Abstract
Background
By 2030, the global population of people older than 60 years is expected to be higher than the number of children under 10 years, resulting in major health and social care system implications worldwide. Without a supportive environment, whether social or built, diminished functional ability may arise in older people. Functional ability comprises an individual's intrinsic capacity and people's interaction with their environment enabling them to be and do what they value.
Objectives
This evidence and gap map aims to identify primary studies and systematic reviews of health and social support services as well as assistive devices designed to support functional ability among older adults living at home or in other places of residence.
Search Methods
We systematically searched from inception to August 2018 in: MEDLINE, EMBASE, Cochrane Database of Systematic Reviews, CENTRAL, CINAHL, PsycINFO, AgeLine, Campbell Library, ASSIA, Social Science Citation Index and Social Policy & Practice. We conducted a focused search for grey literature and protocols of studies (e.g., ProQuest Theses and Dissertation Global, conference abstract databases, Help Age, PROSPERO, Cochrane and Campbell libraries and ClinicalTrials.gov).
Selection Criteria
Screening and data extraction were performed independently in duplicate according to our intervention and outcome framework. We included completed and on‐going systematic reviews and randomized controlled trials of effectiveness on health and social support services provided at home, assistive products and technology for personal indoor and outdoor mobility and transportation as well as design, construction and building products and technology of buildings for private use such as wheelchairs, and ramps.
Data Collection and Analysis
We coded interventions and outcomes, and the number of studies that assessed health inequities across equity factors. We mapped outcomes based on the International Classification of Function, Disability and Health (ICF) adapted categories: intrinsic capacities (body function and structures) and functional abilities (activities). We assessed methodological quality of systematic reviews using the AMSTAR II checklist.
Main Results
After de‐duplication, 10,783 records were screened. The map includes 548 studies (120 systematic reviews and 428 randomized controlled trials). Interventions and outcomes were classified using domains from the International Classification of Function, Disability and Health (ICF) framework. Most systematic reviews (n = 71, 59%) were rated low or critically low for methodological quality.
The most common interventions were home‐based rehabilitation for older adults (n = 276) and home‐based health services for disease prevention (n = 233), mostly delivered by visiting healthcare professionals (n = 474). There was a relative paucity of studies on personal mobility, building adaptations, family support, personal support and befriending or friendly visits. The most measured intrinsic capacity domains were mental function (n = 269) and neuromusculoskeletal function (n = 164). The most measured outcomes for functional ability were basic needs (n = 277) and mobility (n = 160). There were few studies which evaluated outcome domains of social participation, financial security, ability to maintain relationships and communication.
There was a lack of studies in low‐ and middle‐income countries (LMICs) and a gap in the assessment of health equity issues.
Authors' Conclusions
There is substantial evidence for interventions to promote functional ability in older adults at home including mostly home‐based rehabilitation for older adults and home‐based health services for disease prevention. Remotely delivered home‐based services are of greater importance to policy‐makers and practitioners in the context of the COVID‐19 pandemic. This map of studies published prior to the pandemic provides an initial resource to identify relevant home‐based services which may be of interest for policy‐makers and practitioners, such as home‐based rehabilitation and social support, although these interventions would likely require further adaptation for online delivery during the COVID‐19 pandemic. There is a need to strengthen assessment of social support and mobility interventions and outcomes related to making decisions, building relationships, financial security, and communication in future studies. More studies are needed to assess LMIC contexts and health equity issues.
Abbreviations
- EGM
evidence and gap map
- ICF framework
International Classification of Function, Disability and Health framework
- LGBTQ2+
lesbian, gay, bisexual, transgender, queer (or sometimes questioning), and two‐spirited
- LMIC
low‐ and middle‐income countries
- PICO
population, intervention, comparison, outcome
- RCT
randomized control trials
- SR
systematic review
- WHO
World Health Organization
1. PLAIN LANGUAGE SUMMARY
[The evidence for health, social care and technological interventions to improve functional ability of older adults are unevenly distributed across intervention areas]
The evidence for health, social care and mobility interventions to improve functional ability of older adults includes mostly home‐based rehabilitation and health services delivered by visiting healthcare professionals, and is of low or critically low quality.
1.1. What is this evidence and gap map (EGM) about?
By 2030, the global population of people older than 60 years is expected to be higher than the number of children under 10 years, resulting in major health and social care system implications worldwide. Without a supportive environment, whether social or built, diminished functional ability may arise in older people.
Functional ability comprises an individual's intrinsic capacity and people's interaction with their environment, enabling them to be and do what they value. This map assesses the evidence on home‐based health and social care as well as mobility interventions to improve functional ability of older adults living at home.
What is the aim of this evidence and gap map (EGM)?
The aim of this EGM is to identify primary studies and systematic reviews of health and social support services as well as assistive devices designed to support functional ability among older adults living at home or in other places of residence.
1.2. What studies are included?
The EGM includes randomized controlled studies and systematic reviews that assess the effect of interventions to improve functional ability of older adults living at home or in other places of residence. The interventions were classified as home‐based health, social care, and mobility interventions. Impact on body function and structures as well as activities were considered as outcomes.
There are 548 included studies (120 systematic reviews and 428 randomized controlled trials) in the map.
1.3. What is the distribution of evidence?
The most common interventions were home‐based rehabilitation for older adults (n = 276) and home‐based health services for disease prevention (n = 233), mostly delivered by visiting healthcare professionals (n = 474).
There was a relative paucity of studies on personal mobility, building adaptations, family support, personal support and befriending or friendly visits.
The most measured intrinsic capacity domains were mental function (n = 269) and neuromusculoskeletal function (n = 164). The most measured outcomes for functional ability were basic needs (n = 277) and mobility (n = 160). There were few studies which evaluated outcome domains of social participation, financial security, ability to maintain relationships and communication.
There was a lack of studies in low‐ and middle‐income countries (LMICs) and a gap in the assessment of health equity issues.
1.4. What do the findings of the map mean?
There is substantial evidence for interventions to promote functional ability in older adults at home, including mostly home‐based rehabilitation for older adults and home‐based health services for disease prevention. Remotely delivered home‐based services are of greater importance to policy‐makers and practitioners in the context of the COVID‐19 pandemic.
This map of studies published prior to the pandemic provides an initial resource to identify relevant home‐based services which may be of interest for policymakers and practitioners, such as home‐based rehabilitation and social support, although these interventions would likely require further adaptation for online delivery during the COVID‐19 pandemic.
There is need to strengthen assessment of social support and mobility interventions and outcomes related to making decisions, building relationships, financial security and communication in future studies.
More studies are needed to assess LMIC contexts and health equity issues.
1.5. How up‐to‐date is this EGM?
The authors searched for studies up to August 2018.
2. BACKGROUND
2.1. Introduction
2.1.1. The problem, condition or issue
There is an increasing proportion of older adults in the global population, with UN population projections predicting that before 2020, people aged >65 years will outnumber children aged <10 years for the first time in history (UNDESA, 2017). LMICs such as China and India are expected to experience a rapid rise in population ageing, compared to Western Europe (UNDESA, 2017). Currently, over two‐thirds of people over 65 years of age are living with multimorbidities (Banerjee, 2015). When combined with parallel increases in disparities to health care and broader determinants of health (Sadana et al., 2016), there are major implications for health and social care systems (Beard et al., 2016; Chatterji et al., 2015; Prince et al., 2015). While many nations are becoming wealthy with the influx of global socioeconomic developments, many countries, especially LMICs, have experienced increasing health and social disparities, especially among older adults (World Health Organization [WHO], 2015). Older adults with the greatest health needs are also often those with the fewest resources to support them (Beard et al., 2016). For example, older adults in LMICs have poor access to assistive technologies and medical devices, as a result of a confluence of factors that affect the availability and accessibility of these products in local markets, including affordability and appropriateness. These factors can influence their integration into health and social systems (Garçon et al., 2016; Marasinghe et al., 2015). Furthermore, the privatization of health and social services becomes a barrier to quality of care if costs impact access to appropriate and timely care for older adults.
Functional ability is complex and comprises an individual's intrinsic capacity and people's interaction with their environment enabling them to be and do what they value (Cesari et al., 2018; WHO, 2015). The WHO considers intrinsic capacity to include the physical and mental capacities of a person. The environment defined by the WHO, includes all factors in the extrinsic world that form the context of an individual's life. For example, the home, community and society are included alongside the built environment, interpersonal relationships, attitudes, values, health and social policies, and the systems that support individuals and services (WHO, 2015).The Priority Assistive Products List of essential assistive devices includes wheelchairs, pill organizers, hearing aids, and other essential items for many older people and people with disabilities to be able to live a healthy and dignified life and mitigate declines in intrinsic capacity (WHO, 2016b).
The accumulation of exposures and environmental influences throughout life can influence the development of different risk factors that lead to chronic diseases, injuries, or other age‐related issues that contribute to declines in intrinsic capacities. Without a supportive environment, whether social or built, this will result in diminished functional ability. The gradual decline in intrinsic capacities as some people age can require increased health and social care services from informal (i.e., family or friends) and formal caregivers (i.e., healthcare professionals). Increased care needs lead to increased burden on families, stress for older adults, and costs to society. For this reason, efforts to deliver cost efficient, effective interventions that optimize functional ability at any level of intrinsic capacity, is critical for older adults. Health and social care interventions (including assistive health technologies), and related systems, services and policies may include technological tools and devices and provision of health and social supports in the home.
While it is important to offer home‐based supports that promote functional ability, we need to be mindful that existing health inequities may be worsened (Sadana et al., 2016). For example, if health and social services are provided privately and not covered by the health system or health insurance, all individuals will not have the same opportunities to achieve optimal health. Age‐based bias is seen in research on conditions that affect older adults such as stroke and osteoarthritis, with the median age of participants in research over 10 years younger than the typical patient (Gaynor et al., 2014; Liberopoulos et al., 2009).
2.2. Why it is important to develop the EGM
Over 85% of research investment is wasted (Chalmers & Glasziou, 2009), some of which could be avoided by prioritizing research directions and including rigorous evaluation of existing evidence using systematic reviews prior to funding or carrying out new research (Chalmers et al., 2014). An EGM is a decision‐making and research‐prioritization tool that highlights gaps in research to inform strategic health and social policy, program, and research priorities (Snilstveit et al., 2013). EGMs can be used to avoid needless duplication, and can also be used to identify where sufficient, high quality evidence from systematic reviews and randomized trials are available as a basis for decisions or where sufficient studies are available for knowledge synthesis (Snilstveit et al., 2016).
This EGM is important to inform policy and research prioritization. It is aligned with the WHO Strategy and Action Plan on Ageing and Health 2016–2020. At the 69th World Health Assembly in May 2016, the WHO launched and received endorsement from all 193 member states for the WHO Strategy and Action Plan on Ageing and Health 2016–2020. This plan outlined five strategic objectives: (1) commitment to action on healthy ageing in every country, (2) developing age‐friendly environments; (3) aligning health systems to the needs of older populations; (4) developing sustainable and equitable systems for providing long‐term care; (5) improving measurement, monitoring, and research on healthy active ageing. The WHO aims to meet these by implementing evidence‐based actions to maximize functional ability of every individual (WHO, 2016). In this way the process of “optimizing opportunities for health, participation and security will enhance the quality of life as people age” (WHO, 2015). This EGM is relevant to the first objective—a commitment to action on healthy ageing in every country. Furthermore, our objectives align with the United Nations Sustainable Development Goals and the objectives of the UN High Level meeting on preventing and controlling noncommunicable diseases (United Nations, 2019; WHO, 2018).
We took a health systems perspective to extend the focus from health care to include social care and technological interventions. The evidence is presented in terms of functional ability. We also considered determinants of health inequity. This EGM considers the multifaceted and complex nature of functional ability and the various mechanisms (e.g., services, products and individuals) involved in supporting functional ability among ageing adults.
Currently, no EGMs exist that identify and assess the available evidence on health, social care and technological interventions to support functional ability among older adults living at home.
There are three primary audiences for this EGM. First, we expect researchers (e.g., universities, government, etc.) will use the results to inform further investigations on these topics, including new empirical research and evidence synthesis products. The second main anticipated audience is decision‐makers for whom intrinsic capacity, functional ability and process outcomes are already or potentially of interest. This includes relevant ministries and programs within governments and/or donor agencies, as well as nongovernmental organizations and other advocacy and implementing organization staff. From a policy perspective, it is especially useful to know what kinds of interventions might most effectively affect intrinsic capacity, functional ability, and process outcomes. The third main anticipated audience is health and social care providers who can use the map to identify quality assessed synthesized evidence of health, social care, and technological interventions for their practice.
3. OBJECTIVES
The objectives of this Campbell EGM are to:
Identify and assess the available evidence on health, social care and technological interventions to improve functional ability among older adults living at home
Identify available systematic reviews and randomized trials
Identify areas where systematic reviews are needed
Identify gaps in evidence where further primary research is needed
Assess equity considerations in available systematic reviews and randomized trials
Assess gaps and evidence related to health equity
4. METHODS
4.1. EGM: Definition and purpose
This EGM is based on a published protocol (Welch et al., 2019). We adapted evidence gap map methods from various key papers (Bragge et al., 2011; Lum et al., 2011; Snilstveit et al., 2013, 2016) and followed a five stage process:
Define a framework
Identify the available evidence
Appraise the quality of the evidence
Extract, code and summarize the data that relate to the objectives
Visualize and present the findings in a user‐friendly manner
This five stage process aligns with current Campbell Collaboration guidance (White et al., 2020). We used the Campbell Collaboration mapping tool developed by Digital Solution Foundary and EPPI‐Centre (Digital Solution Foundary and EPPI‐Centre, 2020) to display identified studies using the framework described below.
4.2. Framework development and scope
The framework was developed following a meeting with methodologists, practitioners, decision makers and consumers at the Cochrane Colloquium during the 2017 Global Evidence Summit. The colloquium participants suggested using the International Classification of Functioning, Disability and Health (ICF) framework (Sadana & Posarac, 2018; WHO 2001) to define the interventions and outcomes for this EGM. We further defined the scope of the framework in consultation with our research team which includes input from the public (A. L.), practitioners (L. S., P. T., K. P., J. B., E. T., P. W. and M. C.), information scientist (M. R.), policy‐makers (R. S. and H. S.) and researchers (V. W., S. M., J. T. C., T. H., M. C., E. K., B. S., A. S. and W. Z.). The ICF is a comprehensive framework used by the WHO to measure health and disability at both individual and population levels, as well as to operationalize the measurement of intrinsic capacities, functional ability and enabling environments (Sadana & Posarac, 2018).
As such, the EGM framework informed the inclusion and exclusion criteria. We followed the standard EGM framework as a matrix where the rows show intervention domains and the columns show outcome domains. Key dimensions of the framework and their sub‐categories are detailed in the subsequent sections.
We further limited the scope to interventions that were provided in the home of older adults. Maintaining autonomy and independence, especially being able to make their own choices and decisions, are important for older adults in all settings (Hillcoat‐Nalletamby, 2014; Plath, 2009; Welford et al., 2012). We defined the concept of home broadly, as the place of dwelling in which older adults seek to maintain their autonomy. This definition included any nonacute care places of residence such as housing units (detached and semi‐detached houses or apartments), long‐term care facilities (including hospices, and nursing homes), independent living or assisted living facilities.
4.3. Stakeholder engagement
We created an Advisory Group comprised of methodologists, physicians (and other healthcare professionals), policy organizations, consumers and researchers with expertise in assistive health technology, healthy ageing, long‐term care, rehabilitation, disability, memory and cognitive impairment. We held an exploratory meeting to invite feedback on the development of our EGM framework at the Global Evidence Summit in Cape Town, September 2017. The participants included family practitioners, geriatricians, social workers and methodologists. We also held a seminar at the Bruyère Research Institute Grand Rounds (26 October 2017) with family practitioner researchers, where participants provided feedback on the intervention‐outcome framework. Our decision to focus on the selected intervention categories was also informed by engaging with our public representative (A. L.). Our central team (V. W., T. H., S. M., P. B. and C. M.) met at least once a month to discuss the direction and scope of the EGM. Preliminary findings were presented at the peer review meeting of WHO Consortium on Metrics and Evidence for Healthy Ageing, 10–11 October 2019. Feedback from the reviewers was included in the final document.
4.4. Conceptual framework
Figure 1 below demonstrates the conceptual framework through which the inputs lead to the intended outcomes. A person's intrinsic capacity is dependent on their health characteristics (e.g., body functions, health related behaviors, disease or injuries), genetic inheritance, and personal characteristics (e.g., sex/gender or ethnicity). However, the extent to which an individual accomplishes activities that they value, functional ability, is also dependent on their interactions with the environment. Enabling environments may include services, systems and policies, and products and technology which, when implemented within a home context, can influence outcomes such as improved neuromusculoskeletal functioning, through the use of an external aid, assistance by another person or improvement in the built environment. Supportive environments can strongly influence functional ability. We also included health inequalities as an outcome of interest because we are aware that certain characteristics may stratify or impact health opportunities and outcome, such as socioeconomic status or place of residence.
Figure 1.
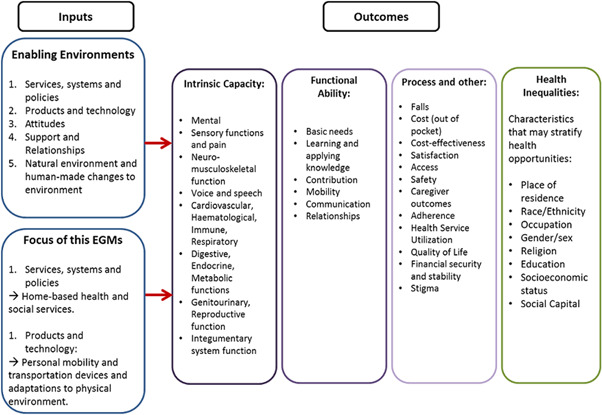
Conceptual framework adapted from the WHO International Classification of Functioning, Disability and Health (ICF)
4.5. Dimensions
4.5.1. Types of study design
We included completed and on‐going systematic reviews and randomized controlled trials of effectiveness. We defined a systematic review according to the PRISMA definition (Moher et al., 2015), where the article explicitly states the methods used to identify studies (i.e., a search strategy), strategies for study selection (e.g., eligibility criteria and selection process) and explicitly detail methods of synthesis. We included studies published in grey literature such as reports, dissertations and conference abstracts.
We excluded systematic reviews of predictive factors, prognostic and diagnostic studies, and studies that primarily analyzed implementation, barriers and facilitators to effectiveness (Snilstveit et al., 2013). Literature reviews that did not describe methods used for search, data collection, and/or synthesis were excluded. We also excluded theoretical or modeling studies, editorials and commentaries. We did not include qualitative research.
4.5.2. Types of intervention/problem
We contextualized interventions according to the International Classification of Functioning, Disability and Health (ICF) categorization of environmental factors. This was further divided into:
-
1.
Health and social services, systems and policies: While we recognize that systems and policies can have an impact on the individual, we specifically focused on sections e5750 and e5800 from the ICF, which includes health and social support services provided at home such as homemaking, personal care, healthcare professional home visits, or long‐term care.
-
2.
Products and technology related to mobility: The ICF provides a very comprehensive list of eligible interventions. We used sections e1201 and e155 that focused on assistive products and technology for personal indoor and outdoor mobility and transportation as well as design, construction and building products and technology of buildings for private use. This includes products such as wheelchairs, walking devices, transfer devices and ramps.
We decided to limit the scope of the ICF framework due to feasibility. Specifically, we excluded studies of pharmacological interventions, therapies, telemedicine or telecare, educational programs and any hospital‐based programs. We also excluded any studies that examine caregiver support services exclusively without evaluating outcomes related to older adults. A comprehensive list of interventions in each category may be found in Table 1.
Table 1.
Interventions framework (based on the ICF)
| Intervention category | Focus | Definition | Specific examples |
|---|---|---|---|
| Services, systems and policies | e575 General social support services, systems and policies |
Services, systems and policies aimed at providing support to those requiring assistance in areas such as shopping, housework, transport, child care, self‐care and care of others, in order to function more fully in society. Exclusions: social security services, systems and policies (e570); personal care providers and personal assistants (e340); health services, systems and policies (e580) |
e5750 General social support services: Services and programs aimed at providing social support to people who, because of age, poverty, unemployment, health condition or disability, require public assistance in the areas of shopping, housework, transport, self‐care and care of others, in order to function more fully in society |
| e580 Health services, systems and policies | Services, systems and policies for preventing and treating health problems, providing medical rehabilitation and promoting a healthy lifestyle. Exclusions: general social support services, systems and policies | e5800 Health services: Services and programmes at a local, community, regional, state or national level, aimed at delivering interventions to individuals for their physical, psychological and social well‐being, such as health promotion and disease prevention services, primary care services, acute care, rehabilitation and long‐term care services; services that are publicly or privately funded, delivered on a short‐term, long‐term, periodic or one‐time basis, in a variety of service settings such as community, home‐based, school and work settings, general hospitals, specialty hospitals, clinics, and residential and nonresidential | |
| Products and technology | e120 Products and technology for personal indoor and outdoor mobility and transportation |
Equipment, products and technologies used by people in activities of moving inside and outside buildings, including those adapted or specially designed, located in, on or near the person using them. Inclusions: general and assistive products and technology for personal indoor and outdoor mobility and transportation |
e1201 Assistive products and technology for personal indoor and outdoor mobility and transportation. Adapted or specially designed equipment, products and technologies that assist people to move inside and outside buildings, such as walking devices (such as canes or crutches), special cars and vans, adaptations to vehicles, wheelchairs, scooters and transfer devices |
| e155 Design, construction and building products and technology of buildings for private use |
Products and technology that constitute an individual's indoor and outdoor human‐made environment that is planned, designed and constructed for private use (e.g., home, dwelling), including those adapted or specially designed. Inclusions: entry and exits, facilities and routing |
e1550 Design, construction and building products and technology for entering and exiting of buildings for private use. Products and technology of entry and exit from the human‐made environment that is planned, designed and constructed for private use, such as entries and exits to private homes, portable and stationary ramps, power‐assisted doors, lever door handles and level door thresholds |
4.5.3. Types of population (as applicable)
This EGM focused on adults over the age of 60 years, using the United Nations cut off for older adults (United Nations, 2015). Studies and reviews were included if at least 50% of the sample population was greater than 60 years old.
4.5.4. Types of outcome measures (as applicable)
We mapped the evidence on outcomes that fell into one of the following ICF (WHO, 2001) adapted categories: intrinsic capacities (body function and structures) and functional abilities (activities). We also included process and other outcomes that may impact a particular outcome. We considered health inequities by examining environmental and personal attributes that may stratify health opportunities and outcomes, using the PROGRESS framework (O'Neill et al., 2014). PROGRESS is an acronym which stands for: place of residence, race/ethnicity, occupation, gender, religion, education, socioeconomic status and social capital. Our outcomes framework is provided in Table 2.
Table 2.
Outcomes framework
| Outcome category | Measure/construct |
|---|---|
| Intrinsic capacity |
|
| Functional ability |
|
| Process and other |
|
| Health inequalities |
|
The intrinsic capacity outcome category consisted of mental (e.g., depression, sleep, vitality); sensory functions and pain (e.g., vision, hearing); neuromusculoskeletal function (e.g., gait, balance); voice and speech (e.g., articulation); cardiovascular, haematological, immune, respiratory system function (e.g., blood pressure, respiration); digestive, endocrine, metabolic functions (e.g., thyroid, glucose); genitourinary and reproductive function (e.g., bladder control); and integumentary system function (e.g., skin, nails).
The functional ability outcome category consisted of the following constructs: basic needs (e.g., self‐care, acquisition of goods and services); learning and applying knowledge; contribution (e.g., community life, employment); mobility (e.g., walking); relationships (e.g., interpersonal interactions); and communication (e.g., language).
Process and other outcomes included cost (out of pocket), cost‐effectiveness, falls, satisfaction of older adult, safety, caregiver outcomes, adherence, health service utilization, quality of life, financial security, access and stigma. Access is a multifaceted concept and can be understood as the opportunity or ease with which consumers or communities are able to use appropriate services in proportion to their needs (Daniels, 1982; Whitehead, 1992). As such, the concept of access included: acceptability, approachability, availability and accommodation, affordability and appropriateness (Levesque et al., 2013).
4.5.5. Other eligibility criteria
Types of settings
We included interventions which were provided in the home setting for older adults. We defined home as an individual's place of residence that can include housing units (houses/apartments), long‐term care (including nursing homes, and hospices), independent living (e.g., retirement residences), and assisted living facilities. We did not include any acute or sub‐acute care and convalescent care settings (e.g., geriatric rehabilitation in subacute care). Studies of mixed settings were included if the intervention took place in the home setting at least 50% of the time. We coded the settings so that the evidence can be filtered according to setting.
4.6. Search methods and sources
We developed and piloted a search strategy (with a selection of studies that met our inclusion criteria) with the guidance of an information scientist (M. R.). This search comprised medical and health databases (MEDLINE (via OvidSp), EMBASE (via OvidSp), Cochrane Database of Systematic Reviews, CENTRAL, CINAHL (Via EBSCOhost), APA PsycINFO (via OvidSp), AgeLine (via EBSCOhost) and databases relevant to social care and social policy (Campbell Library, ASSIA (via ProQuest), Social Science Citation Index (via Web of Science) and Social Policy & Practice (via OvidSp). The database searches were run between 26 July 2018 and 1 August 2018. No limits for language or date were used. See Table 3 for full search strategy as used in MEDLINE, and adapted for the other databases (see Appendix 1, 2, 3, 4, 5, 6, 7, 8).
Table 3.
Search strategy for MEDLINE
| Category | Terms |
|---|---|
| Population |
1 exp Aged/pc, px, rh [Prevention & Control, Psychology, Rehabilitation] (8053) 2 "Aged, 80 and over"/(806254) 3 Frail Elderly/(9588) 4 elderly.ti,ab. (219354) 5 older people.ti,ab. (23442) 6 older adult*.ti,ab. (61366) 7 older men.ti,ab. (7857) 8 older women.ti,ab. (12791) 9 old* age*.ti,ab. (65408) 10 pensioners.ti,ab. (793) 11 retirement.ti,ab. (11779) 12 "end of life".ti,ab. (18653) 13 (Resident* and (old* or home* or retirement or nursing)).ti,ab. (38765) 14 geriatric*.ti,ab. (41516) 15 (veteran* and (old* or home* or retire*)).ti,ab. (5047) 16 or/1‐15 (1121318) |
| Intervention |
17 exp Self‐Help Devices/(10537) 18 exp Orthopedic Equipment/(92047) 19 assistive devices.ti,ab. (1494) 20 assistive equipment.ti,ab. (39) 21 mobility equipment.ti,ab. (20) 22 mobility device*.ti,ab. (311) 23 mobility aid*.ti,ab. (276) 24 motility.ti,ab. (85101) 25 (walking adj2 (device* or aid* or equipment)).ti,ab. (1248) 26 cane*.ti,ab. (5734) 27 crutches.ti,ab. (1155) 28 walking stick*.ti,ab. (202) 29 (Adapt* adj3 (cars or transport or vehicles)).ti,ab. (506) 30 (Adapt* adj3 (home* or house*)).ti,ab. (1545) 31 Wheelchair*.ti,ab. (6462) 32 exp Bathroom Equipment/(10) 33 scooter*.ti,ab. (368) 34 transfer device*.ti,ab. (231) 35 (communication adj (aid* or device*)).ti,ab. (858) 36 exp Optical devices/(88276) 37 Hearing aids/(7984) 38 eyeglasses.ti,ab. (683) 39 glasses.ti,ab. (10746) 40 spectacles.ti,ab. (2316) 41 hearing device*.ti,ab. (512) 42 hearing aid*.ti,ab. (8346) 43 vision aid*.ti,ab. (364) 44 ((Adapt* or adjust*) adj3 (door* or entry or exit)).ti,ab. (239) 45 Stair lift*.ti,ab. (2) 46 stair climbing.ti,ab. (1444) 47 stairs.ti,ab. (2902) 48 stair rails.ti,ab. (2) 49 shallow steps.ti,ab. (0) 50 (ramp or ramps).ti,ab. (7094) 51 Home Care Services/(31353) 52 home care service*.ti,ab. (1605) 53 home support service*.ti,ab. (59) 54 home visit*.ti,ab. (7662) 55 community services.ti,ab. (2375) 56 shopping.ti,ab. (3322) 57 house help.ti,ab. (1) 58 home help.ti,ab. (411) 59 (food adj (preparation or assistance or help or service or delivery)).ti,ab. (3932) 60 (meal* adj3 (provision or assistance or help or service* or preparation or delivery)).ti,ab. (1137) 61 homemaking.ti,ab. (109) 62 housekeeping.ti,ab. (8477) 63 ((household or ktichen or routine) adj (jobs or tasks or chores)).ti,ab. (888) 64 bathing.ti,ab. (9571) 65 grooming.ti,ab. (5015) 66 personal hygiene.ti,ab. (1847) 67 toileting.ti,ab. (857) 68 foot care.ti,ab. (1270) 69 (medication adj2 reminders).ti,ab. (147) 70 (kitchen or bathroom or bedroom).ti,ab. (5694) 71 or/17‐70 (400411) |
| Outcomes |
72 exp "Activities of Daily Living"/(63476) 73 Human Activities/(2170) 74 Automobile Driving/(17307) 75 Leisure Activities/(7897) 76 "activities of daily living".ti,ab. (22139) 77 "quality of life".ti,ab. (229433) 78 "Quality of Life"/(164112) 79 independence.ti,ab. (36023)80 wellbeing.ti,ab. (11362) 81 social life.ti,ab. (3877) 82 social participation.ti,ab. (2177) 83 happiness.ti,ab. (5642) 84 happier.ti,ab. (734) 85 mental health.ti,ab. (116393) 86 functional ability.ti,ab. (4311)87 depression.ti,ab. (289365) 88 cognitive.ti,ab. (296200) 89 sensory function*.ti,ab. (3884) 90 pain.ti,ab. (543562) 91 distress.ti,ab. (97018) 92 vitality.ti,ab. (10533) 93 energy.ti,ab. (544017) 94 fatigue.ti,ab. (80717) 95 tiredness.ti,ab. (3430) 96 self care.ti,ab. (14789) 97 self efficacy.ti,ab. (21966) 98 mobility.ti,ab. (123516)99 community life.ti,ab. (457) 100 security.ti,ab. (38430) 101 relationships.ti,ab. (322577) 102 satisfaction.ti,ab. (113208) 103 adherence.ti,ab. (98155) 104 reablement.ti,ab. (49) 105 institutionali?ation.ti,ab. (4370)106 or/72‐105 (2682926) |
| Study design |
107 systematic*.ti,ab. (374866) 108 (meta‐analysis or metaanalysis).ti,ab. (112568) 109 (review* and (literature or studies or trials)).ab. (693115) 110 review.ti. (393065) 111 (evidence adj2 synthesi*).ti,ab. (5932) 112 overview.ti,ab. (139107) 113 pubmed.ab. (82182) 114 medline.ab. (94705) 115 or/107‐114 (1336239) 116 randomized controlled trial.pt. (464926) 117 controlled clinical trial.pt. (92516) 118 randomized.ti,ab. (448898) 119 randomly.ab. (294026) 120 trial.ti,ab. (509010) 121 groups.ab. (1815046)122 usual care.ab. (13020) 123 or/116‐122 (2634734) 124 115 or 123 (3780045) 125 16 and 71 and 106 and 124 (3987) |
We searched for relevant trials and systematic reviews in the grey literature via ProQuest Theses and Dissertation Global, and via Conference Proceedings Citation Index. We also searched for relevant unpublished studies via relevant international organizations (e.g., Help Age, WHO, and Institute for Research on Public Policy).
We searched for ongoing systematic reviews in PROSPERO and the Cochrane and Campbell libraries as well as on the open science framework (https://osf.io/). We searched for ongoing randomized trials in ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform.
4.7. Analysis and presentation
4.7.1. Filters for presentation
Our EGM is presented as a matrix of interventions (rows) and outcomes (columns) and reports the evidence base that met our inclusion criteria.
Users of the interactive EGM can additionally filter studies by the following filters:
Publication status: completed studies and on‐going studies (i.e., study protocols).
Age groups: 65 years and under, 65 years and above, over 75 years, and over 85 years.
Health conditions/status: communicable disease (e.g., flu, HIV/AIDS), noncommunicable disease (e.g., dementias, diabetes, cancer, depression), injury (e.g., fractures, falls), discharged from hospital, end‐of‐life, physical frailty (e.g., at risk of functional decline), social frailty (e.g., social isolation), care dependent (e.g., when older adult is no longer able to undertake tasks necessary for daily life without the assistance of others (WHO, 2015), and dementia.
WHO regions: South‐east Asia, Western Pacific, Europe, Africa, the Americas, Eastern Mediterranean.
World Bank Classifications: high‐income economies, upper‐middle income economies, lower‐middle income economies, low‐income economies.
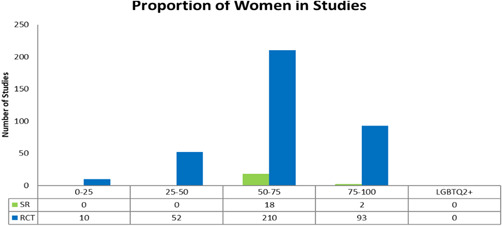
Proportion of women included in study: 0%–25%, 25%–50%, 50%–75% and 75%–100%.
4.7.2. Dependency
We linked all publications of the same study to count as one study (this included protocols if published and any secondary analyses). It is important to note that systematic reviews are likely to include the RCTs included in the map and there may be more than one systematic review which includes the same RCT(s). All relevant randomized trials were included regardless of whether they were included in a systematic review. We elaborate further in the discussion on how the interactive map should be interpreted.
4.8. Data collection and analysis
4.8.1. Screening and study selection
Two reviewers independently screened the titles and abstracts of all retrieved articles. We screened titles and abstracts by intervention, study design, setting and population. We did not use outcomes as an inclusion criterion. Full‐texts of potentially eligible studies were screened independently in duplicate and any conflicts were resolved through discussion or by a third reviewer (V. W.). We did not contact authors of studies or reviews for missing information. Studies published in languages other than English or French, were translated using Google Translate and/or a native speaker, recruited through professional networks. This was done at the full‐text screening and coding stages.
4.8.2. Data extraction and management
Once the eligible studies were identified, we tested and piloted the data extraction form on a sample of studies, generated a draft map, and met with our advisory board to make any modifications. We also invited feedback from our larger team. Two reviewers independently extracted data on published and ongoing systematic reviews and randomized trials related to the population, intervention, comparison, outcomes, setting and other categories we used as filters. We also coded studies to indicate whether the population was socially disadvantaged across PROGRESS (O'Neill et al., 2014) and identified whether any analyses were conducted across sex/gender or any other PROGRESS characteristics. Our complete list of coding categories for data extraction is found in Appendix 9. We coded systematic reviews using the research question or eligibility criteria. We did not go back to included primary studies within a review for more details. Differences in extraction were resolved by discussion.
4.8.3. Tools for assessing risk of bias/study quality of included reviews
Since systematic reviews are often used for decision making, we appraised the methodological quality of systematic reviews using the AMSTAR‐2 (Assessing the Methodological Quality of Systematic Reviews) checklist (Shea et al., 2017) in duplicate for 10% of eligible studies. κ statistics were also used to check agreement for each item. If agreement was over 80%, we proceeded with single data extraction with verification by a second reviewer for the remainder of studies.
The quality of randomized trials is not usually assessed in EGMs since the purpose is to identify the randomized trials available, and not to make decisions based on single trials. As such, we did not assess quality of randomized trials (Snilstveit et al., 2017).
4.8.4. Methods for mapping
We used the EPPI‐Reviewer 4 software (Thomas et al., 2010) for screening and coding, and the EPPI‐Mapper (Digital Solution Foundary and EPPI‐Centre, 2020) for generating the map. EPPI‐Reviewer and EPPI‐Mapper are developed by the EPPI‐Centre at the Social Science Research Unit of the UCL Institute of Education, University of London, UK (http://eppi.ioe.ac.uk/cms/Default.aspx?alias=eppi.ioe.ac.uk/cms/er4).
5. RESULTS
5.1. Description of studies
5.1.1. Results of the search
Our search retrieved 16,083 records from database searching with 4 additional records identified through other sources. After deduplication, 10,783 articles were screened in duplicate by title and abstract. From this, full texts of 1194 articles were screened in duplicate for eligibility. When full texts were not available, we used an interlibrary loan service. We included 548 studies in this map, of which 120 were systematic reviews (22%) and 428 were randomized controlled trials (78%). There were 502 completed studies including 117 completed systematic reviews (23%) and 385 completed randomized controlled trials (77%). Among the 46 on‐going studies, three were systematic reviews (7%) and 43 were randomized controlled trials (93%). See PRISMA flow chart in Figure 2.
Figure 2.
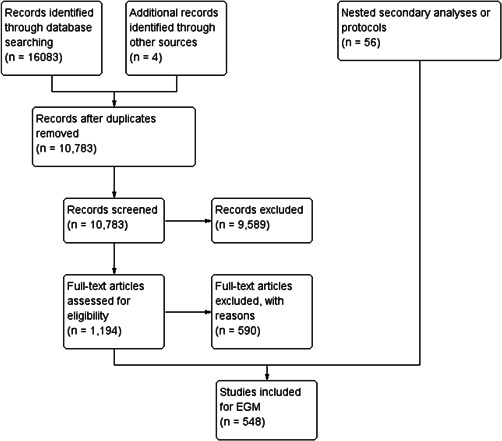
PRISMA flow chart
5.1.2. Excluded studies
The main reasons for exclusion at the full‐text screening stage were due to inappropriate intervention (n = 192), target population (n = 44), study design (n = 213), and setting (n = 141). See Supporting Information material for table of excluded studies and references.
5.2. Synthesis of included studies
Since many of the studies included in this EGM have been coded under multiple output indicators (e.g., more than one intervention category), a single study may appear in multiple cells. See Supporting Information interactive EGM map https://globalageing.cochrane.org/sites/globalageing.cochrane.org/files/public/uploads/ageing_egm_interactive_map_may5_20.html.
5.2.1. Interventions
As described earlier, we focused on four sections of the two broad domains of enabling environments within the ICF framework: health services, social support services, personal indoor and outdoor mobility and transportation, and design, construction and building products and technology. See Figure 3 for distribution of studies across our broad intervention categories.
Figure 3.
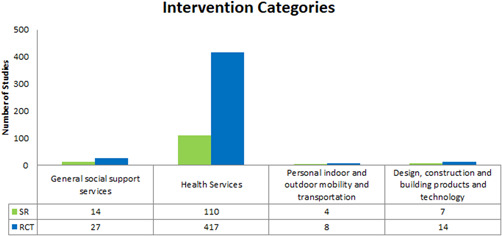
Intervention categories
Evidence, however, is not distributed evenly across the interventions and outcomes. Large clusters of randomized controlled trials and systematic reviews are present in some intervention areas (e.g., health services—rehabilitation services) while other intervention areas have very few studies (e.g., general social support services, systems and policies—transportation).
For visiting healthcare professional interventions these clusters of randomized controlled trials and systematic reviews include mental functions (n = 230, 186 RCTs and 104 SRs), neuro‐musculoskeletal (n = 138, 106 RCTs and 32 SRs), basic needs (n = 241, 190 RCTs and 51 SRs), mobility (n = 128, 115 RCTs and 13 SRs), quality of life (n = 189, 147 RCTs and 42 SRs), and health service utilization (n = 191, 147 RCTs and 44 SRs). For rehabilitation interventions these clusters include mental functions (n = 132, 105 RCTs and 27 SRs), neuro‐musculoskeletal (n = 134, 106 RCTs and 28 SRs), basic needs (n = 149, 111 RCTs and 38 SRs), mobility (n = 123, 111 RCTs and 12 SRs), quality of life (n = 115, 91 RCTs and 24 SRs), and health service utilization (n = 191, 48 RCTs and 143 SRs). For general health services for disease prevention interventions these clusters include mental functions (n = 118, 97 RCTs and 21 SRs), basic needs (n = 119, 97 RCTs and 22 SRs) and quality of life (n = 189, 77 RCTs and 112 SRs), and health service utilization (n = 129, 104 RCTs and 25 SRs).
There are few randomized controlled trials and systematic reviews that assess the following interventions across any outcomes; transportation (n = 2 RCTs), befriending or friendly visits (n = 3 RCTs), home making (n = 8, 7 RCTs and 1 SR), visiting lay service providers (n = 11 RCTs), caregiver support (n = 12, 8 RCTs and 4 SRs), personal mobility and transportation devices (n = 12, 8 RCTs and 4 SRs), adaptations to physical environments (n = 21, 14 RCTS and 7 SRs), personal care (n = 23, 14 RCTs and 9 SRs), long term care services (n = 14, 7 RCTs and 7 SRs), health promotion services (n = 27, 20 RCTs and 7 SRs).
It is important to recognize that these clusters are not suggestive of greater evidence for a (positive or negative) impact of an intervention on outcome indicators. Rather, they suggest that these relations have been investigated with greater frequency, irrespective of the actual impact documented.
5.2.2. Outcomes
Our EGM framework maps thirteen interventions to 26 outcomes; 8 intrinsic capacity, 9 functional ability and 9 process and other. The most frequently measured are intrinsic capacity outcomes related to mental functions (n = 269, 216 RCTs and 53 SRs), neuromusculoskeletal (n = 164, 130 RCTs and 34 SRs), sensory and pain (n = 73, 58 RCTS and 15 SRs) (see Figure 4); functional ability outcomes related to basic needs (n = 277, 216 RCTs and 61 SRs), quality of life (n = 222, 172 RCTs and 50 SRs) and mobility (n = 160, 146 RCTs and 14 SRs) (see Figure 5); and process and other outcomes related to health service utilization (n = 206, 159 RCTs and 47 SRs), falls (n = 106, 81 RCTs and 25 SRs), cost‐effectiveness (n = 97, 74 RCTs and 23 SRs), satisfaction of older adults (n = 86, 56 RCTs and 30 SRs), and caregiver outcomes (n = 71, 50 RCTs and 21 SRs) (see Figure 6).
Figure 4.
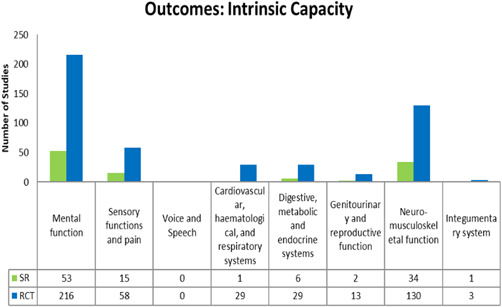
Intrinsic capacity outcomes
Figure 5.
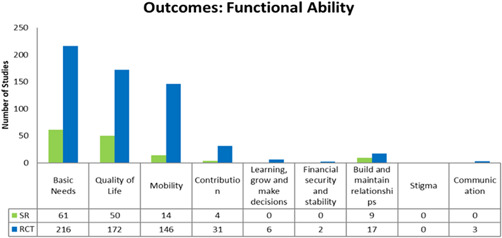
Functional ability outcomes
Figure 6.
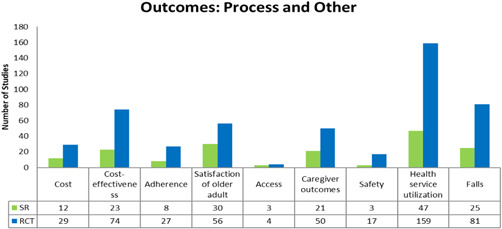
Process and other outcomes
For any intervention type there are no studies that assess voice and speech, and stigma. Furthermore, there are few studies that assess the following outcomes for any intervention type; financial security and stability (n = 2 RCTs), communication (n = 3 RCTs), integumentary system (n = 4, 3 RCTS and 1 SR), learning, grow and make decisions (n = 6 RCTs), access (n = 7, 4 RCTs and 2 SRs), genitourinary and reproductive functions (n = 15, 13 RCTs and 2 SRs), safety (n = 20, 17 RCTs and 3 SRs) (see Figures 4, 5, 6).
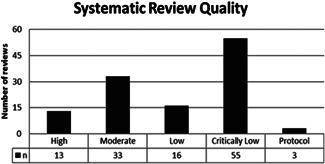
5.3. Risk of bias in included reviews
We assessed the methodological quality of 10% (12) systematic reviews in duplicate and once agreement was reached, we proceeded with single assessment of the rest. In total, 120 systematic reviews were assessed, of which, only 13 (11%) were high quality reviews, while the remaining rated moderate (28%), low (13%) and critically low (46%). We did not assess the methodological quality of the three on‐going systematic reviews (2%) (see Figure 7).
Figure 7.
Methodological quality of systematic reviews
The main reasons for low quality are: (a) not reporting sources of funding for the studies included in the reviews, (b) not providing a list of excluded studies and justification for exclusion, (c) not accounting for risk of bias assessment in primary studies when interpreting or discussing the results, and (d) not using a satisfactory technique to assess risk of bias in individual studies included in the reviews.
5.4. Additional dimensions (if applicable)
5.4.1. Health equity
Gender Inequalities
We assessed gender inequalities by:
Checking the proportion of women included in systematic reviews and randomized controlled trials (completed and on‐going),
We assessed whether the studies analyzed (O'Neill et al., 2014) effects of interventions by sex/gender or other PROGRESS factors.
In 323 randomized controlled trials and 20 systematic reviews, women comprised >50% of the study participants (Figure 8). There were no studies that reported on including individuals from the LGBTQ2+ (lesbian, gay, bisexual, transgender, queer (or sometimes questioning), and two‐spirited) community.
Figure 8.
Proportion of women in studies
Only 11 of the 548 included studies (2%) described the population as being socially disadvantaged across a PROGRESS characteristic: race/ethnicity, culture, language (n = 3 RCTs), socioeconomic status (n = 4, 3 RCTs and 1 SR), and social capital (n = 4, 2RCTs and 2 SRs).
Only one out of 548 included studies assessed effects of interventions across sex/gender and four studies assessed effects across another PROGRESS factor.
Region
Across WHO regions, most of the studies evaluated describe and assess interventions in Europe (n = 272 (192 RCTs and 80 SRs); 49%), followed by the Americas (n = 158 (137 RCTs and 21 SRs); 29%) and Western Pacific (n = 112 (3 RCTs and 19 SRs); 20%) and with 5 or less studies in South‐East Asia, Africa and Eastern Mediterranean (see Figure 9). We also coded studies following the World Bank Classifications by economies. The majority of studies were from high‐income economies (n = 532, 415 RCTS and 117 SRs), with no studies from low‐income economies (see Figure 10). As stated earlier, please note that some studies were coded under more than one category. For example, a single study might have covered Europe and the Americas and will have been counted in both categories.
Figure 9.
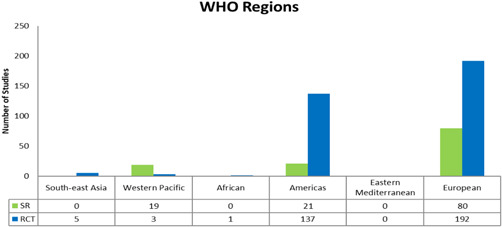
WHO regions
Figure 10.
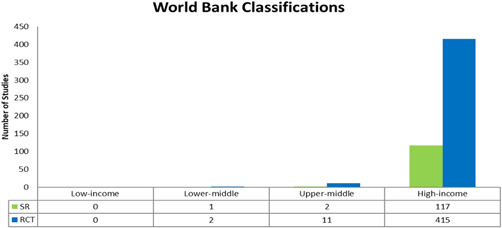
World Bank classifications
Setting
The majority of studies (n = 475, 370 RCTs and 105 SRs) took place in a housing unit (house or apartment) (see Figure 11). A single study may be coded in more than one setting.
Figure 11.
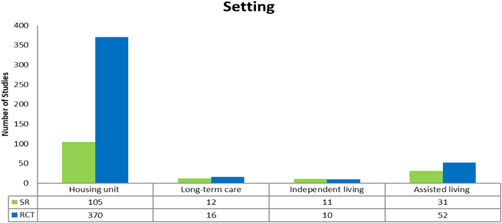
Setting
Health condition/status
We coded studies by health conditions of populations. The majority of studies included people with noncommunicable diseases (n = 248, 189 RCTs and 59 SRs). Very few studies (n = 7, 3 RCTs and 4 SRs) assessed loneliness and social isolation in older adults. We used the author's description of the population to identify studies in this domain. Most studies included populations that were coded under multiple categories (see Figure 12).
Figure 12.
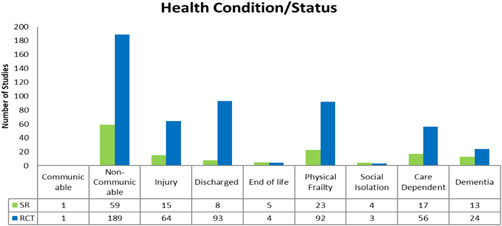
Health condition/status
6. DISCUSSION
6.1. Summary of main results
The distribution of evidence in this EGM of health, social care and technological interventions to improve functional ability of older adults living at home or in other places of residence is not uniform. Home‐based health care has received more attention than social care or mobility support. Furthermore, the most common ICF outcome domains assessed were basic needs, quality of life and mobility, with relatively few studies reporting outcomes on societal contribution, learning, relationships, financial security. There were very few studies in LMICs (only 3%).
6.2. Areas of evidence clusters
The main cluster of evidence in this EGM is where interventions involve visiting healthcare professionals (n = 474); this is compared to a paucity of evidence exploring interventions provided by visiting lay service providers (n = 11). This may be because most studies took place in high‐income countries where there is greater use of home visits by healthcare professionals. However, many LMICs do not have access to home visiting healthcare professionals (Bashour et al., 2008; Ndiok & Ncama, 2019).
The evidence for rehabilitation services is clustered around neuro‐musculoskeletal function (n = 134) and mental health function (n = 131) outcomes. This may be explained in that over 20% of adults aged 60 and over suffer from a mental or neurological disorder (excluding headache disorders) and 6.6% of all disability adjusted life years (DALYs) among people over 60 years is attributed to mental and neurological disorders (WHO, 2017). Analysis of data from a WHO Study on global AGEing and adult health (SAGE) also points to the high prevalence of arthritis in low‐ and middle‐income settings, particularly among those in a lower socioeconomic position (WHO, 2001).
6.3. Areas of major gaps in the evidence
Our study reveals that systematic review evidence on the effects of home‐based health and social care and mobility support interventions is of limited methodological quality, with only 13 out of 120 reviews (11%) being rated as high methodological quality. Quality of systematic reviews in this area needs to be improved by adhering to methodological standards such as the Cochrane Handbook methods (Higgins et al., 2019) which include describing a clearly formulated question, describing eligibility criteria, search strategies, reasons for exclusion, publishing an a priori protocol and transparent reporting of methods (e.g., using the Preferred Reporting Items for Systematic Reviews and Meta‐analyses (Moher et al., 2015)). Importantly, quality is based on the methods of the review, not on the strength or quality of evidence within the review.
Furthermore, our EGM illustrates that studies are unevenly distributed across our full intervention‐outcome framework. Clusters emerge for some intervention—outcome combinations, in contrast with some noticeable evidence gaps. There is significant evidence (both randomized trials and systematic reviews) on health services, systems and policies (n = 525). Studies focusing on home‐based rehabilitation (n = 276) and general health services (n = 233) make up the largest proportion of studies in this map. There is a lack of data available on general social support services and policies (n = 41), personal indoor and outdoor mobility and transportation (n = 12), and design, construction and building products and technology (n = 21).
It is known that caregiver burden is a significant risk factor for depressive symptoms in carers of older people and may precipitate clinical depression (del‐Pino‐Casado et al., 2019) however, only 71 studies in the EGM explored caregiver outcomes. There were very few studies focused on loneliness and social isolation which is an important dimension for older adults (n = 7). Mobility limitations can contribute to social isolation and loneliness that may affect the mental and physical health of older adults (WHO, 2015).
Included studies mostly covered three WHO regions; Western Pacific, the Americas, and Europe. There were a small number of studies that covered South‐East Asia (n = 5) and Africa (n = 1). No studies covered the Eastern Mediterranean region. A significant proportion of studies are from high‐income economies (97%). The lack of evidence from low‐ and lower‐middle income countries points to the need for more high‐quality reviews and trials in these settings. This is particularly important since these regions, as previously mentioned, are experiencing a quicker growth in population ageing when compared to high‐income countries (UNDESA, 2017).
Diversity of characteristics and settings of older adults across age, sex/gender, ethnicity, medical conditions, settings, environments and culture may influence the impact of interventions. Over 90% of studies did not assess possible differences in effects across PROGRESS characteristics. The lack of health equity considerations within studies raise the need for future studies to consider health inequities, particularly since home‐based health, social and technology supports may not be accessible to all or require out of pocket costs, acceptability may differ across culture, country contexts and sex/gender, and programs may thus worsen or exacerbate existing health inequities.
6.4. Potential biases in the mapping process
We followed a systematic process with the help of an information scientist to develop our search strategy. As health and social care interventions and outcomes have different names in different contexts and languages, it is possible that we missed studies with our search strategy, even though the terms we used were developed in consultation with a search specialist and our advisory team, which included several experts in this field. In addition, we may have missed studies that were not indexed as home‐based. To mitigate this risk, we also reviewed the lists of included studies in eligible systematic reviews.
6.5. Limitations of the EGM
We focused on randomized trials for reasons of feasibility, thus our EGM may over‐represent interventions that lend themselves better to randomization. We mitigated the risk of over‐representing “randomizable” interventions by including systematic reviews of nonrandomized studies of interventions. However, users need to keep in mind that this EGM represents mostly randomized study evidence.
As with other EGMs, trials in our map may also be included in systematic reviews in this map and studies with multiple interventions or multiple outcomes will appear in multiple quadrants of the map. This is important to consider when interpreting the map.
Systematic reviews were assessed for eligibility and coded on the basis of their PICO question. That could mean that reviews with a broad focus could be excluded if home setting was not part of the PICO.
7. AUTHORS' CONCLUSIONS
This EGM is a starting point for identifying priority areas for systematic reviews and primary studies of home‐based health and social care and technological supports to support older adults at home.
7.1. Implications for research, practice and/or policy
There is a need for rigorous evaluation studies of home‐based social care and mobility support to promote functional ability for older adults. Despite substantial evidence on home‐based health services interventions, only 10% of included systematic reviews were high quality, thus limiting their usefulness for decision‐making.
There is a need to consider assessing outcomes of importance to older adults such as financial security, societal contribution and participation, stigma, loneliness and social isolation, caregiver outcomes, cost, and safety which were assessed in <20% of included evidence sources.
There is a need to consider analyses to assess effects of interventions across equity factors. Without evaluation of gender and health inequities, we risk promoting interventions that could exacerbate or worsen existing gender and health inequities.
At the time of publication of this map, there is a huge need to understand how to best promote functional capacity of older adults who are unable to leave their homes due to social distancing restrictions levied in the interests of slowing the spread of SARS‐Cov‐2 in the population. This map provides an initial resource to identify relevant home‐based services which may be of interest to policy‐makers and healthcare professionals such as home‐based rehabilitation and social support. Some interventions may require further adaptation for online delivery during the COVID‐19 pandemic.
CONTRIBUTIONS OF AUTHORS
Content: Tracey E. Howe, Vivian Welch, Heidi Sveistrup, Sue Marcus, provide content expertise in rehabilitation, assistive devices and memory and cognitive impairment. Christine M. Mathew, Lisa Sheehy, and MC also have expertise in ageing and rehabilitation. Elizabeth Kristjansson has expertise in built environments and in healthy aging. Lisa Sheehy, Johan Borg, Wei Zhang, Joanna Thompson‐Coon, Anne Lyddiatt, Jason W. Nickerson, Peter Tanuseputro, Peter Walker, and Beverly Shea provided content expertise on classifying outcomes and interventions, and will provide critical comments on final manuscript.
EGM methods: Vivian Welch, Ashrita Saran, Sue Marcus, Tracey E. Howe, Kevin Pottie, Elizabeth T. Ghogomu and Elizabeth Kristjansson are experts in systematic review methods.
Information retrieval: Morwenna Rogers is an information specialist with experience in designing searches for systematic reviews.
DECLARATIONS OF INTEREST
VW is Editor in Chief of the Campbell Collaboration.
Johan Borg is employed as research manager at a commercial assistive technology company that may have an interest in the results or conclusions of this review.
JTC and MR were supported by the National Institute for Health Research Applied Research Collaboration South West Peninsula (PenARC) and this article therefore presents independent research supported by the National Institute for Health Research Applied Research Collaboration South West Peninsula (PenARC). The views expressed in this publication are those of the author(s) and not necessarily those of the National Health Service, the NIHR or the Department of Health and Social Care. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The rest of the authors have no conflicts of interest with respect to the content of the EGM.
PRELIMINARY TIMEFRAME
Approximate date for submission of the EGM: October 2019.
Please note this should be no longer than 1 year after protocol approval.
PLANS FOR UPDATING THE EGM
Vivian Welch, Tracey Howe and Sue Marcus, as directors of Cochrane Global Ageing, have an interest in continuing to update this EGM. Frequency of updating will depend on availability of resources to do so.
REFERENCES TO STUDIES
INCLUDED STUDIES
| Study | Publication status | Study design | Population‐age group | Population‐sex/gender | Health status/condition | WHO region | World Bank classification by income | Intervention: general social support services, systems and policies | Intervention: for personal indoor and outdoor mobility and transportation | Intervention: health services, systems and policies |
|---|---|---|---|---|---|---|---|---|---|---|
| Acton (2016) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | Personal care | General health services for disease prevention | ||
| Includes 65+ | Rehabilitation services | |||||||||
| Visiting health professionals | ||||||||||
| Aimonino (2008) | ||||||||||
| Complete | RCT | Includes 75+ | 25%‐50% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Alexander (2001) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Care dependent | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting lay service providers | ||||||||||
| Alexopoulos (2016) | ||||||||||
| Complete | RCT | Includes <65 | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Physical frailty | Visiting health professionals | ||||||||
| Amjad (2018) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Dementia | The Americas | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Andersen (2000) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | Visiting health professionals | |||
| Includes 65+ | ||||||||||
| Anonymous (2004) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Araujo (2015) | ||||||||||
| On‐going | RCT | Includes 65+ | Care dependent | European | High‐income economies | Transportation | ||||
| Discharged from hospital | Personal care | |||||||||
| Family and caregiver support | ||||||||||
| Arean (2015) | ||||||||||
| Complete | RCT | Includes 65+ | Care dependent | The Americas | High‐income economies | General health services for disease prevention | ||||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Arrieta (2018) | ||||||||||
| On‐going | RCT | Includes 65+ | 50%‐75% female included | Care dependent | European | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Ashburn (2007) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Avlund (2002) | ||||||||||
| Complete | RCT | Includes <65 | Discharged from hospital | European | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Baker (2007) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Banerjee (1996) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Physical frailty | Visiting health professionals | |||||||||
| Barnes (2017) | ||||||||||
| On‐going | RCT | Includes <65 | 75%‐100% female included | Dementia | The Americas | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Barreto (2018) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | Health promotion services | |||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Batchelor‐Murphy (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Care dependent | The Americas | High‐income economies | Personal care | Visiting health professionals | ||
| Dementia | ||||||||||
| Noncommunicable disease | ||||||||||
| Beck (2013) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | Family and caregiver support | General health services for disease prevention | ||
| Visiting health professionals | ||||||||||
| Beck (2016) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Care dependent | European | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Rehabilitation services | |||||||||
| Visiting health professionals | ||||||||||
| Behm (2014) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | European | High‐income economies | General health services for disease prevention | ||||
| Health promotion services | ||||||||||
| Visiting health professionals | ||||||||||
| Behm (2016) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Physical frailty | European | High‐income economies | General health services for disease prevention | |||
| Health promotion services | ||||||||||
| Visiting health professionals | ||||||||||
| Beland (2006) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Care dependent | The Americas | High‐income economies | Homemaking | General health services for disease prevention | ||
| Noncommunicable disease | Personal care | Visiting health professionals | ||||||||
| Bennell (2018) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Injury | Western Pacific | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Bernabei (1998) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | Personal care | General health services for disease prevention | ||
| Physical frailty | Visiting health professionals | |||||||||
| Bjerk (2017) | ||||||||||
| On‐going | RCT | Includes 65+ | Care dependent | European | High‐income economies | Rehabilitation services | ||||
| Injury | Visiting health professionals | |||||||||
| Blanchard (1999) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Bleijenberg (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Bonnefoy (2012) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Physical frailty | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Boongird (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | South‐East Asia | Upper‐middle‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Bouman (2008) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Boxall (2005) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Brannstrom (2014) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Long term care services | ||||||||||
| Visiting health professionals | ||||||||||
| Brettschneider (2014) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Brovold (2012) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Bruce (2015) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Bruce (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Brumley (2007) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | End‐of‐life | The Americas | High‐income economies | Long term care services | |||
| Visiting health professionals | ||||||||||
| Burton (2013) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Physical frailty | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Buurman (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Buys (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Discharged from hospital | The Americas | High‐income economies | Homemaking | |||
| Byles (2004) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Western Pacific | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Byrnes (2015) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Discharged from hospital | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Callahan (2012) | ||||||||||
| On‐going | RCT | Includes <65 | Noncommunicable disease | The Americas | High‐income economies | Personal care | General health services for disease prevention | |||
| Includes 65+ | Family and caregiver support | Visiting health professionals | ||||||||
| Campbell (1997) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Injury | Western Pacific | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Campbell (2005) | ||||||||||
| Complete | RCT | Includes 75+ | Noncommunicable disease | Western Pacific | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Canning (2015) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Noncommunicable disease | Western Pacific | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Caplan (1999) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Communicable disease | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Caplan (2004) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Caplan (2006) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Physical frailty | ||||||||||
| Carroll (2007) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Chaiyawat (2012) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Noncommunicable disease | South‐East Asia | Upper‐middle‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Chan et al. (2016) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Chandler (1998) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Physical frailty | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Chang (2015) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Chee (2013) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Physical frailty | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Chen (2015) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Care dependent | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Chen (2015) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Physical frailty | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Chen (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Cho (1998) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Injury | The Americas | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Chow (2014) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Chu (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | Western Pacific | High‐income economies | Personal mobility and transportation devices | General health services for disease prevention | ||
| Visiting health professionals | ||||||||||
| Cichocki (2015) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Care dependent | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Ciechanowski (2004) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Claffey (1976) | ||||||||||
| Complete | RCT | Includes <65 | Care dependent | The Americas | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Clegg (2014) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Clemson (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Comans (2010) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | Western Pacific | High‐income economies | Rehabilitation services | |||
| Physical frailty | Visiting health professionals | |||||||||
| Conradsson (2010) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Care dependent | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Cornu (2003) | ||||||||||
| On‐going | RCT | Includes 75+ | Care dependent | European | High‐income economies | Rehabilitation services | ||||
| Corr (1995) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Discharged from hospital | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Counsell (2007) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Courtney (2009) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Courtney (2011) | ||||||||||
| On‐going | RCT | Includes 65+ | Discharged from hospital | South‐East Asia | High‐income economies | General health services for disease prevention | ||||
| Physical frailty | Rehabilitation services | |||||||||
| Visiting health professionals | ||||||||||
| Courtney (2012) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Crotty (2002) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | Rehabilitation services | |||
| Physical frailty | Visiting health professionals | |||||||||
| Crotty (2003) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Crotty (2008) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Cumming (2000) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | Rehabilitation services | |||
| Physical frailty | Visiting health professionals | |||||||||
| Cummings (1990) | ||||||||||
| Complete | RCT | Includes 65+ | End‐of‐life | The Americas | High‐income economies | General health services for disease prevention | ||||
| Physical frailty | Visiting health professionals | |||||||||
| Cunliffe (2004) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Cutchin (2009) | ||||||||||
| On‐going | RCT | Includes 75+ | 50%‐75% female included | Physical frailty | The Americas | High‐income economies | Health promotion services | |||
| Visiting health professionals | ||||||||||
| Dalby (2000) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | The Americas | High‐income economies | General health services for disease prevention | |||
| Injury | Visiting health professionals | |||||||||
| Physical frailty | ||||||||||
| Daly (2015) | ||||||||||
| On‐going | RCT | Includes 65+ | Injury | Western Pacific | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Danilovich et al. (2017) | ||||||||||
| On‐going | RCT | Includes <65 | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Physical frailty | Visiting health professionals | ||||||||
| Dano (2016) | ||||||||||
| Complete | RCT | Includes <65 | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Dechamps (2010) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Di Monaco (2008) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Di Pollina (2017) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Physical frailty | European | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Dias (2008) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Dementia | South‐East Asia | Lower‐middle‐income economies | General health services for disease prevention | |||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Donald (1995) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Donat (2007) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Dorner (2013) | ||||||||||
| On‐going | RCT | Includes 65+ | Physical frailty | European | High‐income economies | Health promotion services | ||||
| Rehabilitation services | ||||||||||
| Visiting lay service providers | ||||||||||
| Dorresteijn (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | European | High‐income economies | General health services for disease prevention | |||
| Physical frailty | Visiting health professionals | |||||||||
| Dow (2013) | ||||||||||
| On‐going | RCT | Includes <65 | Physical frailty | Western Pacific | High‐income economies | Family and caregiver support | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Draper (2008) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Dementia | European | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Draper (2016) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Duffy (2010) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Edgren (2015) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Eloniemi‐Sulkava (2001) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | Family and caregiver support | General health services for disease prevention | ||
| Visiting health professionals | ||||||||||
| Eloniemi‐Sulkava (2009) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Dementia | European | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Noncommunicable disease | Rehabilitation services | ||||||||
| Visiting health professionals | ||||||||||
| Engberg (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Enguidanos (2012) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Discharged from hospital | The Americas | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Eriksen (2016) | ||||||||||
| On‐going | RCT | Includes <65 | 50%‐75% female included | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Fabacher (1994) | ||||||||||
| Complete | RCT | Includes 65+ | 0%‐25% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Visiting lay service providers | ||||||||||
| Faber (2006) | ||||||||||
| Complete | RCT | Includes <65 | 75%‐100% female included | Physical frailty | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Fahlström (2018) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Fairhall (2012) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Fairhall (2014) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | Western Pacific | High‐income economies | Personal mobility and transportation devices | General health services for disease prevention | ||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Fairhall et al. (2015) | ||||||||||
| On‐going | RCT | Includes 65+ | Physical frailty | Western Pacific | High‐income economies | Personal mobility and transportation devices | General health services for disease prevention | |||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Fairhall (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Farag (2015) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Farag (2016) | ||||||||||
| Complete | RCT | Includes <65 | 75%‐100% female included | Discharged from hospital | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Rehabilitation services | |||||||||
| Visiting health professionals | ||||||||||
| Fasce (2018) | ||||||||||
| On‐going | RCT | Includes <65 | Discharged from hospital | The Americas | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Noncommunicable disease | Rehabilitation services | ||||||||
| Visiting health professionals | ||||||||||
| Favela (2013) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Discharged from hospital | The Americas | Upper‐middle‐income economies | General health services for disease prevention | |||
| Includes 65+ | Physical frailty | Visiting health professionals | ||||||||
| Feldman (2004) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Ferrer (2014) | ||||||||||
| Complete | RCT | Includes 85+ | 50%‐75% female included | Injury | The Americas | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Ferrer‐Garcia (2011) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Fiatarone (1994) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | The Americas | High‐income economies | Rehabilitation services | |||
| Finnema (2005) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Care dependent | European | High‐income economies | General health services for disease prevention | |||
| Dementia | Visiting health professionals | |||||||||
| Noncommunicable disease | ||||||||||
| Fleming (2004) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Flood (2005) | ||||||||||
| Complete | RCT | Physical frailty | European | High‐income economies | Rehabilitation services | |||||
| Visiting health professionals | ||||||||||
| Fontan (2010) | ||||||||||
| Complete | RCT | Includes 65+ | European | High‐income economies | General health services for disease prevention | |||||
| Visiting health professionals | ||||||||||
| Forsberg (2011) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Forster (1996) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Noncommunicable disease | European | High‐income economies | Visiting health professionals | |||
| Includes 65+ | ||||||||||
| Frese (2012) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Friedman (2014) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Physical frailty | Visiting health professionals | |||||||||
| Gagnon (1999) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | The Americas | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Garcia‐Pena (2001) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Noncommunicable disease | The Americas | Upper‐middle‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Garcia‐Pena (2002) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Noncommunicable disease | The Americas | Upper‐middle‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Gawler (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Giangregorio (2018) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Injury | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Gill (2002) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Physical frailty | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Gill (2004) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Physical frailty | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Gitlin (2001) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Dementia | The Americas | High‐income economies | Visiting health professionals | |||
| Noncommunicable disease | ||||||||||
| Gitlin (2006) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Physical frailty | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Gitlin (2008) | ||||||||||
| Complete | RCT | Includes 75+ | 25%‐50% female included | Dementia | The Americas | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Gitlin (2009) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Physical frailty | The Americas | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Gitlin (2010) | ||||||||||
| Complete | RCT | Includes <65 | Dementia | The Americas | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Gitlin (2014) | ||||||||||
| Complete | RCT | Includes <65 | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Gitlin (2018) | ||||||||||
| Complete | RCT | Includes 65+ | 0%‐25% female included | Dementia | The Americas | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Physical frailty | ||||||||||
| Gladman (1993) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Godwin (2016) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | The Americas | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Gozalo (2014) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Care dependent | The Americas | High‐income economies | Personal care | |||
| Dementia | ||||||||||
| Noncommunicable disease | ||||||||||
| Graff (2008) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Dementia | European | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Granbom (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Graves (2009) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Grimmer (2013) | ||||||||||
| On‐going | RCT | Includes 65+ | Discharged from hospital | Western Pacific | High‐income economies | Health promotion services | ||||
| Visiting health professionals | ||||||||||
| Gronstedt (2013) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Physical frailty | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Gustafsson (2012) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | European | High‐income economies | General health services for disease prevention | ||||
| Includes 85+ | Visiting health professionals | |||||||||
| Haastregt (2000) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | European | High‐income economies | Visiting health professionals | |||
| Includes 75+ | ||||||||||
| Haider (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Physical frailty | European | High‐income economies | Rehabilitation services | |||
| Includes 75+ | Visiting lay service providers | |||||||||
| Includes 85+ | ||||||||||
| Haider (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Physical frailty | European | High‐income economies | Rehabilitation services | |||
| Includes 75+ | Visiting lay service providers | |||||||||
| Includes 85+ | ||||||||||
| Hall (1992) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Physical frailty | The Americas | High‐income economies | Health promotion services | |||
| Includes 75+ | Visiting health professionals | |||||||||
| Includes 85+ | ||||||||||
| Hammar (2009) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Hansen (1992) | ||||||||||
| Complete | RCT | Includes 75+ | 25%‐50% female included | Discharged from hospital | European | High‐income economies | Health promotion services | |||
| Visiting health professionals | ||||||||||
| Hansen (1995) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Includes 75+ | ||||||||||
| Includes 85+ | ||||||||||
| Harris (2005) | ||||||||||
| Complete | RCT | Includes <65 | 75%‐100% female included | Discharged from hospital | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Harvey (2014) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Includes 75+ | Visiting health professionals | |||||||||
| Includes 85+ | ||||||||||
| Hauer (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Discharged from hospital | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Helbostad (2004) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Injury | European | High‐income economies | ||||
| Noncommunicable disease | ||||||||||
| Hendriks (2008) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Herfjord (2014) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Includes 85+ | Rehabilitation services | |||||||||
| Visiting health professionals | ||||||||||
| Hewitt (2018) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Care dependent | Western Pacific | High‐income economies | Rehabilitation services | |||
| Includes 75+ | ||||||||||
| Includes 85+ | ||||||||||
| Hinrichs (2015) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | Rehabilitation services | |||
| Includes 85+ | ||||||||||
| Hinrichs (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Care dependent | European | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Rehabilitation services | |||||||||
| Visiting health professionals | ||||||||||
| Hoenig (2015) | ||||||||||
| Complete | RCT | Includes 65+ | 0%‐25% female included | The Americas | High‐income economies | Personal mobility and transportation devices | ||||
| Includes 75+ | ||||||||||
| Holland (2005) | ||||||||||
| Complete | RCT | Includes 85+ | Discharged from hospital | European | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Holland (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | Western Pacific | High‐income economies | Rehabilitation services | |||
| Includes 75+ | ||||||||||
| Houles (2010) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Physical frailty | European | High‐income economies | General health services for disease prevention | |||
| Includes 85+ | Visiting health professionals | |||||||||
| Hsu (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Hsu (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Care dependent | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Huang (1998) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Western Pacific | High‐income economies | General health services for disease prevention | ||||
| Includes 75+ | Visiting health professionals | |||||||||
| Huang (2013) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Dementia | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Includes 75+ | Noncommunicable disease | |||||||||
| Includes 85+ | ||||||||||
| Hughes (1992) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Physical frailty | The Americas | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Hughes (2000) | ||||||||||
| Complete | RCT | Includes <65 | 0%‐25% female included | Discharged from hospital | The Americas | High‐income economies | Health promotion services | |||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Physical frailty | ||||||||||
| Hunger (2015) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Wang et al. (2016) | ||||||||||
| Complete | RCT | Includes <65 | 75%‐100% female included | Injury | Western Pacific | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Iliffe (2014) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Imhof (2012) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Care dependent | European | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Inglis (2006) | ||||||||||
| Complete | RCT | Includes 65+ | 0%‐25% female included | Noncommunicable disease | Western Pacific | High‐income economies | Visiting health professionals | |||
| Includes 75+ | ||||||||||
| Isrctn (2018) | ||||||||||
| On‐going | RCT | Includes <65 | Dementia | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Jakobsen (2007) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | Visiting health professionals | |||
| Jensen (2002) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Injury | European | High‐income economies | Personal mobility and transportation devices | Rehabilitation services | ||
| Jingna (2012) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Physical frailty | Western Pacific | Upper‐middle‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Joaquim (2017) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Noncommunicable disease | The Americas | Upper‐middle‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Johansson (2001) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Johansson (2003) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Includes 75+ | Visiting health professionals | |||||||||
| Jolly (2009) | ||||||||||
| Complete | RCT | Includes <65 | 0%‐25% female included | Discharged from hospital | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Kalra (2000) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Kane (1984) | ||||||||||
| Complete | RCT | Includes <65 | 0%‐25% female included | End‐of‐life | The Americas | High‐income economies | Long term care services | |||
| Kanemaru (2010) | ||||||||||
| Complete | RCT | Includes <65 | 75%‐100% female included | Noncommunicable disease | Western Pacific | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Kapan (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Physical frailty | European | High‐income economies | Friendly visits | Rehabilitation services | ||
| Includes 75+ | Visiting lay service providers | |||||||||
| Includes 85+ | ||||||||||
| Kapan (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Physical frailty | European | High‐income economies | General health services for disease prevention | |||
| Rehabilitation services | ||||||||||
| Visiting lay service providers | ||||||||||
| Karinkanta (2007) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | European | High‐income economies | Rehabilitation services | ||||
| Includes 75+ | ||||||||||
| Karlsson (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Kerr (2018) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | The Americas | High‐income economies | Rehabilitation services | ||||
| Includes 75+ | ||||||||||
| Includes 85+ | ||||||||||
| Kerse (2010) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Noncommunicable disease | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Kim (2011) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | South‐East Asia | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| King et al. (2012) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| King et al. (2012) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Care dependent | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Kjerstad (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Klug (2011) | ||||||||||
| Complete | RCT | Includes <65 | 75%‐100% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Kocic (2018) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | European | Upper‐middle‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Kohei (2016) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Noncommunicable disease | Western Pacific | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Kono (2004) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Care dependent | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Physical frailty | Visiting health professionals | |||||||||
| Kono (2012) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Care dependent | Western Pacific | High‐income economies | Health promotion services | |||
| Physical frailty | Visiting health professionals | |||||||||
| Kono (2013) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Care dependent | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Kono (2014) | ||||||||||
| On‐going | RCT | Includes 65+ | Physical frailty | Western Pacific | High‐income economies | Visiting health professionals | ||||
| Kono (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Care dependent | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Kronborg (2006) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Care dependent | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Kukkonen‐Harjula (2018) | ||||||||||
| On‐going | RCT | Includes 75+ | 75%‐100% female included | Physical frailty | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Kwok (2004) | ||||||||||
| Complete | RCT | Includes 75+ | 25%‐50% female included | Discharged from hospital | Western Pacific | High‐income economies | Visiting health professionals | |||
| Noncommunicable disease | ||||||||||
| Kwok (2016) | ||||||||||
| Complete | RCT | Includes <65 | Noncommunicable disease | Western Pacific | High‐income economies | Health promotion services | ||||
| Includes 65+ | ||||||||||
| Kyrdalen (2014) | ||||||||||
| Complete | RCT | Includes 75+ | 25%‐50% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Lam (2018) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Physical frailty | Western Pacific | High‐income economies | Rehabilitation services | |||
| Lannin (2007) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Discharged from hospital | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Latham (2014) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | The Americas | High‐income economies | Rehabilitation services | |||
| Includes 75+ | ||||||||||
| Latour (2007) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Lattanzio (2001) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Leavitt (2018) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Discharged from hospital | The Americas | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Lee (2006) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Lenaghan (2007) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Levine (2012) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Physical frailty | Visiting health professionals | |||||||||
| Lewin (2013) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Care dependent | Western Pacific | High‐income economies | Rehabilitation services | |||
| Lewin (2014) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | Western Pacific | High‐income economies | Rehabilitation services | |||
| Li (2013) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Care dependent | The Americas | High‐income economies | Personal care | General health services for disease prevention | ||
| Visiting health professionals | ||||||||||
| Li (2015) | ||||||||||
| Complete | RCT | Includes 75+ | 0%‐25% female included | Discharged from hospital | Western Pacific | Upper‐middle‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Liang (1984) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Liang (1986) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Care dependent | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Liddle (1996) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Western Pacific | High‐income economies | Visiting health professionals | ||||
| Includes 75+ | ||||||||||
| Includes 85+ | ||||||||||
| Liimatta (2017) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Lin (2007) | ||||||||||
| Complete | RCT | Includes 65+ | Injury | Western Pacific | High‐income economies | Rehabilitation services | ||||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Lin (2010) | ||||||||||
| Complete | RCT | Includes 75+ | 25%‐50% female included | Dementia | Western Pacific | High‐income economies | Rehabilitation services | |||
| Includes 85+ | 50%‐75% female included | Noncommunicable disease | ||||||||
| Lindegaard (2017) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Care dependent | European | High‐income economies | General health services for disease prevention | |||
| Discharged from hospital | Visiting health professionals | |||||||||
| Noncommunicable disease | ||||||||||
| Lindegaard‐Pedersen (2015) | ||||||||||
| On‐going | RCT | Includes 75+ | Discharged from hospital | European | High‐income economies | General health services for disease prevention | ||||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Liu and Lai (2014) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Liu (2015) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Dementia | The Americas | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Locher (2013) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | Visiting health professionals | |||
| Includes 75+ | ||||||||||
| Includes 85+ | ||||||||||
| Logan (2004) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | Rehabilitation services | |||
| Includes 75+ | ||||||||||
| Lok (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | European | Upper‐middle‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Luck (2013) | ||||||||||
| Complete | RCT | Includes 85+ | Physical frailty | European | High‐income economies | Visiting health professionals | ||||
| Lyons (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| MacIntyre (1999) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Care dependent | The Americas | High‐income economies | Friendly visits | |||
| Social isolation | ||||||||||
| Mahoney (2007) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Injury | The Americas | High‐income economies | Rehabilitation services | |||
| Includes 85+ | Visiting health professionals | |||||||||
| Maiers (2014) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Includes 75+ | ||||||||||
| Mangione (2005) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Discharged from hospital | The Americas | High‐income economies | Rehabilitation services | |||
| Injury | Visiting health professionals | |||||||||
| Mangione et al. (2010) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Injury | The Americas | High‐income economies | Rehabilitation services | |||
| Includes 85+ | ||||||||||
| Mann (1999) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Physical frailty | The Americas | High‐income economies | Personal mobility and transportation devices | Visiting health professionals | ||
| Marek (2014) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Noncommunicable disease | The Americas | High‐income economies | Visiting health professionals | |||
| Markle‐Reid (2003) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Physical frailty | The Americas | High‐income economies | General health services for disease prevention | |||
| Health promotion services | ||||||||||
| Visiting health professionals | ||||||||||
| Markle‐Reid (2006) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Physical frailty | The Americas | High‐income economies | Homemaking | General health services for disease prevention | ||
| Includes 85+ | Personal care | Visiting health professionals | ||||||||
| Markle‐Reid (2010) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Injury | The Americas | High‐income economies | Transportation | General health services for disease prevention | ||
| Visiting health professionals | ||||||||||
| Markle‐Reid et al. (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Health promotion services | ||||||||||
| Visiting health professionals | ||||||||||
| Martin (1994) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Maru (2015) | ||||||||||
| Complete | RCT | Includes 65+ | Discharged from hospital | Western Pacific | High‐income economies | General health services for disease prevention | ||||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Matzen (2007) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Mayo (2008) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Discharged from hospital | The Americas | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| McCorkle (1989) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| McCorkle (2000) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Discharged from hospital | The Americas | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| McMurdo (1995) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Physical frailty | European | High‐income economies | Rehabilitation services | |||
| Includes 85+ | Visiting health professionals | |||||||||
| McWilliam (1999) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | The Americas | High‐income economies | Health promotion services | |||
| Includes 75+ | Noncommunicable disease | Visiting health professionals | ||||||||
| McWilliam (1999) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | The Americas | High‐income economies | Health promotion services | |||
| Includes 75+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Meisinger (2013) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Includes 75+ | Visiting health professionals | |||||||||
| Melin (1992) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Discharged from hospital | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Includes 75+ | ||||||||||
| Includes 85+ | ||||||||||
| Melin (1993) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Physical frailty | Visiting health professionals | |||||||||
| Melin (1993) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | Rehabilitation services | |||
| Includes 75+ | Visiting health professionals | |||||||||
| Includes 85+ | ||||||||||
| Melin (1995) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | Visiting health professionals | |||
| Includes 75+ | ||||||||||
| Melis (2008) | ||||||||||
| Complete | RCT | Includes 65+ | Care dependent | European | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Melis (2008) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Care dependent | European | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Mihalko (1996) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Physical frailty | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Miller (2005) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Milte (2016) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Injury | Western Pacific | High‐income economies | Rehabilitation services | |||
| Includes 85+ | 75%‐100% female included | Visiting health professionals | ||||||||
| Mitchell (2005) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Mohide (1990) | ||||||||||
| Complete | RCT | Includes 75+ | 25%‐50% female included | Dementia | The Americas | High‐income economies | Visiting health professionals | |||
| Noncommunicable disease | ||||||||||
| Molassiotis (2009) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Moller (2014) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | European | High‐income economies | Health promotion services | |||
| Physical frailty | Visiting health professionals | |||||||||
| Montgomery (2003) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Physical frailty | The Americas | High‐income economies | General health services for disease prevention | |||
| Includes 85+ | ||||||||||
| Morris (2017) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Noncommunicable disease | Western Pacific | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Includes 75+ | ||||||||||
| Mortensen (2016) | ||||||||||
| Complete | RCT | Includes <65 | Noncommunicable disease | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Mulrow (1994) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Murphy (2005) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Discharged from hospital | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Naunton (2003) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Naylor (1999) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | The Americas | High‐income economies | General health services for disease prevention | |||
| Includes 75+ | Visiting health professionals | |||||||||
| Naylor (2004) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | The Americas | High‐income economies | Visiting health professionals | |||
| Includes 75+ | ||||||||||
| Naylor (2004) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | The Americas | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Nazareth (2001) | ||||||||||
| Complete | RCT | Includes 75+ | Discharged from hospital | European | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Nct (2005) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | European | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Nct (2006) | ||||||||||
| Complete | RCT | Includes 85+ | 50%‐75% female included | European | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Nct (2011) | ||||||||||
| On‐going | RCT | Includes <65 | Discharged from hospital | The Americas | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Nct (2011) | ||||||||||
| On‐going | RCT | Includes 65+ | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | ||||
| Includes 75+ | ||||||||||
| Nct (2012) | ||||||||||
| On‐going | RCT | Includes 65+ | Injury | The Americas | High‐income economies | General health services for disease prevention | ||||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Nct (2013) | ||||||||||
| Complete | RCT | Includes 65+ | Social isolation | European | High‐income economies | Homemaking | ||||
| Friendly visits | ||||||||||
| Nct (2014) | ||||||||||
| On‐going | RCT | Includes 65+ | Care dependent | Western Pacific | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Nct (2014) | ||||||||||
| On‐going | RCT | Includes 65+ | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Nct (2014) | ||||||||||
| On‐going | RCT | Includes 65+ | Discharged from hospital | The Americas | High‐income economies | Visiting health professionals | ||||
| Nct (2015) | ||||||||||
| On‐going | RCT | Includes 75+ | Care dependent | The Americas | High‐income economies | Personal mobility and transportation devices | Rehabilitation services | |||
| Injury | Visiting health professionals | |||||||||
| Nct (2017) | ||||||||||
| On‐going | RCT | Includes 65+ | Western Pacific | High‐income economies | General health services for disease prevention | |||||
| Health promotion services | ||||||||||
| Visiting health professionals | ||||||||||
| Nct (2017) | ||||||||||
| On‐going | RCT | Includes 65+ | Physical frailty | The Americas | High‐income economies | Rehabilitation services | ||||
| Nct (2017) | ||||||||||
| On‐going | RCT | Includes 65+ | Injury | The Americas | High‐income economies | General health services for disease prevention | ||||
| Includes 75+ | Health promotion services | |||||||||
| Nct (2017) | ||||||||||
| On‐going | RCT | Includes <65 | End‐of‐life | Western Pacific | High‐income economies | Long term care services | ||||
| Includes 65+ | ||||||||||
| Nct (2018) | ||||||||||
| On‐going | RCT | Includes 65+ | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | ||||
| Physical frailty | Visiting health professionals | |||||||||
| Nct (2018) | ||||||||||
| On‐going | RCT | Includes 65+ | Injury | European | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Neumann (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | European | High‐income economies | General health services for disease prevention | ||||
| Includes 75+ | Health promotion services | |||||||||
| Visiting health professionals | ||||||||||
| Nicolaides‐Bouman (2004) | ||||||||||
| On‐going | RCT | Includes 65+ | 50%‐75% female included | Care dependent | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Nielsen (1972) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | The Americas | High‐income economies | Homemaking | |||
| Injury | Personal care | |||||||||
| Noncommunicable disease | ||||||||||
| Nikolaus (1999) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Includes 75+ | Visiting health professionals | |||||||||
| Nikolaus (2003) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Injury | Visiting health professionals | |||||||||
| Nobili (2004) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Care dependent | European | High‐income economies | Family and caregiver support | Rehabilitation services | ||
| Dementia | Visiting health professionals | |||||||||
| Noncommunicable disease | ||||||||||
| Nowalk (2001) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | The Americas | High‐income economies | Rehabilitation services | ||||
| Includes 75+ | ||||||||||
| Includes 85+ | ||||||||||
| Oerkild (2011) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Oerkild (2012) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | European | High‐income economies | Rehabilitation services | |||
| Includes 75+ | ||||||||||
| Olaleye (2014) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Noncommunicable disease | African | Lower‐middle‐income economies | Rehabilitation services | |||
| Includes 65+ | ||||||||||
| Olesen (2014) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | Visiting health professionals | |||
| Includes 75+ | ||||||||||
| Olson (2011) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Injury | The Americas | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Oosting (2012) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | European | High‐income economies | Rehabilitation services | |||
| Includes 75+ | 75%‐100% female included | |||||||||
| Orrell (2017) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Dementia | European | High‐income economies | Rehabilitation services | |||
| Includes 85+ | Noncommunicable disease | |||||||||
| Ouslander (2005) | ||||||||||
| Complete | RCT | Includes <65 | 0%‐25% female included | Care dependent | The Americas | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Özdemir (2001) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Noncommunicable disease | European | Upper‐middle‐income economies | Rehabilitation services | |||
| Includes 65+ | ||||||||||
| Padala (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Includes 75+ | ||||||||||
| Padula (2009) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Papaioannou (2003) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Includes 75+ | ||||||||||
| Pardessus (2002) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Injury | Visiting health professionals | |||||||||
| Parker (2009) | ||||||||||
| Complete | RCT | Includes <65 | 75%‐100% female included | Care dependent | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Parker (2011) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Noncommunicable disease | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Parsons et al. (2013) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Care dependent | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Parsons (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | European | High‐income economies | General health services for disease prevention | |||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Patterson (2009) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Western Pacific | High‐income economies | General health services for disease prevention | ||||
| Visiting lay service providers | ||||||||||
| Pedersen (2016) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Physical frailty | Visiting health professionals | |||||||||
| Peeters (2007) | ||||||||||
| On‐going | RCT | Includes 65+ | Injury | European | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Pizzi (2014) | ||||||||||
| Complete | RCT | Includes <65 | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Includes 75+ | ||||||||||
| Portegijs (2013) | ||||||||||
| Complete | RCT | Includes 65+ | European | High‐income economies | Rehabilitation services | |||||
| Visiting health professionals | ||||||||||
| Prick (2015) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Dementia | European | High‐income economies | Family and caregiver support | Rehabilitation services | ||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Pröfener (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Physical frailty | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Radwany (2014) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Long term care services | |||||||||
| Visiting health professionals | ||||||||||
| Rasmussen (2016) | ||||||||||
| Complete | RCT | Includes 65+ | European | High‐income economies | Rehabilitation services | |||||
| Visiting health professionals | ||||||||||
| Ray (1997) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Injury | The Americas | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Reckrey (2018) | ||||||||||
| On‐going | RCT | Includes 65+ | Care dependent | The Americas | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Reeves (2004) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Regan (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | Western Pacific | High‐income economies | Rehabilitation services | |||
| Includes 75+ | 50%‐75% female included | |||||||||
| Resnick (2009) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Richards (1998) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | European | High‐income economies | General health services for disease prevention | |||
| Includes 75+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Robertson et al. (2001) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Care dependent | Western Pacific | High‐income economies | Rehabilitation services | |||
| Injury | Visiting health professionals | |||||||||
| Noncommunicable disease | ||||||||||
| Roderick (2001) | ||||||||||
| Complete | RCT | Includes 65+ | Noncommunicable disease | European | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Rosendahl (2006) | ||||||||||
| Complete | RCT | Includes 65+ | Physical frailty | European | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Rosstad (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Rossum (1993) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Care dependent | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Rubenstein (1994) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Care dependent | The Americas | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Runciman (1996) | ||||||||||
| Complete | RCT | Includes 75+ | Discharged from hospital | European | High‐income economies | Visiting health professionals | ||||
| Ryan (2006) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Rytter (2010) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Sackley (2007) | ||||||||||
| Complete | RCT | Includes <65 | 75%‐100% female included | Care dependent | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Physical frailty | Visiting health professionals | ||||||||
| Social isolation | ||||||||||
| Sackley (2009) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Care dependent | European | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Sackley (2015) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | Personal mobility and transportation devices | Rehabilitation services | ||
| Visiting health professionals | ||||||||||
| Sahlen (2016) | ||||||||||
| Complete | RCT | Noncommunicable disease | European | High‐income economies | Long term care services | |||||
| Salminen (2009) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Injury | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Salpakoski (2014) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Samus (2014) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Care dependent | The Americas | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Sandberg (2015) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Sandberg (2015) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Care dependent | European | High‐income economies | General health services for disease prevention | |||
| Physical frailty | Visiting health professionals | |||||||||
| Sanford (2006) | ||||||||||
| Complete | RCT | Includes <65 | Care dependent | The Americas | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Schnelle (1996) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Physical frailty | Visiting health professionals | |||||||||
| Schnelle (2010) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | Personal care | Rehabilitation services | ||
| Visiting health professionals | ||||||||||
| Seidl (2015) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Includes 75+ | Visiting health professionals | |||||||||
| Senior (2014) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Physical frailty | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Serra‐Rexach (2011) | ||||||||||
| Complete | RCT | Includes 85+ | 75%‐100% female included | Care dependent | European | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Physical frailty | ||||||||||
| Sheffield (2013) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Physical frailty | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Shepperd and Iliffe (1998) | ||||||||||
| Complete | RCT | Includes <65 | Discharged from hospital | European | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Shepperd and Iliffe (1998) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Injury | European | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Shepperd (2017) | ||||||||||
| On‐going | RCT | Includes 65+ | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Sherman (2016) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | European | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Sherrington (2015) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Sherrington (2016) | ||||||||||
| On‐going | RCT | Includes <65 | Injury | Western Pacific | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Shyu (2008) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Discharged from hospital | Western Pacific | High‐income economies | Family and caregiver support | General health services for disease prevention | ||
| Visiting health professionals | ||||||||||
| Shyu (2016) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Injury | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Rehabilitation services | |||||||||
| Includes 75+ | ||||||||||
| Siggeirsdottir (2005) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Simmons (2002) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Simmons (2005) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | Personal care | |||
| Sloane (2004) | ||||||||||
| Complete | RCT | Includes <65 | 75%‐100% female included | Care dependent | The Americas | High‐income economies | Personal care | |||
| Includes 65+ | Dementia | |||||||||
| Noncommunicable disease | ||||||||||
| Steele (2008) | ||||||||||
| Complete | RCT | Includes <65 | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Steinberg (2009) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Dementia | The Americas | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Stelmack et al. (2007) | ||||||||||
| Complete | RCT | Includes 65+ | 0%‐25% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Stevens (2001) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Western Pacific | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Stevens‐Lapsley (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Discharged from hospital | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Stewart et al. (2005) | ||||||||||
| Complete | RCT | Includes 65+ | Physical frailty | European | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Stewart (2012) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Noncommunicable disease | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Stuck et al. (1995) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Stuck et al. (1995) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | The Americas | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Stuck (2000) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Care dependent | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Suominen (2015) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Care dependent | European | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Suttanon (2013) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Szanton (2014) | ||||||||||
| On‐going | RCT | Includes 65+ | Physical frailty | The Americas | High‐income economies | General health services for disease prevention | ||||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Talley (2017) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | |||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Taube (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Thomas (2016) | ||||||||||
| Complete | RCT | Includes 65+ | Care dependent | The Americas | High‐income economies | Homemaking | ||||
| Thomas (2018) | ||||||||||
| Complete | RCT | Includes 65+ | Physical frailty | The Americas | High‐income economies | Homemaking | ||||
| Thygesen (2015) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Tibaldi (2004) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Physical frailty | Visiting health professionals | |||||||||
| Tibaldi (2009) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Tinetti (1999) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Discharged from hospital | The Americas | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Toots (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Dementia | European | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Townsend (1988) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Tsaih (2011) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Injury | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Tseng (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Tsuchihashi‐Makaya (2013) | ||||||||||
| Complete | RCT | Includes 65+ | 25%‐50% female included | Noncommunicable disease | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Turunen (2017) | ||||||||||
| On‐going | RCT | Includes 65+ | Discharged from hospital | European | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Underwood (2013) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Valdes (2015) | ||||||||||
| Complete | RCT | Includes <65 | 75%‐100% female included | Injury | The Americas | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Van Der Pols‐Vijlbrief (2016) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| van Haastregt (2000) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Injury | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| van Hout (2010) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| van Houten (2007) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Noncommunicable disease | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Vass (2007) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | European | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Verweij (2018) | ||||||||||
| On‐going | RCT | Includes 65+ | Discharged from hospital | European | High‐income economies | General health services for disease prevention | ||||
| Noncommunicable disease | Rehabilitation services | |||||||||
| Visiting health professionals | ||||||||||
| Vogler (2009) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | Rehabilitation services | |||
| 75%‐100% female included | Visiting health professionals | |||||||||
| Weir (1998) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Discharged from hospital | The Americas | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Rehabilitation services | |||||||||
| Visiting health professionals | ||||||||||
| Whitehead (2014) | ||||||||||
| On‐going | RCT | Includes <65 | European | High‐income economies | Rehabilitation services | |||||
| Includes 65+ | Visiting health professionals | |||||||||
| Wilhelmson (2013) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Physical frailty | European | High‐income economies | Health promotion services | |||
| Visiting health professionals | ||||||||||
| Wilson (2009) | ||||||||||
| Complete | RCT | Includes <65 | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Wishart (2000) | ||||||||||
| Complete | RCT | Includes 75+ | 75%‐100% female included | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||
| Visiting lay service providers | ||||||||||
| Wisniowska‐Szurlej (2017) | ||||||||||
| On‐going | RCT | Includes 65+ | Care dependent | European | High‐income economies | Rehabilitation services | ||||
| Wong (2015) | ||||||||||
| Complete | RCT | Includes <65 | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | General health services for disease prevention | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Wong (2016) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Discharged from hospital | Western Pacific | High‐income economies | Long term care services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Visiting lay service providers | ||||||||||
| Wylie (2017) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Injury | European | High‐income economies | Personal care | Rehabilitation services | ||
| Young (1992) | ||||||||||
| Complete | RCT | Includes <65 | 25%‐50% female included | Discharged from hospital | The Americas | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Ziden (2008) | ||||||||||
| Complete | RCT | Includes 75+ | 50%‐75% female included | Care dependent | European | High‐income economies | Rehabilitation services | |||
| Injury | Visiting health professionals | |||||||||
| Ziden (2010) | ||||||||||
| Complete | RCT | Includes 65+ | 75%‐100% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Ziden (2014) | ||||||||||
| Complete | RCT | Includes 85+ | 50%‐75% female included | Injury | European | High‐income economies | General health services for disease prevention | |||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Zimmer (1985) | ||||||||||
| Complete | RCT | Includes 65+ | 50%‐75% female included | Care dependent | The Americas | High‐income economies | General health services for disease prevention | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Physical frailty | Visiting lay service providers | |||||||||
| Abdulla (2013) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | European | High‐income economies | Rehabilitation services | ||||
| Physical frailty | Visiting health professionals | |||||||||
| Allen et al. (2014) | ||||||||||
| Complete | Systematic review | Includes <65 | Discharged from hospital | Western Pacific | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Andy (2016) | ||||||||||
| Complete | Systematic review | Includes 65+ | 50%‐75% female included | Care dependent | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Apostolo (2018) | ||||||||||
| Complete | Systematic review | Includes 65+ | Physical frailty | European | High‐income economies | General health services for disease prevention | ||||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Baldwin (2011) | ||||||||||
| Complete | Systematic review | Includes <65 | Physical frailty | European | High‐income economies | Health promotion services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Baxter (2016) | ||||||||||
| Complete | Systematic review | Includes <65 | European | High‐income economies | Rehabilitation services | |||||
| Includes 65+ | Visiting health professionals | |||||||||
| Berger (2013) | ||||||||||
| Complete | Systematic review | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | |||||
| Visiting health professionals | ||||||||||
| Beswick (2010) | ||||||||||
| Complete | Systematic review | Includes 65+ | Discharged from hospital | European | High‐income economies | General health services for disease prevention | ||||
| Injury | Visiting health professionals | |||||||||
| Physical frailty | ||||||||||
| Blythe (2009) | ||||||||||
| Complete | Systematic review | Includes <65 | Care dependent | Western Pacific | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Dementia | Visiting health professionals | ||||||||
| Noncommunicable disease | ||||||||||
| Bryant‐Lukosius (2015) | ||||||||||
| Complete | Systematic review | Includes <65 | Communicable disease | The Americas | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Discharged from hospital | Visiting health professionals | ||||||||
| Bula (2011) | ||||||||||
| Complete | Systematic review | Includes <65 | Injury | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Bunn (2016) | ||||||||||
| Complete | Systematic review | Includes <65 | Dementia | European | High‐income economies | Homemaking | ||||
| Includes 65+ | Noncommunicable disease | |||||||||
| Burns (2001) | ||||||||||
| Complete | Systematic review | Includes <65 | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Burton (2015) | ||||||||||
| Complete | Systematic review | Includes 65+ | Dementia | Western Pacific | High‐income economies | Rehabilitation services | ||||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Burton (2015) | ||||||||||
| Complete | Systematic review | Includes 65+ | 75%‐100% female included | Physical frailty | Western Pacific | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Cadore (2013) | ||||||||||
| Complete | Systematic review | Includes 65+ | Physical frailty | European | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Candy (2011) | ||||||||||
| Complete | Systematic review | End‐of‐life | European | High‐income economies | Long term care services | |||||
| Visiting health professionals | ||||||||||
| Cattan (2005) | ||||||||||
| Complete | Systematic review | Includes <65 | Social isolation | European | High‐income economies | Family and caregiver support | Health promotion services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Chiung‐Ju (2013) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Chou (2012) | ||||||||||
| Complete | Systematic review | Includes 75+ | 50%‐75% female included | Care dependent | Western Pacific | Upper‐middle‐income economies | Rehabilitation services | |||
| Physical frailty | Visiting health professionals | |||||||||
| Clarkson (2018) | ||||||||||
| Complete | Systematic review | Includes <65 | Dementia | European | High‐income economies | Family and caregiver support | General health services for disease prevention | |||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Clegg (2012) | ||||||||||
| Complete | Systematic review | Includes 65+ | Physical frailty | European | High‐income economies | Rehabilitation services | ||||
| Includes 75+ | Visiting health professionals | |||||||||
| Cobban (2012) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | ||||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Cochrane (2014) | ||||||||||
| Complete | Systematic review | Includes 65+ | 50%‐75% female included | Care dependent | European | High‐income economies | Rehabilitation services | |||
| Visiting health professionals | ||||||||||
| Corrieri (2011) | ||||||||||
| Complete | Systematic review | Includes 65+ | European | High‐income economies | General health services for disease prevention | |||||
| Health promotion services | ||||||||||
| Visiting health professionals | ||||||||||
| Crocker (2013) | ||||||||||
| Complete | Systematic review | Includes <65 | Care dependent | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Daniels (2008) | ||||||||||
| Complete | Systematic review | Includes 75+ | Physical frailty | European | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Davis (2015) | ||||||||||
| Complete | Systematic review | Includes <65 | End‐of‐life | The Americas | High‐income economies | Long term care services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| De Coninck (2017) | ||||||||||
| Complete | Systematic review | Includes <65 | Injury | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Noncommunicable disease | Long term care services | ||||||||
| de Vries (2012) | ||||||||||
| Complete | Systematic review | Includes 65+ | Physical frailty | European | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Desheng (2018) | ||||||||||
| Complete | Systematic review | Includes 65+ | Injury | Western Pacific | Upper‐middle‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Dickens (2011) | ||||||||||
| Complete | Systematic review | Includes <65 | Social isolation | European | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Eklund (2009) | ||||||||||
| Complete | Systematic review | Includes 65+ | Physical frailty | European | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Elkan (2001) | ||||||||||
| Complete | Systematic review | Includes 65+ | Physical frailty | European | High‐income economies | Family and caregiver support | General health services for disease prevention | |||
| Health promotion services | ||||||||||
| Visiting health professionals | ||||||||||
| Evans (2003) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | European | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Fletcher‐Smith (2013) | ||||||||||
| Complete | Systematic review | Includes <65 | Noncommunicable disease | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Fomiatti (2013) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | Western Pacific | High‐income economies | Personal mobility and transportation devices | ||||
| Forbes (2015) | ||||||||||
| Complete | Systematic review | Includes 65+ | Dementia | The Americas | High‐income economies | Rehabilitation services | ||||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Franck (2016) | ||||||||||
| Complete | Systematic review | Includes <65 | Social isolation | Western Pacific | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Rehabilitation services | |||||||||
| Visiting health professionals | ||||||||||
| Gillespie (2012) | ||||||||||
| Complete | Systematic review | Includes <65 | 50%‐75% female included | Injury | European | High‐income economies | Personal mobility and transportation devices | Rehabilitation services | ||
| Includes 65+ | Visiting health professionals | |||||||||
| Gine‐Garriga (2014) | ||||||||||
| Complete | Systematic review | Includes <65 | Physical frailty | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Golding‐Day (2017) | ||||||||||
| Complete | Systematic review | Includes <65 | Physical frailty | European | High‐income economies | Personal care | Visiting health professionals | |||
| Includes 65+ | ||||||||||
| Gomes (2013) | ||||||||||
| Complete | Systematic review | Includes <65 | End‐of‐life | European | High‐income economies | Long term care services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Grant (2014) | ||||||||||
| Complete | Systematic review | Includes 65+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Graybill (2014) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | European | High‐income economies | |||||
| Physical frailty | ||||||||||
| Hall (2011) | ||||||||||
| Complete | Systematic review | Includes 75+ | 75%‐100% female included | End‐of‐life | European | High‐income economies | Long term care services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Handoll (2009) | ||||||||||
| Complete | Systematic review | Includes 65+ | Injury | European | High‐income economies | Rehabilitation services | ||||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Handoll (2015) | ||||||||||
| Complete | Systematic review | Includes <65 | 50%‐75% female included | Injury | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Hill (2015) | ||||||||||
| Complete | Systematic review | Includes <65 | Injury | Western Pacific | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Hobbs (2013) | ||||||||||
| Complete | Systematic review | Includes <65 | Noncommunicable disease | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Howe (2011) | ||||||||||
| Complete | Systematic review | Includes <65 | Physical frailty | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Hunter (2018) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Huss (2008) | ||||||||||
| Complete | Systematic review | Includes 65+ | European | High‐income economies | General health services for disease prevention | |||||
| Visiting health professionals | ||||||||||
| Jane (2017) | ||||||||||
| Complete | Systematic review | Includes 65+ | Care dependent | European | High‐income economies | |||||
| Noncommunicable disease | ||||||||||
| Kang‐Yi (2010) | ||||||||||
| Complete | Systematic review | Includes 65+ | Care dependent | The Americas | High‐income economies | Rehabilitation services | ||||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Konno (2011) | ||||||||||
| On‐going | Systematic review | Includes <65 | Dementia | Western Pacific | High‐income economies | Personal care | Visiting health professionals | |||
| Includes 65+ | Noncommunicable disease | |||||||||
| Konno (2013) | ||||||||||
| Complete | Systematic review | Dementia | Western Pacific | High‐income economies | Personal care | Visiting health professionals | ||||
| Noncommunicable disease | ||||||||||
| Konno (2014) | ||||||||||
| Complete | Systematic review | Includes <65 | Care dependent | Western Pacific | High‐income economies | Personal care | ||||
| Includes 65+ | Dementia | |||||||||
| Noncommunicable disease | ||||||||||
| Kurz (2011) | ||||||||||
| Complete | Systematic review | Includes <65 | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Rehabilitation services | |||||||||
| Visiting health professionals | ||||||||||
| Lacroix (2017) | ||||||||||
| Complete | Systematic review | Includes 65+ | European | High‐income economies | Rehabilitation services | |||||
| Visiting health professionals | ||||||||||
| Legg (2004) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | European | High‐income economies | Rehabilitation services | ||||
| Legg (2017) | ||||||||||
| Complete | Systematic review | Includes <65 | Noncommunicable disease | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Lewis (2017) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | Western Pacific | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Liimatta (2016) | ||||||||||
| Complete | Systematic review | Includes 65+ | 50%‐75% female included | Physical frailty | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Liu (2015) | ||||||||||
| Complete | Systematic review | Includes 65+ | Dementia | The Americas | High‐income economies | Personal care | ||||
| Noncommunicable disease | ||||||||||
| Liu (2018) | ||||||||||
| Complete | Systematic review | Includes 65+ | Care dependent | The Americas | High‐income economies | Rehabilitation services | ||||
| Discharged from hospital | Visiting health professionals | |||||||||
| Injury | ||||||||||
| Physical frailty | ||||||||||
| Low (2011) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | Western Pacific | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Martin (2011) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | ||||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Mayo‐Wilson (2014) | ||||||||||
| Complete | Systematic review | Includes 65+ | European | High‐income economies | General health services for disease prevention | |||||
| Visiting health professionals | ||||||||||
| McClure (2005) | ||||||||||
| Complete | Systematic review | Includes 65+ | Injury | Western Pacific | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| McWilliam (2000) | ||||||||||
| Complete | Systematic review | Includes 65+ | The Americas | High‐income economies | Personal mobility and transportation devices | General health services for disease prevention | ||||
| Health promotion services | ||||||||||
| Rehabilitation services | ||||||||||
| Visiting health professionals | ||||||||||
| Meinck (2004) | ||||||||||
| Complete | Systematic review | Includes <65 | European | High‐income economies | General health services for disease prevention | |||||
| Includes 65+ | Visiting health professionals | |||||||||
| Montgomery (2008) | ||||||||||
| Complete | Systematic review | Includes 65+ | Care dependent | European | High‐income economies | Personal care | ||||
| Munk (2016) | ||||||||||
| Complete | Systematic review | Includes <65 | Physical frailty | European | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Oliver (2007) | ||||||||||
| Complete | Systematic review | Injury | European | High‐income economies | General health services for disease prevention | |||||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Outpatient (2003) | ||||||||||
| Complete | Systematic review | Includes <65 | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Ozdemir (2017) | ||||||||||
| Complete | Systematic review | Includes <65 | Discharged from hospital | European | Lower‐middle‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Patterson (1999) | ||||||||||
| Complete | Systematic review | Includes 65+ | Discharged from hospital | European | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Pitkala (2013) | ||||||||||
| Complete | Systematic review | Includes 75+ | 50%‐75% female included | Dementia | European | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Poscia (2018) | ||||||||||
| Complete | Systematic review | Includes 65+ | 50%‐75% female included | Social isolation | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Potter (2011) | ||||||||||
| Complete | Systematic review | Includes <65 | Dementia | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Noncommunicable disease | |||||||||
| Reilly (2015) | ||||||||||
| Complete | Systematic review | Includes <65 | Dementia | European | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Renz (2017) | ||||||||||
| Complete | Systematic review | Includes <65 | European | High‐income economies | General health services for disease prevention | |||||
| Includes 65+ | Visiting health professionals | |||||||||
| Resnick (2016) | ||||||||||
| Complete | Systematic review | Includes 65+ | Injury | The Americas | High‐income economies | Rehabilitation services | ||||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Roe (2015) | ||||||||||
| Complete | Systematic review | Includes <65 | Noncommunicable disease | European | High‐income economies | Personal care | Health promotion services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Roets‐Merken (2015) | ||||||||||
| Complete | Systematic review | Includes <65 | Care dependent | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Santomassino (2012) | ||||||||||
| Complete | Systematic review | Includes <65 | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Sean (2014) | ||||||||||
| Complete | Systematic review | Includes 65+ | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Shaw (2009) | ||||||||||
| Complete | Systematic review | Includes 65+ | 50%‐75% female included | Physical frailty | European | High‐income economies | Family and caregiver support | |||
| Shepperd (2005) | ||||||||||
| Complete | Systematic review | Includes 65+ | Discharged from hospital | European | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Shepperd (2011) | ||||||||||
| Complete | Systematic review | Includes <65 | End‐of‐life | European | High‐income economies | Long term care services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Shepperd (2016) | ||||||||||
| Complete | Systematic review | Includes <65 | European | High‐income economies | General health services for disease prevention | |||||
| Includes 65+ | Visiting health professionals | |||||||||
| Shvedko (2018) | ||||||||||
| Complete | Systematic review | Includes <65 | 50%‐75% female included | Noncommunicable disease | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Visiting health professionals | |||||||||
| Simek (2012) | ||||||||||
| Complete | Systematic review | Includes <65 | Injury | Western Pacific | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Sims‐Gould (2017) | ||||||||||
| Complete | Systematic review | Includes 65+ | 50%‐75% female included | Care dependent | The Americas | High‐income economies | Rehabilitation services | |||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Physical frailty | ||||||||||
| Skelton (2013) | ||||||||||
| Complete | Systematic review | Includes <65 | Noncommunicable disease | European | High‐income economies | |||||
| Includes 65+ | ||||||||||
| Smeeth (2006) | ||||||||||
| Complete | Systematic review | Includes 65+ | European | High‐income economies | General health services for disease prevention | |||||
| Visiting health professionals | ||||||||||
| Smith (2016) | ||||||||||
| Complete | Systematic review | Includes <65 | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | ||||||||||
| Stall (2014) | ||||||||||
| Complete | Systematic review | Includes 65+ | Care dependent | The Americas | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Steultjens (2004) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | European | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Steultjens (2004) | ||||||||||
| Complete | Systematic review | Includes <65 | European | High‐income economies | Rehabilitation services | |||||
| Includes 65+ | Visiting health professionals | |||||||||
| Stolee (2012) | ||||||||||
| Complete | Systematic review | Includes <65 | Noncommunicable disease | The Americas | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| Stuck (2002) | ||||||||||
| Complete | Systematic review | Includes 65+ | European | High‐income economies | General health services for disease prevention | |||||
| Visiting health professionals | ||||||||||
| Talley (2011) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Tappenden (2012) | ||||||||||
| Complete | Systematic review | Includes 75+ | Physical frailty | European | High‐income economies | Health promotion services | ||||
| Visiting health professionals | ||||||||||
| Therapy‐based rehabilitation (2003) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | European | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Thiebaud (2014) | ||||||||||
| Complete | Systematic review | Includes 75+ | 50%‐75% female included | The Americas | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Toles (2016) | ||||||||||
| Complete | Systematic review | Includes 75+ | 50%‐75% female included | Discharged from hospital | The Americas | High‐income economies | General health services for disease prevention | |||
| Visiting health professionals | ||||||||||
| Tseng (2011) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | Western Pacific | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Vaapio (2009) | ||||||||||
| Complete | Systematic review | Includes <65 | Injury | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals | |||||||||
| van Abbema (2015) | ||||||||||
| Complete | Systematic review | Includes 65+ | Physical frailty | European | High‐income economies | Rehabilitation services | ||||
| Visiting health professionals | ||||||||||
| Van Citters (2004) | ||||||||||
| Complete | Systematic review | Includes 65+ | Noncommunicable disease | The Americas | High‐income economies | General health services for disease prevention | ||||
| Visiting health professionals | ||||||||||
| Ward (2003) | ||||||||||
| Complete | Systematic review | Includes <65 | Care dependent | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Watanabe (2015) | ||||||||||
| On‐going | Systematic review | Includes <65 | Noncommunicable disease | Western Pacific | High‐income economies | Personal mobility and transportation devices | ||||
| Includes 65+ | ||||||||||
| Weber (2018) | ||||||||||
| Complete | Systematic review | Includes <65 | 50%‐75% female included | Care dependent | European | High‐income economies | Rehabilitation services | |||
| Includes 65+ | Injury | Visiting health professionals | ||||||||
| Winkel (2008) | ||||||||||
| Complete | Systematic review | Includes <65 | Noncommunicable disease | European | High‐income economies | General health services for disease prevention | ||||
| Includes 65+ | Rehabilitation services | |||||||||
| Yi (2015) | ||||||||||
| On‐going | Systematic review | Includes <65 | Dementia | Western Pacific | High‐income economies | Personal care | General health services for disease prevention | |||
| Includes 65+ | Noncommunicable disease | Visiting health professionals | ||||||||
| Young (2017) | ||||||||||
| Complete | Systematic review | Includes 65+ | Care dependent | European | High‐income economies | Long term care services | ||||
| Noncommunicable disease | Visiting health professionals | |||||||||
| Zhu (2013) | ||||||||||
| Complete | Systematic review | Includes <65 | Care dependent | The Americas | High‐income economies | Personal care | ||||
| Includes 65+ | Noncommunicable disease | |||||||||
| Zubala (2017) | ||||||||||
| Complete | Systematic review | Includes <65 | 50%‐75% female included | European | High‐income economies | Rehabilitation services | ||||
| Includes 65+ | Visiting health professionals |
| Study | Intervention: design, construction and building products and technology of buildings for private use | Outcomes: intrinsic capacity | Outcomes: functional ability | Outcomes: process and other outcomes | Setting | Comparison | PROGRESS factors | Gender inequalities | Other health inequalities | Study quality |
|---|---|---|---|---|---|---|---|---|---|---|
| Acton (2016) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Sensory functions and pain | Quality of life | |||||||||
| Aimonino (2008) | ||||||||||
| Mental functions | Basic needs | Cost (e.g.,out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Functions of the digestive, metabolic and endocrine systems | Quality of life | Satisfaction of older adult | ||||||||
| Mobility | Caregiver outcomes | |||||||||
| Health service utilization | ||||||||||
| Alexander (2001) | ||||||||||
| Mobility | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Alexopoulos (2016) | ||||||||||
| Mental functions | Learning, grow and make decisions | Residential home/apartment | Other | Socioeconomic status | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Amjad (2018) | ||||||||||
| Quality of life | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Health service utilization | Independent living | |||||||||
| Andersen (2000) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Mobility | |||||||||
| Anonymous (2004) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Usual care | Social capital | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Araujo (2015) | ||||||||||
| Basic needs | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | Health service utilization | |||||||||
| Mobility | ||||||||||
| Arean (2015) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Other | Socioeconomic status | No ‐ assessment of effects by sex/gender NOT present | Yes ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Mobility | ||||||||||
| Arrieta (2018) | ||||||||||
| Mental functions | Basic needs | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Quality of life | |||||||||
| Mobility | ||||||||||
| Contribution | ||||||||||
| Financial security and stability | ||||||||||
| Ashburn (2007) | ||||||||||
| Basic needs | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | ||||||||||
| Avlund (2002) | ||||||||||
| Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Mobility | ||||||||||
| Baker (2007) | ||||||||||
| Neuromusculoskeletal function | Mobility | Independent living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Banerjee (1996) | ||||||||||
| Mental functions | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Barnes (2017) | ||||||||||
| Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Quality of life | ||||||||||
| Mobility | ||||||||||
| Barreto (2018) | ||||||||||
| Neuromusculoskeletal function | Mobility | Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Batchelor‐Murphy (2017) | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | Basic needs | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Beck (2013) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Mobility | |||||||||
| Contribution | ||||||||||
| Beck (2016) | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Quality of life | Assisted living | ||||||||
| Mobility | ||||||||||
| Behm (2014) | ||||||||||
| Mental functions | Quality of life | Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | ||||||||||
| Neuromusculoskeletal function | ||||||||||
| Behm (2016) | ||||||||||
| Mental functions | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Sensory functions and pain | ||||||||||
| Neuromusculoskeletal function | ||||||||||
| Beland (2006) | ||||||||||
| Mental functions | Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Mobility | Satisfaction of older adult | |||||||||
| Cost‐effectiveness | ||||||||||
| Health service utilization | ||||||||||
| Bennell (2018) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Sensory functions and pain | ||||||||||
| Bernabei (1998) | ||||||||||
| Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | Health service utilization | |||||||||
| Bjerk (2017) | ||||||||||
| Neuromusculoskeletal function | Quality of life | Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Mobility | Falls | |||||||||
| Blanchard (1999) | ||||||||||
| Mental functions | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Bleijenberg (2016) | ||||||||||
| Basic needs | Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | Caregiver outcomes | |||||||||
| Health service utilization | ||||||||||
| Bonnefoy (2012) | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | Basic needs | Adherence | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Mobility | Safety | ||||||||
| Boongird (2017) | ||||||||||
| Mental functions | Quality of life | Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Falls | |||||||||
| Bouman (2008) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | ||||||||||
| Boxall (2005) | ||||||||||
| Mental functions | Quality of life | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Mobility | |||||||||
| Neuromusculoskeletal function | ||||||||||
| Brannstrom (2014) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Quality of life | |||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Mobility | |||||||||
| Brettschneider (2014) | ||||||||||
| Mental functions | Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Quality of life | Health service utilization | ||||||||
| Brovold (2012) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Sensory functions and pain | Mobility | |||||||||
| Neuromusculoskeletal function | Build and maintain relationships | |||||||||
| Bruce (2015) | ||||||||||
| Mental functions | Mobility | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Bruce (2016) | ||||||||||
| Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Brumley (2007) | ||||||||||
| Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Satisfaction of older adult | ||||||||||
| Burton (2013) | ||||||||||
| Mental functions | Basic needs | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Mobility | |||||||||
| Buurman (2016) | ||||||||||
| Quality of life | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | Health service utilization | Assisted living | ||||||||
| Buys (2017) | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Access | ||||||||||
| Health service utilization | ||||||||||
| Byles (2004) | ||||||||||
| Mental functions | Quality of life | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Contribution | |||||||||
| Neuromusculoskeletal function | ||||||||||
| Byrnes (2015) | ||||||||||
| Quality of life | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Cost‐effectiveness | ||||||||||
| Health service utilization | ||||||||||
| Callahan (2012) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | ||||||||||
| Campbell (1997) | ||||||||||
| Neuromusculoskeletal function | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Campbell (2005) | ||||||||||
| Adaptations to physical environment | Cost‐effectiveness | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Falls | ||||||||||
| Canning (2015) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Caplan (1999) | ||||||||||
| Mental functions | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Functions of the digestive, metabolic and endocrine systems | Caregiver outcomes | |||||||||
| Genitourinary and reproductive functions | Safety | |||||||||
| Integumentary system | Health service utilization | |||||||||
| Falls | ||||||||||
| Caplan (2004) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Caplan (2006) | ||||||||||
| Mental functions | Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Cost‐effectiveness | ||||||||||
| Health service utilization | ||||||||||
| Carroll (2007) | ||||||||||
| Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Health service utilization | ||||||||||
| Chaiyawat (2012) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | ||||||||||
| Chan et al. (2016) | ||||||||||
| Learning, grow and make decisions | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Chandler (1998) | ||||||||||
| Mental functions | Mobility | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | ||||||||||
| Chang (2015) | ||||||||||
| Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Mobility | ||||||||||
| Chee (2013) | ||||||||||
| Adaptations to physical environment | Mental functions | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Chen (2015) | ||||||||||
| Mental functions | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Chen (2015) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | ||||||||||
| Chen (2016) | ||||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Basic needs | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Mobility | |||||||||
| Cho (1998) | ||||||||||
| Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Chow (2014) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Quality of life | |||||||||
| Chu (2017) | ||||||||||
| Adaptations to physical environment | Mental functions | Basic needs | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||
| Falls | ||||||||||
| Cichocki (2015) | ||||||||||
| Mental functions | Quality of life | Satisfaction of older adult | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Mobility | |||||||||
| Neuromusculoskeletal function | Build and maintain relationships | |||||||||
| Ciechanowski (2004) | ||||||||||
| Mental functions | Quality of life | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Health service utilization | ||||||||||
| Claffey (1976) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Clegg (2014) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | ||||||||||
| Mobility | ||||||||||
| Clemson (2016) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Comans (2010) | ||||||||||
| Mental functions | Basic needs | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Quality of life | |||||||||
| Functions of the digestive, metabolic and endocrine systems | Contribution | |||||||||
| Genitourinary and reproductive functions | ||||||||||
| Neuromusculoskeletal function | ||||||||||
| Conradsson (2010) | ||||||||||
| Mental functions | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Cornu (2003) | ||||||||||
| Basic needs | Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Health service utilization | ||||||||||
| Corr (1995) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Counsell (2007) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | Race, ethnicity, culture, language | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||
| Sensory functions and pain | Socioeconomic status | |||||||||
| Courtney (2009) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | ||||||||||
| Courtney (2011) | ||||||||||
| Mental functions | Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Health service utilization | ||||||||||
| Courtney (2012) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | ||||||||||
| Contribution | ||||||||||
| Crotty (2002) | ||||||||||
| Mental functions | Quality of life | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Caregiver outcomes | ||||||||||
| Health service utilization | ||||||||||
| Falls | ||||||||||
| Crotty (2003) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | ||||||||||
| Mobility | ||||||||||
| Crotty (2008) | ||||||||||
| Mental functions | Basic needs | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | ||||||||||
| Cumming (2000) | ||||||||||
| Mental functions | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Cummings (1990) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Cost‐effectiveness | ||||||||||
| Caregiver outcomes | ||||||||||
| Health service utilization | ||||||||||
| Cunliffe (2004) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Communication | |||||||||
| Functions of the digestive, metabolic and endocrine systems | ||||||||||
| Neuromusculoskeletal function | ||||||||||
| Cutchin (2009) | ||||||||||
| Mental functions | Contribution | Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Cost‐effectiveness | |||||||||
| Health service utilization | ||||||||||
| Dalby (2000) | ||||||||||
| Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Daly (2015) | ||||||||||
| Mental functions | Basic needs | Adherence | Independent living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Functions of the digestive, metabolic and endocrine systems | Quality of life | Cost‐effectiveness | ||||||||
| Neuromusculoskeletal function | Mobility | Safety | ||||||||
| Falls | ||||||||||
| Danilovich et al. (2017) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | Caregiver outcomes | |||||||||
| Contribution | ||||||||||
| Dano (2016) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | ||||||||||
| Dechamps (2010) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Long‐term care | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Assisted living | ||||||||||
| Di Monaco (2008) | ||||||||||
| Basic needs | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Di Pollina (2017) | ||||||||||
| Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Falls | ||||||||||
| Dias (2008) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Donald (1995) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Genitourinary and reproductive functions | ||||||||||
| Neuromusculoskeletal function | ||||||||||
| Donat (2007) | ||||||||||
| Mental functions | Mobility | Independent living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Sensory functions and pain | ||||||||||
| Neuromusculoskeletal function | ||||||||||
| Dorner (2013) | ||||||||||
| Mental functions | Quality of life | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Mobility | |||||||||
| Dorresteijn (2016) | ||||||||||
| Basic needs | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Dow (2013) | ||||||||||
| Mental functions | Cost‐effectiveness | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Caregiver outcomes | |||||||||
| Health service utilization | ||||||||||
| Draper (2008) | ||||||||||
| Mental functions | Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Caregiver outcomes | ||||||||||
| Draper (2016) | ||||||||||
| Sensory functions and pain | Mobility | Residential home/apartment | Usual care | Race, ethnicity, culture, language | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Duffy (2010) | ||||||||||
| Quality of life | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Satisfaction of older adult | ||||||||||
| Health service utilization | ||||||||||
| Edgren (2015) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | ||||||||||
| Mobility | ||||||||||
| Eloniemi‐Sulkava (2001) | ||||||||||
| Mental functions | Caregiver outcomes | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Health service utilization | ||||||||||
| Eloniemi‐Sulkava (2009) | ||||||||||
| Mental functions | Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Cost‐effectiveness | ||||||||||
| Caregiver outcomes | ||||||||||
| Health service utilization | ||||||||||
| Engberg (2016) | ||||||||||
| Genitourinary and reproductive functions | Quality of life | Adherence | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Enguidanos (2012) | ||||||||||
| Basic needs | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Health service utilization | ||||||||||
| Eriksen (2016) | ||||||||||
| Mental functions | Quality of life | Adherence | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Functions of the digestive, metabolic and endocrine systems | Mobility | |||||||||
| Neuromusculoskeletal function | ||||||||||
| Fabacher (1994) | ||||||||||
| Sensory functions and pain | Basic needs | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | ||||||||||
| Neuromusculoskeletal function | ||||||||||
| Faber (2006) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Mobility | Assisted living | |||||||||
| Fahlström (2018) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | Falls | |||||||||
| Mobility | ||||||||||
| Fairhall (2012) | ||||||||||
| Mental functions | Mobility | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | ||||||||||
| Fairhall (2014) | ||||||||||
| Adaptations to physical environment | Sensory functions and pain | Mobility | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||
| Neuromusculoskeletal function | ||||||||||
| Fairhall et al. (2015) | ||||||||||
| Adaptations to physical environment | Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||
| Neuromusculoskeletal function | Quality of life | Falls | ||||||||
| Mobility | ||||||||||
| Fairhall (2017) | ||||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Mobility | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | ||||||||||
| Farag (2015) | ||||||||||
| Neuromusculoskeletal function | Quality of life | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Mobility | Falls | |||||||||
| Farag (2016) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Health service utilization | ||||||||||
| Fasce (2018) | ||||||||||
| Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Favela (2013) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | ||||||||||
| Mobility | ||||||||||
| Feldman (2004) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | Health service utilization | |||||||||
| Ferrer (2014) | ||||||||||
| Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Ferrer‐Garcia (2011) | ||||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Quality of life | Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Fiatarone (1994) | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | Mobility | Long‐term care | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | ||||||||||
| Finnema (2005) | ||||||||||
| Mental functions | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Fleming (2004) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Long‐term care | ||||||||||
| Flood (2005) | ||||||||||
| Adaptations to physical environment | Quality of life | Cost‐effectiveness | Residential home/apartment | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Fontan (2010) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | ||||||||||
| Build and maintain relationships | ||||||||||
| Forsberg (2011) | ||||||||||
| Sensory functions and pain | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Quality of life | Falls | ||||||||
| Forster (1996) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Mobility | |||||||||
| Genitourinary and reproductive functions | Contribution | |||||||||
| Frese (2012) | ||||||||||
| Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Friedman (2014) | ||||||||||
| Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Gagnon (1999) | ||||||||||
| Basic needs | Caregiver outcomes | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | Health service utilization | |||||||||
| Garcia‐Pena (2001) | ||||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Garcia‐Pena (2002) | ||||||||||
| Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Cost‐effectiveness | ||||||||||
| Gawler (2016) | ||||||||||
| Neuromusculoskeletal function | Mobility | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Giangregorio (2018) | ||||||||||
| Neuromusculoskeletal function | Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Falls | ||||||||||
| Gill (2002) | ||||||||||
| Adaptations to physical environment | Mental functions | Mobility | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Gill (2004) | ||||||||||
| Basic needs | Residential home/apartment | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||||
| Mobility | ||||||||||
| Gitlin (2001) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Gitlin (2006) | ||||||||||
| Adaptations to physical environment | Mental functions | Basic needs | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | ||||||||||
| Gitlin (2008) | ||||||||||
| Mental functions | Quality of life | Caregiver outcomes | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Genitourinary and reproductive functions | ||||||||||
| Gitlin (2009) | ||||||||||
| Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | Yes ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||||
| Gitlin (2010) | ||||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Quality of life | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Genitourinary and reproductive functions | ||||||||||
| Gitlin (2014) | ||||||||||
| Mental functions | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Gitlin (2018) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | ||||||||||
| Gladman (1993) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Mobility | Health service utilization | ||||||||
| Contribution | ||||||||||
| Godwin (2016) | ||||||||||
| Mental functions | Quality of life | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Contribution | Access | ||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Health service utilization | |||||||||
| Functions of the digestive, metabolic and endocrine systems | ||||||||||
| Genitourinary and reproductive functions | ||||||||||
| Neuromusculoskeletal function | ||||||||||
| Gozalo (2014) | ||||||||||
| Mental functions | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Graff (2008) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Granbom (2017) | ||||||||||
| Contribution | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Build and maintain relationships | ||||||||||
| Graves (2009) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Grimmer (2013) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | Falls | |||||||||
| Mobility | ||||||||||
| Gronstedt (2013) | ||||||||||
| Neuromusculoskeletal function | Mobility | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Gustafsson (2012) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Mobility | |||||||||
| Haastregt (2000) | ||||||||||
| Mental functions | Basic needs | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Mobility | ||||||||||
| Contribution | ||||||||||
| Haider (2017) | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | Mobility | Adherence | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Safety | |||||||||
| Haider (2017) | ||||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Mobility | Adherence | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Functions of the digestive, metabolic and endocrine systems | ||||||||||
| Neuromusculoskeletal function | ||||||||||
| Hall (1992) | ||||||||||
| Mental functions | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Hammar (2009) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Hansen (1992) | ||||||||||
| Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Hansen (1995) | ||||||||||
| Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Harris (2005) | ||||||||||
| Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Cost‐effectiveness | ||||||||||
| Harvey (2014) | ||||||||||
| Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Health service utilization | ||||||||||
| Hauer (2017) | ||||||||||
| Neuromusculoskeletal function | Mobility | Falls | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Helbostad (2004) | ||||||||||
| Neuromusculoskeletal function | Mobility | Adherence | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Falls | ||||||||||
| Hendriks (2008) | ||||||||||
| Mental functions | Basic needs | Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | Falls | |||||||||
| Contribution | ||||||||||
| Herfjord (2014) | ||||||||||
| Sensory functions and pain | Basic needs | Cost‐effectiveness | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | Health service utilization | |||||||||
| Hewitt (2018) | ||||||||||
| Mental functions | Quality of life | Falls | Long‐term care | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Mobility | |||||||||
| Hinrichs (2015) | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | Mobility | Safety | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Hinrichs (2016) | ||||||||||
| Neuromusculoskeletal function | Mobility | Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Safety | ||||||||||
| Hoenig (2015) | ||||||||||
| Mental functions | Mobility | Safety | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | ||||||||||
| Holland (2005) | ||||||||||
| Quality of life | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Holland (2017) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Quality of life | |||||||||
| Mobility | ||||||||||
| Houles (2010) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | ||||||||||
| Mobility | ||||||||||
| Hsu (2016) | ||||||||||
| Mental functions | Long‐term care | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Hsu (2016) | ||||||||||
| Mental functions | Quality of life | Long‐term care | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Huang (1998) | ||||||||||
| Mental functions | Safety | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Falls | ||||||||||
| Huang (2013) | ||||||||||
| Mental functions | Caregiver outcomes | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Hughes (1992) | ||||||||||
| Basic needs | Cost (e.g., out of pocket) | Long‐term care | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Cost‐effectiveness | Independent living | |||||||||
| Caregiver outcomes | ||||||||||
| Health service utilization | ||||||||||
| Hughes (2000) | ||||||||||
| Mental functions | Quality of life | Satisfaction of older adult | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Cost‐effectiveness | ||||||||||
| Caregiver outcomes | ||||||||||
| Hunger (2015) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | ||||||||||
| Wang et al. (2016) | ||||||||||
| Mental functions | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | ||||||||||
| Iliffe (2014) | ||||||||||
| Neuromusculoskeletal function | Quality of life | Cost (e.g., out of pocket) | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Imhof (2012) | ||||||||||
| Quality of life | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Falls | ||||||||||
| Inglis (2006) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Health service utilization | ||||||||||
| Isrctn (2018) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Quality of life | |||||||||
| Build and maintain relationships | ||||||||||
| Jakobsen (2007) | ||||||||||
| Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Cost‐effectiveness | ||||||||||
| Health service utilization | ||||||||||
| Jensen (2002) | ||||||||||
| Adaptations to physical environment | Falls | Long‐term care | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Jingna (2012) | ||||||||||
| Mental functions | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Joaquim (2017) | ||||||||||
| Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Johansson (2001) | ||||||||||
| Mental functions | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Johansson (2003) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Health service utilization | ||||||||||
| Jolly (2009) | ||||||||||
| Mental functions | Cost‐effectiveness | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Health service utilization | |||||||||
| Kalra (2000) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Kane (1984) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Learning, grow and make decisions | Caregiver outcomes | Long‐term care | |||||||
| Kanemaru (2010) | ||||||||||
| Neuromusculoskeletal function | Quality of life | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Kapan (2017) | ||||||||||
| Mental functions | Basic needs | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Mobility | |||||||||
| Kapan (2017) | ||||||||||
| Quality of life | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Karinkanta (2007) | ||||||||||
| Neuromusculoskeletal function | Mobility | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Karlsson (2016) | ||||||||||
| Mobility | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Kerr (2018) | ||||||||||
| Mental functions | Quality of life | Independent living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Sensory functions and pain | Mobility | |||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | ||||||||||
| Kerse (2010) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | ||||||||||
| Kim (2011) | ||||||||||
| Neuromusculoskeletal function | Quality of life | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | ||||||||||
| King et al. (2012) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | ||||||||||
| King et al. (2012) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | ||||||||||
| Kjerstad (2016) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Klug (2011) | ||||||||||
| Mental functions | Quality of life | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Kocic (2018) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Kohei (2016) | ||||||||||
| Neuromusculoskeletal function | Quality of life | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | ||||||||||
| Kono (2004) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Kono (2012) | ||||||||||
| Mental functions | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Kono (2013) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Health service utilization | ||||||||||
| Kono (2014) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | Health service utilization | |||||||||
| Falls | ||||||||||
| Kono (2016) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Health service utilization | ||||||||||
| Falls | ||||||||||
| Kronborg (2006) | ||||||||||
| Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Kukkonen‐Harjula (2018) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Quality of life | |||||||||
| Kwok (2004) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Health service utilization | |||||||||
| Kwok (2016) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Sensory functions and pain | Quality of life | |||||||||
| Mobility | ||||||||||
| Kyrdalen (2014) | ||||||||||
| Mental functions | Quality of life | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Mobility | |||||||||
| Lam (2018) | ||||||||||
| Neuromusculoskeletal function | Mobility | Falls | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Lannin (2007) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | Falls | |||||||||
| Mobility | ||||||||||
| Latham (2014) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Adherence | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Mobility | Safety | |||||||||
| Falls | ||||||||||
| Latour (2007) | ||||||||||
| Mental functions | Quality of life | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Health service utilization | ||||||||||
| Lattanzio (2001) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Quality of life | |||||||||
| Leavitt (2018) | ||||||||||
| Quality of life | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Learning, grow and make decisions | Health service utilization | |||||||||
| Lee (2006) | ||||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Mobility | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Lenaghan (2007) | ||||||||||
| Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Levine (2012) | ||||||||||
| Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Cost‐effectiveness | ||||||||||
| Health service utilization | ||||||||||
| Lewin (2013) | ||||||||||
| Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Quality of life | ||||||||||
| Lewin (2014) | ||||||||||
| Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Health service utilization | ||||||||||
| Li (2013) | ||||||||||
| Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Li (2015) | ||||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Quality of life | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | ||||||||||
| Liang (1984) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | Falls | |||||||||
| Mobility | ||||||||||
| Liang (1986) | ||||||||||
| Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | Health service utilization | |||||||||
| Falls | ||||||||||
| Liddle (1996) | ||||||||||
| Adaptations to physical environment | Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||
| Quality of life | ||||||||||
| Mobility | ||||||||||
| Liimatta (2017) | ||||||||||
| Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Lin (2007) | ||||||||||
| Mental functions | Basic needs | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Quality of life | |||||||||
| Mobility | ||||||||||
| Lin (2010) | ||||||||||
| Mental functions | Basic needs | Long‐term care | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Functions of the digestive, metabolic and endocrine systems | ||||||||||
| Lindegaard (2017) | ||||||||||
| Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Lindegaard‐Pedersen (2015) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Quality of life | |||||||||
| Liu and Lai (2014) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Liu (2015) | ||||||||||
| Mental functions | Basic needs | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | ||||||||||
| Locher (2013) | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Logan (2004) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Mobility | ||||||||||
| Contribution | ||||||||||
| Lok (2017) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Sensory functions and pain | ||||||||||
| Luck (2013) | ||||||||||
| Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Falls | ||||||||||
| Lyons (2016) | ||||||||||
| Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Mobility | ||||||||||
| Learning, grow and make decisions | ||||||||||
| Build and maintain relationships | ||||||||||
| MacIntyre (1999) | ||||||||||
| Mental functions | Quality of life | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Build and maintain relationships | |||||||||
| Mahoney (2007) | ||||||||||
| Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Falls | ||||||||||
| Maiers (2014) | ||||||||||
| Mental functions | Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Sensory functions and pain | ||||||||||
| Neuromusculoskeletal function | ||||||||||
| Mangione (2005) | ||||||||||
| Mental functions | Mobility | Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | ||||||||||
| Mangione et al. (2010) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | ||||||||||
| Mann (1999) | ||||||||||
| Adaptations to physical environment | Mental functions | Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||
| Sensory functions and pain | Mobility | Cost‐effectiveness | ||||||||
| Contribution | ||||||||||
| Build and maintain relationships | ||||||||||
| Marek (2014) | ||||||||||
| Mental functions | Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Quality of life | Cost‐effectiveness | ||||||||
| Markle‐Reid (2003) | ||||||||||
| Mental functions | Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Quality of life | Cost‐effectiveness | ||||||||
| Contribution | Caregiver outcomes | |||||||||
| Build and maintain relationships | Health service utilization | |||||||||
| Markle‐Reid (2006) | ||||||||||
| Mental functions | Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Quality of life | |||||||||
| Contribution | ||||||||||
| Markle‐Reid (2010) | ||||||||||
| Mental functions | Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Quality of life | Cost‐effectiveness | ||||||||
| Falls | ||||||||||
| Markle‐Reid et al. (2017) | ||||||||||
| Mental functions | Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Functions of the digestive, metabolic and endocrine systems | Quality of life | Cost‐effectiveness | ||||||||
| Caregiver outcomes | ||||||||||
| Martin (1994) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Maru (2015) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Health service utilization | ||||||||||
| Matzen (2007) | ||||||||||
| Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Health service utilization | Assisted living | |||||||||
| Mayo (2008) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Quality of life | |||||||||
| McCorkle (1989) | ||||||||||
| Mental functions | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Sensory functions and pain | ||||||||||
| McCorkle (2000) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Contribution | ||||||||||
| McMurdo (1995) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | ||||||||||
| Mobility | ||||||||||
| McWilliam (1999) | ||||||||||
| Mental functions | Quality of life | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| McWilliam (1999) | ||||||||||
| Mental functions | Quality of life | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Meisinger (2013) | ||||||||||
| Mental functions | Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Quality of life | Health service utilization | ||||||||
| Melin (1992) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Mobility | ||||||||||
| Contribution | ||||||||||
| Build and maintain relationships | ||||||||||
| Melin (1993) | ||||||||||
| Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Mobility | ||||||||||
| Contribution | ||||||||||
| Melin (1993) | ||||||||||
| Mental functions | Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Mobility | Cost‐effectiveness | |||||||||
| Contribution | Safety | |||||||||
| Build and maintain relationships | Health service utilization | |||||||||
| Melin (1995) | ||||||||||
| Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | Health service utilization | |||||||||
| Melis (2008) | ||||||||||
| Mental functions | Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Assisted living | ||||||||||
| Melis (2008) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | ||||||||||
| Mobility | ||||||||||
| Mihalko (1996) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | ||||||||||
| Miller (2005) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Milte (2016) | ||||||||||
| Quality of life | Cost‐effectiveness | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mitchell (2005) | ||||||||||
| Sensory functions and pain | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Health service utilization | |||||||||
| Mohide (1990) | ||||||||||
| Caregiver outcomes | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Health service utilization | Long‐term care | |||||||||
| Molassiotis (2009) | ||||||||||
| Mental functions | Quality of life | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | ||||||||||
| Moller (2014) | ||||||||||
| Sensory functions and pain | Mobility | Residential home/apartment | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Montgomery (2003) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Mobility | ||||||||||
| Morris (2017) | ||||||||||
| Neuromusculoskeletal function | Quality of life | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Cost‐effectiveness | ||||||||||
| Falls | ||||||||||
| Mortensen (2016) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Contribution | |||||||||
| Mulrow (1994) | ||||||||||
| Mental functions | Basic needs | Falls | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | ||||||||||
| Murphy (2005) | ||||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Quality of life | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Mobility | |||||||||
| Naunton (2003) | ||||||||||
| Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Health service utilization | ||||||||||
| Naylor (1999) | ||||||||||
| Mental functions | Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Satisfaction of older adult | ||||||||||
| Health service utilization | ||||||||||
| Naylor (2004) | ||||||||||
| Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | Satisfaction of older adult | |||||||||
| Health service utilization | ||||||||||
| Naylor (2004) | ||||||||||
| Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | Health service utilization | |||||||||
| Nazareth (2001) | ||||||||||
| Quality of life | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Adherence | ||||||||||
| Health service utilization | ||||||||||
| Nct (2005) | ||||||||||
| Quality of life | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Nct (2006) | ||||||||||
| Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Nct (2011) | ||||||||||
| Quality of life | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Nct (2011) | ||||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Quality of life | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Mobility | Falls | ||||||||
| Nct (2012) | ||||||||||
| Mental functions | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Nct (2013) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Functions of the digestive, metabolic and endocrine systems | Quality of life | |||||||||
| Neuromusculoskeletal function | Build and maintain relationships | |||||||||
| Nct (2014) | ||||||||||
| Sensory functions and pain | Basic needs | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Quality of life | |||||||||
| Nct (2014) | ||||||||||
| Mental functions | Quality of life | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Caregiver outcomes | |||||||||
| Health service utilization | ||||||||||
| Nct (2014) | ||||||||||
| Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Nct (2015) | ||||||||||
| Basic needs | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | ||||||||||
| Nct (2017) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Quality of life | |||||||||
| Functions of the digestive, metabolic and endocrine systems | Mobility | |||||||||
| Learning, grow and make decisions | ||||||||||
| Build and maintain relationships | ||||||||||
| Nct (2017) | ||||||||||
| Mental functions | Basic needs | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Mobility | |||||||||
| Neuromusculoskeletal function | ||||||||||
| Nct (2017) | ||||||||||
| Mental functions | Mobility | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Nct (2017) | ||||||||||
| Mental functions | Quality of life | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Contribution | Long‐term care | |||||||||
| Build and maintain relationships | ||||||||||
| Nct (2018) | ||||||||||
| Mental functions | Quality of life | Safety | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | ||||||||||
| Nct (2018) | ||||||||||
| Neuromusculoskeletal function | Mobility | Adherence | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Cost‐effectiveness | ||||||||||
| Health service utilization | ||||||||||
| Falls | ||||||||||
| Neumann (2017) | ||||||||||
| Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Nicolaides‐Bouman (2004) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | ||||||||||
| Nielsen (1972) | ||||||||||
| Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Nikolaus (1999) | ||||||||||
| Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | Satisfaction of older adult | Long‐term care | ||||||||
| Health service utilization | ||||||||||
| Nikolaus (2003) | ||||||||||
| Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Nobili (2004) | ||||||||||
| Mental functions | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Nowalk (2001) | ||||||||||
| Mental functions | Mobility | Falls | Long‐term care | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | ||||||||||
| Oerkild (2011) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Mobility | |||||||||
| Oerkild (2012) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Quality of life | |||||||||
| Functions of the digestive, metabolic and endocrine systems | Mobility | |||||||||
| Olaleye (2014) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | ||||||||||
| Olesen (2014) | ||||||||||
| Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Health service utilization | ||||||||||
| Olson (2011) | ||||||||||
| Neuromusculoskeletal function | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Oosting (2012) | ||||||||||
| Sensory functions and pain | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Quality of life | Adherence | ||||||||
| Mobility | Safety | |||||||||
| Orrell (2017) | ||||||||||
| Mental functions | Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | Cost‐effectiveness | |||||||||
| Communication | Caregiver outcomes | |||||||||
| Ouslander (2005) | ||||||||||
| Mental functions | Basic needs | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Genitourinary and reproductive functions | Mobility | |||||||||
| Neuromusculoskeletal function | ||||||||||
| Özdemir (2001) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | ||||||||||
| Padala (2017) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Quality of life | |||||||||
| Padula (2009) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Quality of life | |||||||||
| Neuromusculoskeletal function | ||||||||||
| Papaioannou (2003) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Mobility | |||||||||
| Pardessus (2002) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Falls | ||||||||||
| Parker (2009) | ||||||||||
| Mental functions | Basic needs | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | ||||||||||
| Parker (2011) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Health service utilization | ||||||||||
| Parsons et al. (2013) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Parsons (2017) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Quality of life | Health service utilization | ||||||||
| Patterson (2009) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Pedersen (2016) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | ||||||||||
| Peeters (2007) | ||||||||||
| Basic needs | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | ||||||||||
| Pizzi (2014) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Other | Race, ethnicity, culture, language | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Portegijs (2013) | ||||||||||
| Sensory functions and pain | Mobility | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Prick (2015) | ||||||||||
| Mental functions | Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Caregiver outcomes | Other | |||||||||
| Pröfener (2016) | ||||||||||
| Mental functions | Access | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Radwany (2014) | ||||||||||
| Mental functions | Quality of life | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Rasmussen (2016) | ||||||||||
| Mental functions | Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Functions of the digestive, metabolic and endocrine systems | Quality of life | |||||||||
| Neuromusculoskeletal function | Mobility | |||||||||
| Ray (1997) | ||||||||||
| Falls | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Reckrey (2018) | ||||||||||
| Mental functions | Quality of life | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Health service utilization | |||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | ||||||||||
| Reeves (2004) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Quality of life | |||||||||
| Regan (2017) | ||||||||||
| Mental functions | Quality of life | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Caregiver outcomes | ||||||||||
| Resnick (2009) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | ||||||||||
| Mobility | ||||||||||
| Richards (1998) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | Access | |||||||||
| Contribution | ||||||||||
| Robertson et al. (2001) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Falls | ||||||||||
| Roderick (2001) | ||||||||||
| Mental functions | Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | Cost‐effectiveness | |||||||||
| Mobility | ||||||||||
| Contribution | ||||||||||
| Rosendahl (2006) | ||||||||||
| Mental functions | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | ||||||||||
| Rosstad (2017) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | ||||||||||
| Rossum (1993) | ||||||||||
| Mental functions | Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Health service utilization | ||||||||||
| Rubenstein (1994) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Independent living | ||||||||||
| Runciman (1996) | ||||||||||
| Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Health service utilization | ||||||||||
| Ryan (2006) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | ||||||||||
| Build and maintain relationships | ||||||||||
| Rytter (2010) | ||||||||||
| Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Satisfaction of older adult | ||||||||||
| Cost‐effectiveness | ||||||||||
| Health service utilization | ||||||||||
| Sackley (2007) | ||||||||||
| Mobility | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Sackley (2009) | ||||||||||
| Mental functions | Basic needs | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | ||||||||||
| Sackley (2015) | ||||||||||
| Adaptations to physical environment | Mental functions | Basic needs | Cost‐effectiveness | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||
| Quality of life | Safety | |||||||||
| Mobility | Falls | |||||||||
| Sahlen (2016) | ||||||||||
| Quality of life | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Salminen (2009) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | Falls | Assisted living | ||||||||
| Mobility | ||||||||||
| Salpakoski (2014) | ||||||||||
| Sensory functions and pain | Mobility | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | ||||||||||
| Samus (2014) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Sandberg (2015) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | Satisfaction of older adult | Assisted living | ||||||||
| Cost‐effectiveness | ||||||||||
| Sandberg (2015) | ||||||||||
| Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Sanford (2006) | ||||||||||
| Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Schnelle (1996) | ||||||||||
| Neuromusculoskeletal function | Mobility | Safety | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Schnelle (2010) | ||||||||||
| Mental functions | Mobility | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Functions of the digestive, metabolic and endocrine systems | ||||||||||
| Genitourinary and reproductive functions | ||||||||||
| Neuromusculoskeletal function | ||||||||||
| Seidl (2015) | ||||||||||
| Sensory functions and pain | Quality of life | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Senior (2014) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Quality of life | Health service utilization | Independent living | |||||||
| Serra‐Rexach (2011) | ||||||||||
| Neuromusculoskeletal function | Mobility | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Sheffield (2013) | ||||||||||
| Adaptations to physical environment | Mental functions | Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||
| Quality of life | Falls | |||||||||
| Shepperd and Iliffe (1998) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Health service utilization | ||||||||||
| Shepperd and Iliffe (1998) | ||||||||||
| Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | Health service utilization | |||||||||
| Shepperd (2017) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Independent living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Health service utilization | Assisted living | |||||||||
| Sherman (2016) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Mobility | |||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Communication | |||||||||
| Functions of the digestive, metabolic and endocrine systems | ||||||||||
| Integumentary system | ||||||||||
| Sherrington (2015) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | Safety | |||||||||
| Mobility | Health service utilization | |||||||||
| Contribution | Falls | |||||||||
| Sherrington (2016) | ||||||||||
| Mental functions | Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Quality of life | Safety | ||||||||
| Neuromusculoskeletal function | Mobility | Health service utilization | ||||||||
| Falls | ||||||||||
| Shyu (2008) | ||||||||||
| Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Caregiver outcomes | ||||||||||
| Shyu (2016) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Siggeirsdottir (2005) | ||||||||||
| Sensory functions and pain | Quality of life | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | ||||||||||
| Simmons (2002) | ||||||||||
| Sensory functions and pain | Mobility | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Simmons (2005) | ||||||||||
| Genitourinary and reproductive functions | Quality of life | Satisfaction of older adult | Long‐term care | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Mobility | ||||||||||
| Sloane (2004) | ||||||||||
| Mental functions | Basic needs | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Integumentary system | ||||||||||
| Steele (2008) | ||||||||||
| Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Mobility | ||||||||||
| Steinberg (2009) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Quality of life | |||||||||
| Mobility | ||||||||||
| Stelmack et al. (2007) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Sensory functions and pain | Mobility | |||||||||
| Stevens (2001) | ||||||||||
| Adaptations to physical environment | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Stevens‐Lapsley (2016) | ||||||||||
| Neuromusculoskeletal function | Mobility | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Stewart et al. (2005) | ||||||||||
| Mental functions | Quality of life | Caregiver outcomes | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Health service utilization | ||||||||||
| Stewart (2012) | ||||||||||
| Quality of life | Cost (e.g., out of pocket) | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Cost‐effectiveness | ||||||||||
| Health service utilization | ||||||||||
| Stuck et al. (1995) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Stuck et al. (1995) | ||||||||||
| Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Health service utilization | ||||||||||
| Stuck (2000) | ||||||||||
| Mental functions | Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Health service utilization | |||||||||
| Suominen (2015) | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | Quality of life | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Suttanon (2013) | ||||||||||
| Neuromusculoskeletal function | Quality of life | Adherence | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Mobility | Caregiver outcomes | |||||||||
| Falls | ||||||||||
| Szanton (2014) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Cost‐effectiveness | Residential home/apartment | Other | Socioeconomic status | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||
| Mobility | Health service utilization | |||||||||
| Talley (2017) | ||||||||||
| Genitourinary and reproductive functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Mobility | |||||||||
| Taube (2017) | ||||||||||
| Mental functions | Quality of life | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Thomas (2016) | ||||||||||
| Mental functions | Residential home/apartment | Usual care | Social capital | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Thomas (2018) | ||||||||||
| Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Thygesen (2015) | ||||||||||
| Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Tibaldi (2004) | ||||||||||
| Mental functions | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Tibaldi (2009) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Tinetti (1999) | ||||||||||
| Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Contribution | ||||||||||
| Build and maintain relationships | ||||||||||
| Toots (2017) | ||||||||||
| Mental functions | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Townsend (1988) | ||||||||||
| Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Health service utilization | ||||||||||
| Tsaih (2011) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Long‐term care | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | Assisted living | |||||||||
| Tseng (2016) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Sensory functions and pain | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | ||||||||||
| Tsuchihashi‐Makaya (2013) | ||||||||||
| Mental functions | Quality of life | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Turunen (2017) | ||||||||||
| Sensory functions and pain | Mobility | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | ||||||||||
| Underwood (2013) | ||||||||||
| Mental functions | Quality of life | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Sensory functions and pain | Contribution | |||||||||
| Valdes (2015) | ||||||||||
| Sensory functions and pain | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Neuromusculoskeletal function | ||||||||||
| Van Der Pols‐Vijlbrief (2016) | ||||||||||
| Mental functions | Basic needs | Cost‐effectiveness | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Functions of the digestive, metabolic and endocrine systems | Quality of life | Health service utilization | ||||||||
| Neuromusculoskeletal function | Mobility | |||||||||
| van Haastregt (2000) | ||||||||||
| Mental functions | Basic needs | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Mobility | |||||||||
| Contribution | ||||||||||
| van Hout (2010) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| van Houten (2007) | ||||||||||
| Genitourinary and reproductive functions | Basic needs | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Vass (2007) | ||||||||||
| Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Verweij (2018) | ||||||||||
| Mental functions | Basic needs | Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | Caregiver outcomes | |||||||||
| Health service utilization | ||||||||||
| Vogler (2009) | ||||||||||
| Mental functions | Basic needs | Safety | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Quality of life | Falls | Independent living | |||||||
| Mobility | ||||||||||
| Weir (1998) | ||||||||||
| Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Cost‐effectiveness | ||||||||||
| Caregiver outcomes | ||||||||||
| Whitehead (2014) | ||||||||||
| Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | Health service utilization | |||||||||
| Wilhelmson (2013) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Financial security and stability | ||||||||||
| Build and maintain relationships | ||||||||||
| Wilson (2009) | ||||||||||
| Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Wishart (2000) | ||||||||||
| Basic needs | Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Quality of life | Cost‐effectiveness | |||||||||
| Caregiver outcomes | ||||||||||
| Health service utilization | ||||||||||
| Wisniowska‐Szurlej (2017) | ||||||||||
| Mental functions | Quality of life | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Mobility | |||||||||
| Wong (2015) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | Health service utilization | |||||||||
| Wong (2016) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Quality of life | Health service utilization | ||||||||
| Wylie (2017) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Adherence | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Quality of life | Falls | |||||||||
| Mobility | ||||||||||
| Young (1992) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Sensory functions and pain | Mobility | |||||||||
| Neuromusculoskeletal function | Contribution | |||||||||
| Ziden (2008) | ||||||||||
| Basic needs | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Mobility | ||||||||||
| Contribution | ||||||||||
| Ziden (2010) | ||||||||||
| Mental functions | Basic needs | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||
| Neuromusculoskeletal function | Quality of life | |||||||||
| Mobility | ||||||||||
| Ziden (2014) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | ||||
| Neuromusculoskeletal function | Mobility | |||||||||
| Zimmer (1985) | ||||||||||
| Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | RCT | |||||
| Health service utilization | ||||||||||
| Abdulla (2013) | ||||||||||
| Adaptations to physical environment | Mental functions | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Sensory functions and pain | Quality of life | |||||||||
| Neuromusculoskeletal function | ||||||||||
| Allen et al. (2014) | ||||||||||
| Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||||
| Satisfaction of older adult | ||||||||||
| Caregiver outcomes | ||||||||||
| Safety | ||||||||||
| Health service utilization | ||||||||||
| Andy (2016) | ||||||||||
| Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | High quality SR | ||||
| Quality of life | Cost‐effectiveness | |||||||||
| Health service utilization | ||||||||||
| Apostolo (2018) | ||||||||||
| Mental functions | Basic needs | Cost (e.g., out of pocket) | Assisted living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Neuromusculoskeletal function | Quality of life | Cost‐effectiveness | ||||||||
| Caregiver outcomes | ||||||||||
| Baldwin (2011) | ||||||||||
| Functions of the cardiovascular, haematological, immunological and respiratory systems | Quality of life | Cost‐effectiveness | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | Planned but not reported | High quality SR | |||
| Functions of the digestive, metabolic and endocrine systems | ||||||||||
| Baxter (2016) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Independent living | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Mobility | Other | |||||||||
| Berger (2013) | ||||||||||
| Adaptations to physical environment | Contribution | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Other | ||||||||||
| Beswick (2010) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Falls | ||||||||||
| Blythe (2009) | ||||||||||
| Mental functions | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Bryant‐Lukosius (2015) | ||||||||||
| Quality of life | Cost (e.g., out of pocket) | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Satisfaction of older adult | ||||||||||
| Cost‐effectiveness | ||||||||||
| Caregiver outcomes | ||||||||||
| Health service utilization | ||||||||||
| Bula (2011) | ||||||||||
| Neuromusculoskeletal function | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Bunn (2016) | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | Basic needs | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Burns (2001) | ||||||||||
| Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | High quality SR | |||||
| Burton (2015) | ||||||||||
| Mental functions | Mobility | Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Neuromusculoskeletal function | Falls | |||||||||
| Burton (2015) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Mobility | ||||||||||
| Cadore (2013) | ||||||||||
| Neuromusculoskeletal function | Falls | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Other | ||||||||||
| Candy (2011) | ||||||||||
| Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||||
| Cost‐effectiveness | Long‐term care | |||||||||
| Assisted living | ||||||||||
| Cattan (2005) | ||||||||||
| Mental functions | Build and maintain relationships | Residential home/apartment | Social capital | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Independent living | ||||||||||
| Chiung‐Ju (2013) | ||||||||||
| Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Chou (2012) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Quality of life | Assisted living | |||||||||
| Clarkson (2018) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Neuromusculoskeletal function | ||||||||||
| Clegg (2012) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Quality of life | Falls | |||||||||
| Mobility | ||||||||||
| Cobban (2012) | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | Basic needs | Long‐term care | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | ||||
| Assisted living | ||||||||||
| Cochrane (2014) | ||||||||||
| Basic needs | Satisfaction of older adult | Residential home/apartment | No ‐ assessment of effects by sex/gender NOT present | Planned but not reported | High quality SR | |||||
| Quality of life | Cost‐effectiveness | |||||||||
| Health service utilization | ||||||||||
| Corrieri (2011) | ||||||||||
| Cost‐effectiveness | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Falls | ||||||||||
| Crocker (2013) | ||||||||||
| Mental functions | Basic needs | Cost‐effectiveness | Long‐term care | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Neuromusculoskeletal function | Falls | |||||||||
| Daniels (2008) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Davis (2015) | ||||||||||
| Mental functions | Quality of life | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Cost‐effectiveness | ||||||||||
| Caregiver outcomes | ||||||||||
| Health service utilization | ||||||||||
| De Coninck (2017) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | ||||
| de Vries (2012) | ||||||||||
| Neuromusculoskeletal function | Quality of life | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Mobility | ||||||||||
| Desheng (2018) | ||||||||||
| Sensory functions and pain | Mobility | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Dickens (2011) | ||||||||||
| Mental functions | Build and maintain relationships | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | ||||
| Independent living | ||||||||||
| Assisted living | ||||||||||
| Eklund (2009) | ||||||||||
| Caregiver outcomes | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Health service utilization | ||||||||||
| Elkan (2001) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Evans (2003) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Independent living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Assisted living | ||||||||||
| Fletcher‐Smith (2013) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Long‐term care | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Quality of life | Cost‐effectiveness | Assisted living | ||||||||
| Mobility | Health service utilization | |||||||||
| Fomiatti (2013) | ||||||||||
| Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Contribution | ||||||||||
| Forbes (2015) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Health service utilization | Long‐term care | Other | ||||||||
| Assisted living | ||||||||||
| Franck (2016) | ||||||||||
| Mental functions | Assisted living | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | ||||||
| Gillespie (2012) | ||||||||||
| Adaptations to physical environment | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | ||||
| Safety | Independent living | |||||||||
| Falls | ||||||||||
| Gine‐Garriga (2014) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Residential home/apartment | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Mobility | ||||||||||
| Golding‐Day (2017) | ||||||||||
| Adaptations to physical environment | Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | ||
| Quality of life | Cost‐effectiveness | |||||||||
| Caregiver outcomes | ||||||||||
| Health service utilization | ||||||||||
| Falls | ||||||||||
| Gomes (2013) | ||||||||||
| Sensory functions and pain | Quality of life | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Satisfaction of older adult | ||||||||||
| Cost‐effectiveness | ||||||||||
| Caregiver outcomes | ||||||||||
| Grant (2014) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | High quality SR | |||
| Quality of life | Falls | |||||||||
| Graybill (2014) | ||||||||||
| Adaptations to physical environment | Sensory functions and pain | Basic needs | Cost‐effectiveness | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||
| Quality of life | ||||||||||
| Hall (2011) | ||||||||||
| Sensory functions and pain | Quality of life | Satisfaction of older adult | Long‐term care | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Independent living | ||||||||||
| Assisted living | ||||||||||
| Handoll (2009) | ||||||||||
| Mental functions | Basic needs | Adherence | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Quality of life | Cost‐effectiveness | Assisted living | ||||||||
| Caregiver outcomes | ||||||||||
| Health service utilization | ||||||||||
| Handoll (2015) | ||||||||||
| Sensory functions and pain | Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | High quality SR | |||
| Neuromusculoskeletal function | Mobility | Satisfaction of older adult | ||||||||
| Adherence | ||||||||||
| Hill (2015) | ||||||||||
| Mental functions | Basic needs | Adherence | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Neuromusculoskeletal function | Falls | Other | ||||||||
| Hobbs (2013) | ||||||||||
| Neuromusculoskeletal function | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||||
| Other | ||||||||||
| Howe (2011) | ||||||||||
| Neuromusculoskeletal function | Mobility | Adherence | Residential home/apartment | Other | Planned but not reported | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | High quality SR | |||
| Independent living | ||||||||||
| Assisted living | ||||||||||
| Hunter (2018) | ||||||||||
| Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||||
| Huss (2008) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Jane (2017) | ||||||||||
| Adaptations to physical environment | Mental functions | Basic needs | Cost‐effectiveness | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||
| Falls | ||||||||||
| Kang‐Yi (2010) | ||||||||||
| Mental functions | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Konno (2011) | ||||||||||
| Mental functions | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | |||||
| Caregiver outcomes | Assisted living | |||||||||
| Konno (2013) | ||||||||||
| Mental functions | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Caregiver outcomes | Assisted living | |||||||||
| Konno (2014) | ||||||||||
| Mental functions | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Kurz (2011) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Quality of life | Caregiver outcomes | Assisted living | ||||||||
| Lacroix (2017) | ||||||||||
| Neuromusculoskeletal function | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Legg (2004) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Quality of life | Health service utilization | |||||||||
| Legg (2017) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | High quality SR | |||
| Quality of life | Caregiver outcomes | |||||||||
| Health service utilization | ||||||||||
| Lewis (2017) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Falls | ||||||||||
| Liimatta (2016) | ||||||||||
| Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Quality of life | Cost‐effectiveness | |||||||||
| Health service utilization | ||||||||||
| Liu (2015) | ||||||||||
| Mental functions | Long‐term care | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Functions of the digestive, metabolic and endocrine systems | ||||||||||
| Liu (2018) | ||||||||||
| Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Low (2011) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Sensory functions and pain | Quality of life | Caregiver outcomes | ||||||||
| Build and maintain relationships | Health service utilization | |||||||||
| Martin (2011) | ||||||||||
| Mental functions | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||||
| Independent living | ||||||||||
| Mayo‐Wilson (2014) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Quality of life | Falls | |||||||||
| McClure (2005) | ||||||||||
| Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| McWilliam (2000) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Quality of life | Assisted living | |||||||||
| Build and maintain relationships | ||||||||||
| Meinck (2004) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Montgomery (2008) | ||||||||||
| Mental functions | Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Sensory functions and pain | Quality of life | Satisfaction of older adult | ||||||||
| Neuromusculoskeletal function | Contribution | Cost‐effectiveness | ||||||||
| Build and maintain relationships | Health service utilization | |||||||||
| Munk (2016) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Quality of life | ||||||||||
| Oliver (2007) | ||||||||||
| Falls | Long‐term care | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Outpatient (2003) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Quality of life | Caregiver outcomes | |||||||||
| Health service utilization | ||||||||||
| Ozdemir (2017) | ||||||||||
| Sensory functions and pain | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Quality of life | ||||||||||
| Patterson (1999) | ||||||||||
| Cost (e.g., out of pocket) | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Access | ||||||||||
| Pitkala (2013) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Mobility | Assisted living | |||||||||
| Poscia (2018) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Neuromusculoskeletal function | Build and maintain relationships | Assisted living | ||||||||
| Potter (2011) | ||||||||||
| Mental functions | Quality of life | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Neuromusculoskeletal function | Assisted living | |||||||||
| Reilly (2015) | ||||||||||
| Mental functions | Basic needs | Caregiver outcomes | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | High quality SR | |||
| Quality of life | Health service utilization | Assisted living | ||||||||
| Renz (2017) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | ||||
| Quality of life | Falls | |||||||||
| Resnick (2016) | ||||||||||
| Mental functions | Basic needs | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Neuromusculoskeletal function | Assisted living | |||||||||
| Roe (2015) | ||||||||||
| Genitourinary and reproductive functions | Assisted living | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Roets‐Merken (2015) | ||||||||||
| Sensory functions and pain | Residential home/apartment | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||||
| Santomassino (2012) | ||||||||||
| Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Health service utilization | ||||||||||
| Sean (2014) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | High quality SR | |||
| Quality of life | Falls | |||||||||
| Shaw (2009) | ||||||||||
| Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Cost‐effectiveness | Long‐term care | |||||||||
| Caregiver outcomes | ||||||||||
| Shepperd (2005) | ||||||||||
| Mental functions | Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | ||||
| Neuromusculoskeletal function | Caregiver outcomes | |||||||||
| Health service utilization | ||||||||||
| Shepperd (2011) | ||||||||||
| Mental functions | Quality of life | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Sensory functions and pain | Health service utilization | Other | ||||||||
| Functions of the digestive, metabolic and endocrine systems | ||||||||||
| Shepperd (2016) | ||||||||||
| Mental functions | Quality of life | Cost (e.g., out of pocket) | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Satisfaction of older adult | ||||||||||
| Health service utilization | ||||||||||
| Shvedko (2018) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Usual care | Social capital | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Build and maintain relationships | ||||||||||
| Simek (2012) | ||||||||||
| Adherence | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||||
| Falls | ||||||||||
| Sims‐Gould (2017) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Build and maintain relationships | Assisted living | |||||||||
| Skelton (2013) | ||||||||||
| Adaptations to physical environment | Mental functions | Quality of life | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | High quality SR | ||
| Smeeth (2006) | ||||||||||
| Sensory functions and pain | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||||
| Smith (2016) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | High quality SR | |||
| Quality of life | Adherence | |||||||||
| Cost‐effectiveness | ||||||||||
| Access | ||||||||||
| Health service utilization | ||||||||||
| Stall (2014) | ||||||||||
| Quality of life | Cost (e.g., out of pocket) | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Satisfaction of older adult | ||||||||||
| Cost‐effectiveness | ||||||||||
| Caregiver outcomes | ||||||||||
| Health service utilization | ||||||||||
| Steultjens (2004) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Sensory functions and pain | Quality of life | Falls | ||||||||
| Build and maintain relationships | ||||||||||
| Steultjens (2004) | ||||||||||
| Mental functions | Basic needs | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Sensory functions and pain | Quality of life | Falls | ||||||||
| Neuromusculoskeletal function | Contribution | |||||||||
| Stolee (2012) | ||||||||||
| Mental functions | Quality of life | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Stuck (2002) | ||||||||||
| Basic needs | Health service utilization | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Talley (2011) | ||||||||||
| Genitourinary and reproductive functions | Quality of life | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Tappenden (2012) | ||||||||||
| Mental functions | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | ||||
| Cost‐effectiveness | ||||||||||
| Health service utilization | ||||||||||
| Falls | ||||||||||
| Therapy‐based rehabilitation. . . (2003) | ||||||||||
| Mental functions | Basic needs | Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||
| Quality of life | Caregiver outcomes | Independent living | ||||||||
| Health service utilization | ||||||||||
| Thiebaud (2014) | ||||||||||
| Neuromusculoskeletal function | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Mobility | ||||||||||
| Toles (2016) | ||||||||||
| Basic needs | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | ||||
| Quality of life | Health service utilization | Assisted living | ||||||||
| Tseng (2011) | ||||||||||
| Mental functions | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Vaapio (2009) | ||||||||||
| Quality of life | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Assisted living | ||||||||||
| van Abbema (2015) | ||||||||||
| Neuromusculoskeletal function | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Van Citters (2004) | ||||||||||
| Mental functions | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Ward (2003) | ||||||||||
| Basic needs | Satisfaction of older adult | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Quality of life | Cost‐effectiveness | Long‐term care | ||||||||
| Health service utilization | Independent living | |||||||||
| Assisted living | ||||||||||
| Watanabe (2015) | ||||||||||
| Sensory functions and pain | Basic needs | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | |||||
| Quality of life | ||||||||||
| Mobility | ||||||||||
| Weber (2018) | ||||||||||
| Mental functions | Mobility | Falls | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | |||
| Neuromusculoskeletal function | ||||||||||
| Winkel (2008) | ||||||||||
| Basic needs | Cost (e.g., out of pocket) | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | ||||
| Quality of life | Satisfaction of older adult | |||||||||
| Access | ||||||||||
| Safety | ||||||||||
| Yi (2015) | ||||||||||
| Integumentary system | Long‐term care | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | ||||||
| Assisted living | ||||||||||
| Young (2017) | ||||||||||
| Quality of life | Satisfaction of older adult | Residential home/apartment | Usual care | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | High quality SR | ||||
| Health service utilization | Long‐term care | |||||||||
| Zhu (2013) | ||||||||||
| Functions of the digestive, metabolic and endocrine systems | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Low/critically low quality SR | |||||
| Zubala (2017) | ||||||||||
| Mental functions | Adherence | Residential home/apartment | Other | No ‐ assessment of effects by sex/gender NOT present | No ‐ assessment of effects across any other PROGRESS characteristics? For example, socioeconomic status | Moderate quality SR | ||||
| Neuromusculoskeletal function | Independent living | |||||||||
| Assisted living |
EXCLUDED STUDIES
| Study | Reason for Exclusion |
|---|---|
| Aasgaard et al. (2012) | EXCLUDE on study design |
| Abrisqueta‐Gomez et al. (2013) | EXCLUDE on study design |
| Aceros et al. (2016) | EXCLUDE on intervention |
| Achterberg (2016) | EXCLUDE on intervention |
| Acierno et al. (2017) | EXCLUDE on target group |
| Acorn (2008) | EXCLUDE on study design |
| Adachi et al. (2001) | EXCLUDE on intervention |
| Ades et al. (2003) | EXCLUDE on intervention |
| Afifi et al. (2014) | EXCLUDE on study design |
| Agmon and Embon‐Magal (2018) | EXCLUDE on setting |
| Agree (1999) | EXCLUDE on study design |
| Agree et al. (2005) | EXCLUDE on study design |
| Aguado et al. (2010) | EXCLUDE on intervention |
| Aguglia et al. (2004) | EXCLUDE on intervention |
| Aguila (2006) | EXCLUDE on study design |
| Ahlner‐Elmqvist et al. (2008) | EXCLUDE on study design |
| Ahmad (2016) | EXCLUDE on intervention |
| Ahmad (2018) | EXCLUDE on intervention |
| Aiken et al. (2006) | EXCLUDE on target group |
| Åkesson et al. (2018) | EXCLUDE on setting |
| Akiyama (2011) | EXCLUDE on study design |
| Albertsen (2011) | EXCLUDE on intervention |
| Albornos‐Muñoz et al. (2018) | EXCLUDE on setting |
| Alessi et al. (1997) | EXCLUDE on study design |
| Alkan et al. (2011) | EXCLUDE on intervention |
| Alldred et al. (2013) | EXCLUDE on intervention |
| Allen (1996) | EXCLUDE on study design |
| Allen (1999) | EXCLUDE on study design |
| Allen et al. (2012) | EXCLUDE on study design |
| Allen et al. (2014) | EXCLUDE on intervention |
| Allen et al. (2014) | EXCLUDE on intervention |
| Al‐Sari et al. (2018) | EXCLUDE on intervention |
| Anderson et al. (2012) | EXCLUDE on setting |
| Antoniak and Greig (2017) | EXCLUDE on setting |
| Anttila et al. (2011) | EXCLUDE on study design |
| Anttila et al. (2012) | EXCLUDE on study design |
| Aoun et al. (2015) | EXCLUDE on study design |
| Apóstolo (2016) | EXCLUDE on intervention |
| Applebaum and Phillips (1990) | EXCLUDE on study design |
| Applegate (1991) | EXCLUDE on study design |
| Arai et al. (2007) | EXCLUDE on setting |
| Aranda (1974) | EXCLUDE on study design |
| Arbesman and Mosley (2012) | EXCLUDE on setting |
| Arean et al. (2008) | EXCLUDE on setting |
| Arif et al. (2014) | EXCLUDE on study design |
| Armstrong et al. (2016) | EXCLUDE on study design |
| Arnall et al. (2012) | EXCLUDE on setting |
| Aronson and Neysmith (1996) | EXCLUDE on study design |
| Arthur (2000) | EXCLUDE on intervention |
| Ashok (2017) | EXCLUDE on study design |
| Ashworth et al. (2005) | EXCLUDE on target group |
| Assumpção (2014) | EXCLUDE on study design |
| Atienza (2001) | EXCLUDE on study design |
| Auger et al. (2008) | EXCLUDE on target group |
| Bahar‐Fuchs et al. (2017) | EXCLUDE on intervention |
| Bainbridge et al. (2016) | EXCLUDE on target group |
| Baker et al. (2001) | EXCLUDE on target group |
| Baker et al. (2016) | EXCLUDE on intervention |
| Bakker et al. (2011) | EXCLUDE on intervention |
| Baldwin et al. (2016) | EXCLUDE on intervention |
| Barnes et al. (2013) | EXCLUDE on intervention |
| Bateni and Maki (2005) | EXCLUDE on study design |
| Bates et al. (2018) | EXCLUDE on intervention |
| Belqaid et al. (2016) | EXCLUDE on intervention |
| Bentur et al. (1996) | EXCLUDE on intervention |
| Best and Solomon (1971) | EXCLUDE on study design |
| Best et al. (2014) | EXCLUDE on setting |
| Best et al. (2016) | EXCLUDE on setting |
| Beurskens (2016) | EXCLUDE on study design |
| Binder (2004) | EXCLUDE on setting |
| Bischoff‐Ferrari (2017) | EXCLUDE on intervention |
| Bishop et al. (2015) | EXCLUDE on intervention |
| Bismuth et al. (2012) | EXCLUDE on intervention |
| Blackwood et al. (2016) | EXCLUDE on intervention |
| Blake et al. (2009) | EXCLUDE on setting |
| Bleijenberg et al. (2013) | EXCLUDE on target group |
| Bleijenberg et al. (2017) | EXCLUDE on study design |
| Blohm (1998) | EXCLUDE on intervention |
| Boland et al. (2017) | EXCLUDE on study design |
| Bolscher‐Niehuis et al. (2016) | EXCLUDE on intervention |
| Borell (2018) | EXCLUDE on study design |
| Boucher et al. (2013) | EXCLUDE on study design |
| Boyd et al. (1996) | EXCLUDE on study design |
| Braun and Rose (1987) | EXCLUDE on study design |
| Braun et al. (1991) | EXCLUDE on study design |
| Brettschneider et al. (2015) | EXCLUDE on study design |
| Brismee et al. (2007) | EXCLUDE on setting |
| Britian (1999) | EXCLUDE on study design |
| Bruun‐Olsen et al. (2013) | EXCLUDE on setting |
| Bull (1994) | EXCLUDE on study design |
| Cabilan et al. (2013) | EXCLUDE on target group |
| Caplan et al. (2010) | EXCLUDE on intervention |
| Cardemil et al. (2013) | EXCLUDE on setting |
| Carlson et al. (2007) | EXCLUDE on intervention |
| Carlson et al. (2017) | EXCLUDE on target group |
| Challis et al. (1991) | EXCLUDE on study design |
| Chan et al. (2016) | EXCLUDE on setting |
| Chan et al. (2016) | EXCLUDE on setting |
| Chan et al. (2017) | EXCLUDE on setting |
| Chandler and Knackert (1997) | EXCLUDE on study design |
| Chesbro et al. (2005) | EXCLUDE on intervention |
| Chiatti et al. (2015) | EXCLUDE on target group |
| ChiCtr (2013) | EXCLUDE on intervention |
| Chien et al. (2008) | EXCLUDE on target group |
| Childress et al. (2008) | EXCLUDE on intervention |
| Chippendale (2012) | EXCLUDE on intervention |
| Chiu and Man (2004) | EXCLUDE on intervention |
| Chiu et al. (2015) | EXCLUDE on study design |
| Choi et al. (2014) | EXCLUDE on intervention |
| Chou (2011) | EXCLUDE on setting |
| Choyce et al. (2017) | EXCLUDE on target group |
| Chung and Zhao (2016) | EXCLUDE on setting |
| Cifu (2010) | EXCLUDE on study design |
| Ciliska et al.(1996) | EXCLUDE on target group |
| Clark (1998) | EXCLUDE on study design |
| Clarke and Colantonio (2005) | EXCLUDE on study design |
| Clegg (2014) | EXCLUDE on intervention |
| Clemson et al. (2012) | EXCLUDE on intervention |
| Coleman (1995) | EXCLUDE on study design |
| Coster et al. (2018) | EXCLUDE on study design |
| Cumming (2015) | EXCLUDE on setting |
| Cyarto et al. (2006) | EXCLUDE on study design |
| Dale and Brown (2006) | EXCLUDE on intervention |
| Dalton et al. (2018) | EXCLUDE on target group |
| Danilovich et al. (2017) | EXCLUDE on target group |
| Dapp et al. (2011) | EXCLUDE on intervention |
| Davison et al. (2016) | EXCLUDE on intervention |
| Day (2000) | EXCLUDE on intervention |
| Day et al. (2012) | EXCLUDE on setting |
| De Almeida (2015) | EXCLUDE on intervention |
| De Roos (2018) | EXCLUDE on setting |
| De van der Schueren (2017) | EXCLUDE on intervention |
| De Vriendt et al. (2016) | EXCLUDE on setting |
| De Vries (2016) | EXCLUDE on setting |
| Delbaere et al. (2006) | EXCLUDE on study design |
| Dellasega and Zerbe (2002) | EXCLUDE on target group |
| Der‐Fa et al. (2013) | EXCLUDE on intervention |
| Dohrn et al. (2017) | EXCLUDE on setting |
| Donaldson (1990) | EXCLUDE on study design |
| Donaldson and Bond (1991) | EXCLUDE on intervention |
| Douglas and Lawrence (2015) | EXCLUDE on study design |
| Douma et al. (2015) | EXCLUDE on intervention |
| Dozeman et al. (2011) | EXCLUDE on intervention |
| Dozeman et al. (2012) | EXCLUDE on intervention |
| Dreizler et al. (2014) | EXCLUDE on study design |
| Drummond et al. (2013) | EXCLUDE on setting |
| Duckworth et al. (2013) | EXCLUDE on study design |
| Dumoulin et al. (2014) | EXCLUDE on intervention |
| Effectiveness and cost‐effectiveness. . . (2016) | EXCLUDE on study design |
| Eklund et al. (2013) | EXCLUDE on setting |
| Elbadawy (2017) | EXCLUDE on setting |
| El‐Khoury et al. (2015) | EXCLUDE on setting |
| Eloranta (2010) | EXCLUDE on study design |
| Engberg et al. (1997) | EXCLUDE on study design |
| Evans (2007) | EXCLUDE on study design |
| Fahlman et al. (2007) | EXCLUDE on setting |
| Fairhall et al. (2015) | EXCLUDE on study design |
| Fanning et al. (2018) | EXCLUDE on setting |
| Farmer et al. (2006) | EXCLUDE on study design |
| Feldman et al. (2005) | EXCLUDE on intervention |
| Fernandez‐Barres et al. (2017) | EXCLUDE on intervention |
| Fields et al. (2014) | EXCLUDE on setting |
| Finkelstein and Fuller (2012) | EXCLUDE on study design |
| Fischer et al. (2015) | EXCLUDE on study design |
| Fitzgerald et al. (1994) | EXCLUDE on setting |
| Fleet et al. (2014) | EXCLUDE on intervention |
| Flora and Faulkner (2006) | EXCLUDE on study design |
| Forbes (2002) | EXCLUDE on study design |
| Forster et al. (2008) | EXCLUDE on setting |
| Forster et al. (2017) | EXCLUDE on intervention |
| Fowler and Kim (2015) | EXCLUDE on study design |
| Galle et al. (2017) | EXCLUDE on setting |
| Gary (2006) | EXCLUDE on intervention |
| Ghassemzadeh et al. (2013) | EXCLUDE on study design |
| Gianoudis et al. (2011) | EXCLUDE on setting |
| Gibson (2002) | EXCLUDE on study design |
| Gielen et al. (2013) | EXCLUDE on intervention |
| Giesbrecht et al. (2012) | EXCLUDE on study design |
| Gine‐Garriga et al. (2010) | EXCLUDE on setting |
| Giordano et al. (2016) | EXCLUDE on intervention |
| Gleeson et al. (2014) | EXCLUDE on intervention |
| Goedendorp et al. (2017) | EXCLUDE on intervention |
| Gollub (2002) | EXCLUDE on study design |
| Gomes (2018) | EXCLUDE on intervention |
| Gordon (1990) | EXCLUDE on study design |
| Gosman‐Hedstrom et al. (2002) | EXCLUDE on setting |
| Gothe et al. (2014) | EXCLUDE on setting |
| Graff et al. (2003) | EXCLUDE on study design |
| Graham‐Phillips et al. (2016) | EXCLUDE on study design |
| Gray and Sedhom (1997) | EXCLUDE on study design |
| Griffiths (2000) | EXCLUDE on study design |
| Griffiths (2013) | EXCLUDE on intervention |
| Gros et al. (2016) | EXCLUDE on study design |
| Guidetti et al. (2010) | EXCLUDE on setting |
| Guidon and McGee (2013) | EXCLUDE on setting |
| Guitard et al. (2013) | EXCLUDE on intervention |
| Haines et al. (2009) | EXCLUDE on intervention |
| Halvarsson et al. (2015) | EXCLUDE on setting |
| Hariprasad et al. (2013) | EXCLUDE on intervention |
| Harrison et al. (2008) | EXCLUDE on setting |
| Hauer (2015) | EXCLUDE on intervention |
| Hayashi et al. (2011) | EXCLUDE on setting |
| Healey (2011) | EXCLUDE on setting |
| Health (2008) | EXCLUDE on intervention |
| Heneka et al. (2016) | EXCLUDE on setting |
| Hennig et al. (2012) | EXCLUDE on study design |
| Henrard (1991) | EXCLUDE on study design |
| Herke et al. (2018) | EXCLUDE on intervention |
| Hile et al. (2018) | EXCLUDE on study design |
| Hinkka et al. (2007) | EXCLUDE on setting |
| Hinrichs et al. (2011) | EXCLUDE on intervention |
| Hirsch (2015) | EXCLUDE on study design |
| Hofstad et al. (2013) | EXCLUDE on study design |
| Holthe et al. (2018) | EXCLUDE on intervention |
| Hooper et al. (2014) | EXCLUDE on intervention |
| Hori et al. (2014) | EXCLUDE on intervention |
| Hu (2007) | EXCLUDE on intervention |
| Huang and Acton (2004) | EXCLUDE on intervention |
| Hughes et al. (1987) | EXCLUDE on study design |
| Hum et al. (2018) | EXCLUDE on study design |
| Humbert et al. (2007) | EXCLUDE on study design |
| Hummel et al. (2017) | EXCLUDE on intervention |
| Hung et al. (2003) | EXCLUDE on study design |
| Hussain (2013) | EXCLUDE on intervention |
| Iecovich (2007) | EXCLUDE on study design |
| Ifudu et al. (1994) | EXCLUDE on target group |
| Ilieva et al. (2013) | EXCLUDE on study design |
| Iliffe, Kendrick, et al. (2015) | EXCLUDE on intervention |
| Iliffe, Kendrick, et al. (2015) | EXCLUDE on intervention |
| Intiso et al. (2012) | EXCLUDE on study design |
| Istvandity (2017) | EXCLUDE on intervention |
| Iversen (2012) | EXCLUDE on study design |
| Iyengar et al. (2007) | EXCLUDE on study design |
| Jacobson et al. (2011) | EXCLUDE on intervention |
| Jame (2016) | EXCLUDE on intervention |
| Jansen et al. (2013) | EXCLUDE on setting |
| Jeon and Jeong (2015) | EXCLUDE on setting |
| Jessup et al. (2003) | EXCLUDE on setting |
| Jobe et al. (2001) | EXCLUDE on intervention |
| Johnen and Schott (2018) | EXCLUDE on study design |
| Johnson and Cockburn (1988) | EXCLUDE on study design |
| Joranson et al. (2017) | EXCLUDE on intervention |
| Jung et al. (2018) | EXCLUDE on intervention |
| Jyvakorpi et al. (2012) | EXCLUDE on intervention |
| Kamioka et al. (2004) | EXCLUDE on intervention |
| Kamioka et al. (2006) | EXCLUDE on intervention |
| Karlsson et al. (2013) | EXCLUDE on study design |
| Karmarkar (2009) | EXCLUDE on study design |
| Karmarkar (2009) | EXCLUDE on study design |
| Karmarkar et al. (2010) | EXCLUDE on study design |
| Katzel (2016) | EXCLUDE on setting |
| Kawagoshi et al. (2015) | EXCLUDE on setting |
| Keall et al. (2017) | EXCLUDE on intervention |
| Keeney et al. (2017) | EXCLUDE on study design |
| Kegelmeyer et al. (2013) | EXCLUDE on study design |
| Kelly et al. (2014) | EXCLUDE on intervention |
| Kemmler et al. (2010) | EXCLUDE on intervention |
| Kendall et al. (2018) | EXCLUDE on setting |
| Kerschan et al. (1998) | EXCLUDE on study design |
| Kerski et al. (1987) | EXCLUDE on study design |
| Kerwin et al. (2012) | EXCLUDE on study design |
| Kimura (2003) | EXCLUDE on intervention |
| Kind (2016) | EXCLUDE on intervention |
| King et al. (2012) | EXCLUDE on study design |
| Kiosses et al. (2010) | EXCLUDE on intervention |
| Kiosses et al. (2015) | EXCLUDE on study design |
| Kiosses et al. (2018) | EXCLUDE on study design |
| Kolt et al. (2009) | EXCLUDE on intervention |
| Konick‐McMahan et al. (2003) | EXCLUDE on study design |
| Konno (2012) | EXCLUDE on study design |
| Kono et al. (2009) | EXCLUDE on study design |
| Kravitz et al. (1994) | EXCLUDE on study design |
| Kruse et al. (2013) | EXCLUDE on study design |
| Kumar et al. (2017) | EXCLUDE on intervention |
| Kunik et al. (2017) | EXCLUDE on intervention |
| Kuo et al. (2013) | EXCLUDE on target group |
| Kuo et al. (2016) | EXCLUDE on target group |
| Kusumoto et al. (2007) | EXCLUDE on intervention |
| Lacroix et al. (2016) | EXCLUDE on setting |
| Lahtinen et al. (2015) | EXCLUDE on setting |
| Lahtinen et al. (2017) | EXCLUDE on setting |
| Lai (2004) | EXCLUDE on intervention |
| Lai (2017) | EXCLUDE on intervention |
| Lam et al. (2012) | EXCLUDE on setting |
| Laming (2017) | EXCLUDE on study design |
| Lapid et al. (2006) | EXCLUDE on setting |
| Laufer (2002) | EXCLUDE on setting |
| Leinonen et al. (2007) | EXCLUDE on intervention |
| Leone et al. (2012) | EXCLUDE on intervention |
| Leung (2005) | EXCLUDE on study design |
| Levine and Gitlin (1993) | EXCLUDE on study design |
| Levy‐Storms (2008) | EXCLUDE on study design |
| Liebel (2008) | EXCLUDE on study design |
| Lim et al. (2003) | EXCLUDE on setting |
| Lim et al. (2005) | EXCLUDE on target group |
| Lin et al. (2012) | EXCLUDE on setting |
| Lindegaard (2016) | EXCLUDE on study design |
| Lingler et al. (2014) | EXCLUDE on intervention |
| Littlewood et al. (2016) | EXCLUDE on intervention |
| Liu and Lai (2014) | EXCLUDE on setting |
| Liu and Lai (2014) | EXCLUDE on intervention |
| Liu et al. (2016) | EXCLUDE on intervention |
| Livingston et al. (2013) | EXCLUDE on target group |
| Lord et al. (2003) | EXCLUDE on setting |
| Low et al. (2013) | EXCLUDE on intervention |
| Low and Fletcher (2015) | EXCLUDE on study design |
| Luger et al. (2016) | EXCLUDE on intervention |
| Lundqvist et al. (2015) | EXCLUDE on study design |
| Luukinen et al. (2006) | EXCLUDE on intervention |
| MacNeil (2012) | EXCLUDE on intervention |
| Madara (2016) | EXCLUDE on target group |
| Maghsoudi et al. (2015) | EXCLUDE on study design |
| Majewski et al. (2015) | EXCLUDE on study design |
| Maki et al. (2008) | EXCLUDE on study design |
| Mameletzi et al. (2011) | EXCLUDE on setting |
| Mangione et al. (2010) | EXCLUDE on setting |
| Marioni et al. (2013) | EXCLUDE on intervention |
| Markle‐Reid et al. (2013) | EXCLUDE on study design |
| Marston (2007) | EXCLUDE on setting |
| Martini et al. (2018) | EXCLUDE on setting |
| Mason et al. (2007) | EXCLUDE on target group |
| Mazzuca et al. (1997) | EXCLUDE on intervention |
| McCusker et al. (2001) | EXCLUDE on setting |
| McEwan (1992) | EXCLUDE on study design |
| McMillan (2005) | EXCLUDE on study design |
| McNeil (1995) | EXCLUDE on study design |
| Mehlhorn et al. (2014) | EXCLUDE on setting |
| Mehrholz et al. (2015) | EXCLUDE on setting |
| Mehrholz (2017) | EXCLUDE on setting |
| Melin (1995) | EXCLUDE on setting |
| Melis et al. (2005) | EXCLUDE on intervention |
| Melis et al. (2010) | EXCLUDE on study design |
| Meng (2004) | EXCLUDE on intervention |
| Mercadante et al. (2011) | EXCLUDE on study design |
| Merom et al. (2016) | EXCLUDE on intervention |
| Messecar (1999) | EXCLUDE on study design |
| Messecar (2003) | EXCLUDE on study design |
| Michaud and Duchesne (2017) | EXCLUDE on setting |
| Mikkelsen et al. (2017) | EXCLUDE on study design |
| Miller et al. (2010) | EXCLUDE on study design |
| Miriam (2013) | EXCLUDE on study design |
| Mitchell (1987) | EXCLUDE on study design |
| Mitseva et al. (2012) | EXCLUDE on study design |
| Moffa‐Trotter and Anemaet (1996) | EXCLUDE on study design |
| Moholdt et al. (2012) | EXCLUDE on intervention |
| Molloy et al. (2006) | EXCLUDE on setting |
| Moniz (2012) | EXCLUDE on intervention |
| Monteau (2010) | EXCLUDE on study design |
| Montgomery (2010) | EXCLUDE on setting |
| Moore et al. (2016) | EXCLUDE on setting |
| Morag (2017) | EXCLUDE on intervention |
| Morey et al. (2015) | EXCLUDE on setting |
| Moriarty et al. (2016) | EXCLUDE on target group |
| Morin (2017) | EXCLUDE on setting |
| Mortenson et al. (2013) | EXCLUDE on intervention |
| Mottram et al. (2007) | EXCLUDE on study design |
| Mozley et al. (2007) | EXCLUDE on study design |
| Mozolic et al. (2008) | EXCLUDE on setting |
| Mukamel et al. (2007) | EXCLUDE on study design |
| Muller et al. (2014) | EXCLUDE on study design |
| Mustian et al. (2009) | EXCLUDE on intervention |
| Nelson et al. (2016) | EXCLUDE on study design |
| Ness et al. (2018) | EXCLUDE on setting |
| Neville (2015) | EXCLUDE on setting |
| Newbury and Marley (2000) | EXCLUDE on study design |
| Newcomer et al. (1999) | EXCLUDE on target group |
| Nguyen et al. (2015) | EXCLUDE on study design |
| Nieman et al. (2017) | EXCLUDE on intervention |
| Niemelä (2011) | EXCLUDE on setting |
| Niemela et al. (2012) | EXCLUDE on study design |
| Nijs et al. (2006) | EXCLUDE on intervention |
| Nikolaus et al. (1995) | EXCLUDE on intervention |
| Nikoletou et al. (2016) | EXCLUDE on intervention |
| Nilsson et al. (2012) | EXCLUDE on study design |
| Nishiguchi et al. (2015) | EXCLUDE on setting |
| Noelker and Bass (1989) | EXCLUDE on study design |
| Norrbom (1991) | EXCLUDE on intervention |
| Northey et al. (2018) | EXCLUDE on setting |
| Nour et al. (2002) | EXCLUDE on intervention |
| Nourhashemi (2015) | EXCLUDE on setting |
| Nowak et al. (1998) | EXCLUDE on target group |
| Oleske and Hauck (1988) | EXCLUDE on intervention |
| Oliveira et al. (2016) | EXCLUDE on setting |
| Ollonqvist et al. (2008) | EXCLUDE on setting |
| Olsen (2016) | EXCLUDE on setting |
| Orrell et al. (2007) | EXCLUDE on intervention |
| Orrell et al. (2014) | EXCLUDE on intervention |
| Ostaszkiewicz (2004) | EXCLUDE on intervention |
| Ottmann et al. (2013) | EXCLUDE on study design |
| Overbeek et al. (2018) | EXCLUDE on intervention |
| Padulo et al. (2018) | EXCLUDE on study design |
| Palvanen et al. (2012) | EXCLUDE on setting |
| Pan (2018) | EXCLUDE on setting |
| Park et al. (2017) | EXCLUDE on intervention |
| Parlevliet et al. (2010) | EXCLUDE on intervention |
| Parsons et al. (2013) | EXCLUDE on intervention |
| Pathy et al. (1992) | EXCLUDE on intervention |
| Payette et al. (2002) | EXCLUDE on intervention |
| Pearson et al. (2007) | EXCLUDE on intervention |
| Pedersen (2005) | EXCLUDE on study design |
| Perula et al. (2012) | EXCLUDE on setting |
| Pflaum et al. (2016) | EXCLUDE on study design |
| PG (1989) | EXCLUDE on study design |
| Pihl et al. (2011) | EXCLUDE on study design |
| Pine et al. (2002) | EXCLUDE on study design |
| Ploeg et al. (2010) | EXCLUDE on intervention |
| Podd et al. (2015) | EXCLUDE on setting |
| Pollack (1998) | EXCLUDE on study design |
| Pollock et al. (2012) | EXCLUDE on setting |
| Pozet et al. (2016) | EXCLUDE on target group |
| Pressler (2015) | EXCLUDE on study design |
| Prizer and Zimmerman (2018) | EXCLUDE on study design |
| Pynnonen et al. (2018) | EXCLUDE on setting |
| Ramsay et al. (2011) | EXCLUDE on intervention |
| Rana et al. (2010) | EXCLUDE on study design |
| Ranganathan et al. (2012) | EXCLUDE on study design |
| Rantanen et al. (2012) | EXCLUDE on setting |
| Ratzka (1986) | EXCLUDE on study design |
| Redford (1993) | EXCLUDE on study design |
| Reeder et al. (2013) | EXCLUDE on intervention |
| Reid and Ploeg (2002) | EXCLUDE on study design |
| Reid et al. (2017) | EXCLUDE on intervention |
| Rentschler et al. (2008) | EXCLUDE on study design |
| Resnick and Galik (2013) | EXCLUDE on study design |
| Ricauda et al. (2004) | EXCLUDE on setting |
| Richardson et al. (1989) | EXCLUDE on study design |
| Rideout (2004) | EXCLUDE on study design |
| Rizzo et al. (1996) | EXCLUDE on intervention |
| Robertson et al. (2001) | EXCLUDE on study design |
| Robinson et al. (2013) | EXCLUDE on setting |
| Rogers et al. (2018) | EXCLUDE on study design |
| Romskaug et al. (2017) | EXCLUDE on intervention |
| Rossi et al. (2014) | EXCLUDE on setting |
| Routasalo et al. (2009) | EXCLUDE on setting |
| Rubin et al. (1992) | EXCLUDE on setting |
| Rudilla et al. (2016) | EXCLUDE on intervention |
| Ruikes et al. (2016) | EXCLUDE on study design |
| Ryburn et al. (2009) | EXCLUDE on study design |
| Rydwik et al. (2010) | EXCLUDE on intervention |
| Sahota (2016) | EXCLUDE on setting |
| Sahyoun and Vaudin (2014) | EXCLUDE on study design |
| Sakurai et al. (2011) | EXCLUDE on setting |
| Sakurai et al. (2013) | EXCLUDE on setting |
| Salazar et al. (2000) | EXCLUDE on target group |
| Sampedro (2015) | EXCLUDE on intervention |
| Sampson et al. (2009) | EXCLUDE on intervention |
| Sanford et al. (1995) | EXCLUDE on intervention |
| Sayers et al. (2003) | EXCLUDE on setting |
| Schoenmakers et al. (2010) | EXCLUDE on target group |
| Schoonhoven et al. (2015) | EXCLUDE on intervention |
| Schwartz et al. (1990) | EXCLUDE on study design |
| Seitz et al. (2014) | EXCLUDE on study design |
| Sharpe et al. (2016) | EXCLUDE on setting |
| Shaw and Page (2008) | EXCLUDE on setting |
| Sheppard (1998) | EXCLUDE on target group |
| Shepperd and Iliffe (1998) | EXCLUDE on target group |
| Sherrington et al. (2004) | EXCLUDE on intervention |
| Sherwood (1980) | EXCLUDE on study design |
| Sherwood et al. (1986) | EXCLUDE on study design |
| Shimada et al. (2017) | EXCLUDE on intervention |
| Shishehgar et al. (2018) | EXCLUDE on intervention |
| Sidel et al. (1990) | EXCLUDE on intervention |
| Signe and Elmstahl (2008) | EXCLUDE on study design |
| Simmons et al. (1995) | EXCLUDE on study design |
| Simmons et al. (1996) | EXCLUDE on study design |
| Singh (2017) | EXCLUDE on setting |
| Singh (2018) | EXCLUDE on setting |
| Siragusa et al. (2005) | EXCLUDE on study design |
| Sjosten et al. (2008) | EXCLUDE on intervention |
| Sladek et al. (2011) | EXCLUDE on intervention |
| Smith et al. (2006) | EXCLUDE on study design |
| Sorensen et al. (2002) | EXCLUDE on target group |
| Sosnoff et al. (2014) | EXCLUDE on intervention |
| Sprange et al. (2013) | EXCLUDE on setting |
| Stark et al. (2017) | EXCLUDE on intervention |
| Stathi et al. (2018) | EXCLUDE on setting |
| Stein et al. (1981) | EXCLUDE on study design |
| Stelmack (2005) | EXCLUDE on intervention |
| Stenvall et al. (2007) | EXCLUDE on setting |
| Steultjens and Clemson (2006) | EXCLUDE on study design |
| Stevens‐Lapsley (2016) | EXCLUDE on setting |
| Stevenson and Gray (1981) | EXCLUDE on study design |
| Stewart et al. (2005) | EXCLUDE on intervention |
| Stewart (2006) | EXCLUDE on study design |
| Stewart et al. (2016) | EXCLUDE on study design |
| Stolle et al. (2012) | EXCLUDE on intervention |
| Stoltz (2004) | EXCLUDE on target group |
| Stow et al. (2015) | EXCLUDE on study design |
| Straw and Harley (1991) | EXCLUDE on study design |
| Stuck et al. (1995) | EXCLUDE on study design |
| Stuck et al. (2007) | EXCLUDE on intervention |
| Student (2013) | EXCLUDE on target group |
| Sturkenboom et al. (2016) | EXCLUDE on study design |
| Sungkarat et al. (2017) | EXCLUDE on setting |
| Suwanwela et al. (2002) | EXCLUDE on target group |
| Swank et al. (2011) | EXCLUDE on setting |
| Tappen and Debra (2014) | EXCLUDE on intervention |
| Tasiemski et al. (2005) | EXCLUDE on setting |
| Taule et al. (2015) | EXCLUDE on study design |
| Tennsledt et al. (1998) | EXCLUDE on intervention |
| Wolinksy (2011) | EXCLUDE on intervention |
| Thomas (1989) | EXCLUDE on study design |
| Thomas et al. (2007) | EXCLUDE on intervention |
| Thoreau (2015) | EXCLUDE on study design |
| Thulesius et al. (2002) | EXCLUDE on target group |
| Tibaek et al. (2014) | EXCLUDE on setting |
| Tiedemann et al. (2013) | EXCLUDE on setting |
| Tiedemann et al. (2015) | EXCLUDE on intervention |
| Tiedemann et al. (2016) | EXCLUDE on intervention |
| Timonen, Rantanen, Ryynanen, et al. (2002) | EXCLUDE on intervention |
| Timonen, Rantanen, Ryynanen, et al. (2002) | EXCLUDE on setting |
| Tinetti et al. (1993) | EXCLUDE on study design |
| Toevs (2000) | EXCLUDE on study design |
| Toot et al. (2011) | EXCLUDE on intervention |
| Torres et al. (2017) | EXCLUDE on intervention |
| Torres‐Arreola et al. (2009) | EXCLUDE on setting |
| Toseland et al. (1990) | EXCLUDE on target group |
| Towfighi et al. (2017) | EXCLUDE on target group |
| Troyer et al. (2010) | EXCLUDE on intervention |
| Tsai et al. (2017) | EXCLUDE on setting |
| Tse et al. (2016) | EXCLUDE on study design |
| Tsuchihashi‐Makaya et al. (2011) | EXCLUDE on target group |
| Ukawa, Satoh, et al. (2012) | EXCLUDE on intervention |
| Ukawa, Satoh, et al. (2012) | EXCLUDE on study design |
| Ukawa, Satoh, et al. (2012) | EXCLUDE on intervention |
| Ukawa (2015) | EXCLUDE on study design |
| Ullmann and Li (2017) | EXCLUDE on setting |
| Uy (2008) | EXCLUDE on setting |
| Vaapio et al. (2007) | EXCLUDE on setting |
| Vahlberg et al. (2017) | EXCLUDE on setting |
| van Ginneken et al. (2013) | EXCLUDE on target group |
| van Hout et al. (2005) | EXCLUDE on intervention |
| van Mulligen‐van (2013) | EXCLUDE on study design |
| van Ooijen et al. (2013) | EXCLUDE on setting |
| Van Spall (2018) | EXCLUDE on setting |
| Vandepitte, Noortgate, et al. (2016) | EXCLUDE on setting |
| VanDeVelde‐Coke (2004) | EXCLUDE on setting |
| Vass et al. (2004) | EXCLUDE on intervention |
| Vass (2005) | EXCLUDE on intervention |
| Venturelli et al. (2010) | EXCLUDE on setting |
| Verloo et al. (2015) | EXCLUDE on setting |
| Vetter et al. (1984) | EXCLUDE on intervention |
| Victor and Vetter (1988) | EXCLUDE on study design |
| Viswanathan et al. (2007) | EXCLUDE on study design |
| von Humboldt and Leal (2014) | EXCLUDE on intervention |
| Wallace et al. (2004) | EXCLUDE on intervention |
| Wanderley et al. (2015) | EXCLUDE on setting |
| Wang (2008) | EXCLUDE on study design |
| Wang et al. (2011) | EXCLUDE on intervention |
| Wang et al. (2013) | EXCLUDE on intervention |
| Wang et al. (2016) | EXCLUDE on target group |
| Wang and Wu (2017) | EXCLUDE on study design |
| Ward et al. (1978) | EXCLUDE on intervention |
| Warland and Tonning (1991) | EXCLUDE on study design |
| Warner et al. (2016) | EXCLUDE on intervention |
| Waterman et al. (2016) | EXCLUDE on study design |
| Weiss et al. (2004) | EXCLUDE on study design |
| Whitehead, Walker, et al. (2016) | EXCLUDE on study design |
| Whitehead, Walker, et al. (2016) | EXCLUDE on intervention |
| Whittemore et al. (2014) | EXCLUDE on study design |
| Whitten and Mickus (2007) | EXCLUDE on intervention |
| Wilhelmson et al. (2011) | EXCLUDE on intervention |
| Williams (2013) | EXCLUDE on study design |
| Williams et al. (2015) | EXCLUDE on study design |
| Wilson et al. (1999) | EXCLUDE on setting |
| Wilson and Truman (2005) | EXCLUDE on study design |
| Winter et al. (2016) | EXCLUDE on target group |
| Wittwer (2016) | EXCLUDE on intervention |
| Wong et al. (2014) | EXCLUDE on setting |
| Wong (2015) | EXCLUDE on study design |
| Wong et al. (2018) | EXCLUDE on setting |
| Wongcharoen et al. (2017) | EXCLUDE on intervention |
| Woolrych (2016) | EXCLUDE on study design |
| Wu (2007) | EXCLUDE on setting |
| Wu (2008) | EXCLUDE on target group |
| Wu (2017) | EXCLUDE on intervention |
| Wyatt et al. (2004) | EXCLUDE on target group |
| Wyers et al. (2010) | EXCLUDE on intervention |
| Xueyu et al. (2017) | EXCLUDE on intervention |
| Yoon et al. (2018) | EXCLUDE on setting |
| Yu (2016) | EXCLUDE on setting |
| Yusif et al. (2016) | EXCLUDE on study design |
| Yu‐Yahiro et al. (2009) | EXCLUDE on study design |
| Zarit et al. (2017) | EXCLUDE on study design |
| Zeeuwe et al. (2006) | EXCLUDE on intervention |
| Zhang et al. (2014) | EXCLUDE on setting |
| Zhao et al. (2017) | EXCLUDE on study design |
| Zheng et al. (2016) | EXCLUDE on setting |
| Zimmer (1984) | EXCLUDE on study design |
| Zimmer et al. (1990) | EXCLUDE on study design |
SOURCES OF SUPPORT
Internal sources
No sources of support provided
External sources
World Health Organization (WHO)
Canadian Institute of Health Research (CIHR), Canada
DATA AND ANALYSES
Supporting information
Supporting information
Supporting information
Supporting information
ACKNOWLEDGEMENTS
We would like to acknowledge Fariha Alam, Hovhannes Gasparyan, William McLeod, Khalid Miganeh, Jennifer Ogborogu, Agatha Park, Sabrina Price, Astha Saxena, Jashanpreet Sidhu and Ziyue Wang for their time in screening and selecting articles and retrieving full texts; and Victoria Barbeau for helping with the figures and supplementary material. We also acknowledge Jeff Brunton, Zak Ghouze and Sergio Graziosi for their technical support with EPPI‐Reviewer/EPPI‐Mapper.
APPENDIX 1. AGELINE SEARCH STRATEGY
| # | Query | Limiters/expanders | Last run via | Results |
|---|---|---|---|---|
| S117 | S114 AND S115 AND S116 | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
1620 |
| S116 | S97 OR S98 OR S99 OR S100 OR S101 OR S102 OR S103 OR S104 OR S105 OR S106 OR S107 OR S108 OR S109 OR S110 OR S111 OR S112 | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
50,309 |
| S115 | S63 OR S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 OR S80 OR S81 OR S82 OR S83 OR S84 OR S85 OR S86 OR S87 OR S88 OR S89 OR S90 OR S91 OR S92 OR S93 OR S94 OR S95 OR S96 | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
76,717 |
| S114 | S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58 OR S59 OR S60 OR S61 OR S62 | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
9488 |
| S113 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
105,340 |
| S112 | AB "usual care" or "usual practices" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
472 |
| S111 | AB groups | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
36,075 |
| S110 | TI trial OR AB trial | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
4922 |
| S109 | TI randomly OR AB randomly | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
2580 |
| S108 | TI randomized OR AB randomized | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
2866 |
| S107 | TI controlled N study OR AB controlled N2 study | Search modes—Boolean/Phrase |
Interface——EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
347 |
| S106 | DE "Randomized Controlled Trials" OR DE "Controlled Clinical Trials" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
2002 |
| S105 | AB medline | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
745 |
| S104 | AB pubmed | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
363 |
| S103 | TI overview OR AB overview | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
3185 |
| S102 | TI evidence N2 synthesi* OR AB evidence N2 synthesi* | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
44 |
| S101 | TI review | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
2612 |
| S100 | AB review* and (literature or studies or trials) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
8168 |
| S99 | TI (meta‐analysis or metaanalysis) OR AB (meta‐analysis or metaanalysis) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
697 |
| S98 | TI (meta‐analysis or metaanalysis) OR (meta‐analysis or metaanalysis) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
870 |
| S97 | TI systematic* OR AB systematic* | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
2823 |
| S96 | TI institutionali?ation OR AB institutionali?ation | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
1701 |
| S95 | TI reablement OR AB reablement | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
8 |
| S94 | TI adherence OR AB adherence | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
1010 |
| S93 | TI satisfaction OR AB satisfaction | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
6127 |
| S92 | TI relationships OR AB relationships | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
20,928 |
| S91 | TI security OR AB security | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
9802 |
| S90 | TI "community life" OR AB "community life" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
106 |
| S89 | TI mobility OR AB mobility | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
3638 |
| S88 | TI "self efficacy" OR AB "self efficacy" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
1155 |
| S87 | TI "self care" OR AB "self care" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
1221 |
| S86 | TI tiredness OR AB tiredness | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
72 |
| S85 | TI fatigue OR AB fatigue | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
678 |
| S84 | TI energy OR AB energy | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
1789 |
| S83 | TI vitality OR AB vitality | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
391 |
| S82 | TI distress OR AB distress | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
1763 |
| S81 | TI pain OR AB pain | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced SearchDatabase—AgeLine |
3778 |
| S80 | TI "sensory function*" OR AB "sensory function*" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
91 |
| S79 | TI cognitive OR AB cognitive | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
16,478 |
| S78 | TI depression OR AB depression | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
12,698 |
| S77 | TI "functional ability" OR AB "functional ability" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
865 |
| S76 | TI "mental health" OR AB "mental health" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
6757 |
| S75 | TI (happiness or happier) OR AB (happiness or happier) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
755 |
| S74 | TI "social participation" OR AB "social participation" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
315 |
| S73 | TI "social life" OR AB "social life" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
343 |
| S72 | TI wellbeing OR AB wellbeing | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
328 |
| S71 | TI independence OR AB independence | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
3181 |
| S70 | TI "quality of life" OR AB "quality of life" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
6388 |
| S69 | TI "activities of daily living" OR AB "activities of daily living" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
4863 |
| S68 | DE "Quality of Life" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
5646 |
| S67 | DE "Functional Ability" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
3318 |
| S66 | DE "Leisure Activities" OR DE "Games" OR DE "Hobbies" OR DE "Reading" OR DE "Recreation" OR DE "Travel" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
3271 |
| S65 | DE "Instrumental Activities of Daily Living" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
676 |
| S64 | DE "Daily Activities" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
394 |
| S63 | DE "Activities of Daily Living" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
3306 |
| S62 | TI ((kitchen or bathroom or bedroom)) OR AB ((kitchen or bathroom or bedroom)) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
662 |
| S61 | TI (medication N2 reminders) OR AB (medication N2 reminders) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
21 |
| S60 | TI "foot care" OR AB "foot care" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
56 |
| S59 | TI toileting OR AB toileting | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
268 |
| S58 | TI "personal hygiene" OR AB "personal hygiene" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
85 |
| S57 | TI grooming OR AB grooming | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
151 |
| S56 | TI bathing OR AB bathing | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
425 |
| S55 | TI (((household or routine) N (jobs or tasks or chores))) OR AB (((household or routine) N (jobs or tasks or chores))) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
117 |
| S54 | TI housekeeping OR AB housekeeping | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
294 |
| S53 | TI homemaking OR AB homemaking | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
91 |
| S52 | TI ((meal* N3 (provision or assistance or help or service* or preparation or delivery))) OR AB ((meal* N3 (provision or assistance or help or service* or preparation or delivery))) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
575 |
| S51 | TI ((food N (preparation or assistance or help or service or delivery))) OR AB ((food N (preparation or assistance or help or service or delivery))) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
4 |
| S50 | TI "house help" OR AB "house help" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
5 |
| S49 | TI shopping OR AB shopping | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
873 |
| S48 | TI "community services" OR AB "community services" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
949 |
| S47 | TI "home visit*" OR AB "home visit*" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
630 |
| S46 | TI "home support service*" OR AB "home support service*" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
44 |
| S45 | TI "home care service*" OR AB "home care service*" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
668 |
| S44 | DE "Home Care" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
3133 |
| S43 | TI (ramp or ramps) OR AB (ramp or ramps) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
66 |
| S42 | TI "shallow steps" OR AB "shallow steps" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
1 |
| S41 | TI "stair rails" OR AB "stair rails" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
2 |
| S40 | TI stairs OR AB stairs | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
330 |
| S39 | TI "stair climbing" OR AB "stair climbing" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
46 |
| S38 | TI Stair lift*" OR AB "Stair lift*" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
5 |
| S37 | TI (((Adapt* or adjust*) N3 (door* or entry or exit))) OR AB (((Adapt* or adjust*) N3 (door* or entry or exit))) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
12 |
| S36 | TI "vision aid*" OR AB "vision aid*" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
18 |
| S35 | TI "hearing aid*" OR AB "hearing aid*" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
317 |
| S34 | TI "hearing device*" OR AB "hearing device*" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
11 |
| S33 | TI spectacles OR AB spectacles | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
20 |
| S32 | TI glasses OR AB glasses | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
104 |
| S31 | TI eyeglasses OR AB eyeglasses | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
61 |
| S30 | DE "Hearing Aids" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
214 |
| S29 | TI ((communication N (aid* or device*))) OR AB ((communication N (aid* or device*))) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
1 |
| S28 | TI "transfer device*" OR AB "transfer device*" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
5 |
| S27 | TI scooter* OR AB scooter* | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
22 |
| S26 | TI Wheelchair* OR AB Wheelchair* | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
435 |
| S25 | TI ((Adapt* N3 (home* or house*))) OR AB ((Adapt* N3 (home* or house*))) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
168 |
| S24 | TI ((Adapt* N3 (cars or transport or vehicles))) OR AB ((Adapt* N3 (cars or transport or vehicles))) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
13 |
| S23 | TI "walking stick*" OR AB "walking stick*" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
8 |
| S22 | TI crutches OR AB crutches | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
20 |
| S21 | TI cane* OR AB cane* | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
140 |
| S20 | TI ((walking N2 (device* or aid* or equipment))) OR AB ((walking N2 (device* or aid* or equipment))) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
79 |
| S19 | TI motility OR AB motility | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
16 |
| S18 | TI "mobility aid*" OR AB "mobility aid*" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
26 |
| S17 | TI "mobility device*" OR AB "mobility device*" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
34 |
| S16 | TI "mobility equipment" OR AB "mobility equipment" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
5 |
| S15 | TI "assistive equipment" OR AB "assistive equipment" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
9 |
| S14 | TI "assistive devices" OR AB "assistive devices" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
284 |
| S13 | DE "Assistive Devices" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
751 |
| S12 | TI ((veteran* and (old* or home* or retire*))) OR AB ((veteran* and (old* or home* or retire*))) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
1576 |
| S11 | TI geriatric* OR AB geriatric* | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
16,521 |
| S10 | TI ((Resident* and (old* or home* or retirement or nursing))) OR AB ((Resident* and (old* or home* or retirement or nursing))) | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
14,367 |
| S9 | TI "end of life" OR AB "end of life" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
2172 |
| S8 | TI retirement OR AB retirement | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
16,495 |
| S7 | TI pensioners OR AB pensioners | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
286 |
| S6 | TI old* age* OR AB old* age* | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
34,385 |
| S5 | TI "older women" OR AB "older women" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
3854 |
| S4 | TI "older men" OR AB "older men" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
1695 |
| S3 | TI "older adult*" OR AB "older adult*" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
37,102 |
| S2 | TI "older people" OR AB "older people" | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
9585 |
| S1 | TI elderly OR AB elderly | Search modes—Boolean/Phrase |
Interface—EBSCOhost Research Databases Search Screen—Advanced Search Database—AgeLine |
32,088 |
APPENDIX 2. ASSIA SEARCH STRATEGY
(MAINSUBJECT.EXACT("Elderly people") OR MAINSUBJECT.EXACT("Elderly people") OR ti(elderly OR "older people" OR "older men" OR older women " or " older age " or " old age " or pensioners or retirement or " end of life " or geriatric") OR ab(elderly OR "older people" OR "older men" OR older women " or " older age " or " old age " or pensioners or retirement or " end of life " or geriatric") OR ti((Resident* AND (old* OR home* OR retirement OR nursing))) OR ti((Resident* AND (old* OR home* OR retirement OR nursing))) OR ab((veteran* AND (old* OR home* OR retire*)))) AND ((ti,ab("assistive devices" or "assistive equipment" or "mobility equipment" or "mobility devices" or "mobility aid*" or motility) OR ti,ab(walking near/2 (device* or aid* or equipment)) OR ti,ab(cane* or crutch* or "walking stick" or wheelchair* or scooter) OR ti,ab(adapt* near/3 (cars or transport or vehicles or home* or house*)) OR ti,ab(communication near/2 (device* or aid* or equipment)) OR ti,ab("hearing aid*" or hearing device* or eyeglasses or glasses or spectacles or "vision aid*") OR ti,ab((adapt* or adjust) near/3 (door* or entry or exit)) OR ti,ab(stair*) OR ti,ab(ramp or ramps) OR MAINSUBJECT.EXACT.EXPLODE("Home care")) OR (ti("home care" OR "home support" OR home visit " or " community services " or shopping or " house help " or " home help " or homemaking or housekeeping or bathing or grooming or " personal hygiene " or toileting or " footcare "") OR ab("home care" OR "home support" OR home visit " or " community services " or shopping or " house help " or " home help " or homemaking or housekeeping or bathing or grooming or " personal hygiene " or toileting or " footcare "")) OR ti,ab(food near (preparation or assistance or help or service or delivery)) OR ti,ab(meal* near/3 (provision or preparation or assistance or help or service or delivery)) OR ti,ab(kitchen or bathroom or bedroom))
APPENDIX 3. CINAHL SEARCH STRATEGY
| Query | Results | |
|---|---|---|
| S122 | S16 AND S68 AND S103 AND S121 | 1,915 |
| S121 | S104 OR S105 OR S106 OR S107 OR S108 OR S109 OR S110 OR S111 OR S112 OR S113 OR S114 OR S115 OR S116 OR S117 OR S118 OR S119 OR S120 | 1,059,185 |
| S120 | AB "usual care" or "usual practices" | 7,133 |
| S119 | AB groups | 535,924 |
| S118 | TI trial OR AB trial | 241,739 |
| S117 | TI randomly OR AB randomly | 66,660 |
| S116 | TI randomized OR AB randomized | 147,898 |
| S115 | TI controlled N study OR AB controlled N2 study | 19,862 |
| S114 | (MH "Randomized Controlled Trials") | 75,376 |
| S113 | AB medline | 34,544 |
| S112 | AB pubmed | 27,376 |
| S111 | TI overview OR AB overview | 36,219 |
| S110 | TI evidence N2 synthesi* OR AB evidence N2 synthesi* | 2,611 |
| S109 | TI review | 147,301 |
| S108 | AB review* and (literature or studies or trials) | 230,546 |
| S107 | TI (meta‐analysis or metaanalysis) OR AB (meta‐analysis or metaanalysis) | 47,271 |
| S106 | TI (meta‐analysis or metaanalysis) OR (meta‐analysis or metaanalysis) | 59,045 |
| S105 | TI systematic* OR AB systematic* | 111,442 |
| S104 | (MH "Systematic Review") | 65,382 |
| S103 | (S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 OR S80 OR S81 OR S82 OR S83 OR S84 OR S85 OR S86 OR S87 OR S88 OR S89 OR S90 OR S91 OR S92 OR S93 OR S94 OR S95 OR S96 OR S97 OR S98 OR S99 OR S100 OR S101 OR S102) | 899,122 |
| S102 | TI institutionali?ation OR AB institutionali?ation | 1,956 |
| S101 | TI reablement OR AB reablement | 59 |
| S100 | TI adherence OR AB adherence | 34,819 |
| S99 | TI satisfaction OR AB satisfaction | 58,116 |
| S98 | TI relationships OR AB relationships | 221,114 |
| S97 | TI security OR AB security | 14,091 |
| S96 | TI "community life" OR AB "community life" | 293 |
| S95 | TI mobility OR AB mobility | 20,472 |
| S94 | TI "self efficacy" OR AB "self efficacy" | 16,170 |
| S93 | TI "self care" OR AB "self care" | 12,062 |
| S92 | TI tiredness OR AB tiredness | 1,133 |
| S91 | TI fatigue OR AB fatigue | 28,761 |
| S90 | TI energy OR AB energy | 45,433 |
| S89 | TI vitality OR AB vitality | 2,603 |
| S88 | TI distress OR AB distress | 37,058 |
| S87 | TI pain OR AB pain | 191,463 |
| S86 | TI "sensory function*" OR AB "sensory function*" | 671 |
| S85 | TI cognitive OR AB cognitive | 96,135 |
| S84 | TI depression OR AB depression | 92,125 |
| S83 | TI "functional ability" OR AB "functional ability" | 2,170 |
| S82 | TI "mental health" OR AB "mental health" | 78,164 |
| S81 | TI (happiness or happier) OR AB (happiness or happier) | 3,585 |
| S80 | TI "social participation" OR AB "social participation" | 1,462 |
| S79 | TI "social life" OR AB "social life" | 1,416 |
| S78 | TI wellbeing OR AB wellbeing | 8,393 |
| S77 | TI independence OR AB independence | 13,126 |
| S76 | TI "quality of life" OR AB "quality of life" | 90,744 |
| S75 | TI "activities of daily living" OR AB "activities of daily living" | 11,299 |
| S74 | (MM "Automobile Driving") | 5,878 |
| S73 | (MM "Quality of Life + ") | 45,014 |
| S72 | (MM "Human Activities") | 619 |
| S71 | (MM "Home Maintenance") | 751 |
| S70 | (MM "Leisure Activities") | 3,321 |
| S69 | (MH "Activities of Daily Living + ") | 55,234 |
| S68 | S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58 OR S59 OR S60 OR S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 | 53,724 |
| S67 | TI ((kitchen or bathroom or bedroom)) OR AB ((kitchen or bathroom or bedroom)) | 2,693 |
| S66 | TI (medication N2 reminders) OR AB (medication N2 reminders) | 141 |
| S65 | TI "foot care" OR AB "foot care" | 1,048 |
| S64 | TI toileting OR AB toileting | 543 |
| S63 | TI "personal hygiene" OR AB "personal hygiene" | 503 |
| S62 | TI grooming OR AB grooming | 458 |
| S61 | TI bathing OR AB bathing | 1,784 |
| S60 | TI (((household or routine) N (jobs or tasks or chores))) OR AB (((household or routine) N (jobs or tasks or chores))) | 5 |
| S59 | TI housekeeping OR AB housekeeping | 662 |
| S58 | TI homemaking OR AB homemaking | 64 |
| S57 | TI ((meal* N3 (provision or assistance or help or service* or preparation or delivery))) OR AB ((meal* N3 (provision or assistance or help or service* or preparation or delivery))) | 674 |
| S56 | TI ((food N (preparation or assistance or help or service or delivery))) OR AB ((food N (preparation or assistance or help or service or delivery))) | 18 |
| S55 | TI "house help" OR AB "house help" | 2 |
| S54 | TI shopping OR AB shopping | 2,202 |
| S53 | TI "community services" OR AB "community services" | 1,494 |
| S52 | TI "home visit*" OR AB "home visit*" | 4,651 |
| S51 | TI "home support service*" OR AB "home support service*" | 43 |
| S50 | TI "home care service*" OR AB "home care service*" | 1,128 |
| S49 | (MM "Home Care Equipment and Supplies") | 247 |
| S48 | (MH "Home Rehabilitation + ") | 1,802 |
| S47 | TI (ramp or ramps) OR AB (ramp or ramps) | 1,036 |
| S46 | TI "shallow steps" OR AB "shallow steps" | 12 |
| S45 | TI "stair rails" OR AB "stair rails" | 2 |
| S44 | TI stairs OR AB stairs | 2,309 |
| S43 | TI "stair climbing" OR AB "stair climbing" | 671 |
| S42 | TI Stair lift*" OR AB "Stair lift*" | 12 |
| S41 | TI (((Adapt* or adjust*) N3 (door* or entry or exit))) OR AB (((Adapt* or adjust*) N3 (door* or entry or exit))) | 126 |
| S40 | TI "vision aid*" OR AB "vision aid*" | 53 |
| S39 | TI "hearing aid*" OR AB "hearing aid*" | 4,815 |
| S38 | TI "hearing device*" OR AB "hearing device*" | 296 |
| S37 | TI spectacles OR AB spectacles | 505 |
| S36 | TI glasses OR AB glasses | 885 |
| S35 | TI eyeglasses OR AB eyeglasses | 121 |
| S34 | (MH "Hearing Aids + ") | 14,658 |
| S33 | TI ((communication N (aid* or device*))) OR AB ((communication N (aid* or device*))) | 3 |
| S32 | TI "transfer device*" OR AB "transfer device*" | 102 |
| S31 | TI scooter* OR AB scooter* | 231 |
| S30 | TI Wheelchair* OR AB Wheelchair* | 4,427 |
| S29 | TI ((Adapt* N3 (home* or house*))) OR AB ((Adapt* N3 (home* or house*))) | 514 |
| S28 | TI ((Adapt* N3 (cars or transport or vehicles))) OR AB ((Adapt* N3 (cars or transport or vehicles))) | 79 |
| S27 | TI "walking stick*" OR AB "walking stick*" | 70 |
| S26 | TI crutches OR AB crutches | 398 |
| S25 | TI cane* OR AB cane* | 870 |
| S24 | TI ((walking N2 (device* or aid* or equipment))) OR AB ((walking N2 (device* or aid* or equipment))) | 682 |
| S23 | TI motility OR AB motility | 3,562 |
| S22 | TI "mobility aid*" OR AB "mobility aid*" | Display |
| S21 | TI "mobility device*" OR AB "mobility device*" | Display |
| S20 | TI "mobility equipment" OR AB "mobility equipment" | Display |
| S19 | TI "assistive equipment" OR AB "assistive equipment" | Display |
| S18 | TI "assistive devices" OR AB "assistive devices" | Display |
| S17 | (MM "Assistive Technology Devices") | Display |
| S16 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 | Display |
| S15 | TI ((veteran* and (old* or home* or retire*))) OR AB ((veteran* and (old* or home* or retire*))) | Display |
| S14 | TI geriatric* OR AB geriatric* | Display |
| S13 | TI ((Resident* and (old* or home* or retirement or nursing))) OR AB ((Resident* and (old* or home* or retirement or nursing))) | Display |
| S12 | TI "end of life" OR AB "end of life" | Display |
| S11 | TI retirement OR AB retirement | Display |
| S10 | TI pensioners OR AB pensioners | Display |
| S9 | TI old* age* OR AB old* age* | Display |
| S8 | TI "older women" OR AB "older women" | Display |
| S7 | TI "older men" OR AB "older men" | Display |
| S6 | TI "older adult*" OR AB "older adult*" | Display |
| S5 | TI "older people" OR AB "older people" | Display |
| S4 | TI elderly OR AB elderly | Display |
| S3 | (MM "Frail Elderly") | Display |
| S2 | (MH "Aged, 80 and Over") | Display |
| S1 | (MM "Aged") | Display |
APPENDIX 4. COCHRANE LIBRARY SEARCH STRATEGY
Search Name:
Date Run: 31/07/18 14:52:15.684
Description:
ID Search Hits
#1 MeSH descriptor: [Aged] explode all trees 1381
#2 MeSH descriptor: [Aged, 80 and over] explode all trees 176
#3 MeSH descriptor: [Frail Elderly] explode all trees 707
#4 elderly:ti,ab 23565
#5 "older people":ti,ab 2886
#6 "older adult*":ti,ab 8626
#7 "older men":ti,ab 1070
#8 "older women":ti,ab 1656
#9 "old* age*":ti,ab 3327
#10 pensioners:ti,ab 23
#11 retirement:ti,ab 270
#12 "end of life":ti,ab 923
#13 (Resident* and (old* or home* or retirement or nursing)):ti,ab 3257
#14 geriatric*:ti,ab 4492
#15 (veteran* and (old* or home* or retire*)):ti,ab 930
#16 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 43904
#17 MeSH descriptor: [Self‐Help Devices] explode all trees 440
#18 "assistive devices":ti,ab 154
#19 "assistive equipment":ti,ab 5
#20 "mobility equipment":ti,ab 0
#21 "mobility device*":ti,ab 24
#22 "mobility aid*":ti,ab 22
#23 motility:ti,ab 3258
#24 (walking near/2 (device* or aid* or equipment)):ti,ab 233
#25 cane*:ti,ab 262
#26 crutches:ti,ab 101
#27 "walking stick*":ti,ab 11
#28 (Adapt* near/3 (cars or transport or vehicles)):ti,ab 7
#29 (Adapt* near/3 (home* or house*)):ti,ab 103
#30 Wheelchair*:ti,ab 564
#31 scooter*:ti,ab 11
#32 "transfer device*":ti,ab 8
#33 (communication near (aid* or device*)):ti,ab 208
#34 MeSH descriptor: [Optical Devices] explode all trees 3992
#35 MeSH descriptor: [Hearing Aids] explode all trees 489
#36 eyeglasses:ti,ab 52
#37 glasses:ti,ab 619
#38 spectacles:ti,ab 386
#39 "hearing device*":ti,ab 24
#40 "hearing aid*":ti,ab 571
#41 "vision aid*":ti,ab 44
#42 ((Adapt* or adjust*) near/3 (door* or entry or exit)):ti,ab 31
#43 "Stair lift*":ti,ab 1
#44 "stair climbing":ti,ab 343
#45 stairs:ti,ab 450
#46 "stair rails":ti,ab 1
#47 "shallow steps":ti,ab 0
#48 (ramp or ramps):ti,ab 474
#49 MeSH descriptor: [Home Care Services] explode all trees 2709
#50 "home care service*":ti,ab 123
#51 "home support service*":ti,ab 3
#52 "home visit*":ti,ab 2466
#53 "community services":ti,ab 252
#54 shopping:ti,ab 257
#55 "house help":ti,ab 0
#56 "home help":ti,ab 46
#57 (food near (preparation or assistance or help or service or delivery)):ti,ab 432
#58 (meal* near/3 (provision or assistance or help or service* or preparation or delivery)):ti,ab 181
#59 homemaking:ti,ab 3
#60 housekeeping:ti,ab 65
#61 ((household or routine) near (jobs or tasks or chores)):ti,ab 74
#62 bathing:ti,ab 531
#63 grooming:ti,ab 58
#64 personal hygiene:ti,ab 257
#65 toileting:ti,ab 122
#66 "foot care":ti,ab 161
#67 (medication near/2 reminders):ti,ab 95
#68 (kitchen or bathroom or bedroom):ti,ab 400
#69 #17 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 or #46 or #47 or #48 or #49 or #50 or #51 or #52 or #53 or #54 or #55 or #56 or #57 or #58 or #59 or #60 or #61 or #62 or #63 or #64 or #65 or #66 or #67 or #68 19187
#70 #16 and #69 1814
APPENDIX 5. EMBASE SEARCH STRATEGY
Database: Embase <1974 to 2018 July 30>
Search Strategy:
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 Frail Elderly/(8986)
2 elderly.ti,ab. (307606)
3 older people.ti,ab. (28244)
4 older adult*.ti,ab. (77298)
5 older men.ti,ab. (10061)
6 older women.ti,ab. (16183)
7 old* age*.ti,ab. (91882)
8 pensioners.ti,ab. (1069)
9 retirement.ti,ab. (13626)
10 "end of life".ti,ab. (26578)
11 (Resident* and (old* or home* or retirement or nursing)).ti,ab. (50626)
12 geriatric*.ti,ab. (66412)
13 (veteran* and (old* or home* or retire*)).ti,ab. (7328)
14 or/1‐13 (597440)
15 self help device/(686)
16 orthopedic equipment/(7113)
17 assistive devices.ti,ab. (2030)
18 assistive equipment.ti,ab. (67)
19 mobility equipment.ti,ab. (40)
20 mobility device*.ti,ab. (366)
21 mobility aid*.ti,ab. (423)
22 motility.ti,ab. (107762)
23 (walking adj2 (device* or aid* or equipment)).ti,ab. (1867)
24 cane*.ti,ab. (7668)
25 crutch/(907)
26 crutches.ti,ab. (1592)
27 walking stick*.ti,ab. (314)
28 (Adapt* adj3 (cars or transport or vehicles)).ti,ab. (570)
29 (Adapt* adj3 (home* or house*)).ti,ab. (1916)
30 Wheelchair*.ti,ab. (9414)
31 scooter*.ti,ab. (455)
32 transfer device*.ti,ab. (324)
33 (communication adj (aid* or device*)).ti,ab. (1123)
34 eyeglasses.ti,ab. (737)
35 glasses.ti,ab. (9279)
36 spectacles.ti,ab. (2696)
37 exp hearing aid/(24552)
38 hearing aid*.ti,ab. (9542)
39 hearing device*.ti,ab. (588)
40 vision aid*.ti,ab. (467)
41 ((Adapt* or adjust*) adj3 (door* or entry or exit)).ti,ab. (302)
42 Stair lift*.ti,ab. (5)
43 stair climbing.ti,ab. (1871)
44 stairs.ti,ab. (4629)
45 stair rails.ti,ab. (4)
46 shallow steps.ti,ab. (1)
47 (ramp or ramps).ti,ab. (8753)
48 exp home care/(67776)
49 home care service*.ti,ab. (1915)
50 home support service*.ti,ab. (62)
51 home visit*.ti,ab. (9825)
52 community services.ti,ab. (3077)
53 shopping.ti,ab. (4729)
54 house help.ti,ab. (3)
55 home help.ti,ab. (526)
56 (food adj (preparation or assistance or help or service or delivery)).ti,ab. (4484)
57 (meal* adj3 (provision or assistance or help or service* or preparation or delivery)).ti,ab. (1594)
58 homemaking.ti,ab. (141)
59 housekeeping.ti,ab. (10998)
60 ((household or ktichen or routine) adj (jobs or tasks or chores)).ti,ab. (1136)
61 bathing.ti,ab. (11145)
62 grooming.ti,ab. (6112)
63 personal hygiene.ti,ab. (2422)
64 toileting.ti,ab. (1310)
65 foot care.ti,ab. (1788)
66 (medication adj2 reminders).ti,ab. (242)
67 (kitchen or bathroom or bedroom).ti,ab. (7945)
68 or/15‐67 (322386)
69 daily life activity/(78117)
70 Human Activities/(3185)
71 independent living/(3089)
72 recreation/(18512)
73 shopping/(1911)
74 social participation/(4612)
75 "activities of daily living".ti,ab. (30943)
76 "quality of life".ti,ab. (359513)
77 independence.ti,ab. (47534)
78 wellbeing.ti,ab. (18483)
79 social life.ti,ab. (5685)
80 social participation.ti,ab. (2771)
81 happiness.ti,ab. (6798)
82 happier.ti,ab. (909)
83 mental health.ti,ab. (147320)
84 functional ability.ti,ab. (6217)
85 depression.ti,ab. (400172)
86 cognitive.ti,ab. (416634)
87 sensory function*.ti,ab. (4984)
88 pain.ti,ab. (796354)
89 distress.ti,ab. (135545)
90 vitality.ti,ab. (14572)
91 energy.ti,ab. (546309)
92 fatigue.ti,ab. (127854)
93 tiredness.ti,ab. (5785)
94 self care.ti,ab. (20633)
95 self efficacy.ti,ab. (26490)
96 mobility.ti,ab. (142390)
97 community life.ti,ab. (577)
98 security.ti,ab. (47760)
99 relationships.ti,ab. (378690)
100 satisfaction.ti,ab. (157439)
101 adherence.ti,ab. (146634)
102 reablement.ti,ab. (63)
103 institutionali?ation.ti,ab. (5821)
104 or/69‐103 (3385736)
105 "systematic review"/(174301)
106 systematic*.ti,ab. (453751)
107 (meta‐analysis or metaanalysis).ti,ab. (148557)
108 (review* and (literature or studies or trials)).ab. (880084)
109 review.ti. (455568)
110 (evidence adj2 synthesi*).ti,ab. (6614)
111 overview.ti,ab. (167411)
112 pubmed.ab. (104333)
113 medline.ab. (118298)
114 or/106‐113 (1650752)
115 exp controlled clinical trial/(694556)
116 randomized.ti,ab. (638306)
117 randomly.ab. (384901)
118 trial.ti,ab. (727369)
119 groups.ab. (2487203)
120 usual care.ab. (18552)
121 or/115‐120 (3623667)
122 114 or 121 (5002455)
123 14 and 68 and 104 and 122 (3448)
***************************
APPENDIX 6. PSYCINFO SEARCH STRATEGY
Database: PsycINFO <1806 to July Week 4 2018>
Search Strategy:
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 elderly.ti,ab. (54174)
2 older people.ti,ab. (12110)
3 older adult*.ti,ab. (41115)
4 older men.ti,ab. (2189)
5 older women.ti,ab. (4109)
6 old* age*.ti,ab. (20699)
7 pensioners.ti,ab. (185)
8 retirement.ti,ab. (9183)
9 "end of life".ti,ab. (8017)
10 (Resident* and (old* or home* or retirement or nursing)).ti,ab. (20000)
11 geriatric*.ti,ab. (14314)
12 (veteran* and (old* or home* or retire*)).ti,ab. (3282)
13 or/1‐12 (152396)
14 assistive devices.ti,ab. (459)
15 assistive equipment.ti,ab. (12)
16 mobility equipment.ti,ab. (9)
17 mobility device*.ti,ab. (109)
18 mobility aid*.ti,ab. (96)
19 motility.ti,ab. (2556)
20 (walking adj2 (device* or aid* or equipment)).ti,ab. (158)
21 cane*.ti,ab. (672)
22 crutches.ti,ab. (96)
23 walking stick*.ti,ab. (38)
24 (Adapt* adj3 (cars or transport or vehicles)).ti,ab. (31)
25 (Adapt* adj3 (home* or house*)).ti,ab. (515)
26 Wheelchair*.ti,ab. (1489)
27 scooter*.ti,ab. (87)
28 transfer device*.ti,ab. (11)
29 (communication adj (aid* or device*)).ti,ab. (660)
30 Hearing aids/(1719)
31 eyeglasses.ti,ab. (133)
32 glasses.ti,ab. (1145)
33 spectacles.ti,ab. (464)
34 hearing device*.ti,ab. (93)
35 hearing aid*.ti,ab. (2472)
36 vision aid*.ti,ab. (53)
37 ((Adapt* or adjust*) adj3 (door* or entry or exit)).ti,ab. (116)
38 Stair lift*.ti,ab. (1)
39 stair climbing.ti,ab. (166)
40 stairs.ti,ab. (563)
41 stair rails.ti,ab. (1)
42 (ramp or ramps).ti,ab. (1042)
43 home care service*.ti,ab. (497)
44 home support service*.ti,ab. (30)
45 home visit*.ti,ab. (3811)
46 community services.ti,ab. (2062)
47 shopping.ti,ab. (5054)
48 house help.ti,ab. (1)
49 home help.ti,ab. (168)
50 (food adj (preparation or assistance or help or service or delivery)).ti,ab. (1559)
51 (meal* adj3 (provision or assistance or help or service* or preparation or delivery)).ti,ab. (474)
52 homemaking.ti,ab. (248)
53 housekeeping.ti,ab. (531)
54 ((household or ktichen or routine) adj (jobs or tasks or chores)).ti,ab. (995)
55 bathing.ti,ab. (838)
56 grooming.ti,ab. (4042)
57 personal hygiene.ti,ab. (415)
58 toileting.ti,ab. (515)
59 foot care.ti,ab. (123)
60 (medication adj2 reminders).ti,ab. (43)
61 (kitchen or bathroom or bedroom).ti,ab. (1808)
62 or/14‐61 (35245)
63 exp "Activities of Daily Living"/(5520)
64 "activities of daily living".ti,ab. (8352)
65 "quality of life".ti,ab. (59139)
66 "Quality of Life"/(37055)
67 independence.ti,ab. (24287)
68 wellbeing.ti,ab. (10013)
69 social life.ti,ab. (5978)
70 social participation.ti,ab. (2191)
71 happiness.ti,ab. (13763)
72 happier.ti,ab. (1484)
73 mental health.ti,ab. (157706)
74 functional ability.ti,ab. (1345)
75 depression.ti,ab. (219164)
76 cognitive.ti,ab. (370295)
77 sensory function*.ti,ab. (1264)
78 pain.ti,ab. (83792)
79 distress.ti,ab. (57532)
80 vitality.ti,ab. (3953)
81 energy.ti,ab. (33607)
82 fatigue.ti,ab. (22222)
83 tiredness.ti,ab. (1251)
84 self care.ti,ab. (8094)
85 self efficacy.ti,ab. (34497)
86 mobility.ti,ab. (16761)
87 community life.ti,ab. (1109)
88 security.ti,ab. (25264)
89 relationships.ti,ab. (258664)
90 satisfaction.ti,ab. (95291)
91 adherence.ti,ab. (24737)
92 reablement.ti,ab. (16)
93 institutionali?ation.ti,ab. (4822)
94 or/63‐93 (1229400)
95 systematic*.ti,ab. (108262)
96 (meta‐analysis or metaanalysis).ti,ab. (23648)
97 (review* and (literature or studies or trials)).ab. (201906)
98 review.ti. (142171)
99 (evidence adj2 synthesi*).ti,ab. (1195)
100 overview.ti,ab. (69147)
101 pubmed.ab. (9463)
102 medline.ab. (11506)
103 or/95‐102 (435243)
104 randomized.ti,ab. (63903)
105 randomly.ab. (66378)
106 trial.ti,ab. (94392)
107 groups.ab. (454479)
108 usual care.ab. (3673)
109 or/104‐108 (591784)
110 103 or 109 (980597)
111 13 and 62 and 94 and 110 (539)
***************************
APPENDIX 7. SOCIAL POLICY AND PRACTICE SEARCH STRATEGY
Database: Social Policy and Practice <201804>
Search Strategy:
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 elderly.ti,ab. (13983)
2 older people.ti,ab. (24556)
3 older adult*.ti,ab. (5159)
4 older men.ti,ab. (545)
5 older women.ti,ab. (1322)
6 old* age*.ti,ab. (4684)
7 pensioners.ti,ab. (876)
8 retirement.ti,ab. (3880)
9 "end of life".ti,ab. (1661)
10 (Resident* and (old* or home* or retirement or nursing)).ti,ab. (11855)
11 geriatric*.ti,ab. (2842)
12 (veteran* and (old* or home* or retire*)).ti,ab. (184)
13 or/1‐12 (55038)
14 assistive devices.ti,ab. (74)
15 assistive equipment.ti,ab. (8)
16 mobility equipment.ti,ab. (9)
17 mobility device*.ti,ab. (14)
18 mobility aid*.ti,ab. (17)
19 motility.ti,ab. (1)
20 (walking adj2 (device* or aid* or equipment)).ti,ab. (19)
21 cane*.ti,ab. (51)
22 crutches.ti,ab. (3)
23 walking stick*.ti,ab. (7)
24 (Adapt* adj3 (cars or transport or vehicles)).ti,ab. (13)
25 (Adapt* adj3 (home* or house*)).ti,ab. (310)
26 Wheelchair*.ti,ab. (316)
27 scooter*.ti,ab. (19)
28 transfer device*.ti,ab. (3)
29 (communication adj (aid* or device*)).ti,ab. (50)
30 [Hearing aids/] (0)
31 eyeglasses.ti,ab. (1)
32 glasses.ti,ab. (29)
33 spectacles.ti,ab. (17)
34 hearing device*.ti,ab. (1)
35 hearing aid*.ti,ab. (85)
36 vision aid*.ti,ab. (7)
37 ((Adapt* or adjust*) adj3 (door* or entry or exit)).ti,ab. (1)
38 Stair lift*.ti,ab. (5)
39 stair climbing.ti,ab. (10)
40 stairs.ti,ab. (70)
41 stair rails.ti,ab. (1)
42 (ramp or ramps).ti,ab. (40)
43 home care service*.ti,ab. (684)
44 home support service*.ti,ab. (49)
45 home visit*.ti,ab. (670)
46 community services.ti,ab. (1160)
47 shopping.ti,ab. (884)
48 house help.ti,ab. (0)
49 home help.ti,ab. (382)
50 (food adj (preparation or assistance or help or service or delivery)).ti,ab. (67)
51 (meal* adj3 (provision or assistance or help or service* or preparation or delivery)).ti,ab. (241)
52 homemaking.ti,ab. (12)
53 housekeeping.ti,ab. (40)
54 ((household or ktichen or routine) adj (jobs or tasks or chores)).ti,ab. (84)
55 bathing.ti,ab. (142)
56 grooming.ti,ab. (273)
57 personal hygiene.ti,ab. (47)
58 toileting.ti,ab. (61)
59 foot care.ti,ab. (26)
60 (medication adj2 reminders).ti,ab. (2)
61 (kitchen or bathroom or bedroom).ti,ab. (311)
62 or/14‐61 (5918)
63 [exp "Activities of Daily Living"/] (0)
64 "activities of daily living".ti,ab. (1300)
65 "quality of life".ti,ab. (6357)
66 ["Quality of Life"/] (0)
67 independence.ti,ab. (3826)
68 wellbeing.ti,ab. (4416)
69 social life.ti,ab. (337)
70 social participation.ti,ab. (347)
71 happiness.ti,ab. (405)
72 happier.ti,ab. (118)
73 mental health.ti,ab. (23759)
74 functional ability.ti,ab. (211)
75 depression.ti,ab. (7846)
76 cognitive.ti,ab. (7353)
77 sensory function*.ti,ab. (23)
78 pain.ti,ab. (1266)
79 distress.ti,ab. (2687)
80 vitality.ti,ab. (167)
81 energy.ti,ab. (2664)
82 fatigue.ti,ab. (320)
83 tiredness.ti,ab. (32)
84 self care.ti,ab. (659)
85 self efficacy.ti,ab. (842)
86 mobility.ti,ab. (2688)
87 community life.ti,ab. (244)
88 security.ti,ab. (5575)
89 relationships.ti,ab. (13857)
90 satisfaction.ti,ab. (4829)
91 adherence.ti,ab. (688)
92 reablement.ti,ab. (163)
93 institutionali?ation.ti,ab. (581)
94 or/63‐93 (74744)
95 systematic*.ti,ab. (5049)
96 (meta‐analysis or metaanalysis).ti,ab. (684)
97 (review* and (literature or studies or trials)).ab. (11073)
98 review.ti. (9726)
99 (evidence adj2 synthesi*).ti,ab. (113)
100 overview.ti,ab. (9080)
101 pubmed.ab. (196)
102 medline.ab. (471)
103 or/95‐102 (28484)
104 randomized.ti,ab. (634)
105 randomly.ab. (1161)
106 trial.ti,ab. (2435)
107 groups.ab. (25738)
108 usual care.ab. (230)
109 or/104‐108 (28684)
110 103 or 109 (54320)
111 13 and 62 and 94 and 110 (196)
***************************
APPENDIX 8. SOCIAL SCIENCE CITATION INDEX (SSCI) VIA WEB OF SCIENCE SEARCH STRATEGY
SSCI via Web of Science
| # 4 | 640 | #3 AND #2 AND #1Indexes = SSCI Timespan = 1900‐2018 | |
| # 3 | 40,698 | TITLE: ("systematic review" or "controlled trial")Indexes = SSCI Timespan = 1900‐2018 | |
| # 2 | 501,019 | TI = (mobility or function* or "quality of life" or independence or wellbeing or social or activities)Indexes = SSCI Timespan = 1900‐2018 | |
| # 1 | 258,485 | TITLE: (old* or elderly or aged)Indexes = SSCI Timespan = 1900‐2018 |
APPENDIX 9. CODING TOOL
| Category | Answer | |
|---|---|---|
| Geographical information | WHO Regions |
|
| World Bank Region (2019 FY) |
|
|
| Study design | Design |
|
| Publication status |
|
|
| Population | Age Group |
|
| Sex/Gender |
|
|
| Health Conditions |
|
|
| Intervention | General Social support services, systems and policies |
|
| Health services, systems and policies |
|
|
| Products and Technology |
|
|
| Outcome | Intrinsic Capacity |
|
| Functional Ability |
|
|
| Process and other |
|
|
| Setting |
|
|
|
||
|
||
|
||
| Comparison |
|
|
| Systematic Review quality |
|
|
| PROGRESS |
|
|
| Gender Inequalities | Is there an assessment of effects by sex/gender |
|
| Other inequalities | Is there an assessment of effects by other characteristics, for example, socioeconomic status, income, race/ethnicity, etc |
|
APPENDIX 10. LINK TO ONLINE INTERACTIVE EGM
The online interactive EGM is available at https://globalageing.cochrane.org/sites/globalageing.cochrane.org/files/public/uploads/ageing_egm_interactive_map_may5_20.html.
Welch, V. , Mathew, C. M. , Babelmorad, P. , et al. (2021). Health, social care and technological interventions to improve functional ability of older adults living at home: An evidence and gap map. Campbell Systematic Reviews, 17, e1175. 10.1002/cl2.1175
OTHER REFERENCES
ADDITIONAL REFERENCES
- Banerjee, S. (2015). Multimorbidity—Older adults need health care that can count past one. The Lancet, 385(9968), 587–589. [DOI] [PubMed] [Google Scholar]
- Bashour, H. N. , Kharouf, M. H. , AbdulSalam, A. A. , El Asmar, K. , Tabbaa, M. A. , & Cheikha, S. A. (2008). Effect of postnatal home visits on maternal/infant outcomes in Syria: A randomized controlled trial. Public Health Nursing, 25(2), 115–125. [DOI] [PubMed] [Google Scholar]
- Beard, J. R. , Officer, A. , de Carvalho, I. A. , Sadana, R. , Pot, A. M. , Michel, J.‐P. , Lloyd‐Sherlock, P. , Epping‐Jordan, J. E. , Peeters, G. M. E. E. , Mahanani, W. R. , Thiyagarajan, J. A. , & Chatterji, S. (2016). The world report on ageing and health: A policy framework for healthy ageing. The Lancet, 387(10033), 2145–2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bragge, P. , Clavisi, O. , Turner, T. , Tavender, E. , Collie, A. , Gruen, & Russell, L. (2011). The Global Evidence Mapping Initiative: Scoping research in broad topic areas. BMC Medical Research Methodology, 11(1), 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cesari, M. , Araujo, C. I. , & Amuthavalli, T. J. (2018). Evidence for the domains supporting the construct of intrinsic capacity. The Journals of Gerontology: Series A, 73(12), 1653–1660. [DOI] [PubMed] [Google Scholar]
- Chalmers, I. , & Glasziou, P. (2009). Avoidable waste in the production and reporting of research evidence. The Lancet, 374(9683), 86–89. [DOI] [PubMed] [Google Scholar]
- Chalmers, I. , Bracken Michael, B. , Djulbegovic, B. , Garattini, S. , Grant, J. , Gülmezoglu, A. M. , Howells, D. W. , Ioannidis, J. P. A. , & Oliver, S. (2014). How to increase value and reduce waste when research priorities are set. The Lancet, 383(9912), 156–165. [DOI] [PubMed] [Google Scholar]
- Chatterji, S. , Byles, J. , Cutler, D. , Seeman, T. , & Verdes, E. (2015). Health, functioning, and disability in older adults‐‐present status and future implications. The Lancet, 385(9967), 563–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherubini, A. , Corsonello, A. , & Lattanzio, F. (2012). Underprescription of beneficial medicines in older people. Drugs & Aging, 29(6), 463–475. [DOI] [PubMed] [Google Scholar]
- Daniels, N. (1982). Equity of access to health care: Some conceptual and ethical issues. The Milbank Memorial Fund Quarterly. Health and Society, 60(1), 51–81. [PubMed] [Google Scholar]
- del‐Pino‐Casado, R. , Rodríguez Cardosa, M. , López‐Martínez, C. , & Orgeta, V. (2019). The association between subjective caregiver burden and depressive symptoms in carers of older relatives: A systematic review and meta‐analysis. PLOS One, 14(5), e0217648. 10.1371/journal.pone.0217648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Digital Solution Foundary and EPPI‐Centre (2020). EPPI‐Mapper, Version 1.2.5. EPPI‐Centre, UCL Social Research Institute, University College London.
- Drury, L. , Abrams, D. , Swift Hannah, J. , Lamont Ruth, A. , & Gerocova, K. (2017). Can caring create prejudice? An investigation of positive and negative intergenerational contact in care settings and the generalisation of blatant and subtle age prejudice to other older people. Journal of Community & Applied Social Psychology, 27(1), 65–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirch, W. (Ed.). (2008). Functional ability. Encyclopedia of Public Health. Springer. 10.1007/978-1-4020-5614-7_1209 [DOI] [Google Scholar]
- Esbensen Anna, J. , Johnson, E. B. , Amaral Joseph, L. , Tan Christine, M. , & Macks, R. (2016). Differentiating aging among adults with Down syndrome and comorbid dementia or psychopathology. American Journal on Intellectual and Developmental Disabilities, 121(1), 13–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garçon, L. , Khasnabis, C. , Walker, L. , Nakatani, Y. , Lapitan, J. , Borg, J. , Ross, A. , & Velazquez Berumen, A. (2016). Medical and assistive health technology: Meeting the needs of aging populations. The Gerontologist, 56(Suppl 2), S293–S302. [DOI] [PubMed] [Google Scholar]
- Gaynor, E. J. , Geoghegan, S. E. , & O'Neill, D. (2014). Ageism in stroke rehabilitation studies. Age and Ageing, 43(3), 429–431. [DOI] [PubMed] [Google Scholar]
- Gottlieb, L. M. , & Alderwick, H. (2019). Integrating social and medical care: Could it worsen health and increase inequity? Annals of Family Medicine, 17(1), 77–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P. T. , Thomas, J. , Chandler, J. , Cumpston, M. , Li, T. , Page, M. J. & Welch, V. A. (Eds.). (2019). Cochrane handbook for systematic reviews of interventions (2nd ed.). John Wiley & Sons. [Google Scholar]
- Hillcoat‐Nalletamby, S. (2014). The meaning of “independence” for older people in different residential settings. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 69(3), 419–430. [DOI] [PubMed] [Google Scholar]
- Levesque, J.‐F. , Harris Mark, F. , & Russell, G. (2013). Patient‐centred access to health care: Conceptualising access at the interface of health systems and populations. International Journal for Equity in Health, 12(1), 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberopoulos, G. , Trikalinos Nikolaos, A. , Ioannidis, & John, P. A. (2009). The elderly were under‐represented in osteoarthritis clinical trials. Journal of Clinical Epidemiology, 62(11), 1218–1223. [DOI] [PubMed] [Google Scholar]
- Lum, C. , Koper Christopher, S. , & Telep Cody, W. (2011). The evidence‐based policing matrix. Journal of Experimental Criminology, 7(1), 3–26. [Google Scholar]
- Marasinghe, K. M. , Lapitan, J. M. , & R, A. (2015). Assistive technologies for ageing populations in six low‐income and middle‐income countries: A systematic review. BMJ Innovations, 1, 182–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher, D. , Shamseer, L. , Clarke, M. , Ghersi, D. , Liberati, A. , Petticrew, M. , Shekelle, P. , Stewart, L. A. , & Prisma‐p, G. (2015). Preferred reporting items for systematic review and meta‐analysis protocols (PRISMA‐P) 2015 statement. Systematic Reviews, 4, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ndiok, A. , & Ncama, B. (2019). A qualitative study of home visiting as a palliative care strategy to follow‐up cancer patients by nurses in clinical setting in a developing country. Scandinavian Journal of Caring Sciences, 33(1), 185–196. [DOI] [PubMed] [Google Scholar]
- O'Neill, J. , Tabish, H. , Welch, V. , Petticrew, M. , Pottie, K. , Clarke, M. , Evans, T. , Pardo Pardo, J. , Waters, E. , White, H. , & Tugwell, P. (2014). Applying an equity lens to interventions: Using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. Journal of Clinical Epidemiology, 67(1), 56–64. [DOI] [PubMed] [Google Scholar]
- Plath, D. (2009). International policy perspectives on independence in old age international policy perspectives. Journal of Aging & Social Policy, 21(2), 209–223. [DOI] [PubMed] [Google Scholar]
- Prince, M. J. , Wu, F. , Guo, Y. , Gutierrez Robledo, L. M. , O'Donnell, M. , Sullivan, R. , & Yusuf, S. (2015). The burden of disease in older people and implications for health policy and practice. The Lancet, 385(9967), 549–562. [DOI] [PubMed] [Google Scholar]
- Sadana, R. , Blas, E. , Budhwani, S. , Koller, T. , & Paraje, G. (2016). Healthy ageing: Raising awareness of inequalities, determinants, and what could be done to improve health equity. The Gerontologist, 56(Suppl 2), S178–S193. [DOI] [PubMed] [Google Scholar]
- Sadana, R. , & Posarac, A. (2018). Need, use of services and relationship with intrinsic capacity. Department of Ageing and Life Course. World Health Organization, Geneva.
- Shea, B. J. , Reeves, B. C. , Wells, G. , Thuku, M. , Hamel, C. , Moran, J. , Moher, D. , Tugwell, P. , Welch, V. , Kristjansson, E. , & Henry, D. A. (2017). AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non‐randomised studies of healthcare interventions, or both. BMJ, 358(j4008), 4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snilstveit, B. , Vojtkova, M. , Bhavsar, A. , & Gaarder, M. (2013, December). Evidence gap maps: A tool for promoting evidence‐informed policy and prioritizing future research. The World Bank Independent Evaluation Group, Policy Research Working Paper. pp. 1–34.
- Snilstveit, B. , Vojtkova, M. , Bhavsar, A. , Stevenson, J. , & Gaarder, M. (2016). Evidence & gap maps: A tool for promoting evidence informed policy and strategic research agendas. Journal of Clinical Epidemiology, 79, 120–129. [DOI] [PubMed] [Google Scholar]
- Snilstveit, B. , Bhatia, R. , Rankin, K. , & Leach, B. (2017, February). 3ie evidence gap maps: A starting point for strategic evidence production and use. New Delhi: International Initiative for Impact Evaluation (3ie).
- Thomas, J. , Brunton, J. , Graziosi, S. (2010). EPPI‐Reviewer 4: Software for research synthesis. EPPI‐Centre Software. London: Social Science Research Unit, UCL Institute of Education. [Google Scholar]
- Thomas, J. , Graziosi, S. , Brunton, J. , Ghouze, Z. , O'Driscoll, P. , & Bond, M. EPPI‐reviewer: Advanced software for systematic reviews, maps and evidence synthesis. EPPI‐Centre Software, London: UCL Social Research Unit.
- United Nations, Department of Economic and Social Affairs, Population Division (UNDESA) (2017). World population prospects: The 2017 revision, key findings and advance tables. Working Paper No. ESA/P/WP/248:1–53.
- United Nations . World population ageing 2015. (ST/ESA/SER. A/390).
- United Nations (2019). Sustainable development goals. https://www.un.org/sustainabledevelopment/sustainable-development-goals/
- Welch, V. , Howe, T. E. , Marcus, S. , Mathew, C. M. , Sadana, R. , Rogers, M. , Sheehy, L. , Borg, J. , Pottie, K. , Thompson‐Coon, J. , Lyddiatt, A. , Kristjansson, E. , Nickerson, J. W. , Walker, P. , Tanuseputro, P. , Shea, B. , Sveistrup, H. , Babelmorad, P. , & Zhang, W. (2019). PROTOCOL: Health, social care and technological interventions to improve functional ability of older adults: Evidence and gap map. Campbell Systematic Reviews, 15, e1054. 10.1002/cl2.1054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welford, C. , Murphy, K. , Rodgers, V. , & Frauenlob, T. (2012). Autonomy for older people in residential care: A selective literature review. International Journal of Older People Nursing, 7(1), 65–69. [DOI] [PubMed] [Google Scholar]
- White, H. , Albers, B. , Gaarder, M. , Kornør, H. , Littell, J. , Marshall, Z. , Matthew, C. , Pigott, T. , Snilstveit, B. , Waddington, H. , & Welch, V. (2020). Guidance for producing a Campbell evidence and gap map. Campbell Systematic Reviews, 16, e1125. 10.1002/cl2.1125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead, M. (1992). The concepts and principles of equity and health. International Journal of Health Services, 22(3), 429–445. [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2001). International Classification of Functioning, Disability and Health: ICF. https://apps.who.int/iris/handle/10665/42407
- World Health Organization . (2011). WHO study on global AGEing and adult health (SAGE). WHO. [Google Scholar]
- World Health Organization . (2015). World report on ageing and health. https://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf?sequence=1 [Google Scholar]
- World Health Organization (2016a). World Health Assembly, 69: Multisectoral action for a life course approach to healthy ageing: Draft global strategy and plan of action on ageing and health. Report by the Secretariat. https://apps.who.int/iris/handle/10665/252671
- World Health Organization (2016b). Priority assistive products list: Improving access to assistive technology for everyone, everywhere (pp. 1–16). https://apps.who.int/iris/bitstream/handle/10665/207694/WHO_EMP_PHI_2016.01_eng.pdf [Google Scholar]
- World Health Organization . (2017). Mental health of older adults. WHO Newsroom Fact Sheets. https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults
- World Health Organization . (2018). Third United Nations high‐level meeting on NCDs. https://www.who.int/ncds/governance/third-un-meeting/en/
EXCLUDED STUDIES
- Aasgaard, H. S. , Landmark, B. , & Karlsson, B. (2012). Creating at‐homeness in a care setting environment. Klinisk Sygepleje, 26(1), 23–33. http://search.ebscohost.com/login.aspx?direct=true%26db=ccm%26AN=108161533%26site=ehost-live [Google Scholar]
- Abrisqueta‐Gomez, J. , Rosangela, K. , Ponce, C. S. C. , Locatelli, F. L. V. , & Batista, D. L. F. (2013). Non‐pharmacologic intervention in people with dementia in Brazil: An overview. Alzheimer's and Dementia, 1, P495–P496. 10.1016/j.jalz.2013.05.1021 [DOI] [Google Scholar]
- Aceros, J. C. , Cavalcante, M. T. , & Domenech, M. (2016). Aging at home with telecare in Spain. A dicourse analysis. Ciencia & saude coletiva, 21(8), 2413–2422. 10.1590/1413-81232015218.13472015 [DOI] [PubMed] [Google Scholar]
- Acierno, R. , Knapp, R. , Tuerk, P. , Gilmore, A. K. , Lejuez, C. , Ruggiero, K. , Muzzy, W. , Egede, L. , Hernandez‐Tejada, M. A. , & Foa, E. B. (2017). A non‐inferiority trial of Prolonged Exposure for posttraumatic stress disorder: In person versus home‐based telehealth. Behaviour Research and Therapy, 89, 57–65. 10.1016/j.brat.2016.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acorn, M. (2008). In‐home palliative care increased patient satisfaction and reduced use and costs of medical services. Evidence Based Nursing, 11(1), 22. http://search.ebscohost.com/login.aspx?direct=true%26db=ccm%26AN=105748671%26site=ehost-live [DOI] [PubMed] [Google Scholar]
- Adachi, K. , Sasaki, H. , Kakuta, M. , & Sasaki, M. (2001). How to support the death at home. Japanese Journal of Cancer & Chemotherapy, 28(Suppl 1), 133–135. [PubMed] [Google Scholar]
- Ades, P. A. , Savage, P. , Cress, M. E. , Brochu, M. , Lee, N. M. , & Poehlman, E. T. (2003). Resistance training on physical performance in disabled older female cardiac patients. Medicine & Science in Sports & Exercise, 35(8), 1265–1270. [DOI] [PubMed] [Google Scholar]
- Afifi, M. , Parke, B. , & Al‐Hussein, M. (2014). Evidence‐based evaluation of staircase architectural design to reduce the risk of falling for older adults. Journal of Housing for the Elderly, 28(1), 107–132. 10.1080/02763893.2013.858095 [DOI] [Google Scholar]
- Agmon, M. , & Embon‐Magal, S. (2018). Is thinking with the body effective for cogntive training? A randomized clinical trial “thinking in motion” study. Neurorehabilitation and Neural Repair, 32(4‐5), 354. 10.1177/1545968318765497 [DOI] [Google Scholar]
- Agree, E. M. (1999). The influence of personal care and assistive devices on the measurement of disability. Social Science and Medicine, 48(4), 427–443. [DOI] [PubMed] [Google Scholar]
- Agree, E. M. , Freedman, V. A. , Cornman, J. C. , Wolf, D. A. , & Marcotte, J. E. (2005). Reconsidering substitution in long‐term care: When does assistive technology take the place of personal care? Journals of Gerontology Series B‐Psychological Sciences & Social Sciences, 60(5), S272–S280. [DOI] [PubMed] [Google Scholar]
- Aguado, O. , Morcillo, C. , Delas, J. , Rennie, M. , Bechich, S. , Schembari, A. , Fernandez, F. , & Rosell, F. (2010). Long‐term implications of a single home‐based educational intervention in patients with heart failure. Heart & Lung, 39(6 Suppl), S14–S22. 10.1016/j.hrtlng.2010.04.010 [DOI] [PubMed] [Google Scholar]
- Aguglia, E. , Onor, M. L. , Trevisiol, M. , Negro, C. , Saina, M. , & Maso, E. (2004). Stress in the caregivers of Alzheimer's patients: An experimental investigation in Italy. American Journal of Alzheimer's Disease & Other Dementias, 19(4), 248–252. http://search.ebscohost.com/login.aspx?direct=true%26db=ccm%26AN=106560005%26site=ehost-live [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahlner‐Elmqvist, M. , Jordhoy, M. S. , Bjordal, K. , Jannert, M. , & Kaasa, S. (2008). Characteristics and quality of life of patients who choose home care at the end of life. Journal of Pain and Symptom Management, 36(3), 217–227. 10.1016/j.jpainsymman.2007.10.010 [DOI] [PubMed] [Google Scholar]
- Aiken, L. S. , Butner, J. , Lockhart, C. A. , Volk‐Craft, B. E. , Hamilton, G. , & Williams, F. G. (2006). Outcome evaluation of a randomized trial of the PhoenixCare intervention: Program of case management and coordinated care for the seriously chronically ill. Journal of Palliative Medicine, 9(1), 111–126. 10.1089/jpm.2006.9.111 [DOI] [PubMed] [Google Scholar]
- Aj, K. , Gilmore‐Bykovskyi, A. , Kennelty, K. , Jensen, L. , Schmitz, E. , Hermann, C. , & Mineau, J. (2016). The coordinated‐transitional care (CTRAC) program: Supporting patients with Alzheimer's dementia (AD) and their caregivers during care transitions from the hospital to the community. Alzheimer's and Dementia. Conference: Alzheimer's Association International Conference 2016. Canada. Conference Start: 20160722. Conference End: 20160728, 12(7 Supplement), pp. 221–222. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/246/CN-01251246/frame.html
- Åkesson, N. , Leffler, A. S. , & Rydwik, E. (2018). Evaluation of feasibility of a balance and strength training program for new users of a Wheeled Walker in an outpatient rehabilitation clinic. Physical and Occupational Therapy in Geriatrics, 36(1), 14–28. http://search.ebscohost.com/login.aspx?direct=true%26db=gnh%26AN=EP128746805%26site=ehost-live [Google Scholar]
- Akiko, A. , Hiroo, H. , & Hiroshi, M. (2011). Characteristics of home care supporting clinics providing home care for frail elderly persons living alone in Japan. Archives of Gerontology and Geriatrics, 52(2), e85–e88. 10.1016/j.archger.2010.07.011 [DOI] [PubMed] [Google Scholar]
- Al, M. (1995). A randomized trial of multidisciplinary in‐home care for frail elderly patients awaiting hospital discharge. Aging, 7(3), 247–250. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/323/CN-00119323/frame.html [DOI] [PubMed] [Google Scholar]
- Albornos‐Muñoz, L. , Moreno‐Casbas, M. T. , Sánchez‐Pablo, C. , Bays‐Moneo, A. , Fernández‐Domínguez, J. C. , Rich‐Ruiz, M. , & Gea‐Sánchez, M. (2018). Efficacy of the Otago Exercise Programme to reduce falls in community‐dwelling adults aged 65‐80 years old when delivered as group or individual training. Journal of Advanced Nursing, 74(7), 1700–1711. 10.1111/jan.13583 [DOI] [PubMed] [Google Scholar]
- Alessi, C. A. , Stuck, A. E. , Aronow, H. U. , Yuhas, K. E. , Bula, C. J. , Madison, R. , Gold, M. , Segal‐Gidan, F. , Fanello, R. , Rubenstein, L. Z. , & Beck, J. C. (1997). The process of care in preventive in‐home comprehensive geriatric assessment. Journal of the American Geriatrics Society, 45(9), 1044–1050. [DOI] [PubMed] [Google Scholar]
- Alkan, H. , Topuz, O. , Yildiz, N. , Alkan, S. , Sarsan, A. , & Ardic, F. (2011). Efficacy of home based exercise program and postural biofeedback therapy in reducing risk of falling among osteoporotic women over 65 years of age. Turk Geriatri Dergisi, 14(1), 26–34. http://geriatri.dergisi.org/pdf/pdf_TJG_535.pdf [Google Scholar]
- Alldred, D. P. , Raynor, D. K. , Hughes, C. , Barber, N. , Chen, T. F. , & Spoor, P. (2013). Interventions to optimise prescribing for older people in care homes. Cochrane Database of Systematic Reviews, 2013(2), CD009095. 10.1002/14651858.CD009095.pub2 [DOI] [PubMed] [Google Scholar]
- Allen, K. R. , Hazelett, S. E. , Radwany, S. , Ertle, D. , Fosnight, S. M. , & Moore, P. S. (2012). The Promoting Effective Advance Care for Elders (PEACE) randomized pilot study: Theoretical framework and study design. Population Health Management, 15(2), 71–77. 10.1089/pop.2011.0004 [DOI] [PubMed] [Google Scholar]
- Allen, R. S. , Harris, G. M. , Burgio, L. D. , Azuero, C. B. , Miller, L. A. , Shin, H. J. , Eichorst, M. K. , Csikai, E. L. , DeCoster, J. , Dunn, L. L. , Kvale, E. , & Parmelee, P. (2014). Can senior volunteers deliver reminiscence and creative activity interventions? Results of the legacy intervention family enactment randomized controlled trial. Journal of Pain & Symptom Management, 48(4), 590–601. 10.1016/j.jpainsymman.2013.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen, S. A. (1996). Case management by nurses in the home: An examination of Medicare management and evaluation of the patient plan of care.
- Allen, S. A. (1999). Description and outcomes of a Medicare case management program by nurses. Home Health Care Services Quarterly, 18(2), 43–68. [DOI] [PubMed] [Google Scholar]
- Allen, V. J. , Methven, L. , & Gosney, M. (2014). Impact of serving method on the consumption of nutritional supplement drinks: Randomized trial in older adults with cognitive impairment. Journal of Advanced Nursing, 70(6), 1323–1333. [DOI] [PubMed] [Google Scholar]
- Al‐Sari, U. A. , Tobias, J. H. , & Clark, E. M. (2018). Self‐reported everyday physical activities in older people with osteoporotic vertebral fractures: A systematic review and meta‐analysis. Osteoporosis International, 29(1), 19–29. 10.1007/s00198-017-4287-6 [DOI] [PubMed] [Google Scholar]
- Anderson, O. , Boshier, P. , & Hanna, G. (2012). Interventions designed to prevent healthcare bed‐related injuries in patients. Cochrane Database of Systematic Reviews, 1, CD008931. 10.1002/14651858.CD008931.pub3 [DOI] [PubMed] [Google Scholar]
- Andrew, C. , Najma, S. , Anne, H. , John, Y. , & Rachel, H. (2014). Interventions for preventing delirium in older people in institutional long‐term care. Cochrane Database of Systematic Reviews, 1, CD009537. 10.1002/14651858.CD009537.pub2 [DOI] [PubMed] [Google Scholar]
- Ann, B. K. (1998). The use of a group reminiscence intervention with newly‐admitted nursing home residents. Dissertation Abstracts International: Section B: The Sciences and Engineering, 58(9‐B), 5106. [Google Scholar]
- Ann, G. E. (2002). Effect of a breakfast program on nutritional status, quality of life, and health care use among frail homebound older adults. UMI Dissertation Services, ProQuest Information and Learning, Ann Arbor, MI. http://search.ebscohost.com/login.aspx?direct=true%26db=gnh%26AN=912814%26site=ehost-live
- Antoniak, A. E. , & Greig, C. A. (2017). The effect of combined resistance exercise training and vitamin D‐3 supplementation on musculoskeletal health and function in older adults: A systematic review and meta‐analysis. BMJ Open, 7(7), 014619. 10.1136/bmjopen-2016-014619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anttila, H. , Samuelsson, K. , Salminen, A. L. , & Brandt, A. (2011). Effectiveness of assistive technology interventions for people with disabilities: An overview of systematic reviews. Physiotherapy (United Kingdom), 1, eS74–eS75. 10.1016/j.physio.2011.04.002 [DOI] [Google Scholar]
- Anttila, H. , Samuelsson, K. , Salminen, A. L. , & Brandt, S. (2012). Quality of evidence of assistive technology interventions for people with disability: An overview of systematic reviews. Technology and Disability, 24(1), 9–48. doi 10.3233/TAD‐2012‐0332. [Google Scholar]
- Aoun, S. M. , Grande, G. , Howting, D. , Deas, K. , Toye, C. , Troeung, L. , Stajduhar, K. , & Ewing, G. (2015). The impact of the carer support needs assessment tool (CSNAT) in community palliative care using a stepped wedge cluster trial. PLOS One, 10(4), e0123012. 10.1371/journal.pone.0123012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Applebaum, R. , & Phillips, P. (1990). Assuring the quality of in‐home care: The “other” challenge for long‐term care. Gerontologist, 30, 444–450. [DOI] [PubMed] [Google Scholar]
- Arai, T. , Obuchi, S. , Inaba, Y. , Nagasawa, H. , Shiba, Y. , Watanabe, S. , Kimura, K. , & Kojima, M. (2007). The effects of short‐term exercise intervention on falls self‐efficacy and the relationship between changes in physical function and falls self‐efficacy in Japanese older people—A Randomized controlled trial. American Journal of Physical Medicine & Rehabilitation, 86(2), 133–141. 10.1097/PHM.0b013e31802ef29d [DOI] [PubMed] [Google Scholar]
- Aranda, R. R. (1974). CILS: A model for the social rehabilitation of older persons with severe visual impairment. New York Infirmary, Center for Independent Living, New York, NY. http://search.ebscohost.com/login.aspx?direct=true%26db=gnh%26AN=279%26site=ehost-live
- Arbesman, M. , & Mosley, L. J. (2012). Systematic review of occupation‐ and activity‐based health management and maintenance interventions for community‐dwelling older adults. American Journal of Occupational Therapy, 66(3), 277–283. 10.5014/ajot.2012.003327 [DOI] [PubMed] [Google Scholar]
- Arean, P. A. , Ayalon, L. , Jin, C. , McCulloch, C. E. , Linkins, K. , Chen, H. , McDonnell‐Herr, B. , Levkoff, S. , & Estes, C. (2008). Integrated specialty mental health care among older minorities improves access but not outcomes: Results of the PRISMe study. International Journal of Geriatric Psychiatry, 23(10), 1086–1092. 10.1002/gps.2100 [DOI] [PubMed] [Google Scholar]
- Arif, M. J. , El Emary, I. M. , & Koutsouris, D. D. (2014). A review on the technologies and services used in the self‐management of health and independent living of elderly. Technology & Health Care, 22(5), 677–687. 10.3233/THC-140851 [DOI] [PubMed] [Google Scholar]
- Armstrong, J. J. , Sims‐Gould, J. , & Stolee, P. (2016). Allocation of rehabilitation services for older adults in the ontario home care system. Physiotherapy Canada, 68(4), 346–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnall, D. A. , Iranzo, M. A. C. , Miguel, J. M. T. , Camacho, C. I. , Moral, J. C. M. , & Webb, J. R. (2012). Comparison of patient satisfaction and compliance with two respiratory muscle training programs in the frail elderly. American Journal of Respiratory and Critical Care Medicine. Conference: American Thoracic Society International Conference, ATS, 185(MeetingAbstracts). http://www.atsjournals.org/doi/pdf/10.1164/ajrccm-conference.2012.185.1_MeetingAbstracts.A2881
- Aronson, J. , & Neysmith, S. M. (1996). “You're not just in there to do the work”: Depersonalizing policies and the exploitation of home care workers’ labor. Gender and Society, 10(1), 59–77. 10.1177/0891243296010001005 [DOI] [Google Scholar]
- Ashok, S. (2017). High‐level hands‐free control of wheelchair—A review. Journal of Medical Engineering & Technology, 41(1), 46–64. [DOI] [PubMed] [Google Scholar]
- Ashworth, N. L. , Chad, K. E. , Harrison, E. L. , Reeder, B. A. , & Marshall, S. C. (2005). Home versus center based physical activity programs in older adults. Cochrane Database of Systematic Reviews, 1, CD004017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atienza, A. (2001). Home‐based physical activity programs for middle‐aged and older adults: Summary of empirical research. Journal of aging and physical activity, 9(Suppl), S38–S58. http://search.ebscohost.com/login.aspx?direct=true%26db=gnh%26AN=85431%26site=ehost-live [Google Scholar]
- Auger, C. , Demers, L. , Gelinas, I. , Jutai, J. , Fuhrer, M. J. , & DeRuyter, F. (2008). Powered mobility for middle‐aged and older adults: Systematic review of outcomes and appraisal of published evidence. American Journal of Physical Medicine & Rehabilitation, 87(8), 666–680. 10.1097/PHM.0b013e31816de163 [DOI] [PubMed] [Google Scholar]
- Bahar‐Fuchs, A. , Webb, S. , Bartsch, L. , Clare, L. , Rebok, G. , Cherbuin, N. , & Anstey, K. J. (2017). Tailored and adaptive computerized cognitive training in older adults at risk for dementia: A randomized controlled trial. Journal of Alzheimer's Disease, 60(3), 889–911. 10.3233/JAD-170404 [DOI] [PubMed] [Google Scholar]
- Bainbridge, D. , Seow, H. , & Sussman, J. (2016). Common components of efficacious in‐home end‐of‐life care programs: A review of systematic reviews. Journal of the American Geriatrics Society, 64(3), 632–639. 10.1111/jgs.14025 [DOI] [PubMed] [Google Scholar]
- Baker, K. R. , Nelson, M. E. , Felson, D. T. , Layne, J. E. , Sarno, R. , & Roubenoff, R. (2001). The efficacy of home based progressive strength training in older adults with knee osteoarthritis: A randomized controlled trial. Journal of Rheumatology, 28(7), 1655–1665. [PubMed] [Google Scholar]
- Baker, P. R. , Francis, D. P. , Hairi, N. N. , Othman, S. , & Choo, W. Y. (2016). Interventions for preventing abuse in the elderly. Cochrane Database of Systematic Reviews, 2016(8), CD010321. 10.1002/14651858.CD010321.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakker, T. J. , Duivenvoorden, H. J. , van der Lee, J. , Olde Rikkert, M. G. , Beekman, A. T. , & Ribbe, M. W. (2011). Integrative psychotherapeutic nursing home program to reduce multiple psychiatric symptoms of cognitively impaired patients and caregiver burden: Randomized controlled trial. American Journal of Geriatric Psychiatry, 19(6), 507–520. 10.1097/JGP.0b013e3181eafdc6 [DOI] [PubMed] [Google Scholar]
- Baldwin, C. , Kimber, K. , Gibbs, M. , & Weekes, C. E. (2016). Supportive interventions for enhancing dietary intake in malnourished or nutritionally at‐risk adults. Cochrane Database of Systematic Reviews, 12, CD009840. 10.1002/14651858.CD009840.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes, D. E. , Santos‐Modesitt, W. , Poelke, G. , Kramer, A. F. , Castro, C. , Middleton, L. E. , & Yaffe, K. (2013). The Mental Activity and eXercise (MAX) Trial a randomized controlled trial to enhance cognitive function in older adults. Jama Internal Medicine, 173(9), 797–804. 10.1001/jamainternmed.2013.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bateni, H. , & Maki, B. E. (2005). Assistive devices for balance and mobility: Benefits, demands, and adverse consequences. Archives of Physical Medicine & Rehabilitation, 86(1), 134–145. [DOI] [PubMed] [Google Scholar]
- Bates, A. , Furber, S. , Tiedemann, A. , Ginn, K. , van den Dolder, P. , Kirsten, Howard , Bauman, A. , Chittenden, C. , Franco, L. , Kershaw, M. , & Sherrington, C. (2018). Trial Protocol: Home‐based exercise programs to prevent falls and upper limb dysfunction among community‐dwelling older people: Study protocol for the BEST (Balance Exercise Strength Training) at Home randomised, controlled trial. Journal of Physiotherapy (Elsevier), 64(2), 121. 10.1016/j.jphys.2017.10.001 [DOI] [PubMed] [Google Scholar]
- Belqaid, K. , Brandt, C. F. , Lugnet, K. , Nielsen, A. L. , Pohju, A. , Rasmussen, H. H. , Rasmussen, N. M. L. , & Beck, A. M. (2016). Adding a dietitian to a discharge follow‐home team is cost‐effective for geriatric patients at nutritional risk. Clinical Nutrition. Conference: 38th European Society for Clinical Nutrition and Metabolism Congress, ESPEN. Denmark, 35, S160. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/430/CN-01361430/frame.html
- Bentur, N. , Barnea, T. , & Mizrahi, I. (1996). A follow‐up study of elderly buyers of an assistive chair. Physical and Occupational Therapy in Geriatrics, 14(3), 51–60. [Google Scholar]
- Best, K. L. , Miller, W. C. , Eng, J. J. , Routhier, F. , & Goldsmith, C. (2014). Randomized controlled trial protocol feasibility: The Wheelchair Self‐Efficacy Enhanced for Use (WheelSeeU). Canadian Journal of Occupational Therapy—Revue Canadienne d Ergotherapie, 81(5), 308–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Best, K. L. , Miller, W. C. , Huston, G. , Routhier, F. , & Eng, J. J. (2016). Pilot study of a peer‐led wheelchair training program to improve self‐efficacy using a manual wheelchair: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 97(1), 37–44. 10.1016/j.apmr.2015.08.425 [DOI] [PubMed] [Google Scholar]
- Best, P. M. , & Solomon, B. (1971). Hot meals for the elderly, a meal service with education. Senior Citizen Association of Los Angeles, Los Angeles, CA. http://search.ebscohost.com/login.aspx?direct=true%26db=gnh%26AN=235%26site=ehost-live
- Beurskens, R. (2016). Falls in the elderly and their prevention. Pravention Und Rehabilitation, 28(2), 39–44. 10.5414/NHX01713 [DOI] [Google Scholar]
- Binder, E. F. , Brown, M. , Sinacore, D. R. , Steger‐May, K. , Yarasheski, K. E. , & Schechtman, K. B. (2005). Effects of extended outpatient rehabilitation after hip fracture: A randomized controlled trial. Evidence‐Based Healthcare and Public Health, 292(7), 837–846. 10.1016/j.ehbc.2004.11.002 [DOI] [PubMed] [Google Scholar]
- Bischoff‐Ferrari, H. (2017). Spitex‐SpiTal‐Autonomie‐Reha‐Kraft. https://Clinicaltrials.Gov/Show/Nct03154684. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/203/CN-01494203/frame.html
- Bishop, M. , Dennis, K. , Bishop, L. , Sheppard‐Jones, K. , Bishop, F. , & Frain, M. (2015). The prevalence and nature of modified housing and assistive devices use among Americans with multiple sclerosis. Journal of Vocational Rehabilitation, 42(2), 153–165. 10.3233/JVR-150732 [DOI] [Google Scholar]
- Bismuth, S. , Villars, H. , Durliat, I. , Boyer, P. , & Oustric, S. (2012). Gerontotechnologies likely to enable patients with Soft Cognitive Deficit and Alzheimer's disease at the light stage to stay home. Cahiers de l'Annee Gerontologique, 4(3), 310–319. 10.1007/s12612-012-0308-4 [DOI] [Google Scholar]
- Blackwood, J. , Shubert, T. , Fogarty, K. , & Chase, C. (2016). The impact of a home‐based computerized cognitive training intervention on fall risk measure performance in community dwelling older adults, a pilot study. Journal of Nutrition, Health & Aging, 20(2), 138–145. 10.1007/s12603-015-0598-5 [DOI] [PubMed] [Google Scholar]
- Blake, H. , Mo, P. , Malik, S. , & Thomas, S. (2009). How effective are physical activity interventions for alleviating depressive symptoms in older people? A systematic review. Clinical Rehabilitation, 23(10), 873–887. 10.1177/0269215509337449 [DOI] [PubMed] [Google Scholar]
- Bleijenberg, N. , Imhof, L. , Mahrer‐Imhof, R. , Wallhagen, M. I. , de Wit, N. J. , & Schuurmans, M. J. (2017). Patient characteristics associated with a successful response to nurse‐led care programs targeting the oldest‐old: A comparison of two RCTs. Worldviews on Evidence‐Based Nursing, 14(3), 210–222. 10.1111/wvn.12235 [DOI] [PubMed] [Google Scholar]
- Bleijenberg, N. , Ten Dam, V. H. , Steunenberg, B. , Drubbel, I. , Numans, M. E. , De Wit, N. J. , & Schuurmans, M. J. (2013). Exploring the expectations, needs and experiences of general practitioners and nurses towards a proactive and structured care programme for frail older patients: A mixed‐methods study. Journal of Advanced Nursing, 69(10), 2262–2273. 10.1111/jan.12110 [DOI] [PubMed] [Google Scholar]
- Boland, L. , Legare, F. , Perez, M. M. , Menear, M. , Garvelink, M. M. , McIsaac, D. I. , Guerard, P. G. , Emond, J. , Briere, N. , & Stacey, D. (2017). Impact of home care versus alternative locations of care on elder health outcomes: An overview of systematic reviews. BMC Geriatrics, 17(1), 20. 10.1186/s12877-016-0395-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolscher‐Niehuis, M. J. T. V. , den Ouden, M. E. M. , de Vocht, H. M. , & Francke, A. L. (2016). Effects of self‐management support programmes on activities of daily living of older adults: A systematic review. International Journal of Nursing Studies, 61, 230–247. 10.1016/j.ijnurstu.2016.06.014 [DOI] [PubMed] [Google Scholar]
- Borell, L. (2018). ASSIST 1.0 an Intervention Program Addressing Reablement Services. https://Clinicaltrials.Gov/Show/Nct03505619. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/291/CN-01568291/frame.html
- Boucher, P. , Atrash, A. , Kelouwani, S. , Honore, W. , Nguyen, H. , Villemure, J. , Routhier, F. , Cohen, P. , Demers, L. , Forget, R. , & Pineau, J. (2013). Design and validation of an intelligent wheelchair towards a clinically‐functional outcome. Journal of Neuroengineering & Rehabilitation, 10(1), 58. 10.1186/1743-0003-10-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd, M. L. , Fisher, B. , Davidson, A. W. , & Neilsen, C. A. (1996). Community‐based case management for chronically ill older adults. Nursing Management, 27(11), 31–32. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/679/CN-00134679/frame.html [PubMed] [Google Scholar]
- Brandao, G. S. , Gomes, G. S. B. F. , Callou Sampaio, A. A. , Donner, C. F. , Oliveira, L. V. F. , & Camelier, A. A. (2018). Home exercise improves the quality of sleep and daytime sleepiness of elderlies: A randomized controlled trial. Multidisciplinary Respiratory Medicine, 13(1), 10.1186/s40248-017-0114-3. (no(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun, K. L. , & Rose, C. L. (1987). Geriatric patient outcomes and costs in three settings: Nursing home, foster family, and own home. Journal of the American Geriatrics Society, 35(5), 387–397. [DOI] [PubMed] [Google Scholar]
- Braun, K. L. , Rose, C. L. , & Finch, M. D. (1991). Patient characteristics and outcomes in institutional and community long‐term care. The Gerontologist, 31(5), 648–656. [DOI] [PubMed] [Google Scholar]
- Brettschneider, C. , Luck, T. , Fleischer, S. , Roling, G. , Beutner, K. , Luppa, M. , Behrens, J. , Riedel‐Heller, S. G. , & Konig, H. H. (2015). Cost‐utility analysis of a preventive home visit program for older adults in Germany. BMC Health Services Research, 15, 141. 10.1186/s12913-015-0817-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brismee, J. M. , Paige, R. L. , Chyu, M. C. , Boatright, J. D. , Hagar, J. M. , McCaleb, J. A. , Quintela, M. M. , Feng, D. , Xu, K. T. , & Shen, C. L. (2007). Group and home‐based tai chi in elderly subjects with knee osteoarthritis: A randomized controlled trial. Clinical Rehabilitation, 21(2), 99–111. 10.1177/0269215506070505 [DOI] [PubMed] [Google Scholar]
- Britian, O. (1999). Integration of services for elderly people reduced costs and use of health services [commentary on Bernabei R, Landi F, Gambassi G et al. Randomized trial of impact of model of integrated care and case management for older people living in the community]. Evidence Based Nursing, 2, 20. [Google Scholar]
- Bruun‐Olsen, V. , Heiberg, K. E. , Wahl, A. K. , & Mengshoel, A. M. (2013). The immediate and long‐term effects of a walking‐skill program compared to usual physiotherapy care in patients who have undergone total knee arthroplasty (TKA): A randomized controlled trial. Disability & Rehabilitation, 35(23), 2008–2015. 10.3109/09638288.2013.770084 [DOI] [PubMed] [Google Scholar]
- Bull, M. J. (1994). Use of formal community services by elders and their family caregivers 2 weeks following hospital discharge. Journal of Advanced Nursing, 19(3), 503–508. [DOI] [PubMed] [Google Scholar]
- Cabilan, C. J. , Hines, S. , & Munday, J. (2013). Prehabilitation for surgical patients: A systematic review protocol. JBI Database of Systematic Reviews and Implementation Reports, 11(5), 112–122. [DOI] [PubMed] [Google Scholar]
- Caplan, G. A. , Sulaiman, N. S. , Mangin, D. A. , Ricauda, A. N. , Wilson, A. D. , & Barclay, L. (2010). Is hospital in the home a good option for older people? Journal of the American Geriatrics Society, 1, S7. 10.1111/j.1532-5415.2010.02850.x [DOI] [Google Scholar]
- Cardemil, F. , Esquivel, P. , Barria, T. , Aguayo, L. , Fuente, A. , & Espejo, M. R. (2013). Randomized controlled trial to assess the ace program for rehabilitation in patients with hearing loss. Otolaryngology—Head and Neck Surgery, 1, P108–P109. 10.1177/0194599813495815a223 [DOI] [Google Scholar]
- Carlson, B. L. , Foster, L. , Dale, S. B. , & Brown, R. (2007). Effects of cash and counseling on personal care and well‐being. Health Services Research, 42(1 Pt 2), 467–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson, M. , Vigen, C. L. P. , Rubayi, S. , Blanche, E. I. , Blanchard, J. , Atkins, M. , Bates‐Jensen, B. , Garber, S. , Pyatak, E. , Diaz, J. , Florindez, L. , Hay, J. , Mallinson, T. , Unger, J. , Azen, S. P. , Scott, M. , Cogan, A. , & Clark, F. (2017). Lifestyle intervention for adults with spinal cord injury: Results of the USC‐RLANRC Pressure Ulcer Prevention Study. The Journal of Spinal Cord Medicine, 1–18. 10.1080/10790268.2017.1313931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Challis, D. , Darton, R. , Johnson, L. , Stone, M. , & Traske, K. (1991). An evaluation of an alternative to long‐stay hospital care for frail elderly patients: II. Costs and effectiveness. Age and Ageing, 20(4), 245–254. [DOI] [PubMed] [Google Scholar]
- Chan, A. W. K. , Yu, D. S. F. , Choi, K. C. , Chan, H. Y. L. , & Wong, E. M. L. (2016). Effects of a peer‐assisted tai‐chi‐qigong programme on social isolation and psychological wellbeing in Chinese hidden elders: A pilot randomised controlled trial. The Lancet, 388, S23. [Google Scholar]
- Chan, A. W. , Yu, D. S. , & Choi, K. C. (2017). Effects of tai chi qigong on psychosocial well‐being among hidden elderly, using elderly neighborhood volunteer approach: A pilot randomized controlled trial. Clinical Interventions in Aging, 12, 85–96. 10.2147/CIA.S124604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, R. J. , Webster, J. , & Bowers, A. (2016). End‐of‐life care pathways for improving outcomes in caring for the dying. The Cochrane Database of Systematic Reviews, 2, CD008006. 10.1002/14651858.CD008006.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler, D. , & Knackert, B. (1997). Positioners for wheelchairs in long‐term‐care facilities. American Journal of Occupational Therapy, 51(10), 921–924. [DOI] [PubMed] [Google Scholar]
- Chesbro, S. , Conti, G. , & Williams, B. (2005). Using the assessing the learning strategies of adults tool with older adults: Comparisons based on age and functional ability. Topics in Geriatric Rehabilitation, 21(4), 323–331. [Google Scholar]
- Chiatti, C. , Rimland, J. , Bonfranceschi, F. , Masera, F. , Bustacchini, S. , & Cassetta, L. (2015). The UP‐TECH project, an intervention to support caregivers of Alzheimer's disease patients in Italy: Preliminary findings on recruitment and caregiving burden in the baseline population. Aging and Mental Health, 19(6), 517–525. [DOI] [PubMed] [Google Scholar]
- Chien, C. L. , Lee, C. M. , Wu, Y. W. , Chen, T. A. , & Wu, Y. T. (2008). Home‐based exercise increases exercise capacity but not quality of life in people with chronic heart failure: A systematic review. Australian Journal of Physiotherapy, 54(2), 87–93. [DOI] [PubMed] [Google Scholar]
- Childress, S. , Brubaker, P. H. , Amico, L. A. , Nesbit, B. A. , Williams, C. M. , & Rejeski, J. W. (2008). Patterns of physical activity before and after an exercise intervention in overweight/obese older adults with CVD or the metabolic syndrome. Journal of Cardiopulmonary Rehabilitation and Prevention, 28(4), 268. [Google Scholar]
- Chiu, C. W. , & Man, D. W. (2004). The effect of training older adults with stroke to use home‐based assistive devices. OTJR Occupation, Participation and Health, 24(3), 113–120. [Google Scholar]
- Chiu, M. , Pauley, T. , Wesson, V. , Pushpakumar, D. , & Sadavoy, J. (2015). Evaluation of a problem‐solving (PS) techniques‐based intervention for informal carers of patients with dementia receiving in‐home care. International Psychogeriatrics, 27(6), 937–948. [DOI] [PubMed] [Google Scholar]
- Choi, N. G. , Hegel, M. T. , Marti, C. N. , Marinucci, M. L. , Sirrianni, L. , & Bruce, M. L. (2014). Telehealth problem‐solving therapy for depressed low‐income homebound older adults. American Journal of Geriatric Psychiatry, 22(3), 263–271. 10.1016/j.jagp.2013.01.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choyce, J. , Shaw, K. L. , Sitch, A. J. , Mistry, H. , Whitehouse, J. L. , & Nash, E. F. (2017). A prospective pilot study of home monitoring in adults with cystic fibrosis (HOME‐CF): Protocol for a randomised controlled trial. BMC Pulmonary Medicine, 17(1), 22. 10.1186/s12890-017-0366-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christine, O. , Ingeborg, P. , Astrid, B. , Marie‐José, E.‐S. , & Camilla, I. (2016). Effect of animal‐assisted activity on balance and quality of life in home‐dwelling persons with dementia. Geriatric Nursing, 37(4), 284–291. [DOI] [PubMed] [Google Scholar]
- Chung, P. K. , & Zhao, Y. N. (2016). Effectiveness of a balance‐improved exercise prorgam for enhancing functional fitness of older adults: A randomized, controlled trial. International journal of behavioral medicine, 23, S247. [Google Scholar]
- Cifu, D. (2010). Geriatric rehabilitation services in the veterans health administration. Generations, 34(2), 64–73. [Google Scholar]
- Ciliska, D. , Hayward, S. , Thomas, H. , Mitchell, A. , Dobbins, M. , Underwood, J. , Rafael, A. , & Martin, E. (1996). A systematic overview of the effectiveness of home visiting as a delivery strategy for public health nursing interventions. Canadian Journal of Public Health. Revue Canadienne de Sante Publique, 87(3), 193–198. [PubMed] [Google Scholar]
- Cky, L. , & Wan, X. (2017). Using prompted voiding to manage urinary incontinence in nursing homes: Can it be sustained? Journal of the American Medical Directors Association, 18(6), 509–514. 10.1016/j.jamda.2016.12.084 [DOI] [PubMed] [Google Scholar]
- Claes‐Eric, N. , & Agneta, S. (1991). Mobility and transport for elderly and disabled persons: Proceedings of a conference held at Stockholmsmassan, Alvsjo, Sweden, May 21–24, 1989, organized by the Swedish Board of Transport in co‐operation with the Department of Traffic Planning and Engineer. Transportation studies, v. 13. Gordon and Breach Science Publishers, Philadelphia, PA.
- Clark, H. (1998). Keeping the house up. Community Care, 16, 22–23. [Google Scholar]
- Clarke, P. , & Colantonio, A. (2005). Wheelchair use among community‐dwelling older adults: Prevalence and risk factors in a national sample. Canadian Journal on Aging, 24(2), 191–198. [DOI] [PubMed] [Google Scholar]
- Clemson, L. , Singh, M. A. F. , Bundy, A. , Cumming, R. G. , Manollaras, K. , O'Loughlin, P. , & Black, D. (2012). Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): Randomised parallel trial. BMJ, 345, e4547. 10.1136/bmj.e4547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman, B. J. (1995). European models of long‐term care in the home and community. International Journal of Health Services, 25(3), 455–474. [DOI] [PubMed] [Google Scholar]
- Connell, P. G. O. , & Gnatz, S. (1989). Hemiplegia and amputation: Rehabilitation in the dual disability. Archives of Physical Medicine & Rehabilitation, 70(6), 451–454. [DOI] [PubMed] [Google Scholar]
- Cook, M. , Esme, D. , Katie, S. , Ian, J. , Reem, M. , Vugt, D. , Marjolein, & Frans, V. (2012). Functional analysis‐based interventions for challenging behaviour in dementia. Cochrane Database of Systematic Reviews, 2, CD006929. 10.1002/14651858.CD006929.pub2 [DOI] [PubMed] [Google Scholar]
- Coster, S. , Watkins, M. , & Norman, I. J. (2018). What is the impact of professional nursing on patients’ outcomes globally? An overview of research evidence. International Journal of Nursing Studies, 78, 76–83. 10.1016/j.ijnurstu.2017.10.009 [DOI] [PubMed] [Google Scholar]
- Cyarto, E. V. , Brown, W. J. , & Marshall, A. L. (2006). Retention, adherence and compliance: Important considerations for home‐ and group‐based resistance training programs for older adults. Journal of Science and Medicine in Sport, 9(5), 402–412. 10.1016/j.jsams.2006.06.020 [DOI] [PubMed] [Google Scholar]
- Dale, S. B. , & Brown, R. (2006). Reducing nursing home use through consumer‐directed personal care services. Medical Care, 44(8), 760–767. [DOI] [PubMed] [Google Scholar]
- Dalton, J. , Thomas, S. , Harden, M. , Eastwood, A. , & Parker, G. (2018). Updated meta‐review of evidence on support for carers. Journal of Health Services Research and Policy, 23, 196–207. 10.1177/1355819618766559 [DOI] [PubMed] [Google Scholar]
- Daly, I. M. (2012). Rehabilitation interventions for pain and disability in osteoarthritis: A review of interventions including exercise, manual techniques, and assistive devices. Orthopaedic Nursing, 31(2), 103–108. 10.1079/nor.0b013e31824fce07 [DOI] [PubMed] [Google Scholar]
- Danilovich, M. K. , Hughes, S. L. , Corcos, D. M. , Marquez, D. X. , & Eisenstein, A. R. (2017). Translating strong for life into the community care program: Lessons learned. Journal of Applied Gerontology, 36(5), 553–569. 10.1177/0733464815625833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dapp, U. , Anders, J. A. , Renteln‐Kruse, W. , Minder, C. E. , Meier‐Baumgartner, H. P. , Swift, C. G. , Gillmann, G. , Egger, M. , Beck, J. C. , & Stuck, A. E. (2011). A randomized trial of effects of health risk appraisal combined with group sessions or home visits on preventive behaviors in older adults. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 66(5), 591–598. 10.1093/gerona/glr021 [DOI] [PubMed] [Google Scholar]
- Davison, T. E. , Nayer, K. B. I. , Coxon, S. , De Bono, A. , Eppingstall, B. , Jeon, Y.‐H. , van der Ploeg, E. S. , & O'Connor, D. W. (2016). A personalized multimedia device to treat agitated behavior and improve mood in people with dementia: A pilot study. Geriatric Nursing, 37(1), 25–29. [DOI] [PubMed] [Google Scholar]
- Day, L. , Hill, K. D. , Jolley, D. , Cicuttini, F. M. , Flicker, L. , & Segal, L. (2012). Impact of Tai Chi on impairment, functional limitation, and disability among preclinically disabled older people: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 93(8), 1400–1407. 10.1016/j.apmr.2012.03.018 [DOI] [PubMed] [Google Scholar]
- de Roos, P. , Lucas, C. , Strijbos, J. H. , & van Trijffel, E. (2018). Effectiveness of a combined exercise training and home‐based walking programme on physical activity compared with standard medical care in moderate COPD: A randomised controlled trial. Physiotherapy, 104(1), 116–121. 10.1016/j.physio.2016.08.005 [DOI] [PubMed] [Google Scholar]
- de van der Schueren, M. , & Roodenburg, A. (2017). Increase protein intake of older meal service clients with readymade protein‐rich meals and foods. https://Clinicaltrials.Gov/Show/Nct03032237. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/535/CN-01561535/frame.html
- de Vries, N. M. , Staal, J. B. , van der Wees, P. J. , Adang, E. M. , Akkermans, R. , Olde Rikkert, M. G. , & Nijhuis‐van der Sanden, M. W. (2016). Patient‐centred physical therapy is (cost‐) effective in increasing physical activity and reducing frailty in older adults with mobility problems: A randomized controlled trial with 6months follow‐up. Journal of Cachexia, Sarcopenia and Muscle, 7(4), 422–435. 10.1002/jcsm.12091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del, A. M. , Lisa, C. , & Louisa, L. (2006). Functional interdependence. Australasian Journal on Ageing, 25(3), 134–139. [Google Scholar]
- Delbaere, K. , Bourgois, J. , Noortgate, V. , Den, N. , Vanderstraeten, G. , Willems, T. , & Cambier, D. (2006). A home‐based multidimensional exercise program reduced physical impairment and fear of falling. Acta Clinica Belgica, 61(6), 340–350. [DOI] [PubMed] [Google Scholar]
- Dellasega, C. , & Zerbe, T. (2002). Caregivers of frail rural older adults: Effects of an advanced practice nursing intervention. Journal of Gerontological Nursing, 28(10), 40–49. [DOI] [PubMed] [Google Scholar]
- Der‐Fa, L. , Hart, L. , Lutgendorf, S. , & Perkhounkova, Y. (2013). The effect of healing touch on the pain and mobility of persons with osteoarthritis: A feasibility study. Geriatric Nursing, 34(4), 314–322. [DOI] [PubMed] [Google Scholar]
- Dohrn, I. M. , Hagstromer, M. , Hellenius, M. L. , & Stahle, A. (2017). Short‐ and long‐term effects of balance training on physical activity in older adults with osteoporosis: A randomized controlled trial. Journal of Geriatric Physical Therapy, 40(2), 102–111. 10.1519/jpt.0000000000000077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson, C. (1990). Willingness to pay for publicly‐provided goods—A possible measure of benefit? Journal of Health Economics, 9(1), 103–118. [DOI] [PubMed] [Google Scholar]
- Donaldson, C. , & Bond, J. (1991). Cost of continuing‐care facilities in the evaluation of experimental national health service nursing homes. Age and Ageing, 20(May 91), 160–168. [DOI] [PubMed] [Google Scholar]
- Douglas, J. W. , & Lawrence, J. C. (2015). Environmental considerations for improving nutritional status in older adults with dementia: A narrative review. Journal of the Academy of Nutrition & Dietetics, 115(11), 1815–1831. 10.1016/j.jand.2015.06.376 [DOI] [PubMed] [Google Scholar]
- Douma, J. G. , Volkers, K. M. , Vuijk, J. P. , Sonneveld, M. H. , Goossens, R. H. , & Scherder, E. J. (2015). The effects of observation of walking in a living room environment, on physical, cognitive, and quality of life related outcomes in older adults with dementia: A study protocol of a randomized controlled trial. BMC Geriatrics, 15, 26. 10.1186/s12877-015-0024-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dozeman, E. , van Marwijk, H. W. J. , van Schaik, D. J. F. , Smit, F. , Stek, M. L. , van der Horst, H. E. , Bohlmeijer, E. T. , & Beekman, A. T. F. (2012). Contradictory effects for prevention of depression and anxiety in residents in homes for the elderly: A pragmatic randomized controlled trial. International Psychogeriatrics, 24(8), 1242–1251. 10.1017/S1041610212000178 [DOI] [PubMed] [Google Scholar]
- Dozeman, E. , van Schaik, D. J. F. , van Marwijk, H. W. J. , Stek, M. L. , Beekman, A. T. , & van der Horst, H. E. (2011). Feasibility and effectiveness of activity‐scheduling as a guided self‐help intervention for the prevention of depression and anxiety in residents in homes for the elderly: A pragmatic randomized controlled trial. International Psychogeriatrics, 23(6), 969–978. 10.1017/s1041610211000202 [DOI] [PubMed] [Google Scholar]
- Dreizler, J. , Koppitz, A. , Probst, S. , & Mahrer‐Imhof, R. (2014). Including nurses in care models for older people with mild to moderate depression: An integrative review. Journal of Clinical Nursing, 23(7–8), 911–926. 10.1111/jocn.12237 [DOI] [PubMed] [Google Scholar]
- Drummond, A. E. , Whitehead, P. , Fellows, K. , Sprigg, N. , Sampson, C. J. , Edwards, C. , & Lincoln, N. B. (2013). Occupational therapy predischarge home visits for patients with a stroke (HOVIS): Results of a feasibility randomized controlled trial. Clinical Rehabilitation, 27(5), 387–397. 10.1177/0269215512462145 [DOI] [PubMed] [Google Scholar]
- Duckworth, J. , Repede, E. , & Elliott, L. (2013). Nurse practitioners aiding frail elderly through home visits. Home Health Care Management & Practice, 25(5), 212–216. 10.1177/1084822313484760 [DOI] [Google Scholar]
- Dumoulin, C. , Hay‐Smith, J. , Habée‐Séguin, G. , Mac, & Mercier, J. (2014). Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews, 10(10), CD005654. [DOI] [PubMed] [Google Scholar]
- Eklund, K. , Wilhelmson, K. , Gustafsson, H. , Landahl, S. , & Dahlin‐Ivanoff, S. (2013). One‐year outcome of frailty indicators and activities of daily living following the randomised controlled trial: “Continuum of care for frail older people”. BMC Geriatrics, 13, 76. 10.1186/1471-2318-13-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbadawy, M. A. (2017). Effectiveness of periosteal stimulation therapy and home exercise program in the rehabilitation of patients with advanced knee osteoarthritis. Clinical Journal of Pain, 33(3), 254–263. 10.1097/AJP.0000000000000404 [DOI] [PubMed] [Google Scholar]
- El‐Khoury, F. , Cassou, B. , Latouche, A. , Aegerter, P. , Charles, M. A. , & Dargent‐Molina, P. (2015). Effectiveness of two year balance training programme on prevention of fall induced injuries in at risk women aged 75‐85 living in community: Ossebo randomised controlled trial. BMJ, 351, h3830. 10.1136/bmj.h3830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engberg, S. , McDowell, B. J. , Weber, E. , Brodak, I. , Donovan, N. , & Engberg, R. (1997). Assessment and management of urinary incontinence among homebound older adults: A clinical trial protocol. Advanced Practice Nursing Quarterly, 3(2), 48–56. [PubMed] [Google Scholar]
- Fahlman, M. M. , Topp, R. , McNevin, N. , Morgan, A. L. , & Boardley, D. J. (2007). Structured exercise in older adults with limited functional ability. Journal of Gerontological Nursing, 33(6), 32–39. [DOI] [PubMed] [Google Scholar]
- Fairhall, N. , Sherrington, C. , Lord, S. , Susan, K. , & Cameron, I. D. (2015). A multifactorial interdisciplinary intervention reduces frailty, increases function and is cost‐effective in older adults who are frail: Randomised controlled trial. Physiotherapy (United Kingdom), 1, eS371–eS372. 10.1016/j.physio.2015.03.588 [DOI] [Google Scholar]
- Fances, M. H. (2011). The prevention of patient falls in healthcare settings, with particular emphasis on the effect of bedrail use on falls and injury as part of multi‐faceted interventions.
- Fanning, J. , Walkup, M. , Ambrosius, W. , Brawley, L. , Ip, E. , Marsh, A. , & Rejeski, J. W. (2018). Change in health‐related quality of life and social cognitive outcomes in obese, older adults in a randomized controlled weight loss trial: Does physical activity behavior matter? Journal of Behavioral Medicine, 41(3), 299–308. 10.1007/s10865-017-9903-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer, B. C. , Croteau, K. A. , Richeson, N. E. , & Jones, D. B. (2006). Using pedometers as a strategy to increase the daily steps of older adults with chronic illness: From research to practice. Home Healthcare Nurse, 24(7), 449–456. [DOI] [PubMed] [Google Scholar]
- Feldman, P. H. , Murtaugh, C. M. , Pezzin, L. E. , McDonald, M. V. , & Peng, T. R. (2005). Just‐in‐time evidence‐based e‐mail “reminders” in home health care: Impact on patient outcomes. Health Services Research, 40(3), 865–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez‐Barres, S. , Garcia‐Barco, M. , Basora, J. , Martinez, T. , Pedret, R. , & Arija, V. (2017). The efficacy of a nutrition education intervention to prevent risk of malnutrition for dependent elderly patients receiving Home Care: A randomized controlled trial. International Journal of Nursing Studies, 70, 131–141. 10.1016/j.ijnurstu.2017.02.020 [DOI] [PubMed] [Google Scholar]
- Fields, N. L. , Anderson, K. A. , & Dabelko‐Schoeny, H. (2014). The effectiveness of adult day services for older adults: A review of the literature from 2000 to 2011. Journal of Applied Gerontology, 33(2), 130–163. 10.1177/0733464812443308 [DOI] [PubMed] [Google Scholar]
- Finkelstein, E. , & Fuller, K. (2012). Measuring the benefit to the homebound, frail older adult of a collaborative effort between a social services agency and an academic geriatric house call program. Journal of the American Geriatrics Society, 4, S174–S175. 10.1111/j.1532-5415.2012.04000.x [DOI] [Google Scholar]
- Fischer, S. M. , Cervantes, L. , Fink, R. M. , & Kutner, J. S. (2015). Apoyo con Carino: A pilot randomized controlled trial of a patient navigator intervention to improve palliative care outcomes for Latinos with serious illness. Journal of Pain & Symptom Management, 49(4), 657–665. 10.1016/j.jpainsymman.2014.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgerald, J. F. , Smith, D. M. , Martin, D. K. , Freedman, J. A. , & Katz, B. P. (1994). A case manager intervention to reduce readmissions. Archives of Internal Medicine, 154(15), 1721–1729. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/240/CN-00103240/frame.html [PubMed] [Google Scholar]
- Fleet, E. , Gopal, R. G. , Patel, B. , Cookson, B. , Charlett, A. , Bowman, C. , & Davey, P. (2014). Impact of implementation of a novel antimicrobial stewardship tool on antibiotic use in nursing homes: A prospective cluster randomized control pilot study. Journal of Antimicrobial Chemotherapy, 69(8), 2265–2273. 10.1093/jac/dku115 [DOI] [PubMed] [Google Scholar]
- Flora, P. , & Faulkner, G. E. (2006). Physical activity: An innovative context for intergenerational programming. Journal of Intergenerational Relationships, 4(4), 63–74. [Google Scholar]
- Forbes, D. (2002). Review: Home visiting with multidimensional assessment and multiple visits reduces nursing home admissions in low risk elderly people. Evidence Based Nursing, 5(4), 118. [DOI] [PubMed] [Google Scholar]
- Forster, A. , Airlie, J. , Birch, K. , Cicero, R. , Cundill, B. , Ellwood, A. , Godfrey, M. , Graham, L. , Green, J. , Hulme, C. , Lawton, R. , McLellan, V. , McMaster, N. , & Farrin, A. (2017). Research Exploring Physical Activity in Care Homes (REACH): Study protocol for a randomised controlled trial. Trials, 18(1), 182. 10.1186/s13063-017-1921-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forster, A. , Young, J. , Lambley, R. , & Langhorne, P. (2008). Medical day hospital care for the elderly versus alternative forms of care. Cochrane Database of Systematic Reviews, 4, CD001730. 10.1002/14651858.CD001730.pub2 [DOI] [PubMed] [Google Scholar]
- Fowler, C. , & Kim, M. T. (2015). Home visits by care providers—Influences on health outcomes for caregivers of homebound older adults with dementia. Geriatric Nursing, 36(1), 25–29. 10.1016/j.gerinurse.2014.09.002 [DOI] [PubMed] [Google Scholar]
- Galle, F. , Onofrio, D. , V., Spica, V. R. , Mastronuzzi, R. , Krauss, P. R. , Belfiore, P. , Buono, P. , & Liguori, G. (2017). Improving physical fitness and health status perception in community‐dwelling older adults through a structured program for physical activity promotion in the city of Naples, Italy: A randomized controlled trial. Geriatrics & Gerontology International, 17(10), 1421–1428. 10.1111/ggi.12879 [DOI] [PubMed] [Google Scholar]
- Gary, R. (2006). Exercise self‐efficacy in older women with diastolic heart failure: Results of a walking program and education intervention. Journal of Gerontological Nursing, 32(7), 31–39. [DOI] [PubMed] [Google Scholar]
- Ghassemzadeh, R. , Nasseh, H. , Arastoo, A. A. , Kamali, M. , Foroushani, R. , A., & Arzaghi, M. (2013). Quality of life in elderly diabetic: Comparison between home and nursing home. Acta Medica Iranica, 51(4), 254–259. [PubMed] [Google Scholar]
- Gianoudis, J. , Bailey, C. , Ebeling, P. , Nowson, C. , Sanders, K. , Hill, K. , & Daly, R. (2011). Effects of a targeted multimodal exercise program incorporating high‐speed power training on falls and fracture risk factors in older adults: A community‐based randomized controlled trial. Journal of Science and Medicine in Sport, 14, e12. 10.1016/j.jsams.2011.11.026 [DOI] [PubMed] [Google Scholar]
- Gibson, T. S. (2002). Effects of a home‐based resistance training program on physical function and strength in a group of older adults.
- Gielen, A. C. , Shields, W. , Frattaroli, S. , McDonald, E. , Jones, V. , Bishai, D. , O'Brocki, R. , Perry, E. C. , Bates‐Hopkins, B. , Tracey, P. , & Parsons, S. (2013). Enhancing fire department home visiting programs: Results of a community intervention trial. Journal of Burn Care & Research, 34(4), e250–e256. 10.1097/BCR.0b013e3182685b3a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giesbrecht, E. M. , Mortenson, W. B. , & Miller, W. C. (2012). Prevalence and facility level correlates of need for wheelchair seating assessment among long‐term care residents. Gerontology, 58(4), 378–384. 10.1159/000334819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gine‐Garriga, M. , Guerra, M. , Pages, E. , Manini, T. M. , Jimenez, R. , & Unnithan, V. B. (2010). The effect of functional circuit training on physical frailty in frail older adults: A randomized controlled trial. Journal of aging and physical activity, 18(4), 401–424. 10.1123/japa.18.4.401 [DOI] [PubMed] [Google Scholar]
- Giordano, A. , Bonometti, G. P. , Vanoglio, F. , Paneroni, M. , Bernocchi, P. , Comini, L. , & Giordano, A. (2016). Feasibility and cost‐effectiveness of a multidisciplinary home‐telehealth intervention programme to reduce falls among elderly discharged from hospital: Study protocol for a randomized controlled trial. BMC Geriatrics, 16(1), 209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gleeson, M. , Sherrington, C. , Borkowski, E. , & Keay, L. (2014). Improving balance and mobility in people over 50 years of age with vision impairments: Can the Alexander Technique help? A study protocol for the VISIBILITY randomised controlled trial. Injury Prevention, 20(1), 3. 10.1136/injuryprev-2012-040726 [DOI] [PubMed] [Google Scholar]
- Goedendorp, M. M. , Kuiper, D. , Reijneveld, S. A. , Sanderman, R. , & Steverink, N. (2017). Sustaining program effectiveness after implementation: The case of the self‐management of well‐being group intervention for older adults. Patient Education and Counseling, 100(6), 1177–1184. 10.1016/j.pec.2017.01.006 [DOI] [PubMed] [Google Scholar]
- Gordon, D. S. (1990). Night care: The evaluation of an experimental night sitter service in Aberdeen. Social Services Research, 1990(1), 24–36. [Google Scholar]
- Gosman‐Hedstrom, G. , Claesson, L. , Blomstrand, C. , Fagerberg, B. , & Lundgren‐Lindquist, B. (2002). Use and cost of assistive technology the first year after stroke. A randomized controlled trial. International Journal of Technology Assessment in Health Care, 18(3), 520–527. [PubMed] [Google Scholar]
- Gothe, N. P. , Fanning, J. , Awick, E. , Chung, D. , Wojcicki, T. R. , Olson, E. A. , Mullen, S. P. , Voss, M. , Erickson, K. I. , Kramer, A. F. , & McAuley, E. (2014). Executive function processes predict mobility outcomes in older adults. Journal of the American Geriatrics Society, 62(2), 285–290. 10.1111/jgs.12654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graff, M. J. , Vernooij‐Dassen, M. J. , Hoefnagels, W. H. , Dekker, J. , & de Witte, P. L. (2003). Occupational therapy at home for older individuals with mild to moderate cognitive impairments and their primary caregivers: A pilot study. Occupation, Participation & Health, 23(4), 155–164. [Google Scholar]
- Graham‐Phillips, A. , Roth, D. L. , Huang, J. , Dilworth‐Anderson, P. , & Gitlin, L. N. (2016). Racial and ethnic differences in the delivery of the resources for enhancing Alzheimer's caregiver health II intervention. Journal of the American Geriatrics Society, 64(8), 1662–1667. 10.1111/jgs.14204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray, Y. L. , & Sedhom, L. (1997). Client satisfaction: Traditional care versus cluster care. Journal of Professional Nursing, 13(1), 56–61. [DOI] [PubMed] [Google Scholar]
- Griffiths, P. (2000). Early discharge plus home based rehabilitation reduced length of initial hospital stay but did not improve health related quality of life in patients with acute stroke. Evidence Based Nursing, 3, 127. http://search.ebscohost.com/login.aspx?direct=true%26db=ccm%26AN=107143327%26site=ehost-live [Google Scholar]
- Griffiths, P. (2013). PROTOCOL: Evaluating the CG ASSIST Program for Caregiving Dyads. https://Clinicaltrials.Gov/Show/Nct02021565. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/006/CN-01480006/frame.html
- Gros, A. , David, R. , Chung, P.‐C. , Chicheportiche, L. , Moy, L. , Stoutz, D. J. , Guetin, S. , Bremond, F. , & Robert, P. (2016). First results from the SafEE project: Safe & Easy Environment for Alzheimer's disease and related disorders. Gerontechnology, 15, 80. [Google Scholar]
- Guidetti, S. , Andersson, K. , Andersson, M. , Tham, K. , & Koch, V. L. (2010). Client‐centred self‐care intervention after stroke: A feasibility study. Scandinavian journal of occupational therapy, 17(4), 276–285. 10.3109/11038120903281169 [DOI] [PubMed] [Google Scholar]
- Guidon, M. , & McGee, H. (2013). One‐year effect of a supervised exercise programme on functional capacity and quality of life in peripheral arterial disease. Disability & Rehabilitation, 35(5), 397–404. 10.3109/09638288.2012.694963 [DOI] [PubMed] [Google Scholar]
- Guitard, P. , Sveistrup, H. , Fahim, A. , & Leonard, C. (2013). Smart grab bars: A potential initiative to encourage bath grab bar use in community dwelling older adults. Assistive Technology, 25(3), 139–148. 10.1080/10400435.2012.732654 [DOI] [PubMed] [Google Scholar]
- Haines, T. P. , Russell, T. , Brauer, S. G. , Erwin, S. , Lane, P. , Urry, S. , Jasiewicz, J. , & Condie, P. (2009). Effectiveness of a video‐based exercise programme to reduce falls and improve health‐related quality of life among older adults discharged from hospital: A pilot randomized controlled trial. Clinical Rehabilitation, 23(11), 973–985. 10.1177/0269215509338998 [DOI] [PubMed] [Google Scholar]
- Halvarsson, A. , Franzen, E. , & Stahle, A. (2015). Balance training with multi‐task exercises improves fall‐related self‐efficacy, gait, balance performance and physical function in older adults with osteoporosis: A randomized controlled trial. Clinical Rehabilitation, 29(4), 365–375. 10.1177/0269215514544983 [DOI] [PubMed] [Google Scholar]
- Hariprasad, V. R. , Sivakumar, P. T. , Koparde, V. , Varambally, S. , Thirthalli, J. , Varghese, M. , Basavaraddi, I. V. , & Gangadhar, B. N. (2013). Effects of yoga intervention on sleep and quality‐of‐life in elderly: A randomized controlled trial. Indian Journal of Psychiatry, 55(7), S364–S368. 10.4103/0019-5545.116310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison, M. B. , Graham, I. D. , Lorimer, K. , Vandenkerkhof, E. , Buchanan, M. , Wells, P. S. , Brandys, T. , & Pierscianowski, T. (2008). Nurse clinic versus home delivery of evidence‐based community leg ulcer care: A randomized health services trial. BMC Health Services Research, 8, 243. 10.1186/1472-6963-8-243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauer, K. (2015). Home‐based exercise training following ward-based rehabilitation in geriatric patients with cognitive impairment. http://Isrctn.Com/Isrctn82378327. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/168/CN-01308168/frame.html
- Hayashi, N. , Morihara, T. , Kazui, H. , Kono, A. , Iwase, M. , Hamasaki, T. , Hata, Y. , Kuwata, N. , Murata, K. , Shinke, A. , Okuda, M. , & Takeda, M. (2011). Cognitive training on elderly Japanese in Osaka: Major outcome (ADAS) from prospective, randomized, open, blindendpoint trial. Alzheimer's and Dementia, 1, S644. 10.1016/j.jalz.2011.05.1846 [DOI] [Google Scholar]
- Health Quality Ontario (2008). Social isolation in community-dwelling seniors: An evidence-based analysis. Ontario Health Technology Assessment Series, 8(5), 1–49. http://ovidsp.ovid.com/ovidweb.cgi?T=JS%26CSC=Y%26NEWS=N%26PAGE=fulltext%26D=prem%26AN=23074510 [PMC free article] [PubMed] [Google Scholar]
- Heneka, N. , Shaw, T. , Rowett, D. , & Phillips, J. (2016). Identifying the scope and impact of opioid medication errors in adult palliative care and oncology settings: A systematic review. Palliative Medicine, 30(6), NP184–NP185. 10.1177/0269216316646056 [DOI] [PubMed] [Google Scholar]
- Hennig, T. R. , Costa, M. J. , Rossi, A. G. , & Moraes, A. B. (2012). Auditory rehabilitation effects on the temporal ordering ability in elderly hearing aids users. Jornal Da Sociedade Brasileira de Fonoaudiologia, 24(1), 26–33. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/638/CN-00849638/frame.html [DOI] [PubMed] [Google Scholar]
- Henrard, J. C. (1991). Care for elderly people in the European Community. Social Policy and Administration, 25, 184–192. [Google Scholar]
- Herke, M. , Fink, A. , Langer, G. , Wustmann, T. , Watzke, S. , Hanff, A.‐M. , & Burckhardt, M. (2018). Environmental and behavioural modifications for improving food and fluid intake in people with dementia. The Cochrane Database of Systematic Reviews, 7, CD011542. 10.1002/14651858.CD011542.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hile, E. , Neuhold, R. , & Davidson, V. (2018). Training for the fight: Adherence to a novel prehab approach in pancreaticoduodenectomy. Rehabilitation Oncology, 36(1), E8. 10.1097/01.REO.0000000000000098 [DOI] [Google Scholar]
- Hinkka, K. , Karppi, S. L. , Pohjolainen, T. , Rantanen, T. , Puukka, P. , & Tilvis, R. (2007). Network‐based geriatric rehabilitation for frail elderly people: Feasibility and effects on subjective health and pain at one year. Journal of Rehabilitation Medicine, 39(6), 473–478. [DOI] [PubMed] [Google Scholar]
- Hinrichs, T. , Moschny, A. , Brach, M. , Wilm, S. , Klaassen‐Mielke, R. , Trampisch, M. , & Platen, P. (2011). Effects of an exercise programme for chronically ill and mobility‐restricted elderly with structured support by the general practitioner's practice (HOMEfit)—Study protocol of a randomised controlled trial. Trials, 12, 263. 10.1186/1745-6215-12-263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiroko, K. (2003). The effects of aromatherapy with the scent of lavender on the psychological well‐being on elderly adults.
- Hirsch, C. (2015). 2015—An elastic band exercise program improved fitness in older adults who use wheelchairs in nursing homes. ACP Journal Club, 162(4), 1. http://search.ebscohost.com/login.aspx?direct=true%26db=ccm%26AN=103760304%26site=ehost-live [DOI] [PubMed] [Google Scholar]
- Hofstad, H. , Naess, H. , Moe‐Nilssen, R. , & Skouen, J. S. (2013). Early supported discharge after stroke in Bergen (ESD Stroke Bergen): A randomized controlled trial comparing rehabilitation in a day unit or in the patients’ homes with conventional treatment. International Journal of Stroke, 8(7), 582–587. 10.1111/j.1747-4949.2012.00825.x [DOI] [PubMed] [Google Scholar]
- Holthe, T. , Halvorsrud, L. , Karterud, D. , Hoel, K. A. , & Lund, A. (2018). Usability and acceptability of technology for community‐dwelling older adults with mild cognitive impairment and dementia: A systematic literature review. Clinical interventions in aging, 13, 863–886. 10.2147/CIA.S154717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hongdao, M. (2004). The demand for personal assistance: Do price and information matter?
- Hooper, L. , Bunn, K. , Jimoh, F. O. , & Wilsher, H. S. (2014). Effectiveness of factors to reduce the risk of dehydration in older people living in residential care: A systematic review. European Geriatric Medicine, 1, S70. [Google Scholar]
- Hori, M. , Iizuka, M. , Nakamura, M. , Aiba, I. , Saito, Y. , Kubota, M. , Urabe, M. , & Kinoshita, A. (2014). At‐home music therapy intervention using video phone (Skype) for elderly people with dementia. Gan to kagaku ryoho. Cancer & Chemotherapy, 41(Suppl 1), 33–35. [PubMed] [Google Scholar]
- Hu, X. (2007). The effectiveness of Tai Chi on mental health status and functional fitness in older Japanese returnees from China: A randomized controlled trial. Japanese Journal of Physical Fitness and Sports Medicine, 56(4), 409–418. https://www.jstage.jst.go.jp/article/jspfsm/56/4/56_4_409/_pdf/-char/en [Google Scholar]
- Huang, T. T. , & Acton, G. J. (2004). Effectiveness of home visit falls prevention strategy for Taiwanese community‐dwelling elders: Randomized trial. Public Health Nursing, 21(3), 247–256. [DOI] [PubMed] [Google Scholar]
- Hughes, S. , Manheim, L. , Edelman, P. , & Conrad, K. (1987). Impact of long‐term home care on hospital and nursing home use and cost. Health Services Research, 22(1), 19–47. [PMC free article] [PubMed] [Google Scholar]
- Hum, A. Y. M. , Wu, H. Y. , Ali, N. B. , Leong, I. Y. O. , Chin, J. J. , Lee, A. O. K. , Tay, R. Y. , & Koh, M. Y. H. (2018). The dignity in advanced dementia (diadem) study: Developing an integrated geriatric palliative homecare program. Progress in Palliative Care, 26(2), 65–72. 10.1080/09699260.2018.1442286 [DOI] [Google Scholar]
- Humbert, J. , Legault, F. , Dahrouge, S. , Halabisky, B. , Boyce, G. , Hogg, W. , & Amos, S. (2007). Integration of nurse practitioners into a family health network. Canadian Nurse, 103(9), 30–34. [PubMed] [Google Scholar]
- Hummel, S. L. , Karmally, W. , Gillespie, B. W. , Helmke, S. T. , Teruya, S. , Wessler, J. D. , Wells, J. M. , Jimenez, O. , Trumble, E. , Cornellier, M. , Marolt, C. , & Maurer, M. S. (2017). Geriatric out‐of‐hospital randomized meal trial in heart failure (GOURMETHF) pilot randomized trial: Primary results. Journal of Cardiac Failure, 23(11), 830. 10.1016/j.cardfail.2017.10.005 [DOI] [Google Scholar]
- Hung, L. C. , Liu, C. C. , Hung, H. C. , & Kuo, H. W. (2003). Effects of a nursing intervention program on disabled patients and their caregivers. Archives of Gerontology & Geriatrics, 36(3), 259–272. [DOI] [PubMed] [Google Scholar]
- Iecovich, E. (2007). Client satisfaction with live‐in and live‐out home care workers in Israel. Journal of Aging & Social Policy, 19(4), 105–122. [DOI] [PubMed] [Google Scholar]
- Ifudu, O. , Paul, H. , Mayers, J. D. , Cohen, L. S. , Brezsnyak, W. F. , Herman, A. I. , Avram, M. M. , & Friedman, E. A. (1994). Pervasive failed rehabilitation in center‐based maintenance hemodialysis patients. American Journal of Kidney Diseases, 23(3), 394–400. [DOI] [PubMed] [Google Scholar]
- Ihsan, H. Z. (2013). Improving the quality of care for patients with faecal incontinence.
- Ilieva, E. M. , Oral, A. , Kucukdeveci, A. A. , Varela, E. , Valero, R. , Berteanu, M. , & Christodoulou, N. (2013). Osteoarthritis. The role of physical and rehabilitation medicine physicians. The European perspective based on the best evidence. A paper by the UEMS‐PRM Section Professional Practice Committee. European Journal of Physical & Rehabilitation Medicine, 49(4), 579–593. [PubMed] [Google Scholar]
- Iliffe, S. , Kendrick, D. , Morris, R. , Griffin, M. , Haworth, D. , Carpenter, H. , Masud, T. , Skelton, D. A. , Dinan‐Young, S. , Bowling, A. , Gage, H. , Res, P. , & Team (2015). Promoting physical activity in older people in general practice: ProAct65+cluster randomised controlled trial. British Journal of General Practice, 65(640), E731–E738. 10.3399/bjgp15X687361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iliffe, S. , Wilcock, J. , Drennan, V. , Goodman, C. , Griffin, M. , Knapp, M. , Lowery, D. , Manthorpe, J. , Rait, G. , & Warner, J. (2015). Changing practice in dementia care in the community: Developing and testing evidence‐based interventions, from timely diagnosis to end of life (EVIDEM). NIHR Journals Library, 10.3310/pgfar03030 [DOI] [PubMed] [Google Scholar]
- Intiso, D. , Rienzo, D. F. , Russo, M. , Pazienza, L. , Tolfa, M. , Iarossi, A. , & Maruzzi, G. (2012). Rehabilitation strategy in the elderly. Journal of Nephrology, 25(Suppl 1), S90–S95. 10.5301/jn.5000138 [DOI] [PubMed] [Google Scholar]
- Istvandity, L. (2017). Combining music and reminiscence therapy interventions for wellbeing in elderly populations: A systematic review. Complementary therapies in clinical practice, 28, 18–25. 10.1016/j.ctcp.2017.03.003 [DOI] [PubMed] [Google Scholar]
- Iyengar, K. P. , Nadkarni, J. B. , Ivanovic, N. , & Mahale, A. (2007). Targeted early rehabilitation at home after total hip and knee joint replacement: Does it work? Disability & Rehabilitation, 29(6), 495–502. [DOI] [PubMed] [Google Scholar]
- Jacobson, B. H. , Thompson, B. , Wallace, T. , Brown, L. , & Rial, C. (2011). Independent static balance training contributes to increased stability and functional capacity in community‐dwelling elderly people: A randomized controlled trial. Clinical Rehabilitation, 25(6), 549–556. 10.1177/0269215510392390 [DOI] [PubMed] [Google Scholar]
- Jame Bozorgi, A. A. , Ghamkhar, L. , Kahlaee, A. H. , & Sabouri, H. (2016). The effectiveness of occupational therapy supervised usage of adaptive devices on functional outcomes and independence after total hip replacement in iranian elderly: A randomized controlled trial. Occupational Therapy International, 23(2), 143–153. 10.1002/oti.1419 [DOI] [PubMed] [Google Scholar]
- Jan, M. , Simone, T. , & Bernhard, E. (2017). Treadmill training and body weight support for walking after stroke. Cochrane Database of Systematic Reviews, 8, CD002840. 10.1002/14651858.CD002840.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jane, C. , Steve, B. , & Howe, T. (2015). Prosthetic rehabilitation for older dysvascular people following a unilateral transfemoral amputation. Cochrane Database of Systematic Reviews, 1, 10.1002/14651858.CD005260.pub3 [DOI] [PubMed] [Google Scholar]
- Jansen, C. P. , Classen, K. , Wahl, H. W. , & Hauer, K. (2013). Promote physical activity of older people in nursing homes: A systematic review. Zeitschrift fur Gerontologie und Geriatrie, 46, 26. [Google Scholar]
- Jeon, M. Y. , & Jeong, H. (2015). Effects of a stroke primary prevention program on risk factors for at‐home elderly. Medical Science Monitor, 21, 3696–3703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jessup, J. V. , Horne, C. , Vishen, R. K. , & Wheeler, D. (2003). Effects of exercise on bone density, balance, and self‐efficacy in older women. Biological Research for Nursing, 4(3), 171–180. [DOI] [PubMed] [Google Scholar]
- Joan, O. , Linda, J. , & Brenda, R. (2004). Timed voiding for the management of urinary incontinence in adults. Cochrane Database of Systematic Reviews, 1, CD002802. 10.1002/14651858.CD002802.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- João, A. , Elzbieta, B.‐C. , Manuel, R. , Inês, C. , & Daniela, C. (2016). The effectiveness of nonpharmacological interventions in older adults with depressive disorders: A systematic review. International Journal of Nursing Studies, 58, 59–70. [DOI] [PubMed] [Google Scholar]
- Jobe, J. B. , Smith, D. M. , Ball, K. , Tennstedt, S. L. , Marsiske, M. , Willis, S. L. , Rebok, G. W. , Morris, J. N. , Helmers, K. F. , Leveck, M. D. , & Kleinman, K. (2001). ACTIVE: A cognitive intervention trial to promote independence in older adults. Controlled Clinical Trials, 22(4), 453–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John, A. A. (2000). Identification and management of late life depression: Working across primary care and community service boundaries.
- Johnen, B. , & Schott, N. (2018). Feasibility of a machine vs free weight strength training program and its effects on physical performance in nursing home residents: A pilot study. Aging Clinical and Experimental Research, 30(7), 819–828. 10.1007/s40520-017-0830-8 [DOI] [PubMed] [Google Scholar]
- Johnson, S. , & Cockburn, M. (1988). The Marie Curie/St Luke's relative support scheme: A home care service for relatives of the terminally ill. Journal of Advanced Nursing, 13, 565–570. https://search.proquest.com/docview/57562350?accountid=10792 [DOI] [PubMed] [Google Scholar]
- Joranson, N. , Pedersen, I. , Rokstad, A. M. , & Ihlebaek, C. (2017). Change in quality of life in older people with dementia participating in paroactivity: A cluster‐randomized controlled trial. Journal of Advanced Nursing, 73(6), 1531. 10.1111/jan.13307 [DOI] [PubMed] [Google Scholar]
- Jung, S. , Lee, S. , Bae, S. , Lee, S. , Makino, K. , Shinkai, Y. , & Shimada, H. (2018). Effectiveness of the KENKOJISEICHI local revitalization system on cognitive function change in older adults with mild cognitive impairment: Study protocol for a randomized controlled trial. Trials, 19, 276. 10.1186/s13063-018-2642-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jyvakorpi, S. K. , Puranen, T. , Pitkala, K. H. , & Suominen, M. H. (2012). Nutritional treatment of aged individuals with Alzheimer disease living at home with their spouses: Study protocol for a randomized controlled trial. Trials, 13, 66. 10.1186/1745-6215-13-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamioka, H. , Nakamura, Y. , Yazaki, T. , Uebaba, K. , Mutoh, Y. , Okada, S. , & Takahashi, M. (2004). Effectiveness of comprehensive health education combining hot spa bathing and lifestyle education in middle‐aged and elderly women: Randomized controlled trial of three‐ and six‐month interventions. Journal of the Japanese Society of Balneology, Climatology & Physical Medicine, 67(4), 202–214. [Google Scholar]
- Kamioka, H. , Nakamura, Y. , Yazaki, T. , Uebaba, K. , Mutoh, Y. , Okada, S. , & Takahashi, M. (2006). Comprehensive health education combining hot spa bathing and lifestyle education in middle‐aged and elderly women: One‐year follow‐up on randomized controlled trial of three‐ and six‐month interventions. Journal of Epidemiology, 16(1), 35–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson, M. K. , Magnusson, H. , Schewelov, von, T. , & Rosengren, B. E. (2013). Prevention of falls in the elderly‐‐a review. Osteoporosis International, 24(3), 747–762. 10.1007/s00198-012-2256-7 [DOI] [PubMed] [Google Scholar]
- Karmarkar, A. M. (2009). Prescription, outcomes, and risk assessment of wheelchairs for aging population. http://search.ebscohost.com/login.aspx?direct=true%26db=ccm%26AN=109852907%26site=ehost-live
- Karmarkar, A. M. , Collins, D. M. , Kelleher, A. , & Cooper, R. A. (2009). Satisfaction related to wheelchair use in older adults in both nursing homes and community dwelling. Disability & Rehabilitation Assistive Technology, 4(5), 337–343. 10.1080/17483100903038543 [DOI] [PubMed] [Google Scholar]
- Karmarkar, A. M. , Collins, D. M. , Kelleher, A. , Ding, D. , Oyster, M. , & Cooper, R. A. (2010). Manual wheelchair‐related mobility characteristics of older adults in nursing homes. Disability & Rehabilitation Assistive Technology, 5(6), 428–437. 10.3109/17483107.2010.481346 [DOI] [PubMed] [Google Scholar]
- Katzel, L. I. (2016). Multimodel exercise and weight loss in older obese veterans with dysmobility. https://Clinicaltrials.Gov/Show/Nct02806336. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/260/CN-01578260/frame.html
- Kawagoshi, A. , Kiyokawa, N. , Sugawara, K. , Takahashi, H. , Sakata, S. , Satake, M. , & Shioya, T. (2015). Effects of low‐intensity exercise and home‐based pulmonary rehabilitation with pedometer feedback on physical activity in elderly patients with chronic obstructive pulmonary disease. Respiratory Medicine, 109(3), 364–371. 10.1016/j.rmed.2015.01.008 [DOI] [PubMed] [Google Scholar]
- Keall, M. D. , Pierse, N. , Howden‐Chapman, P. , Guria, J. , Cunningham, C. W. , & Baker, M. G. (2017). Cost‐benefit analysis of fall injuries prevented by a programme of home modifications: A cluster randomised controlled trial. Injury Prevention, 23(1), 22–26. 10.1136/injuryprev-2015-041947 [DOI] [PubMed] [Google Scholar]
- Keeney, T. , Jette, A. , Freedman, V. , & Cabral, H. (2017). Racial differences in patterns of use of rehabilitation services for adults aged 65 and older. Journal of the American Geriatrics Society, 65(12), 2707–2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kegelmeyer, D. A. , Parthasarathy, S. , Kostyk, S. K. , White, S. E. , & Kloos, A. D. (2013). Assistive devices alter gait patterns in Parkinson disease: Advantages of the four‐wheeled walker. Gait & Posture, 38(1), 20–24. 10.1016/j.gaitpost.2012.10.027 [DOI] [PubMed] [Google Scholar]
- Kelly, M. E. , Loughrey, D. , Lawlor, B. A. , Robertson, I. H. , Walsh, C. , & Brennan, S. (2014). The impact of cognitive training and mental stimulation on cognitive and everyday functioning of healthy older adults: A systematic review and meta‐analysis. Ageing Research Reviews, 15, 28–43. 10.1016/j.arr.2014.02.004 [DOI] [PubMed] [Google Scholar]
- Kemmler, W. , von Stengel, S. , Engelke, K. , Haberle, L. , Mayhew, J. L. , & Kalender, W. A. (2010). Exercise, body composition, and functional ability. A randomized controlled trial. American Journal of Preventive Medicine, 38(3), 279–287. 10.1016/j.amepre.2009.10.042 [DOI] [PubMed] [Google Scholar]
- Kendall, J. C. , French, S. D. , Hartvigsen, J. , & Azari, M. F. (2018). Chiropractic treatment including instrument‐assisted manipulation for non‐specific dizziness and neck pain in community‐dwelling older people: A feasibility randomised sham‐controlled trial. Chiropractic and Manual Therapies, 26(1), 14. 10.1186/s12998-018-0183-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerschan, K. , Alacamlioglu, Y. , Kollmitzer, J. , Wober, C. , Kaider, A. , Hartard, M. , Ghanem, A. H. , & Preisinger, E. (1998). Functional impact of unvarying exercise program in women after menopause. American Journal of Physical Medicine & Rehabilitation, 77(4), 326–332. [DOI] [PubMed] [Google Scholar]
- Kerski, D. , Drinka, T. , Carnes, M. , Golob, K. , & Craig, W. A. (1987). Post‐geriatric evaluation unit follow‐up: Team versus nonteam. Journal of Gerontology, 42(2), 191–195. [DOI] [PubMed] [Google Scholar]
- Kerwin, M. , Nunes, F. , & Silva, P. A. (2012). Dance! Don't fall—Preventing falls and promoting exercise at home. Studies in Health Technology and Informatics, 177, 254–259. [PubMed] [Google Scholar]
- King, A. I. , Parsons, M. , & Robinson, E. (2012). A restorative home care intervention in New Zealand: Perceptions of paid caregivers. Health and Social Care in the Community, 20, 70–79. [DOI] [PubMed] [Google Scholar]
- Kiosses, D. N. , Arean, P. A. , Teri, L. , & Alexopoulos, G. S. (2010). Home‐delivered problem adaptation therapy (PATH) for depressed, cognitively impaired, disabled elders: A preliminary study. American Journal of Geriatric Psychiatry, 18(11), 988–998. 10.1097/JGP.0b013e3181d6947d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiosses, D. N. , Rosenberg, P. B. , McGovern, A. , Fonzetti, P. , Zaydens, H. , & Alexopoulos, G. S. (2015). Depression and suicidal ideation during two psychosocial treatments in older adults with major depression and dementia. Journal of Alzheimer's Disease, 48(2), 453–462. 10.3233/JAD-150200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiosses, D. , Ceide, M. E. , & Korenblatt, J. (2018). A path forward: A culturally relevant psychosocial intervention for depression in cognitive impaired older adults. American Journal of Geriatric Psychiatry, 26(3 Supp), S3–S4. [Google Scholar]
- Kolt, G. S. , Schofield, G. M. , Kerse, N. , Garrett, N. , Schluter, P. J. , Ashton, T. , & Patel, A. (2009). The healthy steps study: A randomized controlled trial of a pedometer‐based green prescription for older adults. Trial protocol. BMC Public Health, 9, 404. 10.1186/1471-2458-9-404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konick‐McMahan, J. , Bixby, B. , & McKenna, C. (2003). Heart failure in older adults. Providing nursing care to improve outcomes. Journal of Gerontological Nursing, 29(12), 35–41. [DOI] [PubMed] [Google Scholar]
- Kono, A. , Fujita, T. , Tsumura, C. , Kondo, T. , Kushiyama, K. , & Rubenstein, L. Z. (2009). Preventive home visit model targeted to specific care needs of ambulatory frail elders: Preliminary report of a randomized trial design. Aging‐Clinical & Experimental Research, 21(2), 167–173. [DOI] [PubMed] [Google Scholar]
- Kravitz, R. L. , Reuben, D. B. , Davis, J. W. , Mitchell, A. , Hemmerling, K. , Kington, R. S. , & Siu, A. L. (1994). Geriatric home assessment after hospital discharge. Journal of the American Geriatrics Society, 42(12), 1229–1234. [DOI] [PubMed] [Google Scholar]
- Kristen, D. , Daisy, C. , & Cheryl, S. (2000). Therapeutic design of environments for people with dementia: A review of the empirical research. Gerontologist, 40(4), 397–416. [DOI] [PubMed] [Google Scholar]
- Kristiina, N. , Ilkka, V. , Raija, L. , & Pia, L. (2011). Benefits of home‐based rocking‐chair exercise for physical performance in community‐dwelling elderly women: A randomized controlled trial. Aging Clinical and Experimental Research, 23(4), 279–287. [DOI] [PubMed] [Google Scholar]
- Kruse, R. L. , Oliver, D. P. , Wittenberg‐Lyles, E. , & Demiris, G. (2013). Conducting the ACTIVE randomized trial in hospice care: Keys to success. Clinical Trials, 10(1), 160–169. 10.1177/1740774512461858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar, K. S. , Samuelkamaleshkumar, S. , Viswanathan, A. , & Macaden, A. S. (2017). Cognitive rehabilitation for adults with traumatic brain injury to improve occupational outcomes. Cochrane Database of Systematic Reviews, 2017(6), CD007935. 10.1002/14651858.CD007935.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunik, M. E. , Snow, A. L. , Wilson, N. , Amspoker, A. B. , Sansgiry, S. , Morgan, R. O. , Ying, J. , Hersch, G. , & Stanley, M. A. (2017). Teaching caregivers of persons with dementia to address pain. American Journal of Geriatric Psychiatry, 25(2), 144–154. 10.1016/j.jagp.2016.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo, L. M. , Huang, H. L. , Hsu, W. C. , Wang, Y. T. , & Shyu, Y. L. (2016). Home‐based caregiver training: Benefits differ by care receivers’ dementia diagnosis. Geriatric Nursing, 37(5), 376–384. 10.1016/j.gerinurse.2016.05.005 [DOI] [PubMed] [Google Scholar]
- Kuo, L. , Huang, H. , Huang, H. , Liang, J. , Chiu, Y. , Chen, S. , Kwok, Y. , Hsu, W. , & Shyu, Y. (2013). A home‐based training program improves Taiwanese family caregivers’ quality of life and decreases their risk for depression: A randomized controlled trial. International Journal of Geriatric Psychiatry, 28(5), 504–513. [DOI] [PubMed] [Google Scholar]
- Kusumoto, A. , Suzuki, T. , Yoshida, H. , & Kwon, J. (2007). Intervention study to improve quality of life and health problems of community‐living elderly women in Japan by shoe fitting and custom‐made insoles. Gerontology, 53(6), 348–356. [DOI] [PubMed] [Google Scholar]
- Lacroix, A. , Kressig, R. , Muehlbauer, T. , Gschwind, Y. , Pfenninger, B. , Bruegger, O. , & Granacher, U. (2016). Effects of a supervised versus an unsupervised combined balance and strength training program on balance and muscle power in healthy older adults: A randomized controlled trial. Gerontology, 62(3), 275–288. 10.1159/000442087 [DOI] [PubMed] [Google Scholar]
- Lahtinen, A. , Leppilahti, J. , Harmainen, S. , Sipila, J. , Antikainen, R. , Seppanen, M. L. , Willig, R. , Vahanikkila, H. , Ristiniemi, J. , Rissanen, P. , & Jalovaara, P. (2015). Geriatric and physically oriented rehabilitation improves the ability of independent living and physical rehabilitation reduces mortality: A randomised comparison of 538 patients. Clinical Rehabilitation, 29(9), 892–906. 10.1177/0269215514559423 [DOI] [PubMed] [Google Scholar]
- Lahtinen, A. , Leppilahti, J. , Vahanikkila, H. , Harmainen, S. , Koistinen, P. , Rissanen, P. , & Jalovaara, P. (2017). Costs after hip fracture in independently living patients: A randomised comparison of three rehabilitation modalities. Clinical Rehabilitation, 31(5), 672–685. 10.1177/0269215516651480 [DOI] [PubMed] [Google Scholar]
- Lam, L. C. , Chau, R. C. , Wong, B. M. , Fung, A. W. , Tam, C. W. , Leung, G. T. , Kwok, T. C. , Leung, T. Y. , Ng, S. P. , & Chan, W. M. (2012). A 1‐year randomized controlled trial comparing mind body exercise (tai chi) with stretching and toning exercise on cognitive function in older chinese adults at risk of cognitive decline. Journal of the American Medical Directors Association, 13(6), 568. 10.1016/j.jamda.2012.03.008 [DOI] [PubMed] [Google Scholar]
- Laming, N. (2017). POSTER: A systematic review investigating the effectiveness of occupational therapy for older people in care homes in improving physical function and quality of life. British Journal of Occupational Therapy, 80, 73–88. [Google Scholar]
- Lapid, M. I. , Rummans, T. A. , Brown, P. D. , Frost, M. H. , Johnson, M. E. , Huschka, M. M. , Sloan, J. A. , Richardson, J. W. , Hanson, J. M. , & Clark, M. M. (2006). Impacting the quality of life in elderly cancer patients with a structured multidisciplinary intervention: A randomized controlled trial. Journal of the American Geriatrics Society, 54(4), S196. [Google Scholar]
- Laufer, Y. (2002). Effects of one‐point and four‐point canes on balance and weight distribution in patients with hemiparesis. Clinical Rehabilitation, 16(2), 141–148. 10.1191/0269215502cr481oa [DOI] [PubMed] [Google Scholar]
- Leinonen, R. , Heikkinen, E. , Hirvensalo, M. , Lintunen, T. , Rasinaho, M. , Sakari‐Rantala, R. , Kallinen, M. , Koski, J. , Mottonen, S. , Kannas, S. , Huovinen, P. , & Rantanen, T. (2007). Customer‐oriented counseling for physical activity in older people: Study protocol and selected baseline results of a randomized‐controlled trial (ISRCTN 07330512). Scandinavian Journal of Medicine & Science in Sports, 17(2), 156–164. 10.1111/j.1600-0838.2006.00536.x [DOI] [PubMed] [Google Scholar]
- Leone, E. , Deudon, A. , & Robert, P. (2012). Motivation, engagement and verbal/motor stimulation in severe dementia‐The STIM‐EHPAD study. Revue de Neuropsychologie, Neurosciences Cognitives et Cliniques, 4(2), 114–122. 10.3917/rne.042.0114 [DOI] [Google Scholar]
- Levine, R. E. , & Gitlin, L. N. (1993). A model to promote activity competence in elders. American Journal of Occupational Therapy, 47(2), 147–153. [DOI] [PubMed] [Google Scholar]
- Levy‐Storms, L. (2008). Therapeutic communication training in long‐term care institutions: Recommendations for future research. Patient Education and Counseling, 73(1), 8–21. 10.1016/j.pec.2008.05.026 [DOI] [PubMed] [Google Scholar]
- Liebel, D. (2008). Process evaluation of a nurse home visiting intervention that postpones disability worsening in older adults. Dissertation Abstracts International: Section B: The Sciences and Engineering, 68(9‐B), 5860. [Google Scholar]
- Lim, W. K. , Berlowitz, D. , Murphy, M. C. , & Jackson, B. (2005). Abstract: Effectiveness of pharmacist home visits for patients with congestive cardiac failure: the COPE (community pharmacy care) study. Internal Medicine Journal, 35, A54–A55. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/872/CN-00604872/frame.html [Google Scholar]
- Lim, W. K. , Lambert, S. F. , & Gray, L. C. (2003). Effectiveness of case management and post‐acute services in older people after hospital discharge. Medical Journal of Australia, 178(6), 262–266. [DOI] [PubMed] [Google Scholar]
- Lin, J. S. , Whitlock, E. P. , Eckstrom, E. , Fu, R. W. , Perdue, L. A. , Beil, T. L. , & Leipzig, R. M. (2012). Challenges in synthesizing and interpreting the evidence from a systematic review of multifactorial interventions to prevent functional decline in older adults. Journal of the American Geriatrics Society, 60(11), 2157–2166. 10.1111/j.1532-5415.2012.04214.x [DOI] [PubMed] [Google Scholar]
- Lingler, J. H. , Arida, J. , Happ, M. B. , Sereika, S. M. M. , Tamres, L. , Tang, F. , & Erlen, J. (2014). Medication errors and related deficiencies by caregivers of persons with memory loss: Preliminary results of an intervention to maximize medication management (3M). Alzheimer's and Dementia, 10, P737. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/753/CN-01056753/frame.html [Google Scholar]
- Littlewood, C. , Bateman, M. , Brown, K. , Bury, J. , Mawson, S. , May, S. , & Walters, S. (2016). A self‐managed single exercise programme versus usual physiotherapy treatment for rotator cuff tendinopathy: A randomised controlled trial (the SELF study). Clinical Rehabilitation, 30(7), 686–696. 10.1177/0269215515593784 [DOI] [PubMed] [Google Scholar]
- Liu, J. Y. , & Lai, C. (2014). Implementation of observational pain management protocol to improve pain management for long‐term institutionalized older care residents with dementia: Study protocol for a cluster‐randomized controlled trial. Trials, 15(1), 78. 10.1186/1745-6215-15-78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, L. , Stroulia, E. , Nikolaidis, I. , Miguel‐Cruz, A. , & Rincon, R. A. (2016). Smart homes and home health monitoring technologies for older adults: A systematic review. International Journal of Medical Informatics, 91, 44–59. 10.1016/j.ijmedinf.2016.04.007 [DOI] [PubMed] [Google Scholar]
- Liu, Y. W. , & Tsui, C. M. (2014). A randomized trial comparing Tai Chi with and without cognitive‐behavioral intervention (CBI) to reduce fear of falling in community‐dwelling elderly people. Archives of Gerontology & Geriatrics, 59(2), 317–325. 10.1016/j.archger.2014.05.008 [DOI] [PubMed] [Google Scholar]
- Livingston, G. , Barber, J. , Rapaport, P. , Knapp, M. , Griffin, M. , King, D. , Livingston, D. , Mummery, C. , Walker, Z. , Hoe, J. , Sampson, E. L. , & Cooper, C. (2013). Clinical effectiveness of a manual based coping strategy programme (START, STrAtegies for RelaTives) in promoting the mental health of carers of family members with dementia: Pragmatic randomised controlled trial. BMJ, 347, f6276. 10.1136/bmj.f6276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord, S. R. , Castell, S. , Corcoran, J. , Dayhew, J. , Matters, B. , Shan, A. , & Williams, P. (2003). The effect of group exercise on physical functioning and falls in frail older people living in retirement villages: A randomized, controlled trial. Journal of the American Geriatrics Society, 51(12), 1685–1692. 10.1046/j.1532-5415.2003.51551.x [DOI] [PubMed] [Google Scholar]
- Low, L. F. , & Fletcher, J. (2015). Models of home care services for persons with dementia: A narrative review. International Psychogeriatrics, 27(10), 1593–1600. 10.1017/S1041610215000137 [DOI] [PubMed] [Google Scholar]
- Low, L. F. , Baker, J. R. , Jeon, Y. H. , Camp, C. , Haertsch, M. , & Skropeta, M. (2013). Study protocol: Translating and implementing psychosocial interventions in aged home care the lifestyle engagement activity program (LEAP) for life. BMC Geriatrics, 13, 124. 10.1186/1471-2318-13-124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luger, E. , Dorner, T. E. , Haider, S. , Kapan, A. , Lackinger, C. , & Schindler, K. (2016). Effects of a home‐based and volunteer‐administered physical training, nutritional, and social support program on malnutrition and frailty in older persons: A randomized controlled trial. Journal of the American Medical Directors Association, 17(7), 671.e9–671.e16. 10.1016/j.jamda.2016.04.018 [DOI] [PubMed] [Google Scholar]
- Lundqvist, M. , Davidson, T. , Ordell, S. , Sjostrom, O. , Zimmerman, M. , & Sjogren, P. (2015). Health economic analyses of domiciliary dental care and care at fixed clinics for elderly nursing home residents in Sweden. Community Dental Health, 32(1), 39–43. [PubMed] [Google Scholar]
- Luukinen, H. , Lehtola, S. , Jokelainen, J. , Vaananen‐Sainio, R. , Lotvonen, S. , & Koistinen, P. (2006). Prevention of disability by exercise among the elderly: A population‐based, randomized, controlled trial. Scandinavian Journal of Primary Health Care, 24(4), 199–205. 10.1080/02813430600958476 [DOI] [PubMed] [Google Scholar]
- Maghsoudi, E. , Pak, M. H. M. , Zareei, F. , Rashid, S. P. , Sofiyani, A. , & Shahidi, L. (2015). The effect of care plan application based on Roy adaptation model on the self‐efficacy in elderly people in urmia nursing homes. Research Journal of Pharmaceutical, Biological and Chemical Sciences, 6(1), 793–799. http://www.rjpbcs.com/pdf/2015_6(1)/[100].pdf [Google Scholar]
- Maire, A. I. , Jean‐Jacques, T. , & Berton, B. (2012). Effect of Haptic Supplementation Provided By A Fixed Or Mobile Stick On Postural Stabilization In Elderly People. Gerontology, 58, 419–429. 10.1159/000337495 [DOI] [PubMed] [Google Scholar]
- Majewski, M. , Dabrowska, G. , Pawik, M. , & Rozek, K. (2015). Evaluation of a home‐based pulmonary rehabilitation program for older females suffering from bronchial asthma. Advances in Clinical & Experimental Medicine, 24(6), 1079–1083. 10.17219/acem/31679 [DOI] [PubMed] [Google Scholar]
- Maki, B. E. , Cheng, K. C. , Mansfield, A. , Scovil, C. Y. , Perry, S. D. , Peters, A. L. , McKay, S. , Lee, T. , Marquis, A. , Corbeil, P. , Fernie, G. R. , Liu, B. , & McIlroy, W. E. (2008). Preventing falls in older adults: New interventions to promote more effective change‐in‐support balance reactions. Journal of Electromyography & Kinesiology, 18(2), 243–254. [DOI] [PubMed] [Google Scholar]
- Mameletzi, D. , Kouidi, E. , Koutlianos, N. , & Deligiannis, A. (2011). Effects of long‐term exercise training on cardiac baroreflex sensitivity in patients with coronary artery disease: A randomized controlled trial. Clinical Rehabilitation, 25(3), 217–227. 10.1177/0269215510380825 [DOI] [PubMed] [Google Scholar]
- Mangione, K. K. , Miller, A. H. , & Naughton, I. V. (2010). Cochrane review: Improving physical function and performance with progressive resistance strength training in older adults. Physical Therapy, 90(12), 1711–1715. 10.2522/ptj.20100270 [DOI] [PubMed] [Google Scholar]
- Marasinghe, M. K. (2016). Assistive technologies in reducing caregiver burden among informal caregivers of older adults: A systematic review. Disability & Rehabilitation Assistive Technology, 11(5), 353–360. 10.3109/17483107.2015.1087061 [DOI] [PubMed] [Google Scholar]
- Marioni, G. , Fermo, S. , Lionello, M. , Fasanaro, E. , Giacomelli, L. , Zanon, S. , Staffieri, C. , Dall'Igna, F. , Manzato, E. , & Staffieri, A. (2013). Vestibular rehabilitation in elderly patients with central vestibular dysfunction: A prospective, randomized pilot study. Age, 35(6), 2315–2327. 10.1007/s11357-012-9494-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markle‐Reid, M. , Browne, G. , & Gafni, A. (2013). Nurse‐led health promotion interventions improve quality of life in frail older home care clients: Lessons learned from three randomized trials in Ontario, Canada. Journal of Evaluation in Clinical Practice, 19(1), 118–131. 10.1111/j.1365-2753.2011.01782.x [DOI] [PubMed] [Google Scholar]
- Marston, A. (2007). Can the type of walking stick issued effect mobility, confidence or fear of falling? International Journal of Therapy & Rehabilitation, 14(5), 229–234. [Google Scholar]
- Martini, D. , Zeeboer, E. , Hildebrand, A. , Fling, B. , Hugos, C. , & Cameron, M. (2018). ADSTEP: Preliminary investigation of a multicomponent walking aid program in people with multiple sclerosis. Archives of Physical Medicine and Rehabilitation, 99, 2050–2058. 10.1016/j.apmr.2018.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason, A. , Weatherly, H. , Spilsbury, K. , Golder, S. , Arksey, H. , Adamson, J. , & Drummond, M. (2007). The effectiveness and cost‐effectiveness of respite for caregivers of frail older people. Journal of the American Geriatrics Society, 55(2), 290–299. 10.1111/j.1532-5415.2006.01037.x [DOI] [PubMed] [Google Scholar]
- Mazzuca, K. B. , Farris, N. A. , Mendenhall, J. , & Stoupa, R. A. (1997). Demonstrating the added value of community health nursing for clients with insulin-dependent diabetes. Journal of Community Health Nursing, 14(4), 211–224. [DOI] [PubMed] [Google Scholar]
- McCusker, J. , Verdon, J. , Tousignant, P. , De Courval, L. P. , Dendukuri, N. , & Belzile, E. (2001). Rapid emergency department intervention for older people reduces risk of functional decline: Results of a multicenter randomized trial. Journal of the American Geriatrics Society, 49(10), 1272–1281. [DOI] [PubMed] [Google Scholar]
- McEwan, R. T. (1992). Screening the elderly in general practice: Evaluation of a comprehensive functional assessment programme. https://search.proquest.com/docview/301491909?accountid=10792 http://resolver.ebscohost.com/openurl?ctx_ver=Z39.88-2004%26ctx_enc=info:ofi/enc:UTF-8%26rfr_id=info:sid/ProQuest+Dissertations+%26+Theses+Global%26rft_val_fmt=info:ofi/fmt:kev:mtx:dissertation%26rft.g
- McMillan, S. C. (2005). Interventions to facilitate family caregiving at the end of life. Journal of Palliative Medicine, 8(Suppl. 1), S–132. [DOI] [PubMed] [Google Scholar]
- McNeil, J. K. (1995). Effects of nonprofessional home visit programs for subclinically unhappy and unhealthy older adults. Journal of Applied Gerontology, 14(3), 333–342. 10.1177/073346489501400307 [DOI] [Google Scholar]
- Mehlhorn, J. , Freytag, A. , Schmidt, K. , Brunkhorst, F. M. , Graf, J. , Troitzsch, U. , Schlattmann, P. , Wensing, M. , & Gensichen, J. (2014). Rehabilitation interventions for postintensive care syndrome: A systematic review. Critical Care Medicine, 42(5), 1263–1271. 10.1097/CCM.0000000000000148 [DOI] [PubMed] [Google Scholar]
- Mehrholz, J. , Pohl, M. , Platz, T. , Kugler, J. , & Elsner, B. (2015). Electromechanical and robot‐assisted arm training for improving activities of daily living, arm function, and arm muscle strength after stroke. Cochrane Database of Systematic Reviews, 11, CD006876. 10.1002/14651858.CD006876.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melis, R. J. , van Eijken, M. I. , Boon, M. E. , Olde Rikkert, M. G. , & van Achterberg, T. (2010). Process evaluation of a trial evaluating a multidisciplinary nurse‐led home visiting programme for vulnerable older people. Disability & Rehabilitation, 32(11), 937–946. 10.3109/09638280903381006 [DOI] [PubMed] [Google Scholar]
- Melis, R. J. , van Eijken, M. I. , Borm, G. F. , Wensing, M. , Adang, E. , van de Lisdonk, E. H. , van Achterberg, T. , & Olde Rikkert, M. G. (2005). The design of the Dutch EASYcare study: A randomised controlled trial on the effectiveness of a problem‐based community intervention model for frail elderly people [NCT00105378]. BMC Health Services Research, 5, 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mello, J. D. A. , Hermans, K. , Van Audenhove, C. , Macq, J. , & Declercq, A. (2015). Evaluations of home care interventions for frail older persons using the interRAI Home Care instrument: A systematic review of the literature. Journal of the American Medical Directors Association, 16(2), 173. 10.1016/j.jamda.2014.11.007 [DOI] [PubMed] [Google Scholar]
- Mercadante, S. , Porzio, G. , Valle, A. , Fusco, F. , Aielli, F. , & Costanzo, V. (2011). Palliative sedation in patients with advanced cancer followed at home: A systematic review. Journal of Pain & Symptom Management, 41(4), 754–760. 10.1016/j.jpainsymman.2010.07.013 [DOI] [PubMed] [Google Scholar]
- Merom, D. , Mathieu, E. , Cerin, E. , Morton, R. L. , Simpson, J. M. , Rissel, C. , Anstey, K. J. , Sherrington, C. , Lord, S. R. , & Cumming, R. G. (2016). Social dancing and incidence of falls in older adults: A cluster randomised controlled trial. PLOS Medicine, 13(8), 1002112. 10.1371/journal.pmed.1002112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messecar, D. (1999). “Hospital at home” care was as effective as routine hospital care for older adults. Evidence‐Based Nursing, 2(2), 50–51. [Google Scholar]
- Messecar, D. (2003). Commentary: An exercise and incontinence intervention did not reduce the incidence or cost of acute conditions in nursing home residents. Evidence Based Nursing, 6(4), 116–117. http://search.ebscohost.com/login.aspx?direct=true%26db=ccm%26AN=106733418%26site=ehost-live [PubMed] [Google Scholar]
- Michaud, H. N. , & Duchesne, L. (2017). Aural rehabilitation for older adults with hearing loss: Impacts on quality of life‐a systematic review of randomized controlled trials. Journal of the American Academy of Audiology, 28(7), 596–609. 10.3766/jaaa.15090 [DOI] [PubMed] [Google Scholar]
- Mikkel, V. , Kirsten, A. , Jorgen, L. , & Carsten, H. (2005). Feasible model for prevention of functional decline in older people: Municipality‐randomized, controlled trial. Journal of the American Geriatrics Society, 53(4), 563–568. http://search.ebscohost.com/login.aspx?direct=true%26db=gnh%26AN=107201%26site=ehost-live [DOI] [PubMed] [Google Scholar]
- Mikkelsen, L. , Petersen, A. , Mechlenburg, I. , Mikkelsen, S. , Søballe, K. , & Bandholm, T. (2017). Description of load progression and pain response during progressive resistance training early after total hip arthroplasty: Secondary analyses from a randomized controlled trial. Clinical Rehabilitation, 31(1), 11–22. 10.1177/0269215516628305 [DOI] [PubMed] [Google Scholar]
- Miller, K. L. , Magel, J. R. , & Hayes, J. G. (2010). The effects of a home‐based exercise program on balance confidence, balance performance, and gait in debilitated, ambulatory community‐dwelling older adults: A pilot study. Journal of Geriatric Physical Therapy, 33(2), 85–91. [PubMed] [Google Scholar]
- Mitchell, S. (1987). Homing in on help. Social Services Insight, 2, 15–17. https://search.proquest.com/docview/57710877?accountid=10792 [Google Scholar]
- Mitseva, A. , Peterson, C. B. , Karamberi, C. , LCh, O. , Ballis, A. V. , Giannakakos, C. , & Dafoulas, G. E. (2012). Gerontechnology: Providing a helping hand when caring for cognitively impaired older adults‐intermediate results from a controlled study on the satisfaction and acceptance of informal caregivers. Current Gerontology & Geriatrics Research, 2012, 401705. 10.1155/2012/401705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffa‐Trotter, M. , & Anemaet, W. (1996). Home care for hip fracture survivors and fallers: The “Be HIP!” program. Topics in Geriatric Rehabilitation, 12(1), 46–58. [Google Scholar]
- Moholdt, T. , Vold, B. M. , Grimsmo, J. , Slordahl, S. A. , & Wisloff, U. (2012). Home‐based aerobic interval training improves peak oxygen uptake equal to residential cardiac rehabilitation: A randomized, controlled trial. PLOS One, 7(7), e41199. 10.1371/journal.pone.0041199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molloy, G. J. , Johnston, D. W. , Gao, C. , Witham, M. D. , Gray, J. M. , Argo, I. S. , Struthers, A. D. , & McMurdo, M. E. (2006). Effects of an exercise intervention for older heart failure patients on caregiver burden and emotional distress. European Journal of Cardiovascular Prevention & Rehabilitation, 13(3), 381–387. [DOI] [PubMed] [Google Scholar]
- Monteau, D. (2010). COMMENTARY: Effects of a programme of home visits on health status, the use of health care and its cost in elderly subjects in poor health. Cahiers de l'annee Gerontologique, 2(3), 176–179. 10.1007/s12612-010-0123-8 [DOI] [Google Scholar]
- Montgomery, C. (2010). Effects of quantitative progressive exercise rehabilitation on muscle function, functional performance, and quality of life of assisted living residents. http://search.ebscohost.com/login.aspx?direct=true%26db=ccm%26AN=109853663%26site=ehost-live
- Moore, M. , Warburton, J. , O'Halloran, P. D. , Shields, N. , & Kingsley, M. (2016). Effective community‐based physical activity interventions for older adults living in rural and regional areas: A systematic review. Journal of aging and physical activity, 24(1), 158–167. 10.1123/japa.2014-0218 [DOI] [PubMed] [Google Scholar]
- Morag, T. (2017). PROTOCOL: The effect of cognitive training on cognitive function in older people with mild to moderate dementia: A single‐blind randomised control trial. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/964/CN-01456964/frame.html [DOI] [PubMed]
- Morey, M. C. , Blair, C. K. , Sloane, R. , Cohen, H. J. , Snyder, D. C. , & Demark‐Wahnefried, W. (2015). Group trajectory analysis helps to identify older cancer survivors who benefit from distance‐based lifestyle interventions. Cancer, 121(24), 4433–4440. 10.1002/cncr.29684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriarty, H. , Winter, L. , Robinson, K. , Piersol, C. V. , Vause‐Earland, T. , Iacovone, D. B. , Newhart, B. , True, G. , Fishman, D. , Hodgson, N. , & Gitlin, L. N. (2016). A randomized controlled trial to evaluate the veterans’ in‐home program for military veterans with traumatic brain injury and their families: Report on impact for family members. Pm & R, 8(6), 495–509. 10.1016/j.pmrj.2015.10.008 [DOI] [PubMed] [Google Scholar]
- Morin, S. (2017). PROTOCOL: HIP mobile: A community‐based monitoring, rehabilitation and learning e‐system for patients following a hip fracture. https://Clinicaltrials.Gov/Show/Nct03153943. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/102/CN-01575102/frame.html
- Mortenson, W. B. , Demers, L. , Fuhrer, M. J. , Jutai, J. W. , Lenker, J. , & DeRuyter, F. (2013). Effects of an assistive technology intervention on older adults with disabilities and their informal caregivers: An exploratory randomized controlled trial. American Journal of Physical Medicine & Rehabilitation, 92(4), 297–306. 10.1097/PHM.0b013e31827d65bf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mottram, P. , Pitkala, K. , & Lees, C. (2007). WITHDRAWN: Institutional versus at‐home long term care for functionally dependent older people: Systematic review. Cochrane Database of Systematic Reviews, 4, CD003542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozley, C. G. , Schneider, J. , Cordingley, L. , Molineux, M. , Duggan, S. , Hart, C. , Stoker, B. , Williamson, R. , Lovegrove, R. , & Cruickshank, A. (2007). The care home activity project: Does introducing an occupational therapy programme reduce depression in care homes? Aging & Mental Health, 11(1), 99–107. [DOI] [PubMed] [Google Scholar]
- Mozolic, J. , Morgan, A. , & Laurienti, P. (2008). Cognitive training impacts brain structure and function of healthy older adults in a randomized controlled trial. Gerontologist, 48, 492. [Google Scholar]
- Mukamel, D. , Peterson, D. , Temkin‐Greener, H. , Delavan, R. , Gross, D. , Kunitz, S. , & T, F. W. (2007). Program characteristics and enrollees’ outcomes in the Program of All‐inclusive Care for the Elderly (PACE). The Milbank Quarterly, 85(3), 499–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller, C. , Glassel, A. , Marotzki, U. , & Voigt‐Radloff, S. (2014). Potential analyses for research on occupational therapy‐led training of activities of daily living in stroke patients. Zeitschrift Fur Evidenz Fortbildung Und Qualitat Im Gesundheitswesen, 108(Suppl), S36–S44. 10.1016/j.zefq.2014.09.003 [DOI] [PubMed] [Google Scholar]
- Mustian, K. M. , Peppone, L. , Darling, T. V. , Palesh, O. , Heckler, C. E. , & Morrow, G. R. (2009). A 4‐week home‐based aerobic and resistance exercise program during radiation therapy: A pilot randomized clinical trial. The Journal of Supportive Oncology, 7(5), 158–167. [PMC free article] [PubMed] [Google Scholar]
- Neil, T. (1989). Reviews—Matching resources to needs in community care by bleddyn davies and david challis/case management in community care—An evaluated experiment in the home care of the elderly by David Challis and Bleddyn Davies. Journal of Social Policy, 18(3), 465–469. [Google Scholar]
- Nelson, K. , Fennell, T. , Gray, K. E. , Williams, J. L. , Lutton, M. C. , Silverman, J. , Jain, K. , Augustine, M. R. , Kopf, W. , Taylor, L. , Sayre, G. , & Vanderwarker, C. (2016). PRotocol: Veteran peer coaches optimizing and advancing cardiac health. https://Clinicaltrials.Gov/Show/Nct02697422. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/212/CN-01556212/frame.html [DOI] [PubMed]
- Ness, A. , Symonds, N. , Siarkowski, M. , Broadfoot, M. , McBrien, K. , Lang, E. S. , Holroyd‐Leduc, J. , & Ronksley, P. (2018). Effectiveness of hospital avoidance interventions among elderly patients: A systematic review. Canadian Journal of Emergency Medicine, 20(Supple), S6. 10.1017/cem.2018.62 [DOI] [PubMed] [Google Scholar]
- Neville, C. (2015). The Watermemories swimming club for people with dementia: Cluster randomised controlled trial. http://Www.Anzctr.Org.Au/Actrn12615000458538.Aspx. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/068/CN-01308068/frame.html
- Newbury, J. , & Marley, J. (2000). Preventive home visits to elderly people in the community. Visits are most useful for people aged>/= 75. BMJ, 321(7259), 512. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/677/CN-00360677/frame.html [PMC free article] [PubMed] [Google Scholar]
- Newcomer, R. , Yordi, C. , DuNah, R. , Fox, P. , & Wilkinson, A. (1999). Effects of the medicare Alzheimer's disease demonstration on caregiver burden and depression. Health Services Research, 34(3), 669–689. [PMC free article] [PubMed] [Google Scholar]
- Nguyen, S. A. , Korenblatt, J. , & Ceide, M. E. (2015). Does a geriatric psychiatrist colocated in a home care agency improve recognition of mental disorders by primary care providers? American Journal of Geriatric Psychiatry, 1, S71. [Google Scholar]
- Nieman, C. L. , Marrone, N. , Mamo, S. K. , Betz, J. , Choi, J. S. , Contrera, K. J. , Thorpe, R. J. , Gitlin, L. N. , Tanner, E. K. , Han, H. R. , Szanton, S. L. , & Lin, F. R. (2017). The Baltimore HEARS Pilot Study: An affordable, accessible, community‐delivered hearing care intervention. Gerontologist, 57(6), 1173–1186. 10.1093/geront/gnw153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niemela, K. , Leinonen, R. , & Laukkanen, P. (2012). A supportive home visit program for older adults implemented by nonprofessionals: Feasibility and effects on physical performance and quality of life at one year—A pilot study. Archives of Gerontology & Geriatrics, 54(3), e376–e382. 10.1016/j.archger.2011.10.006 [DOI] [PubMed] [Google Scholar]
- Nijs, K. A. N. D. , De Graaf, C. , & Siebelink, E. (2006). Effect of family style meals on energy intake and risk of malnutrition in Dutch nursing home residents. Journals of Gerontology: Series A, Biological Sciences and Medical Sciences, 61(9), 935–942. [DOI] [PubMed] [Google Scholar]
- Nikolaus, T. , Specht‐Leible, N. , Bach, M. , Wittmann‐Jennewein, C. , Oster, P. , & Schlierf, G. (1995). Effectiveness of hospital‐based geriatric evaluation and management and home intervention team (GEM‐HIT). Rationale and design of a 5‐year randomized trial. Zeitschrift fur Gerontologie und Geriatrie, 28(1), 47–53. [PubMed] [Google Scholar]
- Nikoletou, D. , Man, W. D. , Mustfa, N. , Moore, J. , Rafferty, G. , Grant, R. L. , Johnson, L. , & Moxham, J. (2016). Evaluation of the effectiveness of a home‐based inspiratory muscle training programme in patients with chronic obstructive pulmonary disease using multiple inspiratory muscle tests. Disability & Rehabilitation, 38(3), 250–259. 10.3109/09638288.2015.1036171 [DOI] [PubMed] [Google Scholar]
- Nilsson, P. , Baigi, A. , Sward, L. , Moller, M. , & Mansson, J. (2012). Lateral epicondylalgia: A structured programme better than corticosteroids and NSAID. Scandinavian journal of occupational therapy, 19(5), 404–410. 10.3109/11038128.2011.620983 [DOI] [PubMed] [Google Scholar]
- Nishiguchi, S. , Yamada, M. , Tanigawa, T. , Sekiyama, K. , Kawagoe, T. , Suzuki, M. , Yoshikawa, S. , Abe, N. , Otsuka, Y. , Nakai, R. , Aoyama, T. , & Tsuboyama, T. (2015). A 12‐week physical and cognitive exercise program can improve cognitive function and neural efficiency in community‐dwelling older adults: A randomized controlled trial. Journal of the American Geriatrics Society, 63(7), 1355–1363. 10.1111/jgs.13481 [DOI] [PubMed] [Google Scholar]
- Noelker, L. S. , & Bass, D. M. (1989). Home care for elderly persons: Linkages between formal and informal caregivers. Journals of Gerontology, 44, S63–S70. [DOI] [PubMed] [Google Scholar]
- Northey, J. M. , Cherbuin, N. , Pumpa, K. L. , Smee, D. J. , & Rattray, B. (2018). Exercise interventions for cognitive function in adults older than 50: A systematic review with meta‐analysis. British Journal of Sports Medicine, 52(3), 154–160. 10.1136/bjsports-2016-096587 [DOI] [PubMed] [Google Scholar]
- Nour, K. , Desrosiers, J. , Gauthier, P. , & Carbonneau, H. (2002). Impact of a home leisure educational program for older adults who have had a stroke (Home Leisure Educational Program). Therapeutic Recreation Journal, 36(1), 48–64. [Google Scholar]
- Nourhashemi, F. (2015). PROTOCOL: SAFEWALKER contribution to the rehabilitation of older people after a post‐fall syndrome. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/281/CN-01553281/frame.html
- Nowak, F. , Nagle, L. , & Bernardo, A. (1998). Review: Case management programmes improve patient outcomes [commentary on Ferguson JA, Weinberger M. Case management programs in primary care. J GEN INTERN MED 1998 Feb;13:123‐6]. Evidence Based Nursing, 1, 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oleske, D. M. , & Hauck, W. W. (1988). A population‐based evaluation of the impact of interventions for improving care to cancer patients in the home setting. Home Health Care Services Quarterly, 9(1), 45–61. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/432/CN-01448432/frame.html [DOI] [PubMed] [Google Scholar]
- Oliveira, J. , Sherrington, C. , Amorim, A. , Dario, A. , & Tiedemann, A. (2016). What is the effect of health coaching on physical activity participation in older people?: A systematic review of randomised controlled trials. Journal of aging and physical activity, 24, S108. S108. [Google Scholar]
- Ollonqvist, K. , Aaltonen, T. , Karppi, S. L. , Hinkka, K. , & Pontinen, S. (2008). Network‐based rehabilitation increases formal support of frail elderly home‐dwelling persons in Finland: Randomised controlled trial. Health & Social Care in the Community, 16(2), 115–125. 10.1111/j.1365-2524.2007.00733.x [DOI] [PubMed] [Google Scholar]
- Opinder, S. , Ruth, P.‐J. , Fiona, M. , Alan, M. , Wei, T. , Tracey, S. , Pip, L. , Denise, K. , Alison, W. , Maria, W. , & Justin, W. (2016). Comparing the cost‐effectiveness and clinical effectiveness of a new community in‐reach rehabilitation service with the cost‐effectiveness and clinical effectiveness of an established hospital‐based rehabilitation service for older people: A pragmatic randomised controlled trial with microcost and qualitative analysis the Community In‐reach Rehabilitation And Care Transition (CIRACT) study. Health Services and Delivery Research, 4(7), 10.3310/hsdr04070 [DOI] [PubMed] [Google Scholar]
- Orrell, M. , Aguirre, E. , Spector, A. , Hoare, Z. , Woods, R. T. , Streater, A. , Donovan, H. , Hoe, J. , Knapp, M. , Whitaker, C. , & Russell, I. (2014). Maintenance cognitive stimulation therapy for dementia: Single‐blind, multicentre, pragmatic randomised controlled trial. British Journal of Psychiatry, 204(6), 454–461. 10.1192/bjp.bp.113.137414 [DOI] [PubMed] [Google Scholar]
- Orrell, M. , Hancock, G. , Hoe, J. , Woods, B. , Livingston, G. , & Challis, D. (2007). A cluster randomised controlled trial to reduce the unmet needs of people with dementia living in residential care. International Journal of Geriatric Psychiatry, 22(11), 1127–1134. [DOI] [PubMed] [Google Scholar]
- Ottmann, G. , Allen, J. , & Feldman, P. (2013). A systematic narrative review of consumer‐directed care for older people: Implications for model development. Health and Social Care in the Community, 21(6), 563–581. 10.1111/hsc.12025 [DOI] [PubMed] [Google Scholar]
- Overbeek, A. , Korfage, I. J. , Jabbarian, L. J. , Billekens, P. , Hammes, B. J. , Polinder, S. , Severijnen, J. , Swart, S. J. , Witkamp, F. E. , van der Heide, A. , & Rietjens, J. A. C. (2018). Advance care planning in frail older adults: A cluster randomized controlled trial. Journal of the American Geriatrics Society, 66(6), 1089–1095. 10.1111/jgs.15333 [DOI] [PubMed] [Google Scholar]
- Padulo, J. , Giorgio, D. A. , & Kuvacic, G. (2018). Comments on: Improving physical fitness and health status perception in community‐dwelling older adults through a structured program for physical activity promotion in the city of Naples, Italy: A randomized controlled trial. Geriatrics & Gerontology International, 18(4), 658–660. [DOI] [PubMed] [Google Scholar]
- Palvanen, M. , Kannus, P. , Piirtola, M. , Niemi, S. , Parkkari, J. , & Jarvinen, M. (2012). The chaos falls clinic in preventing falls and injuries among home‐dwelling older adults: A randomised controlled trial. Osteoporosis International, 2, S140–S171. 10.1007/s00198-012-1928-7 [DOI] [PubMed] [Google Scholar]
- Park, J. , McCaffrey, R. , Newman, D. , Liehr, P. , & Ouslander, J. G. (2017). A pilot randomized controlled trial of the effects of chair yoga on pain and physical function among community‐dwelling older adults with lower extremity osteoarthritis. Journal of the American Geriatrics Society, 65(3), 592–597. 10.1111/jgs.14717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parlevliet, J. , Hodac, M. , Buurman, B. , Boeschoten, E. , & Rooij, D. S. (2010). Systematic comprehensive geriatric assessment in elderly patients on chronic dialysis. European Geriatric Medicine, 1, S129–S130. 10.1016/j.eurger.2010.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons, M. , Senior, H. , Chen, M.‐H. X. , Jacobs, S. , Parsons, J. , Sheridan, N. , & Kenealy, T. (2013). Assessment without action; a randomised evaluation of the interRAI home care compared to a national assessment tool on identification of needs and service provision for older people in New Zealand. Health & Social Care in the Community, 21(5), 536–544. 10.1111/hsc.12045 [DOI] [PubMed] [Google Scholar]
- Pathy, M. S. , Bayer, A. , Harding, K. , & Dibble, A. (1992). Randomised trial of case finding and surveillance of elderly people at home. Lancet, 340(8824), 890–893. [DOI] [PubMed] [Google Scholar]
- Payette, H. , Boutier, V. , Coulombe, C. , & Gray‐Donald, K. (2002). Benefits of nutritional supplementation in free‐living, frail, undernourished elderly people: A prospective randomized community trial. Journal of the American Dietetic Association, 102(8), 1088–1095. [PubMed] [Google Scholar]
- Pearson, N. K. , Gibson, B. J. , Davis, D. M. , Gelbier, S. , & Robinson, P. G. (2007). The effect of a domiciliary denture service on oral health related quality of life: A randomised controlled trial. British Dental Journal, 203(2), E3. [DOI] [PubMed] [Google Scholar]
- Pedersen, L. J. (2016). Early nutritional follow‐up after discharge prevents deterioration of adl functions in malnourished, independent, geriatric patients who live alone—A randomized clinical trial. In Suzuki T., Maeda K. & Wakabayashi H. (Eds.), Effect of early nutritional follow‐up (Vol. 20, p. 584). Springer Science & Business Media B.V. https://pubmed.ncbi.nlm.nih.gov/27102800/ [DOI] [PubMed] [Google Scholar]
- Perula, L. A. , Varas‐Fabra, F. , Rodriguez, V. , Ruiz‐Moral, R. , Fernandez, J. A. , Gonzalez, J. , Perula, C. J. , Roldan, A. M. , & De Dios, C. (2012). Effectiveness of a multifactorial intervention program to reduce falls incidence among community‐living older adults: A randomized controlled trial. Archives of Physical Medicine & Rehabilitation, 93(10), 1677–1684. 10.1016/j.apmr.2012.03.035 [DOI] [PubMed] [Google Scholar]
- Peter, S. , Giggi, U. , & Ania, W. (2004). Support for family carers who care for an elderly person at home—A systematic literature review. Scandinavian Journal of Caring Sciences, 18(2), 111–119. [DOI] [PubMed] [Google Scholar]
- Pflaum, M. , Lang, F. R. , & Freiberger, E. (2016). Active and safe with wheeled walkers: Pilot study on feasibility of mobility exercises for wheeled walker users. Zeitschrift fur Gerontologie und Geriatrie, 49(5), 366–371. 10.1007/s00391-015-1007-8 [DOI] [PubMed] [Google Scholar]
- Picorelli, A. , Miranda, A. , Pereira, M. , Souza, L. , Pereira, S. , Daniele, Diogo, F. , & Catherine, S. (2014). Adherence to exercise programs for older people is influenced by program characteristics and personal factors: A systematic review. Journal of Physiotherapy, 60(3), 151–156. 10.1016/j.jphys.2014.06.012 [DOI] [PubMed] [Google Scholar]
- Pihl, E. , Cider, A. , Stromberg, A. , Fridlund, B. , & Martensson, J. (2011). Exercise in elderly patients with chronic heart failure in primary care: Effects on physical capacity and health‐related quality of life. European Journal of Cardiovascular Nursing, 10(3), 150–158. 10.1016/j.ejcnurse.2011.03.002 [DOI] [PubMed] [Google Scholar]
- Pine, Z. M. , Gurland, B. , & Chren, M. M. (2002). Use of a cane for ambulation: Marker and mitigator of impairment in older people who report no difficulty walking. Journal of the American Geriatrics Society, 50(2), 263–268. [DOI] [PubMed] [Google Scholar]
- Ploeg, J. , Brazil, K. , Hutchison, B. , Kaczorowski, J. , Dalby, D. M. , Goldsmith, C. H. , & Furlong, W. (2010). Effect of preventive primary care outreach on health related quality of life among older adults at risk of functional decline: Randomised controlled trial. BMJ, 340, c1480. 10.1136/bmj.c1480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podd, S. J. , Hunt, J. , & Sulke, N. (2015). Home orthostatic training in elderly patients with vasovagal syncope—A prospective randomised controlled trial. European Cardiology Review, 10(2), 123–127. 10.15420/ecr.2015.10.2.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack, C. D. (1998). Post‐hospitalization referral to home health care and subsequent rehospitalization for Medicare patients with congestive heart failure (Thesis).
- Pollock, R. D. , Martin, F. C. , & Newham, D. J. (2012). Whole‐body vibration in addition to strength and balance exercise for falls‐related functional mobility of frail older adults: A single‐blind randomized controlled trial. Clinical Rehabilitation, 26(10), 915–923. 10.1177/0269215511435688 [DOI] [PubMed] [Google Scholar]
- Pozet, A. , Lejeune, C. , Bonnet, M. , Dabakuyo, S. , Dion, M. , Fagnoni, P. , Gaimard, M. , Imbert, G. , Nerich, V. , Foubert, A. , Chotard, M. , Bonin, M. , Anota, A. , & Bonnetain, F. (2016). Evaluation of efficacy and efficiency of a pragmatic intervention by a social worker to support informal caregivers of elderly patients (The ICE Study): Study protocol for a randomized controlled trial. Trials, 17, 531. 10.1186/s13063-016-1622-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pressler, K. (2015). “They'll think it's a good thing”: Examining the dynamics of walker, cane and wheelchair use among older adults and their social ties. Dissertation Abstracts International Section A: Humanities and Social Sciences, 76(5‐A(E).
- Prizer, L. , & Zimmerman, S. (2018). Progressive support for activities of daily living for persons living with dementia. The Gerontologist, 58(suppl_1), S74–S87. 10.1093/geront/gnx103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pynnonen, K. , Tormakangas, T. , Rantanen, T. , Tiikkainen, P. , & Kallinen, M. (2018). Effect of a social intervention of choice vs. control on depressive symptoms, melancholy, feeling of loneliness, and perceived togetherness in older Finnish people: A randomized controlled trial. Aging & Mental Health, 22(1), 77–84. 10.1080/13607863.2016.1232367 [DOI] [PubMed] [Google Scholar]
- Ramsay, E. , Sherrington, C. , Close, J. , Lord, S. , Barraclough, E. , Kirkham, C. , O'Rourke, S. , Vogler, C. , Dean, C. , & Clemson, L. (2011). A home‐based exercise intervention designed to prevent falls in older people recently discharged from hospital: Overview, safety and adherence. Physiotherapy, 1, eS1034. 10.1016/j.physio.2011.04.002 [DOI] [Google Scholar]
- Rana, A. K. M. M. , Kabir, Z. N. , Lundborg, C. S. , & Wahlin, A. (2010). Health education improves both arthritis‐related illness and self‐rated health: An intervention study among older people in rural Bangladesh. Public Health, 124(12), 705–712. 10.1016/j.puhe.2010.07.005 [DOI] [PubMed] [Google Scholar]
- Ranganathan, M. , Ezhumalai, S. , & Praharaj, S. K. (2012). Pattern of disability among persons who availed half‐way home‐care services for psychosocial rehabilitation. Industrial Psychiatry Journal, 21(2), 173–177. 10.4103/0972-6748.119655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rantanen, T. , Rantakokko, M. , Ayravainen, I. , Khalil, H. , Honkala, S. , Eronen, J. , Lyyra, T. M. , & Vaarama, M. (2012). Mobility limitation, access to outdoors and quality of life: A randomised controlled trial delivered by older volunteers. Journal of aging and physical activity, 20, S320–S321. [Google Scholar]
- Ratzka, A. D. (1986). Independent living and attendant care in Sweden: A consumer perspective. In World Rehabilitation Fund, monograph No. 34. World Rehabilitation Fund, International Exchange of Experts and Information in Rehabilitation, New York, NY.
- Redford, J. B. (1993). Seating and wheeled mobility in the disabled elderly population. Archives of Physical Medicine & Rehabilitation, 74(8), 877–885. [DOI] [PubMed] [Google Scholar]
- Reeder, B. , Meyer, E. , Lazar, A. , Chaudhuri, S. , Thompson, H. J. , & Demiris, G. (2013). Framing the evidence for health smart homes and home‐based consumer health technologies as a public health intervention for independent aging: A systematic review. International Journal of Medical Informatics, 82(7), 565–579. 10.1016/j.ijmedinf.2013.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid, M. C. , Henderson, C. R. , Trachtenberg, M. A. , Beissner, K. L. , Bach, E. , Barron, Y. , Sridharan, S. , & Murtaugh, C. M. (2017). Implementing a pain self‐management protocol in home care: A cluster‐randomized pragmatic trial. Journal of the American Geriatrics Society, 65(8), 1667–1675. 10.1111/jgs.14836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid, U. V. , & Ploeg, J. (2002). An outpatient geriatric evaluation and management programme was more effective than usual care in preventing functional decline in high risk older adults. Evidence Based Nursing, 5, 19. [DOI] [PubMed] [Google Scholar]
- Rentschler, A. J. , Simpson, R. , Cooper, R. A. , & Boninger, M. L. (2008). Clinical evaluation of Guido robotic walker. Journal of Rehabilitation Research & Development, 45(9), 1281–1293. [PubMed] [Google Scholar]
- Resnick, B. , & Galik, E. (2013). Using function‐focused care to increase physical activity among older adults. Annual Review of Nursing Research, 31, 175–208. 10.1891/0739-6686.31.175 [DOI] [PubMed] [Google Scholar]
- Ricauda, N. A. , Bo, M. , Molaschi, M. , Massaia, M. , Salerno, D. , Amati, D. , Tibaldi, V. , & Fabris, F. (2004). Home hospitalization service for acute uncomplicated first ischemic stroke in elderly patients: A randomized trial. Journal of the American Geriatrics Society, 52(2), 278–283. 10.1111/j.1532-5415.2004.52069.x [DOI] [PubMed] [Google Scholar]
- Richardson, J. P. , Daly, M. P. , & Adelman, A. M. (1989). Rehabilitation in the elderly. Maryland Medical Journal, 38(2), 149–153. [PubMed] [Google Scholar]
- Rideout, E. (2004). Cardiac rehabilitation improved exercise tolerance after a myocardial infarction in older patients. Evidence Based Nursing, 7(1), 20. [DOI] [PubMed] [Google Scholar]
- Rie, K. , Sun, K. H. , & Kiyoko, M. (2012). The best evidence for minimizing resistance‐to-care during assisted personal care for older adults with dementia in nursing homes: A systematic review. JBI Library of Systematic Reviews, 10(58), 4622–4632. [DOI] [PubMed] [Google Scholar]
- Rizzo, J. A. , Baker, D. I. , McAvay, G. , & Tinetti, M. E. (1996). The cost-effectiveness of a multifactorial targeted prevention program for falls among community elderly persons. Medical Care, 34(9), 954–969. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/607/CN-00129607/frame.html [DOI] [PubMed] [Google Scholar]
- Robertson, M. C. , Gardner, M. M. , Devlin, N. , McGee, R. , & Campbell, A. J. (2001). Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 2: Controlled trial in multiple centres. BMJ, 322(7288), 701–704. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/603/CN-00325603/frame.html [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson, H. , MacDonald, B. , Kerse, N. , & Broadbent, E. (2013). The psychosocial effects of a companion robot: A randomized controlled trial. Journal of the American Medical Directors Association, 14(9), 661–667. 10.1016/j.jamda.2013.02.007 [DOI] [PubMed] [Google Scholar]
- Roger, C. , Tracy, D. , Christina, B. , Craig, F. , & Tracy, B. (2011). Screening for hearing loss in adults ages 50 years and older: A review of the evidence for the U.S. Preventive Services Task Force. http://0-ovidsp.ovid.com.lib.exeter.ac.uk/ovidweb.cgi?T=JS%26PAGE=reference%26D=medp%26NEWS=N%26AN=21542547 [PubMed]
- Rogers, C. , Johnson, J. , Nueslein, B. , Edmunds, D. , & Valdez, R. (2018). “I love fruit but i can't afford it”: Using participatory action research to develop community‐based initiatives to mitigate challenges to chronic disease management in an African American community living in public housing. Journal of Racial and Ethnic Health Disparities, 5, 1315–1327. 10.1007/s40615-018-0480-3 [DOI] [PubMed] [Google Scholar]
- Romskaug, R. , Molden, E. , Straand, J. , Kersten, H. , Skovlund, E. , Pitkala, K. H. , & Wyller, T. B. (2017). Cooperation between geriatricians and general practitioners for improved pharmacotherapy in home‐dwelling elderly people receiving polypharmacy—The COOP Study: Study protocol for a cluster randomised controlled trial. Trials, 18(1), 158. 10.1186/s13063-017-1900-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roselle, T. (2015). The impact of mobility scooters on their users. Does their usage help or hinder?: A state of the art review. Journal of Transport & Health, 2(2), 269–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi, L. P. , Brandalize, M. , Pereira, R. , & Gomes, A. R. (2014). The effects of a perturbation‐based balance training on neuromuscular recruitment and functional mobility in community‐dwelling older women: A randomized controlled trial. Topics in Geriatric Rehabilitation, 30(4), 256–263. 10.1097/tgr.0000000000000035 [DOI] [Google Scholar]
- Routasalo, P. E. , Tilvis, R. S. , Kautiainen, H. , & Pitkala, K. H. (2009). Effects of psychosocial group rehabilitation on social functioning, loneliness and well‐being of lonely, older people: Randomized controlled trial. Journal of Advanced Nursing, 65(2), 297–305. 10.1111/j.1365-2648.2008.04837.x [DOI] [PubMed] [Google Scholar]
- Rubin, C. D. , Sizemore, M. T. , Loftis, P. A. , Adams‐Huet, B. , & Anderson, R. J. (1992). The effect of geriatric evaluation and management on Medicare reimbursement in a large public hospital: A randomized clinical trial. Journal of the American Geriatrics Society, 40(10), 989–995. [DOI] [PubMed] [Google Scholar]
- Rubio Acuña, M. (2013). Effectiveness of home visits in the elderly on functional status, mortality and nurse home admission. Gerokomos, 24(2), 78–80. [Google Scholar]
- Rudilla, D. , Galiana, L. , Oliver, A. , & Barreto, P. (2016). Comparing counseling and dignity therapies in home care patients: A pilot study. Palliative & supportive care, 14(4), 321–329. 10.1017/S1478951515001182 [DOI] [PubMed] [Google Scholar]
- Ruihuan, P. , Mingchao, Z. , Hao, C. , Youhua, G. , Lechang, Z. , Mei, L. , Zhijing, Y. , Leying, Z. , Jie, Z. , & Hongxia, C. (2018). A randomized controlled trial of a modified wheelchair arm‐support to reduce shoulder pain in stroke patients. Clinical Rehabilitation, 32(1), 37–47. 10.1177/0269215517714830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruikes, F. G. H. , Zuidema, S. U. , Akkermans, R. P. , Assendelft, W. J. J. , Schers, H. J. , & Koopmans, R. T. C. M. (2016). Multicomponent program to reduce functional decline in frail elderly people: A cluster controlled trial. Journal of the American Board of Family Medicine, 29(2), 209–217. 10.3122/jabfm.2016.02.150214 [DOI] [PubMed] [Google Scholar]
- Ryburn, B. , Wells, Y. , & Foreman, P. (2009). Enabling independence: Restorative approaches to home care provision for frail older adults: Systematic review. Health & Social Care in the Community, 17(3), 225–234. 10.1111/j.1365-2524.2008.00809.x [DOI] [PubMed] [Google Scholar]
- Rydwik, E. , Frandin, K. , & Akner, G. (2010). Effects of a physical training and nutritional intervention program in frail elderly people regarding habitual physical activity level and activities of daily living—A randomized controlled pilot study. Archives of Gerontology and Geriatrics, 51(3), 283–289. 10.1016/j.archger.2009.12.001 [DOI] [PubMed] [Google Scholar]
- Sahyoun, N. , & Vaudin, A. (2014). Home‐delivered meals and nutrition status among older adults. Nutrition in Clinical Practice, 29(4), 459–465. [DOI] [PubMed] [Google Scholar]
- Sakurai, R. , Fujiwara, Y. , Kim, H. , Saito, K. , Yasunaga, M. , Nonaka, K. , Kobayashi, K. , Ogawa, K. , Yoshida, H. , Tanaka, C. , Uchida, H. , Suzuki, K. , Watanabe, S. , & Shinkai, S. (2011). A randomized controlled trial of the effects of a comprehensive intervention program for community‐dwelling older adults. Nippon Ronen Igakkai Zasshi—Japanese Journal of Geriatrics, 48(4), 352–360. [DOI] [PubMed] [Google Scholar]
- Sakurai, R. , Yasunaga, M. , Saito, K. , Fukaya, T. , Kim, M. J. , Tsunoda, N. , Muraki, E. , Suzuki, H. , Shinkai, S. , Watanabe, S. , & Fujiwara, Y. (2013). Effects of a comprehensive intervention program, including hot bathing, on physical function in community‐dwelling healthy older adults: A pilot randomized controlled trial. Aging‐Clinical & Experimental Research, 25(4), 453–461. 10.1007/s40520-013-0080-3 [DOI] [PubMed] [Google Scholar]
- Salazar, A. M. , Warden, D. L. , Schwab, K. , Spector, J. , Braverman, S. , Walter, J. , Cole, R. , Rosner, M. M. , Martin, E. M. , Ecklund, J. , & Ellenbogen, R. G. (2000). Cognitive rehabilitation for traumatic brain injury: A randomized trial. Defense and Veterans Head Injury Program (DVHIP) study group. Journal of the American Medical Association, 283(23), 3075–3081. 10.1001/jama.283.23.3075 [DOI] [PubMed] [Google Scholar]
- Sampedro, M. (2015). Protocol: Workshop for primary prevention of falls. Changing to Never Fall. CTNF. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/826/CN-01554826/frame.html
- Sampson, E. , Candy, B. , & Jones, L. (2009). Enteral tube feeding for older people with advanced dementia. Cochrane Database of Systematic Reviews, 2, 10.1002/14651858.CD007209.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanford, J. A. , Arch, M. , & Megrew, M. B. (1995). An evaluation of grab bars to meet the needs of elderly people. Assistive Technology, 7(1), 36–47. [DOI] [PubMed] [Google Scholar]
- Sayers, S. P. , Bean, J. , Cuoco, A. , LeBrasseur, N. K. , Jette, A. , & Fielding, R. A. (2003). Changes in function and disability after resistance training: Does velocity matter? A pilot study. American Journal of Physical Medicine & Rehabilitation, 82(8), 605–613. [DOI] [PubMed] [Google Scholar]
- Schoenmakers, B. , Buntinx, F. , & DeLepeleire, J. (2010). Supporting the dementia family caregiver: The effect of home care intervention on general well‐being: Systematic review. Aging and Mental Health, 14(1), 44–56. [DOI] [PubMed] [Google Scholar]
- Schoonhoven, L. , Gaal, B. G. , Teerenstra, S. , Adang, E. , Vleuten, C. , & Achterberg, T. (2015). Cost‐consequence analysis of “washing without water” for nursing home residents: A cluster randomized trial. International Journal of Nursing Studies, 52(1), 112–120. 10.1016/j.ijnurstu.2014.08.001 [DOI] [PubMed] [Google Scholar]
- Schwartz, P. J. , Blumenfield, S. , & Simon, E. P. (1990). The Interim Homecare Program: An innovative discharge planning alternative. Health and Social Work, 15, 152–160. [DOI] [PubMed] [Google Scholar]
- Seitz, D. , Gill, S. , Austin, P. , Bell, C. , Gruneir, A. , Anderson, G. , & Rochon, P. (2014). Access to rehabilitation and outcomes following hip fracture for older adults with dementia. Alzheimer's and Dementia, 4, P736. [Google Scholar]
- Sharoni, S. K. A. , Minhat, H. S. , Zulkefli, N. A. M. , & Baharom, A. (2016). Health education programmes to improve foot self‐care practices and foot problems among older people with diabetes: A systematic review. International Journal of Older People Nursing, 11(3), 214–239. 10.1111/opn.12112 [DOI] [PubMed] [Google Scholar]
- Sharoni, S. K. A. , Rahman, H. A. , Minhat, H. S. , Shariff‐Ghazali, S. , & Ong, M. H. A. (2018). The effects of self‐efficacy enhancing program on foot self‐care behaviour of older adults with diabetes: A randomised controlled trial in elderly care facility, Peninsular Malaysia. PLOS One, 13(3), e0192417. 10.1371/journal.pone.0192417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpe, R. , Smith, J. R. , Orr, N. , Phoenix, C. , Bethel, A. , Goodwin, V. , Lang, I. , & Garside, R. (2016). Physical activity interventions in older adults: A systematic review of reviewS. International journal of behavioral medicine, 23, S248–S249. [Google Scholar]
- Shaw, K. L. , & Page, C. (2008). A pilot community‐based walking‐for‐exercise program for senior women. Topics in Geriatric Rehabilitation, 24(4), 315–324. 10.1097/TGR.0b013e31818cd005 [DOI] [Google Scholar]
- Sheppad, S. (1998). A randomised controlled trial comparing hospital at home with in-patient hospital care. http://resolver.ebscohost.com/openurl?ctx_ver=Z39.88-2004%26ctx_enc=info:ofi/enc:UTF-8%26rfr_id=info:sid/ProQuest+Dissertations+%26+Theses+Global%26rft_val_fmt=info:ofi/fmt:kev:mtx:dissertation%26rft.g
- Shepperd, S. , & Iliffe, S. (1998). The effectiveness of hospital at home compared with in‐patient hospital care: A systematic review. Journal of Public Health Medicine, 20(3), 344–350. [DOI] [PubMed] [Google Scholar]
- Sherrington, C. , Lord, S. R. , & Herbert, R. D. (2004). A randomized controlled trial of weight-bearing versus non-weight-bearing exercise for improving physical ability after usual care for hip fracture. Archives of Physical Medicine and Rehabilitation, 85(5), 710–716. 10.1016/S0003-9993(03)00620-8 [DOI] [PubMed] [Google Scholar]
- Sherwood, D. A. (1980). The effects of homemaker and day care services on the association of elderly recipients with their family networks. http://resolver.ebscohost.com/openurl?sid=OVID:embase%26id=pmid:%26id=doi:%26issn=%26isbn=%26volume=%26issue=%26spage=%26pages=%26date=1980%26title=%3D%3D%3D%26atitle=The+effects+of+homemake
- Sherwood, S. , John, M. , & Ruchlin, S. H. (1986). Alternative paths to long‐term care: Nursing home, geriatric day hospital, senior center, and domiciliary care options. American Journal of Public Health, 76, 38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shigekazu, U. , Akiko, T. , & Kota, O. (2015). A randomized controlled trial of a long‐term functioning improvement tool home visit program for frail older Japanese people. International Journal of Geriatric Psychiatry, 30(8), 887–888. [DOI] [PubMed] [Google Scholar]
- Shigekazu, U. , Motoyuki, Y. , Tamiko, I. , Katsunori, I. , & Reiko, K. (2012). Letter to the editor: The effect of a functioning improvement tool home visit program on instrumental activities of daily living and depressive status in older people. International Journal of Geriatric Psychiatry, 27(11), 1206–1208. 10.1002/gps.2835 [DOI] [PubMed] [Google Scholar]
- Shimada, H. , Ishii, K. , Makizako, H. , Ishiwata, K. , Oda, K. , & Suzukawa, M. (2017). Effects of exercise on brain activity during walking in older adults: A randomized controlled trial. Journal of NeuroEngineering and Rehabilitation, 14, 50. 10.1186/s12984-017-0263-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shishehgar, M. , Kerr, D. , & Blake, J. (2018). A systematic review of research into how robotic technology can help older people. Smart Health, 25, 892–918. 10.1016/j.smhl.2018.03.002 [DOI] [Google Scholar]
- Sidel, V. W. , Beizer, J. L. , Lisi‐Fazio, D. , Kleinmann, K. , Wenston, J. , Thomas, C. , & Kelman, H. R. (1990). Controlled study of the impact of educational home visits by pharmacists to high‐risk older patients. Journal of Community Health, 15(3), 163–174. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/757/CN-00068757/frame.html [DOI] [PubMed] [Google Scholar]
- Signe, A. , & Elmstahl, S. (2008). Psychosocial intervention for family caregivers of people with dementia reduces caregiver's burden: Development and effect after 6 and 12 months. Scandinavian Journal of Caring Sciences, 22(1), 98–109. 10.1111/j.1471-6712.2007.00498.x [DOI] [PubMed] [Google Scholar]
- Simmons, S. F. , Schnelle, J. F. , MacRae, P. G. , & Ouslander, J. G. (1995). Wheelchairs as mobility restraints: Predictors of wheelchair activity in nonambulatory nursing home residents. Journal of the American Geriatrics Society, 43(4), 384–388. [DOI] [PubMed] [Google Scholar]
- Simmons, S. , Rahman, A. , & Dietz, P. (1996). Improving wheelchair mobility. Nursing Homes Long Term Care Management, 45(5), 32. [Google Scholar]
- Singh, M. A. F. (2018). PROTOCOL: HOMeCare: Caring for the dementia caregiver and their loved one via the HOMeCare exercise and mindfulness for health program. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/984/CN-01456984/frame.html
- Singh, M. F. (2017). PROTOCOL: BRAIN training trial: Balance, resistance, or interval training trial: A randomised controlled trial of three exercise modalities in mild cognitive impairment. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/942/CN-01456942/frame.html [DOI] [PMC free article] [PubMed]
- Sini, E. , Anthony, W. , Seija, A. , & Pirkko, R. (2010). A collaborative approach to home care delivery for older clients: Perspectives of home care providers. Journal of Interprofessional Care, 24(2), 198–200. 10.3109/13561820903078272 [DOI] [PubMed] [Google Scholar]
- Siragusa, S. , Arcara, C. , Malato, A. , Anastasio, R. , Valerio, M. R. , Fulfaro, F. , Coco, L. L. , Grimaudo, S. , Bajardi, G. , Abbadessa, V. , & Gebbia, N. (2005). Home therapy for deep vein thrombosis and pulmonary embolism in cancer patients. Annals of Oncology, 16(Suppl 4), iv136–iv139. [DOI] [PubMed] [Google Scholar]
- Sjosten, N. M. , Vahlberg, T. J. , & Kivela, S. L. (2008). The effects of multifactorial fall prevention on depressive symptoms among the aged at increased risk of falling. International Journal of Geriatric Psychiatry, 23(5), 504–510. 10.1002/gps.1927 [DOI] [PubMed] [Google Scholar]
- Sladek, R. M. , Jones, T. , Phillips, P. A. , Luszcz, M. , Rowett, D. , Eckermann, S. , Woodman, R. J. , & Frith, P. (2011). Health, economic, psychological and social impact of educating carers of patients with advanced pulmonary disease (protocol). Contemporary Clinical Trials, 32(5), 717–723. 10.1016/j.cct.2011.05.004 [DOI] [PubMed] [Google Scholar]
- Smith, N. , Ivaldi, A. , Kellard, K. , & Beckhelling, J. (2006). Evidence base review on mobility: Choices and barriers for different social groups. Department for Transport. Sep 2006 162 2006. [Google Scholar]
- Sorensen, S. , Pinquart, M. , & Duberstein, P. (2002). How effective are interventions with caregivers? An updated meta‐analysis. Gerontologist, 42(3), 356–372. [DOI] [PubMed] [Google Scholar]
- Sosnoff, J. J. , Finlayson, M. , McAuley, E. , Morrison, S. , & Motl, R. W. (2014). Home‐based exercise program and fall‐risk reduction in older adults with multiple sclerosis: Phase 1 randomized controlled trial. Clinical Rehabilitation, 28(3), 254–263. 10.1177/0269215513501092 [DOI] [PubMed] [Google Scholar]
- Sprange, K. , Mountain, G. A. , Brazier, J. , Cook, S. P. , Craig, C. , Hind, D. , Walters, S. J. , Windle, G. , Woods, R. , Keetharuth, A. D. , Chater, T. , & Horner, K. (2013). Lifestyle Matters for maintenance of health and wellbeing in people aged 65 years and over: Study protocol for a randomised controlled trial. Trials, 14, 302. 10.1186/1745-6215-14-302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark, S. , Somerville, E. , Keglovits, M. , Conte, J. , Li, M. , Hu, Y. L. , & Yan, Y. (2017). Protocol for the home hazards removal program (HARP) study: A pragmatic, randomized clinical trial and implementation study. BMC Geriatrics, 17(1), 90. 10.1186/s12877-017-0478-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stathi, A. , Withall, J. , Greaves, C. J. , Thompson, J. L. , Taylor, G. , Medina‐Lara, A. , Green, C. , Bilzon, J. , Gray, S. , Johansen‐Berg, H. , Sexton, C. E. , Western, M. J. , de Koning, J. L. , Bollen, J. C. , Moorlock, S. J. , Demnitz, N. , Seager, P. , Guralnik, J. M. , Rejeski, W. J. , & Fox, K. R. (2018). A community‐based physical activity intervention to prevent mobility‐related disability for retired older people (REtirement in ACTion (REACT)): Study protocol for a randomised controlled trial. Trials, 19, 228. 10.1186/s13063-018-2603-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein, S. R. , Linn, M. W. , & Weiner, A. S. (1981). Effectiveness of Service Workers’ Action Team (SWAT) for the elderly. Journal of the American Geriatrics Society, 29(9), 411–417. [DOI] [PubMed] [Google Scholar]
- Stelmack, J. A. , Tang, X. C. , Reda, D. J. , Rinne, S. , Mancil, R. M. , & Massof, R. W. (2007). Veterans affairs low vision intervention trial. IOVS, 2005, 46, ARVO E‐abstract 1920. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/027/CN-00624027/frame.html [DOI] [PubMed]
- Stenvall, M. , Olofsson, B. , Nyberg, L. , Lundstrom, M. , & Gustafson, Y. (2007). Improved performance in activities of daily living and mobility after a multidisciplinary postoperative rehabilitation in older people with femoral neck fracture: A randomized controlled trial with 1‐year follow‐up. Journal of Rehabilitation Medicine, 39(3), 232–238. [DOI] [PubMed] [Google Scholar]
- Steultjens, E. , & Clemson, L. (2006). A preventative home safety programme for community‐dwelling older people with low vision reduced falls and was more cost‐effective than an exercise programme: Commentary. Australian Occupational Therapy Journal, 53(3), 243–244. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/316/CN-00615316/frame.html [Google Scholar]
- Stevens‐Lapsley, J. E. (2016). Improving rehabilitation outcomes after total hip arthroplasty. https://Clinicaltrials.Gov/Show/Nct02920866. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/244/CN-01521244/frame.html
- Stevenson, J. , & Gray, P. (1981). Rehabilitation for long‐term residents. Geriatric Nursing, 2(2), 127–131. [DOI] [PubMed] [Google Scholar]
- Stewart, S. (2006). Review: Multidisciplinary interventions reduce hospital admission and all cause mortality in heart failure. Evidence Based Nursing, 9(1), 23. [DOI] [PubMed] [Google Scholar]
- Stewart, S. , Harvey, I. , Poland, F. , Lloyd‐Smith, W. , Mugford, M. , & Flood, C. (2005). Are occupational therapists more effective than social workers when assessing frail older people? Results of CAMELOT, a randomised controlled trial. Age and Ageing, 34(1), 41–46. 10.1093/ageing/afh230 [DOI] [PubMed] [Google Scholar]
- Stewart, S. , Wiley, J. F. , Ball, J. , Chan, Y. K. , Ahamed, Y. , Thompson, D. R. , & Carrington, M. J. (2016). Impact of nurse‐led, multidisciplinary home‐based intervention on event‐free survival across the spectrum of chronic heart disease: Composite analysis of health outcomes in 1226 patients from 3 randomized trials. Circulation, 133(19), 1867–1877. 10.1161/CIRCULATIONAHA.116.020730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolle, C. , Wolter, A. , Roth, G. , & Rothgang, H. (2012). Effects of the resident assessment instrument in home care settings: Results of a cluster randomized controlled trial. Zeitschrift fur Gerontologie und Geriatrie, 45(4), 315–322. 10.1007/s00391-011-0221-2 [DOI] [PubMed] [Google Scholar]
- Stow, R. , Ives, N. , Smith, C. , Rick, C. , & Rushton, A. (2015). A cluster randomised feasibility trial evaluating nutritional interventions in the treatment of malnutrition in care home adult residents. Trials, 16(1), 433. 10.1186/s13063-015-0952-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straw, L. B. , & Harley, R. K. (1991). Assessment and training in orientation and mobility for older persons: Program development and testing. Journal of Visual Impairment and Blindness, 87(7), 291–296. [Google Scholar]
- Stuck, A. E. , Kharicha, K. , Dapp, U. , Anders, J. , Renteln‐Kruse, W. , Meier‐Baumgartner, H. P. , Iliffe, S. , Harari, D. , Bachmann, M. D. , Egger, M. , Gillmann, G. , Beck, J. C. , & Swift, C. G. (2007). The PRO‐AGE study: An international randomised controlled study of health risk appraisal for older persons based in general practice. BMC Medical Research Methodology, 7, 2. 10.1186/1471-2288-7-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuck, A. E. , Zwahlen, H. G. , Neuenschwander, B. E. , Schweizer, R. A. M. , Bauen, G. , & Beck, J. C. (1995). Methodologic challenges of randomized controlled studies on in‐home comprehensive geriatric assessment: The EIGER project. Evaluation of In‐Home Geriatric Health Visits in Elderly Residents. Aging‐Clinical & Experimental Research, 7(3), 218–223. [DOI] [PubMed] [Google Scholar]
- Sturkenboom, I. H. , Nijhuis‐van der Sanden, M. W. , & Graff, M. J. (2016). A process evaluation of a home‐based occupational therapy intervention for Parkinson's patients and their caregivers performed alongside: A randomized controlled trial. Clinical Rehabilitation, 30(12), 1186–1199. [DOI] [PubMed] [Google Scholar]
- Subhadra, E. , Andrew, F. , Neophytou, C. , & de Souza, L. (2007). Older adults’ use of, and satisfaction with, electric powered indoor/outdoor wheelchairs. Age and Ageing, 36(4), 431–435. 10.1093/ageing/afm034 [DOI] [PubMed] [Google Scholar]
- Sungkarat, S. , Boripuntakul, S. , Chattipakorn, N. , Watcharasaksilp, K. , & Lord, S. R. (2017). Effects of Tai Chi on cognition and fall risk in older adults with mild cognitive impairment: A randomized controlled trial. Journal of the American Geriatrics Society, 65(4), 721–727. 10.1111/jgs.14594 [DOI] [PubMed] [Google Scholar]
- Suwanwela, N. C. , Phanthumchinda, K. , Limtongkul, S. , Suvanprakorn, P. , Volunteers, T. R. C. , & Bureau (2002). Comparison of short (3‐day) hospitalization followed by home care treatment and conventional (10‐day) hospitalization for acute ischemic stroke. Cerebrovascular Diseases, 13(4), 267–271. [DOI] [PubMed] [Google Scholar]
- Swank, A. M. , Kachelman, J. B. , Bibeau, W. , Quesada, P. M. , Nyland, J. , Malkani, A. , & Topp, R. V. (2011). Prehabilitation before total knee arthroplasty increases strength and function in older adults with severe osteoarthritis. Journal of Strength & Conditioning Research, 25(2), 318–325. 10.1519/JSC.0b013e318202e431 [DOI] [PubMed] [Google Scholar]
- Tanner, J. A. , Black, B. S. , Johnston, D. , Hess, E. , Rabins, P. V. , Lyketsos, C. , & Samus, Q. (2013). Effectiveness of a multicomponent care coordination intervention on dementia caregivers in the community—A randomized control trial. American Journal of Geriatric Psychiatry, 1, S97–S98. [Google Scholar]
- Tappen, R. M. , & Debra, H. (2014). The effect of in‐home cognitive training on functional performance of individuals with mild cognitive impairment and early‐stage Alzheimer's disease. Research in Gerontological Nursing, 7(1), 14–24. [DOI] [PubMed] [Google Scholar]
- Tasiemski, T. , Kennedy, P. , Gardner, B. P. , & Taylor, N. (2005). The association of sports and physical recreation with life satisfaction in a community sample of people with spinal cord injuries. Neurorehabilitation, 20(4), 253–265. [PubMed] [Google Scholar]
- Taule, T. , Strand, L. I. , Skouen, J. S. , & Raheim, M. (2015). Striving for a life worth living: Stroke survivors’ experiences of home rehabilitation. Scandinavian Journal of Caring Sciences, 29(4), 651–661. 10.1111/scs.12193 [DOI] [PubMed] [Google Scholar]
- Tennsledt, S. , Howland, J. , Lachman, M. , Peterson, E. , Kasten, L. , & Jette, A. (1998). A randomized, controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. Journals of Gerontology Series B‐Psychological Sciences and Social Sciences, 53(6), P384–P392. 10.1093/geronb/53B.6.P384 [DOI] [PubMed] [Google Scholar]
- The impact of home‐visit, pharmacists‐led medication management programme among single‐living, hypertensive elderly with suboptimal compliance to multiple medications: A randomized controlled trial . (2013). ChiCTR. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/952/CN-01134952/frame.html
- Thomas, R. , Worrall, G. , Elgar, F. , & Knight, J. (2007). Can they keep going on their own? A four‐year randomized trial of functional assessments of community residents. Canadian Journal on Aging, 26(4), 379–390. [DOI] [PubMed] [Google Scholar]
- Thulesius, H. , Petersson, C. , Petersson, K. , & Hakansson, A. (2002). Learner‐centred education in end‐of‐life care improved well being in home care staff: A prospective controlled study. Palliative Medicine, 16(4), 347–354. [DOI] [PubMed] [Google Scholar]
- Tibaek, S. , Andersen, C. W. , Pedersen, S. F. , & Rudolf, K. S. (2014). Does progressive resistance strength training as additional training have any measured effect on functional outcomes in older hospitalized patients? A single‐blinded randomized controlled trial. Clinical Rehabilitation, 28(4), 319–328. 10.1177/0269215513501524 [DOI] [PubMed] [Google Scholar]
- Tiedemann, A. , O'Rourke, S. , Sesto, R. , & Sherrington, C. (2013). A 12‐week iyengar yoga program improved balance and mobility in older community‐dwelling people: A pilot randomized controlled trial. Journals of Gerontology Series A‐Biological Sciences and Medical Sciences, 68(9), 1068–1075. 10.1093/gerona/glt087 [DOI] [PubMed] [Google Scholar]
- Tiedemann, A. , Paul, S. , Ramsay, E. , O'Rourke, S. D. , Chamberlain, K. , Kirkham, C. , Merom, D. , Fairhall, N. , Oliveira, J. S. , Hassett, L. , & Sherrington, C. (2015). What is the effect of a combined physical activity and fall prevention intervention enhanced with health coaching and pedometers on older adults’ physical activity levels and mobility‐related goals?: Study protocol for a randomised controlled trial. BMC Public Health, 15, 477. 10.1186/s12889-015-1380-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiedemann, A. , Rissel, C. , Howard, K. , Tong, A. , Merom, D. , Smith, S. , Wickham, J. , Bauman, A. , Lindley, R. , Lord, S. , Vogler, C. , Lester, D. , & Sherrington, C. (2016). Health coaching to enhance physical activity and prevent falls in community‐dwelling people aged 60 years and over: Study protocol for the CHAnGE cluster randomised controlled trial. Journal of Aging and Physical Activity, 24, S101. [Google Scholar]
- Timonen, L. , Rantanen, T. , Ryynanen, O. P. , Taimela, S. , Timonen, T. E. , & Sulkava, R. (2002). A randomized controlled trial of rehabilitation after hospitalization in frail older women: Effects on strength, balance and mobility. Scandinavian Journal of Medicine & Science in Sports, 12(3), 186–192. 10.1034/j.1600-0838.2002.120310.x [DOI] [PubMed] [Google Scholar]
- Timonen, L. , Rantanen, T. , Timonen, T. E. , & Sulkava, R. (2002). Effects of a group‐based exercise program on the mood state of frail older women after discharge from hospital. International Journal of Geriatric Psychiatry, 17(12), 1106–1111. [DOI] [PubMed] [Google Scholar]
- Tinetti, M. E. , Baker, D. I. , Garrett, P. A. , Gottschalk, M. , Koch, M. L. , & Horwitz, R. I. (1993). Yale FICSIT: Risk factor abatement strategy for fall prevention. Journal of the American Geriatrics Society, 41(3), 315–320. [DOI] [PubMed] [Google Scholar]
- Toevs, S. E. (2000). Effect of an in‐home oral assessment and education on the oral health status of older adults receiving home health care services. UMI Dissertation Services, ProQuest Information and Learning, Ann Arbor, MI.
- Toot, S. , Devine, M. , & Orrell, M. (2011). The effectiveness of crisis resolution/home treatment teams for older people with mental health problems: A systematic review and scoping exercise. International Journal of Geriatric Psychiatry, 26(12), 1221–1230. 10.1002/gps.2686 [DOI] [PubMed] [Google Scholar]
- Torres, S. J. , Robinson, S. , Orellana, L. , O'Connell, S. L. , Grimes, C. A. , Mundell, N. L. , Dunstan, D. W. , Nowson, C. A. , & Daly, R. M. (2017). Effects of progressive resistance training combined with a protein‐enriched lean red meat diet on health‐related quality of life in elderly women: Secondary analysis of a 4‐month cluster randomised controlled trial. British Journal of Nutrition, 117(11), 1550–1559. 10.1017/s0007114517001507 [DOI] [PubMed] [Google Scholar]
- Torres‐Arreola, L. , del, P. , Doubova, V. S. , Hernandez, S. , Torres‐Valdez, L. , Constantino‐Casas, N. , Garcia‐Contreras, F. , & Torres‐Castro, S. (2009). Effectiveness of two rehabilitation strategies provided by nurses for stroke patients in Mexico. Journal of Clinical Nursing, 18(21), 2993–3002. [DOI] [PubMed] [Google Scholar]
- Toseland, R. W. , Rossiter, C. M. , Peak, T. , & Smith, G. C. (1990). Comparative effectiveness of individual and group interventions to support family caregivers. Social Work, 35(3), 209–217. [PubMed] [Google Scholar]
- Towfighi, A. , Cheng, E. M. , Ayala‐Rivera, M. , McCreath, H. , Sanossian, N. , Dutta, T. , Mehta, B. , Bryg, R. , Rao, N. , Song, S. , Razmara, A. , Ramirez, M. , Sivers‐Teixeira, T. , Tran, J. , Mojarro‐Huang, E. , Montoya, A. , Corrales, M. , Martinez, B. , Willis, P. , … Vickrey, B. G. (2017). Randomized controlled trial of a coordinated care intervention to improve risk factor control after stroke or transient ischemic attack in the safety net: Secondary stroke prevention by Uniting Community and Chronic care model teams Early to End Disparities (SUCCEED). BMC Neurology, 17(1), 24. 10.1186/s12883-017-0792-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracy, C. (2012). The effects of life review through writing on depressive symptoms and life satisfaction in older adults. Dissertation Abstracts International: Section B: The Sciences and Engineering, 73(1‐B), 237. [Google Scholar]
- Troyer, J. L. , McAuley, W. J. , & McCutcheon, M. E. (2010). Cost‐effectiveness of medical nutrition therapy and therapeutically designed meals for older adults with cardiovascular disease. Journal of the American Dietetic Association, 110(12), 1840–1851. 10.1016/j.jada.2010.09.013 [DOI] [PubMed] [Google Scholar]
- Tsai, C. L. , Pan, C. Y. , Chen, F. C. , & Tseng, Y. T. (2017). Open‐ and closed‐skill exercise interventions produce different neurocognitive effects on executive functions in the elderly: A 6‐month randomized, controlled trial. Frontiers in Aging Neuroscience, 9. 10.3389/fnagi.2017.00294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tse, M. M. , Ng, S. S. , Lee, P. H. , Lai, C. , Kwong, E. , Liu, J. Y. , Yuen, J. , Bai, X. , & Yeung, S. S. (2016). Play activities program to relieve chronic pain and enhance functional mobility and psychological well‐being for frail older adults: A pilot cluster randomized controlled trial. Journal of the American Geriatrics Society, 64(10), E86–E88. 10.1111/jgs.14374 [DOI] [PubMed] [Google Scholar]
- Tsuchihashi‐Makaya, M. , Matsuo, H. , Kakinoki, S. , Takechi, S. , Tsutsui, H. , & Homecare, I. J. (2011). Rationale and design of the Japanese heart failure outpatients disease management and cardiac evaluation (J‐HOMECARE). Journal of Cardiology, 58(2), 165–172. 10.1016/j.jjcc.2011.04.004 [DOI] [PubMed] [Google Scholar]
- Ukawa, S. , Satoh, H. , Yuasa, M. , Ikeno, T. , Kawabata, T. , Araki, A. , Yoshioka, E. , Murata, W. , Ikoma, K. , & Kishi, R. (2012). A randomized controlled trial of a Functioning Improvement Tool home‐visit program and its effect on cognitive function in older persons. International Journal of Geriatric Psychiatry, 27(6), 557–564. 10.1002/gps.2753 [DOI] [PubMed] [Google Scholar]
- Ukawa, S. , Yuasa, M. , Ikeno, T. , Yoshioka, E. , Satoh, H. , Murata, W. , Ikoma, K. , & Kishi, R. (2012). Randomised controlled pilot study in Japan comparing a home visit program using a Functioning Improvement Tool with a home visit with conversation alone. Australasian Journal on Ageing, 31(3), 187–189. 10.1111/j.1741-6612.2012.00589.x [DOI] [PubMed] [Google Scholar]
- Ullmann, G. , & Li, Y. (2017). Health benefits of seated Tai Chi. BMC Complementary and Alternative Medicine. Conference: World Congress Integrative Medicine and Health, 17(Suppl. 1), 317. 10.1186/s12906-017-1783-3 [DOI] [Google Scholar]
- Ulrich, P. P. (2005). Nutritional care: The effectiveness of actively involving older patients. Journal of Clinical Nursing, 14(2), 247–255. [DOI] [PubMed] [Google Scholar]
- Uy, C. , Kurrle, S. E. , & Cameron, I. D. (2008). Inpatient multidisciplinary rehabilitation after hip fracture for residents of nursing homes: A randomised trial. Australasian Journal on Ageing, 27(1), 43–44. 10.1111/j.1741-6612.2007.00277.x [DOI] [PubMed] [Google Scholar]
- Vaapio, S. , Salminen, M. , Vahlberg, T. , Sjosten, N. , Isoaho, R. , Aarnio, P. , & Kivela, S. L. (2007). Effects of risk‐based multifactorial fall prevention on health‐related quality of life among the community‐dwelling aged: A randomized controlled trial. Health and Quality of Life Outcomes, 5, 20. 10.1186/1477-7525-5-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahlberg, B. , Lindmark, B. , Zetterberg, L. , Hellstrom, K. , & Cederholm, T. (2017). Body composition and physical function after progressive resistance and balance training among older adults after stroke: An exploratory randomized controlled trial. Disability and Rehabilitation, 39(12), 1207–1214. 10.1080/09638288.2016.1191551 [DOI] [PubMed] [Google Scholar]
- van Achterberg, T. , van Gaal, B. G. , Geense, W. W. , Verbeke, G. , van der Vleuten, C. , & Schoonhoven, L. (2016). Completeness of assisted bathing in nursing homes related to dementia and bathing method: Results from a secondary analysis of cluster‐randomised trial data. International Journal of Older People Nursing, 11(2), 121–129. 10.1111/opn.12104 [DOI] [PubMed] [Google Scholar]
- van Ginneken, N. , Tharyan, P. , Lewin, S. , Rao, G. N. , Meera, S. M. , Pian, J. , Chandrashekar, S. , & Patel, V. (2013). Non‐specialist health worker interventions for the care of mental, neurological and substance‐abuse disorders in low‐ and middle‐income countries. Cochrane Database of Systematic Reviews, 11, CD009149. 10.1002/14651858.CD009149.pub2 [DOI] [PubMed] [Google Scholar]
- van Hout, H. P. J. , Nijpels, G. , van Marwijk, H. W. J. , Jansen, A. P. D. , van't Veer, P. J. , Tybout, W. , & Stalman, W. A. (2005). Design and pilot results of a single blind randomized controlled trial of systematic demand‐led home visits by nurses to frail elderly persons in primary care [ISRCTN05358495]. BMC Geriatrics, 5, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Mulligen‐van de Belt, E. C. , Smalbrugge, M. , & Depla, M. F. (2013). Meagre evidence so far for effectiveness of in‐home comprehensive geriatric assessment: A literature review. Tijdschrift Voor Gerontologie En Geriatrie, 44(5), 215–227. 10.1007/s12439-013-0042-4 [DOI] [PubMed] [Google Scholar]
- van Ooijen, M. W. , Roerdink, M. , Trekop, M. , Visschedijk, J. , Janssen, T. W. , & Beek, P. J. (2013). Functional gait rehabilitation in elderly people following a fall‐related hip fracture using a treadmill with visual context: Design of a randomized controlled trial. BMC Geriatrics, 13, 13. 10.1186/1471-2318-13-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Spall, H. G. C. , Lee, S. F. , Xie, F. , Ko, D. , Thabane, L. , Ibrahim, Q. , Mitoff, P. , Heffernan, M. , Maingi, M. , Tjandrawidjaja, M. , Zia, M. , Panju, M. , Perez, R. , Simek, K. , Porepa, L. , Graham, I. , Haynes, B. , Haughton, D. , & Connolly, S. (2018). Knowledge to action: Rationale and design of the Patient‐Centered Care Transitions in Heart Failure (PACT‐HF) stepped wedge cluster randomized trial. American Heart Journal, 199, 75–82. 10.1016/j.ahj.2017.12.013 [DOI] [PubMed] [Google Scholar]
- Vandepitte, S. , Noortgate, V. , Den, N. , Putman, K. , Verhaeghe, S. , Verdonck, C. , & Annemans, L. (2016). Effectiveness of respite care in supporting informal caregivers of persons with dementia: A systematic review. International Journal of Geriatric Psychiatry, 31(12), 1277–1288. 10.1002/gps.4504 [DOI] [PubMed] [Google Scholar]
- Vandepitte, S. , Van Den Noortgate, N. , Putman, K. , Verhaeghe, S. , & Annemans, L. (2016). Effectiveness and cost‐effectiveness of an in‐home respite care program in supporting informal caregivers of people with dementia: Design of a comparative study. BMC Geriatrics, 16(1), 207. 10.1186/s12877-016-0373-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanDeVelde‐Coke, S. (2004). Effectiveness and efficiency of providing home care visits in nursing clinics versus the traditional home setting. UMI Dissertation Services, ProQuest Information and Learning, Ann Arbor, MI.
- Vass, M. , Hendriksen, C. , & Avlund, K. (2004). A feasible model for promoting health and prevent functional decline in older people. A municipality randomised controlled trial. Gerontologist, 44, 360. [Google Scholar]
- Venturelli, M. , Lanza, M. , Muti, E. , & Schena, F. (2010). Positive effects of physical training in activity of daily living‐dependent older adults. Experimental Aging Research, 36(2), 190–205. 10.1080/03610731003613771 [DOI] [PubMed] [Google Scholar]
- Verloo, H. , Goulet, C. , Morin, D. , & von Gunten, A. (2015). Effect estimation of an innovative nursing intervention to improve delirium among home‐dwelling older adults: A randomized controlled pilot trial. Dementia and Geriatric Cognitive Disorders Extra, 5(1), 176–190. 10.1159/000375444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vetter, N. J. , Jones, D. A. , & Victor, C. R. (1984). Effect of health visitors working with elderly patients in general practice: A randomised controlled trial. British Medical Journal, 288(6414), 369–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor, C. R. , & Vetter, N. J. (1988). Rearranging the deckchairs on the Titanic: Failure of an augmented home help scheme after discharge to reduce the length of stay in hospital. Archives of Gerontology and Geriatrics, 7(1), 83–91. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/094/CN-00351094/frame.html [DOI] [PubMed] [Google Scholar]
- Vincent, L. , Colantonio, A. , & Santaguida, P. L. (2005). Wheelchair use, pain, and satisfaction with life in a national sample of older adults. Gerontechnology, 3(3), 159–164. [Google Scholar]
- Viswanathan, P. , Boger, J. , Hoey, J. , Elinas, P. , & Mihailidis, A. (2007). Technology in medicine: The future of wheelchairs: Intelligent collision avoidance and navigation assistance. Geriatrics and Aging, 10(4), 253–256. [Google Scholar]
- von Humboldt, S. , & Leal, I. (2014). What influences the subjective wellbeing of older adults?: A systematic review of the literature. Revista Argentina De Clinica Psicologica, 23(3), 219–230. [Google Scholar]
- Vriendt, D. P. , Peersman, W. , Florus, A. , Verbeke, M. , Velde, V. , & De, D. (2016). Improving health related quality of life and independence in community dwelling frail older adults through a client‐centred and activity‐oriented program. A pragmatic randomized controlled trial. Journal of Nutrition, Health & Aging, 20(1), 35–40. 10.1007/s12603-016-0673-6 [DOI] [PubMed] [Google Scholar]
- Vroomen, J. L. M. , Boorsma, M. , Bosmans, J. E. , Frijters, D. H. M. , Nijpels, G. , & van Hout, H. P. J. (2012). Is it time for a change? A cost‐effectiveness analysis comparing a multidisciplinary integrated care model for residential homes to usual care. PLOS One, 7(5), e37444. 10.1371/journal.pone.0037444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace, S. A. , Roe, B. , Williams, K. , & Palmer, M. (2004). Bladder training for urinary incontinence in adults. Cochrane Database of Systematic Reviews, 1, CD001308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wanderley, F. A. C. , Oliveira, N. L. , Marques, E. , Moreira, P. , Oliveira, J. , & Carvalho, J. (2015). Aerobic versus resistance training effects on health‐related quality of life, body composition, and function of older adults. Journal of Applied Gerontology, 34(3), NP143–NP165. [DOI] [PubMed] [Google Scholar]
- Wang, C. J. , Fetzer, S. J. , Yang, Y. C. , & Wang, J. J. (2013). The impacts of using community health volunteers to coach medication safety behaviors among rural elders with chronic illnesses. Geriatric Nursing, 34(2), 138–145. 10.1016/j.gerinurse.2012.12.013 [DOI] [PubMed] [Google Scholar]
- Wang, J. , & Wu, B. (2017). Domestic helpers as frontline workers in China's home‐based elder care: A systematic review. Journal of Women & Aging, 29(4), 294–305. 10.1080/08952841.2016.1187536 [DOI] [PubMed] [Google Scholar]
- Wang, R. , Gorski, S. , Holliday, P. , & Fernie, G. (2011). Evaluation of a contact sensor skirt for an anti‐collision power wheelchair for older adult nursing home residents with dementia: Safety and mobility. Assistive Technology, 23(3), 117–134. 10.1080/10400435.2010.541406 [DOI] [Google Scholar]
- Wang, W. , Jiang, Y. , He, H. G. , & Koh, K. W. (2016). A randomised controlled trial on the effectiveness of a home‐based self‐management programme for community‐dwelling patients with myocardial infarction. European Journal of Cardiovascular Nursing, 15(6), 398–408. 10.1177/1474515115586904 [DOI] [PubMed] [Google Scholar]
- Ward, P. R. , Tudor, C. A. , & Gowers, J. I. (1978). Evaluation of follow up services for elderly people prescribed hearing aids: Report of a pilot project. British Journal of Audiology, 12, 127–134. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/936/CN-00996936/frame.html [DOI] [PubMed] [Google Scholar]
- Warland, A. , & Tonning, F. (1991). Assistive devices for hard‐of‐hearing persons—Distribution system and costs. British Journal of Audiology, 25(Dec 91), 399–404. [DOI] [PubMed] [Google Scholar]
- Warner, L. M. , Wolff, J. K. , Ziegelmann, J. P. , Schwarzer, R. , & Wurm, S. (2016). Revisiting self‐regulatory techniques to promote physical activity in older adults: Null‐findings from a randomised controlled trial. Psychology & Health, 31(10), 1145–1165. 10.1080/08870446.2016.1185523 [DOI] [PubMed] [Google Scholar]
- Waterman, H. , Ballinger, C. , Brundle, C. , Chastin, S. , Gage, H. , Harper, R. , Henson, D. , Laventure, B. , McEvoy, L. , Pilling, M. , Olleveant, N. , Skelton, D. A. , Stanford, P. , & Todd, C. (2016). A feasibility study to prevent falls in older people who are sight impaired: The VIP2UK randomised controlled trial. Trials, 17(1), 464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss, Z. , Snir, D. , Klein, B. , Avraham, I. , Shani, R. , Zetler, H. , Eyal, P. , Dynia, A. , & Eldar, R. (2004). Effectiveness of home rehabilitation after stroke in Israel. International Journal of Rehabilitation Research, 27(2), 119–125. [DOI] [PubMed] [Google Scholar]
- Whitehead, P. J. , James, M. , Belshaw, S. , Dawson, T. , Day, M. R. , & Walker, M. F. (2016). Bathing adaptations in the homes of older adults (BATH‐OUT): Protocol for a feasibility randomised controlled trial (RCT). BMJ Open, 6(10), e013448. 10.1136/bmjopen-2016-013448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead, P. J. , Walker, M. F. , Parry, R. H. , Latif, Z. , McGeorge, I. D. , & Drummond, A. E. (2016). Occupational Therapy in HomEcare Re‐ablement Services (OTHERS): Results of a feasibility randomised controlled trial. BMJ Open, 6(8), e011868. 10.1136/bmjopen-2016-011868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittemore, R. , Rosenberg, A. , Gilmore, L. , Withey, M. , & Breault, A. (2014). Implementation of a diabetes prevention program in public housing communities. Public Health Nursing (Boston, Mass.), 31(4), 317–326. 10.1111/phn.12093 [DOI] [PubMed] [Google Scholar]
- Whitten, P. , & Mickus, M. (2007). Home telecare for COPD/CHF patients: Outcomes and perceptions: Randomized controlled trial. Journal of Telemedicine & Telecare, 13(2), 69–73. [DOI] [PubMed] [Google Scholar]
- Wilhelmson, K. , Duner, A. , Eklund, K. , Gosman‐Hedstrom, G. , Blomberg, S. , Hasson, H. , Gustafsson, H. , Landahl, S. , & Dahlin‐Ivanoff, S. (2011). Design of a randomized controlled study of a multi‐professional and multidimensional intervention targeting frail elderly people. BMC Geriatrics, 11, 24. 10.1186/1471-2318-11-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- William, A. , Richard, D. , Andrew, K. , & Shirley, M . (1991). Geriatric evaluation and management: Current status and future research directions. Journal of the American Geriatrics Society, 39(9, Suppl.), 2S–7S. [DOI] [PubMed] [Google Scholar]
- Williams, K. (2013). Evidence‐based strategies for communicating with older adults in long‐term care. Journal of Clinical Outcomes Management, 20(11), 507–512. http://www.turner-white.com/pdf/jcom_nov13_longterm.pdf [Google Scholar]
- Williams, S. , Meyer, C. , Batchelor, F. , & Hill, K. (2015). Exercise for mild balance dysfunction: Research into practice. Journal of aging and physical activity, 23(4), 588–596. [DOI] [PubMed] [Google Scholar]
- Wilson, A. , Parker, H. , Wynn, A. , Jagger, C. , Spiers, N. , Jones, J. , & Parker, G. (1999). Randomised controlled trial of effectiveness of Leicester hospital at home scheme compared with hospital care. BMJ, 319(7224), 1542–1546. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/891/CN-00264891/frame.html [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson, D. , & Truman, C. (2005). Comparing the health services utilization of long‐term‐care residents, home‐care recipients, and the well elderly. The Canadian Journal of Nursing Research, 37(4), 138–154. [PubMed] [Google Scholar]
- Winter, L. , Moriarty, H. , Robinson, K. , Piersol, C. , Vause‐Earland, T. , Newhart, B. , Iacovone, D. B. , Hodgson, N. , & Gitlin, L. (2016). Efficacy and acceptability of a home‐based, family‐inclusive intervention for veterans with TBI: A randomized controlled trial. Brain Injury, 30(4), 373–387. 10.3109/02699052.2016.1144080 [DOI] [PubMed] [Google Scholar]
- Wittwer, J. (2016). Protocol: Move to the music—The effect of music cues on walking in people with 2 types of progressive neurological disorder. http://www.Anzctr.Org.Au/Actrn12616000851460.Aspx. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/099/CN-01308099/frame.html
- Wolinksy, F. D. (2011). The Iowa Healthy and Active Minds Study (IHAMS): A randomized controlled trial to improve cognitive functioning in older adults. Gerontologist, 51, 580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong, E. Y. , Lee, A. H. , James, A. P. , & Jancey, J. (2018). Physical activity and nutrition intervention for Singaporean women aged 50 years and above: study protocol for a randomised controlled trial. Trials, 19. 10.1186/s13063-018-2562-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong, F. K. , Chow, S. K. , Chan, T. M. , & Tam, S. K. (2014). Comparison of effects between home visits with telephone calls and telephone calls only for transitional discharge support: A randomised controlled trial. Age & Ageing, 43(1), 91–97. 10.1093/ageing/aft123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wongcharoen, S. , Sungkarat, S. , Munkhetvit, P. , Lugade, V. , & Silsupadol, P. (2017). Home-based interventions improve trained, but not novel, dual-task balance performance in older adults: A randomized controlled trial. Gait and Posture, 52, 147–152. 10.1016/j.gaitpost.2016.11.036 [DOI] [PubMed] [Google Scholar]
- Woolrych, R. (2016). Gerontechnology: Creating enabling environments to meet the challenges and opportunities of an aging society. Medicina, 49(Suppl), 5–6. http://revista.fmrp.usp.br/2016/suplementos/2016-suplemento2.pdfhttp://ovidsp.ovid.com/ovidweb.cgi?T=JS%26CSC=Y%26NEWS=N%26PAGE=fulltext%26D=emexb%26AN=619950826 [Google Scholar]
- Wu, C. Y. , Chen, C. L. , Tsai, W. C. , Lin, K. C. , & Chou, S. H. (2007). A randomized controlled trial of modified constraint‐induced movement therapy for elderly stroke survivors: Changes in motor impairment, daily functioning, and quality of life. Archives of Physical Medicine and Rehabilitation, 88(3), 273–278. 10.1016/j.apmr.2006.11.021 [DOI] [PubMed] [Google Scholar]
- Wu, Y. (2017). Diet, ExerCIse and carDiovascular hEalth (DECIDE)—Salt reduction strategies for the elderly in nursing homes in China. https://Clinicaltrials.Gov/Show/Nct03290716. http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/296/CN-01564296/frame.html
- Wu, Y. T. , Chien, C. L. , Chou, N. K. , Wang, S. S. , Lai, J. S. , & Wu, Y. W. (2008). Efficacy of a home-based exercise program for orthotopic heart transplant recipients. Cardiology, 111(2), 87–93. 10.1159/000119695 [DOI] [PubMed] [Google Scholar]
- Wyatt, G. K. , Donze, L. F. , & Beckrow, K. C. (2004). Efficacy of an in-home nursing intervention following short-stay breast cancer surgery. Research in Nursing & Health, 27(5), 322–331. http://ovidsp.ovid.com/ovidweb.cgi?T=JS%26CSC=Y%26NEWS=N%26PAGE=fulltext%26D=med5%26AN=15362143 [DOI] [PubMed] [Google Scholar]
- Wyers, C. E. , Breedveld‐Peters, J. J. , Reijven, P. L. , Helden, S. , Guldemond, N. A. , Severens, J. L. , Verburg, A. D. , Meesters, B. , Rhijn, L. W. , & Dagnelie, P. C. (2010). Efficacy and cost‐effectiveness of nutritional intervention in elderly after hip fracture: Design of a randomized controlled trial. BMC Public Health, 10, 212. 10.1186/1471-2458-10-212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xueyu, L. , Hao, Y. , Shunlin, X. , Rongbin, L. , & Yuan, G. (2017). Effects of low‐intensity exercise in older adults with chronic heart failure during the transitional period from hospital to home in China: A randomized controlled trial. Research in Gerontological Nursing, 10(3), 121–128. 10.3928/19404921-20170411-02 [DOI] [PubMed] [Google Scholar]
- Yoon, J. , Chang, E. , Rubenstein, L. V. , Park, A. , Zulman, D. M. , Stockdale, S. , Ong, M. K. , Atkins, D. , Schectman, G. , & Sm, A. (2018). Impact of primary care intensive management on high-risk veterans’ costs and utilization: A randomized quality improvement trial. Annals of Internal Medicine, 168(12), 846–854. 10.7326/M17-3039 [DOI] [PubMed] [Google Scholar]
- Yu, D. S. F. (2016). Effects of a health and social collaborative case management model on health outcomes of family caregivers of frail older adults: Preliminary data from a pilot randomized controlled trial. Journal of the American Geriatrics Society, 64(10), 2144–2148. 10.1111/jgs.14259 [DOI] [PubMed] [Google Scholar]
- Yuet, W. F. K. , Ching, S. , June, C. , Pui, L. A. K. , Fu, T. S. K. , & Sarah, M. (2015). Economic evaluation of the differential benefits of home visits with telephone calls and telephone calls only in transitional discharge support. Age & Ageing, 44(1), 143–147. ageing/afu166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuk, L. K. (2004). Improving the quality of life for nursing home residents with dementia: A life story approach. http://resolver.ebscohost.com/openurl?ctx_ver=Z39.88-2004%26ctx_enc=info:ofi/enc:UTF-8%26rfr_id=info:sid/ProQuest+Dissertations+%26+Theses+Global%26rft_val_fmt=info:ofi/fmt:kev:mtx:dissertation%26rft.g
- Yusif, S. , Soar, J. , & Hafeez‐Baig, A. (2016). Older people, assistive technologies, and the barriers to adoption: A systematic review. International Journal of Medical Informatics, 94, 112–116. 10.1016/j.ijmedinf.2016.07.004 [DOI] [PubMed] [Google Scholar]
- Yu‐Yahiro, J. A. , Resnick, B. , Orwig, D. , Hicks, G. , & Magaziner, J. (2009). Design and implementation of a home‐based exercise program post‐hip fracture: The Baltimore hip studies experience. PM & R, 1(4), 308–318. 10.1016/j.pmrj.2009.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarit, S. , Bangerter, L. , Liu, Y. , & Rovine, M. (2017). Exploring the benefits of respite services to family caregivers: Methodological issues and current findings. Aging and Mental Health, 21(3), 224–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeeuwe, P. E. M. , Verhagen, A. P. , Bierma‐Zeinstra, S. M. A. , Rossum, E. , Faber, M. J. , & Koes, B. W. (2006). The effect of Tai Chi Chuan in reducing falls among elderly people: Design of a randomized clinical trial in the Netherlands. BMC Geriatrics, 6, 6. 10.1186/1471-2318-6-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, L. , Weng, C. S. , Liu, M. , Wang, Q. H. , Liu, L. M. , & He, Y. (2014). Effect of whole‐ body vibration exercise on mobility, balance ability and general health status in frail elderly patients: A pilot randomized controlled trial. Clinical Rehabilitation, 28(1), 59–68. 10.1177/0269215513492162 [DOI] [PubMed] [Google Scholar]
- Zhao, Y. A. , Chung, P. K. , & Tong, T. K. (2017). Effectiveness of a balance‐focused exercise program for enhancing functional fitness of older adults at risk of falling: A randomised controlled trial. Geriatric Nursing, 38(6), 491–497. 10.1016/j.gerinurse.2017.02.011 [DOI] [PubMed] [Google Scholar]
- Zhe, W. , & McCuskey, S. M. (2008). Site‐level environmental support of active behavior and fall prevention for seniors: Systematic review. Seniors Housing and Care Journal, 16(1), 97–121. [Google Scholar]
- Zheng, G. H. , Xia, R. , Zhou, W. J. , Tao, J. , & Chen, L. D. (2016). Aerobic exercise ameliorates cognitive function in older adults with mild cognitive impairment: A systematic review and meta‐analysis of randomised controlled trials. British Journal of Sports Medicine, 50(23), 1443. 10.1136/bjsports-2015-095699 [DOI] [PubMed] [Google Scholar]
- Zimmer, J. G. , Eggert, G. M. , & Chiverton, P. (1990). Individual versus team case management in optimizing community care for chronically ill patients with dementia. Journal of Aging & Health, 2(3), 357–372. [DOI] [PubMed] [Google Scholar]
- Zimmer, J. G. , Groth‐Juncker, A. , & McCusker, J. (1984). Effects of a physician‐led home care team on terminal care. Journal of the American Geriatrics Society, 32(4), 288–292. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information
Supporting information
Supporting information


