Abstract
Introduction
Though the WHO Framework Convention for Tobacco Control (FCTC) calls for the implementation of large graphic warning labels (GWLs) on cigarette boxes, the courts have blocked the implementation of 50% labels in the United States. We conducted an experiment to explore whether changing the size of GWLs is associated with changes in visual attention, negative affect, risk beliefs, and behavioral intentions.
Method
We recruited adult smokers (N = 238) and middle-school youth (N = 237) throughout the state of New York in May 2016. We randomly assigned participants to one of three between-subject conditions (no GWL [control], 30% GWL, 50% GWL).
Results
Adult and youth participants looked at the GWLs longer when the GWL covered 50% versus 30% of the pack’s front. Increasing GWL size from 30% to 50% did not influence negative affect or risk beliefs, though both GWL sizes increased negative affect relative to the no-GWL control group. Exposure to 50% GWLs increased adult smokers’ intentions to quit compared to no-GWL, but smokers exposed to 30% GWLs did not differ from control. There were no differences between 50% GWLs, 30% GWLs, and control on youth smoking susceptibility.
Conclusions
Findings provide some evidence of the benefits of a 50% versus 30% GWL covering the front of the pack for adult smokers and at-risk youth from socioeconomically disadvantaged backgrounds—though not on all outcomes.
Implications
This research shows that 30% GWLs on cigarette packages increase negative affect relative to packages without front-of-package GWLs. Larger GWLs on cigarette packages (50% vs. 30%) increase visual attention to the warning and its pictorial content among low-SES smokers and at-risk youth but do not further increase negative affect. A 50% GWL increased adults’ quit intention compared to no GWL at all, but we were underpowered to detect modest differences in quit intentions between a 50% and 30% GWL. Future work should thus continue to explore the boundary conditions under which relatively larger GWLs influence cognitive, affective, and behavioral outcomes.
Introduction
Graphic warning labels (GWLs) on cigarette packages use text and images to communicate the health risks associated with cigarette smoking. GWLs are effective at promoting cessation-related outcomes such as quitting intentions,1,2 prompting researchers to investigate the relative importance of various GWL characteristics. Although one study suggests no effect of increasing GWL size on visual attention,3 other studies have suggested that larger warnings are easier to read at a distance,4 are more likely to be noticed,5–7 evoke stronger negative emotions,8,9 foster stronger risk beliefs about smoking’s harms,7,10–12 reduce positive pack perceptions,13 and are perceived to be more effective,8,9,14 probably because they serve as a heuristic conveying the magnitude of health threats posed by smoking.1 Nonetheless, increases in GWL size typically accompany other changes (eg, content, placement, brand marketing restrictions), confounding the causal interpretation for much of the evidence on the influence of the GWL size.
The 2003 World Health Organization’s Framework Convention on Tobacco Control (FCTC) originally recommended that GWLs be 50% or more, but no less than 30%, of the cigarette pack’s principal display areas.15 The 2008 FCTC implementation guidelines adopted stronger language, recommending that GWLs ‘cover more than 50% of the principal display areas and aim to cover as much of the principal display area as possible’ (paragraph 12).15 Just under half (86) of the 181 FCTC-ratifying countries have therefore adopted larger GWLs that cover more than 50% of the pack. However, further data on the impact of GWL size are needed to support tobacco control in the 97 countries that have not yet implemented GWLs covering more than 50%.16
Regulators in the United States, especially, can benefit from such research because US courts protect a more robust right of commercial speech than do courts in other countries due to the way the courts have interpreted the First Amendment of the US Constitution. Currently, the United States has text-only warnings sponsored by the Surgeon General, but they appear on the side of the pack. There have been no major changes to the size or placement of these labels since the Cigarette Labeling and Advertising Act of 1965 instituted them. The Family Smoking Prevention and Tobacco Control Act of 2009, which gave the US Food and Drug Administration (FDA) the power to regulate tobacco products, states that warnings should cover 50% of the pack’s front and back. The FDA proposed nine full-color GWLs to appear on the top half of all cigarette packs sold in the United States. However, a federal appeals court ruled in favor of five major tobacco companies on the grounds the proposed labels violated their First Amendment rights. At issue was whether the GWLs were no more extensive or restrictive than necessary to serve the public health interest. The tobacco companies successfully argued that the proposed labels infringed upon their commercial speech rights.17 The FDA declined to appeal the ruling to the Supreme Court and has yet to offer alternative GWLs.
Thus, a key question for the FDA and US courts is whether a 50% GWL is overly restrictive (as tobacco companies claim) or whether a smaller size would be sufficient to communicate smoking-related risks and further the government interest in public health. Researchers have not yet conducted an unconfounded test of whether a smaller version would be as effective as a 50% version of the FDA-proposed GWLs—a question with ramifications for the legality and impact of future GWLs the FDA may propose. Based on the relevant literature, we expected that 50% GWLs would produce greater negative affect and risk beliefs than 30% GWLs and packs without GWLs. Because the research has not yet demonstrated an effect of increasing size on visual attention and smoking-related intentions, we asked whether such differences would emerge between 30% and 50% GWLs.
Rather than using a general smoking population, this study compared the effects of 50% versus 30% GWLs among two priority populations: socioeconomically disadvantaged adult smokers and primarily nonsmoking youth. The US smoking rates are higher among individuals below the poverty line and individuals without a college degree compared to those with higher income and formal education.18 People of low socioeconomic status (SES) face more difficulty quitting smoking18 and suffer disproportionately from tobacco-related afflictions.19 Similarly, youth from low-SES families have an increased risk for initiating smoking.20 Thirteen percent of eighth graders (ages 13–14) have tried cigarettes, yet the vast majority of kids under 10 years (94%) have not smoked,21 suggesting that middle-school youth are a critical group for tobacco control efforts. Further, low-SES populations are underrepresented in GWL research22 and may respond differently to GWLs.23–25
Method
Procedure
We recruited adult smokers (N = 238) from low-income neighborhoods in rural and urban communities in the Northeast United States. We located zip codes where the median household income level was ≤$35K (using US census data) and collaborated with organizations that work with low-SES populations. Our adult recruitment strategy involved word-of-mouth advertising through partner organizations and in-person flyer and street-intercept recruitment on site. We advertised the adult smoker study as a ‘Health Messaging Study’ in which participants would look at images of cigarette packaging, complete a survey providing feedback on the images, and receive $20 compensation. We confirmed adults’ smoking status biochemically by administering a CoVita breath test, which assesses exhaled carbon monoxide or (by request) an Alere saliva test, which screens for cotinine. We required that adults be able to read text in English on a computer screen.
We recruited middle-school youth (N = 237, not required to be smokers) through Northeastern urban and rural schools in which 40%–100% of students received free or reduced price lunch. We worked with local administrations for permission to conduct the study, sending letters to parents/guardians of students in grades 6–8 to allow them to opt their children out of participating.
After obtaining consent (adults) or assent (from youth not opted out), we escorted participants into a mobile laboratory equipped with five eye-tracking stations using TobiiStudio 3.4.4 software and Tobii T60XL 24″ monitors to assess visual attention. Tobii is nonintrusive insofar as it captures eye movements while the participant sits at a comfortable distance from the screen. We calibrated participants’ gaze with a short eye-tracking exercise. If Tobii could not calibrate eye movements (eg, bifocals, makeup, or visual impairment), the participant viewed study images in preview mode, and no eye-tracking data were collected. A lab assistant read all instructions aloud to participants, which were also displayed on the monitor. We then randomly assigned participants to one of three between-subject conditions (control, 30% GWL, or 50% GWL). Participants watched a 9-image slideshow of cigarette packs. In the control condition, participants saw images of the front of branded cigarette packs (Marlboro, Camel, Newport) without any GWLs (3 repetitions of each brand). We chose front-only images as our control stimuli because in the two GWL conditions, we showed only the fronts of cigarette packs. In the GWL conditions, participants saw images of the front of branded cigarette packs with GWLs covering either 30% or 50% of the top of the front of the pack (Figure 1). We adapted the 9 FDA-proposed GWLs, pairing each GWL with one of the three cigarette brands. We rotated the pairing of GWLs with brands to ensure that brands were not associated with particular GWLs. Each image appeared for 10 s followed by a fixation cross to reset visual attention. We randomized the order in which the pack images appeared in all conditions.
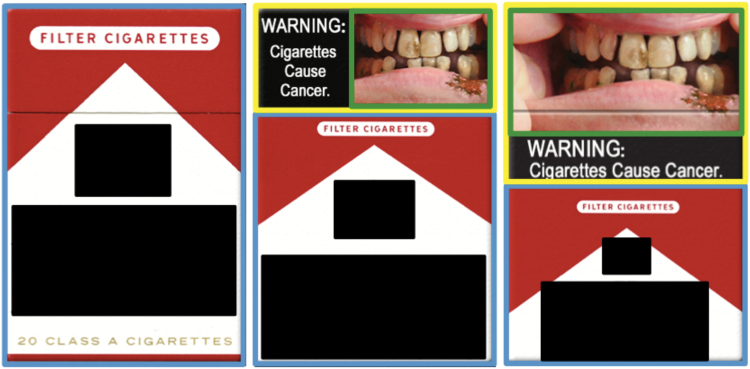
Figure 1.
Sample images of GWLs in each experimental condition with areas of interest, May 2016. Conditions from left to right: control, 30%, and 50%. Colored boxes indicate areas of interest (AOIs) imposed to analyze visual attention: brand (blue), warning (yellow), and image (green). No AOIs for warning or image were imposed on the control condition images. Cigarette brand imagery redacted for publication. Graphic design credit: L. Scolere.
Participants then used iPads to complete a self-report survey. For this study, we focused only on measures of their negative affect, health risk beliefs related to smoking cigarettes, and intention to quit smoking (adults) or susceptibility to smoking (youth). We debriefed participants and compensated them with $20 (adults) or a $10 school donation (youth). The researchers’ IRB and local school districts (where required) approved study protocols.
Measures
Visual attention
We measured how long participants looked at three areas of interest (AOIs): (1) cigarette brand imagery (covering 100%, 70%, or 50% of the box), (2) the GWL itself (0%, 30%, or 50%), (3) images within each warning (Figure 1). We summed fixation times for all nine images and report total fixation time (in seconds) for each AOI (see Supplementary Table A for descriptive statistics).
Negative affect
To measure negative affect, participants reported how much they felt afraid, angry, annoyed, disturbed, grossed out, guilty, sad, and scared on a Likert-type scale of 1 (not at all) to 5 (extremely) after seeing the images.26 Inter-item reliability was high (Cronbach’s αadults = .93, αyouth = .85); we averaged responses into an index.
Old risk beliefs
We assessed what we termed ‘old’ risk beliefs about smoking consequences described in the existing Surgeon General’s Warning (SGW) labels by asking participants to indicate their agreement with statements adapted from the Population Assessment of Tobacco and Health.27 Four items gauged old risk beliefs among adults-that smoking cigarettes causes: babies to be born with low birth weight from the mother smoking during pregnancy, heart disease in smokers, lung disease (such as emphysema) in smokers, and lung cancer in smokers.28 We dichotomized responses with 1 = yes and 0 = no/not sure. We summed them to create an old risk beliefs index ranging from 0 to 4. Four items gauged old risk beliefs among youth: whether they believe cigarette smoking is related to problems in babies whose moms smoke, heart disease, lung disease, and cancer. We coded responses as 1 (definitely yes) or 0 (probably yes/probably not/definitely not) and summed them to form a 0–4 index.
New risk beliefs
We also measured beliefs included in the newly proposed FDA GWLs that have not yet appeared on cigarette packs in the US Four items assessed these new risk beliefs among adults:27 that smoking cigarettes causes (1) stroke and (2) mouth cancer in smokers, and (3) heart attacks and (4) lung disease in nonsmokers from secondhand smoke.28 Coding yes = 1 and no/not sure = 0, we created a summative new risk beliefs index from 0 to 4. For youth, we used a similar set of items: that smoking cigarettes is related to health problems in nonsmokers, stroke, and hole in the throat—and two questions—Can smoking cigarettes kill you? and Are cigarettes very addictive? We collapsed responses to these items into dichotomous variables (1 = definitely yes, 0 = other responses) and summed them to create an index from 0 to 5. We pilot-tested these measures to ensure adults and youth understood their respective versions.
Quit intentions (adults)
Adult participants who indicated they wanted to quit smoking for good and had a time frame in mind29 also reported when they planned to quit. We created a dummy variable for intention to quit within the next 6 months, coding 1 = 7 days, 30 days, 6 months, and 0 = next year, more than 1 year, no quit intention.
Smoking susceptibility (youth)
Youth participants responded to five questions using a 1 (definitely not) to 4 (definitely yes) scale: Do you think that (1) you will smoke a cigarette soon?, (2) you will smoke a cigarette in the next year?, (3) you will be smoking cigarettes in high school?, (4) in the future you might try a cigarette?, and (5) if one of your best friends offered you a cigarette would you smoke it?30,31 We considered participants susceptible to smoking if they did not select ‘definitely not’ for any of the five questions.
Covariates
For both samples, we measured various demographic factors including age, gender identity, ethnicity, and race. Adults reported their income, education, smoking dependence,32 quit attempts in the past year, food insecurity, and receipt of government-funded benefits in the past year. For youth, we also measured having ever tried a cigarette, living in a smoking environment, and sensation seeking. A series of chi-square tests for independence and one-way ANOVAs demonstrated that, apart from the ‘other race’ variable for youth (N = 59 youth participants overall), covariates did not differ significantly across the experimental conditions.
Analytic strategy
We used IBM SPSS (version 20.0.0) for all analyses. We computed means and 95% confidence intervals (CI) for each condition (Table 1). To control for potential confounders, we ran two sets of multivariable linear regression models for the noncategorical dependent variables (fixation times, negative affect, and risk beliefs) and multivariable logistic regression models for intention to quit (adults) and susceptibility to smoking (youth). We used the 50% condition as our reference group in both tables (Tables 2 and 3) but re-ran the models setting the brand-only control group as our reference (see supplementary tables) to permit tests of statistical equivalence between all conditions. Prior to data analysis, we excluded 5 youth and 6 adult participants for being distracted while completing the study, not being proficient English speakers, or completing a similar previous study in the lab. We based these exclusions on a red flag system of noting odd behavior during data collection. A graduate research assistant later reviewed the data for patterns reflecting the reported issue, and the research team met to reach consensus on final exclusion decisions.
Table 1.
Means (or proportions) and 95% confidence intervals by condition, May 2016
| Fixation time on brand | Fixation time on warning | Fixation time on image | Negative affect | Old risk beliefs | New risk beliefs | Quit intentions/ susceptibility to smoking | ||
|---|---|---|---|---|---|---|---|---|
| Adults | 50% | 13.81 [11.59–16.04] |
41.55 [37.33–45.76] |
20.85 [18.40–23.29] |
2.60 [2.38–2.82] |
3.68 [3.50–3.86] |
3.32 [3.11–3.53] |
0.35 [0.25–0.47] |
| 30% | 19.54 [16.48–22.61] |
35.35 [31.18–39.52] |
15.14 [12.95–17.34] |
2.78 [2.51–3.06] |
3.61 [3.41–3.81] |
3.20 [2.94–3.46] |
0.30 [0.20–0.41] |
|
| Control | 54.04 [49.29–58.79] |
— | — | 1.37 [1.23–1.51] |
3.48 [3.26–3.70] |
2.88 [2.61–3.15] |
0.20 [0.12–0.30] |
|
| Youth | 50% | 17.34 [15.46–19.21] |
43.20 [39.92–46.48] |
22.95 [20.75–25.14] |
2.59 [2.36–2.82] |
3.30 [2.98–3.61] |
4.07 [3.79–4.35] |
0.43 [0.31–0.55] |
| 30% | 20.99 [18.52–23.46] |
37.39 [34.16–40.62] |
16.33 [14.57–18.09] |
2.46 [2.25–2.68] |
3.48 [3.23–3.73] |
4.07 [3.81–4.33] |
0.31 [0.21–0.42] |
|
| Control | 52.52 [47.53–57.51] |
— | — | 1.97 [1.75–2.20] |
3.07 [2.75–3.39] |
3.73 [3.43–4.03] |
0.40 [0.29–0.52] |
|
Fixation time variables were measured in seconds. Negative affect was measured on a scale of 1–5. Old risk beliefs were measured on a scale of 0–4. New risk beliefs were measured on a scale of 0–4 for adults and 0–5 for youth. Values for smoking intentions/susceptibility to smoking are proportions indicating percentage of participants in each condition who reported intention to quit in 7 days, 30 days, or 6 months (adults) or who reported they would try smoking (youth).
Table 2.
Regression coefficients (unstandardized) with standard errors or odds ratios predicting adult outcomes, May 2016
| Fixation time on brand | Fixation time on warning | Fixation time on image | Negative affect | Old risk beliefs | New risk beliefs | Intention to quit OR [95% CI] |
|
|---|---|---|---|---|---|---|---|
| Condition (vs. 50%) | |||||||
| Control | 43.92 (2.49)*** | — | — | −1.19 (0.15)*** | −0.07 (0.15) | −0.27 (0.18) | 0.32 [0.13, 0.77]* |
| 30% | 7.08 (2.43)** | −7.40 (3.18)* | −6.40 (1.78)*** | 0.15 (0.15) | −0.12 (0.14) | −0.10 (0.17) | 0.60 [0.28, 1.30] |
| Covariates | |||||||
| Age | −0.19 (0.08)* | 0.12 (0.13) | 0.05 (0.07) | 0.02 (0.01)** | 0.01 (0.01) | −0.004 (0.01) | 1.03 [1.003, 1.06]* |
| Male (vs. female) | −4.27 (2.13)* | 1.19 (3.29) | 0.69 (1.84) | −0.17 (0.13) | −0.06 (0.13) | −0.33 (0.15)* | 0.81 [0.40, 1.63] |
| Hispanic (vs. nonHispanic) | −0.15 (2.92) | 3.06 (4.84) | 2.72 (2.71) | 0.32 (0.18)# | 0.20 (0.17) | 0.02 (0.21) | 1.89 [0.75, 4.73] |
| Black | −0.78 (2.75) | −3.69 (4.40) | −2.00 (2.46) | 0.41 (0.17)* | 0.12 (0.16) | 0.06 (0.20) | 2.06 [0.86, 4.98] |
| Other, nonWhite race | −2.07 (3.39) | −1.51 (5.56) | −0.77 (3.11) | −0.04 (0.20) | −0.19 (0.20) | −0.12 (0.24) | 1.14 [0.39, 3.28] |
| $10K–$19,999 (vs. <$10K) | 1.38 (2.73) | 5.17 (4.22) | 1.33 (2.36) | 0.09 (0.16) | 0.25 (0.16) | 0.30 (0.19) | 2.47 [1.02, 5.98]* |
| $20K+ (vs. < $10K) | −0.30 (2.63) | 7.05# (4.16) | 3.13 (2.32) | 0.21 (0.16) | 0.27 (0.16)# | 0.08 (0.19) | 1.44 [0.60, 3.42] |
| High school (vs. no HS) | −0.92 (2.26) | −3.48 (3.56) | −0.65 (1.99) | −0.23 (0.14)# | 0.08 (0.13) | 0.15 (0.16) | 0.74 [0.34, 1.57] |
| College (vs. no college) | −1.73 (3.19) | 2.43 (4.75) | 1.51 (2.65) | 0.08 (0.19) | −0.06 (0.19) | −0.02 (0.22) | 1.82 [0.68, 4.87] |
| Nicotine dependence | −0.13 (0.50) | −0.68 (0.77) | −0.24 (0.43) | 0.01 (0.03) | 0.01 (0.03) | −0.02 (0.04) | 0.88 [0.75, 1.03] |
| Previous quit attempt | −0.85 (2.22) | −0.39 (3.60) | 0.25 (2.02) | 0.43 (0.13)*** | 0.06 (0.13) | 0.21 (0.16) | 3.57 [1.63, 7.79]*** |
| Emergency food | 0.59 (2.39) | −1.94 (3.83) | −0.18 (2.14) | 0.24 (0.15)# | 0.27 (0.14)# | 0.24 (0.17) | 1.26 [0.56, 2.80] |
| WIC recipient | 3.27 (3.22) | −3.49 (4.81) | −2.31 (2.69) | −0.13 (0.19) | −0.06 (0.19) | 0.04 (0.23) | 1.01 [0.34, 3.01] |
| SNAP recipient | −4.30 (2.74) | 1.75 (4.28) | 1.97 (2.39) | −0.04 (0.17) | −0.08 (0.16) | 0.12 (0.20) | 0.40 [0.16, 1.01]# |
| Colorblind | 11.07 (4.48)* | −1.74 (7.42) | −1.70 (4.15) | −0.16 (0.26) | −0.12 (0.25) | 0.27 (0.31) | 1.15 [0.28, 4.71] |
| Camel preference (vs. other) | −5.37 (7.02) | −32.46 (14.15)* | −15.86 (7.91)* | 0.26 (0.43) | 0.25 (0.42) | −0.13 (0.51) | 2.65 [0.21, 33.07] |
| Marlboro (vs. other) | 0.52 (3.02) | 1.52 (4.66) | −2.17 (2.61) | 0.58 (0.18)** | 0.36 (0.18)* | 0.02 (0.22) | 1.75 [0.61, 5.00] |
| Newport (vs. other) | 1.08 (2.79) | 2.25 (4.52) | −1.57 (2.53) | 0.37 (0.17)* | 0.16 (0.17) | 0.02 (0.20) | 2.38 [0.90, 6.29]# |
| Constant | 26.05(5.56)*** | 38.89(8.56)*** | 19.56 (4.79)*** | 1.28 (0.34)*** | 2.96 (0.33)*** | 3.19 (0.40)*** | 0.08* |
| Adjusted R 2 | 0.63 | 0.01 | 0.03 | 0.39 | −0.01 | 0.01 | — |
| N | 224 | 151 | 151 | 226 | 230 | 230 | 230 |
OR = odds ratio. CI = confidence interval. #p ≤ .10, *p ≤ .05, **p ≤ .01, ***p ≤ .001. All regressions are linear except intention to quit, which is binary logistic.
Table 3.
Regression coefficients (unstandardized) with standard errors predicting youth outcomes, May 2016
| Fixation time on brand | Fixation time on warning | Fixation time on image | Negative affect | Old risk beliefs | New risk beliefs | Susceptibility OR [95% CI] |
|
|---|---|---|---|---|---|---|---|
| Condition (vs. 50%) | |||||||
| Control | 36.39(2.33)*** | — | — | −0.61 (0.16)*** | −0.08 (0.21) | −0.30 (0.20) | 0.85 [0.43, 1.70] |
| 30% | 3.23 (2.31) | −5.80 (2.26)* | −6.38 (1.39)*** | −0.07 (0.16) | 0.30 (0.21) | 0.07 (0.20) | 0.70 [0.35, 1.40] |
| Covariates | |||||||
| Age | 1.22 (0.98) | −2.34 (1.20)# | −1.67 (0.74)* | −0.07 (0.07) | 0.05 (0.09) | 0.14 (0.08) | 0.93 [0.69, 1.26] |
| Male (vs. female) | 0.03 (1.89) | −5.31 (2.25)* | −2.95 (1.38)* | −0.35 (0.13)** | −0.12 (0.17) | −0.31 (0.16)# | 0.63 [0.35, 1.13] |
| Other sex (vs. female) | −1.28 (6.45) | −4.42 (7.05) | −2.07 (4.34) | −0.04 (0.43) | 0.10 (0.54) | 0.24 (0.51) | 1.65 [0.30, 8.97] |
| Hispanic (vs. nonHispanic) | 0.98 (2.39) | −3.59 (2.90) | −3.38 (1.79)# | −0.08 (0.16) | 0.25 (0.21) | 0.18 (0.20) | 1.39 [0.70, 2.78] |
| Black | −2.34 (2.01) | −1.78 (2.38) | −2.55 (1.46)# | −0.05 (0.13) | −0.10 (0.18) | 0.09 (0.17) | 0.68 [0.37, 1.25] |
| Other, nonWhite race | 0.11 (2.22) | −1.70 (2.51) | 0.53 (1.55) | 0.17 (0.15) | −0.03 (0.20) | −0.14 (0.19) | 0.64 [0.32, 1.27] |
| Previous smoking | −9.31 (3.55)** | −8.25 (4.61)# | −2.64 (2.84) | 0.38 (0.22)# | −0.16 (0.31) | 0.09 (0.20) | 3.38 [1.20, 9.48]* |
| Smoking environment | −1.21 (1.93) | 2.87 (2.28) | 1.46 (1.41) | −0.00 (0.13) | 0.11 (0.17) | 0.09 (0.16) | 1.54 [0.87, 2.73] |
| Sensation seeking | 1.80 (1.32) | 0.76 (1.55) | 0.86 (0.96) | 0.02 (0.09) | −0.07 (0.12) | −0.01 (0.11) | 1.21 [0.81, 1.79] |
| Colorblind | 4.15 (3.37) | −10.30 (4.20)* | −3.98 (2.59) | 0.48 (0.23)* | 0.14 (0.31) | 0.16 (0.29) | 2.14 [0.78, 5.83] |
| Constant | 0.52 (12.76) | 75.94(15.34)*** | 45.25 (9.45)*** | 3.45 (0.86)*** | 2.74 (1.15)* | 2.38 (1.08)* | 1.20 |
| Adjusted R 2 | 0.58 | 0.11 | 0.18 | 0.12 | −0.02 | 0.01 | — |
| N | 223 | 149 | 149 | 226 | 233 | 233 | 233 |
OR = odds ratio. CI = confidence interval. #p ≤ .10, *p ≤ .05, **p ≤ .01, ***p ≤ .001. All regressions are linear except susceptibility to smoking, which is binary logistic.
Results
Sample
The adult sample was, on average, middle-aged (M = 40.7, SD = 13.9) and approximately gender-balanced (44% female; see Supplementary Table A). Although the majority identified as nonHispanic White (63%), 32% identified as African American. Only 13% had a college degree (compared to 20.8% of adults over 25 years in the United States).33 About 64% reported a yearly household income of under $20K (vs. 15.8% of the US population),33 and a majority said they received benefits from at least one welfare program in the prior year. Our youth sample averaged 12.5 years (SD = 0.99) and was gender-balanced (52% female). Half (50%) identified as African American (32% nonHispanic White), and 44% reported living with a smoker.
Effects of GWL size
Visual attention
Adults spent significantly less time looking at the cigarette brand imagery in the 30% condition than in control (b = −36.85, p < .001) and less time looking at the brand in 50% versus control (b = −43.92, p < .001; see supplementary tables). Additionally, adults dwelled on the brand less in the 50% GWL compared to 30% (Table 2). Compared to control, youth also spent less time looking at the brand in the 30% (b = −33.17, p < .001) and 50% conditions (b = −36.39, p < .001; see supplementary tables). However, increasing GWL size from 30% to 50% did not decrease the time youth spent looking at the brand (Table 3). Both adults and youth dwelled significantly less on the 30% warning than on the 50% warning (Table 2 and 3). The same pattern emerged for fixation time on images in the GWLs, with adults and youth spending less time on images in the 30% condition than 50% (Table 2 and 3).
Negative affect
Relative to the no-GWL control group, both adults and youth felt significantly more negative affect upon exposure to the 30% GWL (badults = 1.34, p < .001; byouth = .53, p < .001) and 50% GWL (badults = 1.19, p < .001; byouth = .61, p < .001; see supplementary tables). Adults and youth responded to the size change in GWLs similarly in that increasing the size from 30% to 50% had no influence on negative affect (Table 2 and 3).
Old risk beliefs
No statistically significant differences emerged between the three conditions regarding old risk beliefs for either sample. For adults, neither the 30% (b = −.05, p = .76) nor 50% GWL (b = .07, p = .63) increased endorsement of old risk beliefs compared to control (see supplementary tables). Moreover, no difference emerged for the adults between 30% and 50% (Table 2). For youth, neither the 30% (b = .38, p = .07) nor 50% GWL (b = .08, p = .71) significantly increased old risk beliefs relative to control (see supplementary tables). Further, youth participants’ old risk beliefs were similar between the two GWL conditions (Table 3).
New risk beliefs
Adults’ new beliefs about the risks associated with smoking cigarettes did not differ between control and 30% (b = .17, p = .35) or between control and 50% (b = .27, p = .13; see supplementary tables). New risk beliefs did not differ for adults assigned to the 30% and 50% conditions (Table 2). For youth, the 30% GWL marginally increased new risk beliefs relative to control (b = .37, p = .06), and the 50% GWL did not increase new risk beliefs compared to control (b = .30, p = .14; see supplementary tables). Increasing the GWL from 30% to 50% did not influence youth’s new risk beliefs (Table 3).
Quit intentions (adults)
The 50% GWL produced significantly higher intentions to quit compared to control (OR = 3.13, 95% CI = 1.30 to 7.54), but quit intentions were not different between the 30% GWL and the control condition (OR = 1.89, 95% CI = 0.79 to 4.52; see supplementary tables). There was no difference in adults’ intention to quit between 30% and 50% (Table 2).
Smoking susceptibility (youth)
Susceptibility to smoking was statistically equivalent between control and 30% (OR = 0.82, 95% CI = 0.41 to 1.65) and between control and 50% (OR = 1.18, 95% CI = 0.59 to 2.35; see supplementary tables). There was no difference in youth’s susceptibility to smoking between 30% and 50% (Table 3).
Discussion
This study reports five main findings. First, exposure to GWLs, whether covering 30% or 50% of the front of a cigarette pack and among both adult smokers and (at-risk but largely nonsmoking) youth, (a) decreased time spent looking at cigarette brand imagery and (b) increased negative affect relative to packs with fully branded content and no visible GWL. Second, increasing GWL size from 30% to 50% reduced adult smokers’ visual attention to branded content and, among both youth and adults, increased visual attention to both the overall warning and the GWLs’ pictorial content. Third, exposure to GWLs (at either size) did not influence any measured risk beliefs among either population, relative to packs featuring only branded content. Fourth, exposure to 50% GWLs increased adult smokers’ intentions to quit smoking in the next 6 months compared to those exposed to only branded content, but smokers exposed to 30% GWLs were not significantly different from the branded control group. Fifth, there were no differences between 50% GWLs, 30% GWLs, or brand-only content on youth smoking susceptibility.
Public health implications
Generally, our findings were mixed on the effects of 50% versus 30% GWLs, with stronger evidence for differences among adult smokers than (largely nonsmoking) youth. We observed consistent evidence, among adults and youth, in support of 50% versus 30% GWLs on two of three eye-tracking measures. Increased visual attention is likely necessary for meaningful impact over the long-term; findings from a systematic eye-tracking review regarding tobacco control messaging suggest that longer dwell time is associated with greater recall of warning content.34 Further, visual representations of health information can aid in comprehension and recall among low-literacy groups,35 and emotionally evocative media messages can encourage socioeconomically disadvantaged smokers to quit.36 Thus, increasing the visibility of emotional warning images may be important given the high level of exposure that low-income populations have to tobacco industry messaging.37 If one purpose of GWLs is to draw attention to the health consequences of smoking (making the information visible at a distance), devoting more space on packages to communicate these risks is a logical method to achieve such an end.
Furthermore, adult smokers spent less time looking at the brand when the GWL was 50% of the pack’s front than when the GWL was 30%, but larger GWLs did not influence the amount of time youth spent looking at branded content. Tobacco industry documents make clear that cigarette packaging is critical in cultivating brand loyalty and—perhaps more importantly—attracting new users.38 It is thus noteworthy that larger GWLs did not affect the amount of time youth spent looking at branded content. Although we can only speculate, it is possible that adult smokers are more familiar with cigarette brand imagery than (largely nonsmoking) youth. This (comparatively novel) cigarette-branded imagery may attract youth attention regardless of the size of branded content.
Across both samples, GWLs covering 50% versus 30% of the pack did not produce significantly stronger risk beliefs, greater levels of negative affect, higher quit intentions (among adults), or lower smoking susceptibility (among youth). Unlike some studies documenting an association between GWL size changes and stronger risk beliefs about smoking’s harms,7,10–12 we found no direct effects of size increases on old or new risk beliefs.
Many studies finding that larger GWLs are more efficacious than small GWLs have examined relatively large GWLs,8,9,12,13 but the difference between GWL sizes in our studies (50% vs. 30%) may have been insufficient to replicate such findings. Alternatively, it is possible that there are thresholds for the effects of different GWL sizes, such that incremental increases only matter when the GWL covers a sufficient portion of the pack (by extension, reducing the proportion of the pack devoted to cigarette branding). Lending credence to these assertions, Klein and colleagues3 found no difference in visual attention to a 33% versus 20% GWL on a cigarette advertisement, yet we detected significant attention differences comparing 50% to 30%. In addition, other studies have found larger effects of GWLs (independent of size) among youth than adults.23,39 We did not observe such age differences, perhaps again due to insufficient differentiation between GWL sizes. About 91% of our youth sample had never tried cigarettes, so perhaps larger GWLs may be more effective than smaller GWLs among youth who have already experimented with cigarettes—a group for which we were underpowered to detect such an impact.
Notably, the odds of smokers intending to quit were three times higher in the 50% GWL condition than among smokers exposed to cigarette-branded packaging content. This is consistent with results from a randomized controlled trial that exposed smokers to GWLs over a 4-week period.40 Our detection of differences in quit intentions following brief exposure (90 s total) is striking and supports the FDA’s argument that GWLs are narrowly tailored to advance the compelling government interest in promoting public health by encouraging smokers to quit. However, this finding warrants experimental replication in low-SES and general smoking populations.
Limitations
We relied on measures of quit intentions and smoking susceptibility as indicators of potential behavioral impact, so we are unable to provide evidence of behavioral impact over time. We also exposed participants to images of the front of cigarette packs not actual packs. Therefore, the control condition did not include the Surgeon General’s warning that appears on one side of packs sold in the United States. Finally, we did not power the study to be able to detect small but possibly meaningful differences between conditions on quit intentions (where we observed a nonsignificant but five percentage-point difference between the 30% and 50% GWL conditions). Post hoc analyses suggest sufficient statistical power on measures of visual attention and negative affect (probability of detecting an effect ranged from .79 to .99) but less power for risk beliefs (.47 to .86) and quit intentions or susceptibility (.08 to .82).
Conclusions
As many nations have increased their GWLs’ size and the US government considers similar legislation, more experimental evidence is needed to assess smokers’ and youth’s responses to variations in GWL size—particularly among populations most at risk for the harms associated with tobacco use. Together, these experiments demonstrate that a GWL covering 30% of the front of the package is generally preferable to not having any GWL and that increasing GWL size from 30% to 50% can draw visual attention to the label and its imagery. Despite the findings that changing GWL size did not impact negative affect, risk beliefs, or smoking-related intentions, our results suggest that a 50% GWL can promote quit intentions relative to no GWL among adult smokers from socioeconomically disadvantaged groups. This finding implies that GWLs may advance public health when they cover a sufficient portion of the front of a cigarette pack—a claim that merits continued empirical scrutiny.
Supplementary Material
Supplementary materials are available at Nicotine & Tobacco Research online.
Funding
This work was supported by the National Institute of Child Health and Human Development (NICHD) and FDA Center for Tobacco Products (CTP) (grant number R01-HD079612). The funders played no role in the study design; collection, analysis and interpretation of data; the writing of the manuscript; or the decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Food and Drug Administration.
Declaration of Interests
None declared.
References
- 1. Hammond D. Health warning messages on tobacco products: a review. Tob Control. 2011;20(5):327–337. [DOI] [PubMed] [Google Scholar]
- 2. Noar SM, Hall MG, Francis DB, Ribisl KM, Pepper JK, Brewer NT. Pictorial cigarette pack warnings: a meta-analysis of experimental studies. Tob Control. 2016;25(3):341–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Klein EG, Shoben AB, Krygowski S, et al. . Does Size Impact Attention and Recall of Graphic Health Warnings?Tob Regul Sci. 2015;1(2):175–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nilsson T. Legibility and visual effectivness of some proposed and current health warnings on cigarette packages. Report of research done under contract to the Bureau of Tobacco Control, Health Protection Branch, Environmental Health Division, Health Canada; 1999. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.528.9304&rep=rep1&type=pdf. Accessed April 27, 2017. [Google Scholar]
- 5. Hammond D, Fong GT, Borland R, Cummings KM, McNeill A, Driezen P. Text and graphic warnings on cigarette packages: findings from the international tobacco control four country study. Am J Prev Med. 2007;32(3):202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hassan LM, Shiu E, Thrasher JF, et al. . Exploring the effectiveness of cigarette warning labels: findings from the United States and United Kingdom arms of the International Tobacco Control (ITC) Four Country Survey. Int J Nonprofit Volunt Sect Mark. 2008;13(3):263–274. [Google Scholar]
- 7. Thrasher JF, Pérez-Hernández R, Arillo-Santillán E, Barrientos-Gutiérrez I. [Towards informed tobacco consumption in Mexico: effect of pictorial warning labels in smokers]. Salud Publica Mex. 2012;54(3):242–253. [PMC free article] [PubMed] [Google Scholar]
- 8. Les Études de Marché Créatec. Quantitative study of Canadian youth smokers and vulnerable non-smokers: effects of modified packaging through increasing the size of warnings on cigarette packages. Montréal, Québec: Prepared for Health Canada; 2008. [Google Scholar]
- 9. Les Études de Marché Créatec. Quantitative study of Canadian adults: effects of modified packaging through increasing the size of warnings on cigarette packages. Montréal, Québec: Prepared for Health Canada; 2008. [Google Scholar]
- 10. Borland R, Hill D. Initial impact of the new Australian tobacco health warnings on knowledge and beliefs. Tob Control. 1997;6(4):317–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. White V, Webster B, Wakefield M. Do graphic health warning labels have an impact on adolescents’ smoking-related beliefs and behaviours?Addiction. 2008;103(9):1562–1571. [DOI] [PubMed] [Google Scholar]
- 12. Kotnowski K, Fong GT, Gallopel-Morvan K, Islam T, Hammond D. The Impact of Cigarette Packaging Design Among Young Females in Canada: Findings From a Discrete Choice Experiment. Nicotine Tob Res. 2016;18(5):1348–1356. [DOI] [PubMed] [Google Scholar]
- 13. Wakefield M, Germain D, Durkin S, Hammond D, Goldberg M, Borland R. Do larger pictorial health warnings diminish the need for plain packaging of cigarettes?Addiction. 2012;107(6):1159–1167. [DOI] [PubMed] [Google Scholar]
- 14. Bansal-Travers M, Hammond D, Smith P, Cummings KM. The impact of cigarette pack design, descriptors, and warning labels on risk perception in the U.S. Am J Prev Med. 2011;40(6):674–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. WHO Report on the Global Tobacco Epidemic, 2008: The MPOWER Package. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 16. Canadian Cancer Society. Cigarette package health warnings: international status report. Canada; 2014. [Google Scholar]
- 17. RJ Reynolds Tobacco Co. v. US Food and Drug Administration, 696 F.3d 1205, 1214 (DC Cir 2012) https://www.cadc.uscourts.gov/internet/opinions.nsf/4C0311C78EB11C5785257A64004EBFB5/$file/11-5332-1391191.pdf. Accessed April 27, 2017.
- 18. Department of Health and Human Services. The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta, Georgia: Dept of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Washington, DC; 2004. [Google Scholar]
- 19. Henley SJ, Thomas CC, Sharapova SR, et al. . Vital signs: Disparities in tobacco-related cancer incidence and mortality—United States, 2004–2013. MMWR Morb Mortal Wkly Rep. 2016;65. [DOI] [PubMed] [Google Scholar]
- 20 Campaign for Tobacco-Free Kids. Tobacco and Socioeconomic Status. Washington, D.C; 2015. https://www.tobaccofreekids.org/research/factsheets/pdf/0260.pdf. Accessed April 27, 2017. [Google Scholar]
- 21. Bach L. The path to tobacco addiction starts at very young ages. In Campaign for Tobacco Free Kids, 2017. https://www.tobaccofreekids.org/assets/factsheets/0127.pdf. Accessed September 13, 2017. [Google Scholar]
- 22. Noar SM, Francis DB, Bridges C, et al. . Effects of strengthening cigarette pack warnings on attention and message processing: a systematic review. Journal Mass Commun Q. 2016;0:1–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Thrasher JF, Arillo-Santillán E, Villalobos V, et al. . Can pictorial warning labels on cigarette packages address smoking-related health disparities? Field experiments in Mexico to assess pictorial warning label content. Cancer Causes Control. 2012;23(suppl 1):69–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Thrasher JF, Carpenter MJ, Andrews JO, et al. . Cigarette warning label policy alternatives and smoking-related health disparities. Am J Prev Med. 2012;43(6):590–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Thrasher JF, Villalobos V, Szklo A, et al. . Assessing the impact of cigarette package health warning labels: a cross-country comparison in Brazil, Uruguay and Mexico. Salud Publica Mex. 2010;52(suppl 2):S206–S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Watson D, Clark L.. PANAS-X manual for positive and negative affect schedule-expanded form. Iowa City: University of Iowa; 1999. http://ir.uiowa.edu/cgi/viewcontent.cgi?article=1011&context=psychology_pubs. Accessed April 27, 2017. [Google Scholar]
- 27. Hyland A, Ambrose BK, Conway KP, et al. . Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob Control. 2017;26(4):371–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Byrne S, Greiner Safi A, Kemp DG, et al. . Effects of varying color, imagery and text of cigarette package warning labels among socioeconomically disadvantaged middle school youth and adult smokers. Health Commun. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Centers for Disease Control and Prevention. National Adult Tobacco Survey (NATS) https://www.cdc.gov/tobacco/data_statistics/surveys/nats/. Accessed April 27, 2017.
- 30. Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Merritt RK. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychol. 1996;15(5):355–361. [DOI] [PubMed] [Google Scholar]
- 31. Jackson C. Cognitive susceptibility to smoking and initiation of smoking during childhood: a longitudinal study. Prev Med. 1998;27(1):129–134. [DOI] [PubMed] [Google Scholar]
- 32. Fagerström K. Determinants of tobacco use and renaming the FTND to the Fagerstrom Test for Cigarette Dependence. Nicotine Tob Res. 2012;14(1):75–78. [DOI] [PubMed] [Google Scholar]
- 33. U.S. Census Bureau. Current Population Survey: 2016 Annual Social and Economic Supplement Last revised March 31, 2017 and August 10, 2017. https://www.census.gov/programs-surveys/cps.html. Accessed August 20, 2017.
- 34. Meernik C, Jarman K, Wright ST, Klein EG, Goldstein AO, Ranney L. Eye Tracking Outcomes in Tobacco Control Regulation and Communication: A Systematic Review. Tob Regul Sci. 2016;2(4):377–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Houts PS, Doak CC, Doak LG, Loscalzo MJ. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns. 2006;61(2):173–190. [DOI] [PubMed] [Google Scholar]
- 36. Durkin SJ, Biener L, Wakefield MA. Effects of different types of antismoking ads on reducing disparities in smoking cessation among socioeconomic subgroups. Am J Public Health. 2009;99(12):2217–2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lee JG, Henriksen L, Rose SW, Moreland-Russell S, Ribisl KM. A Systematic Review of Neighborhood Disparities in Point-of-Sale Tobacco Marketing. Am J Public Health. 2015;105(9):e8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Difranza JR, Clark DM, Pollay RW. Cigarette package design: opportunities for disease prevention. Tob Induc Dis. 2002;1(2):97–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hammond D, Thrasher J, Reid JL, Driezen P, Boudreau C, Santillán EA. Perceived effectiveness of pictorial health warnings among Mexican youth and adults: a population-level intervention with potential to reduce tobacco-related inequities. Cancer Causes Control. 2012;23 (suppl 1):57–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Brewer NT, Hall MG, Noar SM, et al. . Effect of Pictorial Cigarette Pack Warnings on Changes in Smoking Behavior: A Randomized Clinical Trial. JAMA Intern Med. 2016;176(7):905–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.