Highlights
-
•
Children most probably stayed in their initial weight category.
-
•
Probabilities of transitioning across weight categories differ between genders.
-
•
Girls of nuclear families transition to obesity at a lower rate than their peers.
-
•
Experiences of crises and bullying are related to obesity development among boys.
-
•
Multistate models are useful for analyzing childhood obesity development.
Keywords: Childhood overweight, Multistate model, Psychosocial factors, School health care, Transition
Abstract
For targeted prevention and treatment of childhood obesity, primary health care needs methods to identify children potentially developing obesity. The objectives of this study were to examine transitions across weight categories and their association with psychosocial family- and school-related factors, data on which were retrieved from health records. This longitudinal cohort study comprised 507 Finnish children with overweight, identified from a random sample of 2000 sixth graders in Helsinki in 2013. We applied Markov multistate models to analyze the transition rates over six primary school years between BMI SDS categories of normal weight, overweight and obesity, as assessed by Finnish BMI-for-age reference, and to examine relations between transition rates and family- and school-related factors. Among 3116 pairs of consecutive growth measurements from 225 girls and 282 boys aged 6–14, 719 transitions from weight category to another occurred. The highest 1-year probabilities were 0.76 for girls to stay in overweight and 0.80 for boys to stay in obesity. Transitions from normal weight to overweight and from obesity to overweight were more probable than vice versa. Transitions from overweight into obesity were among girls associated with older age (HR 2.63) and divorced or single parents (HR 2.29), as well as among boys with experiences of crises (HR 2.40) and being bullied (HR 1.66). Factors identifiable in school health care and associated with the probability of transition towards obesity should be considered when planning individual support and intervention programs.
1. Introduction
Growth measurements display essential information on children’s health. In several countries, primary school children are monitored regularly (Davidson et al., 2018). In Finland, all pupils visit school nurses at least annually and school physicians meet families in extensive health checks during grades 1 and 5 (Government decree 338/2011, 2011). Supplementing comprehensive prevention, regular monitoring offers excellent opportunities to detect and treat obesity. Both are needed (Report of the Commission on Ending Childhood Obesity, 2017), as the prevalence of childhood overweight and obesity is increasing globally, including Finland (NCD Risk Factor Collaboration, 2017, Ng et al., 2014, Vuorela et al., 2011, COSI factsheet, 2018).
To direct limited school health care resources and to enhance school health care gains, personnel need tools to recognize children at greatest risk of developing obesity and suffering from related physical and mental consequences. Knowledge on obesity incidence and recovery rates, critical time-points and factors associated with unfavorable weight development becomes critical (Juonala et al., 2020, Report of the Commission on Ending Childhood Obesity, 2017).
Early-life factors, known to be associated with childhood obesity (Juonala et al., 2020, Mattsson et al., 2019, Schellong et al., 2012, Woo Baidal et al., 2016), can be used in risk assessment (Welten et al., 2020, Ziauddeen et al., 2018) but may be unidentifiable during school health care visits. Family- and school-related factors later in childhood, such as bullying and study difficulties, prevail among children with obesity (Kautiainen et al., 2009, van Geel et al., 2014) and can potentially be ameliorated with appropriate support.
Recently, research utilizing longitudinal data and advanced statistical methods, such as latent class analysis and multistate models, has expanded the comprehension of obesity development during childhood (Häkkänen et al., 2020, Mattsson et al., 2019, Moreira et al., 2019, Tran et al., 2016, Wu et al., 2019). Yet, little is known about transition probabilities between weight categories among children with overweight. Especially knowledge on family- and school-related factors associated with transitions remains scarce (Moreira et al., 2019, Tran et al., 2016).
1.1. Aim
In this study, we explored transition rates across weight categories during primary school in a longitudinal cohort of at some point overweight children. Based on BMI SDS classification and utilizing multistate modelling, we estimated sex-specific transition rates from a weight category to another, 1-year probabilities of transitions and the total length of time spent per category. We also probed associations between family- and school-related psychosocial factors and transition rates.
2. Methods
2.1. Study population
The study cohort consisted of randomly selected 2000 primary school children from all sixth-graders in Helsinki in spring 2013 (n = 4968), of which 517 were affected by overweight at some point during primary school both by the weight-for-height reference (Sorva et al., 1984) used in clinical work in Finland (Obesity: Current Care Guidelines, 2020), and by the Finnish BMI-for-age reference (Saari et al., 2011).
To investigate weight development, further analyses included 507 children with two or more weight and height measurements in Electronic Health Records (EHR) during their six primary school years. From their EHRs, we retrospectively collected all primary school growth measurements and data on pubertal development and relevant psychosocial factors. We adopted the Finnish BMI-for-age reference to place children in normal weight, overweight or obesity categories. The reference determines BMI SDS cut-offs for overweight, obesity and severe obesity as 1.16, 2.11 and 2.76 for girls and 0.78, 1.70 and 2.36 for boys, respectively.
Menarcheal statuses of girls are recorded at annual health checks and school physicians define pubertal statuses of girls and boys by Tanner staging during grade 5. We divided girls as having early pubertal development (menarche or M4 by grade 5 health check), average (M2 or M3 at grade 5 or menarche by grade 6 health check) or late (M1 at grade 5, M2 at grade 5 but age over 11.5 and no menarche at grade 6 or by 13.5 years of age). Based on fifth-grade health check assessments, boys were placed either to puberty started (G2) or not-started (G1) groups. We included a not known pubertal status for both genders.
2.2. Definition of family- and school-related factors
Psychosocial factors utilized include family- and school-related factors presumably associated with weight development and consistently recorded in EHRs. We retrieved all EHR data to construct dichotomous family- and school-related covariates of interest.
Relations of parents were described by the family structure covariate (married/cohabiting or single/divorced). EHRs lacked detailed information allowing reliable division into further subgroups. Parents were considered native speakers for Finnish or Swedish if no information showing otherwise came up for either parent (non-native families or native families). Covariate of crises (crises or no crises) included: contacting child protection services, legal dispute over child custody, parental mental health problem or drug or alcohol abuse, death of a parent or sibling and domestic violence or sexual harassment.
Children were classified as being bullied if related experiences were mentioned at least once in EHR. Furthermore, we deemed children to have had special study needs if information turned up on delayed starting of school, repeating a class, preparatory instruction classes for immigrants, or various forms of special education (performed in regular classes or schools or classes for special education).
2.3. Statistical methods
2.3.1. Descriptive statistics
Distribution of children with respect to family- and school-related factors was described by frequencies and corresponding proportions. We also examined the distribution into three weight categories in the beginning and end of primary school utilizing the highest BMI SDS measurements at grades 1 and 6.
2.3.2. Multistate models for transition rates
We applied Markov multistate models (Jackson, 2011) to estimate rates of transition (transition intensities) between three weight states, later called weight categories: normal weight, overweight and obesity. Following the results of our previous study (Häkkänen et al., 2020), we analyzed genders separately. We only allowed transitions between two adjacent categories. Our 3-state model consisted of four possible transitions: 1) “normal weight to overweight”, 2) “overweight to obesity”, 3) “overweight to normal weight”, and 4) “obesity to overweight”.
All observed transitions, except one for boys, were between adjacent weight categories (Table S3). This, combined with frequent measurement data and the gradual nature of weight development, led us to assume that we could observe state-to-state transitions although their exact timing remains censored. For the one boy who exceptionally transitioned directly from normal weight to obesity, we assumed the transition through overweight occurred at halfway.
We started the modelling by fitting sex-specific time-homogeneous Markov multistate models, which assume time-constant transition rates (Supplementary material). To gain more accurate estimates, we modelled the rates as a function of time since the first measurement, rather than age, thus allowing for a common starting point. For the same purpose of reducing random fluctuation, we retained only the first growth measurement with measurement time exceeding six years for children with such records.
As the results of our previous study (Häkkänen et al., 2020) suggest that age is related to weight trajectories and the above-mentioned assumption of time homogeneity is not necessarily met, we continued by fitting proportional intensities models with age divided into two categories (cut-off 9.5 years for girls, 10.5 for boys) as a covariate.
To identify candidate explanatory covariates of family- and school related factors, we examined each covariate as added to the model including age (Table S1). Next, we constructed multivariable proportional intensities models for girls and boys by adding candidate covariates one by one. The selection of covariates to the final models was based on Akaike Information Criterion (AIC) and the likelihood ratio test for comparing nested models (Table S2). Lastly, we inspected the goodness-of-fit of the final models (Supplementary material and Figures S1, S2).
From the models without covariates, we estimated 1-year probabilities of transitions between weight categories, durations (mean sojourn time) of visits in each category, and the total length of time spent in each category during the six years. The bootstrap 95% confidence intervals (CI) for these estimates were calculated by drawing 1000 bootstrap datasets formed by pairs of consecutive transitions. Differences between intensities related to categories of each covariate were assessed by means of hazard ratios (HR) and 95% CIs. All analyses were conducted with the msm-library available in R (Jackson, 2011, R-project, , 2017).
3. Results
3.1. Study population
The median follow-up time was 5.4 years (IQR 5.1–5.6), being approximately the same for both genders. The median number of growth measurements per child was 7. Of the 225 girls, 16% were affected by obesity at some point during primary school and of the 282 boys, a distinctly higher proportion (41%) (Table 1). The prevalence of obesity for girls was 10% both in the beginning and in the end of primary school, while the proportion of girls with overweight (obesity excluded) increased from 47% to 58%. With boys, the prevalence of obesity increased from 22% to 28% but stayed the same, around 52% for overweight.
Table 1.
Background characteristics of the 225 girls and 282 boys affected by overweight at some point over six primary school years.
| Girls (n = 225) | Boys (n = 282) | |||
|---|---|---|---|---|
| n | % | n | % | |
| Obesity (including severe obesity)a | 36 | 16.0 | 117 | 41.5 |
| Sever obesity (% of obesity) | 3 | 8.3 | 21 | 17.9 |
| Pubertal development | ||||
| Early (girls) | 65 | 28.9 | na | na |
| Average (girls)/started (boys) | 114 | 50.7 | 107 | 37.9 |
| Late (girls)/not-started (boys) | 33 | 14.7 | 124 | 44.0 |
| Not known | 13 | 5.8 | 51 | 18.1 |
| Psychosocial characteristics | ||||
| Family structure | ||||
| Married or cohabiting parents | 133 | 59.1 | 160 | 56.7 |
| Divorced or single parents | 92 | 40.9 | 122 | 43.3 |
| Parents native for Finnish or Swedish | ||||
| Non-native | 54 | 24.0 | 61 | 21.6 |
| Nativeb | 171 | 76.0 | 221 | 78.4 |
| Crises | ||||
| Yes | 31 | 13.8 | 40 | 14.2 |
| No | 194 | 86.2 | 242 | 85.8 |
| Being bullied | ||||
| Yes | 75 | 33.3 | 107 | 37.9 |
| No | 150 | 66.7 | 175 | 62.1 |
| Special study needs | ||||
| Yes | 29 | 12.9 | 61 | 21.6 |
| No | 196 | 87.1 | 221 | 78.4 |
507 sixth graders in 2013 in Helsinki, Finland
Abbreviations: na, not applicable
At least one obesity measurement during primary school by the Finnish BMI-for-age reference (Saari et al., 2011)
Both parents native Finnish or Swedish speakers
The distribution of family-related factors was similar with girls and boys (Table 1). School-related factors were more often present in boys. Of girls, 33.3% and of boys, 37.9% had experiences in being bullied and 12.9% and 21.6%, respectively, had needed special help in studies.
Furthermore, among children with adverse family- and school-related events the proportion affected by obesity was higher than amid children without these experiences. Of boys with experiences of crises, bullying or special needs in studying, 60%, 51% and 51%, respectively, were affected by obesity versus 38%, 35% and 39% of those without said experiences. For girls, the corresponding figures were 26%, 20% and 28% versus 6%, 6% and 7%. Among girls with divorced or single parents, the proportion of obesity was higher than among girls of nuclear families (21% vs. 13%) but girls of non-native and native families were equally often affected by obesity (15% vs. 16%).
According to pubertal development classifications applied, 51% of girls belonged to average, 29% to early and 15% to late groups. Of boys, 38% had entered puberty by grade 5 health check, where their medium age was 11.6. EHR entries for pubertal status proved inadequate for 6% of the girls and for 18% of the boys (Table 1).
3.2. Transitions between weight categories
Of all the 3116 pairs of consecutive BMI SDS measurements recorded (girls 1400, boys 1716), 719 were transitions from weight category to another. Most of the non-transitioning pairs were in overweight category; 47% of all measurements for girls and 42% for boys (Table S3).
In line with frequencies displayed in Table S3, the estimated 1-year probabilities of transitioning showed that staying in current categories was more probable than transitioning to previous or next ones (Table 2). Highest 1-year probabilities were 0.76 for girls staying in overweight category and 0.80 for boys staying in obesity (Table 2). Similarly, durations of single visits in weight categories were estimated to be the longest for girls in overweight (2.82 years) and boys in obesity (4.10 years) (Table 2). The probability to stay in obesity as compared to transitioning to overweight was two-fold for girls and four-fold for boys. Both girls and boys with normal weight stayed more probably in normal weight category (0.63 and 0.60 respectively) than moved to overweight (0.36 and 0.38) (Table 2).
Table 2.
Estimated 1-year probabilities of transitioning between BMI SDS categories over the ages of 6 to 14 and the mean sojourn time (duration in years of a single visit in a category) for girls (n = 225) and boys (n = 282) having been affected by overweight or obesity.
| BMI SDS category | BMI SDS category for same child 1 year later |
Mean sojourn time |
||||||
|---|---|---|---|---|---|---|---|---|
| Normal weight |
Overweight |
Obesity |
||||||
| MLE | 95% CI | MLE | 95% CI | MLE | 95% CI | MST | 95% CI | |
| Girls | ||||||||
| Normal weight | 0.634 | 0.587, 0.682 | 0.356 | 0.310, 0.403 | 0.010 | 0.006, 0.014 | 1.857 | 1.548, 2.216 |
| Overweight | 0.198 | 0.169, 0.228 | 0.763 | 0.731, 0.795 | 0.039 | 0.026, 0.053 | 2.821 | 2.411, 3.365 |
| Obesity | 0.040 | 0.027, 0.055 | 0.283 | 0.203, 0.366 | 0.677 | 0.579, 0.770 | 2.490 | 1.792, 3.688 |
| Boys | ||||||||
| Normal weight | 0.597 | 0.538, 0.650 | 0.378 | 0.328, 0.431 | 0.025 | 0.019, 0.033 | 1.733 | 1.440, 2.116 |
| Overweight | 0.128 | 0.107, 0.151 | 0.775 | 0.749, 0.802 | 0.097 | 0.077, 0.120 | 3.111 | 2.693, 3.638 |
| Obesity | 0.017 | 0.012, 0.021 | 0.188 | 0.146, 0.229 | 0.795 | 0.751, 0.842 | 4.101 | 3.282, 5.519 |
507 sixth graders in 2013 in Helsinki, Finland
Results from time-homogenous model. Bootstrap 95% CIs were calculated by drawing 1000 bootstrap datasets of the same number of transitions i.e. bootstrap datasets were formed by pairs of consecutive states
Abbreviations: BMI SDS, body mass index standard deviation score; MLE, maximum likelihood estimate of the transition intensities; CI, confidence interval; MST, mean sojourn time; SE, standard error.
When transitions occurred, 1-year probabilities of remission from overweight were lower than of overweight development (Table 2). Furthermore, staying in overweight category was 3.8 times more probable for girls and 5.9 times for boys than remission from overweight to normal weight. Girls with overweight were five times more likely to move within a year to normal weight than to obesity (0.20 vs. 0.04), whereas boys with overweight were almost equally likely to move to normal weight (0.13) or obesity (0.10).
Contrary to transitions between normal weight and overweight categories, the 1-year probability of remission from obesity was higher, 7-fold for girls and almost 2-fold for boys, than that of advancing into obesity. Still, it was most probable to remain in obesity (Table 2). Within a year, girls moved from overweight to obesity less probably than boys.
Girls and boys having initially been affected by overweight spent four years in overweight. This was the longest duration of all the estimated total times spent in each category (Table 3). When initially in obesity, estimates of total time spent in obesity and overweight were almost equal for girls (2.5 and 2.6 years), whereas boys were estimated to spend most of the time (3.6 years) in obesity.
Table 3.
Estimated total length of time spent in each category during six primary school years according to the initial weight category of the 225 girls and 282 boys.
| Initial weight category | Total length of time spent (years) |
|||||
|---|---|---|---|---|---|---|
| Normal weight |
Overweight |
Obesity |
||||
| Time spent | 95%CI | Time spent | 95%CI | Time spent | 95%CI | |
| Girls | ||||||
| Normal weight | 2.85 | 2.58, 3.11 | 2.92 | 2.67, 3.19 | 0.23 | 0.15, 0.32 |
| Overweight | 1.62 | 1.40, 1.83 | 4.02 | 3.81, 4.24 | 0.36 | 0.24, 0.49 |
| Obesity | 0.93 | 0.71, 1.13 | 2.60 | 2.11, 3.02 | 2.47 | 1.92, 3.13 |
| Boys | ||||||
| Normal weight | 2.36 | 2.10, 2.65 | 2.97 | 2.71, 3.21 | 0.67 | 0.53, 0.79 |
| Overweight | 1.01 | 0.85, 1.18 | 3.96 | 3.74, 4.18 | 1.03 | 0.84, 1.25 |
| Obesity | 0.44 | 0.34, 0.54 | 2.00 | 1.68, 2.31 | 3.57 | 3.20, 3.96 |
507 sixth graders in 2013 in Helsinki, Finland
Results from time-homogenous model
Abbreviations: CI, confidence interval
3.3. Associations with covariates
3.3.1. Multivariable analysis
Table 4 demonstrates HRs from models including age and one psychosocial covariate at a time, and from final models. Based on assessments of former models (Table S1), five psychosocial covariates were further studied with multivariable analysis (Table S2) and, along with age, included in the final models: family structure for both genders; native language of parents for girls; crises, bullying and special needs in studies for boys. Other covariates were omitted as after inclusion of them no further improvement of model fit was seen (Supplementary material).
Table 4.
Hazard ratios and 95% confidence intervals for transition rates across BMI SDS categories by age, pubertal development and psychosocial factors.
| From Normal weight to overweight |
From Overweight to Normal Weight |
From overweight to Obesity |
From Obesity to Overweight |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model controlling the effect of age |
Multivariable model |
Model controlling the effect of age |
Multivariable model |
Model controlling the effect of age |
Multivariable model |
Model controlling the effect of age |
Multivariable model |
|||||||||
| HR | 95%CI | HR | 95%CI | HR | 95%CI | HR | 95%CI | HR | 95%CI | HR | 95%CI | HR | 95%CI | HR | 95%CI | |
| Girls | ||||||||||||||||
| Age ≥ 9.5 (ref < 9.5)* | 1.42 | 0.99, 2.02 | 1.42 | 0.99, 2.03 | 1.31 | 0.89, 1.94 | 1.32 | 0.89, 1.95 | 2.56 | 1.11, 5.87 | 2.63 | 1.14, 6.09 | 1.30 | 0.62, 2.71 | 1.30 | 0.62, 2.72 |
| Pubertal development | ||||||||||||||||
| Early (ref Average) | 1.43 | 0.95, 2.15 | 1.39 | 0.89, 2.16 | 0.90 | 0.35, 2.28 | 1.00 | 0.40, 2.50 | ||||||||
| Late (ref Average) | 0.96 | 0.56, 1.64 | 1.34 | 0.78, 2.32 | 2.63 | 0.99, 7.00 | 2.82 | 1.15, 6.91 | ||||||||
| Not known (ref Average) | 0.77 | 0.36, 1.64 | 1.03 | 0.35, 3.06 | 2.10 | 0.44, 10.00 | 0.90 | 0.12, 7.00 | ||||||||
| Divorced or single parents (ref All other) | 0.89 | 0.62, 1.28 | 0.89 | 0.62, 1.28 | 0.69 | 0.46, 1.03 | 0.70 | 0.47, 1.04 | 2.40 | 1.11, 5.18 | 2.29 | 1.05, 4.98 | 1.38 | 0.67, 2.86 | 0.86 | 0.40, 1.86 |
| Parent(s) non-native (ref Native) | 1.06 | 0.71, 1.59 | 1.07 | 0.71, 1.59 | 1.06 | 0.66, 1.70 | 1.07 | 0.66, 1.72 | 0.34 | 0.10, 1.12 | 0.32 | 0.10, 1.06 | 0.24 | 0.07, 0.80 | 0.22 | 0.06, 0.79 |
| Crises (ref No crises) | 1.15 | 0.67, 1.97 | 1.24 | 0.69, 2.21 | 1.93 | 0.76, 4.86 | 0.83 | 0.33, 2.04 | ||||||||
| Being bullied (ref Not bullied) | 0.89 | 0.61, 1.30 | 0.74 | 0.49, 1.12 | 0.74 | 0.32, 1.71 | 0.88 | 0.42, 1.85 | ||||||||
| Special study needs (ref No needs) | 1.13 | 0.64, 1.97 | 0.56 | 0.29, 1.09 | 0.59 | 0.18, 1.97 | 0.62 | 0.23, 1.63 | ||||||||
| Boys | ||||||||||||||||
| Age ≥ 10.5 (ref < 10.5)* | 1.49 | 1.00, 2.22 | 1.46 | 0.97, 2.20 | 1.42 | 0.92, 2.19 | 1.37 | 0.88, 2.13 | 1.21 | 0.77, 1.90 | 1.21 | 0.77, 1.90 | 0.72 | 0.43, 1.22 | 0.72 | 0.43, 1.22 |
| Pubertal development | ||||||||||||||||
| Not started (ref Started) | 1.00 | 0.65, 1.55 | 0.98 | 0.62, 1.54 | 0.65 | 0.41, 1.04 | 0.84 | 0.49, 1.45 | ||||||||
| Not known (ref Started) | 0.78 | 0.44, 1.38 | 0.57 | 0.29, 1.10 | 0.46 | 0.23, 0.93 | 0.79 | 0.39, 1.59 | ||||||||
| Divorced or single parents (ref All other) | 1.73 | 1.17, 2.56 | 1.82 | 1.20, 2.76 | 1.54 | 1.00, 2.36 | 1.77 | 1.12, 2.80 | 0.91 | 0.59, 1.41 | 0.64 | 0.40, 1.04 | 0.68 | 0.41, 1.14 | 0.71 | 0.37, 1.33 |
| Parent(s) non-native (ref Native) | 1.15 | 0.72, 1.86 | 0.81 | 0.47, 1.40 | 1.27 | 0.77, 2.09 | 1.10 | 0.63, 1.93 | ||||||||
| Crises (ref No crises) | 0.99 | 0.58, 1.71 | 0.74 | 0.39, 1.43 | 0.57 | 0.26, 1.21 | 0.42 | 0.19, 0.95 | 2.20 | 1.32, 3.66 | 2.40 | 1.37, 4.21 | 0.77 | 0.39, 1.53 | 1.13 | 0.47, 2.69 |
| Being bullied (ref Not bullied) | 1.27 | 0.83, 1.93 | 1.18 | 0.75, 1.84 | 0.69 | 0.43, 1.10 | 0.64 | 0.39, 1.03 | 1.63 | 1.05, 2.52 | 1.66 | 1.06, 2.57 | 0.76 | 0.46, 1.24 | 0.83 | 0.49, 1.38 |
| Special study needs (ref No needs) | 1.34 | 0.85, 2.09 | 1.26 | 0.77, 2.08 | 1.64 | 0.98, 2.74 | 1.67 | 0.97, 2.85 | 1.79 | 1.10, 2.91 | 1.63 | 0.98, 2.70 | 0.79 | 0.45, 1.36 | 0.80 | 0.46, 1.41 |
507 sixth graders (225 girls, 282 boys) in 2013 in Helsinki, Finland
All figures were assessed from the proportional intensities models controlling for the effect of age or from the final multivariable proportional intensities models
Abbreviations: HR, hazard ratio; CI, confidence interval
Univariate model
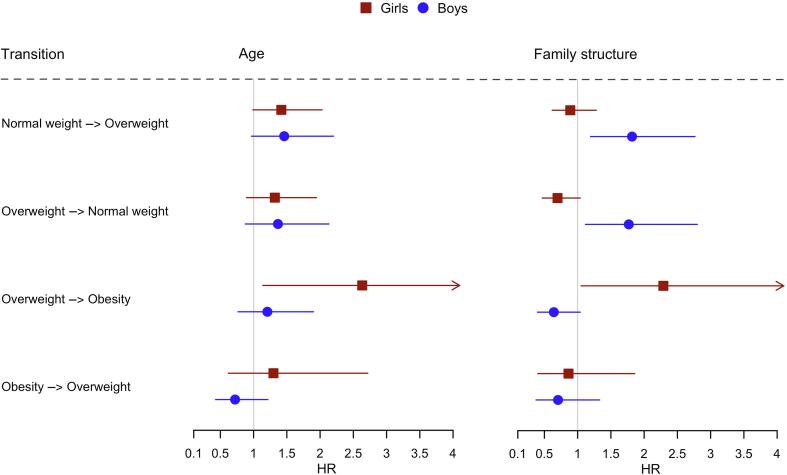
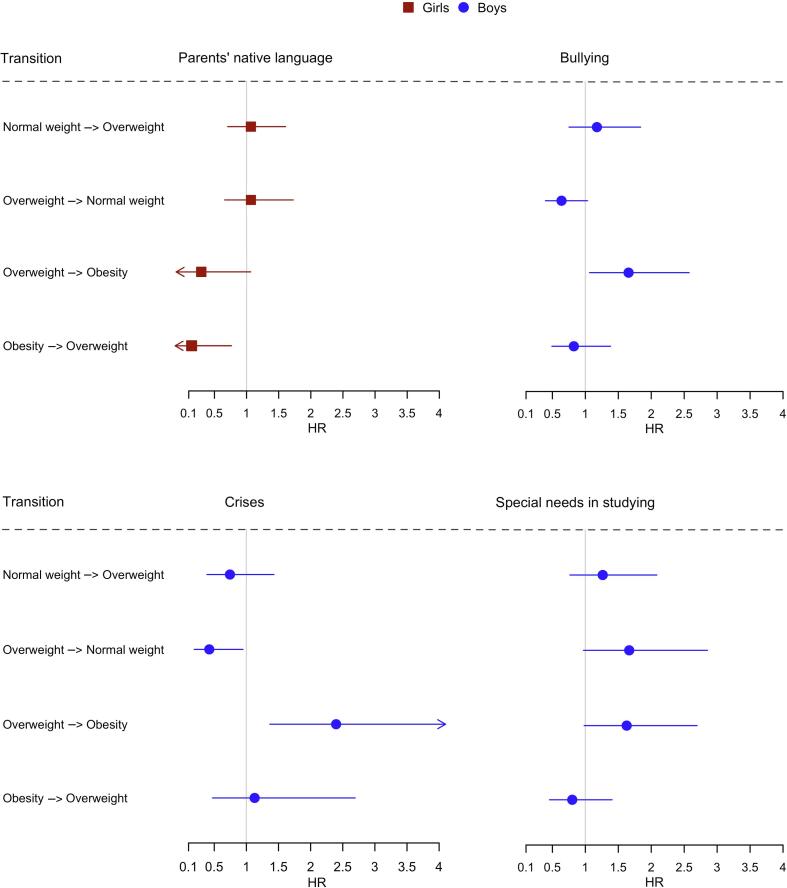
Fig. 1 and Fig. 2 summarize results of the final models. For girls, the transition rate from overweight to obesity was higher for ≥ 9.5-years-olds versus younger (HR 2.63) and for those having divorced or single parents versus nuclear family (HR 2.29) (Fig. 1, Table 4). Additionally, girls of non-native families had a lower transition rate from obesity to overweight than their peers of native families (HR 0.22, 95%CI 0.06–0.79) (Fig. 2, Table 4).
Fig. 1.
Hazard ratios and 95% confidence intervals assessed from the final multivariable proportional intensities models for the rates of transitioning across BMI SDS categories by age and family structure among 225 girls (red) and 282 boys (blue) (sixth graders in 2013 in Helsinki, Finland) Age (older versus younger age, cut-offs: girls 9.5 years, boys 10.5 years). Family structure (living in families with divorced or single parents versus living with married or cohabiting parents) Abbreviations: HR, hazard ratio. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 2.
Hazard ratios and 95% confidence intervals assessed from the final multivariable proportional intensities models for the rates of transitioning across BMI SDS categories by parent native language among 225 girls (red), and bullying, special needs in studying and crisis among 282 boys (blue) (sixth graders in 2013 in Helsinki, Finland) Bullying (bullying versus no bullying), special needs in studying (special needs in studying versus no special needs), crises (crises versus no crises), parents’ native language (non-native versus native for Finnish/Swedish) Abbreviations: HR, hazard ratio. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Boys living in divorced or single parent families, as compared with boys from nuclear families, transitioned at higher rates from normal weight to overweight and vice versa. On the contrary, boys having experienced crises transitioned from overweight to normal weight at a lower rate (HR 0.42) and from overweight to obesity at a higher rate (HR 2.40). The results were similar for boys having experiences in being bullied. Moreover, the HRs suggested that boys having needed extra support in studying, compared with boys who managed without, transitioned from overweight to obesity and to normal weight at a higher rate.
4. Discussion
4.1. Principal findings
This study showed that girls and boys initially affected by overweight and boys by obesity were estimated to stay a considerable part of the six primary school years at the same weight category. Overall, the 1-year probability of developing overweight or maintaining it exceeded that of remission into normal weight. Similarly, children stayed in the obesity category multiple times more likely than experienced remission into overweight. However, remission from obesity was multiple times more probable than advancing from overweight to obesity, especially for girls.
Several psychosocial factors were associated with transition rates between weight categories. Family-related factors were pronounced for girls, school-related for boys. For girls, having divorced or single parents was related to the development of obesity and living in non-native families to the persistence of obesity. Experiences of crises and in being bullied were associated with transitions to obesity among boys. Our results also suggested similar association with the needs for special help in studies.
4.2. Strengths and limitations
The study analyzed a cohort from a randomly selected sample of children by utilizing longitudinal data from real-life EHR recordings, therefore providing advantage over cross-sectional studies. As we excluded children exclusively in normal weight area, the results apply to similar populations only and are limited in comparability with recent studies on weight transition rates, which include all weight categories (Moreira et al., 2019, Tran et al., 2016, Wu et al., 2019).
Multistate models offer a valuable method to study weight changes over time. Still, the performance of the method depends on the number of transitions, which in turn depends on sample size, duration of follow-up and intensity of changes in the population under study. As the number of transitions was limited, the uncertainty of the results deserves attention. To capture associations between psychosocial factors and transition rates, we used less-conservative thresholds when selecting covariates and constructing final models. This may have provided associations due to chance only. Yet, some may have stayed undetected due to the lack of statistical power.
Our work offers insight into data available in EHRs, although under-reporting is possible. To diminish this bias, the data from all six grades were consolidated. Data collected may include surveillance bias, as data of children who were offered intensive treatment may be more comprehensive. This bias is presumably minor in Finnish school health care as all parents and children fill out nationally adopted questionnaires before health checks and the coverage of health checks is adequate (Häkkänen et al., 2018). Psychosocial factors identifiable at school health care were of interest due to potential support by health care, social work and teachers. However, this study offers no possibility to deduct whether the studied factors represent causes or consequences.
Collected EHR data lacked important predictors for childhood obesity, such as early-life factors and parental SES, BMI and education (Juonala et al., 2020, Moreira et al., 2019, Wang and Lim, 2012, Welten et al., 2020, Ziauddeen et al., 2018). Against our assumption, overweight issues of families were mainly unavailable in primary health care EHRs. However, information on bullying, special needs in studying, family structure and even crises are routinely recorded at school health checks.
4.3. Findings in relation to other studies
4.3.1. Overweight development
Children developed overweight more probably than returned from overweight to normal weight. This is in line with earlier studies indicating that prevalence of overweight and obesity increases with age (Cunningham et al., 2014, Juonala et al., 2020, Moreira et al., 2019, von Kries et al., 2012, von Kries et al., 2013). Low remission rates were presumed to explain the increase. However, according to our results, children, especially girls, returned from obesity to overweight more probably than developed obesity.
Transitions from overweight to obesity were rare (girls 29/1400, boys 85/1716), even though 41% of all boys were at least once in obesity category. This indicates that many children with obesity had it before school age, this being in line with earlier knowledge of obesity starting early (Woo Baidal et al., 2016).
In addition to confirming earlier findings of higher 1-year probabilities of staying in overweight or obesity than of moving to lower weight categories (Moreira et al., 2019, Tran et al., 2016), our study noticed gender differences. The 1-year probability of girls with overweight transitioning into normal weight was five-fold to the probability of them transitioning into obesity. For boys, these probabilities were almost equal, similarly to earlier studies without division by gender (Moreira et al., 2019, Wu et al., 2019).
Pubertal development failed to improve models controlled for effects of age. The growth of girls accelerating during puberty could explain them having a higher probability than boys of transitioning from obesity to overweight, as girls on average enter puberty already during primary school. Although the prevalence of obesity stayed the same for girls between school grades 1 and 6, transitions from overweight to obesity were more probable for older girls.
4.3.2. Family-related factors
Earlier studies show that children, especially girls, living with single parents are at greater risk for obesity (Duriancik and Goff, 2019) and girls aged 11–16 living in nuclear families are less likely to have overweight than other girls (Parikka et al., 2015). Our results are congruent with these findings adding that, during primary school, girls of divorced or single parents, when compared with girls from nuclear families, transitioned at higher rates from overweight to obesity.
4.3.3. Native language of parents
According to a study of children with immigrant background, adolescent girls with Somalian background were affected by overweight and obesity more often than native Finnish girls (Alitolppa-Niitamo et al., 2014). Our results on primary school girls lacked this difference. Furthermore, the percentage of boys with obesity was higher among boys from non-native families. However, girls with non-native parents had lower transition rates from obesity to overweight. This lower remission rate could explain the aforementioned finding of higher prevalence of obesity among teenage girls from non-native families (Alitolppa-Niitamo et al., 2014).
4.3.4. Special needs in studying
Knowledge on the relation of special needs in studying to weight status or weight change is scarce. Academic achievements and weight status have been studied deeper (Faught et al., 2017, Martin et al., 2017). With proper special support, learning may proceed well and therefore academic achievements and special study needs are not necessarily comparable.
Research supports the relation of obesity to lower academic achievements in adolescence, yet the relation lacked in earlier school age (Martin et al., 2017). However, healthy lifestyle seems to be more important to learning than actual weight status (Faught et al., 2017). Our results, among boys, suggesting that special needs in studying were associated with transitioning to obesity may therefore be mediated by lifestyle factors (Faught et al., 2017) or by obesity- or bullying-induced distress (Martin et al., 2017).
4.3.5. Bullying
Bullying is related to overweight and obesity and can be either a cause or a consequence, or even both (van Geel et al., 2014). This was seen in our study, in which a higher proportion of children having experiences in being bullied were affected by obesity and among boys bullying was associated with transitioning to obesity. Apparently, boys with obesity are more prone to being bullied or bullying itself is favorable for gaining and maintaining weight. Self-esteem and body satisfaction remain possible mediators, as poor body image has been associated with bullying independently from weight (Reulbach et al., 2013).
4.3.6. Crises and stress
Parental and offspring stress are related to childhood obesity (Garasky et al., 2009, Parks et al., 2012, Shankardass et al., 2014). Therefore, the associations observed between crises and unfavorable weight development are likely to reflect effects of stress (Hemmingsson, 2018, Miller and Lumeng, 2018). Other family- and school-related factors examined in our study undoubtedly may provoke distress both to children and parents. Also, low SES may induce distress and, additionally, act behind observed family- and school-related factors (Garasky et al., 2009, Hemmingsson, 2018, Wang and Lim, 2012).
5. Conclusions
Our study revealed that psychosocial factors retrievable from EHRs are associated with weight transitions. During primary school years, probabilities of staying at overweight or obesity were high, and remission was low. Even less-favorable transition rates between weight categories could be seen for subgroups of girls with divorced or single parents or from non-native families, and for boys with experiences of crises or being bullied. Early-life family factors, such as parental BMI and education, although inalterable at primary school age, are essential for assessing the probability of obesity development. It is moreover relevant to identify family- and school-related factors which are associated with obesity development and which potentially ameliorate with proper support.
The results of this study could be used to plan future studies and interventions on obesity. Further studies could apply multistate models to weight development data of larger populations with longer follow-up, along with both early-life and school-related factors.
Ethical approval
Approval to conduct this register-based study was received from The City of Helsinki Department of Health Care in December 2012. Per the Finnish legislation ethical approval is not required for pure register-based studies.
CRediT authorship contribution statement
Paula Häkkänen: Conceptualization, Investigation, Data curation, Writing - original draft. Anna But: Methodology, Software, Formal analysis, Validation, Writing - review & editing. Eeva Ketola: Conceptualization, Writing - review & editing. Tiina Laatikainen: Conceptualization, Writing - review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
We thank Juhana Häkkänen for language revision.
Funding
This work was supported by the Foundation of Outpatient Care (Avohoidon tutkimussäätiö). The funding source had no involvement in the study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2020.101239.
Contributor Information
Paula Häkkänen, Email: paula.hakkanen@helsinki.fi.
Anna But, Email: anna.but@helsinki.fi.
Eeva Ketola, Email: eeva.ketola@esperi.fi.
Tiina Laatikainen, Email: tiina.laatikainen@thl.fi.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Alitolppa-Niitamo, A., Haikkola, L., Laatikainen, T., Le, T., Leinonen, E., Levälahti, E., Malin, M., Markkula, J., Mäki, P., et al., 2014. Health and wellbeing among children with immigrant background [in Finnish]. Maahanmuuttajataustaisten nuorten terveys ja hyvinvointi. Tutkimus pääkaupunkiseudun somali- ja kurditaustaisista nuorista. Työpaperi 17/2014. Finnish Institute of Health and Welfare, Helsinki. http://urn.fi/URN:ISBN:978-952-302-212-6 (Accessed June 26 2020).
- COSI factsheet, 2018. Childhood Obesity Surveillance Initiative factsheet, highlights 2015-2017. World Health Organization [Online]. http://www.euro.who.int/__data/assets/pdf_file/0006/372426/WH14_COSI_factsheets_v2.pdf?ua=1 (Accessed June 26 2020).
- Cunningham S.A., Kramer M.R., Narayan K.M. Incidence of childhood obesity in the United States. N. Engl. J. Med. 2014;370:403–411. doi: 10.1056/NEJMoa1309753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson K., Vidgen H., Denney-Wilson E., Daniels L. How is children's weight status assessed for early identification of overweight and obesity? - Narrative review of programs for weight status assessment. J Child Health Care. 2018;22:486–500. doi: 10.1177/1367493518759238. [DOI] [PubMed] [Google Scholar]
- Duriancik D.M., Goff C.R. Children of single-parent households are at a higher risk of obesity: A systematic review. J Child Health Care. 2019;23:358–369. doi: 10.1177/1367493519852463. [DOI] [PubMed] [Google Scholar]
- Faught E.L., Ekwaru J.P., Gleddie D., Storey K.E., Asbridge M., Veugelers P.J. The combined impact of diet, physical activity, sleep and screen time on academic achievement: a prospective study of elementary school students in Nova Scotia, Canada. Int. J. Behav. Nutr. Phys. Act. 2017;14:29. doi: 10.1186/s12966-017-0476-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garasky S., Stewart S.D., Gundersen C., Lohman B.J., Eisenmann J.C. Family stressors and child obesity. Soc. Sci. Res. 2009;38:755–766. doi: 10.1016/j.ssresearch.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Government decree 338/2011, 2011. Valtioneuvoston asetus neuvolatoiminnasta, koulu- ja opiskeluterveydenhuollosta sekä lasten ja nuorten ehkäisevästä suun terveydenhuollosta (The government decree on maternity and child health clinic services, school and student health services and preventive oral health services for children and youth). Ministry of Social Affairs and Health. https://www.finlex.fi/en/laki/kaannokset/2011/20110338 (Accessed June 26 2020).
- Häkkänen P., But A., Ketola E., Laatikainen T. Distinct age-related patterns of overweight development to guide school healthcare interventions. Acta Paediatr. 2020;109:807–816. doi: 10.1111/apa.15036. [DOI] [PubMed] [Google Scholar]
- Häkkänen P., Ketola E., Laatikainen T. Screening and treatment of obesity in school health care - the gap between clinical guidelines and reality. Scand. J. Caring Sci. 2018;32:1332–1341. doi: 10.1111/scs.12578. [DOI] [PubMed] [Google Scholar]
- Hemmingsson E. Early Childhood Obesity Risk Factors: Socioeconomic Adversity, Family Dysfunction, Offspring Distress, and Junk Food Self-Medication. Curr Obes Rep. 2018;7:204–209. doi: 10.1007/s13679-018-0310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson, C.H., 2011. Multi-State Models for Panel Data: The msm Package for R. Journal of Statistical Software 38:1-29. 10.18637/jss.v038.i08.
- Juonala M., Lau T., Wake M., Grobler A., Kerr J.A., Magnussen C.G., Sabin M.A., Burgner D.P., Lycett K. Early clinical markers of overweight/obesity onset and resolution by adolescence. Int. J. Obes. (Lond.) 2020;44:82–93. doi: 10.1038/s41366-019-0457-2. [DOI] [PubMed] [Google Scholar]
- Kautiainen S., Koivisto A.M., Koivusilta L., Lintonen T., Virtanen S.M., Rimpela A. Sociodemographic factors and a secular trend of adolescent overweight in Finland. Int. J. Pediatr. Obes. 2009;4:360–370. doi: 10.3109/17477160902811173. [DOI] [PubMed] [Google Scholar]
- Martin A., Booth J.N., McGeown S., Niven A., Sproule J., Saunders D.H., Reilly J.J. Longitudinal Associations Between Childhood Obesity and Academic Achievement: Systematic Review with Focus Group Data. Curr Obes Rep. 2017;6:297–313. doi: 10.1007/s13679-017-0272-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattsson M., Maher G.M., Boland F., Fitzgerald A.P., Murray D.M., Biesma R. Group-based trajectory modelling for BMI trajectories in childhood: A systematic review. Obes. Rev. 2019;20:998–1015. doi: 10.1111/obr.12842. [DOI] [PubMed] [Google Scholar]
- Miller A.L., Lumeng J.C. Pathways of Association from Stress to Obesity in Early Childhood. Obesity (Silver Spring) 2018;26:1117–1124. doi: 10.1002/oby.22155. [DOI] [PubMed] [Google Scholar]
- Moreira C., Meira-Machado L., Fonseca M.J., Santos A.C. A Multistate Model for Analyzing Transitions Between Body Mass Index Categories During Childhood: The Generation XXI Birth Cohort Study. Am. J. Epidemiol. 2019;188:305–313. doi: 10.1093/aje/kwy232. [DOI] [PubMed] [Google Scholar]
- NCD Risk Factor Collaboration Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng M., Fleming T., Robinson M., Thomson B., Graetz N., Margono C., Mullany E.C., Biryukov S., Abbafati C. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obesity: Current Care Guidelines, 2020. (Children, adolescents and adults). Working group appointed by the Finnish Medical Society Duodecim, the Finnish Association for the Study of Obesity and the Finnish Paediatric Society. https://www.kaypahoito.fi (Accessed June 26 2020).
- Parikka S., Maki P., Levalahti E., Lehtinen-Jacks S., Martelin T., Laatikainen T. Associations between parental BMI, socioeconomic factors, family structure and overweight in Finnish children: a path model approach. BMC Public Health. 2015;15:271. doi: 10.1186/s12889-015-1548-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks E.P., Kumanyika S., Moore R.H., Stettler N., Wrotniak B.H., Kazak A. Influence of stress in parents on child obesity and related behaviors. Pediatrics. 2012;130:e1096–e1104. doi: 10.1542/peds.2012-0895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R-project, 2017. R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/ (Accessed June 26 2020).
- Report of the Commission on Ending Childhood Obesity, 2017. Implementation plan: executive summary. Licence: CC BY-NC-SA 3.0 IGO. World Health Organization, Geneva. http://apps.who.int/iris/bitstream/handle/10665/259349/WHO-NMH-PND-ECHO-17.1-eng.pdf?sequence=1 (Accessed June 26 2020).
- Reulbach U., Ladewig E.L., Nixon E., O'Moore M., Williams J., O'Dowd T. Weight, body image and bullying in 9-year-old children. J. Paediatr. Child Health. 2013;49:E288–E293. doi: 10.1111/jpc.12159. [DOI] [PubMed] [Google Scholar]
- Saari A., Sankilampi U., Hannila M.L., Kiviniemi V., Kesseli K., Dunkel L. New Finnish growth references for children and adolescents aged 0 to 20 years: Length/height-for-age, weight-for-length/height, and body mass index-for-age. Ann. Med. 2011;43:235–248. doi: 10.3109/07853890.2010.515603. [DOI] [PubMed] [Google Scholar]
- Schellong K., Schulz S., Harder T., Plagemann A. Birth weight and long-term overweight risk: systematic review and a meta-analysis including 643,902 persons from 66 studies and 26 countries globally. PLoS One. 2012;7 doi: 10.1371/journal.pone.0047776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankardass K., McConnell R., Jerrett M., Lam C., Wolch J., Milam J., Gilliland F., Berhane K. Parental stress increases body mass index trajectory in pre-adolescents. Pediatr. Obes. 2014;9:435–442. doi: 10.1111/j.2047-6310.2013.00208.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorva R., Perheentupa J., Tolppanen E.M. A novel format for a growth chart. Acta Paediatr. Scand. 1984;73:527–529. doi: 10.1111/j.1651-2227.1984.tb09965.x. [DOI] [PubMed] [Google Scholar]
- Tran M.K., Krueger P.M., McCormick E., Davidson A., Main D.S. Body Mass Transitions Through Childhood and Early Adolescence: A Multistate Life Table Approach. Am. J. Epidemiol. 2016;183:643–649. doi: 10.1093/aje/kwv233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Geel M., Vedder P., Tanilon J. Are overweight and obese youths more often bullied by their peers? A meta-analysis on the correlation between weight status and bullying. Int. J. Obes. (Lond.) 2014;38:1263–1267. doi: 10.1038/ijo.2014.117. [DOI] [PubMed] [Google Scholar]
- von Kries R., Beyerlein A., Muller M.J., Heinrich J., Landsberg B., Bolte G., Chmitorz A., Plachta-Danielzik S. Different age-specific incidence and remission rates in pre-school and primary school suggest need for targeted obesity prevention in childhood. Int. J. Obes. (Lond.) 2012;36:505–510. doi: 10.1038/ijo.2011.251. [DOI] [PubMed] [Google Scholar]
- von Kries R., Reulen H., Bayer O., Riedel C., Diethelm K., Buyken A.E. Increase in prevalence of adiposity between the ages of 7 and 11 years reflects lower remission rates during this period. Pediatr. Obes. 2013;8:13–20. doi: 10.1111/j.2047-6310.2012.00084.x. [DOI] [PubMed] [Google Scholar]
- Vuorela N., Saha M.T., Salo M.K. Change in prevalence of overweight and obesity in Finnish children - comparison between 1974 and 2001. Acta Paediatr. 2011;100:109–115. doi: 10.1111/j.1651-2227.2010.01980.x. [DOI] [PubMed] [Google Scholar]
- Wang Y., Lim H. The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int. Rev. Psychiatry. 2012;24:176–188. doi: 10.3109/09540261.2012.688195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welten M., Wijga A.H., Hamoen M., Gehring U., Koppelman G.H., Twisk J.W.R., Raat H., Heymans M.W., de Kroon M.L.A. Dynamic prediction model to identify young children at high risk of future overweight: Development and internal validation in a cohort study. Pediatr. 2020;Obes.:e12647 doi: 10.1111/ijpo.12647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo Baidal J.A., Locks L.M., Cheng E.R., Blake-Lamb T.L., Perkins M.E., Taveras E.M. Risk Factors for Childhood Obesity in the First 1,000 Days: A Systematic Review. Am. J. Prev. Med. 2016;50:761–779. doi: 10.1016/j.amepre.2015.11.012. [DOI] [PubMed] [Google Scholar]
- Wu T., Song G., Liu Q., Hu D., Li G., Tang X. Transition Patterns of Weight Status and Their Associated Factors among Elementary School Children: A Longitudinal Cohort Study Using Multistate Markov Model. Child Obes. 2019;15:306–312. doi: 10.1089/chi.2018.0345. [DOI] [PubMed] [Google Scholar]
- Ziauddeen N., Roderick P.J., Macklon N.S., Alwan N.A. Predicting childhood overweight and obesity using maternal and early life risk factors: a systematic review. Obes. Rev. 2018;19:302–312. doi: 10.1111/obr.12640. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.