Abstract
Background The SIMS‐Trial (ISRCTN81072971) proved the effectiveness, in terms of patient’s knowledge and care satisfaction, of an add‐on information aid (personal interview with a physician using a navigable CD and take‐home booklet) in 120 newly diagnosed patients with multiple sclerosis (MS) from five Italian centres.
Objective To scrutinize the experience of SIMS‐Trial participants in order to gain better understanding of the effectiveness of the information aid and its components.
Design We performed (i) nine individual semi‐structured interviews with a purposeful sample of SIMS‐Trial patients who received the information aid, (ii) focus group meeting (FGM) with the physicians who conducted the personal interview, and (iii) FGM with patients’ caring neurologists.
Results Patients’ experience with the information aid was positive as it enhanced their understanding of their disease, being viewed as a guided tour of their medical condition. The physicians who conducted the personal interviews were also positive in their overall evaluation but noted an initial difficulty in using the CD. The caring neurologists had limited direct experience of the aid, and their views were confined to utility of the information aid in general. All participants considered the combination of personal interview, CD navigation and take‐home booklet essential, but urged a more flexible scheduling of the personal interview. It also emerged that some content required revision and that the aid was unsuitable for patients with primary progressive MS.
Conclusions The results of the study further support the value of the aid and also provide important indications for improving it and refining indications for use.
Keywords: complex intervention, diagnosis communication, multiple sclerosis, qualitative study, shared decision making
Introduction
Multiple sclerosis (MS) is a chronic dysimmune neurodegenerative disease of the central nervous system that affects about 2.5 million people worldwide. 1 MS commonly manifests in early adulthood, and it is the leading disabling neurologic disorder of young and middle‐aged adults after trauma. Current diagnostic criteria for MS allow disease diagnosis earlier than in the past. 2 Since the affirmation of disease‐modifying treatments for early MS, diagnosis and treatment decision making have moved much closer together and often coincide. 3 However, no definite improvement in communication as a consequence of these changes has been found, and recent studies reveal communication and information deficits in the context of care of people with MS. 4 , 5 , 6 , 7
Engaging patients in clinical decision making has become an ethical principle underpinning much contemporary clinical practice. 8 , 9 , 10 , 11 Patient information aids are increasingly regarded as important components of clinical practice: They improve adaptive coping, sense of control and satisfaction with care and enable shared decision making with physicians. 8 , 9 , 10 , 12 , 13 However, published experience on information aids in MS is limited. 14
This article describes part of the second phase of a project (Fig. 1), carried out according to recognized criteria, 15 , 16 to develop and evaluate an information aid for newly diagnosed patients with MS. The first phase was the development of the information aid, which aimed to provide unbiased, high‐quality information about MS and was intended to supplement, rather than replace, patient–practitioner interaction. 7 The aid consisted of an add‐on personal interview conducted by a trained physician, during which information about MS was presented with the aid of a specially developed CD. At the end of the personal interview, the patient was given a specially developed take‐home information booklet.
Figure 1.
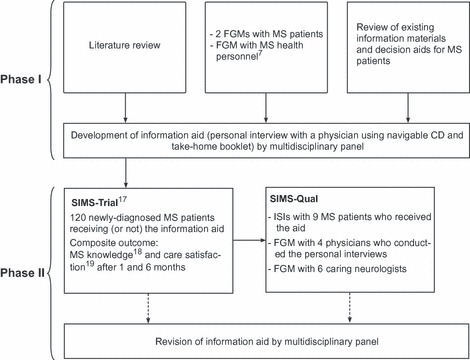
Flowchart of our phased approach 15 , 16 to developing and evaluating the information aid. FGM, focus group meeting; ISI, individual semi‐structured interview.
In the second phase of the project, we assessed the usefulness of the aid using mixed methodologies. In the SIMS‐Trial (ISRCTN81072971), we compared the aid with usual practice in 120 newly diagnosed patients with MS from five Italian centres (three high‐volume MS centres attached to university hospitals, one medium‐volume MS centre in a research hospital and one medium‐volume MS centre part of a university hospital). 17 The primary composite endpoint, assessed 1 and 6 months after diagnosis disclosure, was score in the highest tertile of MS knowledge 18 and satisfaction with care. 19 Other endpoints were safety; treatment adherence; extra contacts/consultations; switching of care centre; and changes in scores in the Hospital Anxiety and Depression Scale 20 , 21 and Control Preference Scale. 22 , 23 The information aid was safe and significantly associated with attainment of the primary outcome at 1 and 6 months.
The second phase continued with SIMS‐Qual, here described, which elicited the experiences and views, about the intervention, of patients and physicians who participated in the SIMS‐Trial. By means of this qualitative approach, we aimed to enhance understanding of the information aid and its components, revealing its strengths and weaknesses and refining it before use in every‐day practice (third phase).
Methods
SIMS‐Qual involved (i) individual semi‐structured interviews (ISIs) with a purposeful sample of people with MS who received the information aid in the SIMS‐Trial, and (ii) focus group meetings (FGMs): one with the physicians who conducted the SIMS‐Trial personal interviews (interviewing physicians) and the other with the neurologists caring for patients with MS (caring neurologists) (Fig. 1). The study protocol was approved by the Institutional Review Board of each participating centre.
ISIs
Selection of participants
We selected a purposeful pool of candidate patients with the following characteristics: either positive (high knowledge and care satisfaction scores at 1 and 6 months) or negative (low scores) outcomes from the SIMS‐Trial intervention group. We recruited patients from the three areas of Italy represented in the trial, seeking a sample with varied general and clinical characteristics.
To define positive and negative outcome groups, we obtained an overall score by averaging knowledge and satisfaction scale scores at the 1‐ and 6‐month follow‐ups (range of possible scores, 0–42.5). From the range of intervention group scores (19.5–41.7), we considered positive outcome patients those with an overall score ≥ 30, and negative outcome patients those with an overall score <30. Eligible patients were informed (orally and in writing) of the aims and requirements of the study, and those who gave written consent were scheduled for an ISI.
ISI setting and content
ISIs took place at the centre where the patient was followed; they were face‐to‐face with a single psychologist (MF) experienced in MS who had not participated in the SIMS‐Trial. The psychologist explained the purposes of the interview emphasizing that (i) the patient’s own experience with the information pack was essential to refine/improve the intervention, and (ii) there were no correct or incorrect answers.
Based on our original hypotheses, seven investigative categories were identified a priori (Table 1), and an interview template (Table S1) was produced from these. The interviews were audio‐recorded and transcribed verbatim into documents containing no personal identifiers. Interviews were held until no new themes emerged (data saturation); 24 the protocol specified a minimum of six interviews.
Table 1.
Categories for ISIs and FGMs
| Categories | ISIs with patients | FGM with interviewing physicians | FGM with caring neurologists |
|---|---|---|---|
| Experience with personal interview and relation with/suitability of interviewing physician | X | X | |
| Effect of information aid on disease knowledge/treatment choices | X | X | |
| Effect of aid on relation with the caring neurologist/team | X | X | |
| Evaluation of each aid component (strength/criticism/preference) | X | X | X |
| Effect of aid on attitude to the disease/disease coping/relation with relatives and friends | X | X | |
| Effect of aid on information needs | X | X | |
| Suitability of aid (and its components)/recommendations for newly diagnosed patients with multiple sclerosis | X | X | X |
FGM, focus group meeting; ISIs, individual semi‐structured interviews.
FGMs
Two FGMs were held, one with the interviewing physicians and the other with the caring neurologists. In the SIMS‐Trial, there was one interviewing physician from each centre; those who gave at least three personal interviews were invited to the interviewing physician FGM. One to two caring neurologists from each centre were invited to the caring neurologist FGM.
Both FGMs were presided over by a moderator (NA) and comoderator (AS). The moderator was a hired professional experienced in group dynamics, with no involvement in MS diagnosis or care. He engaged all participants in the discussion, promoted exchange, ensured that all pre‐specified topics (Tables S2 and S3) were adequately covered and allowed sufficient exploration of any pertinent issues arising. The comoderator was a neurologist experienced in MS.
Data analysis
The data were assessed by the methods of framework analysis 24 , 25 , 26 in the successive stages shown in Table 2. 27 The analytical categories were defined a priori (Table 1) and sought inductively from the data. To enhance validity, pairs of researchers analysed the ISIs (CB and EB) and FGMs (NA and AS).
Table 2.
Stages in the analysis of ISIs and FGMs by two researchers
| Stage | Working method | ISIs | FGMs |
|---|---|---|---|
| Identification of and commenting on significant propositions, without considering relation to other parts of the interview/meeting | Independent | X | X |
| Comments expanded and contextualized within interview/meeting | Independent | X | X |
| Relations established between comments by reordering and regrouping by subject matter | Independent | X | X |
| Themes most relevant to study objectives extracted and ordered hierarchically into categories, moving from general to specific; redundancies removed | Independent | X | X |
| Transcript analyses compared with each other to identify common and contrasting themes | Independent | X | – |
| Analyses compared, and consensus arrived at | Joint | X | X |
| Consensus report submitted to participants for review (respondent validation) | – | X |
FGM, focus group meeting; ISIs, individual semi‐structured interviews.
Results
ISIs
Data saturation was achieved after nine ISIs had been analysed. Five patients had positive outcomes and four had negative outcomes. All had relapsing MS and varied in terms of age, education, preference for participation in medical decisions (evaluated with the Control Preference Scale 22 , 23 ) and main clinical characteristics (Table 3). The ISIs lasted 22–52 min and were conducted in northern (n = 3), central (n = 4) and southern Italy (n = 2) between October 2009 and March 2010; the time from delivery of the information aid to ISIs ranged from 8 to 20 months.
Table 3.
Characteristics of the nine patients with multiple sclerosis who participated in the ISIs
| Characteristics | |
|---|---|
| Median age in years (range) | 29.6 (22–47) |
| Women (%) | 6 (66.7) |
| Education (%) | |
| Up to high school | 7 (77.8) |
| College diploma or degree | 2 (22.2) |
| Median years from 1st symptoms to diagnosis (range) | 2.3 (1–32) |
| Median days from start of diagnostic workup to diagnosis communication (range) | 35 (4–197) |
| Median EDSS score (range) | 2.0 (0.0–3.0) |
| Median HADS Anxiety score (range) | 4 (0–13) |
| Median HADS Depression score (range) | 2 (0–8) |
| Role preference (CPS score) (%) | |
| Passive | 4 (44.4) |
| Collaborative | 4 (44.4) |
| Active | 1 (11.1) |
| Median overall score (range)* | |
| Positive outcomes group (n = 5) | 32.7 (31.0–40.7) |
| Negative outcomes group (n = 4) | 26.0 (25.0–28.7) |
| Median months from trial completion to ISI* | 11.4 (5.5–14.1) |
CPS, Control Preference Scale; EDSS, Expanded Disability Status Scale; HADS, Hospital Anxiety and Depression Scale; ISIs, individual semi‐structured interviews.
*Findings obtained when the ISIs were conducted; all other data are from SIMS‐Trial baseline visit.
Overall patients’ experience was first synthesized. Subsequently, three major aspects of that experience were examined in detail: the personal interview, the CD and the booklet. Caveats emerging from overall experience and individual aspects thereof were also noted. Subsequently, effects on patients’ relations with family, acquaintances and the caring neurologist; the need for information; and attitudes to the disease (and its treatment) were derived. Patients’ proposals for use of the aid in routine clinical practice were recorded.
Overall experience
All patients emphasized that the information pack was useful because it enhanced their understanding of their disease. In general, it was viewed as a guided tour of the patient’s medical condition.
A very positive experience, because it guides you… helps you understand better; provides reassurance.
Although no negative experiences were reported, some patients emphasized the importance of tailoring the information to the needs of each individual.
In my view it was OK, but perhaps it should be tailored to the individual. If it remains general it suits everyone but if you want to enter into detail you must consider the individual.
The personal interview
The interview was experienced as something warm, serene and reassuring. All patients considered that the physician was the most appropriate partner. No criticisms emerged.
I felt comfortable and free to ask any question….
The rapport generated was more one friendship than doctor‐patient relation.
Everything I wanted to know about my illness was explained in great detail.
It’s important that the person [interviewer] is open and friendly, whoever he is… but perhaps a neurologist would know more. A doctor I’ve never met before would be OK, but if I asked a question and he wasn’t able to reply, that wouldn’t be OK.
CD
All patients emphasized that the CD was a valuable source of information that helped them enhance their understanding of their disease. The aspects best remembered were descriptions of disease mechanisms and symptoms. When asked whether an interview without CD or a CD without the physician would have been preferred (Table S1), all patients said that both were essential. One patient would have liked to take the CD home, instead of the booklet.
I remember she asked me what things about my illness were most important to me […] then we went to that exact point on the CD, and went through it together.
Yes, I understood what I had… [it was] very well done, anyone could grasp it.
I much appreciated this approach […] very useful… it’s particularly good if someone like a neurologist is there, giving backing explanations to the images. I liked having the opportunity to ask questions, and go over things raised.
The contents of the CD were considered comprehensive but not excessive, except for a patient who commented that the CD (and booklet) did not include enough information about diet for MS and another who considered the two pictures of thalidomide children (therapies section) too direct and distressing.
It affected me perhaps because of those pictures of [malformed] children… I don’t know… but it made me feel bad.
Booklet
All patients said that they looked at the booklet and considered it clear and understandable. Most patients kept it in an accessible place, such as a bookshelf or the medicine cabinet. They viewed the booklet as useful for resolving uncertainties and considered it an adjunct to the personal interview (i.e. not sufficient as a stand‐alone tool).
It served mainly to clarify doubts that hadn’t been made clear when I talked to the neurologist.
By reading it, I better understood why I had been given that test.
It’s in the tray, with my medicines.
It’s in the bag where I keep my medications.
Most patients said that they read the booklet immediately after the personal interview; subsequent consultation was reported only occasionally.
I took it out again when my daughter wanted to know…. she asked me if she could read it.
I don’t remember it particularly well […] you look at it once, every now and then you have to dip into it. It’s always there [if you need it].
Effect of the information aid
Patients thought that the aid did not significantly change their relation with the caring neurologist or team. In some instances, however, the aid was considered to improve communication with them. It was also noted that it became easier to share information on the disease with their significant others.
Thanks to the booklet I was better able to communicate with her [the caring neurologist], just by referring to knowledge […] common knowledge we shared.
The booklet did not reassure anyone, nevertheless, even they [wife and son] got a clearer picture of my disease.
Patients’ views about effects of the aid on their information needs were varied. Some patients reported that the aid did not satisfy all their needs, so they sought information on the web or elsewhere. Other patients said that they obtained all information they needed by participating in the trial.
No, at the beginning I must admit I went on the internet….
I didn’t need to. I mean it. Not at all… Because all I wanted to know […] was explained by the booklet, the CD and also by the physician.
The information aid seemed to influence patients’ attitude to their disease (and therapies) as well as increase their knowledge and understanding. The quality of the information and the way it was conveyed reassured the patients, helping them to cope with the shock of receiving the diagnosis and its attendant uncertainties.
It helps you face up to the disease […] not as something negative but as something normal, or not a disease so severe to….
Initially I felt bad, but I felt better after seeing the CD and reading the booklet, which helped me understand what I really had.
I think it helped me to overcome […] to get through that moment immediately after the diagnosis […] the critical period….
Having information that is not terrorizing […] is appreciated even more, particularly by someone who’s just learned she has the disease.
It’s unusual when you get a new treatment to also be given something with explanations about things you don’t know about or that worry you. And, when you leave, there are still things that bother you, so the only thing you can do is go back and ask [the doctor] […]. But [with the booklet] that didn’t happen.
I looked through it to learn about [treatments], what the side effects were, everything.
Proposals
There were few suggestions as to how to improve the information aid. Two people suggested that a psychologist should be available to take care of emotional aspects in the peri‐diagnostic period; one wanted a more flexible timing of the personal interview; another suggested a website for home consultation.
A psychologist [would be a good idea] to keep an eye on emotional status… because some people need someone external to lean on emotionally, someone other than just a relative.
FGM with interviewing physicians
The FGM lasted 2 h. All four eligible physicians (two neurologists and two neurological interns, all women, aged 30–42 years, MS expertise 3–8 years) took part. General experience of the personal interview was first examined, followed by evaluation of the quality of the relation with patients and the use of the CD. The analysis aimed to identify positive and negative elements of the experience and to elicit suggestions for use of the information pack in routine practice.
Experience
Overall experience was positive, and the combination of the personal interview with the CD (and booklet) was appreciated. Five elements were identified: (i) most patients expressed satisfaction, (ii) enough time was given for the interview, in an adequately secluded environment that reduced pressure, (ii) effective information exchange took place and patient feedback was obtained, (iv) appropriate and consistent medical terms were used to communicate with patients, and (v) the figures, flowcharts and other visual aids improved and simplified the delivery of information.
Some physicians stated that they changed their attitude to disclosing the MS diagnosis to patients in everyday practice as a result of trial participation.
The strength of this instrument is the combination of three elements: neurologist, CD‐plus‐booklet, and extra time….
The setting is vital, in the outpatient unit [even though] you try to do your best in terms of time and attention dedicated to the patient [it isn’t enough]. Here it was different, and the patients appreciated this.
It’s a good occasion to communicate about the diagnosis […] like a second chance for the patient.
Used clear terms instead of euphemisms….
The diagrams and other structured aids help to keep to a logical path….
A negative experience was reported in a patient with primary progressive MS (there were seven SIMS‐Trial participants [three in study arm] with primary progressive MS, none of whom participated in the ISIs), owing to the poor prognosis and lack of disease‐modifying treatments for this type of MS.
If the patient looks at the prognoses for the different disease he realizes that his form [primary progressive MS] is the worst […] as he receives more detailed information, he understands there is no treatment for him […] the prognosis is worse […] I would suggest a more specific information aid for these patients.
All physicians thought that the interview times should be better tailored to patients’ needs.
Some patients didn’t have time enough to realize [what they had]. It would be better to have two personal interviews… the first to provide information via the CD and dialogue, the second, after the patient has enough time to digest things, to ask questions.
We should schedule the personal interview at times that suit the individual patient.
In an ideal world more than one interview would be better, because imparting information is a process, not a one‐hour event.
The information aid and the extra time dedicated to the patient via the personal interview had a positive effect on relationships between the patient and physician/medical team. This was particularly the case for larger MS centres that are often relatively inflexible in their procedures. In small centres, it was easier to integrate the information aid seamlessly into the current practice.
At our center, which is not large, the information aid was useful but it did not dramatically change relations between patients and the MS team.
CD
All physicians appreciated the CD as a way to improve communication. It was reported that patients’ interest in the CD contents increased as the personal interview progressed. At the beginning, the choice of navigation route tended to be left to the physician, later patients started making the choices. The physicians also reported that they felt uneasy about using the CD when they did the first personal interviews.
With the neurologist and booklet only there wouldn’t have been the same impact. The CD made information exchange more effective.
Initially the CD was viewed with some suspicion and skepticism. At first patients preferred to discuss points with me. […] Later then they asked to go to things they had seen on the CD menu, as if they needed to familiarize themselves with the CD.
At the beginning I was also a bit uneasy, I didn’t know how to introduce the CD. Later I learned to perceive what the patient was interested in, what he knew, how anxious he was.
The first thing to be decided was who had to choose where to go on the CD … was it up to me? Or was it up to the patient?
According to the physicians, the CD items that most interested patients were disease‐modifying therapies, genetics, causes, prognosis and FAQs. Information on clinical research (study phases and ethics) only interested patients followed in centres heavily committed to clinical trials.
The section about emotions (and its accompanying movie) was viewed rarely. Some physicians considered the movie inappropriate and preferred to skip it, particularly because a scene showed a sitting MS patient with her crutches close by.
I tended to skip some parts of the CD, I didn’t show the movie because in my view it was too much… it bothered some patients… even though its intent was to support the patient, it tended to increase anxiety.
A negative experience with the CD was reported: a patient was upset by pictures of thalidomide children (see also patient interview results above). Another negative experience was reported about a patient bothered by the affirmation that MS ‘is not a lethal disease’ (FAQ section).
At one centre, the CD sometimes stopped working, and it was necessary to shift to the booklet.
Some (particularly younger) patients would have liked to take home the CD instead of the booklet.
SIMS‐Trial personal interview
All interviewing physicians agreed that a neurologist or doctor with MS expertise was necessary for the personal interview. It was considered that such an interview was not part of the professional duty of MS nurses.
A nurse cannot substitute the physician as interviewer. A nurse doesn’t have the professional expertise or knowledge to discuss detailed aspects of the disease and its treatment.
Emotional reactions associated with the diagnosis communication emerged as an additional (and not strictly relevant) theme during discussions. It was considered that the physician rather than a psychologist should deal with these emotional reactions. A psychologist could support the patient if required, in a separate setting.
Physicians’ views about participation of patient significant others in the personal interview were mixed. Some thought that such a person would be useful to aid recall of key points subsequently; others reported experience that a significant other tended to dominate the interview or filter information.
The delivery of the booklet at the end of the interview was considered positive.
After receiving the booklet some patients said – you’ve given me something to take home and look through later on – thus it was a way of helping the patient become autonomous.
Overall evaluation
Positive. There was a consensus that the combination of the physician, the CD and take‐home booklet was the main strength of the intervention.
Negative. The information aid in its present form was considered unsuitable for patients with primary progressive MS. The movie on emotions, the images of thalidomide children and the affirmation that MS ‘is not a lethal disease’ were aspects of the CD that required modification.
Proposals
The following suggestions emerged: reconsider the timing of the personal interview (to be sensitive to patients’ needs); evaluate the possibility of doing two interviews; and improve the training of the interviewing physician.
FGM with caring neurologists
The FGM lasted 2 h. Six neurologists (two men) who communicated the MS diagnosis and cared for the patients at the MS centres took part. Age was 34–52 years and MS expertise was 6–25 years. All examined the CD and booklet before the FGM (one also contributed to aid development). General impressions of the information aid were first elicited, followed by its perceived utility, as well as its impact, if any, on relations with patients. As before, the aims were to identify positive and negative aspects of the experience and derive suggestions for use of the aid in routine practice.
Experience
Some caring neurologists had difficulty identifying patients who had actually received the aid, because both study and control patients appeared very satisfied with the way they had been dealt with. Few other specific experiences were reported; most comments centred on the neurologists’ views of the information aid and what they expected of it. Their overall judgment was positive because (i) it offered an additional occasion for information exchange, subsequent to the MS diagnosis disclosure, (ii) the CD was explored under the guidance of a physician expert in MS, and (ii) a booklet was given for home consultation.
The interview with the CD after diagnosis disclosure was a way of overcoming the ‘blackout’ that frequently occurs when the diagnosis is disclosed […]. At that point the patient is able to pay more attention to the contents.
A particularly anxious patient refused to the information aid, but all those who participated were satisfied.
Most neurologists did not notice any effect of the aid on patient’s knowledge. However, one neurologist reported that study patients had less difficulty (were more at ease) completing the questionnaire on MS knowledge than control patients.
I have no way to evaluate whether [the information aid] had any effect on MS knowledge.
I had no feedback [on MS knowledge] from my patients.
Those who did not receive [the information aid] were more uneasy about filling in the questionnaire on MS knowledge and often asked for clarifications.
Because the aid answered common questions about MS, it was often able to reassure patients.
A positive impact for many common questions, e.g. about life expectancy and pregnancy […] most were reassured.
The timing of the personal interview was considered too rigid, and it should have been more sensitive to the patient’s needs. One neurologist thought that the aid could be challenging or frustrating for poorly educated patients.
A major challenge for educationally deprived patients.
Overall evaluation
Positive: The overall judgment of the caring neurologists was positive because the aid was thought to improve information delivery and exchange in an appropriate and effective way. All aid components were considered necessary.
Negative: No major criticisms, except that the timing of the interview should be tailored to the patient’s wishes, and the aid was probably less suitable for very poorly educated patients.
Proposals: Develop a specific aid for patients with clinically isolated syndrome (CIS) and possible MS.
Discussion
Engaging people with MS in clinical decision making has become increasingly important in recent years. 14 When we devised the SIMS‐Trial, the UK National Institute for Health and Clinical Excellence (NICE) grade A recommendation for an information pack specific for newly diagnosed MS patients was based on evidence obtained in patients with stroke and cancer, but not MS. 28 This situation is changing rapidly, with some randomized controlled trials on information 17 and decision support techniques 14 , 29 published or on‐going (ISRCTN12440282; ISRCTN83438362).
The SIMS‐Trial information aid was experienced as positive by patients and interviewing physicians as it improved patient’s knowledge of, and attitude to, their disease. All agreed that no prioritization of aid components was possible, but that its strength derived from the combination of components. It was also agreed that the personal interview should be scheduled for patient convenience. The interviewing physicians considered that the aid was unsuitable for patients with primary progressive MS (10–15% of all MS cases) and suggested improved training in CD use in the personal interview. It was also agreed that the CD and booklet should be revised by removing the images of thalidomide children and adding information on diet in MS (see Box 1).
Patients’ assessment of the medical information presented in the aid was mixed: most welcomed the detailed and clear information provided, but some objected to the sentence ‘MS is not a lethal disease’ (FAQ section) probably in relation to the emotional stress they were experiencing in the period around diagnosis disclosure. The issue of emotional stress emerged repeatedly during the ISIs (although the interviewing psychologist guided the discussion towards themes more connected to the information aid) and some interviewed patients thought that psychological support should be available for newly diagnosed patients. These findings illustrate that anxiety is prominent in newly diagnosed patients with MS 30 in whom post‐traumatic stress disorder has even been reported, 31 and emphasize the importance of the presence of an interviewer sensitive to this aspect, and not simply a CD or booklet. It is noteworthy that the negative comments about the movie on emotions came from the interviewing physicians and not from patients. It is possible that the physicians felt uncomfortable dealing with disability in newly diagnosed patients and thus did not encourage them to view the movie.
The interviewing physicians reported initial difficulty in using the CD in the SIMS‐Trial personal interview, even though all received training on its use and content. However, this difficulty soon passed, and they expressed appreciation for the flowcharts and visual aids present on the CD. Some said that their experience with the CD improved their communication with patients in general.
The caring neurologists judged the information aid positively, but their comments were centred on their views of the information aid in general; importantly, they did not comment on whether the information aid had any effect on their relation with their patients. We interpreted this as evidence that the aid had no major effect on the caring physician–patient relation (in agreement with secondary trial outcomes). 17
To minimize bias, ISIs were conducted by a psychologist who had not participated in the SIMS‐Trial, the analysis panel included an independent qualitative researcher (GM), and the FGM reports were reviewed by participants (respondent validation).
One limitation of this qualitative study is that we did not identify the most valuable component(s) of the intervention. Only nine patients were interviewed. We stopped after nine interviews because of data saturation. 24 However, those interviewed had diverse general and clinical features and, importantly, by conducting FGMs of interviewing physicians and caring neurologists, the issue of the inappropriateness of the aid for the minority of MS patients with primary progressive MS was raised.
Another limitation is that there were no patients with truly negative outcomes. We sampled patients with the lowest (most negative) scores, but overall scores were high (minimum 25; possible range 0–42.5) for intervention effectiveness.
Furthermore, the ISIs were conducted a considerable time (8–20 months) after delivery of the information aid, and this could have affected patient recall. We considered the option of interviewing patients shortly after the personal interview, but discarded it because we thought that sufficient time was necessary to allow the patients to develop a balanced view of their experience.
Structural barriers can limit the implementation of the information aid in routine practice. Even in the trial setting, it was often difficult to find a free room and the time for the personal interview; this was particularly the case for the largest centres.
The SIMS‐Trial required a physician for the personal interview. And this raises an important issue, because in several countries, cost and other considerations would probably mean another professional (e.g. nurse) would be more suitable for conducting the interview. That a physician was most appropriate person in our study emerged from meetings with MS patients and health professionals when the aid was being devised 7 (Fig. 1). In Italy, such an interview is not part of the traditional duty of nurses, so a physician was the only choice. However in recent years, the training and professional status of nurses has improved markedly in Italy, and MS nurses may now be the appropriate persons for conducting the personal interview, provided they are trained to conduct the interview and present the CD.
Further work is necessary to clarify the value of the information aid as a whole and its components in routine clinical practice: in the next (third) phase of the SIMS project, the effectiveness of the personal interview plus the information materials (updated and revised based on results of the first two phases) will be compared with the information materials alone in 30 Italian MS centres.
Table Box 1.
Conclusions of SIMS‐Qual study
| Positive |
| The aid improved information delivery, patient understanding and communication with MS team and significant others, as well as attitude to disease |
| All components of the aid were considered necessary |
| Negative |
| Timing of personal interview too insensitive to patient wishes |
| Aid unsuitable for patients with primary progressive MS |
| Difficult to integrate personal interview within working practice of MS centres (particularly high‐volume ones) for structural and personnel limitations |
| Proposals |
| Improve training on CD use in the personal interview |
| Revise of the following aspects of the CD/booklet: |
| Remove images of thalidomide children |
| Add information on diet in MS |
| Develop a specific aid for patients with clinically isolated syndrome (CIS) and possible MS (and for primary progressive MS) |
MS, multiple sclerosis.
Conclusions
The results of this study further support the value of the information aid and also provide important indications for improving the aid and refining indications for its use (Box 1).
Conflicts of Interest
AL has served as a consultant to Fondazione Serono and has received speaker honoraria or research grants from Bayer Schering, Biogen‐Dompé, Merck Serono, Novartis Pharma, Sanofi Aventis and funding for travels from Bayer Schering, Biogen‐Dompè, Sanofi Aventis, Merck Serono and Teva, Novartis. VM has received speaker honoraria and funding for travels from Biogen‐Dompé SG, Merck Serono, Bayer Schering Pharma, Novartis and Sanofi Aventis and has served as a consultant to Bayer Schering Pharma, Sanofi Aventis and Teva Pharmaceutical Industries. FG has received speaker honoraria and funding for travels from Biogen‐Dompè, Merck Serono, Sanofi‐Aventis, Bayer Schering and Novartis. AS has received board membership fee from Novartis and speaker honoraria from Sanofi Aventis. CB, AG, MF, CT, IP, MR, DF, ED, EB, NA and GM have no conflicts of interest.
Source of funding
The Fondazione Italiana Sclerosi Multipla (FISM) funded the study (Grant No. 2009/R/4 to CB) and supported AG with a research fellowship. The funding source had no role in study design, data collection, data analysis, data interpretation or report writing. The corresponding author had full access to all data and had final responsibility for decision to submit the paper.
Supporting information
Table S1. Template for individual semi‐structured interviews.
Table S2. Template of the FGM with the SIMS‐Trial interviewing physicians.
Table S3. Template of the FGM with the SIMS‐Trial caring neurologists.
Appendix S1. This file includes the SIMS‐Trial group investigators.
Supporting info item
Supporting info item
Supporting info item
Supporting info item
Acknowledgements
We thank Don Ward for help with the English, Giusi Ferrari for organizing interviews and meetings, and all of the patients with MS who participated in the study.
References
- 1. Cooper GS, Stroehla BC. The epidemiology of autoimmune diseases. Autoimmunity Reviews, 2003; 2: 119–125. [DOI] [PubMed] [Google Scholar]
- 2. Polman CH, Reingold SC, Edan G et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the McDonald’s criteria. Annals of Neurology, 2005; 58: 840–846. [DOI] [PubMed] [Google Scholar]
- 3. Comi G, Filippi M, Barkhof F, the Early Treatment of Multiple Sclerosis Study Group . Effects of early interferon‐beta treatment on conversion to definite multiple sclerosis: a randomized study. Lancet, 2001; 357: 1576–1582. [DOI] [PubMed] [Google Scholar]
- 4. Heesen C, Kolbeck J, Gold SM, Schulz H, Schulz KH. Delivering the diagnosis of multiple sclerosis. Results of a survey among patients and neurologists. Acta Neurologica Scandinavica, 2003; 107: 363–368. [DOI] [PubMed] [Google Scholar]
- 5. Johnson J. On receiving the diagnosis of multiple sclerosis: managing the transition. Multiple Sclerosis, 2003; 9: 82–88. [DOI] [PubMed] [Google Scholar]
- 6. Janssens ACJW, de Boer JB, Kalkers NF, Passchier J, van Doorna PA, Hintzen RQ. Patients with multiple sclerosis prefer early diagnosis. European Journal of Neurology, 2004; 11: 335–337. [DOI] [PubMed] [Google Scholar]
- 7. Solari A, Acquarone N, Pucci E et al. Communicating the diagnosis of multiple sclerosis – a qualitative study. Multiple Sclerosis, 2007; 13: 763–769. [DOI] [PubMed] [Google Scholar]
- 8. Terry K. Telling patients more will save you time. Medical Economics, 1994; 71: 40–52. [PubMed] [Google Scholar]
- 9. Nease RF, Brooks WB. Patient desire for information and decision making in health care decisions: the Autonomy Preference Index and the Health Opinion Survey. Journal of General Internal Medicine, 1995; 10: 593–600. [DOI] [PubMed] [Google Scholar]
- 10. Charles C, Gafni A, Whelan T. Shared decision‐making in the medical encounter: what does it mean? (Or, it takes at least two to tango) Social Science & Medicine, 1997; 44: 681–692. [DOI] [PubMed] [Google Scholar]
- 11. Woolf SH, Chan EC, Harris R et al. Promoting informed choice: transforming health care to dispense knowledge for decision making. Annals of Internal Medicine, 2005; 143: 293–300. [DOI] [PubMed] [Google Scholar]
- 12. Stewart M. Effective physician‐patient communication and health outcomes: a review. Canadian Medical Association Journal, 1995; 152: 1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 13. Edwards A, Elwyn G. Evidence Based Patient Choice. Oxford: Oxford University Press, 2001. [Google Scholar]
- 14. Heesen C, Solari A, Giordano A, Kasper J, Köpke S. Decisions on multiple sclerosis immunotherapy: new treatment complexities urge patient engagement. Journal of the Neurological Sciences, 2011; 306: 192–197. [DOI] [PubMed] [Google Scholar]
- 15. Campbell M, Fitzpatrick R, Haines A et al. Framework for design and evaluation of complex interventions to improve health. BMJ, 2000; 321: 694–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ, 2008; 337: 979–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Solari A, Martinelli V, Trojano M, on behalf of the SIMS‐Trial group . An information aid for newly diagnosed multiple sclerosis patients improves disease knowledge and satisfaction with care. Multiple Sclerosis, 2010; 16: 1393–1405. [DOI] [PubMed] [Google Scholar]
- 18. Giordano A, Uccelli MM, Pucci E, on behalf of the SIMS‐Trial group . The Multiple Sclerosis Knowledge Questionnaire: a self‐administered instrument for recently diagnosed patients. Multiple Sclerosis, 2010; 16: 100–111. [DOI] [PubMed] [Google Scholar]
- 19. Solari A, Mattarozzi K, Vignatelli L, on behalf of the SIMS‐Trial group and of the GERONIMUS group . Development and validation of a patient self‐assessed questionnaire on satisfaction with communication of the multiple sclerosis diagnosis. Multiple Sclerosis, 2010; 16: 1237–1247. [DOI] [PubMed] [Google Scholar]
- 20. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 1983; 67: 361–370. [DOI] [PubMed] [Google Scholar]
- 21. Costantini M, Musso M, Viterbori P et al. Detecting psychological distress in cancer patients: validity of the Italian version of the Hospital Anxiety and Depression Scale. Supportive Care in Cancer, 1999; 7: 121–127. [DOI] [PubMed] [Google Scholar]
- 22. Degner LF, Sloan JA, Venkatesh P. The control preference scale. The Canadian Journal of Nursing Research, 1997; 29: 21–43. [PubMed] [Google Scholar]
- 23. Giordano A, Mattarozzi K, Pucci E et al. Participation in medical decision‐making: attitudes of Italians with multiple sclerosis. Journal of the Neurological Sciences, 2008; 275: 86–91. [DOI] [PubMed] [Google Scholar]
- 24. Denzin NK, Lincoln YS. Handbook of Qualitative Research. London: Sage, 2000. [Google Scholar]
- 25. Silverman D. Interpreting Qualitative Data. London: Sage, 1993. [Google Scholar]
- 26. Crabtree BF, Miller WL. Doing Qualitative Research. London: Sage, 1992. [Google Scholar]
- 27. Mc Cracken G. The Long Interview. London: Sage, 1988. [Google Scholar]
- 28. National Collaborating Centre for Chronic Conditions . Multiple Sclerosis: National Clinical Guideline for Diagnosis and Management in Primary and Secondary Care (NICE Clinical Guideline 8). London, GB: Royal College of Physicians, 2004. [PubMed] [Google Scholar]
- 29. Prunty MC, Sharpe L, Butow P, Fulcher G. The motherhood choice: a decision aid for women with multiple sclerosis. Patient Education and Counseling, 2008; 71: 108–115. [DOI] [PubMed] [Google Scholar]
- 30. Janssens AC, van Doorn PA, de Boer JB, van der Meché FG, Passchier J, Hintzen RQ. Impact of recently diagnosed multiple sclerosis on quality of life, anxiety, depression and distress of patients and partners. Acta Neurologica Scandinavica, 2003; 108: 389–395. [DOI] [PubMed] [Google Scholar]
- 31. Chalfant AM, Richard A, Bryant RA, Fulcher G. Posttraumatic stress disorder following diagnosis of multiple sclerosis. Journal of Traumatic Stress, 2004; 17: 423–428. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Template for individual semi‐structured interviews.
Table S2. Template of the FGM with the SIMS‐Trial interviewing physicians.
Table S3. Template of the FGM with the SIMS‐Trial caring neurologists.
Appendix S1. This file includes the SIMS‐Trial group investigators.
Supporting info item
Supporting info item
Supporting info item
Supporting info item


