Abstract
Increased fructose consumption has been suggested to contribute to non-alcoholic fatty liver disease (NAFLD), dyslipidemia, and insulin resistance, but a causal role of fructose in these metabolic diseases remains debated. Mechanistically, hepatic fructose metabolism yields precursors that can be used for gluconeogenesis and de novo lipogenesis (DNL). Fructose-derived precursors also act as nutritional regulators of the transcription factors, including ChREBP and SREBP1c, that regulate the expression of hepatic gluconeogenesis and DNL genes. In support of these mechanisms, fructose intake increases hepatic gluconeogenesis and DNL and raises plasma glucose and triglyceride levels in humans. However, epidemiological and fructose-intervention studies have had inconclusive results with respect to liver fat, and there is currently no good human evidence that fructose, when consumed in isocaloric amounts, causes more liver fat accumulation than other energy-dense nutrients. In this review, we aim to provide an overview of the seemingly contradicting literature on fructose and NAFLD. We outline fructose physiology, the mechanisms that link fructose to NAFLD, and the available evidence from human studies. From this framework, we conclude that the cellular mechanisms underlying hepatic fructose metabolism will likely reveal novel targets for the treatment of NAFLD, dyslipidemia, and hepatic insulin resistance. Finally, fructose-containing sugars are a major source of excess calories, suggesting that a reduction of their intake has potential for the prevention of NAFLD and other obesity-related diseases.
Keywords: fructose, hepatic steatosis, NAFLD, de novo lipogenesis, lipid synthesis, ChREBP, insulin resistance, obesity, metabolic syndrome
1. Introduction
Obesity and obesity-related cardiometabolic conditions are an epidemic threat to public health [1]. Globally, more than one in three adults is now overweight or obese, and the prevalence of overweight and obesity continues to rise in both developed and developing countries [2]. Obesity predisposes to several medical complications, including, but not limited to hypertension, dyslipidemia, non-alcoholic fatty liver disease (NAFLD), type 2 diabetes, atherosclerosis, and some forms of cancer [3]. As a consequence, overweight and obesity are associated with increased risks for all-cause and cause-specific mortality [4,5].
Often considered the hepatic manifestation of the metabolic syndrome, NAFLD is defined by hepatic steatosis (that is, intrahepatic lipid accumulation) in the absence of apparent liver disease or excessive alcohol intake [6]. Hepatic steatosis is commonly diagnosed when ≥5% of hepatocytes contain large lipid droplets or when intrahepatic triglyceride content is >5.6% [7,8], but note that the definition of normal liver fat content depends on the assessment method. In this regard, the magnetic resonance spectroscopy-based cutoff of 5.6% (that is, liver volume comprised of fat) corresponds to approximately 15% histologically confirmed steatosis (that is, hepatocytes with macrovesicular steatosis) [9]. Alarmingly, on the basis of a recent meta-analysis of 45 imaging studies, an estimated quarter of the global adult population suffers from NAFLD [10]. This is a cause for major concern, because NAFLD increases the risk for type 2 diabetes and cardiovascular disease [11]. Moreover, simple steatosis in the context of NAFLD may progress to non-alcoholic steatohepatitis (NASH) and liver fibrosis [12,13,14]. As such, NAFLD/NASH is now the third leading cause for liver transplantation [15,16].
Intrahepatic lipid accumulation may be the result of, in parts, increased delivery of fatty acids (FA) to the liver, increased hepatic FA synthesis from de novo lipogenesis (DNL), and/or decreased lipid clearance through secretion or oxidation [17,18,19]. Although the relative contribution of these pathways to the development of clinical NAFLD is only partially known, several human trials have demonstrated that increased DNL is a particularly important abnormality in NAFLD [18,19,20]. Overconsumption of added sugar, the intake of which has increased dramatically over the past century [20], is associated with obesity, NAFLD, and insulin resistance [21,22,23,24,25,26]. Some of these associations may be the result of stimulation of hepatic DNL by dietary sugars [27,28,29]. Notably, most added sugars, including sucrose and high-fructose corn syrup, are made up of near-equal shares glucose and fructose, but fructose is emerging as the potentially harmful component [29]. Unlike glucose, ingested fructose is preferentially metabolized by the liver [30]. This and several other features of fructose metabolism make it an exceptionally lipogenic sugar [20,29,31].
In this review, we will focus on the role of fructose consumption in the development of hepatic steatosis. To this end, we will first discuss fructose physiology and the molecular mechanisms that may link fructose to NAFLD and insulin resistance. We will then consider the available evidence from studies in humans to determine the impact of fructose metabolism on clinically relevant outcomes. Finally, we will use this framework to discuss opportunities for therapy. Our review methods are summarized in Appendix A. Recommendations for further reading are listed in Appendix B.
2. Fructose Metabolism in Physiology
Food and drink contain fructose as monosaccharide (free fructose), disaccharide (sucrose), or polysaccharide (fructan). Whereas free fructose is absorbed directly from the intestinal lumen, fructose in larger carbohydrate molecules is first cleaved off at the lumenal membrane of enterocytes [32]. Intestinal fructose transport is mainly facilitated by glucose transporter 5 (GLUT5/SLC2A5) on the lumenal side and glucose transporter 2 (GLUT2/SLC2A2) on the basolateral side [33,34,35]. Once in the portal circulation, ingested fructose is transported into the liver via specific hexose transporters. Hepatic GLUT2 is thought to be the primary glucose and fructose transporter [35,36]; however, glucose transporter 8 (GLUT8/SLC2A8) has also been shown to mediate fructose transport into hepatocytes and hepatic fructose metabolism [37]. Other glucose transporter family members are likely involved as well [38]. Ingested fructose is almost completely extracted from the portal blood upon first-pass [30]. In contrast to ingested glucose, only a small fraction of ingested fructose will ultimately enter systemic circulation [39,40].
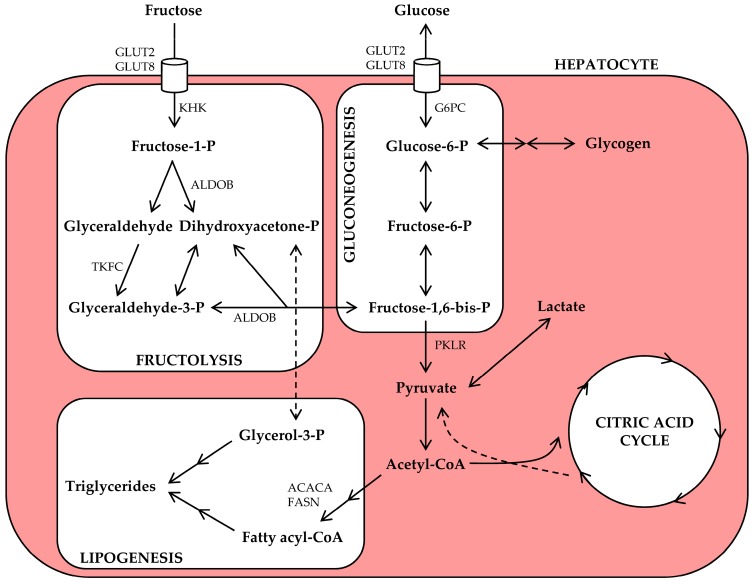
An overview of hepatic fructose metabolism is presented in Figure 1. Briefly, hepatic fructolysis is initiated by phosphorylation of fructose into fructose-1-phosphate by ketohexokinase (KHK). Through aldolase B (ALDOB) and triokinase (TKFC) activity, fructose-1-phosphate is then split into two triose phosphate intermediaries. Fructolysis bypasses the rate-limiting steps of glycolysis and is therefore much faster; ingestion of fructose rapidly results in the availability of downstream (triose phosphate) intermediaries [30,41,42]. At this point, fructose and glucose metabolic pathways converge, and the triose phosphate intermediaries may now enter the gluconeogenesis, lipogenesis, or oxidation pathways [42].
Figure 1.
Hepatic fructose metabolism provides substrate for multiple metabolic pathways. Ingested fructose is transported from the portal vein into hepatocytes via glucose transporter 2 (GLUT2) and glucose transporter 8 (GLUT8). Ketohexokinase (KHK) converts intracellular fructose to fructose-1-phosphate (fructose-1-P), which is then split into glyceraldehyde and dihydroxyacetone-phosphate (dihydroxyacetone-P) by aldolase B (ALDOB). Glyceraldehyde is further phosphorylated to glyceraldehyde-3-phosphate (glyceraldehyde-3-P). Fructolysis-derived triose phosphates can now be used for gluconeogenesis, glycogen synthesis, lactate production, or acetyl-CoA production, and the latter can be oxidized or used for lipogenesis. Other abbreviations: ACACA, acetyl-CoA carboxylase α; FASN, fatty acid synthase; G6PC, glucose-6-phosphatase; P, phosphate; PKLR, pyruvate kinase; TKFC, triokinase.
Although hepatocytes possess the enzymatic machineries to convert fructose-derived carbon into glucose, glycogen, lactate, lipid, carbon dioxide, and/or other metabolites [42], the actual metabolic fate of ingested fructose likely depends on various factors, including nutritional status, long-term dietary patterns, and/or genetic make-up. Isotope-labeled metabolic tracer techniques offer attractive means to quantitatively evaluate the conversion and oxidation of ingested fructose, and several of such tracer studies have been performed in humans. After administration of an acute oral fructose load to healthy non-exercising subjects, most ingested fructose is converted to glucose (29–54%, part of which may then be incorporated into glycogen) or lactate (~28%). A small percentage (~1%) enters the DNL pathway for conversion into lipid [39]. Despite these estimated conversion rates, acute fructose ingestion produces only minor increases in plasma glucose and insulin levels [43], whereas it consistently raises plasma triglyceride levels [43,44,45,46,47]. Isotope tracer studies also show that 31–59% of ingested fructose is oxidized (and ultimately converted into carbon dioxide) within 3–6 h after ingestion [39]. Thus, the hypertriglyceridemic effect of an acute fructose dose may involve metabolic pathways other than DNL, including a shift towards carbohydrate oxidation, thereby sparing lipids [39], or a decrease in peripheral tissue lipid uptake [45]. Chronic fructose consumption induces additional changes that promote hepatic lipid synthesis, and this will be discussed below.
3. What Are the Mechanisms Linking Fructose to NAFLD?
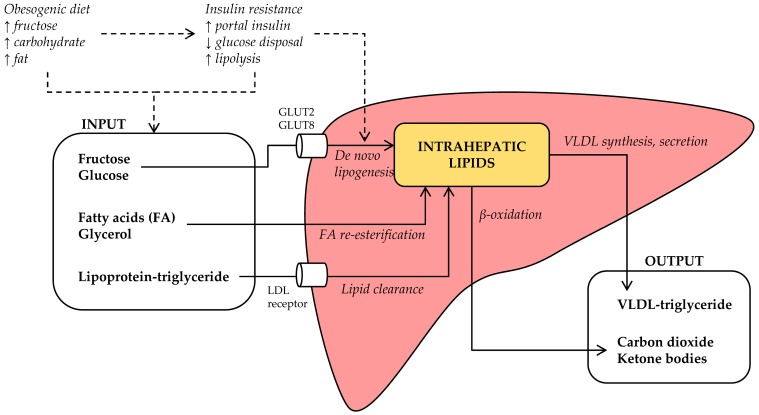
Intrahepatic lipids accumulate when the rate of hepatic lipid input exceeds the rate of hepatic lipid output (Figure 2). On the input side, lipids may be synthesized (de novo) from carbohydrates or other precursors, imported as lipolysis-derived FA, or imported as lipoprotein-derived triglyceride. Tracer experiments have demonstrated that all three input sources contribute significantly to intrahepatic lipid stores: ~59% of intrahepatic triglycerides in NAFLD patients derives from circulating FA, whereas ~26% derives from DNL and ~15% from dietary fat [18]. However, when NAFLD patients were compared to matched controls without steatosis, there was no meaningful difference in the FA flux from adipose tissue to liver [19]. In contrast, DNL was 3-fold greater in NAFLD compared to the control subjects [19], suggesting that increased DNL is a distinct pathophysiological feature of human NAFLD.
Figure 2.
Hepatic steatosis develops when lipid input exceeds lipid output. Lipid input consists of (i) de novo lipogenesis from (primarily carbohydrate) precursors, (ii) re-esterification of lipolysis-derived fatty acids (FA) and glycerol, and (iii) low-density lipoprotein (LDL) receptor-mediated endocytosis of remnant-triglycerides. Lipid output consists of (i) β-oxidation and (ii) secretion of triglycerides in very low-density lipoprotein (VLDL) particles. Other abbreviation: GLUT2, glucose transporter 2; GLUT8, glucose transporter 8.
On the output side, intrahepatic lipids may be utilized in β-oxidation, leading to the production of carbon dioxide or ketone bodies, or secreted as triglyceride in very low-density lipoprotein (VLDL) particles. Defects in these pathways have also been demonstrated, although interpretation of these data seems more complicated. Under fasting conditions, hepatic lipid oxidation rates are unchanged in NAFLD patients [48]; however, high fructose consumption may promote a shift towards carbohydrate oxidation [39]. In addition, NAFLD was associated with increased hepatic VLDL secretion in some [49,50,51], but not in all trials [19], whereas NASH was associated with decreased VLDL production [52]. In the following sections, we will discuss if and how fructose consumption influences these mechanisms.
3.1. Fructose and Lipid Synthesis
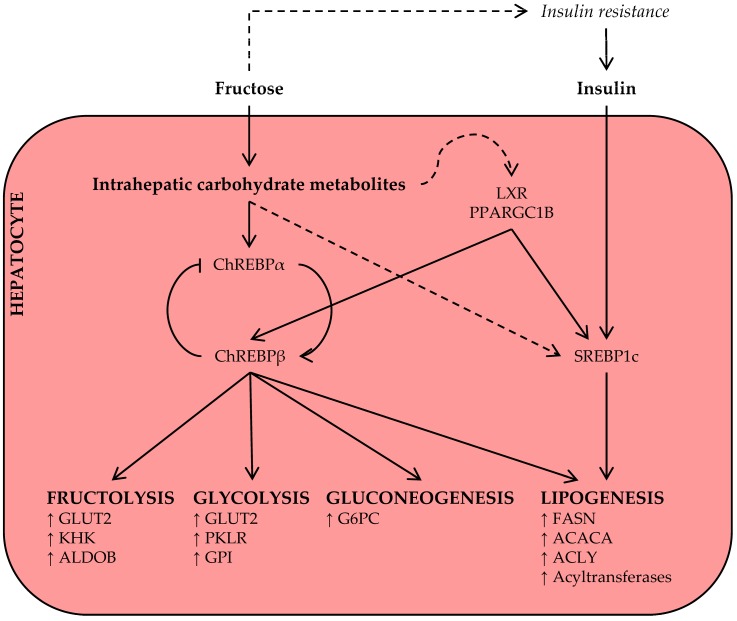
As discussed above, acute hepatic fructose metabolism rapidly results in the availability of DNL substrate, and some authors have suggested that this may largely drive the increase in plasma triglyceride levels after acute fructose ingestion [29]. This, however, has yet to be confirmed in human metabolic tracer studies [39]. The available evidence suggests that only a small percentage of fructose-derived carbon is directly converted into lipid within 4–6 h [45,53]. However, labeled acetate infusion studies do support DNL-promoting effects of fructose in the subacute-to-long term [46,54,55], suggesting that chronic fructose exposure induces prolipogenic mechanisms (Figure 3), in addition to increasing the availability of DNL substrate.
Figure 3.
Chronic fructose consumption promotes mechanisms that upregulate the hepatic lipogenesis program. Hepatic metabolism of ingested fructose increases levels of intrahepatic carbohydrate metabolites. These act as nutritional regulators of key transcription factors, including carbohydrate response element-binding protein (ChREBP) and sterol regulatory element-binding protein 1c (SREBP1c), and coactivators for genes in multiple metabolic pathways. Stimulation of the lipogenesis program is further amplified by hyperinsulinemia in the context of insulin resistance. Other abbreviations: ACACA, acetyl-CoA carboxylase α; ACLY, ATP citrate lyase; ALDOB, aldolase B; FASN, fatty acid synthase; G6PC, glucose-6-phosphatase; GLUT2, glucose transporter 2; GPI, glucose-6-phosphate isomerase; KHK, ketohexokinase; LXR, liver X receptor; PKLR, pyruvate kinase; PPARGC1B, peroxisome proliferator-activated receptor γ coactivator 1β.
Carbohydrate response element-binding protein (ChREBP), also known as Mlx interacting protein-like (MLXIPL), is a key transcription factor for enzymes in the fructolysis, glycolysis, gluconeogenesis, and DNL pathways [56,57,58]. The least potent isoform, ChREBPα, is inhibited under conditions of low glucose [59]; however, upon activation by intracellular carbohydrate metabolites, ChREBPα induces the transcription of a more potent isoform, ChREBPβ, from an alternative promotor [60]. Thus, the ChREBPα/β mechanism senses intracellular carbohydrate signals and regulates the expression of metabolic gene programs in response to increased carbohydrate availability [61].
As fructose is primarily metabolized by the liver [30], fructose, more than glucose, may give rise to the intrahepatic carbohydrate metabolites that activate hepatic ChREBP independently of hepatic insulin signaling [29,62,63,64]. Observations in multiple species now support an important role for hepatic ChREBP in fructose metabolism and metabolic disease. In rats, high-fructose feeding, as compared to glucose, was associated with increased ChREBP activity and expression of its target genes [65]. In accordance, high-fructose feeding to mice increased hepatocellular carbohydrate metabolites, expression of ChREBP target genes, and hepatic steatosis, and these adverse metabolic effects of the high-fructose diet were fully dependent on hepatic ChREBP activation [58]. In another recent rodent study, fructose-activated ChREBP induced the hepatic expression and secretion of fibroblast growth factor 21 (FGF21), a response that was essential for adaptive fructose metabolism [66]. Fructose ingestion also acutely raised circulating FGF21 levels in humans [43,67], warranting further investigation into the ChREBP-FGF21 signaling axis in fructose metabolism.
Notably, in the absence of ChREBP, high-fructose diets do not cause hepatic lipid accumulation, but inflammation and early signs of fibrosis instead [68]. It thus seems that ChREBP-mediated lipogenesis is required to prevent even more adverse hepatotoxicity upon fructose consumption, but that this adaptive mechanism may cause hepatic steatosis when too much fructose is consumed [69]. Increased hepatic ChREBP expression is also associated with NAFLD and insulin resistance in obese humans [70], but a direct effect of ingested fructose on ChREBP in human liver has not yet been demonstrated.
Sterol regulatory element-binding protein 1c (SREPB1c) is another key transcription factor for genes in the DNL pathway and implicated in the development of NAFLD [71]. The expression and post-translational activation of SREBP1c are strongly stimulated by insulin signaling; this mechanism ensures a coordinated DNL response under conditions of high glucose availability [57]. High-fructose diets commonly induce systemic insulin resistance and fasting hyperinsulinemia [58,72,73,74], thereby promoting insulin-mediated SREBP1c activation and hepatic lipid synthesis. However, the observations that insulin-depleted [75] and liver-specific insulin receptor knockout [76] mice also display an induction of SREBP1c upon acute sugar administration or on a short-term high-fructose diet indicate that this transcription factor is also regulated by nutrient signals, independent of insulin signaling. Finally, monosaccharides activate other transcriptional coactivators, including liver X receptor (LXR) [77] and peroxisome proliferator-activated receptor γ coactivator 1β (PPARGC1B) [78], that may amplify the ChREBP and SREBP1c-mediated lipogenesis response.
In summary, ingested fructose, unlike glucose, is primarily handled by hepatocytes, increasing the availability of intrahepatic carbohydrate metabolites. These provide hepatocytes with both DNL substrate and regulatory signals, mediated via several key lipogenesis transcription factors, for effective hepatic lipid synthesis.
3.2. Fructose and Lipolysis
In healthy human subjects, acute fructose ingestion is associated with a decrease in circulating FA levels [79], suggesting inhibition of adipose tissue lipolysis or increased FA clearance, but the signaling mechanism is currently unknown. An antilipolytic effect of fructose was also demonstrated in isolated rat adipocytes [80] and in healthy subjects after a 7-day high-fructose diet [81]. Adipose tissue lipolysis is primarily suppressed by insulin [82], but fructose ingestion does not stimulate a strong insulin excursion [43]. Another as-yet-unknown signal likely mediates this physiological effect of fructose ingestion.
Obesity, inflammation, and other mechanisms promote resistance to insulin’s antilipolytic effect [83]. This phenomenon is commonly referred to as adipose tissue insulin resistance and contributes to the increased release of FA from fat depots [84], which may contribute to intrahepatic lipid accumulation and the pathogenesis of NAFLD [85]. In obese insulin-resistant subjects, a relatively small increase in insulin following a fructose-rich meal or drink may not be sufficient to suppress adipose tissue lipolysis [86]. This would result in the continuous mobilization of endogenous energy stores under conditions of sufficient nutrient (ingested fructose) availability. These calories may then be diverted to the liver.
Increased visceral adiposity is strongly associated with adipocyte insulin resistance [87]. Since visceral adipose tissue releases FA into the portal circulation, which directly drains to the liver, this adipose compartment is particularly important in the context of NAFLD [26]. In one 10-week diet-intervention trial, the consumption of fructose, but not glucose, promoted the accumulation of visceral adipose tissue [55]. At the same time, 24-h average plasma FA levels were unchanged after the fructose diet, and the authors conclude that the harmful effects of fructose are not likely due to an effect on FA mobilization. However, since visceral lipolysis and/or portal FA levels were not quantified, these data do not exclude the possibility that chronic high fructose consumption contributes to an increased adipose tissue-liver FA flux.
There is some indirect evidence in support of this possibility. Insulin signaling in visceral white adipose tissue of rats is attenuated after 2 months of fructose, but not glucose, supplementation [88]. In another rat study, the administration of a high-fructose diet increased FA release from isolated adipocytes, as compared to glucose [89]. Human observational studies link the increased consumption of sugar-sweetened (fructose-containing) beverages to the accumulation of visceral adipose tissue [90] as well as intrahepatic lipids [91]. In addition, the consumption of excess calories from fructose contributes to weight gain [92], which promotes visceral adiposity, inflammation, and insulin resistance [83]. Thus, it remains debated whether fructose consumption directly influences adipocyte lipolysis and/or visceral adiposity, but it may contribute to an increase in adipose-to-liver FA trafficking through several indirect mechanisms.
3.3. Fructose and Hepatic Lipoprotein-Triglyceride Uptake
Approximately 15% of intrahepatic lipids are derived from dietary fat [18], and specific types of dietary fat, such as saturated FA [93], may increase intrahepatic lipid accumulation. Triglycerides from chylomicrons are hydrolyzed by lipoprotein lipase (LPL) for storage or oxidation in peripheral tissues. Spillover of FA from lipolysis of chylomicron-triglycerides is one route by which dietary lipids may end up in the liver [94]. Another is the clearance of chylomicron remnants, which carry triglycerides in addition to cholesteryl esters, after binding to the low-density lipoprotein (LDL) receptor on hepatocytes [95,96].
Hepatic lipoprotein metabolism also involves the secretion of VLDL particles (discussed below), remodeling of VLDL remnants, and clearance of cholesterol-rich LDL particles through LDL receptor-mediated endocytosis (for reviews, see [94,97]). This last route may also contribute, albeit limitedly, to hepatic triglyceride import. However, the hypertriglyceridemia associated with visceral adiposity is primarily due to impaired clearance of VLDL-triglycerides and lipoprotein remnants [94,97], suggesting that lipoprotein-triglyceride uptake is not necessarily increased in the context of the metabolic syndrome. In fact, tracer studies of triglyceride kinetics in obese humans suggest that liver fat is a determinant of lipoprotein synthesis, but not of lipoprotein clearance [50].
Short-to-medium-term high-fructose diets (conditionally) raise VLDL-associated plasma triglycerides in humans [55,98,99]. It is therefore likely that such diets also increase VLDL remnant concentrations and, by extension, hepatic remnant uptake [100]. We are, however, not aware of studies that have directly investigated the effect of an acute fructose load or chronic fructose consumption on hepatic lipoprotein (remnant) uptake in humans. In hamsters, high-fructose feeding was recently associated with the development of dyslipidemia and increased PCSK9-mediated hepatic LDL receptor degradation [101]. This suggests that decreased hepatic lipoprotein-triglyceride uptake may be one mechanism by which fructose contributes to dyslipidemia. However, the effect of fructose on hepatic lipoprotein handling in the context of NAFLD needs further exploration.
3.4. Fructose and β-Oxidation
Fructose is a high-energy nutrient. Its triose phosphate metabolites can enter the citric acid cycle for intrahepatic oxidation or the synthesis of glucose, lactate, and/or lipids (Figure 1). Most human cells lack the fructolysis machinery, but will readily use the newly synthesized glucose and lactate as energy source. Thus, via this two-step mechanism [102], fructose produces an energy source shift from lipid to carbohydrate oxidation [39,41], and this may influence the accumulation of intrahepatic lipids by decreasing hepatic lipid oxidation and output (Figure 2). This was demonstrated in rat livers, where perfusion with fructose-spiked blood inhibited hepatic β-oxidation of FA by substrate competition [103,104], as well as in healthy subjects, where the ingestion of fructose acutely increased carbohydrate oxidation and suppressed fat oxidation rates [79]. It is noteworthy that the inhibitory effect of fructose on FA oxidation in rat livers was amplified by co-administration of insulin [103], suggesting that it may be altered in the context of insulin resistance. Nevertheless, whether impaired β-oxidation is quantitatively relevant to clinical NAFLD remains inconclusive [26,48,105].
3.5. Fructose and Hepatic VLDL Secretion
Excess triglycerides are secreted from the liver in triglyceride-rich VLDL, which functions as a transporter for endogenous lipids in otherwise hydrophobic plasma. Most [49,50,51], but not all [19] of the available evidence indicates that the increased availability of liver fat in the context of NAFLD drives up hepatic VLDL secretion. Thus, in order for hepatic steatosis to progress, the rate of triglyceride synthesis (from DNL or FA re-esterification) must overcome the increased rate of VLDL secretion [105]. To our knowledge, it is unknown if fructose metabolites directly influence hepatic VLDL synthesis or secretion pathways. It is, however, generally thought that chronic fructose consumption and the increase in lipid synthesis will provide the liver with excess triglycerides, allowing for increased VLDL secretion [106].
Under postprandial conditions, insulin enhances LPL activity and triglyceride uptake in adipose tissue [106]. Fructose ingestion, however, does not induce high insulin levels and is, therefore, associated with relatively lower postprandial (insulin-stimulated) triglyceride clearance. This leads to large chylomicron and VLDL particles in circulation, hypertriglyceridemia, and, possibly, more remnants to circle back to the liver.
Finally, long-term exposure to intrahepatic lipid species results in endoplasmic reticulum (ER) and oxidative stress, which increases the degradation of apolipoprotein B100 and reduces VLDL secretion [107], suggesting that impaired hepatic triglyceride export may worsen hepatic steatosis in the long term. Accordingly, patients with NASH are characterized by distinctly impaired apolipoprotein B100, but not global protein, synthesis [52].
4. Does Fructose Consumption Cause Hepatic Steatosis in Humans?
4.1. Epidemiological Evidence
Several epidemiological studies have evaluated the association between average daily fructose intake and hepatic steatosis. In practice, human fructose consumption is largely driven by added sugars, and the intake of sugar-sweetened beverages generally corresponds to total fructose intake [108]. Data from the Framingham cohort indicated that the increased consumption of sugar-sweetened beverages is associated with fatty liver, independent of possible confounders such as overall energy intake [91]. In another study, patients with NAFLD consumed two-to-three times more fructose than matched controls [109]. Contrary, data from a large Finnish cohort did not support an association between fructose intake and NAFLD [110], and the NASH Clinical Research Network suggested that fructose intake is associated with reduced hepatic steatosis, but increased disease progression (that is, hepatic fibrosis) [111]. Thus, although there is some evidence linking real-world fructose consumption to the development of fatty liver, the epidemiological evidence is largely inconsistent and, as we stand, does not support definitive conclusions [112]. Moreover, dietary sugar intake has clearly been linked to weight gain [113], indicating that any association between fructose intake and NAFLD may be confounded by a positive energy balance and/or obesity.
4.2. Controlled Diet-Intervention Studies
Controlled diet-intervention trials prospectively compare the effects of a fructose-intervention diet to the effects of a control diet. As such, they are less susceptible to bias than epidemiological studies. These trials can be categorized as isocaloric, where the fructose-intervention diet and the control diet have the same energy content, or hypercaloric, where fructose supplementation provides extra energy relative to the control diet. Although short-term hypercaloric fructose-intervention trials may provide mechanistic insight into specific effects of fructose [114], they do not control for energy balance and their results cannot be easily generalized. Isocaloric fructose-intervention trials are most valuable to evaluate whether fructose, more than other nutrients, causes metabolic disease.
Two meta-analyses of data from four isocaloric fructose vs. glucose-intervention trials in a total of 63 healthy or overweight participants suggested that fructose, in and of itself, does not contribute to increased intrahepatic lipids during short-term (1–8 weeks) studies [112,115]. Both analyses did indicate that hypercaloric fructose, when compared to a weight-maintenance control diet, contributes to NAFLD, suggesting that excess calorie consumption, regardless of the source of these calories, induces liver fat accumulation. We are aware of two more isocaloric trials that have assessed the effects of fructose on liver fat since the synthesis of these meta-analyses. Schwarz et al. [116] compared high doses of fructose to isocaloric doses of complex carbohydrates during consecutive 9-day periods in a crossover design. All eight participants had higher rates of DNL and higher hepatic fat content after the fructose diets. Agebratt et al. [117] compared 2-month high-fruit vs. high-nut diets in 30 healthy participants. Here, the 3-fold increase in fructose intake in the fruit group was not associated with a change in liver fat.
Thus, so far, only one of the six available isocaloric comparisons supports the hypothesis that fructose, in and of itself, has adverse effects on clinically meaningful outcomes of NAFLD. It should, however, be noted that these observations are limited by the small sample sizes and short durations of the available trials. We are in clear need of large, long-term trials to determine if real-world fructose exposure contributes to the development of NAFLD and other metabolic diseases. In addition, fructose-containing sugars are an important source of excess calories, suggesting that a reduction of their intake may still have potential for the prevention of NAFLD [114].
4.3. Fructose Reduction as a Therapeutic Strategy
Current management of NAFLD primarily involves diet and lifestyle recommendations. Both caloric restriction and physical activity effectively reduce hepatic steatosis, but most patients are unable to stick with such lifestyles in the long term [118]. Targeting fructose-associated hepatic DNL may offer an alternative strategy to the management of NAFLD. Already, rodents can be protected from fructose-induced hepatic fat accumulation by several molecular interventions, including liver-specific activation of AMP-activated protein kinase [119] or activation of glutamate dehydrogenase, which promotes a metabolic shift from lipogenesis and gluconeogenesis toward glutamate synthesis [120]. Specific antilipogenic agents are not currently available for humans, but a better understanding of fructose metabolism will undoubtedly facilitate the development of novel pharmacological therapies. In addition, if fructose consumption plays an important role in the development and progression of NAFLD [121], then targeted low-fructose lifestyle interventions may have a beneficial effect on liver fat; but is there evidence for this?
A reduction in fructose intake can be achieved by several means, including low-carbohydrate diets, low-sugar diets, and/or the substitution of dietary fructose with low-fructose sweeteners. Volynets et al. [122] assessed the effects of a 6-month dietary intervention that focused on a reduction of fructose intake (~50% of baseline) in 10 subjects with NAFLD. Liver fat reduced significantly, but, as this was an uncontrolled trial, it cannot be ruled out that this was driven by a reduction in total energy intake and associated weight loss. Schwartz et al. [123] recently provided 41 obese children with metabolic syndrome features with isocaloric, but fructose-restricted (~33% of baseline) meals for 9 days. Both fractional DNL and liver fat were markedly lower after 9 days of fructose restriction. Although this was an uncontrolled trial as well, the dietary intervention was isocaloric and weight loss was minimal, suggesting that short-term fructose restriction reduces DNL and liver fat in obese children. We are not aware of any trials that have evaluated the effects of fructose reduction on liver fat in NAFLD in a controlled study design. In one 6-month pilot study, children with NAFLD tended to have lower plasma levels of liver enzymes with diet education aimed at reducing fructose intake [124], but this finding has yet to be replicated in a larger sample.
Finally, a recent meta-analysis of four trials indicated that the consumption of a low-carbohydrate diet is associated with improved liver fat content in subjects with NAFLD [125]. In two of the included trials, the low-carbohydrate/high-fat diet was adequately compared to a control diet, suggesting that low-carbohydrate diets may be more effective for liver fat reduction than low-fat diets. It remains to be determined if a reduction in fructose intake in the context of a low-carbohydrate diet is responsible for part of these results.
5. Does Fructose Consumption Cause Disease Progression in Humans?
5.1. Fructose and Hepatic Insulin Resistance
Hepatic lipid accumulation in the context of NAFLD is often associated with hepatic insulin resistance [126,127,128,129,130,131,132,133,134], and NAFLD is considered an important risk factor for type 2 diabetes [11]. Emerging evidence points to the accumulation of specific intrahepatic lipid species, most importantly diacylglycerol (DAG), as a cause of lipid-mediated insulin resistance. Increased hepatic DAG content activates protein kinase Cε (PKCε) in genetic or diet-induced obese animal models [135,136,137]. This results in its translocation from the cytosol to the cell membrane, where it phosphorylates insulin receptor threonine1160 and inhibits insulin receptor kinase activity/downstream signaling [138]. We have recently demonstrated that obese humans with hepatic insulin resistance are also characterized by intrahepatic DAG accumulation and PKCε activation/translocation [139], supporting the translational relevance of this mechanism of hepatic insulin resistance.
There is also preclinical evidence to suggest that fructose itself promotes hepatic DAG accumulation. Short-term high-fructose feeding to rodents increased hepatic DAG content [140,141,142] and was associated with PKCε activation and impaired insulin signaling [78]. In addition, fructose activates ChREBP and promotes hepatic gluconeogenesis independently of hepatic insulin signaling, which may contribute to hepatic insulin resistance (Figure 3) [58]. In support of these mechanisms linking fructose to hepatic insulin resistance, data from our recent systematic review and meta-analysis of diet-intervention trials in nondiabetic humans demonstrate that fructose consumption has more harmful effects on hepatic insulin sensitivity than the isocaloric consumption of glucose or other carbohydrates [25].
5.2. Fructose and NASH
Fructose metabolism has been suggested to induce hepatotoxic changes that contribute to disease severity in the context of NAFLD. Epidemiological studies have linked increased daily fructose intake to NASH in children and adolescents [143] as well as to increased hepatic fibrosis in adults [111]. It has been suggested that uric acid mediates some of the hepatotoxic effects of fructose. Ingested fructose is phosphorylated by hepatic KHK to produce fructose-1-phosphate (Figure 1). This reaction rapidly depletes intrahepatic adenosine triphosphate (ATP) levels and promotes adenosine monophosphate (AMP) production [144]. Elevated levels of AMP stimulate the production of uric acid, which is the final product of purine metabolism [145]. Uric acid, in turn, has been shown to induce intracellular oxidative stress [146], which is considered an important driver of progression to NASH [147]. Circulating uric acid levels are independently associated with NASH [143].
Short-term fructose-intervention trials are not designed to evaluate the effect of fructose on NASH directly, but some of these trials have studied the effect of fructose on serum uric acid levels. In one meta-analysis, short-term hypercaloric fructose supplementation increased circulating levels of uric acid [148]. Accordingly, daily fructose intake is predictive of uric acids levels in epidemiology [143], and a low-fructose diet was associated with a decrease in uric acid in overweight or obese individuals [149].
We also point out that hyperuricemia increases the risk for gout [150], the metabolic syndrome [151], and, possibly, cardiovascular mortality [152]. It may also contribute to insulin resistance by hindering endothelial function [153,154]. Consequently, while direct evidence linking fructose ingestion to increased liver fat in humans remains inconclusive, several lines of evidence, including preclinical, epidemiological, and interventional, support effects of fructose consumption on the development of hepatic insulin resistance, hyperuricemia, and NASH. This further underlines the potential of fructose avoidance for the prevention of NAFLD-associated diseases.
6. Conclusions
The scientific literature regarding the role of fructose consumption in the development of hepatic steatosis may seem somewhat inconsistent. On one hand, the available evidence from human epidemiological and interventional studies does not support the hypothesis that fructose, when consumed in isocaloric amounts, causes more liver fat accumulation than other energy-dense nutrients. The observed prosteatotic effect of fructose in hypercaloric trials [115] is likely confounded by associated weight gain [92], and this level of evidence is insufficient to adequately guide the public and policy makers on the use of dietary fructose vs. other products.
On the other hand, observations from numerous mechanistic studies in cells, animals, healthy volunteers, and patients clearly demonstrate that fructose has lipogenic potential. Hepatic fructose metabolism rapidly produces gluconeogenesis and lipogenesis precursors, while intermediary fructose metabolites also act as nutritional regulators of the major transcription factors that control these pathways. Accordingly, fructose ingestion increases plasma triglyceride levels [43,44,45,46,47], and high-fructose diets promote hepatic DNL [46,54,55]. Hepatic DNL is an important contributor to intrahepatic lipids in human NAFLD [18,19,20], suggesting that long-term fructose overconsumption may promote mechanisms that drive NAFLD development. Moreover, the overall evidence linking increased fructose intake to hepatic insulin resistance, increased uric acid concentrations, and NAFLD severity/progression is more convincing.
Finally, we are confident that a deeper understanding of the cellular mechanisms governing hepatic fructose metabolism will reveal novel targets for NAFLD/NASH, hypertriglyceridemia, and hepatic insulin resistance/type 2 diabetes.
Acknowledgments
No specific funding was received for the present study.
Appendix A. Literature Search and Selection Strategy
We searched for relevant peer-reviewed English-language publications in the MEDLINE (www.ncbi.nlm.nih.gov/pubmed), EMBASE (ovidsp.tx.ovid.com), and Cochrane Library (www.cochranelibrary.com) databases from inception through 26 June 2017. The literature search was focused on fructose, lipogenesis, NAFLD, NASH, and related terms. We manually reviewed reference lists of selected articles for additional publications. Entries identified through the search were screened for relevance, and full-text articles were retrieved for in-depth review and methodological quality assessment.
Appendix B. Recommended Further Reading
Mosca et al. [155] discussed the roll of soft drink consumption in pediatric metabolic disease. Rippe and Angelopoulos [156] evaluated recent observations from randomized controlled trials and meta-analyses into the effects of sugar consumption on important metabolic outcomes and health-related issues. Alwahsh and Gebhardt [157] approached the issue from different angles and highlight how fructose consumption may be related to inflammation, gut microbiota, and central nervous system mechanisms. Finally, Kahn and Sievenpiper [158] take the counterpoint stand and argue that there is no convincing evidence to implicate sugar in the development of obesity and its related diseases.
Author Contributions
K.W.t.H. drafted the manuscript; M.J.S. revised the manuscript.
Conflicts of Interest
K.W.t.H. and M.J.S. are supported by the European Union (grant FP7-EU 305707). M.J.S. received an unrestricted grant from Mediq TEFA. Previous or current sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
References
- 1.Zimmet P., Alberti K.G., Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001;414:782–787. doi: 10.1038/414782a. [DOI] [PubMed] [Google Scholar]
- 2.Ng M., Fleming T., Robinson M., Thomson B., Graetz N., Margono C., Mullany E.C., Biryukov S., Abbafati C., Abera S.F., et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the global burden of disease study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malnick S.D., Knobler H. The medical complications of obesity. QJM. 2006;99:565–579. doi: 10.1093/qjmed/hcl085. [DOI] [PubMed] [Google Scholar]
- 4.Global BMI Mortality Collaboration Body-mass index and all-cause mortality: Individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388:776–786. doi: 10.1016/S0140-6736(16)30175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu E., Ley S.H., Manson J.E., Willet W., Satija A., Hu F.B., Stokes A. Weight history and all-cause and cause-specific mortality in three prospective cohort studies. Ann. Intern. Med. 2017;166:613–620. doi: 10.7326/M16-1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chalasani N., Younossi Z., Lavine J.E., Diehl A.M., Brunt E.M., Cusi K., Charlton M., Sanyal A.J. The diagnosis and management of non-alcoholic fatty liver disease: Practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592–1609. doi: 10.1053/j.gastro.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 7.Szczepaniak L.S., Nurenberg P., Leonard D., Browning J.D., Reingold J.S., Grundy S., Hobbs H.H., Dobbins R.L. Magnetic resonance spectroscopy to measure hepatic triglyceride content: Prevalence of hepatic steatosis in the general population. Am. J. Physiol. Endocrinol. Metab. 2005;288:E462–E468. doi: 10.1152/ajpendo.00064.2004. [DOI] [PubMed] [Google Scholar]
- 8.Donhoffer H. Quantitative estimation of lipids in needle biopsy sized specimens of cadaver liver. Acta Med. Acad. Sci. Hung. 1974;31:47–49. [PubMed] [Google Scholar]
- 9.Petäjä E.M., Yki-Järvinen H. Definitions of normal liver fat and the association of insulin sensitivity with acquired and genetic nafld—A systematic review. Int. J. Mol. Sci. 2016;17:633. doi: 10.3390/ijms17050633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Younossi Z.M., Koenig A.B., Abdelatif D., Fazel Y., Henry L., Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 11.Anstee Q.M., Targher G., Day C.P. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat. Rev. Gastroenterol. Hepatol. 2013;10:330–344. doi: 10.1038/nrgastro.2013.41. [DOI] [PubMed] [Google Scholar]
- 12.McPherson S., Hardy T., Henderson E., Burt A.D., Day C.P., Anstee Q.M. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: Implications for prognosis and clinical management. J. Hepatol. 2015;62:1148–1155. doi: 10.1016/j.jhep.2014.11.034. [DOI] [PubMed] [Google Scholar]
- 13.Wong V.W., Wong G.L., Choi P.C., Chan A.W., Li M.K., Chan H.Y., Chim A.M., Yu J., Sung J.J., Chan H.L. Disease progression of non-alcoholic fatty liver disease: A prospective study with paired liver biopsies at 3 years. Gut. 2010;59:969–974. doi: 10.1136/gut.2009.205088. [DOI] [PubMed] [Google Scholar]
- 14.Pais R., Charlotte F., Fedchuk L., Bedossa P., Lebray P., Poynard T., Ratziu V. A systematic review of follow-up biopsies reveals disease progression in patients with non-alcoholic fatty liver. J. Hepatol. 2013;59:550–556. doi: 10.1016/j.jhep.2013.04.027. [DOI] [PubMed] [Google Scholar]
- 15.Wong R.J., Cheung R., Ahmed A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U.S. Hepatology. 2014;59:2188–2195. doi: 10.1002/hep.26986. [DOI] [PubMed] [Google Scholar]
- 16.Zezos P., Renner E.L. Liver transplantation and non-alcoholic fatty liver disease. World J. Gastroenterol. 2014;20:15532–15538. doi: 10.3748/wjg.v20.i42.15532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nassir F., Rector R.S., Hammoud G.M., Ibdah J.A. Pathogenesis and prevention of hepatic steatosis. Gastroenterol. Hepatol. 2015;11:167–175. [PMC free article] [PubMed] [Google Scholar]
- 18.Donnelly K.L., Smith C.I., Schwarzenberg S.J., Jessurun J., Boldt M.D., Parks E.J. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J. Clin. Investig. 2005;115:1343–1351. doi: 10.1172/JCI23621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lambert J.E., Ramos-Roman M.A., Browning J.D., Parks E.J. Increased de novo lipogenesis is a distinct characteristic of individuals with nonalcoholic fatty liver disease. Gastroenterology. 2014;146:726–735. doi: 10.1053/j.gastro.2013.11.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Softic S., Cohen D.E., Kahn C.R. Role of dietary fructose and hepatic de novo lipogenesis in fatty liver disease. Dig. Dis. Sci. 2016;61:1282–1293. doi: 10.1007/s10620-016-4054-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bray G.A. Soft drink consumption and obesity: It is all about fructose. Curr. Opin. Lipidol. 2010;21:51–57. doi: 10.1097/MOL.0b013e3283346ca2. [DOI] [PubMed] [Google Scholar]
- 22.Bray G.A., Nielsen S.J., Popkin B.M. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am. J. Clin. Nutr. 2004;79:537–543. doi: 10.1093/ajcn/79.4.537. [DOI] [PubMed] [Google Scholar]
- 23.Bray G.A., Popkin B.M. Dietary sugar and body weight: Have we reached a crisis in the epidemic of obesity and diabetes? Health be damned! Pour on the sugar. Diabetes Care. 2014;37:950–956. doi: 10.2337/dc13-2085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malik V.S., Popkin B.M., Bray G.A., Després J.P., Hu F.B. Sugar sweetened beverages, obesity, type 2 diabetes and cardiovascular disease risk. Circulation. 2010;121:1356–1364. doi: 10.1161/CIRCULATIONAHA.109.876185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ter Horst K.W., Schene M.R., Holman R., Romijn J.A., Serlie M.J. Effect of fructose consumption on insulin sensitivity in nondiabetic subjects: A systematic review and meta-analysis of diet-intervention trials. Am. J. Clin. Nutr. 2016;104:1562–1576. doi: 10.3945/ajcn.116.137786. [DOI] [PubMed] [Google Scholar]
- 26.Lim J.S., Mietus-Snyder M., Valente A., Schwarz J.-M., Lustig R.H. The role of fructose in the pathogenesis of NAFLD and the metabolic syndrome. Nat. Rev. Gastroenterol. Hepatol. 2010;7:251–264. doi: 10.1038/nrgastro.2010.41. [DOI] [PubMed] [Google Scholar]
- 27.Diraison F., Yankah V., Letexier D., Dusserre E., Jones P., Beylot M. Differences in the regulation of adipose tissue and liver lipogenesis by carbohydrates in humans. J. Lipid Res. 2003;44:846–853. doi: 10.1194/jlr.M200461-JLR200. [DOI] [PubMed] [Google Scholar]
- 28.Jones P.J. Tracing lipogenesis in humans using deuterated water. Can. J. Physiol. Pharmacol. 1996;74:755–760. doi: 10.1139/y96-070. [DOI] [PubMed] [Google Scholar]
- 29.Herman M.A., Samuel V.T. The sweet path to metabolic demise: Fructose and lipid synthesis. Trends Endocrinol. Metab. 2016;27:719–730. doi: 10.1016/j.tem.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mayes P.A. Intermediary metabolism of fructose. Am. J. Clin. Nutr. 1993;58:754s–765s. doi: 10.1093/ajcn/58.5.754S. [DOI] [PubMed] [Google Scholar]
- 31.Samuel V.T. Fructose induced lipogenesis: From sugar to fat to insulin resistance. Trends Endocrinol. Metab. 2011;22:60–65. doi: 10.1016/j.tem.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 32.Drozdowski L.A., Thomson A.B.R. Intestinal sugar transport. World J. Gastroenterol. 2006;12:1657–1670. doi: 10.3748/wjg.v12.i11.1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ebert K., Witt H. Fructose malabsorption. Mol. Cell. Pediatr. 2016;3:10. doi: 10.1186/s40348-016-0035-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barone S., Fussell S.L., Singh A.K., Lucas F., Xu J., Kim C., Wu X., Yu Y., Amlal H., Seidler U., et al. Slc2a5 (Glut5) is essential for the absorption of fructose in the intestine and generation of fructose-induced hypertension. J. Biol. Chem. 2009;284:5056–5066. doi: 10.1074/jbc.M808128200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Douard V., Ferraris R.P. Regulation of the fructose transporter Glut5 in health and disease. Am. J. Physiol. Endocrinol. Metab. 2008;295:E227–E237. doi: 10.1152/ajpendo.90245.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leturque A., Brot-Laroche E., Le Gall M., Stolarczyk E., Tobin V. The role of Glut2 in dietary sugar handling. J. Physiol. Biochem. 2005;61:529–537. doi: 10.1007/BF03168378. [DOI] [PubMed] [Google Scholar]
- 37.Debosch B.J., Chen Z., Saben J.L., Finck B.N., Moley K.H. Glucose transporter 8 (GLUT8) mediates fructose-induced de novo lipogenesis and macrosteatosis. J. Biol. Chem. 2014;289:10989–10998. doi: 10.1074/jbc.M113.527002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Karim S., Adams D.H., Lalor P.F. Hepatic expression and cellular distribution of the glucose transporter family. World J. Gastroenterol. 2012;18:6771–6781. doi: 10.3748/wjg.v18.i46.6771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sun S.Z., Empie M.W. Fructose metabolism in humans—What isotopic tracer studies tell us. Nutr. Metab. 2012;9:89. doi: 10.1186/1743-7075-9-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vos M.B., Lavine J.E. Dietary fructose in nonalcoholic fatty liver disease. Hepatology. 2013;57:2525–2531. doi: 10.1002/hep.26299. [DOI] [PubMed] [Google Scholar]
- 41.Tappy L., Le K.A. Metabolic effects of fructose and the worldwide increase in obesity. Physiol. Rev. 2010;90:23–46. doi: 10.1152/physrev.00019.2009. [DOI] [PubMed] [Google Scholar]
- 42.Iizuka K. The role of carbohydrate response element binding protein in intestinal and hepatic fructose metabolism. Nutrients. 2017;9:181. doi: 10.3390/nu9020181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dushay J., Toschi E., Mitten E.K., Fisher F.M., Herman M.A., Maratos-Flier E. Fructose ingestion acutely stimulates circulating FGF21 levels in humans. Mol. Metab. 2014;4:51–57. doi: 10.1016/j.molmet.2014.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Theytaz F., de Giorgi S., Hodson L., Stefanoni N., Rey V., Schneiter P., Giusti V., Tappy L. Metabolic fate of fructose ingested with and without glucose in a mixed meal. Nutrients. 2014;6:2632–2649. doi: 10.3390/nu6072632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chong M.F., Fielding B.A., Frayn K.N. Mechanisms for the acute effect of fructose on postprandial lipemia. Am. J. Clin. Nutr. 2007;85:1511–1520. doi: 10.1093/ajcn/85.6.1511. [DOI] [PubMed] [Google Scholar]
- 46.Parks E.J., Skokan L.E., Timlin M.T., Dingfelder C.S. Dietary sugars stimulate fatty acid synthesis in adults. J. Nutr. 2008;138:1039–1046. doi: 10.1093/jn/138.6.1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Teff K.L., Grudziak J., Townsend R.R., Dunn T.N., Grant R.W., Adams S.H., Keim N.L., Cummings B.P., Stanhope K.L., Havel P.J. Endocrine and metabolic effects of consuming fructose- and glucose-sweetened beverages with meals in obese men and women: Influence of insulin resistance on plasma triglyceride responses. J. Clin. Endocrinol. Metab. 2009;94:1562–1569. doi: 10.1210/jc.2008-2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kotronen A., Seppala-Lindroos A., Vehkavaara S., Bergholm R., Frayn K.N., Fielding B.A., Yki-Jarvinen H. Liver fat and lipid oxidation in humans. Liver Int. 2009;29:1439–1446. doi: 10.1111/j.1478-3231.2009.02076.x. [DOI] [PubMed] [Google Scholar]
- 49.Cassader M., Gambino R., Musso G., Depetris N., Mecca F., Cavallo-Perin P., Pacini G., Rizzetto M., Pagano G. Postprandial triglyceride-rich lipoprotein metabolism and insulin sensitivity in nonalcoholic steatohepatitis patients. Lipids. 2001;36:1117–1124. doi: 10.1007/s11745-001-0822-5. [DOI] [PubMed] [Google Scholar]
- 50.Boren J., Watts G.F., Adiels M., Soderlund S., Chan D.C., Hakkarainen A., Lundbom N., Matikainen N., Kahri J., Verges B., et al. Kinetic and related determinants of plasma triglyceride concentration in abdominal obesity: Multicenter tracer kinetic study. Arterioscler. Thromb. Vasc. Biol. 2015;35:2218–2224. doi: 10.1161/ATVBAHA.115.305614. [DOI] [PubMed] [Google Scholar]
- 51.Adiels M., Taskinen M.R., Packard C., Caslake M.J., Soro-Paavonen A., Westerbacka J., Vehkavaara S., Hakkinen A., Olofsson S.O., Yki-Jarvinen H., et al. Overproduction of large VLDL particles is driven by increased liver fat content in man. Diabetologia. 2006;49:755–765. doi: 10.1007/s00125-005-0125-z. [DOI] [PubMed] [Google Scholar]
- 52.Charlton M., Sreekumar R., Rasmussen D., Lindor K., Nair K.S. Apolipoprotein synthesis in nonalcoholic steatohepatitis. Hepatology. 2002;35:898–904. doi: 10.1053/jhep.2002.32527. [DOI] [PubMed] [Google Scholar]
- 53.Tran C., Jacot-Descombes D., Lecoultre V., Fielding B.A., Carrel G., Le K.A., Schneiter P., Bortolotti M., Frayn K.N., Tappy L. Sex differences in lipid and glucose kinetics after ingestion of an acute oral fructose load. Br. J. Nutr. 2010;104:1139–1147. doi: 10.1017/S000711451000190X. [DOI] [PubMed] [Google Scholar]
- 54.Faeh D., Minehira K., Schwarz J.M., Periasamy R., Park S., Tappy L. Effect of fructose overfeeding and fish oil administration on hepatic de novo lipogenesis and insulin sensitivity in healthy men. Diabetes. 2005;54:1907–1913. doi: 10.2337/diabetes.54.7.1907. [DOI] [PubMed] [Google Scholar]
- 55.Stanhope K.L., Schwarz J.M., Keim N.L., Griffen S.C., Bremer A.A., Graham J.L., Hatcher B., Cox C.L., Dyachenko A., Zhang W., et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J. Clin. Investig. 2009;119:1322–1334. doi: 10.1172/JCI37385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Iizuka K., Bruick R.K., Liang G., Horton J.D., Uyeda K. Deficiency of carbohydrate response element-binding protein (ChREBP) reduces lipogenesis as well as glycolysis. Proc. Natl. Acad. Sci. USA. 2004;101:7281–7286. doi: 10.1073/pnas.0401516101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Iizuka K., Horikawa Y. ChREBP: A glucose-activated transcription factor involved in the development of metabolic syndrome. Endocr. J. 2008;55:617–624. doi: 10.1507/endocrj.K07E-110. [DOI] [PubMed] [Google Scholar]
- 58.Kim M.S., Krawczyk S.A., Doridot L., Fowler A.J., Wang J.X., Trauger S.A., Noh H.L., Kang H.J., Meissen J.K., Blatnik M., et al. ChREBP regulates fructose-induced glucose production independently of insulin signaling. J. Clin. Investig. 2016;126:4372–4386. doi: 10.1172/JCI81993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Li M.V., Chang B., Imamura M., Poungvarin N., Chan L. Glucose-dependent transcriptional regulation by an evolutionarily conserved glucose-sensing module. Diabetes. 2006;55:1179–1189. doi: 10.2337/db05-0822. [DOI] [PubMed] [Google Scholar]
- 60.Herman M.A., Peroni O.D., Villoria J., Schön M.R., Abumrad N.A., Blüher M., Klein S., Kahn B.B. A novel ChREBP isoform in adipose tissue regulates systemic glucose metabolism. Nature. 2012;484:333–338. doi: 10.1038/nature10986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Iizuka K. The transcription factor carbohydrate-response element-binding protein (ChREBP): A possible link between metabolic disease and cancer. Biochim. Biophys. Acta. 2017;1863:474–485. doi: 10.1016/j.bbadis.2016.11.029. [DOI] [PubMed] [Google Scholar]
- 62.Li M.V., Chen W., Harmancey R.N., Nuotio-Antar A.M., Imamura M., Saha P., Taegtmeyer H., Chan L. Glucose-6-phosphate mediates activation of the carbohydrate responsive binding protein (ChREBP) Biochem. Biophys. Res. Commun. 2010;395:395–400. doi: 10.1016/j.bbrc.2010.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Arden C., Tudhope S.J., Petrie J.L., Al-Oanzi Z.H., Cullen K.S., Lange A.J., Towle H.C., Agius L. Fructose-2,6-bisphosphate is essential for glucose-regulated gene transcription of glucose-6-phosphatase and other ChREBP target genes in hepatocytes. Biochem. J. 2012;443:111–123. doi: 10.1042/BJ20111280. [DOI] [PubMed] [Google Scholar]
- 64.Kabashima T., Kawaguchi T., Wadzinski B.E., Uyeda K. Xylulose-5-phosphate mediates glucose-induced lipogenesis by xylulose-5-phosphate-activated protein phosphatase in rat liver. Proc. Natl. Acad. Sci. USA. 2003;100:5107–5112. doi: 10.1073/pnas.0730817100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Koo H.Y., Miyashita M., Cho B.H., Nakamura M.T. Replacing dietary glucose with fructose increases ChREBP activity and SREBP-1 protein in rat liver nucleus. Biochem. Biophys. Res. Commun. 2009;390:285–289. doi: 10.1016/j.bbrc.2009.09.109. [DOI] [PubMed] [Google Scholar]
- 66.Fisher F.M., Kim M., Doridot L., Cunniff J.C., Parker T.S., Levine D.M., Hellerstein M.K., Hudgins L.C., Maratos-Flier E., Herman M.A. A critical role for ChREBP-mediated FGF21 secretion in hepatic fructose metabolism. Mol. Metab. 2017;6:14–21. doi: 10.1016/j.molmet.2016.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.ter Horst K.W., Gilijamse P.W., Demirkiran A., van Wagensveld B.A., Ackermans M.T., Verheij J., Romijn J.A., Nieuwdorp M., Maratos-Flier E., Herman M.A., et al. The FGF21 response to fructose predicts metabolic health and persists after bariatric surgery in obese humans. Mol. Metab. 2017 doi: 10.1016/j.molmet.2017.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang D., Tong X., VanDommelen K., Gupta N., Stamper K., Brady G.F., Meng Z., Lin J., Rui L., Omary M.B., et al. Lipogenic transcription factor ChREBP mediates fructose-induced metabolic adaptations to prevent hepatotoxicity. J. Clin. Investig. 2017;127:2855–2867. doi: 10.1172/JCI89934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hall A.M., Finck B.N. ChREBP refines the hepatic response to fructose to protect the liver from injury. J. Clin. Investig. 2017;127:2533–2535. doi: 10.1172/JCI95008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Eissing L., Scherer T., Tödter K., Knippschild U., Greve J.W., Buurman W.A., Pinnschmidt H.O., Rensen S.S., Wolf A.M., Bartelt A., et al. De novo lipogenesis in human fat and liver is linked to ChREBP-β and metabolic health. Nat. Commun. 2013;4:1528. doi: 10.1038/ncomms2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Aragno M., Tomasinelli C.E., Vercellinatto I., Catalano M.G., Collino M., Fantozzi R., Danni O., Boccuzzi G. SREBP-1c in nonalcoholic fatty liver disease induced by western-type high-fat diet plus fructose in rats. Free Radic. Biol. Med. 2009;47:1067–1074. doi: 10.1016/j.freeradbiomed.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 72.Bezerra R.M., Ueno M., Silva M.S., Tavares D.Q., Carvalho C.R., Saad M.J., Gontijo J.A. A high-fructose diet induces insulin resistance but not blood pressure changes in normotensive rats. Braz. J. Med. Biol. Res. 2001;34:1155–1160. doi: 10.1590/S0100-879X2001000900008. [DOI] [PubMed] [Google Scholar]
- 73.Martinez F.J., Rizza R.A., Romero J.C. High-fructose feeding elicits insulin resistance, hyperinsulinism, and hypertension in normal mongrel dogs. Hypertension. 1994;23:456–463. doi: 10.1161/01.HYP.23.4.456. [DOI] [PubMed] [Google Scholar]
- 74.Tran L.T., Yuen V.G., McNeill J.H. The fructose-fed rat: A review on the mechanisms of fructose-induced insulin resistance and hypertension. Mol. Cell. Biochem. 2009;332:145–159. doi: 10.1007/s11010-009-0184-4. [DOI] [PubMed] [Google Scholar]
- 75.Matsuzaka T., Shimano H., Yahagi N., Amemiya-Kudo M., Okazaki H., Tamura Y., Iizuka Y., Ohashi K., Tomita S., Sekiya M., et al. Insulin-independent induction of sterol regulatory element-binding protein-1c expression in the livers of streptozotocin-treated mice. Diabetes. 2004;53:560–569. doi: 10.2337/diabetes.53.3.560. [DOI] [PubMed] [Google Scholar]
- 76.Miyazaki M., Dobrzyn A., Man W.C., Chu K., Sampath H., Kim H.J., Ntambi J.M. Stearoyl-CoA desaturase 1 gene expression is necessary for fructose-mediated induction of lipogenic gene expression by sterol regulatory element-binding protein-1c-dependent and -independent mechanisms. J. Biol. Chem. 2004;279:25164–25171. doi: 10.1074/jbc.M402781200. [DOI] [PubMed] [Google Scholar]
- 77.Bindesboll C., Fan Q., Norgaard R.C., MacPherson L., Ruan H.B., Wu J., Pedersen T.A., Steffensen K.R., Yang X., Matthews J., et al. Liver X receptor regulates hepatic nuclear o-glcnac signaling and carbohydrate responsive element-binding protein activity. J. Lipid Res. 2015;56:771–785. doi: 10.1194/jlr.M049130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nagai Y., Yonemitsu S., Erion D.M., Iwasaki T., Stark R., Weismann D., Dong J., Zhang D., Jurczak M.J., Loffler M.G., et al. The role of peroxisome proliferator-activated receptor gamma coactivator-1 beta in the pathogenesis of fructose-induced insulin resistance. Cell Metab. 2009;9:252–264. doi: 10.1016/j.cmet.2009.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tappy L., Randin J.P., Felber J.P., Chiolero R., Simonson D.C., Jequier E., DeFronzo R.A. Comparison of thermogenic effect of fructose and glucose in normal humans. Am. J. Physiol. 1986;250:E718–E724. doi: 10.1152/ajpendo.1986.250.6.E718. [DOI] [PubMed] [Google Scholar]
- 80.Rizkalla S.W., Luo J., Guilhem I., Boillot J., Bruzzo F., Chevalier A., Slama G. Comparative effects of 6 week fructose, dextrose and starch feeding on fat-cell lipolysis in normal rats: Effects of isoproterenol, theophylline and insulin. Mol. Cell. Biochem. 1992;109:127–132. doi: 10.1007/BF00229766. [DOI] [PubMed] [Google Scholar]
- 81.Abdel-Sayed A., Binnert C., Le K.A., Bortolotti M., Schneiter P., Tappy L. A high-fructose diet impairs basal and stress-mediated lipid metabolism in healthy male subjects. Br. J. Nutr. 2008;100:393–399. doi: 10.1017/S000711450789547X. [DOI] [PubMed] [Google Scholar]
- 82.Lafontan M., Langin D. Lipolysis and lipid mobilization in human adipose tissue. Prog. Lipid Res. 2009;48:275–297. doi: 10.1016/j.plipres.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 83.Perry R.J., Camporez J.P., Kursawe R., Titchenell P.M., Zhang D., Perry C.J., Jurczak M.J., Abudukadier A., Han M.S., Zhang X.M., et al. Hepatic acetyl CoA links adipose tissue inflammation to hepatic insulin resistance and type 2 diabetes. Cell. 2015;160:745–758. doi: 10.1016/j.cell.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sondergaard E., Jensen M.D. Quantification of adipose tissue insulin sensitivity. J. Investig. Med. 2016;64:989–991. doi: 10.1136/jim-2016-000098. [DOI] [PubMed] [Google Scholar]
- 85.Boren J., Taskinen M.R., Olofsson S.O., Levin M. Ectopic lipid storage and insulin resistance: A harmful relationship. J. Int. Med. 2013;274:25–40. doi: 10.1111/joim.12071. [DOI] [PubMed] [Google Scholar]
- 86.ter Horst K.W., van Galen K.A., Gilijamse P.W., Hartstra A.V., de Groot P.F., van der Valk F.M., Ackermans M.T., Nieuwdorp M., Romijn J.A., Serlie M.J. Methods for quantifying adipose tissue insulin resistance in overweight/obese humans. Int. J. Obes. 2017;41:1288–1294. doi: 10.1038/ijo.2017.110. [DOI] [PubMed] [Google Scholar]
- 87.Jensen M.D., Haymond M.W., Rizza R.A., Cryer P.E., Miles J.M. Influence of body fat distribution on free fatty acid metabolism in obesity. J. Clin. Investig. 1989;83:1168–1173. doi: 10.1172/JCI113997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Baena M., Sangüesa G., Dávalos A., Latasa M.-J., Sala-Vila A., Sánchez R.M., Roglans N., Laguna J.C., Alegret M. Fructose, but not glucose, impairs insulin signaling in the three major insulin-sensitive tissues. Sci. Rep. 2016;6:26149. doi: 10.1038/srep26149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Vrana A., Fabry P., Slabochova Z., Kazdova L. Effect of dietary fructose on free fatty acid release from adipose tissue and serum free fatty acid concentration in the rat. Nutr. Metab. 1974;17:74–83. [PubMed] [Google Scholar]
- 90.Ma J., Sloan M., Fox C.S., Hoffmann U., Smith C.E., Saltzman E., Rogers G.T., Jacques P.F., McKeown N.M. Sugar-sweetened beverage consumption is associated with abdominal fat partitioning in healthy adults. J. Nutr. 2014;144:1283–1290. doi: 10.3945/jn.113.188599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ma J., Fox C., Speliotes E., Hoffmann U., Smith C., Saltzman E., Jacques P., McKeown N. Sugar-sweetened beverage intake is associated with fatty liver in the Framingham offspring study. J. Hepatol. 2015;63:462–469. doi: 10.1016/j.jhep.2015.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sievenpiper J.L., de Souza R.J., Mirrahimi A., Yu M.E., Carleton A.J., Beyene J., Chiavaroli L., Di Buono M., Jenkins A.L., Leiter L.A., et al. Effect of fructose on body weight in controlled feeding trials: A systematic review and meta-analysis. Ann. Intern. Med. 2012;156:291–304. doi: 10.7326/0003-4819-156-4-201202210-00007. [DOI] [PubMed] [Google Scholar]
- 93.Sullivan S. Implications of diet on nonalcoholic fatty liver disease. Curr. Opin. Gastroenterol. 2010;26:160–164. doi: 10.1097/MOG.0b013e3283358a58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bjornson E., Adiels M., Taskinen M.R., Boren J. Kinetics of plasma triglycerides in abdominal obesity. Curr. Opin. Lipidol. 2017;28:11–18. doi: 10.1097/MOL.0000000000000375. [DOI] [PubMed] [Google Scholar]
- 95.Parks E.J., Hellerstein M.K. Thematic review series: Patient-oriented research. Recent advances in liver triacylglycerol and fatty acid metabolism using stable isotope labeling techniques. J. Lipid Res. 2006;47:1651–1660. doi: 10.1194/jlr.R600018-JLR200. [DOI] [PubMed] [Google Scholar]
- 96.Barrows B.R., Parks E.J. Contributions of different fatty acid sources to very low-density lipoprotein-triacylglycerol in the fasted and fed states. J. Clin. Endocrinol. Metab. 2006;91:1446–1452. doi: 10.1210/jc.2005-1709. [DOI] [PubMed] [Google Scholar]
- 97.Nemes K., Aberg F. Interpreting lipoproteins in nonalcoholic fatty liver disease. Curr. Opin. Lipidol. 2017;28:355–360. doi: 10.1097/MOL.0000000000000427. [DOI] [PubMed] [Google Scholar]
- 98.David Wang D., Sievenpiper J.L., de Souza R.J., Cozma A.I., Chiavaroli L., Ha V., Mirrahimi A., Carleton A.J., Di Buono M., Jenkins A.L., et al. Effect of fructose on postprandial triglycerides: A systematic review and meta-analysis of controlled feeding trials. Atherosclerosis. 2014;232:125–133. doi: 10.1016/j.atherosclerosis.2013.10.019. [DOI] [PubMed] [Google Scholar]
- 99.Sievenpiper J.L., Carleton A.J., Chatha S., Jiang H.Y., de Souza R.J., Beyene J., Kendall C.W., Jenkins D.J. Heterogeneous effects of fructose on blood lipids in individuals with type 2 diabetes: Systematic review and meta-analysis of experimental trials in humans. Diabetes Care. 2009;32:1930–1937. doi: 10.2337/dc09-0619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Stanhope K.L., Havel P.J. Fructose consumption: Potential mechanisms for its effects to increase visceral adiposity and induce dyslipidemia and insulin resistance. Curr. Opin. Lipidol. 2008;19:16–24. doi: 10.1097/MOL.0b013e3282f2b24a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dong B., Singh A.B., Azhar S., Seidah N.G., Liu J. High-fructose feeding promotes accelerated degradation of hepatic LDL receptor and hypercholesterolemia in hamsters via elevated circulating Pcsk9 levels. Atherosclerosis. 2015;239:364–374. doi: 10.1016/j.atherosclerosis.2015.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Campos V.C., Tappy L. Physiological handling of dietary fructose-containing sugars: Implications for health. Int. J. Obes. 2016;40(Suppl. 1):S6–S11. doi: 10.1038/ijo.2016.8. [DOI] [PubMed] [Google Scholar]
- 103.Topping D.L., Mayes P.A. The immediate effects of insulin and fructose on the metabolism of the perfused liver. Changes in lipoprotein secretion, fatty acid oxidation and esterification, lipogenesis and carbohydrate metabolism. Biochem. J. 1972;126:295–311. doi: 10.1042/bj1260295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Prager G.N., Ontko J.A. Direct effects of fructose metabolism on fatty acid oxidation in a recombined rat liver mitochondria-hish speed supernatant system. Biochim. Biophys. Acta. 1976;424:386–395. doi: 10.1016/0005-2760(76)90028-X. [DOI] [PubMed] [Google Scholar]
- 105.Koo S.H. Nonalcoholic fatty liver disease: Molecular mechanisms for the hepatic steatosis. Clin. Mol. Hepatol. 2013;19:210–215. doi: 10.3350/cmh.2013.19.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Stanhope K.L., Havel P.J. Fructose consumption: Recent results and their potential implications. Ann. N. Y. Acad. Sci. 2010;1190:15–24. doi: 10.1111/j.1749-6632.2009.05266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Pan M., Cederbaum A.I., Zhang Y.L., Ginsberg H.N., Williams K.J., Fisher E.A. Lipid peroxidation and oxidant stress regulate hepatic apolipoprotein B degradation and VLDL production. J. Clin. Investig. 2004;113:1277–1287. doi: 10.1172/JCI19197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Marriott B.P., Cole N., Lee E. National estimates of dietary fructose intake increased from 1977 to 2004 in the United States. J. Nutr. 2009;139:1228s–1235s. doi: 10.3945/jn.108.098277. [DOI] [PubMed] [Google Scholar]
- 109.Ouyang X., Cirillo P., Sautin Y., McCall S., Bruchette J.L., Diehl A.M., Johnson R.J., Abdelmalek M.F. Fructose consumption as a risk factor for non-alcoholic fatty liver disease. J. Hepatol. 2008;48:993–999. doi: 10.1016/j.jhep.2008.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kanerva N., Sandboge S., Kaartinen N.E., Mannisto S., Eriksson J.G. Higher fructose intake is inversely associated with risk of nonalcoholic fatty liver disease in older Finnish adults. Am. J. Clin. Nutr. 2014;100:1133–1138. doi: 10.3945/ajcn.114.086074. [DOI] [PubMed] [Google Scholar]
- 111.Abdelmalek M.F., Suzuki A., Guy C., Unalp-Arida A., Colvin R., Johnson R.J., Diehl A.M. Increased fructose consumption is associated with fibrosis severity in patients with NAFLD. Hepatology. 2010;51:1961–1971. doi: 10.1002/hep.23535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chung M., Ma J., Patel K., Berger S., Lau J., Lichtenstein A.H. Fructose, high-fructose corn syrup, sucrose, and nonalcoholic fatty liver disease or indexes of liver health: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2014;100:833–849. doi: 10.3945/ajcn.114.086314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Te Morenga L., Mallard S., Mann J. Dietary sugars and body weight: Systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ. 2012;346:e7492. doi: 10.1136/bmj.e7492. [DOI] [PubMed] [Google Scholar]
- 114.Tappy L., Le K.A. Health effects of fructose and fructose-containing caloric sweeteners: Where do we stand 10 years after the initial whistle blowings? Curr. Diabetes Rep. 2015;15:627. doi: 10.1007/s11892-015-0627-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Chiu S., Sievenpiper J.L., de Souza R.J., Cozma A.I., Mirrahimi A., Carleton A.J., Ha V., Di Buono M., Jenkins A.L., Leiter L.A., et al. Effect of fructose on markers of non-alcoholic fatty liver disease (NAFLD): A systematic review and meta-analysis of controlled feeding trials. Eur. J. Clin. Nutr. 2014;68:416–423. doi: 10.1038/ejcn.2014.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Schwarz J.M., Noworolski S.M., Wen M.J., Dyachenko A., Prior J.L., Weinberg M.E., Herraiz L.A., Tai V.W., Bergeron N., Bersot T.P., et al. Effect of a high-fructose weight-maintaining diet on lipogenesis and liver fat. J. Clin. Endocrinol. Metab. 2015;100:2434–2442. doi: 10.1210/jc.2014-3678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Agebratt C., Strom E., Romu T., Dahlqvist-Leinhard O., Borga M., Leandersson P., Nystrom F.H. A randomized study of the effects of additional fruit and nuts consumption on hepatic fat content, cardiovascular risk factors and basal metabolic rate. PLoS ONE. 2016;11:e0147149. doi: 10.1371/journal.pone.0147149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Munteanu M.A., Nagy G.A., Mircea P.A. Current management of NAFLD. Clujul Med. 2016;89:19–23. doi: 10.15386/cjmed-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Woods A., Williams J.R., Muckett P.J., Mayer F.V., Liljevald M., Bohlooly Y.M., Carling D. Liver-specific activation of AMPK prevents steatosis on a high-fructose diet. Cell Rep. 2017;18:3043–3051. doi: 10.1016/j.celrep.2017.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Han S.J., Choi S.E., Yi S.A., Jung J.G., Jung I.R., Shin M., Kang S., Oh H., Kim H.J., Kim D.J., et al. Glutamate dehydrogenase activator BCH stimulating reductive amination prevents high fat/high fructose diet-induced steatohepatitis and hyperglycemia in C57Bl/6J mice. Sci. Rep. 2016;5:37468. doi: 10.1038/srep37468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jegatheesan P., De Bandt J.P. Fructose and NAFLD: The multifaceted aspects of fructose metabolism. Nutrients. 2017;9:230. doi: 10.3390/nu9030230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Volynets V., Machann J., Kuper M.A., Maier I.B., Spruss A., Konigsrainer A., Bischoff S.C., Bergheim I. A moderate weight reduction through dietary intervention decreases hepatic fat content in patients with non-alcoholic fatty liver disease (NAFLD): A pilot study. Eur. J. Nutr. 2013;52:527–535. doi: 10.1007/s00394-012-0355-z. [DOI] [PubMed] [Google Scholar]
- 123.Schwarz J.M., Noworolski S.M., Erkin-Cakmak A., Korn N.J., Wen M.J., Tai V.W., Jones G.M., Palii S.P., Velasco-Alin M., Pan K., et al. Effects of dietary fructose restriction on liver fat, de novo lipogenesis, and insulin kinetics in children with obesity. Gastroenterology. 2017 doi: 10.1053/j.gastro.2017.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Vos M.B., Weber M.B., Welsh J., Khatoon F., Jones D.P., Whitington P.F., McClain C.J. Fructose and oxidized low-density lipoprotein in pediatric nonalcoholic fatty liver disease: A pilot study. Arch. Pediatr. Adolesc. Med. 2009;163:674–675. doi: 10.1001/archpediatrics.2009.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Haghighatdoost F., Salehi-Abargouei A., Surkan P.J., Azadbakht L. The effects of low carbohydrate diets on liver function tests in nonalcoholic fatty liver disease: A systematic review and meta-analysis of clinical trials. J. Res. Med. Sci. 2016;21:53. doi: 10.4103/1735-1995.187269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Sanyal A.J., Campbell-Sargent C., Mirshahi F., Rizzo W.B., Contos M.J., Sterling R.K., Luketic V.A., Shiffman M.L., Clore J.N. Nonalcoholic steatohepatitis: Association of insulin resistance and mitochondrial abnormalities. Gastroenterology. 2001;120:1183–1192. doi: 10.1053/gast.2001.23256. [DOI] [PubMed] [Google Scholar]
- 127.Seppala-Lindroos A., Vehkavaara S., Hakkinen A.M., Goto T., Westerbacka J., Sovijarvi A., Halavaara J., Yki-Jarvinen H. Fat accumulation in the liver is associated with defects in insulin suppression of glucose production and serum free fatty acids independent of obesity in normal men. J. Clin. Endocrinol. Metab. 2002;87:3023–3028. doi: 10.1210/jcem.87.7.8638. [DOI] [PubMed] [Google Scholar]
- 128.Petersen K.F., Oral E.A., Dufour S., Befroy D., Ariyan C., Yu C., Cline G.W., DePaoli A.M., Taylor S.I., Gorden P., et al. Leptin reverses insulin resistance and hepatic steatosis in patients with severe lipodystrophy. J. Clin. Investig. 2002;109:1345–1350. doi: 10.1172/JCI0215001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Petersen K.F., Dufour S., Befroy D., Lehrke M., Hendler R.E., Shulman G.I. Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes. Diabetes. 2005;54:603–608. doi: 10.2337/diabetes.54.3.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Bugianesi E., Gastaldelli A., Vanni E., Gambino R., Cassader M., Baldi S., Ponti V., Pagano G., Ferrannini E., Rizzetto M. Insulin resistance in non-diabetic patients with non-alcoholic fatty liver disease: Sites and mechanisms. Diabetologia. 2005;48:634–642. doi: 10.1007/s00125-005-1682-x. [DOI] [PubMed] [Google Scholar]
- 131.Gastaldelli A., Cusi K., Pettiti M., Hardies J., Miyazaki Y., Berria R., Buzzigoli E., Sironi A.M., Cersosimo E., Ferrannini E., et al. Relationship between hepatic/visceral fat and hepatic insulin resistance in nondiabetic and type 2 diabetic subjects. Gastroenterology. 2007;133:496–506. doi: 10.1053/j.gastro.2007.04.068. [DOI] [PubMed] [Google Scholar]
- 132.Deivanayagam S., Mohammed B.S., Vitola B.E., Naguib G.H., Keshen T.H., Kirk E.P., Klein S. Nonalcoholic fatty liver disease is associated with hepatic and skeletal muscle insulin resistance in overweight adolescents. Am. J. Clin. Nutr. 2008;88:257–262. doi: 10.1093/ajcn/88.2.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kotronen A., Juurinen L., Tiikkainen M., Vehkavaara S., Yki-Jarvinen H. Increased liver fat, impaired insulin clearance, and hepatic and adipose tissue insulin resistance in type 2 diabetes. Gastroenterology. 2008;135:122–130. doi: 10.1053/j.gastro.2008.03.021. [DOI] [PubMed] [Google Scholar]
- 134.Korenblat K.M., Fabbrini E., Mohammed B.S., Klein S. Liver, muscle, and adipose tissue insulin action is directly related to intrahepatic triglyceride content in obese subjects. Gastroenterology. 2008;134:1369–1375. doi: 10.1053/j.gastro.2008.01.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Jornayvaz F.R., Birkenfeld A.L., Jurczak M.J., Kanda S., Guigni B.A., Jiang D.C., Zhang D., Lee H.Y., Samuel V.T., Shulman G.I. Hepatic insulin resistance in mice with hepatic overexpression of diacylglycerol acyltransferase 2. Proc. Natl. Acad. Sci. USA. 2011;108:5748–5752. doi: 10.1073/pnas.1103451108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Samuel V.T., Liu Z.X., Qu X., Elder B.D., Bilz S., Befroy D., Romanelli A.J., Shulman G.I. Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease. J. Biol. Chem. 2004;279:32345–32353. doi: 10.1074/jbc.M313478200. [DOI] [PubMed] [Google Scholar]
- 137.Samuel V.T., Liu Z.X., Wang A., Beddow S.A., Geisler J.G., Kahn M., Zhang X.M., Monia B.P., Bhanot S., Shulman G.I. Inhibition of protein kinase Cepsilon prevents hepatic insulin resistance in nonalcoholic fatty liver disease. J. Clin. Investig. 2007;117:739–745. doi: 10.1172/JCI30400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Petersen M.C., Madiraju A.K., Gassaway B.M., Marcel M., Nasiri A.R., Butrico G., Marcucci M.J., Zhang D., Abulizi A., Zhang X.M., et al. Insulin receptor Thr1160 phosphorylation mediates lipid-induced hepatic insulin resistance. J. Clin. Investig. 2016;126:4361–4371. doi: 10.1172/JCI86013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.ter Horst K.W., Gilijamse P.W., Versteeg R.I., Ackermans M.T., Nederveen A.J., la Fleur S.E., Romijn J.A., Nieuwdorp M., Zhang D., Samuel V.T., et al. Hepatic diacylglycerol-associated protein kinase cε translocation links hepatic steatosis to hepatic insulin resistance in humans. Cell Rep. 2017;19:1997–2004. doi: 10.1016/j.celrep.2017.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Chan S.M., Sun R.Q., Zeng X.Y., Choong Z.H., Wang H., Watt M.J., Ye J.M. Activation of PPARalpha ameliorates hepatic insulin resistance and steatosis in high fructose-fed mice despite increased endoplasmic reticulum stress. Diabetes. 2013;62:2095–2105. doi: 10.2337/db12-1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Jurczak M.J., Lee A.H., Jornayvaz F.R., Lee H.Y., Birkenfeld A.L., Guigni B.A., Kahn M., Samuel V.T., Glimcher L.H., Shulman G.I. Dissociation of inositol-requiring enzyme (IRE1alpha)-mediated C-jun n-terminal kinase activation from hepatic insulin resistance in conditional x-box-binding protein-1 (XPB1) knock-out mice. J. Biol. Chem. 2012;287:2558–2567. doi: 10.1074/jbc.M111.316760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kopf T., Schaefer H.L., Troetzmueller M., Koefeler H., Broenstrup M., Konovalova T., Schmitz G. Influence of fenofibrate treatment on triacylglycerides, diacylglycerides and fatty acids in fructose fed rats. PLoS ONE. 2014;9:e106849. doi: 10.1371/journal.pone.0106849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Mosca A., Nobili V., De Vito R., Crudele A., Scorletti E., Villani A., Alisi A., Byrne C.D. Serum uric acid concentrations and fructose consumption are independently associated with nash in children and adolescents. J. Hepatol. 2017;66:1031–1036. doi: 10.1016/j.jhep.2016.12.025. [DOI] [PubMed] [Google Scholar]
- 144.Caliceti C., Calabria D., Roda A., Cicero A.F.G. Fructose intake, serum uric acid, and cardiometabolic disorders: A critical review. Nutrients. 2017;9:395. doi: 10.3390/nu9040395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Johnson R.J., Sautin Y.Y., Oliver W.J., Roncal C., Mu W., Gabriela Sanchez-Lozada L., Rodriguez-Iturbe B., Nakagawa T., Benner S.A. Lessons from comparative physiology: Could uric acid represent a physiologic alarm signal gone awry in western society? J. Comp. Physiol. B. 2009;179:67–76. doi: 10.1007/s00360-008-0291-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kang D.H., Park S.K., Lee I.K., Johnson R.J. Uric acid-induced C-reactive protein expression: Implication on cell proliferation and nitric oxide production of human vascular cells. J. Am. Soc. Nephrol. 2005;16:3553–3562. doi: 10.1681/ASN.2005050572. [DOI] [PubMed] [Google Scholar]
- 147.Takaki A., Kawai D., Yamamoto K. Multiple hits, including oxidative stress, as pathogenesis and treatment target in non-alcoholic steatohepatitis (NASH) Int. J. Mol. Sci. 2013;14:20704–20728. doi: 10.3390/ijms141020704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Wang D.D., Sievenpiper J.L., de Souza R.J., Chiavaroli L., Ha V., Cozma A.I., Mirrahimi A., Yu M.E., Carleton A.J., Di Buono M., et al. The effects of fructose intake on serum uric acid vary among controlled dietary trials. J. Nutr. 2012;142:916–923. doi: 10.3945/jn.111.151951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Madero M., Arriaga J.C., Jalal D., Rivard C., McFann K., Perez-Mendez O., Vazquez A., Ruiz A., Lanaspa M.A., Jimenez C.R., et al. The effect of two energy-restricted diets, a low-fructose diet versus a moderate natural fructose diet, on weight loss and metabolic syndrome parameters: A randomized controlled trial. Metabolism. 2011;60:1551–1559. doi: 10.1016/j.metabol.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 150.Zamudio-Cuevas Y., Hernandez-Diaz C., Pineda C., Reginato A.M., Cerna-Cortes J.F., Ventura-Rios L., Lopez-Reyes A. Molecular basis of oxidative stress in gouty arthropathy. Clin. Rheumatol. 2015;34:1667–1672. doi: 10.1007/s10067-015-2933-y. [DOI] [PubMed] [Google Scholar]
- 151.Nakagawa T., Hu H., Zharikov S., Tuttle K.R., Short R.A., Glushakova O., Ouyang X., Feig D.I., Block E.R., Herrera-Acosta J., et al. A causal role for uric acid in fructose-induced metabolic syndrome. Am. J. Physiol. Ren. Physiol. 2006;290:F625–F631. doi: 10.1152/ajprenal.00140.2005. [DOI] [PubMed] [Google Scholar]
- 152.Stack A.G., Hanley A., Casserly L.F., Cronin C.J., Abdalla A.A., Kiernan T.J., Murthy B.V., Hegarty A., Hannigan A., Nguyen H.T. Independent and conjoint associations of gout and hyperuricaemia with total and cardiovascular mortality. QJM. 2013;106:647–658. doi: 10.1093/qjmed/hct083. [DOI] [PubMed] [Google Scholar]
- 153.Cui Y., Bu H., Ma X., Zhao S., Li X., Lu S. The relation between serum uric acid and HbA1c is dependent upon hyperinsulinemia in patients with newly diagnosed type 2 diabetes mellitus. J. Diabetes Res. 2016;2016:7184123. doi: 10.1155/2016/7184123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Moulin S., Seematter G., Seyssel K. Fructose use in clinical nutrition: Metabolic effects and potential consequences. Curr. Opin. Clin. Nutr. Metab. Care. 2017;20:272–278. doi: 10.1097/MCO.0000000000000376. [DOI] [PubMed] [Google Scholar]
- 155.Mosca A., Della Corte C., Sartorelli M.R., Ferretti F., Nicita F., Vania A., Nobili V. Beverage consumption and paediatric NAFLD. Eat. Weight Disord. 2016;21:581–588. doi: 10.1007/s40519-016-0315-3. [DOI] [PubMed] [Google Scholar]
- 156.Rippe J.M., Angelopoulos T.J. Sugars, obesity, and cardiovascular disease: Results from recent randomized control trials. Eur. J. Nutr. 2016;55:45–53. doi: 10.1007/s00394-016-1257-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Alwahsh S.M., Gebhardt R. Dietary fructose as a risk factor for non-alcoholic fatty liver disease (NAFLD) Arch. Toxicol. 2017;91:1545–1563. doi: 10.1007/s00204-016-1892-7. [DOI] [PubMed] [Google Scholar]
- 158.Kahn R., Sievenpiper J.L. Dietary sugar and body weight: Have we reached a crisis in the epidemic of obesity and diabetes? We have, but the pox on sugar is overwrought and overworked. Diabetes Care. 2014;37:957–962. doi: 10.2337/dc13-2506. [DOI] [PubMed] [Google Scholar]