation and industry. American journal of epidemiology. 2013;178(9):1442–1451. doi: 10.1093/aje/kwt159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brimah P, Oulds F, Olafiranye O, et al. Sleep duration and reported functional capacity among black and white US adults. J Clin Sleep Med. 2013;9(6):605–609. doi: 10.5664/jcsm.2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Theis KA, Murphy L, Hootman JM, Wilkie R. Social participation restriction among US adults with arthritis: a population-based study using the International Classification of Functioning, Disability and Health. Arthritis care & research. 2013;65(7):1059–1069. doi: 10.1002/acr.21977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arlinghaus A, Lombardi DA, Willetts JL, Folkard S, Christiani DC. A structural equation modeling approach to fatigue-related risk factors for occupational injury. American journal of epidemiology. 2012;176(7):597–607. doi: 10.1093/aje/kws219. [DOI] [PubMed] [Google Scholar]
- 7.Stipelman BA, Augustson E, McNeel T. The relationship among smoking, sleep, and chronic rheumatic conditions commonly associated with pain in the National Health Interview Survey. J Behav Med. 2013;36(5):539–548. doi: 10.1007/s10865-012-9447-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lombardi DA, Wirtz A, Willetts JL, Folkard S. Independent effects of sleep duration and body mass index on the risk of a work-related injury: evidence from the US National Health Interview Survey (2004-2010) Chronobiology international. 2012;29(5):556–564. doi: 10.3109/07420528.2012.675253. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease C, Prevention. Short sleep duration among workers--United States, 2010. MMWR. Morbidity and mortality weekly report. 2012;61(16):281–285. [PubMed] [Google Scholar]
- 10.Wirtz A, Lombardi DA, Willetts JL, Folkard S, Christiani DC. Gender differences in the effect of weekly working hours on occupational injury risk in the United States working population. Scandinavian journal of work, environment & health. 2012;38(4):349–357. doi: 10.5271/sjweh.3295. [DOI] [PubMed] [Google Scholar]
- 11.Anderson JG, Taylor AG. Use of complementary therapies for cancer symptom management: results of the 2007 National Health Interview Survey. Journal of alternative and complementary medicine. 2012;18(3):235–241. doi: 10.1089/acm.2011.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zizi F, Pandey A, Murrray-Bachmann R, et al. Race/ethnicity, sleep duration, and diabetes mellitus: analysis of the National Health Interview Survey. The American journal of medicine. 2012;125(2):162–167. doi: 10.1016/j.amjmed.2011.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sabanayagam C, Shankar A. Sleep duration and hypercholesterolaemia: Results from the National Health Interview Survey 2008. Sleep Med. 2012;13(2):145–150. doi: 10.1016/j.sleep.2011.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goral A, Lipsitz JD, Muhsen K, Gross R. Depressive symptoms, risk factors and sleep in asthma: results from a national Israeli health survey. Gen Hosp Psychiatry. 2012;34(1):17–23. doi: 10.1016/j.genhosppsych.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 15.Krueger PM, Saint Onge JM, Chang VW. Race/ethnic differences in adult mortality: the role of perceived stress and health behaviors. Social science & medicine. 2011;73(9):1312–1322. doi: 10.1016/j.socscimed.2011.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shankar A, Charumathi S, Kalidindi S. Sleep duration and self-rated health: the national health interview survey 2008. Sleep. 2011;34(9):1173–1177. doi: 10.5665/SLEEP.1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Louie GH, Tektonidou MG, Caban-Martinez AJ, Ward MM. Sleep disturbances in adults with arthritis: prevalence, mediators, and subgroups at greatest risk. Data from the 2007 National Health Interview Survey. Arthritis care & research. 2011;63(2):247–260. doi: 10.1002/acr.20362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sabanayagam C, Shankar A. Sleep duration and cardiovascular disease: results from the National Health Interview Survey. Sleep. 2010;33(8):1037–1042. doi: 10.1093/sleep/33.8.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schoenborn CA, Adams PE. Health behaviors of adults: United States, 2005-2007. Vital and health statistics. Series 10, Data from the National Health Survey. 2010;(245):1–132. [PubMed] [Google Scholar]
- 20.Lombardi DA, Folkard S, Willetts JL, Smith GS. Daily sleep, weekly working hours, and risk of work-related injury: US National Health Interview Survey (2004-2008) Chronobiology international. 2010;27(5):1013–1030. doi: 10.3109/07420528.2010.489466. [DOI] [PubMed] [Google Scholar]
- 21.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Social science & medicine. 2010;71(5):1027–1036. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 22.Luckhaupt SE, Tak S, Calvert GM. The prevalence of short sleep duration by industry and occupation in the National Health Interview Survey. Sleep. 2010;33(2):149–159. doi: 10.1093/sleep/33.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hale L, Rivero-Fuentes E. Negative acculturation in sleep duration among Mexican immigrants and Mexican Americans. Journal of immigrant and minority health / Center for Minority Public Health. 2011;13(2):402–407. doi: 10.1007/s10903-009-9284-1. [DOI] [PubMed] [Google Scholar]
- 24.Krueger PM, Friedman EM. Sleep duration in the United States: a cross-sectional population-based study. American journal of epidemiology. 2009;169(9):1052–1063. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wetzler H. Responses to the result of the National Health Interview Survey on sleep duration among Black and White Americans. Journal of the National Medical Association. 2008;100(7):868. doi: 10.1016/s0027-9684(15)31386-9. [DOI] [PubMed] [Google Scholar]
- 26.Nunes J, Jean-Louis G, Zizi F, et al. Sleep duration among black and white Americans: results of the National Health Interview Survey. Journal of the National Medical Association. 2008;100(3):317–322. doi: 10.1016/s0027-9684(15)31244-x. [DOI] [PubMed] [Google Scholar]
- 27.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30(9):1096–1103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bliwise DL, Ansari FP. Insomnia associated with valerian and melatonin usage in the 2002 National Health Interview Survey. Sleep. 2007;30(7):881–884. doi: 10.1093/sleep/30.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pearson NJ, Johnson LL, Nahin RL. Insomnia, trouble sleeping, and complementary and alternative medicine: Analysis of the 2002 national health interview survey data. Archives of internal medicine. 2006;166(16):1775–1782. doi: 10.1001/archinte.166.16.1775. [DOI] [PubMed] [Google Scholar]
- 30.Brassington GS, King AC, Bliwise DL. Sleep problems as a risk factor for falls in a sample of community-dwelling adults aged 64-99 years. J Am Geriatr Soc. 2000;48(10):1234–1240. doi: 10.1111/j.1532-5415.2000.tb02596.x. [DOI] [PubMed] [Google Scholar]
- 31.Crain EF, Weiss KB, Bijur PE, Hersh M, Westbrook L, Stein RE. An estimate of the prevalence of asthma and wheezing among inner-city children. Pediatrics. 1994;94(3):356–362. [PubMed] [Google Scholar]
- 32.Prescott E, Jacobsen S, Kjoller M, Bulow PM, Danneskiold-Samsoe B, Kamper-Jorgensen F. Fibromyalgia in the adult Danish population: II. A study of clinical features. Scandinavian journal of rheumatology. 1993;22(5):238–242. doi: 10.3109/03009749309095130. [DOI] [PubMed] [Google Scholar]
- 33.Wetzler HP, Cruess DF. Self-reported physical health practices and health care utilization: findings from the National Health Interview Survey. American journal of public health. 1985;75(11):1329–1330. doi: 10.2105/ajph.75.11.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
National Health and Nutrition Examination Survey
- 1.Liu R, Liu X, Zee PC, et al. Association between sleep quality and C-reactive protein: results from national health and nutrition examination survey, 2005-2008. PLoS ONE. 2014;9(3):e92607. doi: 10.1371/journal.pone.0092607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Park SH, Jang SY, Kim H, Lee SW. An association rule mining-based framework for understanding lifestyle risk behaviors. PLoS ONE. 2014;9(2):e88859. doi: 10.1371/journal.pone.0088859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grandner MA, Chakravorty S, Perlis ML, Oliver L, Gurubhagavatula I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med. 2014;15(1):42–50. doi: 10.1016/j.sleep.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buman MP, Winkler EA, Kurka JM, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005-2006. American journal of epidemiology. 2014;179(3):323–334. doi: 10.1093/aje/kwt292. [DOI] [PubMed] [Google Scholar]
- 5.Mehari A, Weir NA, Gillum RF. Gender and the association of smoking with sleep quantity and quality in American adults. Women & health. 2014;54(1):1–14. doi: 10.1080/03630242.2013.858097. [DOI] [PubMed] [Google Scholar]
- 6.Lee JA, Park HS. Relation between sleep duration, overweight, and metabolic syndrome in Korean adolescents. Nutrition, metabolism, and cardiovascular diseases : NMCD. 2014;24(1):65–71. doi: 10.1016/j.numecd.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Stefani KM, Kim HC, Kim J, Oh K, Suh I. The influence of sex and age on the relationship between sleep duration and metabolic syndrome in Korean adults. Diabetes research and clinical practice. 2013;102(3):250–259. doi: 10.1016/j.diabres.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Ford ES, Wheaton AG, Chapman DP, Li C, Perry GS, Croft JB. Associations between self-reported sleep duration and sleeping disorder with concentrations of fasting and 2-h glucose, insulin, and glycosylated hemoglobin among adults without diagnosed diabetes. Journal of diabetes. 2014;6(4):338–350. doi: 10.1111/1753-0407.12101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chong Y, Fryer CD, Gu Q. Prescription sleep aid use among adults: United States, 2005-2010. NCHS data brief. 2013;(127):1–8. [PubMed] [Google Scholar]
- 10.Ansarin K, Sahebi L, Sabur S. Obstructive sleep apnea syndrome: complaints and housing characteristics in a population in the United States. Sao Paulo medical journal = Revista paulista de medicina. 2013;131(4):220–227. doi: 10.1590/1516-3180.2013.1314451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim JH, Kim KR, Cho KH, Yoo KB, Kwon JA, Park EC. The association between sleep duration and self-rated health in the Korean general population. J Clin Sleep Med. 2013;9(10):1057–1064. doi: 10.5664/jcsm.3082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aggarwal S, Loomba RS, Arora RR, Molnar J. Associations between sleep duration and prevalence of cardiovascular events. Clinical cardiology. 2013;36(11):671–676. doi: 10.1002/clc.22160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim JH, Park EC, Cho WH, Park CY, Choi WJ, Chang HS. Association between total sleep duration and suicidal ideation among the Korean general adult population. Sleep. 2013;36(10):1563–1572. doi: 10.5665/sleep.3058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McNamara JP, Wang J, Holiday DB, et al. Sleep disturbances associated with cigarette smoking. Psychol Health Med. 2014;19(4):410–419. doi: 10.1080/13548506.2013.832782. [DOI] [PubMed] [Google Scholar]
- 15.Akinbami LJ, Kit BK, Simon AE. Impact of environmental tobacco smoke on children with asthma, United States, 2003-2010. Academic pediatrics. 2013;13(6):508–516. doi: 10.1016/j.acap.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim BK, Kim BS, An SY, et al. Sleep duration and glycemic control in patients with diabetes mellitus: Korea National Health and Nutrition Examination Survey 2007-2010. Journal of Korean medical science. 2013;28(9):1334–1339. doi: 10.3346/jkms.2013.28.9.1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grandner MA, Petrov ME, Rattanaumpawan P, Jackson N, Platt A, Patel NP. Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med. 2013;9(9):897–905. 905A–905D. doi: 10.5664/jcsm.2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grandner MA, Jackson N, Gerstner JR, Knutson KL. Sleep symptoms associated with intake of specific dietary nutrients. J Sleep Res. 2014;23(1):22–34. doi: 10.1111/jsr.12084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patel MR, Janevic MR, Heeringa SG, Baptist AP, Clark NM. An examination of adverse asthma outcomes in U.S. Adults with multiple morbidities. Annals of the American Thoracic Society. 2013;10(5):426–431. doi: 10.1513/AnnalsATS.201302-032OC. [DOI] [PubMed] [Google Scholar]
- 20.Kim KH, Cho YY, Shin DW, Lee JH, Ko YJ, Park SM. Comparison of physical and mental health status between cancer survivors and the general population: a Korean population-based survey (KNHANES II-IV) Support Care Cancer. 2013;21(12):3471–3481. doi: 10.1007/s00520-013-1939-8. [DOI] [PubMed] [Google Scholar]
- 21.Flynn-Evans EE, Mucci L, Stevens RG, Lockley SW. Shiftwork and prostate-specific antigen in the National Health and Nutrition Examination Survey. Journal of the National Cancer Institute. 2013;105(17):1292–1297. doi: 10.1093/jnci/djt169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jang TW, Kim HR, Lee HE, Myong JP, Koo JW. Long work hours and obesity in Korean adult workers. Journal of occupational health. 2014;55(5):359–366. doi: 10.1539/joh.13-0043-oa. [DOI] [PubMed] [Google Scholar]
- 23.Sands-Lincoln M, Grandner M, Whinnery J, Keenan BT, Jackson N, Gurubhagavatula I. The association between obstructive sleep apnea and hypertension by race/ethnicity in a nationally representative sample. Journal of clinical hypertension. 2013;15(8):593–599. doi: 10.1111/jch.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen X, Gelaye B, Williams MA. Sleep characteristics and health-related quality of life among a national sample of American young adults: assessment of possible health disparities. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2014;23(2):613–625. doi: 10.1007/s11136-013-0475-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ford ES, Li C, Wheaton AG, Chapman DP, Perry GS, Croft JB. Sleep duration and body mass index and waist circumference among U.S. adults. Obesity. 2014;22(2):598–607. doi: 10.1002/oby.20558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grandner MA, Buxton OM, Jackson N, Sands-Lincoln M, Pandey A, Jean-Louis G. Extreme sleep durations and increased C-reactive protein: effects of sex and ethnoracial group. Sleep. 2013;36(5):769–779E. doi: 10.5665/sleep.2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang J, Lamers F, Hickie IB, He JP, Feig E, Merikangas KR. Differentiating nonrestorative sleep from nocturnal insomnia symptoms: demographic, clinical, inflammatory, and functional correlates. Sleep. 2013;36(5):671–679. doi: 10.5665/sleep.2624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. American journal of epidemiology. 2013;177(9):1006–1014. doi: 10.1093/aje/kws342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Engeda J, Mezuk B, Ratliff S, Ning Y. Association between duration and quality of sleep and the risk of pre-diabetes: evidence from NHANES. Diabetic medicine : a journal of the British Diabetic Association. 2013;30(6):676–680. doi: 10.1111/dme.12165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grandner MA, Jackson N, Gerstner JR, Knutson KL. Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Appetite. 2013;64:71–80. doi: 10.1016/j.appet.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walia H, Strohl K, Koo B, Seicean A, Seicean S. Are sleep symptoms predictors of resistant hypertension in a population-based sample? Findings from the National Health and Nutritional Examination Survey. Journal of clinical hypertension. 2012;14(8):530–536. doi: 10.1111/j.1751-7176.2012.00646.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alshaarawy O, Teppala S, Shankar A. Markers of Sleep-Disordered Breathing and Prediabetes in US Adults. International journal of endocrinology. 2012;2012:902324. doi: 10.1155/2012/902324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sabanayagam C, Zhang R, Shankar A. Markers of Sleep-Disordered Breathing and Metabolic Syndrome in a Multiethnic Sample of US Adults: Results from the National Health and Nutrition Examination Survey 2005-2008. Cardiology research and practice. 2012;2012:630802. doi: 10.1155/2012/630802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sabanayagam C, Teppala S, Shankar A. Markers of Sleep Disordered Breathing and Diabetes Mellitus in a Multiethnic Sample of US Adults: Results from the National Health and Nutrition Examination Survey (2005-2008) International journal of endocrinology. 2012;2012:879134. doi: 10.1155/2012/879134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wheaton AG, Perry GS, Chapman DP, Croft JB. Sleep disordered breathing and depression among U.S. adults: National Health and Nutrition Examination Survey, 2005-2008. Sleep. 2012;35(4):461–467. doi: 10.5665/sleep.1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Plantinga L, Rao MN, Schillinger D. Prevalence of self-reported sleep problems among people with diabetes in the United States, 2005-2008. Preventing chronic disease. 2012;9:E76. [PMC free article] [PubMed] [Google Scholar]
- 37.Thakre TP, Mamtani M, Ujaoney S, Kulkarni H. Association of plasma homocysteine with self-reported sleep apnea is confounded by age: results from the national health and nutrition examination survey 2005-2006. Sleep disorders. 2012;2012:634920. doi: 10.1155/2012/634920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bansil P, Kuklina EV, Merritt RK, Yoon PW. Associations between sleep disorders, sleep duration, quality of sleep, and hypertension: results from the National Health and Nutrition Examination Survey, 2005 to 2008. Journal of clinical hypertension. 2011;13(10):739–743. doi: 10.1111/j.1751-7176.2011.00500.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Plantinga L, Lee K, Inker LA, et al. Association of sleep-related problems with CKD in the United States, 2005-2008. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2011;58(4):554–564. doi: 10.1053/j.ajkd.2011.05.024. [DOI] [PubMed] [Google Scholar]
- 40.Chasens ER, Yang K. Insomnia and physical activity in adults with prediabetes. Clinical nursing research. 2012;21(3):294–308. doi: 10.1177/1054773811411295. [DOI] [PubMed] [Google Scholar]
- 41.Khang YH, Lynch JW. Exploring determinants of secular decreases in childhood blood pressure and hypertension. Circulation. 2011;124(4):397–405. doi: 10.1161/CIRCULATIONAHA.110.014399. [DOI] [PubMed] [Google Scholar]
- 42.Chin YR, Lee HY, So ES. Suicidal ideation and associated factors by sex in Korean adults: a population-based cross-sectional survey. International journal of public health. 2011;56(4):429–439. doi: 10.1007/s00038-011-0245-9. [DOI] [PubMed] [Google Scholar]
- 43.Centers for Disease C, Prevention. Effect of short sleep duration on daily activities--United States, 2005-2008. MMWR. Morbidity and mortality weekly report. 2011;60(8):239–242. [PubMed] [Google Scholar]
- 44.Hoffmann RG, Kotchen JM, Kotchen TA, Cowley T, Dasgupta M, Cowley AW., Jr. Temporomandibular disorders and associated clinical comorbidities. The Clinical journal of pain. 2011;27(3):268–274. doi: 10.1097/AJP.0b013e31820215f5. [DOI] [PubMed] [Google Scholar]
- 45.Kupelian V, Fitzgerald MP, Kaplan SA, Norgaard JP, Chiu GR, Rosen RC. Association of nocturia and mortality: results from the Third National Health and Nutrition Examination Survey. The Journal of urology. 2011;185(2):571–577. doi: 10.1016/j.juro.2010.09.108. [DOI] [PubMed] [Google Scholar]
- 46.Kim J, Jo I. Age-dependent association between sleep duration and hypertension in the adult Korean population. Am J Hypertens. 2010;23(12):1286–1291. doi: 10.1038/ajh.2010.166. [DOI] [PubMed] [Google Scholar]
- 47.Oh EG, Kim SH, Kim BH, Park MS, Kim SK, Kim YS. Health behaviour and quality of life in Korean adults with respiratory disease: National Health Survey, 2005. The international journal of tuberculosis and lung disease : the official journal of the International Union against Tuberculosis and Lung Disease. 2010;14(6):772–778. [PubMed] [Google Scholar]
- 48.Kim HJ, Ruger JP. Socioeconomic disparities in behavioral risk factors and health outcomes by gender in the Republic of Korea. BMC public health. 2010;10:195. doi: 10.1186/1471-2458-10-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li C, Ford ES, Zhao G, Croft JB, Balluz LS, Mokdad AH. Prevalence of self-reported clinically diagnosed sleep apnea according to obesity status in men and women: National Health and Nutrition Examination Survey, 2005-2006. Preventive medicine. 2010;51(1):18–23. doi: 10.1016/j.ypmed.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 50.Lee K. Sociodemographic status and self-reported BMI-related morbidity in Koreans. Yonsei medical journal. 2010;51(2):171–177. doi: 10.3349/ymj.2010.51.2.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Davila EP, Lee DJ, Fleming LE, et al. Sleep disorders and secondhand smoke exposure in the U.S. population. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2010;12(3):294–299. doi: 10.1093/ntr/ntp193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gangwisch JE, Malaspina D, Posner K, et al. Insomnia and sleep duration as mediators of the relationship between depression and hypertension incidence. Am J Hypertens. 2010;23(1):62–69. doi: 10.1038/ajh.2009.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kim J, Kim HM, Kim KM, Kim DJ. The association of sleep duration and type 2 diabetes in Korean male adults with abdominal obesity: the Korean National Health and Nutrition Examination Survey 2005. Diabetes research and clinical practice. 2009;86(2):e34–36. doi: 10.1016/j.diabres.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 54.Ram S, Seirawan H, Kumar SK, Clark GT. Prevalence and impact of sleep disorders and sleep habits in the United States. Sleep Breath. 2010;14(1):63–70. doi: 10.1007/s11325-009-0281-3. [DOI] [PubMed] [Google Scholar]
- 55.Pratt LA, Brody DJ. Depression in the United States household population, 2005-2006. NCHS data brief. 2008;(7):1–8. [PubMed] [Google Scholar]
- 56.Park SE, Kim HM, Kim DH, Kim J, Cha BS, Kim DJ. The association between sleep duration and general and abdominal obesity in Koreans: data from the Korean National Health and Nutrition Examination Survey, 2001 and 2005. Obesity. 2009;17(4):767–771. doi: 10.1038/oby.2008.586. [DOI] [PubMed] [Google Scholar]
- 57.Vgontzas AN. Does obesity play a major role in the pathogenesis of sleep apnoea and its associated manifestations via inflammation, visceral adiposity, and insulin resistance? Archives of physiology and biochemistry. 2008;114(4):211–223. doi: 10.1080/13813450802364627. [DOI] [PubMed] [Google Scholar]
- 58.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large US sample. Sleep. 2008;31(8):1087–1096. [PMC free article] [PubMed] [Google Scholar]
- 59.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration as a risk factor for diabetes incidence in a large U.S. sample. Sleep. 2007;30(12):1667–1673. doi: 10.1093/sleep/30.12.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Resnick HE, Carter EA, Aloia M, Phillips B. Cross-sectional relationship of reported fatigue to obesity, diet, and physical activity: results from the third national health and nutrition examination survey. J Clin Sleep Med. 2006;2(2):163–169. [PubMed] [Google Scholar]
- 61.Paek KW, Chun KH, Cho JP. Risk factors influencing the occurrence of injuries in koreans requiring hospitalization. Yonsei medical journal. 2007;48(2):164–170. doi: 10.3349/ymj.2007.48.2.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47(5):833–839. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 63.Vgontzas AN, Bixler EO, Chrousos GP. Sleep apnea is a manifestation of the metabolic syndrome. Sleep Med Rev. 2005;9(3):211–224. doi: 10.1016/j.smrv.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 64.Eisenmann JC. Secular trends in variables associated with the metabolic syndrome of North American children and adolescents: a review and synthesis. American journal of human biology : the official journal of the Human Biology Council. 2003;15(6):786–794. doi: 10.1002/ajhb.10214. [DOI] [PubMed] [Google Scholar]
- 65.Crescente Pippi JL, Martin Acero R, Cardesin Villaverde JM, Romero Nieves JL, Pinto Guedes D. [Overweight and risk of overweight in schoolchildren aged 6-17 years old in Galicia (Spain)] Anales de pediatria. 2003;58(6):523–528. doi: 10.1016/s1695-4033(03)78116-8. [DOI] [PubMed] [Google Scholar]
- 66.Krieg EF, Jr., Chrislip DW, Letz RE, et al. Neurobehavioral test performance in the third National Health and Nutrition Examination Survey. Neurotoxicology and teratology. 2001;23(6):569–589. doi: 10.1016/s0892-0362(01)00177-5. [DOI] [PubMed] [Google Scholar]
- 67.Qureshi AI, Giles WH, Croft JB, Bliwise DL. Habitual sleep patterns and risk for stroke and coronary heart disease: a 10-year follow-up from NHANES I. Neurology. 1997;48(4):904–911. doi: 10.1212/wnl.48.4.904. [DOI] [PubMed] [Google Scholar]
National Survey of Children's Health
- 1.Singh GK, Yu SM, Kogan MD. Health, chronic conditions, and behavioral risk disparities among U.S. immigrant children and adolescents. Public health reports. 2013;128(6):463–479. doi: 10.1177/003335491312800606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh GK, Kenney MK. Rising Prevalence and Neighborhood, Social, and Behavioral Determinants of Sleep Problems in US Children and Adolescents, 2003-2012. Sleep disorders. 2013;2013:394320. doi: 10.1155/2013/394320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silverberg JI, Simpson EL. Association between severe eczema in children and multiple comorbid conditions and increased healthcare utilization. Pediatric allergy and immunology : official publication of the European Society of Pediatric Allergy and Immunology. 2013;24(5):476–486. doi: 10.1111/pai.12095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh GK, Yu SM. The Impact of Ethnic-Immigrant Status and Obesity-Related Risk Factors on Behavioral Problems among US Children and Adolescents. Scientifica. 2012;2012:648152. doi: 10.6064/2012/648152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sisson SB, Broyles ST. Social-ecological correlates of excessive TV viewing: difference by race and sex. Journal of physical activity & health. 2012;9(3):449–455. doi: 10.1123/jpah.9.3.449. [DOI] [PubMed] [Google Scholar]
- 6.Hassan F, Davis MM, Chervin RD. No independent association between insufficient sleep and childhood obesity in the National Survey of Children's Health. J Clin Sleep Med. 2011;7(2):153–157. [PMC free article] [PubMed] [Google Scholar]
- 7.Smaldone A, Honig JC, Byrne MW. Does assessing sleep inadequacy across its continuum inform associations with child and family health? Journal of pediatric health care : official publication of National Association of Pediatric Nurse Associates & Practitioners. 2009;23(6):394–404. doi: 10.1016/j.pedhc.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Singh GK, Kogan MD, Siahpush M, van Dyck PC. Prevalence and correlates of state and regional disparities in vigorous physical activity levels among US children and adolescents. Journal of physical activity & health. 2009;6(1):73–87. doi: 10.1123/jpah.6.1.73. [DOI] [PubMed] [Google Scholar]
- 9.Singh GK, Kogan MD, Siahpush M, van Dyck PC. Independent and joint effects of socioeconomic, behavioral, and neighborhood characteristics on physical inactivity and activity levels among US children and adolescents. Journal of community health. 2008;33(4):206–216. doi: 10.1007/s10900-008-9094-8. [DOI] [PubMed] [Google Scholar]
- 10.Smaldone A, Honig JC, Byrne MW. Sleepless in America: inadequate sleep and relationships to health and well-being of our nation's children. Pediatrics. 2007;119(Suppl 1):S29–37. doi: 10.1542/peds.2006-2089F. [DOI] [PubMed] [Google Scholar]
National Comorbidity Survey
- 1.Selby EA. Chronic sleep disturbances and borderline personality disorder symptoms. Journal of consulting and clinical psychology. 2013;81(5):941–947. doi: 10.1037/a0033201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lamers F, Hickie I, Merikangas KR. Prevalence and correlates of prolonged fatigue in a U.S. sample of adolescents. The American journal of psychiatry. 2013;170(5):502–510. doi: 10.1176/appi.ajp.2012.12040454. [DOI] [PubMed] [Google Scholar]
- 3.Silverstein B, Edwards T, Gamma A, Ajdacic-Gross V, Rossler W, Angst J. The role played by depression associated with somatic symptomatology in accounting for the gender difference in the prevalence of depression. Social psychiatry and psychiatric epidemiology. 2013;48(2):257–263. doi: 10.1007/s00127-012-0540-7. [DOI] [PubMed] [Google Scholar]
- 4.Parhami I, Siani A, Rosenthal RJ, Fong TW. Pathological gambling, problem gambling and sleep complaints: an analysis of the National Comorbidity Survey: Replication (NCS-R) Journal of gambling studies / co-sponsored by the National Council on Problem Gambling and Institute for the Study of Gambling and Commercial Gaming. 2013;29(2):241–253. doi: 10.1007/s10899-012-9299-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lauterbach D, Behnke C, McSweeney LB. Sleep problems among persons with a lifetime history of posttraumatic stress disorder alone and in combination with a lifetime history of other psychiatric disorders: a replication and extension. Comprehensive psychiatry. 2011;52(6):580–586. doi: 10.1016/j.comppsych.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Lateef T, Swanson S, Cui L, Nelson K, Nakamura E, Merikangas K. Headaches and sleep problems among adults in the United States: findings from the National Comorbidity Survey-Replication study. Cephalalgia : an international journal of headache. 2011;31(6):648–653. doi: 10.1177/0333102410390395. [DOI] [PubMed] [Google Scholar]
- 7.Vincent N, Cox B, Clara I. Are personality dimensions associated with sleep length in a large nationally representative sample? Comprehensive psychiatry. 2009;50(2):158–163. doi: 10.1016/j.comppsych.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Wojnar M, Ilgen MA, Wojnar J, McCammon RJ, Valenstein M, Brower KJ. Sleep problems and suicidality in the National Comorbidity Survey Replication. Journal of psychiatric research. 2009;43(5):526–531. doi: 10.1016/j.jpsychires.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goodwin RD, Marusic A. Association between short sleep and suicidal ideation and suicide attempt among adults in the general population. Sleep. 2008;31(8):1097–1101. [PMC free article] [PubMed] [Google Scholar]
- 10.Roth T, Jaeger S, Jin R, Kalsekar A, Stang PE, Kessler RC. Sleep problems, comorbid mental disorders, and role functioning in the national comorbidity survey replication. Biological psychiatry. 2006;60(12):1364–1371. doi: 10.1016/j.biopsych.2006.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leskin GA, Woodward SH, Young HE, Sheikh JI. Effects of comorbid diagnoses on sleep disturbance in PTSD. Journal of psychiatric research. 2002;36(6):449–452. doi: 10.1016/s0022-3956(02)00025-0. [DOI] [PubMed] [Google Scholar]
- 12.Silverstein B. Gender differences in the prevalence of somatic versus pure depression: a replication. The American journal of psychiatry. 2002;159(6):1051–1052. doi: 10.1176/appi.ajp.159.6.1051. [DOI] [PubMed] [Google Scholar]
- 13.Wittchen HU, Lieb R, Wunderlich U, Schuster P. Comorbidity in primary care: presentation and consequences. J Clin Psychiatry. 1999;60(Suppl 7):29–36. discussion 37-28. [PubMed] [Google Scholar]
- 14.Silverstein B. Gender difference in the prevalence of clinical depression: the role played by depression associated with somatic symptoms. The American journal of psychiatry. 1999;156(3):480–482. doi: 10.1176/ajp.156.3.480. [DOI] [PubMed] [Google Scholar]
- 15.Kessler RC, Rubinow DR, Holmes C, Abelson JM, Zhao S. The epidemiology of DSM-III-R bipolar I disorder in a general population survey. Psychological medicine. 1997;27(5):1079–1089. doi: 10.1017/s0033291797005333. [DOI] [PubMed] [Google Scholar]
- 16.Weissman MM, Greenwald S, Wickramaratne P, et al. What happens to depressed men? Application of the Stirling County criteria. Harvard review of psychiatry. 1997;5(1):1–6. doi: 10.3109/10673229709034719. [DOI] [PubMed] [Google Scholar]
American Time Use Survey
- 1.Dolan P, Kudrna L. More years, less yawns: fresh evidence on tiredness by age and other factors. The journals of gerontology. Series B, Psychological sciences and social sciences. 2015;70(4):576–580. doi: 10.1093/geronb/gbt118. [DOI] [PubMed] [Google Scholar]
- 2.Tudor-Locke C, Leonardi C, Johnson WD, Katzmarzyk PT. Time spent in physical activity and sedentary behaviors on the working day: the American time use survey. J Occup Environ Med. 2011;53(12):1382–1387. doi: 10.1097/JOM.0b013e31823c1402. [DOI] [PubMed] [Google Scholar]
- 3.Basner M, Dinges DF. Dubious bargain: trading sleep for Leno and Letterman. Sleep. 2009;32(6):747–752. doi: 10.1093/sleep/32.6.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knutson KL, Lauderdale DS. Sociodemographic and behavioral predictors of bed time and wake time among US adolescents aged 15 to 17 years. J Pediatr. 2009;154(3):426–430. 430, e421. doi: 10.1016/j.jpeds.2008.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Basner M, Fomberstein KM, Razavi FM, et al. American time use survey: sleep time and its relationship to waking activities. Sleep. 2007;30(9):1085–1095. doi: 10.1093/sleep/30.9.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
PatientsLikeMe
- 1.Frost J, Okun S, Vaughan T, Heywood J, Wicks P. Patient-reported outcomes as a source of evidence in off-label prescribing: analysis of data from PatientsLikeMe. Journal of medical Internet research. 2011;13(1):e6. doi: 10.2196/jmir.1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sleep in America Poll/National Sleep Foundation
- 1.Gradisar M, Wolfson AR, Harvey AG, Hale L, Rosenberg R, Czeisler CA. The sleep and technology use of Americans: findings from the National Sleep Foundation's 2011 Sleep in America poll. J Clin Sleep Med. 2013;9(12):1291–1299. doi: 10.5664/jcsm.3272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Calamaro CJ, Yang K, Ratcliffe S, Chasens ER. Wired at a young age: the effect of caffeine and technology on sleep duration and body mass index in school-aged children. Journal of pediatric health care : official publication of National Association of Pediatric Nurse Associates & Practitioners. 2012;26(4):276–282. doi: 10.1016/j.pedhc.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Swanson LM, Arnedt JT, Rosekind MR, Belenky G, Balkin TJ, Drake C. Sleep disorders and work performance: findings from the 2008 National Sleep Foundation Sleep in America poll. J Sleep Res. 2011;20(3):487–494. doi: 10.1111/j.1365-2869.2010.00890.x. [DOI] [PubMed] [Google Scholar]
- 4.Chasens ER, Twerski SR, Yang K, Umlauf MG. Sleepiness and health in midlife women: results of the National Sleep Foundation's 2007 Sleep in America poll. Behavioral sleep medicine. 2010;8(3):157–171. doi: 10.1080/15402002.2010.487462. [DOI] [PubMed] [Google Scholar]
- 5.Kapsimalis F, Kryger M. Sleep breathing disorders in the U.S. female population. Journal of women's health. 2009;18(8):1211–1219. doi: 10.1089/jwh.2008.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baker FC, Wolfson AR, Lee KA. Association of sociodemographic, lifestyle, and health factors with sleep quality and daytime sleepiness in women: findings from the 2007 National Sleep Foundation “Sleep in America Poll”. Journal of women's health. 2009;18(6):841–849. doi: 10.1089/jwh.2008.0986. [DOI] [PubMed] [Google Scholar]
- 7.Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Med. 2009;10(7):771–779. doi: 10.1016/j.sleep.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 8.Foley DJ, Vitiello MV, Bliwise DL, Ancoli-Israel S, Monjan AA, Walsh JK. Frequent napping is associated with excessive daytime sleepiness, depression, pain, and nocturia in older adults: findings from the National Sleep Foundation ‘2003 Sleep in America’ Poll. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2007;15(4):344–350. doi: 10.1097/01.JGP.0000249385.50101.67. [DOI] [PubMed] [Google Scholar]
- 9.Chasens ER, Sereika SM, Weaver TE, Umlauf MG. Daytime sleepiness, exercise, and physical function in older adults. J Sleep Res. 2007;16(1):60–65. doi: 10.1111/j.1365-2869.2007.00576.x. [DOI] [PubMed] [Google Scholar]
- 10.Hiestand DM, Britz P, Goldman M, Phillips B. Prevalence of symptoms and risk of sleep apnea in the US population: Results from the national sleep foundation sleep in America 2005 poll. Chest. 2006;130(3):780–786. doi: 10.1378/chest.130.3.780. [DOI] [PubMed] [Google Scholar]
- 11.Phillips B, Hening W, Britz P, Mannino D. Prevalence and correlates of restless legs syndrome: results from the 2005 National Sleep Foundation Poll. Chest. 2006;129(1):76–80. doi: 10.1378/chest.129.1.76. [DOI] [PubMed] [Google Scholar]
- 12.Foley D, Ancoli-Israel S, Britz P, Walsh J. Sleep disturbances and chronic disease in older adults: results of the 2003 National Sleep Foundation Sleep in America Survey. J Psychosom Res. 2004;56(5):497–502. doi: 10.1016/j.jpsychores.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 13.Grandner MA, Kripke DF. Self-reported sleep complaints with long and short sleep: a nationally representative sample. Psychosomatic medicine. 2004;66(2):239–241. doi: 10.1097/01.psy.0000107881.53228.4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Covarrubias-Gomez A, Mendoza-Reyes JJ. Evaluation of sleep quality in subjects with chronic nononcologic pain. Journal of pain & palliative care pharmacotherapy. 2013;27(3):220–224. doi: 10.3109/15360288.2013.816405. [DOI] [PubMed] [Google Scholar]
- 15.Swanson LM, Drake C, Arnedt JT. Employment and drowsy driving: a survey of American workers. Behavioral sleep medicine. 2012;10(4):250–257. doi: 10.1080/15402002.2011.624231. [DOI] [PubMed] [Google Scholar]
- 16.Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2010;46(2):124–132. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 17.Bliwise DL, Foley DJ, Vitiello MV, Ansari FP, Ancoli-Israel S, Walsh JK. Nocturia and disturbed sleep in the elderly. Sleep Med. 2009;10(5):540–548. doi: 10.1016/j.sleep.2008.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ondo WG, Dat Vuong K, Khan H, Atassi F, Kwak C, Jankovic J. Daytime sleepiness and other sleep disorders in Parkinson's disease. Neurology. 2001;57(8):1392–1396. doi: 10.1212/wnl.57.8.1392. [DOI] [PubMed] [Google Scholar]
- 19.Roth T, Ancoli-Israel S. Daytime consequences and correlates of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. II. Sleep. 1999;22(Suppl 2):S354–358. [PubMed] [Google Scholar]
- 20.Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. I. Sleep. 1999;22(Suppl 2):S347–353. [PubMed] [Google Scholar]
Pregnancy Risk Assessment Monitoring System
- 1.Hwang SS, Barfield WD, Smith RA, et al. Discharge timing, outpatient follow-up, and home care of late-preterm and early-term infants. Pediatrics. 2013;132(1):101–108. doi: 10.1542/peds.2012-3892. [DOI] [PubMed] [Google Scholar]
- 2.Broussard DL, Sappenfield WM, Goodman DA. The Black and White of infant back sleeping and infant bed sharing in Florida, 2004-2005. Maternal and child health journal. 2012;16(3):713–724. doi: 10.1007/s10995-011-0768-y. [DOI] [PubMed] [Google Scholar]
- 3.Smith MG, Liu JH, Helms KH, Wilkerson KL. Racial differences in trends and predictors of infant sleep positioning in South Carolina, 1996-2007. Maternal and child health journal. 2012;16(1):72–82. doi: 10.1007/s10995-010-0718-0. [DOI] [PubMed] [Google Scholar]
- 4.Blabey MH, Gessner BD. Infant bed-sharing practices and associated risk factors among births and infant deaths in Alaska. Public health reports. 2009;124(4):527–534. doi: 10.1177/003335490912400409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bruckner TA. Economic antecedents of prone infant sleep placement among black mothers. Annals of epidemiology. 2008;18(9):678–681. doi: 10.1016/j.annepidem.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 6.Patrick P, Lincoln A, Lorenz D, DeVault M, Dooley S. Infant sleep position in Oklahoma: evidence from PRAMS. The Journal of the Oklahoma State Medical Association. 2008;101(8):182–187. [PubMed] [Google Scholar]
- 7.McKinney CM, Holt VL, Cunningham ML, Leroux BG, Starr JR. Maternal and infant characteristics associated with prone and lateral infant sleep positioning in Washington state, 1996-2002. J Pediatr. 2008;153(2):194–198. 198, e191–193. doi: 10.1016/j.jpeds.2008.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Suellentrop K, Morrow B, Williams L, D'Angelo D Centers for Disease C, Prevention. yMonitoring progress toward achieving Maternal and Infant Healthy People 2010 objectives--19 states, Pregnancy Risk Assessment Monitoring System (PRAMS), 2000-2003. Morbidity and mortality weekly report. Surveillance summaries. 2006;55(9):1–11. [PubMed] [Google Scholar]
- 9.Lahr MB, Rosenberg KD, Lapidus JA. Bedsharing and maternal smoking in a population-based survey of new mothers. Pediatrics. 2005;116(4):e530–542. doi: 10.1542/peds.2005-0354. [DOI] [PubMed] [Google Scholar]
- 10.Lahr MB, Rosenberg KD, Lapidus JA. Health departments do it better: prenatal care site and prone infant sleep position. Maternal and child health journal. 2005;9(2):165–172. doi: 10.1007/s10995-005-4868-4. [DOI] [PubMed] [Google Scholar]
- 11.Phares TM, Morrow B, Lansky A, et al. Surveillance for disparities in maternal health-related behaviors--selected states, Pregnancy Risk Assessment Monitoring System (PRAMS), 2000-2001. Morbidity and mortality weekly report. Surveillance summaries. 2004;53(4):1–13. [PubMed] [Google Scholar]
- 12.Beck LF, Morrow B, Lipscomb LE, et al. Prevalence of selected maternal behaviors and experiences, Pregnancy Risk Assessment Monitoring System (PRAMS), 1999. Morbidity and mortality weekly report. Surveillance summaries. 2002;51(2):1–27. [PubMed] [Google Scholar]
- 13.Pollack HA, Frohna JG. Infant sleep placement after the back to sleep campaign. Pediatrics. 2002;109(4):608–614. doi: 10.1542/peds.109.4.608. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease C, Prevention. Progress in reducing risky infant sleeping positions--13 states, 1996-1997. MMWR. Morbidity and mortality weekly report. 1999;48(39):878–882. [PubMed] [Google Scholar]
- 15.Centers for Disease C, Prevention. Assessment of infant sleeping position-selected states, 1996. MMWR. Morbidity and mortality weekly report. 1998;47(41):873–877. [PubMed] [Google Scholar]
National Survey of Early Childhood Health
- 1.Thompson DA, Christakis DA. The association between television viewing and irregular sleep schedules among children less than 3 years of age. Pediatrics. 2005;116(4):851–856. doi: 10.1542/peds.2004-2788. [DOI] [PubMed] [Google Scholar]
- 2.Olson LM, Inkelas M, Halfon N, Schuster MA, O'Connor KG, Mistry R. Overview of the content of health supervision for young children: reports from parents and pediatricians. Pediatrics. 2004;113(6 Suppl):1907–1916. [PubMed] [Google Scholar]
Nurses' Health Study
- 1.Zhang X, Giovannucci EL, Wu K, et al. Associations of self-reported sleep duration and snoring with colorectal cancer risk in men and women. Sleep. 2013;36(5):681–688. doi: 10.5665/sleep.2626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gangwisch JE, Feskanich D, Malaspina D, Shen S, Forman JP. Sleep duration and risk for hypertension in women: results from the nurses' health study. Am J Hypertens. 2013;26(7):903–911. doi: 10.1093/ajh/hpt044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McMullan CJ, Schernhammer ES, Rimm EB, Hu FB, Forman JP. Melatonin secretion and the incidence of type 2 diabetes. JAMA. 2013;309(13):1388–1396. doi: 10.1001/jama.2013.2710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pan A, Malik VS, Hao T, Willett WC, Mozaffarian D, Hu FB. Changes in water and beverage intake and long-term weight changes: results from three prospective cohort studies. International journal of obesity. 2013;37(10):1378–1385. doi: 10.1038/ijo.2012.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Y, Munger KL, Batool-Anwar S, De Vito K, Ascherio A, Gao X. Association of multiple sclerosis with restless legs syndrome and other sleep disorders in women. Neurology. 2012;78(19):1500–1506. doi: 10.1212/WNL.0b013e3182553c5b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel SR, Malhotra A, Gao X, Hu FB, Neuman MI, Fawzi WW. A prospective study of sleep duration and pneumonia risk in women. Sleep. 2012;35(1):97–101. doi: 10.5665/sleep.1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lieu SJ, Curhan GC, Schernhammer ES, Forman JP. Rotating night shift work and disparate hypertension risk in African-Americans. Journal of hypertension. 2012;30(1):61–66. doi: 10.1097/HJH.0b013e32834e1ea3. [DOI] [PubMed] [Google Scholar]
- 8.Batool-Anwar S, Malhotra A, Forman J, Winkelman J, Li Y, Gao X. Restless legs syndrome and hypertension in middle-aged women. Hypertension. 2011;58(5):791–796. doi: 10.1161/HYPERTENSIONAHA.111.174037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liang G, Schernhammer E, Qi L, Gao X, De Vivo I, Han J. Associations between rotating night shifts, sleep duration, and telomere length in women. PLoS ONE. 2011;6(8):e23462. doi: 10.1371/journal.pone.0023462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lawson CC, Whelan EA, Lividoti Hibert EN, Spiegelman D, Schernhammer ES, Rich-Edwards JW. Rotating shift work and menstrual cycle characteristics. Epidemiology. 2011;22(3):305–312. doi: 10.1097/EDE.0b013e3182130016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown DL, Feskanich D, Sanchez BN, Rexrode KM, Schernhammer ES, Lisabeth LD. Rotating night shift work and the risk of ischemic stroke. American journal of epidemiology. 2009;169(11):1370–1377. doi: 10.1093/aje/kwp056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gao X, Schwarzschild MA, Wang H, Ascherio A. Obesity and restless legs syndrome in men and women. Neurology. 2009;72(14):1255–1261. doi: 10.1212/01.wnl.0000345673.35676.1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams CJ, Hu FB, Patel SR, Mantzoros CS. Sleep duration and snoring in relation to biomarkers of cardiovascular disease risk among women with type 2 diabetes. Diabetes care. 2007;30(5):1233–1240. doi: 10.2337/dc06-2107. [DOI] [PubMed] [Google Scholar]
- 14.Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. American journal of epidemiology. 2006;164(10):947–954. doi: 10.1093/aje/kwj280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pinheiro SP, Schernhammer ES, Tworoger SS, Michels KB. A prospective study on habitual duration of sleep and incidence of breast cancer in a large cohort of women. Cancer research. 2006;66(10):5521–5525. doi: 10.1158/0008-5472.CAN-05-4652. [DOI] [PubMed] [Google Scholar]
- 16.Schernhammer E, Chen H, Ritz B. Circulating melatonin levels: possible link between Parkinson's disease and cancer risk? Cancer causes & control : CCC. 2006;17(4):577–582. doi: 10.1007/s10552-005-9002-9. [DOI] [PubMed] [Google Scholar]
- 17.Chen H, Schernhammer E, Schwarzschild MA, Ascherio A. A prospective study of night shift work, sleep duration, and risk of Parkinson's disease. American journal of epidemiology. 2006;163(8):726–730. doi: 10.1093/aje/kwj096. [DOI] [PubMed] [Google Scholar]
- 18.Tworoger SS, Lee S, Schernhammer ES, Grodstein F. The association of self-reported sleep duration, difficulty sleeping, and snoring with cognitive function in older women. Alzheimer disease and associated disorders. 2006;20(1):41–48. doi: 10.1097/01.wad.0000201850.52707.80. [DOI] [PubMed] [Google Scholar]
- 19.Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Archives of internal medicine. 2003;163(2):205–209. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 20.Al-Delaimy WK, Manson JE, Willett WC, Stampfer MJ, Hu FB. Snoring as a risk factor for type II diabetes mellitus: a prospective study. American journal of epidemiology. 2002;155(5):387–393. doi: 10.1093/aje/155.5.387. [DOI] [PubMed] [Google Scholar]
- 21.Harding SM. Complications and consequences of obstructive sleep apnea. Current opinion in pulmonary medicine. 2000;6(6):485–489. doi: 10.1097/00063198-200011000-00004. [DOI] [PubMed] [Google Scholar]
General Social Survey
- 1.Romans SE, Cohen MM, Forte T, Du Mont J, Hyman I. Gender and psychotropic medication use: the role of intimate partner violence. Preventive medicine. 2008;46(6):615–621. doi: 10.1016/j.ypmed.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 2.Pentland W, Harvey AS, Smith T, Walker J. The impact of spinal cord injury on men's time use. Spinal cord. 1999;37(11):786–792. doi: 10.1038/sj.sc.3100908. [DOI] [PubMed] [Google Scholar]
Sleep Heart Health Study
- 1.Shah N, Rice T, Tracy D, et al. Sleep and insulin-like growth factors in the Cardiovascular Health Study. J Clin Sleep Med. 2013;9(12):1245–1251. doi: 10.5664/jcsm.3260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woodard DB, Crainiceanu C, Ruppert D. Hierarchical Adaptive Regression Kernels for Regression with Functional Predictors. Journal of computational and graphical statistics : a joint publication of American Statistical Association, Institute of Mathematical Statistics, Interface Foundation of North America. 2013;22(4) doi: 10.1080/10618600.2012.694765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas RJ, Mietus JE, Peng CK, et al. Relationship between delta power and the electrocardiogram-derived cardiopulmonary spectrogram: possible implications for assessing the effectiveness of sleep. Sleep Med. 2014;15(1):125–131. doi: 10.1016/j.sleep.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Selvaraj N, Narasimhan R. Detection of sleep apnea on a per-second basis using respiratory signals. Conference proceedings : Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual Conference. 2013;2013:2124–2127. doi: 10.1109/EMBC.2013.6609953. [DOI] [PubMed] [Google Scholar]
- 5.Ebrahimi F, Setarehdan SK, Ayala-Moyeda J, Nazeran H. Automatic sleep staging using empirical mode decomposition, discrete wavelet transform, time-domain, and nonlinear dynamics features of heart rate variability signals. Computer methods and programs in biomedicine. 2013;112(1):47–57. doi: 10.1016/j.cmpb.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 6.Lane JM, Tare A, Cade BE, et al. Common variants in CLOCK are not associated with measures of sleep duration in people of european ancestry from the sleep heart health study. Biological psychiatry. 2013;74(12):e33–35. doi: 10.1016/j.biopsych.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chami HA, Fontes JD, Vasan RS, et al. Vascular inflammation and sleep disordered breathing in a community-based cohort. Sleep. 2013;36(5):763–768C. doi: 10.5665/sleep.2644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Langrock R, Swihart BJ, Caffo BS, Punjabi NM, Crainiceanu CM. Combining hidden Markov models for comparing the dynamics of multiple sleep electroencephalograms. Statistics in medicine. 2013;32(19):3342–3356. doi: 10.1002/sim.5747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel SR, Goodloe R, De G, et al. Association of genetic loci with sleep apnea in European Americans and African-Americans: the Candidate Gene Association Resource (CARe) PLoS ONE. 2012;7(11):e48836. doi: 10.1371/journal.pone.0048836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crainiceanu CM, Staicu AM, Ray S, Punjabi N. Bootstrap-based inference on the difference in the means of two correlated functional processes. Statistics in medicine. 2012;31(26):3223–3240. doi: 10.1002/sim.5439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baldwin CM, Choi M, McClain DB, Celaya A, Quan SF. Spanish translation and cross-language validation of a sleep habits questionnaire for use in clinical and research settings. J Clin Sleep Med. 2012;8(2):137–146. doi: 10.5664/jcsm.1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Budhiraja P, Budhiraja R, Goodwin JL, et al. Incidence of restless legs syndrome and its correlates. J Clin Sleep Med. 2012;8(2):119–124. doi: 10.5664/jcsm.1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aurora RN, Crainiceanu C, Caffo B, Punjabi NM. Sleep-disordered breathing and caffeine consumption: results of a community-based study. Chest. 2012;142(3):631–638. doi: 10.1378/chest.11-2894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parthasarathy S, Fitzgerald M, Goodwin JL, Unruh M, Guerra S, Quan SF. Nocturia, sleep-disordered breathing, and cardiovascular morbidity in a community-based cohort. PLoS ONE. 2012;7(2):e30969. doi: 10.1371/journal.pone.0030969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown MA, Goodwin JL, Silva GE, et al. The Impact of Sleep-Disordered Breathing on Body Mass Index (BMI): The Sleep Heart Health Study (SHHS) Southwest journal of pulmonary & critical care. 2011;3:159–168. [PMC free article] [PubMed] [Google Scholar]
- 16.Al-Angari HM, Sahakian AV. Automated recognition of obstructive sleep apnea syndrome using support vector machine classifier. IEEE transactions on information technology in biomedicine : a publication of the IEEE Engineering in Medicine and Biology Society. 2012;16(3):463–468. doi: 10.1109/TITB.2012.2185809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Swihart BJ, Caffo BS, Crainiceanu CM, Punjabi NM. Mixed effect Poisson log-linear models for clinical and epidemiological sleep hypnogram data. Statistics in medicine. 2012;31(9):855–870. doi: 10.1002/sim.4457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Silva GE, Vana KD, Goodwin JL, Sherrill DL, Quan SF. Identification of patients with sleep disordered breathing: comparing the four-variable screening tool, STOP, STOP-Bang, and Epworth Sleepiness Scales. J Clin Sleep Med. 2011;7(5):467–472. doi: 10.5664/JCSM.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bianchi MT, Eiseman NA, Cash SS, Mietus J, Peng CK, Thomas RJ. Probabilistic sleep architecture models in patients with and without sleep apnea. J Sleep Res. 2012;21(3):330–341. doi: 10.1111/j.1365-2869.2011.00937.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eiseman NA, Westover MB, Mietus JE, Thomas RJ, Bianchi MT. Classification algorithms for predicting sleepiness and sleep apnea severity. J Sleep Res. 2012;21(1):101–112. doi: 10.1111/j.1365-2869.2011.00935.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kokkarinen J. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. American journal of respiratory and critical care medicine. 2011;183(7):950. doi: 10.1164/ajrccm.183.7.950. author reply 950. [DOI] [PubMed] [Google Scholar]
- 22.Ng CY. Letter by ng regarding article, “prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study”. Circulation. 2011;123(11):e384. doi: 10.1161/CIRCULATIONAHA.110.988857. [DOI] [PubMed] [Google Scholar]
- 23.Chami HA, Resnick HE, Quan SF, Gottlieb DJ. Association of incident cardiovascular disease with progression of sleep-disordered breathing. Circulation. 2011;123(12):1280–1286. doi: 10.1161/CIRCULATIONAHA.110.974022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crainiceanu CM, Caffo BS, Luo S, Zipunnikov VM, Punjabi NM. Population Value Decomposition, a Framework for the Analysis of Image Populations. Journal of the American Statistical Association. 2011;106(495) doi: 10.1198/jasa.2011.ap10089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Laffan A, Caffo B, Swihart BJ, Punjabi NM. Utility of sleep stage transitions in assessing sleep continuity. Sleep. 2010;33(12):1681–1686. doi: 10.1093/sleep/33.12.1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Caffo B, Diener-West M, Punjabi NM, Samet J. A novel approach to prediction of mild obstructive sleep disordered breathing in a population-based sample: the Sleep Heart Health Study. Sleep. 2010;33(12):1641–1648. doi: 10.1093/sleep/33.12.1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bruce EN, Bruce MC, Ramanand P, Hayes D., Jr. Progressive changes in cortical state before and after spontaneous arousals from sleep in elderly and middle-aged women. Neuroscience. 2011;175:184–197. doi: 10.1016/j.neuroscience.2010.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Munoz R, Duran-Cantolla J, Martinez-Vila E. Obstructive sleep apneahypopnea and incident stroke: the sleep heart health study. American journal of respiratory and critical care medicine. 2010;182(10):1332. doi: 10.1164/ajrccm.182.10.1332. author reply 1332–1333. [DOI] [PubMed] [Google Scholar]
- 29.Goldstein C, Zee PC. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. American journal of respiratory and critical care medicine. 2010;182(10):1332. doi: 10.1164/ajrccm.182.10.1332a. author reply 1332–1333. [DOI] [PubMed] [Google Scholar]
- 30.Trotti LM, Bliwise DL. No increased risk of obstructive sleep apnea in Parkinson's disease. Mov Disord. 2010;25(13):2246–2249. doi: 10.1002/mds.23231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Djonlagic I, Malhotra A. Risk of stroke from sleep apnea in men and women. Expert review of neurotherapeutics. 2010;10(8):1267–1271. doi: 10.1586/ern.10.102. [DOI] [PubMed] [Google Scholar]
- 32.Crainiceanu CM, Staicu AM, Di CZ. Generalized Multilevel Functional Regression. Journal of the American Statistical Association. 2009;104(488):1550–1561. doi: 10.1198/jasa.2009.tm08564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gottlieb DJ, Yenokyan G, Newman AB, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122(4):352–360. doi: 10.1161/CIRCULATIONAHA.109.901801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bianchi MT, Cash SS, Mietus J, Peng CK, Thomas R. Obstructive sleep apnea alters sleep stage transition dynamics. PLoS ONE. 2010;5(6):e11356. doi: 10.1371/journal.pone.0011356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Campbell AJ, Neill AM. Home set-up polysomnography in the assessment of suspected obstructive sleep apnea. J Sleep Res. 2011;20(1 Pt 2):207–213. doi: 10.1111/j.1365-2869.2010.00854.x. [DOI] [PubMed] [Google Scholar]
- 36.Zanobetti A, Redline S, Schwartz J, et al. Associations of PM10 with sleep and sleep-disordered breathing in adults from seven U.S. urban areas. American journal of respiratory and critical care medicine. 2010;182(6):819–825. doi: 10.1164/rccm.200912-1797OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baldwin CM, Ervin AM, Mays MZ, et al. Sleep disturbances, quality of life, and ethnicity: the Sleep Heart Health Study. J Clin Sleep Med. 2010;6(2):176–183. [PMC free article] [PubMed] [Google Scholar]
- 38.Redline S, Yenokyan G, Gottlieb DJ, et al. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. American journal of respiratory and critical care medicine. 2010;182(2):269–277. doi: 10.1164/rccm.200911-1746OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Di CZ, Crainiceanu CM, Caffo BS, Punjabi NM. Multilevel Functional Principal Component Analysis. The annals of applied statistics. 2009;3(1):458–488. doi: 10.1214/08-AOAS206SUPP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chami HA, Baldwin CM, Silverman A, et al. Sleepiness, quality of life, and sleep maintenance in REM versus non-REM sleep-disordered breathing. American journal of respiratory and critical care medicine. 2010;181(9):997–1002. doi: 10.1164/rccm.200908-1304OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Crainiceanu CM, Caffo BS, Di CZ, Punjabi NM. Nonparametric Signal Extraction and Measurement Error in the Analysis of Electroencephalographic Activity During Sleep. Journal of the American Statistical Association. 2009;104(486):541–555. doi: 10.1198/jasa.2009.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peppard PE. Is obstructive sleep apnea a risk factor for hypertension?--differences between the Wisconsin Sleep Cohort and the Sleep Heart Health Study. J Clin Sleep Med. 2009;5(5):404–405. [PMC free article] [PubMed] [Google Scholar]
- 43.Neubauer DN. Sleep-disordered breathing and all-cause mortality in the sleep heart health study. Commentary. Postgrad Med. 2009;121(6):197–199. doi: 10.3810/pgm.2009.11.2088. [DOI] [PubMed] [Google Scholar]
- 44.Monahan K, Storfer-Isser A, Mehra R, et al. Triggering of nocturnal arrhythmias by sleep-disordered breathing events. Journal of the American College of Cardiology. 2009;54(19):1797–1804. doi: 10.1016/j.jacc.2009.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chami HA, Keyes MJ, Vita JA, et al. Brachial artery diameter, blood flow and flow-mediated dilation in sleep-disordered breathing. Vascular medicine. 2009;14(4):351–360. doi: 10.1177/1358863X09105132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Silva GE, An MW, Goodwin JL, et al. Longitudinal evaluation of sleep-disordered breathing and sleep symptoms with change in quality of life: the Sleep Heart Health Study (SHHS) Sleep. 2009;32(8):1049–1057. doi: 10.1093/sleep/32.8.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS medicine. 2009;6(8):e1000132. doi: 10.1371/journal.pmed.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thomas RJ, Weiss MD, Mietus JE, Peng CK, Goldberger AL, Gottlieb DJ. Prevalent hypertension and stroke in the Sleep Heart Health Study: association with an ECG-derived spectrographic marker of cardiopulmonary coupling. Sleep. 2009;32(7):897–904. [PMC free article] [PubMed] [Google Scholar]
- 49.Bruce EN, Bruce MC, Vennelaganti S. Sample entropy tracks changes in electroencephalogram power spectrum with sleep state and aging. J Clin Neurophysiol. 2009;26(4):257–266. doi: 10.1097/WNP.0b013e3181b2f1e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Winkelman JW, Redline S, Baldwin CM, Resnick HE, Newman AB, Gottlieb DJ. Polysomnographic and health-related quality of life correlates of restless legs syndrome in the Sleep Heart Health Study. Sleep. 2009;32(6):772–778. doi: 10.1093/sleep/32.6.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.O'Connor GT, Caffo B, Newman AB, et al. Prospective study of sleep-disordered breathing and hypertension: the Sleep Heart Health Study. American journal of respiratory and critical care medicine. 2009;179(12):1159–1164. doi: 10.1164/rccm.200712-1809OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jamasebi R, Johnson NL, Kaffashi F, Redline S, Loparo KA. A watermarking algorithm for polysomnography data. Conference proceedings : Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual Conference. 2008;2008:5720–5723. doi: 10.1109/IEMBS.2008.4650513. [DOI] [PubMed] [Google Scholar]
- 53.Sharief I, Silva GE, Goodwin JL, Quan SF. Effect of sleep disordered breathing on the sleep of bed partners in the Sleep Heart Health Study. Sleep. 2008;31(10):1449–1456. [PMC free article] [PubMed] [Google Scholar]
- 54.Gottlieb DJ. The Sleep Heart Health Study: a progress report. Current opinion in pulmonary medicine. 2008;14(6):537–542. doi: 10.1097/MCP.0b013e328312ed61. [DOI] [PubMed] [Google Scholar]
- 55.Swihart BJ, Caffo B, Bandeen-Roche K, Punjabi NM. Characterizing sleep structure using the hypnogram. J Clin Sleep Med. 2008;4(4):349–355. [PMC free article] [PubMed] [Google Scholar]
- 56.Kapur VK, Resnick HE, Gottlieb DJ Sleep Heart Health Study G. Sleep disordered breathing and hypertension: does self-reported sleepiness modify the association? Sleep. 2008;31(8):1127–1132. [PMC free article] [PubMed] [Google Scholar]
- 57.Stamatakis K, Sanders MH, Caffo B, et al. Fasting glycemia in sleep disordered breathing: lowering the threshold on oxyhemoglobin desaturation. Sleep. 2008;31(7):1018–1024. [PMC free article] [PubMed] [Google Scholar]
- 58.Unruh ML, Sanders MH, Redline S, et al. Subjective and objective sleep quality in patients on conventional thrice-weekly hemodialysis: comparison with matched controls from the sleep heart health study. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2008;52(2):305–313. doi: 10.1053/j.ajkd.2008.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang W, Tretriluxana S, Redline S, Surovec S, Gottlieb DJ, Khoo MC. Association of cardiac autonomic function measures with severity of sleep-disordered breathing in a community-based sample. J Sleep Res. 2008;17(3):251–262. doi: 10.1111/j.1365-2869.2008.00652.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Unruh ML, Redline S, An MW, et al. Subjective and objective sleep quality and aging in the sleep heart health study. J Am Geriatr Soc. 2008;56(7):1218–1227. doi: 10.1111/j.1532-5415.2008.01755.x. [DOI] [PubMed] [Google Scholar]
- 61.Chami HA, Devereux RB, Gottdiener JS, et al. Left ventricular morphology and systolic function in sleep-disordered breathing: the Sleep Heart Health Study. Circulation. 2008;117(20):2599–2607. doi: 10.1161/CIRCULATIONAHA.107.717892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Quan SF, Redline S. Hypopnea scoring in the Sleep Heart Health Study. Chest. 2008;133(4):1054–1055. doi: 10.1378/chest.07-2877. discussion 1055. [DOI] [PubMed] [Google Scholar]
- 63.Punjabi NM, Newman AB, Young TB, Resnick HE, Sanders MH. Sleep-disordered breathing and cardiovascular disease: an outcome-based definition of hypopneas. American journal of respiratory and critical care medicine. 2008;177(10):1150–1155. doi: 10.1164/rccm.200712-1884OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Seicean S, Kirchner HL, Gottlieb DJ, et al. Sleep-disordered breathing and impaired glucose metabolism in normal-weight and overweight/ obese individuals: the Sleep Heart Health Study. Diabetes care. 2008;31(5):1001–1006. doi: 10.2337/dc07-2003. [DOI] [PubMed] [Google Scholar]
- 65.Thomas RJ, Mietus JE, Peng CK, et al. Differentiating obstructive from central and complex sleep apnea using an automated electrocardiogram-based method. Sleep. 2007;30(12):1756–1769. doi: 10.1093/sleep/30.12.1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Winkelman JW, Shahar E, Sharief I, Gottlieb DJ. Association of restless legs syndrome and cardiovascular disease in the Sleep Heart Health Study. Neurology. 2008;70(1):35–42. doi: 10.1212/01.wnl.0000287072.93277.c9. [DOI] [PubMed] [Google Scholar]
- 67.Silva GE, Goodwin JL, Sherrill DL, et al. Relationship between reported and measured sleep times: the sleep heart health study (SHHS) J Clin Sleep Med. 2007;3(6):622–630. [PMC free article] [PubMed] [Google Scholar]
- 68.Gottlieb DJ, O'Connor GT, Wilk JB. Genome-wide association of sleep and circadian phenotypes. BMC medical genetics. 2007;8(Suppl 1):S9. doi: 10.1186/1471-2350-8-S1-S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dickman R, Green C, Fass SS, et al. Relationships between sleep quality and pH monitoring findings in persons with gastroesophageal reflux disease. J Clin Sleep Med. 2007;3(5):505–513. [PMC free article] [PubMed] [Google Scholar]
- 70.Schmitt DT, Ivanov P. Fractal scale-invariant and nonlinear properties of cardiac dynamics remain stable with advanced age: a new mechanistic picture of cardiac control in healthy elderly. American journal of physiology. Regulatory, integrative and comparative physiology. 2007;293(5):R1923–1937. doi: 10.1152/ajpregu.00372.2007. [DOI] [PubMed] [Google Scholar]
- 71.Chowdhuri S. Continuous positive airway pressure for the treatment of sleep apnea. Otolaryngologic clinics of North America. 2007;40(4):807–827. doi: 10.1016/j.otc.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 72.Robbins J, Redline S, Ervin A, Walsleben JA, Ding J, Nieto FJ. Associations of sleep-disordered breathing and cerebral changes on MRI. J Clin Sleep Med. 2005;1(2):159–165. [PubMed] [Google Scholar]
- 73.Redline S, Budhiraja R, Kapur V, et al. The scoring of respiratory events in sleep: reliability and validity. J Clin Sleep Med. 2007;3(2):169–200. [PubMed] [Google Scholar]
- 74.Wattanakit K, Boland L, Punjabi NM, Shahar E. Relation of sleep-disordered breathing to carotid plaque and intima-media thickness. Atherosclerosis. 2008;197(1):125–131. doi: 10.1016/j.atherosclerosis.2007.02.029. [DOI] [PubMed] [Google Scholar]
- 75.Tretriluxana S, M KK, Redline S, Surovec S, Gottlieb D. Cardiac autonomic function in older adults with sleep-disordered breathing. Conference proceedings : Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual Conference. 2005;4:4424–4426. doi: 10.1109/IEMBS.2005.1615447. [DOI] [PubMed] [Google Scholar]
- 76.Tretriluxana S, Khoo MC, Redline S, Surovec SA, Gottlieb DJ. Cardiac autonomic function in older adults with sleep-disordered breathing. Conference proceedings : Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual Conference. 2005;2:1103–1105. doi: 10.1109/IEMBS.2005.1616612. [DOI] [PubMed] [Google Scholar]
- 77.Quan SF, O'Connor GT, Quan JS, et al. Association of physical activity with sleep-disordered breathing. Sleep Breath. 2007;11(3):149–157. doi: 10.1007/s11325-006-0095-5. [DOI] [PubMed] [Google Scholar]
- 78.Unruh ML, Sanders MH, Redline S, et al. Sleep apnea in patients on conventional thrice-weekly hemodialysis: comparison with matched controls from the Sleep Heart Health Study. Journal of the American Society of Nephrology : JASN. 2006;17(12):3503–3509. doi: 10.1681/ASN.2006060659. [DOI] [PubMed] [Google Scholar]
- 79.Patwardhan AA, Larson MG, Levy D, et al. Obstructive sleep apnea and plasma natriuretic peptide levels in a community-based sample. Sleep. 2006;29(10):1301–1306. doi: 10.1093/sleep/29.10.1301. [DOI] [PubMed] [Google Scholar]
- 80.Gottlieb DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29(8):1009–1014. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 81.Zhang L, Samet J, Caffo B, Punjabi NM. Cigarette smoking and nocturnal sleep architecture. American journal of epidemiology. 2006;164(6):529–537. doi: 10.1093/aje/kwj231. [DOI] [PubMed] [Google Scholar]
- 82.Quan SF, Wright R, Baldwin CM, et al. Obstructive sleep apnea-hypopnea and neurocognitive functioning in the Sleep Heart Health Study. Sleep Med. 2006;7(6):498–507. doi: 10.1016/j.sleep.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 83.Grigg-Damberger M. Why a polysomnogram should become part of the diagnostic evaluation of stroke and transient ischemic attack. J Clin Neurophysiol. 2006;23(1):21–38. doi: 10.1097/01.wnp.0000201077.44102.80. [DOI] [PubMed] [Google Scholar]
- 84.Mehra R, Benjamin EJ, Shahar E, et al. Association of nocturnal arrhythmias with sleep-disordered breathing: The Sleep Heart Health Study. American journal of respiratory and critical care medicine. 2006;173(8):910–916. doi: 10.1164/rccm.200509-1442OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Health Quality O. Polysomnography in patients with obstructive sleep apnea: an evidence-based analysis. Ontario health technology assessment series. 2006;6(13):1–38. [PMC free article] [PubMed] [Google Scholar]
- 86.Newman AB, Foster G, Givelber R, Nieto FJ, Redline S, Young T. Progression and regression of sleep-disordered breathing with changes in weight: the Sleep Heart Health Study. Archives of internal medicine. 2005;165(20):2408–2413. doi: 10.1001/archinte.165.20.2408. [DOI] [PubMed] [Google Scholar]
- 87.Redline S, Min NI, Shahar E, Rapoport D, O'Connor G. Polysomnographic predictors of blood pressure and hypertension: is one index best? Sleep. 2005;28(9):1122–1130. doi: 10.1093/sleep/28.9.1122. [DOI] [PubMed] [Google Scholar]
- 88.Kapur VK, Baldwin CM, Resnick HE, Gottlieb DJ, Nieto FJ. Sleepiness in patients with moderate to severe sleep-disordered breathing. Sleep. 2005;28(4):472–477. doi: 10.1093/sleep/28.4.472. [DOI] [PubMed] [Google Scholar]
- 89.Levy AP, Zhang L, Miller-Lotan R, et al. Haptoglobin phenotype, sleep-disordered breathing, and the prevalence of cardiovascular disease: the Sleep Heart Health Study. Sleep. 2005;28(2):207–213. doi: 10.1093/sleep/28.2.207. [DOI] [PubMed] [Google Scholar]
- 90.Baldwin CM, Bell IR, Guerra S, Quan SF. Obstructive sleep apnea and ischemic heart disease in southwestern US veterans: implications for clinical practice. Sleep Breath. 2005;9(3):111–118. doi: 10.1007/s11325-005-0025-y. [DOI] [PubMed] [Google Scholar]
- 91.Fass R, Quan SF, O'Connor GT, Ervin A, Iber C. Predictors of heartburn during sleep in a large prospective cohort study. Chest. 2005;127(5):1658–1666. doi: 10.1378/chest.127.5.1658. [DOI] [PubMed] [Google Scholar]
- 92.Gottlieb DJ, Punjabi NM, Newman AB, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Archives of internal medicine. 2005;165(8):863–867. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- 93.Haas DC, Foster GL, Nieto FJ, et al. Age-dependent associations between sleep-disordered breathing and hypertension: importance of discriminating between systolic/diastolic hypertension and isolated systolic hypertension in the Sleep Heart Health Study. Circulation. 2005;111(5):614–621. doi: 10.1161/01.CIR.0000154540.62381.CF. [DOI] [PubMed] [Google Scholar]
- 94.Pittman SD, MacDonald MM, Fogel RB, et al. Assessment of automated scoring of polysomnographic recordings in a population with suspected sleep-disordered breathing. Sleep. 2004;27(7):1394–1403. doi: 10.1093/sleep/27.7.1394. [DOI] [PubMed] [Google Scholar]
- 95.Morse CA, Quan SF, Mays MZ, Green C, Stephen G, Fass R. Is there a relationship between obstructive sleep apnea and gastroesophageal reflux disease? Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2004;2(9):761–768. doi: 10.1016/s1542-3565(04)00347-7. [DOI] [PubMed] [Google Scholar]
- 96.Punjabi NM, Shahar E, Redline S, et al. Sleep-disordered breathing, glucose intolerance, and insulin resistance: the Sleep Heart Health Study. American journal of epidemiology. 2004;160(6):521–530. doi: 10.1093/aje/kwh261. [DOI] [PubMed] [Google Scholar]
- 97.Gottlieb DJ, DeStefano AL, Foley DJ, et al. APOE epsilon4 is associated with obstructive sleep apnea/hypopnea: the Sleep Heart Health Study. Neurology. 2004;63(4):664–668. doi: 10.1212/01.wnl.0000134671.99649.32. [DOI] [PubMed] [Google Scholar]
- 98.Iber C, Redline S, Kaplan Gilpin AM, et al. Polysomnography performed in the unattended home versus the attended laboratory setting--Sleep Heart Health Study methodology. Sleep. 2004;27(3):536–540. doi: 10.1093/sleep/27.3.536. [DOI] [PubMed] [Google Scholar]
- 99.Ding J, Nieto FJ, Beauchamp NJ, Jr., et al. Sleep-disordered breathing and white matter disease in the brainstem in older adults. Sleep. 2004;27(3):474–479. doi: 10.1093/sleep/27.3.474. [DOI] [PubMed] [Google Scholar]
- 100.Boland LL, Shahar E, Wong TY, et al. Sleep-disordered breathing is not associated with the presence of retinal microvascular abnormalities: the Sleep Heart Health Study. Sleep. 2004;27(3):467–473. doi: 10.1093/sleep/27.3.467. [DOI] [PubMed] [Google Scholar]
- 101.Baldwin CM, Kapur VK, Holberg CJ, Rosen C, Nieto FJ Sleep Heart Health Study G. Associations between gender and measures of daytime somnolence in the Sleep Heart Health Study. Sleep. 2004;27(2):305–311. doi: 10.1093/sleep/27.2.305. [DOI] [PubMed] [Google Scholar]
- 102.Walsleben JA, Kapur VK, Newman AB, et al. Sleep and reported daytime sleepiness in normal subjects: the Sleep Heart Health Study. Sleep. 2004;27(2):293–298. doi: 10.1093/sleep/27.2.293. [DOI] [PubMed] [Google Scholar]
- 103.Sanders MH, Givelber R. Sleep disordered breathing may not be an independent risk factor for diabetes, but diabetes may contribute to the occurrence of periodic breathing in sleep. Sleep Med. 2003;4(4):349–350. doi: 10.1016/s1389-9457(03)00118-7. [DOI] [PubMed] [Google Scholar]
- 104.Lind BK, Goodwin JL, Hill JG, Ali T, Redline S, Quan SF. Recruitment of healthy adults into a study of overnight sleep monitoring in the home: experience of the Sleep Heart Health Study. Sleep Breath. 2003;7(1):13–24. doi: 10.1007/s11325-003-0013-z. [DOI] [PubMed] [Google Scholar]
- 105.O'Connor GT, Lind BK, Lee ET, et al. Variation in symptoms of sleep-disordered breathing with race and ethnicity: the Sleep Heart Health Study. Sleep. 2003;26(1):74–79. [PubMed] [Google Scholar]
- 106.Resnick HE, Redline S, Shahar E, et al. Diabetes and sleep disturbances: findings from the Sleep Heart Health Study. Diabetes care. 2003;26(3):702–709. doi: 10.2337/diacare.26.3.702. [DOI] [PubMed] [Google Scholar]
- 107.Shahar E, Redline S, Young T, et al. Hormone replacement therapy and sleep-disordered breathing. American journal of respiratory and critical care medicine. 2003;167(9):1186–1192. doi: 10.1164/rccm.200210-1238OC. [DOI] [PubMed] [Google Scholar]
- 108.Sanders MH, Newman AB, Haggerty CL, et al. Sleep and sleep-disordered breathing in adults with predominantly mild obstructive airway disease. American journal of respiratory and critical care medicine. 2003;167(1):7–14. doi: 10.1164/rccm.2203046. [DOI] [PubMed] [Google Scholar]
- 109.Quan SF, Griswold ME, Iber C, et al. Short-term variability of respiration and sleep during unattended nonlaboratory polysomnography--the Sleep Heart Health Study. Sleep. 2002;25(8):843–849. [PubMed] [Google Scholar]
- 110.Boland LL, Shahar E, Iber C, et al. Measures of cognitive function in persons with varying degrees of sleep-disordered breathing: the Sleep Heart Health Study. J Sleep Res. 2002;11(3):265–272. doi: 10.1046/j.1365-2869.2002.00308.x. [DOI] [PubMed] [Google Scholar]
- 111.Kapur V, Strohl KP, Redline S, Iber C, O'Connor G, Nieto J. Underdiagnosis of sleep apnea syndrome in U.S. communities. Sleep Breath. 2002;6(2):49–54. doi: 10.1007/s11325-002-0049-5. [DOI] [PubMed] [Google Scholar]
- 112.Kapur VK, Redline S, Nieto FJ, et al. The relationship between chronically disrupted sleep and healthcare use. Sleep. 2002;25(3):289–296. [PubMed] [Google Scholar]
- 113.Young T, Shahar E, Nieto FJ, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Archives of internal medicine. 2002;162(8):893–900. doi: 10.1001/archinte.162.8.893. [DOI] [PubMed] [Google Scholar]
- 114.Guidry UC, Mendes LA, Evans JC, et al. Echocardiographic features of the right heart in sleep-disordered breathing: the Framingham Heart Study. American journal of respiratory and critical care medicine. 2001;164(6):933–938. doi: 10.1164/ajrccm.164.6.2001092. [DOI] [PubMed] [Google Scholar]
- 115.Newman AB, Nieto FJ, Guidry U, et al. Relation of sleep-disordered breathing to cardiovascular disease risk factors: the Sleep Heart Health Study. American journal of epidemiology. 2001;154(1):50–59. doi: 10.1093/aje/154.1.50. [DOI] [PubMed] [Google Scholar]
- 116.Redline S, Sanders MH, Lind BK, et al. Methods for obtaining and analyzing unattended polysomnography data for a multicenter study. Sleep Heart Health Research Group. Sleep. 1998;21(7):759–767. [PubMed] [Google Scholar]
- 117.Whitney CW, Gottlieb DJ, Redline S, et al. Reliability of scoring respiratory disturbance indices and sleep staging. Sleep. 1998;21(7):749–757. doi: 10.1093/sleep/21.7.749. [DOI] [PubMed] [Google Scholar]
- 118.Baldwin CM, Griffith KA, Nieto FJ, O'Connor GT, Walsleben JA, Redline S. The association of sleep-disordered breathing and sleep symptoms with quality of life in the Sleep Heart Health Study. Sleep. 2001;24(1):96–105. doi: 10.1093/sleep/24.1.96. [DOI] [PubMed] [Google Scholar]
- 119.Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. American journal of respiratory and critical care medicine. 2001;163(1):19–25. doi: 10.1164/ajrccm.163.1.2001008. [DOI] [PubMed] [Google Scholar]
- 120.Harding SM. Complications and consequences of obstructive sleep apnea. Current opinion in pulmonary medicine. 2000;6(6):485–489. doi: 10.1097/00063198-200011000-00004. [DOI] [PubMed] [Google Scholar]
- 121.Boehlecke BA. Epidemiology and pathogenesis of sleep-disordered breathing. Current opinion in pulmonary medicine. 2000;6(6):471–478. doi: 10.1097/00063198-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 122.Gottlieb DJ, Yao Q, Redline S, Ali T, Mahowald MW. Does snoring predict sleepiness independently of apnea and hypopnea frequency? American journal of respiratory and critical care medicine. 2000;162(4 Pt 1):1512–1517. doi: 10.1164/ajrccm.162.4.9911073. [DOI] [PubMed] [Google Scholar]
- 123.Kapur VK, Rapoport DM, Sanders MH, et al. Rates of sensor loss in unattended home polysomnography: the influence of age, gender, obesity, and sleep-disordered breathing. Sleep. 2000;23(5):682–688. [PubMed] [Google Scholar]
- 124.Young T, Peppard P. Sleep-disordered breathing and cardiovascular disease: epidemiologic evidence for a relationship. Sleep. 2000;23(Suppl 4):S122–126. [PubMed] [Google Scholar]
- 125.Nieto FJ, Young TB, Lind BK, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA. 2000;283(14):1829–1836. doi: 10.1001/jama.283.14.1829. [DOI] [PubMed] [Google Scholar]
- 126.Redline S, Kapur VK, Sanders MH, et al. Effects of varying approaches for identifying respiratory disturbances on sleep apnea assessment. American journal of respiratory and critical care medicine. 2000;161(2 Pt 1):369–374. doi: 10.1164/ajrccm.161.2.9904031. [DOI] [PubMed] [Google Scholar]
- 127.Loube DI, Gay PC, Strohl KP, Pack AI, White DP, Collop NA. Indications for positive airway pressure treatment of adult obstructive sleep apnea patients: a consensus statement. Chest. 1999;115(3):863–866. doi: 10.1378/chest.115.3.863. [DOI] [PubMed] [Google Scholar]
- 128.Gottlieb DJ, Whitney CW, Bonekat WH, et al. Relation of sleepiness to respiratory disturbance index: the Sleep Heart Health Study. American journal of respiratory and critical care medicine. 1999;159(2):502–507. doi: 10.1164/ajrccm.159.2.9804051. [DOI] [PubMed] [Google Scholar]
- 129.Phillips BA, Anstead MI, Gottlieb DJ. Monitoring sleep and breathing: methodology. Part I: Monitoring breathing. Clinics in chest medicine. 1998;19(1):203–212. doi: 10.1016/s0272-5231(05)70442-1. [DOI] [PubMed] [Google Scholar]
- 130.Quan SF, Howard BV, Iber C, et al. The Sleep Heart Health Study: design, rationale, and methods. Sleep. 1997;20(12):1077–1085. [PubMed] [Google Scholar]
REFERENCES
- 1.United States Department of Health & Human Services. Prevention. 2015. [Accessed March 13, 2015]. Available at: http://www.hhs.gov/safety.
- 2.United States Department of Health & Human Services. Healthy People 2020 Topics & Objectives: Sleep Health. 2015. [Accessed March 13, 2015]. Available at: http://www.healthypeople.gov/2020/topics-objectives/topic/sleep-health.
- 3.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. 2014. [Accessed March 13, 2015]. Available at: http://www.cdc.gov/brfss/questionnaires.htm.
- 4.National Institutes of Health National Heart Lung and Blood Institute National Center on Sleep Disorders Research. Guide to Selected Publicly Available Sleep-Related Data Resources. 2006. [Accessed December 10, 2013]. Available at: http://www.nhlbi.nih.gov/files/docs/ncsdr/sleep-datasets-july-06.pdf.
- 5.Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38:843–4. doi: 10.5665/sleep.4716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Watson NF, Badr MS, Belenky G, et al. Joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and discussion. Sleep. 2015;38:1161–83. doi: 10.5665/sleep.4886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health: Journal of the National Sleep Foundation. 1:40–3. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 8.Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37:9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caffo B, Diener-West M, Punjabi NM, Samet J. A novel approach to prediction of mild obstructive sleep disordered breathing in a population-based sample: the Sleep Heart Health Study. Sleep. 2010;33:1641–8. doi: 10.1093/sleep/33.12.1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fowler FJ. Improving survey questions: design and evaluation. Thousand Oaks, CA: Sage Publications; 1995. [Google Scholar]
- 11.Madans J, Miller K, Maitland A, Willis G. Contributing to the science of data quality. New Jersey: John Wiley and Sons; 2011. [Google Scholar]
- 12.Centers for Disease Control and Prevention. Questionnaire Design Research Laboratory. 2014. [Accessed March 13, 2015]. Available at: http://www.cdc.gov/qdrl/