Abstract
The most common manifestation of cardiovascular (CV) diseases is the presence of arterial hypertension (AH), which impacts on endothelial dysfunction. CV risk is associated with high values of systolic and diastolic blood pressure and depends on the presence of risk factors, both modifiable and not modifiable, such as overweight, obesity, physical exercise, smoking, age, family history, and gender. The main target organs affected by AH are the heart, brain, vessels, kidneys, and eye retina. AH onset can be counteracted or delayed by adopting a proper diet, characterized by a low saturated fat and sodium intake, a high fruit and vegetable intake, a moderate alcohol consumption, and achieving and maintaining over time the ideal body weight. In this review, we analyzed how a new nutritional approach, named caloric restriction diet (CRD), can provide a significant reduction in blood pressure values and an improvement of the endothelial dysfunction. In fact, CRD is able to counteract aging and delay the onset of CV and neurodegenerative diseases through the reduction of body fat mass, systolic and diastolic values, free radicals production, and oxidative stress. Currently, there are few studies on CRD effects in the long term, and it would be advisable to perform observational studies with longer follow-up.
Keywords: arterial hypertension, endothelial dysfunction, organ damage, caloric restriction diet, intermittent fasting
1. Introduction
As is well known, high blood pressure (BP) is one of the most important public health problems worldwide. High BP values may be caused by elevated cardiac output, enhancement of peripheral vascular resistance, or by a combination of both, and they negatively impact on the average life expectancy [1,2]. In fact, it is estimated that the prevalence of arterial hypertension (AH) among adults will increase from 26.4% to 29.2% in the year 2025. Currently, the World Health Organization (WHO) states that it affects one in four men and one in five women, meaning more than 1 billion people [3]. Therefore, cardiovascular (CV) diseases are one of the main causes of death in the word, together with newly arising infectious causes such as SARS-CoV-2 [4]. The most frequent CV diseases are myocardial infarction and stroke [5]. The affected target organs by AH are heart, brain, kidneys, vessels, and eye retina [3]. According to the degree of AH, clinicians should provide the most appropriate pharmacological and non-pharmacological therapy, as well [6]. The latter include undertake a healthy lifestyle, practice habitual physical exercise, avoid smoke, follow a diet with low-sodium intake (<100 mEq/day), and lose weight (in case of overweight or obese subjects). If lifestyle changes are not able to normalize BP, it is mandatory to begin a pharmacological treatment in order to restore BP values in the range of normality [7].
Currently, it is speculated that one of the possible nutritional strategies useful for the management of AH is a caloric restriction diet (CRD) [8,9].
Numerous studies have shown that eating habits are able to modify CV risk factors [10,11,12]. These impact on endothelial function, favoring the inflammatory processes underlying atherosclerosis [13]. In physiological conditions, the vascular endothelium maintains its tone through the release of signaling molecules with vasodilator (such as nitric oxide- (NO)) and vasoconstrictor (such as angiotensin II) action [14]. The endothelial dysfunction occurs when there is an abnormal production of reactive oxygen species (ROS) of pro-inflammatory cytokines, such as interleukin (IL)-1 and tumor necrosis factor (TNF)-α, and a decrease release of NO [15]. This condition triggers the atherosclerosis process [14]. For this reason, it is important, if not essential, undertake a nutritional treatment in patients with high BP. In this review, we focused on the possible beneficial effect of CRD on the BP control, highlighting the main antihypertensive mechanisms exerted by this nutritional approach.
2. Definition, Classification, and Management of Arterial Hypertension
AH is defined as a “condition characterized by increased blood pressure in the blood vessels” and when it becomes too high, and persists over time, it can damage the arteries and organs, leading the heart to a greater cardiac output [16]. Therefore, a condition in which systolic BP (SBP) is higher than 140 mm Hg and/or diastolic BP (DBP) is more than 90 mm Hg is defined as AH, as reported by the latest 2018 European Society of Cardiology (ESC) and European Society of Hypertension guidelines (ESH) [17].
Specifically, BP is optimal when SPB values are <120 mm Hg and DBP values are <80 mm Hg, and it is normal when SPB values are between 120 and 129 mm Hg and DBP values are between 80 and 84 mm Hg. BP is considered high-normal for SBP values between 130 and 139 mm Hg and for DPB values between 85 and 89 mm Hg. It defines grade 1 AH when SPB values are between 140 and 159 mm Hg and/or DPB values are between 90 and 99 mm Hg; grade 2 AH when SPB values are between 160 and 179 mm Hg and/or DPB values are between 100 and 109 mm Hg; grade 3 AH when SPB values are ≥180 mm Hg and/or DPB values are ≥110 mm Hg [17].
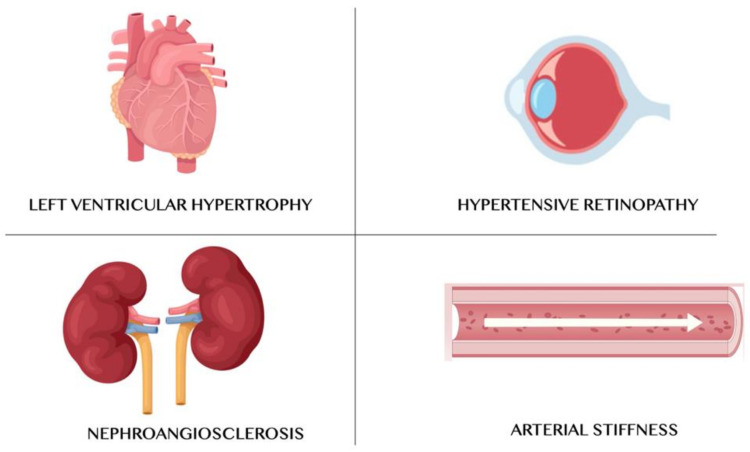
High BP can cause left ventricular hypertrophy and then heart failure, renal failure (nephroangiosclerosis), accelerated atherosclerosis, and hypertensive retinopathy (Figure 1). AH arises from the combination of genetic and environmental factors. Therefore, it should be useful to identify predisposed patients and instruct them to lifestyle changes. Such lifestyle changes concern to the adoption of healthy diet, in order to avoid high alcohol consumption, to promote regular physical activity, to maintain the normal BW, to stop smoking and to avoid passive smoking [18]. In Italy, it is estimated that there are about 15 million hypertensive subjects; in fact, 28.3% of the population is affected by AH [19,20]. Several clinical trials have shown that a lifestyle change can delay or prevent AH onset in people who are not hypertensive, delay or prevent drug therapy in subjects with grade I AH, contribute to the BP reduction in hypertensive individuals already in pharmacological therapy, and reduce the number and dosage of antihypertensive drugs [21].
Figure 1.
Main target organs of arterial hypertension.
The wide availability of drugs offers the possibility to obtain a fast-hypotensive effect and to act positively on the mechanisms that predispose to CV events.
3. Arterial Hypertension and Endothelial Alterations
AH is the most important risk factor for CV diseases [22]. In fact, vascular alterations (such as endothelial dysfunction) are a pathophysiological response mechanism to the development of organ damage, and they should be taken into account for the global CV risk assessment. The endothelium plays a pivotal role, and it consists of 1.2 billion cells, with a weight exceeding 1.5 kg and an area of 400 m2 [23]. It forms a thin cellular lamina in direct contact with the bloodstream, representing the innermost layer of the vessel wall. The most important functions performed by endothelium are the modulation of the inflammation, the regulation of the vasomotor tone, the promotion and inhibition of cell proliferation and the modulation of the coagulative cascade [24,25,26]. The main physiological mediator of endothelium is NO, but it displays also other important functions at the level of the central nervous and immune systems. Endothelial cells produce NO through the enzyme NO-synthase (NOS), which transforms L-arginine amino acid into citrulline [27]. The activity of NOS is stimulated by numerous mediators, such as bradykinin and acetylcholine, or by mechanical forces, mainly “shear stress” [27]. NO is a volatile gas that has few seconds half-life and that, spreading towards the vessel wall smooth muscle cells, causes the release of cyclic guanosine-monophosphate (cGMP) with the consequent reduction of intracellular calcium [28].
The term “endothelial dysfunction” identifies a pathophysiological condition characterized by anatomically intact endothelial cells, but when stimulated, instead of solely determining the production of NO, activates in parallel the production of ROS, which causes the degradation of NO [29]. Although the endothelial dysfunction is mainly caused by increased destruction of NO, it may also depend on its reduced production due to L-arginine substrate deficiency, or by vasoconstriction induced by factors derived from cyclooxygenase [23].
The endothelial damage is instead represented by the destruction of endothelial cells, where the regeneration of these cells is difficult to achieve [30]. The BP increase causes an enhancement in the production of superoxide and a decrease in the bioavailability of NO [31]. There is also another mechanism involving the renin–angiotensin–aldosterone system (RAAS). The angiotensin conversion enzyme (ACE) acts on the endothelium by converting angiotensin I to angiotensin II, an endocrine vasoactive peptide. The latter is an active protein able to induce vasoconstriction through the calcium-dependent myosin phosphorylation with the contraction of arterial smooth cells, inducing an enhancement of BP levels. Moreover, angiotensin II stimulates in the kidneys the sodium reabsorption which, in turn, induces water retention. Angiotensin II promotes also the production of endothelin, a class of proteins with paracrine/vasoconstrictive action, causing an increase in blood pressure [32,33]. Endothelin is synthetized in the endothelial cells through two different pathways. The first is named “constitutive”, and it is characterized by a continuous release of endothelin from macrovesicles which, in turn, interact with their own receptors, maintaining the vascular tone. The second is defined as a “regulated” mechanism and is activated by external physiological or pathophysiological stimuli. In fact, the endothelin that is released by the endothelial cells through this system, interacts with two types of receptors, namely, ETA, placed on the smooth muscle layer of the vessel, and, to a lesser extent, with ETB, which mediate the vasoconstrictive action [34].
Normally, there is a balance between vasoconstrictive and vasodilating substances in the bloodstream, but in the case of AH, the bioavailability of endothelin can be increased in parallel with a reduction in the bioavailability of NO. Angiotensin conversion enzyme inhibitors (ACE-I) and angiotensin receptor blockers (ARB) represent the first-line therapies for AH [7,17]. Dysfunctional endothelium shows a poor vasomotor function, which leads to an elevated BP at rest [35]. To date, it is speculated that there is a correlation between AH and endothelial dysfunction, but the issue is still unresolved due to the few studies in this regard [36,37,38,39].
4. Methods
PubMed, Web of Science, and Scopus online libraries were searched up until November 2020 in order to assess the most interesting and recent evidences about CRD and AH. The search was performed manually, using a combination of MeSH terms and keywords such as “caloric restriction diet”, “arterial hypertension”, “endothelial dysfunction”, and “dietary protocol”. All the studies were in the English language.
5. Caloric Restriction Diet
The CRD innovative approach consists of a chronic reduction in daily caloric intake of about 25–30% compared to the normal caloric intake, without any exclusion of food groups [40]. Although this regimen is not standardized, numerous studies show its effectiveness. Currently, according to the Calorie Restriction Society, subjects who follow a self-imposed CRD regimen are characterized by an increase in life expectancy. This regime consists of a caloric restriction with a daily consumption lower than 1800 kcal for an average period of 15 years and with an energy intake 30% lower than a group of individuals (homogeneous for age, gender, and socio-economic status) who consumed a Western diet model [40,41].
The first animal study to assess the beneficial effects of the CRD was carried out in rats in the 1900s [42]. Following studies showed that restricting food intake in mice delayed their growth but also extended their lifespan by to two times. Compared to a group that did not follow any restrictions, the CRD mice group showed anti-aging effects [43]. The most reliable hypothesis of the anti-aging effect of CRD is associated with reduced oxidative stress (OS). During the cellular respiration, oxygen is converted into ROS. ROS are able to react with macromolecules within cells causing the process of cellular aging. Therefore, CRD was initially designed for its antioxidant effect and consequently for its anti-aging action [44]. At this regard, numerous studies have been carried out, although contrasting results have been obtained. In fact, in some mice, without the superoxide dismutase enzyme, there was not increase in the aging, despite the enhanced of oxidative damage [45,46]. Animal studies on CRD showed that initial food restriction followed by alternating fasting acted positively on glycemic control, body weight (BW) reduction, insulin sensitivity, and BP control [47]. Anisimov and Bartke confirmed that serum values of glycemia and insulin were lower under CRD treatment [48]. In this context, the key role exerted by CRD is due to the decrease in insulin and insulin-like growth factor-1 (IGF-1) release and to the insulin sensitivity enhancement, observed both in rodents and in monkeys [49,50]. The results obtained in these studies confirm that the aging-related pathologies’ arose later in the CRD group compared to ad libitum diet group [51].
In recent years, many theories have been developed to explain the CRD beneficial effects. Most of them focused their attention on the sirtuin family. Sirtuins are proteins nicotinamide dinucleotide (NAD+)-dependent deacylases able to prevent some diseases and to modulate several aspects of cellular aging, promoting DNA integrity through the maintenance of the normal degree of chromatin condensation and repairing promptly DNA damage [52,53,54,55]. In mammals, sirtuin1 (SIRT1) cytoplasmatic protein acts on the control of cell cycle, particularly on the apoptosis and on the mitochondrial metabolism [56]. Several studies showed that sirtuins levels after CRD increased in some specific tissues such as the gut, brain, kidney, adipose tissue, and skeletal muscle [57,58,59]. In a study conducted by Meyer et al., the authors demonstrated a significant effect of CRD on cardiovascular aging [60]. Twenty-five healthy subjects (mean age 53 ± 12 years) that followed CRD were matched with 25 subjects homogeneous for age and gender (control group) that followed a typical Western diet. All enrolled subjects underwent to diastolic function evaluation by transmitral flow, Doppler tissue imaging, and model-based image processing (MBIP) of E waves and inflammatory status assessment thanks to C-reactive protein (CRP), TNF-α, and transforming growth factor-beta1 (TGF-β1) blood sampling. Results showed that parameters such as Doppler flow diastolic function mean indexes, BP, CRP, TNF-α, and TGF-β1 were significantly lower in the CRD subject, compared to the control group. The results of this study highlighted that CRD is able to ameliorate cardiac function, slowing the cardiac-aging process and decreasing systemic inflammation and BP values. Furthermore, it is confirmed that CRD increases life expectancy.
Following a CRD, it is possible counteract aging in all living forms, lengthening both the median and the maximum duration of life, and delaying over time the appearance of CV and neurodegenerative diseases [61,62].
Human’s life span has increased considerably due to the improvement of hygienic conditions and greater availability of pharmacological therapies. Taking into account the idea that the caloric restriction prolongs the life span, the mechanism of action by which this is possible, is not fully understood yet. Recent studies have shown that CRD can determine the damaged DNA repair and decrease fat mass, SBP and DBP values, the production of free radicals. The results obtained from the CRD can occur quickly, but they can mitigate in case of its suspension [63].
6. Caloric Restriction Diet and Arterial Hypertension
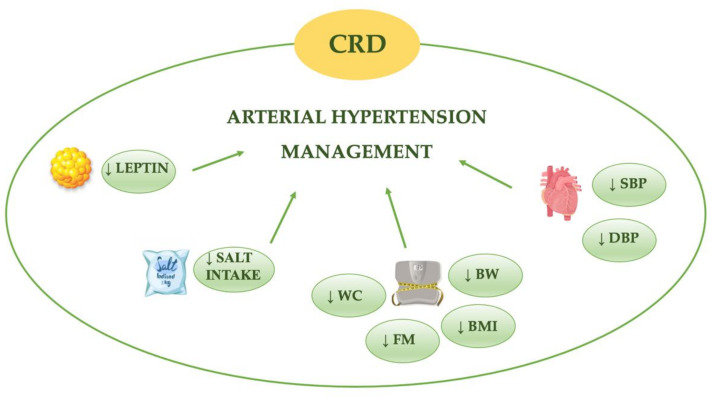
The CRD would seem to exert a beneficial effect against AH (Table 1) and for this reason represents a useful tool for its clinical management (Figure 2).
Table 1.
Dietary approaches in the arterial hypertension management.
| Nutritional Treatment | Type of the Study | Authors | Year | Organ/System/Metabolic Target |
Duration of Intervention | Impact of Intervention |
|---|---|---|---|---|---|---|
| CRD | Animal study | Zanetti et al. [64] | 2010 |
|
3 weeks | ↓ Oxidative stress ↓ iNOS ↓ Total nitrite ↓ Calcium-independent NOS activity ↑ SOD activity |
| CRD | Animal study | Rippe et al. [65] | 2010 |
|
8 weeks | ↓ Oxidative stress ↓ Blood glucose ↓ TG ↑ NO bioavailability ↑ Arterial expression of SIRT1 |
| CRD | Animal study | Donato et al. [66] | 2013 |
|
30–31 months | ↓ NADPH oxidase activity ↓ Oxidative stress ↓ TG ↓ BW ↑ SOD activity ↑ Catalase |
| CRD | Animal study | Kobara et al. [67] | 2015 |
|
4 weeks | ↓ ROS ↓ Cardiac hypertrophy and fibrosis |
| CRD | Animal study | Waldman et al. [68] | 2018 |
|
4 weeks | ↓ Oxidative stress ↓ Inflammation ↑ SIRT1 |
| CRD | Animal study | An et al. [69] | 2020 |
|
12 weeks | ↓ Cardiac hypertrophy and fibrosis ↓ Cardiac inflammation ⇅ Cellular regulation of iron homeostasis |
| CRD | Human study | Wadden et al. [70] | 1998 |
|
40 weeks | ↓ BW ↓ FM ↓ Serum leptin |
| CRD | Human study | Nakano et al. [71] | 2001 |
|
2 weeks | ↓ BMI ↓ BW ↓ TG ↓ HOMA-index ↓ SBP ↓ DBP |
| CRD | Human study | Facchini et al. [72] | 2003 |
|
3 weeks | ↓ BMI ↓ Heart rate ↑ Parasympathetic activity |
| CRD | Human study | Das et al. [73] | 2007 |
|
12 months | ↓ FM ↓ BW ↓ TG ↓ insulin ↓ LDL-c ↓ TC ↑ HDL-c |
| CRD | Human study | Lecoultre et al. [74] | 2011 |
|
6 months | ↓ BW ↓ Mean 24 h circulating leptin ↓ Urinary norepinephrine |
| CRD | Human study | Stewart et al. [75] | 2013 |
|
24 months | ↓ LDL-c ↓ TC/HDL-c↓ TG ↓ DBP ↓ BW ↓ BMI ↓ FM ↓ MSS ↑ IS |
| CRD | Human study | Ruggenenti et al. [76] | 2017 |
|
6 months | ↓ WC ↓ BW ↓ BMI ↓ BG ↓ HbA1c |
| CRD | Human study | Most et al. [77] | 2018 |
|
24 months | ↓ VAT ↓ SAAT ↓ SBP ↓ DBP ↓ TC ↓ LDL-c ↓ IR |
| CRD | Human study | Kraus et al. [78] | 2019 |
|
24 months | ↓ LDL-c ↓ TC/HDL-c ↓ SBP ↓ DBP ↓ MSS ↑ IS |
| DASH DIET | Human study | Harsha et al. [79] | 1999 |
|
8 weeks | ↓ SBP ↓ DBP |
| IF | Human study | Arnason et al. [80] | 2017 |
|
6 weeks | ↓ BW ↓ BMI |
| IF | Human study | Erdem et al. [81] | 2018 |
|
- | ↓ SBP ↓ Heart rate ↓ USE |
| IF | Human study | Furmli et al. [82] | 2018 |
|
12 weeks | ↓ HbA1c ↓ BW ↓ WC |
| IF | Human study | Wilhelmi de Toledo et al. [83] | 2019 |
|
24 months | ↓ SBP ↓ DBP ↓ BW ↓ Abdominal circumference ↓ Blood glucose ↓ TG ↓ LDL-c ↓ HDL-c ↓ TC ↑ Physical and emotional well-being |
| CRD vs IF | Animal study | Magger et al. [84] | 2006 |
|
16 weeks | ↓ BW ↓ Heart rate ↓ SBP ↓ DBP ↓ Blood glucose |
Abbreviations: ANS, autonomic nervous system; BG, blood glucose; BMI, body mass index; BW, body weight; CRD, caloric restriction diet; DBP, diastolic blood pressure; FM, fat mass; HbA1c, glycated hemoglobin; HDL-c, high-density lipoprotein cholesterol; IF, intermittent fasting; iNOS, inducible nitric oxide synthase; IR, insulin resistance; IS, insulin sensitivity; LDL-c, low density lipoprotein cholesterol; MSS, metabolic syndrome score; NADPH, nicotinamide adenine dinucleotide phosphate; NO, nitric oxide; ROS, reactive oxygen species; SAAT, subcutaneus abdominal adipose tissue; SBP, systolic blood pressure; SIRT1, sirtuin 1; SOD, superoxide dismutase; TC, total cholesterol; TG, triglycerides; USE, urinary sodium excretion; VAT, visceral adipose tissue; WC, waist circumference, ↑ increase, ↓ decrease.
Figure 2.
Beneficial effects of caloric restriction diet (CRD) on arterial hypertension. BMI, body mass index; BW, body weight; DBP, diastolic blood pressure; FM, fat mass; SBP, systolic blood pressure; WC, waist circumference, ↓ decrease.
An important study conducted in this regard was the CALERIE (Comprehensive Assessment of Long-term Effects of Reducing Intake of Energy) [85]. The CALERIE study was a randomized controlled trial with a two-year follow up. This study was divided in two phases: CALERIE-1 and CALERIE-2 [73,75]. CALERIE-1 study was performed to assess the possible effects induced by a reduction of 10-30% of caloric intake on body composition parameters and lipid profile after 6 and 12 months in a population of middle-aged non-obese subjects. CALERIE-1 results showed an improvement in lipid and glycemic profile and a reduction in BW and fat mass. CALERIE-2 was the largest multi-center study on CRD, involving three centers, namely the Pennington Biomedical Research Center (Baton Rouge, LA, USA), Tufts University (Boston, MA, USA), and Washington University School of Medicine (St. Louis, MO, USA), and was coordinated by Duke Clinical Research Institute (Durham, NC, USA). A total of 2020 subjects were enrolled randomly with a 2:1 allocation into two subgroups: 145 in the CRD group and 75 in the ad libitum group. The CRD group followed 25% caloric restriction for two-years [78]. After two years of diet treatment, cardiometabolic risk factors such as low-density lipoprotein cholesterol (LDL-c), total cholesterol/high-density lipoprotein cholesterol (HDL-c) ratio, SBP and DBP decreased. Moreover, serum biomarkers such as CRP, insulin sensitivity index and metabolic syndrome score were reduced. Moreover, BW was significantly lower in the CRD group when compared to the ad libitum group (average weight loss in CRD group was 7,5 kg vs average BW increase of 0,1 kg in ad libitum group). These data showed that a period of two–years of CRD was able to decrease cardiometabolic risk factors in middle-aged non-obese subjects. For this reason, it is possible to consider CRD as nutritional therapeutic approach to enhance life expectation and reduce the onset of chronic non-communicable diseases such as diabetes mellitus, cancer, chronic kidney disease, and AH, among others [86,87].
Other studies have been conducted to investigate the role of CRD in the control of AH. In particular, a study performed by Most et al. on caloric restriction (25%), with two years follow–up, evaluated the possible reduction of CV risk factors and insulin resistance in non-obese subjects and whether the results obtained were maintained over time or were limited to the period study. The authors showed a significant weight loss associated to a decrease in SBP and DBP and an improvement in other parameters, such as lipid profile and insulin resistance. These improvements, with the exception of insulin sensitivity, appeared to be maintained over time [77].
Another study examined the impact of CRD (25%) for six–month follow-up period in patients affected by type 2 diabetes mellitus, AH, and glomerular hyperfiltration. The results were positive, since the authors observed that the CRD reduced glomerular hyperfiltration and, improved insulin sensitivity and SBP and DBP values, compared to the control the group that followed a standard diet. In general, it is speculated that CRD ameliorates CV risk factors [76]. To explain the mechanism underlying the reduction in BP induced by CRD, it has been hypothesized that it may act through the activation of the autonomic nervous system. This hypothesis was investigated by Nakano et al, who observed a reduction in SBP and DBP in obese hypertensive patients in CRD treatment (800 kcal/day) with normal sodium content for two weeks [71]. In obese individuals, CRD would appear to improve the balance of night activation between the vagal/sympathetic system. In fact, in obese subjects, there is an alteration of the autonomic control of the heart due to a prevalence of the sympathetic component over the parasympathetic component one in the autonomic equilibrium. A subsequent study confirmed the effects of short-term CRD (three weeks) in combination with a high–intensity exercise program on heart rate variability (HRV) in normotensive obese subjects, demonstrating that a short-term program of CRD associated with high intensity exercise can positively change the autonomic profile, leading to a reduction in HRV and an increase of parasympathetic activity [72]. The long-term effects of CRD on autonomic nervous system activity are relevant. In an animal study, long-term CRD intake would appear to be able to slow down age-related functional changes in the autonomic system. In fact, in male rats, CRD causes an increase in HRV of the highest frequency components (biomarkers of parasympathetic nervous system activity) and reduces the low-frequency component of diastolic pressure variability (biomarkers of sympathetic tone) [84].
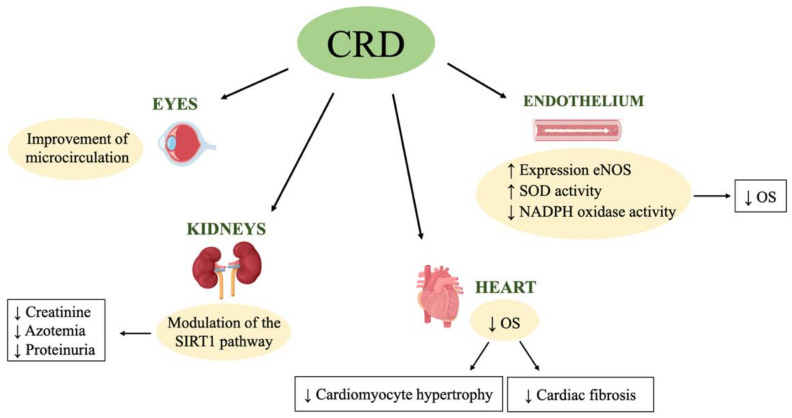
7. Caloric Restriction Diet and Hypertensive Organ Damages
The damage caused by AH is directed to important target organs and develops essentially as a direct and/or indirect consequence of vascular pathology (Figure 3) [88]. In the majority of patients with high BP, the increased values may not be too severe, and the direct damage may develop after years of the AH onset. As previously mentioned, the organs most affected by AH are the heart, kidneys, eye retina, vessels and brain. The pathogenesis of organ damages is complex and varied [89].
Figure 3.
Improvement of caloric restriction diet on hypertensive organ damage. CRD, caloric restriction diet; eNOS, endothelial nitric oxide synthase; NADPH, nicotinamide adenine dinucleotide phosphate hydrogen; OS, oxidative stress; SIRT1, sirtuin 1; SOD, superoxide dismutase, ↑ increase, ↓ decrease.
Increased BP, in addition to the direct damage to the vessel walls, can cause additional pathogenic pathways that include endothelial dysfunction, inflammation, and OS, as well as, all the changes that induce vascular structure alteration, namely arterial rigidity, already underlining to the aging. Therefore, AH is considered to be an accelerated form of cardiovascular aging. Several studies have highlighted a protective action exerted by CRD against hypertensive organ damage.
7.1. Left Ventricular Hypertrophy
Over time, in hypertensive patients, the left ventricular becomes increasingly rigid and diastolic filling is compromised. Left ventricular hypertrophy (LVH) can be described as the thickening of the ventricular wall caused to cope with the overload imposed to the heart for offset peripheral resistances, hence the increase in BP. LVH may occur in both sexes and leads to an increase in either oxygen consumption or energy expenditure of cardiac output [90,91].
It has recently been observed that in hypertensive subjects, LVH is related to hemodynamic and non-hemodynamic mechanisms, which are observed in particular in obese and overweight subjects. In fact, LVH is observed mainly in these patients. The non-hemodynamic mechanisms involve an impairment of lipid metabolism but also the production by adipose tissue of adipokines, such as adiponectin, leptin, and TNF-α [92]. In confirmation of this, recent animal studies have demonstrated that leptin-deficient and leptin-resistant mice exhibit obesity, insulin resistance, and LVH, although the mechanisms that related LVH and alteration of leptin metabolism are not fully understood [93]. Most obese and hypertensive subjects show leptin resistance, and their leptin plasma level is directly related to cardiac hypertrophy [94]. Leptin is involved in heart complications typical of obesity, including AH. It has been shown that an acute increase in leptin does not appear to have any effect on the BP values. On the contrary, a chronic enhancement in leptin increases BP values, stimulating the sympathetic nervous system and simultaneously altering the mechanisms designed to counteract it, such as the natriuresis and the synthesis of NO [95]. Finally, chronic hyperleptinemia appears to be directly related with BP levels [96].
However, leptin may play also a cardioprotective role, related to BW reduction and improvement of myocardial metabolism. Leptin avoids an excessive accumulation of lipids in the heart in obese subjects and inhibits the formation of toxic lipid derivatives, which induce a condition called “cardiac lipotoxicity” [97]. This cardioprotective role exerted by leptin in obese patients, was confirmed only in a study conducted on 1172 black obese women, which revealing an inverse correlation between leptin and LVH severity [98].
CRD is capable of reducing leptin blood levels [74]. This reduction would initially seem to be related to the degree of caloric restriction, but in the long time it appears to be related to the reduction of BW and visceral fat [70]. The CRD seems to exert a cardioprotective action derived from the decrease of OS and inflammation, from the cellular regulation of iron homeostasis and from cardiac remodeling. For these reasons, CRD is definitely a new adjuvant treatment, in combination with pharmacological therapy, for cardiomyopathy in hypertensive patients [99].
Moreover, CRD helps to improve the picture of cardiac hypertrophy through SIRT1 and peroxisome proliferator-activated receptor gamma coactivator 1(PGC1)-α pathways [68]. In fact, as previously reported, CRD would seem to increase the activity of SIRT1, which in turn stimulates PGC1-α, involved in inflammatory signaling pathways. The protective action induced by SIRT1 is related to glucose metabolism as it counteracts the accumulation of cardiac fatty acids, exerting a protective action against cardiotoxicity [68]. Another CRD cardioprotective effect is related to suppression of OS present in AH condition. In fact, recent studies show how ROS production is involved in cardiomyocyte hypertrophy and cardiac fibrosis [100]. Kobara et al., demonstrated that CRD reduces ROS production at the cardiac level, improving the condition of OS and ameliorating cardiac hypertrophy and fibrosis in hypertensive mice, subjected to a 40% reduction in caloric intake compared to the control group, after four weeks [67]. Finally, the last cardioprotective effect induced by CRD is related to the regulation of cellular iron homeostasis. The authors observed a reduction in inflammation, OS, and LVH, associated with a normalization of iron overload in leptin-resistant obese mice subjected to 12 weeks of CRD. This effect would appear to be due to the modulation of gene expression induced by CRD of the genes involved in iron homeostasis at the level of heart tissue [69].
Further studies will be needed for demonstrate if factors such as age and period of following CRD impact on obtained results.
7.2. Kidney Damage—Nephroangiosclerosis
Classically, the term nephroangiosclerosis (NAS) refers to the presence of non-immune-mediated vascular lesions and it is a very common condition in presence of high BP values [101]. The organ damage caused by AH on the renal parenchyma shows up by the increase in plasma creatinine and in early stage by the presence of albuminuria [102]. The classic definition has been revised as the immune cells contribute to determining kidney organ damage. In fact, it has been highlighted how different stimuli, including an increase in angiotensin II production or a diet with a high salt content, can induce a response by the immune system that causes an inflammatory reaction mainly at the level of the organs involved in the control of BP values (such as kidneys, heart and nervous system) [103,104,105]. This observation is confirmed by the fact that hypertensive patients usually present a low-grade chronic inflammatory state. It has also been shown that a high salt diet can stimulate cells of the immune system, including T lymphocytes, which in turn produce pro-inflammatory cytokines, while the activation of monocytes and macrophages can induce both vasoconstriction and renal sodium retention [106]. The three mechanisms described above, taken together, contribute to producing organ damage at the level of the kidney, such as NAS [107]. In terms of NAS, it is important to reduce BP values and proteinuria since they are related to the progression of the nephropathy and to cardiovascular events [108].
According to a recent meta-analysis that examined 27 studies, CRD appears to exert a protective effect against renal damage induced by AH [109]. This meta-analysis demonstrated that in chronic kidney disease (CKD) rat models undergoing CRD, there was a higher reduction in BP, creatinine, azotemia, and proteinuria, compared to a control group fed ad libitum [109]. The authors also demonstrated a survival rate increase at 700-800 days. This nephroprotective effect of CRD would seem to be exerted through the activation of AMP-activated protein kinase (AMPK) and the modulation of the SIRT1 pathways, the latter having been previously described [110]. In particular, the CRD seems to impact, in CKD rat models, on the activity of the AMPK and of the mammalian target of rapamycin (m-TOR) pathways, both implicated in cellular energy metabolism. Increased expression of m-TOR has been shown to accelerate kidney aging, while phosphorylation of AMPK inhibits this process. A short-term, CRD has been seen to induce an up-regulation of AMPK and a down-regulation of m-TOR, resulting in slowing the aging process of renal tubular cells [111]. Therefore, CRD in combination with a reduced sodium intake could be a valid nutritional alternative in the treatment of NAS patients.
In fact, a meta-analysis conducted by D’Elia et al. [112] confirmed the nephroprotective role of sodium restriction, pointing out the relation among dietary sodium restriction and urinary albumin excretion (UAE), a biomarker of CKD progression. The authors considered a total of 11 studies who agreed on the close association between the reduction of UAE induced by a decrease of dietary sodium intake. Moreover, as previously demonstrated in the literature, the authors confirmed that this nutritional approach could ameliorate the therapy based on RAAS-blocking drugs in hypertensive patients. In this perspective, the reduction of UAE induced by low dietary sodium intake could impact on slowing down the progression of CKD, rather than reducing cardiovascular morbidity and mortality.
7.3. Arterial Stiffness
Arterial stiffness (AS) is an important CV risk factor [108], and it induces the rigidity of the arterial wall [113,114]. BP is the main determinant of AS, and the aortic rigidity is accentuated by other concomitant diseases such as diabetes mellitus, metabolic syndrome, CKD, and obesity [115].
The aortic pulsating wave velocity (PWV) correlates with the presence of organ damage and in the heart, an increased AS induces ventricular afterload, ventricular hypertrophy, and reduced coronary perfusion [116]. Sustained increases in BP promote collagen matrix synthesis, causing subsequent vascular thickening and vasal stiffening [117].
The protective role of CRD on AS has been extensively studied. Specifically, CRD seems to exert a protective effect on the endothelium through an antioxidant action and thanks to an increased NO bioavailability [64]. Rippe et al. observed an improvement in carotid artery endothelium-dependent dilation mediated by the enhancer of the expression of endothelial nitric oxide synthase (eNOS) in mice undergoing CRD (approximately 30% of caloric restriction) compared to the control group (fed ad libitum) after 8 weeks [65]. Similar results were observed in a subsequent study, where the authors demonstrated a reduction in nicotinamide adenine dinucleotide phosphate hydrogen (NADPH) oxidase activity and an increase in superoxide dismutase (SOD) and in catalase activities, confirming that the CRD has an important antioxidant action, in animal models [66]. The effect on the increase of NO availability would seem to be exerted by the action of CRD on SIRT1, which deacetylases and activates eNOS and increases the expression of antioxidant genes [118].
A recent meta-analysis [119] examined 11 clinical trials on the correlation between dietary salt restriction and AS. In the analyzed studies, an average decrease in dietary salt restriction highlighted a 2.38% reduction of PWV. This data would seem of great interest, but there are some concerns, common to all the studies examined, such as the duration of the intervention (ranging from a minimum of 1 to a maximum of 6 weeks) and the small samples of enrolled subjects in each study.
7.4. Hypertensive Retinopathy
Hypertensive retinopathy is an ocular disease involving the arteries and veins of the retina, the optic nerve, and the choroid. The cause of this condition is AH. In subjects that have high BP values, over the time, a modification of the retinal arteries takes place, which tends to shrink, and the retinal veins instead tend to assume a different course, no longer linear. These changes can impair normal vision and lead to the formation of ischemic areas of the retina, with the formation of exudates [120]. In more advanced forms, the vision can be compromised and become blurred or distorted. The diagnosis is made by examining the ocular fund which allows the physician to assess the vision, or to see if there are small bleeding or edema. Depending on what can be observable, it can be possible to evaluate the stage of the disease. When AH is associated with diabetes mellitus, both increase the risk of CV complications and the retinopathy becomes more severe. Since the retina is one of the organs most sensitive to changes in microcirculation, signs of damage to this organ have a high prognostic value for myocardial ischemia, carotid sclerosis and coronary artery damage [121].
The role of CRD on the eye has been extensively investigated, especially with regard to age-related eye diseases [122], but no studies have been conducted to investigate the in vivo effect of CRD on hypertensive retinopathy. However, as reported above, it is well known that the control of BP within the normal range, also through CRD, exerts a preventive role against the onset of eye microvascular abnormalities leading to hypertensive retinopathy [123].
8. Secondary AH: Traditional Dietary Nutritional Protocols
To date, secondary AH affects about 5-10% of the hypertensive subjects. In the greater percentage of these cases, it is possible to observe reversible causes [124]. In the population over 65 years of age, the etiology of secondary AH is due to conditions such as renal artery stenosis, CKD, hypothyroidism, hyperaldosteronism, obstructive sleep apnea, and Cushing syndrome [125]. Resistant AH is a condition characterized by high levels of BP (i.e. >140/90 mmHg in the general population and 130/80 mm Hg in diabetic or nephropathic patients) that could not be controlled by medications (for example the combination of three or more antihypertensive drugs belonging to different classes, including diuretics at their maximum tolerated dosage), according to current guidelines [126].
A large number of scientific evidences supports the notion that multiple dietary factors influence BP levels in the general population both in cases of primary and secondary AH [127]. Secondary forms of AH are relatively rare, but their recognition is very important if we consider that some of them can heal permanently after the removal of the cause.
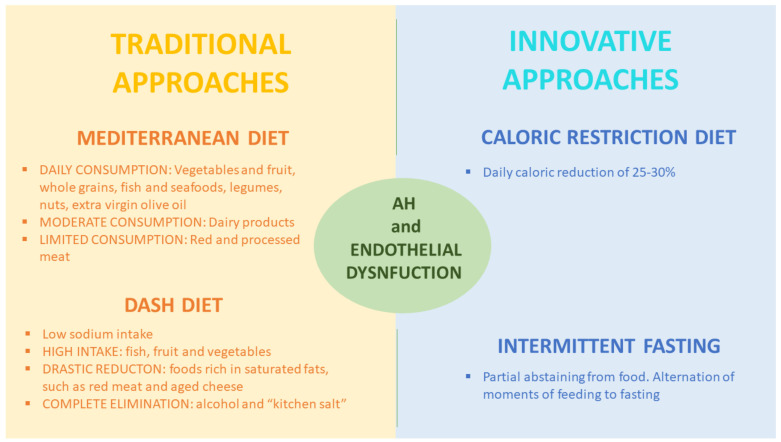
The suspicion of a AH secondary form should raise if (i) AH is resistant to a triple drug therapy that includes a diuretic drug, (ii) AH, characterized by particularly high BP values, diagnosed in young people (about 30 years of age), especially in women, (iii) in case of accelerated or malignant hypertension (renovascular hypertension), (iv) AH becomes suddenly uncontrollable with poly-pharmacological therapy or (v) there is an excessive BP values reduction after administration of RAAS blocking drugs [128]. For the prevention and treatment of secondary AH, as well as for the primary, is used a dietary model similar to the Mediterranean diet called DASH diet is used, which stands for “Dietary approaches to Stop Hypertension”. The DASH diet was developed by studies supported by the U.S National Institute of Health (NIH), as a nutritional approach for the treatment of AH that could be of valuable assistance in terms of reaching optimal BP values, with minimal use of antihypertensive drugs (Figure 4) [129]. The purpose of the DASH diet is to restore homeostasis in all AH patients with an incorrect and unhealthy lifestyle. The DASH diet is considered to be the dietary “gold standard” approach by the American Society of Hypertension in reducing multiple CV risk factors, related to primary and secondary AH [130]. The DASH diet is characterized by a high intake of fish, fruit, and vegetables; a drastic reduction of the consumption of foods rich in saturated fats, such as red meat and aged cheeses; and a complete elimination of alcohol and “kitchen salt” assumption. While CRD, previously discussed, focuses on the number of calories consumed, reducing them by 25–30%, the DASH diet mainly focuses on the quality of micro- and macro-nutrients assumed. Numerous studies have shown that the DASH diet induces a greater reduction in BP values than other dietary interventions or physical exercise programs [131].
Figure 4.
Traditional vs. innovative nutritional approaches for arterial hypertensions and endothelial dysfunction treatment. AH, arterial hypertension.
Most of the studies on salt reduction and weight loss were carried out on middle-aged subjects. In particular, the Trial of Nonpharmacological Interventions in The Elderly (TONE) study showed that, in AH subjects, a moderate salt restriction and weight loss allow the reduction of the number and dosage of antihypertensive drugs [131].
The study carried out by Harsha et al. on 459 adults with SBP values lower than 160 mm Hg and DBP values between 80 and 95 mm Hg demonstrated that the DASH diet reduced BP and represent a nutritional approach to prevent and treat AH [79].
For this reason, the Joint National Committee for Prevention, Treatment and Evaluation of High Blood Pressure strongly recommends following this dietary-nutritional approach to counteract high BP values [132].
Moreover, a recent meta-analysis conducted by D’Elia et al. [133] examined the impact of dietary sodium restriction on central blood pressure (cBP). In fact, if the effects of sodium restriction on peripheral BP are well known, its effects on cBP are scarce. The authors found a statistically significant association between the reduction of BP and central pulse pressure, speculating that sodium restriction also impacts on central BP values. For this reason, a diet with a low sodium intake is a useful tool to counteract the onset and/or the progression of CV disease, especially in normotensive subjects and in prehypertensive patients. This effect supports previous studies that exhort the benefits of a low sodium intake diet for the optimal control of BP values.
9. Other Innovative Nutritional Approaches for Essential AH Treatment
Among the innovative nutritional approaches for AH, considerable interest was aroused by intermittent fasting (IF) [134], which is less restrictive when compared to CRD [135]. IF consists in the assumption of the normal daily caloric quote in a well-defined time gap, daily or weekly [136]. In the IF panorama, two basics scenarios are commonly used. The first one is time-restricted feeding (TRF), and it can be applied in three different alternatives: (i) 16/8, (ii) 18/6, or (iii) 20/4. For example, in the case of “16/8” the first value indicates 16 hours of fast, and 8 indicates the nutritional window. This scheme can be applied to the different variants [136]. An alternative to TRF is a 24-h fasting period (meaning caloric assumption of around 400-600 kcal/day) followed by a 24-h eating period twice or three times per week. In this scenario, there are two possible combinations: (i) 5/2 or (ii) 4/3. For instance, in the “5/2” plan caloric restriction is applied for two days, while normal diet is followed for five days [137].
The overview of the mechanisms that have been hypothesized to assess the correlation between IF and human health are the reduction of OS, improvement of cognition function, and anti-inflammatory effects. With regard to the cardioprotective effects, research has observed a reduction of adipose tissue (visceral); an increased concentration of adiponectin; a decrease of leptin and LDL-c; and prevention of CV diseases, particularly AH [138].
According to recent studies, it is assumed that there are mechanisms to assess the correlation between IF and human health [139], namely circadian rhythm (if disturbed, it can cause an energy imbalance and it means an enhanced risk of chronic non-communicable diseases onset [140]) and gut microbiota dysbiosis (if the microbiota is altered there is an impaired gut permeability, with the promotion of systemic inflammation [141,142,143]). Fasting regiments can also impact on modifiable CV risk factors such as energy intake [144], energy expenditure, [145] and sleep quality [146].
The IF diet has shown positive effects in lowering BP, with a recent study conducted by Erdem et al. [81] evaluating, in 60 subjects, the possible effects on BP values. The obtained results showed that IF significantly reduced 24-hour urinary sodium excretion, being associated with a decrease in SBP (p < 0.001) and DBP (p < 0.039) values. The authors concluded that this reduction is partly related to the decrease sodium consumption during the IF period.
Another interesting study was conducted by Wilhelmi de Toledo et al. [83] on 1422 subjects with one-year follow-up. IF period was comprised between 4 and 21 days, and the enrolled patients were instructed to perform a moderate-intensity physical exercise. Enrolled patients were grouped into four subgroups of 5, 10, 15, and 20 ± 2 days of IF. Every meal contained 200–250 kcal on average. The authors observed a decrease of SBP and DBP in patients who followed IF for a longer period of time; however, in this study, the authors did not specify the amount of salt introduced during the IF period and in particular whether there were any changes in its intake respect to the non-fasting period. They speculated that the drop of BP was due to the enhancement of parasympathetic nervous system activity, of norepinephrine excretion by the kidney and natriuretic peptides, and greater insulin sensitivity. Moreover, it has been observed that the positive effects induced by IF were limited to the nutritional intervention time; in fact, when the nutritional treatment was suspended, the BP values returned to their initial values [84]. To understand whether the reduction of the BP values during the IF are related to reduced caloric intake or reduced salt intake, further randomized clinical trials are needed to assess the impact of each variable on BP values.
During IF, the concentration of plasma glucose decreases. The glycogen reserves in the liver are consumed, and at the same time the gluconeogenesis process is activated. Insulin and IGF-1 levels are reduced in the bloodstream, while glucagon levels are increased. During the lipolysis process, fatty acids are released to be converted through beta oxidation, to be released in the blood and used as a source of energy [147]. An IF nutritional plan improves glucose metabolism even in patients with type 2 diabetes mellitus. As reported in a study conducted by Furmili et al. [82], after 12 weeks of almost 850 kcal daily meals, enrolled subjects showed a weight loss with a normalized fasting glycemia, reduced values of glycated hemoglobin (Hba1c) and increased insulin sensitivity [80].
In animal and in human studies, it has been showed that IF is able to improve physical function, moreover, in mice kept in an IF state, showed greater resistance to running. Other parameters such as balance and coordination were also positive [148].
10. Conclusions
In recent years, there has been a growing interest in identifying an alternative food strategy for achieving and maintaining weight loss in overweight people and to counteract the onset of CV disease. The high BP is one of the main risk factors of serious disabling diseases such as stroke, myocardial ischemia, and heart and kidney failure. In all AH forms, from the milder ones to those refractories to the pharmacotherapy, the correct nutritional approach turns out to be effective in order to reduce in a short period of time the BP values until the target range is obtained. The use of CRD, as an innovative nutritional-dietary approach, highlighted a significant reduction in BP values, an improvement in endothelial dysfunction, causing a decrease in metabolic and inflammatory parameters related to chronic non-communicable diseases. The results of the clinical intervention studies do not allow us to reach solid and definitive conclusions about the long-term efficacy and safety of this nutritional approach, especially in terms of the risk of developing side effects and nutritional inadequacy from lack of macro and micronutrients.
List of Acronyms
| ACE | angiotensin conversion enzyme |
| AH | arterial hypertension |
| AMPK | AMP-activated protein kinase |
| ARB | angiotensin receptor blockers |
| AS | arterial stiffness |
| BMI | body mass index |
| BP | blood pressure |
| BW | body weight |
| CALERIE | Comprehensive Assessment of Long-term Effects of Reducing Intake of Energy |
| cBP | central blood pressure |
| cGMP | cyclic guanosine monophosphate |
| CKD | chronic kidney disease |
| CRD | caloric restriction diet |
| CRP | c-reactive protein |
| CV | cardiovascular diseases |
| DBP | diastolic blood pressure |
| eNOS | endothelial nitric oxide synthase |
| ESC | European Society of Cardiology |
| ESH | European Society of Hypertension |
| HDL-c | high-density lipoprotein cholesterol |
| HRV | heart rate variability |
| IF | intermittent fasting |
| IGF-1 | insulin-like growth factor-1 |
| IL | interleukin |
| LDL-c | low-density lipoprotein cholesterol |
| LVH | left ventricular hypertrophy |
| m-TOR | mammalian target of rapamycin |
| MBIP | model-based image processing |
| MDRD | modification of diet in real disease study |
| NAD | nicotinamide dinucleotide |
| NAS | nephroangiosclerosis |
| NIH | National Institute of Health |
| NO | nitric oxide |
| NOS | nitric oxide-synthase |
| OS | oxidative stress |
| PGC1-α | peroxisome proliferator-activated receptor gamma coactivator 1-α |
| PWV | pulsating wave velocity |
| RAAS | renin–angiotensin–aldosterone system |
| ROS | reactive oxygen species |
| SBP | systolic bloody pressure |
| SIRT1 | sirtuin1 |
| SOD | superoxide dismutase |
| TGF- β1 | transforming growth factor-β1 |
| TNF | tumor necrosis factor |
| TRF | time-restricted feeding |
| UAE | urinary albumin excretion |
| WHO | World Health Organization |
Author Contributions
Conceptualization, N.D.D. and A.N.; writing—original draft preparation, G.M., M.D.L., F.D.D., D.P., and C.G.; writing—review and editing, N.D.D. and A.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kitt J., Fox R., Tucker K.L., McManus R.J. New Approaches in Hypertension Management: A Review of Current and Developing Technologies and Their Potential Impact on Hypertension Care. Curr. Hypertens. Rep. 2019;21:44. doi: 10.1007/s11906-019-0949-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jordan J., Kurschat C., Reuter H. Arterial Hypertension. Dtsch. Arztebl. Int. 2018;115:557–568. doi: 10.3238/arztebl.2018.0557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Healt Organization (WHO) Hypertension. [(accessed on 13 November 2020)]; Available online: https://www.who.int/health-topics/hypertension/#tab=tab_1.
- 4.Lawes C.M., Vander Hoorn S., Rodgers A., International Society of Hypertension Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–1518. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 5.Yusuf S., Hawken S., Ounpuu S., Dans T., Avezum A., Lanas F., McQueen M., Budaj A., Pais P., Varigos J., et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 6.Volpe M., Rosei E.A., Ambrosioni E., Cottone S., Cuspidi C., Borghi C., de Luca N., Fallo F., Ferri C., Morganti A., et al. 2012 consensus document of the Italian Society of Hypertension (SIIA): Strategies to improve blood pressure control in Italy: From global cardiovascular risk stratification to combination therapy. High Blood Press Cardiovasc. Prev. 2013;20:45–52. doi: 10.1007/s40292-013-0007-2. [DOI] [PubMed] [Google Scholar]
- 7.Flack J.M., Adekola B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc. Med. 2020;30:160–164. doi: 10.1016/j.tcm.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 8.Brandhorst S., Longo V.D. Dietary Restrictions and Nutrition in the Prevention and Treatment of Cardiovascular Disease. Circ. Res. 2019;124:952–965. doi: 10.1161/CIRCRESAHA.118.313352. [DOI] [PubMed] [Google Scholar]
- 9.Kord-Varkaneh H., Nazary-Vannani A., Mokhtari Z., Salehi-Sahlabadi A., Rahmani J., Clark C.C.T., Fatahi S., Zanghelini F., Hekmatdoost A., Okunade K., et al. The Influence of Fasting and Energy Restricting Diets on Blood Pressure in Humans: A Systematic Review and Meta-Analysis. High Blood Press Cardiovasc. Prev. 2020;27:271–280. doi: 10.1007/s40292-020-00391-0. [DOI] [PubMed] [Google Scholar]
- 10.Ross R., Faggiotto A., Bowen-Pope D., Raines E. The role of endothelial injury and platelet and macrophage interactions in atherosclerosis. Circulation. 1984;70:III77–III82. [PubMed] [Google Scholar]
- 11.Lerman A., Zeiher A.M. Endothelial function: Cardiac events. Circulation. 2005;111:363–368. doi: 10.1161/01.CIR.0000153339.27064.14. [DOI] [PubMed] [Google Scholar]
- 12.Behrendt D., Ganz P. Endothelial function. From vascular biology to clinical applications. Am. J. Cardiol. 2002;90:40L–48L. doi: 10.1016/S0002-9149(02)02963-6. [DOI] [PubMed] [Google Scholar]
- 13.Davis N., Katz S., Wylie-Rosett J. The effect of diet on endothelial function. Cardiol. Rev. 2007;15:62–66. doi: 10.1097/01.crd.0000218824.79018.cd. [DOI] [PubMed] [Google Scholar]
- 14.Davignon J., Ganz P. Role of endothelial dysfunction in atherosclerosis. Circulation. 2004;109:III27–III32. doi: 10.1161/01.CIR.0000131515.03336.f8. [DOI] [PubMed] [Google Scholar]
- 15.Gonzalez M.A., Selwyn A.P. Endothelial function, inflammation, and prognosis in cardiovascular disease. Am. J. Med. 2003;115:99S–106S. doi: 10.1016/j.amjmed.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan D. The Effects of Hypertension on the Body. [(accessed on 10 November 2020)]; Available online: https://www.healthline.com/health/high-blood-pressure-hypertension/effect-on-body.
- 17.Williams B., Mancia G., Spiering W., Agabiti Rosei E., Azizi M., Burnier M., Clement D.L., Coca A., de Simone G., Dominiczak A., et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 18.Frisoli T.M., Schmieder R.E., Grodzicki T., Messerli F.H. Beyond salt: Lifestyle modifications and blood pressure. Eur. Heart J. 2011;32:3081–3087. doi: 10.1093/eurheartj/ehr379. [DOI] [PubMed] [Google Scholar]
- 19.OsMed Appropriatezza Prescrittiva e Aderenza alle Terapie. Il Quadro Emerso dagli Indicatori OsMed per Alcune Aree Terapeutiche. [(accessed on 15 October 2020)]; Available online: http://www.agenziafarmaco.gov.it/content/appropriatezza-prescrittiva-e-aderenza-alle-terapie-il-quadro-emerso-dagli-indicatori-osmed-
- 20.Scuteri A., Modestino A., Frattari A., di Daniele N., Tesauro M. Occurrence of Hypotension in Older Participants. Which 24-hour ABPM Parameter Better Correlate With? J. Gerontol. A Biol. Sci. Med. Sci. 2012;67:804–810. doi: 10.1093/gerona/glr232. [DOI] [PubMed] [Google Scholar]
- 21.Li J., Zheng H., Du H.B., Tian X.P., Jiang Y.J., Zhang S.L., Kang Y., Li X., Chen J., Lu C., et al. The multiple lifestyle modification for patients with prehypertension and hypertension patients: A systematic review protocol. BMJ Open. 2014;4:e004920. doi: 10.1136/bmjopen-2014-004920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fuchs F.D., Whelton P.K. High Blood Pressure and Cardiovascular Disease. Hypertension. 2020;75:285–292. doi: 10.1161/HYPERTENSIONAHA.119.14240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Versari D., Daghini E., Virdis A., Ghiadoni L., Taddei S. Endothelial dysfunction as a target for prevention of cardiovascular disease. Diabetes Care. 2009;32:S314–S321. doi: 10.2337/dc09-S330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sandoo A., van Zanten J.J., Metsios G.S., Carroll D., Kitas G.D. The endothelium and its role in regulating vascular tone. Open Cardiovasc. Med. J. 2010;4:302–312. doi: 10.2174/1874192401004010302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van Hinsbergh V.W. Endothelium--role in regulation of coagulation and inflammation. Semin. Immunopathol. 2012;34:93–106. doi: 10.1007/s00281-011-0285-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Godo S., Shimokawa H. Endothelial Functions. Arterioscler. Thromb Vasc. Biol. 2017;37:e108–e114. doi: 10.1161/ATVBAHA.117.309813. [DOI] [PubMed] [Google Scholar]
- 27.Forstermann U., Sessa W.C. Nitric oxide synthases: Regulation and function. Eur. Heart J. 2012;33:829–837. doi: 10.1093/eurheartj/ehr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sriram K., Laughlin J.G., Rangamani P., Tartakovsky D.M. Shear-Induced Nitric Oxide Production by Endothelial Cells. Biophys. J. 2016;111:208–221. doi: 10.1016/j.bpj.2016.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee M.Y., Griendling K.K. Redox signaling, vascular function, and hypertension. Antioxid. Redox Signal. 2008;10:1045–1059. doi: 10.1089/ars.2007.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gimbrone M.A., Jr., Garcia-Cardena G. Endothelial Cell Dysfunction and the Pathobiology of Atherosclerosis. Circ. Res. 2016;118:620–636. doi: 10.1161/CIRCRESAHA.115.306301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gryglewski R.J., Palmer R.M., Moncada S. Superoxide anion is involved in the breakdown of endothelium-derived vascular relaxing factor. Nature. 1986;320:454–456. doi: 10.1038/320454a0. [DOI] [PubMed] [Google Scholar]
- 32.Luscher T.F. Endothelial dysfunction: The role and impact of the renin-angiotensin system. Heart. 2000;84:i20–i22:discussion i50. doi: 10.1136/heart.84.suppl_1.i20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Campia U., Tesauro M., di Daniele N., Cardillo C. The vascular endothelin system in obesity and type 2 diabetes: Pathophysiology and therapeutic implications. Life Sci. 2014;118:149–155. doi: 10.1016/j.lfs.2014.02.028. [DOI] [PubMed] [Google Scholar]
- 34.Davenport A.P., Hyndman K.A., Dhaun N., Southan C., Kohan D.E., Pollock J.S., Pollock D.M., Webb D.J., Maguire J.J. Endothelin. Pharmacol. Rev. 2016;68:357–418. doi: 10.1124/pr.115.011833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Flammer A.J., Anderson T., Celermajer D.S., Creager M.A., Deanfield J., Ganz P., Hamburg N.M., Luscher T.F., Shechter M., Taddei S., et al. The assessment of endothelial function: From research into clinical practice. Circulation. 2012;126:753–767. doi: 10.1161/CIRCULATIONAHA.112.093245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dharmashankar K., Widlansky M.E. Vascular endothelial function and hypertension: Insights and directions. Curr. Hypertens. Rep. 2010;12:448–455. doi: 10.1007/s11906-010-0150-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dinh Q.N., Drummond G.R., Sobey C.G., Chrissobolis S. Roles of inflammation, oxidative stress, and vascular dysfunction in hypertension. Biomed. Res. Int. 2014;2014:406960. doi: 10.1155/2014/406960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mordi I., Mordi N., Delles C., Tzemos N. Endothelial dysfunction in human essential hypertension. J. Hypertens. 2016;34:1464–1472. doi: 10.1097/HJH.0000000000000965. [DOI] [PubMed] [Google Scholar]
- 39.Yannoutsos A., Levy B.I., Safar M.E., Slama G., Blacher J. Pathophysiology of hypertension: Interactions between macro and microvascular alterations through endothelial dysfunction. J. Hypertens. 2014;32:216–224. doi: 10.1097/HJH.0000000000000021. [DOI] [PubMed] [Google Scholar]
- 40.Most J., Tosti V., Redman L.M., Fontana L. Calorie restriction in humans: An update. Ageing Res. Rev. 2017;39:36–45. doi: 10.1016/j.arr.2016.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fontana L., Meyer T.E., Klein S., Holloszy J.O. Long-term calorie restriction is highly effective in reducing the risk for atherosclerosis in humans. Proc. Natl. Acad. Sci. USA. 2004;101:6659–6663. doi: 10.1073/pnas.0308291101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Osborne T.B., Mendel L.B., Ferry E.L. The Effect of Retardation of Growth Upon the Breeding Period and Duration of Life of Rats. Science. 1917;45:294–295. doi: 10.1126/science.45.1160.294. [DOI] [PubMed] [Google Scholar]
- 43.Weindruch R., Walford R.L., Fligiel S., Guthrie D. The retardation of aging in mice by dietary restriction: Longevity, cancer, immunity and lifetime energy intake. J. Nutr. 1986;116:641–654. doi: 10.1093/jn/116.4.641. [DOI] [PubMed] [Google Scholar]
- 44.Lee S.H., Min K.J. Caloric restriction and its mimetics. BMB Rep. 2013;46:181–187. doi: 10.5483/BMBRep.2013.46.4.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang Y., Ikeno Y., Qi W., Chaudhuri A., Li Y., Bokov A., Thorpe S.R., Baynes J.W., Epstein C., Richardson A., et al. Mice deficient in both Mn superoxide dismutase and glutathione peroxidase-1 have increased oxidative damage and a greater incidence of pathology but no reduction in longevity. J. Gerontol. A Biol. Sci. Med. Sci. 2009;64:1212–1220. doi: 10.1093/gerona/glp132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smirnov A., Panatta E., Lena A., Castiglia D., di Daniele N., Melino G., Candi E. FOXM1 regulates proliferation, senescence and oxidative stress in keratinocytes and cancer cells. Aging (Albany N. Y.) 2016;8:1384–1397. doi: 10.18632/aging.100988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Singh R., Lakhanpal D., Kumar S., Sharma S., Kataria H., Kaur M., Kaur G. Late-onset intermittent fasting dietary restriction as a potential intervention to retard age-associated brain function impairments in male rats. Age. 2012;34:917–933. doi: 10.1007/s11357-011-9289-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Anisimov V.N., Bartke A. The key role of growth hormone-insulin-IGF-1 signaling in aging and cancer. Crit. Rev. Oncol. Hematol. 2013;87:201–223. doi: 10.1016/j.critrevonc.2013.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Willcox D.C., Willcox B.J., Todoriki H., Curb J.D., Suzuki M. Caloric restriction and human longevity: What can we learn from the Okinawans? Biogerontology. 2006;7:173–177. doi: 10.1007/s10522-006-9008-z. [DOI] [PubMed] [Google Scholar]
- 50.Colman R.J., Anderson R.M., Johnson S.C., Kastman E.K., Kosmatka K.J., Beasley T.M., Allison D.B., Cruzen C., Simmons H.A., Kemnitz J.W., et al. Caloric restriction delays disease onset and mortality in rhesus monkeys. Science. 2009;325:201–204. doi: 10.1126/science.1173635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mattison J.A., Roth G.S., Beasley T.M., Tilmont E.M., Handy A.M., Herbert R.L., Longo D.L., Allison D.B., Young J.E., Bryant M., et al. Impact of caloric restriction on health and survival in rhesus monkeys from the NIA study. Nature. 2012;489:318–321. doi: 10.1038/nature11432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Guarente L. Sir2 links chromatin silencing, metabolism, and aging. Genes Dev. 2000;14:1021–1026. [PubMed] [Google Scholar]
- 53.Toiber D., Sebastian C., Mostoslavsky R. Characterization of nuclear sirtuins: Molecular mechanisms and physiological relevance. Handb. Exp. Pharmacol. 2011;206:189–224. doi: 10.1007/978-3-642-21631-2_9. [DOI] [PubMed] [Google Scholar]
- 54.Lee S.H., Lee J.H., Lee H.Y., Min K.J. Sirtuin signaling in cellular senescence and aging. BMB Rep. 2019;52:24–34. doi: 10.5483/BMBRep.2019.52.1.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yamashita S., Ogawa K., Ikei T., Udono M., Fujiki T., Katakura Y. SIRT1 prevents replicative senescence of normal human umbilical cord fibroblast through potentiating the transcription of human telomerase reverse transcriptase gene. Biochem. Biophys. Res. Commun. 2012;417:630–634. doi: 10.1016/j.bbrc.2011.12.021. [DOI] [PubMed] [Google Scholar]
- 56.Jeong S.M., Xiao C., Finley L.W., Lahusen T., Souza A.L., Pierce K., Li Y.H., Wang X., Laurent G., German N.J., et al. SIRT4 has tumor-suppressive activity and regulates the cellular metabolic response to DNA damage by inhibiting mitochondrial glutamine metabolism. Cancer Cell. 2013;23:450–463. doi: 10.1016/j.ccr.2013.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cohen H.Y., Miller C., Bitterman K.J., Wall N.R., Hekking B., Kessler B., Howitz K.T., Gorospe M., de Cabo R., Sinclair D.A. Calorie restriction promotes mammalian cell survival by inducing the SIRT1 deacetylase. Science. 2004;305:390–392. doi: 10.1126/science.1099196. [DOI] [PubMed] [Google Scholar]
- 58.Chen D., Bruno J., Easlon E., Lin S.J., Cheng H.L., Alt F.W., Guarente L. Tissue-specific regulation of SIRT1 by calorie restriction. Genes Dev. 2008;22:1753–1757. doi: 10.1101/gad.1650608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Deota S., Chattopadhyay T., Ramachandran D., Armstrong E., Camacho B., Maniyadath B., Fulzele A., Gonzalez-de-Peredo A., Denu J.M., Kolthur-Seetharam U. Identification of a Tissue-Restricted Isoform of SIRT1 Defines a Regulatory Domain that Encodes Specificity. Cell Rep. 2017;18:3069–3077. doi: 10.1016/j.celrep.2017.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Meyer T.E., Kovacs S.J., Ehsani A.A., Klein S., Holloszy J.O., Fontana L. Long-term caloric restriction ameliorates the decline in diastolic function in humans. J. Am. Coll. Cardiol. 2006;47:398–402. doi: 10.1016/j.jacc.2005.08.069. [DOI] [PubMed] [Google Scholar]
- 61.Sohal R.S., Weindruch R. Oxidative stress, caloric restriction, and aging. Science. 1996;273:59–63. doi: 10.1126/science.273.5271.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liguori I., Russo G., Curcio F., Bulli G., Aran L., Della-Morte D., Gargiulo G., Testa G., Cacciatore F., Bonaduce D., et al. Oxidative stress, aging, and diseases. Clin. Interv. Aging. 2018;13:757–772. doi: 10.2147/CIA.S158513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ingram D.K., Cutler R.G., Weindruch R., Renquist D.M., Knapka J.J., April M., Belcher C.T., Clark M.A., Hatcherson C.D., Marriott B.M., et al. Dietary restriction and aging: The initiation of a primate study. J. Gerontol. 1990;45:B148–B163. doi: 10.1093/geronj/45.5.B148. [DOI] [PubMed] [Google Scholar]
- 64.Zanetti M., Gortan Cappellari G., Burekovic I., Barazzoni R., Stebel M., Guarnieri G. Caloric restriction improves endothelial dysfunction during vascular aging: Effects on nitric oxide synthase isoforms and oxidative stress in rat aorta. Exp. Gerontol. 2010;45:848–855. doi: 10.1016/j.exger.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 65.Rippe C., Lesniewski L., Connell M., LaRocca T., Donato A., Seals D. Short-term calorie restriction reverses vascular endothelial dysfunction in old mice by increasing nitric oxide and reducing oxidative stress. Aging Cell. 2010;9:304–312. doi: 10.1111/j.1474-9726.2010.00557.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Donato A.J., Walker A.E., Magerko K.A., Bramwell R.C., Black A.D., Henson G.D., Lawson B.R., Lesniewski L.A., Seals D.R. Life-long caloric restriction reduces oxidative stress and preserves nitric oxide bioavailability and function in arteries of old mice. Aging Cell. 2013;12:772–783. doi: 10.1111/acel.12103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kobara M., Furumori-Yukiya A., Kitamura M., Matsumura M., Ohigashi M., Toba H., Nakata T. Short-Term Caloric Restriction Suppresses Cardiac Oxidative Stress and Hypertrophy Caused by Chronic Pressure Overload. J. Card. Fail. 2015;21:656–666. doi: 10.1016/j.cardfail.2015.04.016. [DOI] [PubMed] [Google Scholar]
- 68.Waldman M., Cohen K., Yadin D., Nudelman V., Gorfil D., Laniado-Schwartzman M., Kornwoski R., Aravot D., Abraham N.G., Arad M., et al. Regulation of diabetic cardiomyopathy by caloric restriction is mediated by intracellular signaling pathways involving ‘SIRT1 and PGC-1alpha’. Cardiovasc. Diabetol. 2018;17:111. doi: 10.1186/s12933-018-0754-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.An H.S., Lee J.Y., Choi E.B., Jeong E.A., Shin H.J., Kim K.E., Park K.A., Jin Z., Lee J.E., Koh J.S., et al. Caloric restriction reverses left ventricular hypertrophy through the regulation of cardiac iron homeostasis in impaired leptin signaling mice. Sci. Rep. 2020;10:7176. doi: 10.1038/s41598-020-64201-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wadden T.A., Considine R.V., Foster G.D., Anderson D.A., Sarwer D.B., Caro J.S. Short- and long-term changes in serum leptin dieting obese women: Effects of caloric restriction and weight loss. J. Clin. Endocrinol. Metab. 1998;83:214–218. doi: 10.1210/jc.83.1.214. [DOI] [PubMed] [Google Scholar]
- 71.Nakano Y., Oshima T., Sasaki S., Higashi Y., Ozono R., Takenaka S., Miura F., Hirao H., Matsuura H., Chayama K., et al. Calorie restriction reduced blood pressure in obesity hypertensives by improvement of autonomic nerve activity and insulin sensitivity. J. Cardiovasc. Pharmacol. 2001;38:S69–S74. doi: 10.1097/00005344-200110001-00015. [DOI] [PubMed] [Google Scholar]
- 72.Facchini M., Malfatto G., Sala L., Silvestri G., Fontana P., Lafortuna C., Sartorio A. Changes of autonomic cardiac profile after a 3-week integrated body weight reduction program in severely obese patients. J. Endocrinol. Invest. 2003;26:138–142. doi: 10.1007/BF03345142. [DOI] [PubMed] [Google Scholar]
- 73.Das S.K., Gilhooly C.H., Golden J.K., Pittas A.G., Fuss P.J., Cheatham R.A., Tyler S., Tsay M., McCrory M.A., Lichtenstein A.H., et al. Long-term effects of 2 energy-restricted diets differing in glycemic load on dietary adherence, body composition, and metabolism in CALERIE: A 1-y randomized controlled trial. Am. J. Clin. Nutr. 2007;85:1023–1030. doi: 10.1093/ajcn/85.4.1023. [DOI] [PubMed] [Google Scholar]
- 74.Lecoultre V., Ravussin E., Redman L.M. The fall in leptin concentration is a major determinant of the metabolic adaptation induced by caloric restriction independently of the changes in leptin circadian rhythms. J. Clin. Endocrinol. Metab. 2011;96:E1512–E1516. doi: 10.1210/jc.2011-1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Stewart T.M., Bhapkar M., Das S., Galan K., Martin C.K., McAdams L., Pieper C., Redman L., Roberts S., Stein R.I., et al. Comprehensive Assessment of Long-term Effects of Reducing Intake of Energy Phase 2 (CALERIE Phase 2) screening and recruitment: Methods and results. Contemp. Clin. Trials. 2013;34:10–20. doi: 10.1016/j.cct.2012.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ruggenenti P., Abbate M., Ruggiero B., Rota S., Trillini M., Aparicio C., Parvanova A., Petrov Iliev I., Pisanu G., Perna A., et al. Renal and Systemic Effects of Calorie Restriction in Patients With Type 2 Diabetes With Abdominal Obesity: A Randomized Controlled Trial. Diabetes. 2017;66:75–86. doi: 10.2337/db16-0607. [DOI] [PubMed] [Google Scholar]
- 77.Most J., Gilmore L.A., Smith S.R., Han H., Ravussin E., Redman L.M. Significant improvement in cardiometabolic health in healthy nonobese individuals during caloric restriction-induced weight loss and weight loss maintenance. Am. J. Physiol. Endocrinol. Metab. 2018;314:E396–E405. doi: 10.1152/ajpendo.00261.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kraus W.E., Bhapkar M., Huffman K.M., Pieper C.F., Krupa Das S., Redman L.M., Villareal D.T., Rochon J., Roberts S.B., Ravussin E., et al. 2 years of calorie restriction and cardiometabolic risk (CALERIE): Exploratory outcomes of a multicentre, phase 2, randomised controlled trial. Lancet Diabetes Endocrinol. 2019;7:673–683. doi: 10.1016/S2213-8587(19)30151-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Harsha D.W., Lin P.H., Obarzanek E., Karanja N.M., Moore T.J., Caballero B., DASH Collaborative Research Group Dietary Approaches to Stop Hypertension: A summary of study results. J. Am. Diet Assoc. 1999;99:S35–S39. doi: 10.1016/S0002-8223(99)00414-9. [DOI] [PubMed] [Google Scholar]
- 80.Arnason T.G., Bowen M.W., Mansell K.D. Effects of intermittent fasting on health markers in those with type 2 diabetes: A pilot study. World J. Diabetes. 2017;8:154–164. doi: 10.4239/wjd.v8.i4.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Erdem Y., Ozkan G., Ulusoy S., Arici M., Derici U., Sengul S., Sindel S., Erturk S., Turkish Society of H., Renal D. The effect of intermittent fasting on blood pressure variability in patients with newly diagnosed hypertension or prehypertension. J. Am. Soc. Hypertens. 2018;12:42–49. doi: 10.1016/j.jash.2017.11.008. [DOI] [PubMed] [Google Scholar]
- 82.Furmli S., Elmasry R., Ramos M., Fung J. Therapeutic use of intermittent fasting for people with type 2 diabetes as an alternative to insulin. BMJ Case Rep. 2018;2018 doi: 10.1136/bcr-2017-221854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wilhelmi de Toledo F., Grundler F., Bergouignan A., Drinda S., Michalsen A. Safety, health improvement and well-being during a 4 to 21-day fasting period in an observational study including 1422 subjects. PLoS ONE. 2019;14:e0209353. doi: 10.1371/journal.pone.0209353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mager D.E., Wan R., Brown M., Cheng A., Wareski P., Abernethy D.R., Mattson M.P. Caloric restriction and intermittent fasting alter spectral measures of heart rate and blood pressure variability in rats. FASEB J. 2006;20:631–637. doi: 10.1096/fj.05-5263com. [DOI] [PubMed] [Google Scholar]
- 85.Rickman A.D., Williamson D.A., Martin C.K., Gilhooly C.H., Stein R.I., Bales C.W., Roberts S., Das S.K. The CALERIE Study: Design and methods of an innovative 25% caloric restriction intervention. Contemp. Clin. Trials. 2011;32:874–881. doi: 10.1016/j.cct.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Di Renzo L., Gualtieri P., Romano L., Marrone G., Noce A., Pujia A., Perrone M.A., Aiello V., Colica C., de Lorenzo A. Role of Personalized Nutrition in Chronic-Degenerative Diseases. Nutrients. 2019;11:1707. doi: 10.3390/nu11081707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Di Daniele N. The Role of Preventive Nutrition in Chronic Non-Communicable Diseases. Nutrients. 2019;11:1074. doi: 10.3390/nu11051074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bidani A.K., Griffin K.A. Basic science: Hypertensive target organ damage. J. Am. Soc. Hypertens. 2015;9:235–237; quiz 238. doi: 10.1016/j.jash.2015.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mensah G.A., Croft J.B., Giles W.H. The heart, kidney, and brain as target organs in hypertension. Cardiol. Clin. 2002;20:225–247. doi: 10.1016/S0733-8651(02)00004-8. [DOI] [PubMed] [Google Scholar]
- 90.Aronow W.S. Hypertension and left ventricular hypertrophy. Ann. Transl. Med. 2017;5:310. doi: 10.21037/atm.2017.06.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gallu M., Marrone G., Legramante J.M., de Lorenzo A., Di Daniele N., Noce A. Female Sex as a Thromboembolic Risk Factor in the Era of Nonvitamin K Antagonist Oral Anticoagulants. Cardiovasc. Ther. 2020;2020:1743927. doi: 10.1155/2020/1743927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Landecho M.F., Tuero C., Valenti V., Bilbao I., de la Higuera M., Fruhbeck G. Relevance of Leptin and Other Adipokines in Obesity-Associated Cardiovascular Risk. Nutrients. 2019;11:2664. doi: 10.3390/nu11112664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hall M.E., Harmancey R., Stec D.E. Lean heart: Role of leptin in cardiac hypertrophy and metabolism. World J. Cardiol. 2015;7:511–524. doi: 10.4330/wjc.v7.i9.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Raju S.V., Zheng M., Schuleri K.H., Phan A.C., Bedja D., Saraiva R.M., Yiginer O., Vandegaer K., Gabrielson K.L., O’Donnell C.P., et al. Activation of the cardiac ciliary neurotrophic factor receptor reverses left ventricular hypertrophy in leptin-deficient and leptin-resistant obesity. Proc. Natl. Acad. Sci. USA. 2006;103:4222–4227. doi: 10.1073/pnas.0510460103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Beltowski J. Role of leptin in blood pressure regulation and arterial hypertension. J. Hypertens. 2006;24:789–801. doi: 10.1097/01.hjh.0000222743.06584.66. [DOI] [PubMed] [Google Scholar]
- 96.Bravo P.E., Morse S., Borne D.M., Aguilar E.A., Reisin E. Leptin and hypertension in obesity. Vasc. Health Risk Manag. 2006;2:163–169. doi: 10.2147/vhrm.2006.2.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chiu H.C., Kovacs A., Ford D.A., Hsu F.F., Garcia R., Herrero P., Saffitz J.E., Schaffer J.E. A novel mouse model of lipotoxic cardiomyopathy. J. Clin. Invest. 2001;107:813–822. doi: 10.1172/JCI10947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kamimura D., Suzuki T., Wang W., deShazo M., Hall J.E., Winniford M.D., Kullo I.J., Mosley T.H., Butler K.R., Hall M.E. Higher plasma leptin levels are associated with reduced left ventricular mass and left ventricular diastolic stiffness in black women: Insights from the Genetic Epidemiology Network of Arteriopathy (GENOA) study. Hypertens. Res. 2018;41:629–638. doi: 10.1038/s41440-018-0062-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Abel E.D., Litwin S.E., Sweeney G. Cardiac remodeling in obesity. Physiol. Rev. 2008;88:389–419. doi: 10.1152/physrev.00017.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Maulik S.K., Kumar S. Oxidative stress and cardiac hypertrophy: A review. Toxicol. Mech. Methods. 2012;22:359–366. doi: 10.3109/15376516.2012.666650. [DOI] [PubMed] [Google Scholar]
- 101.Cianci R., Barbano B., Martina P., Gigante A., Polidori L., Lai S., Ascoli G., de Francesco I., di Donato D., Fuiano G., et al. Nephroangiosclerosis and its pharmacological approach. Curr. Vasc. Pharmacol. 2011;9:238–243. doi: 10.2174/157016111794519309. [DOI] [PubMed] [Google Scholar]
- 102.Yamanouchi M., Hoshino J., Ubara Y., Takaichi K., Kinowaki K., Fujii T., Ohashi K., Mise K., Toyama T., Hara A., et al. Clinicopathological predictors for progression of chronic kidney disease in nephrosclerosis: A biopsy-based cohort study. Nephrol. Dial. Transplant. 2019;34:1182–1188. doi: 10.1093/ndt/gfy121. [DOI] [PubMed] [Google Scholar]
- 103.O’Donnell M., Mente A., Yusuf S. Sodium intake and cardiovascular health. Circ. Res. 2015;116:1046–1057. doi: 10.1161/CIRCRESAHA.116.303771. [DOI] [PubMed] [Google Scholar]
- 104.Wade B., Petrova G., Mattson D.L. Role of immune factors in angiotensin II-induced hypertension and renal damage in Dahl salt-sensitive rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2018;314:R323–R333. doi: 10.1152/ajpregu.00044.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Noce A., Marrone G., di Lauro M., Urciuoli S., Pietroboni Zaitseva A., Wilson Jones G., di Daniele N., Romani A. Cardiovascular Protection of Nephropathic Male Patients by Oral Food Supplements. Cardiovasc. Ther. 2020;2020:1807941. doi: 10.1155/2020/1807941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mattson D.L., James L., Berdan E.A., Meister C.J. Immune suppression attenuates hypertension and renal disease in the Dahl salt-sensitive rat. Hypertension. 2006;48:149–156. doi: 10.1161/01.HYP.0000228320.23697.29. [DOI] [PubMed] [Google Scholar]
- 107.Lu X., Crowley S.D. Inflammation in Salt-Sensitive Hypertension and Renal Damage. Curr. Hypertens. Rep. 2018;20:103. doi: 10.1007/s11906-018-0903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hildebrand A.M., Garg A.X. Blood pressure targets in chronic kidney disease: Does proteinuria dictate how low we go? CMAJ. 2013;185:941–942. doi: 10.1503/cmaj.130168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Xu X.M., Cai G.Y., Bu R., Wang W.J., Bai X.Y., Sun X.F., Chen X.M. Beneficial Effects of Caloric Restriction on Chronic Kidney Disease in Rodent Models: A Meta-Analysis and Systematic Review. PLoS ONE. 2015;10:e0144442. doi: 10.1371/journal.pone.0144442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wang S.Y., Cai G.Y., Chen X.M. Energy restriction in renal protection. Br. J. Nutr. 2018;120:1149–1158. doi: 10.1017/S0007114518002684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Dong D., Cai G.Y., Ning Y.C., Wang J.C., Lv Y., Hong Q., Cui S.Y., Fu B., Guo Y.N., Chen X.M. Alleviation of senescence and epithelial-mesenchymal transition in aging kidney by short-term caloric restriction and caloric restriction mimetics via modulation of AMPK/mTOR signaling. Oncotarget. 2017;8:16109–16121. doi: 10.18632/oncotarget.14884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.D’Elia L., Rossi G., Schiano di Cola M., Savino I., Galletti F., Strazzullo P. Meta-Analysis of the Effect of Dietary Sodium Restriction with or without Concomitant Renin-Angiotensin-Aldosterone System-Inhibiting Treatment on Albuminuria. Clin. J. Am. Soc. Nephrol. 2015;10:1542–1552. doi: 10.2215/CJN.09110914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Cheung Y.F. Arterial stiffness in the young: Assessment, determinants, and implications. Korean Circ. J. 2010;40:153–162. doi: 10.4070/kcj.2010.40.4.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Schinzari F., Iantorno M., Campia U., Mores N., Rovella V., Tesauro M., di Daniele N., Cardillo C. Vasodilator responses and endothelin-dependent vasoconstriction in metabolically healthy obesity and the metabolic syndrome. Am. J. Physiol. Endocrinol. Metab. 2015;309:E787–E792. doi: 10.1152/ajpendo.00278.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Noce A., Fabrini R., Dessi M., Bocedi A., Santini S., Rovella V., Pastore A., Tesauro M., Bernardini S., di Daniele N., et al. Erythrocyte glutathione transferase activity: A possible early biomarker for blood toxicity in uremic diabetic patients. Acta Diabetol. 2014;51:219–224. doi: 10.1007/s00592-013-0497-3. [DOI] [PubMed] [Google Scholar]
- 116.Covic A., Gusbeth-Tatomir P., Goldsmith D.J. Arterial stiffness in renal patients: An update. Am. J. Kidney Dis. 2005;45:965–977. doi: 10.1053/j.ajkd.2005.02.026. [DOI] [PubMed] [Google Scholar]
- 117.Sun Z. Aging, arterial stiffness, and hypertension. Hypertension. 2015;65:252–256. doi: 10.1161/HYPERTENSIONAHA.114.03617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Martens C.R., Seals D.R. Practical alternatives to chronic caloric restriction for optimizing vascular function with ageing. J. Physiol. 2016;594:7177–7195. doi: 10.1113/JP272348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.D’Elia L., Galletti F., La Fata E., Sabino P., Strazzullo P. Effect of dietary sodium restriction on arterial stiffness: Systematic review and meta-analysis of the randomized controlled trials. J. Hypertens. 2018;36:734–743. doi: 10.1097/HJH.0000000000001604. [DOI] [PubMed] [Google Scholar]
- 120.Henderson A.D., Bruce B.B., Newman N.J., Biousse V. Hypertension-related eye abnormalities and the risk of stroke. Rev. Neurol. Dis. 2011;8:1–9. [PMC free article] [PubMed] [Google Scholar]
- 121.Chatterjee S., Chattopadhyay S., Hope-Ross M., Lip P.L. Hypertension and the eye: Changing perspectives. J. Hum. Hypertens. 2002;16:667–675. doi: 10.1038/sj.jhh.1001472. [DOI] [PubMed] [Google Scholar]
- 122.Kawashima M., Ozawa Y., Shinmura K., Inaba T., Nakamura S., Kawakita T., Watanabe M., Tsubota K. Calorie restriction (CR) and CR mimetics for the prevention and treatment of age-related eye disorders. Exp. Gerontol. 2013;48:1096–1100. doi: 10.1016/j.exger.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 123.Katsi V., Marketou M., Vlachopoulos C., Tousoulis D., Souretis G., Papageorgiou N., Stefanadis C., Vardas P., Kallikazaros I. Impact of arterial hypertension on the eye. Curr. Hypertens. Rep. 2012;14:581–590. doi: 10.1007/s11906-012-0283-6. [DOI] [PubMed] [Google Scholar]
- 124.Viera A.J., Neutze D.M. Diagnosis of secondary hypertension: An age-based approach. Am. Fam. Phys. 2010;82:1471–1478. [PubMed] [Google Scholar]
- 125.Charles L., Triscott J., Dobbs B. Secondary Hypertension: Discovering the Underlying Cause. Am. Fam. Phys. 2017;96:453–461. [PubMed] [Google Scholar]
- 126.Calhoun D.A., Jones D., Textor S., Goff D.C., Murphy T.P., Toto R.D., White A., Cushman W.C., White W., Sica D., et al. Resistant hypertension: Diagnosis, evaluation, and treatment: A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation. 2008;117:e510–e526. doi: 10.1161/CIRCULATIONAHA.108.189141. [DOI] [PubMed] [Google Scholar]
- 127.Siddiqui M.A., Mittal P.K., Little B.P., Miller F.H., Akduman E.I., Ali K., Sartaj S., Moreno C.C. Secondary Hypertension and Complications: Diagnosis and Role of Imaging. Radiographics. 2019;39:1036–1055. doi: 10.1148/rg.2019180184. [DOI] [PubMed] [Google Scholar]
- 128.Acelajado M.C., Calhoun D.A. Resistant hypertension, secondary hypertension, and hypertensive crises: Diagnostic evaluation and treatment. Cardiol. Clin. 2010;28:639–654. doi: 10.1016/j.ccl.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 129.Filippou C.D., Tsioufis C.P., Thomopoulos C.G., Mihas C.C., Dimitriadis K.S., Sotiropoulou L.I., Chrysochoou C.A., Nihoyannopoulos P.I., Tousoulis D.M. Dietary Approaches to Stop Hypertension (DASH) Diet and Blood Pressure Reduction in Adults with and without Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. 2020;11:1150–1160. doi: 10.1093/advances/nmaa041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Troyer J.L., Racine E.F., Ngugi G.W., McAuley W.J. The effect of home-delivered Dietary Approach to Stop Hypertension (DASH) meals on the diets of older adults with cardiovascular disease. Am. J. Clin. Nutr. 2010;91:1204–1212. doi: 10.3945/ajcn.2009.28780. [DOI] [PubMed] [Google Scholar]
- 131.Fu J., Liu Y., Zhang L., Zhou L., Li D., Quan H., Zhu L., Hu F., Li X., Meng S., et al. Nonpharmacologic Interventions for Reducing Blood Pressure in Adults With Prehypertension to Established Hypertension. J. Am. Heart Assoc. 2020;9:e016804. doi: 10.1161/JAHA.120.016804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch. Intern. Med. 1997;157:2413–2446. doi: 10.1001/archinte.1997.00440420033005. [DOI] [PubMed] [Google Scholar]
- 133.D’Elia L., La Fata E., Giaquinto A., Strazzullo P., Galletti F. Effect of dietary salt restriction on central blood pressure: A systematic review and meta-analysis of the intervention studies. J. Clin. Hypertens. 2020;22:814–825. doi: 10.1111/jch.13852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Malinowski B., Zalewska K., Wesierska A., Sokolowska M.M., Socha M., Liczner G., Pawlak-Osinska K., Wicinski M. Intermittent Fasting in Cardiovascular Disorders-An Overview. Nutrients. 2019;11:673. doi: 10.3390/nu11030673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Barnosky A.R., Hoddy K.K., Unterman T.G., Varady K.A. Intermittent fasting vs daily calorie restriction for type 2 diabetes prevention: A review of human findings. Transl. Res. 2014;164:302–311. doi: 10.1016/j.trsl.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 136.Johnstone A. Fasting for weight loss: An effective strategy or latest dieting trend? Int. J. Obes. 2015;39:727–733. doi: 10.1038/ijo.2014.214. [DOI] [PubMed] [Google Scholar]
- 137.Harvie M., Howell A. Potential Benefits and Harms of Intermittent Energy Restriction and Intermittent Fasting Amongst Obese, Overweight and Normal Weight Subjects-A Narrative Review of Human and Animal Evidence. Behav. Sci. 2017;7:4. doi: 10.3390/bs7010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Aly S.M. Role of intermittent fasting on improving health and reducing diseases. Int. J. Health Sci. 2014;8:V–VI. doi: 10.12816/0023985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Patterson R.E., Sears D.D. Metabolic Effects of Intermittent Fasting. Annu. Rev. Nutr. 2017;37:371–393. doi: 10.1146/annurev-nutr-071816-064634. [DOI] [PubMed] [Google Scholar]
- 140.Eckel-Mahan K.L., Patel V.R., de Mateo S., Orozco-Solis R., Ceglia N.J., Sahar S., Dilag-Penilla S.A., Dyar K.A., Baldi P., Sassone-Corsi P. Reprogramming of the circadian clock by nutritional challenge. Cell. 2013;155:1464–1478. doi: 10.1016/j.cell.2013.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Turnbaugh P.J., Ley R.E., Mahowald M.A., Magrini V., Mardis E.R., Gordon J.I. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–1031. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- 142.Noce A., Marrone G., Di Daniele F., Ottaviani E., Wilson Jones G., Bernini R., Romani A., Rovella V. Impact of Gut Microbiota Composition on Onset and Progression of Chronic Non-Communicable Diseases. Nutrients. 2019;11:1073. doi: 10.3390/nu11051073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Noce A., Tarantino A., Tsague Djoutsop C., Erald V., de Lorenzo A., di Daniele N. Gut Microbioma Population: An Indicator Really Sensible to Any Change in Age, Diet, Metabolic Syndrome, and Life-Style. Mediat. Inflam. 2014;2014 doi: 10.1155/2014/901308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Chowdhury E.A., Richardson J.D., Tsintzas K., Thompson D., Betts J.A. Effect of extended morning fasting upon ad libitum lunch intake and associated metabolic and hormonal responses in obese adults. Int. J. Obes. 2016;40:305–311. doi: 10.1038/ijo.2015.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Hatori M., Vollmers C., Zarrinpar A., DiTacchio L., Bushong E.A., Gill S., Leblanc M., Chaix A., Joens M., Fitzpatrick J.A., et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. 2012;15:848–860. doi: 10.1016/j.cmet.2012.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Yamaguchi M., Uemura H., Katsuura-Kamano S., Nakamoto M., Hiyoshi M., Takami H., Sawachika F., Juta T., Arisawa K. Relationship of dietary factors and habits with sleep-wake regularity. Asia Pac. J. Clin. Nutr. 2013;22:457–465. doi: 10.6133/apjcn.2013.22.3.01. [DOI] [PubMed] [Google Scholar]
- 147.Camandola S., Mattson M.P. Brain metabolism in health, aging, and neurodegeneration. EMBO J. 2017;36:1474–1492. doi: 10.15252/embj.201695810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Mattson M.P., Longo V.D., Harvie M. Impact of intermittent fasting on health and disease processes. Ageing Res. Rev. 2017;39:46–58. doi: 10.1016/j.arr.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.