Abstract
Non-suicidal self-injury (NSSI) affects 15–20% of adolescents—disproportionately girls—and is a strong predictor of eventual suicide attempts and suicide. Many girls now initiate NSSI before age 10. These early-starters exhibit greater frequency of NSSI, use more diverse methods, and are hospitalized more often, yet there are no empirically supported prevention programs for preadolescents. Obstacles to prevention include ascertaining who is sufficiently vulnerable and specifying mechanistic intervention targets. Recent research indicates that (1) preadolescent girls with ADHD who are also maltreated are at alarming risk for NSSI and suicide attempts by adolescence, and (2) the conjoint effects of these vulnerabilities are sufficiently potent for targeted prevention. Research also indicates that existing interventions are effective in altering child- and family-level mechanisms of NSSI. These interventions alter neurobiological markers of vulnerability, which can be used as proximal efficacy signals of prevention response, without waiting for NSSI and suicide attempts to emerge.
Keywords: self-injury, suicidal behavior, suicide, self-harm, impulsivity, maltreatment, prevention
Non-suicidal self-injury (NSSI)—defined as deliberate self-harm without intent to die (Nock, 2009)—affects 15–20% of adolescents, disproportionately girls (Swannell, Martin, Page, Hasking, & St John, 2014). In clinical samples, prevalence rates approach 50% (Asarnow et al., 2011; Nock, 2010), and over 400,000 in the US receive medical attention for NSSI each year (CDC, 2006). Furthermore, NSSI—including behaviors such as banging/hitting, burning, carving, and cutting oneself—is a strong predictor of eventual suicide (Hamza, Stewart, & Willoughby, 2012; Klonsky, May, & Glenn, 2013). In fact, about 75% of inpatients who engage in NSSI eventually attempt suicide (Nock, Joiner, Gordon, Lloyd-Richardson, & Prinstein, 2006), and about 10% eventually die by suicide (Berman, Jobes, & Silverman, 2006). In turn, suicide is the second leading cause of death among teens and young adults in the US (CDC, 2014), and is the second leading cause of death worldwide for 15–19-year-old girls (WHO, 2018). Increasing prevalence rates of NSSI are therefore quite troubling (CDC, 2008; Nock, 2008), especially given that many young girls now initiate before age 10 (Ammerman, Jacobucci, Kleiman, Uyeji, & McCloskey, 2017). These early-starters exhibit greater frequency of NSSI, use more diverse and dangerous methods, and are hospitalized more often than later starters. NSSI is also associated with marked functional impairment, including poor academic performance, adverse peer relations, and vulnerability to various psychiatric morbidities (Crowell, Beauchaine, & Linehan, 2009; Klonsky, 2011). Suicidal behaviors are similarly impairing and require expensive, restrictive interventions.
Such findings suggest that early prevention of NSSI should be a major public health priority (Crowell, Derbidge, & Beauchaine, 2014), yet no empirically supported prevention programs exist for pre-adolescents (Nock, 2010; O’Connor, & Nock, 2014). Rather, interventions are typically initiated in adolescence—the period of highest risk during which many have already engaged in NSSI and suicidal behaviors (SBs) and affiliate with deviant peers who reinforce self-harm (Asarnow, Hughes, Babeva, & Sugar, 2017; Garraza, Walrath, Goldston, Reid, & McKeon, 2015; Muehlenkamp, Walsh, & McDade, 2010; Prinstein, Boergers, & Spirito 2001). This timing is problematic because once established, NSSI and its psychological correlates—particularly emotion dysregulation—are difficult to treat (Asarnow et al., 2011; Crowell et al., 2009).
Research on NSSI and SBs has existed for years (Ammerman et al., 2017; Asarnow et al., 2011; Auerbach et al., 2014; Chronis-Tuscano et al., 2010; Joiner et al., 2009; Klonsky, 2007; Nock, 2010; Zalsman et al., 2016), but to date, three obstacles have precluded development of effective prevention programs. First, recruitment into preventive interventions requires valid prospective identification of vulnerability (Franklin et al., 2017). Despite increasing prevalence, SBs and suicide—distal but nevertheless principal prevention targets—remain low-base-rate phenomena. As with all low-base-rate behaviors, difficulties ascertaining prospective vulnerability present challenges for prevention (Baldessarini, Finklestein, & Arana, 1983). It is therefore sobering that prospective prediction of suicidal thoughts and behaviors by psychiatric diagnosis (mood, substance use, psychosis), sample characteristics (community, clinical), age (adolescent, adult), and other factors remains poor (Franklin et al., 2017). Second, even if recruitment efficiency could be improved, malleable, mechanistic prevention targets must be identified to make prevention practical. Third, because primary prevention outcomes are distal, effects of prevention programs on known predictors and mediators of self-harm—both biological and social—must be evaluated to assess response. Thus, if NSSI and eventual suicide attempts are to be prevented, vulnerable individuals must be identified, and mechanisms of behavior change must be specified, engaged, and measured effectively—before the onset of self-harm (Nielsen, Riddle, King, & The NIH Science of Behavior Change Implementation Team, 2017).
In sections to follow, we review evidence that (1) current understanding of etiology—at least for a sizable subset of girls—is sufficient to identify vulnerable individuals before they engage in NSSI or SBs and before they affiliate with deviant peers who reinforce self-harm1; (2) family, peer, and other social mechanisms that reinforce self-harm are malleable using existing interventions; and (3) carefully selected neurobiological markers of vulnerability can be used to evaluate prevention response without waiting to assess distal outcomes of NSSI and SBs. Although perfect prediction of complex human behaviors such as NSSI and SBs is impossible over any extended interval, we can now identify girls who are at high enough probabilistic vulnerability to make targeted prevention practical. Given the inordinate level of pain and suffering associated with NSSI and SBs, and given their resistance to treatment once established, it is incumbent on the research community to develop and evaluate new prevention programs. Specifying etiology requires that we adopt a developmental psychopathology perspective (Hinshaw, 2017) in which child-level vulnerabilities, environmental risk factors, and their transactions are considered in the ontogenesis of NSSI and SBs. Thus, we must abandon simple main effects models of single vulnerabilities and single risk factors in favor of interactive developmental pathways if we are to prevent these costly public health concerns (Beauchaine, Klein, Crowell, Derbidge, & Gatzke-Kopp, 2009).
Although the literature is fractionated across subtypes of psychopathology (depression, borderline personality disorder [BPD]), ages of participants (adolescents, adults), biological vulnerabilities (genetic, neural, neurohormonal, peripheral), and environmental risk factors (abuse, trauma, invalidation), much is known about the etiology of NSSI and the more distal outcome of suicide. Recent research shows that highly impulsive preadolescent girls who also incur maltreatment, including physical and sexual abuse, are at 50% risk for developing NSSI, and at 33% risk for suicide attempts by late adolescence and early adulthood (Guendelman Owens, Galan, Gard, & Hinshaw, 2016; Hinshaw et al., 2012; Owens, & Hinshaw, 2016; Swanson, Owens, & Hinshaw, 2014; Stepp, Burke, Hipwell, & Loeber, 2012). Notably, impulsivity, maltreatment, and sex—all established vulnerabilities/risk factors for NSSI and suicide in their own rights (Allely, 2014; Auerbach et al., 2014; Fox, Millner, Mukerji, & Nock, 2017)—do not confer enough independent (main effects) vulnerability to make recruitment into prevention programs efficient. In combination, however, these predictors confer an alarming level of risk that makes targeted prevention both feasible and necessary (Chronis-Tuscano et al., 2010).
The etiological model we present below also identifies prevention targets that are linked concurrently and prospectively to NSSI and SBs. We acknowledge that other developmental pathways to NSSI and SBs exist. Our model therefore does not apply to all who engage in these behaviors. In fact, some who die by suicide never engage in NSSI. Nevertheless, an impressive body of research conducted in the past decade identifies individual-level (impulsivity, emotion dysregulation), family-level (maltreatment, coercion, invalidation), and peer-level (social reinforcement, contagion) targets for prevention, as well neural, neurohormonal, and autonomic markers of vulnerability. Some of these biological markers identify vulnerability prospectively, and are malleable to intervention. These markers can therefore be used—along with observable behavior—to evaluate prevention response prior to the anticipated onset age of NSSI and SBs. In sum, we present an etiological model that captures complex interactions among individual-level vulnerabilities and environmental risk factors, identifying targets for prevention. We also present evidence that existing interventions are effective in engaging these prevention targets and in altering mechanisms that give rise to NSSI and SBs. It bears repeating that NSSI and SBs emerge not from single vulnerabilities (impulsivity, emotion dysregulation) or risk factors (abuse, maltreatment), but from their interdependent and interactive effects, which reinforce, entrench, and embed the behaviors in neurobiological and social systems over time. Once NSSI and SBs become “canalized” and serve self-regulatory and other psychological functions, treatment becomes inordinately challenging. Preventive interventions that target mechanisms directly and teach adaptive self-regulatory strategies before NSSI and SBs emerge hold considerable promise in forestalling untoward developmental trajectories that are difficult to reverse once established.
Traditional Conceptualizations of NSSI and Suicidal Behavior
Etiological conceptualizations of NSSI and SBs first appeared in the 1990s (Blumenthal, & Kupfer, 1990; Leenaars, 1991). These models were descriptive, and focused on adolescents/young adults—not children. This stemmed from the assumption that self-injury was associated with personality disorders that did not emerge in childhood. We now recognize that personality disturbance is almost always preceded by childhood adjustment problems (Beauchaine et al., 2009) and that many girls engage in NSSI before age 10, with a mean onset age of 13 (Ammerman et al., 2017; Kovacs, Goldston, & Gatsonis, 1993). Early models were also untested empirically (Linehan, 1993), and focused on either biology or environment. Such reductionism is problematic because alone, main effects of biology (genes, neural functions, neurohormones) and environment (family dysfunction, peer affiliations) account for limited variance in NSSI and SBs (Crowell et al., 2008). As with many forms of psychopathology (Beauchaine, Zisner, & Sauder, 2017; Cicchetti, 2016), complex interactions between biology and environment shape and maintain self-injury (Beauchaine et al., 2009; Crowell et al., 2009). Accordingly, contemporary models of NSSI and SBs must be transactional and evaluate conjoint and interactive effects of biological vulnerabilities and environmental risk factors. As already noted, main effects of single vulnerabilities have proven unfruitful for prospective predictive purposes (Franklin et al., 2017). Instead, NSSI and SBs—much like other multifactorially determined psychiatric and medical conditions—are best understood as endpoints of complex interactions between heritable vulnerabilities and environmental risk exposures over time (cf. Beauchaine & Constantino, 2017).
Linehan’s Model of Emotion Dysregulation
Linehan (1993) was among the first to propose a developmental-transactional model of NSSI and SBs, as outlined in her influential theory of BPD. She surmised correctly that most individuals with BPD exhibit some form of self-injury and that developmentally, NSSI usually precedes SBs (Brent, 2011; Klonsky et al., 2013). Although not all who engage in NSSI develop BPD, Linehan described NSSI as a core vulnerability. The crux of her theory is that NSSI emerges from emotion dysregulation—defined as the inability to modulate negative affective states—especially anger, fear, and sadness—in the service of goal directed behavior (Beauchaine, 2015; Linehan, 1993). Linehan proposed that emotion dysregulation itself develops via transactions between predisposing biological vulnerabilities and family environments that invalidate emotional experience and reinforce emotional lability. As a result, vulnerable children become emotionally reactive, an interpersonal response style that later generalizes to extrafamilial relationships.
Consistent with Linehan’s (1993) predictions, negative reinforcement of emotional lability is well documented in families of self-injuring adolescent girls (Crowell et al., 2013, 2017; Crowell, Kaufman, & Beauchaine, 2014; Fruzzetti, Shenk, & Hoffman, 2005). Thus, emotion dysregulation is indeed shaped within families and characterizes NSSI (Adrian, Zeman, Erdley, Lisa, & Sim, 2011; Beauchaine & Zalewski, 2016). More broadly, the emotion dysregulation hypothesis of NSSI and SBs is supported across multiple levels of analysis, including self-report (Gratz & Roemer, 2008; Klonsky, 2007; Nock, 2008, 2009, 2010), network analyses of symptoms (Southward & Cheavens, 2018), and patterns of neural responding (Davis et al., 2014; Groschwitz, Plener, Groen, Bonenberger, & Abler, 2016; Hazlett et al., 2012; Lis, Greenfield, Henry, Guile, & Dougherty, 2007). Adolescents and adults who engage in NSSI self-report extreme emotion dysregulation (Bresin, 2014; Voon, Hasking, & Graham, 2014), and show both volumetric irregularities and abnormal BOLD responding in cortical structures (mPFC, vlPFC, insular cortex) implicated in self- and emotion regulation (Beauchaine, Sauder, Derbidge, & Uyeji, 2018; Davis et al., 2014; King-Casas et al., 2008).
These findings, as summarized in recent meta-analyses, support the emotion dysregulation hypothesis (e.g., Wolff et al., 2018), yet it is important to note that some sources of evidence are less conclusive. For example, although numerous studies demonstrate low parasympathetic nervous system (PNS) tone and excessive PNS withdrawal during negative emotion inductions among those who engage in NSSI and SBs (Crowell et al., 2005, 2008, 2013, 2014, 2017; Kuo & Linehan, 2009), autonomic hyper-reactivity is not as consistent when using (1) other markers, such as sympathetic nervous system (SNS) responding; and (2) non-emotion-induction paradigms, such as cold-pressor, acoustic startle, and public speaking tasks. In addition, although ecological momentary assessment indicates increased negative affect before NSSI episodes (Rodríguez-Blanco, Carballo, & Baca-García, 2018), effect sizes are modest. Given core self-regulatory functions of the PNS (see e.g., Porges, 2007), our view is that PNS assessments are most valid for assessing emotion dysregulation (see Zisner & Beauchaine, 2016a). Nevertheless, disagreement in the literature should be noted. Furthermore, the emotion dysregulation hypothesis does not preclude other mechanisms of NSSI not discussed herein, such as abnormal pain processing (Bresin & Gordon, 2013).
Research on PNS responding in particular, which we discuss in more detail in later sections, suggests that physiological dysregulation and emotion dysregulation—and aversive family interaction patterns that shape and maintain them—are important targets for prevention of NSSI and SBs (Crowell et al., 2017; Gratz, 2007; Gratz, Tull, & Levy, 2014; Ougrin, Tranah, Stahl, & Moran, 2015). It is essential to note, however, that by itself emotion dysregulation is insufficient to account for NSSI or SBs. Many forms of psychopathology are characterized by emotion dysregulation (Beauchaine & Crowell, in press; Cole, Hall, & Hajal, 2017), but most are not marked by self-injury. Emotion dysregulation is a transdiagnostic vulnerability that is not specific to NSSI, SBs, or even BPD. This fact has important implications for prospectively identifying individuals who are most vulnerable to self-injury and eventual suicide. Because emotion dysregulation is transdiagnostic, by itself it is a limited prospective predictor of NSSI and SBs. Rather, it interacts with other vulnerabilities to maximize risk.
An Elaborated Transactional Perspective
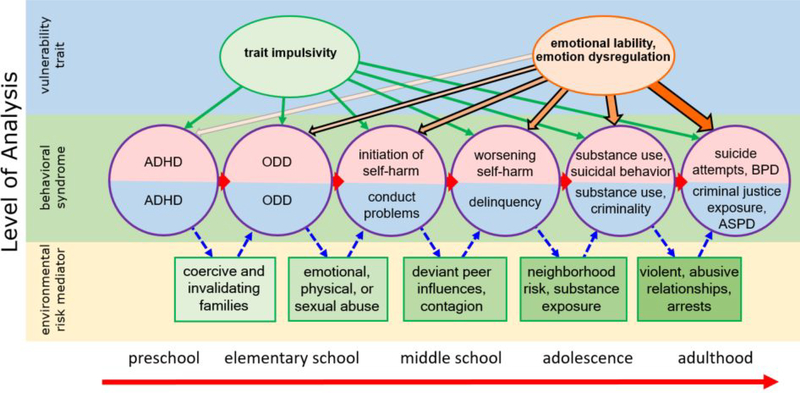
In collaboration with Linehan, we refined her original theory (Beauchaine et al., 2009; Crowell et al., 2009, 2014). In this reformulation, emotion dysregulation confers vulnerability to, but alone is insufficient for, development of NSSI and SBs. Instead, NSSI is most likely when highly heritable trait impulsivity—indexed in childhood by hyperactive-impulsive (not inattentive) symptoms of ADHD (Ahmad & Hinshaw, 2016)—co-occur with emotion dysregulation. As outlined above, emotion dysregulation is shaped and maintained across development by aversive socialization mechanisms including maltreatment, coercion, and family reinforcement of emotional lability (Cicchetti, 2016; Crowell et al., 2017; Narayan, Cicchetti, Rogosch, & Toth, 2015). This model is summarized in Figure 1. In this article, we focus on NSSI and SBs as outcomes, and do not discuss more distal endpoints (substance use, borderline traits). We emphasize again that NSSI and SBs cannot be understood adevelopmentally, or by focusing on single vulnerabilities, single risk factors, or single levels of analysis.
Figure 1.
Progression of early life impulsivity for boys (blue semi-circles) versus girls (pink semi-circles) given similar environmental risk exposures. Impulsive girls who incur adversity—particularly physical and/or sexual abuse—are likely to progress to NSSI, SBs, and eventual BPD (see text). In the absence of these adversities, emotion dysregulation is unlikely to develop, and impulsivity is unlikely to progress beyond ADHD. Adapted with permission from Beauchaine (in press).
Impulsivity as a predisposing vulnerability.
When defined by high hyperactivity-impulsivity (HI) scores on ADHD scales, trait impulsivity yields heritability coefficients of about.80 (Nikolas & Burt, 2010). It also confers vulnerability to increasingly severe externalizing comportment across development, particularly in contexts of coercion, maltreatment, and deviant peer affiliations (Figure 1; Beauchaine, & McNulty, 2013; Beauchaine et al., 2017). Thus, a highly heritable trait, expressed early in life as HI, interacts with environmental risk to promote adverse behavioral outcomes (Beauchaine et al., 2017; Meier, Slutske, Arndt, & Cadoret, 2008; Patterson, DeGarmo, & Knutson, 2000). Although many early findings derived from studies of boys, similarly untoward outcomes occur for impulsive girls who experience adversity (Ahmad & Hinshaw, 2017; Meier et al., 2008).
It has long been known that (1) many girls who engage in NSSI are reared in families with impulsive, externalizing boys (Goldman, D’Angelo, & DeMaso, 1993); (2) family dysfunction, including coercion, maltreatment, and invalidation, is often experienced by both self-injuring girls and externalizing boys (Crowell et al., 2017; Glassman, Weierich, Hooley, Deliberto, & Nock, 2007); (3) both self-injuring girls and externalizing boys are at elevated risk for suicide (Asarnow et al., 2011; Thompson, Kingree, & Ho, 2006); and (4) girls who engage in NSSI score high on externalizing measures and affiliate with delinquent peers (Auerbach et al., 2014; Barker, Arseneault, Brendgen, Fontaine, & Maughan, 2008; Crowell et al., 2005, 2008). Collectively, these findings suggest that NSSI among girls and externalizing behavior among boys may derive from a common, sex-moderated etiology (Beauchaine et al., 2009; Crowell et al., 2009, 2014). Furthermore, like emotion dysregulation, trait impulsivity confers vulnerability to, but alone is insufficient for, development of NSSI (Crowell et al., 2009). Instead, two transdiagnostic vulnerabilities—trait impulsivity and emotion dysregulation—combine and interact to maximize risk (Figure 1). Here, we focus specifically on girls because they are more vulnerable to NSSI and SBs in adolescence/young adulthood (Beauchaine et al., 2009; Olfson, Gameroff, Marcus, Greenberg, & Shaffer, 2005).
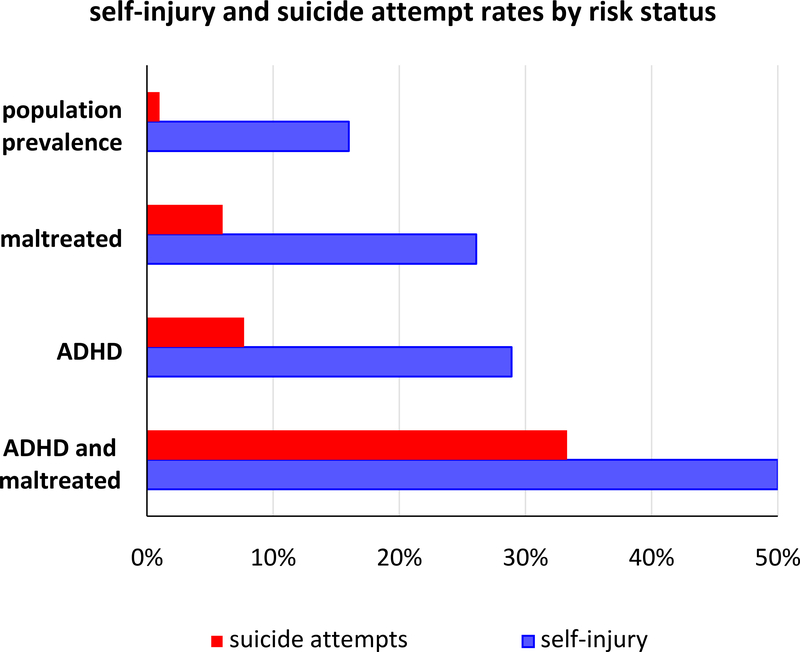
Several predictions with prevention implications follow from this model. Girls with high levels of HI who are reared in coercive, invalidating, and maltreating families that reinforce emotional lability and emotion dysregulation should be vulnerable to NSSI and SBs—more so than girls who experience HI but are not reared in such contexts, and more so than girls who are reared in such contexts but do not experience HI. When we offered this hypothesis a decade ago (Beauchaine et al., 2009; Crowell et al., 2009), no relevant data were available, yet substantial support has since emerged. Although rates of self-harm are elevated among girls with ADHD (Allely, 2014), this risk is concentrated almost entirely among those with the HI and combined subtypes/presentations (Chronis-Tuscano et al., 2010)—especially those who have been maltreated (Guendelman et al., 2016; Hinshaw et al., 2012). Among girls with ADHD with predominantly HI symptoms at ages 6–12 years, those who also incur maltreatment—whether physical abuse, sexual abuse, or neglect—are at over 50% risk of significant NSSI by ages 1723, and at over 33% risk of one or more serious suicide attempts (Guendelman et al., 2016; Swanson et al., 2014). Thus, prospective identification of risk is now possible (Allely, 2014; CDC, 2014; Owens & Hinshaw, 2016; Guendelman et al., 2016). Although ADHD and maltreatment elevate risk, their combined effects are alarmingly potent (see Figure 2).
Figure 2.
Rates of self-injury and suicide attempts among late adolescent/young adult females by risk status. See text for details.
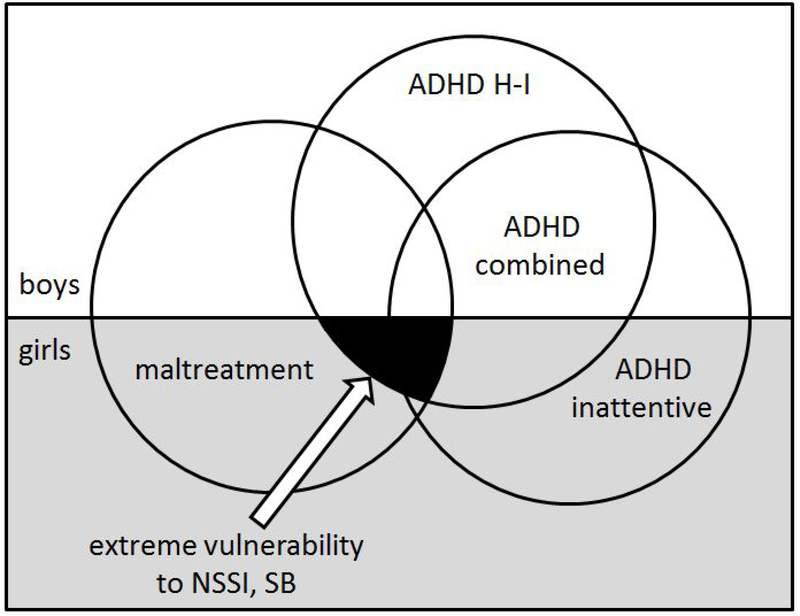
These findings indicate that NSSI and SBs are etiologically complex, which must be accounted for, accommodated, and targeted by prevention programs. Figure 3 provides a visual depiction of how risk status is determined by multiple, only partly overlapping vulnerabilities, including sex, subtype/presentation of ADHD, and maltreatment status. None of these three factors—either alone or in pairs—confers sufficient prospective vulnerability to enroll individuals into prevention programs before NSSI and SBs emerge. Instead, recruitment must target those affected by all three etiological influences. Such targeted recruitment dovetails with calls to embrace etiological complexity in formulating more effective treatments for diverse forms of mental and physical illness (Cohen, 2016).
Figure 3.
Conjoint effects of sex, ADHD status, and maltreatment on prospective vulnerability to NSSI and SBs. None of these characteristics—either singly or in pairs—confers sufficient vulnerability for recruitment into prevention programs. In combination, however, they mark considerable vulnerability.
In sections to follow, we elaborate on complex etiological mechanisms of NSSI and SBs across levels of analysis including neural, autonomic, temperamental, familial, emotional, and social. Given failure of main effects models to prospectively predict NSSI and SBs (Franklin et al., 2017), we emphasize interactions across levels of analysis and consider which mechanisms are the most suitable candidates for engagement in prevention programs. Before discussing prevention, however, we briefly summarize existing treatment programs, as typically delivered in adolescence. These programs can be used to inform prevention strategies.
Existing Treatment Programs
Despite extensive functional impairment associated with NSSI—and the risk it portends for eventual suicide (Hamza et al., 2012; Hawton, Saunders, & O’Connor, 2012)—prevention programs for preadolescents are lacking (Nock, 2010; O’Connor, & Nock, 2014). We believe this is a critical oversight. As outlined above, an increasing number of girls now initiate NSSI before age 10. As with most physical and mental health conditions (cf. Moffitt, 2003), earlier age of onset is associated with greater functional impairment, including more severe self-harm (Ammerman et al., 2017). Such findings have led to calls for targeted prevention programs in the elementary school years, but these have yet to be developed. In addition, NSSI usually precedes SBs, and both often precede impairing psychiatric conditions including BPD (Crowell et al., 2014; Hawton et al., 2012; Whitlock et al., 2013). Ironically, the current dearth of prevention programs may stem from the status of NSSI as a transdiagnostic feature of impairing psychiatric conditions for which considerable prevention efforts have been expended. These include major depression, eating disorders, PTSD, conduct disorder, and BPD (Beauchaine et al., 2009; Hoertel et al., 2015). Despite prospective associations with these and other disorders, NSSI has not been targeted for prevention independently among children (Ammerman et al., 2017).
In contrast, community-based and clinical prevention programs that target adolescents who engage in NSSI, SBs, and suicide have existed for some time (Asarnow, Berk, & Baraff, 2009; Calear et al., 2016; Zalsman et al., 2016). Some of these are clearly effective in reducing suicide attempts (Asarnow et al., 2017; Muehlenkamp et al., 2010). For example, the Garrett Lee Smith Memorial Suicide Prevention Program halves suicide attempts among 16–23-yr-olds (Garraza et al., 2015; Walrath, Garraza, Reid, Goldston, & McKeon, 2015), reduces suicide rates, and is cost-effective. Although essential, these programs are expensive. Even when targeted they must be cast somewhat widely. Clinical programs are more expensive, and require coordination across adolescents, parents, teachers, and service providers (Asarnow et al., 2009). Moreover, by themselves such programs do not achieve ‘Zero Suicide’ objectives of the National Action Alliance for Suicide Prevention, endorsed by both the Surgeon General (Surgeon General’s Report, 2012) and NIMH (2016). Because existing prevention and intervention programs enroll those who are already at an age of maximal risk (adolescence) and/or who have already engaged in NSSI/suicide attempts, “the train may have left the station” for some—and reversing course is formidable (Asarnow et al., 2011; Hawton et al., 2012; Klonsky et al., 2013).
As NSSI develops, it becomes increasingly embedded in peer reinforcement systems (Guendelman et al., 2016; Jarvi, Jackson, Swenson, & Crawford, 2013; Owens & Hinshaw, 2016) and takes on emotion-regulation functions in its own right (Klonsky, 2007; Nock, 2009). Repeated NSSI also desensitizes neurobiological stress response systems that ordinarily promote self-preservation (Beauchaine, Crowell, & Hsiao, 2015; Joiner et al., 2009). Over time, NSSI therefore becomes self-reinforcing, and more difficult to reverse than to prevent. Because prevention and treatment effectiveness usually improve when we understand etiology and target it directly (e.g., Beauchaine, Neuhaus, Brenner, & Gatzke-Kopp, 2008), we now discuss candidate etiological mechanisms that might be targeted in prevention programs.
A Conceptual Model for Prevention: Identifying Mechanistic Targets
According to our transactional perspective, trait impulsivity interacts with emotion dysregulation, which is shaped and maintained by maltreatment and associated family dynamics to confer vulnerability to NSSI and SBs. These family relationship dynamics can be targeted by existing interventions that improve parenting and children’s self-regulation. The importance of altering family dynamics cannot be over-emphasized; successful programs for treating self-injury almost all target family interactions directly (Brent et al., 2013). Family interventions improve impulsive children’s physiological, self-, and emotion regulation (Bell et al., 2018), all of which show associations with distal prevention targets, including NSSI and SBs. A core assumption is that prevention should be initiated early given (1) an expected age of onset for NSSI before age 10 for many, and by age 13 for at least half of young girls who engage in the behavior; and (2) more severe self-harm and greater functional impairment for early starters (see above; Ammerman et al., 2017). Below we offer several tenets of prevention that follow from our model.
Tenet 1: Halting Ongoing Maltreatment is the Top Prevention Priority
Halting ongoing maltreatment is the clear first step for any prevention program. Abuse and maltreatment must be reported to local Child Protective Services agencies. Because many individuals are recruited into prevention programs through CPS, child maltreatment may have already been addressed. Nevertheless, active monitoring is important given high rates of recidivism (Dakil, Sakai, Lin, & Flores, 2011). In some cases, the current family environment may be supportive enough for interventions to be delivered primarily to the child. This approach may be appropriate for children who are not impulsive and are placed with competent caregivers. However, maltreatment often casts a long shadow on children’s biological, socioemotional, and self-regulatory development (Cicchetti, 2016; Cicchetti & Toth, 2016). Impulsive children who are maltreated are therefore likely to require additional, intensive prevention and intervention components that target parenting, family dynamics, and child behaviors to forestall ongoing and progressive functional impairment.
Child maltreatment occurs in broader contexts of family dysfunction (Cicchetti & Toth, 2016). A voluminous literature demonstrates that parents who maltreat (1) engage in harsh, aversive parenting, including yelling, coercion, and physical punishment; (2) reinforce hostility, physical aggression, and emotional lability via escape conditioning mechanisms (negative reinforcement); (3) use inconsistent discipline that wavers between lax and punitive; and (4) are less positive and warm toward their children than parents who do not maltreat (Skowron, & Reinemann, 2005; Wilson, Rack, Shi, & Norris, 2008). Furthermore, maltreating parents exhibit poor self-regulation themselves (Dix, 1991). Given high heritability of ADHD, they are likely to be impulsive if they have children who are impulsive. In turn, parental impulsivity and emotion dysregulation exert strong effects on children’s emerging and future self-regulation (Bariola, Eleonora, & Hughes, 2007; Crowell et al., 2017).
Although these family dynamics are resistant to change (Dakil et al., 2011), several effective interventions exist that improve both parenting and child behavior in both maltreating families and families of children with ADHD (Chaffin et al., 2004, Webster-Stratton, Reid, & Beauchaine, 2013). These interventions are most effective when they target parent-, child-, and family-level mechanisms together as opposed to being disaggregated to target single mechanisms (Chronis-Tuscano et al., 2016; Webster-Stratton, Reid, & Hammond, 2004). Such programs exert positive effects on parenting, child internalizing and externalizing behaviors, and both parent and child ER. To date, they have not been applied to prevent NSSI and SBs, yet considerable evidence indicates promise toward doing so given the shared mechanisms reviewed above.
Tenet 2: Emotion Dysregulation—Not Impulsivity—Should be the Primary Child-Level Prevention Target
Given interactive effects of impulsivity and emotion dysregulation on development of NSSI and SBs (see above), one might conclude that both should be primary targets of prevention. Yet prioritizing emotion dysregulation over impulsivity follows from several considerations. First, trait impulsivity, as manifested early in life as HI symptoms of ADHD, arises primarily from genetically mediated temperamental predispositions/individual differences that are relatively stable across the lifespan (Saudino, 2009; Schmidt, Fox, Perez-Edgar, & Hamer, 2009). Although improvements in impulsivity (including ADHD) following behavioral, pharmacological, and multimodal treatments are observed (MTA Cooperative Group, 1999; Webster-Stratton et al., 2013), these are usually time-limited, and therefore wane without ongoing treatment, whether behavioral, pharmacological, or both (Swanson et al., in press). Thus, children’s temperamental predispositions—including trait impulsivity—must be accommodated if we wish to improve prevention efficacy (Harold, Leve, & Sellers, 2017).
Although partly heritable (Goldsmith et al., 2008), ER is shaped strongly across development by environments, particularly parent-child relationship dynamics (Beauchaine & Crowell, in press; Bernier, Carlson, & Whipple, 2010; Hostinar & Cicchetti, 2018). Furthermore, ER and other self-regulatory capabilities follow a protracted developmental time course that is highly dependent on prefrontal cortex (PFC) neuromaturation (Casey, Getz, & Galvan, 2008). As elaborated below, volitional ER requires top-down, cortical modulation of bottom-up, subcortically generated affect (Heatherton, 2011). Subcortical structures that generate emotion— including emotions associated with impulsivity such as wanting and enthusiasm—mature early in life, whereas cortical structures that regulate emotion mature into young adulthood and exhibit socially-mediated neuroplastic changes in structure and function (Brain Development Cooperative Group, 2012; Casey et al., 2008). Prefrontal neuromaturation is enhanced by environmental enrichment (Kolb et al., 2012) and compromised by maltreatment (Hanson et al., 2010, 2012). Interventions that target ER improve PFC function and increase cortical-subcortical connectivity, facilitating top-down control over emotion and behavior (Opialla et al., 2015; Wheeler, Arnkoff, & Glass, 2017).
In addition, targeting ER reduces risk for emerging internalizing disorders that are (a) themselves developmental sequelae of maltreatment (Cicchetti & Toth, 2016; Hostinar & Cicchetti, in press), (b) experienced at high levels by adult women who were treated for ADHD in childhood (Babinski et al., 2011), and (c) associated with NSSI and SBs (Asarnow et al., 2011; Beauchaine, Neuhaus et al., 2015; Crowell et al., 2005, 2008; Kovacs et al., 1993). Parent and child interventions that target ER reduce both internalizing and externalizing symptoms, with effects that persist at long term follow-ups (Webster-Stratton et al., 2013).
Of note, associations between family relationship problems and NSSI are mediated by adolescent girls’ emotion dysregulation (Fruzzetti et al., 2005), as are associations between parental psychopathology and girls’ later behavior problems (Kaufman, Puzia et al., 2017). Moreover, interventions that improve children’s ER buffer them from effects of existing family relationship problems that portend NSSI (Greenberg, 2006). Finally, interventions that improve ER are effective in treating NSSI and SB among adolescents and adults (Gratz et al., 2014; Ougrin et al., 2015).
Interventions that target ER directly among young children are less common than such interventions for adolescents and adults (Kehoe & Havighurst, in press; Winiarski, Brown, Karnik, & Brennan, in press), yet recent studies indicate promise specifically for girls with ADHD (Beauchaine et al., 2015; Webster-Stratton et al., 2013). In our work using the Incredible Years (IY) parent- and child-interventions, we targeted and evaluated ER—measured multimodally via behavior observation, parent-reports, teacher-reports, and PNS responding (Beauchaine, Neuhaus et al., 2015; Bell, Shader, Webster-Stratton, Reid, & Beauchaine, 2018). IY teaches ER strategies to children, including social problem solving, coping with anger, and effective communication of emotions. In our investigations, children improved from pre- to post treatment on all measures of internalizing and externalizing behavior and on all measures of ER (Webster-Stratton et al., 2013). Effect sizes were large, and several increased at one-year followup. These improvements were accompanied by intervention-induced increases in both parentreports and behavior observations of problem solving with peers—a primary target of child training. Findings of ER improvement were replicated by an independent research group (Scott & O’Connor, 2012). Physiologically, children exhibited increases in RSA—an index of parasympathetic cardiac control—that were over 20 times larger than age-normative developmental shifts (Bell et al., 2018). Such changes in RSA are noteworthy given (1) established associations between RSA and ER (Beauchaine, 2015, Shader et al., 2018), and (2) well replicated deficits in RSA among those who engage in NSSI, suicidal ideation, and SBs (Crowell et al., 2005, 2014, 2017; Wielgus, Aldrich, Mezulis, & Crowell, 2016).
Tenet 3: Prevention Must Address Emerging Psychopathology and Peer Rejection, which Mediate Pathways from Early ADHD to Later NSSI and SB Among Girls
The Berkeley Girls with ADHD Longitudinal Study (BGALS; Hinshaw, 2002) identified three individual-level, mediators through which childhood ADHD leads to later NSSI and SBs among maltreated girls. Longitudinal analyses from BGALS indicate that (1) both externalizing and internalizing psychopathology in adolescence mediate longitudinal associations between childhood HI and adolescent/young adult NSSI and SBs, (2) early adolescent peer victimization mediates associations between childhood HI and later NSSI, and (3) early-adolescent peer rejection mediates associations between childhood HI and later suicide attempts (Meza, Owens, & Hinshaw, 2016; Owens & Hinshaw, 2016). Thus, internalizing and externalizing psychopathology, both of which are characterized by emotion dysregulation (Beauchaine et al., 2007; Hostinar & Cicchetti, in press), and peer difficulties, which are exacerbated by emotion dysregulation (Shields, Ryan, & Cicchetti, 2001), mediate development of NSSI and SB among girls with ADHD.
Virtually all interventions for ADHD—whether behavioral or pharmacological—target HI behaviors. A smaller subset also targets more severe externalizing outcomes (e.g., delinquency, aggression). Very few target ER directly or seek to prevent internalizing outcomes (depression, withdrawal). As noted above, ADHD interventions yield short-term improvements in impulsivity, but long-term effects across multiple functional domains are limited (Swanson et al., in press). For maltreated girls with ADHD, targeting HI may even be disjunctive. Without treatment, impulsivity among girls with ADHD abates in adolescence, whereas more severe externalizing behaviors, internalizing behaviors, functional impairment, NSSI, and SBs increase (Guendelman et al., 2016; Hinshaw, Owens, Sami, & Fargeon, 2006; Swanson et al., 2014). Moreover, many children who are treated for ADHD—whether male or female—experience problems in adolescence with externalizing behaviors, emotional lability, mood disorders, anxiety disorders, and peer relationships (Hechtman et al., 2016).
We have adapted empirically supported behavioral interventions for conduct problems for use with young children with HI/combined ADHD to prevent progression to oppositional behavior, delinquency, internalizing symptoms, and emotional lability in later childhood (Beauchaine et al., 2015; Webster-Stratton et al., 2013). These interventions—including parent, child, and teacher components—are effective in improving externalizing outcomes, internalizing outcomes, and peer relations among racially and ethnically diverse samples in clinic, school, foster care, CPS, and community settings (Leijten, Raaijmakers, Orobio de Castro, van den Ban, & Matthys, 2017; Letarte, Normandeau, & Allard, 2010; Webster-Stratton et al., 2013).
Such findings suggest promise in targeting known mediators of associations between ADHD in childhood and NSSI/SBs in adolescence and young adulthood among girls. Still, longer-term follow-ups are needed. Although effects maintain at two years (Reid, Webster-Stratton, & Hammond, 2003), progression of ADHD to NSSI and SBs occurs over longer time intervals, and effectiveness of the program specifically for maltreated girls with ADHD is unknown. Notably, the intervention, although developed for children with ADHD and CD, targets behaviors that characterize maltreating families, and is effective among such families (Hurlburt, Nguyen, Reid, Webster-Stratton, & Zhang, 2013). This is unsurprising given high rates of maltreatment and abuse incurred by externalizing children. To date however, no studies have evaluated long-term NSSI or SB outcomes or more proximal efficacy signals specifically among maltreated girls.
Tenet 4: Parent Training Targeting both Parenting Effectiveness and Children’s ER is an Essential Component of Prevention
Maltreating families are characterized by harsh, punitive, labile, and inconsistent parenting practices that prospectively predict a range of adverse outcomes for adolescents including psychopathology, emotion dysregulation, and both autonomic and neuroendocrine dysregulation (Bariola et al., 2007; Cicchetti, 2016; Crowell et al., 2017; Patterson et al., 2000; Nanni, Uher, & Danese, 2012). These same family dynamics and mental health outcomes characterize many children with externalizing disorders—including ADHD—even when maltreatment status is unknown, a common state-of-affairs in published studies. It is therefore unsurprising that a large literature supports the need for well-designed parent training programs to prevent diverse forms of child psychopathology, including internalizing disorders, externalizing disorders, and other conditions associated with NSSI and SBs (e.g., Eyberg, Nelson, & Boggs, 2008; McKee et al., 2014). Notably, parent training is essential for successful treatment of NSSI after it emerges (Brent et al., 2013).
In most families, parents are primary socialization agents for their children through mid-adolescence (Arnon, Shamai, & Ilatov, 2008; Cole et al., 2017). During this time, fundamental roles of parents are to model and modulate—through appropriate behavioral and emotional responding—affective reactions of their children, until children’s ER is internalized (Graziano, Calkins, & Keane, 2011). Parent-child relationships in which emotional lability is reinforced rather than regulated confer risk for offspring adjustment problems throughout life, beyond effects of heritable impulsivity (Beauchaine et al., 2017; Patterson et al., 2000). Girls with ADHD who experience family adversity, including maltreatment, exhibit more impairment in adolescence and young adulthood than those with positive parent-child relations, and are at risk for NSSI and SBs (Guendelman et al., 2016; Hinshaw et al., 2012; Swanson et al., 2014).
In families of self-injuring adolescent girls, most of whom score high on ADHD (Crowell et al., 2005), mothers escalate conflict and reinforce emotional lability rather than dampening such behaviors (Crowell et al., 2013, 2017; Stepp et al., 2012). Effective parent training reduces aversive parenting behaviors that confer risk for NSSI and SBs, including emotion dysregulation, coercion, invalidation, and maltreatment (Forgatch & Rodríguez, 2016; Skowron & Reinemann, 2005). Such programs also improve children’s ER, as indexed by behavior observation, parent- and self-reports, and autonomic reactivity during dyadic interactions (Beauchaine et al., 2015; Bell et al., 2018).
Improvements in children’s ER are mediated by reductions in the very parental behaviors (harshness, criticism, coercion, invalidation) that characterize maltreating families and families of children with ADHD and other externalizing problems (McKee et al., 2014; Wilson et al., 2008) and that increase risk for NSSI and SBs (Adrian et al., 2011). Such findings are unsurprising given that adolescent girls who engage in NSSI and SBs are exquisitely sensitive to maternal negativity, as assessed by both behavioral and RSA reactivity (Crowell et al., 2013, 2014, 2017; Stepp, Scott, Jones, Whalen, & Hipwell, 2016). Notably, treatment-induced reductions in negative parenting—including criticism, negative commands, and physical intrusions—mediate improvements in autonomic reactivity among young girls and boys with ADHD (Bell et al., 2018). Finally, parent emotion dysregulation mediates intergenerational transmission of maltreatment, making it a legitimate target of prevention on this basis alone (Smith, Cross, Winkler, Jovanovic, & Bradley, 2014).
In final important target for parent training is peer-group monitoring. By adolescence, NSSI and SBs are reinforced in peer groups via contagion, often following rejection of maltreated girls with ADHD by well-adjusted peers (Meza et al., 2016; Owens & Hinshaw, 2016). In fact, initial engagement in NSSI is usually determined by deviant peer influences (Jarvi et al., 2013). For some, self-injury engenders positive social outcomes in such peer groups (Bentley, Nock, & Barlow, 2014). Although it is difficult to alter established peer affiliations, parents have far more influence when they monitor their children before such affiliations form. Parental monitoring of adolescents’ whereabouts reduces high risk sexual activity and substance use (DiClemente et al., 2001) and confers protection from SBs among those who are bullied (Jantzer, Haffner, Parzer, Resch & Kaess, 2015). Strikingly, only about 3% of parents whose children engage in NSSI are aware of it (Baetens et al., 2015). Improved monitoring is an essential component of intervention for NSSI (Asarnow et al., 2009) and is likely to be just as important for prevention.
This emphasis on parent training to (1) eliminate reinforcement of emotional lability; (2) reduce emotion invalidation, coercion, and maltreatment; (3) increase positive interactions between parents and children; and (4) improve monitoring is a departure from programs that treat NSSI and SBs after they emerge and deviant peer groups coalesce. Despite reducing SBs and to a lesser extent NSSI (Asarnow et al., 2009, 2011; Calear et al., 2016; Garraza et al., 2015; Zalsman et al., 2016), existing programs target adolescents, who—via age-normative individuation processes—are influenced more by peers than by parents. Earlier intervention provides opportunities to leverage parental influences in prevention. Parents are included in existing community-based and clinical prevention programs for adolescents (Asarnow et al., 2017; Katz et al., 2013), but they often participate in brief educational components (Hooven, Herting, & Snedker, 2010; Hooven, Walsh, Pike, & Herting, 2012).
There is a long tradition of effective parent training that targets specific parenting behaviors discussed in this section, including interventions that are empirically supported for use with mothers who themselves have ADHD and for use among maltreating families—groups that often overlap (Chronis-Tuscano, Wang, Woods, Strickland, & Stein, 2017; Skowron & Reinemann, 2005). As outlined above, such treatments are most effective when they are multifaceted and multicomponent (parent, child) (Chronis-Tuscano et al., 2016; Webster-Stratton et al., 2004).
Evaluating Neurobiological Markers of Prevention Response
Thus far we have argued for prevention of NSSI and SBs based on identifying vulnerability and risk among girls behaviorally (by ADHD and maltreatment status)—and intervening on behavioral targets. Although we have mentioned important neurodevelopmental processes, such as bidirectional effects of PFC neuromaturation and socialization of self-control, we have not reviewed detailed findings regarding neurobiological sequelae of maltreatment or neurobiological mechanisms/correlates of self-harm. Regardless of the specific treatment target, there are several reasons why specifying neurobiological processes involved in development, maintenance, and persistence of psychopathology is advantageous for formulating more effective prevention programs (Beauchaine et al., 2008). For NSSI and SBs, a number of issues stand out as especially relevant. Perhaps most importantly, persistent impairment in children’s stress response systems and prefrontal cortex structure and function are often observed following maltreatment (e.g., Cicchetti, & Rogosch, 2012; Hanson et al., 2010). Without intervention, maltreatment-induced alterations to these neural and neurohormonal systems can confer lifelong adverse effects on motivation, mood regulation, and social affiliation—all of which have implications for emerging self-harm (Beauchaine, Neuhaus, Zalewski, Crowell, & Potapova, 2011; McEwen, Nasca, & Gray, 2016). As we review in sections to follow, maltreatment-induced functional alterations in these systems become increasingly difficult to reverse with age, but show considerable neuroplasticity in childhood following existing family interventions. Thus, prevention and early intervention may in some cases halt and even reverse neurobiological mechanisms, correlates, and sequelae of NSSI and SBs.
As this brief discussion suggests, valid biomarkers of vulnerability can be used as proximal efficacy signals of prevention response—well before more distal outcomes including NSSI and SBs can be observed or assessed. Given that highly vulnerable girls with ADHD who incur maltreatment can be identified years before the onset of NSSI and SBs, specifying proximal efficacy signals is essential if we are to evaluate immediate prevention response. The alternative of waiting until vulnerable girls develop NSSI and SBs almost certainly reduces prevention and treatment efficacy because (1) family mechanisms that promote self-harm continue into adolescence unabated, (2) additional maintaining factors including deviant peer affiliations emerge, and (3) neurobiological sequelae of maltreatment become canalized.
We now turn our attention to describing important biomechanisms and correlates of NSSI and SBs, emphasizing findings from adolescents where data are unavailable for pre-adolescents. Notably, several biological markers and correlates of self-harm that were identified initially among adults with BPD are already present among teens who engage in NSSI and SBs. We begin with autonomic function, which has been studied extensively in self-harming samples.
Autonomic Function
Numerous studies demonstrate low resting RSA among adolescent and adult females who self-injure, including those with BPD (Crowell et al., 2013; Kuo & Linehan, 2009). Excessive RSA withdrawal to strong negative emotion inductions—particularly sadness and family conflict—is also observed among self-injurers (Crowell et al., 2005, 2017). These findings are consistent with research linking low resting RSA—and in some studies RSA reactivity—to difficulties with ER in a wide range of psychiatric conditions across the lifespan (Beauchaine, 2015; Beauchaine & Crowell, in press; Geisler, Kubiak, Siewert, & Weber, 2013; Shader et al., 2018). According to contemporary theory, low RSA and excessive RSA reactivity mark tendencies toward emotion dysregulation (e.g., Beauchaine, Gatzke-Kopp, & Mead, 2007; Fortunato, Gatzke-Kopp, & Ram, 2015; Yaroslavsky, Bylsma, Rottenberg, & Kovacs, 2013). These tendencies are shaped and maintained within families at least in part through negative reinforcement of emotional lability and aggression (Beauchaine & Zalewski, 2016; Hastings et al., 2008; Skowron, Cipriano-Essel, Benjamin, Pincus, & Van Ryzin, 2013).
Several findings support this view among self-injuring adolescents. For example, Crowell and colleagues (2013) used painstaking microanalytic coding, combined with psychophysiological data acquisition, to demonstrate both behavioral and autonomic dysregulation among self-injuring adolescent girls—many of whom scored high on ADHD— during mother-daughter conflict discussions. Compared with controls, these dyads showed more conflict escalation, including anger, coercion, and maternal invalidation. Self-injuring adolescents also showed greater RSA withdrawal to their mothers’ aversive behaviors during the conflict and stronger time-linked correspondences between behavioral dysregulation (aversive outbursts) and physiological dysregulation (RSA withdrawal) (Crowell et al., 2014).
In a follow-up, Crowell et al. (2017) used nonlinear dynamic modeling to show that maternal aversive behaviors evoked RSA withdrawal for self-injuring adolescent girls but not for their depressed-only or healthy peers. Thus, self-injuring adolescent girls are exquisitely sensitive, both behaviorally and autonomically, to negative parenting practices of their mothers, including anger, coercion, criticism, and invalidation (Crowell et al., 2008, 2017). Notably, these very parenting behaviors (1) characterize maltreating families (McKee et al., 2014; Wilson et al., 2008), for whom similar findings have been reported; and (2) are targeted directly and effectively by existing interventions for both ADHD and maltreatment (e.g., Bell et al., 2018; Skowron et al., 2011).
Effects of family interventions on children’s autonomic function.
Historically, it was assumed that operating ranges of biological systems that subserve self-regulation were heritable and fixed. Yet contemporary accounts suggest otherwise. Allostatic load, adaptive calibration, and ontogenic process models all suggest that environment plays a fundamental role in functional development of virtually all biological systems (Ellis, Del Giudice, & Shirtcliff, 2017; Hinshaw, 2017; McEwen, 2017), and that extreme and protracted stress have widespread adverse effects on neural and neurohormonal development and function (Cicchetti, & Rogosch, 2012; Hanson et al., 2010, 2012; McEwen et al., 2016). Nevertheless, early intervention may forestall or even reverse impairment.
Among young children with both externalizing and internalizing disorders, autonomic dysfunction—as indexed by low resting RSA—develops gradually throughout childhood (Beauchaine et al., 2007; Koenig, Kemp, Beauchaine, Thayer, & Kaess, 2016). This finding is consistent with theories that link development of emotion dysregulation—and by extension RSA—to socialization mechanisms (Beauchaine & Zalewski, 2016; Hastings et al., 2008). As noted above, early interventions that improve parents’ and children’s ER increase children’s resting RSA in surprisingly brief periods of time. In a summer prevention program aimed at averting escalation of ADHD into more severe psychopathology among 4–6-year-olds, Bell et al. (2018) reported RSA increases among treated children that were over 20 times larger than agenormative developmental shifts. This effect was mediated by reductions in angry, coercive, critical, and invalidating parenting by mothers—behaviors that are common in maltreating families and families of children with ADHD. Moreover, both mothers and children exhibited improved ER as evaluated by behavior observations of blinded coders (Webster-Stratton et al., 2013). Thus, a multicomponent preventive intervention improved ER among both parents and children, and reductions in aversive parenting mediated intervention effects on resting RSA—a consistent correlate of NSSI, SBs, and emotion dysregulation. Such findings are important because they indicate that self-regulatory systems can be engaged and assessed—without waiting for NSSI and SBs to emerge (Sumner et al., 2018).
Limbic-hypothalamic-adrenal (L-HPA) Axis Function
A voluminous literature documents severe and often lifelong effects of maltreatment on the L-HPA axis (Carpenter, Shattuck, Tyrka, Geracioti, & Price, 2011)—the major human stress response system (Jacoby, Overfeld, Binder, & Heim, 2017; Lupien, McEwen, Gunnar, & Heim, 2009). In turn, maltreatment-induced alterations in L-HPA axis function—assessed via cortisol responding—are associated concurrently and prospectively with internalizing disorders, externalizing disorders, and problems with social competence among children and adolescents (Alink, Cicchetti, Kim, & Rogosch, 2012; Hart, Gunnar, & Cicchetti, 1995). Notably, all of these symptoms mediate progression of childhood ADHD to later NSSI and SBs among maltreated girls (Meza et al., 2016; Owens & Hinshaw, 2016).
Cortisol responding has a long history in research on SBs—particularly among adults (O’Connor, Ferguson, Green, O’Carroll, & O’Connor, 2016; O’Connor, Green, Ferguson, O’Carroll, & O’Connor, 2017). Recent studies also evaluate its associations with NSSI and SBs in adolescence (Beauchaine, Crowell et al., 2015; Kaess et al., 2012). Although findings are complex, L-HPA axis reactivity to dexamethasone (DST) challenge has been linked to prospective vulnerability to SBs and suicide across impressively long intervals (Coryell & Schlesser, 2008; although see Black, Monahan, & Winokur, 2002 for divergent findings). To date, however, such findings are restricted to adults, who sometimes show negative associations between cortisol responding and SBs, whereas adolescents and young adults often show positive associations (O’Connor, Furguson et al., 2016; Tarullo, & Gunnar, 2006).
Such discrepancies may be explained by developmental timing effects of maltreatment on neuromaturation of the L-HPA axis. Maltreated children often exhibit elevated basal cortisol (Tarullo, & Gunnar, 2006) and cortisol hyper-responding to stress (Harkness, Stewart, & Wynne-Edwards, 2011; O’Connor, Ferguson et al., 2016). Early life cortisol hyper-reactivity appears to be a neurodevelopmental adaptation to maltreatment and other forms of adversity (Lupien et al., 2009). Without intervention, repeated over-activation of the L-HPA axis results in eventual down-regulation via allostatic load (Herman et al., 2016; Lupien et al., 2009). Yet to date, only a handful of studies have evaluated L-HPA axis function specifically in NSSI samples, with mixed findings. Many of these studies include small samples of mostly males (Beauchaine, Crowell et al., 2015), even though (1) NSSI is more prevalent among girls and (2) large sex differences in L-HPA axis function exist (Kirschbaum, Wüst, & Hellhammer, 1992). Thus, whereas cortisol reactivity may be an important marker of prevention response, much remains to be learned about developmental timing effects and its value as an index of vulnerability. According to acquired capacity models (Joiner et al., 2009), repeated self-exposure to physical pain via NSSI downregulates and desensitizes normal stress responding—including L-HPA axis reactivity. Although NSSI should evoke a strong stress response, resulting habituation to pain leads to suppressed L-HPA axis function, with increased likelihood of more severe self-harm and potential for SB. Thus, girls who are maltreated and engage in NSSI may dampen an already compromised L-HPA axis.
Effects of early intervention on children and adolescents’ L-HPA axis function.
Early interventions consistently improve L-HPA axis function among children who incur early adversity (Slopen, McLaughlin, & Shonkoff, 2014). Such findings apply to pre-post assessments, assessments of diurnal rhythm, and assessments of stress reactivity. For maltreated children, interventions delivered early in life that focus on improving parent-child relationships are especially effective. For example, Cicchetti, Rogosch, Toth, and Sturge-Apple (2011) reported normalizing effects on cortisol responding among 1–3-year-old maltreated children who participated in a parent-child intervention. In an older sample of maltreated 3–6-year-olds, Fisher, Stoolmiller, Gunnar, and Burraston (2007) reported a normalized pattern of diurnal cortisol among those who received a family-based intervention compared with those who did not.
Few studies of intervention effects on cortisol responding have included older children or adolescents. Among those that have, none have recruited ADHD or maltreated samples (Slopen et al., 2014). However, children and adolescents who participated in an intervention to improve caregiver–child relationships following death of a parent showed greater cortisol responding six years post-treatment compared with controls (Luecken et al., 2010). Such findings are potentially important because early life bereavement produces patterns of cortisol responding that are similar to those induced by maltreatment, with effects that last into adulthood without intervention (Tyrka et al., 2008). Thus, early intervention holds considerable promise in altering potentially lifelong patterns of aberrant stress responding among those who incur maltreatment. Such findings have led to calls to initiate early preventive interventions that forestall adverse neurobiological and psychological sequelae of trauma (Dyregrov & Regel, 2011). For girls with ADHD who are maltreated, such sequelae include L-HPA axis dysfunction, NSSI, and SBs.
Central Nervous System Function
Very little is known about central nervous system (CNS) substrates of NSSI and SBs, or about prospective CNS vulnerabilities vs. sequelae among pre-adolescent girls. Yet hypotheses about relevant brain regions and circuits can be derived from research conducted with young adults and adolescents, and from imaging literatures on comorbidities (depression, BPD) and transdiagnostic vulnerabilities (impulsivity, emotion dysregulation) associated with NSSI.
Subcortical neural function.
A well replicated transdiagnostic vulnerability to ADHD and internalizing disorders is deficient striatal responding in anticipation of incentives (see Beauchaine & Constantino, 2017; Luking, Pagliaccio, Luby, & Barch, 2016). Altered striatal reward processing likely confers vulnerability to heterotypic comorbidity through reduced positive affectivity and hedonic capacity (Forbes & Dahl, 2005; Zisner & Beauchaine, 2016b). Blunted striatal responding is associated with lower self-reports of positive affect, and low levels of striatal DA predict trait irritability, which characterizes ADHD, NSSI, and internalizing disorders (Forbes et al., 2009; Zisner & Beauchaine, 2016b). In addition, although very little research has been conducted with children or adolescents, the amygdala has received particular attention in relation to NSSI and related traits such as BPD among adults. This attention follows from the role the amygdala plays in valuing emotional salience, and, when lesioned, impulsivity (Bechara, Damasio, Damasio, & Lee, 1999; Winstanley, Theobald, Cardinal, & Robbins, 2004).
Limited research that evaluates neural function in these subcortical brain regions with self-injuring adolescents finds effects consistent with expectations. For example, we recently found— in a substance-free sample of self-injuring adolescent girls, most of whom also scored high on ADHD—reduced neural activation in both the striatum and the orbitofrontal cortex (OFC) during reward anticipation using a monetary-incentive delay task in which participants earned money on some trials and lost money on others (Sauder, Derbidge, & Beauchaine, 2016). The OFC is a cortical structure implicated in valuing reward magnitudes, planning, and impulse control, among other functions (Stalnaker, Cooch & Schoenbaum, 2015). We also found reduced amygdala activation in the same task. Consistent with its role in salience detection, the amygdala is implicated in tracking hedonic value of incentives (Liu et al., 2011).
These findings indicate that self-injuring adolescents are less responsive to external incentives than controls, and exhibit patterns of neural responding that are similar to those observed in ADHD and depression. The same pattern of findings during reward anticipation characterizes adults with BPD (Herbort et al., 2016; Lis, Greenfield, Henry, Guile, & Dougherty, 2007). Other research finds amygdala hypoactivation to emotionally evocative cues among self-injuring adolescents and adults with BPD (Plener, Bubalo, Fladung, Ludolph, & Lulé, 2012; Rosenthal et al., 2008). Thus, self-harming adolescents and adults with BPD show similar patterns of neural responding to incentives and emotion evocation. These findings provide support for initiating prevention before adolescence, given that deficiencies in structural and functional neuromaturation of subcortical structures (1) are implicated in development of both ADHD and NSSI, and (2) are exacerbated by stress, maltreatment, and other environmental adversities (Brain Development Research Group, 2012; Birn, Roeber, & Pollak, 2017; Hanson et al., 2010, 2012).
Cortical neural function and cortical-subcortical interactions.
The brain functions as a set of distributed neural networks that coordinate to subserve behavioral and emotional responding (Casey, Galván, & Somerville, 2016). The striatum and amygdala, discussed above, are subcortical structures involved in generating emotional responses (Beauchaine, 2015; Birn et al., 2017; Panksepp, 2017), whereas volitional regulation of emotion occurs through top-down inhibition of subcortical structures by functional subdivisions of the PFC. Top-down regulation of impulsivity and anxiety are effected through inhibition of striatal activity and reactivity by the OFC and dlPFC, and inhibition of amygdalar activity and reactivity by the lateral and medial PFC, respectively (Davidson, 2002; Heatherton, 2011; Tone, Garn, & Pine, 2016). Furthermore, the insular cortex, which integrates perceptual, emotional, and cognitive information (Kurth, Zilles, Fox, Laird, & Eickhoff, 2010), plays an integral role in regulating negative emotion (Goldin, McRae, Ramel, & Gross, 2008).
Structural and functional abnormalities in these cortical regions are observed among adults with BPD, most of whom are impulsive, many of whom self-injure, and many of whom incurred maltreatment earlier in life. Among other findings, adults with BPD exhibit reduced resting blood flow in the OFC (Wolf et al., 2012), decreased ventromedial PFC activation during negative mood induction (Silbersweig et al., 2010), impaired amygdala-frontal connectivity when exposed to emotion cues (Krause-Utz et al., 2014), and abnormalities in both structure and function of the insular cortex (King-Cases et al., 2008; Krause-Utz, Winter, Niedtfeld, & Schmahl, 2014; Lis et al., 2007).
Studies of self-injuring adolescent girls who score high on ADHD yield similar results. For example, reduced insular cortex and inferior frontal gyrus (IFG) volumes are observed among such girls compared with controls (Beauchaine et al., 2018). The IFG is adjacent to the insular cortex and is also implicated in emotion regulation (Grecucci, 2013). Decreased insular cortex volumes are also observed among adolescents at first presentation with BPD (Takahashi et al., 2009), and correlate positively with ER capabilities among adults with BPD (Bruehl et al., 2013).
Thus, research on neuroanatomical and functional correlates of NSSI among adolescents indicates neural correlates of emotion dysregulation. It also demonstrates that at least some CNS correlates of BPD are present in the teen years. Whether such structural and functional abnormalities are evident in childhood, or whether they are amenable to intervention, is unknown. However, it is well established that environmental adversity during childhood—including maltreatment and other forms of trauma—alters subcortical and cortical neurodevelopment in these very structures beginning as early as infancy, with effects that persist at least into adolescence and likely beyond (Birn et al., 2017; Dannlowski et al., 2012; Hanson et al., 2010, 2012; Whittle et al., 2013).
This review suggests that prevention and early intervention may be essential for halting/reversing vulnerability to NSSI and SBs among maltreated young girls with ADHD. Cortical brain regions undergo massive structural and functional reorganization and neuromaturation throughout adolescence (Brain Development Cooperative Group, 2012; Casey et al., 2016). This restructuring affects executive control and ER, both of which improve markedly among typically developing teens (Heller, Cohen, Dreyfuss, & Casey, 2016) but are compromised among self-injuring girls with ADHD. Effects of trauma—including maltreatment—on neuromaturation are often wide-ranging across neural systems and far-reaching across development (Gee & Casey, 2015). Prevention programs hold potential to capitalize on neural plasticity during childhood and emerging adolescence in brain regions that are critical to ER, mood regulation, executive function, and social affiliation (Beauchaine et al., 2008; Davidson & McEwen, 2012). Given their protracted developmental courses and neuroplasticity in response to environments, cortical structure and function are likely to mark prevention response.
Summary and Conclusions
We are not the first authors to (1) call attention to the need for early intervention for NSSI and SBs; (2) identify ADHD, maltreatment, and their interaction as risk factors for NSSI and SBs; (3) specify neurobiological correlates of NSSI and SBs; or (4) review the roles of parenting and maltreatment on developing self-regulatory functions brain systems among children. These points have been made more elegantly and thoroughly by others cited herein. The fundamental contribution of this review lies in combining these principles and applying them in an integrated strategy for preventing the second leading cause of death in the US among adolescents and young adults: suicide. NSSI remains a strong predictor of eventual suicide, yet despite our best efforts in formulating interventions, it remains exceedingly difficult to treat once established. Thus, even though existing prevention and intervention programs are essential for reducing morbidity and mortality among self-injuring adolescents, much work remains toward reducing vulnerability if we are to approach Zero Suicide objectives.
To date, low base rates of SBs and suicide have precluded ascertainment of vulnerability with enough validity/efficiency to make recruitment into prevention programs feasible. Yet data from multiple sources now indicate that preadolescent girls with ADHD who incur maltreatment are at alarming risk for NSSI (33%) and SBs (50%) by late adolescence and early adulthood. Alone, sex, ADHD, and maltreatment do not confer sufficient vulnerability for recruitment into prevention programs. Combined, however, their effects are so potent that devising effective prevention programs should be a national priority for this growing public health concern. In fact, this level of risk places the onus on the research community to devise prevention programs for preadolescents—particularly given limits of current interventions for adolescents who already engage in self-harm. Notably, rates of NSSI and SBs are projected to increase into the future as current early starters move into an age range in which attempts become more common (AFSP, 2017; Owens, Zalecki, Gillette, & Hinshaw, 2017).
Existing, effective interventions alter family and peer socialization mechanisms through which emotional lability, emotion dysregulation, and eventual NSSI and SBs are shaped and maintained. These mechanisms, including aversive parenting, invalidation, negative reinforcement of emotional lability and anger, peer contagion, peer reinforcement, and maltreatment itself, are targeted and altered by multifaceted parent- and child-interventions that are effective among children with ADHD and other externalizing behaviors—including those reared in families with histories of maltreatment (Hurlburt et al., 2013; Skowron & Reinemann, 2005). Although not yet used specifically for targeted prevention of NSSI and SBs among maltreated girls with ADHD, such interventions exert measurable changes in proximal biological outcomes including PNS and L-HPA axis function. CNS targets are also likely malleable, engaged, and changed by effective prevention. These biological efficacy signals provide means of assessing prevention response in “real time,” which is essential given that ultimate behavioral targets—including NSSI and suicide attempts—are distal. As we review herein, alarmingly high premorbid risk can now be identified through conjoint effects of sex, ADHD status, and maltreatment. Given known capacity for early identification, waiting to intervene until NSSI and SBs are imminent or have already emerged is analogous to waiting for chest pains to evolve before attempting “prevention” of coronary artery disease.
Taken together, the literature reviewed above indicates that the time has come to target preadolescent girls with ADHD who have also incurred maltreatment for prevention of NSSI, SBs, and eventual suicide. Although Zero Suicide is still an extremely ambitious long-term goal, the research community must begin to address this growing public health concern earlier in life for vulnerable individuals.
Acknowledgments
Research reported in this article was supported by Grants DE025980, MH63699, MH67192, MH12209, MH074196, and MH86198 from the National Institutes of Health, and by the National Institutes of Health Science of Behavior Change (SoBC) Common Fund.
Footnotes
More boys die by suicide than girls. Our focus on girls is not intended to overlook boys. Rather, no known combination of vulnerabilities and adversities identifies boys who are at similar levels of risk for NSSI and SBs as the girls discussed herein.
Contributor Information
Theodore P. Beauchaine, Department of Psychology, The Ohio State University
Stephen P. Hinshaw, Departments of Psychology and Psychiatry, The University of California, Berkeley; University of California, San Francisco
Jeffrey A. Bridge, Center for Suicide Prevention and Research, The Research Institute at Nationwide Children’s Hospital, Columbus, OH
References
- Adrian M, Zeman J, Erdley C, Lisa L, & Sim L (2011). Emotional dysregulation and interpersonal difficulties as risk factors for nonsuicidal self-injury in adolescent girls. Journal of Abnormal Child Psychology, 39, 389–400. doi: 10.1007/s10802-010-9465-3 [DOI] [PubMed] [Google Scholar]
- Ahmad SI, & Hinshaw SP (2016). ADHD, trait impulsivity, and externalizing behavior in a longitudinal sample. Journal of Abnormal Child Psychology, 45, 1077–1089. doi: 10.1007/s10802-016-0226-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alink LRA, Cicchetti D, Kim J, & Rogosch FA (2012). Longitudinal associations among child maltreatment, social functioning, and cortisol regulation. Developmental Psychology, 48, 224–236. doi: 10.1037/a0024892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allely CS (2014). The association of ADHD symptoms to self-harm behaviours: A systematic PRISMA review. BMC Psychiatry, 14, 133. doi: 10.1186/1471-244X-14-133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Foundation for Suicide Prevention (2017). Suicide statistics. Retrieved from https://afsp.org/about-suicide/suicide-statistics/on11/22/2017.
- Ammerman BA, Jacobucci R, Kleiman EM, Uyeji L, & McCloskey MS (2017). The relationship between nonsuicidal self-injury age of onset and severity of self-harm. Suicide and Life-Threatening Behavior. epublished ahead of print. doi: 10.1111/sltb.12330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnon S, Shamai S, & Ilatov Z (2008). Socialization agents and activities of young adolescents. Adolescence, 43, 373–397. [PubMed] [Google Scholar]
- Auerbach RP, Kim JC, Chango JM, Spiro WJ, Cha C, Gold J, …Nock MK (2014). Adolescent nonsuicidal self-injury: Examining the role of child abuse, comorbidity, and disinhibition. Psychiatry Research, 220, 579–584. doi: 10.1016/j.psychres.2014.07.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow JR, Berk MS, & Baraff LJ (2009). Family Intervention for Suicide Prevention: A specialized emergency department intervention for suicidal youths. Professional Psychology: Research and Practice, 40, 118–125. doi: 10.1037/a0012599 [DOI] [Google Scholar]
- Asarnow JR, Hughes JL, Babeva KN, & Sugar CA (2017). Cognitive-behavioral family treatment for suicide attempt prevention: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 56, 506–514. doi: 10.1016/j.jaac.2017.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow JR, Porta G, Spirito A, Emslie G, Clarke G, Wagner KD, …Brent DA (2011). Suicide attempts and nonsuicidal self-injury in the treatment of resistant depression in adolescents: Findings from the TORDIA study. Journal of the American Academy of Child and Adolescent Psychiatry, 50, 772–781. doi: 10.1016/j.jaac.2011.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach RP, Kim JC, Chango JM, Spiro WJ, Cha C, Gold J, Esterman M, & Nock MK (2014). Adolescent nonsuicidal self-injury: Examining the role of child abuse, comorbidity, and disinhibition. Psychiatry Research, 220, 579–584. doi: 10.1016/j.psychres.2014.07.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babinski DE, Pelham WE, Molina BSG, Gnagy EM, Waschbusch DA, Yu J, …Karch KM (2011). Late adolescent and young adult outcomes of girls diagnosed with ADHD in childhood: An exploratory investigation. Journal of Attention Disorders, 15, 204–214. doi: 10.1177/1087054710361586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baetens I, Claes L, Onghena P, Grietens H, Van Leeuwen K, Pieters C, …Griffith JW (2015). The effects of nonsuicidal self-injury on parenting behaviors: A longitudinal analysis of the perspective of the parent. Child and Adolescent Psychiatry and Mental Health, 9, 24. doi: 10.1186/s13034-015-0059-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldessarini RJ, Finklestein S, & Arana GW (1983). The predictive power of diagnostic tests and the effect of prevalence of illness. Archives of General Psychiatry, 40, 569–573. doi: 10.1001/archpsyc.1983.01790050095011 [DOI] [PubMed] [Google Scholar]
- Bariola E, Eleonora E, & Hughes EK (2007). Child and adolescent emotion regulation: The role of parental emotion regulation and expression. Clinical Child and Family Psychology Review, 14, 198–212. doi.org/10.1007/s10567-011-0092-5 [DOI] [PubMed] [Google Scholar]
- Barker ED, Arseneault L, Brendgen M, Fontaine N, & Maughan B (2008). Joint development of bullying and victimization in adolescence: Relations to delinquency and selfharm. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 1030–1038. doi: 10.1097/CHI.ObO13e31817eec98 [DOI] [PubMed] [Google Scholar]
- Beauchaine TP (2015). Future directions in emotion dysregulation and youth psychopathology. Journal of Clinical Child and Adolescent Psychology, 44, 875–896. doi: 10.1080/15374416.2015.1038827 [DOI] [PubMed] [Google Scholar]
- Beauchaine TP (in press). A developmental psychopathology perspective on the emergence of antisocial and borderline personality pathologies across the lifespan In Lejuez CW & Gratz KL (Eds.), Handbook of personality disorders. New York: Cambridge University Press. [Google Scholar]
- Beauchaine TP, & Constantino JN (2017). Redefining the endophenotype concept to accommodate transdiagnostic vulnerabilities and etiological complexity. Biomarkers in Medicine, 11, 769–780. doi: 10.221/bmm-2017-0002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, & Crowell SE (eds.) (in press). The Oxford handbook of emotion dysregulation. New York: Oxford University Press. [Google Scholar]
- Beauchaine TP, Crowell SE, & Hsiao R (2015). Post-dexamethasone cortisol, self-inflicted injury, and suicidal ideation among depressed adolescent girls. Journal of Abnormal Child Psychology, 43, 619–632. doi: 10.1007/s10802-014-9933-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Gatzke-Kopp L, & Mead HK (2007). Polyvagal theory and developmental psychopathology: Emotion dysregulation and conduct problems from preschool to adolescence. Biological Psychology, 74, 174–184. doi: 10.1016/j.biopsycho.2005.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Klein DN, Crowell SE, Derbidge C, & Gatzke-Kopp LM (2009). Multifinality in the development of personality disorders: A Biology × Sex × Environment interaction model of antisocial and borderline traits. Development and Psychopathology, 21, 735–770. doi: 10.1017/S0954579409000418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, & McNulty T (2013). Comorbidities and continuities as ontogenic processes: Toward a developmental spectrum model of externalizing behavior. Development and Psychopathology, 25, 1505–1528. doi: 10.1017/S0954579413000746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Neuhaus E, Brenner SL, & Gatzke-Kopp L (2008). Ten good reasons to consider biological processes in prevention and intervention research. Development and Psychopathology, 20, 745–774. doi: 10.1017/S0954579408000369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Neuhaus E, Gatzke-Kopp LM, Reid MJ, Brekke A, Olliges A, Welch S, & Webster-Stratton C (2015). Electrodermal responding predicts responses to, and may be altered by, preschool intervention for ADHD. Journal of Consulting and Clinical Psychology, 83, 293–303. doi: 10.1037/a0038405 [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Neuhaus E, Zalewski M, Crowell SE, & Potapova N (2011). Effects of allostatic load on neural systems subserving motivation, mood regulation, and social affiliation. Development and Psychopathology, 23, 975–999. doi: 10.1017/S0954579411000459 [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Sauder CL, Derbidge CM, & Uyeji LL (2018). Self-injuring adolescent girls exhibit insular cortex volumetric abnormalities that are similar to those seen in adults with borderline personality disorder. Manuscript under revision. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP & Zalewski M (2016). Physiological and developmental mechanisms of emotional lability in coercive relationships In Dishion TJ & Snyder JJ (Eds.), Oxford handbook of coercive relationship dynamics (pp. 39–52). New York: Oxford University Press. [Google Scholar]
- Beauchaine TP, Zisner A, & Sauder CL (2017). Trait impulsivity and the externalizing spectrum. Annual Review of Clinical Psychology, 13, 343–368. doi: 10.1146/annurev-clinpsy-021815-093253 [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio H, Damasio AR, & Lee GP (1999). Different contributions of the human amygdala and ventromedial prefrontal cortex to decision-making. Journal of Neuroscience, 19, 5473–5481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell Z, Shader TM, Webster-Stratton C, Reid MJ, & Beauchaine TP (2018). Improvements in negative parenting mediate changes in children’s autonomic responding following a preschool intervention for ADHD. Clinical Psychological Science, 6, 134–144. doi: 10.1177/2167702617727559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman AL, Jobes DA, & Silverman MM (2006). Adolescent suicide: Assessment and intervention (2nd ed.). Washington, DC: American Psychological Association. [Google Scholar]
- Bernier A, Carlson SM, & Whipple N (2010). From external regulation to self-regulation: Early parenting precursors of young children’s executive functioning. Child Development, 81, 326–339. doi: 10.1111/j.1467-8624.2009.01397.x [DOI] [PubMed] [Google Scholar]
- Belsky J, & de Haan M (2010). Annual Research Review: Parenting and children’s brain development: The end of the beginning. Journal of Child Psychology and Psychiatry, 52, 409–428. doi: 10.1111/j.1469-7610.2010.02281.x [DOI] [PubMed] [Google Scholar]
- Bentley KH, Nock MK, & Barlow DH (2014). The four-function model of nonsuicidal self-injury: Key directions for future research. Clinical Psychological Science, 2, 638–656. doi: 10.1177/2167702613514563 [DOI] [Google Scholar]
- Birn RM, Roeber BJ, & Pollak SD (2017). Early childhood stress exposure, reward pathways, and adult decision making. Proceedings of the National Academy of Sciences. Epublished ahead of print. doi: 10.1073/pnas.1708791114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black DW, Monahan PO, & Winokur G (2002) The relationship between DST results and suicidal behavior. Annals of Clinical Psychiatry, 14, 83–88. doi: 10.1023/A:101683940 [DOI] [PubMed] [Google Scholar]
- Blumenthal SJ, & Kupfer DJ (Eds.). (1990). Suicide over the life cycle. Washington, DC: American Psychiatric Press. [Google Scholar]
- Brain Development Cooperative Group (2012). Total and regional brain volumes in a population-based normative sample from 4 to 18 years: The NIH MRI Study of Normal Brain Development. Cerebral Cortex, 22, 1–12. doi: 10.1093/cercor/bhr018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent D (2011). Nonsuicidal self-injury as a predictor of suicidal behavior in depressed adolescents. American Journal of Psychiatry, 168, 452–454. doi: 10.1176/appi.ajp.2011.11020215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent D, McMakin DL, Kennard BD, Goldstein TR, Mayes TL, & Douaihy AB (2013). Protecting adolescents from self-harm: A critical review of intervention studies. Journal of the American Academy of Child and Adolescent Psychiatry, 52, 1260–1271. doi: 10.1016/j.jaac.2013.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bresin K (2014). Five indices of emotion regulation in participants with a history of nonsuicidal self-injury: A daily diary study. Behavior Therapy, 45, 56–66. doi: 10.1016/j.beth.2013.09.005 [DOI] [PubMed] [Google Scholar]
- Bresin K, & Gordon KH (2013). Endogenous opioids and nonsuicidal self-injury: A mechanism of affect regulation. Neuroscience and Biobehavioral Reviews, 37, 374–383. doi: 10.1016/j.neubiorev.2013.01.020 [DOI] [PubMed] [Google Scholar]
- Bruehl H, Preißler S, Heuser I, Heekeren HR, Roepke S, & Dziobek I (2013). Increased prefrontal cortical thickness is associated with enhanced abilities to regulate emotions in PTSD-free women with borderline personality disorder. PLOS One, 8, e65584. doi: 10.1371/journal.pone.0065584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calear AL, Christensen H, Freeman A, Fenton K, Busby J, Bregje G, …Donker T (2016). A systematic review of psychosocial suicide prevention interventions for youth. European Child and Adolescent Psychiatry, 25, 467–482. doi: 10.1007/s00787-015-0783-4 [DOI] [PubMed] [Google Scholar]
- Carpenter LL, Shattuck TT, Tyrka AR, Geracioti TD, & Price LH (2011). Effect of childhood physical abuse on cortisol stress response. Psychopharmacology, 214, 367–375. doi: 10.1007/s00213-010-2007-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BJ, Galván A, & Somerville LH, (2016) Beyond simple models of adolescence to an integrated circuit-based account: A commentary. Developmental Cognitive Neuroscience, 17, 128–130. doi: 10.1016/j.dcn.2015.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BJ, Getz S, & Galvan A (2008). The adolescent brain. Developmental Review, 28, 62–77. doi: 10.1016/j.dr.2007.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control. (2014). National suicide statistics. Retrieved from https://www.cdc.gov/violenceprevention/suicide/statistics/on11/8/2017.
- Centers for Disease Control. (2008). Web-based injury statistics query and reporting system (WISQARS) nonfatal injuries: Nonfatal injury reports. Atlanta, GA: National Center for Injury Prevention Control. [Google Scholar]
- Centers for Disease Control. (2006). CDC injury fact book. Atlanta, GA: National Center for Injury Prevention Control. [Google Scholar]
- Chaffin M, Silovsky JF, Funderburk B, Valle LA, Brestan EV, Balachova T, …Bonner BL (2004). Parent–child interaction therapy with physically abusive parents: Efficacy for reducing future abuse reports. Journal of Consulting and Clinical Psychology, 72, 500–510. doi: 10.1037/0022-006X.72.3.500 [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Lewis-Morrarty E, Woods KE, O’Brien KA, Mazursky-Horowitz H, & Thomas SR (2016). Parent–Child Interaction Therapy with emotion coaching for preschoolers with ADHD. Cognitive and Behavioral Practice, 23, 62–78. doi: 10.1016/j.cbpra.2014.11.001 [DOI] [Google Scholar]
- Chronis-Tuscano A, Molina BSG, Pelham WE, Applegate B, Dahlke A, Overmyer M, & Lahey BB (2010). Very early predictors of adolescent depression and suicide attempts in children with ADHD. Archives of General Psychiatry, 67, 1044–1051. doi: 10.1001/archgenpsychiatry.2010.127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Wang CH, Woods KE, Strickland J, & Stein MA (2017). Parent ADHD and evidence-based treatment for their children: Review and directions for future research. Journal of Abnormal Child Psychology, 45, 501–517. doi: 10.1007/s10802-016-0238-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D (2016). Socioemotional, personality, and biological development: Illustrations from a multilevel developmental psychopathology perspective on child maltreatment. Annual Review of Psychology, 67, 187–211. doi: 10.1146/annurev-psych-122414-033259 [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Rogosch FA (2012). Neuroendocrine regulation and emotional adaptation in the context of child maltreatment. Monographs of the Society for Research in Child Development, 77, 87–95. doi: 10.1111/j.1540-5834.2011.00666.x [DOI] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL, & Sturge-Apple ML (2011). Normalizing the development of cortisol regulation in maltreated infants through preventive interventions. Development and Psychopathology, 23, 789–800. doi: 10.1017/S0954579411000307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, & Toth SL (2016). Child maltreatment and developmental psychopathology: A multilevel perspective In Cicchetti D (ed.), Developmental psychopathology Vol. 3: Maladaptation and psychopathology (pp. 1–56). Hoboken, NJ: Wiley; [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole PM, Hall SE, & Hajal NJ (2017). Emotion dysregulation as a vulnerability to psychopathology In Beauchaine TP & Hinshaw SP (eds.), Child and adolescent psychopathology (3rd ed., pp. 346–386). Hoboken, NJ: Wiley. [Google Scholar]
- Coryell W, & Schlesser MA (2008). The dexamethasone suppression test and suicide prediction. American Journal of Psychiatry, 158, 748–753. doi: 10.1176/appi.ajp.158.5.748 [DOI] [PubMed] [Google Scholar]
- Crowell SE, Baucom BR, McCauley E, Potapova NV, Fitelson M, Barth H, …Beauchaine TP (2013). Mechanisms of contextual risk for adolescent self-injury: Invalidation and conflict escalation in mother–child interactions. Journal of Clinical Child and Adolescent Psychology, 42, 467–480. doi.org/10.1080/15374416.2013.785360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowell SE, Baucom BR, Yaptangco M, Bride D, Hsiao R, McCauley E, & Beauchaine TP (2014). Emotion dysregulation and dyadic conflict in depressed and typical adolescents: Evaluating concordance across psychophysiological and observational measures. Biological Psychology, 98, 50–58. doi: 10.1016/j.biopsycho.2014.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, & Linehan M (2009). A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin, 135, 495–510. doi: 10.1037/a0015616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, McCauley E, Smith C, Stevens AL, & Sylvers P (2005). Psychological, autonomic, and serotonergic correlates of parasuicidal behavior in adolescent girls. Development and Psychopathology, 17, 1105–1127. doi: 10.1037/0022-006X.73.3.371 [DOI] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, McCauley E, Smith CJ, Vasilev CA, & Stevens AL (2008). Parent-child interactions, peripheral serotonin, and self-inflicted injury in adolescents. Journal of Consulting and Clinical Psychology, 76, 15–21. doi: 10.1037/0022-006X.76.1.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowell SE, Butner J, Wiltshire TJ, Munion AK, Yaptangco M, & Beauchaine TP (2017). Evaluating emotional and biological sensitivity to maternal behavior among depressed and self-injuring adolescent girls using nonlinear dynamics. Clinical Psychological Science, 5, 272–285. doi: 10.1177/2167702617692861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowell SE, Derbidge C, & Beauchaine TP(2014). Developmental approaches to understanding self-injury and suicidal behaviors In Nock MK (Ed.), Oxford handbook of suicide and self-injury (pp. 183–205). New York: Oxford University Press. [Google Scholar]
- Crowell SE, Kaufman E, & Beauchaine TP (2014). A biopsychosocial model of borderline personality development: Theory and empirical evidence In Tackett J & Sharp C (Eds.), Handbook of borderline personality disorder in children and adolescents (pp. 143–158). New York: Springer. [Google Scholar]
- Dakil SR, Sakai C, Lin H, & Flores G (2011). Recidivism in the child protection system. Archives of Pediatric and Adolescent Medicine, 165, 1006–1012. doi: 10.1001/archpediatrics.2011.129 [DOI] [PubMed] [Google Scholar]
- Dannlowski U, Stuhrmann A, Beutelmann V, Zwanzger P, Lenzen T, Grotegerd D, …Bauer J (2012). Limbic scars: Long-term consequences of childhood maltreatment revealed by functional and structural magnetic resonance imaging. Biological Psychiatry, 71, 286–293. doi: 10.1016/j.biopsych.2011.10.021 [DOI] [PubMed] [Google Scholar]
- Davidson RJ (2002). Anxiety and affective style: Role of prefrontal cortex and amygdala. Biological Psychiatry, 51, 68–80. doi:10.1016=S0006-3223(01)01328-2 [DOI] [PubMed] [Google Scholar]
- Davidson RJ, & McEwen BS (2012). Social influences on neuroplasticity: Stress and interventions to promote well-being. Nature Neuroscience, 15, 689–695. doi: 10.1038/nn.3093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis T, Mauss I, Lumian D, Troy AS, Shallcross AJ, Zarolia P, …McRae K (2014). Emotional reactivity and emotion regulation among adults with a history of self-harm: Laboratory self-report and functional MRI evidence. Journal of Abnormal Psychology, 123, 499–509. doi: 10.1037/a0036962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Crosby R, Sionean C, Cobb BK, Harrington K, …Oh MK. (2001). Parental monitoring: Association with adolescents’ risk behaviors. Pediatrics, 107, 1363–1368. doi: 10.1542/peds.107.6.1363 [DOI] [PubMed] [Google Scholar]
- Dix T (1991). The affective organization of parenting: Adaptive and maladaptive processes. Psychological Bulletin, 110, 3–25. doi: 10.1037/0033-2909.110.1.3 [DOI] [PubMed] [Google Scholar]
- Dyregrov A, & Regel S (2011). Early interventions following exposure to traumatic events: Implications for practice from recent research. Journal of Loss and Trauma, 17, 271–291. doi.org/10.1080/15325024.2011.616832 [Google Scholar]
- Ellis BJ, Del Giudice M, & Shirtcliff EA (2017). The adaptive calibration model of stress responsivity: Concepts, findings, and implications for developmental psychopathology In Beauchaine TP & Hinshaw SP (Eds.), Child and adolescent psychopathology (3rd ed., pp. 237–276). Hoboken, NJ: Wiley. [Google Scholar]
- Eyberg SM, Nelson MM, & Boggs SR (2008). Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child and Adolescent Psychology, 37, 215–237. doi: 10.1080/15374410701820117 [DOI] [PubMed] [Google Scholar]
- Fisher PA, Stoolmiller M, Gunnar MR, & Burraston BO (2007). Effects of a therapeutic intervention for foster preschoolers on diurnal cortisol activity. Psychoneuroendocrinology, 32, 892–905. doi: 10.1016/j.psyneuen.2007.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes EE, & Dahl RE (2005). Neural systems of positive affect: Relevance to understanding child and adolescent depression? Development and Psychopathology, 17, 827–850. doi: 10.1017/S095457940505039X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes EE, Hariri AH, Martin SL, Silk JS, Moyles DL, Fisher PM, …Dahl RE (2009). Altered striatal activation predicting real-world positive affect in adolescent major depressive disorder. American Journal of Psychiatry, 166, 64–73. doi: 10.1176/appi.ajp.2008.07081336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forgatch MS, & Rodríguez MMD (2016). Interrupting coercion: The iterative loops among theory, science, and practice. In Dishion TJ & Snyder JJ (eds.), Oxford handbook of coercive relationship dynamics (pp. 194–214). New York: Oxford University Press. [Google Scholar]
- Fortunato CK, Gatzke-Kopp LM, & Ram N (2015). Associations between respiratory sinus arrhythmia reactivity and internalizing and externalizing symptoms are emotion specific. Cognitive and Affective Behavioral Neuroscience, 13, 238–251. doi: 10.3758/s13415-012-0136-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox KR, Millner AJ, Mukerji CE, & Nock MK (2017). Examining the role of sex in self-injurious thoughts and behaviors. Clinical Psychology Review. Epublished ahead of print. doi: 10.1016/j.cpr.2017.09.009 [DOI] [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, …Nock MK (2017). Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin, 143, 187–232. doi: 10.1037/bul0000084 [DOI] [PubMed] [Google Scholar]
- Fruzzetti AE, Shenk C, & Hoffman PD (2005). Family interaction and the development of borderline personality disorder: A transactional model. Development and Psychopathology, 17, 1007–1030. doi: 10.1017/S0954579405050479 [DOI] [PubMed] [Google Scholar]
- Garraza LG, Walrath C, Goldston DB, Reid H, & McKeon R (2015). Effect of the Garrett Lee Smith Memorial Suicide Prevention Program on suicide attempts among youths. JAMA Psychiatry, 72, 1143–1149. doi: 10.1001/jamapsychiatry.2015.1933 [DOI] [PubMed] [Google Scholar]
- Gee DG, & Casey BJ (2015). The impact of developmental timing for stress and recovery. Neurobiology of Stress, 1, 184–194. doi: 10.1016/j.ynstr.2015.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisler FCM, Kubiak T, Siewert K, & Weber H (2013). Cardiac vagal tone is associated with social engagement and self-regulation. Biological Psychology, 93, 279–286. doi: 10.1016/j.biopsycho.2013.02.013 [DOI] [PubMed] [Google Scholar]
- Goldin PR, McRae K, Ramel W, & Gross JJ (2008). The neural bases of emotion regulation: Reappraisal and suppression of negative emotion. Biological Psychiatry, 63, 577–586. doi: 10.1016/j.biopsych.2007.05.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman SJ, D’Angelo EJ, & DeMaso DR (1993). Psychopathology in the families of children and adolescents with borderline personality disorder. American Journal of Psychiatry, 150, 1832–1835. doi: 10.1176/ajp.150.12.1832 [DOI] [PubMed] [Google Scholar]
- Goldsmith HH, Pollak SD, & Davidson RJ (2008). Developmental neuroscience perspectives on emotion regulation. Child Development Perspectives, 2, 132–140. doi: 10.1111/j.1750-8606.2008.00055.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL (2007). Targeting emotion dysregulation in the treatment of self-injury. Journal of Clinical Psychology, 63, 1091–1103. doi: 10.1002/jclp.20417 [DOI] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2008). The relationship between emotion dysregulation and deliberate self-harm among female undergraduate students at an urban commuter university. Cognitive Behaviour Therapy, 37, 14–25. doi: 10.1080/16506070701819524 [DOI] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, & Levy R (2014). Randomized controlled trial and uncontrolled 9month follow-up of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality disorder. Psychological Medicine, 44, 2099–2112. doi: 10.1017/S0033291713002134 [DOI] [PubMed] [Google Scholar]
- Graziano PA, Calkins SD, & Keane SP (2011). Sustained attention development during the toddlerhood to preschool period: associations with toddlers’ emotion regulation strategies and maternal behaviour. Infant and child development 20, 389–408. doi: 10.1002/icd.731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grecucci A, Giorgetta C, Bonini N, & Sanfey AG (2013). Reappraising social emotions: The role of inferior frontal gyrus, temporo-parietal junction and insula in interpersonal emotion regulation. Frontiers in Human Neuroscience, 7, 523. doi: 10.3389/fnhum.2013.00523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg MT (2006). Promoting resilience in children and youth: Preventive interventions and their interface with neuroscience. Annals of the New York Academy of Sciences, 1094, 139–150. doi: 10.1196/annals.1376.013 [DOI] [PubMed] [Google Scholar]
- Groschwitz RC, Plener PL, Groen G, Bonenberger M, & Abler B (2016). Differential neural processing of social exclusion in adolescents with non-suicidal self-injury: An fMRI study. Psychiatry Research: Neuroimaging, 255, 43–49. doi:0.1016/j.pscychresns.2016.08.001 [DOI] [PubMed] [Google Scholar]
- Guendelman M, Owens EB, Galan C, Gard A, & Hinshaw SP (2016). Early adult correlates of maltreatment in girls with ADHD: Increased risk for internalizing problems and suicidality. Development and Psychopathology, 28, 1–14. doi: 10.1017/S0954579414001485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamza CA, Stewart SL, & Willoughby T (2012). Examining the link between nonsuicidal self-injury and suicidal behavior: A review of the literature and an integrated model. Clinical Psychology Review, 32, 482–495. doi: 10.1016/j.cpr.2012.05.003 [DOI] [PubMed] [Google Scholar]
- Hanson JL, Chung MK, Avants BB, Shirtcliff EA, Gee JC, Davidson RJ, & Pollak SD (2010). Early stress is associated with alterations in the orbitofrontal cortex: A tensor-based morphometry investigation of brain structure and behavioral risk. Journal of Neuroscience, 30, 7466–7472. doi: 10.1523/JNEUROSCI.0859-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson JL, Chung MK, Avants BB, Rudolph KD, Shirtcliff EA, Gee JC,... Pollak SD (2012). Structural variations in PFC mediate the relationship between early childhood stress and spatial working memory. Journal of Neuroscience, 32, 7917–7925. doi: 10.1523/JNEUROSCI.0307-12.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkness KL, Stewart JG, & Wynne-Edwards KE (2011). Cortisol reactivity to social stress in adolescents: Role of depression severity and child maltreatment. Psychoneuroendocrinology, 36, 173–181. doi: 10.1016/j.psyneuen.2010.07.006 [DOI] [PubMed] [Google Scholar]
- Harold GT, Leve LD, & Sellers R (2017). How can genetically-informed research help inform the next generation of interparental and parenting interventions? Child Development, 88, 446–458. 10.1111/cdev.12742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart J, Gunnar M, & Cicchetti D (1995). Salivary cortisol in maltreated children: Evidence of relations between neuroendocrine activity and social competence. Development and Psychopathology, 7, 11–26. doi: 10.1017/S0954579400006313 [DOI] [Google Scholar]
- Hastings PD, Nuselovici JN, Utendale WT, Coutya J, McShane KE, & Sullivan C (2008). Applying the polyvagal theory to children’s emotion regulation: Social context, socialization, and adjustment. Biological Psychology, 79, 299–306. doi: 10.1016/j.biopsycho.2008.07.005 [DOI] [PubMed] [Google Scholar]
- Hawton K, Saunders KEA, & O’Connor R (2012). Self-harm and suicide in adolescents. Lancet, 379, 2373–2382. doi: 10.1016/S0140-6736(12)60322-5 [DOI] [PubMed] [Google Scholar]
- Hazlett EA, Zhang J, New AS, Zelmanova Y, Goldstein KE, Haznedar MM, …Chu KW (2012). Potentiated amygdala response to repeated emotional pictures in borderline personality disorder. Biological Psychiatry, 72, 448–456. doi: 10.1016/j.biopsych.2012.03.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF (2011). Neuroscience of self and self-regulation. Annual Review of Psychology, 62, 363–390. doi: 10.1146/annurev.psych.121208.131616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hechtman L, Swanson JM, Sibley MH, Stehli A, Arnold LE, Owens EB, …Nichols JQ (2016). Functional adult outcomes 16 years after childhood diagnosis of ADHD: MTA Results. Journal of the American Academy of Child and Adolescent Psychiatry, 55, 945–952. doi: 10.1016/j.jaac.2016.07.774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heller AS, Cohen AO, Dreyfuss MFW, & Casey BJ (2016). Changes in cortico-subcortical and subcortico-subcortical connectivity impact cognitive control to emotional cues across development. Social Cognitive and Affective Neuroscience, 11, 1910–1918. doi: 10.1093/scan/nsw097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbort MC, Soch J, Wüstenberg T, Krauel K, Pujara M, Koenigs M, …Schott BH (2016). A negative relationship between ventral striatal loss anticipation response and impulsivity in borderline personality disorder. NeuroImage: Clinical, 12, 724–736. doi: 10.1016/j.nicl.2016.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman JP, McKlveen JM, Ghosal S, Kopp B, Wulsin A, Makinson R, …Myers B (2016). Regulation of the hypothalamic-pituitary-adrenocortical stress response. Comprehensive Physiology, 6, 603–621. doi: 10.1002/cphy.c150015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw SP (2002). Preadolescent girls with ADHD: I. Background characteristics, comorbidity, cognitive and social functioning, and parenting practices. Journal of Consulting and Clinical Psychology, 70, 1086–1098. doi: 10.1037/0022-006X.70.5.1086 [DOI] [PubMed] [Google Scholar]
- Hinshaw SP (2017). Developmental psychopathology as a scientific discipline: A twenty-first century perspective In Beauchaine TP & Hinshaw SP (Eds.), Child and adolescent psychopathology (3rd ed., pp. 3–32). Hoboken, NJ: Wiley. [Google Scholar]
- Hinshaw SP, Owens EB, Sami N, & Fargeon S (2006). Prospective follow-up of girls with ADHD into adolescence: Evidence for continuing cross-domain impairment. Journal of Consulting and Clinical Psychology, 74, 489–499. doi: 10.1037/0022-006X.74.3.489 [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Zalecki C, Huggins SP, Montenegro-Nevado AJ, Schrodek E, & Swanson EN (2012). Prospective follow-up of girls with ADHD into early adulthood: Continuing impairment includes elevated risk for suicide attempts and self-injury. Journal of Consulting and Clinical Psychology, 80, 1041–1051. doi: 10.1037/a0029451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoertel N, Franco S, Wall MM, Oquendo MA, Kerridge BT, Limosin F, & Blanco C (2015). Mental disorders and risk of suicide attempt: A national prospective study. Molecular Psychiatry, 20, 718–726. doi: 10.1038/mp.2015.19 [DOI] [PubMed] [Google Scholar]
- Hooven C, Herting JR, & Snedker KA (2010). Long-term outcomes for the Promoting CARE Suicide Prevention Program. American Journal of Health Behavior, 34, 721–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooven C, Walsh E, Pike KC, & Herting JR (2012). Promoting CARE: Including parents in youth suicide prevention. Family and Community Health, 35, 225–235. doi: 10.1097/FCH.0b013e318250bcf9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostinar CE, & Cicchetti D (2018). Emotion dysregulation and internalizing spectrum disorders In Beauchaine TP & Crowell SE (Eds.), Oxford handbook of emotion dysregulation. New York: Oxford University Press. Epublished ahead of print. [Google Scholar]
- Hurlburt MS, Nguyen K, Reid J, Webster-Stratton C, & Zhang J (2013). Efficacy of the Incredible Years group parent program with families in Head Start who self-reported a history of child maltreatment. Child Abuse and Neglect, 37, 531–543. doi: 10.1016/j.chiabu.2012.10.008 [DOI] [PubMed] [Google Scholar]
- Jacoby N, Overfeld J, Binder E, & Heim C (2017). Stress neurobiology and developmental psychopathology In Cicchetti D (Ed.), Developmental psychopathology, Vol. 2: Developmental neuroscience (3rd ed., pp. 787–831). Hoboken, NJ: Wiley. [Google Scholar]
- Jantzer V, Haffner J, Parzer P, Resch F, & Kaess M (2015). Does parental monitoring moderate the relationship between bullying and adolescent nonsuicidal self-injury and suicidal behavior? A community-based self-report study of adolescents in Germany. BMC Public Health, 15, 583. doi: 10.1186/s12889-015-1940-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarvi S, Jackson B, Swenson L, & Crawford H (2013). The impact of social contagion on non-suicidal self-injury: A review of the literature. Archives of Suicide Research, 17, 1–19. 10.1080/13811118.2013.748404 [DOI] [PubMed] [Google Scholar]
- Joiner TE, Van Orden KA, Witte TK, Selby EA, Ribeiro JD, Lewis R, & Rudd MD (2009). Main predictions of the interpersonal–psychological theory of suicidal behavior: Empirical tests in two samples of young adults. Journal of Abnormal Psychology, 118, 634–646. doi: 10.1037/a0016500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaess M, Hille M, Parzer P, Maser-Gluth C, Resch F, & Brunner R (2012). Alterations in the neuroendocrinological stress response to acute psychosocial stress in adolescents engaging in nonsuicidal self-injury. Psychoneuroendocrinology, 37, 157–161. doi: 10.1016/j.psyneuen.2011.05.009 [DOI] [PubMed] [Google Scholar]
- Katz C, Bolton S-L, Katz LY, Isaak C, Tilston-Jones T, Sareen J, …Swampy Creek Suicide Prevention Team. (2013). A systematic review of school-based suicide prevention programs. Depression and Anxiety, 30, 1030–1045. doi: 10.1002/da.22114 [DOI] [PubMed] [Google Scholar]
- Kaufman E, Puzia MF, Mead HK, Crowell SE, McEachern A, & Beauchaine TP (2017). Children’s emotion regulation difficulties mediate the association between maternal borderline and antisocial symptoms and youth behavior problems over one year. Journal of Personality Disorders, 31, 170–192. doi: 10.1521/pedi_2016_30_244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kehoe C, & Havighurst S (in press). Treating emotion dysregulation in internalizing disorders In Beauchaine TP & Crowell SE (Eds.), Oxford handbook of emotion dysregulation. New York: Oxford University Press. [Google Scholar]
- King-Casas B, Sharp C, Lomax-Bream L, Lohrenz T, Fonagy P, & Montague PR (2008). The rupture and repair of cooperation in borderline personality disorder. Science, 321, 806810. doi: 10.1126/science.1156902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirschbaum C, Wüst S, & Hellhammer D (1992). Consistent sex differences in cortisol responses to psychological stress. Psychosomatic Medicine, 54, 648–657. doi: 10.1097/00006842-199211000-00004 [DOI] [PubMed] [Google Scholar]
- Klonsky ED (2011). Non-suicidal self-injury in US adults: Prevalence, socio-demographics, topography and functions. Psychological Medicine, 41, 1981–1986. doi: 10.1017/S0033291710002497 [DOI] [PubMed] [Google Scholar]
- Klonsky ED (2007). The functions of deliberate self-injury: A review of the evidence. Clinical Psychology Review, 27, 226–239. doi: 10.1016/j.cpr.2006.08.002 [DOI] [PubMed] [Google Scholar]
- Klonsky ED, May AM, & Glenn CR (2013). The relationship between nonsuicidal self-injury and attempted suicide: Converging evidence from four samples. Journal of Abnormal Psychology, 122, 231–237. doi: 10.1037/a0030278 [DOI] [PubMed] [Google Scholar]
- Kolb B, Mychasiuk R, Muhammad A, Lia Y, Frost DO, & Gibb R (2012). Experience and the developing prefrontal cortex. Proceedings of the National Academy of Sciences, 109, S17186–17193. doi: 10.1073/pnas.1121251109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M, Goldston D, & Gatsonis C (1993). Suicidal behaviors and childhood-onset depressive disorders: A longitudinal investigation. Journal of the American Academy of Child and Adolescent Psychiatry, 32, 8–20. doi: 10.1097/00004583-199301000-00003 [DOI] [PubMed] [Google Scholar]
- Krause-Utz A, Elzinga BM, Oei NYL, Paret C, Niedtfeld I, Spinhoven P, …Schmahl C (2014). Amygdala and dorsal anterior cingulate connectivity during an emotional working memory task in borderline personality disorder patients with interpersonal trauma history. Frontiers in Human Neuroscience, 8, 848. doi: 10.3389/fnhum.2014.00848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause-Utz A, Winter D, Niedtfeld I, & Schmahl C (2014). The latest neuroimaging findings in borderline personality disorder. Current Psychiatry Reports, 16, 438. doi: 10.1007/s11920-014-0438-z [DOI] [PubMed] [Google Scholar]
- Kuo JR, & Linehan MM (2009). Disentangling emotion processes in borderline personality disorder: Physiological and self-reported assessment of biological vulnerability, baseline intensity, and reactivity to emotionally evocative stimuli. Journal of Abnormal Psychology, 118, 531–544. doi: 10.1037/a0016392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurth F, Zilles K, Fox PT, Laird AR, & Eickhoff SB (2010). A link between the systems: Functional differentiation and integration within the human insula revealed by meta-analysis. Brain Structure and Function, 214, 519–534. doi: 10.1007/s00429-010-0255-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leenaars AA (Ed.). (1991). Life span perspectives of suicide: Timelines in the suicide process. New York: Plenum. [Google Scholar]
- Leijten P, Raaijmakers MAJ, Orobio de Castro B, van den Ban E, & Matthys W (2017). Effectiveness of the Incredible Years parenting program for families with socioeconomically disadvantaged and ethnic minority backgrounds. Journal of Clinical Child and Adolescent Psychology, 46, 59–73. doi: 10.1080/15374416.2015.1038823 [DOI] [PubMed] [Google Scholar]
- Letarte M-J, Normandeau S, & Allard J (2010). Effectiveness of a parent training program “Incredible Years” in a child protection service. Child Abuse and Neglect, 34, 253–261. doi: 10.1016/j.chiabu.2009.06.003 [DOI] [PubMed] [Google Scholar]
- Linehan MM (1993). Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford. [Google Scholar]
- Lis E, Greenfield B, Henry M, Guile JM, & Dougherty G (2007). Neuroimaging and genetics of borderline personality disorder: A review. Review of Psychiatric Neuroscience, 32, 162–173. [PMC free article] [PubMed] [Google Scholar]
- Liu X, Hairston J, Schrier M, & Fan J (2011). Common and distinct networks underlying reward valence and processing stages: A meta-analysis of functional neuroimaging studies. Neuroscience and Biobehavioral Reviews, 35, 1219–1236. doi: 10.1016/j.neubiorev.2010.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luecken LJ, Hagan MJ, Sandler IN, Tein J-Y, Ayers TS, & Wolchik SA (2010). Cortisol levels six-years after participation in the Family Bereavement Program. Psychoneuroendocrinology, 35, 785–789. 10.1016/j.psyneuen.2009.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luking KR, Pagliaccio D, Luby JL, & Barch DM (2016). Reward processing and risk for depression across development. Trends in Cognitive Sciences, 20, 456–468. doi: 10.1016/j.tics.2016.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupien SJ, McEwen BS, Gunnar MR, & Heim C (2009). Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews Neuroscience, 10, 434–445. doi: 10.1038/nrn2639 [DOI] [PubMed] [Google Scholar]
- McEwen BS (2017). Allostasis and the epigenetics of brain and body health over the life course: The brain on stress. JAMA Psychiatry, 74, 551–552. doi: 10.1001/jamapsychiatry.2017.0270. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Nasca C, & Gray JD (2016). Stress effects on neuronal structure: Hippocampus, amygdala, and prefrontal cortex. Neuropsychopharmacology Reviews, 41, 3–23. doi: 10.1038/npp.2015.171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee LG, Parent J, Forehand R, Rakow A, Watson KH, Dunbar JP, …Compas BE (2014). Reducing youth internalizing symptoms: Effects of a family-based preventive intervention on parental guilt induction and youth cognitive style. Development and Psychopathology, 26, 319–332. doi: 10.1017/S0954579413001016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier MH, Slutske WS, Arndt S, & Cadoret RJ (2008). Impulsive and callous traits are more strongly associated with delinquent behavior in higher risk neighborhoods among boys and girls. Journal of Consulting and Clinical Psychology, 117, 377–385. doi: 10.1037/0021-843X.117.2.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meza J, Owens EB, & Hinshaw SP (2016). Response inhibition, peer preference and victimization, and self-harm: Longitudinal associations in young adult women with and without ADHD. Journal of Abnormal Child Psychology, 44, 323–334. doi: 10.1007/s10802-015-0036-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE (2003). Life-course-persistent and adolescence-limited antisocial behavior: A 10year research review and a research agenda In Lahey BB, Moffitt TE, & Caspi A (Eds.), Causes of conduct disorder and juvenile delinquency (pp. 49–75). New York: Guilford. [Google Scholar]
- MTA Cooperative Group. (1999). A 14-month randomized clinical trial of treatment strategies for ADHD. Archives of General Psychiatry, 56, 1073–1086. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp JJ, Walsh BW, & McDade M (2010). Preventing non-suicidal self-injury in adolescents: The signs of self-injury program. Journal of Youth and Adolescence, 39, 306–314. doi: 10.1007/s10964-009-9450-8 [DOI] [PubMed] [Google Scholar]
- Nanni V, Uher R, & Danese A (2012). Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: A meta-analysis. American Journal of Psychiatry, 169, 141–151. doi: 10.1176/appi.ajp.2011.11020335 [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health (2016). NIMH funds 3 ‘Zero Suicide’ grants. Retrieved from https://www.nimh.nih.gov/news/science-news/2016/nimh-funds-3-zero-suicide-grants.shtml_on11/8/2017.
- Narayan A, Cicchetti D, Rogosch FA, & Toth SL (2015). Interrelations of maternal expressed emotion, maltreatment, and separation/divorce and links to family conflict and children’s externalizing behavior. Journal of Abnormal Child Psychology, 43, 217–228. doi: 10.1007/s10802-014-9911-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen L, Riddle M, King JW, & The NIH Science of Behavior Change Implementation Team (2018). The NIH Science of Behavior Change Program: Transforming the science through a focus on mechanisms of change. Behavior Research and Therapy, 101, 3–11. doi.org/10.1016/j.brat.2017.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolas MA, & Burt SA (2010). Genetic and environmental influences on ADHD symptom dimensions of inattention and hyperactivity: A meta-analysis. Journal of Abnormal Psychology, 119, 1–17. doi: 10.1037/a0018010 [DOI] [PubMed] [Google Scholar]
- Nock MK (2010). Self-injury. Annual Review of Clinical Psychology, 6, 339–363. doi: 10.1146/annurev.clinpsy.121208.131258 [DOI] [PubMed] [Google Scholar]
- Nock MK (2009). Why do people hurt themselves? New insights into the nature and functions of self-injury. Current Directions in Psychological Science, 18, 78–83. doi: 10.1111/j.1467-8721.2009.01613.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK (2008). Actions speak louder than words: An elaborated theoretical model of the social functions of self-injury and other harmful behaviors. Applied and Preventive Psychology, 12, 159–168. doi: 10.1016/j.appsy.2008.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Joiner TE, Gordon KH, Lloyd-Richardson E, & Prinstein MJ (2006). Nonsuicidal self-injury among adolescents: Diagnostic correlates and relation to suicide attempts. Psychiatry Research, 144, 65–72. doi: 10.1016/j.psychres.2006.05.010 [DOI] [PubMed] [Google Scholar]
- O’Connor DB, Ferguson E, Green JA, O’Carroll RE, & O’Connor RC (2016). Cortisol levels and suicidal behavior: A meta-analysis. Psychoneuroendocrinology, 63, 370–379. doi: 10.1016/j.psyneuen.2015.10.011 [DOI] [PubMed] [Google Scholar]
- O’Connor DB, Green JA, Ferguson E, O’Carroll RE, & O’Connor RC (2017). Cortisol reactivity and suicidal behavior: Investigating the role of hypothalamic-pituitary-adrenal axis responses to stress in suicide attempters and ideators. Psychoneuroendocrinology, 75, 183–191. doi: 10.1016/j.psyneuen.2016.10.019 [DOI] [PubMed] [Google Scholar]
- O’Connor RC, & Nock MK (2014). The psychology of suicidal behaviour. Lancet Psychiatry, 1, 73–85. doi: 10.1016/S2215-0366(14)70222-6 [DOI] [PubMed] [Google Scholar]
- Olfson M, Gameroff MJ, Marcus SC, Greenberg T, & Shaffer D (2005). Emergency treatment of young people following deliberate self-harm. Archives of General Psychiatry, 62, 1122–1128. doi: 10.1001/archpsyc.62.10.1122 [DOI] [PubMed] [Google Scholar]
- Opialla S, Lutz J, Scherpiet S, Hittmeyer A, Jäncke L, Rufer M, … Brühl AB (2015). Neural circuits of emotion regulation: A comparison of mindfulness-based and cognitive reappraisal strategies. European Archives of Psychiatry and Clinical Neuroscience, 265, 45–55. doi: 10.1007/s00406-014-0510-z [DOI] [PubMed] [Google Scholar]
- Ougrin D, Tranah T, Stahl D, & Moran P (2015). Therapeutic interventions for suicide attempts and self-harm in adolescents: Systematic review and meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 54, 97–107. doi.org/10.1016/j.jaac.2014.10.009 [DOI] [PubMed] [Google Scholar]
- Owens EB, & Hinshaw SP (2016). Pathways from neurocognitive vulnerability to co-occurring internalizing and externalizing problems among women with and without ADHD followed prospectively for 16 years. Development and Psychopathology, 28, 1013–1031. doi: 10.1017/S0954579416000675 [DOI] [PubMed] [Google Scholar]
- Owens EB, Zalecki C, Gillette P, & Hinshaw SP (2017). Girls with childhood ADHD as adults: Cross-domain outcomes by diagnostic status. Journal of Consulting and Clinical Psychology, 85, 723–736. doi: 10.1037/ccp0000217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panksepp J (2017). The psycho-neurology of cross-species affective/social neuroscience: Understanding animal affective states as a guide to development of novel psychiatric treatments. Current Topics in Behavioral Neuroscience, 30, 109–125. doi: 10.1007/7854_2016_458. [DOI] [PubMed] [Google Scholar]
- Patterson GR, DeGarmo DS, & Knutson NM (2000). Hyperactive and antisocial behaviors: Comorbid or two points in the same process? Development and Psychopathology, 12, 91–107. doi: 10.1017/S0954579400001061 [DOI] [PubMed] [Google Scholar]
- Plener PL, Bubalo N, Fladung AK, Ludolph AG, & Lulé D (2012). Prone to excitement: adolescent females with non-suicidal self-injury (NSSI) show altered cortical pattern to emotional and NSS-related material. Psychiatry Research, 203, 146–152. doi: 10.1016/j.pscychresns.2011.12.012 [DOI] [PubMed] [Google Scholar]
- Porges SW (2007). The polyvagal perspective. Biological Psychology, 74, 116–143. doi:10.1016=j.biopsycho.2006.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prinstein MJ, Boergers J, & Spirito A (2001). Adolescents’ and their friends’ health-risk behavior: Factors that alter or add to peer influence. Journal of Pediatric Psychology, 26, 287–298. doi: 10.1093/jpepsy/26.5.287 [DOI] [PubMed] [Google Scholar]
- Reid MJ, Webster-Stratton C, & Hammond M (2003). Follow-up of children who received the Incredible Years intervention for oppositional-defiant disorder: Maintenance and prediction of 2-year outcome. Behavior Therapy, 34, 471–491. doi: 10.1016/S0005-7894(03)80031-X [DOI] [Google Scholar]
- Rodríguez-Blanco L, Carballo JJ, & Baca-García E (2018). Use of ecological momentary assessment (EMA) in non-suicidal self-injury): A systematic review. Psychiatry Research, 263, 212–219. doi: 10.1016/j.psychres.2018.02.051 [DOI] [PubMed] [Google Scholar]
- Rosenthal MZ, Gratz KL, Kosson DS, Cheavens JS, Lejuez CW, & Lynch TR (2008). Borderline personality disorder and emotional responding: A review of the research literature. Clinical Psychology Review, 28, 75–91. doi: 10.1016/j.cpr.2007.04.001 [DOI] [PubMed] [Google Scholar]
- Sauder CL, Derbidge CM, & Beauchaine TP (2016). Neural responses to monetary incentives among self-injuring adolescent girls. Development and Psychopathology, 28, 277–291. doi: 10.1017/S0954579415000449 [DOI] [PubMed] [Google Scholar]
- Saudino LJ (2009). The development of temperament from a behavioral genetics perspective. Advances in Child Development and Behavior, 37, 201–231. doi: 10.1016/S0065-2407(09)03705-7 [DOI] [PubMed] [Google Scholar]
- Schmidt LA, Fox NA, Perez-Edgar K, & Hamer DH (2009). Linking gene, brain, and behavior: DRD4, frontal asymmetry, and temperament. Psychological Science, 20, 831–837. doi: 10.1111/j.1467-9280.2009.02374.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott S, & O’Connor TG (2012). An experimental test of differential susceptibility to parenting among emotionally dysregulated children in a randomized controlled trial for oppositional behavior. Journal of Child Psychology and Psychiatry, 53, 1184–1193. doi: 10.1111/j.1469-7610.2012.02586.x [DOI] [PubMed] [Google Scholar]
- Shader TM, Gatzke-Kopp LM, Crowell SE, Reid MJ, Thayer JF, Vasey MW, …Beauchaine TP (2018). Quantifying respiratory sinus arrhythmia: Effects of misspecifying breathing frequencies across development. Development and Psychopathology, 30, 351–366. doi: 10.1017/S0954579417000669 [DOI] [PubMed] [Google Scholar]
- Shields A, Ryan RM, & Cicchetti D (2001). Narrative representations of caregivers and emotion dysregulation as predictors of maltreated children’s rejection by peers. Developmental Psychology, 37, 321–337. doi: 10.1037/0012-1649.37.3.321 [DOI] [PubMed] [Google Scholar]
- Silbersweig D, Clarkin JF, Goldstein M, Kernberg OF, Tuescher O, Levy KN, …Stern E (2010). Failure of frontolimbic inhibitory function in the context of negative emotion in borderline personality disorder. Focus, 8, 250–260. doi: 10.1176/foc.8.2.foc250 [DOI] [PubMed] [Google Scholar]
- Skowron EA, Cipriano-Essel E, Benjamin LS, Pincus AL, & Van Ryzin MJ (2013). Cardiac vagal tone and quality of parenting show concurrent and time-ordered associations that diverge in abusive, neglectful, and non-maltreating mothers. Couple and Family Psychology: Research and Practice, 2, 95–115. doi: 10.1037/cfp0000005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skowron EA, Loke E, Gatzke-Kopp LM, Cipriano-Essel EA, Woehrle PL, Van Epps JJ, …Ammerman RT (2011). Mapping cardiac physiology and parenting processes in maltreating mother-child dyads. Journal of Family Psychology, 25, 663–674. doi: 10.1037/a0024528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skowron EA, & Reinemann DHS (2005). Psychological interventions for child maltreatment: A meta-analysis. Psychotherapy: Theory, Research, Practice, and Training, 42, 52–71. doi:10.1037/0033-3204.42.1.52 [Google Scholar]
- Slopen N, McLaughlin KA, & Shonkoff JP (2014). Interventions to improve cortisol regulation in children: A systematic review. Pediatrics, 133, 312–326. doi: 10.1542/peds.2013-1632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith AL, Cross D, Winkler J, Jovanovic T, & Bradley B (2014). Emotional dysregulation and negative affect mediate the relationship between maternal history of child maltreatment and maternal child abuse potential. Journal of Family Violence, 29, 483–494. doi: 10.1007/s10896-014-9606-5 [DOI] [Google Scholar]
- Southward MW, & Cheavens JS (2018). Identifying core deficits in a dimensional model of borderline personality disorder features: A network analysis. Clinical Psychological Science. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stalnaker TA, Cooch NK, & Schoenbaum G (2015). What the orbitofrontal cortex does not do. Nature Neuroscience, 18, 620–627. doi: 10.1038/nn.3982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepp SD, Burke JD, Hipwell AE, & Loeber R (2012). Trajectories of ADHD and ODD as precursors of borderline personality disorder symptoms in adolescent girls. Journal of Abnormal Child Psychology, 40, 7–20. doi: 10.1007/s10802-9530-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepp SD, Scott LN, Jones NP, Whalen DJ, & Hipwell AE (2016). Negative emotional reactivity as a marker of vulnerability in the development of borderline personality disorder symptoms. Development and Psychopathology, 28, 213–224. doi: 10.1017/S0954579415000395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surgeon General’s Report (2012). National Strategy for Suicide Prevention: Goals and Objectives for Action, 2012. Retrieved from https://www.surgeongeneral.gov/library/reports/national-strategy-suicideprevention/index.htmlon11/8/2017.
- Swanson EN, Owens EB, & Hinshaw SP (2014). Pathways to self-harmful behaviors in young women with and without ADHD: A longitudinal investigation of mediating factors. Journal of Child Psychology and Psychiatry, 44, 505–515. doi: 10.1111/jcpp.12193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson JM, Sibley MH, Arnold LE, Hechtman LT, Stehli A, Molina BSG, …MTA Cooperative Group. (in press). Outcomes in the 16-year follow-up of the Multimodal Treatment Study of ADHD (MTA): Persistence of symptoms and medication side effects in early adulthood. Journal of Child Psychology and Psychiatry. [Google Scholar]
- Takahashi T, Chanen AM, Wood SJ, Yücel M, Tanino R, Suzuki M,... McGorry PD (2009). Insular cortex volume and impulsivity in teenagers with first-presentation borderline personality disorder. Progress in Neuropsychopharmacology and Biological Psychiatry, 33, 1395–1400. doi: 10.1016/j.pnpbp.2009.07.017 [DOI] [PubMed] [Google Scholar]
- Tarullo AR, & Gunnar MR (2006). Child maltreatment and the developing HPA axis. Hormones and Behavior, 50, 632–639. doi: 10.1016/j.yhbeh.2006.06.010 [DOI] [PubMed] [Google Scholar]
- Thompson MP, Kingree JB, & Ho CH (2006). Associations between delinquency and suicidal behaviors in a nationally representative sample of adolescents. Suicide and Life-Threatening Behavior, 36, 57–64. doi: 10.1521/suli.2006.36.1.57 [DOI] [PubMed] [Google Scholar]
- Tone EB, Garn CL, & Pine DS (2016). Anxiety regulation: A developmental psychopathology perspective In Cicchetti D (Ed.), Developmental psychopathology, Vol. 2: Developmental neuroscience (3rd ed., pp. 523–556). Hoboken, NJ: Wiley. [Google Scholar]
- Tyrka AR, Wier L, Price LH, Ross N, Anderson GM, Wilkinson CW, & Carpenter LL (2008). Childhood parental loss and adult hypothalamic-pituitary-adrenal function. Biological Psychiatry, 63, 1147–1154. doi: 10.1016/j.biopsych.2008.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voon D, Hasking P, & Graham M (2014). Change in emotion regulation strategy use and its impact on adolescent nonsuicidal self-injury: A three-year longitudinal analysis using latent growth modeling. Journal of Abnormal Psychology, 123, 487–498. doi: 10.1037/a0037024 [DOI] [PubMed] [Google Scholar]
- Walrath C, Garraza LG, Reid H, Goldston DB, & McKeon R (2015). Impact of the Garrett Lee Smith youth suicide prevention program on suicide mortality. American Journal of Public Health, 105, 986–993. doi: 10.2105/AJPH.2014.302496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster-Stratton C, & Hammond M (1997). Treating children with early-onset conduct problems: A comparison of child and parent training interventions. Journal of Consulting and Clinical Psychology, 65, 93–109. doi: 10.1037/0022-006X.65.1.93 [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Reid MJ, & Beauchaine TP (2013). One-year follow-up of combined parent and child intervention for young children with ADHD. Journal of Clinical Child and Adolescent Psychology, 42, 251–261. doi: 10.1080/15374416.2012.723263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster-Stratton C, Reid MJ, & Hammond M (2004). Treating children with early-conduct problems: Intervention outcomes for parent, child, and teacher training. Journal of Clinical Child and Adolescent Psychology, 33, 105–124. doi: 10.1207/S15374424JCCP3301_11 [DOI] [PubMed] [Google Scholar]
- Wheeler MS, Arnkoff DB, & Glass CR (2017). The neuroscience of mindfulness: How mindfulness alters the brain and facilitates emotion regulation. Mindfulness, 8, 1471–1487. doi: 10.1007/s12671-017-0742-x [DOI] [Google Scholar]
- Whitlock J, Muehlenkamp J, Eckenrode J, Purington A, Abrams GB, & Barreira P (2013). Nonsuicidal self-injury as a gateway to suicide in young adults. Journal of Adolescent Health, 52, 486–492. doi: 10.1016/j.jadohealth.2012.09.010 [DOI] [PubMed] [Google Scholar]
- Whittle S, Dennison M, Vijayakumar N, Simmons JG, Yücel M, Lubman DI, …Allen NB (2013). Childhood maltreatment and psychopathology affect brain development during adolescence. Journal of the American Academy of Child and Adolescent Psychiatry, 52, 940–952. doi: 10.1016/j.jaac.2013.06.007 [DOI] [PubMed] [Google Scholar]
- Wielgus MD, Aldrich JT, Mezulis AH, & Crowell SE (2016). Respiratory sinus arrhythmia as a predictor of self-injurious thoughts and behaviors among adolescents. International Journal of Psychophysiology, 106, 127–134. doi: 10.1016/j.ijpsycho.2016.05.005 [DOI] [PubMed] [Google Scholar]
- Wilson SR, Rack JJ, Shi X, & Norris AM (2008). Comparing physically abusive, neglectful, and non-maltreating parents during interactions with their children: A meta-analysis of observational studies. Child Abuse and Neglect, 32, 897–911. doi: 10.1016/j.chiabu.2008.01.003 [DOI] [PubMed] [Google Scholar]
- Winiarski DA, Brown AL, Karnik NS, & Brennan PA (in press). Treating emotion dysregulation in externalizing disorders In Beauchaine TP & Crowell SE (Eds.), Oxford handbook of emotion dysregulation. New York: Oxford University Press. [Google Scholar]
- Winstanley CA, Theobald DE, Cardinal RN, & Robbins TW (2004). Contrasting roles of basolateral amygdala and orbitofrontal cortex in impulsive choice. Journal of Neuroscience, 24, 4718–4722. doi: 10.1523/JNEUROSCI.5606-03.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff J, Thompson E, Thomas S, Nesi J, Ransford B, Scopelliti KM, …Liu R (2018). Emotion Dysregulation and NSSI: A systematic review and meta-analysis. Manuscript under review [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf RC, Thomann PA, Sambataro F, Vasic N, Schmid M, & Wolf ND (2012). Orbitofrontal cortex and impulsivity in borderline personality disorder: An MRI study of baseline brain perfusion. European Archives of Psychiatry and Clinical Neuroscience, 262, 677–685. doi: 10.1007/s00406-012-0303-1 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2018). Suicide data Downloaded from http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/on5/19/2018.
- Yaroslavsky I, Bylsma LM, Rottenberg J, & Kovacs M (2013). Combinations of resting RSA and RSA reactivity impact maladaptive mood repair and depression symptoms. Biological Psychology, 94, 272–281. doi: 10.1016/j.biopsycho.2013.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalsman G, Hawton K, Wasserman D, van Heeringen K, Arensman E, Sarchiapone M, …Zohar J (2016). Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry, 3, 646–659. doi: 10.1016/S2215-0366(16)30030-X [DOI] [PubMed] [Google Scholar]
- Zisner A, & Beauchaine TP (2016a). Psychophysiological methods and developmental psychopathology In Cicchetti D (Ed.), Developmental psychopathology. Vol. 2: Developmental neuroscience (3rd ed., pp. 832–884). Hoboken, NJ: Wile [Google Scholar]
- Zisner A, & Beauchaine TP (2016b). Neural substrates of trait impulsivity, anhedonia, and irritability: Mechanisms of heterotypic comorbidity between externalizing disorders and unipolar depression. Development and Psychopathology, 28, 1179–1210. doi: 10.1017/S0954579416000754 [DOI] [PubMed] [Google Scholar]