Abstract
Mounting an efficient immune response to pathogens while avoiding damage to host tissues is the central task of the immune system. Emerging evidence has highlighted the contribution of the CD8+ lineage of regulatory T cells to the maintenance of self-tolerance. Specific recognition of the MHC class Ib molecule Qa-1 complexed to peptides expressed by activated CD4+ T cells by regulatory CD8+ T cells triggers an inhibitory interaction that prevents autoimmune responses. Conversely, defective Qa-1-restricted CD8+ regulatory activity can result in development of systemic autoimmune disease. Here, we review recent research into the cellular and molecular basis of these regulatory T cells, their mechanism of suppressive activity and the potential application of these insights into new treatments for autoimmune disease and cancer.
Keywords: CD8+ regulatory T cells, Qa-1, HLA-E, IL-15, autoimmunity
1. Introduction
The stochastic process that produces T cell clones that express high affinity receptors to self-antigen also generates the potential for autoimmunity. This outcome is generally avoided by a contribution of cell-intrinsic and -extrinsic mechanisms that include deletion of self-reactive T cell clones in the thymus and active immune suppression by regulatory T cells in the periphery. A well-studied example of regulation is the subset of CD4+ T cells expressing FoxP3 that prevents inflammatory damage during the course of normal immune responses. Recent advances in analysis of the CD8+ lineage of regulatory T cells (hereafter CD8+ Treg) have underscored the contribution of Qa-1-restricted CD8+ Treg to the maintenance of self-tolerance. Here we discuss the cellular and molecular basis for development and function of Qa-1-restricted CD8+ Treg. We also discuss recent insights into the biology of Qa-1-restricted CD8+ Treg that suggest novel therapeutic applications of CD8+ Treg in the context of autoimmune disease and cancer.
2. Qa-1 and HLA-E
Qa-1 is the murine homolog of human leukocyte antigen-E (HLA-E), a non-classical MHC class Ib molecule encoded by the H2-T23 gene on chromosome 17. Qa-1 was first described as essential to the generation of CD8+ T cell suppression [1,2] and is expressed mainly at the surface of activated T and B lymphoctyes and dendritic cells. Qa-1 is relatively nonpolymorphic (Qa-1a and Qa-1b) and is expressed at somewhat lower levels than MHC class Ia molecules [3]. Qa-1 binds two receptors with opposing functions: (1) engagement of the T cell receptor (TCR) by Qa-1–peptide complexes leads to activation and expansion of antigen-specific CD8+ T cells, while (2) engagement of the CD94/NKG2A receptor expressed by CD8+ T cells, natural killer (NK) and NKT cells by Qa-1–Qdm peptide ligands attenuates the activities of these cells (Fig. 1).
Fig. 1.
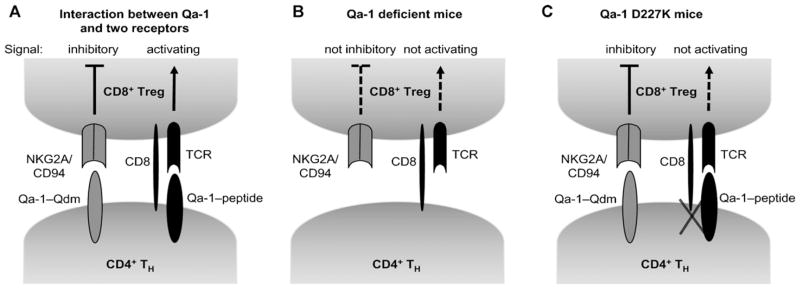
Dual binding activity of Qa-1 and generation of Qa-1 mutant mice. (A) Engagement of Qa-1 with NKG2A/CD94 and TCR delivers opposing signal. (B) Lack of two opposing signals in Qa-1 deficient mice results in compensated phenotype. (C) Qa-1 D227K mutation leads to the interruption of TCR and Qa-1–peptide binding that leads to the lack of CD8+ Treg activity. Qa-1 D227K mice develop lupus-like autoimmune disorder.
Qa-1 and HLA-E present a dominant set of peptides derived from the signal sequence of MHC class Ia molecules, termed Qdm for Qa-1 determinant modifier [4–6]. However, since Qa-1 forms a relatively unstable complex with the Qdm peptide (AMAPRTLLL), most of surface Qa-1–Qdm reflects newly complexed Qdm peptide, and thus an accurate monitor of the cell’s class I MHC expression [7]. Qa-1–Qdm complexes depend on TAP function, consistent with the release of Qdm-containing fragments from H-2D/L leader sequences into the cytoplasm after cleavage by signal peptide peptidases [8–10]. In addition to the major Qdm peptide, Qa-1 presents peptides derived from proteins associated with infection or inflammatory responses, e.g. a peptide from Heat Shock Protein 60 (GMKFDRGYI) is a dominant peptide bound to Qa-1 [11]. Qa-1 binding peptides display a conserved motif consisting of a nonamer with termini embedded in the antigen-binding groove and two dominant anchors (Met at position 2 and Leu at position 9) as well as additional subdominant anchors [5,6,12,13]. In addition to dominant peptides presented by Qa-1, additional peptides have been reported to bind Qa-1, including a peptide from the leader sequence of preproinsulin, peptides from the TCR Vβ sequence [14–16], an unknown peptide derived from Listeria monocytogenes, an immunodominant epitope from Salmonella typhimurium GroEL (GMQFDRGYL) [17] and a signal peptide derived from the leader sequence of heat shock protein (HSP60sp). A recent study suggested that Qa-1–Hsp60sp presented by a subset of autoreactive CD4+ cells with intermediate affinity for antigen are targeted by Qa-1-restricted CD8+ T cells [18,19]. The limited polymorphism and restricted peptide-binding repertoire of Qa-1 may dampen cross-reactive recognition and reduce non-specific suppression of activated CD4 cells by Qa-1-restricted CD8+ Treg [20]. In contrast, transformed cells express a surprisingly broad array of peptides that bind to Qa-1 [21], opening the possibility that defects in Qa-1–peptide processing associated with transformation may alter the Qa-1–peptide repertoire expressed by tumors.
At the protein level, HLA-E shares 73% homology with Qa-1, consistent with their similar functions and peptide repertoires [22,23]. HLA-E is the least polymorphic of all the MHC class I molecules [24] and, like Qa-1, selectively binds MHC class Ia leader sequence-derived peptides with sequences similar to Qdm [12,25]. The crystal structure of HLA-E bound to a human leader sequence-derived peptide demonstrates a modified hydrogen bond network and other structural features that suggest that HLA-E has evolved to bind selectively and tightly to a highly homologous set of MHC class Ia-derived leader sequence peptides, B7sp [26]. In addition to the dominant peptide B7sp, HLA-E binding peptides derived from viruses, including the gpUL4015–23-leader sequence from human CMV [27], a peptide derived from BZLF-39–47 protein of Epstein–Barr Virus (EBV), and a peptide derived from influenza virus (InflM59–67) [28], or from heat shock proteins (Hsp60) have been identified. HLA-E dependent presentation of a Mycobacterium tuberculosis-derived antigen and a peptide derived from the trans-membrane domain of the human ATP-binding cassette protein, MRP7 to human CD8+ T cells has also been reported [29,30]. In addition, it has been proposed that TCR Vβ-derived peptides may be associated with HLA-E molecules expressed by CD4+ T cells, rendering these cells susceptible to CTL-mediated lysis [31].
Recognition of Qa-1 (and HLA-E) by NKG2A/CD94 receptors depends on the associated Qdm peptide [6]. Thus, Qdm dissociation or replacement with other peptides results in loss of recognition by NKG2A/CD94, relieving the inhibitory signal. A recent study demonstrated that an interaction between Qa-1 and NKG2A protects activated CD4+ T cells from lysis by NKG2A+ NK cells. CD4+ T cells from mice expressing a Qa-1 point mutation (R72A) that selectively abolishes Qa-1–Qdm binding to CD94/NKG2A receptors fail to undergo antigen-induced or homeostatic expansion secondary to increased susceptibility to lysis by NK cells [32].
3. Qa-1 restricted CD8+ regulatory T cells and autoimmunity
Early studies detected a subpopulation of CD8+ T cells that efficiently suppressed T helper activity for B cells in a Qa-1-dependent fashion [33–35]. This activity was termed feedback inhibition since levels of suppressive activity exerted by CD8+ T cells increased in proportion to the numbers of activated CD4+ T cells [1]. In the early 1980s it was demonstrated that intravenous inoculation of syngeneic rats with a myelin basic protein (MBP)-reactive cell line attenuated by irradiation or treatment with mitomycin C augmented resistance to EAE caused by challenge with MBP. This beneficial effect of “T cell vaccination” (TCV) with self-reactive T cells was attributed to the exposure of CD8+ T cells to autologous, activated CD4+ T cells [36,37]. A series of subsequent studies demonstrated that depletion of CD8+ T cells, by using anti-CD8 monoclonal antibodies or CD8-deficient mice, completely abrogated TCV-induced protection of EAE [36,38], suggesting the regulatory role of CD8+ T cells in TCV-induced immune suppression. Further studies firmly established that immune regulation mediated by CD8+ T cells was dependent on an interaction between Qa-1–peptide on activated CD4+ T cells and TCR on CD8+ T cells in multiple murine models of autoimmune disease, including EAE, Herpes Stromal Keratitis and Type I Diabetes (T1D) [15,39–41].
An HLA-E-restricted regulatory pathway has also been implicated in the immunopathogenesis of human autoimmune disease. Individuals with recent-onset T1D display defects in the ability of CD8+ T cells to suppress autoreactive CD4+ T cells in vitro. This deficit could be restored by in vitro stimulation with DC loaded with HLA-E binding peptide, suggesting HLA-E-restricted CD8+ Treg for immunotherapy of T1D [42]. In addition, CD8+ T cell clones that specifically recognize and lyse activated myelin-reactive CD4+ T cells in an HLA-E-restricted manner were identified in peripheral blood and cerebrospinal fluid of patients with multiple sclerosis (MS) [43]. The frequency of these regulatory CD8+ T cells was substantially decreased in peripheral blood and CSF of MS patients during disease exacerbation compared with patients in remission and disease-free controls, suggesting an inverse correlation between CD8+ Treg activity and disease progression. By contrast, studies of human CMV infection suggest that downregulation of HLA class Ia molecules and upregulation of HLA-E contribute to the generation of HLA-E-restricted anti-viral CTL [44]. Whether HLA-E-restricted CD8+ T cells observed in these different immunological settings represent functionally distinct CD8+ subsets with identical MHC restriction is not understood.
3.1. Qa-1 mutant mice
Insight into the physiological role of Qa-1-restricted CD8+ T cells in control of the immune response has come from studies of mice deficient in Qa-1 expression [41]. Qa-1 deficient mice develop exaggerated secondary CD4 responses after viral infection (Herpes simplex virus, KOS strain) or immunization with self-peptides (PLP) leading to the autoimmune disorders, Herpes Stromal Keratitis and EAE, respectively. A prominent feature of CD8+ Treg identified in studies of Qa-1 deficient mice is that they arise late in the immune response and become functionally apparent after restimulation by antigen, when they inhibit antigen-activated CD4+ T cells. This observation suggests that development of Qa-1-restricted suppressive activity may closely resemble that of CD8+ cell-dependent cytolytic activity rather than that of CD4+CD25+ regulatory activity. Both CD8+ T cell-dependent activities require primary immunization to achieve either TCR-dependent lysis of virally infected target cells or Qa-1-restricted elimination of activated CD4+ T cells [41]. Nevertheless, although Qa-1 deficient mice display dysregulated immune responses to self and foreign antigens, they did not develop spontaneous autoimmune disease. This phenotype of Qa-1 deficient mice reflects functionally opposed interactions between Qa-1–peptide and its two receptors: diminished interactions between Qa-1-restricted CD8+ T cells and Qa-1 deficient CD4+ T cells resulted in enhanced CD4 responses, while enhanced NK lysis of activated CD4+ T cells prevented generation of CD4 memory responses (Fig. 1) [32,41].
To define the distinct contribution of these two receptor interactions, two Qa-1 knock-in mouse strains that express mutant Qa-1 molecules that differentially engage the TCR and NKG2 receptors have allowed a molecular dissection of the contribution of these Qa-1-dependent recognition events to suppressive CD8+ T cells activity. These mutant C57BL/6 mice contain an amino acid exchange mutation at Qa-1 position 227 (D → K) that disrupts Qa-1 binding to the TCR/CD8 co-receptor, but has no effect on Qa-1 engagement of the inhibitory NKG2A receptor on CD8 and NK cells, as judged by tetramer studies and functional analyses (Fig. 1) [45]. At approximately 6 months of age, Qa-1 (D227K) mice develop severe autoimmune disease marked by generation of autoantibodies to multiple tissues, lymphocyte/monocyte infiltration into non-lymphoid tissues, and membranous glomerulonephritis. Activation of the immune system by microbial and non-microbial foreign antigens accelerates the tempo and intensity of this autoimmune disorder. The lupus-like syndrome that develops in Qa-1 D227K mice reflects dysregulated activity of follicular T helper (TFH) cells. This CD4+ TH subset expresses high levels of Qa-1 in the steady state and is the preferential cellular target of Qa-1-restricted regulation by CD8+ T cells. Disruption of Qa-1-dependent regulation of TFH cells in Qa-1 D227K mice results in the production of autoantibodies, highlighting the importance of regulation of this specialized CD4+ TH subset to self-tolerance.
Qa-1-restricted CD8+ Treg cells exert suppressive activity via perforin-dependent elimination of target CD4+ T cells, e.g. perforin-deficient CD8+ Treg cells fail to mediate significant Qa-1-restricted suppression of TFH target cells. Elimination of target TFH cells, rather than induction of anergy or inhibition of proliferation, may represent the most efficient suppressive mechanism, which can remove self-reactive CD4+ T cell clones from the T cell pool. An important feature of Qa-1-restricted CD8+ Treg is their dependence on IL-15 for development and activity [46]: (1) CD8+ T cells from IL-15 deficient donors lack inhibitory activity; (2) injection of anti-IL-15 antibody into adoptive hosts prevented suppression by CD8+ Treg cells obtained from IL-15 WT B6 donors. The IL-15-dependence of Qa-1-restricted CD8+ Treg has led to identification of specific surface markers expressed on Qa-1-restricted CD8+ T cells ([47] and see below) and opened the possibility of expanding this specialized CD8+ T cell lineage without contamination by conventional CD8 cells.
4. Expression of inhibitory NK-cell receptors on CD8+ regulatory T cells
4.1. Ly49 expression on Qa-1 restricted CD8+ Treg
The finding that IL-15 is required for the development and function of Qa-1-restricted CD8 Treg facilitated identification of a triad of surface markers – CD44, CD122, and the class I MHC inhibitory receptor Ly49 – that reliably isolate this specialized CD8+ T cell lineage [47]. Analysis of IL-15 deficient mice revealed that the small CD8+ subset expresses CD44, CD122 and Ly49 is not detectable [47]. Moreover, Ly49+ CD8+ T cells efficiently suppressed CD4+ T cells from WT mice, but not Qa-1 D227K mice, suggesting that Ly49+ CD8+ T cells display Qa-1-dependent suppressive activity. Ly49− CD8+ T cells, by contrast, did not suppress CD4+ cell responses [47]. Impaired suppressive activity of IL-15 deficient CD8+ T cells observed in adoptive transfer experiments reflected the absence of this subpopulation. CD44+CD122+Ly49+ CD8+ T cells, which represent 3–5% of all CD8+ T cells and account for virtually all Qa-1-restricted suppressive activity invested in CD8+ T cells. These characteristics of Qa-1-restricted CD8+ T cells suggest that they display several features of NK cells that belong to the innate immune system. Inhibitory Ly49 receptors belonging to a multigenic/multiallelic family recognize classical MHC class I molecules, and can transduce inhibitory signals by associating ITIM-bearing adaptors [48]. Ly49+ T cells are CD8+ αβ-TCR+ T cells and express memory phenotype surface markers (CD44, CD122 and Ly6c). The size of the Ly49+ subset increases with age, possibly by repeated exposure to self-antigen. Generation of this subset of CD8+ T cells also appears to depend on the presence of CD4+ T cells [49]. Possibly, generation of this sublineage of CD8+ T cells includes signals that depend on an interaction between Qa-1–peptide expressed on CD4+ T cells and TCR on CD8+ T cells. Studies of TAP1−/− and Kb−/−Db−/− mice indicate a dramatic reduction of Ly49+ CD8+ T cells, suggesting that the development of Ly49+CD8+ T cells is MHC class Ia dependent [50]. Alternatively, these findings may reflect TAP-dependent processing of dominant Qdm peptides (derived from class I leader sequences).
The phenotype of Ly49+ CD8+ T cells is stable in vitro upon provision of the IL-15 cytokine, and Ly49− CD8+ T cells do not acquire Ly49 expression, even in the presence of high concentrations of IL-15 [47]. Interestingly, surface expression levels of Ly49 increase with the concentrations of IL-15 (unpublished data), indicating an interconnection of the IL-15 pathway with the Ly49 class I receptor. One particular Ly49 receptor, Ly49F, is expressed by ~90% of Ly49+CD8+αβ-TCR+ T cells in B6 mice, whereas less than 10% of NK cells express this subtype of Ly49 receptor. Ly49F does not bind to H-2b and displays weak binding activity with H-2d. A strong ligand for Ly49F remains to be identified.
The significance of inhibitory NK-receptor expression by specialized CD8+ Treg is unclear. Although engagement of Ly49 can inhibit CD8+ T-cell activation [50], ligation of inhibitory Ly49 molecules also may decrease activation-induced cell death and thereby protect these CD8+ T cells from premature elimination [51–54]. Since many of these cells may display self-reactivity through recognizing Qa-1–self-peptide recognition, this inhibitory machinery may limit suppression of target T cells expressing low levels of Qa-1–peptide while prolonging survival of CD8+ Treg, resulting in a balanced immune response.
4.2. KIR expression on HLA-E-restricted CD8+ cells
Killer cell immunoglobulin-like receptors (KIR) in humans correspond functionally to murine Ly49 receptors. KIR+CD8+ T cells, which can be isolated from spleen, tonsils, lymph nodes and peripheral blood, represent ~4.5% of T cells in healthy individuals [55,56]. Similar to Ly49+ CD8+ T cells in mouse, CD8+ T cells mainly express inhibitory, rather than activating KIR:KIR2DL1, KIR2DL2/3, KIR3DL2, KIR3DL1 [57]. KIR+ T cells in normal donors represent oligoclonal or monoclonal expansion that may reflect chronic, antigen-driven stimulation [58]. The size of the KIR+CD8+αβ-TCR+ T cell compartment increases with age, similar to Ly49+ CD8+ T cells in mouse. KIR+CD8+αβ-TCR+ T cells have a memory phenotype characterized by a lack of expression of CCR7 and failure to detect cell-surface CD28 and CD27. Intracytoplasmic expression of perforin is a hallmark of KIR+ CD8+ T cells, in keeping with CD56 expression, both characteristics of cells with cytolytic potential [59]. Human CD8+ T cell clones isolated from KIR+CD8+αβ-TCR+ T cells recognize HLA-E, consistent with findings that Ly49+CD8+ T cells in mice exert Qa-1-dependent suppression [27,47,60,61]. In contrast to the phenotypic stability of Ly49+CD8+ T cells in mouse, KIR expression along with the acquisition of NK receptors (NKG2A, NKG2D and CD56) on human CD8+ T cells can be induced by the IL-15 cytokine in vitro. Acquisition of these NK receptors correlates with increased levels of granzyme B and perforin [59]. Further analysis is needed to determine whether this subset of human CD8+ T cells mediates HLA-E-dependent suppression of activated human CD4+ memory helper T cells.
5. CD8+ T cells that express a memory phenotype and suppressive function
Although expression of CD122 on CD8+ T cells is associated with acquisition of memory function, studies of CD122−/− (IL-2β−/−) mice has suggested that CD122 expression may be an important component of regulatory T cells. Thus, CD122−/− mice have high levels of serum IgG and autoantibodies as well as a myeloproliferative disorder, which may be attributed to dysregulated CD4+ T cell responses [62]. Since CD122 deficient mice lack not only CD8+CD122+ Treg but also functional CD4+CD25+ Treg (because a signal from the IL-2 receptor-β chain is essential for FoxP3-dependent development of CD4+CD25+ Treg [63,64]), experiments to define the contribution of CD4+ and CD8+ Treg were necessary. The contribution of CD122+ CD8+ T cells to maintenance of T cell homeostasis was evident from transfer studies of CD122+ CD8+ T cells into CD122-deficient neonates, which completely prevented the development of abnormal T cells. Moreover, transfer of CD8 T cells depleted of the CD122+ fraction into Rag2−/− hosts was lethal in secondary hosts due to dysregulation of hematopoietic cells [65]. Interestingly, Treg activity cannot be induced from CD8+CD122− cells even if CD122 expression is restored, suggesting that expression of CD122 is not sufficient to provide regulatory activity [65]. In retrospect, this observation may indicate the existence of a subpopulation within the CD122+CD8+ T cell pool that displays Qa-1-restricted suppressive activity (e.g., the Ly49+ fraction of CD122+ CD8+ T cells). Further studies using murine autoimmune disease models (EAE, CD4+ T cell-induced colitis, Grave’s disease) clearly demonstrated the regulatory role of CD122-expressing memory phenotype CD8+ T cells. In accord with these observations, CD122+CD8+ T cells also inhibited tumor-specific T cell responses, resulting in suppression of vaccine-induced anti-tumor responses [66]. These CD122+CD8+ Treg produced IL-10 and suppressed IFNγ production by CD4+ and CD8+ target cells [67–69]. MHC class Ia dependent and non-cytolytic mechanisms have been suggested to account for suppressive activity of CD122+CD8+ T cells according to in vitro co-culture and Ab-blocking assays. These suppressive mechanisms are distinct from those of Qa-1-restricted CD8+ Treg cells, although expression of the CD122 cytokine receptor is common to both regulatory cell populations [46]. In humans, CXCR3+CD45RA−CD62L+ CD8+ T cells are the counterpart of murine CD8+CD122+ Treg, and also exert their regulatory activity via IL-10 production and inhibit IFNγ production by target T cells [70].
In addition to naturally occurring CD122+CD8+ Treg, recent studies have shown that chronic antigen exposure induces accumulation of anergic/memory-like CD8+ T cells in secondary lymphoid organs. NOD mice carrying a high-affinity autoreactive TCR transgene develop accelerated autoimmune diabetes, while NOD mice carrying a low-affinity transgene of the same antigenic specificity are relatively resistant to diabetes development [71,72]. Resistance is mediated by a population of low-affinity, memory-like autoregulatory CD8+ T cells; CD44hiCD122+CD8+ T cells that proliferate in response to IL-2 and IL-15 [72,73]. Antigen-specific activation of this subset of low avidity autoreactive CD8+ T cells leads to APC-dependent down-regulation of other pathogenic T cell responses through a mechanism involving perforin-dependent lysis of APC, IFNγ secretion, and IDO-dependent suppression of antigen presentation [72]. In contrast to the CD122+CD8+ natural Treg described above, but similar to Qa-1-restricted CD8+ Treg, suppressive activity does not depend on IL-10 secretion. An interesting feature of this CD8+ Treg subset is its dependency on APC for suppressive activity. Whether CD122+ CD8+ Treg represent distinct regulatory lineages or whether there is a level of redundancy among these CD8+ Treg is not yet established.
6. CD4+ and CD8+ regulatory T cells: division of labor and/or collaboration?
The contribution of FoxP3+ CD4+ Treg to immune homeostasis has been well studied. Defects in FoxP3 expression underlie lymphoproliferative and multiorgan autoimmune disorders of scurfy mutant mice as well as patients with immunodysregulation, polyendocrinopathy and enteropathy, X-linked (IPEX) syndrome [74]. CD4+ Treg isolated from either the thymus or the periphery can suppress effector T (Teff) cell proliferation in vitro by cell contact-dependent mechanisms, and in vivo, where additional cytokine-dependent suppression can be achieved by IL-10, transforming growth factor-β (TGF-β) and IL-35 [75]. Although most studies regard FoxP3+ Treg as a homogeneous population, CD4+ Treg can adopt an effector phenotype after activation and display heterogeneous expression of chemokine receptors and effector cytokines such as IL-10 and TGF-β [76–78]. Moreover, recent studies have demonstrated that CD4+ Treg might require a target cell-specific genetic program (expression of T-bet or IRF-4) to efficiently suppress TH1 or TH2 dominant inflammatory responses, respectively. These observations suggest that peripheral CD4+ Treg develop in response to distinct inflammatory cues [79–81]. There also may be a temporal or spatial division of labor between CD4+ Treg and CD8+ Treg (Table 1). Evidence supports the idea that CD4+ Treg are involved during the initial priming phase of innate and adaptive immune responses and suppress the extent of inflammatory response that may cause collateral damage of tissues. In contrast, immune suppression mediated by Qa-1-restricted CD8+ Treg depends on a previous immune reaction, since upregulation of Qa-1 on activated cells is a prerequisite for the efficient generation of CD8+ Treg. Since TFH express Qa-1 without deliberate immunization, inhibition of Ab-mediated immune responses, particularly suppression of the autoantibody response, may be the primary task of Qa-1-restricted CD8+ Treg in the steady state. In addition, diverse types of immune response initiated by different TH effector cells may also be regulated by subtypes of CD8+ Treg. Possibly, the repertoire of Qa-1-bound peptides expressed by TH subsets, itself determined by differential processing/presentation of relevant self-peptides and the cytokine milieu, may dictate expansion and phenotype of CD8+ Treg. Experimental evidence that CD8+ T cells generated after TCV with MBP-specific TH1 cells preferentially suppress TH1 but not TH2 cells, despite the two having identical TCR, supports this hypothesis [82]. Ultimately, to limit the extent of the immune response mediated by multiple cell types during inflammation, coordinate suppression by CD4+ and CD8+ Treg that target distinct cell types may be necessary for durable and complete regulation of immune responses.
Table 1.
Comparison of CD4+ and CD8+ regulatory T cells.
| CD4+ Treg | CD8+ Trega | |
|---|---|---|
| Selection in thymus | Thymic epithelial cells | Thymic hematopoietic cells |
| Cytokine dependence | IL-2 | IL-15 |
| MHC restriction | MHC class II | Qa-1 |
| Induction in the periphery | TGF-β, antigen | Qa-1-peptide |
| Identification markers | FoxP3, CD25, GITR, Nrp-1, Lag3, FolR4, CD103 | Ly49 |
| Effector cytokines | IL-10, TGF-β, Granzyme-B | perforin |
| Phenotype of deficient mice | Lethal multi-organ autoimmune disease | SLE-like disease |
Due to the heterogeneity of CD8+ Treg populations, only the Qa-1-restricted CD8+ Treg subset is compared to CD4+ Treg cells.
7. Open issues
7.1. Thymic development of Qa-1 restricted CD8+ Treg
The molecular requirements for the development of Qa-1-restricted CD8+ T cells in the thymus are poorly understood. Unlike MHC class Ia restricted CD8+ T cells, MHC class Ib restricted cells are, in general, selected on hematopoietic cells. Thymic selection of this CD8+ T cell lineage on hematopoietic cells appears to be associated with acquisition of a memory phenotype. Listeria specific H2-M3 restricted CD8+ T cells develop efficiently on hematopoietic cells [83]. NKT cells are routinely selected on hematopoietic cells in the thymus and exhibit a memory phenotype [84,85]. Deficiency of Tec kinase (Rlk−/−Itk−/− mice) prevents conventional CD8+ T cell development and leads to the generation of a large population of nonconventional innate-type CD8+ T cells whose thymic selection is also strongly dependent on cells of hematopoietic origin [86–88]. Studies with Tec kinase deficient mice also suggests that the strength of TCR signaling during development determines whether T cells mature into conventional versus innate lymphocyte lineages [88].
Clues that Qa-1-restricted CD8+ T cells follow the same principles of thymic development as other MHC class Ib-restricted T cells have come from studies of the 6C5 transgenic mouse [89]. 6C5 TCR transgenic mice recognize (pig) insulin peptide presented by Qa-1. Efficient selection of 6C5+CD8+ T cells can be mediated by interactions with Qa-1+ hematopoietic cells in the thymus. Although TAP expression is required for selection of 6C5 T cells, TAP is not required for presentation of insulin to these cells. Although Qa-1 preferentially binds to short (nonameric) peptides, the apparent requirement for the 30 amino-acid peptide for the response of 6C5 T cells is intriguing.
The basis for the differences in cellular requirements for selection of class Ib-restricted T cells is not yet determined. It may result from differences in the expression levels of selecting ligands (Qa-1–peptide) compared to MHC class Ia or their associated peptide ligands in different cell types in the thymus. Whether the observations obtained with 6C5 transgenic mice can be generalized to the developmental requirements for Qa-1-restricted CD8+ T cells awaits further studies of the cellular and molecular interactions needed for thymic development of Qa-1-restricted CD8+ Treg.
7.2. Identification of target cell-specific Qa-1 bound peptides
Although induction of CD8+ Treg requires expression of Qa-1 by activated cells, additional factors may play a role in the efficient recognition of target cells by Qa-1-restricted CD8+ Treg. For example, activated B cells are not efficiently targeted by CD8+ Treg, although they express surface Qa-1 at levels similar to activated TH cells [46]. A specialized processing and loading pathway for Qa-1-dependent presentation by activated CD4+ T cells may play a critical role in priming CD8+ Treg. Possibly, the availability of Qa-1 binding peptides may differ between these two cell types, resulting in different sets of Qa-1–peptide complexes on the cell’s surface. Analysis of peptides eluted from Qa-1 expressed by different cell types (CD4+ TH lineages, B cells and dendritic cells) may provide insight into target cell specific immune regulation by CD8+ Treg cells. Due to the generally low affinity of Qa-1 binding peptides, appropriate methodologies may be required for the elution of an unbiased repertoire of peptides from primary cell cultures in order to reduce false-positives. Immunoprecipitation of Qa-1–peptide complexes followed by gentle disruption prior to analysis by tandem mass spec (MS/MS) may be required for analysis of cell type-specific Qa-1 binding peptides. Techniques such as stable isotope labeling with amino acids in cell culture (SILAC) can be adopted to reduce signal-noise ratios. A number of label free methods for quantitative comparison are also currently being developed.
7.3. Targeting CD8+ Treg in disease
The dependence of CD8+ Treg on IL-15 facilitates expansion of these cells in vitro. CD8+ Treg expand at a remarkable rate in vitro in the presence of IL-15 without obvious changes in phenotype [47]. Further experiments are needed to determine the ability of these in vitro expanded cells to mediate Qa-1-restricted suppressive activity. KIR+CD8+ T cells in humans also display this sensitivity to IL-15. Identification of KIR subtype+ CD8+ T cells that display HLA-E-restricted suppressive activity will facilitate development of CD8+ T cell-based immunotherapy. In particular, expansion of CD8+ Treg without phenotypic and functional changes will open the possibility that autologous CD8+ Treg can be harvested, expanded and reinfused into patients with autoimmune disorders.
In addition, since CD8+ Treg-mediated suppression may hamper effective anti-tumor immune responses, blockade of Qa-1-mediated interaction between effector cells and CD8+ Treg may enhance the immune response against tumors. Development of blocking Abs (anti-Qa-1 and anti-HLA-E) that specifically interrupt the interaction between Qa-1 (HLA-E) and TCR will advance our understanding of the contribution of CD8+ Treg-mediated suppression of tumor immunity.
Acknowledgments
This work was supported in part by grants from the NIH (AI 037562), National Multiple Sclerosis Foundation, Lupus Research Institute, and a gift from the LeRoy Schecter Research Foundation to HC and NRSA Fellowship (DFCI/NCI T32 CA070083) to H-JK. The authors wish to thank L.B. Goodman for critical reading and A. Angel for editorial assistance.
Abbreviations
- CD8+ Treg
Qa-1 restricted regulatory T cells
- HLA-E
human leukocyte antigen-E
- Qdm
Qa-1 determinant modifier
- MBP
myelin basic protein
- EAE
experimental autoimmune encephalomyelitis
- MS
multiple sclerosis
- CSF
cerebrospinal fluid
- CMV
cytomegalovirus
- TCV
T cell vaccination
- T1D
type 1 diabetes mellitus
- TFH
follicular helper T cells
- NK
natural killer
- KIR
killer cell immunoglobulin-like receptors
- NOD
non-obese diabetic
- APC
antigen presenting cell
- IDO
Indoleamine 2,3-dioxygenase
- TAP
transporter associated with antigen processing
References
- 1.Eardley DD, Hugenberger J, McVay-Boudreau L, Shen FW, Gershon RK, Cantor H. Immunoregulatory circuits among T-cell sets. I. T-helper cells induce T-cell sets to exert feedback inhibition. J Exp Med. 1978;147:1106–15. doi: 10.1084/jem.147.4.1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cantor H. Reviving suppression? Nat Immunol. 2004;5:347–9. doi: 10.1038/ni0404-347. [DOI] [PubMed] [Google Scholar]
- 3.Wolf PR, Cook RG. The TLregion gene 37 encodes a Qa-1 antigen. J Exp Med. 1990;172:1795–804. doi: 10.1084/jem.172.6.1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aldrich CJ, Waltrip R, Hermel E, Attaya M, Lindahl KF, Monaco JJ, et al. T cell recognition of QA-1b antigens on cells lacking a functional Tap-2 transporter. J Immunol. 1992;149:3773–7. [PubMed] [Google Scholar]
- 5.Miller JD, Weber DA, Ibegbu C, Pohl J, Altman JD, Jensen PE. Analysis of HLA-E peptide-binding specificity and contact residues in bound peptide required for recognition by CD94/NKG2. J Immunol. 2003;171:1369–75. doi: 10.4049/jimmunol.171.3.1369. [DOI] [PubMed] [Google Scholar]
- 6.Kraft JR, Vance RE, Pohl J, Martin AM, Raulet DH, Jensen PE. Analysis of Qa-1b peptide binding specificity and the capacity of CD94/NKG2A to discriminate between Qa-1–peptide complexes. J Exp Med. 2000;192:613–23. doi: 10.1084/jem.192.5.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kambayashi T, Kraft-Leavy JR, Dauner JG, Sullivan BA, Laur O, Jensen PE. The nonclassical MHC class I molecule Qa-1 forms unstable peptide complexes. J Immunol. 2004;172:1661–9. doi: 10.4049/jimmunol.172.3.1661. [DOI] [PubMed] [Google Scholar]
- 8.Aldrich CJ, DeCloux A, Woods AS, Cotter RJ, Soloski MJ, Forman J. Identification of a Tap-dependent leader peptide recognized by alloreactive T cells specific for a class Ib antigen. Cell. 1994;79:649–58. doi: 10.1016/0092-8674(94)90550-9. [DOI] [PubMed] [Google Scholar]
- 9.Bai A, Broen J, Forman J. The pathway for processing leader-derived peptides that regulate the maturation and expression of Qa-1b. Immunity. 1998;9:413–21. doi: 10.1016/s1074-7613(00)80624-x. [DOI] [PubMed] [Google Scholar]
- 10.Lemberg MK, Bland FA, Weihofen A, Braud VM, Martoglio B. Intramembrane proteolysis of signal peptides: an essential step in the generation of HLA-E epitopes. J Immunol. 2001;167:6441–6. doi: 10.4049/jimmunol.167.11.6441. [DOI] [PubMed] [Google Scholar]
- 11.Davies A, Kalb S, Liang B, Aldrich CJ, Lemonnier FA, Jiang H, et al. A peptide from heat shock protein 60 is the dominant peptide bound to Qa-1 in the absence of the MHC class Ia leader sequence peptide Qdm. J Immunol. 2003;170:5027–33. doi: 10.4049/jimmunol.170.10.5027. [DOI] [PubMed] [Google Scholar]
- 12.Braud V, Jones EY, McMichael A. The human major histocompatibility complex class Ib molecule HLA-E binds signal sequence-derived peptides with primary anchor residues at positions 2 and 9. Eur J Immunol. 1997;27:1164–9. doi: 10.1002/eji.1830270517. [DOI] [PubMed] [Google Scholar]
- 13.Stevens J, Joly E, Trowsdale J, Butcher GW. Peptide binding characteristics of the non-classical class Ib MHC molecule HLA-E assessed by a recombinant random peptide approach. BMC Immunol. 2001;2:5. doi: 10.1186/1471-2172-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiang H, Ware R, Stall A, Flaherty L, Chess L, Pernis B. Murine CD8+ T cells that specifically delete autologous CD4+ T cells expressing Vβ8 TCR: role of the Qa-1 molecule. Immunity. 1995;2:185–94. doi: 10.1016/s1074-7613(95)80079-4. [DOI] [PubMed] [Google Scholar]
- 15.Jiang H, Kashleva H, Xu LX, Forman J, Flaherty L, Pernis B, et al. T cell vaccination induces TCR Vβ specific, Qa-1 restricted regulatory CD8+ T cells. Proc Natl Acad Sci USA. 1998;95:4533–7. doi: 10.1073/pnas.95.8.4533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tang X, Maricic I, Purohit N, Bakamjian B, Reed-Loisel LM, Beeston T, et al. Regulation of immunity by a novel population of Qa-1-restricted CD8alphaalpha+TCRalphabeta+ T cells. J Immunol. 2006;177:7645–55. doi: 10.4049/jimmunol.177.11.7645. [DOI] [PubMed] [Google Scholar]
- 17.Lo WF, Woods AS, DeCloux A, Cotter RJ, Metcalf ES, Soloski MJ. Molecular mimicry mediated by MHC class Ib molecules after infection with gram-negative pathogens. Nat Med. 2000;6:215–8. doi: 10.1038/72329. [DOI] [PubMed] [Google Scholar]
- 18.Chen W, Zhang L, Liang B, Saenger Y, Li J, Chess L, et al. Perceiving the avidity of T cell activation can be translated into peripheral T cell regulation. Proc Natl Acad Sci USA. 2007;104:20472–7. doi: 10.1073/pnas.0709878104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jiang H, Chess L. How the immune system achieves self-nonself discrimination during adaptive immunity. Adv Immunol. 2009;102:95–133. doi: 10.1016/S0065-2776(09)01202-4. [DOI] [PubMed] [Google Scholar]
- 20.Connolly DJ, Cotterill LA, Hederer RA, Thorpe CJ, Travers PJ, McVey JH, et al. A cDNA clone encoding the mouse Qa-1a histocompatibility antigen and proposed structure of the putative peptide binding site. J Immunol. 1993;151:6089–98. [PubMed] [Google Scholar]
- 21.Oliveira CC, van Veelen PA, Querido B, de Ru A, Sluijter M, Laban S, et al. The nonpolymorphic MHC Qa-1b mediates CD8+ T cell surveillance of antigen-processing defects. J Exp Med. 2010;207:207–21. doi: 10.1084/jem.20091429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jensen PE, Sullivan BA, Reed-Loisel LM, Weber DA. Qa-1, a nonclassical class I histocompatibility molecule with roles in innate and adaptive immunity. Immunol Res. 2004;29:81–92. doi: 10.1385/IR:29:1-3:081. [DOI] [PubMed] [Google Scholar]
- 23.Rodgers JR, Cook RG. MHC class Ib molecules bridge innate and acquired immunity. Nat Rev Immunol. 2005;5:459–71. doi: 10.1038/nri1635. [DOI] [PubMed] [Google Scholar]
- 24.Grimsley C, Kawasaki A, Gassner C, Sageshima N, Nose Y, Hatake K, et al. Definitive high resolution typing of HLA-E allelic polymorphisms: Identifying potential errors in existing allele data. Tissue Antigens. 2002;60:206–12. doi: 10.1034/j.1399-0039.2002.600302.x. [DOI] [PubMed] [Google Scholar]
- 25.Lee N, Goodlett DR, Ishitani A, Marquardt H, Geraghty DE. HLA-E surface expression depends on binding of TAP-dependent peptides derived from certain HLA class I signal sequences. J Immunol. 1998;160:4951–60. [PubMed] [Google Scholar]
- 26.O’Callaghan CA, Tormo J, Willcox BE, Braud VM, Jakobsen BK, Stuart DI, et al. Structural features impose tight peptide binding specificity in the nonclassical MHC molecule HLA-E. Mol Cell. 1998;1:531–41. doi: 10.1016/s1097-2765(00)80053-2. [DOI] [PubMed] [Google Scholar]
- 27.Pietra G, Romagnani C, Mazzarino P, Falco M, Millo E, Moretta A, et al. HLA-E-restricted recognition of cytomegalovirus-derived peptides by human CD8+ cytolytic T lymphocytes. Proc Natl Acad Sci USA. 2003;100:10896–901. doi: 10.1073/pnas.1834449100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ulbrecht M, Modrow S, Srivastava R, Peterson PA, Weiss EH. Interaction of HLA-E with peptides and the peptide transporter in vitro: implications for its function in antigen presentation. J Immunol. 1998;160:4375–85. [PubMed] [Google Scholar]
- 29.Heinzel AS, Grotzke JE, Lines RA, Lewinsohn DA, McNabb AL, Streblow DN, et al. HLA-E-dependent presentation of Mtb-derived antigen to human CD8+ T cells. J Exp Med. 2002;196:1473–81. doi: 10.1084/jem.20020609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wooden SL, Kalb SR, Cotter RJ, Soloski MJ. Cutting edge: HLA-E binds a peptide derived from the ATP-binding cassette transporter multidrug resistance-associated protein 7 and inhibits NK cell-mediated lysis. J Immunol. 2005;175:1383–7. doi: 10.4049/jimmunol.175.3.1383. [DOI] [PubMed] [Google Scholar]
- 31.Li J, Goldstein I, Glickman-Nir E, Jiang H, Chess L. Induction of TCR Vbeta-specific CD8+ CTLs by TCR Vbeta-derived peptides bound to HLA-E. J Immunol. 2001;167:3800–8. doi: 10.4049/jimmunol.167.7.3800. [DOI] [PubMed] [Google Scholar]
- 32.Lu L, Ikizawa K, Hu D, Werneck MBF, Wucherpfennig KW, Cantor H. Regulation of activated CD4+ T cells by NK cells via the Qa-1-NKG2A pathway. Immunity. 2007;26:593–604. doi: 10.1016/j.immuni.2007.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cantor H, Boyse EA. Functional subclasses of T-lymphocytes bearing different Ly antigens. I. The generation of functionally distinct T-cell subclasses is a differentiative process independent of antigen. J Exp Med. 1975;141:1376–89. doi: 10.1084/jem.141.6.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cantor H, Shen FW, Boyse EA. Separation of helper T cells from suppressor T cells expressing different Ly components. II. Activation by antigen: after immunization, antigen-specific suppressor and helper activities are mediated by distinct T-cell subclasses. J Exp Med. 1976;143:1391–440. doi: 10.1084/jem.143.6.1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Noble A, Zhao ZS, Cantor H. Suppression of immune responses by CD8 cells: II. Qa-1 on activated B-cells stimulates CD8 cell suppression of T helper 2 responses. J Immunol. 1998;160:566–71. [PubMed] [Google Scholar]
- 36.Koh DR, Fung-Leung WP, Ho A, Gray D, Acha-Orbea H, Mak TW. Less mortality but more relapses in experimental allergic encephalomyelitis in CD8−/− mice. Science. 1992;256:1210–3. doi: 10.1126/science.256.5060.1210. [DOI] [PubMed] [Google Scholar]
- 37.Gaur A, Haspel R, Mayer JP, Fathman CG. Requirement for CD8+ cells in T cell receptor peptide-induced clonal unresponsiveness. Science. 1993;259:91–4. doi: 10.1126/science.8418501. [DOI] [PubMed] [Google Scholar]
- 38.Jiang H, Zhang SL, Pernis B. Role of CD8+ T cells in murine experimental allergic encephalomyelitis. Science. 1992;256:1213–5. doi: 10.1126/science.256.5060.1213. [DOI] [PubMed] [Google Scholar]
- 39.Jiang H, Curran S, Ruiz-Vazquez E, Liang B, Winchester R, Chess L. Regulatory CD8+ T cells fine-tune the myelin basic protein-reactive T cell receptor V beta repertoire during experimental autoimmune encephalomyelitis. Proc Natl Acad Sci USA. 2003;100:8378–83. doi: 10.1073/pnas.1432871100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Panoutsakopoulou V, Huster KM, McCarty N, Feinberg E, Wang R, Wucherpfennig KW, et al. Suppression of autoimmune disease after vaccination with autoreactive T cells that express Qa-1 peptide complexes. J Clin Invest. 2004;113:1218–24. doi: 10.1172/JCI20772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hu D, Ikizawa K, Lu L, Sanchirico ME, Shinohara ML, Cantor H. Analysis of regulatory CD8 T cells in Qa-1-deficient mice. Nat Immunol. 2004;5:516–23. doi: 10.1038/ni1063. [DOI] [PubMed] [Google Scholar]
- 42.Jiang H, Canfield SM, Gallagher MP, Jiang HH, Jiang Y, Zheng Z, et al. HLA-E-restricted regulatory CD8(+) T cells are involved in development and control of human autoimmune type 1 diabetes. J Clin Invest. 2010;120:3641–50. doi: 10.1172/JCI43522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Correale J, Villa A. Isolation and characterization of CD8+ regulatory T cells in multiple sclerosis. J Neuroimmunol. 2008;195:121–34. doi: 10.1016/j.jneuroim.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 44.Mazzarino P, Pietra G, Vacca P, Falco M, Colau D, Coulie P, et al. Identification of effector-memory CMV-specific T lymphocytes that kill CMV-infected target cells in an HLA-E-restricted fashion. Eur J Immunol. 2005;35:3240–7. doi: 10.1002/eji.200535343. [DOI] [PubMed] [Google Scholar]
- 45.Lu L, Kim HJ, Werneck MB, Cantor H. Regulation of CD8+ regulatory T cells: interruption of the NKG2A-Qa-1 interaction allows robust suppressive activity and resolution of autoimmune disease. Proc Natl Acad Sci USA. 2008;105:19420–5. doi: 10.1073/pnas.0810383105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim HJ, Verbinnen B, Tang X, Lu L, Cantor H. Inhibition of follicular T helper cells by CD8+ Treg is essential for self tolerance. Nature. 2010;467:328–32. doi: 10.1038/nature09370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim HJ, Wang X, Radfar S, Sproule TJ, Roopenian DC, Cantor H. CD8+ T regulatory cells express the Ly49 class I MHC receptor and are defective in autoimmune-prone B6-Yaa mice. Proc Natl Acad Sci USA. 2011;108:2010–5. doi: 10.1073/pnas.1018974108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Raulet DH, Vance RE, McMahon CW. Regulation of the natural killer cell receptor repertoire. Annu Rev Immunol. 2001;19:291–330. doi: 10.1146/annurev.immunol.19.1.291. [DOI] [PubMed] [Google Scholar]
- 49.Anfossi N, Robbins SH, Ugolini S, Georgel P, Hoebe K, Bouneaud C, et al. Expansion and function of CD8+ T cells expressing Ly49 inhibitory receptors specific for MHC class I molecules. J Immunol. 2004;173:3773–82. doi: 10.4049/jimmunol.173.6.3773. [DOI] [PubMed] [Google Scholar]
- 50.Coles MC, McMahon CW, Takizawa H, Raulet DH. Memory CD8 T lymphocytes express inhibitory MHC-specific Ly49 receptors. Eur J Immunol. 2000;30:236–44. doi: 10.1002/1521-4141(200001)30:1<236::AID-IMMU236>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 51.Ugolini S, Arpin C, Anfossi N, Walzer T, Cambiaggi A, Forster R, et al. Involvement of inhibitory NKRs in the survival of a subset of memory-phenotype CD8+ T cells. Nat Immunol. 2001;2:430–5. doi: 10.1038/87740. [DOI] [PubMed] [Google Scholar]
- 52.Young NT, Uhrberg M, Phillips JH, Lanier LL, Parham P. Differential expression of leukocyte receptor complex-encoded Ig-like receptors correlates with the transition from effector to memory CTL. J Immunol. 2001;166:3933–41. doi: 10.4049/jimmunol.166.6.3933. [DOI] [PubMed] [Google Scholar]
- 53.Roger J, Chalifour A, Lemieux S, Duplay P. Cutting edge: Ly49A inhibits TCR/CD3-induced apoptosis and IL-2 secretion. J Immunol. 2001;167:6–10. doi: 10.4049/jimmunol.167.1.6. [DOI] [PubMed] [Google Scholar]
- 54.Chwae YJ, Chang MJ, Park SM, Yoon H, Park HJ, Kim SJ, et al. Molecular mechanism of the activation-induced cell death inhibition mediated by a p70 inhibitory killer cell Ig-like receptor in Jurkat T cells. J Immunol. 2002;169:3726–35. doi: 10.4049/jimmunol.169.7.3726. [DOI] [PubMed] [Google Scholar]
- 55.Mingari MC, Ponte M, Cantoni C, Vitale C, Schiavetti F, Bertone S, et al. HLA-class I-specific inhibitory receptors in human cytolytic T lymphocytes: molecular characterization, distribution in lymphoid tissues and co-expression by individual T cells. Int Immunol. 1997;9:485–91. doi: 10.1093/intimm/9.4.485. [DOI] [PubMed] [Google Scholar]
- 56.Anfossi N, Pascal V, Vivier E, Ugolini S. Biology of T memory type 1 cells. Immunol Rev. 2001;181:269–78. doi: 10.1034/j.1600-065x.2001.1810123.x. [DOI] [PubMed] [Google Scholar]
- 57.Moretta L, Romagnani C, Pietra G, Moretta A, Mingari MC. NK-CTLs, a novel HLA-E-restricted T-cell subset. Trends Immunol. 2003;24:136–43. doi: 10.1016/s1471-4906(03)00031-0. [DOI] [PubMed] [Google Scholar]
- 58.Pietra G, Romagnani C, Manzini C, Moretta L, Mingari MC. The emerging role of HLA-E-restricted CD8+ T lymphocytes in the adaptive immune response to pathogens and tumors. J Biomed Biotechnol. 2010:907092. doi: 10.1155/2010/907092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Correia MP, Costa AV, Uhrberg M, Cardoso EM, Arosa FA. IL-15 induces CD8+ T cells to acquire functional NK receptors capable of modulating cytotoxicity and cytokine secretion. Immunobiology. 2011;216:604–12. doi: 10.1016/j.imbio.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 60.Pietra G, Romagnani C, Falco M, Vitale M, Castriconi R, Pende D, et al. The analysis of the natural killer-like activity of human cytolytic T lymphocytes revealed HLA-E as a novel target for TCR alpha/beta-mediated recognition. Eur J Immunol. 2001;31:3687–93. doi: 10.1002/1521-4141(200112)31:12<3687::aid-immu3687>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 61.Romagnani C, Pietra G, Falco M, Millo E, Mazzarino P, Biassoni R, et al. Identification of HLA-E-specific alloreactive T lymphocytes: a cell subset that undergoes preferential expansion in mixed lymphocyte culture and displays a broad cytolytic activity against allogeneic cells. Proc Natl Acad Sci USA. 2002;99:11328–33. doi: 10.1073/pnas.172369799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Suzuki H, Kundig TM, Furlonger C, Wakeham A, Timms E, Matsuyama T, et al. Deregulated T cell activation and autoimmunity in mice lacking interleukin-2 receptor beta. Science. 1995;268:1472–6. doi: 10.1126/science.7770771. [DOI] [PubMed] [Google Scholar]
- 63.Burchill MA, Yang J, Vogtenhuber C, Blazar BR, Farrar MA. IL-2 receptor beta-dependent STAT5 activation is required for the development of Foxp3+ regulatory T cells. J Immunol. 2007;178:280–90. doi: 10.4049/jimmunol.178.1.280. [DOI] [PubMed] [Google Scholar]
- 64.Soper DM, Kasprowicz DJ, Ziegler SF. IL-2Rbeta links IL-2R signaling with Foxp3 expression. Eur J Immunol. 2007;37:1817–26. doi: 10.1002/eji.200737101. [DOI] [PubMed] [Google Scholar]
- 65.Rifa’i M, Kawamoto Y, Nakashima I, Suzuki H. Essential roles of CD8+CD122+ regulatory T cells in the maintenance of T cell homeostasis. J Exp Med. 2004;200:1123–34. doi: 10.1084/jem.20040395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang LX, Li Y, Yang G, Pang PY, Haley D, Walker EB, et al. CD122+CD8+ Treg suppress vaccine-induced antitumor immune responses in lymphodepleted mice. Eur J Immunol. 2010;40:1375–85. doi: 10.1002/eji.200839210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Endharti AT, Rifa’i M, Shi Z, Fukuoka Y, Nakahara Y, Kawamoto Y, et al. Cutting edge: CD8+CD122+ regulatory T cells produce IL-10 to suppress IFN-gamma production and proliferation of CD8+ T cells. J Immunol. 2005;175:7093–7. doi: 10.4049/jimmunol.175.11.7093. [DOI] [PubMed] [Google Scholar]
- 68.Saitoh O, Abiru N, Nakahara M, Nagayama Y. CD8+CD122+ T cells, a newly identified regulatory T subset, negatively regulate Graves’ hyperthyroidism in a murine model. Endocrin. 2007;148:6040–6. doi: 10.1210/en.2007-0300. [DOI] [PubMed] [Google Scholar]
- 69.Rifa’i M, Shi Z, Zhang SY, Lee YH, Shiku H, Isobe K, et al. CD8+CD122+ regulatory T cells recognize activated T cells via conventional MHC class I-alphabetaTCR interaction and become IL-10-producing active regulatory cells. Int Immunol. 2008;20:937–47. doi: 10.1093/intimm/dxn052. [DOI] [PubMed] [Google Scholar]
- 70.Shi Z, Okuno Y, Rifa’i M, Endharti AT, Akane K, Isobe K, et al. Human CD8+CXCR3+ T cells have the same function as murine CD8+CD122+ Treg. Eur J Immunol. 2009;39:2106–19. doi: 10.1002/eji.200939314. [DOI] [PubMed] [Google Scholar]
- 71.Han B, Serra P, Yamanouchi J, Amrani A, Elliott JF, Dickie P, et al. Developmental control of CD8 T cell-avidity maturation in autoimmune diabetes. J Clin Invest. 2005;115:1879–87. doi: 10.1172/JCI24219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tsai S, Shameli A, Yamanouchi J, Clemente-Casares X, Wang J, Serra P, et al. Reversal of autoimmunity by boosting memory-like autoregulatory T cells. Immunity. 2010;32:568–80. doi: 10.1016/j.immuni.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 73.Khadra A, Tsai S, Santamaria P, Edelstein-Keshet L. On how monospecific memory-like autoregulatory CD8+ T cells can blunt diabetogenic autoimmunity: a computational approach. J Immunol. 2010;185:5962–72. doi: 10.4049/jimmunol.1001306. [DOI] [PubMed] [Google Scholar]
- 74.Ziegler SF. FOXP3: of mice and men. Annu Rev Immunol. 2006;24:209–26. doi: 10.1146/annurev.immunol.24.021605.090547. [DOI] [PubMed] [Google Scholar]
- 75.Izcue A, Coombes JL, Powrie F. Regulatory lymphocytes and intestinal inflammation. Annu Rev Immunol. 2009;27:313–38. doi: 10.1146/annurev.immunol.021908.132657. [DOI] [PubMed] [Google Scholar]
- 76.Huehn J, Siegmund K, Lehmann JC, Siewert C, Haubold U, Feuerer M, et al. Developmental stage, phenotype, and migration distinguish naive- and effector/memory-like CD4+ regulatory T cells. J Exp Med. 2004;199:303–13. doi: 10.1084/jem.20031562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Maynard CL, Harrington LE, Janowski KM, Oliver JR, Zindl CL, Rudensky AY, et al. Regulatory T cells expressing interleukin 10 develop from Foxp3+ and Foxp3-precursor cells in the absence of interleukin 10. Nat Immunol. 2007;8:931–41. doi: 10.1038/ni1504. [DOI] [PubMed] [Google Scholar]
- 78.Sather BD, Treuting P, Perdue N, Miazgowicz M, Fontenot JD, Rudensky AY, et al. Altering the distribution of Foxp3(+) regulatory T cells results in tissue-specific inflammatory disease. J Exp Med. 2007;204:1335–47. doi: 10.1084/jem.20070081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Barnes MJ, Powrie F. Hybrid Treg cells: steel frames and plastic exteriors. Nat Immunol. 2009;10:563–4. doi: 10.1038/ni0609-563. [DOI] [PubMed] [Google Scholar]
- 80.Koch MA, Tucker-Heard G, Perdue NR, Killebrew JR, Urdahl KB, Campbell DJ. The transcription factor T-bet controls regulatory T cell homeostasis and function during type 1 inflammation. Nat Immunol. 2009;10:595–602. doi: 10.1038/ni.1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zheng Y, Josefowicz S, Chaudhry A, Peng XP, Forbush K, Rudensky AY. Role of conserved non-coding DNA elements in the Foxp3 gene in regulatory T-cell fate. Nature. 2010;463:808–12. doi: 10.1038/nature08750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jiang H, Braunstein NS, Yu B, Winchester R, Chess L. CD8+ T cells control the TH phenotype of MBP-reactive CD4+ T cells in EAE mice. Proc Natl Acad Sci USA. 2001;98:6301–6. doi: 10.1073/pnas.101123098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Urdahl KB, Sun JC, Bevan MJ. Positive selection of MHC class Ib-restricted CD8(+) T cells on hematopoietic cells. Nat Immunol. 2002;3:772–9. doi: 10.1038/ni814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bendelac A, Killeen N, Littman DR, Schwartz RH. A subset of CD4+ thymocytes selected by MHC class I molecules. Science. 1994;263:1774–8. doi: 10.1126/science.7907820. [DOI] [PubMed] [Google Scholar]
- 85.Bendelac A. Positive selection of mouse NK1+ T cells by CD1-expressing cortical thymocytes. J Exp Med. 1995;182:2091–6. doi: 10.1084/jem.182.6.2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Broussard C, Fleischacker C, Horai R, Chetana M, Venegas AM, Sharp LL, et al. Altered development of CD8+ T cell lineages in mice deficient for the Tec kinases Itk and Rlk. Immunity. 2006;25:93–104. doi: 10.1016/j.immuni.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 87.Atherly LO, Lucas JA, Felices M, Yin CC, Reiner SL, Berg LJ. The Tec family tyrosine kinases Itk and Rlk regulate the development of conventional CD8+ T cells. Immunity. 2006;25:79–91. doi: 10.1016/j.immuni.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 88.Prince AL, Yin CC, Enos ME, Felices M, Berg LJ. The Tec kinases Itk and Rlk regulate conventional versus innate T-cell development. Immunol Rev. 2009;228:115–31. doi: 10.1111/j.1600-065X.2008.00746.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sullivan BA, Kraj P, Weber DA, Ignatowicz L, Jensen PE. Positive selection of a Qa-1-restricted T cell receptor with specificity for insulin. Immunity. 2002;17:95–105. doi: 10.1016/s1074-7613(02)00343-6. [DOI] [PubMed] [Google Scholar]


